Abstract
Purpose:
The purpose of this study was to diagnose CME with the help of optical coherence tomography (OCT) after uneventful cataract surgery to prevent visual deterioration.
Methods:
This study was conducted on 120 patients, who underwent manual small-incision cataract surgery with posterior chamber intra-ocular lens implantation. Follow-up was performed after the first week, sixth week, and 12th week post-operatively. Detailed examination was performed at each visit along with measurements of central macular thickness using OCT. Statistical analysis was performed using SPSS 22.0.
Result:
The mean age of the patients was 61.85 ± 11.41 years having female preponderance. The pre-operative mean best corrected visual acuity (BCVA) was found to be 0.05 ± 0.04, whereas the mean post-operative BCVA was found to be 0.65 ± 0.17 at the first week, 0.66 ± 0.17 at the sixth week, and 0.67 ± 0.17 at the 12th week follow-up. The post-operative mean macular thicknesses at the first week, sixth week, and 12th week post-operatively were documented to be 221.66 ± 8.49 μm, 224.60 ± 8.75 μm, and 219.17 ± 8.22 μm, respectively.
Conclusion:
A sub-clinical increase in macular thickness occurs even after uncomplicated cataract surgery. The maximum increase was observed after 6 weeks of surgery, which returns to near normal values within 3 months. Comparison of central macular thicknesses pre-operatively and post-operatively at the first week, sixth week, and 12th week suggests a significant correlation.
Keywords: Cystoid macular edema, pseudophakic, SICS
Cataract is globally a primary cause of preventable blindness. Cataract surgery is the most common surgery performed in the field of ophthalmology. Small-incision cataract surgery (SICS) and phaco-emulsification are most commonly performed cataract surgeries. Cystoid macular edema (CME) is one of the late complications that may lead to vision deterioration after any intra-ocular surgery if precautions are not taken adequately to avoid, diagnose, or treat it.[1]
SICS with implantation of an intra-ocular lens has been the preferred technique among cataract surgeons, especially beginners. SICS is precise, effective, and less time-consuming without maintenance demand of equipment.[2] Also, it has been proven to be safe and effective in all types and grades of cataract. It has been observed that SICS gives lesser post-operative astigmatism, better post-operative visual outcome, comfort, and faster rehabilitation than the conventional ECCE technique.[3] We can minimize the cylindrical error if we consider the keratometric values of cornea and induced astigmatism during the SICS; it can give nearly the similar outcome as that of phaco-emulsification.[4] However, some degree of macular damage, clinically demonstrable as macular edema, continues to occur even after uneventful cataract surgery.
The overall incidence of clinical CME after uneventful cataract surgery was 1.5%. Following SICS, the incidence of clinical CME was 2%, and that after phaco-emulsification was 1%.[5] Macular edema (ME) is defined as an abnormal increase of fluid volume in the macula. The anatomical process involves intra-cytoplasmic swelling of glial cells leading to cell swelling. Gradually, the fluid starts accumulating in inter-cellular spaces, invading retinal layers and leading to the formation of “cysts”.[6]
CME usually appears within 1–3 months after cataract surgery as either reduced visual acuity or changes on fluorescein angiography or optical coherence tomography (OCT). Most patients recover spontaneously, with full restoration of visual acuity within 6 months; however, it may take up to 1–2 years for complete resolution.[7]
Pseudophakic cystoid macular edema (PCME) (Irvine–Gass syndrome)[8] is a complication of cataract removal or other intra-ocular procedures. It is believed to be caused because of the release of pro-inflammatory mediators after surgical trauma, leading to the alteration of blood-ocular barrier.[9] Surgical trauma leads to release of prostaglandins, which causes a break in the blood-aqueous barrier,[10] with the resultant release of toxins and immune complexes. Prostaglandins pass through the vitreous into the posterior segment and result in outpouring of the serous fluid into Henle’s layer. Increased levels of prostaglandin E (PGE) and prostaglandin F2 (PGF2) have been demonstrated in patients with CME undergoing vitrectomy. The primary cause of CME is the leakage of fluid that is low in lipid and protein content from the peri-foveal capillaries into the extra-cellular spaces because of breakdown of the blood-retinal barrier.[11]
