Abstract
Objectives
To study the impact of COVID-19 on chest CT practice during the different waves using Dose Archiving and Communication System (DACS).
Methods
Retrospective study including data from 86,136 chest CT acquisitions from 27 radiology centers (15 private; 12 public) between January 1, 2020, and October 13, 2021, using a centralized DACS. Daily chest CT activity and dosimetry information such as dose length product (DLP), computed tomography dose index (CTDI), and acquisition parameters were collected. Pandemic indicators (daily tests performed, incidence, and hospital admissions) and vaccination rates were collected from a governmental open-data platform. Descriptive statistics and correlation analysis were performed.
Results
For the first two waves, strong positive and significant correlations were found between all pandemic indicators and total chest CT activity, as high as R = 0.7984 between daily chest CT activity and hospital admissions during the second wave (p < 0.0001). We found differences between public hospitals and private imaging centers during the first wave, with private centers demonstrating a negative correlation between daily chest CT activity and hospital admissions (−0.2819, p = 0.0019). Throughout the third wave, simultaneously with the rise of vaccination rates, total chest CT activity decreased with significant negative correlations with pandemic indicators, such as R = −0.7939 between daily chest CTs and daily incidence (p < 0.0001). Finally, less than 5% of all analyzed chest CTs could be considered as low dose.
Conclusions
During the first waves, COVID-19 had a strong impact on chest CT practice which was lost with the arrival of vaccination. Low-dose protocols remained marginal.
Key Points
• There was a significant correlation between the number of daily chest CTs and pandemic indicators throughout the first two waves. It was lost during the third wave due to vaccination arrival.
• Differences were observed between public and private centers, especially during the first wave, less during the second, and were lost during the third.
• During the first three waves of COVID-19 pandemic, few CT helical acquisitions could be considered as low dose with only 3.8% of the acquisitions according to CTDIvol and 4.3% according to DLP.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00330-023-09426-1.
Keywords: COVID-19; Incidence; Data analysis; Public health; Tomography, X-ray computed
Introduction
Coronavirus disease 2019 (COVID-19) caused by SARS Cov2 virus can be responsible for acute respiratory syndrome. It was first detected in December 2019 and was characterized as a global pandemic by the World Health Organization (WHO) on March 11, 2020 [1, 2]. In France, the first cases were detected in late January 2020 and as of October 13, 2021, 7,274,276 cases and 117,211 deaths had been reported [3]. There was an urgent need to develop, produce, and widely distribute suitable real-time reverse-transcriptase polymerase chain reaction (RT-PCR) tests to detect and thereby isolate infected people in order to slow disease transmission [4]. However, scarce test availability as well as a significant false-negative rate in COVID-19 early stages and their inability to assess disease progression have led in some countries to widespread use of chest CT. Emergency departments needed to identify virus-positive patients as soon as possible for rapid triage [5]. Thus, chest CT stood as the gold standard for COVID-19 imaging since it had shown high sensitivity in detecting COVID-19 patients’ [6–8].
Several radiological societies have published recommendations concerning COVID-19 patients’ imaging management [9–12]. Specifically, they pointed out that chest CT was not always disease specific and should not be used as a screening tool for COVID-19 in asymptomatic patients. Chest CT should be used in patients with moderate to severe symptoms of COVID-19 or presenting risks of disease progression or in hospitalized patients. Furthermore, a single-phase, unenhanced, low-radiation-dose chest CT is sufficient for the evaluation of most COVID-19 patients [10, 12, 13].
Although several studies already related the strong impact that COVID-19 had on imaging departments, to our knowledge, none had used a Dose Archiving and Communication System (DACS) to provide objective multicentric data collection [5, 14–17]. DACS allows automatic feedback on doses delivered to patients during CT examinations. In the present study, using a centralized DACS, we have collected and analyzed data concerning chest CT examinations from 27 different centers in France. Our working hypothesis was that we could establish some correlation between the daily numbers of chest CT and pandemic indicators available on the national open-COVID-19-data project. Used in both public and private centers, the DACS platform was able to provide a unique and multicentric monitoring of low-dose chest CT recommendations, during the pandemic.
The aim of this study was to evaluate the impact of the COVID-19 pandemic on chest CT practice and on the doses delivered during the different waves using the Dose Archiving and Communication System (DACS) in association with public health open data.
Materials and methods
Study design
This study received the ethical approval from our IRB (n° CRM-2202–233), who dismissed the need for informed patient consent since there was no specific patient data collected nor retained.
This is a retrospective multicentric study which included every center connected to the centralized DACS provided by ALARA Expertise (Strasbourg, France), to monitor general CT dosimetry levels.
