Abstract
Otosyphilis can be challenging to diagnose, but, if left unrecognized, it may cause irreversible damage. An immunologic interplay between syphilis and human immunodeficiency virus (HIV) makes coinfection likely and may predispose people with HIV to neurosyphilis. In this study, we present a case of a man in his 50s with hearing loss and vertigo diagnosed with otosyphilis as well as a new diagnosis of HIV. This case and corresponding discussion serve to inform the noninfectious disease-trained clinician of the symptoms, diagnostics, and treatment options for otosyphilis as well as to discuss the relationship between HIV and syphilis and demonstrate the importance of disease recognition.
Keywords: HIV, otosyphilis, syphilis
Syphilis is a sexually transmitted infection (STI) or congenitally acquired disease caused by the Treponema pallidum subspecies pallidum. The “great imitator”, syphilis can have varied clinical presentations including genital ulceration (painful or painless), rash, neurologic dysfunction (cerebral vascular accident, meningitis), and stillbirth [1]. Some of the most debilitating consequences of infection include neurological manifestations that can occur at any time, even years to decades after the initial infection. Prior studies report an increased risk of neurosyphilis in persons with HIV (PWH), especially in those with low CD4 counts and not on antiretroviral therapy (ART) [2, 3].
Otosyphilis is a less common form of neurosyphilis whereby inflammation of the vestibulocochlear nerve, cochleovestibular apparatus, and/or temporal bone may cause sensorineural hearing loss (SNHL) and/or vertigo [1]. Otosyphilis is often challenging to diagnose, because it can present without other symptoms classically associated with syphilis. The recommended treatment regimen for neurosyphilis in the United States is intravenous (IV) penicillin G. In this study, we describe a case of a delayed diagnosis of otosyphilis with a concurrent new diagnosis of HIV that illustrates this important and often misdiagnosed disease.
CASE
A 57-year-old man with a history of hypertension, type II diabetes, and no history of STIs presented with a 2-month history of sudden onset bilateral hearing loss and 1 week of vertigo. He was recently married and denied sex with men or transactional sex. He was evaluated by an otolaryngologist who noted bilateral SNHL. The initial differential diagnosis included exposure to ototoxic drugs, infection, neoplasm, autoimmune disease, vasculitis, or trauma. An magnetic resonance image revealed asymmetric abnormal enhancement of the cochlea and the vestibule and abnormal focal enhancement in the left internal auditory canal. He started prednisone without symptom improvement. Laboratory workup revealed negative antinuclear antibody, antineutrophil cytoplasmic antibodies, and anti-Sjogren’s Syndrome (SS)A/SSB antibodies and hepatitis serologies. Due to lack of improvement with steroids, additional testing was performed. Serum rapid plasma reagin titer was 1:128 with confirmatory treponemal serology.
He was admitted to the hospital for initiation of IV penicillin G for otosyphilis. Subsequent discussions revealed that he had previously had sex with men, although considered himself heterosexual. A lumbar puncture was performed, and cerebrospinal fluid (CSF) studies showed a white blood cell count of 14 cells/mL with elevated protein of 116 mg/dL and a reactive Venereal Disease Research Laboratory (VDRL) at 1:16. Cerebrospinal fluid polymerase chain reaction testing for herpes simplex virus and varicella-zoster virus was negative. Further evaluation revealed a positive fourth-generation HIV antigen/antibody test, HIV-1 ribonucleic acid 54 900 copies/mL, and CD4 cell count of 631 cells/dL. Treatment was initiated for otosyphilis with penicillin G IV 24 million units daily for 14 days, and he was started on anti-retroviral therapy.
Upon follow-up 1 month later, the patient noted improvement in vertigo and left-sided hearing loss but had continued right-sided hearing loss. Human immunodeficiency virus viral load was undetectable within 3 months. A hearing aid provided improvement in hearing, but he required intermittent treatment with meclizine for vertigo.
Patient Consent Statement
The patient involved in this case has provided consent for publication. This publication complies with the requirements set forth by the Emory University Institutional Review Board.
