Abstract
Over the years, we have made considerable progress in our understanding of the biology of various cancers leading to advancements in their management strategies. Consequently, we have witnessed steady improvements in survival rates of cancer patients post-diagnosis. The progress; however, has been slow for some cancer types and the advances in cancer care have not benefited all the communities equally in the United States. The state of Alabama has one of the most diverse demographics in the country and as a result, we witness significant health disparities among our populations. Breast and cervical cancers are the two major cancer types that disparately affect the women in our state. Here, we describe the extent of disparities in the diagnosis and death rates from these cancers in the state of Alabama and discuss potential underlying causes affecting the health outcomes. We also discuss ongoing efforts undertaken to reduce the disparity gaps and provide a perspective for addressing these disparities more effectively.
Keywords: Breast Cancer, Cervical Cancer, Cancer Health Disparities, African American, Caucasian American
Introduction
Cancer is the second leading cause of death in the nation, following only behind heart disease (Nagai and Kim, 2017). This year, nearly 1.9 million new cancer diagnoses and about 609,360 cancer-related deaths are expected to occur in the United States (Siegel et al., 2022). This number is 0.9% and 1% higher than the last year for overall cancer incidence and mortality, respectively (Siegel et al., 2021, Siegel et al., 2022). Among the multiple cancers affecting women, breast cancer (BC) is the most common, with an overall annual incidence of 287,850 nationwide and an estimated death of 43,250 women (Siegel et al., 2022). Cervical cancer (CC) is another common malignancy that affects women with an expected 14,100 diagnoses this year alone in the United States and an estimated death of 4280 women according to the American Cancer Society (ACS). While these statistics might be startling, the state of Alabama has even higher all-site cancer incidence and mortality rates than the national average. From the years 2014–2018, the cancer incidence rate in Alabama was 450.8 compared to 448.6 nationwide per 100,000 persons, and from 2015–2019 the mortality rate was 170.0 for Alabama, compared to 152.4 per 100,000 in all states combined (Profiles, 2014–2018). More importantly, significant health disparities are observed in these two cancer types in terms of disease incidence, aggressiveness, and mortality based on racial background, lifestyle, socioeconomic status (SES), and genetic background (Yedjou et al., 2019). BC incidence has been lower among black women as compared to white women (SEER, 2022a). In contrast, the mortality rate has been observed to be high in black women as compared to white women (SEER, 2022a). In addition to racial background, BC disparity also exists due to SES and insurance status (Newman and Martin, 2007, Bigby and Holmes, 2005). Similarly, CC disparity has been observed among different races in incidence and mortality rates between white and black women. The incidence and mortality rate of CC is found to be high in black women as compared to the white population (SEER, 2022b). Besides, women in rural areas have a higher incidence of CC as compared to women in urban areas (Yu et al., 2019).
In the sections below, we focus on the extent of BC and CC disparities in Alabama and discuss possible underlying causes and the efforts that have been made to reduce the disparity gaps. We anticipate that our analysis will provide guidance in developing effective and collective approaches to address this significant clinical and social problem affecting women’s health in the state of Alabama and nationwide.
BREAST AND CERVICAL CANCER DISPARITIES IN ALABAMA
Alabama is one of the southeastern states in the United States with diverse demographics. As per the most recent American community survey, Alabama state has a diverse racial composition, as given in Table 1 (Worldpopulation, 2022). Among gender distribution, there are 51.5% female and 48.5% male in Alabama. In Alabama only, there is an estimated 30,210 new cancer cases with a mortality of 10,520 in 2022 (Siegel et al., 2022). As per state cancer profiles, BC is the most commonly diagnosed cancer in Alabama after colorectal cancer and the second leading cause of cancer-related death in the state. From 2009–2018 the Alabama Statewide Cancer Registry (ASCR) showed that the incidence of BC was higher for black women than for white women (126.5 vs. 118.1 per 100,000) (Figure 1A). It is interesting since BC incidence is generally higher in white women than in black women. The incidence rate per 100,000 persons is 137.6 cases in white women as compared to 129.6 cases in women of black ethnicity (SEER, 2022a). The mortality rates due to BC were also higher among black women than white women (28.0 vs. 19.9 per 100,000) (Figure 1B). This difference in mortality rate is also greater compared to that observed in a nationwide comparison. As per the Surveillance, Epidemiology, and End Results (SEER) program, the mortality of black women is 28.0 compared to 19.9 in the white population. Besides, black women have a low 5-year survival rate compared to white women (Moormeier, 1996).