Out of all the patients undergoing uncomplicated cataract extraction, only 20% develop angiographically proven CME.[12] However, a clinically significant reduction in visual acuity is observed in about 1% of these eyes.[13] If complications occur during cataract extraction, such as posterior capsule rupture, vitreous loss, severe iris trauma, or vitreous traction at the wound, there is a significant increase in the incidence (up to 20%) of clinically apparent CME.[14] PCME can be defined as angiographical (seen on fluorescein angiography) or clinical (associated with decreased visual acuity) and is labeled as acute (within 6 months) or chronic (over 6 months).[15]
Macular edema can also be found in cases of diabetic retinopathy, age-related macular degeneration, venous occlusion, hypertensive retinopathy, central serous chorio-retinopathy, Irvin–Gass syndrome, pars planitis, uveitis and iridocyclitis, choroiditis, and retinitis pigmentosa.[16]
Macular edema (ME) can be assessed by a number of methods. Traditional methods include contact and non-contact slit lamp biomicroscopy using 60D/78D/90D, indirect ophthalmoscopy, fundus fluorescein angiography, and fundus stereo-photography. OCT has become an important tool in diagnosing and managing retinal disorders such as CME.[17] The aims and objectives of this research were to measure the incidence of CME after manual SICS using OCT. This study was conducted to diagnose and timely cure the CME in post-cataract surgery patients to prevent visual deterioration.
Methods
This prospective, hospital-based observational study was conducted on 120 patients attending the ophthalmology out-patient department of our hospital with a clinical diagnosis of cataract and willing for cataract surgery. The study was approved by the Ethical Committee of our college (Ref. No. MMC/IEC/2020/71). Informed and written consent was taken from all the participants. All patients underwent SICS with posterior chamber intra-ocular lens implantation. Any grade of cataract allowing OCT to measure central macular thickness and patients who underwent uneventful SICS with posterior chamber intra-ocular lens implantation were included in the study.
Patients having traumatic cataract, complicated cataract, any complication during surgery, any retinal or posterior segment pathology, glaucoma, uveitis, previous history of intra-ocular surgery in the same eye, and uncontrolled hypertension/diabetes were excluded from the study.
Follow-up was performed after the first week, sixth week, and 12th week post-operatively. Visual acuity, slit lamp examination, fundus evaluation, and intra-ocular pressure were recorded at each visit along with measurements of central macular thickness with OCT (macula line). Findings were statistically analyzed using SPSS22.0. Data comparisons were made by using paired t-test.
Results
The age of the patients ranged between 40 and 98 years with the mean age being 61.85 ± 11.41 years having 59.17% females and 40.83% males. Right eyes were operated in 62 patients (51.67%), and left eyes were operated in 58 patients (48.33%).
The mean surgical time was 10.50 ± 1.67 minutes. Pre-operative and post-operative best corrected visual acuities (BCVAs) were recorded by Snellen’s chart and converted into decimal values. Pre-operative, PL-positive patients were taken as 0. The pre-operative mean BCVA was found to be 0.05 ± 0.04, whereas the post-operative mean BCVA was found to be 0.65 ± 0.17 at the first week, 0.66 ± 0.17 at the sixth week, 0.67 ± 0.17 at the 12th week follow-up [Fig. 1].
Figure 1.
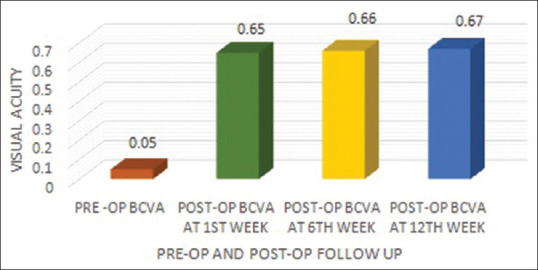
Comparison of best-corrected pre- and post-operative visual acuity. Mean visual acuity at different durations
The pre-operative and post-operative mean macular thicknesses at different follow-up are mentioned in the graph [Fig. 2] in the operated eyes of patients who underwent cataract surgery.
Figure 2.
