Abstract
Background:
Healthcare workers are vulnerable to burnout, especially during the COVID-19 pandemic in the low resource settings. Belize is a small Central American developing country known for its chronic healthcare worker shortage and this is the first study to assess burnout prevalence and its associated factors among healthcare workers in Belize.
Aim:
To evaluate the prevalence of burnout and its associated factors in HCWs in Belize covering multiple domains (mental health, physical symptoms, and coping behaviors) during the COVID-19 pandemic.
Methods:
A cross-sectional survey that was developed and validated by a panel of experts was delivered online to all the healthcare workers in Belize from September to November 2021. Burnout was assessed using Copenhagen Burnout Inventory. Depression and anxiety screening was carried out using the Patient Health Questionnaire – 2 (PHQ-2) and Generalized Anxiety Disorder 2-item (GAD-2). Burnout associated factors were estimated using logistic regression models.
Findings:
Of the total of 263 participants, 27.76% had overall burnout: 56.65% had personal, 54.37% had work-related, and 19.39% had patient-related burnout. Burnout was positively associated with anxiety (OR: 3.14 [1.67, 5.92]), depression (OR: 4.45 [2.30, 8.61]), intentions of quitting their jobs (OR: 2.59 [1.49, 4.51]), health status worsening (OR: 2.21 [1.26, 3.87]), multiple physical symptom presentation (OR: 1.19, [1.10, 1.29]), and use of multiple maladaptive coping behaviors (OR: 1.66, [1.30, 2.12]).
Interpretation:
Healthcare workers in Belize showed substantial levels of burnout which were significantly associated with using maladaptive coping behaviors, presenting multiple physical symptoms, quitting their jobs, health status worsening, and other mental health issues. These findings should be used to develop and implement programs such as regular health check-ups, health promotion awareness campaigns, and worker recruitment strategies which would improve the working conditions, quality of life, and psychological well-being of our healthcare workers.
Keywords: Healthcare workers, Belize, doctors, nurses, pandemic, covid-19, burnout, mental health, anxiety, depression
Introduction
Exposure to high levels of stress in healthcare workers (HCWs) make them prone to experiencing burnout – a chronic occupational stress that has not been successfully managed. Burnout has three main dimensions – emotional exhaustion, depersonalization, and feelings of reduced accomplishment (Ruotsalainen et al., 2015; World Health Organization, 2019). Burnout estimates in HCWs can reach up to 80.5% (Lindblom et al., 2006; Rotenstein et al., 2018). Exposure to a variety of occupational stressors, such as high work load, time pressure, shift working, patient outcome uncertainty, and constant exposure to suffering and dying patients contribute to HCW burnout (McVicar, 2003; Ruotsalainen et al., 2015). Burnout has been linked with higher risks of mental disorders and chronic diseases on the individual level (Salvagioni et al., 2017). Workplace consequences of burnout, specific to healthcare workers, include higher medical errors, patient mortality, and decreased professional work effort resulting in compromised patient safety and poor quality of care (Hall et al., 2016; Shanafelt et al., 2010, 2012; Tawfik & Ioannidis, 2020). Organizational consequences include increased sick leave, staff turnover, and brain drain, which may collapse already strained healthcare systems and increase healthcare costs (Shanafelt et al., 2002, 2010; Shirom et al., 2006; Tawfik et al., 2018).
Since December 2019, Coronavirus disease (COVID-19) has rapidly spread worldwide and as of July 2022, there has been more than half a billion confirmed cases and 6 million confirmed deaths reported globally (World Health Organization, 2022). As seen in previous disease outbreaks, HCW burnout levels have been exacerbated due to heightened levels of stress, anxiety, fear, and uncertainty (Magnavita et al., 2021). COVID-19 pandemic increased the prevalence of burnout among HCWs by up to 80% in some settings when compared to the pre-pandemic era (Morgantini et al., 2020). Most studies on burnout have been conducted in high-income countries (HICs), and the overall single-point prevalence of burnout in 20 low-and middle-income countries (LMICs) during the COVID-19 pandemic ranged from 2.5% to 87.9% (Wright et al., 2022). Such substantial variability could be due to the differences in definitions and assessment methods.
Burnout risk factors and early indicators in HCWs include socio-demographic characteristics such as age, gender, marital status, and profession, however the results are often inconsistent and contradictory, which may be attributable to differences in culture, context, and setting (Cañadas-De la Fuente et al., 2015). Previous studies show that HCWs are hesitant to seek mental health support in the workplace for fear of stigma or harm to their professional career (Gold et al., 2016). Both stress and burnout have been linked to physical symptom manifestations (Chatani et al., 2021). Furthermore, studies have shown that the type of coping behavior when dealing with stress can have a direct influence on burnout (Ben-Zur, 2009; Hastings & Brown, 2002).
Belize is a LMIC in Central America that has long had a significant unmet need for health services, exacerbated by the ongoing COVID-19 pandemic and its chronic shortage of HCWs (Mac Arthur & Woodye, 2014). Studies regarding HCWs mental health have never been done in Belize before. We therefore aimed to evaluate the prevalence of burnout and its associated factors in HCWs in Belize covering mental health, physical symptoms, and coping behaviors to fill the current knowledge gap. The results of this study may provide direction for policy makers and administrators to improve wellbeing of HCWs and prevent burnout in an already strained healthcare system.
