Abstract
Background and aims
The incidence of acute pancreatitis (AP) is increasing in the UK. Patients with severe AP require a significant amount of resources to support them during their admission. The ability to predict which patients will develop multiorgan dysfunction remains poor leading to a delay in the identification of these patients and a window of opportunity for early intervention is missed. Social deprivation has been linked with increased mortality across surgical specialties. Its role in predicting mortality in patients with AP remains unclear but would allow high-risk patients to be identified early and to focus resources on high-risk populations.
Methods
A prospectively collected single-centre database was analysed. English Index of Multiple Deprivation (IMD) was calculated based on postcode. Patients were grouped according to their English IMD quintile. Outcomes measured included all-cause mortality, Intestive care unit (ITU) admission, overall length of stay (LOS) and local pancreatitis-specific complications.
Results
398 patients with AP between 2018 and 2021 were identified. There were significantly more patients with AP in Q1 (IMD 1–2) compared with Q5 (IMD 9–10) (156 vs 38, p<0.001). Patients who were resident in the most deprived areas were significantly younger (52.4 in Q1 vs 65.2 in Q5, p<0.001), and more often smokers (39.1% in Q1 vs 23.7% in Q5, p=0.044) with IHD (95.0% vs 92.1% in Q5, p<0.001). In multivariate modelling, there was no significance difference in pancreatitis-related complications, number of ITU visits, number of organs supported and overall, LOS by IMD quintile.
Conclusions
Although there was a significantly higher number of patients admitted to our unit with AP from the most socially deprived quintiles, there was no correlation between social economic deprivation and mortality following AP.
Keywords: ACUTE PANCREATITIS, PANCREATIC DISEASE, DIABETES MELLITUS
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Social deprivation has been linked with poorer outcomes and increased mortality across many surgical specialties.
Social deprivation has been linked with increased incidence of acute pancreatitis (AP) and its link with increased mortality is unclear.
WHAT THIS STUDY ADDS
This study confirms that social deprivation is not linked with increased mortality in AP.
It has shown for the first time that it is not associated with increased pancreatitis-specific complications or the development of organ failure.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Further research is required to identify high-risk patients with acute pancreatitis allowing resources to be focused early on these patients to improve outcomes.
Introduction
In the UK, the incidence of acute pancreatitis (AP) has more than doubled in the past three decades, accounting for 20 000 hospital admissions1 with estimated NHS costs of £200 million.2 While most patients will have a mild self-limiting episode 20%–30% of patients develop a severe pancreatitis with mortality of up to 50%.3 Patients with severe AP often have a prolonged hospital stay requiring extensive support and resources. Despite advances in the management of AP, patients with severe AP are only identified when organ failure is present and established. The ability to risk stratify patients early would allow for finite resources to be focused on those more likely to have a severe disease phenotype creating a window of opportunity for therapeutic option to prevent multiorgan dysfunction.
Several other surgical specialities have explored the link between deprivation and clinical outcomes suggesting higher mortality, complication rates and longer length of hospital stay3–5 in patients with greater social deprivation (SD). Studies to date in patients with AP have been inconclusive about the association between SD and mortality rates after AP.6–8 To address this question, national linking studies have been performed but due to trial design, these studies lack any evidence regarding surrogates such as length of hospital stay or pancreatitis-specific complications and are often missing key clinical data. Understanding the complex relationship between deprivation, population demographics and AP outcomes may lead to targeted research or strategies to improve outcomes.
This aim of this study is to evaluate associations between SD and short-term and long-term outcomes in patients presenting with AP to a tertiary referral centre.
Methods
Study design
A review of a prospectively maintained database of all AP admissions to Freeman Hospital between 1 January 2018 and 31 December 2021 was undertaken. Freeman hospital has an established hub-and-spoke pathway for management of patients with AP in the North-East England.9
Study population
SD was defined according to the English Index of Multiple Deprivation 2019 (IMD) for the postcode of the patient’s residence, and assigned using the Ministry of Housing, communities and local government postcode look-up tool.10 IMD classifies all areas in the country into five quintiles, with quintile 1 being the most deprived and quintile 5 being the least deprived.
Baseline characteristics and laboratory results were recorded prospectively. Charlson Comorbidity Index was calculated for patients and the associated predicted 10 survival11 on MD calculator (www.mdcalc.com). Length of intensive care (ITU) admission, number of organs requiring support were also collected. Severity of AP was based on the revised Atlanta criteria.12
Follow-up
Information regarding patient follow-up, death, readmission, and impaired endocrine and exocrine function was recorded using online electronic patient records (both in-hospital and general practice).