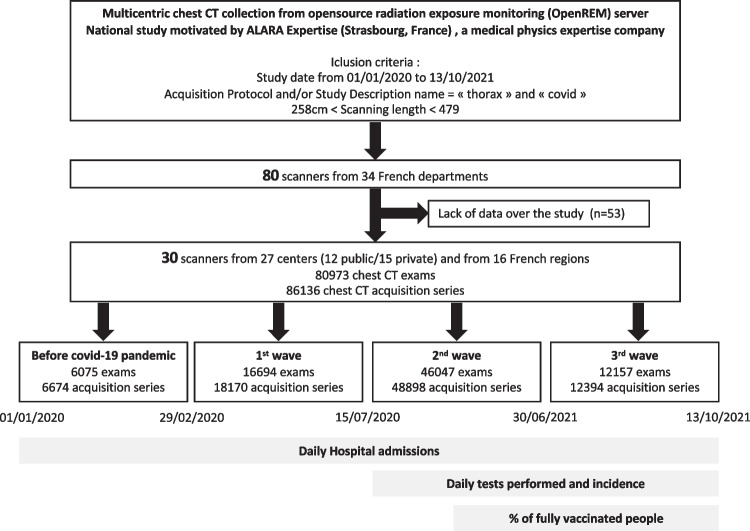
The inclusion period took place from January 1, 2020, to October 13, 2021. During the inclusion period, four distinct periods were taken into consideration: “before COVID-19 pandemic” (01/01/2020 to 01/03/2020), first wave (01/03/2020 to 15/07/2020), second wave (16/07/2020 to 30/06/2021), and third wave (01/07/2021 to 13/10/2021) (Fig. 1). All waves were defined in relation to the national data. The first wave was defined in relation to daily hospitalization data, since this was the only reliable indicator available, whereas the other two waves were defined in relation to daily incidence. For data management reasons and to facilitate the analysis, the mid- and end-of-month dates were preferred.
Fig. 1.
Study flowchart showing the study period, the centers’ characteristics, and the number of examinations and acquisitions analyzed overall and according to the different waves
Chest CT data collection
The centralized DACS is based on OpenREM, an open-source application for patient dose monitoring (0.10.0, GPL 3.0, https://openrem.org/). We used the DACS to collect data on all acquisitions with study description and acquisition protocols including “Chest” and “COVID” on body 32 cm phantom dose estimation with an explored length between 25.8 and 47.9 cm, in the 80 scanners connected to OpenREM. This interval corresponds to 36.8 cm ± 30% of the acquisition length based on the defined dose length product (DLP)/computed tomography dose index—volume (CTDIvol) ratio by the French national diagnostic reference levels (DRLs) for chest CT (https://nrd.irsn.fr/radiologie) and was used to exclude thoracoabdominal acquisitions from our study. Data collection metrics used were daily number of chest CT, CTDI, DLP, and some acquisition parameters (kV, mA, acquisition length, revolution time, pitch). Only centers with complete data for the entire study duration were included.
Pandemic indicator data collection
All pandemic indicators as well as the vaccination rate were extracted from the French government open-data project (http://data.gouv.fr). In this study, we considered either at national level or at a regional level the following pandemic indicators: daily tests performed, daily incidence, and daily hospital admissions. Daily tests performed and daily incidence are represented as a standardized incidence rate according to the studied population. Daily hospital admissions represent the daily number of newly hospitalized COVID-19 patients. The vaccination rate represents the percentage of the population that had received a complete vaccination schedule (two doses). National data for daily incidence and daily tests performed were not available either nationally or for each department during the first wave on data.gouv.fr. The first French vaccination was recorded on December 27, 2020, and the first full vaccination schedule (two-dose) on January 1, 2021.
Data and statistical analysis
Data was exported from the centralized DACS and sorted using Microsoft® Excel (Version 16.57). Statistical analysis was performed using Prism 9 (Version 9.0.0 (86), Graphpad Software Inc.). We performed descriptive statistics on our analysis. Pandemic indicators (i.e., tests performed, daily incidence, and daily hospital admissions) as well as daily chest CTs were processed as a 7-day moving average to avoid large daily variations. For chest CT excess, the number of chest CT exams was averaged over January and February 2020 (before the COVID-19 pandemic) and extended to the entire study period (N = 6075). Concerning chest CT proportion on the overall CT activity in the different centers, the month of January before the COVID-19 pandemic outbreak was taken as reference. Chest CTs, pandemic indicators, and vaccination rate were associated with either data for the entire country (total chest CT exams for the 27 centers, Fig. 2) or corresponding French department data for inter-center comparisons (Fig. 3). The Kolmogorov–Smirnov test rejected the normality of the distribution for every numeric variable. Correlations were therefore tested by Pearson’s correlation test during the three waves for each scanner, combined public and private scanners, and overall chest CT activity. The Mann–Whitney test was used to search statistical differences between CTDIvol and DLP, according to the different waves. Mean CTDIvol and DLP data correspond to a single helical chest CT acquisition. Chest CT dose levels (i.e., diagnostic reference level (DRL), standard (STDR), and low dose (LD)) have been defined according to the French Institute of Radiation-protection and Nuclear Safety (IRSN) and literature [10, 18]. The effective dose was calculated in accordance with International Commission on Radiological Protection (ICRP) publication 103 by multiplying the DLP by a factor of 0.014 [19]. For all tests, p value significance was set at 0.05.