Methods
This cross-sectional study was conducted between 27th Septemberand 29th November 2021. The online questionnaire was developed and validated by a panel of experts that included a medical doctor, nurse, psychologist, and health economist. It was distributed nationwide to all practicing healthcare workers in Belize. Participants were required to provide informed consent prior to answering the questionnaire. Institutional ethical approval was obtained from the Ministry of Health in Belize (GEN/147/01/21[17] Vol. V) and from the National Yang-Ming Chiao Tung University Institutional Review Board in Taiwan (YM110116E).
Burnout was assessed using the Copenhagen Burnout Inventory (CBI), a publicly available validated tool comprised of nineteen 5-point Likert scale items measuring both physical and emotional exhaustion as the primary driver affecting burnout in three dimensions: personal, work-related, and client/patient-related burnout. A score of 50 or more is the cut-off for prevalence estimate for high burnout (Kristensen et al., 2005). Physical symptoms perceived were evaluated using a 9-point Likert scale adapted from a previous study (Chatani et al., 2021). Physical symptoms were defined as those experienced ‘once a week or more’ and summed up as the number of symptoms experienced which included headache, eye symptoms, dizziness, nausea, vomiting, diarrhea, constipation, abdominal pain, musculoskeletal pain, articular pain, backache, chest pain, palpitations, dyspnea, insomnia, and fatigue. Depression and anxiety screening was carried out using the Patient Health Questionnaire – 2 (PHQ-2) and Generalized Anxiety Disorder 2-item (GAD-2), which are both 2-item tools with cut-off scores of 3 (Kroenke et al., 2003; Skapinakis, 2007). Questions regarding coping behaviors were adapted from the Australian National Mental Health Survey (Petrie et al., 2020).
Individual characteristics included socio-demographic information such as age, sex, marital status, district of residence, nationality, having children, profession, and specialty. Other characteristics such as medical history, perceived health status (pre- and post-pandemic), and the number of hours of sleep in the past 30 days were collected. Work-related characteristics such as length of employment in current position, working hours per week, work region, type of work facility, type of shift work, type of ward, COVID-19 unit, and intentions of quitting job were also included. In terms of COVID-related factors, participants were asked whether they received any COVID-19 vaccine, had been diagnosed with COVID-19, and if any family member had been diagnosed with COVID-19.
Statistical analysis
Descriptive statistics were used to summarize burnout prevalence and the distribution of socio-demographic, work-related, and COVID-19 related factors. One-way analysis of variance was used for the analysis of burnout according to the sociodemographic information, profession, work conditions, and level of job strain. Comparisons between categorical variables were performed by chi-square or Fisher’s exact tests, where appropriate.
The association between burnout and each potential risk factor was explored by estimating unadjusted odds ratios (ORs) and 95% confidence interval (CIs) using univariate logistic regression models. Subsequently, multivariable logistic regressions for the same outcomes gave adjusted ORs and 95% CIs. The significance level was set at p-value = .05. Additionally, the number of physical symptoms was expressed as a score and showed the association between the number of symptoms and burnout. Similarly, coping behaviors were summarized and expressed as a score and showed the association between each additional adaptive or maladaptive coping strategy. Cases with the missing data (<1%) were omitted in the analysis. All statistical analyses were carried out with the Stata statistical software: Release 16 (StataCorp, 2019. College Station, TX: StataCorp LP).
Results
Overall burnout was observed in 27.8% of the study population, whereas burnout dimensions were distributed as follows: personal burnout (56.7%), work-related burnout (54.4%), and patient-related burnout (19.4%).
The analytical sample included 263 respondents, with a mean age of 37.4 (±10) years. Most of the participants were female (69.2%), Belizean (90.5%), in a committed relationship (65.0%), resided in the Belize district (45.6%), and had a mean work experience of 10.8 years. Most of the participants were medical doctors (58.9%), followed by nurses (34.6%). The participants worked an average of 47 hr/week, most were employed in the Central Health Region (52.1%) and were required to work night shifts (62.0%).
Burnout group had a significantly higher percentage of women (59 [80.8%] vs. 123 [64.7%]; p = .011), who were younger (34.6 vs. 38.5 years; p = .004), had less work experience (8.9 years vs. 11.5 years; p = .056), more respondents with intentions of quitting their job (57.5% vs. 34.7%; p = .001), health worsening (63.0% vs. 44.2%; p = .019), and screened positively for anxiety (34.3% vs. 14.2%; p ⩽ .001) and depression (35.6% vs. 11.1%; p ⩽ .001) compared with the group without burnout (Table 1).
Table 1.