The Strengthening the Reporting of Observational Studies in Epidemiology guidance was used in reporting of study findings.13
Outcome measures
The primary outcome measure was overall all-cause mortality measured at 30 days, 90 days and at the end of the study period.
Secondary outcomes were: AP-related local and systemic complications, admission to ITU, length of hospital stay and length of stay (LOS) (in days) spent in the tertiary centre until discharge home or to a ‘step-down’ rehabilitation hospital.
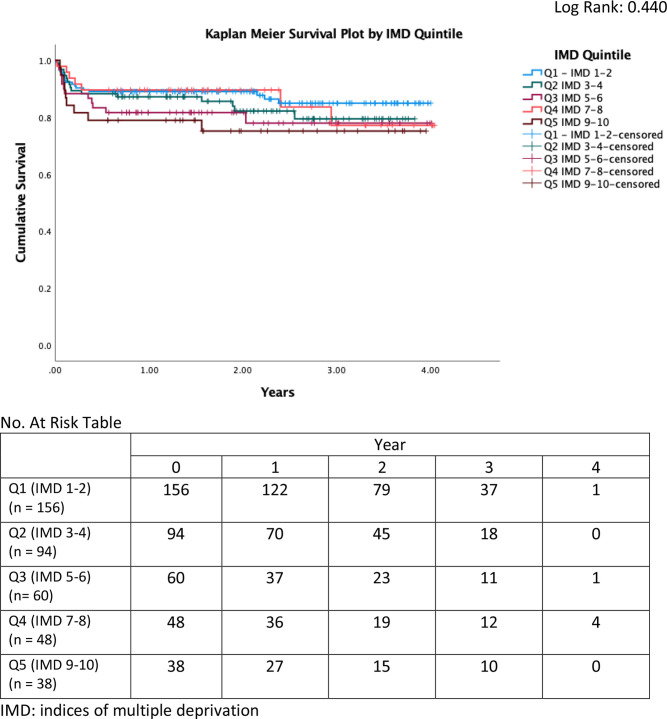
Statistical analysis
Normally distributed data are presented as mean (SD), and hypothesis testing performed with paired and unpaired t-tests. Non-normally distributed data are presented as median (IQR) values with analysis using Mann-Whitney U test or Wilcoxon signed rank test. Categorical data were analysed by means of χ2. Aanalysis of variance (ANOVA) and χ2 tests were used to compare patient characteristics by IMD quintiles. Kaplan-Meier survival curves of overall mortality were created, and log-rank test used to compare mortality by IMD quintiles and with the most socioeconomically deprived (IMD1-3) compared with IMD 4+. A stepwise adjusted Cox regression analysis was performed to understand the impact of SD on survival. Univariate and multivariate logistic regression was performed for admission to ITU. Statistical analysis was performed using SPSS V.26 (SPSS, IBM).
Results
Overall, 396 patients with AP were included with a median follow-up of 22.8 (10.8–33.6) months. There were significantly more patients with AP in Q1 (IMD 1–2) compared with Q5 (IMD 9–10) (156 vs 38, p<0.001).
There were no differences by IMD quintile for patient gender, medical history, premorbidity scores and laboratory results. However, patients resident in the most deprived areas were significantly younger (52.4 in Q1 vs 65.2 in Q5), and more often smokers (39.1% in Q1 vs 23.7% in Q5) with IHD (95.0% vs 92.1% in Q5) (table 1).
Table 1.
