Abstract
Background
To explore the correlation of tumor necrosis factor-α-induced protein 8-like protein 3 (TIPE3) expressions in colorectal cancer (CRC) with tumor-immune infiltration and patient prognosis.
Methods
Formalin-fixed paraffin-embedded tumor samples from CRC patients (n = 110) were used in this study. Immunohistochemistry staining of TIPE3 and three prognostic immune biomarkers (CD8, CD20, and CD66b) was conducted in the tumor tissues and adjacent normal tissues. A Cox regression analysis of univariate and multivariate variables was performed to assess the correlation between TIPE3 and patient prognosis.
Result
We found that TIPE3 was mainly expressed in the cytoplasm, with a small amount in the nucleus. The expression of TIPE3 in tumor tissues is significantly higher than in adjacent normal tissues, and it is significantly correlated with the survival rate of patients in tumor tissues (p = 0.0038) and adjacent normal tissues (p<0.0001). Patients with a high TIPE3 expression had a lower survival rate, while patients with a low TIPE3 expression had a higher survival rate. Univariate regression analysis showed that the TIPE3 expression in tumor tissues (p = 0.007), the TIPE3 expression in adjacent normal tissues (p<0.001), the number of CD8+ T cells in tumor tissues (p = 0.020), the number of CD20+ B cells in tumor tissues (p = 0.023), the number of CD20+ B cells in adjacent normal tissues (p = 0.023), the number of CD66b+ neutrophils in tumor tissues (p = 0.005), the number of CD66b+ neutrophils in adjacent normal tissues (p<0.001), lymphatic metastasis (p = 0.010), TNM stage (p = 0.013), and tumor grade (p = 0.027) were significantly correlated with overall survival (OS). These prognostic factors were then subjected to multivariate regression analysis, and the results showed that the expression of TIPE3, the number of CD8+ T cells, and the number of CD66b+ neutrophils were prognostic factors affecting the OS rate of CRC patients.
Conclusion
We found that the TIPE3 protein is upregulated in CRC cancer tissues and is correlated with survival rate.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-023-10590-2.
Keywords: TIPE3, Colorectal cancer, Immune infiltration, Prognosis
Introduction
Colorectal cancer (CRC) is the most common malignant tumor of the digestive system and is associated with a high mortality rate [1, 2]. The occurrence and development of CRC are closely related to patients’ age, gender, lifestyle, dietary habits, and genetic factors [3].
The tumor necrosis factor-α-induced protein 8 family (TNFAIP8/TIPE) is induced by tumor necrosis factor-α (TNF-α), which is closely related to immune regulation and tumorigenesis [4]. It has been reported that this family contains four members, namely, TNFAIP8/TIPE, TIPE1, TIPE2, and TIPE3 [5]. TIPE is a negative regulator of apoptosis, which can lead to the occurrence of cancer. TIPE1 is an enhancer of cell apoptosis, which can induce cell apoptosis and which has an anti-tumor effect. As a negative regulator of inflammation and immunity, TIPE2 can prevent the occurrence of some tumors [6]. Among these, TIPE3, identified in 2008, is the least studied member of the TIPE family [7]. TIPE3 is highly expressed in most human tumor cell lines, such as lung cancer cell line NCI-H727, bladder cancer cell line T24, and colon adenocarcinoma cell line HT-29, but with a low expression in the gastric cancer cell line. At the same time, it is significantly up-regulated in lung cancer, esophagus cancer, cervical cancer, and colon cancer [8]; it was found that TIPE3 overexpression significantly increased the migration, invasion, and proliferation of MCF-7 and MDA-MB-231 tumor cells in human breast cancer cell lines. On the contrary, knockdown of TIPE3 in MDA-MB-231 cells can significantly reduce the migration, invasion, and proliferation of tumor cells [9]. In human non-small-cell lung cancer (NSCLC), some researchers have found that the expression of TIPE3 on the plasma membrane is positively correlated with the T stage of NSCLC, indicating that TIPE3 located in the plasma membrane may play a role in promoting tumor development, whereas cytoplasmic TIPE3 may exert a negative effect [10]. Meanwhile, in human glioblastoma (GBM), overexpressed TIPE3 inhibits p38 phosphorylation and blocks p38 nuclear translocation, leading to the negative regulation of the p38 MAPK pathway and resulting in GBM cell survival [11]. These results suggest that the role of TIPE3 in different tumors is heterogeneous.
In this work, we mainly used clinical/surgical specimens, focusing on the correlation between the TIPE3 expression and tumor-immune infiltration and the prognosis of CRC patients. The expression level of TIPE3 in the cancer and adjacent tissues of 110 CRC patients was detected by immunohistochemistry (IHC). According to the score statistics of the IHC results, combined with the patients’ prognosis information, the survival curve of the TIPE3 expression in CRC tissues and the prognosis of patients were determined, and the correlation between the TIPE3 expression and prognosis was analyzed. At the same time, we investigated the relationship between the TIPE3 expression level and tumor immune invasion: IHC was used to detect the positive cell numbers of CD8+ T cells, CD20+ B cells, and CD66b+ neutrophils in the cancer and adjacent tissues of 110 CRC patients. Combined with the prognosis information of the patients, a corresponding survival curve was drawn, and we found that patients with a high TIPE3 expression had a lower survival rate, while patients with a low TIPE3 expression had a higher survival rate.