Comparison of demographic characteristics of healthcare workers with and without burnout.
| Population characteristics | No. (%) or mean (±SD) | |||
|---|---|---|---|---|
| With overall burnout (n = 73, 27.8%) | Without overall burnout (n = 190, 72.2%) | Total (N = 263) | p-Value* | |
| Female | 59 (80.8) | 123 (64.7) | 182 (69.2) | .011 |
| Age (years) | 34.6 (±8.4) | 38.5 (±10.4) | 37.4 (±10.0) | .004 |
| Occupation | ||||
| Medical doctor | 33 (45.2) | 122 (64.2) | 155 (58.9) | .003 |
| Nurse | 37 (50.7) | 54 (28.4) | 91 (34.6) | |
| Other † | 3 (4.1) | 14 (7.4) | 17 (6.5) | |
| Marital Status | ||||
| Single | 21 (28.8) | 50 (26.3) | 71 (27.0) | .733 |
| Married/Committed | 45 (61.6) | 126 (66.3) | 171 (65.0) | |
| Other ‡ | 7 (9.6) | 14 (7.4) | 21 (8.0) | |
| District reside | ||||
| Belize | 35 (48.0) | 84 (44.2) | 119 (45.6) | .343 |
| Cayo | 19 (260) | 43 (22.6) | 62 (23.6) | |
| Corozal | 9 (12.3) | 14 (7.4) | 23 (8.8) | |
| Orange Walk | 3 (4.1) | 20 (10.5) | 23 (8.8) | |
| Stann Creek | 2 (2.7) | 15 (7.9) | 17 (6.5) | |
| Toledo | 4 (5.5) | 10 (6.3) | 14 (5.3) | |
| Has children | 42 (57.5) | 117 (61.6) | 159 (60.5) | .548 |
| Belizean | 67 (91.8) | 171 (90.00) | 238 (90.5) | .664 |
| Comorbidity § | 23 (31.5) | 45 (23.7) | 68 (25.9) | .194 |
| Work Institution | .146 | |||
| Public | 52 (71.2) | 108 (56.8) | 160 (60.8) | |
| Private | 13 (17.8) | 50 (26.3) | 63 (24.0) | |
| Both | 7 (9.6) | 30 (15.8) | 37 (14.1) | |
| Work Region | ||||
| Central | 43 (58.9) | 94 (49.5) | 137 (52.1) | .343 |
| Western | 17 (23.3) | 41 (21.6) | 58 (22.1) | |
| Northern | 7 (9.6) | 26 (13.7) | 33 (12.6) | |
| Southern | 6 (8.2) | 24 (12.6) | 30 (11.4) | |
| Work Experience (years) | 8.9 (±7.9) | 11.5 (±10.4) | 10.8 (±9.8) | .056 |
| Work hours per week | 47.6 (±11.7) | 47.6 (±11.7) | 47.6 (±11.7) | .979 |
| Works night shifts | 46 (63.0) | 117 (61.9) | 163 (62.0) | .950 |
| Sleep duration per night (hr) | 5.8 (±1.2) | 6.1 (±1.2) | 6.0 (±1.2) | .085 |
| Considered quitting job | 42 (57.5) | 66 (34.7) | 108 (41.1) | .001 |
| Health status worsened during the pandemic | 46 (63.0) | 84 (44.2) | 130 (49.4) | .019 |
| Anxiety ¶ | 25 (34.3) | 27 (14.2) | 52 (19.8) | <.001 |
| Depression ¶ | 26 (35.6) | 21 (11.1) | 47 (17.9) | <.001 |
| Treated COVID-19 positive patients | 61 (83.6) | 160 (84.2) | 221(84.0) | .430 |
| Worked in COVID-19 isolation unit | 37 (50.7) | 96 (50.5) | 133 (50.6) | .735 |
| Been diagnosed with COVID-19 | 21 (28.8) | 49 (25.8) | 70 (26.6) | .516 |
| Family member with COVID-19 | 43 (58.9) | 111 (58.4) | 154 (58.6) | .999 |
| Received COVID-19 vaccine | 69 (94.5) | 183 (96.3) | 252 (95.8) | .598 |
Includes personal care assistants, nursing supervisors, dentists.
Includes divorced, separated, and widowed.
Comorbidity was evaluated through question ‘Do you suffer from any underlying health conditions (e.g. diabetes, hypertension)?’
Anxiety was evaluated using the generalized anxiety disorder 2-item (GAD-2) and depression was evaluated using the patient health questionnaire − 2 (PHQ-2).
p-Values were obtained by chi-squared or Fisher’s exact tests, for categorical variables, and by two-samples t-test for continuous variables. Bold indicates the significance of p<.005.
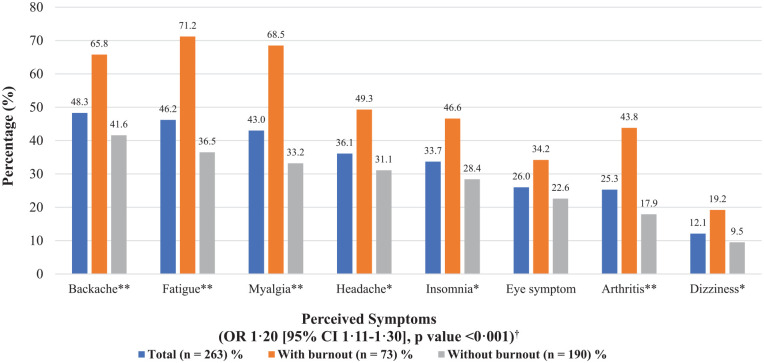
The distribution of the eight most common physical symptoms reported in those with or without burnout is visualized in Figure 1. Backache was the most commonly reported physical symptom perceived once a week or more often by 48.3% of the participants, followed by fatigue (46.2%), and myalgia (43.0%). Perception of multiple physical symptoms was significantly associated with burnout. Additionally, the number of physical symptoms was expressed as a score and showed the association between the number of symptoms and burnout. For each additional physical symptom, the odds of burnout increased by 20% (OR 1.20, 95% CI [1.11, 1.30], p < .001).
