Abstract
INTRODUCTION
This study aims to evaluate the prevalence of xerostomia in a healthy population with e-cigarettes and/or combustible tobacco.
METHODS
The following electronic databases were searched: Web of Science, Chinese Biomedical Literature Database (CBM), PubMed, Cochrane Library, Embase, Chinese National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (VIP), and Wan-Fang Database, from 1 January 2000 to 20 October 2022. The language was limited to Chinese and English. The data were analyzed using Stata 15.0, and the prevalence of xerostomia in different smokers is reported.
RESULTS
A total of 14 studies were included, with a total sample size of 6827 cases. The overall prevalence of xerostomia was 26% (95% CI: 18–35). In the combustible tobacco population, the prevalence of xerostomia was 24% (95% CI: 21–27), while among e-cigarette users it was 33% (95% CI: 18–48).
CONCLUSIONS
Current evidence suggests that the prevalence of xerostomia is high in healthy smoking populations. These findings are restricted by the number and quality of the included studies and need to be validated by additional high-quality studies.
Keywords: e-cigarettes, meta-analysis, tobacco, xerostomia
INTRODUCTION
Nearly 1 billion individuals worldwide suffer from the health risks associated with smoking tobacco1. The World Health Organization (WHO) states that in 2004, tobacco use caused the deaths of nearly 5 million people aged ≥30 years, worldwide2. CDC analyzed data from the 2019 National Health Interview Survey (NHIS) in 2019, and estimated that 50.6 million US adults (20.8%) reported currently using any tobacco product, including combustible tobacco (14.0%) and e-cigarettes (4.5%). E-cigarette use was highest among adults aged 18–24 years (9.3%)3. According to a study in the New England Journal of Medicine, the number of adolescents using e-cigarettes increased by 10% between 2017 and 2018, affecting 1.3 million young people, and continued to rise from 2018 to 20194,5.
It is well known that smoking is a significant factor for oral health problems. Smokers are exposed to more than 7000 chemicals per puff, which alters the salivary component, resulting in impaired oral protection6. Seeme et al.7 showed that active smokers had higher clinical oral dryness (COD) scores and lower salivary flow rate (SFR). Xerostomia, a subjective sensation of dry mouth, is a side effect of e-cigarette use in adults and youth8,9. Lack of saliva secretion can lead to difficulties swallowing, chewing, and speaking, as well as mouth burning, poor breath, altered taste, oral mucosa dryness, tongue inflammation, cracked and flaking lips, oral candidiasis, and dental caries, resulting in poor quality of life for the people10,11. Xerostomia affects 5.5% to 46% of the population, most usually older, and is more common in women than men12. Additionally, 9% of Australians between the ages of 15 and 34 years, have reported experiencing dry mouth which may harm young people13. The prevalence of xerostomia has been related to a worse level of oral health-related quality of life in a study of people in their early 30s14. People who lack saliva are at an increased risk of oral infection and dental caries11.
Combustible tobacco and e-cigarette use may be more prevalent among the risk factors of xerostomia15-18. A study of dental students found that tobacco users (29.3%), e-cigarette users (33.1%), and dual users (28.1%), reported a significantly higher prevalence of xerostomia than non-smokers (23.4%)19. Chaffee et al.20 found that frequent/always dry mouth was more prevalent among frequent (>5 days/month) e-cigarette (14%) and combustible tobacco users (19%). E-cigarette users, including 14.9% of US adolescents aged 13–17 years and 24.4% of medical students, reported dry mouth9-21. Among e-cigarette users aged ≥18 years, the prevalence of xerostomia was 31.0%8. Smokers were more likely to have dry mouths in all ages and sexes22.
The relationship between smoking and xerostomia is crucial for public health. Smoking harms nearly every organ in the body. Severe health effects include the risk of nicotine addiction and potential harm to brain development from e-cigarette use23, as well as potential respiratory and cardiovascular hazards associated with e-cigarette use24. As the potential association of combustible tobacco and e-cigarette use with xerostomia has not been fully explored, this systematic review and meta-analysis sought to provide an evidence-based estimation of the global prevalence of xerostomia among healthy people who used e-cigarettes and combustible tobacco.
METHODS
We conducted a meta-analysis of observational studies comparing the prevalence of xerostomia in healthy populations who smoke. This meta-analysis was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The meta-analysis has been registered on the International Prospective Register of Systematic Reviews (PROSPERO), and the trial registration number is CRD42022319706.
