Abstract
Purpose:
Visual functioning evaluated by the Catquest-9SF questionnaire has shown to be a valid measure for assessing a patient’s prioritization for cataract surgery. This study adapted Catquest-9SF for visual function outcomes post uni-lateral cataract surgery or bi-lateral cataract surgery.
Methods:
Visual functioning was assessed before and after uni-lateral or bi-lateral cataract surgery using the Catquest-9SF questionnaire. Patients were enrolled to this study prior to their cataract surgery between March 29 and April 30, 2021 at Shellharbour Hospital, Australia. Catquest-9SF questionnaires were completed prior to and 3 months post surgery. Resulting data were assessed for fit to a Rasch model using WINSTEPS software (version 4.2.0). Catquest-9SF data analysis of Chi-square, Wilcoxon sum test, and Fischer’s test were performed in R (version 4.1.0). P value <.05 was considered statistically significant.
Results:
Sixty-one patients (mean age = 73.2 years, 62% female) were included for analysis. Catquest-9SF response thresholds, adequate precision (person separation index = 2.58, person reliability = 0.87, Cronbach’s alpha = 0.74), uni-dimensionality, and no misfits (infit range 0.65–1.33; outfit range 0.64–1.31) were recorded. The mean of item calibration for patients was -0.22 post-operatively. There was significant (P <.05) improvement (16.3%) in visual functions across all nine Catquest 9-SF items. There was a significant mean visual function difference between patients with uni-lateral (10.1%) and bi-lateral cataract surgery (22.3%) pre-operatively and post-operatively.
Conclusion:
The Catquest-9SF questionnaire showed excellent psychometric properties and can assess visual functioning in an Australian population. There was a significant improvement in patient visual function post cataract surgery and higher functioning with bi-lateral cataract surgery.
Keywords: Bi-lateral cataract surgery, cataract surgery, Catquest-9SF, Rasch analysis, visual functioning
Cataracts are an opacification of the crystalline lens resulting from normal ageing, trauma, metabolic disorders, medications, or congenital defects.[1] They are the leading cause of blindness worldwide, and over 700,000 Australians are affected.[2-4] Cataracts often develop slowly and can affect one or both eyes, leading to impaired activities of daily living.[1] Cataract surgery has become one of the most common surgical procedures in the developed world, having increased 400% in the past 10 years.[4] The combination of an aging population with increasing chronic diseases and improvements in cataract surgery technology has resulted in 245,797 surgeries between 2014 and 2015 in Australia.[4] Currently, cataract treatment involves removing the cataract through small-incision phaco-emulsification and implanting a synthetic intra-ocular lens (IOL).[1] The expected result is enhanced visual acuity and improved quality of life and activities of daily living.[5,6]
Visual acuity and residual refractive error are important objective outcomes to measure cataract surgery success and overall health status. Self-reported visual functioning is also an important proxy for these outcomes and to additionally encourage patient-centered care.[7] Patient concern, lifestyle, and subjective reports of functioning have gradually become additional factors for surgical referral, rather than visual acuity alone.[8] As it is subjectively defined and patient-centered, higher visual functioning improves satisfaction and follows on to yield greater medical compliance, well-being, and treatment outcomes.[9,10] Therefore, visual functioning post cataract surgery is a salient factor to be considered and can be a surrogate marker of satisfaction toward a hospital or specialist.[11]
Very few studies have addressed visual function outcomes for patients undergoing cataract surgery in Australia with successful Rasch validation.[12,13,14,15] The Catquest-9SF questionnaire is relatively new and has only been validated once in an Australian population.[12,13,14] The purpose of this prospective study were to 1) assess the psychometric properties of the Catquest-9SF questionnaire use in clinical practice in the pre-operative Australian cataract population and 2) assess and compare between uni-lateral cataract surgery (underwent the first surgery in one eye) and bi-lateral cataract surgery (underwent the second surgery in contralateral eye) visual functioning by use of the Catquest-9SF questionnaire.
Methods
The English version of the Catquest-9SF questionnaire is a nine-item Rasch-scaled questionnaire [Fig. 1] that comprises two global assessment questions (Ca and Cb) and seven daily-life questions (C1-C7) [Table 1]. Questions Ca and C1–C7 have five responses ranging from 4= ‘Yes, very great difficulties’ to 1 = ‘No, no difficulties’. For question Cb, responses range from ‘4 = Very dissatisfied’ to 1 = ‘Very satisfied’. All questions have a fifth response of the ‘Cannot decide’ option. Sixty-one patients undergoing routine age-related cataract surgery between March 29 and April 30, 2021 at Shellharbour Hospital, Australia, were recruited. Patients needed to be English-speaking and English-coherent to be eligible in this study. Patients who were not able to understand the questionnaire or had cognitive impairment (obtained from the carer’s history or electronic medical record diagnosis) were excluded. There were no exclusion criteria for age, gender, and past ocular or systemic diseases. The patients completed the same format Catquest-9SF questionnaire 1 week before their surgery and 3 months post cataract surgery.[14] All patients underwent uncomplicated uni-lateral phaco-emulsification and mono-focal IOL insertion by a single ophthalmologist (SA) at Shellharbour public hospital, New South Wales, Australia. Uni-lateral patients were defined as patients who have had no previous cataract surgery, whereas bi-lateral cataract patients had previous cataract surgery in one eye and underwent surgery in the contralateral eye. The results of the Catquest questionnaire were analyzed using Chi-square, Wilcoxon sum, and Fischer’s tests, and the average improvement in visual improvement was compared between the uni-lateral and bi-lateral groups. A P value of < 0.05 was considered statistically significant. The protocol for this study was designed in accordance with the Declaration of Helsinki and was approved by the University of Wollongong/Illawarra Shoalhaven Local Health District Health and Medical Human Research Ethics Committee (Ethics number: 2021/008).
