Abstract
Objective
We aimed to characterize the relationship between severe chronic alcoholism and hepatic arterial wall disorders in humans.
Methods
We obtained hepatic arteries from 165 patients undergoing liver transplantation who were placed into two etiological groups: an Alcoholism group and a Non-alcoholism group. We compared the age, sex, lipid profile, and histologic characteristics of the hepatic arteries (normal, reduction in luminal diameter of ≤10%, or atherosclerosis) of the participants in the two groups using multifactor analyses.
Results
The Alcoholism group comprised 58 men and 40 women and the Non-alcoholism group comprised 63 men and 4 women. The mean ages of the groups were 52.5 ± 9.6 years and 44.2 ± 13.8 years, respectively. There were no circulating lipid abnormalities in any of the participants. In women, arterial disorders were found at a younger age than in men. Hepatic arterial disorders were more frequent in the non-alcoholic participants, and women with alcoholism showed less arterial narrowing.
Conclusion
The heavy consumption of alcoholic beverages is associated with a lower incidence of atherosclerosis of the hepatic artery in humans.
Keywords: Alcoholism, hepatic artery, atherosclerosis, arterial obstruction, thrombosis, endothelium
Introduction
The results of previous studies regarding the relationships between alcohol consumption and vascular disorders have been contradictory. According to the results of several previous experimental, clinical, and epidemiologic studies, the moderate consumption of alcoholic beverages reduces the incidence of cardiovascular diseases by increasing the high-density lipoprotein (HDL)-cholesterol concentration, which prevents endothelial inflammation and reduces the formation of atheromas.1–9 In addition, the consumption of alcoholic beverages has been associated with a larger number of endothelial progenitor cells and a greater capacity for endothelial repair, which prevents atherosclerosis.10,11 Other benefits of the moderate consumption of alcohol have been reported to be a lower risk of occlusive vascular disease, and reductions in the incidences of vascular dementia, diabetes mellitus, and cardiac ischemia, when compared with individuals who do not consume alcohol.12
In contrast, heavy and chronic alcohol consumption is harmful to the cardiovascular system because it causes inflammation and endothelial dysfunction, which are associated with atherosclerosis, vasoconstriction, and a higher risk of arterial hypertension.13–18 The impairment in vascular function is caused by a direct effect of alcohol on endothelial cells, which increases intima-media thickness, and persists even after alcohol consumption has ceased.19–23 Furthermore, a meta-analysis showed no evidence of a protective effect of alcohol consumption on intima-media thickness,24 and there is a higher incidence of hemorrhagic stroke in alcohol consumers, owing to the anticoagulant and hypertensive effects of alcohol.12,15–17,25–27 Severe and prolonged alcoholism is also associated with hepatic dysfunction and a progressive replacement of hepatocytes by fibroadipose tissue, which can ultimately progress to cirrhosis. At this stage, liver function is substantially impaired, and ascites, malabsorption, and portal hypertension develop, along with their consequences. Finally, alcoholism is also a cause of irreversible chronic pancreatitis.28–32
In an attempt to resolve some of the controversies in the literature with regard to the relationship between alcoholism and arteriosclerosis, in the present study, we aimed to characterize the relationship between severe chronic alcoholism and hepatic arterial wall disorders in humans.
Methods
Ethics
The present study is part of a line of research related to alcoholism that was approved by the Human Research Ethics Committee of the Federal University of Minas Gerais (UFMG), Brazil (approval number 124/2012). Written informed consent was obtained from all the participants, and all the data presented has been de-identified.33
Study design
We performed a retrospective study of the medical records of 165 adult patients of both sexes of >18 years of age, with no upper age limit, who underwent liver transplantation at the Hospital of Clinics of the Federal University of Minas Gerais, Brazil. For patients to be included in the study, their medical records were required to include clear information regarding the consumption of alcoholic beverages and circulating lipid concentrations measured <1 month prior to liver transplantation. Another key inclusion criterion was perfect condition of the hepatic artery removed with the cirrhotic liver during liver transplantation and its storage in the Department of Pathology. The participants were placed into an Alcoholism group and a Non-alcoholism group using the following characteristics: patients of both sexes who underwent liver transplantation because of alcoholic cirrhosis and regular heavy alcohol consumption (>90 g alcohol/day)16 for >20 years, and patients of both sexes who underwent liver transplantation because of liver diseases unrelated to alcoholism, with a consumption of alcohol equivalent to <20 g alcohol per week, respectively.