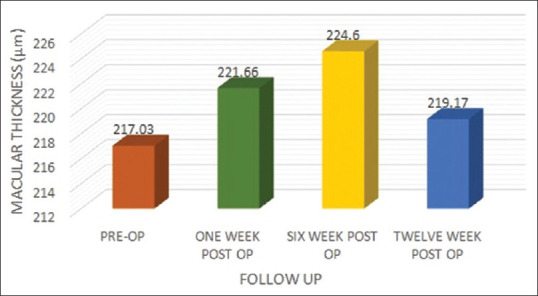
Mean macular thickness at different durations
The pre-operative mean macular thickness was compared with the mean macular thickness at 1 week, 6 weeks, and 12 weeks post-operative follow-up using paired t-test and was found to be a statistically significant P value (<0.00001). The maximum macular edema was observed at the sixth week review, and the minimum was found at 12 weeks follow-up [Table 1].
Table 1.
Comparison between pre-operative and 1 week, 6 week, and 12 week post-operative macular thicknesses
| Paired Differences | T | Df | Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Mean Difference | Std. Deviation | Std. Error of the Mean | 95% Confidence Interval of the Difference | One-Sided p | Two-Sided p | ||||
|
| |||||||||
| Lower | Upper | ||||||||
| Pre-operative - 1-week post- operative macular thickness | -4.63 | 2.72534 | 0.248 | -5.12 | -4.14 | 18.624 | 119 | <0.001 | <0.001 |
| Pre-operative - 6 weeks post- operative macular thickness | -7.175 | 3.518 | 0.321 | -7.81 | -6.53 | 22.338 | 119 | <0.001 | <0.001 |
| Pre-operative - 12 weeks post- operative macular thickness | -2.14 | 1.46 | 0.134 | -2.40 | -1.87 | 15.977 | 119 | <0.001 | <0.001 |
Statistical analysis of the differences between mean pre-operative and mean post-operative values of macular thickness at different follow-up was found to be statistically significant (p value = <0.00001) [Tables 2 and 3]. CME was not noted in any of the patients during any of the follow-up in the current study.
Table 2.
Comparison between 1 week post-operative and sixth and 12th week post-operative macular thicknesses
| Paired Differences | T | df | Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Mean Difference | Std. Deviation | Std. Error of the Mean | 95% Confidence Interval of the Difference | One-Sided p | Two-Sided p | ||||
|
| |||||||||
| Lower | Upper | ||||||||
| One-week post-operative macular thickness - 6-week post- operative macular thickness | -2.54 | 1.65 | 0.151 | -2.84 | -2.24 | 16.776 | 119 | <0.001 | <0.001 |
| One week post-operative and 12th week post-operative macular thickness | 2.491 | 2.45975 | 0.22454 | 2.04705 | 2.9628 | 11.097 | 119 | <0.001 | <0.001 |
Table 3.
Comparison between pre-operative and 1 week, 6 week, and 12 week post-operative macular thicknesses
| Macular Thickness (µm) | t | P |
|---|---|---|
| Pre-operative and post-operative 1 week | 18.624 | <0.00001 |
| Pre-operative and post-operative 6 weeks | 22.338 | <0.00001 |
| Pre-operative and post-operative 12 weeks | 15.977 | <0.00001 |
Discussion
Following cataract surgery, sub-clinical changes may occur in macular thickness with or without the visual acuity being affected. However, PCME is a known complication of cataract surgery, manifesting as effusion of the fluid from the capillaries. Although this phenomenon is most often self-limiting, culminating in spontaneous resolution, it occasionally leads to marked impairment of central vision, which may become chronic or permanent. In this study, an attempt was made to determine alterations in BCVA and macular thickness in patients undergoing SICSs.
The World Health Organization estimates that the current global prevalence of preventable blindness in the world population is 1 billion, with the majority of all blindness occurring in individuals aged 50 and older, predominantly because of cataract (94 million).[18]
The age of the patients ranged from 40 to 98 years with the mean age being 61.85 ± 11.41 years in this study. It was observed that 36.67% of patients were in the age group of 60–70 years, followed by 27.5% in the age group of 50–60 years (which was similar to the studies conducted by Dr. Vimal J. Vyas et al.[19] and Dr Shreya Bhargava et al.)[20] A different age distribution was noted with the study conducted by Dr. Abhishek Salwan et al.[21]
The majority of the enrolled patients were females, that is, 59.17%, versus males contributing 40.83%. Right eyes were operated in 62 patients (51.67%), and the left eyes were operated in 58 patients (48.33%).