Figure 1.
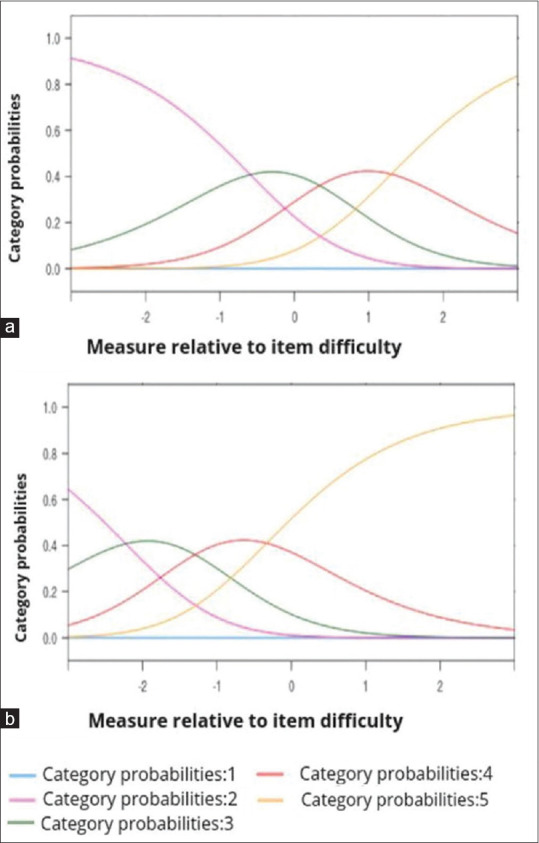
Category probability curve for Catquest-9SF nine-item questionnaire. (a) Global assessment item Cb (satisfaction with vision/sight) only and (b) daily-life activities items C1–C7 and Ca
Table 1.
Rasch analysis results of Catquest-9SF questionnaire
| Item | Parameter | Item calibration (standard error)† | Infit | Outfit | ||
|---|---|---|---|---|---|---|
|
| ||||||
| MNSQ | ZSTD | MNSQ | ZSTD | |||
| Ca | A - Difficulties in any way in daily life | 0.093 (0.152) | 0.65 | -2.59 | 0.64 | -2.62 |
| Cb | B - Satisfaction with vision/sight | 0.771 (0.155) | 0.75 | -1.73 | 0.74 | -1.82 |
| C1 | Reading text in newspaper | 0.502 (0.151) | 1.05 | 0.39 | 1.08 | 0.52 |
| C2 | Recognizing faces of people you meet | -0.970 (0.181) | 1.16 | 0.87 | 1.1 | 0.57 |
| C3 | Seeing prices of shopping goods | -0.548 (0.151) | 0.8 | -1.4 | 0.79 | -1.47 |
| C4 | Seeing to walk on uneven ground | -0.783 (0.173) | 1.01 | 0.1 | 1.08 | 0.48 |
| C5 | Seeing to do needlework, handicraft | -0.238 (0.173) | 1.13 | 0.8 | 1.12 | 0.73 |
| C6 | Reading subtitles on the TV | 0.628 (0.152) | 1.33 | 1.98 | 1.31 | 1.9 |
| C7 | Seeing to carry out a preferred hobby | 0.325 (0.154) | 1.18 | 1.1 | 1.18 | 1.11 |
†Measured in logits. A positive value indicates that the item is easier (requires lower visual function) while a negative value indicates that the item is more difficult (higher visual function is required). Infit; inlier-sensitive or information-weighted fit, Outfit; outlier-sensitive fit, MNSQ; mean squared, ZSTD; z-standardized.