Characteristics of the participants and assessment of pathology
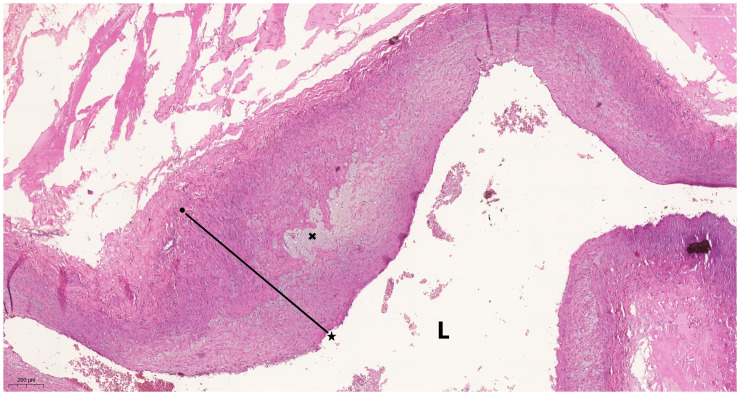
The age, sex, history of alcohol consumption, history of liver disease, and the circulating lipid concentrations prior to transplantation were collected from the medical records of the participants. The histology of the liver sections obtained from the participants was reviewed to confirm the histological diagnosis of cirrhosis and to choose the most representative example of the hepatic hilum, including a perfect section through the hepatic artery. When the sections were not of sufficient quality, new 4-µm sections were prepared for examination of the hepatic artery and stained with hematoxylin and eosin, according to the protocol of the Pathology Service. These slides were analyzed by two pathologists, who are specialists in vascular pathology, and who had no knowledge of the participants. The hepatic arterial wall at the hilum of the liver and in its intrahepatic branches were classified as normal (absence of or minimal changes in the hepatic arterial wall), showing thickening (small, non-specific changes in the subintimal layer of the arterial wall, with chronic inflammation and a <10% reduction in the luminal diameter), or showing atherosclerosis (thickening of the arterial wall, associated with intracellular lipid deposits in the media-intima layer, in macrophages, foam cells, and the interstitium, and with a >10% reduction in luminal diameter) (Figure 1).
Figure 1.
Photomicrograph of the hepatic artery wall in the hilum of a liver obtained from a participant with alcoholic cirrhosis. Atherosclerosis and arterial intimal thickening is apparent, with a >10% reduction in the diameter of the arterial lumen (L). The line defines the distance between the vascular endothelium (★) and the internal elastic limit (arterial intimal layer) (●), and × indicates foam cells. The scale bar (lower left corner) represents 200 µm. Hematoxylin and eosin, 40× magnification.
Statistical analysis
Categorical data are expressed as frequency and percentage. Continuous data are expressed as mean and standard deviation when they are normally distributed, or as median and first and third quartiles when they are not normally distributed. The Shapiro–Wilk test was used to determine whether or not each dataset was normally distributed. The chi-square test was used to analyze categorical data and ANOVA was used to analyze continuous data. Odds ratios were used to compare the risk of arterial disorders in the two groups. The significance level was set as 0.05 and a confidence level of >95% was used. SPSS v.23 (IBM Corp., Armonk, NY, USA) was used the analyze the data.
