Abstract
It is important to consider how identity, culture, and social adversity influence maternal mental health among Latina women both because this community faces unique cultural stressors and also because factors that undermine women’s mental health during pregnancy and postpartum could have injurious consequences that cascade across generations. This study uses data from a questionnaire administered to Latina pregnant and postpartum women in Southern California, examining cultural orientation, discrimination, and mental health. Results demonstrate mental health benefits for both American and Latino cultural orientations, but the latter’s benefit of lower anxiety was only apparent with high discrimination. American and Latino cultural values systems had opposite relationships with depression, with the latter protective and also positively associated with happiness. More traditional gender roles values were associated with greater perceived stress and lower happiness. Different aspects of familism had opposite effects as obligation was associated with less anxiety and referent (defining oneself communally with kin) with more. Results suggest that social adversity and cultural identity and values influence maternal psychology. This study makes a unique contribution by integrating anthropological and biopsychosocial methods and theories towards addressing an issue of public-health importance.
Keywords: cultural stressors, minority health disparities, perinatal, mood disorders, Latino health
RESUMEN
Es importante considerar cómo la identidad, la cultura y la adversidad social influyen en la salud mental materna entre mujeres latinas tanto porque esta comunidad enfrenta factores culturales únicos causantes de estrés como porque factores que socavan la salud mental de las mujeres durante el embarazo y el postparto podrían tener consecuencias perjudiciales en cadena a través de las generaciones. Este estudio utiliza información de una encuesta administrada a mujeres latinas en embarazo o en posparto en el sur de California examinando la orientación cultural, la discriminación y la salud mental. Los resultados demuestran los beneficios de la salud mental tanto para orientaciones culturales estadounidenses como latinas, pero el beneficio de la más baja ansiedad de las últimas fue sólo aparente con baja discriminación. Sistemas de valores culturales estadounidenses y latinos tienen relaciones opuestas con la depresión, con los últimos siendo protectores y también asociados positivamente con la felicidad. Valores más tradicionales sobre los roles de género fueron asociados con un mayor estrés percibido y más baja felicidad. Aspectos diferentes del familismo tuvieron efectos opuestos en la medida en que la obligación estuvo asociada con menor ansiedad y el referente (definirse uno mismo comunalmente con parientes) con mayor. Los resultados sugieren que la adversidad y la identidad cultural y los valores influyen en la psicología materna. Este estudio hace una contribución única al integrar métodos y teorías antropológicas y biopsicosociales hacia el abordaje de una cuestión de importancia en salud pública.
INTRODUCTION
Anthropological scholarship urges the consideration of medicine as a social and evolutionary science, contemplating individuals within sociocultural contexts and biological life cycles (Gurven et al. 2017; Panter-Brick and Eggerman 2018). A potential public health application of an anthropological perspective is to elucidate how the experiences of individuals embedded within cultural communities and positioned within a particular life-history stage contribute to epidemiological trends and health disparities. In this context, it is noteworthy that Latina women exhibit higher rates of mood disorders compared to women in other ethnic groups in the United States (Joiner et al. 2001). Evidence suggests these trends may be partially attributed to the uniquely stressful conditions imposed by cultural stressors, such as acculturation and discrimination (Abraído-Lanza et al. 2006; Flaskerud and Uman 1996; Koneru et al. 2007). Conversely, Latinos may benefit from unique resilience factors afforded by cultural norms, such as familism and religiosity (Abraído-Lanza et al. 2006; Cervantes, Gattamorta, and Berger-Cardoso 2019; Corona et al. 2017). However, little is known about how these dynamics manifest during the life phases of pregnancy and postpartum. Moreover, culture has been operationalized in oversimplified ways in previous studies on acculturation, failing to measure the aspects of cultural schemas that might causally influence mental health (Doucerain 2019). Here, we address these issues.
Various arguments from social sciences justify the importance of our study exploring how the cultural stressors faced by the Latino community and cultural resilience factors relate to mental health in pregnant and postpartum women, described below. We apply biocultural anthropological and biopsychosocial frameworks to explore the dynamic interplay between acculturation, cultural values, and discrimination in a cohort of Latina pregnant and postpartum women. We seek to understand how this constellation of constructs relates to perceived stress, state anxiety, depression, and happiness. We also consider how discrimination moderates the relationships that mental health outcomes have with acculturation and cultural values. This endeavor answers calls from anthropological scholarship in health disparities to utilize a multidimensional approach that investigates multiple levels of analysis (Gravlee 2009) by quantifying not only overarching cultural identity categories (e.g., Latino cultural orientation) but also individual cultural values within those orientations. Also, we answer calls from psychological scholarship to examine how specific cultural elements moderate environmental factors to affect health (Kagawa Singer et al. 2016).
The biopsychosocial turn in medical and psychological research has been beneficial in bridging factors that interact to affect human health and thereby account for epidemiological trends (Engel 1977). However, anthropological perspectives have been generally lacking in the biopsychosocial research arena (Kagawa Singer et al. 2016). Anthropological understandings can contribute to biopsychosocial methods and interpretations of research findings due to sociocultural and evolutionary sciences’ engagements with each element of the biopsychosocial triad. Reciprocally, anthropological methods could be enhanced in terms of applicability to public health by employing better quantitative approaches in order to speak to observed epidemiological trends (Gravlee 2009; Hahn and Inhorn 2009). Reluctance among anthropologists to use quantitative scales to measure individuals’ social and cultural states has been multifariously justified, but there still may be approaches that are tolerable when considered alongside the benefits of bridging anthropology and public health (Hahn and Inhorn 2009).