The mean surgical time was found to be 10.50 ± 1.66 minutes, which was comparable to that of the study conducted by Dr. Shaik Nasreen et al.,[22] quoting a mean surgical time of 9.8 ± 0.50 (9.5 to 10.2) minutes.
The post-operative mean BCVA was found to be 0.65 ± 0.17 at the first week, 0.66 ± 0.17 at the sixth week, and 0.67 ± 0.17 at the 12th week follow-up.
In the study conducted by Jagow B et al.,[23] Cagini et al.,[24] Sandeep K et al.,[25] and Nasreen et al.,[22] there was no correlation found between macular thickening and visual acuity.
In 120 patients who underwent cataract surgery in our study, the pre-operative macular thickness noted was 217 ± 7.97 mm, but Salwan A et al.[21] and Bhargava et al.[20] documented pre-operative macular thicknesses of 223.38 ± 12.61 μm and 230.49 ± 14.42 μm, respectively, in their studies. The study performed by Sharma S[26] reported that the mean macular thickness was 189.34 mm, which was quite less as compared to our study.
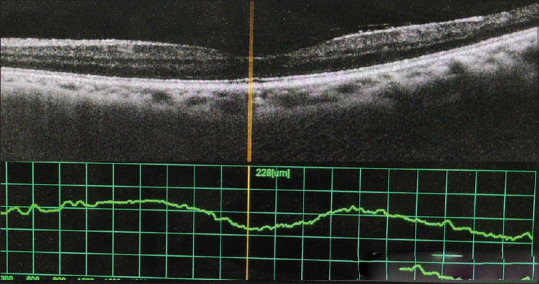
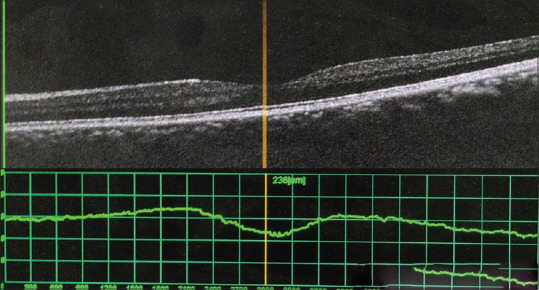
In our study, the post-operative mean macular thickness at the first week, sixth week, and 12th week was documented to be 221.66 ± 8.49 μm, 224.60 ± 8.75 μm, and 219.17 ± 8.22 μm, respectively [Figs. 3-5]. A study conducted by Salwan A et al.[21] found the mean macular thickness at 1 week post-operatively to be 238.28 ± 12.29 μm and that at the 12th week post-operatively to be 227.04 ± 12.58 μm, which was slightly higher as compared to ours.
Figure 3.
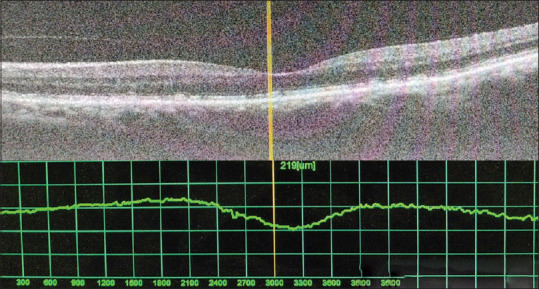
Pre-operative central macular thickness
Figure 5.
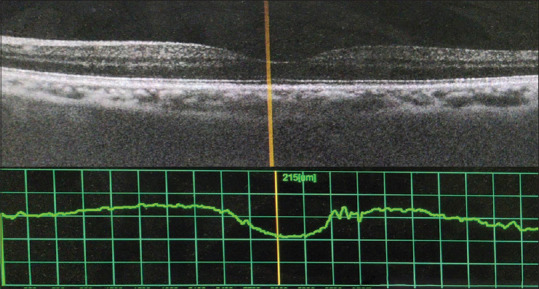
Central macular thickness at 12 weeks
Figure 4.