Rasch and statistical analysis
Rasch analysis combines a person’s ability to perform a task (person ability) with the level of difficulty required to perform that task (item difficulty) on a linear scale. The results are presented as log of odds (logit) units.[16] Lower values show low task difficulty; values <1 indicate that the observation was redundant (the data over-fit the model) and insignificant, whereas values >1 indicate that the model was significant, and the data under-fit the model. People with higher ability combined with an item with a greater difficulty is overall expressed lower on the logit scale. When expressed on a person-item map, a person placed at the lowest unit of the scale has high visual functions and likely responded the questionnaire with ‘no, no difficulties’ to all questions. A person placed at 0 of the scale responded that they had some difficulties performing some of the tasks, with likely the more difficult ones placed at the more negative part of the scale. The option ‘cannot decide’ on the Catquest questionnaire is treated as missing in the Rasch analysis and is included in the likelihood. This ensures that Rasch models are accurate, and the imputation is not required if data fit the model.[2,12,17] Overall, Rasch analysis informs how items fit according to the trait being measured (in this analysis, visual function) and the scale’s ability to distinguish respondents based on ability. Additionally, Rasch analysis uses person separation to classify people as high or low performers in questionnaires where low scores (<2) imply that questionnaire items were insufficient and insensitive. The acceptable values are > 3.00 for differentiation between low, medium, and high abilities.[16] Rasch analysis is commonly reported as the mean of square residual (MNSQ) and z-standardized score (ZSTD).[18] Rasch analysis used version 4.2.0 of the WINSTEPS software (Winsteps.com, Chicago, IL, USA).[19] Rasch analysis was divided into global assessment for item Cb and daily activity items C1–C7 and Ca groups. Uni-lateral and bi-lateral cataract surgery categories were comparatively analyzed for differences in visual functioning. A P value of <.05 was considered significant. All analyses were performed using R 4.0.3 (magrittr package, http://www.R-project.org/, R Foundation for Statistical Computing, Vienna, Austria).[20]
Results
Among 61 patients included, the median age was 74.0 years (mean = 73.2, SD = 8.5), 62.2% were female, 29 (47.5%) had uni-lateral cataract surgery, and 32 (52.4%) bi-lateral cataract surgery [Table 2].
Table 2.
Number of patients with unilateral cataract surgery and bilateral cataract surgery, (total n=61)
| Unilateral cataract surgery | Bilateral cataract surgery | P | ||
|---|---|---|---|---|
| Gender | ||||
| Female | 17 | 21 | 0.76‡ | |
| Male | 12 | 11 | ||
| Age | ||||
| Mean (SD) | 73.59 (13.00) | 72.84 (9.75) | 0.51§ | |
| Median (IQR) | 75.00 (13.00) | 73.50 (9.75) | ||
| Eye operated on | ||||
| Right | 7 | 12 | 0.28¶ | |
| Left | 22 | 20 | ||
|
| ||||
| Pre-surgery Catquest-9SF | Mean unilateral visual functioning | Mean bilateral visual functioning | Bilateral vs unilateral baseline visual functioning (%)♯ | |
|
| ||||
| Difficulties in any way in daily life | 1.7 | 2.9 | 39.9 | <.001 ‡ |
| Satisfaction with vision/sight | 1.7 | 2.6 | 32.3 | <.001 ‡ |
| Reading text in newspaper | 2.5 | 2.6 | 2.0 | 0.04 ‡ |
| Recognising faces of the people you meet | 3.2 | 3.5 | 10.3 | 0.23‡ |
| Seeing prices of shopping goods | 2.1 | 3.0 | 28.1 | 0.004 ‡ |
| Seeing to walk on uneven ground | 3.0 | 3.5 | 12.1 | 0.15‡ |
| Seeing to do needlework, handicraft | 2.9 | 3.3 | 11.3 | 0.02 ‡ |
| Reading subtitles on the TV | 1.8 | 2.9 | 37.4 | <.001 ‡ |
| Seeing to carry out a preferred hobby | 2.3 | 3.2 | 26.9 | 0.006 ‡ |
| Post-surgery Catquest-9SF | ||||
| Difficulties in any way in daily life | 3.1 | 3.2 | 1.5 | 0.76‡ |
| Satisfaction with vision/sight | 2.3 | 3.3 | 28.9 | <.001 ‡ |
| Reading text in newspaper | 3.0 | 3.0 | 1.3 | 0.39‡ |
| Recognising faces of the people you meet | 3.3 | 3.9 | 16.5 | <.001 ‡ |
| Seeing prices of shopping goods | 3.4 | 3.5 | 1.3 | 0.88‡ |
| Seeing to walk on uneven ground | 3.5 | 3.5 | 0.5 | 0.99‡ |
| Seeing to do needlework, handicraft | 3.2 | 3.4 | 4.8 | 0.38‡ |
| Reading subtitles on the TV | 2.5 | 3.2 | 20.1 | 0.04 ‡ |
| Seeing to carry out a preferred hobby | 2.7 | 3.4 | 21.1 | 0.01 ‡ |
‡Chi-square test, §Wilcoxon sum test, ¶Fisher’s exact test. SD=standard deviation, IQR=interquartile range. Chi-square test compared the Catquest-9SF assessment questions between the two cohorts (patients with unilateral cataract surgery, n=29 and patients with bilateral cataract surgery, n=32), P<.05 was considered significant and displayed as bold. ♯Visual function between unilateral and bilateral cataract surgery in before and after cataract surgery. Total mean of nine items pre-surgery=22.3% and post-surgery=10.1%. Overall mean visual functioning increased by 22% in unilateral patients and 10.4% in bilateral patients post cataract surgery.
Rasch analysis
Following Rasch analysis, the Catquest-9SF met acceptable criteria for category threshold order, fit statistics, and precision. Uni-dimensionality was confirmed with principal component analysis, and there was a lack of notable differential item functioning. There was some mis-targeting, indicating that the items were relatively easy for respondent ability.