Sociocultural contexts may influence maternal psychology and become embodied (MacLachlan 2004)—or biologically embedded (Hertzman 1999)—to affect gestational physiology. The embodiment concept derives from social epidemiology and medical anthropology, while the biological embedding concept derives from developmental and medical sciences, but they describe the same phenomenon. This model describes how social experiences and environmental exposures accumulate biological effects across the course of a person’s life to influence disease susceptibility and risk. This conceptual framework has been employed to describe the health effects of socioeconomic status, discrimination, and stress (Zuckerman and Martin 2016). Embodiment and biological embedding have been discussed for understanding the biosocial origins of minority health disparities in nonpregnant populations (Csordas 1994), and we argue for increased application of these frameworks for understanding (and intervening in) transgenerational patterns of minority health disparities (Fox et al. 2018; Fox et al. 2015). Here, we present an empirical test of the critical first step in elucidating this process: measuring how sociocultural stressors relate to maternal mental health.
Latinos exhibit higher and increasing rates of adverse birth outcomes compared to white Americans (Hamilton et al. 2019), and evidence suggests that acculturation is positively correlated with adverse birth outcomes among Latinos (Cobas et al. 1996; Ruiz, Dolbier, and Fleschler 2006; Scribner and Dwyer 1989), although the biopsychosocial mechanism by which this pattern emerges remains understudied (Torres, Driscoll, and Voell 2012). Mental health during pregnancy and postpartum is a crucial public health issue because of its relevance for both women’s and children’s well-being. These phases represent particularly vulnerable periods for women’s onset of mood disorders (Rayburn 2018), and mood dysregulation during pregnancy and postpartum is associated with women’s lifelong psychopathology risk and child developmental deficits (DiPietro et al. 2006; Schetter and Glynn 2011). During pregnancy and postpartum, up to 20 percent of women exhibit depression and 11 percent anxiety (Glynn, Howland, and Fox 2018). Mothers’ depression, anxiety, and stress during pregnancy have been associated with adverse birth outcomes, such as preterm birth and low birth weight (Dunkel-Schetter 1998; Glynn et al. 2008; Hoffman et al. 2016).
Previous Findings
Cultural Orientation and Mental Health.
Acculturation describes the loss of origin cultural orientation and the adoption of host or majority cultural orientation that occurs when individuals from minority cultures, usually immigrants or Indigenous people, live in prolonged contact with the majority culture (Fox, Thayer, and Wadhwa 2017b). Acculturation can involve changes in many domains, such as identity, values, preferences, and behaviors. Berry (2003) conceptualized acculturation as a multidimensional process in which loss of origin and adoption of host cultural orientations occur as independent, orthogonal processes. A large literature suggests that acculturation affects mental health among Latinos and other minority and immigrant groups (Abraído-Lanza et al. 2006; Finch, Frank, and Vega 2004; Finch, Kolody, and Vega 2000; Koneru et al. 2007; Organista, Organista, and Kurasaki 2003).
A few previous studies have explored the links between acculturation and mental health among pregnant Latina women, with observations generally—but not always (Beck, Froman, and Bernal 2005; D’Anna-Hernandez, Aleman, and Flores 2015; Preciado and D’Anna-Hernandez 2017)—suggesting that acculturation is associated with mental health detriments (Barcelona de Mendoza et al. 2016; Campos et al. 2007; Heilemann et al. 2004; Martinez-Schallmoser, Telleen, and Macmullen 2003; Ruiz, Dolbier, and Fleschler 2006; Walker et al. 2012). A qualitative study found that first-generation Mexican American women had more positive feelings and happiness associated with pregnancy compared to second-generation peers (Fleuriet and Sunil 2015), suggesting that acculturation may be associated with poorer prenatal maternal mental health. Our study improves upon previous acculturation study designs by assessing Latino and American cultural orientations separately, as did some (Campos et al. 2007; Preciado and D’Anna-Hernandez 2017; Walker et al. 2012) but not all (Beck, Froman, and Bernal 2005; D’Anna-Hernandez, Aleman, and Flores 2015; Heilemann et al. 2004; Martinez-Schallmoser, Telleen, and Macmullen 2003; Ruiz, Dolbier, and Fleschler 2006) previously, and including more mental health outcomes.
Cultural Values and Mental Health.
Cultural values have been proposed as an explanatory mechanism to understand observed benefits of traditional cultural orientation on mental health, and the loss of these values has been suggested to explain why adoption of host cultural orientation can lead to health detriments (Umaña-Taylor, Updegraff, and Gonzales-Backen 2011).
In nonpregnant populations, previous studies have demonstrated links between cultural values and mental health in Latinos (Corona et al. 2017; Katiria Perez and Cruess 2014; Lorenzo-Blanco et al. 2012; Milan and Wortel 2015; Morcillo et al. 2011; Zeiders et al. 2013,) as well as other ethnic groups (Constantine et al. 2006; Hovey, Kim, and Seligman 2006; Milan and Wortel 2015; Sawrikar and Hunt 2005; Sayegh and Knight 2010). Among Latinos, the majority of research has focused on familism, while other traditionally Latino cultural values have been overlooked (Corona et al. 2017). Knight et al. (2010) developed the Mexican American Cultural Values Scale (MACVS) with nine relevant subscales, expanding the operationalization of these cultural values for quantitative research.
D’Anna-Hernandez, Aleman, and Flores (2015) conducted the only previous study known to the author that investigated links between cultural values and mental health in Latina pregnant women, and they found that none of the nine MACVS subscales (Knight et al. 2010) predicted depressive symptoms using the Center for Epidemiologic Studies Depression (CES-D) scale. We expand upon this study by using a larger cohort size, more gestational ages, and more mental health outcomes beyond depression.
Discrimination and Mental Health.
We are interested in the possibility that discrimination confers not only its own influence on maternal mental health but also acts as a moderator of the correlations mental health outcomes have with acculturation and cultural values (Fox, Thayer, and Wadhwa 2017a). Discrimination has been positively correlated with depression among pregnant Latina women during the first (D’Anna-Hernandez, Aleman, and Flores 2015) and second (Walker et al. 2012) trimesters, although it was not correlated with anxiety (Preciado and D’Anna-Hernandez 2017). An extensive literature has demonstrated links between discrimination and mental health risk in Latino nonpregnant populations (Araújo and Borrell 2006; Corona et al. 2017; Flores et al. 2008; Hwang and Goto 2008). One study found that the interaction between Anglo (but not Latino) orientation and perceived discrimination predicted acculturative stress, a precursor of psychological distress (Torres, Driscoll, and Voell 2012).
