Abstract
COVID-19 burdens are disproportionally high in underserved and vulnerable communities in Arizona. As the pandemic progressed, it is unclear if the initial associated health disparities have changed. This study aims to elicit the dynamic landscape of COVID-19 disparities at the community level and identify newly emerging vulnerable subpopulations. Findings from this study can inform interventions to increase health equity among minoritized communities in the Southwest, other regions of the US, and globally. We compiled biweekly COVID-19 case counts of 274 zip code tabulation areas (ZCTAs) in Arizona from October 21, 2020, to November 25, 2021, a time spanning multiple waves of COVID-19 case growth. Within each biweekly period, we tested the associations between the growth rate of COVID-19 cases and the population composition in a ZCTA including race/ethnicity, income, employment, and age using multiple regression analysis. We then compared the associations across time periods to discover temporal patterns of health disparities. The association between the percentage of Latinx population and the COVID-19 growth rate was positive before April 2021 but gradually converted to negative afterwards. The percentage of Black population was not associated with the COVID-19 growth rate at the beginning of the study but became positive after January 2021 which persisted till the end of the study period. Young median age and high unemployment rate emerged as new risk factors around mid-August 2021. Based on these findings, we identified 37 ZCTAs that were highly vulnerable to future fast escalation of COVID-19 cases. As the pandemic progresses, vulnerabilities associated with Latinx ethnicity improved gradually, possibly bolstered by culturally responsive programs in Arizona to support Latinx. Still communities with disadvantaged social determinants of health continued to struggle. Our findings inform the need to adjust current resource allocations to support the design and implementation of new interventions addressing the emerging vulnerabilities at the community level.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10903-023-01449-6.
Keywords: COVID-19, Health disparity, Population health
Background
During the COVID-19 pandemic, ethnic minority groups and financially disadvantaged populations in the U.S.A. have experienced disproportionately high rates of infection and severe negative health outcomes [1–3]. Associated with the disparities are inequitable distributions of health resources such as COVID-19 testing sites that are geographically underrepresented in historically underserved regions [4–6]. In response to the overwhelming disparities, neighborhoods with high concentrations of racial/ethnic minorities have initiated culturally informed community-based outreach interventions such as home visits by Spanish-speaking health promotoras to improve COVID-19 testing and education [7–9]. Meanwhile, the pandemic has advanced through several waves, each showing different patterns of spread and adding to the complexity of this issue [10]. Given these developments, it is plausible that the disparity landscape has evolved. Tracking such changes will help assess the effectiveness of COVID-19 response programs, identify emerging vulnerabilities, develop precision public health initiatives to mitigate structural inequities, and prevent future disparities effectively.
However, the current literature mainly contains cross-sectional studies capturing static snapshots of the disparities. Reports on changes of COVID-19 disparities over time are rare and the limited research reported inconsistent trends across different geographical regions. A study tracking the nationwide total cases and deaths in the U.S.A. reported that racial gaps narrowed among non-Hispanic White, Black, and Latinx people from June 2020 to September 2021 [11]. Another study examined town-level risk factors of COVID-19 incidence in Massachusetts from March 2020 to October 2020 [12]. It observed reductions in the risk associated with the percent of Black residents but reported sustained increases in the risk associated with the percentage of Latinx residents. This might be due to the availability of supports to different populations in different regions. Latinx residents, who are more likely to be recent immigrants and have lower educational attainment, need specialized resources to meet their cultural and language needs [13–15]. In states with a well-developed cultural and linguistic appropriate health services network, Latinx residents would have a better chance of receiving public health education for social distancing, vaccination, and timely access to COVID-19 testing [16].
