Abstract
Acute gastrointestinal bleeding (AGIB) is a common condition leading to hospitalization and is associated with significant morbidity and mortality. Various endoscopic treatments have been reported for AGIB, while its endoscopic hemostasis treatment by combined modality with PuraStat and endoscopic hemoclips remains less well documented. We report 6 cases of AGIB, i.e., 5 cases of ulcer bleeding and 1 case of ruptured gastric varices in 3 males and 3 females aged 49–97 years (mean age, 77 years), 2 and 1 of whom had been on antithrombotic drugs and nonsteroidal anti-inflammatory drugs, respectively, with 2 of these found to be in critical condition with hemorrhagic shock. Types of bleeding treated included oozing bleeding from visible vessels (n = 3), spurting bleeding from visible vessels (n = 2) and from gastric varices (n = 1). In all cases, complete hemostasis was achieved with no rebleeding. To our knowledge, this report represents a valuable addition to the AGIB literature describing endoscopic hemostasis by combined modality therapy with PuraStat and endoscopic hemoclips.
Keywords: PuraStat, Gastrointestinal bleeding, Hemostasis
Introduction
Acute gastrointestinal bleeding (AGIB) is a common condition leading to hospitalization and is associated with significant morbidity and mortality, especially in the elderly [1, 2]. Thermal devices (e.g., bipolar electrocoagulation, heater probe, argon plasma coagulation), injectable agents (e.g., epinephrine, sclerosants, thrombin/fibrin glue), and mechanical devices (e.g., endoscopic hemoclips) have been reported to be effective endoscopic hemostatic therapies [3]. Endoscopic hemoclips have the theoretical benefit of not causing tissue damage, unlike thermal treatments and sclerosants, and are also preferred in patients taking antithrombotic drugs [4]. Recently, a novel self-assembling peptide matrix-forming gel, PuraStat (3-D matrix Europe SAS, France), has been reported to be useful for hemostasis in AGIB [5, 6]. The mechanism of hemostasis with PuraStat is explained as follows: as it comes into contact with blood or bodily fluids, it rapidly forms nanofibers into a peptide hydrogel, coating the bleeding point and forming a mechanical barrier, and thus triggering blood clotting [7]. While clinical data for PuraStat are limited and its use combined with endoscopic hemoclips remains poorly described, we herein report 6 cases of AGIB successfully treated by combined modality therapy with PuraStat and endoscopic hemoclips.
Case Report/Case Presentation
Case 1
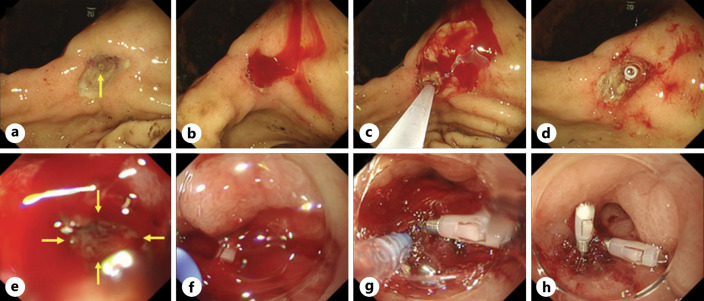
A 78-year-old man undergoing chemotherapy for castration-resistant prostate cancer was raced to our hospital for hematemesis. Found to be severely anemic (Hb, 3.9 g/dL), he was admitted to the intensive care unit (ICU) for a blood transfusion. Emergency esophagogastroduodenoscopy (EGD) revealed gastric ulcer in the lesser curvature of the gastric angle (Fig. 1a). Spurting bleeding occurred during observation, and hemostasis treatment was attempted (Fig. 1b). PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to suppression of the bleeding volume (Fig. 1c). Hemostasis was subsequently achieved with an endoscopic hemoclip (Fig. 1d). Hemostasis was reconfirmed by EGD performed 2 days later.
Fig. 1.
Emergency esophagogastroduodenoscopy (EGD). a EGD revealed gastric ulcer in the lesser curvature of the gastric angle. b Spurting bleeding occurred during observation, and hemostasis was attempted. c PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to suppression of the bleeding volume. d Hemostasis was subsequently achieved with an endoscopic hemoclip. e EGD revealed oozing bleeding from a Dieulafoy’s lesion in the greater curvature of the gastric antrum. f Hemostasis treatment was attempted using an endoscopic hemoclip, but the bleeding persisted. g Thus, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to a reduction in bleeding volume. h Hemostasis was subsequently achieved with an additional endoscopic hemoclip.