Table 1.
Distribution of race in the state of Alabama
| Race | Percentage (%) |
|---|---|
| White | 67.50 |
| Black or African American | 26.59 |
| Two or more races | 2.44 |
| Some other races | 1.53 |
| Asian | 1.39 |
| American Indian and Alaska native | 0.51 |
| Native Hawaiian or Pacific Islander | 0.04 |
Source: World population review.
Figure1. Incidence and mortality of breast and cervical cancer in Alabama.
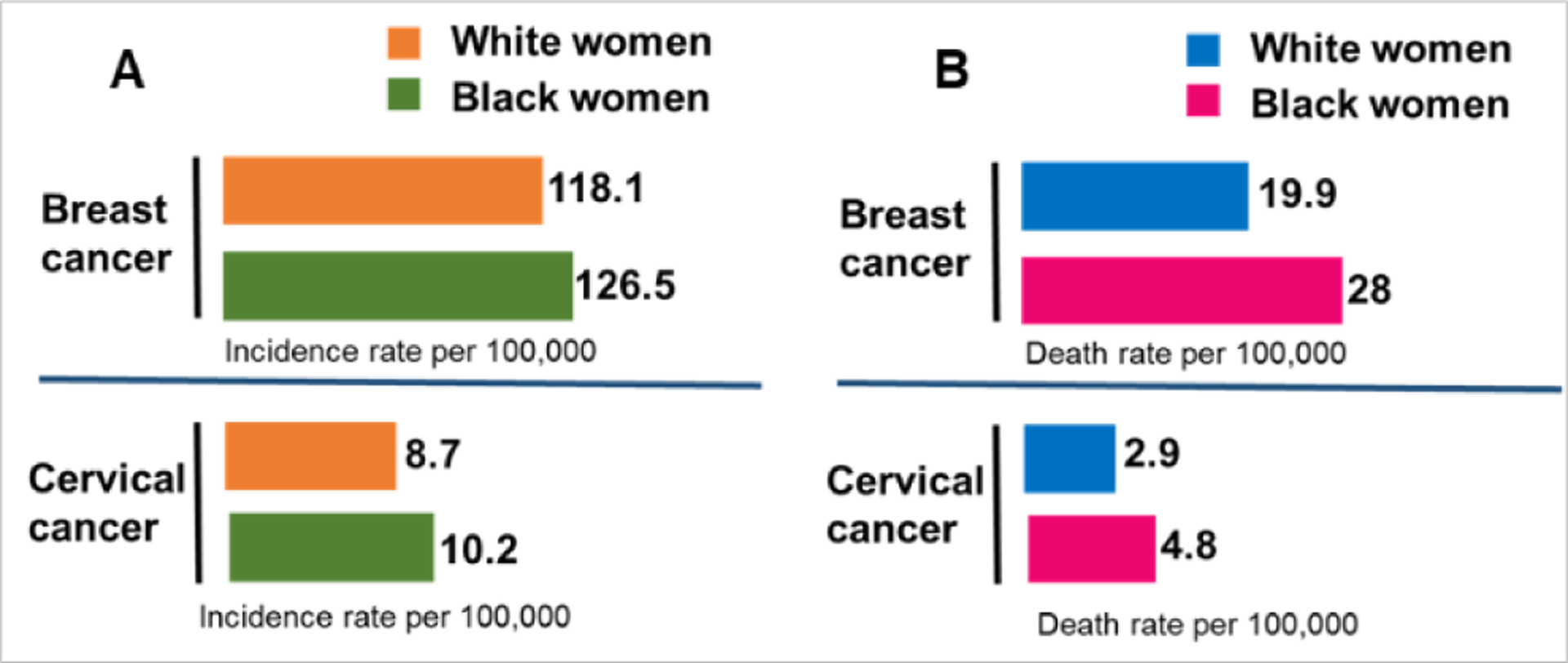
(A) Rate of incidence per 100,000 women with black and white racial background (B) Rate of mortality per 100,000 women with black and white racial background.
