Abstract
Objective
The scar's appearance and psychological burden are the most esthetically challenging issues in acne vulgaris. This study investigated the effectiveness and safety profile of combined radiofrequency‐assisted subcision, which, even though effective on both Icepeak and Rolling subtypes, is only mildly effective on boxcar lesions, and polycaprolactone‐based dermal filler with collagen stimulation potency in managing atrophic postacne scars.
Methods
Our quasi‐experimental single‐arm study, after the inclusion of 10 cases over the age of 18 with moderate to severe mixed atrophic facial acne scarring, was carried out in two 3‐month separate sessions, during and after the intended intervention of which the experienced lesion improvements and also adverse events were documented. Moreover, all cases were followed for 3 months after the last session, evaluating the differences in the mentioned outcomes.
Results
We found the combined intervention to be highly effective in improving the intended outcomes, with the total number of acne lesions (p‐value < 0.001), along with the total number of Ice peak (p‐value = 0.002), Rolling (p‐value < 0.001), and boxcar (p‐value = 0.023) lesions demonstrating statistically significant changes.
Conclusion
Radiofrequency‐assisted subcision combined with polycaprolactone‐based dermal fillers can be an effective intervention in managing postacne scars. However, we recommend that randomized clinical trials with larger sample sizes be carried out for a more precise conclusion.
Keywords: atrophic acne scars, collagen stimulation, polycaprolactone‐based fillers, radiofrequency‐assisted subcision
1. INTRODUCTION
The scar appearance resulting from deep‐lying inflammatory acne and its subsequent psychological burden is the most esthetically challenging issue in acne vulgaris disease. 1 These scars have many well‐understood morphologies but are generally divided into two main subtypes of hypertrophic and atrophic, with the latter (consisting of rolling, icepeak, and boxcar subtypes) being the more common of the two. 2 Managing these scars has also proven to rely on many factors, including the patient's adherence and expectations while accounting for the clinician's initial evaluations. 3 Therefore, these factors, in aggregate, have caused the desired esthetic outcome of these scars to be very challenging.
Although most beneficial for the atrophic subtype of scars, one management technique is the subcutaneous incision, termed subcision, which has led to a renewal of the wound healing process and collagen synthesis. 4 , 5 , 6 However, even though the advantages, including shortened required patient downtime and fewer adverse effects on the adjacent melanin, are very eye‐catching, the side effects, including mechanically induced tissue trauma and the resulting hemorrhage, which in some cases can further complicate the situation by forming large hematomas and fibrosis, are left as the main worries. 7 These adverse events have notably decreased when techniques, including radiofrequency (i.e., radiofrequency‐assisted subcision, RF‐subcision, or rsubcision; using thermal energy to aid in the cannula movement), complementary to conventional subcision are implemented. 7 , 8 , 9 Moreover, studies have also demonstrated additional positive effects when the technique is used. 7 , 9 , 10 , 11
With all the merits, however, reports have indicated that boxcar acne scars were the toughest to resolve following the utilization of the technique. 9 Therefore, we believe the improvement in the outcome could be further increased by utilizing potentially effective complementary interventions, including dermal fillers with collagen‐stimulating potency. 12 , 13
One of the available mentioned fillers is the polycaprolactone‐based dermal fillers, demonstrating their efficacy in stimulating the production of collagens with higher endurance and esthetic properties while also improving the depressed appearance, which had remained postinjury. 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 Moreover, even though the effectiveness of these fillers has not yet been studied on atrophic acne scarring, their rejuvenating capabilities have been demonstrated to be significant when their application was investigated on the striae distensae disappearance, nasolabial folds' correction, and forehead contouring. 22 , 23 , 24 , 25 All of the mentioned favorable results further encouraged us to put our hypothesis to the test. Therefore, this study aimed to evaluate the differences the said addition would lead to in managing atrophic acne scars.
2. METHODS
2.1. Study design and ethical considerations
After being ethically approved by the local ethics committee, our pilot single‐arm study was conducted from July 2021 to February 2022 in a clinic with an outpatient setting while following the ethical principles of the Declaration of Helsinki. Furthermore, written informed consent was obtained from all participants before the study began.
2.2. Participant eligibility criteria
We opted to define our criteria based on the population, intervention, comparator, and outcome framework to achieve the highest possible degree of uniformity and objectiveness in selecting participants and the conduction methodology. 26 However, the framework's comparator aspect was not considered due to our study's design.
