Abstract
Objectives
Although childhood intoxication is avoidable, it remains a leading cause of morbidity and mortality in both developing and developed countries. The aim of this study was to assess the patterns and outcomes of acute pediatric intoxication in Aljouf, KSA.
Methods
A retrospective record-based descriptive study was conducted at the Prince Mutaib bin Abdulaziz hospital, and the Maternity and Children's hospital in Aljouf, KSA. All cases of acute intoxication in children younger than 18 years of age from January 1, 2015 to December 31, 2021 were included. Data analysis included demographic characteristics; year and month of intoxication; place, time, form, and route of toxic agent exposure; manner of intoxication; toxic agent/agents involved; intoxicated child's status upon arrival at the hospital; clinical presentation; treatment; admission history; and outcome.
Results
A total of 540 cases were reported. Most (79%) acutely intoxicated children were in 1 to <6 years of age. The highest frequency of reported acute pediatric intoxication was 23.9% in 2017. Pharmaceutical drugs were responsible for most reported cases (41%). Most children were asymptomatic (84%) at the time of admission. Among symptomatic children, GIT clinical manifestations were the most reported symptoms. Forty percent of the children were admitted to the inpatient ward. Interestingly, 29.4% were discharged against medical advice. Approximately 43% showed complete recovery. The logistic regression model of predictors of accidental intoxication indicated that only age and residence in urban vs rural areas had a statistically significant relationship.
Conclusions
Acute pediatric intoxication is a problem in Aljouf, KSA. Caregivers' awareness of the potentially hazardous toxic agents and risk factors for pediatric intoxication should be enhanced, and effective prevention strategies should be implemented to decrease the incidence of pediatric intoxication.
Keywords: Acute toxicity, Aljouf, Child health, Pediatric toxicity, Toxic agent
الملخص
أهداف البحث
على الرغم من أن تسمم الأطفال يمكن تجنبه ، إلا أنه لا يزال سببًا رئيسيًا للمراضة والوفيات في كل من البلدان النامية والمتقدمة. الهدف من هذه الدراسة هو تقييم نمط ونتائج تسمم الأطفال الحاد في الجوف ، المملكة العربية السعودية.
طرق البحث
أجريت دراسة وصفية بأثر رجعي في كل من مستشفيات الأمير متعب بن عبد العزيز ، ومستشفيات الولادة والأطفال في الجوف بالمملكة العربية السعودية. تم تضمين جميع حالات التسمم الحاد لدى الأطفال الذين تقل أعمارهم عن 18 عامًا من 1 يناير 2015 إلى 31 ديسمبر 2021 في الدراسة. تضمن تحليل البيانات الخصائص الديموغرافية ، سنة وشهر التسمم ، مكان ، وقت ، شكل وطريق التعرض للعامل السام ، طريقة التسمم ، العامل / العوامل السامة المعنية ، حالة الطفل المتسمم عند وصوله إلى المستشفى ، العرض السريري ، تلقي العلاج وتاريخ القبول والمصير.
النتائج
بلغ العدد الإجمالي للحالات المبلغ عنها 540 حالة. وكانت معظم حالات التسمم الحاد لدى الأطفال في الفئة العمرية 1 - أقل من 6 سنوات (79٪). كان أعلى معدل لتسمم الأطفال الحاد المبلغ عنه في عام 2017 (23.9٪). كانت العقاقير الدوائية مسؤولة عن معظم الحالات المبلغ عنها (41٪). كانت معظم الحالات بدون أعراض (84٪) وقت الدخول. فيما يتعلق بحالات الأعراض ، كانت المظاهر السريرية للجهاز الهضمي هي أكثر الأعراض التي تم الإبلاغ عنها. تم قبول أربعين في المائة من الحالات المدروسة بالقسم الداخلي. ومن المثير للاهتمام ، أن 29.4٪ تم تسريحهم ضد الاستشارة الطبية. أظهر حوالي 43 ٪ من الحالات المبلغ عنها الشفاء التام. أظهر نموذج الانحدار اللوجستي للتنبؤ بالطريقة العرضية للتسمم أن العمر والإقامة فقط لهما علاقة ذات دلالة إحصائية.
الاستنتاجات
يعتبر تسمم الأطفال الحاد مشكلة حقيقية في الجوف بالمملكة العربية السعودية. يجب إثارة المخاوف لتعزيز وعي مقدمي الرعاية بالعوامل السامة الخطرة وعوامل الخطر لتسمم الأطفال وتنفيذ استراتيجيات وقائية فعالة لتقليل حدوث تسمم الأطفال.
الكلمات المفتاحية: السمية الحادة, الجوف, صحة الطفل, سمية الأطفال, عامل سام
Introduction
“All things are poison, and nothing is without poison, only the dose permits something not to be poisonous,” according to Paracelsus (1493–1541), the “grandfather of toxicology.”1 Handling of cases of intoxication is a substantial burden for any institution, given that thousands of cases occur each year.2 Although childhood intoxication is avoidable, it remains a leading cause of morbidity and mortality in both developing and developed countries.3,4 Pharmaceutical and substance use have a significant influence in these cases.5 The advent of novel medications and chemicals for home and agricultural use has altered the patterns of intoxication, and new threats develop on a regular basis.6 Furthermore, the increasing use of over-the-counter medications has substantially increased the number of intoxicated patients admitted to hospitals.7 Pharmaceuticals, household items, pesticides, toxic plants, and insect and animal attacks are all common toxic agents in high-income nations. Hydrocarbons such as paraffin and kerosene, medications, and cleaning detergents are common toxic agents in low- and middle-income nations.6
The parameters influencing the severity of pediatric intoxication and its outcomes are interconnected. These parameters include the toxic agent, dosage, form of the toxic agent, route of administration, child's age, exposure to single/multiple agents, and occurrence of additional illnesses or injuries.1 In young children, intoxication can be unintentional or iatrogenic, whereas in adults, it is almost always intentional.7 Clinical symptoms are commonly observed for certain intoxicating agents. However, the signs may be misdiagnosed or unobserved in children, and treatment may consequently be postponed, thus resulting in catastrophic consequences. Intoxication should therefore be avoided to the greatest extent possible. Recognizing patterns of intoxication is essential for both minimizing the risk of inadvertent poisoning and preventing purposeful poisoning.1
Children's intoxication epidemiology differs among nations. Geographical, cultural, and economic aspects within nations have also been shown to affect epidemiological patterns. Consequently, to execute the proper preventive measures, every nation and area should undertake its own epidemiologic studies.4 Moreover, the pattern of acute pediatric intoxication may evolve over time and follow diverse patterns. Therefore, epidemiological studies investigating the changing patterns of acute pediatric intoxication are essential for future health planning and resource allocation.6
Numerous instances of intoxication in children and adolescents in KSA have been reported.2,3,5,7, 8, 9 However, to our knowledge, no studies have examined the epidemiological patterns of acute pediatric intoxication in Aljouf Province, KSA. Accordingly, the purpose of this study was to identify the types of toxic agents involved in acute pediatric intoxication; the route; and manner of intoxication; and the management and outcomes of intoxication cases in Aljouf Province, KSA during 2015–2021.