In this study, we aim to assess the longitudinal trends of COVID-19 infection risk in Arizona. Due to the geographic closeness to Mexico, about 31.7% of Arizonans are Hispanic or Latinx, a great majority (87.6%) of which are of Mexican ancestry [17]. According to reports in 2020, Latinx residents in Arizona suffered from grievous COVID-19 disparities [18, 19]. With an established Spanish-speaking community, Arizona has implemented multiple culturally appropriate programs to alleviate the health burden on Latinx residents during the pandemic [20–22]. Meanwhile, other social determinants of health (SDoH) such as financial status and age also contribute to COVID-19 disparities [6, 23, 24]. Because ethnic minority groups tend to have lower income and are of younger age than non-Hispanic Whites [17], the evaluation and interpretation of COVID-19 disparities need to consider the intersectionality of these factors. With these requirements in mind, we designed this time-series study to examine the evolution of COVID-19 disparities associated with race/ethnicity, financial status, and age using community-level data in Arizona. We then compared the trends observed in Arizona with those in the nation as a whole and with other states to help inform public health officials on how to better prioritize and serve vulnerable groups.
Methods
ZIP Code Tabulation Area (ZCTA) is a generalized areal representation developed by the U.S. Census Bureau to aggregate census blocks in a given ZIP code area [25]. The American Community Survey (ACS) and the Arizona Department of Health Services (ADHS) use ZCTAs to report demographic statistics and COVID-19 case counts, respectively. Using these public data, we examined how the variations of COVID-19 prevalence between ZCTAs were associated with demographic features.
This study was reviewed by Arizona State University Institutional Review Board and found to not include human subjects because only publicly available de-identified data were used.
Datasets
Demographic Data
We chose to use the 2019 ACS data instead of the 2020 ACS data because the latter has nonresponse bias for marginalized populations [26]. We queried the ACS Database [17] to retrieve the total population, population density, and population compositions on sex (ratio of male and female), median age, ethnicity (non-Hispanic White, Hispanic or Latinx, American Indian, Black, and Asian), and household financial status (median income, poverty rate, and unemployment rate) for each ZCTA in Arizona.
COVID-19 Data
We downloaded case counts aggregated by ZCTA from the ADHS Dashboard website [27] every two weeks over a 13-month period from October 21, 2020, to November 25, 2021. The entire time-series data set included 29 time points spanning 28 biweekly intervals. Due to HIPAA compliance, the ADHS Dashboard suppressed case counts fewer than 10 and substituted the values as 5. The ADHS Dashboard also suppressed COVID-19 data for American Indian tribes.
Estimating COVID-19 Prevalence and Growth Rate
At each time point, we calculated the cumulative COVID-19 prevalence in a ZCTA as the total case count per 1000 residents (cases/1 K). For each biweekly interval, the growth rate was the log transformation of the increase of COVID-19 prevalence (new cases/1 K). To identify distinct growth periods at the state level, we aggregated new case counts over all Arizona ZCTAs, computed biweekly growth rates, and applied segmented regression analysis [28]. Breakpoints with a Chow-test p value < 0.05 were boundaries of growth periods.
Discovering COVID-19 Health Disparities
For each biweekly interval, we built a multiple linear regression model to represent the relationship between the growth rate in a ZCTA and a set of demographic features ,
where is the intercept, is the coefficient of the feature, and is Gaussian-distributed error. To correct for multiple comparisons, we adjusted the nominal p value associated with each using the Benjamini–Hochberg method and computed false discovery rate (FDR) [29]. FDR < 0.1 indicated a significant association between a feature and the growth rate of COVID-19 cases, i.e., health disparity. Because demographic features were measured on different units, we converted values to standardized coefficients to represent effect sizes [30]. To examine the change of health disparities, we plotted the effect size of each demographic feature over the biweekly intervals. It is worth noting that we could not compute growth rate at the initial time point (i.e., 0th biweekly interval) and used the cumulative COVID-19 prevalence as in the regression model. Therefore, disparities found at the 0th biweekly interval reflected historical vulnerabilities.
We performed the analyses using R and Python. Data files used in this study are available at the Github website. (Web address masked for blind review and will be available upon publication).