Materials and methods
Patients and specimens
Formalin-fixed paraffin-embedded (FFPE) samples from CRC patients (n = 227) were used in this study. All samples, including CRC tissue specimens and the corresponding adjacent normal mucosal tissue specimens (colorectal mucosal tissue more than 5 cm from the edge of the tumor tissue), were obtained from patients with primary histologically confirmed CRC between June 2015 to June 2016 at the First Affiliated Hospital of Anhui Medical University, Hefei, China. The inclusion criteria were: 1) patients who underwent radical colorectal cancer surgery; 2) patients with available follow-up data and clinicopathological characteristics; 3) patients with no history of cancer treatment, without other malignant tumors; and 4) patients without serious perioperative complications or death. Informed consent was obtained from all participants before the study, which was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University (NO: LLSC2021010).
Follow-up
All patients were followed up on a long-term basis until June 31, 2021, by phone call, outpatient follow-up, and inpatient hospital review. The follow-up period ranged from 1 to 67 months. The details are listed in Table 1.
Table 1.
The Correlation Between TIPE3 Expression and Clinicopathological Features in CRC Patients
| Characteristics | TIPE3 expression in Tumor tissues | p-value | TIPE3 expression in Adjacent normal tissues | p-value | ||
|---|---|---|---|---|---|---|
| Low(n=34) | High(n=76) | Low(n=72) | High(n=38) | |||
| Gender | ||||||
| Male | 24 (70.6) | 46 (60.5) | 0.424 | 49 (68.1) | 21 (55.3) | 0.264 |
| Fmale | 10 (29.4) | 30 (39.5) | 23 (31.9) | 17 (44.7) | ||
| Lymph node metastasis | ||||||
| Negative | 17 (50.0) | 42 (55.3) | 0.761 | 40 (55.6) | 19 (50.0) | 0.723 |
| Postive | 17 (50.0) | 34 (44.7) | 32 (44.4) | 19 (50.0) | ||
| Invasion | ||||||
| I | 1 ( 2.9) | 0 ( 0.0) | 0.489 | 1 ( 1.4) | 0 ( 0.0) | 0.491 |
| II | 4 (11.8) | 11 (14.5) | 12 (16.7) | 3 ( 7.9) | ||
| III | 23 (67.6) | 50 (65.8) | 45 (62.5) | 28 (73.7) | ||
| IV | 6 (17.6) | 15 (19.7) | 14 (19.4) | 7 (18.4) | ||
| TNM | ||||||
| T1 | 5 (14.7) | 11 (14.5) | 0.851 | 13 (18.1) | 3 ( 7.9) | 0.356 |
| T2 | 12 (35.3) | 31 (40.8) | 27 (37.5) | 16 (42.1) | ||
| T3 | 17 (50.0) | 34 (44.7) | 32 (44.4) | 19 (50.0) | ||
| Grade | ||||||
| Low | 4 (11.8) | 17 (22.4) | 0.395 | 13 (18.1) | 8 (21.1) | 0.727 |
| Moderate | 29 (85.3) | 56 (73.7) | 57 (79.2) | 28 (73.7) | ||
| High | 29 (85.3) | 56 (73.7) | 2 ( 2.8) | 2 ( 5.3) | ||
| Location (%) | ||||||
| Location (%) | 29 (85.3) | 56 (73.7) | 0.554 | 28 (38.9) | 17 (44.7) | 0.697 |
| Colon | 22 (64.7) | 43 (56.6) | 44 (61.1) | 21 (55.3) | ||
| Status (%) | ||||||
| Survive | 29 (85.3) | 42 (55.3) | 0.005** | 56 (77.8) | 15 (39.5) | <0.001 |
| Dead | 5 (14.7) | 34 (44.7) | 16 (22.2) | 23 (60.5) | ||
| CEA | 5.61 [2.96, 20.33] | 3.70 [2.31, 7.77] | 0.078 | 3.80 [2.36, 7.93] | 4.96 [2.53, 14.77] | 0.343 |
| CA-199 | 13.71 [9.12, 32.54] | 10.64 [6.11, 26.79] | 0.196 | 11.34 [6.91, 21.13] | 13.61 [6.26, 37.21] | 0.418 |
| Age | 65.50 [57.25, 77.75] | 62.00 [53.75, 68.00] | 0.179 | 63.00 [56.50, 72.00] | 62.00 [53.25, 70.00] | 0.792 |
| Survive Time | 64.00 [63.00, 64.75] | 63.00 [35.50, 64.00] | 0.006** | 64.00 [63.00, 64.00] | 56.00 [22.25, 63.00] | <0.001 |
| WBC | 6.32 [4.88, 6.88] | 5.72 [4.64, 7.35] | 0.874 | 5.74 [4.56, 7.04] | 6.29 [4.91, 7.26] | 0.622 |
| Neutrophil | 3.60 [2.95, 4.69] | 3.23 [2.75, 4.76] | 0.514 | 3.48 [2.80, 4.77] | 3.29 [2.80, 4.73] | 0.664 |
| Lymphocyte | 1.46 [1.23, 1.87] | 1.48 [1.12, 1.95] | 0.828 | 1.40 [1.08, 1.77] | 1.66 [1.29, 2.17] | 0.011* |
| Monocyte | 0.37 [0.30, 0.45] | 0.36 [0.28, 0.48] | 0.864 | 0.36 [0.28, 0.45] | 0.38 [0.28, 0.55] | 0.196 |
| Hb | 131.00 [113.25, 137.00] | 125.50 [97.75, 132.25] | 0.113 | 127.50 [107.25, 134.00] | 122.50 [101.75, 131.50] | 0.336 |
| PLT | 214.50 [171.50, 280.00] | 217.00 [171.00, 265.25] | 0.910 | 1218.00 [169.50, 266.25] | 196.00 [173.00, 270.50] | 0.797 |
CEA Carcinoembryonic antigen, CA-199 Carbohydrate antigen 199, WBC White blood cell, Hb Hemoglobin, PLT Platelet
*p < 0.05, **p < 0.01
Endpoint of study
The endpoint of this study was the overall survival (OS). OS was defined as the time from radical CRC surgery to death or the last follow-up for surviving patients.