The probability curves for global visual satisfaction and daily visual functional categories are illustrated in Fig. 1a and b, respectively. The person separation index was 2.58, and the patient separation reliability was 0.87. All items were within an in-fit range of 0.65–1.33 and an out-fit range of 0.64–1.31. This was within the acceptable range of 0.50–1.50 [Table 1]. Cronbach’s alpha was 0.74, indicating acceptable internal consistency.[21]
The category probability curve showed that average measure values advance with category, demonstrating that the higher patient performance corresponds to higher categories. The category mean-square fit statistics does not exceed the model values. Fig. 1 shows the modeled category probability curves and depicts the expected succession of “hills”. No reversal of categories was observed.
The person–item map [Fig. 2] showed that the two hardest visual function questions were Cb (satisfaction with vision/sight) (0.771) and C6 (reading subtitles on the television) (0.628). The two easiest visual function questions were C4 (seeing to walk on an uneven ground) (-0.783) and C2 (recognizing faces of people you meet) (-0.970).
Figure 2.
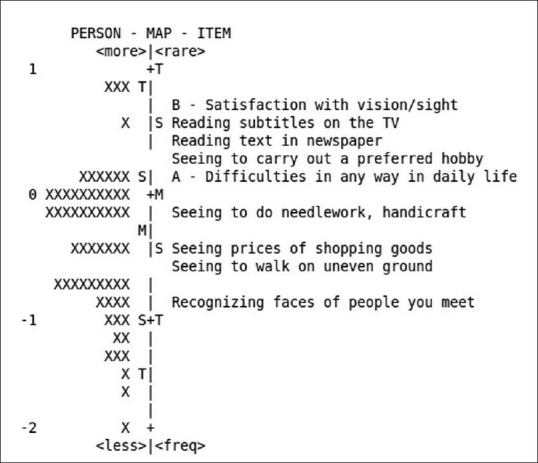
Person–item map for Catquest-9SF nine-item questionnaire (in logits). Patients who are less disabled (have higher visual functions) are at the bottom, and items that are more difficult (patients are more likely to rate having greater difficulties with tasks) are located at the top. Each ‘X’ represents 2 patient, S = 1 standard deviation, T = 2 standard deviation, and M = mean
Overall, there was a significant (P <.05) mean visual functioning improvement (16.3%) in all Catquest-9SF categories [Fig. 3] aside from the categories of ‘recognizing the face of the people you meet’ (C2, P =0.08) and ‘seeing to do needle or handicraft postoperatively’ (C5, P =0.07) [Tables 3 and 4]. Visual function was better both pre-operatively and post-operatively in patients who had already undergone surgery on one eye (bi-lateral group) compared to patients who had not undergone previous surgery (uni-lateral group).
Figure 3.
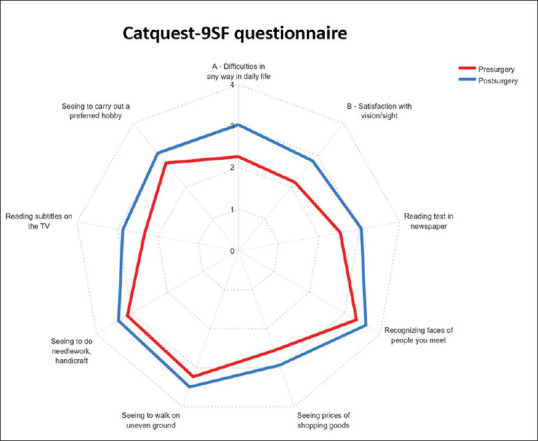
Radar plot of the Catquest-9SF nine-item questionnaire comparison between pre-cataract surgery (in red) and post-cataract surgery (in blue). 0 = no response, 1 = Yes, very great difficultly or very dissatisfied, 2 = Yes, great difficulty or fairly dissatisfied, 3 = Yes, some difficulty or fairly satisfied, 4 = No, no difficulty or very satisfied, 5 = cannot decide. *5 options (n = 3 patients) were excluded to obtain the best-fit graph
Table 3.
Pre-cataract surgery Catquest-9SF questionnaire responses
| Itema | 1 | 2 | 3 | 4 | 5 | Mean (SD) |
|---|---|---|---|---|---|---|
| A - Difficulties in any way in daily life | 12 | 28 | 14 | 7 | 0 | 2.26 (0.90) |
| B - Satisfaction with vision/sight | 16 | 26 | 13 | 6 | 0 | 2.15 (0.92) |
| Reading text in newspaper | 10 | 17 | 26 | 8 | 0 | 2.52 (0.92) |
| Recognizing faces of people you meet | 3 | 10 | 12 | 36 | 0 | 3.32 (0.91) |
| Seeing prices of shopping goods | 10 | 16 | 26 | 9 | 0 | 2.55 (0.93) |
| Seeing to walk on uneven ground | 2 | 6 | 29 | 24 | 0 | 3.22 (0.75) |
| Seeing to do needlework, handicraft | 6 | 11 | 19 | 22 | 3 | 3.08 (1.06) |
| Reading subtitles on the TV | 15 | 21 | 15 | 10 | 0 | 2.32 (1.01) |
| Seeing to carry out a preferred hobby | 9 | 13 | 23 | 16 | 0 | 2.75 (1.0) |
aResponse modalities: 1-Very dissatisfied, 2-Fairly dissatisfied, 3-Fairly satisfied, 4-Very satisfied, 5-Cannot decide. SD=standard deviation
Table 4.