Baseline demographics of all admission with AP by quintile
| Q1 | Q2 | Q3 | Q4 | Q5 | P value | |
| No | 156 | 94 | 60 | 48 | 38 | <0.001* |
| Age, mean (SD) | 52.4 (15.5) | 59.8 (15.) | 58.8 (14.4) | 59.5 (12.8) | 65.2 (13.7) | <0.001* |
| Gender (male %) | 97 (62%) | 58 (62%) | 42 (70%) | 27 (56%( | 19 (50%) | 0.341 |
| Medical history | ||||||
| Type 2 diabetes mellitus | 31 (19.9%) | 17 (18.1%) | 13 (21.7%) | 5 (10.4%) | 7 (18.4%) | 0.578 |
| Past alcohol dependence | 31 (19.9%) | 17 (18.1%) | 13 (21.7%) | 5 (10.4%) | 7 (18.4%) | 0.058 |
| Ischaemic heart disease | 148 (94.9%) | 76 (80.9%) | 55 (91.7%) | 47 (97.9%) | 35 (92.1%) | <0.001* |
| Hypertension | 47 (30.1%) | 30 (31.9%) | 20 (33.3%) | 14 (29.2%) | 16 (42.1%) | 0.627 |
| Chronic kidney disease | 8 (5.13%) | 9 (9.57%) | 2 (3.33%) | 2 (4.17%) | 1 (2.63%) | 0.375 |
| Chronic obstructive pulmonary disease | 14 (8.97%) | 8 (8.51%) | 2 (3.33%) | 1 (2.08%) | 1 (2.63%) | 0.228 |
| Cerebrovascular disease | 4 (2.56%) | 2 (2.13%) | 4 (6.67%) | 1 (2.08%) | 2 (5.26%) | 0.484 |
| Smoker | 61 (39.1%) | 23 (24.5%) | 12 (20%) | 12 (25%) | 9 (23.7%) | 0.044* |
| Alcohol aetiology | 99 (63.5%) | 54 (57.4%) | 28 (46.7%) | 31 (64.6%) | 19 (50%) | 0.119 |
| Gallstone aetiology | 51 (32.7%) | 36 (38.3%) | 22 (36.7%) | 22 (45.8%) | 18 (47.4%) | 0.334 |
| Premorbid ECOG | ||||||
| 1 | 35 (22.4%) | 29 (30.9%) | 16 (26.7%) | 15 (31.3%) | 13 (34.2%) | 0.75 |
| 2 | 14 (8.97%) | 9 (9.57%) | 6 (10%) | 2 (4.17%) | 2 (5.26%) | |
| 3 | 13 (8.33%) | 4 (4.26%) | 7 (11.7%) | 3 (6.25%) | 3 (7.89%) | |
| 4 | 3 (1.92%) | 1 (1.06%) | 0 (0%) | 0 (0%) | 1 (2.63%) | |
| Charlson Comorbidity Index | 2 (0–3) | 2 (1-4) | 2 (1-3) | 2 (1-3) | 3 (1.75–4) | 0.018 |
| Predicted 10-year survival | 90% (77%–98%) | 90% (53%–96%) | 90% (77%–98%) | 90% (77%–98%) | 77% (53%–91.5%) | 0.018 |
| Medical history of acute pancreatitis | 61 (39.1%) | 30 (31.9%) | 18 (30%) | 15 (31.3%) | 8 (21.1%) | 0.313 |
| Laboratory results | ||||||
| Amylase Median (IQR) | 451 (140–1419) | 702 (139–1872) | 939 (165–2054) | 864 (288–1891) | 1248 (86–1931) | 0.487 |
| C reactive protein Median (IQR) | 54 (6.5–190) | 32.1 (6.2–204) | 16.9 (5.0–158.3) | 14 (5.0–164.5) | 79.5 (8.0–185) | 0.914 |
| Albumin Mean (SD) | 37.0 (8.1) | 37.4 (7.2) | 38.8 (8.4) | 38.5 (7.1) | 37.6 (8.9) | 0.585 |
| Total protein Mean (SD) | 68.2 (10.6) | 69.1 (7.5) | 70.8 (7.2) | 69.1 (7.8) | 65.8 (8.2) | 0.152 |
| Alanine aminotransferase Median (IQR) | 38.5 (18-96) | 51 (20–163.5) | 72 (30–208) | 105.0 (29-265) | 106.0 (31.0–187) | 0.345 |
| Alkaline phosphatase Median (IQR) | 127(88-177) | 119.5 (84.5–171.5) | 120.0 (92.0–210) | 101 (84–150.5 | 122 (90–212) | 0.583 |
| Platelets | 290(210-387) | 286(232-376) | 262(218-338) | 268(223-304) | 302(198-386) | 0.660 |
| Prothrombin time | 15.2 (3.3) | 164 (6.7) | 16.0 (5.4) | 14.7 (3.2) | 15.2 (2.3) | 0.245 |
*Statistically significant at<0.05 level
ECOG, Eastern Cooperative Oncology Group
Complications
In multivariate modelling, there was no significant difference in pancreatitis-related complications, number of ITU visits, number of organs supported and overall, LOS by IMD quintile (online supplemental table 1).
bmjgast-2022-001035supp002.pdf (61.2KB, pdf)
Survival analysis
In total, 5% (n=18) died within 30 days, 11% (n=44) died within 90 days of admission and 16% of patients (n=63) had died at follow-up; by quintile this was 13%, 17%, 20%, 15% and 24%, respectively (p=0.146). Kaplan-Meier analysis did not reveal a difference in survival by quintile (figure 1).