CC is the third most common women cancer globally and the second leading cause of cancer-related mortalities in women between 20 to 39 years of age (Abdalla et al., 2021, Siegel et al., 2022). CC disparity has also been observed in incidence and mortality rates between white and black women. Nationwide, the incidence of CC in black women is 9.0 cases per 100,000 women compared to 7.1 cases per 100,000 in women of white ethnicity. In addition, the death rate is different between white (2.0 cases per 100,000) and black women (3.4 cases per 100,000) (SEER, 2022b). Notably, the incidence of CC is significantly higher in Alabama than in the United States average, with a rate of 9.0 versus 7.5, respectively. Besides, the mortality rate of CC has also been significantly higher in Alabama than in the USA, with a rate of 3.3 versus 2.3 (ASCR, 2021). Between black and white women, the incidence rate of CC in black women (10.2) is high as compared to white women (8.7) (Figure 1A). Additionally, black women have an approximately 1.5 times higher mortality rate due to CC than white women in the state of Alabama (Figure 1B) (ASCR, 2021, Abdalla et al., 2021). This disparity is of particular attention since CC is almost entirely preventable and treatable with proper vaccination, screening, and available treatments. Human Papillomavirus (HPV) infection is a significant cause of cervical carcinogenesis, and this malignancy is virtually ubiquitous in sexually active individuals (Braaten and Laufer, 2008, Burd, 2003). Vaccines are available to prevent HPV infection, and with timely screening, CC can be detected early at a more manageable stage (Safaeian et al., 2007, Thomas, 2016). Thus, it becomes essential to understand the underlying reasons behind the unequal distribution of cancer among different races.
Underlying causes of Cervical and Breast cancer disparities in Alabama
When discussing BC and CC, early detection and access to care are critical to decreasing the mortality rate. Among various causes, lack of medical insurance is one of the reasons behind the disparity. About 31.6 million people in the US were uninsured as of 2020 (Cha and Cohen, 2022). To qualify for Medicaid in Alabama, you must be characterized in the low-income or very low-income category, pregnant or responsible for a person under 18, disabled or have a disabled family member, blind, or over 65 years of age (Alabama Medicaid, https://www.benefits.gov/benefit/1618). Although with the help of the Affordable Care Act, there has been an increase in the availability of reasonable insurance options via Medicaid expansion among Black Americans however, Alabama is among the states that have chosen not to expand Medicaid coverage following the ACS, 2010 even though it has some of the lowest eligibility rates in the country (Insurance, 2021) (Health insurance.org). Another important cause for the disparity is accessibility to health care facilities. Even if low-income women in Alabama could get Medicaid coverage, healthcare access becomes the second hurdle in the way. The Black belt describes a series of 17 counties in Alabama that lack access to social and medical services, whose economy depends predominantly on agriculture, and have populations that are at least 50% black and a per capita income of around $13,000. As per 2021 poverty guidelines, the national poverty line for one individual in 2021 is $12,880 and $21,960 for a family of three. Of the 17 counties that fall into the Black belt, only 4 have at least one obstetrician-gynecologist as of 2018, as per the human rights watch report. Proper gynecological care and screening for CC have five-year survival rates of 93% (Flannery, 2018).
Limited screening of black women is also a factor contributing to the health disparities. Mammogram screening has been shown to decrease 10-year mortality by 41% in BC patients (Duffy et al., 2020). The HPV vaccine is the best way to prevent women from developing CC. Still, black women who are statistically less likely to have a primary care provider have reduced access to this preventative measure. According to the KFF analysis of the Centers for Disease Control and Prevention (CDC)’s 2020 Behavioral Risk Factor Surveillance System, in Alabama, 15% of black women were reported to have no personal healthcare provider compared to 12% in the case of women with white racial backgrounds.
The increased incidence of poverty in Alabama’s Black Belt also contributes to the increase in incidence. While a pap smear is routine for many women, an alarming number of lower-income women, a larger percentage of whom are in this region are black, are unable to take time off work to receive this essential standard of care. As per the Center for Health Journalism, 2016, the poverty rate was 32.7% for black individuals compared to 8.1% for white people in the region (Barry-Jester, 2016). While it cannot be doubted that income, insurance status, access, and other heavily economic reasons account for differences in care, even when black women are diagnosed, they are still more likely to die from CC even when compared to white women in their same socioeconomic class (Abdalla et al., 2021).
Another issue that is particular to Alabama is abstinence-only teaching in schools. Education can empower the women with the understanding to go for screening and vaccinations when required to decrease the burden of cancer. In many Alabama counties, a Black belt, in particular, there is no fund in public schools due to state constitution restrictions. Sexual health education has no importance, and it is left unregulated and unmonitored, which further increases the spread of CC (Flannery, 2018). Hence, it becomes imperative to provide education regarding sexually transmitted infections and strategies for their prevention and also provide sufficient funds for their implementation in the curriculum without any biasing (Figure 2).