Results
As recorded in the 2019 ACS data [17], Arizona has 387 active ZCTAs with more than 100 residents. Because ADHS Dashboard suppressed COVID-19 data for American Indian tribes, we removed ZCTAs that overlap with these tribes to avoid biases. The remaining 274 ZCTAs were subject to statistical analyses. Table 1 presents the summary statistics of demographic features of these ZCTAs.
Table 1.
Summary of demographic features of ZCTAs in Arizona
| Min | Max | Median | Mean | Standard deviation | |
|---|---|---|---|---|---|
| Population size (# of residents) | 115 | 73,203 | 17,415 | 20,911 | 19,280 |
| Population density (# of residents/mi2) | 0.3 | 10,635.2 | 382.6 | 1675.9 | 2258.3 |
| Median age | 17.6 | 74.0 | 42.2 | 44.7 | 12.7 |
| % of senior residents (> 65 years old) | 0 | 80.6 | 19.0 | 23.3 | 15.8 |
| Sex ratio (males per 100 females) | 32.2 | 959.4 | 97.8 | 105.6 | 64.5 |
| % of Hispanic or Latinx residents | 0 | 100.0 | 20.4 | 28.1 | 23.1 |
| % of American Indian residents | 0 | 34.6 | 1.1 | 2.0 | 3.6 |
| % of Asian residents | 0 | 16.0 | 1.5 | 2.3 | 2.6 |
| % of Black or African American residents | 0 | 30.4 | 2.1 | 3.1 | 3.9 |
| % of residents living in poverty | 0 | 43.3 | 12.7 | 14.4 | 9.1 |
| % of unemployed residents | 0 | 47.8 | 5.4 | 6.2 | 5.1 |
| Median household income (thousand dollars) | 21.8 | 163.8 | 55.6 | 60.0 | 23.9 |
Surges and Declines of COVID-19 Cases
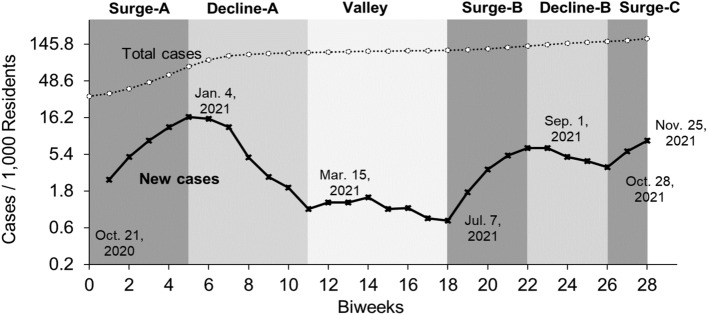
The segmented linear regression model revealed 6 distinct periods between which the growth rate of COVID-19 cases at the state level changed significantly (Fig. 1). The Surge-A period and the Decline-A period marked a wave of COVID-19 new cases between October 21, 2020, and March 15, 2021. It was followed by a four-month Valley period during which the COVID-19 growth rate remained low till July 7, 2022. After that, it spiked again during the Surge-B period, dropped slightly during the Decline-B period, and rose again during the Surge-C period that persisted till the end of our study (November 25, 2021). We confirmed that the growth rates at the ZCTA level were also significantly different between these periods (all t test p < 10–7, Supplementary Fig. S1).
Fig. 1.
Periods with distinct growth rates of COVID-19 cases. Line plots show biweekly counts of new cases (solid) and cumulative cases (dotted) per 1000 residents in Arizona. Distinct periods are shaded with different gray colors with dates marking the boundaries
Evolution of COVID-19 Disparities
The multiple regression models showed that the associations between the growth rate of COVID-19 cases and demographic features varied as the pandemic progressed, shifting between statistically significant and insignificant impact, and sometimes showing opposite effects. These temporal changes implied evolution of COVID-19 disparities.