Search strategy
The following electronic databases were searched in this study: Web of Science, PubMed, Cochrane Library, Embase, Chinese Biomedical Literature Database (CBM), Chinese National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (VIP), and Wan-Fang Database from 1 January 2000 to 20 October 2022, independently by two researchers (XG and PX). There were no limitations on publication status, but the language was limited to Chinese and English. Using the terms: ‘dry mouth’, ‘xerostomia’, ‘cigarette smoking’, ‘tobacco’, ‘cigarette smoking’, ‘smoking’, ‘Electronic Nicotine Delivery Systems’ and ‘e-cigarettes’, articles were searched in all available combinations. The complete search strategy is available in the Supplementary file.
Selection criteria
Xerostomia was defined as the subjective sensation of dry mouth or low salivary flow rates. The inclusion criteria were: 1) focus on healthy people; 2) include data on the prevalence of xerostomia in e-cigarette and/or combustible tobacco users; and 3) observational studies. The researchers excluded articles that: 1) were duplicate publications, reviews, case reports, incomplete, incorrect information, or low-quality evaluation; 2) had restricted access to the full text; 3) were in a language other than English and Chinese.
Extraction of data
Included articles were independently reviewed by two researchers (XG and XP), based on title/abstract first, and full-text second, according to the inclusion criteria. Any controversy was resolved by a discussion or with a third researcher (LH). The following information was extracted using a defined standard data template form: study characteristics, country, participants, and results. Two reviewers (XG and TF) independently extracted and verified data using the template, and any disagreements were settled through discussion.
Bias and quality assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the literature of case-control studies25, which evaluates the quality of the literature in terms of study population selection, comparability, exposure (case-control studies), or outcome (cohort studies), with a score of 0–9. Besides, we used quality evaluation criteria for cross-sectional studies recommended by the Agency for Healthcare Research and Quality (AHRQ). The proposed criteria include 11 items, with one point for each item, and the quality of the literature is based on the total score, which is divided into low (1–3), medium (4–7), and high quality (8–11)26.
Statistical analysis
Stata 15.0 software was used for single-group rate meta-analysis. The I2 statistic detected statistical heterogeneity. The random-effect model was used for data synthesis. Significant clinical heterogeneity was addressed using subgroup analysis. Subgroup analysis factors included type of smoking, country, and age. The potential publication bias of the meta-analysis was determined by Begg’s test and Egger’s test.
RESULTS
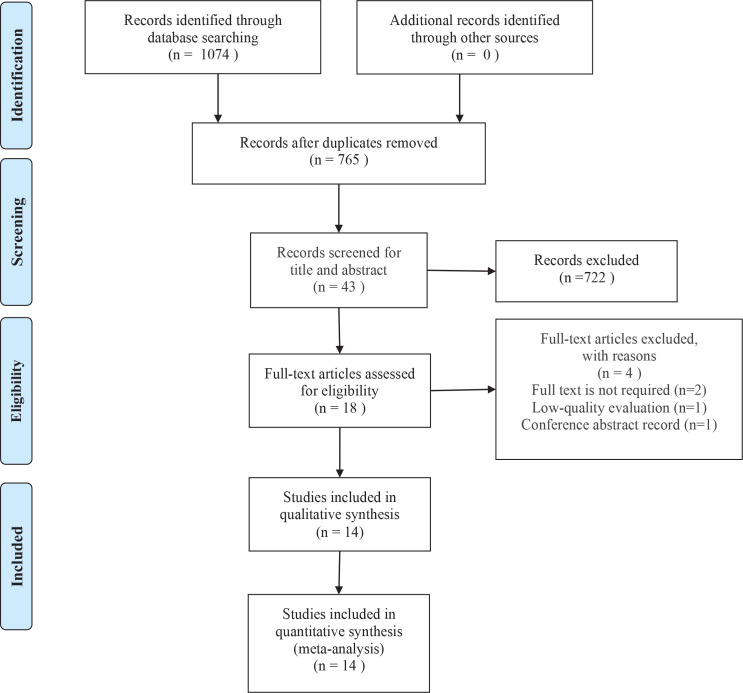
In total, 1074 published articles were collected from online databases, including Web of Science, PubMed, Cochrane Library, Embase, Chinese Biomedical Literature Database (CBM), Chinese National Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), and Wan-Fang Database. All studies were published from 1 January 2000 to 20 October 2022. After deleting duplicates, 765 studies were obtained. After the review of the titles and abstracts, 43 articles were chosen for full-text review. Due to the unavailability of full text or not measuring the outcome of interest, 14 articles were selected for the qualitative synthesis. Finally, 14 articles8,9,19-21,25-33 were included in the quantitative synthesis (meta-analysis), including 12 cross-sectional and 2 case-control studies. The PRISMA flow diagram of study selection is shown in Figure 1.
Figure 1.
