Abstract
The enhanced recovery after surgery (ERAS) pathway was formulated with the aim to reduce surgical stress response, alleviate pain and guarantee the best-fit experience of patients’ perioperative period. However, the application of ERAS in geriatric patients who underwent unicompartmental knee arthroplasty (UKA) was relatively lacking. We hypothesize that UKA patients can benefit from the ERAS protocol. A total of 238 patients were recruited in this retrospective study from August 2018 to December 2021, and Oxford phase III UKA was applied to all patients. ERAS pathway included nutrition support, anesthesia mode, interoperative temperature, and blood pressure control, application of tranexamic acid, early initiation of oral intake and mobilization, and pain management. Demographic data, operation-relative variables, and postoperative complications were analyzed. Forgotten Joint Scores, Oxford Knee Score, Lysholm score, numerical rating scale, and knee range of motion were introduced to estimate the activity function and pain of surgical knee, and these variables were compared between the 2 groups. There were 117 patients in the ERAS group and 121 patients in the traditional group, respectively. The ERAS group had a shorter length of surgical incision and less intraoperative blood loss. Postoperative hemoglobin and albumin of patients in the ERAS group were better than those in the traditional group (P < .05), after 17.0 ± 10.8 months follow-up, the numerical rating scale, Lysholm, Oxford Knee Score, Forgotten Joint Scores, and knee range of motion of patients in the ERAS group were significantly better than the traditional group. The length of hospital stay for patients who underwent ERAS was 11.7 ± 3.8 days and the postoperative complication rate was lower for the ERAS group patients (P = .000 and 0.031). ERAS can reduce the length of hospital stay, and patients can achieve excellent postoperative knee function. The formulation and implementation of the ERAS protocol require good collaboration across multiple disciplines, as well as a deep understanding of the existing clinical evidence and the concept of the ERAS program.
Keywords: enhanced recovery after surgery, geriatric, nutrition support, pain management, unicompartmental knee arthroplasty
1. Introduction
Unicompartmental knee arthroplasty (UKA) has been proven to be an effective surgical option for patients with medial-compartment degenerative knee arthritis. Despite the variability of indications and contraindications in patients’ selection, survivorship of UKA was reported by different authors at 95% at 2 years, 88% to 95% at 5 years, 80% to 98% at 10 years, and 70% at 25 years.[1–6]
Academic surgeons invented the term enhanced recovery after surgery (ERAS) in 2001 in London.[7] The objective of ERAS was to reduce surgical stress response, alleviate pain and improve patients’ perioperative experience by means of literature review and adaptation of treatments. Furthermore, the authentic painless strategy will reduce the incidence of complications and accelerate postoperative functional recovery which is accompanied by well-pleasing satisfaction.
From a global perspective, data from the national joint registry from different countries demonstrated that UKA constituted 16.9% of primary knee arthroplasties in Australia in 2003 and 8.9% in England and Wales in 2017.[8] In China, it is reported that the prevalence of symptomatic knee osteoarthritis (KOA) was 8.1%, and individuals aged ≥60 years accounted for 10.4% of the domestic population in 2015, and this proportion increased to 11.9% by 2018, reaching approximately 166 million.[9] The application of an optimal ERAS in UKA can shorten patients’ hospitalization stay, reduce the expenses of hospital readmission due to adverse events, and consequently relieves the financial burden of family and national healthcare systems.
Currently, many articles report the effectiveness of ERAS in total knee arthroplasty (TKA), total hip arthroplasty, and anther surgical disciplines.[10–12] Some beneficial protocols have been advocated by cooperative groups in pain, nutritional, and wound management; all these ERAS programs are efficacious and cost-effective in orthopedic patients when compared to the traditional pathway. However, high-level evidence which concentrated on the application of ERAS in UKA is relatively lacking.
Given that, we conducted this retrospective cohort study with the aim to evaluate the indispensable role of UKA in the treatment of medial unicompartmental osteoarthritis; assess the efficiency and safety of ERAS in patients who underwent UKA surgery initially; deliberate on whether patients would benefit from this program with clinical-outcome and complications as primary concerns. We hypothesize that the ERAS pathway can accelerate postoperative rehabilitation and UKA patients will benefit from ERAS protocol.