Immunohistochemistry
Based on the findings of previous studies [12, 13], we selected three prognostic immune biomarkers for IHC staining: cytotoxic T cells (CD8), B cells (CD20), and neutrophils (CD66b) [14]. All FFPE samples were cut into 4-μm sections (Leica, Germany) and then processed for the IHC assay, as previously described [15]. Following incubation with an antibody against human TIPE3 (Boster, A14951, Wuhan, China), CD8 (Affinity, AF5126, Changzhou, China), CD20 (Affinity, DF13319, Changzhou, China), and CD66b (Affinity, DF10151, Changzhou, China), the sections were stained using the Envision System (PV6001, ZSGB-BIO, China). The IHC results were evaluated by two independent observers blinded to the clinical outcome. First, the general condition of the tissue section was assessed under an optical microscope (Olympus Upright Microscope BX53, Olympus, Japan) at a low power field (100x). Then, five representative high-power fields (200x) of each tissue section were photographed and scored. Then, the average of five fields was taken as the positive cell score.
Immunohistochemical score
We used different scoring systems for different proteins; for the TIPE3 expression, a combined immunohistochemical score was calculated using the percentage of positively stained cells and signal intensity; the percentage of TIPE3-positive cells was graded as follows: 0, <1%; 1, 1–20%; 2, 21–40%; 3, 41–60%; 4, 61%–80%; 5, ≥81%, and the signal intensity, as follows: 0, no staining; 1, weak staining; 2, moderate staining; 3, strong staining. Then, the individual scores were added to obtain the combined score. For immune cells, the number of positive cells was the score for this field.
Clinicopathological parameters
The basic information of each patient was recorded in this study (Table 1), including gender; age; tumor location; tumor grade; preoperative carcinoembryonic antigen (CEA) level; preoperative carbohydrate antigen 199 (CA199) level; tumor invasion depth; lymph node metastasis status; survival time; and TNM Classification of Malignant Tumors (TNM) stage. Patients with TNM staging were restaged according to the 7th edition of the American Joint Committee on Cancer (AJCC) tumor staging manual. CEA and CA199 levels above 5 ng/mL and 27 µg/mL, respectively, were considered abnormal. The relevant experiments were approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University (NO: LLSC2021010).
Statistical analysis
Data were analyzed using the SPSS software (version 22.0; IBM Corporation) with default parameters and the R software (version 4.1.0). Continuous variables were expressed as the median (interquartile range [IQR]) or mean (standard deviation [SD]), as appropriate. Frequencies and percentages were used to express categorical variables.
Pearson’s χ2 or Fisher’s exact test was conducted to analyze categorical variables, and the Student’s t-test or rank-sum test was used to examine continuous variables. Univariate and multivariate analyses were performed using the Cox proportional risk regression analysis to screen potential prognostic factors for OS. We determined the optimal cutoff values of the TIPE3, CD8, CD20, and CD66b expressions using survminer from the R package (version 0.4.9). Subsequently, a Kaplan–Meier plot and log-rank test were applied in terms of the high- and low-expression TIPE3, CD8, CD20, and CD66b groups (expressed as total survival time [OS]). A p-value of <0.05 was considered statistically significant.
Results
Clinical characteristics
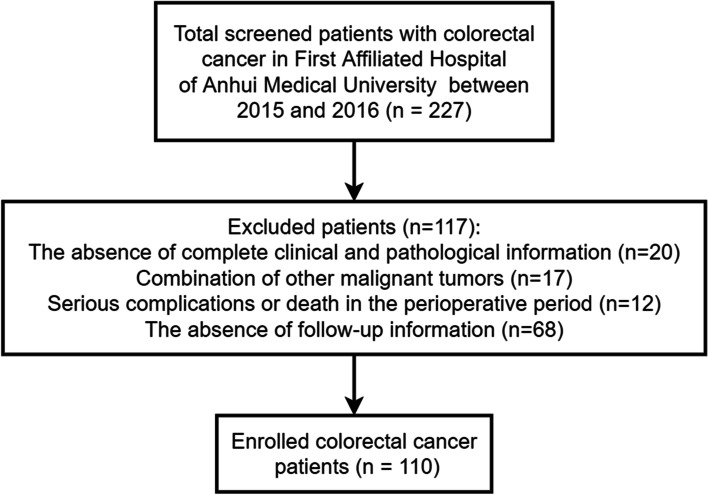
The pathological information of the enrolled CRC patients is presented in Table 1. FFPE samples from CRC patients (n = 227) were collected in this study. Of these, 117 cases were excluded and 110 were eventually enrolled. The patient exclusion criteria were: 1) the absence of complete clinical and pathological information (n = 20), 2) a combination of other malignant tumors (n = 17), 3) serious complications or death in the perioperative period (n = 12), and 4) the absence of follow-up information (n = 68). In total, 110 patients were finally enrolled, with a median age of 62.0 years old (interquartile range: 54.0–71.0 years old), including 70 males and 40 females. The flow chart of the study population is shown in Fig. 1.
Fig. 1.