Figure 2.
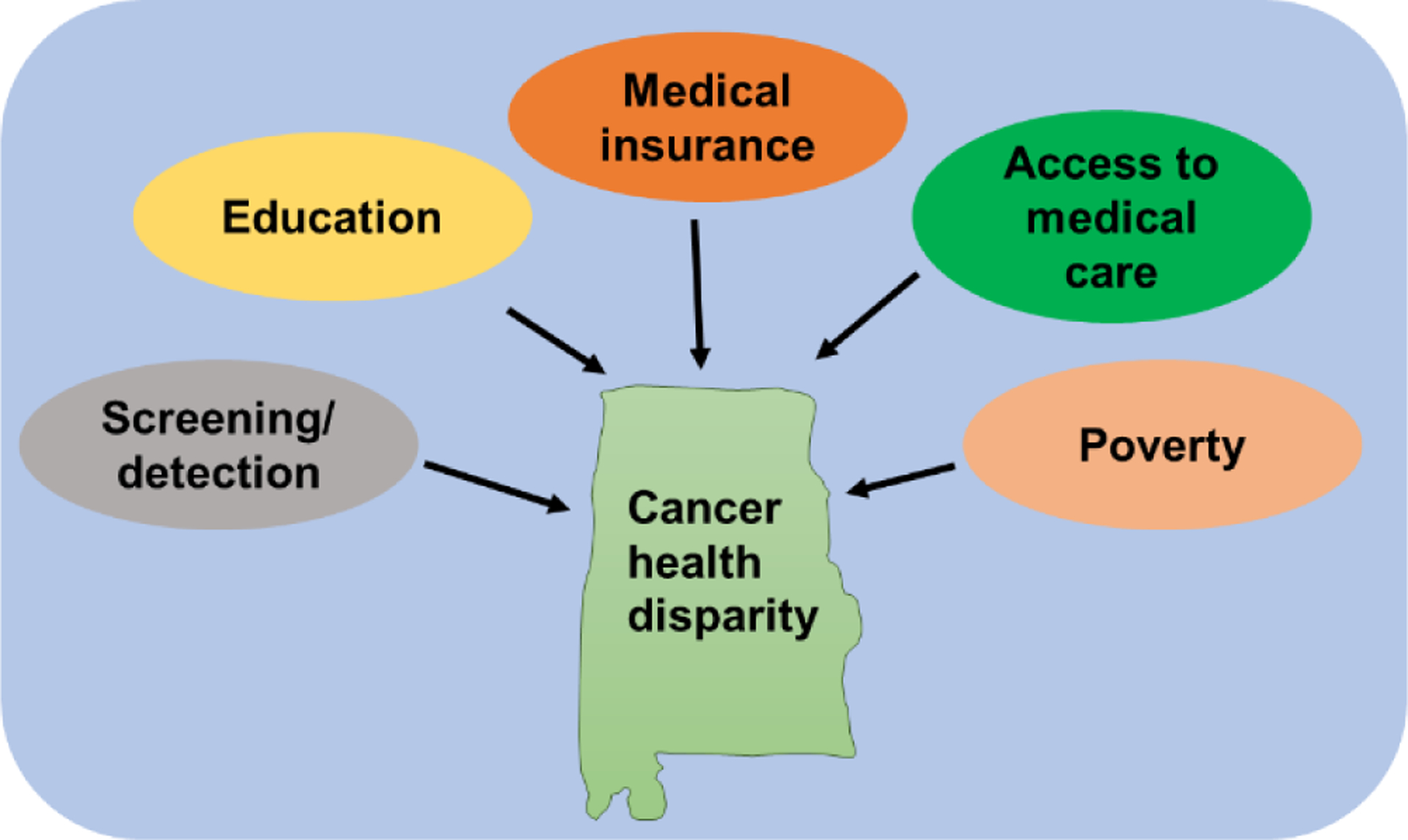
Schematic diagram showing different factors involved in cancer health disparities in Alabama.