2. Materials and methods
2.1. Patient selection
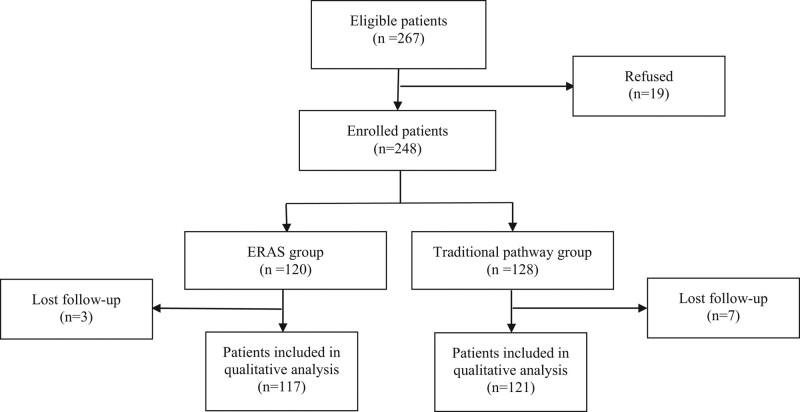
This retrospective study was conducted from August 2018 to December 2021. A total of 238 patients who underwent mobile-bearing Oxford UKA were recruited. The flow diagram of Figure 1 demonstrates the process of patients’ selection through each stage of this study.
Figure 1.
Follow diagram of recruited UKA patients who underwent ERAS and traditional pathway. ERAS = enhanced recovery after surgery, UKA = unicompartmental knee arthroplasty.
The inclusion criteria were anteromedial KOA with bone-on-bone; medial collateral ligament and lateral collateral ligament functionally intact; full-thickness cartilage in lateral compartment; an acceptable patella-femoral joint; fixed flexion deformity ≤10°; the extra-articular varus deformity ranges from 5° to 10°; patients with a functional or structurally intact anterior cruciate ligament; and patients with morbid obesity (body mass index [BMI] ≥ 32 kg/m2).
2.2. Pathway of ERAS group
2.2.1. Preoperative interventions.
Nutrition support: iron supplement, hemopoietin, and other anti-anemic therapy were applied to patients with a diagnosis of anemia; hypoproteinemia, each patient ate 8 egg whites per day regardless of whether the albumin level is normal or not; patients would have clear oral liquids up to 2 hours before surgery.
0.2 g celecoxib was taken orally for each patient for preoperative analgesia; the clinical psychologist gave alprazolam for anti-anxiety treatment according to the results of the patient’s anxiety rating scale; each patient took mosapride 5 mg orally 3 hours before surgery routinely to prevent postoperative nausea and vomiting.
2.2.2. Interoperative interventions.
Anesthesia mode, intraspinal anesthesia combined with femoral never block performed for patients in the ERAS group; a forced-air warming blanket was used to maintain the patients’ normal body temperature, and consequently to prevent intraoperative hypothermia.
Systolic blood pressure was controlled at 90 to 110 mm Hg; dexamethasone (10 mg) was used to prevent postoperative nausea and vomiting before fixation of prosthesis with bone cement or insertion of rod into femoral bone marrow cavity.
Application of tranexamic acid (TXA): 5 to 10 minutes before skin incision and tourniquet release, 1 g of TXA was injected intravenously and respectively, and 1 g of TXA was intraarticularly injected when the incision was closed; all patients received periarticular infiltration with an analgesic “cocktail” therapy which comprised of ropivacaine 20 mL, epinephrine 0.1 mg, methylprednisolone 40 mg, TXA 2 g.
2.2.3. Postoperative interventions.
Early initiation of oral intake and mobilization were encouraged for patients with intraspinal anesthesia when returning to the ward.
Unified patient position (head, 40–50°; foot, 30°), intravenous dexamethasone (10 mg, 4 h/24 h), and mosapride (5 mg, 3/d) were given to the patients to prevent nausea and vomiting.
Nutrition supplement was provided for ERAS patients; ice therapy (2 hours) was introduced as a measure to relieve wound pain and swelling; the knee-flexed position and elastic bandage were applied in patients 2 hours postoperative; patient-controlled analgesia (3–5), patient-controlled analgesia and celecoxib (6–7), dezocine and celecoxib (≥8), continuous femoral never blocks were implemented respectively according to the numerical rating scale (NRS).