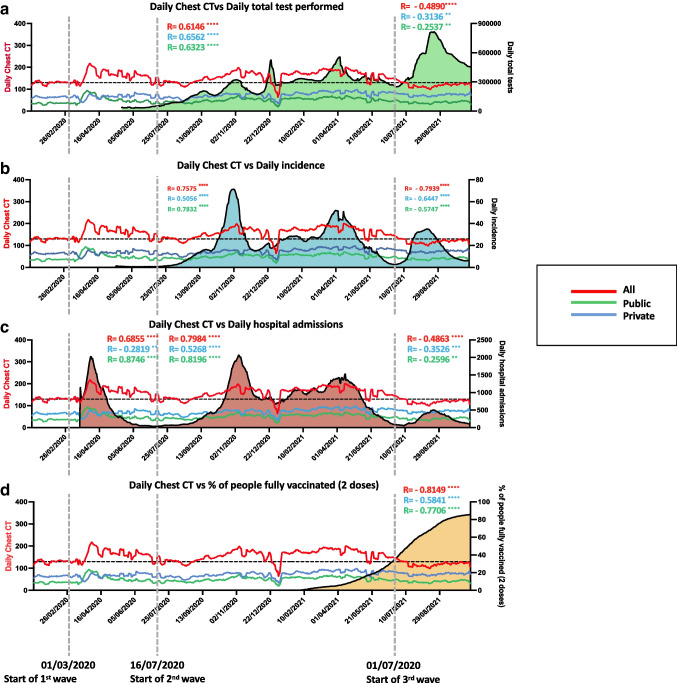
Fig. 2.
Daily chest CTs of all 30 scanners according to national data of daily tests performed (a), daily incidence (b), daily hospital admissions (c), and fully vaccinated people (2 doses) (d). All pandemic indicators as well as the vaccination rate were extracted from the French government open-data project (http://data.gouv.fr). The horizontal black dotted lines represent the average daily chest CT activity over January and February2020 which was considered as normal chest CT activity. The vertical gray dotted lines represent the different waves. The R value for Spearman correlations (RSpearman) between the overall daily chest CT (red), private daily CT (blue), and public daily CT (green) with all pandemic indicators and vaccination rates for the three waves are shown
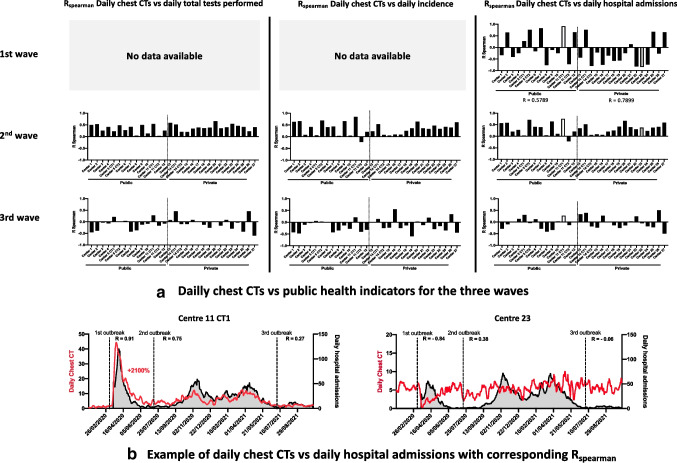
Fig. 3.
R value for Spearman correlations (RSpearman) between daily chest CT of each scanner and the corresponding departmental data of daily tests performed, daily incidence, and daily hospital admissions for each wave (a). In order to show the disparities between chest CT activity and COVID-19 pandemic spread according to the centers and their location, we have shown two examples of daily chest CTs according to daily hospital admissions for the 11-CT1 and 23 centers (b). The Spearman correlation R values in each wave for both centers were also shown to demonstrate the consistency of this choice of method. These R values are highlighted in white for center 11-CT1 and in gray for center 23 in panel a
Results
Study samples
We extracted data from 80 scanners, in 19 French departments. Fifty-three were excluded because of incomplete data sets during the inclusion period. The reasons for missing data were various: either technical problems leading to temporary scanner disconnection, scanner renewal, or implementation of the DACS subsequent to the beginning of the inclusion period. Thirty scanners from 27 centers and in 16 French departments were included (Fig. 1). Twenty were public structures and 15 were private centers. The number of chest CT exams per center ranged from 1175 to 4445 for a mean of 2699 (± 1040.5 SD) per center (Table 1). We analyzed a total of 80,973 CT exams: 6075 in the “before COVID-19 pandemic” period, 16,694 in the first wave, 46,047 in the second wave, and 12,157 in the third wave (Table 2).
Table 1.