Flow diagram of the study selection process
Characteristics and risk of bias evaluation of the included studies
The characteristics of the included studies can be found in Table 1. Data were extracted on the author, year of publication, country, study design, sample size (cases), the prevalence of xerostomia, age, gender, outcome (s) reported, and definition of smokers. The year of publication of the included literature was between 2014 and 2022. We identified studies across multiple countries: USA (n=3), Saudi Arabia (n=3), Pakistan (n=2); and one study in each of India, Poland, Italy, China, Egypt, plus a study with participants from 11 countries (Croatia, Iraq, Jordan, Kuwait, Lebanon, Malaysia, Nigeria, Saudi Arabia, South Africa, Turkey, and Yemen). Overall, 6827 participants were included in this study from all articles. The sample size of studies ranged from 39 to 1624 participants. Type of smoking includes both combustible tobacco and e-cigarettes. The age ranges were between 14 and 65 years. The included studies reported males to be the majority of their participants. The quality appraisal of the included studies is shown in Tables 2 and 3.
Table 1.
Characteristics of the included studies on the prevalence of xerostomia among e-cigarette or combustible tobacco users
| Authors Year | Study design | Country | Sample size (Cases) | Prevalence of xerostomia | Age (years) Mean ± SD | Gender | The outcome(s) reported | Definition of smokers |
|---|---|---|---|---|---|---|---|---|
| Dyasanoor et al.25 2014 | Case-control | India | Combustible tobacco: 60 | 37.00% | 36.98 ± 11.52 | NR | Modified Schirmer test and PROs | Daily smoking for six months |
| Ullah et al.26 2015 | Cross-sectional | Pakistan | E-cigarettes/combustible tobacco: 250 | 10.40% | 21.66 ± 2.07 | 100% male |
PROs | NR |
| King et al.8 2019 | Cross-sectional | USA | E-cigarettes: 1624 | 31.00% | 18–24: 25.5% 25–44: 48.2% ≥45: 26.3% |
56.1% male 43.9% female |
PROs | Ever e-cigarette users |
| Kumar et al.27 2019 | Cross-sectional | Pakistan | E-cigarettes/combustible tobacco: 377 | 15.12% | aged 28–64 | 90.45% male 9.55% female |
PROs | NR |
| Lewek et al.28 2019 | Cross-sectional | Poland | E-cigarettes: 1032 | 8.30% | 25.9 ± 11.1 | 85.6% male 14.4% female |
PROs | Ever smoked or currently smoking |
| Gallus et al.29 2020 | Cross-sectional | Italy | E-cigarettes: 395 | 25.40% | 51.3 ± 13.0 | 53.6% male 46.4% female |
PROs | Current and ex-smokers |
| Habib et al.21 2020 | Cross-sectional | Saudi Arabia | E-cigarettes: 49 | 24.49% | aged 18–23 | NR | PROs | Ever smoked or currently smoking |
| Nazir et al.30 2020 | Cross-sectional | Saudi Arabia | E-cigarettes/combustible tobacco: 199 | 31.20% | <16 | NR | PROs | NR |
| King et al.9 2020 | Cross-sectional | USA | E-cigarettes/combustible tobacco: 141 | 14.18% | 16 | 60.2% male 39.8% female |
PROs | Past 30-day smoking |
| Chaffee et al.20 2021 | Cross-sectional | USA | E-cigarettes: 976 | Occasionally: 54.2% Frequently: 5.4% Always: 0.4% |
<18 | 36.6% male 60.9% female 2.6% other |
PROs | Past 30-day smoking |
| Peng et al.31 2021 | Case-control | China | E-cigarettes: 85 Combustible tobacco: 92 |
E-cigarettes: 35.29% Combustible tobacco: 8.69% |
E-cigarettes: 21.87 ± 1.79 Combustible tobacco: 21.66 ± 2.36 |
E-cigarettes: 65.88% male 34.12% female Combustible tobacco: 58.7% male 41.3% female |
PROs | History of smoking ≥1 year |
| Kabbash et al.32 2022 | Cross-sectional | Egypt | E-cigarettes: 39 | 48% | NR | NR | PROs | NR |
| Tantawi et al.33 2022 | Cross-sectional | Saudi Arabia | E-cigarettes/combustible tobacco: 657 | 18.60% | 18–23 | NR | PROs | NR |
| Alhajj et al.19 2022 | Cross-sectional | 11 countries: Croatia, Iraq, Jordan, Kuwait, Lebanon, Malaysia, Nigeria, Saudi Arabia, South Africa, Turkey, and Yemen | E-cigarettes: 255 Combustible tobacco: 596 |
E-cigarettes: 31.76% Combustible tobacco: 28.86% |
E-cigarettes: ≤20 : 72 >20 : 183 Combustible tobacco: ≤20 : 178 >20 : 418 |
E-cigarettes: 65.88% male 30.98% female Combustible tobacco: 57.72% male 42.28% female |
PROs | NR |
NR: not reported. PROs: patient-reported outcomes.