Flow chart of the study population
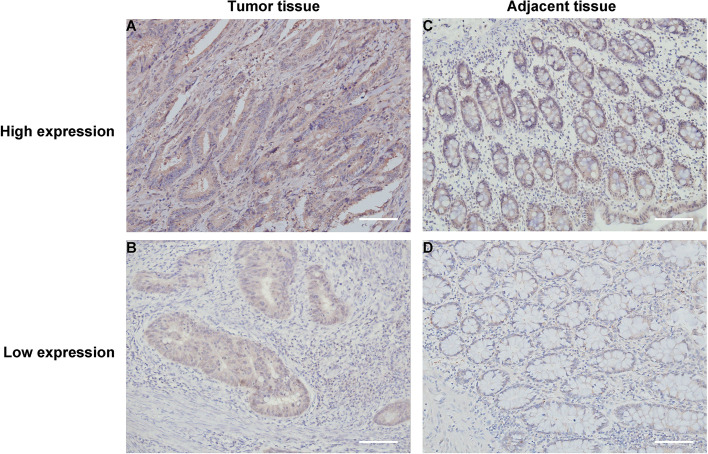
TIPE3 expression in CRC tissues
First, we performed IHC staining of TIPE3 in the tumor tissues and adjacent normal tissues of 110 CRC specimens and found varying levels of the TIPE3 expression in both tissue types, with a high expression in the cytoplasm and low levels in the nucleus (Fig. 2). After IHC scoring, the median score was taken as the cutoff value, and the cancer tissues were divided into a low TIPE3 expression group (≤4.9; n = 34) and a high TIPE3 expression group (>4.9; n = 76). Similarly, the adjacent normal tissues were divided into a low TIPE3 expression group (≤3.4; n = 72) and a high TIPE3 expression group (>3.4; n = 38). A statistical analysis showed that 69.10% (76/110) and 30.90% (34/110) of cases exhibited high and low TIPE3 expression levels in cancer tissues, respectively, while 34.55% (38/110) and 65.45% (72/110) of cases exhibited high and low TIPE3 expressions in adjacent normal tissues, respectively. Overall, the expression of TIPE3 in cancer tissues was significantly higher than in adjacent normal tissues.
Fig. 2.
Images of immunohistochemical staining of TIPE3 in CRC Tumor tissue and Adjacent tissue (200×): A, B Tumor tissue: A TIPE3 high expression; B TIPE3 low expression; C, D Adjacent tissue: C TIPE3 high expression; D TIPE3 low expression. CRC, colorectal cancer; Scale bar = 100 μm
Correlation between TIPE3 expression and clinicopathological features in CRC patients
During the correlation analysis between the TIPE3 expression and clinicopathological factors (Table 1), the TIPE3 expression in tumor tissues was significantly correlated with survival status (p = 0.005) and survival time (p = 0.006). Similarly, the TIPE3 expression in the adjacent normal tissues correlated with survival status (p<0.001) and survival time (p<0.001). Interestingly, there was also a significant correlation between the TIPE3 expression and the blood lymphocyte count (p = 0.011). However, no differences in the TIPE3 expression were found after stratifying by gender, age, TNM stage, depth of tumor invasion, and tumor grade.
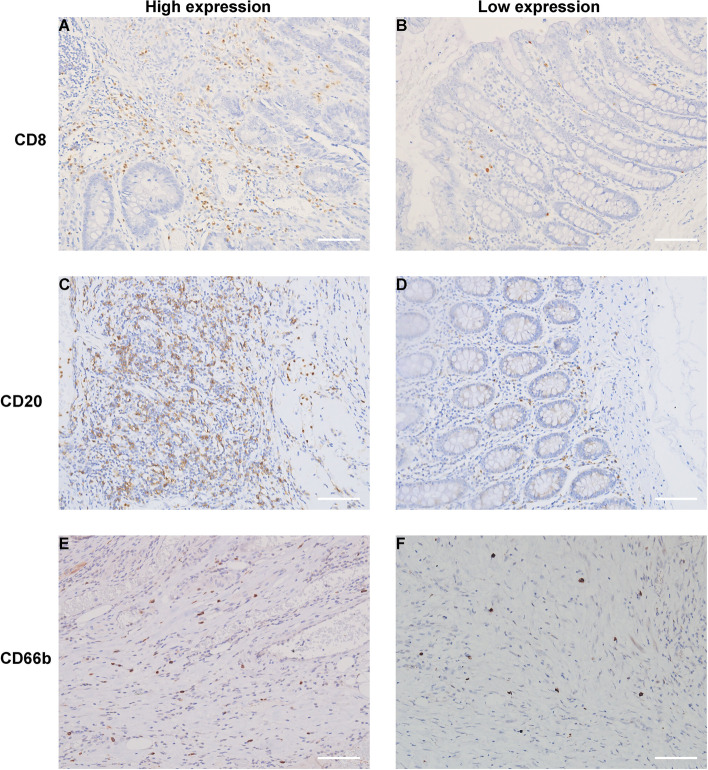
Correlation between TIPE3 expression and tumor-immune infiltration
We performed IHC staining of CD8+ T cells, CD20+ B cells, and CD66b+ neutrophils in the tumor tissues and adjacent normal tissues of the 110 CRC specimens and observed the staining results (Fig. 3). The TIPE3 expression and the number of immune cells were scored (Table 2), and the results showed that TIPE3 was significantly correlated with the number of CD20+ B cells in tumor tissues (p = 0.004), while no significant results were observed for the other markers. Taken together, our results suggest the TIPE3 expression may be associated with tumor-immune infiltration.
Fig. 3.
Images of immunohistochemical staining immune cells in CRC tissue (200×): A, B Immunohistochemical staining of CD8+ T cells: A High expression; B Low expression; C, D Immunohistochemical staining of CD20+ B cells: C High expression; D Low expression; E, F Immunohistochemical staining of CD66b+ neutrophils: E High expression; F Low expression. Scale bar = 100 μm
Table 2.