Figure 1.
Physical symptoms perceived once in a week or more of healthcare workers with or without burnout (N = 263).
*p-value < .05. **p-value < .01. ***p-value < .001.
†Odds ratio expresses increase in odds of burnout for each additional physical symptom.
Table 2 shows the adaptive and maladaptive coping behaviors of healthcare workers with and without burnout. Maladaptive coping behaviors such as eating more than usual (p = .003), drinking more alcohol than usual (p = .009), and taking non-prescribed medication (p < .001) were significantly associated with burnout. Behaviors were summarized and expressed as a score and for each additional maladaptive coping behavior, the odds of burnout increased by 66% (OR 1.66, 95% CI [1.30, 2.12]; p: <.001). However, no difference was seen in terms of adaptive coping behaviors between those with and without burnout.
Table 2.
Coping behaviors of healthcare workers with or without burnout.
| Total (N = 263) | With burnout (n = 73) | Without burnout (n = 190) | p-Value* | |
|---|---|---|---|---|
| % | % | % | ||
| Adaptive coping behaviors (OR 1.01, 95% CI [0.83, 1.23], p-value: .925) † | ||||
| Try to look on the bright side of things | 97.3 | 100 | 96.3 | .096 |
| Do something enjoyable | 96.6 | 97.3 | 96.3 | .696 |
| Talk to others | 89.3 | 93.2 | 87.8 | .211 |
| Pray | 89.3 | 86.3 | 90.5 | .327 |
| Jog or do other exercise | 84.0 | 78.1 | 86.2 | .106 |
| Seek spiritual help | 63.4 | 69.9 | 60.9 | .174 |
| Practice meditation or yoga | 39.1 | 32.9 | 41.5 | .201 |
| Maladaptive Coping Behaviors (OR 1.66, 95% CI [1.30, 2.12], p-value: <.001) † | ||||
| Avoid being with others | 85.1 | 87.7 | 84.1 | .470 |
| Take yourself to bed | 85.1 | 91.8 | 82.4 | .058 |
| Eat more than usual | 83.5 | 94.5 | 79.3 | .003 |
| Drink more alcohol than usual | 44.7 | 57.5 | 39.7 | .009 |
| Take non-prescribed medication | 24.1 | 45.2 | 15.9 | <.001 |
| Smoke more cigarettes than usual | 6.5 | 5.6 | 6.9 | .699 |
Note. CI = confidence interval; OR = odds ratio
p-Values were obtained by crude logistic regression.
Odds ratio expresses increase in odds of burnout for each additional coping behavior.
Bold indicates the significance of p<.005.
The results of multiple regression analysis of risk factors of overall burnout are shown in Table 3. The crude odds ratios (Table 3, model 1) showed significantly higher odds of burnout for female healthcare workers (OR 2.29, 95% CI [1.19, 4.42]) and nurses (OR 2.53, 95% CI [1.44, 4.47]). Burnout was also associated with physical symptoms, maladaptive coping behaviors, health status worsening, dropout intentions, anxiety, and depression. After adjusting for potential covariates (age and sex) in Model 2 and using doctors as the comparison group, burnout prevalence was still significantly higher among nurses (OR 1.98, 95% CI [1.07, 3.65], p = .03). Adjustment for marital status and profession in Model 3 did not influence the direction and significance of the associations.
Table 3.
Crude and adjusted odds ratios of burnout in healthcare workers (N = 263).
| Model 1 OR (95% CI) N = 263 | Model 2 OR (95% CI) N = 263 | Model 3 OR (95% CI) N = 263 | |
|---|---|---|---|
| Age | 0.96 [0.93, 0.99] | ||
| Sex | |||
| Male | 1 [Reference] | ||
| Female | 2.29 [1.19, 4.42] | ||
| Marital status | |||
| Single | 1 [Reference] | 1 [Reference] | |
| Committed/Married | 0.85 [0.46, 1.57] | 1.08 [0.57, 2.05] | |
| Other | 1.02 [0.35, 3.02] | 1.72 [0.56, 5.24] | |
| Occupation | |||
| Doctor | 1 [Reference] | 1 [Reference] | |
| Nurse | 2.53 [1.44, 4.47] | 1.98 [1.07, 3.65] | |
| Other | 0.79 [0.22, 2.92] | 0.90 [0.21, 2.98] | |
| Number of physical symptoms | 1.19 [1.10, 1.29] | 1.16 [1.07, 1.26] | 1.17 [1.07, 1.27] |
| Number of adaptive coping behaviors | 1.01 [0.83, 1.23] | 0.97 [0.79, 1.20] | 0.97 [0.78, 1.20] |
| Number of maladaptive coping behaviors | 1.66 [1.30, 2.12] | 1.59 [1.23, 2.05] | 1.59 [1.21, 2.07] |
| Health status worsened | 2.21 [1.26, 3.87] | 1.86 [1.04, 3.33] | 2.09 [1.15, 3.80] |
| Dropout intentions | 2.59 [1.49, 4.51] | 2.07 [1.16, 3.69] | 2.15 [1.20, 3.87] |
| Anxiety | 3.14 [1.67, 5.92] | 3.09 [1.61, 5.92] | 3.18 [1.64, 6.16] |
| Depression | 4.45 [2.30, 8.61] | 4.26 [2.17, 8.40] | 4.23 [2.13, 8.38] |
Note. CI = confidence interval; OR = odds ratio.