Three months post-cataract surgery Catquest-9SF questionnaire responses
| Itema | 1 | 2 | 3 | 4 | 5 | Mean (SD) | Mean change (%)╪ | P |
|---|---|---|---|---|---|---|---|---|
| A - Difficulties in any way in daily life | 4 | 13 | 21 | 23 | 0 | 3.15 (0.44) | 28.3 | <.001 |
| B - Satisfaction with vision/sight | 6 | 19 | 16 | 20 | 0 | 2.84 (0.34) | 24.3 | <.001 |
| Reading text in newspaper | 1 | 14 | 27 | 19 | 0 | 3.05 (0.26) | 17.1 | 0.009 |
| Recognizing faces of people you meet | 0 | 8 | 9 | 44 | 0 | 3.59 (0.13) | 7.2 | 0.08 |
| Seeing prices of shopping goods | 4 | 12 | 29 | 16 | 0 | 3.49 (0.47) | 26.6 | <.001 |
| Seeing to walk on uneven ground | 0 | 4 | 23 | 34 | 0 | 3.49 (0.13) | 7.4 | 0.03 |
| Seeing to do needlework, handicraft | 2 | 7 | 24 | 25 | 3 | 3.33 (0.12) | 7.5 | 0.09 |
| Reading subtitles on the TV | 6 | 16 | 19 | 20 | 0 | 2.87 (0.27) | 18.9 | 0.003 |
| Seeing to carry out a preferred hobby | 4 | 12 | 21 | 24 | 0 | 3.07 (0.16) | 10.1 | 0.04 |
aResponse modalities: 1-Very dissatisfied, 2-Fairly dissatisfied, 3-Fairly satisfied, 4-Very satisfied, 5-Cannot decide. SD=standard deviation ╪Mean change=difference between pre-surgery responses and post-surgery responses. Higher score indicates better visual functioning. Total mean change of all 9 items=16.3%.
A significant (P <.05) mean visual function improvement was found in patients with bi-lateral cataract surgery compared with uni-lateral pre-operatively (22.3%) in seven categories (Ca, Cb, C1, C3, C5, C6, and C7) and post-operatively (10.1%) in four categories (Ca, C2, C6, and C7) [Table 2]. The overall mean visual functioning increased by 22% in uni-lateral patients and 10.4% in bi-lateral patients post cataract surgery. No significant differences between age, gender, or operated eye were observed.
Discussion
This prospective study concluded that Catquest-9SF was validated by Rasch analysis and showed good psychometric properties for measuring visual functioning in Australian cataract surgery patients. The questionnaire measured significant improvements in seven of nine categories for visual functions post cataract surgery, with the greatest improvements in questions that related vision satisfaction and activities that required reading. As the questionnaire had no mis-fits and demonstrated uni-dimensionality, Catquest-9SF may be used in the Australian population to assess visual functions post cataract surgery and as a clinical tool to triage surgeries and audit for patient-reported outcomes.
There was a significant improvement in visual function in both cohorts; however, bi-lateral cataract surgery patients had the highest scores in post-surgery surveys, and uni-lateral cataract patients saw larger mean improvements relative to the bi-lateral cohort (22% and 10.4%, respectively). Items with insignificant improvements had a higher baseline value pre-operatively, whereas items with a lower baseline value had significant improvements. For example, C3 (seeing prices of shopping goods) and Ca (difficulties in daily life) had the greatest improvements despite low initial scores, whereas C4 (seeing to walk on uneven ground) and C5 (seeing to do needlework, handicraft) showed the least improvement despite higher initial scores. This may be because improvements in items not previously associated with severe impairment are less likely to be subjectively noticed than those that interfered significantly with activities of daily living.[22] Moreover, seven of nine categories showed significant improvements in the uni-lateral cohort in comparison with the bi-lateral cohort, which just showed three categories [Table 2]. Patients who have undergone their second cataract surgery can be expected to have greater overall visual functioning; however, it is a concern that uni-lateral cataract surgery still leaves a patient with unsatisfying and disabling vision. The results on the Catquest-9SF provide feedback about the vision improvements that are appreciated by patients after the first and second cataracts and may help guide ophthalmologists when is best to schedule a second cataract in a uni-lateral cataract patient based on the patients’ needs.