Correlation Between TIPE3 Expression and tumor immune infiltration
| Characteristics | TIPE3 expression in Tumor tissues | p-value | TIPE3 expression in adjacent normal tissues | p-value | ||
|---|---|---|---|---|---|---|
| Low(n=34) | High(n=76) | Low(n=72) | High(n=38) | |||
| CD8_T | 150.00 [80.00, 285.00] | 100.00 [60.00, 200.00] | 0.296 | 150.00 [70.00, 265.00] | 100.00 [50.00, 147.50] | 0.060 |
| CD8_A | 80.00 [40.00, 172.50] | 80.00 [40.00, 175.00] | 0.825 | 80.00 [40.00, 162.50] | 80.00 [42.50, 200.00] | 0.902 |
| CD20_T | 234.00 [145.00, 264.25] | 190.00 [112.00, 267.00] | 0.259 | 235.50 [141.75, 275.00] | 151.50[71.75, 240.50] | 0.004** |
| CD20_A | 94.50 [28.50, 180.50] | 91.50 [38.75, 175.50] | 0.948 | 86.00 [26.75, 176.50] | 98.00 [47.75, 174.50] | 0.432 |
| CD66b_T | 11.80 [8.40, 19.00] | 18.34 [9.00, 63.25] | 0.052 | 14.34 [8.19, 27.50] | 17.34 [10.54, 94.00] | 0.170 |
| CD66b_A | 18.55 [11.32, 27.00] | 19.25 [11.48, 46.00] | 0.520 | 18.25 [11.11, 35.00] | 20.60 [13.18, 48.00] | 0.201 |
CD8 CD8+ T cells, CD20 CD20+ B cells, CD66b CD66b+ neutrophils, T Tumor tissues, A Adjacent normal tissues
**p <0.01
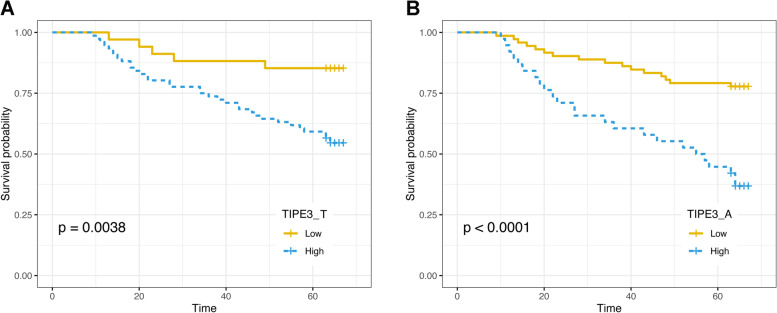
Correlation between TIPE3 expression and prognosis
After long-term follow-up, mortality was observed in 35.35% (n = 39) of CRC patients. Then, based on the prognostic information, we conducted a Kaplan–Meier survival analysis based on the TIPE3 expression (Fig. 4), which was significantly correlated with the survival rate of patients with tumor tissues (p = 0.0038) and adjacent normal tissues (p<0.0001); a high TIPE3 expression correlated with a lower survival rate.
Fig. 4.
Kaplan-Meier survival curves associated with TIPE3 expression of CRC patients: A Survival curve of tumor tissues for CRC patients; B Survival curve of adjacent normal tissues for CRC patients. T, tumor tissues; A, adjacent normal tissues
Finally, we conducted a Cox regression analysis of univariate variables and multivariate variables (Table 3), and a univariate regression analysis showed that the TIPE3 expression in tumor tissues (HR = 3.647, 95% CI: 1.425–9.332, p = 0.007), the TIPE3 expression in adjacent normal tissues (HR = 3.557, 95% CI: 1.884–6.781, p<0.001), the number of CD8+ T cells in tumor tissues (HR = 0.461, 95% CI: 0.240–0.889, p = 0.020), the number of CD20+ B cells in tumor tissues (HR = 0.468, 95% CI: 0.243–0.900, p = 0.023), the number of CD20+ B cells in adjacent normal tissues (HR = 0.496, 95% CI: 0.258–0.955, p=0.023), the number of CD66b+ neutrophils in tumor tissues (HR = 2.696, 95% CI: 1.340–5.424, p = 0.005), the number of CD66b+ neutrophils in adjacent normal tissues (HR = 3.359, 95% CI: 1.634–6.904, p<0.001), lymphatic metastasis (HR = 2.358, 95% CI: 1.224–4.543, p = 0.010), TNM stage (HR = 1.924, 95% CI: 1.15–3.218, p = 0.013), and tumor grade (HR = 0.476, 95% CI: 0.246–0.921, p = 0.027) were significantly correlated with OS. These prognostic factors were then subjected to multivariate regression analysis, and the results showed that the TIPE3 expression in adjacent normal tissues (HR = 3.215, 95% CI: 1.569–6.586, p=0.0014), the number of CD8+ T cells in adjacent normal tissues (HR = 0.387, 95% CI: 0.184–0.813, p = 0.0122), and the number of CD66b+ neutrophils in adjacent normal tissues (HR = 2.474, 95% CI: 1.036–5.905, p = 0.0413) were prognostic factors affecting the OS rate of CRC patients.
Table 3.