Figure 1.
Kaplan-Meier survival plot by IMD quintile
This was also the case when comparing those living in the most deprived areas (IMD 1–3) compared with those in IMD 4 and above (online supplemental figure 1).
bmjgast-2022-001035supp001.pdf (70.9KB, pdf)
In terms of ITU admission, univariate regression, between lower quintiles (IMD 1–3) versus higher quintiles (IMD 4 and above), showed that lower IMD scores were not associated with ITU admission, or short-term and long-term survival outcomes.
Multivariate analysis demonstrated significantly poorer survival outcomes for patients with older age (HR=1.064, p=0.003), higher prothrombin time (HR=0.868, p=0.05) and need for ventilation support in the ICU (HR=0.319, p=0.036). Significant predictors for ICU admission included age (HR=1.054, p=0.001), prothrombin time (HR=0.89, p=0.027) and need for ventilation support (HR=0.198, p=0.000) (online supplemental tables 2 and 3).
bmjgast-2022-001035supp003.pdf (61.5KB, pdf)
bmjgast-2022-001035supp004.pdf (53.6KB, pdf)
Discussion
This study has identified significant differences in some baseline characteristics of patients admitted across social classes with AP. There were no differences seen in overall survival up to 4 years postadmission or in the development of complications related to AP across the groups based on SD was seen. There were observed trends in differences in the frequencies for mortality by deprivation quintile, but this was non-significant (p=0.146).
In our unselected population, a higher number of patients admitted with AP were from IMD quintile 1 (the most deprived areas). Patients with AP in IMD quintile 1 (the most deprived areas) had a non-significantly lower mortality rate that patients in IMD quintile 5 (the least deprived areas). Previous published studies on this have shown conflicting results. In a study by Roberts et al7 investigating incidence and mortality in AP across England, patients in quintile 1 had a significantly higher incidence of AP and when corrected for age, had a significantly higher risk of mortality in AP. In contrast, a study also by Roberts et al6 investigating incidence and mortality in AP across Wales found no relationship between SD and mortality in AP. Despite this, the correlation between SD and increased incidence of AP was seen in this study. A population study in Scotland8 again found no correlation between socioeconomic deprivation (SED) and mortality but did not comment on incidence. Although Roberts et al corrected for age we and other studies have not. The numbers included in our study are lower than national linking databases and, therefore, this is not feasible in our study. In multivariate analysis, age was seen as a significant predictor of mortality and patients in quintile 1 were significantly younger than those in more affluent quintile and, therefore, this may explain the difference seen.
Patients presenting with AP from IMD quintile 1 (the most deprived areas) were significantly younger, more likely to smoke and to have IHD than all other quintiles. Our results have shown that although IMD quintile was not a predictor of overall survival, patient age, raised PT and respiratory failure requiring invasive ventilation (organ failure) were independent predictors of poor outcome. This is in keeping with our understanding of disease severity in AP that organ dysfunction was a predictor of mortality and SD does not appear to impact on survival outcomes.
Interestingly, although SD was not an independent predictor of complications or mortality, significantly more patients admitted to our unit with AP were from lower IMD quintiles. This study was not designed to investigate the impact of SED on the incidence of AP and this data is therefore not normalised to the baseline demographics of the referring population. Previous alcohol intake was similar across the quintiles as was the incidence of gallstone disease and therefore these have not contributed to higher incidence of AP in these groups. Interestingly, the study also highlighted a higher prevalence of IHD in lower quintile groups particularly in the younger population, an observation previously noted by population studies in other countries14 where in two or more diseases and developing multimorbidity is common in people with SD.15
A limitation of this study is that it is an analysis of data from a single centre. Our unit is a tertiary referral centre for severe pancreatitis across the North-East of England and, therefore, the true incidence of AP cannot be estimated from this data as many patients with mild AP are managed in referring units. In contrast to larger national linking studies, the data in our study is complete and from a large single centre providing long-term follow-up data including metrics not limited to socioeconomical status. Previous population studies have shown that prevalence of AP is directly related to socioeconomic status and education,16 however, patient-level data with regard to impact of such SD on postpancreatitis complications and organ failure was lacking. Our data have shown that SD does not impact on these pancreas-specific outcomes following AP.