Although Catquest-9SF showed great precision in the Australian population currently and in previous studies,[13] it still demonstrated some mis-targeting in our cohort. The two hardest visual functioning questions were Cb (satisfaction with vision/sight, 0.771) and C6 (reading sub-titles on the TV, 0.628), whereas the two easiest visual functioning questions were C2 (recognizing the faces of the people you meet, -0.970) and C4 (seeing to walk on uneven ground, -0.783).[23-25] Overall, the current study and previous Australian study did not exhibit the same degree of targeting compared with the Swedish cohort.[26] This may be explained by socio-economic and education factors as the patients recruited for this study were treated in a public health system with a low socio-economic catchment region.[27] This combined with poor vision may limit patient attitudes and ability to fill out the questionnaire accurately. Considering the questions themselves, in Australia, pedestrian areas are well maintained, and most media are from English-speaking companies, which may introduce redundancy in questions in C4 and C6. Despite mis-targeting of these questions, there were no instances of mis-fitting. This is in contrast with Chinese and Danish studies,[28,29] where studies only achieved good psychometric scoring once they completely omitted mis-fitted questions. Instances of mis-fitting have been attributed to ambiguous language translation and cross-cultural differences in activities of daily living and raise the concern that the Catquest-9SF may lead to mis-leading results if not adapted to a target cohort. Although mis-fitting was absent in our English-speaking cohort, future studies using Catquest-9SF in wider Australia where multi-ethnic cohorts exist should consider revising the questionnaire to accommodate for diverse population types.
These findings support previous studies which validate Catquest-9SF as an excellent tool for measuring visual functioning post cataract surgery.[13,30-32] Overall, the Rasch analysis of Catquest-9SF showed that it was a reliable and valid measure for assessing visual functions. Response categories were ordered, had high precision, had internal consistency, and were uni-dimensional (in-fit and out-fit ranges, 0.65–1.33 and 0.64–1.31, respectively). These results echo similar studies that show that Catquest-9SF accurately captures treatment effectiveness when analyzed with Rasch-based psychometric methods.[12,13,32,33,34,35] Its superiority over other alternatives such as the National Eye Institute Visual Function Questionnaire, electronic cataract appropriateness and priority systems and impacts on life questionnaires, and correlation with the newly developed cataract patient-reported outcome measure shows that it can be used as a routine clinical tool for satisfaction and visual functioning.[36]
The Catquest-9SF questionnaire accurately reported significant (P < 0.001) differences in satisfaction with vision and sight which can be an important clinical factor and auditing tool. Olawoye et al.[37] compared public and private patients’ satisfaction post cataract surgery and found that private patients had higher levels of satisfaction because of a shorter waiting time, better interaction with health care staff, and information they received. An Australian study revealed that the five most important decision-making attributes between private health care and public health care for cataract surgery were surgical wait time, cost, travel time, hospital reputation, and surgeon experience.[38] Furthermore, visual outcomes and satisfaction with vision and activities of daily living were better after cataract surgery in private hospitals compared to public health systems.[38] Because Catquest-9SF is able to accurately address visual functioning and visual satisfaction, it can be utilized as a comparison tool which may provide useful auditing information across health care providers or regions.[39]
The reported difference of visual functioning between patients who have had cataract surgery and patients who are currently waiting for another surgery may also support previous studies that indicate that Catquest-9SF can be a useful tool for community screening for cataract surgery or a decision-making tool for surgery prioritization.[28] Public systems are often limited, and clinical tools that accurately prioritize patients when hospitals may be under-staffed, under-resourced, or over-referred are valuable to clinicians. In the Illawarra region of Australia, there is currently a 12 months waiting period for cataract surgery which has further increased because of COVID-19 cancellation of elective surgeries at public hospitals.[40] Considering that worsening visual functioning is associated with high morbidity, using Catquest-9SF as an assistive decision-making tool would allow for people with the poorest visual functioning to be prioritized in public health systems.[30] In a Chinese cohort, a significant correlation between the Lens Opacities Classification System for cataract grading and Catquest-9SF scores was observed, indicating that the questionnaire also accurately reflected cataract severity and was considered as an excellent screening tool.[28] Lim et al.[41] also identified that Catquest-9SF scores were significantly improved when morbidity-related predictors such as safety, injury concerns, and ability to participate in daily activities were considered when prioritizing patients for surgery.
The current study is one of a few to assess the Catquest-9SF questionnaire and the first in an Australian population to validate its use for assessing visual functions in patients preceding and following uni-lateral and bi-lateral cataract surgery. This study is limited by not performing clinical visual function assessments such as visual acuity and not analyzing for significant coexisting eye diseases or systemic co-morbidities that may influence their reported visual functioning. Not initially administering Catquest-9SF to patients obtaining their second cataract surgery and only administering Catquest-9SF questionnaire as a visual functioning measure may also interfere with the generalizability of these results. Additionally, although Rasch analysis met validation criteria and the sample size was large enough for the analysis, ideally, a larger cohort would have been recruited for a higher-powered Rasch analysis and more reliable results. Last, this study only recruited English-speaking patients within the Illawarra region of Australia, which prevents its generalizability to multi-ethnic populations. A larger, multi-center study comparing Catquest-9SF against other visual function questionnaires may be useful in future.
