Abstract
Background
During the Covid-19 health crisis, telerehabilitation provided a solution to ensure the continuity of care. Since then, it has been offered as an alternative to face-to-face rehabilitation in chronic conditions. Data measuring satisfaction are essential to adapt and increase the effectiveness of this type of programme.
Aim and scope
This research focused on determining the most significant determinants of participant satisfaction in a telerehabilitation programme.
Methods
We conducted a retrospective study by analysing the satisfaction questionnaire used from the start of the programme.
Result
Two hundred and ten (210) participants completed the programme; 180 questionnaires were filled in and 175 analyzed of which 70 with chronic low back pain (CLBP), 59 for multiple sclerosis (MS) and 22 with parkinson's disease (PD). Satisfaction was high for all participants (scoring out of 10, mean = 8.22 sd = 1.53), but the determinants reported for the three main conditions involved in the programme differed. Main determinant was “benefice” for CLBP (p = 1.23e-05), “home exercises adapted” for MS (p = 0.000679) and “interest in staying at home” for PD (p = 1.84e-05).
Conclusion
Depending on the context of the condition/disease, the drivers of satisfaction were not identical. Knowledge of these determinants will allow us to further improve the programme. However, some unresolved questions remain regarding the place of therapists, their role and the skills required for a successful telerehabilitation programme. Further studies are required to understand the impact.
Keywords: tele rehabilitation, chronic low back pain, acceptability, neurological desorder, satisfaction
Introduction
For chronic disorders, neurological or musculoskeletal, failure to receive routine rehabilitative care has potential implications for disease progression as well as functional deterioration and psychological distress (1). For these patients,, the negative effects of social distancing may be even greater, as they require regular follow-up to minimize the impact of the disease (2). Exercise therapy has been defined as a series of movements designed to train or develop the body through routine practice or as a physical workout to promote good physical health. They may contain for upper or lower limb: muscle power training, task based training, endurance components or muscle power balance training (3, 4). The implementation of these treatments involves several health professionals, physiotherapists, occupational therapists, but also psychologists to monitor the impact of the disease on mental health. These programs must be adapted to the level of functional independence, fatigability or age.
In the context of SARS-CoV-2 infection and the spread of the COVID-19 pandemic, health services needed to adapt and prioritize the provision of safe care, thus limiting outpatient services. We therefore needed to design an innovative method to offer a rehabilitation programme and ensure the continuity of care (5, 6). Telerehabilitation, which is still uncommon, has emerged as a potential solution. Telehealth is ideal when caring for transmissible conditions thus reducing person-to-person contact (7). It allows therapists to: (1) maintain continuity of care by educating patients through remote consultations directly in their own environment, (2) conduct a physical evaluation and plan a targeted therapeutic exercise programme, and (3) monitor the progress of patients by providing ongoing feedback and follow-up (8–10).
Since all therapists are familiar with face-to-face treatment, several stumbling blocks remain for the roll-out of telerehabilitation programmes. In terms of disadvantages, a problem could be the loss of human contact, face-to-face interaction, with the therapist (11). In fact, it is recognised that the effectiveness of physiotherapy relies not only on direct interventions but also on other contextual factors intrinsic to the experience of patients at the rehabilitation center or practice (12). In addition, during the clinical examination, the inability to palpate the patient and use other tests as diagnostic tools could compromise the follow-up process and objective assessment of the condition of patient or result in a failure to recognise warning signs (9, 13). Equipment problems such as lack of rehabilitation tools (elastic bands, weights, devices) could limit the provision of care and reduce the range of therapeutic exercises (9). Moreover Safety is a major concern to remote physiotherapy, in particular because of the limited possibility of direct intervention by the operator (14). telemedicine encounters are more vulnerable to privacy and security risks (15).
The question of the effectiveness of telerehabilitation was therefore raised very early on and numerous studies have examined the issue of effectiveness (16–20). In the area of neurological rehabilitation, most studies report no difference between face-to-face and telerehabilitation in terms of balance, functionality and quality of life (21). In musculoskeletal areas and especially in chronic lower back pain, the published literature is heterogeneous and that digital intervention studies for low back pain are generally poorly described. The literature does not provide sufficient detail regarding target and participant populations, intervention components, and rationale for the wide variety of outcome measures used. This makes it difficult to get a clear overview of what might work best, for whom, and under what circumstances (22–24).