2.3. Population
Due to the novelty of the intervention and a lack of a prior study on the outcomes' mean differences, the determination of a statistically sufficient sample size was not possible. Therefore, a sample consisting of 10 individuals was deemed convenient.
Individuals over 18 who were referred with a complaint of facial acne scars made up our study population. Our inclusion criteria were those suffering from moderate to severe mixed (i.e., ice peak, boxcar, and rolling subtypes) atrophic postacne scarring. Furthermore, individuals who had underlying diseases that could affect the outcomes of the study were excluded, including:
The presence of cardiac pacemakers or metal implants in the body,
Those with active acne lesions or superimposed infections, or
Participants who had received other possibly effective therapeutic methods (e.g., laser therapy or chemical or physical peeling techniques) in the study's 4 months of the treatment phase.
2.4. Intervention
Regarding the RF‐subcision, the methodology was as follows: first, after appropriate sterilizations, the scar studded areas were anesthetized via a local lidocaine 2% gel application without requiring a tumescent injection or neural blocking. Next, the radiofrequency device (Aphrodite, Iran; electrosurgical unit, 400 mA current, maximum output power of 60 watts, and operating frequency of 4 MHz) was utilized, with the neutral plate being connected to the chest after applying a lubricant gel. Next, the power was set to 30–40 watts to achieve the most suitable temperatures (30‐40 degrees centigrade at dermis) and outcomes, as higher powers would lead to the burning of the skin. Depending on the severity of scarring, either the 18 (the most commonly used), 19, or 21 gauge needle, with the bevel pointing upwards and connected through the opposing end to the monopolar cannula, superficially infiltrated the lesion at a 30–45 degree angle from a periauricular entry point 1 centimeter away from the scar, the depth of insertion of which ranged from mid to deep dermis depending on the lesion's severity. Afterward, the entangled mid to deep dermal fibrous bands were released with a rapid parallel‐to‐skin to‐and‐fro motion while holding down the device's pedal. Furthermore, the area was intermittently monitored to prevent excessive heating and thermal damage to the neighboring tissues. After the intended procedure, the pedal was released, the RF probe removed from the opposite end, the cannula was retrieved, and a sterile gauze was placed adjacent to the entry site to prevent burning.
In each session, a total of 0.5 ml (0.05–0.1 ml of filler in each lesion) of the polycaprolactone‐based dermal filler (Ellansé, Netherlands) was also superficially injected with a 27 gauge needle, via fanning mode, into the deep dermis of the scars. Then, the skin surface was massaged repeatedly to achieve and maintain the desired esthetic and appearance. Additionally, the priorly mentioned photographic assessments and scores were obtained before the session.
In addition, we tried to mitigate the unnecessary infectious and painful side effects by administering topical antibiotics and nonsteroidal anti‐inflammatory drugs for a maximum of 3 days. Moreover, the cases received sunscreen agents to prevent damage to the vulnerable area between the sessions.
2.5. Outcomes
At first, in addition to the demographic data (i.e., the age and sex of each case), the scar characteristics, including numbers, type (ice peak, rolling, or boxcar), and the severity grading, which was based on the Goodman and Baron's qualitative 27 (scored from mild to severe based on whether they are apparent in a distance of 50 cm and above, being covered using make‐up, and being flattened by manual stretching of the skin, respectively) and quantitative 28 (achieved by two independently assessing dermatologists on a scale based on the scar count and type from 0 to a theoretical upper limit of 84; on which mild scarring can score to a maximum of 6 points, moderate scarring potentially scoring up to a maximum of 18 points, and severe scarring being capable of going as high as 36 on the overall scores) Global Acne Scarring Grading Systems (GBGS) were documented as measures of the primary outcome at baseline and 3 months after the last therapy session. Furthermore, the considered lesions were photographed (Sony A7Rii, 42 megapixels, Tokyo, Japan) and appropriately anonymized. Moreover, the secondary outcome of interest, consisting of any noted immediate postprocedural adverse reactions or adverse events during the follow‐up sessions, was documented.
2.6. Follow‐up
Individuals who underwent the therapy session were then followed for 6 months (i.e., three months after the second therapy session), during which the resulting changes in the appearance, grading, and the number of lesions were photographed and also anonymized.
