Abstract
Background
There is a scarcity of data on the effects of duration of bathing and cutaneous properties.
Aims
This study aimed to investigate the changes of capacitance and transepidermal water loss (TEWL) after soaking in water for the different durations.
Method
This experimental biophysical study included healthy volunteers whose forearms were randomized to receive 3, 5, 10, 15, or 20 min of soaking of the volar aspect of the forearm. Skin hydration and integrity were assessed capacitance and TEWL measurement before and after soaking.
Results
Sixty‐five subjects (130 forearms) were enrolled with an average age of 33 ± 10.8 years. The change in capacitance after soaking for durations of 3, 5, 10, 15, and 20 min was 41.54 ± 14.57, 47.13 ± 11.80, 40.25 ± 14.95, 40.48 ± 14.19, and 39.97 ± 9.47 AU, respectively. The highest capacitance was observed after soaking for 5 min; however, there was no significant correlation between bathing duration and capacitance (p = 0.256). The capacitance measured immediately after soaking was at the uppermost level, but it rapidly decreased within 5 min. The change in TEWL after soaking for durations of 3, 5, 10, 15, and 20 min was 30.27 ± 9.74, 30.57 ± 7.45, 33.78 ± 9.25, 33.44 ± 7.24, and 35.13 ± 9.37 g/m2/h, respectively. There was also no significant correlation between duration of soaking and TEWL (p = 0.191); however, TEWL tended to increase with longer soaking duration.
Limitations
This study had a small sample size and measured only capacitance and TEWL. Future studies with more subjects, and that measure other physiologic parameters may further improve our understanding of the effect of bathing on skin.
Conclusions
There was no significant correlation between bathing duration and cutaneous properties including capacitance and TEWL. However, a 5‐min soaking provided the highest skin hydration for healthy skin.
Keywords: bathing, bathing duration, capacitance, skin moisture, soaking, transepidermal water loss
1. INTRODUCTION
The skin is a physical permeability barrier that acts to diminish transepidermal water loss (TEWL) and to prevent penetration of chemical agents and microorganisms. Adequate skin hydration is critical to the maintenance of healthy skin. 1 Healthy skin can remain smooth and soft by binding water. The ability of the skin to hold water is primarily related to the stratum corneum (SC), which is composed of corneocytes, their natural moisturizing factor (NMF), and intercellular lipids. 2 SC intercellular lipids are arranged in an order that forms a barrier to TEWL. Normally, the SC has about 20% water content, of which a fraction is tightly bound to NMF and the lipids found in the skin. 2 The ability of water to diffuse across the SC depends on the water content, and the diffusion pathway for water in the SC is mostly transcellular. 3 , 4 Skin hydration and TEWL have been widely used to evaluate skin barrier function. 5 , 6 Skin hydration reflects the water content of the SC, while TEWL reflects the diffusion of water through the SC. Elevated TEWL values in a disturbed skin barrier are frequently correlated with low SC hydration.
Bathing is the process by which dirt and bacteria are removed from the skin by direct mechanical action. Bathing is also associated with improvement in skin texture and a calming effect. Current skin care practices differ according to tradition, experience, and cultural factors. There is a current scarcity of evidence‐based data specific to the optimal duration of bathing to maximize skin hydration and enhance skin integrity. Inappropriate bathing may have a negative impact on both healthy skin and skin with barrier defects, such as atopic dermatitis (AD). Inappropriate bathing can cause excessive removal of intercellular lipids and NMF from the SC, which results in disturbance of the skin barrier. The current guideline‐based recommendations regarding the optimal duration of bathing for both healthy people and those with dermatoses are based on low‐quality evidence, and the recommendations are inconsistent. However, many guidelines mention an optimal bathing duration of 5–10 min. For example, the European Roundtable Meeting on Best Practice Healthy Infant Skin Care recommends 5–10 min of bathing for healthy newborn infants. 7 Among AD patients, European guideline recommends only 5 min of bathing to avoid epidermal dehydration. 8 A consensus guideline in Korea specifies a recommended duration of bathing of 5–10 min. 9 The American Academy of Dermatology recommends that bathing should be limited to short periods of time (e.g., 5–10 min), but no standard for either the frequency of bathing or the duration of bathing has been established. 10 Japanese guidelines for AD do not mention any recommended duration of bathing. 11
Accordingly, the objective of this study was to investigate the impact of bathing on skin hydration to guide future recommendations regarding the optimal duration of bathing.