2.3. Interventions of the traditional group
Patients undergoing UKA in the traditional group will receive conventionally perioperative management, and there is no standard protocol for each participant. No restrictions on fasting guidelines, choices of anesthetic techniques and intraoperative medications, as well as postoperative analgesia, and indwelling urinary catheter. The same analgesic “cocktail” therapy was used in both groups, drainage tubes were routinely placed at the surgical knee; perioperative medications were individualized according to the actual situation and needs of patients. Perioperative interventions for the ERAS and traditional groups were summarized in Table 1.
Table 1.
Perioperative pathway for patients between ERAS and traditional groups.
| ERAS group | Traditional group |
|---|---|
| Preoperative interventions | |
| Instruction and education Egg white Preoperative analgesia Anxiety management Clear oral liquids up to 2 h before surgery Moxapride (5 mg) 3 h before surgery No urinary catheter (unilateral UKA) |
Instruction and education No egg white No preoperative analgesia No Anxiety management Oral liquids up to 6 h before surgery No prevention of postoperative nausea and vomiting Urinary catheter |
| Intraoperative interventions | |
| Intraspinal anesthesia combined with femoral never block Restricted infusion (<1500 mL) Local injection of cocktail Intra-articular perfusion of tranexamic acid (1 g) Intravenous dexamethasone (10 mg) No drainage tube Controlled blood pressure Warm saline rinses |
Intraspinal anesthesia No restricted infusion Local injection of cocktail No intra-articular perfusion of tranexamic acid No application of dexamethasone Drainage tube (24–48 h) No controlled blood pressure Saline rinses |
| Postoperative interventions | |
| Early initiation of oral intake Intravenous tranexamic acid (1 g, 3 h/6 h/9 h) Ice therapy Multimodal analgesia Intravenous dexamethasone (10 mg, 4 h/24 h) |
No early initiation of oral intake No intravenous tranexamic acid No ice therapy No multimodal analgesia No intravenous dexamethasone |
ERAS = enhanced recovery after surgery, UKA = unicompartmental knee arthroplasty.
2.4. Surgical technique
All the surgical procedures were strictly in accordance with Oxford’s standard UKA principle. The placement of the tibial osteotomy guide was determined according to the preoperative design. Once the tibial saw guide was assembled in situ, the vertical and horizontal tibial cut was performed. The bone fragment of the femoral condyle was cut and removed, and the condyle was milled when the microplasty femoral drill guide (Biomet UK Ltd) was centrally positioned. Second and third milling was necessary in order to ensure the balance of flexion and extension gap. To ensure the correct size of the tibial component, the tibial template should be positioned with its posterior margin flush with the posterior tibial cortex, then the twin peg femoral trial component and meniscal bearing of the chosen thickness should be inserted. All these surgeries were performed by 4 experienced senior physicians and cemented mobile-bearing Oxford III UKA (Biomet UK Ltd) was used. As for patients with metal allergy, we would use a mobile-bearing UKA with either titanium niobium nitride alloy implants or with fixed-bearing oxidized zirconium alloy implants.
2.5. Data collection
The following data were extracted and analyzed. Demographic characteristics including age, gender, BMI, comorbidities, and quality of life were evaluated with Forgotten Joint Scores; Oxford Knee Score (OKS), Lysholm score, and NRS were introduced to estimate the activity function and pain of the surgical knee. Knee range of motion (ROM) was recorded pre and postoperative and at the final follow-up time.
The primary outcomes were to evaluate patients’ length of hospital stay (LOS), operation time, intraoperative blood loss, NRS score, and ROM of the knee pre- and postoperatively; to compare the complication rate of ERAS and traditional pathway, including urinary tract infection, deep vein thrombosis, surgical site dehiscence and infection, abdominal pain and distention.
This study was approved by the Institutional Review Board of our hospital, and written consent from all the study participants was collected.
2.6. Statistical analysis
Descriptive statistics were performed, continuous variables were expressed as the mean ± standard deviation and categorical variables were expressed as frequencies. Mann–Whitney test was carried out for non-normally distributed continuous variables and Student t test for normally distributed variables respectively. Categorical variables were compared using the chi-squared test. A P value <.05 (P < .05) was considered to represent statistically significant results. All the tests were performed using the SPSS 19.0 software package (SPSS Inc., Chicago, IL).