Results
The participants were largely male (121 men (73%) and 44 women (27%); p < 0.001). Furthermore, the Non-alcoholism group comprised 63 men and 4 women. The mean age of the participants in the Alcoholism group was 52.5 ± 9.6 years, with the men ranging from 23 to 71 (53.1 ±8.7) years of age and the women ranging from 29 to 67 (48.9 ± 10.9) years of age (p = 0.194). The mean age of the participants in the Non-alcoholism group was 44.2 ± 13.8 years, with the men ranging from 22 to 67 (44.9 ± 13.8) years of age and the women ranging from 18 to 67 (43.3 ± 14.0) years of age (p = 0.675). There was no age difference between the two groups, either overall or according to sex.
The principal inclusion criterion for the Alcoholism group was cirrhosis owing to alcoholism as the indication for liver transplantation. For the Non-alcoholism group, patients were included that underwent liver transplantation because of hepatitis C-associated cirrhosis (19), chronic hepatitis B-associated cirrhosis (18), autoimmune cirrhosis (15), primary sclerosing cholangitis cirrhosis (9), or cryptogenic cirrhosis (6).
In men, there was no relationship between age and arterial defects, but in women, arterial defects became more common with advancing age (p = 0.019) (Table 1). A higher level of pathology was identified in the hepatic arteries of men than of women of equivalent age (Table 1).
Table 1.
Ages of the male and female participants who had each type of histological change in the hepatic artery.
| Hepatic artery pathology | Men | Women | P |
|---|---|---|---|
| Normal (n = 85) | 49.7 ± 10.6 | 43.4 ± 12.8 | 0.040 |
| Thickening (n = 59) | 52.0 ± 11.7 | 50.2 ± 13.8 | 0.703 |
| Atherosclerosis (n = 21) | 52.2 ± 10.3 | 46.5 ± 13.4 | 0.653 |
Data are mean ± standard deviation and were analyzed using the chi-square test.
The circulating lipid concentrations of all the participants in both groups were within the normal ranges and there were no differences between men and women. Furthermore, no relationships were identified between the lipid concentrations and the arterial disorders (Table 2).
Table 2.
Circulating lipid concentrations associated with histological disorders of the hepatic artery in the participants.
| Lipid species | Normal (n = 85) | Thickening (n = 59) | Atherosclerosis (n = 21) | P |
|---|---|---|---|---|
| Total cholesterol (mmol/L) | 4.050 ± 0.357 | 4.053 ± 0.442 | 4.053 ± 0.463 | 0.891 |
| HDL-C (mmol/L) | 1.198 ± 0.129 | 1.156 ± 0.168 | 1.198 ± 0.323 | 0.472 |
| LDL-C (mmol/L) | 2.398 ± 0.269 | 2.480 ± 0.442 | 2.612 ± 0.507 | 0.600 |
| VLDL-C (mmol/L | 0.489 ± 0.088 | 0.466 ± 0.078 | 0.517 ± 0.179 | 0.891 |
| Triglycerides (mmol/L) | 1.014 ± 0.219 | 0.994 ± 0.181 | 0.964 ± 0.284 | 0.942 |
Data are mean ± standard deviation and were analyzed using the chi-square test. HDL-C, high-density lipoprotein-cholesterol; LDL-C, low-density lipoprotein-cholesterol; VLDL-C, very low-density lipoprotein-cholesterol.
Defects of the hepatic arterial walls were more common in the Non-alcoholism group in both sexes (p = 0.012). Finally, the participants in the Non-alcoholism group (group 2) had an odds ratio for arterial defects of 2.37 versus the Alcoholism group (group 1) (Table 3).
Table 3.
Hepatic arterial wall pathology in the Alcoholism and Non-alcoholism groups.
| Hepatic artery pathology | Alcoholism group |
Non-alcoholism group |
||
|---|---|---|---|---|
| Men (n = 58) | Women (n = 40) | Men (n = 63) | Women (n = 4) | |
| Normal | 31 (53%) | 28 (70%) | 24 (38%) | 2 (50%) |
| Thickening | 20 (35%) | 10 (25%) | 28 (44%) | 1 (25%) |
| Atherosclerosis | 7 (12%) | 2 ( 5%) | 11 (18%) | 1 (25%) |
Data are numbers (percentages). Hepatic arterial thickening and atherosclerosis were more frequent in the Non-alcoholism group than in the Alcoholism group in both sexes (p = 0.012, chi square test). The odds ratio was 2.37 (95% confidence interval 1.25–4.52).