Central macular thickness at 6 weeks
The study performed by Bhargava et al.[20] also documented that the mean macular thickness at post-operative 1 week to be 235.43 ± 14.87 μm, that at post-operative 6 weeks to be 239.1 ± 14.86 μm, and that at post-operative 12 weeks to be 233.31 ± 15.97 μm, which was corroborating with the findings of Salwan A et al.[21] The differences between pre-operative and post-operative macular thicknesses in the studies conducted by Salwan A et al.[21] and Bhargava et al.[20] were nearly similar to our findings.
A total of three patients had a floppy iris, and two had excessive bleed during surgery because of HCV positivity, which extended the operation time. The mean surgical time in these patients was 16.8 minutes [Fig. 6]. The mean macular thickness was found to be higher in these cases as compared to the other patients, that is, 231.4 μm at the first week, 237.8 μm at the sixth week, and 221 μm at the 12th week. These above-mentioned patients were excluded from this study as they were not fulfilling the inclusion criteria, that is, uneventful surgery. Ramakrishnan et al.[27] studied the correlation between the duration of surgery and the increase in macular thickness and confirmed our observation that the patients who had a longer duration of surgery showed an increased central macular thickness.
Figure 6.
Increased central macular thickness in a patient with increased mean surgical duration
Conclusion
Comparisons between pre-operative central macular thickness and post-operative central macular thickness after 1 week, 6 weeks, and 12 weeks suggest a significant correlation. A sub-clinical increase in macular thickness occurs after uncomplicated cataract surgery having a peak by 6 weeks after surgery, which returns to the near normal value by 12th week post-operatively. OCT showed an increase in macular thickness without altering the architecture of the macula. There was no correlation established between the BCVA and macular edema post-operatively. A positive correlation was observed between surgical time and an increase in central macular thickness in our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ho TT, Kaiser R, Benson WE. Retinal complications of cataract surgery. Compr Ophthalmol Update. 2006;7:1–10. [PubMed] [Google Scholar]
- 2.Gogate P, Deshpande M, Nirmalan PK. Why do phacoemulsification?Manual small-incision cataract surgery is almost as effective, but less expensive. Ophthalmology. 2007;114:965–8. doi: 10.1016/j.ophtha.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 3.Minassian DC, Rosen P, Dart JK, Reidy A, Desai P, Sidhu M, et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification:A randomised trial. Br J Ophthalmol. 2001;85:822–9. doi: 10.1136/bjo.85.7.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gogate P, Kulkarni S, Krishnaiah S, Deshpande R, Joshi S, Palimkar A, et al. Safety and efficacy of phacoemulsification compared with manual small-incision cataract surgery by a randomized controlled clinical trial six-week results. Ophthalmology. 2005;112:869–74. doi: 10.1016/j.ophtha.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhary C, Bahadhur H, Gupta N. Study of cystoid macular edema by optical coherent tomography following uneventful cataract surgery. Int Ophthalmol. 2015;35:685–91. doi: 10.1007/s10792-014-9998-5. [DOI] [PubMed] [Google Scholar]
- 6.Yanoff M, Fine BS, Brucker AJ, Eagle RC., Jr Pathology of human cystoid macular edema. Surv Ophthalmol. 1984;28:505–11. doi: 10.1016/0039-6257(84)90233-9. [DOI] [PubMed] [Google Scholar]
- 7.Yanoff M, Duker J. Ophthalmology. 5th ed. Edinburgh: Mosby; 2008. [Google Scholar]
- 8.Irvine SR. A newly defined vitreous syndrome following cataract surgery, interpreted according to recent concepts of the structure of the vitreous. Am J Ophthalmol. 1953;36:599–619. doi: 10.1016/0002-9394(53)90302-x. [DOI] [PubMed] [Google Scholar]