Model 1: crude analysis.
Model 2: adjusted for age, sex.
Model 3: adjusted for age, sex, marital status, and profession group.
Bold indicates the significance of p <.005.
Discussion
In this study we evaluated prevalence of burnout and its associated factors in HCWs in Belize during the COVID-19 outbreak. Our findings identified potential associations between burnout and socio-demographic, physical, mental, and behavioral factors.
More than half of the study population had personal and work-related burnout, as seen with prevalence of 56.7% and 54.4%, respectively. Similarly, a study carried out in the northern bordering country of Mexico found that 49.8% of all healthcare workers reported burnout (Juarez-Garcia et al., 2022). The overall prevalence in our study falls within the range of other assessments conducted during the COVID-19 pandemic, with estimates ranging from 2.5% to 87.9% (Prasad et al., 2021; Wright et al., 2022). Such wide range can be explained by differences in assessment methods, cultural attitudes and epidemiological context of the pandemic.
Absence of burnout assessment before the COVID-19 pandemic in Belize does not allow for comparison with pre-pandemic estimates. In the neighboring country of Guatemala, a study that assessed burnout in medical students found that rates of burnout were high and increased during the pandemic, when compared to pre-pandemic levels (Ruiz et al., 2022). This is in line with recent studies, which confirm similar trends (Morgantini et al., 2020). Cultural and socio-economic differences need to be considered when comparing studies. A recent study in 3,766 medical students from twelve countries across five continents showed that burnout variations are strongly influenced by cultural factors, especially in terms of societal structures, attitudes, religion and sources of stress (Molodynski et al., 2021).
Socio-demographic characteristics such as age, sex, and profession were associated with burnout. Burnout was inversely associated with age, which may be attributed to younger workers having less work experience, knowledge, and ability to adapt to work requirements and demand (Marchand et al., 2018). Younger HCWs also tend to have a more ‘idealistic’ and empathic approach when compared to their older peers (Leo et al., 2021). Younger HCWs would be considered at higher risk and would therefore benefit from more trainings, especially in disease outbreak preparedness. Sex was also correlated with burnout with females being twice more likely to develop burnout than males in the study population. This could also be partially explained due to the greater percentage of females (69.20%) in this study population. It can also be linked to the female predominance in patient-facing roles, gender discrimination, gender expectations in care, and balancing work with home responsibilities (Prasad et al., 2021). Additionally, there may be social pressure, cultural factors, and biological factors that contribute to this association (McPeek-Hinz et al., 2021; Wiederhold et al., 2018). However, this correlation is often debated and would depend on study and cultural setting, assessment tool, and burnout component (Galanis et al., 2021). Nurses were twice more likely to develop burnout than medical doctors in this study, even when controlling for age and sex. Many factors may contribute to this, such as nurses being required to work longer hours and overtime shifts due to the current nurse shortage in Belize as well as their closer proximity and contact with patients and their caregivers, especially in the COVID-19 isolation units. This is comparable to other studies that also revealed a similar association (Chirico et al., 2021). These socio-demographic risk factor findings are consistent with reviews and meta-analyses, which showed that younger female nurses with less clinical experience are more vulnerable to adverse mental health effects (Galanis et al., 2021; Sikaras et al., 2022; Sriharan et al., 2021).
Perception of multiple physical symptoms was associated with higher burnout levels. This can be supported by previous studies that demonstrated burnout impact on physical symptoms, especially fatigue, insomnia, chronic pain or discomfort, and also suggest multiple physical symptoms might be useful for identifying high-risk individuals of burnout (Barello et al., 2020; Chatani et al., 2021). Since burnout is a result of high and chronic levels of stress, it is no surprise that physical symptoms of stress, including myalgias and fatigue, would also be associated to burnout. Furthermore, past studies have identified dose-response relationship between burnout and physical symptoms such as fatigue and myalgias (Shirom, 2009). This study showed that the most frequent symptoms – backache, fatigue, and myalgias – were significantly associated with burnout. This may be incorporated in a practical manner when screening healthcare workers during their periodical health check-ups to identify that those with multiple physical symptoms may be at high risk of burnout and require early interventions and support.
Additional to burnout, HCWs experience several other negative psychological impacts during the COVID-19 pandemic which include depression and anxiety that was found to be significantly associated with burnout. The tools used in this study were only initial screening tools, therefore further clinical assessment may be needed to verify our findings. This would be consistent with other studies that demonstrate a significant association between burnout and depression and burnout and anxiety, and that have established that these are different and robust constructs though they may share similar characteristics. Though related, further longitudinal research to establish causal relationships is needed to investigate whether burnout can predict depression or anxiety and vice versa (Koutsimani et al., 2019).