Case 2
A 97-year-old woman with a history of chronic heart failure was rushed to our hospital for tarry stool. Found to be moderately anemic (Hb, 7.8 g/dL), she was admitted to the hospital for a blood transfusion. Emergency EGD revealed oozing bleeding from a Dieulafoy’s lesion in the greater curvature of the gastric antrum (Fig. 1e). Hemostasis was attempted using an endoscopic hemoclip, but the bleeding persisted (Fig. 1f). Thus, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to a reduction in bleeding volume (Fig. 1g). Hemostasis was subsequently achieved with an additional endoscopic hemoclip (Fig. 1h). Hemostasis was reconfirmed by EGD performed 2 days later.
Case 3
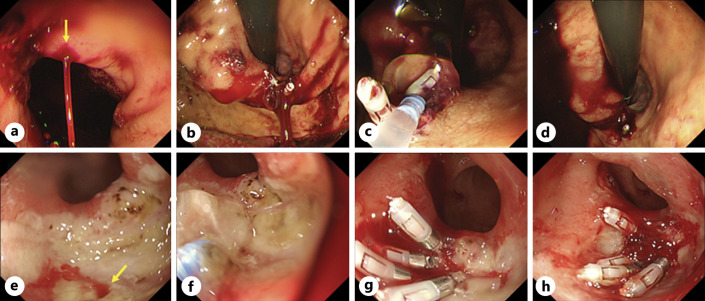
A 49-year-old man with a history of alcoholic cirrhosis was hurried to our hospital for hemorrhagic shock due to hematemesis. Found to be moderately anemic (Hb, 9.0 g/dL), he was admitted to the ICU for a blood transfusion. Computed tomography revealed the presence of gastric varices in the gastric cardia and a hematoma inside the stomach, suggesting ruptured gastric varices. Emergency EGD revealed spurting bleeding from gastric varices (Fig. 2a). Hemostasis therapy was attempted using an endoscopic hemoclip, which led to immediate reduction of bleeding (Fig. 2b). Subsequently, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter (Fig, 2c), and complete hemostasis was achieved (Fig. 2d). Hemostasis was reconfirmed by EGD performed on the following day.
Fig. 2.
Emergency esophagogastroduodenoscopy (EGD). a EGD revealed spurting bleeding from gastric varices. b Hemostasis treatment was attempted using an endoscopic hemoclip, which led to immediate reduction of bleeding. c Subsequently, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, (d) which led to complete hemostasis. e EGD revealed duodenal ulcer and oozing bleeding from a visible vessel in the inferior aspect of the duodenal bulb. f Hemostasis treatment was attempted using PuraStat (1 mL) through a dedicated catheter, followed by an endoscopic hemoclip. g As the bleeding persisted, PuraStat (2 mL) was applied to the bleeding site, (h) and complete hemostasis was achieved.
Case 4
A 79-year-old woman presented to our hospital for tarry stool. She had a history of spinal stenosis and had been taking limaprost alfadex and celecoxib. She was admitted to the hospital for moderate anemia (Hb, 9.4 g/dL). Emergency EGD revealed a duodenal ulcer as well as oozing bleeding from a visible vessel in the inferior aspect of the duodenal bulb (Fig. 2e). Hemostasis was attempted by applying PuraStat (1 mL) through a dedicated catheter (Fig. 2f), followed by an endoscopic hemoclip, but the bleeding persisted (Fig. 2g). Thus, PuraStat (2 mL) was again applied to the bleeding site, and complete hemostasis was achieved (Fig. 2h). Hemostasis was reconfirmed by EGD performed 3 days later.
Case 5
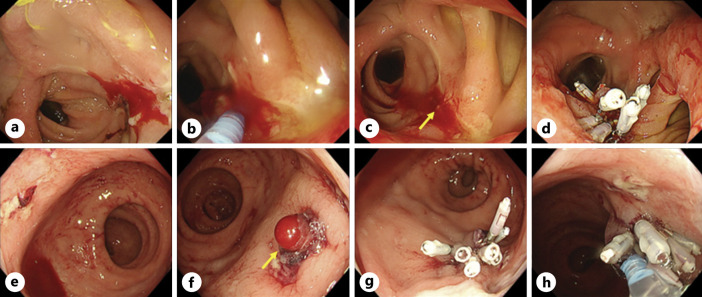
An 86-year-old man with a history of distal gastrectomy and small bowel perforation was rushed to our hospital for tarry stool. Found to be severely anemic (Hb, 5.8 g/dL), he was admitted to the hospital for a blood transfusion. Emergency EGD revealed oozing bleeding from a small intestinal ulcer on the anal side of the anastomosis (Fig. 3a). Thus, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to a reduction in bleeding volume (Fig. 3b), but oozing bleeding continued from a visible vessel (Fig. 3c). Hemostasis was subsequently achieved using an endoscopic hemoclip (Fig. 3d). Hemostasis was reconfirmed on the following day.