Table 2.
Results of the risk of bias evaluation for case-control studies included (score)
| Study | Selection | Comparability | Exposure | Score |
|---|---|---|---|---|
| Diasakos et al. 2014 | 4 | 1 | 2 | 7 |
| Peng et al. 2021 | 4 | 2 | 1 | 7 |
Table 3.
Risk of bias evaluation results for cross-sectional studies included (score)
| Study | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | ⑪ | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ullah et al. 2015 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 7 |
| King et al. 2019 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| Lewek et al. 2019 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 8 |
| Kumar et al. 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| King et al. 2020 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 8 |
| Habib et al. 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 8 |
| Nazir et al. 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Gallus et al. 2020 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| Chaffee et al. 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Alhajj et al. 2022 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Tantawi et al. 2022 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 9 |
| Kabbash et al. 2022 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 9 |
Define the source of information (survey, record review);
List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications;
Indicate time period used for identifying patients;
Indicate whether or not subjects were consecutive if not population-based;
Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants;
Describe any assessments undertaken for quality assurance purposes (e.g. test/retest of primary outcome measurements);
Explain any patient exclusions from analysis;
Describe how confounding was assessed and explain any patient exclusions from analysis;
If applicable, explain how missing data were handled in the analysis;
Summarize patient response rates and completeness of data collection;
Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained.
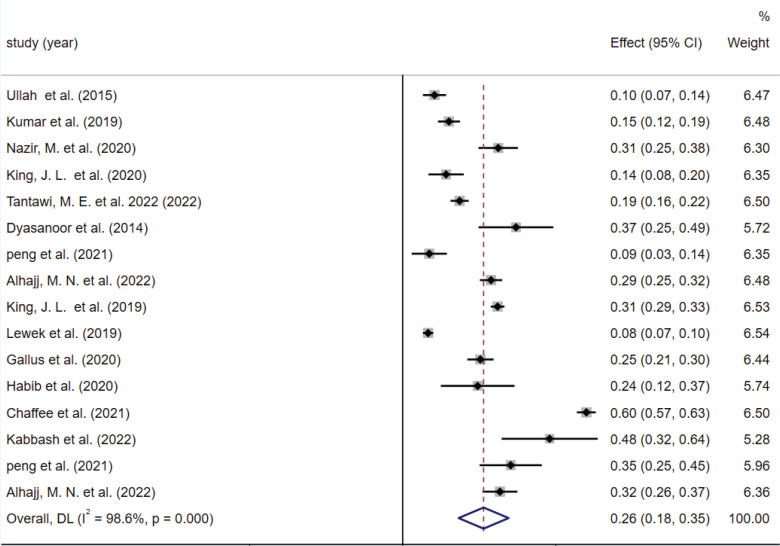
The prevalence of xerostomia
A total of 14 studies were included 8,9,19-21,25-33, with a total sample size of 6827 cases. We summarized the prevalence of xerostomia for all smokers. Two studies25,31 reported the prevalence of xerostomia in both e-cigarette and combustible tobacco populations, and we included these two indexes in meta-analyses to synthesize the data separately. The results of the random-effects model meta-analysis showed that the overall prevalence of xerostomia was 26% (95% CI: 18–35) in the population of smokers (combustible and/or e-cigarette) (Figure 2). The published risk of bias assessment indicated that the risk for publication bias was not statistically identified by the Begg test (p=0.499), but was detected by the Egger test (p=0.007). We present publication bias plots in Supplementary file Material 1.
Figure 2.