2.7. Statistical analysis
The 26th version of the SPSS statistical package (SPSS Inc., Chicago, IL, USA) was used for the analyses. p‐Values <0.05 were considered statistically significant.
Initially, the normality of the data distribution was determined by the One‐Sample Kolmogorov‐Smirnov test. The consistency in the assessors’ ratings before and after the intervention was also evaluated by determining the Spearman's rank correlation coefficient (ρ).
Paired samples t‐test was performed to compare the means of the acquired data with a normal distribution (i.e., the total number of acne lesions, total number of Ice peak lesions, and total number of rolling lesions), while the Wilcoxon rank test was performed for the analysis of the data with without normal distribution (i.e., the total number of boxcar lesions and the changes in the mean of the grading of the Goodman and Baron's score by the two dermatologists).
3. RESULTS
A total of 10 individuals were included in our investigation, seven of whom (70%) were female, averaging 31.3 ± 0.83 years. Moreover, all the included cases completed the study. These individuals had a mean total number of facial acne lesions of 18.70 ± 9.056 (range: 9–35), consisting, in order of frequency, of ice peak (9.7 ± 7.65; range: 2–22), rolling (7 ± 2.70; range: 2–11), and boxcar (2 ± 1.700; range: 0–5 with 20% of the participants not having any boxcar lesions while 50% had two or more lesions) lesions, respectively. Eight individuals suffered from severe postacne scars, while the remaining two had moderate grades. (Tables 1 and 2)
TABLE 1.
Demographic data of the included individuals at baseline
| Age | |
| Mean +/‐ SD | 31.3 ± 0.83 |
| Range | 28–37 |
| Gender | |
| Male (%) | 3 (30%) |
| Female (%) | 7 (70%) |
| Fitzpatrick skin type | |
| III | 6 |
| IV | 4 |
TABLE 2.
Changes in the number of acne lesions before and following the procedure
| Variable | Baseline | After the procedure | Mean difference (SD) | p‐Value |
|---|---|---|---|---|
| Total number of acne lesions (mean ± SD) | 18.70 ± 9.056 | 6.80 ± 4.34 | 11.90 (5.53) | <0.001 |
| Mean total number of ice peak lesions (mean ± SD) | 9.7 ± 7.65 | 4 ± 3.74 | 5.70 (4.24) | 0.002 |
| Mean total number of rolling lesions (mean ± SD) | 7 ± 2.70 | 1.80 ± 0.79 | 5.200 (2.251) | <0.001 |
| Total number of boxcar lesions (mean ± SD) | 2 ± 1.700 | 1 ± 0.943 | 1 (0.943) | 0.023 |
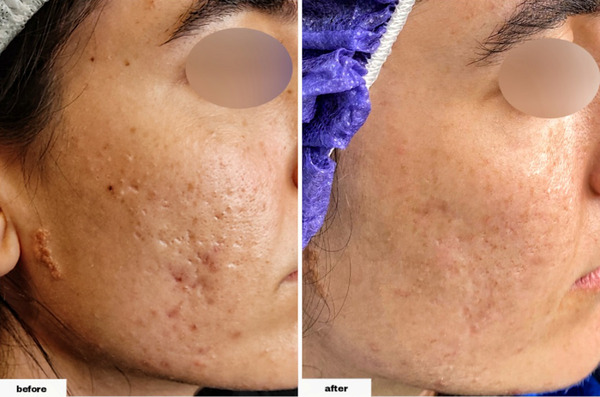
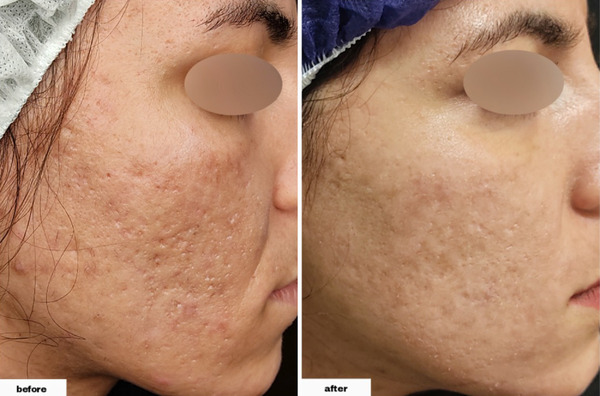
As demonstrated in Table 2, we found that the differences were significant in all types of lesions following the procedure. The total number of acne lesions (postintervention range: 3–15) decreased by 11.90 ± 5.53 (p‐values of <0.001). Furthermore, the total number of ice peak lesions (postintervention range: 0–12) decreased by 5.70 ± 4.24 (p‐value = 0.002), the total number of rolling lesions (postintervention range: 1–3) decreased by 5.20 ± 2.25 (p‐value < 0.001), and the total number of boxcar lesions (postintervention range: 0–3, with 30% of individuals having zero number of the lesion and 80% overall having one or less) decreased by 1 ± 0.94 (p‐value = 0.023). (Figures 1, 2, 3, 4)
FIGURE 1.