On 17 March 2020, the French population went into lockdown to combat the COVID-19 epidemic. This was followed by successive waves of lockdowns and lifting of restrictions that lasted until the summer of 2022. Healthcare teams decided to offer patients the option to continue their rehabilitation via synchronous remote consultations combined with self-rehabilitation exercises. The aim was to bring intensive, interdisciplinary and personalized rehabilitation care into the home of the patient. The question of acceptability and patient satisfaction was therefore raised in a context of restricted choice. Moving forwards, knowledge regarding the level of satisfaction and its determinants will be used to assess and adapt the programme. The aim of this study is to assess the level of satisfaction of participants, to highlight the variables predicting satisfaction levels and to make assumptions regarding possible predictors not measured in our survey.
Method
Switch from face-to-face to remote consultations in a health-emergency context
Based on the face-to-face day hospital model, the programme consisted of one 30-minute session, three days a week, over a period of four weeks. These individual or collective sessions were provided by at least three different types of professionals such as physiotherapists, occupational therapists and adapted physical education teachers. The goal was to recreate at home the rehabilitation care set up in a rehabilitation center: intervention of various professionals (physiotherapist, occupational therapist, sports educator) with a care program focused on each patient face to face. Patients with low back pain received 5 individual sessions and 4 group sessions per week. Patients with neurological diseases received 4 individual sessions and 5 group sessions. Thus, each patient had two or three sessions per day. The session duration was 30 min for individual and 45 min for group. Depending on the patient, other professionals were involved including psychologists, neuropsychologists, social workers, dieticians or speech therapists. At the end of the programme, each patient was reviewed by the prescribing doctor during a teleconsultation. Patients were grouped together according to their condition: chronic lower back pain or neurological disorder (multiple sclerosis, Parkinson's disease or others). Each group was composed of three patients. To perform the telerehabilitation, the therapist and patient each needed a computer or a tablet with a camera. A smartphone can be used but the size of the screen is inadequate for group sessions. We recommended to patients that they should have a mat on the floor for some exercises but this was not essential. The baseline assessment was used to set the goals of the program and to establish the kind of exercises to be included in the training program. A self-education handbook, co-designed with the patient and the therapists, included the selected exercises. The posture of the exercises was selected according to the patient's abilities and preferences (standing, sitting, lying on the bed or on the floor). For patients with low back pain, exercises focused on muscle strengthening, stretching, relaxation and reducing kinesiophobia. For patients with neurological disorders, the exercises were task-oriented, balance improvement, strengthening and stretching.
At each session, the E-Kermed videoconferencing software (a specific videoconferencing platform for the health sector developed for the Brittany region) sent the patient a connection link by email. No software needed to be installed. A connection test was carried out before each session to ensure to check the adequacy of the connection.
The content of the sessions depended on the targets determined with the patient at the beginning of the session. The rehabilitation specialists performed a personalized assessment using validated scales where possible (Oswestry for lower back pain patients, EMIF for multiple sclerosis patients). Daily utensils were very often used as rehabilitation equipment including chairs, stairs, water bottles instead of dumbbells, etc.
Construction of an assessment grid
A questionnaire was quickly prepared to collect patients' satisfaction on their course of treatment.
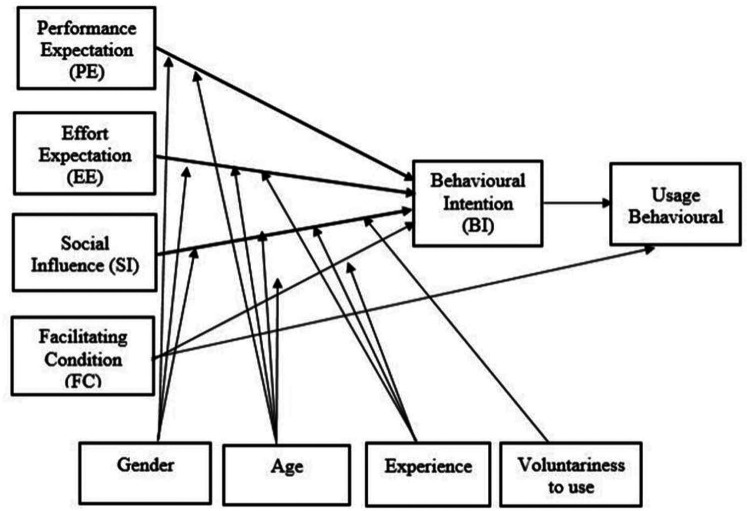
Satisfaction can be considered as the result of a judgment, of a cognitive process, of comparison between the expectations of the subject and the perceived reality (25). Then a series of questions based on the UTAUT were associated with satisfaction to study the determinants. The UTAUT model (Figure 1) uses four core determinants to determine users behavioral intention (BI) to use a technology: Performance expectancy (PE), effort expectancy (EE), social influence (SI) and facilitating conditions (FC) (26). These four major factors are defined as follows: Performance expectancy as “degree to which an individual believes that using the system will help him or her to attain gains in job performance”, effort expectancyas “degree of ease associated with use of the system”,social influence as “degree to which an individual perceives that important others believe he or she should use the new system” and facili-tating conditions as “degree to which an individual believes that an organizational and technical infrastructure exists to support use of the system”. Gender, age, experience, and voluntariness of use are moderating variables assumed to influence the four key variables on usage intention and behavior. The UTAUT theoretical model is derived from eight previous models of technology acceptance. The urgency required for setting up a digital day hospital meant no work was carried out on quality of the questionnaire. Moreover, it was not tested to assess its internal consistency. However, the research teams, familiar with UTAUT, quickly identified issues that could pose stumbling blocks to patient satisfaction (Table 1). Three main dimensions were included but social influence were not able to use due to the health restrictions.Indeed, the confinement did not leave the choice of the participants towards the alternative of face to face. Each question took the form of a Likert scale with parameters ranging from 0 to 10. The final question was an open-ended question about their rehabilitation programme. The questionnaire was upload on-line as a Google form with a link sent at the end of the treatment. Due to the non-secure nature of the questionnaire, responses were anonymous and no health data was requested, It was therefore impossible to analyze the results according to the moderating variables (gender, age)
Figure 1.