3. Results
3.1. Demographic data
A total of 238 patients were finally included in this study. The mean follow-up times were 17.0 ± 10.8 months. In the ERAS group, 117 patients with an average age of 65.8 ± 7.0 years at the time of surgery, there were 35 males and 82 females in this group, and the mean BMI was 27.4 ± 3.9 kg/m2. In the traditional pathway group, 121 patients were enrolled and there were 37 males and 84 females with a mean age and BMI of 66.7 ± 7.1 years and 27.7 ± 3.3 kg/m2, respectively. Finally, there were no significant differences in age, gender, BMI, surgery side, comorbidities, and other demographic data between the 2 groups (Table 2).
Table 2.
Comparison of demographic data of patients between ERAS and traditional groups.
| Variable | Traditional group (n = 121) | ERAS group (n = 117) | χ2/T | P value |
|---|---|---|---|---|
| Age (yr) | 66.7 ± 7.1 | 65.8 ± 7.0 | 0.883 | .378 |
| Gender Male Female BMI (kg/m2) Surgery side Left Right Status of ACL Intact |
37 84 27.7 ± 3.3 68 71 114 |
35 82 27.4 ± 3.9 85 83 114 |
0.012 0.520 0.085 1.533 |
.911 .604 .770 .216 |
| Partial functional deficiency | 7 | 3 |
BMI = body mass index, ERAS = enhanced recovery after surgery.
3.2. Perioperative variables and clinical outcome
A total of 51 patients underwent bilateral UKA in the ERAS group and 18 patients in the traditional group, respectively; 66 patients received unilateral UKA in the ERAS group and 103 patients in the traditional group. There were significant differences in the length of surgical incision, operation time, and intraoperative blood loss between the 2 groups. Postoperative hemoglobin and albumin for patients in the ERAS group were better than those in the traditional pathway group, and the LOS was also shorter for the ERAS group (Table 3). Postoperative NRS, Lysholm, and OKS scores of both groups were prominent improved (P < .05), Forgotten Joint Scores, and postoperative ROM were also better for the ERAS group, and fewer patients suffered from postoperative complications in the ERAS group (Table 4).
Table 3.
Comparison of perioperative variables of patients between the 2 groups.
| Variable | Traditional group (n = 121) | ERAS group (n = 117) | χ2/T | P value |
|---|---|---|---|---|
| Length of incision LOS (d) Operation time (min) |
12.2 ± 1.1 16.3 ± 4.5 115.7 ± 31.4 |
11.8 ± 0.9 11.7 ± 3.8 133.3 ± 49.8 |
3.421 8.524 −3.249 |
.001* .000* .001* |
| Intraoperative blood loss (mL) Hemoglobin (g/L) Preoperative Postoperative Albumin (g/L) Preoperative Postoperative |
101.6 ± 45.9 134.9 ± 14.0 119.9 ± 14.4 40.2 ± 3.0 35.1 ± 3.2 |
80.2 ± 35.4 132.4 ± 13.0 123.9 ± 12.5 41.9 ± 3.2 38.5 ± 2.9 |
4.020 1.404 −2.230 −4.151 −8.480 |
.000* .126 .027* .000* .000* |
ERAS = enhanced recovery after surgery, LOS = length of hospital-stay.
* Statistically significant variables.
Table 4.
Clinical outcome and complication between ERAS and traditional groups.
| Variable | Traditional group (n = 121) | ERAS group (n = 117) | χ2/T | P value |
|---|---|---|---|---|
| NRS score Preoperative Postoperative Lysholm score Preoperative Postoperative OKS score Preoperative Postoperative FJS-12 score ROM Preoperative Postoperative Complications (%) DVT Wound delayed healing Surgical site infection Total |
5.5 ± 1.1 1.7 ± 1.3 58.5 ± 10.8 89.4 ± 5.2 43.0 ± 7.0 21.5 ± 2.5 69.9 ± 3.6 110.7 ± 5.5 127.1 ± 4.7 10.7 3.3 1.6 15.7 |
5.3 ± 1.1 1.3 ± 1.2 60.3 ± 7.6 90.8 ± 6.0 42.4 ± 2.8 18.9 ± 3.0 71.4 ± 3.2 110.4 ± 6.3 129.7 ± 6.6 3.4 1.7 0.8 5.9 |
1.363 2.387 −1.473 −1.996 0.947 7.205 −3.231 0.347 −3.547 4.180 0.587 0.297 4.653 |
.174 .018* .142 .047* .345 .000* .001* .729 .000* .041* .444 .586 .031* |
DVT = deep vein thrombosis, ERAS = enhanced recovery after surgery, FJS-12 = Forgotten Joint Scores, NRS = numerical rating scale, OKS = Oxford Knee Score, ROM = knee range of motion.