The scar appearance in a 34‐year‐old male before and after the procedure
FIGURE 2.

The procedure's effectiveness in decreasing the number of Rolling scars in a 37‐year‐old female
FIGURE 3.
The procedure's effectiveness in decreasing the number of Ice peak scars in a 28‐year‐old female
FIGURE 4.
The procedure's effectiveness in decreasing the number of boxcar scars in a 29‐year‐old female
The ρ values indicating the level of association between the two ratings before and after the intervention were 0.985 and 0.972, respectively, which shows a strong agreement. Moreover, the qualitative and quantitative grading of scars at the end of the investigations indicated significantly favorable responses (p‐values of 0.004 and <0.001, respectively), as all individuals experienced an improvement of at least one grade in the severity of scarring. This finding meant that eight individuals' scarring severity improved to mild (six and two cases with baseline grades indicating severe and moderate scarring, respectively), while two improved to moderate (having severe scarring at baseline). Moreover, this finding translated to a mean improvement of 11.4 ± 3.61 in the quantitative scoring system (Table 3).
TABLE 3.
Goodman and Baron's qualitative and quantitative scores before and after the intervention
| Variable | Baseline | After the procedure | p‐Value | |
|---|---|---|---|---|
| Goodman & Baron's Qualitative Score | Mild | 0 | 8 | 0.004* |
| Moderate | 2 | 2 | ||
| Severe | 8 | 0 | ||
| Goodman & Baron's quantitative score (mean ± SD) | Baseline | After the procedure | Mean difference | <0.001* |
| 19.3 ± 5.31 | 7.9 ± 4.06 | 11.4 ± 3.61 | ||
Analyzed via the Wilcoxon rank test
Regarding the safety profile of the intervention, we found that the individuals primarily complained of mild localized edema (30% of individuals and lasting for a maximum of 1 week), mild ecchymosis (30% of individuals and lasting for a maximum of 1 week), mild burning sensation (10% of individuals), and hypoesthesia (10% of individuals and lasting for a maximum of 3 days) during therapy. However, these complaints did not lead to said individuals abstaining from the study.
4. DISCUSSION
Many studies have investigated whether adding any supplementary techniques or agents would address concerns arising from postacne scars, including their quality of life and mental health. 29 In our study, which, based on our online database search, has been carried out for the first time, we demonstrated that in a study group of majority women individuals suffering from postacne scarring, the relatively novel approach, consisting of a combination of Radiofrequency‐subcision and the polycaprolactone‐based dermal filler, significantly affected the scars’ numbers and appearance through the radiofrequency‐induced heat.
We found that the total number of acne scars not only decreased significantly, and the qualitative and quantitative GBGS gradings indicated highly significant improvements, but so did the three subtypes (rolling, icepeak, and boxcar) individually. This finding indicates that the combined method can potentially improve a broad range of acne scars and not be bound to what had previously hampered the ultimate esthetic outcome of the disease in many individuals. These findings are consistent with the study by Kaur et al. 9 , investigating the effectiveness of RF‐subcision versus conventional subcision. However, our study showed the combined interventions’ superior practical effectiveness in improving the number of boxcar scars compared to RF‐subcision alone, which was improved, although significantly due to the low number of the lesion, but to a lesser extent and only by a few.
The technique also only caused mild to moderate adverse events, including mild localized edema, ecchymosis, and slight hypoesthesia during therapy, most of which were temporary and resolved either during the study or at the end. Furthermore, even though the lattermost complaint was relatively disconcerting for the individuals who underwent the therapy regimen, the positive outcomes outweighed them encouragingly, prompting them to go through the intervention phase and not drop out.