Chest CT median irradiation dose per center
| Centers | Public/private | Manufacturer | N exams | N acquisitions | DLP median | CTDIvol median | Effective median dose |
|---|---|---|---|---|---|---|---|
| Center 1 | Public | General Electric | 2440 | 2520 | 328.9 | 9.57 | 4.604 |
| Center 2 | Public | Siemens | 4134 | 4190 | 219.4 | 5.37 | 3.071 |
| Center 3 | Public | General Electric | 3838 | 3971 | 208.9 | 5.18 | 2.925 |
| Center 4 | Public | General Electric | 1634 | 1663 | 207.8 | 5.51 | 2.909 |
| Center 5 CT1 | Public | Siemens | 1367 | 1484 | 224.6 | 6.42 | 3.144 |
| Center 5 CT2 | Public | Siemens | 3212 | 3354 | 215.9 | 6.045 | 3.023 |
| Center 6 | Public | Siemens | 2733 | 2902 | 211.8 | 5.885 | 2.965 |
| Center 7 | Public | General Electric | 1842 | 1986 | 284.4 | 8.845 | 3.982 |
| Center 8 | Public | General Electric | 1337 | 1361 | 260.3 | 7.33 | 3.644 |
| Center 9 | Public | General Electric | 2427 | 2474 | 257.2 | 7.05 | 3.601 |
| Center 10 | Public | General Electric | 1451 | 1622 | 270.5 | 7.5 | 3.787 |
| Center 11 CT1 | Public | Siemens | 4120 | 4268 | 376.3 | 12.98 | 5.268 |
| Center 11 CT2 | Public | Siemens | 1175 | 1233 | 295.9 | 8.97 | 4.142 |
| Center 12 | Public | Siemens | 2436 | 2513 | 211.7 | 6.05 | 2.964 |
| Center 13 | Private | Philips | 1409 | 1550 | 227.9 | 5.2 | 3.191 |
| Center 14 CT1 | Private | General Electric | 4445 | 4674 | 222.2 | 5.56 | 3.111 |
| Center 14 CT2 | Private | General Electric | 2640 | 2724 | 260.6 | 7.3 | 3.648 |
| Center 15 | Private | General Electric | 2049 | 2095 | 132.9 | 3.46 | 1.861 |
| Center 16 | Private | General Electric | 1567 | 1697 | 311.9 | 8.64 | 4.366 |
| Center 17 | Private | General Electric | 3191 | 3306 | 166.4 | 3.83 | 2.329 |
| Center 18 | Private | Philips | 4328 | 6079 | 297.4 | 8.3 | 4.164 |
| Center 19 | Private | General Electric | 3112 | 3493 | 300.6 | 9.16 | 4.208 |
| Center 20 | Private | General Electric | 2510 | 2587 | 242.6 | 6.66 | 3.397 |
| Center 21 | Private | General Electric | 2957 | 3073 | 247.5 | 6.89 | 3.465 |
| Center 22 | Private | General Electric | 1421 | 1492 | 299.2 | 8.905 | 4.189 |
| Center 23 | Private | General Electric | 3433 | 3652 | 272.6 | 7.455 | 3.817 |
| Center 24 | Private | General Electric | 4146 | 4173 | 267.1 | 7.62 | 3.74 |
| Center 25 | Private | General Electric | 4219 | 4503 | 228.9 | 5.67 | 3.205 |
| Center 26 | Private | General Electric | 2666 | 2696 | 238 | 6.58 | 3.332 |
| Center 27 | Private | General Electric | 2734 | 2801 | 227.7 | 5.93 | 3.188 |
| Total | 80,973 | 86,136 | 243.8 | 6.6 | 3.4 | ||
| Range (max–min) | 4445–1175 | 6079–1233 | 376.3–132.9 | 3.46–12.98 | 1.861–5.268 |
DLP dose length product, CTDIvol computed tomography dose index—volume
Table 2.
Chest CT median irradiation doses before the pandemic and per waves
| N chest CT exams | N chest CT helical acquisitions | DLP median | CTDIvol median | Effective dose median | |
|---|---|---|---|---|---|
|
Before covid-19 pandemic 01/01/2020–29/02/2020 |
6075 | 6674 | 234.2 | 6.29 | 3.279 |
|
First wave 01/03/2020–15/03/2020 |
16,694 | 18,170 | 240.5 | 6.51 | 3.367 |
|
Second wave 16/03/2020–30/06/2021 |
46,047 | 48,898 | 247.1 | 6.73 | 3.459 |
|
Third wave 01/07/2021–13/10/2020 |
12,157 | 12,394 | 239.3 | 6.45 | 3.351 |
| Total | 80,973 | 86,136 | 243.8 | 6.6 | 3.4 |
| Range (max–min) | 6075 – 46,047 | 6674–48,898 | 376.3–132.9 | 3.46–12.98 | 1.861–5.268 |
DLP dose length product, CTDIvol computed tomography dose index—volume
Correlation between daily chest CT, pandemic indicators, and vaccination
First wave
The only open pandemic indicator data available for the first wave was the number of daily hospital admissions. At the national level, there was a high and significant correlation with the total number of daily chest CTs performed in all centers (RSpearman = 0.6855, p < 0.0001) (Fig. 2C). However, data was heterogenous at the departmental level. For example, CT1 from center 11, a public center, reached the highest positive correlation observed between daily number of chest CTs performed and daily hospital admissions, with an RSpearman coefficient of 0.9141 (p < 0.0001). On the opposite, the CT from center 23, a private center, showed a very strong and negative correlation, with an RSpearman coefficient of −0.8395 (p < 0.0001), corresponding to a decreased CT activity. Overall, when combined, there was a significant strong positive correlation in public centers (R = 0.8746, p < 0.0001) and a significant negative correlation in private centers (− 0.2819, p = 0.0019, Supplementary data and Figs. 2 and 3).