Lastly, coping behaviors in HCWs were also explored in this study. Regrettably, coping behaviors used by HCWs are often not the most favorable for dealing with stress and preserving a healthy work-life balance. Research has shown that they are usually reluctant to seek assistance from others, employ maladaptive coping behaviors, and ignore burnout signs and symptoms. This results in them ignoring their own health, delaying necessary medical treatment, and avoiding problems that may affect patient quality of care (King et al., 1992). The most common coping behaviors employed by the participants included trying to look on the bright side of things, doing something enjoyable, talking to others, and praying, all of which are considered adaptive coping behaviors and were not significantly associated with burnout. This requires further research to determine type of adaptive coping behaviors and burnout component to better understand this relationship. Maladaptive coping behaviors, on the other hand, such as eating more than usual, drinking more alcohol than usual, and taking non-prescribed medication were significantly associated with burnout. For each additional maladaptive coping behavior, the odds of burnout increased by 66%. This is consistent with research conducted in other jobs where the use of maladaptive coping behaviors constitutes a risk for burnout and that coping is an important determinant in an individual’s everyday wellbeing (Ben-Zur, 2009; Hastings & Brown, 2002). A study investigating burnout in emergency physicians at three Caribbean teaching hospitals found that burnout levels increased among participants that used alcohol daily, consumed recreational drugs, and sleeping aids (Lovell et al., 2022). Nevertheless, the effects of coping behavior merits further research. Through awareness campaigns and training sessions, effective adaptive coping behaviors can be taught and encouraged while highlighting the negative impacts of maladaptive coping behaviors in this population.
Healthcare administrators must take note of these results and develop strategies to hire more healthcare workers while implementing staff retention programs to incentivize and motivate their employees. Healthcare workers and the organizations that train and employ them must recognize the early signs of stress and burnout, adopt adaptive coping behaviors, and maintain a culture wherein work-life balance and healthcare well-being are shared goals. Interventions, incentives, and support should be designed with at-risk groups such as those healthcare workers that are younger, females, and nurses as priority. Moreover, among those with burnout, more than half of the healthcare workers had intentions of quitting their jobs which were significantly higher when compared to the group without burnout, which is higher than the one-third of registered nurses with burnout who reported intentions to quit their jobs found in a large cross-sectional study carried out in the US (de Cordova et al., 2022). This is alarming since they may contribute to a vicious cycle of burnout in this population. Existing literature also confirms that burnout is indeed a significant predictor of intentions to quit their jobs (Bourdeanu et al., 2020). Burnout was also associated with perceived health status worsening during the COVID-19 pandemic, with approximately two-thirds that experienced their health status worsening during the pandemic. Since burnout reflects a process of depleting energy resources, it is reasonable to make this association. This is of concern since several meta-analytic studies concluded that self-reported health is the most representative construct on one’s own health and is an important predictor of mortality (Shirom, 2009).
The study results need to be interpreted within the acknowledged limitations. It must be mentioned that due to the cross-sectional design of the study it is not possible to infer causal relationships though important associations were observed. In addition, although the findings of this study may not be generalizable to other countries, providing the initial information on Belize might be also relevant to other LMICs that share similar cultures regionally. The online format of the study has its own limitations such as response bias, uncertainty of the population to which they are distributed, and low response rate, although our survey was able to capture 35% of the entire national healthcare worker population in Belize.
Further research should evaluate other individual factors such as ethnicity and income as well as the role of environmental and systemic factors on burnout and the impact of intervention strategies as well as the economic and financial burden of burnout. Future studies can include longitudinal and post-pandemic studies to assess the changes in the prevalence of burnout. Interventional studies can also be performed that focus on burnout alleviation and prevention, which should focus on a systems approach as well as protective factors (Goroll, 2020).
Conclusions
There are significant levels of burnout among healthcare workers in Belize. Burnout should be the focus of concern for health authorities and policy makers due to its impact on the physical and psychological well-being of HCWs. During a disease outbreak, healthcare workers are exposed to higher levels of work and stress that may yield many long-lasting consequences. At-risk groups included those healthcare workers who were younger, females, and nurses. Furthermore, increased number of physical symptoms was associated with increased odds of burnout therefore through regular health check-ups, healthcare workers who are burnt out can be identified through their somatic symptom presentation. Other associations with burnout included the use maladaptive coping behaviors, intentions of quitting their jobs, health status worsening, and other mental health issues. These findings should be used to develop and implement strategies to manage existing burnout and prevent future burnout in HCWs. Adequate training, health promotion awareness campaigns, and worker recruitment strategies would improve the working conditions, quality of life, and psychological well-being of our HCWs.
Acknowledgments
The authors gratefully thank National Yang-Ming Chiao Tung University, the International Cooperation and Development Fund (Taiwan ICDF), the Ministry of Health of Belize, Belize Medical and Dental Association, and Belize Nurses’ Association for their support.
Footnotes
Contributors: All authors were responsible for the design, acquisition, analysis, and interpretation of data. All authors critically revised the manuscript an approved the final version.