UTAUT model (26), available via license: CC bY-NC 4.0.
Table 1.
Presentation of the questionnaire – link between items and UTAUT dimensions.
| Number | Description | UTAUT correspondence |
|---|---|---|
| Q1 | How would you rate your overall satisfaction with the programme? | Effort expectancy |
| Q2 | How would you rate your ease participation given the remote system set up? | Facilitating conditions |
| Q3 | How would you rate the ease of connecting for the first time? | Facilitating conditions |
| Q4 | How would you rate the ease of connecting the next times? | Facilitating conditions |
| Q5 | How would you rate the value of doing the programme at home? | Performance expectancy |
| Q6 | How do you rate the value of remote activities compared to the same activities face-to-face? | Performance expectancy |
| Q7 | How would you rate the value of the inclusion of group activities in addition to individual sessions? | Performance expectancy |
| Q8 | How would you rate the perceived physical intensity of this programme? | Performance expectancy |
| Q9 | How do you rate the relevance of the self-rehabilitation exercises proposed? | Performance expectancy |
| Q10 | Did you find the self-rehabilitation exercises appropriate for your needs? | Performance expectancy |
| Q11 | Did you find the daily length of the self-rehabilitation exercises appropriate? | Performance expectancy |
| Q12 | Did you find the difficulty of the self-rehabilitation exercises appropriate? | Performance expectancy |
| Q13 | How would you rate your perceived benefit from this programme (your experience)? | Performance expectancy |
| Q14 | Do you think you will continue with the self-rehabilitation exercises after this 4-week programme? | Intention to use |
| Q15 | Would you recommend this day hospital programme to other people with the same needs? | Intention to use |
Method of recruiting participants
During the medical consultation, the doctor assessed the potential compliance of the patient, his/her wishes, ability to use the digital tools, connection, indication and need to set up self-exercises. Method of recruiting participants During the medical consultation, the doctor assessed the potential compliance of the patient, his/her wishes, ability to use the digital tools, connection, indication and need to set up self-exercise.For neurological disorders, the patients recruited had an EDSS of less than 5 for MS and a Hoehn and Yahr score of 3 or less for Parkinson's disease. For low back pain an initial bio-psycho-social assessment using the Dallas scale excludes patients with excessive psycho-behavioral impact.
Data collection and analysis method
Data were analysed in R static version 4.01 via Rstudio. Data collection and analysis method Data were analyzed in R static version 4.01 via Rstudio. Cronbach's alpha coefficients was use post hoc to study internal consistency of questionnaire. Bayesian information criterion (BIC) was used as a criterion for model selection among a finite set of models (27). With the criteria resulting from BIC calculation, a linear model (estimated using Ordinary Least Squares, OLS) was perform to predict satisfaction.