- 9.Andrzej G, Kels BD, Grant-Kels JM. Eye and skin disorders:Part II:Ocular signs that help in diagnosis of systemic diseases in dermatology practice. Clin Dermatol. 2016;34:121–3. doi: 10.1016/j.clindermatol.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Kaiya T. Observation of blood-aqueous barrier functions after posterior chamber intraocular lens implantation. J Cataract Reftract Surg. 1990;16:320–24. doi: 10.1016/s0886-3350(13)80702-x. [DOI] [PubMed] [Google Scholar]
- 11.Gass JD, Norton EW. Cystoid macular edema and papilloedema of cataract extraction-a fluorescein funduscopic study. Arch Ophthalmol. 1977;76:81–8. doi: 10.1001/archopht.1966.03850010648005. [DOI] [PubMed] [Google Scholar]
- 12.Peterson M, Yoshizumi MO, Hepler R, Mondino B, Kreiger A. Topical indomethacin in the treatment of chronic cystoid macular edema. Graefes Arch Clin Exp Ophthalmol. 1992;230:401–5. doi: 10.1007/BF00175922. [DOI] [PubMed] [Google Scholar]
- 13.Bergman M, Laatikainen L. Cystoid macular oedema after complicated cataract surgery and implantation of an anterior chamber lens. Acta Ophthalmol (Copenh) 1994;72:178–80. doi: 10.1111/j.1755-3768.1994.tb05013.x. [DOI] [PubMed] [Google Scholar]
- 14.Bradford JD, Wilkinson CP, Bradford RH., Jr Cystoid macular edema following extracapsular cataract extraction and posterior chamber intraocular lens implantation. Retina. 1988;8:161–4. doi: 10.1097/00006982-198808030-00001. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Belair M-L, Bressler NM, Dunn JP, Thorne JE, Kedhar SR, et al. Amethod of reporting macular edema after cataract surgery using optical coherence tomography. Retina. 2008;28:870–76. doi: 10.1097/IAE.0b013e318169d04e. [DOI] [PubMed] [Google Scholar]
- 16.Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE. Macular edema. Surv Ophthalmol. 2004;49:470–90. doi: 10.1016/j.survophthal.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Huang D, Swanson EA, Lin CP, Schumann JS, Stinson WG, Chang W, et al. Optical coherence tomography. Science. 1991;254:1178–81. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. [Last accessed on 2022 Mar 22];Vision impairment and blindness. Who.int. 2022. [Google Scholar]
- 19.Vyas VJ, Matai HD. Analysis of macular thickness by optical coherence tomography (OCT) after 1 month in post-operative patients of cataract surgery. Int J Sci Res. 2018;7:951–4. [Google Scholar]
- 20.Bhargava S, Devendra J. Study of change in macular thickness pre and post small incision cataract surgery and its correlation with Best corrected visual acuity. IOSR J Dental Med Sci (IOSR-JDMS) 2021;20:09–14. [Google Scholar]
- 21.Salwan A, Singh S. A study to assess the macular thickness and visual outcome before and after cataract surgery. Int Surg J. 2021;8:1747–53. [Google Scholar]
- 22.Nasreen S, Sudha R. Study of changes in macular thickness following uneventful cataract surgery. Indian J Clin Exp Ophthalmol. 2020;6:629–32. [Google Scholar]
- 23.von Jagow B, Ohrloff C, Kohnen T. Macular thickness after uneventful cataract surgery determined by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2007;245:1765–71. doi: 10.1007/s00417-007-0605-6. [DOI] [PubMed] [Google Scholar]
- 24.Cagini C, Fiore T, Iaccheri B, Piccinelli F, Ricci M, Fruttini D. Macular thickness measured by optical coherence tomography in a healthy population before and after uncomplicated cataract phacoemulsification surgery. Curr Eye Res. 2009;34:1036–41. doi: 10.3109/02713680903288937. [DOI] [PubMed] [Google Scholar]
- 25.Sandeep K, Bhadbhade K. Irvin-gass syndrome following phacoemulsification and small incision cataract surgery:A comparitive study. Indian J Clin Exp Ophthalmol. 2020;4:152–6. [Google Scholar]
- 26.Sharma S. Comparison of central macular thickness after SICS (Small Incision Cataract Surgery) and phacoemulsification cataract surgery using OCT (Optical Coherence Tomography) Int J Sci Res. 2019;16:2319–22. [Google Scholar]
- 27.Ramakrishnan R, Shrivastava S. Comparison of central macular thickness after SICS and phacoemulsification cataract surgery, using Oct. Int J Opthomology Res. 2019;1:9–12. [Google Scholar]