Data accessibility statement: Data available on request due to privacy/ethical restrictions
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Lila Estephan  https://orcid.org/0000-0002-3328-5490
https://orcid.org/0000-0002-3328-5490
References
- Barello S., Palamenghi L., Graffigna G. (2020). Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Research, 290, 113129. 10.1016/j.psychres.2020.113129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zur H. (2009). Coping styles and affect. International Journal of Stress Management, 16, 87–101. 10.1037/a0015731 [DOI] [Google Scholar]
- Bourdeanu L., Pearl Zhou Q., DeSamper M., Pericak K. A., Pericak A. (2020). Burnout, workplace factors, and intent to leave among hematology/oncology nurse practitioners. Journal of the Advanced Practitioner in Oncology, 11(2), 141–148. 10.6004/jadpro.2020.11.2.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cañadas-De la Fuente G. A., Vargas C., San Luis C., García I., Cañadas G. R., De la Fuente E. I. (2015). Risk factors and prevalence of burnout syndrome in the nursing profession. International Journal of Nursing Studies, 52(1), 240–249. 10.1016/j.ijnurstu.2014.07.001 [DOI] [PubMed] [Google Scholar]
- Chatani Y., Nomura K., Hiraike H., Tsuchiya A., Okinaga H. (2021). Multiple physical symptoms are useful to identify high risk individuals for burnout: A study on faculties and hospital workers in Japan. International Journal of Environmental Research and Public Health, 18(6), 3246. 10.3390/ijerph18063246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico F., Ferrari G., Nucera G., Szarpak L., Crescenzo P., Ilesanmi O. (2021). Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: A rapid umbrella review of systematic reviews. J Health Soc Sci, 6(2), 209–220. [Google Scholar]
- de Cordova P. B., Johansen M. L., Grafova I. B., Crincoli S., Prado J., Pogorzelska-Maziarz M. (2022). Burnout and intent to leave during COVID-19: A cross-sectional study of New Jersey hospital nurses. Journal of Nursing Management, 30, 1913–1921. 10.1111/jonm.13647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. (2021). Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Advanced Nursing, 77(8), 3286–3302. 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold K. J., Andrew L. B., Goldman E. B., Schwenk T. L. (2016). “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. General Hospital Psychiatry, 43, 51–57. [DOI] [PubMed] [Google Scholar]
- Goroll A. H. (2020). Addressing burnout-focus on systems, not resilience. JAMA Network Open, 3(7), e209514. 10.1001/jamanetworkopen.2020.9514 [DOI] [PubMed] [Google Scholar]
- Hall L. H., Johnson J., Watt I., Tsipa A., O’Connor D. B. (2016). Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS One, 11(7), e0159015. 10.1371/journal.pone.0159015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings R. P., Brown T. (2002). Coping strategies and the impact of challenging behaviors on special educators’ burnout. Mental Retardation, 40(2), 148–156. [DOI] [PubMed] [Google Scholar]
- Juárez-García A., Girardo C., Converso D. (2022). Organizational wellbeing in CSOs in Morelos (Mexico): Findings from a qualitative study. Università di Torino. [Google Scholar]
- King M. B., Cockcroft A., Gooch C. (1992). Emotional distress in doctors: Sources, effects and help sought. Journal of the Royal Society of Medicine, 85(10), 605–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutsimani P., Montgomery A., Georganta K. (2019). The relationship between burnout, depression, and anxiety: A systematic review and meta-analysis. Frontiers in Psychology, 10, 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen T. S., Borritz M., Villadsen E., Christensen K. B. (2005). The Copenhagen burnout inventory: A new tool for the assessment of burnout. Work and Stress, 19(3), 192–207. 10.1080/02678370500297720 [DOI] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. (2003). The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Leo C. G., Sabina S., Tumolo M. R., Bodini A., Ponzini G., Sabato E., Mincarone P. (2021). Burnout among healthcare workers in the COVID 19 era: A review of the existing literature. Public Health Frontier, 9, 750529. 10.3389/fpubh.2021.750529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindblom K. M., Linton S. J., Fedeli C., Bryngelsson I.-L. (2006). Burnout in the working population: Relations to psychosocial work factors. International Journal of Behavioral Medicine, 13(1), 51–59. [DOI] [PubMed] [Google Scholar]
- Lovell L. M. P., Atherley A. E., Watson H. R., King R. D. (2022). An exploration of burnout and resilience among emergency physicians at three teaching hospitals in the English-speaking Caribbean: A cross-sectional survey. The Lancet Regional Health-Americas, 15, 100357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mac Arthur I. N., Woodye J., M., (2014). Quality improvement of health care in Belize: Focusing on results. Inter-American Development Bank. [Google Scholar]
- Magnavita N., Chirico F., Garbarino S., Bragazzi N. L., Santacroce E., Zaffina S. (2021). SARS/MERS/SARS-CoV-2 outbreaks and burnout syndrome among healthcare workers. An umbrella systematic review. International Journal of Environmental Research and Public Health, 18(8), 4361. 10.3390/ijerph18084361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand A., Blanc M.-E., Beauregard N. (2018). Do age and gender contribute to workers’ burnout symptoms? Occupational Medicine, 68(6), 405–411. 10.1093/occmed/kqy088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPeek-Hinz E., Boazak M., Sexton J. B., Adair K. C., West V., Goldstein B. A., Alphin R. S., Idris S., Hammond W. E., Hwang S. E., Bae J. (2021). Clinician burnout associated with sex, clinician type, work culture, and use of electronic health records. JAMA Network Open, 4(4), e215686. 10.1001/jamanetworkopen.2021.5686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McVicar A. (2003). Workplace stress in nursing: A literature review. Journal of Advanced Nursing, 44(6), 633–642. 10.1046/j.0309-2402.2003.02853.x [DOI] [PubMed] [Google Scholar]