* Statistically significant variables.
4. Discussion
In this study, we formulated an ERAS program with an emphasis on accelerating recovery in elderly patients who underwent UKA. The present retrospective study evaluated the clinical outcomes, LOS, and incidence of early complications of the ERAS pathway in UKA patients. It was confirmed that the ERAS protocol can enable patients to have a better perioperative experience and quality of life and a larger range of knee motion; meanwhile, it can shorten the LOS and reduce the incidence of postoperative complications.
Although the optimal surgical treatment option for single-compartment KOA is still controversial, UKA has been proven to be successful.[13–15] UKA is characterized by better kinematic peculiarity and low pain scores; some studies demonstrated that UKA had lower complications than TKA in short-term outcomes. Considering the physical status and comorbidities, implanting a knee prosthesis in elderly patients possesses the characteristics of challenges and benefits, the clinical outcomes also argue in favor of UKA in elderly patients even aged >85 years.[16] With the extension of human life expectancy, the elderly also wants to remain active, and there is evidence that more patients return to sports, including low- and higher-impact types of sports after UKA.[17]
In this study, the mean age of the participants was 66.3 ± 7.0 years old, 83.5%, 29.9%, and 5.1% of patients aged ≥60, ≥70, and ≥80 years, respectively. The age distribution of patients who were eligible for UKA made the ERAS more challenging and is of great significance. We demonstrated that UKA is an effective surgical procure in relieving the pain of patients with symptomatic KOA, NRS scores of all patients were decreased remarkably which was consistent with the previous studies.[18,19] Celecoxib was given to UKA patients for preemptive analgesia[20,21] in our ERAS program since celecoxib will not compromise the function of platelet and increase intraoperative bleeding. Alprazolam was introduced in our ERAS pathway to relieve patients’ preoperative anxiety and to help patients get a satisfying sleep. Sleep deprivation has definite negative effects on surgeons’ technique,[22] it also reduces patients’ tolerance to surgery. Some authors even advocate that sleep loss may increase inflammation, expression of stress-related genes, general impairment of protein translation, metabolic imbalance, and thermal deregulation.[23] The multimode of intraspinal anesthesia combined with femoral nerve or saphenous nerve block, intra-articular “cocktail” injection, ice-bag cold compress, application of celecoxib, flurbiprofen axetil, and weak opioids relieve the perioperative pain efficiently. Owing to the mental-and-physical pain management strategy, patients in the ERAS group can achieve a better range of flexion and extension earlier when compared with the traditional group.
The concept of no urinary catheter and drainage tube also contributes to patients’ early activities in the ERAS model and multi-period application of TXA can also reduce blood loss in orthopedic surgery. Simultaneously, in this study, the scientific and multi-links usage of TXA also reduces the amount of intraoperative bleeding, since blood loss and subsequent transfusions are associated with major morbidity and mortality.[24] Correspondingly, patients under the ERAS pathway obtained an ideal OKS score than the traditional group in the early follow-up period; however, along with the persistence of rehabilitation exercise, this difference narrowed gradually. The implementation of our comprehensive ERAS measures has shortened the LOS time by 4.6 days. Similarly, ERAS protocols demonstrated a reduction in LOS by 2.22 days in liver surgery[25] and 1.7 days in TKA surgery.[26] ERAS proved to save 1847 LOS days and save the cost of almost $5 million in a colorectal service center.[27]
FJS was reported by Henrik[28] in 2012, this score reflects patients’ ability to forget the artificial joint in daily life. Similarly, the difference in FJS score between the 2 groups demonstrated ERAS pathway indeed plays an important role in pain control and wound management. Other content of our ERAS model, such as dietary management, nutritional support, prevention of dizziness and vomiting, and fluids infusion, is also indispensable and all these measures guarantee the implementation of this pathway and achieve the expected clinical outcomes. American Society for Enhanced Recovery published a statement on nutrition screening and therapy within a surgical ERAS Pathway in 2018,[29] this discussion led to strong recommendations for the implementation of routine preoperative nutrition, the key role of oral nutrition supplements, enteral nutrition, and parenteral nutrition (implemented in that order) in most perioperative patients was advocated. Clear oral liquids up to 2 hours before surgery, early initiation of oral intake, prevention of nausea and vomiting along with egg white intake provided enteral nutrition, which not only help patients restore gastrointestinal function quickly but also reduce complications such as electrolyte disturbance; meanwhile adequate and cost-effective nutrient elements promote surgical site healing since protein delivery is more important than total calorie delivery.