Conclusion
The Catquest-9SF questionnaire demonstrated the individual value of cataract surgery on visual functioning and QoL. Patients with bi-lateral cataract surgery had higher visual functioning than uni-lateral cataract surgery post-operatively, but uni-lateral cataract surgery patients had greater overall visual functioning improvement. The Catquest-9SF questionnaire is a psychometrically robust instrument that may be used as routine clinical tool to assess visual functioning. Larger multi-ethnic, multi-center studies are needed to confirm its validity across different demographic groups.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rosen E. Cataract surgery is refractive surgery. J Cataract Refract Surg. 2012;38:191–2. doi: 10.1016/j.jcrs.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 2.Hamel JF, Sebille V, Le Neel T, Kubis G, Boyer FC, Hardouin JB. What are the appropriate methods for analyzing patient-reported outcomes in randomized trials when data are missing? Stat Methods Med Res. 2017;26:2897–908. doi: 10.1177/0962280215615158. [DOI] [PubMed] [Google Scholar]
- 3.Pascolini D, Mariotti SP. Global estimates of visual impairment:2010. Br J Ophthalmol. 2012;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 4.Health AIo, Welfare. Eye Health. In. Canberra:AIHW. 2021 [Google Scholar]
- 5.Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, et al. The Vf-14:An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–8. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- 6.Seth I, Bulloch G, Tan A, Thornell E, Agarwal S. Incidence of pseudophakic cystoid macular oedema post-cataract surgery in Illawarra Shoalhaven local health district, Australia. Biomed Hub. 2022;7:1–10. doi: 10.1159/000521053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott A, Smith RD. Keeping the customer satisfied:Issues in the interpretation and use of patient satisfaction surveys. Int J Qual Health Care. 1994;6:353–9. doi: 10.1093/intqhc/6.4.353. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence D, Brogan C, Benjamin L, Pickard D, Stewart-Brown S. Measuring the effectiveness of cataract surgery:The reliability and validity of a visual function outcomes instrument. Br J Ophthalmol. 1999;83:66–70. doi: 10.1136/bjo.83.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoenfelder T. Patient satisfaction:A valid indicator for the quality of primary care. Primary Health Care. 2012;2:e106. [Google Scholar]
- 10.Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care:Description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27:637–44. doi: 10.1016/0277-9536(88)90012-3. [DOI] [PubMed] [Google Scholar]
- 11.Yucelt U. An investigation of causes of patient satisfaction/dissatisfaction with physician services. Health Mark Q. 1995;12:11–28. doi: 10.1300/j026v12n02_03. [DOI] [PubMed] [Google Scholar]
- 12.Lundström M, Pesudovs K. Questionnaires for measuring cataract surgery outcomes. J Cataract Refract Surg. 2011;37:945–59. doi: 10.1016/j.jcrs.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Gothwal VK, Wright TA, Lamoureux EL, Lundström M, Pesudovs K. Catquest questionnaire:Re-validation in an Australian cataract population. Clin Exp Ophthalmol. 2009;37:785–94. doi: 10.1111/j.1442-9071.2009.02133.x. [DOI] [PubMed] [Google Scholar]
- 14.Pesudovs K, Burr JM, Harley C, Elliott DB. The development, assessment, and selection of questionnaires. Optom Vis Sci. 2007;84:663–74. doi: 10.1097/OPX.0b013e318141fe75. [DOI] [PubMed] [Google Scholar]
- 15.Pesudovs K, Gothwal VK, Wright T, Lamoureux EL. Remediating serious flaws in the national eye institute visual function questionnaire. J Cataract Refract Surg. 2010;36:718–32. doi: 10.1016/j.jcrs.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 16.Linacre JM. Winsteps®Rasch Measurement Computer Program User's Guide. Beaverton, Oregon: Winsteps.com; 2012. [Google Scholar]
- 17.Waterbury GT. Missing data and the rasch model:The effects of missing data mechanisms on item parameter estimation. J Appl Meas. 2019;20:154–66. [PubMed] [Google Scholar]
- 18.Wright B. Reasonable mean-square fit values. Rasch Meas Trans. 1994;8:370. [Google Scholar]
- 19.Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. ERIC. 1993 [Google Scholar]
- 20.Fitkov-Norris E, Yeghiazarian A. Validation of vark learning modalities questionnaire using rasch analysis. J Phys:Conf Ser. 2015;588:012048. [Google Scholar]
- 21.Xu Z, Wu S, Li W, Dou Y, Wu Ql. The Chinese Catquest-9SF:validation and application in community screenings. BMC Ophthalmol. 2018;18:77. doi: 10.1186/s12886-018-0743-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yotsukura E, Ayaki M, Nezu N, Torii H, Arai H, Sakatani K, et al. Changes in patient subjective happiness and satisfaction with cataract surgery. Sci Rep. 2020;10:1–8. doi: 10.1038/s41598-020-72846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schlenker MB, Minotti SC, Kabanovski A, Lim M, D'Silva C, Ma J, et al. Catquest-9SF questionnaire and eCAPS:Validation in a Canadian population. PLoS One. 2020;15:e0237788. doi: 10.1371/journal.pone.0237788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adnan TH, Mohamed Apandi M, Kamaruddin H, Salowi MA, Law KB, Haniff J, et al. Catquest-9SF questionnaire:Validation of Malay and Chinese-language versions using rasch analysis. Health Qual Life Outcomes. 2018;16:5. doi: 10.1186/s12955-017-0833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Visser MS, Dieleman M, Klijn S, Timman R, Lundström M, Busschbach JJV, et al. Validation, test-retest reliability and norm scores for the Dutch Catquest-9SF. Acta Ophthalmol. 2017;95:312–9. doi: 10.1111/aos.13287. [DOI] [PubMed] [Google Scholar]
- 26.Lundström M, Kugelberg M, Montan P, Nilsson I, Zetterberg M, Pesudovs K, et al. Catquest-9SF functioning over a decade–a study from the Swedish national cataract register. Eye Vis (Lond) 2020;7:1–10. doi: 10.1186/s40662-020-00220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NSW Government:Illawarra Shoalhaven district data profile. Census. 2017. [Last accessed on 2022 Jun 20]. Available from:https://facs-web.squiz.cloud/__data/assets/pdf_file/0004/725845/Illawarra-Shoalhaven-District-Data-Profile.pdf .