CLOSING THE DISPARITY GAPS: WHAT WE ARE DOING AND WHAT MORE WE COULD DO
Ongoing remediation efforts:
Although the incidence and mortality rates for both BC and CC are alarming, they have not gone entirely unnoticed by the state. One measure to offset the cost and thereby increase diagnosis and treatment is the Alabama Breast and CC Early Detection Program (ABCCEDP). The ABCCEDP provides free breast and CC screenings for women ages 40–64 at or below 250% of the federal poverty line, or an annual income of $33,975 for one individual. There are also certain instances where women of this income level can qualify at younger ages, such as a first-degree family history of BC or previous tubal ligation for CC screening (Medicaid). This program helps bridge the gap for those who would not usually qualify for Medicaid, thus allowing women of all races to receive necessary care. However, a program like ABCCEDP is only helpful if women know about it. This is where the Community Health Advisor Program based at the University of Alabama at Birmingham (UAB) has the potential to be more beneficial. As part of the Deep South Network for Cancer Control (DSN), this program trains individuals that are already leaders in their community to become Community Health Advisors (CHAs) and Community Health Advisors as Research Partners (CHARPs). The DSN works to spread information regarding breast and CC screening and treatment. Funded by the National Cancer Institute, this program helps build infrastructure, partners with state organizations and coalitions, and implements interventions in target communities where cancer disparities are disproportionately high (Lisovicz et al., 2008). The thought process behind this model is that information will be more trusted and highly regarded if it comes from community pillars to whom people are already looking for information. The goal is to build a volunteer, grassroots community infrastructure that provides individuals in that community the opportunity to take control of their health and lessen healthcare disparities (UAB, 2022). In the first three years of the programs, from 2001 to 2004, Alabama CHARPs reported a greater than 700% increase in referral screenings in targeted communities. It is evident that the program is working, and people are receptive to the work being done by the DSN and CHARPs. More such programs need to be developed and federally or state-supported to reach and benefit communities across the state. Moreover, the involvement of advocates from different communities, including minority groups, should be sought to enhance engagement and develop ways to maximize the reach and benefits.
Lessons from the parallel public health efforts:
Currently, the patterns of racial disparity, inequality, and exclusion all contribute to minority women being less likely to receive the reproductive health care services and follow-up they need. While efforts are in place to help combat these problems, more work is still required. The Human Rights Watch identified four critical interventions that can be used to prevent, treat, and cure CC and the same could be applied to BC as well. These include i) vaccination ii) screening, iii) timely follow-up after abnormal test results, and iv) early treatment (Flannery, 2018). The HPV vaccine is highly effective at reducing the incidence of CC compared to unvaccinated women (Lei et al., 2020). Currently, the national average for HPV vaccination in adolescents in this age group is 58.6%, and the Alabama average is 52.9% (Vaccination, 2022). Working with systems already in place, such as the DSN and CHARP, and implementing new strategies to help remind patients and make access to vaccines easier will help increase vaccination rates across the state. CC screening is essential to detect cancer at an initial stage with high chances of cancer treatment. Tests for HPV infection need to be done for screening for CC, and we should make every effort to increase the participation of minority women in the screening process. Moreover, we should also develop ways to provide timely follow-up to the minority women, who come up with abnormal screening. Finally, the women who are diagnosed with malignancy should be provided early and optimal treatment to enhance clinical outcomes.
Implementation hurdles and awareness issues:
Despite medical advances and recognition of cancer health disparities, multiple hurdles restrict the efforts targeted at reducing the existing disparities. The problem lies in rural communities where there is a lack of medical facilities. Additionally, the cost of a visit is also high for those without insurance and for those living at or below the poverty line. For these people, choosing to take care of health problems that may not currently be causing issues may be trumped by basic needs such as food, shelter, and clothing.
Besides, it is essential to inform the public regarding their sexual and reproductive health. The CDC identified that fewer than 43% of high schools and 18% of middle schools teach the key topics for sexual health education in their curriculum (CDC, 2020). This population of adolescents and young adults make up a quarter of the world’s population and is the largest cohort of young people in history (Nguyen et al., 2019). Alabama’s current laws do not mandate that sex education be taught in schools. If it is introduced, the state approaches the conversation from a largely pure culture mindset, emphasizing abstinence-only teaching. While the state mandates that students receive HIV/AIDS education through a school program between the grades of 5–12, and efforts are currently being made to remove anti-homosexuality language in the laws, there is still no requirement for schools to cover these topics in their curriculum.