Forest plot of the overall included studies on the prevalence of xerostomia among e-cigarette or combustible tobacco users
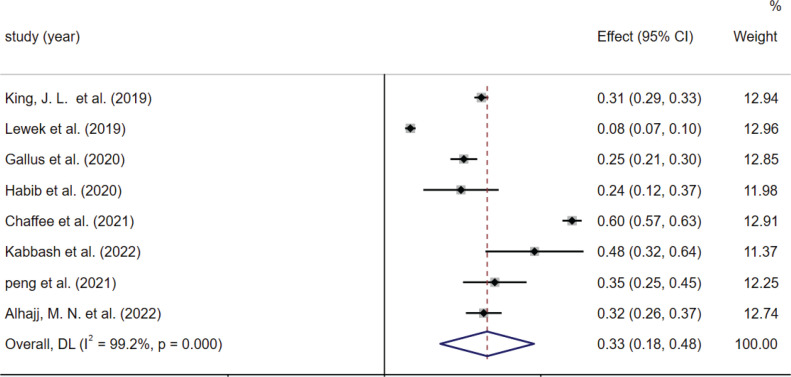
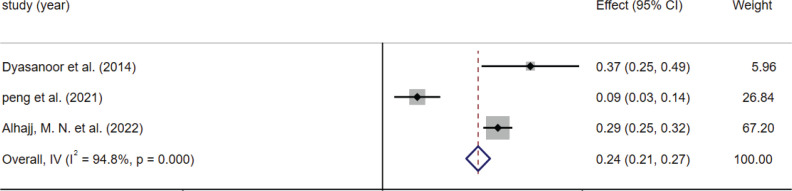
Subgroup analysis
Subgroup analysis was performed according to the type of smoking (Figures 3 and 4), country, and age. The results differed by the type of smoking: the prevalence of dry mouth was 33% (95% CI: 18–48) in the e-cigarette population and 24% (95% CI: 21–27) in the combustible tobacco population. Results also differed by country: the prevalence of xerostomia was 39% (95% CI: 37–40) in the United States, 13% (95% CI: 10–15) in Pakistan, and 21% (95% CI: 18–24) in Saudi Arabia. When the included literature was grouped according to age: the prevalence of dry mouth was 30% (95% CI: 28–32) for those aged <25 years and 20% (95% CI: 18–23) for 25–65 years (Table 4). We presented forest plots of subgroup analyses in Supplementary file Material 2.
Figure 3.
The effect size and 95% CI of included studies based on e-cigarette use
Figure 4.
The effect size and 95% CI of included studies based on combustible tobacco use
Table 4.
Subgroup analyses on the prevalence of xerostomia among e-cigarette or combustible tobacco users
| Variables | Number of studies | % (95% CI) | p | Heterogeneity | |
|---|---|---|---|---|---|
| I2 (%) | p | ||||
| All studies | 14 | 26 (18–35) | <0.001 | 99 | <0.001 |
| Type of smoking | |||||
| E-cigarette | 8 | 33 (18–48) | <0.001 | 99 | <0.001 |
| Combustible tobacco | 3 | 24 (21–27) | <0.001 | 95 | <0.001 |
| Country | |||||
| USA | 3 | 39 (37–40) | <0.001 | 99 | <0.001 |
| Saudi Arabia | 3 | 21 (18–24) | <0.001 | 84 | 0.002 |
| Pakistan | 2 | 13 (10–15) | <0.001 | 68 | 0.077 |
| Age (years) | |||||
| <25 | 6 | 30 (28–32) | <0.001 | 99 | <0.001 |
| 25–65 | 3 | 20 (18–23) | <0.001 | 90 | <0.001 |
DISCUSSION
This systematic review was performed to evaluate the prevalence of xerostomia in healthy populations with e-cigarettes and/or combustible tobacco and assess the influencing factors of dry mouth. The included literature included 12 cross-sectional studie8,9,19-21,26-30,32,33 and 2 case-control studies25,31. We sought to explore the influences of smoking on xerostomia to help better understand the oral health risks of smoking and support healthcare providers in planning viable cessation programs that would help smokers effective and long-term cessation.
Subgroup analysis found significant differences in xerostomia by smoking type, country, and age. The difference for us is that the prevalence of dry mouth is higher for e-cigarettes (33%) than for combustible tobacco (24%), which follows the findings of Peng et al.31 and Alhajj et al.19. In previous reports, e-cigarettes were considered less harmful to users as an aid to smoking cessation and a replacement for regular cigarettes28,34,35. Pop et al.36 found that clinically healthy young tobacco smokers and e-cigarette users presented an increased number of micronuclei in the oral epithelial cells, compared to non-smoking individuals. Bardellini et al.37 reported e-cigarette users to have more frequent oral lesions, burns, or inflammation compared to former or non-smokers. Since aerosol propylene glycol and glycerin are the main components of e-liquid, they are associated with mouth and throat irritation. The adverse effects most frequently mentioned by those surveyed (such as a sore/dry throat, cough, and mouth/throat discomfort) are frequently described in the literature38,39.
In addition, the prevalence of xerostomia was higher in the United States (39%) than in Pakistan (13%) and Saudi Arabia (21%). More than half of the US adults in a large, national sample who had ever used an e-cigarette reported experiencing at least one negative symptom as a result of their usage. Dry mouth is one of the most common symptoms8. Moreover, smokers under 25 years of age (30%) were more likely to report dry mouth, which is similar to the findings of King et al.9. Because of the high level of self-consciousness among young people, e-cigarette use is growing in popularity. Young adults aged 18–24 years were found to have the highest prevalence of smoking, as were both current and former smokers40. In an analysis based on the Eurobarometer 385 survey of 26566 participants, it was found that respondents aged 15–24 years were 3.3 times more likely to be users versus older participants41.