Result
Participants
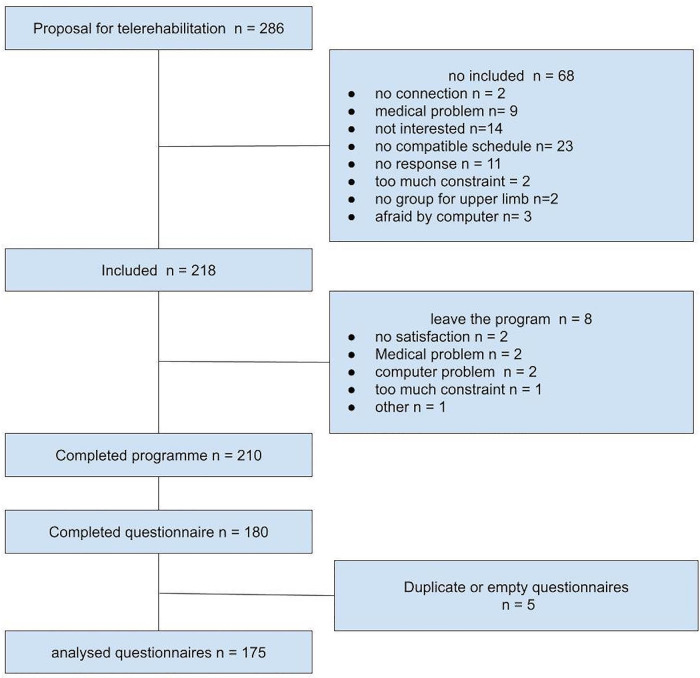
Between 17/04/2020 and 29/08/2022, 218 patients were enrolled in the programme, 210 completed the four weeks, 180 questionnaires were completed, five of which were duplicates. Overall, 175 usable questionnaires were analyzed (Figure 2). Out of a total of 218 patients enrolled, 109 were with low back pain (LBPGroupe), 56 with multiple sclerosis (MSGroupe), 34 with Parkinson‘s disease (PDGroupe) and 19 for other diseases. The majority of patients were female for LBPG (55.99%) and MSG (83.35%) and male for PDG (61.8%) The mean age and standard deviation was for LBPG 48.01 (11.00), MSG 49.48 (11.05) and for PDG 67.41 (7.16).
Figure 2.
Flow chart: program integration of patients.
Results of the questionnaire
Validation of the questionnaire was done post-hoc. Standardised Cronbach coefficient was calculated and is excellent 0.93 [0.91; 0.94]. Questionnaire show a very good internal consistency.
The results showed a good overall level of satisfaction (Table 2): mean(sd) = 8.22 (1.53). In the questions, the lowest score corresponded to the assessment of physical intensity, mean(sd) = 7.53 (1.54), the highest to self-rehabilitation exercises mean(sd) = 8.73 (1.86). The intention to recommend the programme was high, mean(sd) = 8.37 (1.82).
Table 2.
Means and standard deviation of questions, score between 0 (very bad) and 10 (very good), see Table 1 for the definition of questions, N = 175.
| Number | Mean (sd) |
|---|---|
| Q1 | 8.22 (1.53) |
| Q2 | 8.00 (1.80) |
| Q3 | 7.86 (2.39) |
| Q4 | 8.42 (1.87) |
| Q5 | 8.24 (1.74) |
| Q6 | 7.41 (2.01) |
| Q7 | 7.73 (2.28) |
| Q8 | 7.53 (1.54) |
| Q9 | 8.69 (1.30) |
| Q10 | 8.73 (1.86) |
| Q11 | 8.23 (1.42) |
| Q12 | 8.44 (1.52) |
| Q13 | 7.89 (1.97) |
| Q14 | 8.51 (1.50) |
| Q15 | 8.37 (1.82) |
Satisfaction analysis of the entire population
Post-hoc analyses were carried out on the prediction of satisfaction using the other pre-event questions. We used ANOVA to compare differences of means among diseases by examining the amount of variability between the samples relative to the amount of variability within the samples. No difference of satisfaction was observed.
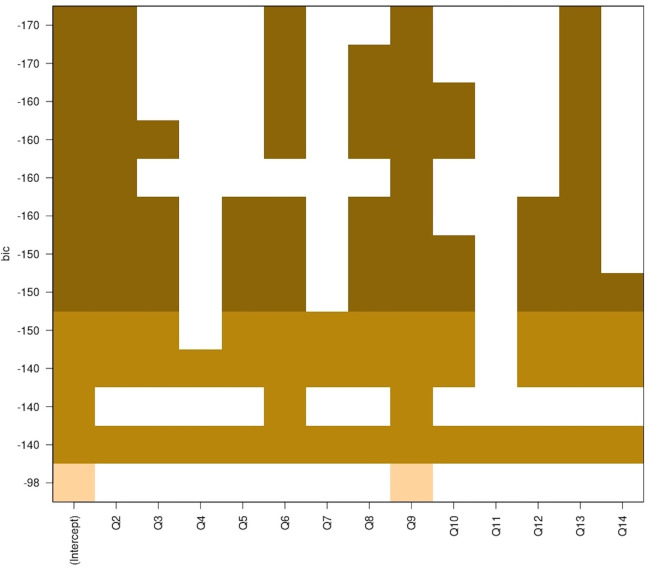
A Bayesian information criterion (BIC) was performed to select the best predictive criterion (Figure 3). Then, a linear regression was performed to model the relationship between “satisfaction” (dependent variable) and the other questions (explanatory variable).