Second wave
Regarding national data, there was a high and significant positive correlation between the total number of daily chest CTs performed in all centers and each pandemic indicator. Daily tests performed, daily incidence, and daily hospital admissions showed an RSpearman of 0.6146 (p < 0.0001), 0.7575 (p < 0.0001), and 0.7984 (p < 0.0001) respectively (Fig. 2A–C). In contrast to the first wave, almost all the correlations were positive for both public and private imaging centers. Still, we observed stronger correlation coefficients in public centers between daily number of chest CT performed with daily incidence and hospital admissions (Fig. 2).
Third wave
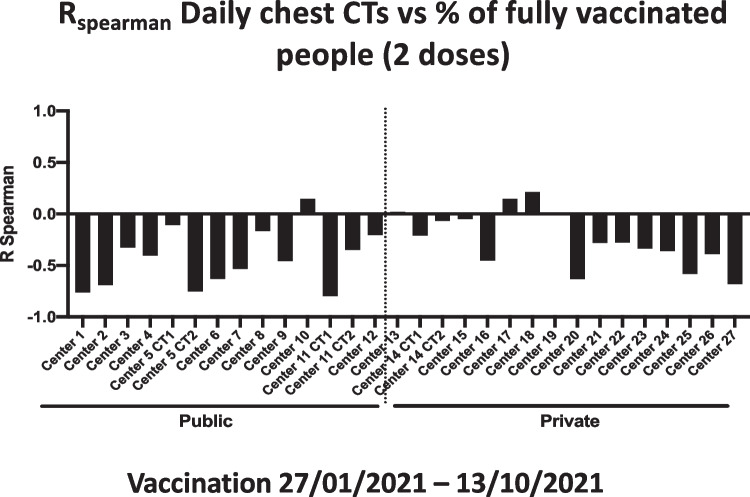
There was a high and a strong inverse correlation between the total number of daily chest CTs performed in all centers and the vaccination rate (R = −0.8149, p < 0.0001). Unlike the first two waves, we found a significant negative correlation between the number of daily chest CTs and each pandemic indicator. RSpearman was −0.49 (p < 0.0001), −0.80 (p < 0.0001), and −0.49 (p < 0.0001) for daily national tests performed, daily incidence, and daily hospital admissions respectively (Fig. 2A–C). The same trend can be seen with departmental data for all pandemic indicators (Supplementary data, Fig. 3). Only 50% of correlations were significant (p < 0.05). Finally, almost all the correlations between daily chest CT activity and daily incidence were negative for both public and private centers.
Chest CT and overall CT activity
Compared to the daily chest CT curve over the whole study and considering that the average corresponds to a normal chest CT activity, there was an excess of 13,022 chest CT exams during the inclusion period, corresponding to an increase of 15.6%. Before the start of the pandemic, the proportion of chest CT on the overall CT activity was 9.6% in private centers and 8.1% in public centers. During the first wave, a decrease of the overall activity was observed, with a higher decline in private centers (Fig. 4A). Overall, there were important disparities between the different centers. Regarding chest CT activity, there was a peak increase of + 6.6% in public centers for the first wave (8.1 to 14.7%) (Fig. 4B), whereas private centers only demonstrated a 2.6% peak increase in chest CT activity during the first wave (9.6 to 12.2%). For both public and private centers, apart from August 2020, the share of chest CT remains higher than in January and February 2020 with a 13.8% peak activity reached in March 2021 for overall activity (Fig. 4B). Throughout the third wave, activity seemed to return to a pre-pandemic level with a lower share of chest CTs for overall activity in public centers than in private centers (9.34% vs. 11.11% during September 2021).
Fig. 4.