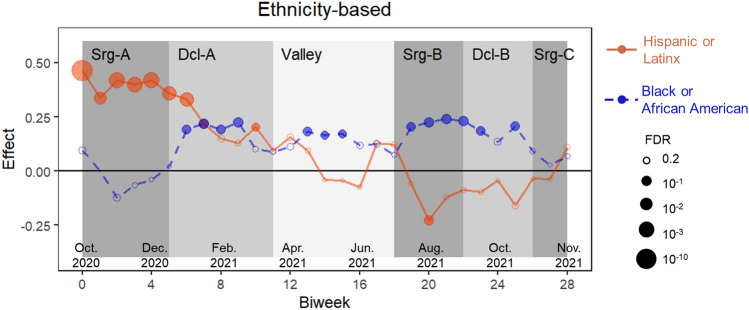
Ethnicity-Based Disparities
People of Latinx background are the largest ethnic minority group in Arizona, representing 31.7% of the total population. In 20.8% of the ZCTAs we examined, the dominant ethnicity was Latinx, surpassing the non-Hispanic White population. Our multiple regression analysis showed that the growth rate of COVID-19 cases increased with the percentage of Latinx population for about three months spanning the Surge-A and early Decline-A periods (all FDR < 0.002, respectively, Fig. 2). As the pandemic continued, the association gradually declined and finally became negative during the Surge-B and Decline-B periods. These findings suggested that the disparity associated with Latinx ethnicity improved since April 2021. However, it is worth noting that the association curve started to rise as we approached to the end of the study. During the Surge-C period, the association became positive again, but it was statistically insignificant (regression p = 0.22).
Fig. 2.
Impact of ethnicity on growth rate of COVID-19 cases. The effect size, measured by standardized coefficient, is a plotted over time for the percentage of Latinx population (orange solid line) and the percentage of African American population (blue dashed line). The size of a circle is proportional to FDR. Solid circles and open circles indicate significant (FDR < 0.1) and insignificant associations, respectively (Color figure online)
American Indians are the second largest ethnic minority group in Arizona, representing 5.3% of the total population. Because COVID-19 case counts did not include American Indian tribes, our data covered only non-tribal ZCTAs, where merely 1.9% of population is American Indian. Using this data set, we did not observe significant disparities associated with the percentage of American Indian population (Supplementary Fig. S2).
Black or African Americans constitute the third largest ethnic/racial minority group in Arizona, representing 5.2% of the total population. At the beginning of the study during the Surge-A period, we did not observe significant associations between the COVID-19 growth rate and the percentage of Black or African American population. Afterwards, a fast and persistent escalation of new cases hit ZCTAs with a high percentage of Black or African American residents in January 2021, which lasted till the end of this study (Fig. 2). These observations suggested that the disparity associated with the Black or African American ethnicity worsened over the time.
For the other ethnicities including non-Hispanic Whites and Asians that respectively represents 54.1% and 3.7% of Arizona populations, we did not detect significant associations with the COVID-19 growth rates (Supplementary Fig. S2).
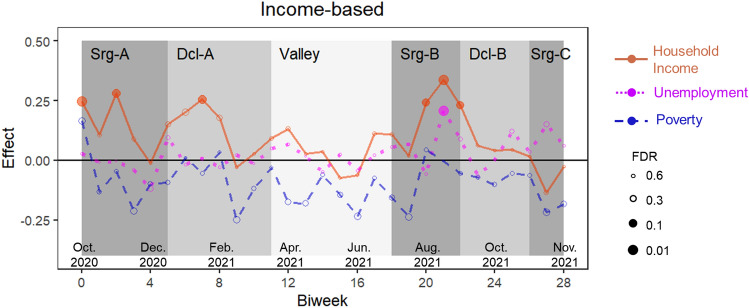
Income-Based Disparities
We examined three financial features including median household income, poverty rate, and unemployment rate. At the initial time point, we observed a marginal positive association between the cumulative COVID-19 prevalence and the poverty rate (regression p = 0.02, FDR = 0.13), implying historical vulnerabilities that were consistent with previous reports [31]. However, the growth rate of new cases showed opposite trends. It was negatively associated with the poverty rate throughout the study period although the associations were statistically insignificant [regression p range (0.01, 0.97), FDR range (0.13, 0.97), Fig. 3]. Accordingly, ZCTAs with high median household income reported faster growth rates of new cases than ZCTAs with low income. These observations suggested that income-based disparities narrowed despite only to a small degree. Meanwhile, the unemployment rate emerged as a new potential factor of COVID-19 disparities. As the pandemic progressed into the Surge-C period, the number of new cases increased disproportionally fast in ZCTAs with a high unemployment rate (Fig. 3).