Fig. 3.
Emergency esophagogastroduodenoscopy (EGD) and colonoscopy (CS). a EGD revealed oozing bleeding from a small intestinal ulcer on the anal side of the anastomosis. b PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, which led to a reduction in bleeding volume, (c) but the oozing bleeding continued from a visible vessel. d Hemostasis was subsequently achieved using an endoscopic hemoclip. e, f CS revealed multiple rectal ulcers and spurting bleeding from a visible vessel in a rectal ulcer. g Hemostasis treatment was attempted using an endoscopic hemoclip, which led to immediate reduction of bleeding. h Subsequently, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, and complete hemostasis was achieved.
Case 6
A 73-year-old woman taking aspirin and limaprost alfadex with a history of chronic renal failure and cerebral infarction was raced to our hospital for hemorrhagic shock due to hematochezia. Found to be severely anemic (Hb, 5.9 g/dL), she was admitted to the ICU for a blood transfusion. Emergency colonoscopy revealed multiple rectal ulcers and spurting bleeding from a visible vessel in a rectal ulcer (Fig. 3e, f). Hemostasis was attempted using an endoscopic hemoclip, which led to immediate reduction of bleeding (Fig. 3g). Subsequently, PuraStat (3 mL) was applied to the bleeding site through a dedicated catheter, and complete hemostasis was achieved (Fig. 3h).
The patients thus treated were 3 males and 3 females aged 49–97 years (mean age, 77 years), 2 of whom had been on antithrombotic drugs and 1 on nonsteroidal anti-inflammatory drugs. All 6 patients had no rebleeding within 1–3 days of initial hemostasis (Table 1).
Table 1.
Patient characteristics
| Case | Age | Sex | Medical history | Antithrombotic drugs | NSAIDs | Location | Cause of bleeding | Type of bleeding | Hemorrhagic shock | Rebleeding |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 78 | M | Prostate cancer | (−) | (−) | Stomach | Ulcer | Spurting | (−) | (−) |
| 2 | 97 | F | Chronic heart failure | (−) | (−) | Stomach | Ulcer | Oozing | (−) | (−) |
| 3 | 49 | M | Alcoholic cirrhosis | (−) | (−) | Stomach | Varices | Spurting | (+) | (−) |
| 4 | 79 | F | Spinal stenosis | Limaprost alfadex | Celecoxib | Duodenum | Ulcer | Oozing | (−) | (−) |
| 5 | 86 | M | Distal gastrectomy, small bowel perforation | (−) | (−) | Small intestine | Ulcer | Oozing | (−) | (−) |
| 6 | 73 | F | Chronic renal failure, cerebral infarction | Aspirin Limaprost alfadex |
(−) | Rectum | Ulcer | Spurting | (+) | (−) |
Conclusion
Our case offers two important implications for clinical practice. First, endoscopic hemostasis treatment by combined modality therapy with PuraStat and endoscopic hemoclips may prove useful for AGIB from (1) a visible vessel regardless of bleeding type and (2) ruptured gastric varices, while its supportive clinical data are very limited and its hemostasis technique remains less well described in the literature.
PuraStat is indicated for hemostasis of oozing bleeding in the parenchyma of solid organs, vascular anastomoses, and small vessels or capillaries of the gastrointestinal tract [6]. To date, PuraStat has been reported to be useful for AGIB as rescue therapy [5] and as primary and secondary therapy [6]. First, de Nucci G et al. reported that hemostasis was achieved in 70/77 (90.9%) with PuraStat as rescue therapy following failure of at least two conventional techniques for refractory AGIB. Next, Branchi F et al. reported 111 cases of AGIB in which PuraStat was used for primary and secondary therapy, demonstrating that hemostasis was achieved with primary therapy in 42/79 (53.2%) and that involving additional techniques in 32/79 (40.5%) and with secondary therapy in 24/32 (75.0%). The profile of our 6 patients is summarized in Table 1. In all cases, complete hemostasis was achieved by combined modality therapy with PuraStat and endoscopic hemoclips. The types of bleeding treated included oozing bleeding from a visible vessel (n = 3), spurting bleeding from a visible vessel (n = 2), and spurting bleeding from gastric varices (n = 1). Current algorithm for the management of gastric varices bleeding recommends band ligation or endoscopic clipping as options for temporary hemostasis for active bleeding [8]. PuraStat proved useful in facilitating subsequent hemostasis with an endoscopic hemoclip for ruptured gastric varices, which is shown to be associated with a high mortality risk in patients with liver cirrhosis. The novelty in this report is that combined modality therapy with PuraStat and endoscopic hemoclips may prove useful for AGIB from (1) a visible vessel regardless of bleeding type and (2) ruptured gastric varices.