Figure 3.
Bayesian criterion information, likelihood of predictive satisfaction combinations.
Thus, several variables were not considered to be predictive of satisfaction (Table 3), i.e.,: the length of the sessions p value = 0.61; the ease of the first connection p value = 0.20, the ease of the connections p value = 0.83, group activities p value = 0.16.
Table 3.
Linear model of predictive values on satisfaction, pooled sample.
| Coefficients | Estimate | Std. Error | t value | Pr (>|t|) |
|---|---|---|---|---|
| (Intercept) | 0.61842 | 0.48228 | 1.282 | 0.20155 |
| Facilite | 0.2041 | 0.04706 | 4.337 | 2.52e-05 *** |
| Interetprogramme | 0.11166 | 0.06235 | 1.791 | 0.07515. |
| Rapportpresentiel | 0.12107 | 0.05687 | 2.129 | 0.03475 * |
| Intesitephysique | 0.1064 | 0.05438 | 1.957 | 0.05209. |
| Autoreeducationadapt | 0.22934 | 0.06579 | 3.486 | 0.00063 *** |
| Benefice | 0.17048 | 0.04951 | 3.443 | 0.00073 *** |
| Multiple R-squared: 0.6756, Adjusted R-squared: 0.6638, p-value: < 2.2e-16 | ||||
Signif. codes: 0 “***” 0.001 “**” 0.01 “*” 0.05 “.” 0.1 “ ” 1, Facile = facilitation of use, Intereteduprogramme = interest to be at home, rapportpresentiel = interest of programme and exercice compare to presentiel, intensitephysique = physical intensity adapted, autoreeducationadaptée = home exercices adapted, benefice = effect size feeling, N = 175.
After refining the model by eliminating the non-predictive variables, the regression model retained three major variables predicting satisfaction (Table 2): ease of use (p value = 2.52e-05), adapted self-rehabilitation (p value = 0.0006) and the perceived benefit (p value = 0.00073). Plus three minor variables: relationship to face-to-face (p value = 0.03475), interest of the programme of being at home (p value = 0.07515) and physical intensity (p value = 0.05209).
Analysis of satisfaction by disease
A variable elimination procedure was conducted to refine the linear regression model by condition. Three groups sufficiently represented in the sample were selected (Table 4): chronic lower back pain (LBP, n = 70), Parkinson's disease patients (PARK, n = 22) and multiple sclerosis patients (MS, n = 59). The refined models showed that ease of use was an item shared by all patients. However, for the performance expectancy dimension, the predictive points for satisfaction diverged. The LBP group emphasized the perceived benefit of the programme (p value = 1.23e-05), the MS group the relevance of the self-rehabilitation exercises (p value = 0.00068) and the PARK group the benefit offered by the programme of being at home (p value = 1.84e-05) and the exercises relative to their expectations. The variance explained was very high in the PARK group (Adjusted R-squared: 0.7914, p-value: 1.322e-07), moderate for the MS group (Adjusted R-squared: 0.5103 p-value: 3.072e-09, and high for the group LBP (Adjusted R-squared: 0.66, p-value: 7.659e-15).
Table 4.
Linear model of predictive values on satisfaction.
| Coefficients | Estimate | Std. Error | t value | Pr (>|t|) |
|---|---|---|---|---|
| LBP n = 70 (Intercept) | 0.56318 | 0.77203 | 0.729 | 0.46837 |
| Facilite | 0.26235 | 0.091 | 2.883 | 0.005359 ** |
| Interetprogramme | 0.32493 | 0.08209 | 3.958 | 0.000192 *** |
| Faciliteconnection1 | −0.1353 | 0.05689 | −2.378 | 0.020416 * |
| Intesitephysique | 0.20706 | 0.09199 | 2.251 | 0.027842 * |
| Benefice | 0.29179 | 0.06154 | 4.742 | 1.23e-05 *** |
| Multiple R-squared: 0.6846, Adjusted R-squared: 0.66 p-value: 7.659e-15 | ||||
| MS n = 59 (Intercept) | 0.2360 | 1.0877 | 0.217 | 0.829002 |
| Facilite | 0.3214 | 0.1026 | 3.133 | 0.002772 ** |
| Autoreeducationadapte | 0.4260 | 0.1183 | 3.602 | 0.000679 *** |
| Benefice | 0.2114 | 0.1009 | 2.096 | 0.040652 * |
| Multiple R-squared: 0.5356, Adjusted R-squared: 0.5103 p-value: 3.072e-09 | ||||
| PARK: n = 22 (Intercept) | 1.75680 | 0.68099 | 2.580 | 0.01836 * |
| Facilite | 0.29153 | 0.07555 | 3.859 | 0.00106 ** |
| Interetprogramme | 0.53394 | 0.09424 | 5.666 | 1.84e-05 *** |
| Multiple R-squared: 0.8112, Adjusted R-squared: 0.7914 p-value: 1.322e-07 | ||||
LBP, low back pain, MS, multiple sclerosis, PARK, Parkinson's disease. Signif. Codes: 0 “***” 0.001 “**” 0.01 “*” 0.05 “.” 0.1 “ ” 1, Facile = facilitation of use, Intereteduprogramme =, rapportpresentiel = interest of programme and exercice compare to face to face, intensitephysique = physical intensity adapted, autoreeducationadaptée = home exercices adapted, benefice = effect size feeling.