5. Strengths and limitations
The follow-up time was relatively short, therefore the influence of ERAS on the long-term clinical outcome of UKA cannot be analyzed. Despite the limitation above, this study had its strengths: we have formulated a comprehensive and cost-effective ERAS pathway, which provides clinical evidence for the application of fast-track surgery in UKA.
6. Conclusion
The ERAS was effective in elderly patients who underwent initial UKA. This model can reduce the LOS, obtain excellent postoperative OKS and FJS scores, and provides patients with a comfortable surgical experience. Formulating and implementing the ERAS protocol requires good collaboration in the orthopedic service center and a deep understanding of the existing clinical evidence along with the core concept of ERAS. Significant and indispensable progress should be made in the application of ERAS in UKA surgery, and to optimize surgical principles to guarantee the life quality of aged patients.
Author contributions
Data curation: Jia Li, Feng Zhao, Xiangming Jiang.
Formal analysis: Jia Li, Jianbao Gao.
Funding acquisition: Guobin Liu.
Investigation: Wei Dong.
Methodology: Jia Li, Sen Liu.
Software: Jia Li, Xiaoguang Yu, Chaohua Zhu, Sen Liu.
Writing – original draft: Jia Li.
Writing – review & editing: Guobin Liu.
Abbreviations:
- BMI
- body mass index
- ERAS
- enhanced recovery after surgery
- KOA
- knee osteoarthritis
- LOS
- length of hospital stay
- NRS
- numerical rating scale
- OKS
- Oxford Knee Score
- ROM
- knee range of motion
- TKA
- total knee arthroplasty
- TXA
- tranexamic acid
- UKA
- unicompartmental knee arthroplasty
JL, FZ, and JG contributed equally to this work.
This study was supported by the Bureau of Science and Technology of Hebei Province (NO. 21377770D) and the Department of Finance of Hebei (NO.LS201902).
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the First Hospital of Hebei Medical University.
Informed consent to publish the relevant data was obtained from all individual participants and patients included in the study.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Li J, Zhao F, Gao J, Dong W, Yu X, Zhu C, Liu S, Jiang X, Liu G. Enhanced recovery after surgery (ERAS) protocol in geriatric patients underwent unicompartmental knee arthroplasty: A retrospective cohort study. Medicine 2023;102:6(e32941).
Contributor Information
Jia Li, Email: lijia1256@163.com.
Feng Zhao, Email: 18633889691@163.com.
Jianbao Gao, Email: 1607287294@qq.com.
Wei Dong, Email: dwmh@163.com.
Xiaoguang Yu, Email: 13498060@qq.com.
Chaohua Zhu, Email: 360172482@qq.com.
Sen Liu, Email: dr_gbliu89@163.com.
Xiangming Jiang, Email: 1004268679@qq.com.
References
- [1].Heaps BM, Blevins JL, Chiu YF, et al. Improving estimates of annual survival rates for medial unicompartmental knee arthroplasty, a meta-analysis. J Arthroplasty. 2019;34:1538–45. [DOI] [PubMed] [Google Scholar]
- [2].Jeschke E, Gehrke T, Günster C, et al. Five-year survival of 20,946 unicondylar knee replacements and patient risk factors for failure: an analysis of German insurance data. J Bone Joint Surg Am. 2016;98:1691–8. [DOI] [PubMed] [Google Scholar]
- [3].Foran JR, Brown NM, Della Valle CJ, et al. Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2013;471:102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006. [DOI] [PubMed] [Google Scholar]
- [5].Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-Year minimum follow-up period. J Arthroplasty. 1996;11:782–8. [DOI] [PubMed] [Google Scholar]
- [6].Evans JT, Walker RW, Evans JP, et al. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ljungqvist O. ERAS--enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J Parenter Enteral Nutr. 2014;38:559–66. [DOI] [PubMed] [Google Scholar]
- [8].Crawford DA, Berend KR, Thienpont E. Unicompartmental knee arthroplasty: US and global perspectives. Orthop Clin North Am. 2020;51:147–59. [DOI] [PubMed] [Google Scholar]
- [9].Tang X, Wang S, Zhan S, et al. The prevalence of symptomatic knee osteoarthritis in China: results from the China Health and Retirement Longitudinal Study. Arthritis Rheumatol. 2016;68:648–53. [DOI] [PubMed] [Google Scholar]