DISCUSSION
Bacteriology of Syphilis
Treponema pallidum enters the body through breaks in the skin or mucosa. It can cause local infection and disseminate to other organs including the central nervous system (CNS) [1]. Although macrophages will phagocytose and kill some spirochetes, many disseminated bacteria persist causing immune activation and latent infection [4, 5]. It is this prolonged infection and maladaptive immune response that contribute to the symptoms associated with secondary syphilis and neurosyphilis.
Immunologic Interplay Between Human Immunodeficiency Virus and Syphilis
Human immunodeficiency virus and syphilis have multiple synergistic interactions from acquisition to disease progression. Syphilitic ulcers can increase the risk of HIV transmission 2- to 9-fold [6], and the inflammation associated with syphilis can increase immune activation in the genitalia leading to higher likelihood of HIV uptake into responding CD4 cells, resulting in increased risk of acquisition estimated to be 2 to 4 times higher [7–9]. Human immunodeficiency virus depresses the immune response, specifically CD4 cells, causing suboptimal clearance of treponemes. This ineffective immune activation likely contributes to increased risk of syphilis dissemination in PWH [3, 5, 10].
Transmission and Epidemiology of Syphilis
Syphilis is acquired by direct contact with T pallidum. The average incubation period from exposure is 3 weeks (range 3 days to 3 months) and may depend on inoculum size [11, 12]. Congenital syphilis can occur in utero but can also be acquired during vaginal delivery if there are lesions present within the birth canal.
Men who have sex with men are disproportionately affected, compromising 53% of male primary and secondary syphilis cases in the United States; however, rates in women have increased 147% between 2016 and 2020, suggesting that heterosexual sex is an increasingly frequent mode of transmission [13]. Persons diagnosed with syphilis should also have testing for HIV, gonorrhea, and chlamydia [6], and they should be offered pre-exposure prophylaxis for HIV if negative [14].
Clinical Manifestations of Syphilis
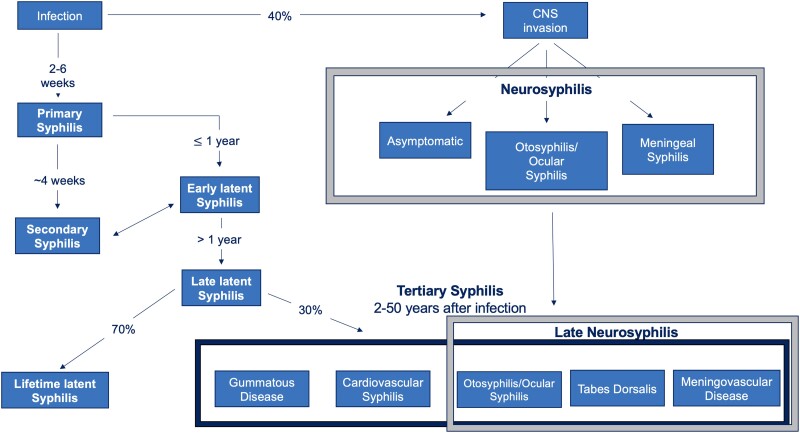
Syphilis can be divided into clinical stages (Figure 1). These include primary syphilis, classically a painless chancre at the site of infection, followed by secondary syphilis, characterized by a disseminated rash or end-organ infection that can involve the kidney, liver, or others. Primary and secondary syphilis presentations may overlap in PWH [10]. Tertiary syphilis, a rare sequela of prolonged infection, can involve aortic inflammation, CNS gummas, or tabes dorsalis. Neurosyphilis, which can present as meningitis, stroke, ocular or otic manifestations, can occur in any stage of infection and without any other associated symptoms [14]. Asymptomatic latent syphilis occurs between stages of syphilis and has no clinical manifestations.
Figure 1.
Syphilis stages. From Ghanem, Ram, and Rice [18]. Copyright © 2020. Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society. CNS, Central Nervous System.
Otosyphilis
Otosyphilis can occur at any stage of infection and independently of other manifestations [14]. Symptoms of otosyphilis include bilateral or unilateral hearing loss, tinnitus, or vestibular abnormalities such as vertigo, imbalance, and gait instability [1]. The changes associated with otosyphilis are often present for weeks to decades at diagnosis. Patients may experience gradual loss of vestibular function leading to ataxia and gait abnormalities without treatment.