Overall CT activity (a) and percentage of chest CTs in overall activity (b) according to the three waves. For the overall activity, January 2020 was considered as a 100% activity. The black line represents the activity of the 30 scanners. The green and red lines represent, respectively, the activity of public centers and private centers
CT dose per center
Median CTDIvol for total chest CT helical acquisitions analyzed was 6.6 mGy. Two scanners had a median that exceeded the national DRL established at 9.5 mGy (Table 1). Median DLP for total chest CT helical acquisitions analyzed was 243.8 mGy.cm. Overall, 24.5% of chest CT acquisitions exceeded the national DRL for CTDIvol (i.e., > 9.5 mGy) and only 3.8% could be considered as low-dose (LD) acquisitions (i.e., < 2.7 mGy) (Fig. 6). Regarding DLP, 10.6% exceeded national DRL (i.e., 350 mGy.cm) and only 4.3% could be considered as low-dose acquisitions (i.e., < 100 mGy.cm). Compared to the levels established in literature on the CTDIvol indicator, 24.5% acquisitions were above the DRL, 71.7% above the STDR, and only 3.8% below the LD (Fig. 6).
Fig. 6.
Tukey box plot showing the distribution of mean CTDIvol (a) per acquisition for each scanner studied. The red dotted line shows the national DRL for a chest CT acquisition, the green dotted line a dose level of a low-dose acquisition, and the blue box the range of dose acquisition considered as standard. The pie chart shows the share of each of these categories in the total acquisition of the 30 scanners for mean CTDIvol (a). Distribution of mean CTDI (b) for the 30 scanners before the COVID-19 pandemic and according to the different waves of the pandemic. The green lines show the 25° and 75° percentiles. The red lines show the medians. Mann–Whitney test was used to search statistical differences between CTDI according to the different waves, and the black stars show the p value summary (**p < 0.01; ****p < 0.0001)
CT dose per wave
Median CTDIvol was also statistically higher during the three waves compared to the pre-COVID-19 pandemic period. It increases from a value of 6.29 mGy before the COVID-19 pandemic to 6.51 mGy for the first wave (p < 0.0001), reaching a peak of 6.73 mGy in the second wave (p < 0.0001) and 6.45 mGy in the third wave (p = 0.0025) (Table 2 and Fig. 6). Median DLP was also statistically higher during the 3 waves compared to that during the pre-COVID-19 pandemic period (p < 0.0033) with a value of 234.2 mGy.cm before the COVID-19 pandemic, reaching a peak of 247.1 mGy during the third wave (Table 2). Before the COVID-19 pandemic, median effective dose (ED) was 3.3 mSv while it was 3.4 mSv throughout the first wave, 3.4 mSv during the second wave, and 3.3 mSv in the third wave (Table 2).
Discussion
The aim of this study was to evaluate the impact of the COVID-19 pandemic on chest CT practices and doses delivered during the different waves using Dose Archiving and Communication System (DACS) and public health open data.
To our knowledge, this is one of the first multicentric studies comparing the first three COVID-19 pandemic waves.
Our results show that chest CTs were increasingly used during COVID-19 pandemic with an increase of 15.6% compared to the pre-COVID activity. There was a strong and significant correlation between daily hospital admissions and daily chest CTs during the first wave. During this period, we observed heterogeneity between public and private centers, with a strong positive correlation for public centers and negative correlation for private ones. This demonstrated a higher impact of the pandemic on public structures during the first wave in our country. These correlations of daily chest CT activity with pandemic indicators were also strong and significant for the second wave. However, they were mostly positive in public and private centers, whether it was for total daily tests performed, daily incidence, or daily hospital admissions. This showed a wider participation of private centers in the management of the second wave. Conversely, these correlations were clearly lost during the third wave with only 8.9% of Rspearman > 0.3 (p < 0.05), which could be explained by the arrival of vaccination. Our analysis found a strong and significant inversed correlation between the total number of daily chest CTs performed in all centers and the vaccination rate (R = −0.8149, p < 0.0001) (Fig. 5).
Fig. 5.
R value of Spearman correlations (RSpearman) between daily chest CTs of each scanner and the corresponding departmental data of % of fully vaccinated people (2 doses)
Some centers equipped with two scanners (i.e., center 5, center 11, and center 14—Fig. 3) systematically displayed important differences and even opposite correlations with all health indicators, when comparing the two scanners’ frequencies (Fig. 6). This could be explained by the fact that one of the two scanners on the site was probably dedicated to COVID-19-related activity, following recommendations [12, 20].
During the first wave, some centers demonstrated a strong inverse correlation between the daily number of chest CTs and COVID-19 pandemic indicators. As shown earlier, most of the centers with a decreased thoracic imaging activity were private centers with a greater overall activity drop than in public centers (Figs. 2, 3, and 4). The fact that private facilities were less solicited than large public facilities could be explained at first by these results [14, 21, 22]. The increased differences between public hospitals and private centers for chest CTs in overall activity are consistent with this assumption. However, this could also be explained by the fact that unlike the second wave, the first-wave lockdown had created great disease spread disparities in the country. Accordingly, this difference strongly faded during the second wave, where the correlation between chest CT and pandemic indicators was much more homogenous (Fig. 3). This is one of the strengths of our study and of our database, which includes these two types of structures.