Analysis of the open-ended text
91 participants responded to the open-text question amounting to a total of 5,168 words. The open-ended text was analyzed using Rstudio, Text Mining Package V 0.7.9 and Wordcloud V 2.6. The analysis of word occurrences listed the 17 most frequently used words (Table 5), represented as a word cloud.
Table 5.
Analysis of the occurrence of vocabulary used in the open-ended text, the 17 most frequent words Physiotherapists and occupational therapists were grouped together under the term therapist.
| Word | Freq |
|---|---|
| très (very) | 47 |
| séance(s) (session(s) | 41 |
| bien, bonne (well) | 41 |
| programme (programme) | 36 |
| plus (more) | 28 |
| exercices (exercises) | 26 |
| merci (thank) | 26 |
| intervenants (therapists) | 24 |
| tout (all) | 21 |
| temps (time) | 20 |
| être (to be) | 15 |
| faire (doing) | 14 |
| moins (less) | 13 |
| rééducation (rehabilitation) | 13 |
| travail (work) | 11 |
| semaines (week) | 10 |
Under the term “therapist”, we grouped together the different names of therapists, sometimes by first name, last name, or simply named as therapists (physiotherapist, occupational therapist, etc.).
Discussion
The results corroborate the high level of satisfaction with telerehabilitation in chronic conditions (28–33). These results corroborate that tele-rehabilitation not only provides access to rehabilitation programs, but also reinforces participant-centered treatment, adherence to rehabilitation and lifestyle changes over time (34). A systematic review (n = 44 studies) investigating the association between telehealth and patient satisfaction found that patients were satisfied when using telehealth programmes, as they produce similar outcomes, are easy to use, improve communication and reduce travel time (35). Our study provided additional information on the key predictors of satisfaction and showed that not all patients have the same sensitivity to the features of the devices and that these differences were related to the condition of the patient. These results are consistent with the feedback received from patients during medical consultations. The population of MS patients are younger and place a high value on self-rehabilitation in unsupervised conditions. Parkinson's patients find it very hard to travel and remote exercising solutions offer them an interesting alternative. The LBP group, unlike the other two, do not suffer from a progressive illness and their condition improves with treatment, meaning that they were more aware of the perceived benefit.
However, the explained variance study reported the presence of other predictive factors not revealed by the questionnaire, especially for the MS group, whose explained variance was only 0.51.
Place and role of therapists
The analysis of the open-ended text reveals a dimension not explored by the questionnaire, i.e., the place of therapists. This word was placed in eighth position among the most commonly used words in the analysis of the open-ended text. Compared to studies on e-learning, therapists may have a significant impact on the success of telerehabilitation. The predictive criteria mentioned in e-learning are: the position of the therapist in terms of distance learning (36, 37), their skills in the area of new communication techniques (38), their capacity for appropriate feedback (38, 39) and the quality of their oral expression (40). These criteria could be transferable to telerehabilitation, as they were associated with other dimensions in the questionnaire such as ease of use, motivation of the subjects (41). This key role of therapists in success has been discussed in studies of other conditions such as COPD (29).
Adverse effects
The teams reported three minor and non-serious falls out of a total of 1,744 supervised sessions. This low rate probably related to the selection criteria and the caution of therapists in terms of the difficulty of the exercises.
Cost
No costing was carried out, however, given the location of the participants, it was calculated that approximately 73,000 transport kilometers were saved. Moreover, no specific investment was required. Some patients took the opportunity to invest in standard communication equipment, but the vast majority already had a good internet connection and a screen. In terms of equipment, everyday objects available in the home were used. This programme therefore provides economic arguments in favor of its widespread roll-out.
Limitation
Some descriptive information and health data are missing that would have allowed work on subgroups.
From a sampling perspective, while the lower back pain and MS groups were sufficiently large, the sample size of the PARK group was small.
Finally, there was a sample selection bias. The programme was based on voluntary participation and the presence of operational connection equipment.