Fig. 3.
Impact of financial status on growth rate of COVID-19 cases over time. The effect is measured by standardized coefficient for the median household income (orange solid line), the unemployment rate (magenta dotted line), and the poverty rate (blue dashed line), for each biweekly interval. The size of a circle is proportional to FDR. Solid and open circles indicate significant (FDR < 0.1) and insignificant associations, respectively (Color figure online)
Because the three financial features are strongly correlated with each other and with the percentage of Latinx population (all pairwise correlation test p < 0.02), we also built regression models by removing percentages of ethnic groups and including only a single financial feature each time. Income-based features in these alternative models showed patterns similar to those in the original models but with more significant p values (Supplementary Fig. S3).
Impact of Other Demographic Features
We included population density in the multiple regression models as a proxy of transmission probability. Overall, areas with high population density experienced fast growth rates of COVID-19 during the entire study period (Supplementary Fig. S4A).
Age was not associated with COVID-19 growth rate at the first half of the study period. But starting around mid-August 2021, younger communities were hit harder than older communities (Supplementary Fig. S4B). This pattern continued until the end of the study period, suggesting young age as a new potential factor of COVID-19 disparities.
Sex was not significantly associated with the growth rate of COVID-19 (Supplementary Fig. S4C).
Risk Stratification
Our analysis showed that high percentage of Black or African Americans, high poverty rate, high unemployment rate, high population density, and young age are risk factors for fast COVID-19 growth. Using the median value of each risk factor as the cutoff, we classified 37 ZCTAs meeting all risk criteria as high risk, 22 ZCTAs meeting no risk criteria as low risk, and the remaining areas as median risk. The high-risk areas were clustered in the central Phoenix metropolitan area and the central Tucson area (Supplementary Fig. S5A). Interestingly and possibly related to housing segregation, many high-risk areas were adjacent to low-risk areas (Supplementary Fig. S5B-C). We confirmed that the high-risk group and the low-risk group had significantly different growth rates during all periods (all t-test p < 0.002, Supplementary Fig. S5D).
Discussion
COVID-19 is placing unprecedented challenges on all communities but especially on socially and economically disadvantaged groups [1]. While most existing studies captured only snapshots of the situation using cross-sectional data, we tracked structural health disparities in Arizona over 13 months and learned that COVID-19 vulnerability related to ethnicity, financial status, and age has evolved.
By summer 2021, ZCTAs with a high proportion of Latinx recovered from the early pandemic’s notably high COVID-19 prevalence and faster growth compared to those with fewer Latinx residents. This is in line with a previous report showing Arizona had the biggest disparities in accessing COVID-19 testing among all states examined, putting Latinx at a disadvantage [5]. From the start of the pandemic, many Latinx were not able to shelter-in-place or work virtually due to many factors such as high representation in the service and agricultural industries, reduced job mobility due to legal status, and reduced opportunities to incorporate mitigation measures in general due to lower levels of educational attainment and language barriers [32].