2. MATERIALS AND METHODS
2.1. Design and instrumentation
An experimental, noninvasive, in vivo, biophysical approach was used in this study. The volar aspect of the forearm was chosen as the study site because it is the most commonly used site for dermatological investigations, and it is easily assessable. Recruitment was conducted through bulletin announcement, and the recruitment goal was 65 volunteers and 130 forearms. Both forearms of each volunteer were randomly selected and were soaked in tap water for duration of 3, 5, 10, 15, and 20 min. Tap water was used for soaking immediately after being drawn from a tap. When soaking was completed, water was removed by dab drying with a towel. Capacitance and TEWL were measured in triplicate before soaking, immediately after soaking, 3 min after soaking, and 5 min after soaking. The same investigator performed all instrument evaluations, and the average of three measurements for each subject was used for analysis.
To evaluate the skin hydration, capacitance was assessed using a Corneometer (model CM825; Courage + Khazaka, Köln, Germany). 12 Skin barrier function was assessed by measuring TEWL with a Tewameter (model TM300; Courage + Khazaka). 13 Both instruments were calibrated according to the manufacturer's instructions.
2.2. Subjects
Sixty‐five healthy volunteer subjects aged 18–60 years were enrolled. The exclusion criteria were: 1. fever on the study date; 2. a preexisting skin condition; 3. preexisting dermatological and/or medical condition(s) resulting in xerosis and/or affecting the dermal vasculature; 4. preexisting conditions that are sensitive to water; 5. current treatment with any vasoactive medication; 6. shaving at the study site within 7 days before the test; 7. application of topical corticosteroids, calcineurin inhibitors, or moisturizer at the study site within 12 h before the test; and/or, 8. excessive exercise, smoking, or drinking of caffeine within 3 h before the test. All measurements were performed in an environmentally controlled room with the temperature and humidity set according to international guidelines for the in vivo assessment of skin properties in non‐clinical settings. 6 Before commencing the study, participants rested for at least 20 min to acclimatize to the study room environment.
The study protocol was approved by the Siriraj Institutional Review Board of the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand (approval number: Si 683/2016), and all participants provided written informed consent to participate.
2.3. Outcome measurement and statistical analysis
The main outcome measures were the differences in the capacitance and TEWL before and after soaking for different duration. The secondary outcome was to evaluate changes over time in capacitance after soaking. All data were quantitatively documented and tested for normal distribution. Data are expressed as number or mean ± standard deviation (SD). A comparison of the baseline data for each group was performed using one‐way analysis of variance (ANOVA). Differences between before and after soakings were determined using paired t‐test. Changes over time were investigated using repeated measures ANOVA. A p‐value of <0.05 was considered statistically significant. All statistical evaluations were performed using SPSS Statistics software (version 18; SPSS, Inc., Chicago, IL, USA).
3. RESULTS
3.1. Baseline data
Sixty‐five healthy volunteers aged 18–60 years (mean ± SD age: 33.0 ± 10.8 years) participated. Thirty‐eight (58.46%) participants were women, and 27 (41.54%) were men. Baseline skin physiological function (capacitance and TEWL) measurements were not significantly different among the 3‐, 5‐, 10‐, 15‐, and 20‐min soaking groups (p = 0.263 and p = 0.430, respectively; Table 1). All volunteers were of Thai ethnicity and had Fitzpatrick skin type III–IV.
TABLE 1.
Baseline characteristics and skin physiological function data for all participant groups (65 healthy volunteers and 130 forearms)
| 3 min | 5 min | 10 min | 15 min | 20 min | Total | p value | ||
|---|---|---|---|---|---|---|---|---|
| Participants, n | 26 | 26 | 26 | 26 | 26 | 130 | ||
| Gender | Male | 9 | 11 | 11 | 10 | 13 | 54 | 0.845 |
| Female | 17 | 15 | 15 | 16 | 13 | 76 | ||
| Age (years) | 31.83 ± 12.57 | 35.95 ± 9.07 | 31.27 ± 11.24 | 33.28 ± 10.56 | 32.95 ± 10.80 | 0.575 | ||
| Capacitance (AU) | 37.57 ± 8.45 | 37.88 ± 8.39 | 38.57 ± 7.38 | 34.33 ± 4.72 | 37.47 ± 7.67 | 0.263 | ||
| TEWL (g/m2/h) | 13.78 ± 5.16 | 13.37 ± 6.02 | 13.70 ± 4.90 | 12.97 ± 4.23 | 16.02 ± 9.33 | 0.430 |
Data presented as number or mean ± standard deviation.