Materials and Methods
A cross-sectional retrospective record-based descriptive study was conducted at the Prince Mutaib bin Abdulaziz hospital, and the Maternity and Children's hospital in Aljouf, KSA. All cases of acute intoxication in children younger than 18 years who presented to both hospitals from January 1, 2015 to December 31, 2021 were included in the study. Cases of chronic pediatric intoxication and those with insufficient data were excluded from the study. The analyzed data included demographic characteristics (age, sex, nationality, and residence in urban vs rural areas), year and month of intoxication, place of toxic agent exposure, time of toxic agent exposure, manner of intoxication, toxic agent/agents involved, form of toxic agent, route of exposure, intoxicated child's status upon arrival at the hospital, clinical presentation, treatment, admission history, and outcome. The data were gathered directly by the researchers to eliminate any potential bias in record retrieval.
Statistical analysis
Data were coded, entered, and analyzed in the basic statistics program Statistical Package for the Social Sciences (SPSS) version 22. Descriptive statistics was used to summarize the data. Data are represented as frequencies (n) and percentages (%) for categorical variables. The chi-square test was used to determine associations between variables. Binary logistic regression analysis was used to estimate the significant predictors of accidental intoxication among the studied cases. Manner of intoxication (accidental vs intentional) was the dependent variable. Demographic characteristics (age, sex, nationality, and residence in urban vs rural areas), type of toxic agent involved, number of toxic agents involved, and form of the toxic agent were the independent variables investigated for the prediction of accidental intoxication. A binary logistic regression analysis was also performed on significant predictors of need for admission among the acutely intoxicated children examined. The dependent variable was need for admission (presence vs absence). Demographic characteristics (age, sex, nationality, and residence in urban vs rural areas), type of toxic agent involved, manner of intoxication, status of the intoxicated child upon arrival at the hospital, and clinical presentation were the independent variables potentially predicting the need for admission of the acutely intoxicated children. Receiver operating characteristic (ROC) curve analysis was used to assess the binary logistic regression models by analysis of the area under the curve (AUC). A P-value < 0.05 was considered statistically significant.
Results
From 2015 to 2021, the total reported number of cases of acute pediatric intoxication admitted to the Prince Mutaib bin Abdulaziz hospital, and the Maternity and Children's hospital at Aljouf, KSA was 540. Table 1 shows the demographic data of the studied cases. Age was divided into four groups: <1 year, 1 to <6 years, 6 to <12 years, and 12 to <18 years. Most acutely intoxicated children were in the age group 1 to <6 years (79%). More than half the reported cases were in boys (54%). Ninety-five percent were Saudi. Seventy-seven percent of the intoxicated children were from urban areas.
Table 1.
Demographic data of cases of acute pediatric intoxication during 2015–2021.
| Variable | Number | % | |
|---|---|---|---|
| Age (in years) | <1 | 45 | 8 |
| 1 to <6 | 424 | 79 | |
| 6 to <12 | 44 | 8 | |
| 12 to <18 | 27 | 5 | |
| Sex | Male | 293 | 54 |
| Female | 247 | 46 | |
| Nationality | Saudi | 512 | 95 |
| Non-Saudi | 28 | 5 | |
| Residence | Urban | 418 | 77 |
| Rural | 119 | 22 | |
| Unknown | 3 | 1 | |
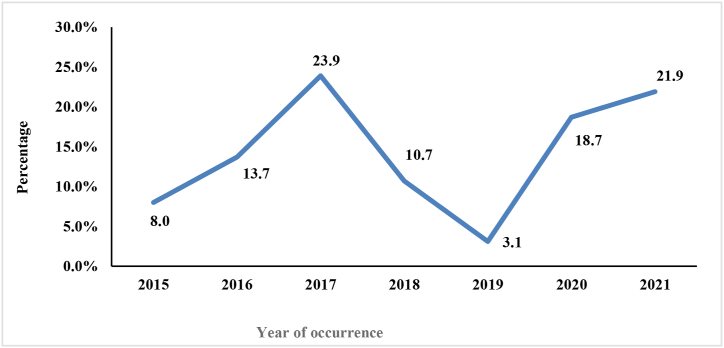
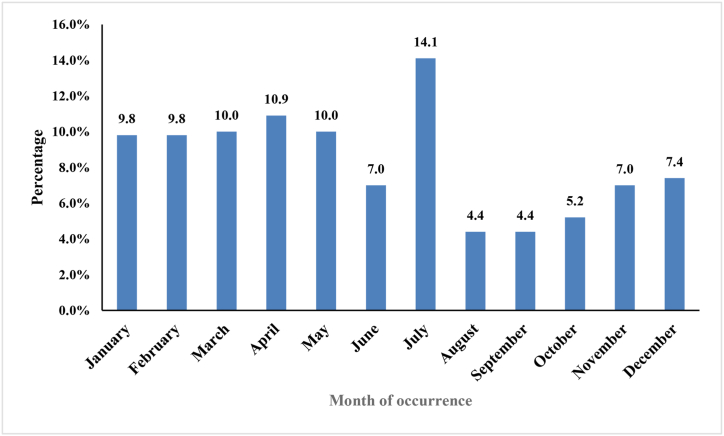
The highest frequency of reported acute pediatric intoxication was in 2017 (23.9%), followed by 2021 (21.9%) (Figure 1). July was the month with the highest frequency of intoxication (14.1%); by contrast, August and September had the fewest cases of acute pediatric intoxication (4.4%) (Figure 2).
Figure 1.
Yearly distribution of pediatric intoxication during 2015–2021.
Figure 2.
Monthly distribution of pediatric intoxication during 2015–2021.
Pharmaceutical drugs were responsible for most reported cases of acute pediatric intoxication (41%). Approximately 78% of cases involved intoxication by a single toxic agent. The most common route of intoxication was oral ingestion (91.7% of acutely intoxicated children). Liquid and solid forms were the most common forms, reported in 40.9% and 39%, respectively. Ninety-two percent of cases of acute intoxication in children occurred in the home. Approximately 23% of the studied cases occurred in the morning. Most of the acutely intoxicated children (89.3%) were accidentally poisoned, whereas 1.7% showed intentional intoxication. Most acutely intoxicated children were in stable condition (82.6%) and were asymptomatic (84%) at the time of admission. Among the symptomatic children, GIT clinical manifestations were the most reported symptoms (12.2%). A total of 20.6% of the children were treated with GIT decontamination, 5.9% were given an antidote, and 2.2% received symptomatic treatment. Forty percent of the studied children were admitted to the inpatient ward, whereas only 0.6% required admission to emergency care. Interestingly, 29.4% were discharged against medical advice. Forty-three percent of the reported acutely intoxicated children showed complete recovery after discharge (Table 2).
Table 2.