We argue that discrimination may alter the relationships between cultural orientation and mental health. For example, an individual who is oriented strongly—compared to weakly—toward Latino culture could be expected to exhibit inferior mental health in a context where Latino identity is denigrated (i.e., high levels of discrimination). It could also be argued that a high-Latino-cultural-orientation individual in the same context could exhibit superior mental health compared to a low-Latino-cultural-orientation peer due to Latino-cultural-specific resilience factors buffering the deleterious impact of discrimination. These hypothetical vignettes underscore the need to examine the ways in which discrimination interacts with cultural orientation and values to influence mental health.
METHODS
Cohort and Protocol
Data for these analyses derive from Wave 1 of the Mothers’ Cultural Experiences (MCE) study. The overarching goal of MCE is to explore how social, cultural, neighborhood, and political factors relate to psychological and biological states in pregnant and postpartum women, birth outcomes, and offspring health and development. Wave 2 is a longitudinal pregnancy cohort study that is currently ongoing. MCE Wave 1 involved an anonymous cross-sectional questionnaire administered in person by study staff to N = 361 pregnant and postpartum women recruited from four sites in Southern California in 2016–2018: Women’s, Infants, and Children (WIC) in Santa Ana, CA; MOMS Orange County in Santa Ana, CA; the Westside Family Health Center in Santa Monica, CA; and Olive View-UCLA Medical Center in Sylmar, CA (Table 1). Potential participants were approached in clinic waiting rooms or at prenatal classes. Eligibility criteria were age 18+, English or Spanish speaking, pregnant or up to one year postpartum, and self-identified as Latina, Hispanic, Chicana, Mexicana, and/or Latin American. Written, informed consent was obtained after full study procedures were described. Participants received cash compensation. This study was approved by the Institutional Review Boards of participating institutions. This study adheres to the tenets of the Declaration of Helsinki.
TABLE 1.
Cohort demographics and descriptive statistics
| Total analytic cohort size | 279 |
| Recruitment site (N (%)) | |
| MOMS Orange County | 56 (20.1) |
| Olive View-UCLA Medical Center | 82 (29.4) |
| Westside Family Health Center | 31 (11.1) |
| WIC | 110 (39.4) |
| Age (mean (SD)) | 28.41 (6.34) |
| Country of birth (N (%)) | |
| U.S. | 139 (49.8) |
| Mexico | 109 (39.1) |
| El Salvador | 12 (4.3) |
| Guatemala | 7 (2.5) |
| Another country | 8 (2.9) |
| NA | 4 (1.4) |
| Age moved to US, foreign-born subset (Years) (mean (SD)) | 14.61 (9.35) |
| Mexican heritage or origin (N (%)) | |
| Yes | 246 (88.2) |
| No | 22 (7.9) |
| NA | 11 (3.9) |
| Education (N (%)) | |
| Elementary or incomplete secondary | 32 (11.5) |
| High school or GED | 132 (47.3) |
| Technical or vocational program | 40 (14.3) |
| Associate degree | 16 (5.7) |
| Bachelors or higher | 40 (14.3) |
| Other | 11 (3.9) |
| NA | 8 (2.9) |
| Food insecure (N (%)) | |
| Yes | 121 (43.4) |
| No | 148 (53.0) |
| NA | 10 (3.6) |
| Household currently receiving Food Stamps / CalFresh / SNAP benefits (N (%)) | |
| Yes | 71 (25.4) |
| No | 199 (71.3) |
| NA | 9 (3.2) |
| Household currently receiving WIC benefits (N (%)) | |
| Yes | 187 (67.0) |
| No | 84 (30.1) |
| NA | 8 (2.9) |
| Subjective SES (1–10) (mean (SD)) | 5.75 (1.89) |
| Reproductive status (N (%)) | |
| Trimester 1 | 20 (7.2) |
| Trimester 2 | 49 (17.6) |
| Trimester 3 | 136 (48.7) |
| Trimester unknown | 15 (5.4) |
| Postpartum | 59 (21.1) |
| Parity (N (%)) | |
| 0 | 75 (26.9) |
| 1 | 82 (29.4) |
| 2 | 62 (22.2) |
| 3 | 27 (9.7) |
| 4 | 14 (5.0) |
| 5 | 4(1.4) |
| 6 | 6 (2.2) |
| NA | 9 (3.2) |
| In a romantic relationship (N (%)) | |
| Yes | 246 (88.2) |
| No | 31 (11.1) |
| NA | 2 (0.7) |
| Marital status (N (%)) | |
| Married | 124 (44.4) |
| Never married | 122 (43.7) |
| Separated | 13 (4.7) |
| Divorced | 13 (4.7) |
| NA | 7(2.5) |
| I speak Spanish ··· (N (%)) | |
| Extremely often or almost always | 139 (49.8) |
| Much or very often | 77 (27.6) |
| Moderately | 36 (12.9) |
| Very little or not very often | 18 (6.5) |
| Not at all | 8 (2.9) |
| NA | 1 (0.4) |
| Acculturation category (ARSMA-II) (N (%)) | |
| Very Mexican oriented | 62 (22.2) |
| Mexican oriented to approximately balanced bicultural | 109 (39.1) |
| Slightly Anglo oriented bicultural | 78 (28.0) |
| Strongly Anglo oriented | 27 (9.7) |
| Very assimilated; Anglicized | 3(1.1) |
| ARSMA-II Mexican orientation subscale (mean (SD)) | 3.77 (0.78) |
| ARSMA-II Anglo orientation subscale (mean (SD)) | 3.32 (0.90) |
| Clinical depression likely (EPDS ≥ 9) = TRUE (N (%)) | 54 (19.4) |
| Perinatal depression (EPDS, 0–30) (mean (SD)) | 5.78 (4.60) |
| State anxiety (STAI, 1–4) (mean (SD)) | 1.70 (0.58) |
| Perceived stress (PSS, 0–16) (mean (SD)) | 5.24 (2.61) |
| Happiness (OHQ, 1–6) (mean (SD)) | 4.58 (0.79) |
Caption: WIC: Women, Infants, and Children; SES: Socioeconomic status; ARSMA-II: Acculturation Rating Scale for Mexican Americans-II (Cuellar, Arnold, and Maldonado 1995); EPDS: Edinburgh Postnatal Depression Scale; STAI: State-trait anxiety inventory (Spielberger 1983); PSS: Perceived stress scale (Cohen, Kamarck, and Mermelstein 1983); OHQ: Oxford happiness questionnaire (Hills and Argyle 2002)
Measurement of Acculturation
Acculturation was assessed using the Acculturation Rating Scale for Mexican Americans II (ARSMA-II) (Cuellar, Arnold, and Maldonado 1995). ARSMA-II is a multidimensional scale, and we implemented the orthogonal Mexican Orientation Subscale (MOS), comprising 13 items, and the Anglo Orientation Subscale (AOS), comprising 17 items. For 7.9 percent of the cohort, their heritage was from a Latin American country other than Mexico, so they were instructed to skip the seven MOS items that specifically reference Mexico. Unexplained missingness was very low (1.5 percent of data points) and was mostly attributable to one item, “My contact with the USA has been . . .” (N = 12 missing). AOS and MOS scores were determined by taking the mean of nonmissing responses. Cronbach’s alpha in our study was 0.92 for the AOS (subsets administered in English 0.83 and Spanish 0.78, lower score mostly attributable to “My contact with the USA has been”—if removed, alpha = 0.81) and 0.90 for the MOS (English 0.89, Spanish 0.90).