Diagnosing Otosyphilis
The diagnosis of otosyphilis can be challenging given the wide differential for SNHL and vertigo including noise-induced injury, presbycusis, medication toxicity, and systemic inflammatory conditions such as diabetes, autoimmune disease, or infection. Many persons with otosyphilis may initially receive alternative diagnoses [15] despite rates of otosyphilis being as high as 653 per 100 000 of those seeking care for auricular complaints [16]. The diagnosis of otosyphilis must be considered with a compatible clinical syndrome and concordant serologic tests for syphilis.
Syphilis Serologic Testing
Serologic testing for syphilis should include both treponemal and nontreponemal serological tests (Table 1) [14]. Treponemal tests directly identify treponeme-associated proteins, whereas nontreponemal tests detect antibodies directed against lipoidal antigens when T pallidum is present. As expected, the less specific nontreponemal tests are subject to false-positive results associated with certain conditions such as autoimmune disorders and can vary in sensitivity depending on the stage of disease. False-negative serologic testing may occur in persons with humoral immunodeficiencies. Nontreponemal tests are advantageous because they provide a quantitative result, which can be used for monitoring serologic response after treatment. Treponemal tests may remain detectable lifelong, making their interpretation difficult in persons with prior infections or treatment [14]. In some PWH, interpretation of diagnostic tests can be challenging, because HIV can be associated with false-positive nontreponemal tests [17], and for some PWH nontreponemal titers may decline more slowly or remain high for long durations [14].
Table 1.
Treponemal and Nontreponemal Syphilis Tests
| Treponemal Tests | Nontreponemal Tests |
|---|---|
| Treponema pallidum enzyme immunoassay | Rapid plasma reagin |
| T pallidum particle agglutination assay | Venereal Disease Research Laboratory |
| Chemiluminescence immunoassay | Toluidine Red Unheated Serum Test |
| Microhemagglutination test for antibodies to T pallidum | |
| Fluorescent treponemal antibody absorption |
Otosyphilis and Cerebrospinal Fluid Testing
Among persons with positive syphilis serologic testing and isolated auditory symptoms, CSF evaluation is usually normal and not recommended before treatment [14]. However, if lumbar puncture is performed in the evaluation of otosyphilis in PWH, CSF leukocyte count, protein, and VDRL should be obtained. Cerebrospinal fluid interpretation can be challenging because HIV can also cause an elevated CSF leukocyte count [19].
Follow-up Testing
Follow up after treatment is important for monitoring of symptoms and serologic improvement. Nontreponemal testing in persons with early syphilis and HIV should be performed every 3 months until clinical and serologic response is achieved. A 4-fold decrease in nontreponemal titers within 12 months indicates successful serologic response [14]. Persons with inadequate serologic response should receive additional clinical and serologic evaluation because this may indicate treatment failure. Despite treatment, patients with otosyphilis may not return to their baseline audiologic function.
Otosyphilis Treatment
The Centers for Disease Control and Prevention (CDC) STI treatment guidelines recommend aqueous crystalline penicillin G (PCN G) 18–24 million units per day for 10–14 days for otosyphilis [14]. If compliance can be ensured, an alternative regimen of procaine PCN G 2.4 million units intramuscularly (IM) once daily plus probenecid 500 mg orally 4 times a day, both for a duration of 10–14 days, may be considered [14]. For nonpregnant persons with a penicillin allergy, ceftriaxone 2 g daily (either IM or IV) for duration of 10–14 days can be considered as an alternative regimen based on limited data per CDC guidelines [14]. If concerns exist regarding ceftriaxone safety, penicillin allergic patients should undergo skin testing to confirm the allergy and can consider penicillin desensitization followed by treatment with IV penicillin [14].
Adjunctive systemic steroids have been used for otosyphilis with some reports of improvement in hearing [15]; however, they were not proven to be effective in controlled studies [20]. Current treatment guidelines do not recommend systematic steroids as adjunctive treatment for otosyphilis given that data on efficacy are limited [14]. In PWH and syphilis, ART has been shown to reduce likelihood of serologic failure and should be promptly initiated [2].
CONCLUSIONS
Otosyphilis can be challenging to diagnose, it can cause debilitating manifestations, and it should be considered when patients present with new onset SNHL and/or vertigo. Treatment should be promptly initiated with guideline-based therapy, and STI testing, specifically HIV, should be performed.