Clinical data for cases of acute pediatric intoxication during 2015–2021.
| Variable | Number | % | |
|---|---|---|---|
| Toxic agent type | Chemicals | 213 | 39.4 |
| Pharmaceutical drugs | 221 | 41 | |
| Unspecified | 106 | 19.6 | |
| Number of toxic agents | Single | 420 | 77.8 |
| Multiple | 14 | 2.6 | |
| Unspecified | 106 | 19.6 | |
| Route of intoxication | Oral | 495 | 91.7 |
| Inhalation | 12 | 2.2 | |
| Dermal | 3 | 0.6 | |
| Unspecified | 30 | 5.6 | |
| Form of toxic agent(s) | Solid | 212 | 39 |
| Liquid | 221 | 40.9 | |
| Gas | 8 | 1.5 | |
| Powder | 26 | 5 | |
| Ointment | 1 | 0.2 | |
| Gel | 2 | 0.4 | |
| Unspecified | 70 | 13 | |
| Place of intoxication | Home | 497 | 92 |
| Others | 43 | 8 | |
| Time of intoxication | Morning | 123 | 22.8 |
| Afternoon | 63 | 11.7 | |
| Evening | 100 | 18.5 | |
| Unspecified | 254 | 47 | |
| Manner of intoxication | Accidental | 482 | 89.3 |
| Intentional | 9 | 1.7 | |
| Unspecified | 49 | 9.1 | |
| Status of the intoxicated child after arrival at hospital | Stable | 446 | 82.6 |
| Deteriorated | 21 | 3.9 | |
| Unspecified | 73 | 13.5 | |
| System involved | Asymptomatic | 454 | 84 |
| Gastrointestinal | 66 | 12.2 | |
| Cardiopulmonary | 2 | 0.4 | |
| Neurological | 10 | 1.9 | |
| Others (skin, eye, nose) | 8 | 1.5 | |
| Treatment | Observation | 25 | 4.6 |
| GIT decontamination | 111 | 20.6 | |
| Antidote | 32 | 5.9 | |
| Symptomatic management | 12 | 2.2 | |
| Unspecified | 360 | 66.7 | |
| Admission history | No admission | 46 | 8.5 |
| Admission to inpatient | 216 | 40 | |
| Discharge against medical advice | 159 | 29.4 | |
| Admission to emergency department | 3 | 0.6 | |
| Unspecified | 116 | 21.5 | |
| Outcome of intoxication | Complete recovery on discharge | 232 | 43 |
| Unspecified | 308 | 57 | |
The distribution of the pharmaceutical drugs and chemicals involved in acute pediatric intoxication cases is shown in Table 3, Table 4. The most common causative toxic agent was hydrocarbons (19.4%). The least frequent toxic agents were amphetamine and methanol (0.2%). Analgesics and antipyretics (10.6%) were the most frequent pharmaceutical drugs involved in acute pediatric intoxication. Hydrocarbons (19.4%) were the chemicals most reported to be involved in acute pediatric intoxication.
Table 3.
Distribution of acute pediatric intoxication cases by toxic agent and age group during 2015–2021.
| Toxic substance | Age groups (in years)a |
Total | ||||
|---|---|---|---|---|---|---|
| <1 | 1 to <6 | 6 to <12 | 12 to <18 | |||
| Single agent | Hydrocarbons | 6 (13.3%) | 90 (21.2) | 8 (18.2%) | 1 (3.7%) | 105 (19.4%) |
| Household cleaning supplies | 6 (13.3%) | 47 (11.1) | 9 (20.5%) | 4 (14.8%) | 66 (12.2%) | |
| Personal care products/cosmetics | 2 (4.4%) | 8 (1.9%) | 0 (0%) | 0 (0%) | 10 (1.9%) | |
| Pesticides | 2 (4.4%) | 14 (3.3%) | 5 (11.4%) | 3 (11.1%) | 24 (4.4%) | |
| Methanol | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Dietary supplements | 5 (11.1%) | 30 (7.1%) | 3 (6.8%) | 0 (0%) | 38 (7.0%) | |
| Analgesics and antipyretics | 2 (4.4%) | 39 (9.2%) | 2 (4.5%) | 6 (22.2%) | 49 (9.1%) | |
| Antibiotics | 1 (2.2%) | 16 (3.8%) | 3 (6.8%) | 1 (3.7%) | 21 (3.9%) | |
| Drugs affecting the GIT | 2 (4.4%) | 10 (2.4%) | 0 (0%) | 0 (0%) | 12 (2.2%) | |
| Antihistamines | 1 (2.2%) | 13 (3.1%) | 1 (2.3%) | 0 (0%) | 15 (2.8%) | |
| Hypoglycemic drugs | 0 (0%) | 7 (1.7%) | 0 (0%) | 0 (0%) | 7 (1.3%) | |
| CVS drugs | 5 (11.1%) | 7 (1.7%) | 0 (0%) | 0 (0%) | 12 (2.2%) | |
| Antiepileptics | 1 (2.2%) | 3 (0.7%) | 2 (4.5%) | 0 (0%) | 6 (1.1%) | |
| Anxiolytics, antidepressants, and antipsychotics | 0 (0%) | 6 (1.4%) | 0 (0%) | 3 (11.1%) | 9 (1.7%) | |
| Muscle relaxants | 0 (0%) | 3 (0.7%) | 0 (0%) | 0 (0%) | 3 (0.6%) | |
| Bronchodilators | 1 (2.2%) | 6 (1.4%) | 0 (0%) | 0 (0%) | 7 (1.3%) | |
| Amphetamines | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Oral contraceptive pills | 0 (0%) | 13 (3.1%) | 2 (4.5%) | 0 (0%) | 15 (2.8%) | |
| Herbal remedies | 0 (0%) | 0 (0%) | 0 (0%) | 3 (11.1%) | 3 (0.6%) | |
| Miscellaneous medications | 1 (2.2%) | 6 (1.4%) | 1 (2.3%) | 1 (3.7%) | 9 (1.7%) | |
| Other agents | 2 (4.4%) | 5 (1.2%) | 0 (0%) | 0 (0%) | 7 (1.3%) | |
| Unknown | 6 (13.3%) | 90 (21.2%) | 6 (13.6%) | 4 (14.8%) | 106 (19.6%) | |
| Multiple agents | Analgesics and antihistamines | 1 (2.2%) | 0 (0%) | 0 (0%) | 1 (3.7%) | 2 (0.4%) |
| Analgesics and antibiotics | 0 (0%) | 1 (0.2%) | 2 (4.5%) | 0 (0%) | 3 (0.6%) | |
| Multiple drugs affecting the CVS | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Hypoglycemic drugs and CVS drugs | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2% | |
| Analgesics and oral contraceptive pills | 0 (0%) | 2 (0.5%) | 0 (0%) | 0 (0%) | 2 (0.4%) | |
| Multiple drugs affecting the GIT | 1 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Antibiotics and antihistamines | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Analgesics, drugs affecting the GIT, and oral contraceptive pills | 0 (0%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Dietary supplements and herbal remedies | 0 (0%) | 2 (0.5%) | 0 (0%) | 0 (0%) | 2 (0.4%) | |
| Total | 45 (100%) | 424 (100%) | 44 (100%) | 27 (100%) | 540 (100%) | |
X2 = 125.124, p-value = 0.008.
p-value significant <0.05.
Table 4.