Univariate and multivariate cox proportional hazards models for the predictors of overall survival
| Variable | Univariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| TIPE3_T | 3.647 | (1.425 – 9.332) | 0.007** | 2.395 | (0.896-6.399) | 0.0816 |
| TIPE3_A | 3.577 | (1.884 – 6.791) | <0.001 | 3.215 | (1.569-6.586) | 0.0014** |
| CD8_T | 0.461 | (0.240 - 0.889) | 0.020* | 0.635 | (0.314-1.284) | 0.2062 |
| CD8_A | 0.542 | (0.288 - 1.018) | 0.057 | 0.387 | (0.184-0.813) | 0.0122* |
| CD20_T | 0.468 | (0.243 - 0.900) | 0.023* | 0.701 | (0.329-1.493) | 0.3568 |
| CD20_A | 0.496 | (0.258 – 0.955) | 0.036* | 0.558 | (0.276-1.128) | 0.1043 |
| CD66b_T | 2.696 | (1.340 – 5.424) | 0.005** | 0.965 | (0.385-2.423) | 0.9401 |
| CD66b_A | 3.359 | (1.634 – 6.904) | <0.001 | 2.474 | (1.036-5.905) | 0.0413* |
| Gender | 1.438 | (0.764 - 2.709) | 0.261 | |||
| Age | 0.985 | (0.964 - 1.007) | 0.188 | |||
| Invasion | 1.638 | (0.962 - 2.791) | 0.069 | 0.972 | (0.417-2.263) | 0.9471 |
| Grade | 0.476 | (0.246 - 0.921) | 0.027* | 0.620 | (0.287-1.338) | 0.2234 |
| TNM | 1.924 | (1.150 - 3.218) | 0.013* | 1.076 | (0.214-5.410) | 0.9292 |
| Lymph node metastasis | 2.358 | (1.224 - 4.543) | 0.010* | 1.553 | (0.213-11.310) | 0.6637 |
| Hb | 0.999 | (0.987 - 1.012) | 0.928 | |||
| WBC | 0.978 | (0.832 - 1.150) | 0.790 | |||
| PLT | 1.001 | (0.997 - 1.005) | 0.674 | |||
| Neutrophil | 0.967 | (0.817 - 1.145) | 0.698 | |||
| Monocyte | 0.805 | (0.109 - 5.971) | 0.832 | |||
| Lymphocyte | 1.132 | (0.663 - 1.932) | 0.651 | |||
HR Hazard ratio, T Tumor tissues, A Adjacent normal tissues, Hb Hemoglobin, WBC White blood cell, PLT Platelet
*p <0.05, **p <0.01
Discussion
The most effective form of prevention and early treatment of CRC is colonoscopy, which can detect precancerous lesions and early cancers to improve survival and prognosis rates significantly [16]. Current evidence suggests that through early screening, diagnosis, and treatment, patients with rectal cancer have a better prognosis, with a five-year survival rate of about 90% and a metastasis rate of only 14% [17]. In recent years, researchers have achieved significant strides in bringing awareness to the importance of early screening [18], made improvements to surgical techniques [19], and developed targeted therapy [20], which have significantly improved the survival rate of CRC patients. In our work, we found that patients with a high TIPE3 expression had a lower survival rate, while patients with a low TIPE3 expression had a higher survival rate. However, the type of TIPE positive cells was not analyzed in detail. Univariate regression analysis showed that the expression of TIPE3 and the number of CD66b+ neutrophils were risk factors for the OS of CRC patients; and the number of CD8+ T cells, the number of CD20+ B cells, and tumor grade were protective factors for the OS of CRC patients. These prognostic factors were then subjected to multivariate regression analysis, and the results show that the expression of TIPE3, the number of CD8+ T cells, and the number of CD66b+ neutrophils are prognostic factors affecting the OS rate of CRC patients, and TIPE3 is correlated with survival rate.
Our study found that the TIPE3 expression in CRC cancer tissues was significantly higher than in adjacent normal tissues, which may be related to the fact that TIPE3 can promote the occurrence and development of tumors. It is widely thought that at the cancerous site, TIPE3 is stimulated by the tumor environment, resulting in a higher TIPE3 expression, which in turn accelerates the transport rates of PIP2 and PIP3, two lipid second messengers; this activates the PI3K/AKT and MEK-ERK signaling pathways, which further promotes the growth, proliferation, and migration of tumor cells, accounting for the malignancy and poor prognosis. Combined with the prognostic information of CRC patients, it is suggested that a high TIPE3 expression predicts a poor prognosis, and the survival rate of these patients is significantly lower than that of patients with a low TIPE3 expression, consistent with the results of the TCGA database analysis (Supplementary Fig. 1). We noted that Zhong’s analysis of 49 CRC samples showed no correlation between TIPE3 mRNA expression levels and patients’ clinicopathological features, while the TIPE3 protein expression level in the tumor group was lower than that in the adjacent group [21]. This contrasts our current results, possibly because of the different number of samples tested or the existence of tumor heterogeneity. In our work, 110 samples were used, and IHC staining was performed to count the number of TIPE3-positive cells in the tumor and adjacent tissues, and two conditions—high and low TIPE3 expressions—in tumor tissues were found, among which the number of high-expression samples was 76 and the number of low-expression samples was 34. This result is consistent with most studies [22, 23].
Tumor-infiltrating immune cells are an important component of tumor tissue and play a crucial role in tumor occurrence and development. T cells are key tumor-infiltrating immune cells [24], and CD8+ T cells, a T-cell subtype, participate in the immune surveillance of tumor antigens during tumor development. T cell antigen receptors activate CD8+ T cells, rapidly proliferate and differentiate into cytotoxic T lymphocytes, and finally eliminate cancer cells through cellular immunity. Ample literature suggests that the extensive infiltration of CD8+ T cells in tumors is associated with good patient prognosis [25–28]. In our work, we found that the expression of TIPE3 and the number of CD8+ T cells were prognostic factors affecting the OS rate of CRC patients. Although our study did not find a significant correlation between the TIPE3 expression and the number of tumor-infiltrating immune cells, a Cox regression analysis showed that the TIPE3 expression and CD8+ T cells jointly affect patient survival (Table 3 and Supplementary Fig. 2), suggesting they have significant prospects for clinical applications as prognostic indicators.