Future studies are required to identify high-risk patients admitted with AP who will develop severe disease and pancreatic complications allowing appropriate focusing of resources to improve outcomes. This study has shown that patients from lower SED are not at higher risk of mortality and complications from AP. Further studies to identify high-risk groups should focus on other groups of patients.
In conclusion, this single-centre study has shown that low SED does not affect pancreatitis-related complications or overall mortality.
Footnotes
Twitter: @sanjay_HPB
Contributors: WBL and FR conceived the idea collected the data and wrote the manuscript. SP, MKN and LS conceived the idea and review the final manuscript. SN performed the statistical analysis and reviewed the final manuscript. SP is the guarantor for this manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data will made available on request on a case-by-case basis.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Newcastle Hospitals research department and was registered on the clinical effectiveness register.
References
- 1.Williams JG, Roberts SE, Ali MF, et al. Gastroenterology services in the UK. The burden of disease, and the organisation and delivery of services for gastrointestinal and liver disorders: a review of the evidence. Gut 2007;56 Suppl 1(Suppl 1):1–113. 10.1136/gut.2006.117598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mole DJ, Gungabissoon U, Johnston P, et al. Identifying risk factors for progression to critical care admission and death among individuals with acute pancreatitis: a record linkage analysis of Scottish healthcare databases. BMJ Open 2016;6:e011474. 10.1136/bmjopen-2016-011474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeevan R, Browne JP, Pereira J, et al. Socioeconomic deprivation and inpatient complication rates following mastectomy and breast reconstruction surgery. Br J Surg 2015;102:1064–70. 10.1002/bjs.9847 [DOI] [PubMed] [Google Scholar]
- 4.Barnard J, Grant SW, Hickey GL, et al. Is social deprivation an independent predictor of outcomes following cardiac surgery? an analysis of 240,221 patients from a national registry. BMJ Open 2015;5:e008287. 10.1136/bmjopen-2015-008287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khashram M, Pitama S, Williman JA, et al. Survival disparity following abdominal aortic aneurysm repair highlights inequality in ethnic and socio-economic status. Eur J Vasc Endovasc Surg 2017;54:689–96. 10.1016/j.ejvs.2017.08.018 [DOI] [PubMed] [Google Scholar]
- 6.Roberts SE, Thorne K, Evans PA, et al. Mortality following acute pancreatitis: social deprivation, hospital size and time of admission: record linkage study. BMC Gastroenterol 2014;14:153. 10.1186/1471-230X-14-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts SE, Williams JG, Meddings D, et al. Incidence and case fatality for acute pancreatitis in England: geographical variation, social deprivation, alcohol consumption and aetiology -- a record linkage study. Aliment Pharmacol Ther 2008;28:931–41. 10.1111/j.1365-2036.2008.03809.x [DOI] [PubMed] [Google Scholar]
- 8.Ventre C, Nowell S, Graham C, et al. Survival and new-onset morbidity after critical care admission for acute pancreatitis in scotland: a national electronic healthcare record linkage cohort study. BMJ Open 2018;8:e023853. 10.1136/bmjopen-2018-023853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nayar MK, Bekkali NLH, Bourne D, et al. Novel multidisciplinary hub-and-spoke tertiary service for the management of severe acute pancreatitis. BMJ Open Gastroenterol 2021;8:e000501. 10.1136/bmjgast-2020-000501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Housing CLG . English indices of deprivation. 2019. Available: https://imd-by-postcode.opendatacommunities.org/imd/2019
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 12.Foster BR, Jensen KK, Bakis G, et al. Revised Atlanta classification for acute pancreatitis: a pictorial essay. Radiographics 2016;36:675–87. 10.1148/rg.2016150097 [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cornman JC, Glei DA, Goldman N, et al. Socioeconomic status and biological markers of health: an examination of adults in the United States and Taiwan. J Aging Health 2015;27:75–102. 10.1177/0898264314538661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schäfer I, Hansen H, Schön G, et al. The influence of age, gender and socio-economic status on multimorbidity patterns in primary care. first results from the multicare cohort study. BMC Health Serv Res 2012;12:89. 10.1186/1472-6963-12-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kivimäki M, Batty GD, Pentti J, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health 2020;5:e140–9. 10.1016/S2468-2667(19)30248-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgast-2022-001035supp002.pdf (61.2KB, pdf)
bmjgast-2022-001035supp001.pdf (70.9KB, pdf)
bmjgast-2022-001035supp003.pdf (61.5KB, pdf)
bmjgast-2022-001035supp004.pdf (53.6KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data will made available on request on a case-by-case basis.