Distribution of acute pediatric intoxication cases according to toxic agent and year of occurrence during 2015–2021.
| Toxic substance | Year of pediatric intoxication occurrencea |
Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | |||
| Single agent | Hydrocarbons | 10 (23.3%) | 8 (10.8%) | 33 (25.6%) | 15 (25.9%) | 1 (5.9%) | 18 (17.8%) | 20 (16.9%) | 105 (19.4%) |
| Household cleaning supplies | 12 (27.9%) | 9 (12.2%) | 13 (10.1%) | 10 (17.2%) | 1 (5.9%) | 14 (13.9%) | 7 (5.9%) | 66 (12.2%) | |
| Personal care products/cosmetics | 0 (0%) | 3 (4.1%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 2 (2.0%) | 3 (2.5%) | 10 (1.9%) | |
| Pesticides | 4 (9.3%) | 3 (4.1%) | 5 (3.9%) | 4 (6.9%) | 0 (0%) | 2 (2.0%) | 6 (5.1%) | 24 (4.4%) | |
| Methanol | 0 (0%) | 0 (0%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Dietary supplements | 1 (2.3%) | 8 (10.8%) | 15 (11.6%) | 3 (5.2%) | 0 (0%) | 5 (5.0%) | 6 (5.1%) | 38 (7.0%) | |
| Analgesics and antipyretics | 4 (9.3%) | 9 (12.2%) | 6 (4.7%) | 5 (8.6%) | 0 (0%) | 12 (11.9%) | 13 (11.0%) | 49 (9.1%) | |
| Antibiotics | 1 (2.3%) | 1 (1.4%) | 9 (7.0%) | 2 (3.4%) | 0 (0%) | 2 (2.0%) | 6 (5.1%) | 21 (3.9%) | |
| Drugs affecting the GIT | 0 (0%) | 3 (4.1%) | 6 (4.7%) | 1 (1.7%) | 0 (0%) | 0 (0%) | 2 (1.7%) | 12 (2.2%) | |
| Antihistamines | 0 (0%) | 5 (6.8%) | 4 (3.1%) | 2 (3.4%) | 0 (0%) | 0 (0%) | 4 (3.4%) | 15 (2.8%) | |
| Hypoglycemic drugs | 0 (0%) | 3 (4.1%) | 3 (2.3%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 0 (0%) | 7 (1.3%) | |
| CVS drugs | 0 (0%) | 0 (0%) | 4 (3.1%) | 5 (8.6%) | 0 (0%) | 0 (0%) | 3 (2.5%) | 12 (2.2%) | |
| Antiepileptics | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 5 (4.2%) | 6 (1.1%) | |
| Anxiolytics, antidepressants, and antipsychotics | 2 (4.7%) | 2 (2.7%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 3 (3.0%) | 0 (0%) | 9 (1.7%) | |
| Muscle relaxants | 1 (2.3%) | 1 (1.4%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (0.6%) | |
| Bronchodilators | 2 (4.7%) | 2 (2.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 2 (1.7%) | 7 (1.3%) | |
| Amphetamines | 0 (0%) | 0 (0%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Oral contraceptive pills | 0 (0%) | 5 (6.8%) | 7 (5.4%) | 3 (5.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 15 (2.8%) | |
| Herbal remedies | 2 (4.7%) | 0 (0%) | 0 (0%) | 1 (1.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (0.6%) | |
| Miscellaneous medications | 0 (0%) | 2 (2.7%) | 2 (1.6%) | 3 (5.2%) | 0 (0%) | 0 (0%) | 2 (1.7%) | 9 (1.7%) | |
| Other agents | 1 (2.3%) | 1 (1.4%) | 2 (1.6%) | 1 (1.7%) | 0 (0%) | 1 (1.0%) | 1 (0.8%) | 7 (1.3%) | |
| Unknown | 2 (4.7%) | 4 (5.4%) | 6 (4.7%) | 2 (3.4%) | 15 (88.2%) | 39 (38.6%) | 38 (32.2%) | 106 (19.6%) | |
| Multiple agents | Analgesics and antihistamines | 0 (0%) | 1 (1.4%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (0.4%) |
| Analgesics and antibiotics | 0 (0%) | 0 (0.0%) | 2 (1.6%) | 1 (1.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (0.6%) | |
| Multiple drugs affecting the CVS | 0 (0%) | 1 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Hypoglycemic drugs and CVS drugs | 0 (0%) | 1 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Analgesics and oral contraceptive pills | 0 (0%) | 0 (0%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (0.4%) | |
| Multiple drugs affecting the GIT | 1 (2.3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Antibiotics and antihistamines | 0 (0%) | 1 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Analgesics, drugs affecting the GIT, and oral contraceptive pills | 0 (0%) | 1 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.2%) | |
| Dietary supplements and herbal remedies | 0 (0%) | 0 (0%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (0.4%) | |
| Total | 43 (100%) | 74 (100%) | 129 (100%) | 58 (100%) | 17 (100%) | 101 (100%) | 118 (100%) | 540 (100%) | |
X2 = 334.009, p-value = 0.000.
p-value significant <0.05.
Table 3 shows a statistically significant relationship between the type of toxic agent and age group (p = 0.008). In children under 1 year of age, hydrocarbons and household cleaning supplies represented the highest percentages of intoxication (13.3% each). For intoxication by multiple agents in this age group, 2.2% showed intoxication due to an analgesic plus an antihistamine, and 2.2% showed intoxication due to multiple drugs affecting the GIT. In the age group of 1 to <6 years), hydrocarbons (21.2%), followed by household cleaning supplies (11.1%), represented the highest percentages of intoxication. A low percentage of acutely intoxicated children showed intoxication by multiple agents in this age group. The age group of 6 to <12 years had the highest percentage of intoxication due to household cleaning supplies (20.5%), followed by hydrocarbons (18.2%). For intoxication by multiple agents in this age group, 4.5% showed intoxication due to an analgesic plus an antibiotic. For the age group of 12 to <18 years, analgesics and antipyretics (22.2%), followed by household cleaning supplies (14.8%) represented the highest percentages of intoxication. For intoxication by multiple agents in this age group, 3.7% showed intoxication due to an analgesic plus an antihistamine.
Table 4 shows a statistically significant relationship between the type of toxic agent and the year of occurrence of pediatric intoxication (p = 0.000). In 2015, household cleaning supplies (27.9%), followed by hydrocarbons (23.3%) represented the highest percentages of intoxication. A total of 2.3% showed intoxication due to multiple drugs affecting the GIT. In 2016, household cleaning supplies, and an analgesic plus an antipyretic (12.2% each), followed by hydrocarbons and dietary supplements (10.8% each) represented the highest percentages of intoxication. Regarding intoxication by multiple agents, an analgesic plus an antihistamine, multiple drugs affecting the CVS, a hypoglycemic drug plus a CVS drug, an antibiotic plus an antihistamine, and an analgesic plus a drug affecting the GIT plus oral contraceptive pills, represented 1.4% each. In 2017, hydrocarbons (25.6%), followed by dietary supplements (11.6%) represented the highest percentages of intoxication. For intoxication by multiple agents, an analgesic plus an antibiotic, an analgesic plus oral contraceptive pills, and dietary supplements with herbal remedies represented 1.6% each. In 2018, hydrocarbons (25.9%), followed by household cleaning supplies (17.2%) represented the highest percentages of intoxication. For intoxication by multiple agents, 1.7% showed intoxication by an analgesic plus an antihistamine. In 2019, 88.2% showed intoxication by unknown agents. No reported cases of intoxication by a single agent were observed except for hydrocarbons (5.9%) and household cleaning supplies (5.9%). In 2020, 38.6% of cases showed intoxication by unknown agents. The highest percentage of intoxication by a known single agent was for hydrocarbons (17.8%), followed by household cleaning supplies (13.9%). In 2021, 32.2% of cases showed intoxication by unknown agents. The highest percentage of intoxication by a known single agent was for hydrocarbons (16.9%), followed by analgesics and antipyretics (11%). No cases of intoxication by multiple agents were reported in 2019, 2020, and 2021.