Contrary to the findings of the Massachusetts study [12], our study found that ZCTAs with a higher Latinx population reversed their negative trend after July 2021, when COVID-19 vaccination became widely available. Since then, fewer new cases were reported in these areas than the state average. This observation is concordant with the trend at the national level [11] that reported racial gaps between Latinx and non-Hispanic White populations had narrowed. It is worth noting that Latinx in the US have a higher COVID-19 vaccination rate than other ethnic/racial groups [33]. This change may also reflect the outcomes of the multiple programs established in Arizona to support Latinx communities and other low-income populations during the pandemic [20–22]. Acquired immunity through previous infection or vaccination may also contribute to the slow-down in infections. However, we observed signs of reappearance of the disparities during the Surge-C period, suggesting needs for augmentation of the support programs.
Meanwhile, COVID-19 cases grew very fast in areas with a high percentage of Black or African American populations. This trend in Arizona is in stark contrast to that at the national level [11] and in Massachusetts [12] where the racial gaps between Black and non-Hispanic White populations had narrowed. Furthermore, a high unemployment rate and a young age emerged as significant risk factors. These observations suggested Arizona might have inadequate public health responses and urgent needs of supporting these vulnerable communities to ameliorate the impact. Vaccination hesitancy and interrelated lower vaccination rates among sectors of the African American community and young populations merit further consideration [34, 35].
Arizona has a large aging population, with senior residents comprising the majority in many zip codes. This group had the highest priority to access COVID-19 vaccination. Our analysis showed that COVID-19 growth rates are relatively low in these areas, suggesting these populations are relatively well supported and protected.
Even though these findings make an important contribution to our understanding of the trends of the pandemic’s health disparities, the present study has several limitations. First, because individual-level data are not readily available, we used ZCTA data. Thus, the identified vulnerable groups and their evolving patterns had restricted precision. However, the publicly available ZCTA data allows us to track COVID-19 disparities easily and continuously throughout the present and into the future. Second, we did not include COVID-19 vaccination data in our analysis, although vaccination rates may have significant associations with COVID-19 prevalence and growth rates. This was again due to data availability. Third, the pandemic has disruptive impact on the financial status of many families [36, 37]. Such changes were not incorporated in our analyses because the population composition data were based on the 2019 US Census. Fourth, disparities are attributes of a large region comprising of multiple neighborhoods. Disproportionally high COVID-19 growth rates in certain ZCTAs could be attributable to lack of health resources in surrounding areas.
Although our study is restricted to Arizona data, we expect that COVID-19 disparities in other regions may have also evolved. To better support disadvantaged populations, we need to monitor the progression and adjust resource allocations accordingly.
Conclusions
As the COVID-19 pandemic is dynamic, so are the structural health disparities, which have intensified during this timeframe. In Arizona, much work remains but Latinx communities and low-income populations in general were able to narrow their health disparities gap. Actions are urgently required, however, to enhance the wellbeing of the Black/African American community and unemployed populations.
The COVID-19 pandemic is disproportionally affecting the most vulnerable groups but diverse communities are demonstrating remarkable resilience and strength. Future research should capture and document their stories and the community-based public health strategies they led. Those findings might explain some of the hopeful trends reported in this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study was supported by the NIMHD/NIH Grant (information masked for blind review).
Author Contributions
LL, HO, FM, and GR conceived the presented idea. FLS, JS, ML and LL conducted the analysis. All authors contributed to the manuscript.
Funding
Funding was provided by NIMHD/NIH Grant (5U54MD002316-14).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Flavio F. Marsiglia, Email: marsiglia@asu.edu
Li Liu, Email: liliu@asu.edu.