CDC data suggests that nearly one-third of high school students in the state of Alabama are sexually active, and these students are the most at risk for engaging in risky sexual behaviors that can lead to HIV infections, sexually transmitted diseases, and unintended pregnancies, which all have long-term effects on their health (Profiles, 2016). By changing the beliefs, attitudes, and behaviors of this population regarding sexual and reproductive health, a shift can be made to change the culture around these topics. Recent guidance from the American College of Obstetrics and Gynecologists suggests that taking a more holistic approach to sexual education may be a first step in overcoming social, economic, and political factors that have negative sexual, psychological, and social influences on reproductive health. While the state is making an effort to be more inclusive and encourage conversations regarding sexual health, future revisions should take a more biological approach and focus on setting clear health goals, reproductive development, consent, communication, recognizing and preventing sexual violence, human rights about LGBTQ+ community and others (Profiles, 2016). Schools can use resources such as the CDC’s Health Education Curriculum Analysis Tool to engage in more comprehensive conversations with their students and provide valuable information regarding sexual and reproductive health. By shifting away from the purist mindset and focusing on a research-based curriculum that addresses social pressures and influences and increases personal perceptions of the risks and harms of engaging in certain behaviors, the culture, and mindset around sexual and reproductive health will shift.
Moving forward:
With this in mind, there are three critical areas that the state can focus on to increase access to care and decrease the burden among populations at the highest risk. By expanding the Medicaid eligibility to cover adults earning 138% of the federal poverty line, Medicaid enrollment would increase by 283,636 patients. While this would cost the state an average of $225.4 million per year above current expenditures, the state could see savings of up to $397.8 million (PARCALABAMA, 2022). This increase in federal revenue would not only help alleviate the financial burden placed on low-income families but also reduces racial and ethnic disparities gaps, strengthens rural health care provider institutions, and would help the state economy.
Expanding Medicaid eligibility would also create an estimated average of 20,083 new jobs annually for the following six years (PARCALABAMA, 2022). This would seem to be a promising work opportunity for the growing number of medical students graduating each year. However, with the average medical student graduating with $194,280 in debt from a public institution, working in a rural community can be daunting, knowing the pay could be significantly reduced (Calonia, 2022). That is why programs such as the University of Alabama’s College of Community Health Sciences Rural Medical Scholars and Rural Community Health Scholars programs and the Blue Cross Blue Shield of Alabama Primary Care Physician Network scholarship are being created to help offset the costs of medical education and encourage students to seek our rural positions (BCBS, 2018, Zganjar, 2021). These programs target medical students from the four medical schools within the state who desire to work in underserved communities, such as the Black belt, and provide better scholarship funding and specialized training to prepare these students for their work in these fields. By funding programs and rural medicine loan forgiveness programs, graduating medical students are incentivized to care for these populations in need without the fear of being unable to pay back the money used for their initial education.
Moreover, increasing the available obstetrician-gynecologists in rural areas will help. Transportation to these offices can still be a major issue for women seeking care. Alabama is one of only three states that does not provide state funding for public transportation. Many seniors, people with disabilities, and low-income families suffer from the lack of this facility. In 2018, the Alabama state legislature created the Public Transportation Trust Fund to combat the lack of available transportation. However, no state funds had been allocated to the fund until February 2022. This initial transit funding is designed to help update current bus fleets and facilities and build new rail cars, tracks, and stations throughout the state. While this is a great first step, we must continue advocating for funding to be allocated to the state to improve transportation throughout the state.
Conclusion
Drastic differences in care between black and white women because of socioeconomic and geographic factors largely contribute to the racial cancer health disparities throughout the state of Alabama. Moreover, lack of information available to the public has made the mindset of many fall into the category of “If I don’t have to go, I won’t go”. In addition, the cost of missing work, traveling throughout the state, or expenses of the care itself far outweigh the perceived benefits. While efforts are being made throughout the state to increase access to care, alleviate financial burdens, and raise awareness regarding sexual and reproductive health, more work is still needed. There is also a need to understand the causes of health disparities beyond socioeconomic and geographical aspects. It is being increasingly recognized that there are significant differences in the tumor biology of minority patients. We all know that African American women are more likely to be diagnosed with an aggressive triple-negative breast tumor subtype, compared to Caucasian American women, which likely also contributes to their greater mortality as per ACS, 2022. There are other biological differences that have been reported between AA and CA women (Deshmukh et al., 2017, Deshmukh et al., 2015, Olusola et al., 2019). Clearly, we need to precisely characterize these differences in tumor biology and genetics and study their impact on patient outcomes. Clinical trials testing new drugs should also enroll minority patients to determine if the drug efficacy is similar or different among diverse racial populations. Altogether, by developing more awareness, developing ways to provide equal healthcare to all, and providing the right treatment based on the genetic makeup of the tumors, the state and the country at large, can succeed in reducing the prevalent health disparities in cancer.