Table 5 shows a statistically significant relationship between the manner of intoxication and age group (p = 0.000). Approximately 80% of the accidentally intoxicated children were in the age group 1 to <6 years. Most of the intentionally intoxicated children (77.8%) were in the age group of 12 to <18 years.
Table 5.
Manner of pediatric intoxication by age group during 2015–2021.
| Age group (years) | Manner of intoxicationa |
Total | ||
|---|---|---|---|---|
| Accidental | Intentional | Unknown | ||
| <1 | 41 (8.5%) | 0 (0%) | 4 (8.2%) | 45 (8.3%) |
| 1 to <6 | 387 (80.3%) | 1 (11.1%) | 36 (73.5%) | 424 (78.5%) |
| 6 to <12 | 38 (7.9%) | 1 (11.1%) | 5 (10.2%) | 44 (8.1%) |
| 12 to <18 | 16 (3.3%) | 7 (77.8%) | 4 (8.2%) | 27 (5.0%) |
| Total | 482 (100%) | 9 (100%) | 49 (100%) | 540 (100%) |
X2 = 105.763, p-value = 0.000.
p-value significant <0.05.
Table 6 shows a statistically non-significant relationship between the system involved and the outcome (p = 0.283).
Table 6.
Distribution of acute pediatric intoxication by system involved and outcome during 2015–2021.
| Outcome | System involved |
Total | ||||
|---|---|---|---|---|---|---|
| Asymptomatic | GIT | Cardio-pulmonary | Neurological | Others (skin, eye, nose) | ||
| No admission | 43 (9.5%) | 3 (4.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 46 (8.5%) |
| Admission to emergency department | 3 (0.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (0.6%) |
| Admission to inpatient ward | 174 (38.3%) | 31 (47.0%) | 0 (0%) | 5 (50.0%) | 6 (75.0%) | 216 (40.0%) |
| Discharge against medical advice | 137 (30.2%) | 18 (27.3%) | 2 (100.0%) | 1 (10.0%) | 1 (12.5%) | 159 (29.4%) |
| Unknown | 97 (21.4%) | 14 (21.2%) | 0 (0%) | 4 (40.0%) | 1 (12.5%) | 116 (21.5%) |
| Total | 454 (100%) | 66 (100%) | 2 (100%) | 10 (100%) | 8 (100%) | 540 (100%) |
X2 = 18.720, p-value = 0.283
p-value significant <0.05.
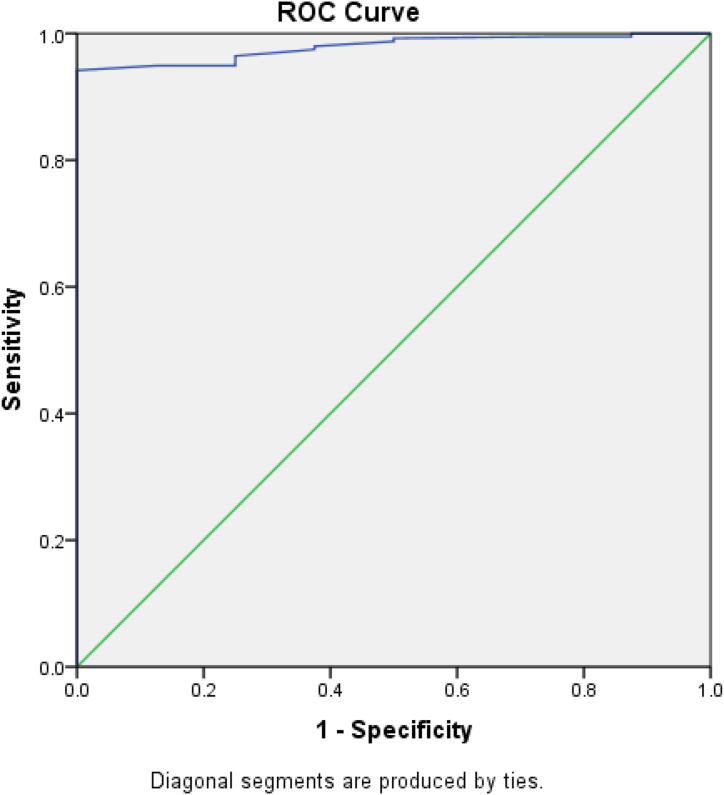
A binary logistic regression analysis of significant predictors of accidental intoxication among the studied cases was performed. For omnibus tests of model coefficients, chi-square = 37.220, df = 7 and p < 0.001; Nagelkerke's r2 was 0.498. The logistic regression model of predictors of accidental intoxication showed that only age and residence in urban vs rural areas had a significant relationship (p < 0.05). As age increased, accidental intoxication became less likely (OR = 0.014, 95% CI = 0.002, 0.096). Acutely intoxicated children in rural areas were significantly less likely to have accidental intoxication than those in urban areas (OR = 0.134, 95% CI = 0.021, 0.868) (Table 7). Our model's ROC curve had a high AUC of approximately 0.979, thus indicating that the logistic regression model significantly predicted accidental pediatric intoxication (p < 0.001) (Figure 3).
Table 7.
Binary logistic regression analysis of predictors of accidental acute pediatric intoxication.
| B | Standard error | p value | Adjusted OR | CI | |
|---|---|---|---|---|---|
| Age groups (years) | −4.265 | 0.982 | <0.001a | 0.014 | 0.002–0.096 |
| Sex | 0.058 | 1.032 | 0.955 | 1.060 | 0.140–8.011 |
| Nationality | −0.255 | 1.370 | 0.852 | 0.775 | 0.053–11.368 |
| Residence | −2.009 | 0.953 | 0.035a | 0.134 | 0.021–0.868 |
| Toxic agent type | 2.054 | 2.026 | 0.311 | 7.799 | 0.147–413.877 |
| Number of toxic agents | −2.784 | 1.592 | 0.080 | 0.062 | 0.003–1.400 |
| Form of toxic agent(s) | 1.421 | 1.947 | 0.465 | 4.143 | 0.091–188.015 |
OR, odds ratio, CI, confidence interval.
p-value significant <0.05.
Figure 3.
Receiver-operating characteristic curve representing the possibilities generated from binary logistic regression analysis for prediction of accidental pediatric intoxication among the studied cases.