Measurement of Cultural Values
Cultural values were assessed using the MACVS (Knight et al. 2010). The subscales were described by the original authors as reflecting either “Mexican” or “mainstream” values, but here we use the terms “Latino” and “American.” We acknowledge the problems with using the term “American” to refer to what can be interpreted as US-Anglo majority cultural values, as the word “American” reflects a wide variety of people and places. However, we use this word because we deemed it more respectful to minority groups than “mainstream.” We also utilized compilation scores by taking the mean of the appropriate subscales to reflect Latino cultural values system comprising subscales for religion, familism support, familism obligation, familism referent, respect, and traditional gender roles, and American cultural values system comprising subscales for material success, independence and self-reliance, and competition and personal achievement. This is the first study known to the author to employ the MACVS in a population that is not exclusively of Mexican origin. A potential limitation could be that this scale was developed for Mexican Americans, while our cohort includes 7.9 percent of individuals from other Latin American descent. Cronbach’s alpha in our study was 0.92 for Latino cultural values system (subsets administered in English 0.91 and Spanish 0.93) and 0.79 for American cultural values system (English 0.80, Spanish 0.78).
Measurement of Mental Health
Maternal prenatal mental health was assessed for depression using the Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, and Sagovsky 1987) validated among Latina pregnant women (Santos et al. 2007), for anxiety using the State form of the State-Trait Anxiety Inventory (STAI) (Spielberger 1983) six-item version validated among pregnant women (Marteau and Bekker 1992), for stress using the Perceived Stress Scale (PSS) (Cohen, Kamarck, and Mermelstein 1983) four-item version validated among pregnant women (Karam et al. 2012), and for happiness using the Oxford Happiness Questionnaire (Hills and Argyle 2002) eight-item short form validated (Cruise, Lewis, and McGuckin 2006) and widely used among diverse pregnant women (Jayasvasti and Kanchanatawan 2005; Türk, Sakar, and Erkaya 2017). Cronbach’s alphas in our study were 0.83 for EPDS (subsets administered in English 0.84 and Spanish 0.83), 0.80 for STAI (English 0.81, Spanish 0.79), 0.50 for PSS (English 0.56, Spanish 0.35), and 0.64 for OHQ (English 0.71, Spanish 0.55).
Measurement of Discrimination
In order to capture information about discrimination specifically related to ethnicity/race, the section was prefaced with the prompt (from the Perceived Ethnic Discrimination Questionnaire Community Version [PEDQ-CV] (Brondolo et al. 2005)) “Because of your ethnicity/race, how often . . .” followed by each item. For participants recruited in April 2016, the Brief PEDQ-CV was used, omitting the discrimination at work/school subscale to avoid issues related to maternity leave. Then, we replaced the PEDQ-CV by the EDS to minimize overall survey length. For participants recruited after April 2016 until the end of data collection in May 2018, we used the Everyday Discrimination Scale (EDS) (Williams et al. 1997), which has been widely used and validated in various US minority groups (Krieger et al. 2005; Reeve et al. 2011). The version we implemented derived from Shariff-Marco et al.’s (2011) evaluation of the scale’s psychometric properties, which involved minor rephrasing drawn from Krieger’s validation of the original Williams scale, as well as Krieger’s one additional item (“Have you have been followed around in stores?”). In order to maximize cohort sample size for our analyses, we included women who were administered the PEDQ-CV by rescaling their 1: 5 scores to mimic the EDS 0: 3 scores. Women who were administered the EDS were on average three years older, higher proportion pregnant versus postpartum, and had higher discrimination scores (Table S1). All statistical models control for which discrimination scale was administered. In the analytic cohort (after omitting women who were ineligible or with missing data, see Results), there were N = 223 whose discrimination scores derived from the EDS and N = 56 whose discrimination scores derived from the PEDQ-CV.
Covariates
In addition to the discrimination instrument covariates, the following four covariates were considered: socioeconomic status (SES), relationship status, age, and pregnant versus postpartum. To assess SES, a compilation variable was created based on participants’ educational attainment, food (in)security, and subjective socioeconomic status. These variables were each coded with higher values reflecting higher SES, normalized by unitization with zero minimum (x-minimum/range), and averaged. Though the survey included household income, these data were deemed too unreliable to include in the SES composite variable because it appeared many participants were not aware of the incomes of other household members, such as their parents. We were less concerned about the omission of income data because Walker et al. (2012) found no significant relationship between income and depression among pregnant Latina women. Relationship status was assessed with the question “Are you currently in a relationship? (example: boyfriend, partner, husband or spouse).” Maternal age was calculated based on month and year of birth, with all dates assumed to be the 15th of each month in order to preserve participant anonymity.