References
- 1.Turner-Musa J, Ajayi O, Kemp L. Examining social determinants of health, stigma, and COVID-19 disparities. Healthcare (Basel) 2020;8(2):168. doi: 10.3390/healthcare8020168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magesh S, John D, Li WT, Li Y, Mattingly-App A, Jain S, Chang EY, Ongkeko WM. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. doi: 10.1001/jamanetworkopen.2021.34147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan AX, Hinman JA, Abdel Magid HS, Nelson LM, Odden MC. Association between income inequality and county-level COVID-19 cases and deaths in the US. JAMA Netw Open. 2021;4(5):e218799. doi: 10.1001/jamanetworkopen.2021.8799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lieberman-Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID-19 testing and positivity in New York city. Am J Prev Med. 2020;59(3):326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalva-Baird NP, Alobuia WM, Bendavid E, Bhattacharya J. Racial and ethnic inequities in the early distribution of U.S. COVID-19 testing sites and mortality. Eur J Clin Invest. 2021;51(11):e13669. doi: 10.1111/eci.13669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Credit K. Neighbourhood inequity: exploring the factors underlying racial and ethnic disparities in COVID-19 testing and infection rates using ZIP code data in Chicago and New York. Reg Sci Policy Pract. 2020;12(6):1249–1271. doi: 10.1111/rsp3.12321. [DOI] [Google Scholar]
- 7.Centers for Disease Control and Prevention. CDC COVID-19 Response Health Equity Strategy: Accelerating progress towards reducing COVID-19 disparities and achieving health equity. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/cdc-strategy.html.
- 8.DeGarmo DS, De Anda S, Cioffi CC, Tavalire HF, Searcy JA, Budd EL, Hawley McWhirter E, Mauricio AM, Halvorson S, Beck EA, Fernandes L, Currey MC, Ramirez Garcia J, Cresko WA, Leve LD. Effectiveness of a COVID-19 testing outreach intervention for Latinx communities: a cluster randomized trial. JAMA Netw Open. 2022;5(6):e2216796. doi: 10.1001/jamanetworkopen.2022.16796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guerra R. Amid pandemic uncertainties, Latino immigrants put trust in their 'promotoras'. National Geographic. 2022.
- 10.Cherednik I. Modeling the waves of Covid-19. Acta Biotheor. 2021;70(1):8. doi: 10.1007/s10441-021-09428-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Artiga S, Hill L, Haldar S. COVID-19 cases and deaths by race/ethnicity: current data and changes over time. Kaiser Family Foundation. 2021.
- 12.Tieskens K, Patil P, Levy JI, Brochu P, Lane KJ, Fabian MP, Carnes F, Haley BM, Spangler KR, Leibler JH. Time-varying associations between COVID-19 case incidence and community-level sociodemographic, occupational, environmental, and mobility risk factors in Massachusetts. BMC Infect Dis. 2021;21:1–9. doi: 10.1186/s12879-021-06389-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider B, Martinez S, Owens A. Barriers to educational opportunities for Hispanics in the United States. Hispanics and the future of America. 2006. pp. 179–227.
- 14.Wallace PM, Pomery EA, Latimer AE, Martinez JL, Salovey P. A review of acculturation measures and their utility in studies promoting Latino health. Hisp J Behav Sci. 2010;32(1):37–54. doi: 10.1177/0739986309352341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jimenez ME, Rivera-Nunez Z, Crabtree BF, Hill D, Pellerano MB, Devance D, Macenat M, Lima D, Martinez Alcaraz E, Ferrante JM, Barrett ES, Blaser MJ, Panettieri RA, Jr, Hudson SV. Black and Latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Netw Open. 2021;4(7):e2117074. doi: 10.1001/jamanetworkopen.2021.17074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodriguez NM. Community health workers in the United States: time to expand a critical workforce. Am J Public Health. 2022;112(5):697–699. doi: 10.2105/AJPH.2022.306775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Census Data. 2019. https://data.census.gov/cedsci/. Accessed 23 Oct 2021.
- 18.Xu JJ, Chen JT, Belin TR, Brookmeyer RS, Suchard MA, Ramirez CM. Racial and ethnic disparities in years of potential life lost attributable to COVID-19 in the United States: an analysis of 45 states and the District of Columbia. Int J Environ Res Public Health. 2021;18(6):2921. doi: 10.3390/ijerph18062921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chesin M. Latino COVID-19 rates continue to rise. 2020. https://www.azcentral.com/story/news/local/arizona-data/2020/06/27/latino-covid-19-rates-continue-rise/3263558001/.