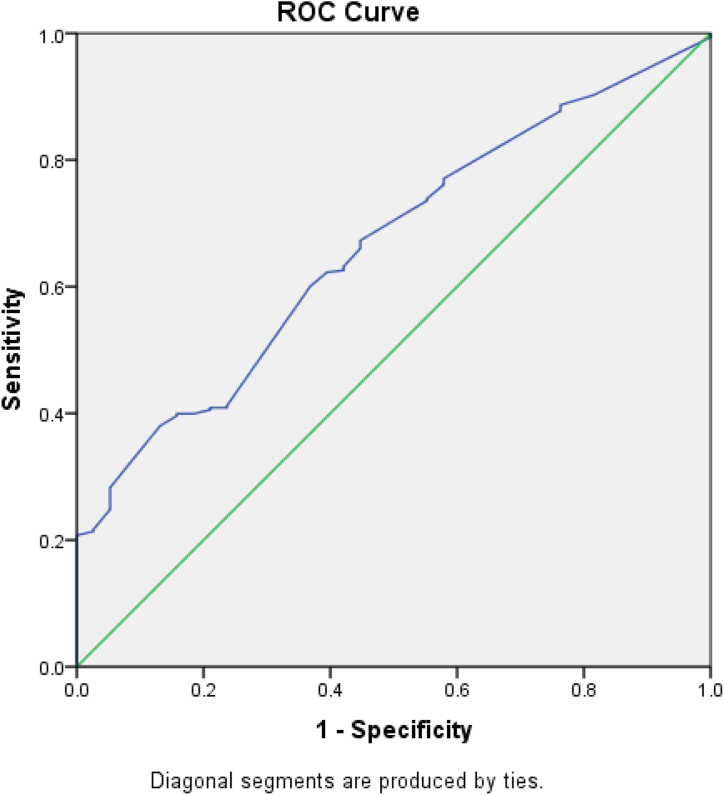
A binary logistic regression analysis of significant predictors of the need for admission among the studied acutely intoxicated children was performed. For omnibus tests of model coefficients, chi-square = 13.395, df = 8, and p = 0.099; Nagelkerke's r2 was 0.075. although the logistic regression model of predictors of the need for admission of the studied acutely intoxicated children was insignificant, it indicated that only the type of toxic agent had a significant relationship with the need for admission (p < 0.05, Table 8). Our model's ROC curve had an AUC of approximately 0.663, thus indicating that the logistic regression model significantly predicted the need for admission of acutely intoxicated children (p = 0.001) (Figure 4).
Table 8.
Binary logistic regression analysis of predictors of the need for admission among acutely intoxicated children.
| B | Standard error | p value | Adjusted OR | CI | |
|---|---|---|---|---|---|
| Age groups (years) | 0.236 | 1.112 | 0.832 | 1.267 | 0.143–11.191 |
| Sex | 0.274 | 0.362 | 0.449 | 1.315 | 0.647–2.674 |
| Nationality | −0.106 | 0.799 | 0.894 | 0.899 | 0.188–4.304 |
| Residence | 0.437 | 0.459 | 0.340 | 1.549 | 0.630–3.805 |
| Toxic agent type | −0.970 | 0.377 | 0.010a | 0.379 | 0.181–0.793 |
| Manner of poisoning | 0.359 | 0.572 | 0.531 | 1.432 | 0.466–4.395 |
| Clinical presentation | 0.874 | 0.561 | 0.119 | 2.397 | 0.798–7.194 |
| Status of the intoxicated child upon arrival at the hospital | 0.057 | 0.298 | 0.848 | 1.059 | 0.590–1.901 |
OR, odds ratio, CI, confidence interval.
p-value significant <0.05.
Figure 4.
Receiver-operating characteristic curve representing the possibilities generated from binary logistic regression analysis for prediction of the need for admission among the studied cases of acute pediatric intoxication.
Discussion
Intoxication is one of the most prevalent crises in pediatric medicine. Instances may conceivably be undiagnosed, particularly if the intoxicated children or their caregivers do not seek medical care, or an incorrect cause is assigned. Even when intoxication is appropriately identified, the responsible agent may be unknown to the healthcare professional or caregiver.1,10 Acute pediatric intoxication in various nations and areas of the world shows significant epidemiological differences. Consequently, every region should investigate its prevalence and influencing factors. Moreover, in developing successful local preventive programs, these differences should be considered.3,11 Accordingly, the current retrospective study was aimed at assessing the pattern and outcome of acute pediatric intoxication at Aljouf, KSA, from 2015 to 2021.
The total reported number of cases of acute pediatric intoxication admitted to the Prince Mutaib bin Abdulaziz hospital, and Maternity and Children's hospital in Aljouf, was 540. This number exceeded the 404 instances of acute chemical intoxication documented at the Preventive Medicine Department in the Qassim Region of KSA from April 1999 to February 2003.7 However, this number was less than the 735 children who presented with intoxication to King Khaled University Hospital Pediatric Emergency Medicine in Riyadh, KSA, from January 2010 to December 2016.2
The highest frequency of reported acute pediatric intoxication was in 2017 (23.9%), followed by 2021 (21.9%). The lowest rate of intoxication was observed in 2019 (3.1%). July was the month with the highest frequency of intoxication (14.1%). The start of summer vacation for children might have been associated with the increase in intoxication observed in July. Summer vacationing children are expected to spend more time engaging in outdoor activities. Sometimes, they may be left alone at home or under the supervision of an older child. In addition, caregivers may be less aware of potential dangers during vacation.1
Most acutely intoxicated children in this study (79%) were in the age group of 1 to <6 years. This finding was consistent to some extent with those of several studies in different regions in KSA and worldwide, during different time periods.2,3,6,9,12, 13, 14 This finding might have been because children become more active at this age and are highly exposed to toxins. They have a proclivity to investigate their environment by placing objects in their mouths, despite their inability to distinguish between harmful and safe agents. Children at this age are also prone to imitating others’ practices, such as medication intake. Therefore, teaching mothers about intoxication prevention methods, such as not referring to pharmaceuticals as candy or purchasing candies that resemble medications, is critical.1,8,9,15,16 More than half of the reported cases in the current study (54%) were in boys. This higher percentage of intoxication in boys than girls has been shown in other studies in different settings.5, 6, 7, 8, 9,12, 13, 14,17 This result might be explained by a tendency for boys to be more mobile and adventurous than girls.9 Furthermore, in certain societies, girls are not encouraged to participate in outdoor pursuits or to take risks.1 However, a female predominance has been shown in other studies.2,18 Regarding nationality, 95% of the studied intoxicated children were Saudi, in agreement with findings from other studies conducted in different regions in KSA.3,5,7 Seventy-seven percent of the studied intoxicated children were from urban areas, a finding consistent with similar studies.6,12,17 However, other studies have shown a higher percentage of pediatric intoxication in rural than urban areas16,18 The logistic regression model of predictors of accidental intoxication in this study indicated that residence in urban vs rural areas had a significant relationship. Acutely intoxicated children in rural areas were significantly less likely to have accidental intoxication than those in urban areas, possibly because of the higher use of hazardous toxic agents in those areas, and varying availability of these agents by location.
Approximately 92% of the acute intoxication cases in children occurred in the home. This result is consistent with findings from previous research conducted in other areas and at various times.5,12, 13, 14,17 A collection of pharmaceuticals, household cleaning agents, and personal care items are frequently inadequately stored and within children's grasp in their homes.8 Intoxication risk is also increased through the use of unlabeled or improperly labeled containers lacking child-resistant closures. Children are inherently inquisitive, and they enjoy discovering their surroundings. Even if harmful materials are stored in well-marked containers with visible warning signs, young children are unlikely to understand what the warnings mean.1
Approximately 22.8% of the studied intoxication cases occurred in the morning, possibly because most children were not noticed by their caregivers, who were engaged in domestic tasks.8
Most acutely intoxicated children in the current study (89.3%) were accidentally intoxicated; by contrast, only 1.7% showed intentional intoxication. This result is consistent with findings from other studies indicating that most intoxicated children are accidentally intoxicated.2,6,7,9,12, 13, 14,17,18 A statistically significant relationship between the manner of intoxication and age group was estimated in the current study. Approximately 80% of the accidentally intoxicated children were in the age group of 1 to <6 years. Most of the intentionally intoxicated children (77.8%) were in the age group of 12 to <18 years. Moreover, the logistic regression model of predictors of accidental intoxication among the studied cases indicated a significant relationship for age: as the age increased, accidental intoxication became less likely. The increased rate of accidental drug intoxication in KSA might be attributable to Saudi families' habits of storing unused pharmaceuticals for later consumption. Furthermore, most drugs can be easily purchased in KSA.2 In addition, accidental pediatric intoxication is considerably increased by the storage of chemicals to which children may be exposed in homes.1 Unintentional intoxication among younger age groups has been associated with a variety of factors, including children's inquisitive nature, natural desire to investigate their surroundings, and a lack of understanding of potential dangers.5 Accordingly, intoxication in children may be avoided in most situations.15 The extremely low rate of deliberate intoxication among the cases analyzed indicated the scarcity of this cultural trend in this part of the world.9 However, such incidents were interestingly observed among the older age group (12 to <18 years). Academic challenges, parental expectations, peer influences, health and psychological issues, and drug abuse are all recognized as factors in purposeful adolescent intoxication.16 To avoid and limit toxicity in the pediatric age group, parents must pay more attention and provide proper care to children of various ages.19
Intoxication prevention strategies must be based on evidence regarding the types of toxic hazards in society.20 Pharmaceutical drugs were responsible for most reported cases of acute pediatric intoxication in the present study (41%), whereas 39.4% were attributed to chemicals.