Acknowledgment
This work was supported, in part, by funding from the NIH/NCI [R01CA231925 (SS), Medical Student Summer Research program of the Whiddon College of Medicine, (KCB, CPS), and Mitchell Cancer Institute, University of South Alabama.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Abdalla E, Habtemariam T, Fall S, Troy R, Tameru B & Nganwa D 2021. A Comparative Study of Health Disparities in Cervical Cancer Mortality Rates Through Time Between Black and Caucasian Women in Alabama and the US. Int J Stud Nurs, 6, 9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASCR, 2021. Alabama Cancer Statistics [Online]. Available: https://www.alabamapublichealth.gov/ASCR/assets/acs2021.pdf [Accessed 2022].
- Barry-Jester AM 2016. In Alabama’s Black Belt, a lasting legacy of racial disparities and deep poverty [Online]. Available: https://centerforhealthjournalism.org/2016/07/14/alabama%E2%80%99s-black-belt-lasting-legacy-racial-disparities-and-deep-poverty [Accessed 2022].
- BCBS. 2018. Blue Cross And Blue Shield Of Alabama Expands Initiative To Further Improve Access To Primary Care Physicians And Advance Quality Of Care For Alabamians [Online]. Available: https://www.bcbs.com/press-releases/blue-cross-and-blue-shield-of-alabama-expands-initiative-further-improve-access [Accessed 2022].
- Bigby J & Holmes MD 2005. Disparities across the breast cancer continuum. Cancer Causes Control, 16, 35–44. [DOI] [PubMed] [Google Scholar]
- Braaten KP & Laufer MR 2008. Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine. Rev Obstet Gynecol, 1, 2–10. [PMC free article] [PubMed] [Google Scholar]
- Burd EM 2003. Human papillomavirus and cervical cancer. Clin Microbiol Rev, 16, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calonia J 2022. What’s The Average Medical School Debt In 2022? [Online]. Available: https://www.forbes.com/advisor/student-loans/average-medical-school-debt/ [Accessed 2022].
- CDC. 2020. Adolescent Health: What Works in Schools [Online]. Available: https://www.cdc.gov/healthyyouth/whatworks/pdf/what-works-sexual-health-education.pdf [Accessed 2022].
- Cha AE & Cohen RA 2022. Demographic Variation in Health Insurance Coverage:United States, 2020. Natl Health Stat Report, 1–15. [PubMed] [Google Scholar]
- Deshmukh SK, Srivastava SK, Bhardwaj A, Singh AP, Tyagi N, Marimuthu S, Dyess DL, Dal Zotto V, Carter JE & Singh S 2015. Resistin and interleukin-6 exhibit racially-disparate expression in breast cancer patients, display molecular association and promote growth and aggressiveness of tumor cells through STAT3 activation. Oncotarget, 6, 11231–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshmukh SK, Srivastava SK, Tyagi N, Ahmad A, Singh AP, Ghadhban AAL, Dyess DL, Carter JE, Dugger K & Singh S 2017. Emerging evidence for the role of differential tumor microenvironment in breast cancer racial disparity: a closer look at the surroundings. Carcinogenesis, 38, 757–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy SW, Tabar L, Yen AM, Dean PB, Smith RA, Jonsson H, Tornberg S, Chen SL, Chiu SY, Fann JC, Ku MM, Wu WY, Hsu CY, Chen YC, Svane G, Azavedo E, Grundstrom H, Sunden P, Leifland K, Frodis E, Ramos J, Epstein B, Akerlund A, Sundbom A, Bordas P, Wallin H, Starck L, Bjorkgren A, Carlson S, Fredriksson I, Ahlgren J, Ohman D, Holmberg L & Chen TH 2020. Mammography screening reduces rates of advanced and fatal breast cancers: Results in 549,091 women. Cancer, 126, 2971–2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery K 2018. It Should Not Happen, Alabama’s Failure to Prevent Cervical Cancer Death in the Black Belt [Online]. Available: https://www.hrw.org/report/2018/11/29/it-should-not-happen/alabamas-failure-prevent-cervical-cancer-death-black-belt#_ftn2 [Accessed 2022].
- Insurance, H. 2021. Alabama and the ACA’s Medicaid expansion [Online]. Available: https://www.healthinsurance.org/medicaid/alabama [Accessed 2022].