Discussion
Previous studies have yielded contradictory results with respect to the relationship of alcoholism with arterial wall disorders, probably because the methods used to assess the amount and timing of alcohol consumption, and the age, sex, and comorbidities of the participants differed.1–9 Most of these studies showed a lower incidence of atherosclerosis in patients who drink a small (<20 g of alcohol per day, which corresponds to approximately one measure of a spirit) to moderate (20 to 70 g of alcohol per day) amount of alcohol each day.10,11,16 By contrast, heavy alcohol consumption (>90 g of alcohol per day, which corresponds to approximately five measures of spirit per day, for ≥5 years) is associated with endocrine, metabolic, hepatic, pancreatic, cardiovascular, bronchopulmonary, esophageal, central nervous system, and head and neck diseases, but the mechanism whereby alcohol affects their etiopathogenesis has yet to be well defined. Furthermore, alcoholism is associated with atherosclerosis and thromboembolism.13–18,34,35,37,38 Previous studies have shown that alcohol consumption tends to increase the stability of atheromatous plaques in large arteries, such as the aorta and the common iliac and femoral arteries, but this benefit has not been demonstrated in small and medium-sized arteries, including the coronary and hepatic arteries.39–42 In the present study, the arterial wall defects of two groups of patients who underwent liver transplantation because of severe cirrhosis, the first because of alcoholism and the second because of other causes, were compared. The indications for liver transplantation in the present study do not differ from those described in the literature.28–31,37
The participants in the Non-alcoholism group 2 rarely consumed alcohol, and most did not drink alcoholic beverages at all, mainly to prevent aggravation of their liver disease. Liver transplantation was typically recommended to individuals in this group at a younger age than for those in the Alcoholism group. This difference was consistent with the results of previous studies, because primary liver diseases and metabolic disorders that affect the liver typically develop at a younger age and progress more rapidly28–31,43 The Hepatdnaviridae, which cause hepatitis B, and the Flaviviridae, which cause hepatitis C, are also able to destroy hepatocytes more rapidly than heavy alcohol consumption.44 Total sclerosing cholangitis prevents biliary drainage, and the resulting intrahepatic cholestasis damages hepatocytes.37 In contrast, most patients with alcoholism do not have a previous history of liver disease, and it takes a long time for their hepatocyte reserve to be substantially depleted by heavy alcohol consumption.28–31
All the hepatic arteries collected by the Pathology Service that were in good enough condition for histological analysis and had been removed from adult patients who had undergone liver transplantation were studied. For each of the participants in the non-Alcoholism group, complete and reliable medical records regarding the non-consumption of alcoholic beverages were available, but although the study was open to both sexes, only four women in this group were found to satisfy the inclusion criteria for the present study. This is a very small number for the purposes of statistical analysis, but it reflects the reality of our patient population and did not compromise the principal findings of the study.
The prevalence of alcoholism in the male participants in the present study is consistent with the results of previous studies, which have shown a higher prevalence in men than women, by factors of 2:1 to 14:128,29,31,45 Although alcoholism typically develops in men at a young age, and generally before it does in women, liver cirrhosis is typically identified in men at an older age than in women.45 In the present study, the age of men with severe alcoholic liver cirrhosis who required transplantation was also higher than that in women. Therefore, women may be less resistant to the effects of chronic alcohol consumption on the liver than men, and it should be noted that women usually tolerate less alcohol than men.14,25 However, we could not find results of any previous studies that support this contention, which therefore requires further investigation.