Approximately 78% of the studied children were intoxicated by a single poisoning agent. The most common causative toxic agent was hydrocarbons (19.4%), followed by household cleaning supplies (12.2%), then analgesics and antipyretics (10.6%). The predominance of pharmaceuticals in pediatric intoxication, with analgesics and antipyretics as the most reported medications, is consistent with findings from similar studies conducted in different regions of KSA at different time periods.2,3,5,8,9 The current study indicated that pharmaceutical drugs were responsible for most reported cases of acute pediatric intoxication, in agreement with similar studies conducted in several regions outside KSA during different time intervals.14,17 This finding might have been due to drug awareness among family members, the availability of free medical treatment, easy access to pharmaceuticals rather than delivery of drugs in child-resistant containers, and careless drug and household product storage.3,8 By contrast, Moazzam et al., in a 2009 study in the Al-Qassim region, KSA, reported that chemicals were responsible for most studied cases of intoxication in children.7 Dayasiri et al., in a 2018 study of acute pediatric intoxication in the North–Central province of Sri Lanka, reported that household chemicals were responsible for 30.2% of acute intoxications, and kerosene oil was the most prevalent toxin. Pharmaceuticals were responsible for 25.3% of intoxications.13 Sobeeh et al., in a 2018 study in Egypt, reported that pediatric intoxication by chemicals was more common than that by pharmaceuticals. This finding might be explained by chemicals, including those used for domestic cleaning, being readily accessible in homes in Egypt and being stored within young children's grasp. Such hazardous chemicals are often kept in easily opened containers, or empty food or drink containers.16 The discrepancy between the results of the current study and these studies may be attributable to the difference in the age groups and regions studied. The results of the current study indicating that hydrocarbons and household cleaning supplies were the most common causative toxic agents is consistent with findings from other studies. In a study in Egypt, the most prevalent sources of intoxication have been found to be household chemicals, with kerosene and chlorine accounting for 43.2% of all cases.15 In a study in central India, most studied children (56%) were found to be intoxicated with household chemicals.6 Furthermore, Tiwari et al. (2021) reported that, because it is a commonly used home item, kerosene remains the most prevalent agent in the pediatric intoxication.10 By contrast, Alghadeer et al. (2018) reported that kerosene is being used less frequently in Saudi Arabian households as a result of recent advancements.2
The most common route of intoxication in the present study was oral ingestion (in 91.7% of acutely intoxicated children). Liquid and solid forms were the most common forms reported, at 40.9% and 39%, respectively. These findings are consistent with pharmaceutical drugs being responsible for most reported cases of acute pediatric intoxication in the present study. Other studies have shown similar results.2,3,5,7,13,14,16,17 The current study indicated a statistically significant relationship between the type of toxic agent and age groups. In children under 12 years of age, hydrocarbons and household cleaning supplies accounted for the highest percentage of intoxication. For the age group of 12 to <18 years, analgesics and antipyretics represented the highest percentage of intoxication. These findings might have been due to how various age groups perceive such dangerous toxic agents. The appeal of a hazardous toxin to children is determined primarily by its physical appearance, whereas its chemical makeup dictates its effect. Size, color, and texture can all influence young children's decisions to handle and consume a material. Liquids have been reported to appeal to young children more than solids, transparent liquids appeal to them more than dark-colored liquids, and small solids appeal to them more than large solids. Solid drugs with bright colors may be relatively more appealing to children.1 For older children, the appeal of a hazardous toxin to them might be due to the delivery of pharmaceuticals in envelopes rather than child-resistant containers, easy access to medications without prescriptions, irresponsible drug storage in homes, and the increase in intentional intoxication ideation at this age.9
The present study indicated a statistically significant relationship between the type of toxic agent and the year of occurrence of pediatric intoxication. On the basis of these findings, hydrocarbons might be potentially hazardous toxic agents almost every calendar year. Preventive measures should be sought to address this continual hazard.
Most acutely intoxicated children in this study were in stable condition (82.6%) and asymptomatic (84%) at the time of admission. Among symptomatic children, GIT clinical manifestations were the most reported symptoms (12.2%). This finding is in agreement with those of several previous studies.3,6,9,13,16,17 By contrast, Sarhan et al. (2018) and Lee et al. (2019) reported that the most prevalent symptoms among symptomatic individuals were neurological.14,18 This finding might have been associated with differences in the types of toxic agent involved in inducing toxicity among the studied cases in each study.
Regarding treatments received, 20.6% were treated through GIT decontamination, 5.9% were given an antidote, and 2.2% received symptomatic treatment. This treatment approach was determined by various aspects, including the type of toxic agent, dosage, general health status at the time of admission, clinical manifestations, age, existence of other illnesses or damage, and time of toxic agent intake before admission to the healthcare facility.5 Several similar studies have followed the same approach.2,9,12
Approximately 40% of the studied children were admitted to the inpatient ward, whereas only 0.6% of children required admission to emergency care. Interestingly, 29.4% were discharged against medical advice. Other studies have shown higher clinical severity than that in this study. Moazzam et al., in 2009, reported a 2.2% mortality rate.7 Tobaiqy et al., in 2020, reported that 11.6% were rushed to the pediatric intensive care unit. A single death has been reported.5 Ramawat and Jain, in 2021, reported that 12% of children were in serious condition and required intensive care, and 6% required ventilator support.6
The statistically non-significant relationship between the system involved and the outcome in the current study suggests that caregivers should be made aware that even mild symptoms may require admission. Accordingly, medical care should be sought whenever intoxication is suspected. In contrast, the logistic regression model of predictors of the need for admission of the studied acutely intoxicated children showed that the type of toxic agent involved had a significant relationship. This finding indicates importance of early identification of the type of toxic agent in intoxicated children.
Consequently, the findings of the current study and similar studies may be applied to enhance the implementation of effective prevention strategies to decrease the incidence of pediatric intoxication.2,3,14 Such preventive measures could include legislation prohibiting over-the-counter drug sales, selling potentially harmful substances in child-resistant containers, and improving accurate and thorough medical record-keeping for better information availability.9,15
The strength of this study is that it was conducted over an extended period from 2015 to 2021, thus providing a broad picture of the pattern of acute pediatric intoxication in Aljouf Province, KSA, and supporting the establishment of preventive measures to address this health concern. Moreover, to our knowledge, no previous studies have studied the epidemiological patterns of acute pediatric intoxication in Aljouf Province, KSA.
