With the greatest interest we read the paper by Harbut et al. [1] describing the role of intrapulmonary shunting and alveolar dead space in patients with acute COVID-19 pneumonitis. We are grateful for them sharing their valuable functional blood and alveolar gas exchange data, pointing out a significant alveolar dead space of nearly 30% in recovered COVID-19 patients, suggesting a persistent pulmonary vascular pathology. Although COVID-19 related hypoxaemia is characterised by preserved oxygen saturation, a ventilation–perfusion mismatch and increased alveolar ventilation/perfusion ratio heterogeneity, the underlying morphological evidence of this physiological enigma has not been fully understood.
Short abstract
A compelling explanation for mosaic-like micro-ischaemia in the severe pathology of COVID-19 pneumonitis, which reflects the vasculopathy affecting the secondary lobule and the interlobular septae http://bit.ly/3GwMkII
To the Editor:
With the greatest interest we read the paper by Harbut et al. [1] describing the role of intrapulmonary shunting and alveolar dead space in patients with acute COVID-19 pneumonitis. We are grateful for them sharing their valuable functional blood and alveolar gas exchange data, pointing out a significant alveolar dead space of nearly 30% in recovered COVID-19 patients, suggesting a persistent pulmonary vascular pathology. Although COVID-19 related hypoxaemia is characterised by preserved oxygen saturation, a ventilation–perfusion mismatch and increased alveolar ventilation/perfusion ratio heterogeneity, the underlying morphological evidence of this physiological enigma has not been fully understood.
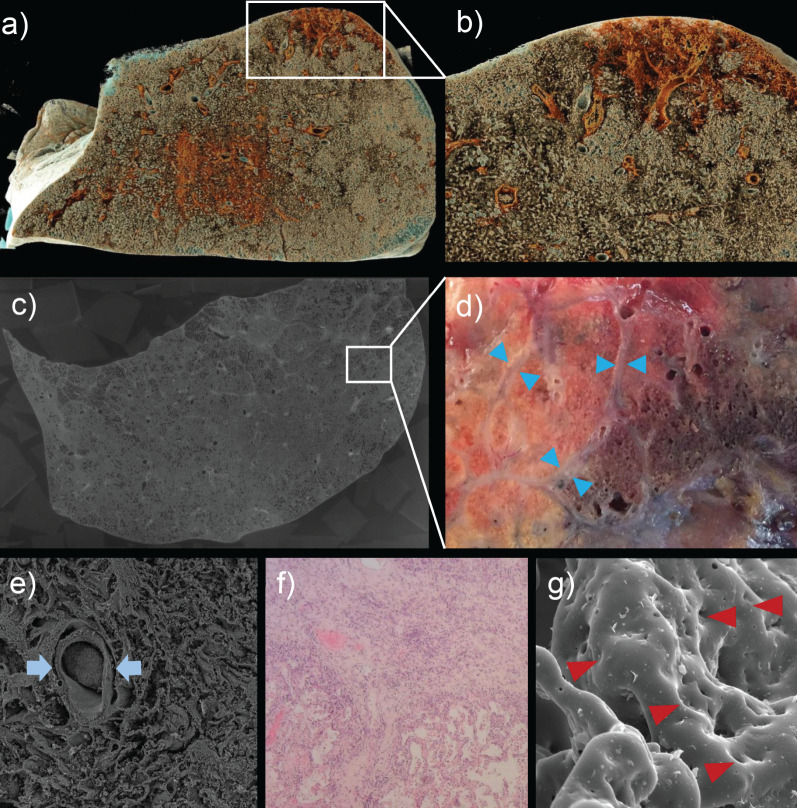
In a recent study [2], we were able to demonstrate the involvement of the secondary pulmonary lobules in the fatal trajectory of COVID-19 using ultra-high resolution synchrotron radiation based hierarchical phase-contrast tomography (HiP-CT) (figure 1a–c) [3]. We observed a distinct, mosaic-like consolidation of individual secondary pulmonary lobules based on microvascular occlusion and secondary lobular micro-ischaemia, reflecting the increased alveolar dead space described by Harbut et al. [1]. Moreover, this septal micro-ischaemia was accompanied by a periseptal thickening and pronounced dilatation and expansion of the bronchial circulation plexus by opening of intrapulmonary bronchopulmonary shunts and “Sperrarterien” (specialised blockade arteries of the bronchial circulation) [4, 5], and an excessive blood vessel neoformation by intussusceptive angiogenesis, especially in the interlobular septae (figure 1d–g) [2, 6, 7]. Intussusceptive angiogenesis is a highly dynamic morphogenetic process involving circulating angiogenic cells, endothelial progenitor cells or monocytes [6] observed in numerous organs of fatal COVID-19 cases (lung, heart, brain or placenta) as well as in, for example, fibrosing interstitial lung diseases and malignant neoplasms.
FIGURE 1.
a) Cinematic rendering of a hierarchical phase-contrast tomography (HiP-CT) study from a 78-year-old male patient who succumbed to COVID-19 highlights the spatial heterogeneity of the affected lung parenchyma. b) Close-up of patchy subpleural consolidations reveals the heterogenous distributions of functional alveolar dead space in COVID-19 patients. c) HiP-CT of a COVID-19 lung imaged at 25 µm per voxel depicts the mosaic distribution of secondary pulmonary lobules with pulmonary microvascular involvement and occlusions. d) Gross appearance of an upper lobectomy of a 62-year-old patient with post COVID conditions (6 months after acute COVID-19 pneumonitis) demonstrating the spatial heterogeneity of consolidated secondary pulmonary lobules. Interlobular septa with a thickness of approximately 0.1 mm (blue arrowheads). e) Scanning electron micrograph revealed the complete occlusion of a centrilobular artery (blue arrows) and f) thickening of interlobular septae (haematoxylin and eosin-stained section). g) Secondary lobular micro-ischaemia in long COVID results in an even, prolonged blood vessel neo-formation by intussusceptive angiogenesis (red arrowheads).