Previous studies of arterial disorders have been imaging studies or studies of arteries obtained from cadavers.4,5,8,16,23,46 Thus, the present study is the first of the relationship between arterial histopathology and alcoholism in a medium-sized artery obtained from live patients. The hepatic artery was chosen for this purpose because it is always removed with the original liver during liver transplantation. The histological details were not included in the data because none of the findings were relevant and this was not an objective of the study.
In the general population, atherosclerosis is more prevalent in people of >50 years of age and in women. By contrast, when atherosclerosis occurs in young individuals, it is more common in men.4,5,8,16,23,47 This angiopathy is the result of a chronic endothelial disorder, and involves vasomotor changes, the release of pro-inflammatory substances, and thromboactive lipoprotein deposits in the arterial walls.10,23,40,47,49 In the present study, the prevalence of atherosclerosis was higher in men, despite only tending to be present in participants of >50 years of age. Factors known to be associated with a higher risk of vascular disease, such as obesity, smoking, diabetes mellitus, and physical inactivity, were not quantified in the present study, and therefore we will not discuss these further. In addition, we found that the circulating concentrations of the cholesterol fractions and triglycerides were within their normal ranges in all of the participants, regardless of the cause of the cirrhosis in both men and women. Thus, the liver cirrhosis and atherosclerosis in the participants were not associated with dyslipidemia.
In the present study, we found that the incidence of atherosclerosis was lower in participants with alcoholism. Previous studies have shown that the moderate consumption of alcoholic beverages, even daily, is associated with lower incidences of ischemic coronary disease and myocardial infarction.1–9 However, in the Alcoholism group, the participants had consumed large amounts of alcohol daily for >20 years. The present findings contrast with previous findings that heavy alcohol consumption is associated with cardiovascular disease, including thromboembolism. Although such an analysis was not an objective of the present study, none of the participants’ records showed a history of cardiovascular disorders. Participants in the Alcoholism group showed less atherosclerosis and hepatic arterial thickening than those in the Non-alcoholism group. It is important to recognize that the women with alcoholism showed less atherosclerosis than the men. Alcohol intoxication has deleterious effects on the liver, especially in women; however, alcoholism seems to protect the endothelium of medium-sized arteries against atherosclerosis. However, we could not find an explanation for the relationship between alcoholism and arterial disorders in the literature. Although a lower prevalence of atherosclerosis was found in participants with alcoholism in the present study, it was not possible to identify a mechanism by which heavy alcohol consumption might affect the etiopathogenesis of atherosclerosis.
More research is needed before a definitive statement can be made regarding the relationship between alcoholism and atherosclerosis. It would also be useful to compare the arterial anastomoses performed during liver transplantation in patients with alcoholic cirrhosis and in those with cirrhosis of other etiologies, to determine whether the lower prevalence of atherosclerosis is associated with less arterial obstruction and stenosis. Patients with alcoholism should also be studied with respect to the link with immunity and the incidence of post-transplantation complications.
Conclusion
The consumption of alcoholic beverages is associated with atherosclerosis and stenosis of the hepatic artery, principally in men, but there is no direct relationship with the amount of alcohol consumed or the severity of alcoholic cirrhosis.
Acknowledgements
The authors gratefully acknowledge the Research Support Foundation of the State of Minas Gerais (FAPEMIG), the National Council for Scientific and Technological Development (CNPq), and the Dean’s Office for Research (Pró-reitoria de Pesquisa) at UFMG for their assistance.
Author Contributions: AP designed the study, participated in all steps of the work, participated in the liver transplantation procedures, performed the histological analyses, drafted the manuscript, takes responsibility for all aspects of the work, and revised the manuscript. CMSLDH collected data, performed statistical analyses, and drafted the manuscript. GAP collected data and drafted the manuscript. PVTV performed the histological analyses, performed statistical analyses, and drafted the manuscript. All the authors approved the final version of the manuscript and its submission for publication.