However, our study suffered from a few limitations, including a low number of participants. Therefore, as the results of our research can be invigorating to many health‐seeking individuals and the relevant clinicians, we recommend that further studies be carried out with the primary intention of addressing the mentioned limitations our study faced. As more similar data become available, we believe that the definite conclusion would incentivize the scientific community greatly.
5. CONCLUSION
The combined intervention of RF‐subcision and polycaprolactone‐based fillers can be regarded as one of the effective and safe methods in managing the acne‐induced atrophic scar appearance and its various lesion subtypes, including boxcar. Moreover, the high adherence rate demonstrated in the study can also be very encouraging.
CONFLICT OF INTEREST
The authors declare that no conflict of or competing interests existed or occurred in the conduction of this manuscript.
FUNDING INFORMATION
No funding or sponsorship was received for the conduct of this study.
ETHICS STATEMENT
This study was approved by the Ethics Committee of Kerman University of Medical Sciences under the license of IR.KMU.AH.REC.1400.245. Written informed consent was also obtained from all the participants before the study began.
Lotfi E, Shafie'ei M, Ahramiyanpour N. Radiofrequency‐assisted subcision combined with polycaprolactone‐based dermal fillers in the management of atrophic facial acne scars: A pilot investigative study. Skin Res Technol. 2022;28:865–871. 10.1111/srt.13228
Contributor Information
Elaheh Lotfi, Email: Elahehlotfiii@gmail.com.
Mohammad Shafie'ei, Email: ms6584@gmail.com.
Najmeh Ahramiyanpour, Email: najmeh.pour@gmail.com.
DATA AVAILABILITY STATEMENT
The dataset supporting the conclusions of this article is available upon request to the corresponding author, Najmeh Ahramiyanpour.
REFERENCES
- 1. Goodman GJ. Management of post‐acne scarring. What are the options for treatment? Am J Clin Dermatol. 2000;1(1):3‐17. [DOI] [PubMed] [Google Scholar]
- 2. Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45(1):109‐117. [DOI] [PubMed] [Google Scholar]
- 3. Boen M, Jacob C. A review and update of treatment options using the acne scar classification system. Dermatol Surg. 2019;45(3):411‐422. [DOI] [PubMed] [Google Scholar]
- 4. Friedmann DP, Vick GL, Mishra V. Cellulite: a review with a focus on subcision. Clin Cosmet Investig Dermatol. 2017;10:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21(6):543‐549. [DOI] [PubMed] [Google Scholar]
- 6. Rotunda AM, Bhupathy AR, Rohrer TE. The new age of acne therapy: light, lasers, and radiofrequency. J Cosmet Laser Ther. 2004;6(4):191‐200. [DOI] [PubMed] [Google Scholar]
- 7. Yadav S, Gupta S. Radiofrequency‐assisted subcision for postacne scars. J Am Acad Dermatol. 2018;78(1):e9‐e10. [DOI] [PubMed] [Google Scholar]
- 8. Faghihi G, Poostiyan N, Asilian A, et al. Efficacy of fractionated microneedle radiofrequency with and without adding subcision for the treatment of atrophic facial acne scars: a randomized split‐face clinical study. J Cosmet Dermatol. 2017;16(2):223‐229. [DOI] [PubMed] [Google Scholar]
- 9. Kaur M, Sharma VK, Sethuraman G, Arava S, Gupta S. A split‐face randomized controlled study comparing the efficacy and safety of intralesional radiofrequency‐assisted subcision vs conventional subcision in postacne scars. J Cosmet Dermatol. 2020;19(5):1086‐1092. [DOI] [PubMed] [Google Scholar]
- 10. Singh S, Dayal M, Walia R, Arava S, Sharma R, Gupta S. Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: a minimally invasive approach. Indian journal of dermatology, Venereol Leprol. 2014;80(5):419. [DOI] [PubMed] [Google Scholar]
- 11. Liu Y, Li Z, Hu J, et al. Treatment of nasal depressed scars using micro‐plasma radiofrequency technology combined with subcision. J Cosmet Dermatol. 2021;21(6):2458‐2462. [DOI] [PubMed] [Google Scholar]