We hypothesise that, reminiscent of the pivotal role of persistent pulmonary vascular pathology in COVID-19, the secondary lobular micro-ischaemia is indeed responsible for the substantial alveolar dead space of patients following COVID-19, as shown by Harbut et al. [1], and for the prolonged excessive angiogenesis and fibrotic remodelling of interlobular septae [2]. While there is evidence for an increase of collateral ventilation in severe airway obstruction by pores of Kohn [8], the disproportion between the degree of lung consolidation and the severity of hypoxaemia may be predominantly related to redistribution of blood flow towards the bronchial circulation and intrapulmonary shunting [4, 9]. In addition, the rapid adaptive expansion of vascularity in the interlobular septae by intussusceptive angiogenesis may contribute to overcome and compensate the persistent hypoxaemia to a certain degree. It is notable that subsequent fibrotic matricellular remodelling is observed exactly in those interlobular septae characterised by an aberrant angiogenesis (figure 1f and g) in patients recovered from acute COVID-19 pneumonitis [2]. In a previous study on pulmonary microvascular alterations in human interstitial lung disease injury patterns [10], we could demonstrate the spatial coincidence of interlobular thickening and the occurrence of intussusceptive angiogenesis contributing to the initial fibrotic remodelling. Regardless of the specific mechanism of fibrotic remodelling, it is worth mentioning that the walls of secondary pulmonary lobules may be clearly identified by conventional computed tomography scans in patients with interstitial lung diseases.
To summarise, we hypothesise that the persistence of high elevated alveolar dead space in COVID-19 convalescent patients reported by Harbut et al. [1] might be linked to the indispensable adaptive response of bronchial circulation, intrapulmonary bronchopulmonary anastomosis [4, 5] and blood vessel neoformation by intussusceptive angiogenesis [2, 6]. These proposed mechanisms can explain the observed COVID-19-related silent hypoxaemia by defining the secondary lobule as the basic morphological unit of COVID-19-induced lung damage [2]. Further investigations should be conducted to elucidate the involvement of the secondary pulmonary lobules in concert with alterations of ventilation–perfusion mismatch and increased alveolar ventilation/perfusion ratio heterogeneities in alveolar dead space, not only of COVID-19 patients, but in other respiratory diseases such as interstitial lung diseases.
Shareable PDF
Footnotes
Conflict of interest: P. Tafforeau, C.L. Walsh and P.D. Lee report grants from Chan Zuckerberg Initiative; outside the submitted work. J. Jacob reports consulting fees from Boehringer Ingelheim, Roche, GlaxoSmithKline and NHSX; lecture honoraria from Boehringer Ingelheim, Roche, GlaxoSmithKline and Takeda; travel support from Boehringer Ingelheim; UK patent application number 2113765.8; advisory board participation with Boehringer Ingelheim and Roche; outside the submitted work. T. Welte reports grants from Bundesminissterium für Bildung und Forschung (Ministry for Research and Education); outside the submitted work. All other authors have nothing to disclose.
References
- 1.Harbut P, Prisk GK, Lindwall R, et al. Intrapulmonary shunt and alveolar dead space in a cohort of patients with acute COVID-19 pneumonitis and early recovery. Eur Respir J 2023; 61: 2201117. doi: 10.1183/13993003.01117-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ackermann M, Kamp JC, Werlein C, et al. The fatal trajectory of pulmonary COVID-19 is driven by lobular ischemia and fibrotic remodelling. EBioMedicine 2022; 85: 104296. doi: 10.1016/j.ebiom.2022.104296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walsh CL, Tafforeau P, Wagner WL, et al. Imaging intact human organs with local resolution of cellular structures using hierarchical phase-contrast tomography. Nat Methods 2021; 18: 1532–1541. doi: 10.1038/s41592-021-01317-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ackermann M, Tafforeau P, Wagner WL, et al. The bronchial circulation in COVID-19 pneumonia. Am J Respir Crit Care Med 2022; 205: 121–125. doi: 10.1164/rccm.202103-0594IM [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galambos C, Bush D, Abman SH. Intrapulmonary bronchopulmonary anastomoses in COVID-19 respiratory failure. Eur Respir J 2021; 58: 2004397. doi: 10.1183/13993003.04397-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ackermann M, Mentzer SJ, Kolb M, et al. Inflammation and intussusceptive angiogenesis in COVID-19: everything in and out of flow. Eur Respir J 2020; 56: 2003147. doi: 10.1183/13993003.03147-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020; 383: 120–128. doi: 10.1056/NEJMoa2015432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vanstapel A, Weynand B, Kaes J, et al. Interalveolar pores increase in aging and severe airway obstruction. Am J Respir Crit Care Med 2021; 204: 862–865. doi: 10.1164/rccm.202102-0530LE [DOI] [PubMed] [Google Scholar]
- 9.Busana M, Camporota L, Gattinoni L. Hypoxaemia in COVID-19: many pieces to a complex puzzle. Eur Respir Rev 2022; 31: 220090. doi: 10.1183/16000617.0090-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ackermann M, Stark H, Neubert L, et al. Morphomolecular motifs of pulmonary neoangiogenesis in interstitial lung diseases. Eur Respir J 2020; 55: 1900933. doi: 10.1183/13993003.00933-2019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-02121-2022.Shareable (480.8KB, pdf)