The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Andy Petroianu https://orcid.org/0000-0002-8659-6866
Data availability
The authors have full control of all data associated with this study, which are available for verification upon request.
References
- 1.Chiva-Blanch G, Badimon L. Benefits and risks of moderate alcohol consumption on cardiovascular disease. Nutrients 2020; 12: 108. doi: 10.3390/nu12010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piano MR. Alcohol’s effects on the cardiovascular system. Alcohol Res 2017; 38: 219–241. PMID: 28988575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cahill PA, Redmond EM. Alcohol and cardiovascular disease–modulation of vascular cell function. Nutrients 2012; 4: 297–318. doi: 10.3390/nu4040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klatsy AL. Alcohol and cardiovascular diseases. J Intern Med 2015; 278: 238–250. doi: 10.1111/joim.12390. [DOI] [PubMed] [Google Scholar]
- 5.Sinn DH, Gwak GY, Cho J, et al. Modest alcohol consumption and carotid plaques or carotid artery stenosis in men with non-alcoholic fatty liver disease. Atherosclerosis 2014; 234: 270–275. doi: 10.1016/j.atherosclerosis. 2014.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Huang PH, Chen YH, Tsai HY, et al. Intake of red wine increases the number and functional capacity of circulating endothelial progenitor cells by enhancing nitric oxide bioavailability. Arterioscler Thromb Vasc Biol 2010; 30: 869–877. doi: 10.1161/ATVBAHA.109.200618. [DOI] [PubMed] [Google Scholar]
- 7.Arranz S, Chiva-Blanch G, Valderas-Martinez P, et al. Wine, beer, alcohol and polyphenols on cardiovascular disease and cancer. Nutrients 2012; 4: 759–781. doi: 10.3390/nu4070759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booyse FM, Pan W, Grenett HE, et al. Mechanism by which alcohol and wine polyphenols affect coronary heart disease risk. Ann Epidemiol 2007; 17: S24–S31. doi: 10.1016/j.annepidem.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Riccardi G, Giosuè A, Calabrese I, et al. Dietary recommendations for prevention of atherosclerosis. Cardiovasc Res 2022; 118: 1188–1204. doi: 10.1093/cvr/cvab173. [DOI] [PubMed] [Google Scholar]
- 10.Liu P, Zhou B, Gu D, et al. Endothelial progenitor cell therapy in atherosclerosis. Ageing Res Rev 2009; 8: 83–93. doi: 10.1016/j.arr.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Brodowski L, Schröder-Heurich B, Kipke B, et al. Low ethanol concentrations promote endothelial progenitor cell capacity and reparative function. Cardiovasc Ther 2020; 2020: 4018478. doi: 10.1155/2020/4018478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel D, Gandhi Z, Desai R, et al. Impact of alcohol use disorder on stroke risk in geriatric patients with prediabetes. Int J Clin Pract 2021; 75: e14477. doi: 10.1111/ijcp.14477. [DOI] [PubMed] [Google Scholar]
- 13.Fuchs FD, Chambless LE. Is the cardioprotective effect of alcohol real? Alcohol 2007; 41: 399–402. doi: 10.1016/j.alcohol.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Global status report on alcohol and health 2018; Genebra.