It is worth mentioning that there is no uniform definition of smokers and assessment of xerostomia, in all the literature. We summarized the definition of smoking: ‘Ever smoked or currently smoking’, ‘Past 30-day smoking’, ‘History of smoking ≥ 1 year’, and ‘Daily smoking for six months’. All included studies defined xerostomia as a subjective patient-reported sensation of dry mouth, and this leads to differences in the prevalence of xerostomia. Chaffee et al.20 categorized dry mouth as ‘Occasionally’, ‘Frequently’, and ‘Always’, which makes the prevalence of dry mouth as high as 60%. While perception is important for understanding, clinical validation may be needed to verify symptoms and determine the severity of symptoms when used. Furthermore, e-cigarette and tobacco products differ significantly, and different product characteristics may be associated with different types and frequencies of symptoms.
Strengths and limitations
To the best of our knowledge, this study is the first meta-analysis to evaluate the prevalence of xerostomia among e-cigarette and/or combustible tobacco users. This review included studies with 6827 participants. Moreover, we also performed subgroup analyses to discuss the prevalence of xerostomia by smoking type, country, and age.
However, this study also has some limitations. First, most of the included studies were short-term observational studies, so some biases could not be avoided due to the limitations of the study design. Moreover, after doing a subgroup analysis, the heterogeneity among various subgroups remained significant, and the variables driving research heterogeneity could not be determined, which may impair the correctness of the results. Furthermore, the subgroup analyses were limited to three characteristics, but future studies could explore additional characteristics such as study setting, the participant’s education level, socioeconomic status, smoking habits, and severity of dry mouth. Finally, the number of studies included in the analyses was limited, needing the inclusion of more high-quality studies to offer evidence.
CONCLUSIONS
Research shows that smokers may be more likely to experience dry mouth. E-cigarette users were more likely to have dry mouth than tobacco users. Dry mouth is more common among young smokers, which suggests that we should perhaps pay more attention to the awareness of the risks of smoking among young people and take appropriate measures to aid cessation. However, more research into the association between smoking and the severity of dry mouth is needed. Because the number of smokers has increased in recent years, and dry mouth can negatively impact people’s quality of life, oral hygienists should give more emphasis to tobacco and e-cigarette use in clinical practice. The above conclusions need to be verified by additional high-quality studies due to the constraints of the number and quality of the included studies.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the authors of the studies included in this meta-analysis.
CONFLICTS OF INTEREST
The authors have each completed and submitted an ICMJE form for disclosure of potential conflicts of interest. The authors declare that they have no competing interests, financial or otherwise, related to the current work. All the authors report that since the initial planning of the work, this study was supported by the Shanghai Association for Science and Technology and the innovation research team of high-level local universities in Shanghai.
FUNDING
This study was supported by the Shanghai Association for Science and Technology (21002411300) and innovation research team of high-level local universities in Shanghai (SHSMU-ZDCX20212802).
ETHICAL APPROVAL AND INFORMED CONSENT
Ethical approval and informed consent were not required for this study.
DATA AVAILABILITY
The data supporting this research can be found in the Supplementary file.
AUTHORS’ CONTRIBUTIONS
XG designed this study, and LH is the guarantor for the article. XG, FT and XP drafted the article, which was revised by LH who serves as an adviser for methodology. The publication of the review has been authorized by all of the authors.
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
REFERENCES
- 1.Organisation for Economic Co-operation and Development, World Health Organization . Health at a Glance: Asia/Pacific 2020. Measuring Progress Towards Universal Health Coverage. OECD Publishing; 2020. [DOI] [Google Scholar]
- 2.World Health Organization . WHO global report: mortality attributable to tobacco. World Health Organization; 2012. Accessed October 2, 2022. https://www.who.int/publications/i/item/9789241564434. [Google Scholar]
- 3.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–1742. doi: 10.15585/mmwr.mm6946a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Final Report. N Engl J Med. 2020;382(10):903–916. doi: 10.1056/NEJMoa1911614. [DOI] [PubMed] [Google Scholar]
- 5.Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Adolescent Vaping and Nicotine Use in 2017-2018 - U.S. National Estimates. N Engl J Med. 2019;380(2):192–193. doi: 10.1056/NEJMc1814130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson JH, Griffith DW, Jr, Conner BT, Crooks EL, Brewer DB., Jr Tobacco-containing smoking article. US 7 726 320 B2. United States Patent. Accessed October 2, 2022. https://scienceon.kisti.re.kr/srch/selectPORSrchPatent.do?cn=USP2010067726320.