A p‐value < 0.05 indicates statistical significance.
Abbreviation: TEWL, transepidermal water loss.
3.2. Differences before and after soaking after different soaking durations
The difference in capacitance compared between before and after soaking for durations of 3, 5, 10, 15, and 20 min was 41.54 ± 14.57, 47.13 ± 11.80, 40.25 ± 14.95, 40.48 ± 14.19, and 39.97 ± 9.47 AU, respectively. No significant changes were observed in skin hydration (p = 0.256); however, 5 min of soaking showed the highest increase in capacitance (Figure 1).
FIGURE 1.
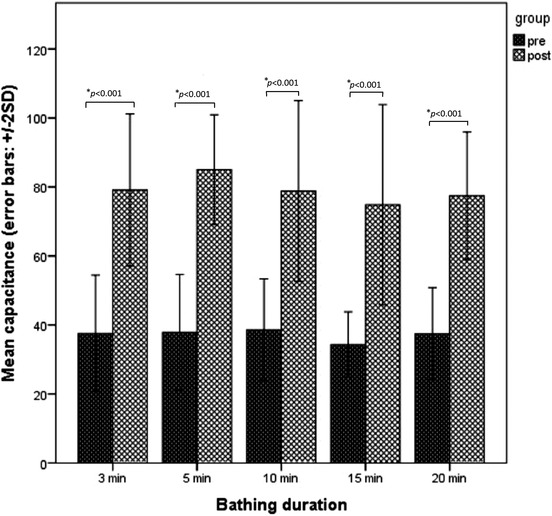
Changes in skin hydration status following soaking for various durations. The result is shown as the mean ± standard deviation of capacitance between baseline and immediately after soaking, and compared among soaking durations. Five minutes of soaking showed the highest increase in capacitance, but there was no significant difference among soaking durations (p = 0.256). (*p < 0.001)
The increment of TEWL compared between before and after soaking for duration of 3, 5, 10, 15, and 20 min was 30.27 ± 9.74, 30.57 ± 7.45, 33.78 ± 9.25, 33.44 ± 7.24, and 35.13 ± 9.37 g/m2/h, respectively (p = 0.191). A nonsignificant increase in TEWL was observed following longer durations of soaking (Figure 2).
FIGURE 2.
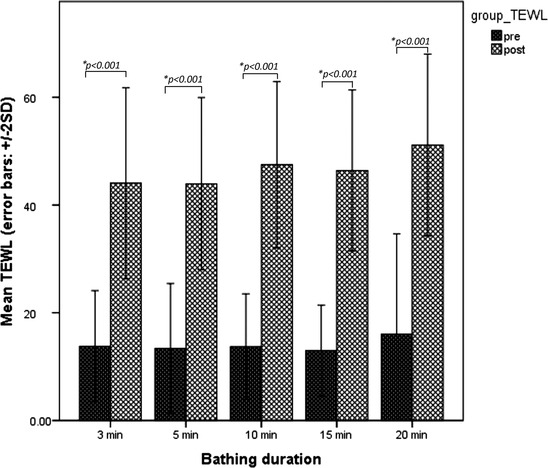
Differences in transepidermal water loss (TEWL) after soaking for different durations. The mean difference in TEWL between baseline and immediately after soaking was assessed, and compared among soaking durations. Although no significant difference was observed among soaking durations (p = 0.191), our results suggest a trend toward a higher TEWL with increased duration of bathing. (*p < 0.001)
3.3. Changes in capacitance at different time points after soaking for different durations
Skin hydration significantly increased after soaking in all study groups (p < 0.001) and then abruptly diminished within 5 min in all groups (p < 0.001) (Figure 3).
FIGURE 3.