- 15.Zilkens RR, Burke V, Hodgson JM, et al. Red wine and beer elevate blood pressure in normotensive men. Hypertension 2005; 45: 874–879. doi: 10.1161/01.HYP.0000164639.83623.76. [DOI] [PubMed] [Google Scholar]
- 16.O’Keefe JH, Bhatti SK, Bajwa A, et al. Alcohol and cardiovascular health: the dose makes the poison or the remedy. Mayo Clin Proc 2014; 89: 382–393. doi: 10.1016/j.mayocp.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Marchi KC, Muniz JJ, Tirapelli CR. Hypertension and chronic ethanol consumption. World J Cardiol 2014; 6: 283–294. doi:10.4330/wjc.v6.i5.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chagas P, Mazocco L, Piccoli JDCE, et al. Association of alcohol consumption with coronary artery disease severity. Clin Nutr 2017; 36: 1036–1039. doi:10.1016/j.clnu.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Lu C, Weng R, Wu W, et al. Moderate alcohol consumption and carotid intima-media thickness in type 2 diabetes. Asia Pacif J Clin Nutr 2021; 30: 497–503. doi: 10.6133/apjcn.202109_30(3).0016. [DOI] [PubMed] [Google Scholar]
- 20.Alber HF, Suessenbacher A, Weidinger F. The role of inflammation in the pathophysiology of acute coronary syndromes. Wien Klin Wochenschr 2005; 117: 445–455. doi: 10.1007/s00508-005-0399-7. [DOI] [PubMed] [Google Scholar]
- 21.Ross R. . Atherosclerosis-an inflammatory disease. N Engl J Med 1999; 340: 115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 22.Mestas J, Ley K. Monocyte-endothelial cell interactions in the development of atherosclerosis. Trends Cardiovasc Med 2008; 18: 228–232. doi:10.1016/j.tcm.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blasi C. The autoimmune origin of atherosclerosis. Atherosclerosis 2008; 201: 17–32. doi: 10.1016/j.atherosclerosis.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 24.Spaggiari G, Cignarelli A, Sansone A, et al. A meta-analysis of the effects of beer consumption on cardiovascular health. PLoS One 2020; 15: e0233619. doi: 10.1371/journal.pone.0233619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ikehara S, Iso H. Alcohol consumption and risks of hypertension and cardiovascular disease in Japanese men and women. Hypertens Res 2020; 43: 477–481. doi: 10.1038/s41440-020-0417-1. [DOI] [PubMed] [Google Scholar]
- 26.Askgaard G, Christensen AI, Nordestgaard B, et al. Alcohol and risk of non-traumatic bleeding events requiring hospital care in the general population. Alcohol 2020; 87: 73–78. doi: 10.1016/j.alcohol.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 27.Djousse L, Himali JJ, Beiser A, et al. Apolipoprotein e, alcohol consumption, and risk of ischemic stroke. J Stroke Cerebrovascr Dis 2009; 18: 384–388. doi: 10.1016/j.jstrokecerebrovasdis.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reuben A. Alcohol and the liver. Curr Opin Gastroenterol 2007; 23: 283–291. doi: 10.1097/MOG.0b013e3280f27582. [DOI] [PubMed] [Google Scholar]
- 29.Buchanan R, Sinclair JMA. Alcohol use disorder and the liver. Addiction 2021; 116: 1270–1278. doi: 10.1111/add.15204. [DOI] [PubMed] [Google Scholar]
- 30.Lotersztajn S, Riva A, Wang S, et al. Inflammation in alcohol-associated liver disease progression. Z Gastroenterol 2022; 60: 58–66. doi: 10.1055/a-1714-9246. [DOI] [PubMed] [Google Scholar]
- 31.Singal AK, Mathurin P. Diagnosis and treatment of alcohol-associated liver disease JAMA 2021; 326: 165–176. doi: 10.1001/jama.2021.7683. [DOI] [PubMed] [Google Scholar]
- 32.Wang YC, Mao XT, Yu D, et al. Alcohol amplifies the association between common variants at PRSS1-PRSS2 locus and chronic pancreatitis in a dose-dependent manner. Gut 2022; 71: 2369–2371. doi: 10.1136/gutjnl-2021-326670. [DOI] [PubMed] [Google Scholar]