Pearson’s correlations (for continuous variables) and two-sided t-tests (for binary variables) were conducted for all combinations of potential covariates and mental health outcomes (Table S2). “Which discrimination scale was administered” was included as a covariate in all models because of our changed study protocol. Age and pregnant versus postpartum had no significant correlations with any of the mental health outcomes, and we had no a priori reason to believe they should confound the relationships between predictors and outcomes, so they were dropped from the models. SES was significantly correlated with OHQ (p = 0.04) and borderline correlated with PSS (p = 0.07) and EPDS (p = 0.08), so it was retained in all models. Relationship status was retained in all models because it had borderline significant relationships with PSS (p = 0.08) and OHQ (p = 0.04), and relationship status affected maternal mental health in other studies.
Statistical Methods
Multiple linear regression was used. Each of the four mental health outcomes had a separate model fitted for predictors reflecting acculturation, cultural values systems, and cultural values items, for a total of 12 models. Bonferroni adjustment for multiple testing was implemented. Each model included the predictors of interest, covariates, and terms reflecting the interaction of discrimination score with each of the predictors of interest. When results suggested an interaction term contributed a significant effect on a significant model fit, we plotted the marginal effects of the predictor of interest with the dataset subsetted by cohort median discrimination scores in order to visualize the interaction effect. Visual interpretation was supplemented by reporting simple slopes and post-hoc regression models with data subsets by median discrimination scores, although we note the caveat that subsetting the cohort also subsets control variables in ways that may have unintended influence on the post-hoc models (Table S3–6).
For missing data in covariate (control) variables, multivariate imputation by chained equations (MICE) (Van Buuren and Groothuis-Oudshoorn 2010) was implemented to preserve sample size. N = 32 individuals in the analytic dataset were missing at least one of the potential covariates: SES, age, or relationship status.
Mental health outcome variables were transformed to improve symmetry of distributions as EPDS cube root of score plus constant transformed, STAI natural log transformed, PSS no transformation, and OHQ second power transformed.
Descriptions of the dataset and statistical analysis plan were pre-registered in Open Science Framework, DOI 10.17605/OSF.IO/4QEXS. Data analysis was conducted using the R statistical programming language and environment. This manuscript was prepared using R Markdown to maximize reproducibility.
RESULTS
Analytic Cohort
From an original sample size of N = 361, ineligibility determined during data analysis was identified for N = 39 due to being more than one year postpartum and N = 8 due to other reasons, so these cases were omitted from further analysis. Analyses were conducted on the subset of eligible individuals who had complete data for all variables of interest, so further cases were omitted due to missing values for acculturation or cultural values (N = 18), mental health (N = 14), and discrimination (N = 3) to ultimately achieve an analytic cohort size of N = 279. While the other mental health assessment instruments do not have standard clinical cutoffs, 19.4 percent of participants exhibited EPDS scores suggestive of clinical depression (Murray and Carothers 1990), within the ranges of other recent studies measuring depression in Latina perinatal cohorts (Lara-Cinisomo, McKenney, and Meltzer-Brody 2017; Lara-Cinisomo et al. 2016).
Below, we describe results concerning the predictors of interest, with all results detailed in Tables 2–4.
TABLE 2.
Multiple regression models reflecting how acculturation relates to mental health outcomes
| Stress (PSS) |
Anxiety (STAI) |
Depression (EPDS) |
Happiness (OHQ) |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictor | β | p | β | p | β | p | β | p |
|
| ||||||||
| Intercept | 8.878 | <0.0001 **** | 0.535 | 0.009 ** | 2.01 | <0.0001 **** | 7.102 | 0.103 |
| American cultural orientation | −0.555 | 0.023 * | −0.01 | 0.738 | 0 | 0.993 | 1.771 | 0.008 ** |
| Latino cultural orientation | −0.257 | 0.343 | −0.009 | 0.799 | −0.05 | 0.259 | 1.334 | 0.071 • |
| Discrimination = Above cohort median | 0.512 | 0.807 | 0.519 | 0.054 • | 0.714 | 0.039 * | −1.052 | 0.854 |
| SES | −0.252 | 0.342 | −0.001 | 0.974 | −0.025 | 0.563 | 0.775 | 0.283 |
| In a romantic relationship = Yes | −0.78 | 0.105 | −0.033 | 0.591 | −0.11 | 0.162 | 2.071 | 0.114 |
| Which discrimination scale = EDS | −0.499 | 0.215 | −0.055 | 0.282 | −0.055 | 0.408 | 2.708 | 0.014 * |
| American cultural orientation : Discrimination (interaction) | 0.208 | 0.546 | 0.004 | 0.928 | −0.078 | 0.169 | −0.69 | 0.461 |
| Latino cultural orientation : Discrimination (interaction) | 0.041 | 0.917 | −0.099 | 0.053 • | −0.039 | 0.548 | 0.017 | 0.988 |
Caption: Model fitting statistics: PSS model: Multiple R2=0.11, F(8.0, 270.0)=4.11, p=0.0001 ***, Bonferroni adjusted p=0.0005 ***
STAI model: Multiple R2=0.09, F(8.0, 270.0)=3.39, p=0.0010 **, Bonferroni adjusted p=0.0040 **
EPDS model: Multiple R2=0.16, F(8.0, 270.0)=6.52, p=<0.0001 ****, Bonferroni adjusted p=<0.0001 ****
OHQ model: Multiple R2=0.12, F(8.0, 270.0)=4.82, p=<0.0001 ****, Bonferroni adjusted p=0.0001 ***
TABLE 4.