Conclusion
Using clinical samples from 110 CRC patients, we found the TIPE3 protein to be upregulated in CRC cancer tissues and to be significantly correlated with patients’ OS rate. The high TIPE3 expression correlated with poor overall survival of the patients.
Supplementary Information
Additional file 1: Supplementary Figure 1. Overall survival curves associated with TIPE3 expression in the TCGA database. Supplementary Figure 2. Kaplan-Meier survival curves associated with immune cells of CRC patients: (A, B) Survival curves associated with CD8+ T cells of CRC patients: (A) Survival curve of tumor tissues; (B) Survival curve of adjacent normal tissue; (C, D) Survival curves associated with CD20+ B cells of CRC patients: (C) Survival curve of tumor tissues; (D) Survival curve of adjacent normal tissue; (E, F) Survival curves associated with CD66b+ neutrophils of CRC patients: (E) Survival curve of tumor tissues; (F) Survival curve of adjacent normal tissue. T, tumor tissues; A, adjacent normal tissue.
Acknowledgments
The authors thank the Center for Scientific Research of Anhui Medical University for their valuable help in our experiments.
Abbreviations
- AJCC
American Joint Committee on Cancer
- B cells
B- T-lymphocyte
- CA199
Carbohydrate antigen 199
- CD
Cluster of Differentiation
- CEA
Carcinoembryonic antigen
- CI
Confidence interval
- CRC
Colorectal cancer
- DED
Death effector domain
- FFPE
Formalin-fixed paraffin-embedded
- HR
Hazard ratio
- IHC
Immunohistochemistry
- IQR
interquartile range
- OS
Overall survival
- PIP2
Phosphatidylinositol 4,5-bisphosphate
- PIP3
Phosphatidylinositol 3,4,5-trisphosphate
- SD
Standard deviation
- T cells
T-lymphocyte
- TNFAIP8L3/TIPE3
Tumor necrosis factor α-induced protein 8 like 3
Authors’ contributions
PPZ, YZ, and JG designed the study. HBX, HW, SPZ, and AMX were involved in the data collection. YX, HBX, and YZ performed the statistical analyses. YZ, HBX, and JG had full access to all the data in the study and takes responsibility for the integrity data and the accuracy of the data analysis. YX, YZ, HBX, YNW, LL, and LCW contributed to the interpretation of the results. All authors critically revised the manuscript, and all authors have read and approved the final manuscript. All authors had access to the data in the study, and all authors accept responsibility for the decision to submit for publication.
Funding
This work was supported by grants from the National Natural Science Foundation of China (81801317, 81571293), the Basic and Clinical Cooperative Research Promotion Program of Anhui Medical University (2019xkjT029), Clinical Medicine Discipline Construction Project of Anhui Medical University (2020lcxk032), National and provincial key specialty construction project (Z155080000004).
Availability of data and materials
The data that support the findings of this study are available from the corresponding authors but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Anhui Medical University and The First Affiliated Hospital of Anhui Medical University.
Declarations
Ethics approval and consent to participate
Informed consent was obtained from all participants before the study. This study was approved by the Ethics Committees of Anhui Medical University and the First Affiliated Hospital of Anhui Medical University. All procedures performed in this study involving human participants were by the Declaration of Helsinki (as revised in 2013).
Consent for publication
Not applicable.
Competing interests
There were no financial or nonfinancial competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yue Xu, Yong Zhu and Hengbo Xia contributed equally to this work.
Contributor Information
Jiao Gong, Email: gongjiao@mail2.sysu.edu.cn.
Pingping Zhang, Email: 791663310@qq.com.
References
- 1.Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. 2021;127(16):3029–3030. doi: 10.1002/cncr.33587. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2019. Geneva: World Health Organization; 2020. http://who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death.
- 3.Yang Y, Han Z, Li X, et al. Epidemiology and risk factors of colorectal cancer in China[J] Chin J Cancer Res. 2020;32(6):729–741. doi: 10.21147/j.issn.1000-9604.2020.06.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Padmavathi G, Banik K, Monisha J, Bordoloi D, Shabnam B, Arfuso F, Sethi G, Fan L, Kunnumakkara AB. Novel tumor necrosis factor-alpha induced protein eight (TNFAIP8/TIPE) family: Functions and downstream targets involved in cancer progression. Cancer Lett. 2018;432:260–271. doi: 10.1016/j.canlet.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Sun H, Gong S, Carmody RJ, Hilliard A, Li L, Sun J, Kong L, Xu L, Hilliard B, Hu S, et al. TIPE2, a negative regulator of innate and adaptive immunity that maintains immune homeostasis. Cell. 2008;133(3):415–426. doi: 10.1016/j.cell.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bordoloi D, Banik K, Shabnam B, Padmavathi G, Monisha J, Arfuso F, Dharmarajan A, Mao X, Lim LHK, Wang L, Fan L, Hui KM, Kumar AP, Sethi G, Kunnumakkara AB. TIPE Family of Proteins and Its Implications in Different Chronic Diseases. Int J Mol Sci. 2018;19(10):2974. doi: 10.3390/ijms19102974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hitomi J, Christofferson DE, Ng A, Yao J, Degterev A, Xavier RJ, Yuan J. Identification of a molecular signaling network that regulates a cellular necrotic cell death pathway. Cell. 2008;135(7):1311–1323. doi: 10.1016/j.cell.2008.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cui J, Zhang G, Hao C, et al. The expression of TIPE1 in murine tissues and human cell lines [J]. Mol Immunol. 2011;48(12-13):1548–55. [DOI] [PubMed]