- 33.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 34.Sabino KR, Petroianu A, Alberti LR. Influence of the acute alcoholism on the phagocytic function of the mononuclear phagocytic system. J Med Life 2011; 4: 421–423. PMID: 22514578. [PMC free article] [PubMed] [Google Scholar]
- 35.Money SR, Petroianu A, Kimura K, et al. The effects of short-term ethanol exposure on the canine jejunal handling of calcium and glucose. Surgery 1990; 107: 167–171. PMID: 2300895. [PubMed] [Google Scholar]
- 36.Petroianu A, Barquete J, Plentz EG, et al. Acute effects of alcohol ingestion on the human serum concentrations of calcium and magnesium. Int J Med Res 1991; 19: 410–413. doi:10.1177/030006059101900508. [DOI] [PubMed] [Google Scholar]
- 37.Diniz GV, Petroianu A. Intravascular and intraparenchymatous hepatic segmentary sclerosis. Acta Cir Bras 2018; 33: 785–791. doi: 10.1590/s0102-865020180090000006. [DOI] [PubMed] [Google Scholar]
- 38.Sabino KR, Petroianu A, Alberti LR, et al. The effect of chronic ethanol consumption on duodenal absorption of iron in mice. Arq Gastroenterol 2010; 47: 193–196. doi: 10.1590/s0004-28032010000200015. [DOI] [PubMed] [Google Scholar]
- 39.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature 2011; 473: 317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 40.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction. Circulation 2007; 115: 1285–1295. doi:10.1161/CIRCULATIONAHA. 106.652859. [DOI] [PubMed] [Google Scholar]
- 41.Castelli WP. Lipids, risk factors and ischaemic heart disease. Atherosclerosis 1996; 124: S1–S9. doi: 10.1016/0021-9150(96)05851-0. [DOI] [PubMed] [Google Scholar]
- 42.Demirovic J, Nabulsi A, Folsom AR, et al. Alcohol consumption and ultrasonographically assessed carotid artery wall thickness and distensibility. Circulation 1993; 88: 2787–2793. doi: 10.1161/01.cir.88.6.2787. [DOI] [PubMed] [Google Scholar]
- 43.Pouwels S, Sakran N, Graham Y, et al. Non-alcoholic fatty liver disease. BMC Endocr Disord 2022; 22: 63. doi: 10.1186/s12902-022-00980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Veracruz N, Gish RG, Cheung R, et al. Global incidence and mortality of hepatitis B and hepatitis C acute infections, cirrhosis and hepatocellular carcinoma from 2010 to 2019. J Viral Hepat 2022; 29: 352–365. doi: 10.1111/jvh.13663. [DOI] [PubMed] [Google Scholar]
- 45.Wester A, Ndegwa N, Hagström H. Risk of fractures and subsequent mortality in alcohol-related cirrhosis: a nationwide population-based cohort study. Clin Gastroenterol Hepatol (in press) 2022; S1542–3565(22)00605-X. doi: 10.1016/j.cgh.2022.05.048. [DOI] [PubMed] [Google Scholar]
- 46.Kiechl S, Willeit J, Egger G, et al. Alcohol consumption and carotid atherosclerosis: evidence of dose-dependent atherogenic and antiatherogenic effects. Results from the Bruneck Study. Stroke 1994; 25: 1593–1598. doi: 10.1161/01.str.25.8.1593. [DOI] [PubMed] [Google Scholar]
- 47.Steinbrecher UP, Parthasarathy S, Leake DS, et al. Modification of low density lipoprotein by endothelial cells involves lipid peroxidation and degradation of low density lipoprotein phospholipids. Proc Natl Acad Sci USA 1984; 81: 3883–3887. doi:10.1073/pnas.81.12.3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cathcart MK, Morel DW, Chisolm GM., 3rd. Monocytes and neutrophils oxidize low density lipoprotein making it cytotoxic. J Leukoc Biol 1985; 38: 341–350. doi: 10.1002/jlb.38.2.341. [DOI] [PubMed] [Google Scholar]
- 49.Hannuksela ML, Liisanantti MK, Savolainen MJ. Effect of alcohol on lipids and lipoproteins in relation to atherosclerosis. Crit Rev Clin Lab Sci 2002; 39: 225–283. doi: 10.1080/10408360290795529. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors have full control of all data associated with this study, which are available for verification upon request.