The second implication is that PuraStat may contribute to the suppression of rebleeding. All 6 patients, including 2 in a serious condition due to hemorrhagic shock, had no rebleeding after hemostasis. PuraStat has been reported (1) to improve damage by downregulating the expression of inflammatory cytokines and upregulating the expression of wound healing-related factors in a rat model [9] as well as (2) to reduce the delayed bleeding rate by promoting mucosal regeneration and ulcer healing after large endoscopic resections in a human study [10]. It is thus speculated that PuraStat contributed to the suppression of rebleeding after hemostasis of AGIB in this study.
In conclusion, endoscopic hemostasis by combined modality therapy with PuraStat and endoscopic hemoclips may prove effective for AGIB. Again, while PuraStat has mainly been reported to be useful as a hemostat for oozing bleeding, it may also prove effective for spurting bleeding and ruptured gastric varices when used in combination with endoscopic hemoclips. The CARE Checklist has been completed by the authors for this case report, attached as supplementary material (for all online suppl. material, see www.karger.com/doi/10.1159/000528896).
Statement of Ethics
This study protocol was reviewed and approved by the Institutional Review Board of National Hospital Organization Hakodate National Hospital (approval number: R4-1014001). Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to disclose in association with this study.
Funding Sources
The authors received no funding for this research.
Author Contributions
Kimitoshi Kubo reported the case series and wrote the manuscript. Kimitoshi Kubo, Shuhei Hayasaka, and Ikko Tanaka were involved in this study as physicians treating the patients. All authors declare that they contributed to the preparation of the manuscript at all stages and that they have read and approved the final version of the manuscript for publication.
Funding Statement
The authors received no funding for this research.
Data Availability Statement
All data generated and/or analyzed during the course of this study are included in the article. Any further query may be addressed to the corresponding author.
References
- 1. Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47(10):a1–46. 10.1055/s-0034-1393172. [DOI] [PubMed] [Google Scholar]
- 2. Triantafyllou K, Gkolfakis P, Gralnek IM, Oakland K, Manes G, Radaelli F, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53(8):850–68. 10.1055/a-1496-8969. [DOI] [PubMed] [Google Scholar]
- 3. Laine L, McQuaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7(1):33–47; quiz 1-2. 10.1016/j.cgh.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 4. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345–60; quiz 361. 10.1038/ajg.2011.480. [DOI] [PubMed] [Google Scholar]
- 5. de Nucci G, Reati R, Arena I, Bezzio C, Devani M, Corte CD, et al. Efficacy of a novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding. Endoscopy. 2020;52(9):773–9. 10.1055/a-1145-3412. [DOI] [PubMed] [Google Scholar]
- 6. Branchi F, Klingenberg-Noftz R, Friedrich K, Bürgel N, Daum S, Buchkremer J, et al. PuraStat in gastrointestinal bleeding: results of a prospective multicentre observational pilot study. Surg Endosc. 2022;36(5):2954–61. 10.1007/s00464-021-08589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Subramaniam S, Kandiah K, Thayalasekaran S, Longcroft-Wheaton G, Bhandari P. Haemostasis and prevention of bleeding related to ER: the role of a novel self-assembling peptide. United Eur Gastroenterol J. 2019;7(1):155–62. 10.1177/2050640618811504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Henry Z, Patel K, Patton H, Saad W. AGA clinical practice update on management of bleeding gastric varices: expert review. Clin Gastroenterol Hepatol. 2021;19(6):1098–107.e1. 10.1016/j.cgh.2021.01.027. [DOI] [PubMed] [Google Scholar]
- 9. Araki T, Mitsuyama K, Yamasaki H, Morita M, Tsuruta K, Mori A, et al. Therapeutic potential of a self-assembling peptide hydrogel to treat colonic injuries associated with inflammatory bowel disease. J Crohns Colitis. 2021;15(9):1517–27. 10.1093/ecco-jcc/jjab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Uraoka T, Ochiai Y, Fujimoto A, Goto O, Kawahara Y, Kobayashi N, et al. A novel fully synthetic and self assembled peptide solution for endoscopic submucosal dissection-induced ulcer in the stomach. Gastrointest Endosc. 2016;83(6):1259–64. 10.1016/j.gie.2015.11.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated and/or analyzed during the course of this study are included in the article. Any further query may be addressed to the corresponding author.