- 7.Nigar S, Hassan S, Maqsood A, et al. An assessment of unstimulated salivary flow rate, IgA and clinical oral dryness among active and passive smokers. Int J Occup Med Environ Health. 2022;35(1):39–51. doi: 10.13075/ijomeh.1896.01829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King JL, Reboussin BA, Wiseman KD, et al. Adverse symptoms users attribute to e-cigarettes: Results from a national survey of US adults. Drug Alcohol Depend. 2019;196:9–13. doi: 10.1016/j.drugalcdep.2018.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King JL, Reboussin BA, Merten JW, Wiseman KD, Wagoner KG, Sutfin EL. Negative health symptoms reported by youth e-cigarette users: Results from a national survey of US youth. Addict Behav. 2020;104:106315. doi: 10.1016/j.addbeh.2020.106315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millsop JW, Wang EA, Fazel N. Etiology, evaluation, and management of xerostomia. Clin Dermatol. 2017;35(5):468–476. doi: 10.1016/j.clindermatol.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Jensen SB, Pedersen AM, Vissink A, et al. A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: prevalence, severity and impact on quality of life. Support Care Cancer. 2010;18(8):1039–1060. doi: 10.1007/s00520-010-0827-8. [DOI] [PubMed] [Google Scholar]
- 12.Rocchi C, Emmerson E. Mouth-Watering Results: Clinical Need, Current Approaches, and Future Directions for Salivary Gland Regeneration. Trends Mol Med. 2020;26(7):649–669. doi: 10.1016/j.molmed.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Jamieson LM, Thomson WM. Xerostomia: its prevalence and associations in the adult Australian population. Aust Dent J. 2020;65(Suppl 1):S67–S70. doi: 10.1111/adj.12767. [DOI] [PubMed] [Google Scholar]
- 14.Thomson WM, Lawrence HP, Broadbent JM, Poulton R. The impact of xerostomia on oral-health-related quality of life among younger adults. Health Qual Life Outcomes. 2006;4:86. doi: 10.1186/1477-7525-4-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.East KA, Reid JL, Rynard VL, Hammond D. Trends and Patterns of Tobacco and Nicotine Product Use Among Youth in Canada, England, and the United States From 2017 to 2019. J Adolesc Health. 2021;69(3):447–456. doi: 10.1016/j.jadohealth.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matilla-Santander N, Fu M, Ballbè M, et al. Use of electronic cigarettes in public and private settings in Barcelona (Spain) Environ Res. 2017;158:685–690. doi: 10.1016/j.envres.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Shi Y, Cummins SE, Zhu SH. Use of electronic cigarettes in smoke-free environments. Tob Control. 2017;26(e1):e19–e22. doi: 10.1136/tobaccocontrol-2016-053118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students - United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276–1277. doi: 10.15585/mmwr.mm6745a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alhajj MN, Al-Maweri SA, Folayan MO, et al. Oral health practices and self-reported adverse effects of E-cigarette use among dental students in 11 countries: an online survey. BMC Oral Health. 2022;22(1):18. doi: 10.1186/s12903-022-02053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaffee BW, Halpern-Felsher B, Cheng J. E-cigarette, cannabis and combustible tobacco use: associations with xerostomia among California adolescents. Community Dent Oral Epidemiol. 2021 doi: 10.1111/cdoe.12721. 10.1111/cdoe.12721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Habib E, Helaly M, Elshaer A, et al. Prevalence and perceptions of e-cigarette use among medical students in a Saudi University. J Family Med Prim Care. 2020;9(6):3070–3075. doi: 10.4103/jfmpc.jfmpc_235_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kakoei S, Nekouei AH, Kakooei S, Najafipour H. The effect of demographic characteristics on the relationship between smoking and dry mouth in Iran: a cross-sectional, case-control study. Epidemiol Health. 2021;43:e2021017. doi: 10.4178/epih.e2021017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health . Smoking Cessation: A Report of the Surgeon General. US Department of Health and Human Services; 2020. Accessed October 2, 2022. https://www.ncbi.nlm.nih.gov/books/NBK555591/pdf/Bookshelf_NBK555591.pdf. [Google Scholar]