During the second wave, the most uniformly correlated indicator was daily total tests performed, suggesting that chest CT was still used as a screening test for COVID-19 despite the recommendations of radiology societies and health authorities [9–12]. This result is consistent with previous studies which show a strong correlation between the overall number of RT-PCRs performed and CTcovid (r = 0.73, p = 3.10−16) [14].
A remarkable point in our results is that the positive correlation between the daily number of chest CTs, total daily tests, daily incidence, and daily hospital admissions is mostly lost in the third wave (Fig. 3A). It can be explained by the strong inverse correlation we observe between the number of daily chest CTs and the rate of full-vaccination pattern (Fig. 5). Once 30% of the total population had been vaccinated, chest CT activity drops and even falls below the average activity calculated in January and February 2020. Vaccination may have led to fewer severe cases among people at risk and therefore the general population leading to fewer chest CTs performed, in line with recommendations [9–12]. Indeed, in France, vaccination was initially prioritized for the elderly and for people at risk of severe forms of COVID-19 disease.
Very few low-dose chest CTs were performed (less than 5%). Despite the fact that the diagnosis appears viable with CTDIvol of 3 mGy or less [10, 13], some studies have shown important variations in imaging practices related to COVID-19 [15–17]. Surprisingly, the comparison of global CTDIvol and DLP between the different waves and the pre-pandemic period even showed a small but significant increase in CT doses (p < 0.01). This is probably due to a slight increase in the body mass index presented by the population under care, compared to “before COVID-19.” Indeed, overweight patients are more likely to develop severe forms of disease and therefore more likely to undergo a chest CT [23]. This slight increase may be related to the morphology which leads to higher doses, due to the automatic modulation of the X-ray intensity [17]. Still, we must keep in mind that there is a part of variability in CT dose metric measurements [24, 25]. However, one study showed that even for an overweight patient cohort, a radiation exposure of only 1.3 mSv (i.e., DLP = 92.9 mGy.cm) was sufficient to diagnose or exclude COVID-19 [26]. Our study estimated the exposure of patients scanned before and during the pandemic to be around 3.4 mSv. The use of low-dose chest CTs has therefore been marginal, remains unrepresentative, and has not evolved during this period. Underuse of low-dose CT protocols is not specific to chest CTs, and other studies have shown that the use of low-dose protocols for other indications is increasing but still remains low [27]. Clearly, a joint work between radiologists and medical physicists remains to be done in order to increase the use of low-dose protocols when it seems possible. This is the application of the as low as reasonably achievable (ALARA) principle. Dose optimization is even more important considering that it has been reported that patients with COVID-19 may be exposed to multiple tests during the follow-up [28]. Furthermore, ionizing radiation from CT is classified as a carcinogen, and unlike low-dose chest CTs, standard chest CTs induce DNA double-strand breaks “which are most likely to be implicated in causing long-term mutations” [29–31].
This study highlights the importance of having multicenter radiation exposure monitoring software in several types of facilities as they offer a large amount of useful information on patient doses and practices. The radiation exposure monitoring software used in our study is open source and available to the community. This work also shows the usefulness of open-data projects.
This study has some limitations. First, even if we analyzed 30 scanners from 27 centers and 16 departments, the entire country was not fully covered with public or private centers in every department. Still, to our knowledge, this is the first report of usage of a centralized DACS implementation to objectively compare clinical practice first at a national and interregional level and also between public and private centers. Then, we analyzed the total chest CT activity and we did not know whether the examination performed was for a COVID-19 patient or not. Nevertheless, variations in daily chest CT practice throughout the different waves leave no doubt about the influence of the pandemic on chest CT workload.
Conclusion
During the first and second waves, chest CT activity was highly correlated to the indicators of the COVID-19 pandemic. However, this correlation was lost during the third wave, concomitantly to the rise of vaccination rates. Ultimately and despite recommendations, low-dose chest CT use has remained marginal during the pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We greatly appreciated the help and support of the whole ALARA, Fibermetrix, and Bicetre Hospital staff.
Funding
The authors state that this work has not received any funding.
Declarations
Guarantor
The scientific guarantor of this publication is Ramiro Moreno.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: ALARA and Fibermetrix.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board (IRB number: CRM-2202-233).
Ethical approval
Institutional Review Board approval was obtained. (IRB number: CRM-2202-233)
Methodology
• retrospective
• observational
• multicenter study
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Olivier Meyrignac and Clément Devic equally contributed to the manuscript.