Acknowledgments
We acknowledge the contribution of Malia Willis to the initial preparation of the case report along with Ahmed Babiker and Wendy Armstrong for their help and guidance.
Author contributions. All authors approve of and contributed to this manuscript.
Financial support. LSW and AWF are funded by in part by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Numbers UL1TR002378 and TL1TR002382. This work was funded by NIH Grant Number Al158080.
Contributor Information
Lucy S Witt, Division of Infectious Diseases, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
A Wendy Fujita, Division of Infectious Diseases, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
Jeanne Ho, Division of General Internal Medicine and Geriatrics, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
Yoo Mee Shin, Division of Hospital Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
Ketino Kobaidze, Division of Hospital Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
Kimberly Workowski, Division of Infectious Diseases, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, USA.
References
- 1. Ramchandani MS, Litvack JR, Marra CM. Otosyphilis: a review of the literature. Sex Transm Dis 2020; 47:296–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ghanem KG, Moore RD, Rompalo AM, Erbelding EJ, Zenilman JM, Gebo KA. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS 2008; 22:1145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johns DR, Tierney M, Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immunodeficiency virus. N Engl J Med 1987; 316:1569–72. [DOI] [PubMed] [Google Scholar]
- 4. Lukehart SA, Hook EW, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med 1988; 109:855–62. [DOI] [PubMed] [Google Scholar]
- 5. Carlson JA, Dabiri G, Cribier B, Sell S. The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity. Am J Dermatopathol 2011; 33:433–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pathela P, Braunstein SL, Blank S, Shepard C, Schillinger JA. The high risk of an HIV diagnosis following a diagnosis of syphilis: a population-level analysis of New York City men. Clin Infect Dis 2015; 61:281–7. [DOI] [PubMed] [Google Scholar]
- 7. Dickerson MC, Johnston J, Delea TE, White A, Andrews E. The causal role for genital ulcer disease as a risk factor for transmission of human immunodeficiency virus: an application of the Bradford Hill criteria. Sex Transm Dis 1996; 23:429–40. [DOI] [PubMed] [Google Scholar]
- 8. Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999; 75:3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chesson HW, Pinkerton SD, Voigt R, Counts GW. HIV infections and associated costs attributable to syphilis coinfection among African Americans. Am J Public Health 2003; 93:943–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zetola NM, Engelman J, Jensen TP, Klausner JD. Syphilis in the United States: an update for clinicians with an emphasis on HIV coinfection. Mayo Clin Proc 2007; 82:1091–102. [DOI] [PubMed] [Google Scholar]
- 11. Hook EW. Diagnosing neurosyphilis. Clin Infect Dis 1994; 18:295–7. Available at: https://www.jstor.org/stable/4457682 [DOI] [PubMed] [Google Scholar]
- 12. French P. Syphilis. BMJ 2007; 334:143–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2020—syphilis. Available at: https://www.cdc.gov/std/statistics/2020/overview.htm#syphilis. Accessed November 3, 2022.
- 14. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021; 70:1–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bradshaw D, Pallawela S, Nelson M, Scott C, Day S. Otosyphilis: missed opportunities for early treatment? Sex Transm Infect 2012; 88:573. [DOI] [PubMed] [Google Scholar]
- 16. Abuzeid WM, Ruckenstein MJ. Spirochetes in otology: are we testing for the right pathogens? Otolaryngol Head Neck Surg 2008; 138:107–9. [DOI] [PubMed] [Google Scholar]
- 17. Tuddenham S, Ghanem KG. Emerging trends and persistent challenges in the management of adult syphilis. BMC Infect Dis 2015; 15:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med 2020; 382(9):845–54. [DOI] [PubMed] [Google Scholar]
- 19. Marra CM. Neurosyphilis. Curr Neurol Neurosci Rep 2004; 4:435–40. [DOI] [PubMed] [Google Scholar]
- 20. Yimtae K, Srirompotong S, Lertsukprasert K. Otosyphilis: a review of 85 cases. Otolaryngol Head Neck Surg 2007; 136:67–71. [DOI] [PubMed] [Google Scholar]