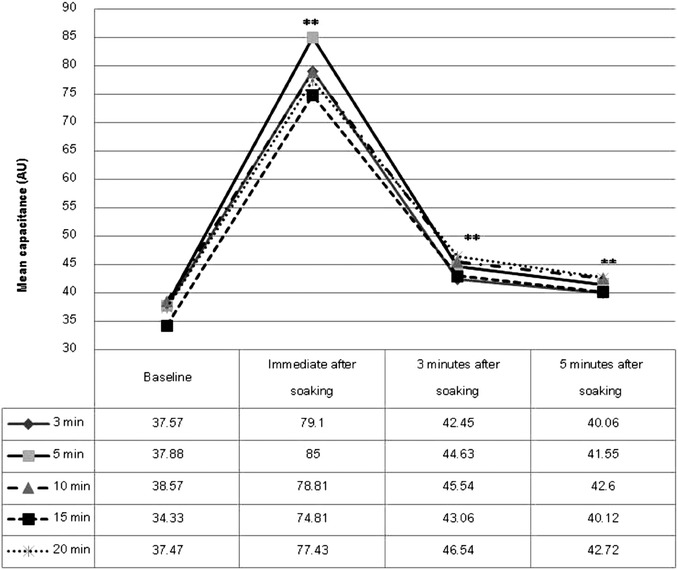
Changes in capacitance at different time points after soaking for different durations. Skin hydration significantly increased after soaking in all study groups (p < 0.001), and then abruptly diminished within 5 min (p < 0.001). (**p < 0.001)
4. DISCUSSION
The main purpose of this study was to investigate the quantitative evidence relating to the effect of tap water on the cutaneous biophysical function of submerged skin in healthy volunteers. Furthermore, we assessed the dynamic changes in skin surface hydration within 5 min after soaking. These data may be beneficial in determining the appropriate length of bathing to provide the highest skin moisture and to prevent skin damage resulting from suboptimal bathing.
This study indicated that soaking in all groups significantly increased cutaneous hydration from baseline. Although there was no significant difference in the mean hydration status of each soaking duration group, a 5‐min soaking provided the highest mean capacitance (47.13 or 133.87% of baseline; p = 0.256). The results of this study differ from those reported from previous studies. Voegeli 14 reported that washing with water did not change skin hydration. Chiang and Eichenfield 15 found that bathing for 10 min slightly increased cutaneous hydration. By comparison, the data from our study may indicate that the skin surface achieved its maximum capacitance when it was soaked for 5 min.
Tagami et al 12 reported on the hygroscopicity and water‐holding capacity of the skin after the application of water to normal skin for 10 s. That study showed a steep increase in capacitance followed by a rapid decrease within 30 s, followed by a gradual return to prehydration state within 2 min. A significant change in skin hydration was observed after soaking in all groups in this study. The highest increment occurred immediately after soaking, but the hydration level declined rapidly within 5 min of soaking. A similar result from previous study by our group 16 showed the capacitance was highest immediately after bathing, and then it decreased over time to the baseline level by 10 min after bathing. The study by Chiang 15 also demonstrated the same outcome that skin hydration after bathing gradually returned to prehydration levels within 10 min. They also found that capacitance decreased to a final value of 89% of baseline at the 120‐min post‐bathing time point. To preserve cutaneous hydration after bathing, moisturizers especially in occlusive type are preferentially applied immediately after a bath.
The present study found that a duration of soaking longer than 5 minutes did not increase capacitance, but the TEWL value increased. A study reported by Warner found that prolonged exposure to water disrupts the SC. 17 The possible explanation of increment of TEWL with longer duration of immersion may result from the evaporation of remaining water in the SC, or barrier disruption by water.
This study has several limitations. First, this was a pilot study and the number of participants/forearms in each group was relatively small, and this may have limited the statistical power of our study to identify all statistically significant differences. As we wanted to find out the optimal duration of bathing, we had to divide the subjects into five groups, which limited the number of participants in each group. As a result, the data showed no statistical significance. Future studies with more subjects in each group may demonstrate significant data. Furthermore, if the studies are done on a pediatric population and patients with skin barrier dysfunctions, the results will impact on the recommendations on the optimal bathing duration. The other limitations were the methods for evaluating the cutaneous biophysical function. We measured only the capacitance and TEWL. If other measurements were made, including skin pH and the moisture accumulation rate, the additional information would help us to assess the effect of bathing on skin physiological functions.
5. CONCLUSION
We compared the effects of various durations of soaking on cutaneous hydration status and TEWL. We also observed the dynamic changes in capacitance after soaking. Our results revealed no statistically significant difference in either capacitance or TEWL among the five studied soaking duration. However, 5 min of soaking provided the highest skin hydration, and TEWL value tended to increase correlated with the duration of soaking. Although soaking with water significantly increased the skin hydration status, the value rapidly diminished within 5 min. From this result, the authors recommended that 5‐min of bathing may be the most appropriate duration to provide the maximum cutaneous hydration and prevent skin disruption.