Conclusion
Acute pediatric intoxication is a genuine problem in Aljouf, KSA. Most acutely intoxicated children were in the age group of 1 to <6 years. Pharmaceutical drugs were responsible for most reported cases. Most acutely intoxicated children were stable and asymptomatic at the time of admission. Nonetheless, most of the studied children were admitted to the inpatient ward. Consequently, our findings might indicate a need for caregivers to be more mindful of potentially harmful toxic agents and their negative consequences. Furthermore, preventive actions are required to decrease acute pediatric intoxication in Aljouf, KSA. Accordingly, our study results highlight the need for implementing such prevention strategies to mitigate future acute pediatric intoxication. Moreover, estimating the significant predictors of the occurrence of accidental intoxication and the need for admission may aid in the design of preventive measures.
Source of funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The ethical approval for the study was obtained from the Local Committee of Bioethics at Jouf University in Sakaka, KSA (#20-04-42).
Authors contributions
MAI, KNA, ATA, NAA, and BHA conceived and designed the study. KNA, ATA, NAA, and BHA collected data. MAI, KNA, ATA, NAA, BHA, and EMA analyzed and interpreted data. MAI, KNA, ATA, NAA, BHA, and EMA wrote the final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgments
The authors thank Community and Family Medicine Department, COM-JU for technical support.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Peden M., Oyegbite K., Ozanne-Smith J., Hyder A.A., Branche C., Rahman F., et al. WHO Press, World Health Organization; 2008. World report on child injury prevention; pp. 123–138.https://apps.who.int/iris/handle/10665/43851 [PubMed] [Google Scholar]
- 2.Alghadeer S., Alrohaimi M., Althiban A., Kalagi N.A., Balkhi B., Khan A.A. The patterns of children poisoning cases in community teaching hospital in Riyadh, Saudi Arabia. Saudi Pharmaceut J. 2018;26(1):93–97. doi: 10.1016/j.jsps.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ragab A.R. Pattern of pediatric toxicity in Saudi Arabia-Eastern province (incidence, demographics and predisposing factors) Pediatr Therapeut. 2015;5(1) doi: 10.4172/2161-0665.1000220. [DOI] [Google Scholar]
- 4.Duyu M. Retrospective evaluation of intoxication cases followed in pediatric intensive care: a 5-year experience. Haydarpasa Numune Med J. 2020;60(4):437–444. doi: 10.14744/hnhj.2020.88709. [DOI] [Google Scholar]
- 5.Tobaiqy M., Asiri B.A., Sholan A.H., Alzahrani Y.A., Alkatheeri A.A., Mahha A.M., et al. Frequency and management of acute poisoning among children attending an emergency department in Saudi Arabia. Pharmacy. 2020;8(4):189. doi: 10.3390/pharmacy8040189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramawat P., Jain N. A study about clinic-epidemiological pattern of acute poisoning in pediatric age group. Asian J Med Sci. 2021;12(4):48–53. doi: 10.3126/ajms.v12i4.30701. [DOI] [Google Scholar]
- 7.Moazzam M., Al Saigul A.M., Naguib M., Al Alfi M.A. Pattern of acute poisoning in Al-Qassim region: a surveillance report from Saudi Arabia, 1999-2003. East Mediterr Health J. 2009;15(4):1005–1010. doi: 10.26719/2009.15.4.1005. [DOI] [PubMed] [Google Scholar]
- 8.Al-Shehri M.A. Pattern of childhood poisoning in Abha city – southwestern Saudi Arabia. J Family Community Med. 2004;11(2):59–63. [PMC free article] [PubMed] [Google Scholar]
- 9.Abd-Elhaleem Z.A.E., Muqhem B.A.A. Pattern of acute poisoning in Al Majmaah region, Saudi Arabia. Am J Clin Exp Med. 2014;2(4):79–85. doi: 10.11648/j.ajcem.20140204.15. [DOI] [Google Scholar]
- 10.Tiwari A., Trivedi P., Mishra S., Sachdev M., Panda S., Chandramohan G.M. Clinical spectrum and outcome of poisoning. Indian J Pediatr. 2021;88(3):289. doi: 10.1007/S12098-020-03551-1. [DOI] [PubMed] [Google Scholar]
- 11.Mintegi S., Azkunaga B., Prego J., Qureshi N., Dalziel S.R., Arana-Arri E., et al. International epidemiological differences in acute poisonings in pediatric emergency departments. Pediatr Emerg Care. 2019;35(1):50–57. doi: 10.1097/PEC.0000000000001031. [DOI] [PubMed] [Google Scholar]
- 12.Hassan B.A., Siam M.G. Patterns of acute poisoning in childhood in Zagazig, Egypt: an epidemiological study. Int Sch Res Notices. 2014;2014 doi: 10.1155/2014/245279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dayasiri M.B.K.C., Jayamanne S.F., Jayasinghe C.Y. Patterns and outcome of acute poisoning among children in rural Sri Lanka. BMC Pediatr. 2018;18:274. doi: 10.1186/s12887-018-1246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee J., Fan N.C., Yao T.C., Hsia S.H., Lee E.P., Huang J.L., et al. Clinical spectrum of acute poisoning in children admitted to the pediatric emergency department. Pediatr Neonatol. 2019;60(1):59–67. doi: 10.1016/j.pedneo.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Seif E., Gomaa R., Eisa M. A retrospective study of acute poisoning in children under 5 Years old admitted to Alexandria poison center in Egypt. World J Prev Med. 2016;4(2):32–39. doi: 10.12691/jpm-4-2-2. [DOI] [Google Scholar]
- 16.Sobeeh F.G., Abd El-Hay N.S.D., Draz E., Saad K. Pattern of acute pediatric poisoning in middle delta poison control centers. Tanta Med J. 2018;46(3):215–224. doi: 10.4103/tmj.tmj_26_17. [DOI] [Google Scholar]
- 17.Farag A.A., Said E.A., Fakher H.M. Patterns of pediatric acute poisoning at Banha poisoning control center, Egypt: one-year prospective study. Asia Pac J Med Toxicol. 2020;9(2):44–51. doi: 10.22038/apjmt.2020.16386. [DOI] [Google Scholar]
- 18.Sarhan D., Ameen S., Saleh R. Pattern of acute toxicity among children at Zagazig University hospitals in 2017: (clinical and demographic data) Egypt Soc Clin Toxicol J. 2018;6(1):1–11. doi: 10.21608/esctj.2018.62428. [DOI] [Google Scholar]
- 19.Shokry D.A. Pattern of pediatric poisoning in Egypt- cases admitted to national poisoning control center. Asian J Biomed Pharmaceut Sci. 2018;8 doi: 10.4066/2249-622X-C2-005. [DOI] [Google Scholar]
- 20.Huynh A., Cairns R., Brown J.A., Lynch A., Robinson J., Wylie C., et al. Patterns of poisoning exposure at different ages: the 2015 annual report of the Australian poisons information centers. Med J Aust. 2018;209(2):74–79. doi: 10.5694/mja17.01063. [DOI] [PubMed] [Google Scholar]