References
- 1.Zhou P, Yang X-L, Wang X-G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.(2022) COVID-19 Map Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html
- 4.Gostic K, Gomez AC, Mummah RO, et al (2020) Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. eLife 9:e55570. 10.7554/eLife.55570 [DOI] [PMC free article] [PubMed]
- 5.Ducray V, Vlachomitrou AS, Bouscambert-Duchamp M, et al. Chest CT for rapid triage of patients in multiple emergency departments during COVID-19 epidemic: experience report from a large French university hospital. Eur Radiol. 2021;31:795–803. doi: 10.1007/s00330-020-07154-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296:E115–E117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296:E32–E40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herpe G, Lederlin M, Naudin M, et al. Efficacy of chest CT for COVID-19 pneumonia diagnosis in France. Radiology. 2021;298:E81–E87. doi: 10.1148/radiol.2020202568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology. 2020;296:172–180. doi: 10.1148/radiol.2020201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalra MK, Homayounieh F, Arru C, et al. Chest CT practice and protocols for COVID-19 from radiation dose management perspective. Eur Radiol. 2020;30:6554–6560. doi: 10.1007/s00330-020-07034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American College of Radiology (2020) ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
- 12.Haute Autorité de Santé (2020) HAS, Réponses rapides dans le cadre de la COVID-19 - Place du scanner thoracique
- 13.Kang Z, Li X, Zhou S. Recommendation of low-dose CT in the detection and management of COVID-2019. Eur Radiol. 2020;30:4356–4357. doi: 10.1007/s00330-020-06809-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herpe G, Naudin M, Léderlin M, et al. COVID-19 impact assessment on the French radiological centers: a nationwide survey. Eur Radiol. 2020;30:6537–6544. doi: 10.1007/s00330-020-07035-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blažić I, Brkljačić B, Frija G. The use of imaging in COVID-19—results of a global survey by the International Society of Radiology. Eur Radiol. 2021;31:1185–1193. doi: 10.1007/s00330-020-07252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Homayounieh F, Holmberg O, Umairi RA, et al. Variations in CT utilization, protocols, and radiation doses in COVID-19 pneumonia: results from 28 countries in the IAEA study. Radiology. 2021;298:E141–E151. doi: 10.1148/radiol.2020203453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernardo M, Homayounieh F, Cuter MCR, et al (2021) Chest CT usage in Covid-19 pneumonia: multicenter study on radiation doses and diagnostic quality in Brazil. Radiat Prot Dosimetry 197:135–145. 10.1093/rpd/ncab171 [DOI] [PMC free article] [PubMed]
- 18.Ohana M, Ludes C, Schaal M, et al. Quel avenir pour la radiographie thoracique face au scanner ultra-low dose ? Rev Pneumol Clin. 2017;73:3–12. doi: 10.1016/j.pneumo.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 19.ICRP (2007) The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP 37(2–4) [DOI] [PubMed]
- 20.Ding J, Fu H, Liu Y, et al. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020;30:3603–3608. doi: 10.1007/s00330-020-06850-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.FNMR (2020) CRISE COVID-19 – Au front de la pandémie pour maintenir la continuité des soins pour tous(tes) les patient(e)s, l’imagerie médicale libérale est en grave péril
- 22.Cavallo JJ, Forman HP. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020;296:E141–E144. doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang Y, Lu Y, Huang Y-M et al (2020) Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism 113:154378. 10.1016/j.metabol.2020.154378 [DOI] [PMC free article] [PubMed]
- 24.Taylor S, Van Muylem A, Howarth N, et al. CT dose survey in adults: what sample size for what precision? Eur Radiol. 2017;27:365–373. doi: 10.1007/s00330-016-4333-3. [DOI] [PubMed] [Google Scholar]
- 25.Vanaudenhove T, Van Muylem A, Howarth N, et al. CT diagnostic reference levels: are they appropriately computed? Eur Radiol. 2019;29:5264–5271. doi: 10.1007/s00330-019-06141-8. [DOI] [PubMed] [Google Scholar]
- 26.Steuwe A, Rademacher C, Valentin B, et al. Dose-optimised chest computed tomography for diagnosis of coronavirus disease 2019 (COVID-19) - evaluation of image quality and diagnostic impact. J Radiol Prot. 2020;40:877–891. doi: 10.1088/1361-6498/aba16a. [DOI] [PubMed] [Google Scholar]
- 27.Weisenthal K, Karthik P, Shaw M, et al. Evaluation of kidney stones with reduced-radiation dose CT: progress from 2011–2012 to 2015–2016-not there yet. Radiology. 2018;286:581–589. doi: 10.1148/radiol.2017170285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yurdaisik I, Nurili F, Aksoy SH, et al. Ionizing radiation exposure in patients with COVID-19: more than needed. Radiat Prot Dosimetry. 2021;194:135–143. doi: 10.1093/rpd/ncab092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United Nations Scientific Comittee on the Effects of Atomic Radiation (2012) UNSCEAR report: biological mechanisms of radiation actions at low doses. A white paper to guide the Scientific Comittee’s future programme of work. https://www.unscear.org/docs/publications/2012/UNSCEAR_2012_Report.pdf
- 30.Lee C. Managing radiation dose from chest CT in patients with COVID-19. Radiology. 2021;298:E158–E159. doi: 10.1148/radiol.2020204129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sakane H, Ishida M, Shi L, et al. Biological effects of low-dose chest CT on chromosomal DNA. Radiology. 2020;295:439–445. doi: 10.1148/radiol.2020190389. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.