Multiple regression models reflecting how cultural values items relate to mental health outcomes
| Stress (PSS) |
Anxiety (STAI) |
Depression (EPDS) |
Happiness (OHQ) |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictor | β | p | β | p | β | p | β | p |
|
| ||||||||
| Intercept | 7.451 | <0.0001 **** | 0.73 | <0.0001 **** | 1.92 | <0.0001 **** | 9.041 | 0.027 * |
| Religion | 0.151 | 0.593 | 0.03 | 0.406 | 0.045 | 0.339 | 0.532 | 0.479 |
| Familism Support | −0.556 | 0.383 | −0.081 | 0.322 | 0.012 | 0.909 | 1.595 | 0.347 |
| Familism Obligation | −0.435 | 0.384 | −0.129 | 0.046 * | −0.111 | 0.185 | −1.778 | 0.181 |
| Familism Referent | 0.944 | 0.054 • | 0.148 | 0.019 * | 0.029 | 0.72 | 1.708 | 0.188 |
| Respect | −1.078 | 0.064 • | −0.043 | 0.563 | −0.107 | 0.268 | 1.218 | 0.43 |
| Material Success | −0.37 | 0.343 | −0.03 | 0.554 | 0.037 | 0.574 | −0.104 | 0.92 |
| Independence and Self-Reliance | 0.348 | 0.266 | −0.007 | 0.858 | 0.093 | 0.076 • | 0.857 | 0.304 |
| Traditional Gender Roles | 0.814 | 0.008 ** | 0.013 | 0.733 | 0.024 | 0.636 | −1.915 | 0.018 * |
| Competition and Personal Achievement | 0.146 | 0.65 | 0.029 | 0.489 | 0.011 | 0.842 | 0.019 | 0.982 |
| Discrimination = Above cohort median | 1.542 | 0.427 | 0.261 | 0.297 | 0.564 | 0.082 • | −4.682 | 0.364 |
| SES | −0.118 | 0.663 | −0.003 | 0.931 | −0.022 | 0.621 | 0.442 | 0.54 |
| In a romantic relationship = Yes | −0.848 | 0.078 • | −0.045 | 0.467 | −0.121 | 0.131 | 1.988 | 0.12 |
| Which discrimination scale = EDS | −0.38 | 0.351 | −0.046 | 0.386 | −0.069 | 0.307 | 2.141 | 0.049 * |
| Religion: Discrimination (interaction) | −0.509 | 0.219 | −0.075 | 0.162 | −0.065 | 0.346 | 1.125 | 0.307 |
| Familism Support: Discrimination (interaction) | 0.43 | 0.611 | 0.153 | 0.163 | 0.021 | 0.88 | −1.926 | 0.392 |
| Familism Obligation: Discrimination (interaction) | 0.796 | 0.256 | 0.156 | 0.086 • | 0.062 | 0.597 | 3.792 | 0.043 * |
| Familism Referent: Discrimination (interaction) | −0.441 | 0.502 | −0.179 | 0.035 * | 0.038 | 0.725 | −2.677 | 0.126 |
| Respect: Discrimination (interaction) | 0.232 | 0.762 | −0.065 | 0.509 | −0.03 | 0.817 | −1.872 | 0.359 |
| Material Success: Discrimination (interaction) | 0.761 | 0.186 | 0.13 | 0.08 • | 0.018 | 0.847 | 0.672 | 0.66 |
| Independence and Self-Reliance: Discrimination (interaction) | −0.497 | 0.299 | 0.005 | 0.935 | −0.111 | 0.166 | 1.559 | 0.221 |
| Traditional Gender Roles: Discrimination (interaction) | −0.564 | 0.182 | −0.036 | 0.515 | 0.024 | 0.728 | 0.066 | 0.953 |
| Competition and Personal Achievement: Discrimination (interaction) | −0.348 | 0.447 | −0.115 | 0.052 • | −0.053 | 0.485 | 1.166 | 0.338 |
Caption: Model fitting statistics: PSS model: Multiple R2=0.17, F(22.0, 256.0)=2.46, p=0.0004 ***, Bonferroni adjusted p=0.0018 **
STAI model: Multiple R2=0.14, F(22.0, 256.0)=1.97, p=0.0072 **, Bonferroni adjusted p=0.0289 *
EPDS model: Multiple R2=0.20, F(22.0, 256.0)=2.90, p=<0.0001 ****, Bonferroni adjusted p=0.0001 ***
OHQ model: Multiple R2=0.23, F(22.0, 256.0)=3.41, p=<0.0001 ****, Bonferroni adjusted p=<0.0001 ****
Acculturation Status and Mental Health
Separate multiple regression models were fitted to measure how acculturation relates to each of the four mental health outcomes, all of which were significant after Bonferroni correction (Table 2; Figure 1, Panel A). In the perceived stress model, only American cultural orientation was significant after adjusting for the effects of the other predictors, exhibiting a negative correlation (β = −0.555, p = 0.023). In the depression model, only discrimination was significantly positively correlated after adjusting for the effects of the other predictors (β= 0.714, p = 0.039). In the happiness model, both greater American cultural orientation (β = 1.771, p = 0.008) and greater Latino cultural orientation (β = 1.334, p = 0.071, borderline) were associated with greater happiness after adjusting for the effects of the other predictors. To contextualize the magnitude of these effects, Campos et al. (2007) found that ARSMA-II MOS was significantly correlated with PSS with R2 of 0.008, and Barcelona de Mendoza et al. (2016) found that Psychological Acculturation Scale score was significantly correlated with STAI with β of −0.55.
FIGURE 1.