- [10].Stowers MD, Manuopangai L, Hill AG, et al. Enhanced recovery after surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J Surg. 2016;86:475–9. [DOI] [PubMed] [Google Scholar]
- [11].Scott NB, McDonald D, Campbell J, et al. The use of enhanced recovery after surgery (ERAS) principles in Scottish orthopaedic units--an implementation and follow-up at 1 year, 2010-2011: a report from the Musculoskeletal Audit, Scotland. Arch Orthop Trauma Surg. 2013;133:117–24. [DOI] [PubMed] [Google Scholar]
- [12].Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37:259–84. [DOI] [PubMed] [Google Scholar]
- [13].D’Ambrosi R, da Silva MJSV, Moura JLM, et al. Radiographic and clinical evolution of the Oxford unicompartmental knee arthroplasty. J Knee Surg. 2021. doi: 10.1055/s-0041-1731718. Epub ahead of print. PMID: 3452056. [DOI] [PubMed] [Google Scholar]
- [14].D’Ambrosi R, Ursino C, Mariani I, et al. No difference in return to amateur sports after medial and lateral unicompartmental knee arthroplasty in patients younger than 65 years. Knee Surg Sports Traumatol Arthrosc. 2022;30:1050–6. [DOI] [PubMed] [Google Scholar]
- [15].D’Ambrosi R, Vaishya R, Verde F. Balancing in unicompartmental knee arthroplasty: balancing in flexion or in extension? J Clin Med. 2022;11:6813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ode Q, Gaillard R, Batailler C, et al. Fewer complications after UKA than TKA in patients over 85 years of age: A case-control study. Orthop Traumatol Surg Res. 2018;104:955–9. [DOI] [PubMed] [Google Scholar]
- [17].Witjes S, Gouttebarge V, Kuijer PP, et al. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46:269–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Stempin R, Stempin K, Kaczmarek W. Medium-term outcome of cementless, mobile-bearing, unicompartmental knee arthroplasty. Ann Transl Med. 2019;7:41–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tadros BJ, Dabis J, Twyman R. Short-term outcome of unicompartmental knee arthroplasty in the octogenarian population. Knee Surg Sports Traumatol Arthrosc. 2018;26:1571–6. [DOI] [PubMed] [Google Scholar]
- [20].Tołoczko-Iwaniuk N, Dziemiańczyk-Pakieła D, Nowaszewska BK, et al. Celecoxib in cancer therapy and prevention - Review. Curr Drug Targets. 2019;20:302–15. [DOI] [PubMed] [Google Scholar]
- [21].Krasselt M, Baerwald C. Celecoxib for the treatment of musculoskeletal arthritis. Expert Opin Pharmacother. 2019;20:1689–702. [DOI] [PubMed] [Google Scholar]
- [22].Parry DA, Oeppen RS, Amin MSA, et al. Sleep: its importance and the effects of deprivation on surgeons and other healthcare professionals. Br J Oral Maxillofac Surg. 2018;56:663–6. [DOI] [PubMed] [Google Scholar]
- [23].da Costa Souza A, Ribeiro S. Sleep deprivation and gene expression. Curr Top Behav Neurosci. 2015;25:65–90. [DOI] [PubMed] [Google Scholar]
- [24].Ng W, Jerath A, Wąsowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 2015;47:339–50. [DOI] [PubMed] [Google Scholar]
- [25].Noba L, Rodgers S, Chandler C, et al. Enhanced Recovery after Surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and meta-analysis. J Gastrointest Surg. 2020;24:918–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Jiang HH, Jian XF, Shangguan YF, et al. Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop Surg. 2019;11:229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Heathcote SS, Duggan K, Rosbrugh J, et al. Enhanced Recovery after Surgery (ERAS) protocols expanded over multiple service lines improves patient care and hospital cost. Am Surg. 2019;85:1044–50. [PubMed] [Google Scholar]
- [28].Behrend H, Giesinger K, Giesinger JM, et al. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27:430–6.e1. [DOI] [PubMed] [Google Scholar]
- [29].Wischmeyer PE, Carli F, Evans DC, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on nutrition screening and therapy within a surgical enhanced recovery pathway. Anesth Analg. 2018;126:1883–95. [DOI] [PubMed] [Google Scholar]