Conclusion
The high level of satisfaction of patients is consistent with the scientific literature. Various determinants were highlighted in our study according to the condition involved. The rarity of adverse events and the low economic set-up cost are positive drivers for the widespread roll-out of such programmes. However, some questions remain, in particular about the role of therapists and their associated skills in the success of these programmes. In addition, long-term follow-up is required to study patient adaptation and acceptance in a normalised health context.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Datasets are available on request: The raw data supporting the conclusions of this article will be made available by the authors. Requests to access these datasets should be directed to patrice.piette@pole-sthelier.com.
Author contributions
The authors confirm contribution to the paper as follows: study conception and design: PG, AD, BF; Data collection: ALR, VL; Analysis and interpretation of results: PP, BF, PGAD, ALR; Draft manuscrit: PP. Preparation: PP, BF, VL. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Liguori S, Moretti A, Paoletta M, Gimigliano F, Iolascon G. Rehabilitation of neuromuscular diseases during COVID-19: pitfalls and opportunities. Front Neurol. (2021) 12:626319. 10.3389/fneur.2021.626319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maciel FKL, Grossklauss LF, Favero FM, Sá CDSC. Neuromuscular diseases and social distance resulting from the COVID-19 pandemic. Arq Neuropsiquiatr. (2022) 80(7):712–7. 10.1055/s-0042-1755232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heine M, van de Port I, Rietberg MB, van Wegen EE, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. (2015) 2015(9):CD009956. 10.1002/14651858.CD009956.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uhrbrand A, Stenager E, Pedersen MS, Dalgas U. Parkinson's disease and intensive exercise therapy–a systematic review and meta-analysis of randomized controlled trials. J Neurol Sci. (2015) 353(1-2):9–19. 10.1016/j.jns.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 5.Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. (2020) 100:1260–4. 10.1093/ptj/pzaa093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bettger JP, Resnik LJ. Telerehabilitation in the age of COVID-19: an opportunity for learning health system research. Phys Ther. (2020) 100:1913–6. 10.1093/ptj/pzaa151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. (2020) 56(11):1069–75. 10.1177/1357633X20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galea MD. Rééducation (rehabilitation)13. Arch Phys Med Rehabil. (2019) 47(4):318–22. 10.1016/j.pmr.2018.12.002 [DOI] [Google Scholar]
- 9.Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. (2018) 49(3):381–5. 10.1038/sc.2010.103 [DOI] [PubMed] [Google Scholar]
- 10.Nizeyimana E, Joseph C, Plastow N, Dawood G, Louw QA. A scoping review of feasibility, cost, access to rehabilitation services and implementation of telerehabilitation: implications for low- and middle-income countries. Digital Health. (2022) 8:20552076221131670. 10.1177/20552076221131670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. (2017) 4(2):e7. 10.2196/rehab.7511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geri T, Viceconti A, Minacci M, Testa M, Rossettini G. Manual therapy: exploiting the role of human touch. Musculoskelet Sci Pract. (2019) 47(4):318–22. 10.1016/j.msksp.2019.07.008 [DOI] [PubMed] [Google Scholar]
- 13.Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. (2021) 17(2):218–21. 10.1016/j.nurpra.2020.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bianchini E, Onelli C, Morabito C, Alborghetti M, Rinaldi D, Anibaldi P, et al. Feasibility, safety, and effectiveness of telerehabilitation in mild-to-moderate Parkinson's disease. Front Neurol. (2022) 13:909197. 10.3389/fneur.2022.909197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cascella M, Marinangeli F, Vittori A, Scala C, Piccinini M, Braga A, et al. Open issues and practical suggestions for telemedicine in chronic pain. Int J Environ Res Public Health. (2021) 18(23):12416. 10.3390/ijerph182312416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johansson T, Wild C. Telerehabilitation in stroke care–a systematic review. J Telemed Telecare. (2009) 47(9):651. 10.1258/jtt.2010.100105 [DOI] [PubMed] [Google Scholar]
- 17.Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: a review of the literature. J Stroke Cerebrovasc Dis. (2018) 56(11):1069–75. 10.1016/j.jstrokecerebrovasdis.2018.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jansson MM, Rantala A, Miettunen J, Puhto AP, Pikkarainen M. The effects and safety of telerehabilitation in patients with lower-limb joint replacement: a systematic review and meta-analysis. J Telemed Telecare. (2022) 56(11):1069–75. 10.1177/1357633X20917868 [DOI] [PubMed] [Google Scholar]