- 12. Sage RJ, Lopiccolo MC, Liu A, Mahmoud BH, Tierney EP, Kouba DJ. Subcuticular incision versus naturally sourced porcine collagen filler for acne scars: a randomized split‐face comparison. Dermatol Surg. 2011;37(4):426‐431. [DOI] [PubMed] [Google Scholar]
- 13. Chen Q, Yang Y, Zhang J, Zhang Q. Long‐lasting treatment for moderate‐severe depressed facial scars: skin and hair derived new autologous tissue filler with subcision. J Dermatol Treat. 2022;33(1):247‐253. [DOI] [PubMed] [Google Scholar]
- 14. Zaleski‐Larsen LA, Fabi SG, McGraw T, Taylor M. Acne scar treatment: a multimodality approach tailored to scar type. Dermatol Surg. 2016;42(Suppl 2):S139‐S149. [DOI] [PubMed] [Google Scholar]
- 15. Johl SS, Burgett RA. Dermal filler agents: a practical review. Curr Opin Ophthalmol. 2006;17(5):471‐479. [DOI] [PubMed] [Google Scholar]
- 16. Kim JA, Van Abel D. Neocollagenesis in human tissue injected with a polycaprolactone‐based dermal filler. J Cosmet Laser Ther. 2015;17(2):99‐101. [DOI] [PubMed] [Google Scholar]
- 17. Pitt CG, Gratzl MM, Kimmel GL, Surles J, Schindler A. Aliphatic polyesters II. The degradation of poly (DL‐lactide), poly (epsilon‐caprolactone), and their copolymers in vivo. Biomaterials. 1981;2(4):215‐220. [DOI] [PubMed] [Google Scholar]
- 18. Laeschke K. Biocompatibility of microparticles into soft tissue fillers. Semin Cutan Med Surg. 2004;23(4):214‐217. [DOI] [PubMed] [Google Scholar]
- 19. Taylor MS, Daniels AU, Andriano KP, Heller J. Six bioabsorbable polymers: in vitro acute toxicity of accumulated degradation products. J Appl Biomater. 1994;5(2):151‐157. [DOI] [PubMed] [Google Scholar]
- 20. Kim JS. Changes in dermal thickness in biopsy study of histologic findings after a single injection of polycaprolactone‐based filler into the dermis. Aesthet Surg J. 2019;39(12):Np484‐Np94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hong JY, Kim JH, Kwon TR, Hong JK, Li K, Kim BJ. In vivo evaluation of novel particle‐free polycaprolactone fillers for safety, degradation, and neocollagenesis in a rat model. Dermatol Ther. 2021;34(2):e14770. [DOI] [PubMed] [Google Scholar]
- 22. Bae B, Lee G, Oh S, Hong K. Safety and long‐term efficacy of forehead contouring with a polycaprolactone‐based dermal filler. Dermatol Surg. 2016;42(11):1256‐1260. [DOI] [PubMed] [Google Scholar]
- 23. Hong JY, Han HS, Kwon TR, Kim JH, Na JT, Kim BJ. Remarkable improvement of striae distensae with polycaprolactone filler injection. J Eur Acad Dermatol Venereol. 2019;33(11):e399‐e400. [DOI] [PubMed] [Google Scholar]
- 24. Moers‐Carpi M, Christen MO, Delmar H, Brun P, Bodokh I, Kestemont P. European multicenter prospective study evaluating long‐term safety and efficacy of the polycaprolactone‐based dermal filler in nasolabial fold correction. Dermatol Surg. 2021;47(7):960‐965. [DOI] [PubMed] [Google Scholar]
- 25. Park JW, Choi SY, Kim KR, et al. A randomized, participant‐and evaluator‐blinded, matched‐pair prospective study to compare the safety and efficacy between polycaprolactone‐based fillers in the correction of nasolabial folds. Dermatol Ther. 2022;. 35:e15508. [DOI] [PubMed] [Google Scholar]
- 26. Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well‐built clinical question: a key to evidence‐based decisions. ACP J Club. 1995;123(3):A12‐A13. [PubMed] [Google Scholar]
- 27. Goodman GJ, Baron JA. Postacne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32(12):1458‐1466. [DOI] [PubMed] [Google Scholar]
- 28. Goodman GJ, Baron JA. Postacne scarring–a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5(1):48‐52. [DOI] [PubMed] [Google Scholar]
- 29. Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol. 2015;172:3‐12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available upon request to the corresponding author, Najmeh Ahramiyanpour.