- Lei J, Ploner A, Elfstrom KM, Wang J, Roth A, Fang F, Sundstrom K, Dillner J & Sparen P 2020. HPV Vaccination and the Risk of Invasive Cervical Cancer. N Engl J Med, 383, 1340–1348. [DOI] [PubMed] [Google Scholar]
- Lisovicz N, Wynn T, Fouad M & Partridge EE 2008. Cancer health disparities: what we have done. Am J Med Sci, 335, 254–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid, A. Breast and Cervical Cancer Program [Online]. Available: https://medicaid.alabama.gov/content/3.0_Apply/3.2_Qualifying/3.2.7_Breast_Cervical_Cancer.aspx [Accessed 2022].
- Moormeier J 1996. Breast cancer in black women. Ann Intern Med, 124, 897–905. [DOI] [PubMed] [Google Scholar]
- Nagai H & Kim YH 2017. Cancer prevention from the perspective of global cancer burden patterns. J Thorac Dis, 9, 448–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman LA & Martin IK 2007. Disparities in breast cancer. Curr Probl Cancer, 31, 134–56. [DOI] [PubMed] [Google Scholar]
- Nguyen G, Costenbader E, Plourde KF, Kerner B & Igras S 2019. Scaling-up Normative Change Interventions for Adolescent and Youth Reproductive Health: An Examination of the Evidence. J Adolesc Health, 64, S16–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olusola P, Banerjee HN, Philley JV & Dasgupta S 2019. Human Papilloma Virus-Associated Cervical Cancer and Health Disparities. Cells, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parcalabama. 2022. The Economic Impact of Expanding Medicaid in Alabama [Online]. Available: https://parcalabama.org/wp-content/uploads/2022/01/Economic-Analysis-of-Alabama-Medicaid-Expansion.pdf [Accessed 2022].
- Profiles. 2016. Analysis of State Health Education Laws [Online]. Available: https://www.cdc.gov/healthyyouth/policy/pdf/summary_report_factsheets/Alabama.pdf [Accessed].
- Profiles, S. C. 2014–2018. Dynamic views of cancer statistics for prioritizing cancer control efforts across the nation [Online]. Available: https://statecancerprofiles.cancer.gov/ [Accessed 2022].
- Safaeian M, Solomon D & Castle PE 2007. Cervical cancer prevention--cervical screening: science in evolution. Obstet Gynecol Clin North Am, 34, 739–60, ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEER. 2022a. Cancer Stat Facts: Female Breast Cancer [Online]. Available: https://seer.cancer.gov/statfacts/html/breast.html [Accessed 2022].
- SEER. 2022b. Cancer Stat Facts: Female Cervical Cancer [Online]. Available: https://seer.cancer.gov/statfacts/html/cervix.html [Accessed 2022].
- Siegel RL, Miller KD, Fuchs HE & Jemal A 2021. Cancer Statistics, 2021. CA Cancer J Clin, 71, 7–33. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Fuchs HE & Jemal A 2022. Cancer statistics, 2022. CA Cancer J Clin, 72, 7–33. [DOI] [PubMed] [Google Scholar]
- Thomas TL 2016. Cancer Prevention: HPV Vaccination. Semin Oncol Nurs, 32, 273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UAB. 2022. Community Health Advisor Program [Online]. Available: https://www.uab.edu/onealcancercenter/outreach/community-health-advisor-program [Accessed 2022].
- Vaccination, H. 2022. America’s Health Rankings analysis of CDC, National Immunization Survey-Teen, United Health Foundation [Online]. Available: https://www.americashealthrankings.org/explore/annual/measure/Immunize_HPV/state/AL [Accessed 2022].
- World population. 2022. Alabama Population [Online]. Available: https://worldpopulationreview.com/states/alabama-population [Accessed 2022].
- Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, Alo RA, Payton M & Tchounwou PB 2019. Health and Racial Disparity in Breast Cancer. Adv Exp Med Biol, 1152, 31–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Sabatino SA & White MC 2019. Rural-Urban and Racial/Ethnic Disparities in Invasive Cervical Cancer Incidence in the United States, 2010–2014. Prev Chronic Dis, 16, E70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zganjar L 2021. UA Programs Welcome Students Studying Rural Health Care [Online]. Available: https://news.ua.edu/2021/10/ua-programs-welcome-students-studying-rural-health-care [Accessed 2022].