- 19.Almojaibel AA. Delivering pulmonary rehabilitation for patients with chronic obstructive pulmonary disease at home using telehealth: a review of the literature. Saudi J Med Med Sci. (2016) 56(11):1069–75. 10.4103/1658-631X.188247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, et al. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed J E Health. (2017) 56(11):1069–75. 10.1089/tmj.2016.0060 [DOI] [PubMed] [Google Scholar]
- 21.Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. (2021) 101(6):pzab053. 10.1093/ptj/pzab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cottrell MA, Galea OA, O'Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. (2017) 56(11):1069–75. 10.1177/0269215516645148 [DOI] [PubMed] [Google Scholar]
- 23.Dario AB, Moreti Cabral A, Almeida L, Ferreira ML, Refshauge K, Simic M, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. (2017) 17(9):1342–51. 10.1016/j.spinee.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 24.Nicholl BI, Sandal LF, Stochkendahl MJ, McCallum M, Suresh N, Vasseljen O, et al. Digital support interventions for the self-management of low back pain: a systematic review. J Med Internet Res. (2017) 19(5):e179. 10.2196/jmir.7290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Millot S. L'enquête de satisfaction: Guide méthodologique. Saint-Denis-La Plaine: Edit Afnor; 1er édition (2007). p. 178. [Google Scholar]
- 26.Venkatesh V, Michael GM, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27(3) INFORM Global:425–78. 10.2307/30036540 [DOI] [Google Scholar]
- 27.Vrieze SI. Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol Methods. (2012) 17(2):228–43. 10.1037/a0027127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brehon K, Carriere J, Churchill K, Loyola-Sanchez A, O'Connell P, Papathanasoglou E, et al. Evaluating the impact of a novel telerehabilitation service to address neurological, musculoskeletal, or coronavirus disease 2019 rehabilitation concerns during the coronavirus disease 2019 pandemic. Digital Health. (2022) 8:20552076221101684. 10.1177/205520762211016844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoaas H, Andreassen HK, Lien LA, Hjalmarsen A, Zanaboni P. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Med Inform Decis Mak. (2016) 16:26. 10.1186/s12911-016-0264-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cox NS, Dal Corso S, Hansen H, McDonald CF, Hill CJ, Zanaboni P, et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev. (2021) 1(1):CD013040. 10.1002/14651858.CD013040.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. (2020) 1(1):CD010255. 10.1002/14651858.CD010255.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buabbas AJ, Albahrouh SE, Alrowayeh HN, Alshawaf H. Telerehabilitation during the COVID-19 pandemic: patients and physical Therapists’ experiences. Med Princ Pract. (2022) 31(2):156–64. 10.1159/000523775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vellata C, Belli S, Balsamo F, Giordano A, Colombo R, Maggioni G. Effectiveness of telerehabilitation on motor impairments, non-motor symptoms and compliance in patients with Parkinson's disease: a systematic review. Front Neurol. (2021) 12:627999. 10.3389/fneur.2021.627999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morimoto Y, Takahashi T, Sawa R, Saitoh M, Morisawa T, Kagiyama N, et al. Web portals for patients with chronic diseases: scoping review of the functional features and theoretical frameworks of telerehabilitation platforms. J Med Internet Res. (2022) 24(1):e27759. 10.2196/27759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. (2017) 7:1–12. 10.1136/bmjopen-2017-016242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liaw S-S, Huang H-M, Chen G-D. Surveying instructor and learner attitudes toward e-learning. Comput Educ. (2007) 49, Elsevier (4):175–87. 10.1016/j.compedu.2006.01.001 [DOI] [Google Scholar]
- 37.Bhuasiri W, Xaymoungkhoun O, Zo H, Rho JJ, Ciganek AP. Critical success factors for e-learning in developing countries: A comparative analysis between ICT experts and faculty. Computers & Education. (2012) 58(2):843–55. 10.1016/J.COMPEDU.2011.10.010 [DOI] [Google Scholar]
- 38.Menchaca MP, Bekele TA. Learner and instructor identified success factors in distance education. Distance Educ. (2008) 29, Elsevier (3):175–87. 10.1080/01587910802395771 [DOI] [Google Scholar]
- 39.Fresen JW. Factors influencing lecturer uptake of e-learning. Teach English Technol. (2011) 11, Elsevier (1):175–87. [Google Scholar]
- 40.FitzPatrick T. Key success factors of eLearning in education: a professional development model to evaluate and support eLearning. US-China Educ Rev. (2012) 9, Elsevier:175–87. [Google Scholar]
- 41.Naveed QN, Qureshi MRN, Tairan N, Mohammad A, Shaikh A, Alsayed AO, et al. Evaluating critical success factors in implementing E-learning system using multi-criteria decision-making. PLoS One. (2020) 15(5):e0231465. 10.1371/journal.pone.0231465 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: Datasets are available on request: The raw data supporting the conclusions of this article will be made available by the authors. Requests to access these datasets should be directed to patrice.piette@pole-sthelier.com.