- 24.Neczypor EW, Mears MJ, Ghosh A, et al. E-Cigarettes and Cardiopulmonary Health: Review for Clinicians. Circulation. 2022;145(3):219–232. doi: 10.1161/CIRCULATIONAHA.121.056777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dyasanoor S, Saddu SC. Association of Xerostomia and Assessment of Salivary Flow Using Modified Schirmer Test among Smokers and Healthy Individuals: A Preliminutesary Study. J Clin Diagn Res. 2014;8(1):211–213. doi: 10.7860/JCDR/2014/6650.3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ullah H, Iqbal U, Azhar S, Khan IU, Murtaza G. Prevalence and Psychological Characterization of Smoking amongst University Students in Abbottabad, Khyber Pakhtunkhwa, Pakistan. Tropical Journal of Pharmaceutical Research. 2015;14(11):2121–2124. doi: 10.4314/tjpr.v14i11.24. [DOI] [Google Scholar]
- 27.Kumar S, Khan A, Nadeem B, Rajput AH, Muneeb M. Prevalence of root caries among cigarette smokers presenting to Liaquat University Hospital. Indo American Journal of Pharmaceutical Sciences. 2019;6(3):5304–5308. Accessed October 2, 2022. https://zenodo.org/record/2593156#.Y4Cm63bP3g4. [Google Scholar]
- 28.Lewek P, Woźniak B, Maludzińska P, Smigielski J, Kardas P. E-cigarette use and its predictors: Results from an online cross-sectional survey in Poland. Tob Induc Dis. 2019;17(November) doi: 10.18332/tid/113093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gallus S, Borroni E, Liu X, et al. Electronic cigarette use among Italian smokers: patterns, settings, and adverse events. Tumori. 2020:300891620915784. doi: 10.1177/0300891620915784. [DOI] [PubMed] [Google Scholar]
- 30.Nazir M, AlAbdullah H, Alhareky M, Al-Ansari A, Alhumaid J. Influence of Dental Pain and Tooth Sensitivity on the Intention to Quit Smoking among Schoolchildren. Int J Dent. 2020;2020:8823146. doi: 10.1155/2020/8823146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng LF, Yi F, Hunan Changsha Stomatological Hospital The effects of e-cigarettes on oral health in youth. Article in Chinese. Journal of Hunan Normal University (Medical Sciences) 2021;18(6):168–170. [Google Scholar]
- 32.Kabbash IA, Awad AE, Farghly AA, Naeem EM, Saied SM. The era of electronic smoking: perceptions and use of E-Cigarettes among university students, Egypt. Int J Health Promot Educ. 2022 doi: 10.1080/14635240.2022.2052146. [DOI] [Google Scholar]
- 33.El Tantawi M, Sabbagh HJ, Alkhateeb NA, et al. Oral manifestations in young adults infected with COVID-19 and impact of smoking: a multi-country cross-sectional study. PeerJ. 2022;10:e13555. doi: 10.7717/peerj.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA. Quit Methods Used by US Adult Cigarette Smokers, 2014-2016. Prev Chronic Dis. 2017;14:E32. doi: 10.5888/pcd14.160600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.East K, Brose LS, McNeill A, Cheeseman H, Arnott D, Hitchman SC. Harm perceptions of electronic cigarettes and nicotine: A nationally representative cross-sectional survey of young people in Great Britain. Drug Alcohol Depend. 2018;192:257–263. doi: 10.1016/j.drugalcdep.2018.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pop AM, Coroș R, Stoica AM, Monea M. Early Diagnosis of Oral Mucosal Alterations in Smokers and E-Cigarette Users Based on Micronuclei Count: A Cross-Sectional Study among Dental Students. Int J Environ Res Public Health. 2021;18(24):13246. doi: 10.3390/ijerph182413246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bardellini E, Amadori F, Conti G, Majorana A. Oral mucosal lesions in electronic cigarettes consumers versus former smokers. Acta Odontol Scand. 2018;76(3):226–228. doi: 10.1080/00016357.2017.1406613. [DOI] [PubMed] [Google Scholar]
- 38.Goniewicz ML, Lingas EO, Hajek P. Patterns of electronic cigarette use and user beliefs about their safety and benefits: an internet survey. Drug Alcohol Rev. 2013;32(2):133–140. doi: 10.1111/j.1465-3362.2012.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106(11):2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 40.Sutfin EL, McCoy TP, Morrell HE, Hoeppner BB, Wolfson M. Electronic cigarette use by college students. Drug Alcohol Depend. 2013;131(3):214–221. doi: 10.1016/j.drugalcdep.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vardavas CI, Filippidis FT, Agaku IT. Determinants and prevalence of e-cigarette use throughout the European Union: a secondary analysis of 26 566 youth and adults from 27 Countries. Tob Control. 2015;24(5):442–448. doi: 10.1136/tobaccocontrol-2013-051394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this research can be found in the Supplementary file.