- 20.Thompson ACL, T. Local Groups Establish Public-Private Partnership to Help Phoenix’s Latino Communities Fight COVID-19. 2020. https://www.equalityhealth.com/members/local-groups-establish-public-private-partnership-to-help-phoenixs-latino-communities-fight-covid-19/.
- 21.American Medical Association. COVID-19 health equity initiatives: Black Arizona COVID-19 Task Force. 2020. https://www.ama-assn.org/delivering-care/population-care/covid-19-health-equity-initiatives-black-arizona-covid-19-task.
- 22.Arizona Department of Revenue. COVID-19 Relief Resources. 2020.
- 23.Monod M, Blenkinsop A, Xi X, Hebert D, Bershan S, Tietze S, Baguelin M, Bradley VC, Chen Y, Coupland H, Filippi S, Ish-Horowicz J, McManus M, Mellan T, Gandy A, Hutchinson M, Unwin HJT, van Elsland SL, Vollmer MAC, Weber S, Zhu H, Bezancon A, Ferguson NM, Mishra S, Flaxman S, Bhatt S, Ratmann O, Imperial College C-RT Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021 doi: 10.1126/science.abe8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiley Z, Kubes JN, Cobb J, Jacob JT, Franks N, Plantinga L, Lea J. Age, comorbid conditions, and racial disparities in COVID-19 outcomes. J Racial Ethn Health Dispar. 2021;9:117–123. doi: 10.1007/s40615-020-00934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.United States Census Bureau. ZIP Code Tabulation Areas (ZCTAs). 2022. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/zctas.html.
- 26.Hest R. U.S. Census Bureau Analytic Report Shows Significant Non-Response Bias in the 2020 American Community Survey. 2021. https://www.shadac.org/news/significant-non-response-bias-in-2020-ACS.
- 27.Arizona COVID-19 Data Portal. https://azdhs.gov/covid19/data/index.php. Accessed 25 Nov 2021.
- 28.Zeileis A, Leisch F, Hornik K, Kleiber C. strucchange: an R package for testing for structural change in linear regression models. J Stat Softw. 2002;7(1):1–38. [Google Scholar]
- 29.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc: Ser B (Methodol) 1995;57(1):289–300. [Google Scholar]
- 30.Newman TB, Browner WS. In defense of standardized regression coefficients. Epidemiology. 1991;2(5):383–386. doi: 10.1097/00001648-199109000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Silversmith S. Report shows several Arizona counties with high poverty and COVID death rates. 2022. https://www.google.com/search?client=firefox-b-1-d&q=arizona+poverty+covid-19+disparities.
- 32.Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, Baral S, Prado GJ, Marzan-Rodriguez M, Beyrer C, Sullivan PS, Millett GA. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. 2020;52(46–53):e2. doi: 10.1016/j.annepidem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Disease Control and Prevention. Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States. 2020. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic.
- 34.Khubchandani J, Macias Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: a review and recommendations for practice. Brain Behav Immun Health. 2021;15:100277. doi: 10.1016/j.bbih.2021.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Center for Disease Control and Prevention. COVID-19 Vaccination Coverage and Intent Among Adults Aged 18–39 Years — United States, March–May 2021. 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7025e2.htm. [DOI] [PMC free article] [PubMed]
- 36.Brewer M, Gardiner L. The initial impact of COVID-19 and policy responses on household incomes. Oxf Rev Econ Policy. 2020;36(1):S187–S199. doi: 10.1093/oxrep/graa024. [DOI] [Google Scholar]
- 37.Acs G, Karpman M. Employment, income, and unemployment insurance during the Covid-19 Pandemic. Urban Institute. 2020. pp. 1–11.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.