- 9.Lian K, Ma C, Hao C, et al. TIPE3 protein promotes breast cancer metastasis through activating AKT and NF-kappaB signaling pathways. Oncotarget. 2017;8(30):48889–48904. doi: 10.18632/oncotarget.16522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang G, Guo C, Zhao H, et al. TIPE3 differentially modulates proliferation and migration of human non-small-cell lung cancer cells via distinct subcellular location[J] BMC Cancer. 2018;18(1):260. doi: 10.1186/s12885-018-4177-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan F, Liu B, Xu Y, Li Y, Sun Q, Xu P, Geng R, Den G, Yang J, Zhang S, Gao L, Liao J, Liu J, Yang X, Tan Y, Chen Q. TIPE3 is a regulator of cell apoptosis in glioblastoma. Cancer Lett. 2019;1(446):1–14. doi: 10.1016/j.canlet.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Galon J, Pages F, Marincola FM, Angell HK, Thurin M, Lugli A, Zlobec I, Berger A, Bifulco C, Botti G, et al. Cancer classification using the Immunoscore: a worldwide task force. J Transl Med. 2012;10:205. doi: 10.1186/1479-5876-10-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galluzzi L, Buque A, Kepp O, Zitvogel L, Kroemer G. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell. 2015;28(6):690–714. doi: 10.1016/j.ccell.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Lee HE, Chae SW, Lee YJ, Kim MA, Lee HS, Lee BL, Kim WH. Prognostic implications of type and density of tumour-infiltrating lymphocytes in gastric cancer. Br J Cancer. 2008;99(10):1704–1711. doi: 10.1038/sj.bjc.6604738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Y, Zhao Q, Peng C, Sun L, Li XF, Kuang DM. Neutrophils promote motility of cancer cells via a hyaluronan-mediated TLR4/PI3K activation loop. J Pathol. 2011;225(3):438–447. doi: 10.1002/path.2947. [DOI] [PubMed] [Google Scholar]
- 16.Ladabaum U, Dominitz JA, Kahi C, Schoen RE. Strategies for Colorectal Cancer Screening. Gastroenterology. 2020;158(2):418–432. doi: 10.1053/j.gastro.2019.06.043. [DOI] [PubMed] [Google Scholar]
- 17.Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–164. doi: 10.3322/caac.21601. [DOI] [PubMed] [Google Scholar]
- 18.Wancata LM, Banerjee M, Muenz DG, Haymart MR, Wong SL. Conditional survival in advanced colorectal cancer and surgery. J Surg Res. 2016;201(1):196–201. doi: 10.1016/j.jss.2015.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruers T, Van Coevorden F, Punt CJ, Pierie JE, Borel-Rinkes I, Ledermann JA, Poston G, Bechstein W, Lentz MA, Mauer M, et al. Local Treatment of Unresectable Colorectal Liver Metastases: Results of a Randomized Phase II Trial. J Natl Cancer Inst. 2017;109(9):djx015. doi: 10.1093/jnci/djx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piawah S, Venook AP. Targeted therapy for colorectal cancer metastases: A review of current methods of molecularly targeted therapy and the use of tumor biomarkers in the treatment of metastatic colorectal cancer. Cancer. 2019;125(23):4139–4147. doi: 10.1002/cncr.32163. [DOI] [PubMed] [Google Scholar]
- 21.Zhong M, Chen Z, Yan Y, Bahet A, Cai X, Chen H, Ran H, Qu K, Han Z, Zhuang G, Zhang S, Wang Y. Expression of TIPE family members in human colorectal cancer. Oncol Lett. 2021;21(2):118. doi: 10.3892/ol.2020.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padmavathi G, Banik K, Monisha J, Bordoloi D, Shabnam B, Arfuso F, Sethi G, Fan L, Kunnumakkara AB. Novel tumor necrosis factor-α induced protein eight (TNFAIP8/TIPE) family: Functions and downstream targets involved in cancer progression. Cancer Lett. 2018;28(432):260–271. doi: 10.1016/j.canlet.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 23.Fayngerts SA, Wu J, Oxley CL, et al. TIPE3 is the transfer protein of lipid second messengers that promote cancer[J] Cancer Cell. 2014;26(4):465–78. doi: 10.1016/j.ccr.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finck A, Gill SI, June CH. Cancer immunotherapy comes of age and looks for maturity. Nat Commun. 2020;11(1):3325. doi: 10.1038/s41467-020-17140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang X, Xu J, Liu M, Xing H, Wang Z, Huang L, Mellor AL, Wang W, Wu S. Adoptive CD8(+) T cell therapy against cancer: Challenges and opportunities. Cancer Lett. 2019;462:23–32. doi: 10.1016/j.canlet.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 26.Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 27.Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol. 2008;8(7):523–532. doi: 10.1038/nri2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shang B, Liu Y, Jiang SJ, Liu Y. Prognostic value of tumor-infiltrating FoxP3+ regulatory T cells in cancers: a systematic review and meta-analysis. Sci Rep. 2015;5:15179. doi: 10.1038/srep15179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Figure 1. Overall survival curves associated with TIPE3 expression in the TCGA database. Supplementary Figure 2. Kaplan-Meier survival curves associated with immune cells of CRC patients: (A, B) Survival curves associated with CD8+ T cells of CRC patients: (A) Survival curve of tumor tissues; (B) Survival curve of adjacent normal tissue; (C, D) Survival curves associated with CD20+ B cells of CRC patients: (C) Survival curve of tumor tissues; (D) Survival curve of adjacent normal tissue; (E, F) Survival curves associated with CD66b+ neutrophils of CRC patients: (E) Survival curve of tumor tissues; (F) Survival curve of adjacent normal tissue. T, tumor tissues; A, adjacent normal tissue.
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Anhui Medical University and The First Affiliated Hospital of Anhui Medical University.