- Molodynski A., Lewis T., Kadhum M., Farrell S. M., Lemtiri Chelieh M., Falcão De Almeida T., Masri R., Kar A., Volpe U., Moir F., Torales J., Castaldelli-Maia J. M., Chau S. W. H., Wilkes C., Bhugra D. (2021). Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. International Review of Psychiatry, 33(1–2), 37–42. [DOI] [PubMed] [Google Scholar]
- Morgantini L. A., Naha U., Wang H., Francavilla S., Acar O., Flores J. M., Crivellaro S., Moreira D., Abern M., Eklund M., Vigneswaran H. T., Weine S. M. (2020). Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS One, 15(9), e0238217. 10.1371/journal.pone.0238217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie K., Crawford J., LaMontagne A. D., Milner A., Dean J., Veness B. G., Christensen H., Harvey S. B. (2020). Working hours, common mental disorder and suicidal ideation among junior doctors in Australia: A cross-sectional survey. BMJ Open, 10(1), e033525. 10.1136/bmjopen-2019-033525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad K., McLoughlin C., Stillman M., Poplau S., Goelz E., Taylor S., Nankivil N., Brown R., Linzer M., Cappelucci K., Barbouche M., Sinsky C. A. (2021). Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine, 35, 100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz R., Fernandes D. A., Vásquez A., Trigueros A., Pemberton M., Gnanapragasam S. N., Torales J., Ventriglio A., Bhugra D. (2022). Prevalence of burnout in medical students in Guatemala: Before and during Covid-19 pandemic comparison. International Journal of Social Psychiatry. Advance online publication. 10.1177/00207640221077015 [DOI] [PubMed]
- Rotenstein L. S., Torre M., Ramos M. A., Rosales R. C., Guille C., Sen S., Mata D. A. (2018). Prevalence of burnout among physicians: A Systematic Review. The Journal of the American Medical Association, 320(11), 1131–1150. 10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruotsalainen J. H., Verbeek J. H., Mariné A., Serra C. (2015). Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews, 2015(4), CD002892. 10.1002/14651858.cd002892.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvagioni D. A. J., Melanda F. N., Mesas A. E., González A. D., Gabani F. L., Andrade S. M. (2017). Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS One, 12(10), e0185781. 10.1371/journal.pone.0185781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T. D., Balch C. M., Bechamps G., Russell T., Dyrbye L., Satele D., Collicott P., Novotny P. J., Sloan J., Freischlag J. (2010). Burnout and medical errors among American surgeons. Annals of Surgery, 251(6), 995–1000. 10.1097/sla.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Boone S., Tan L., Dyrbye L. N., Sotile W., Satele D., West C. P., Sloan J., Oreskovich M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archive of Internal Medicine, 172(18), 1377–1385. 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Bradley K. A., Wipf J. E., Back A. L. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136(5), 358–367. [DOI] [PubMed] [Google Scholar]
- Shirom A. (2009). Burnout and health: Expanding our knowledge. Stress and Health, 25(4), 281–285. 10.1002/smi.1283 [DOI] [Google Scholar]
- Shirom A., Nirel N., Vinokur A. D. (2006). Overload, autonomy, and burnout as predictors of physicians’ quality of care. Journal of Occupational Health Psychology, 11(4), 328–342. [DOI] [PubMed] [Google Scholar]
- Sikaras C., Ilias I., Tselebis A., Pachi A., Zyga S., Tsironi M., Gil A. P. R., Panagiotou A. (2022). Nursing staff fatigue and burnout during the COVID-19 pandemic in Greece. AIMS Public Health, 9(1), 94–105. 10.3934/publichealth.2022008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skapinakis P. (2007). The 2-item generalized anxiety disorder scale had high sensitivity and specificity for detecting GAD in primary care. Evidence-Based Medicine, 12(5), 149. 10.1136/ebm.12.5.149 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2019). Stata statistical software: Release 16. StataCorp LLC. [Google Scholar]
- Sriharan A., West K. J., Almost J., Hamza A. (2021). COVID-19-related occupational burnout and moral distress among nurses: A rapid scoping review. Nursing Leadership (Toronto, Ont.), 34(1), 7–19. [DOI] [PubMed] [Google Scholar]
- Tawfik D. S., Ioannidis J. P. A. (2020). Evidence relating health care provider burnout and quality of care. Annals of Internal Medicine, 172(6), 438–439. 10.7326/L19-0827 [DOI] [PubMed] [Google Scholar]
- Tawfik D. S., Profit J., Morgenthaler T. I., Satele D. V., Sinsky C. A., Dyrbye L. N., Tutty M. A., West C. P., Shanafelt T. D. (2018). Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic Proceedings, 93(11), 1571–1580. 10.1016/j.mayocp.2018.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiederhold B. K., Cipresso P., Pizzioli D., Wiederhold M., Riva G. (2018). Intervention for physician burnout: A systematic review. Open Medicine, 13, 253–263. 10.1515/med-2018-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2019). Burn-out an “occupational phenomenon”: International classification of diseases. Retrieved April from https://bit.ly/2RmL1ll
- World Health Organization. (2022). WHO COVID-19 dashboard. Retrieved July19 from https://covid19.who.int/
- Wright T., Mughal F., Babatunde O. O., Dikomitis L., Mallen C. D., Helliwell T. (2022). Burnout among primary health-care professionals in low- and middle-income countries: Systematic review and meta-analysis. Bulletin of the World Health Organization, 100(6), 385–401a. 10.2471/BLT.22.288300 [DOI] [PMC free article] [PubMed] [Google Scholar]