CONFLICT OF INTEREST
All authors declare no personal or professional conflict of interest and no financial support from the companies that produce and/or distribute the drugs, devices, or materials described in this report.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the volunteers who agreed to participate in this study and Ms. Julaporn Pooliam for assistance with statistical analysis. This study was supported by a Siriraj Grant for Research Development and Medical Education from the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand (grant number: R015931014).
Nitiyarom R, Withitanawanit T, Wisuthsarewong W. Capacitance and transepidermal water loss after soaking in water for different durations: A pilot study. Skin Res Technol. 2022;28:98–103. 10.1111/srt.13097
REFERENCES
- 1. Bouwstra JA, de Graaff A, Gooris GS, Nijsse J, Wiechers JW, van Aelst AC. Water distribution and related morphology in human stratum corneum at different hydration levels. J Invest Dermatol. 2003;120:750–8. [DOI] [PubMed] [Google Scholar]
- 2. Verdier‐Sevrain S, Bonte F. Skin hydration: a review on its molecular mechanisms. J Cosmet Dermatol. 2007;6:75–82. [DOI] [PubMed] [Google Scholar]
- 3. Li X, Johnson R, Kasting GB. On the variation of water diffusion coefficient in stratum corneum with water content. J Pharm Sci. 2016;105:1141–7. [DOI] [PubMed] [Google Scholar]
- 4. Kasting GB, Barai ND, Wang TF, Nitsche JM. Mobility of water in human stratum corneum. J Pharm Sci. 2003;92:2326–40. [DOI] [PubMed] [Google Scholar]
- 5. Constantin MM, Poenaru E, Poenaru C, Constantin T. Skin hydration assessment through modern non‐invasive bioengineering technologies. Maedica (Buchar). 2014;9:33–8. [PMC free article] [PubMed] [Google Scholar]
- 6. du Plessis J, Stefaniak A, Eloff F, John S, Agner T, Chou T‐C, et al. International guidelines for the in vivo assessment of skin properties in non‐clinical settings: Part 2. transepidermal water loss and skin hydration. Skin Res Technol. 2013;19:265–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blume‐Peytavi U, Lavender T, Jenerowicz D, Ryumina I, Stalder JF, Torrelo A, et al. Recommendations from a European Roundtable Meeting on best practice healthy infant skin care. Pediatr Dermatol. 2016;33:311–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wollenberg A, Barbarot S, Bieber T, Christen‐Zaech S, Deleuran M, Fink‐Wagner A, et al. Consensus‐based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32:657–82. [DOI] [PubMed] [Google Scholar]
- 9. Kim JE, Kim HJ, Lew BL, Lee KH, Hong SP, Jang YH, et al. Consensus Guidelines for the treatment of atopic dermatitis in Korea (Part I): General management and topical treatment. Ann Dermatol. 2015;27(5):563–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eichenfield LF, Tom WL, Berger TG, Krol A, Paller AS, Schwarzenberger K, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71:116–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Katayama I, Aihara M, Ohya Y, Saeki H, Shimojo N, Shoji S, et al. Japanese guidelines for atopic dermatitis 2017. Allergol Int. 2017;66:230–47. [DOI] [PubMed] [Google Scholar]
- 12. Tagami H, Ohi M, Iwatsuki K, Kanamaru Y, Yamada M, Ichijo B. Evaluation of the skin surface hydration in vivo by electrical measurement. J Invest Dermatol. 1980;75:500–7. [DOI] [PubMed] [Google Scholar]
- 13. Barel AO, Clarys P. Study of the stratum corneum barrier function by transepidermal water loss measurements: comparison between two commercial instruments: Evaporimeter and Tewameter. Skin Pharmacol. 1995;8:186–95. [DOI] [PubMed] [Google Scholar]
- 14. Voegeli D. The effect of washing and drying practices on skin barrier function. J Wound Ostomy Continence Nurs. 2008;35:84–90. [DOI] [PubMed] [Google Scholar]
- 15. Chiang C, Eichenfield LF. Quantitative assessment of combination bathing and moisturizing regimens on skin hydration in atopic dermatitis. Pediatr Dermatol. 2009;26:273–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nitiyarom R, Anuntarumporn L, Wisuthsarewong W. Skin hydration and transepidermal water loss after bathing compared between immersion and showering. Skin Res Technol. 2021. 10.1111/srt.13039. [DOI] [PubMed] [Google Scholar]
- 17. Warner RR, Stone KJ, Boissy YL. Hydration disrupts human stratum corneum ultrastructure. J Invest Dermatol. 2003;120:275–84. [DOI] [PubMed] [Google Scholar]