- 28.Nielsen E, Lundström M, Pesudovs K, Hjortdal J. Validation of Catquest-9 Sf in Danish:Developing a revised form of the Catquest-9 Sf–the Danish Catquest-7 Sf. Acta Ophthalmol. 2019;97:173–7. doi: 10.1111/aos.13921. [DOI] [PubMed] [Google Scholar]
- 29.Khadka J, Huang J, Chen H, Chen C, Gao R, Bao F, et al. Assessment of cataract surgery outcome using the modified Catquest short-form instrument in China. PLoS One. 2016;11:e0164182. doi: 10.1371/journal.pone.0164182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McAlinden C, Gothwal VK, Khadka J, Wright TA, Lamoureux EL, Pesudovs K. A head-to-head comparison of 16 cataract surgery outcome questionnaires. Ophthalmology. 2011;118:2374–81. doi: 10.1016/j.ophtha.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 31.Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires:Review and recommendations. Optom Vis Sci. 2013;90:720–44. doi: 10.1097/OPX.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 32.Harrer A, Gerstmeyer K, Hirnschall N, Pesudovs K, Lundström M, Findl O. Impact of bilateral cataract surgery on vision-related activity limitations. J Cataract Refract Surg. 2013;39:680–5. doi: 10.1016/j.jcrs.2012.11.028. [DOI] [PubMed] [Google Scholar]
- 33.Lin X, Li M, Wang M, Zuo Y, Zhu S, Zheng Y, et al. Validation of Catquest-9SF questionnaire in a Chinese cataract population. PLoS One. 2014;9:e103860. doi: 10.1371/journal.pone.0103860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lundström M, Llovet F, Llovet A, Del Pozo MM, Mompean B, González J-V, et al. Validation of the Spanish Catquest-9SF in patients with a monofocal or trifocal intraocular lens. J Cataract Refract Surg. 2016;42:1791–6. doi: 10.1016/j.jcrs.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 35.Katz G, Rouquette A, Lignereux F, Mourgues T, Weber M, Lundström M. Validity of the French version of Catquest-9SF and use of an electronic notepad for entering patient-reported outcome measures. Eye Vis (Lond) 2021;8:1–9. doi: 10.1186/s40662-021-00233-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li SS, Misra S, Wallace H, Hunt L, McKelvie J. Patient-reported quality of life for cataract surgery:Prospective validation of the 'Impact on Life'and Catquest-9SF questionnaires in New Zealand. N Z Med J. 2019;132:34–45. [PubMed] [Google Scholar]
- 37.Olawoye O, Ashaye A, Bekibele C, Ajuwon A. A comparative evaluation of patients satisfaction with cataract surgical services in a public tertiary and a private secondary eye care facilities in Nigeria. Ann Afr Med. 2012;11:157–62. doi: 10.4103/1596-3519.96877. [DOI] [PubMed] [Google Scholar]
- 38.Lundström M, Stenevi U, Thorburn W. Quality of life after first- and second-eye cataract surgery:Five-year data collected by the Swedish national cataract register. J Cataract Refract Surg. 2001;27:1553–9. doi: 10.1016/s0886-3350(01)00984-1. [DOI] [PubMed] [Google Scholar]
- 39.Gilbert C, Keay L, Palagyi A, Do VQ, McCluskey P, White A, et al. Investigation of attributes which guide choice in cataract surgery services in urban Sydney, Australia. Clin Exp Optom. 2018;101:363–71. doi: 10.1111/cxo.12653. [DOI] [PubMed] [Google Scholar]
- 40.Porter M. Non-Urgent elective surgery cancelled at all Sydney public hospitals from monday. [Last accessed on 2022 Feb 10]. Available from:https://www.theleader.com.au/story/7365023/elective-surgery-cancelled/
- 41.Lim ME, Minotti SC, D'Silva C, Reid RJ, Schlenker MB, Ahmed IK. Predicting changes in cataract surgery health outcomes using a cataract surgery appropriateness and prioritization instrument. PLoS One. 2021;16:e0246104. doi: 10.1371/journal.pone.0246104. [DOI] [PMC free article] [PubMed] [Google Scholar]