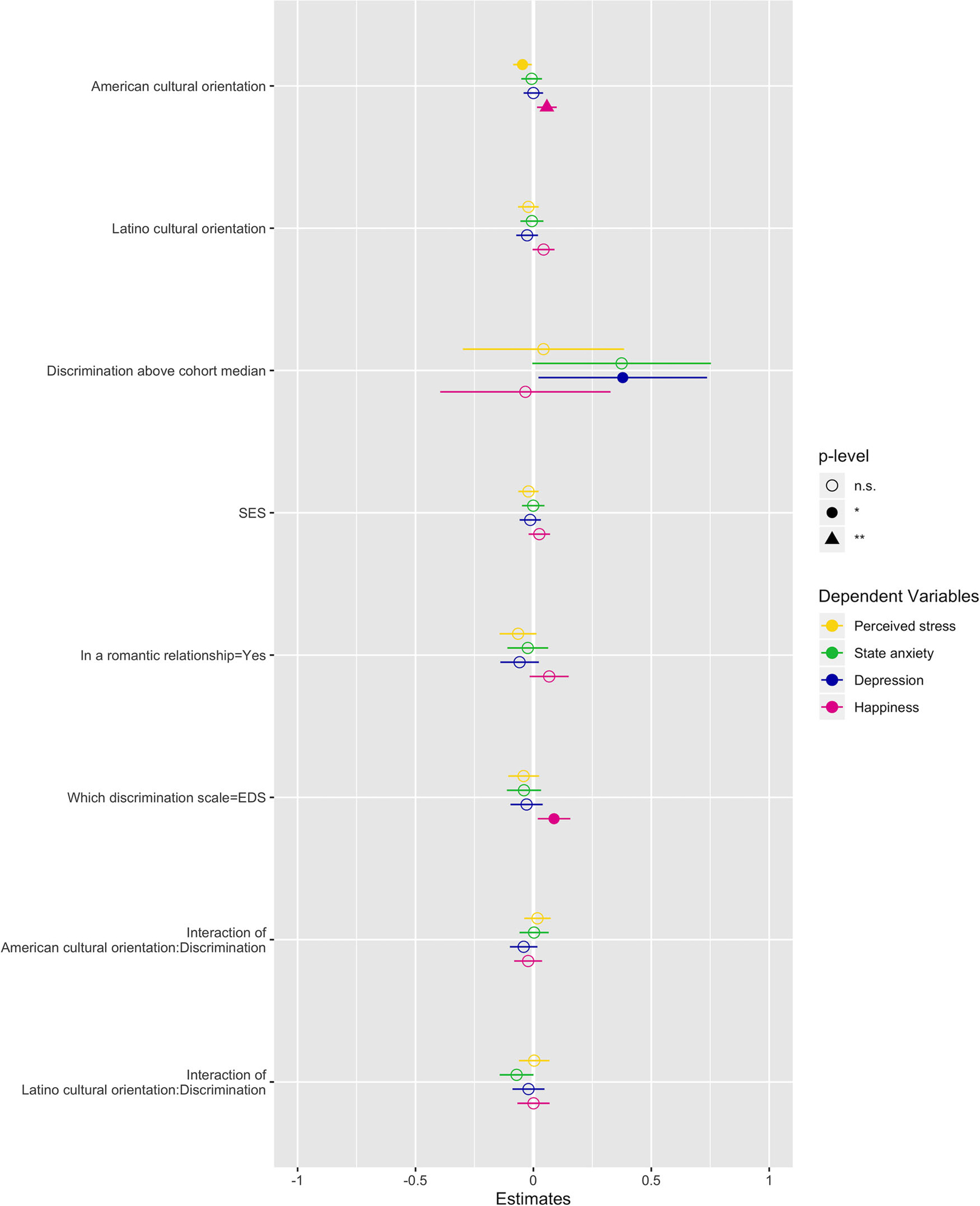
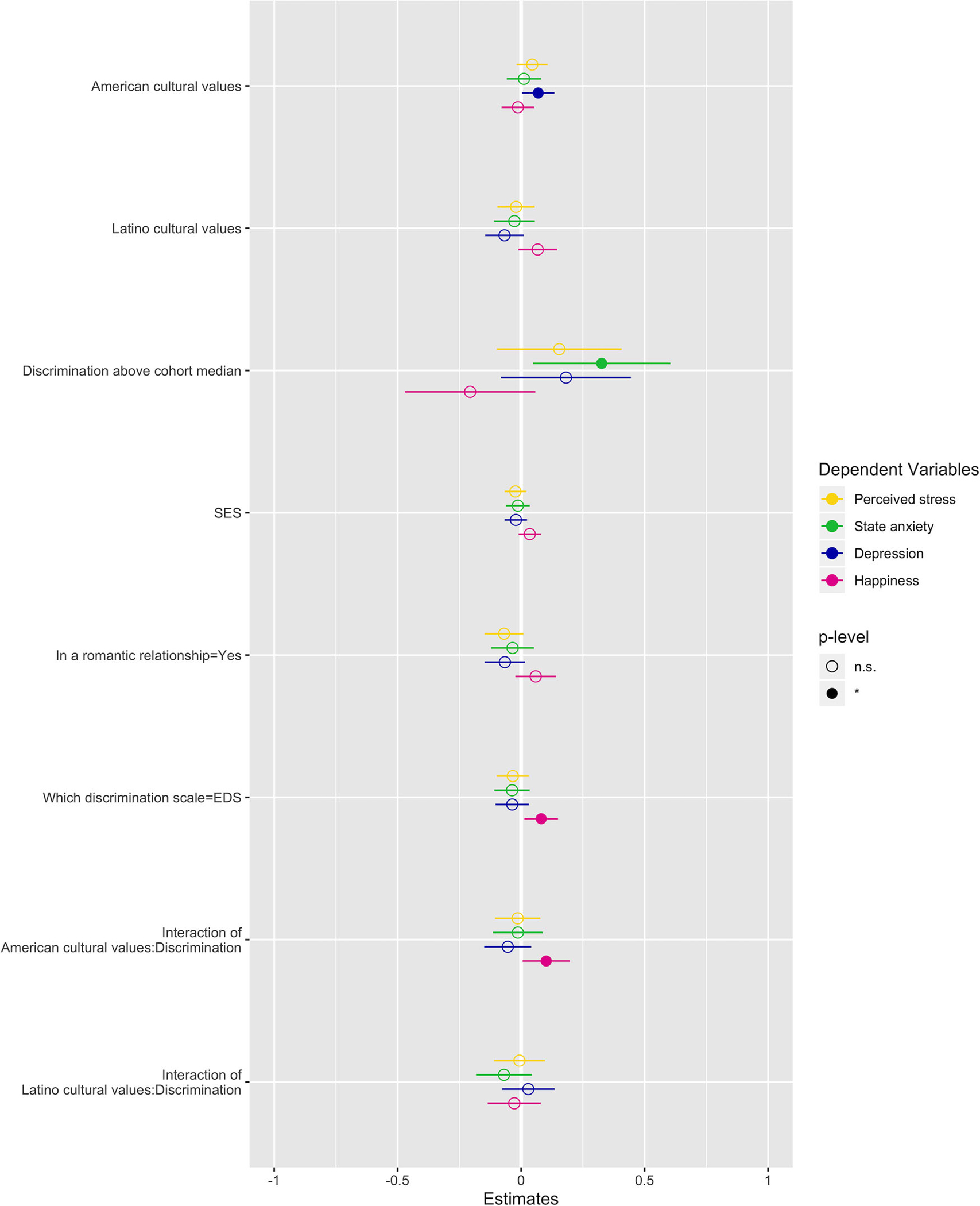
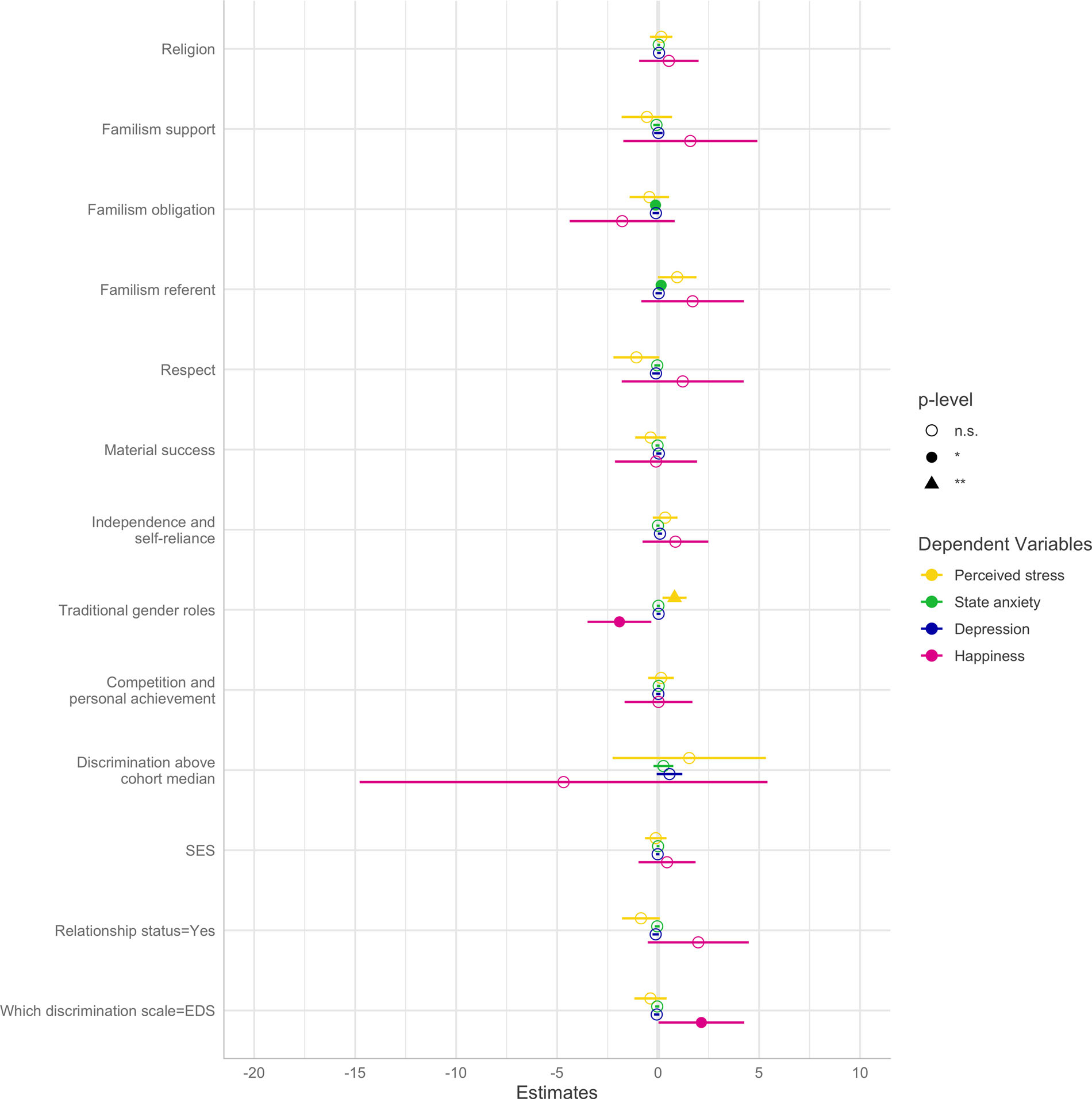
Marginal effects of coefficients for multiple regression models. Visualizations of the coefficients and p-values for the four mental health outcome models using (A) cultural orientation, (B) cultural values systems, and (C) cultural values items as predictors, in addition to control variables. For visualization purposes only, dependent variables were normalized by unitization with zero minimum in order to plot effect sizes together. Numeric information and model fitting statistics are in Tables 2–4.
For state anxiety, there was evidence of a potential interaction between Latino cultural orientation and discrimination (p = 0.053). A plot of the marginal effects and calculations of simple slopes shows how Latino cultural orientation was associated with lower anxiety only for the cohort subset above median discrimination, whereas there was no apparent relationship between Latino cultural orientation and anxiety for the cohort subset below median discrimination (Figure 2, Panel A; Table S3).
FIGURE 2.
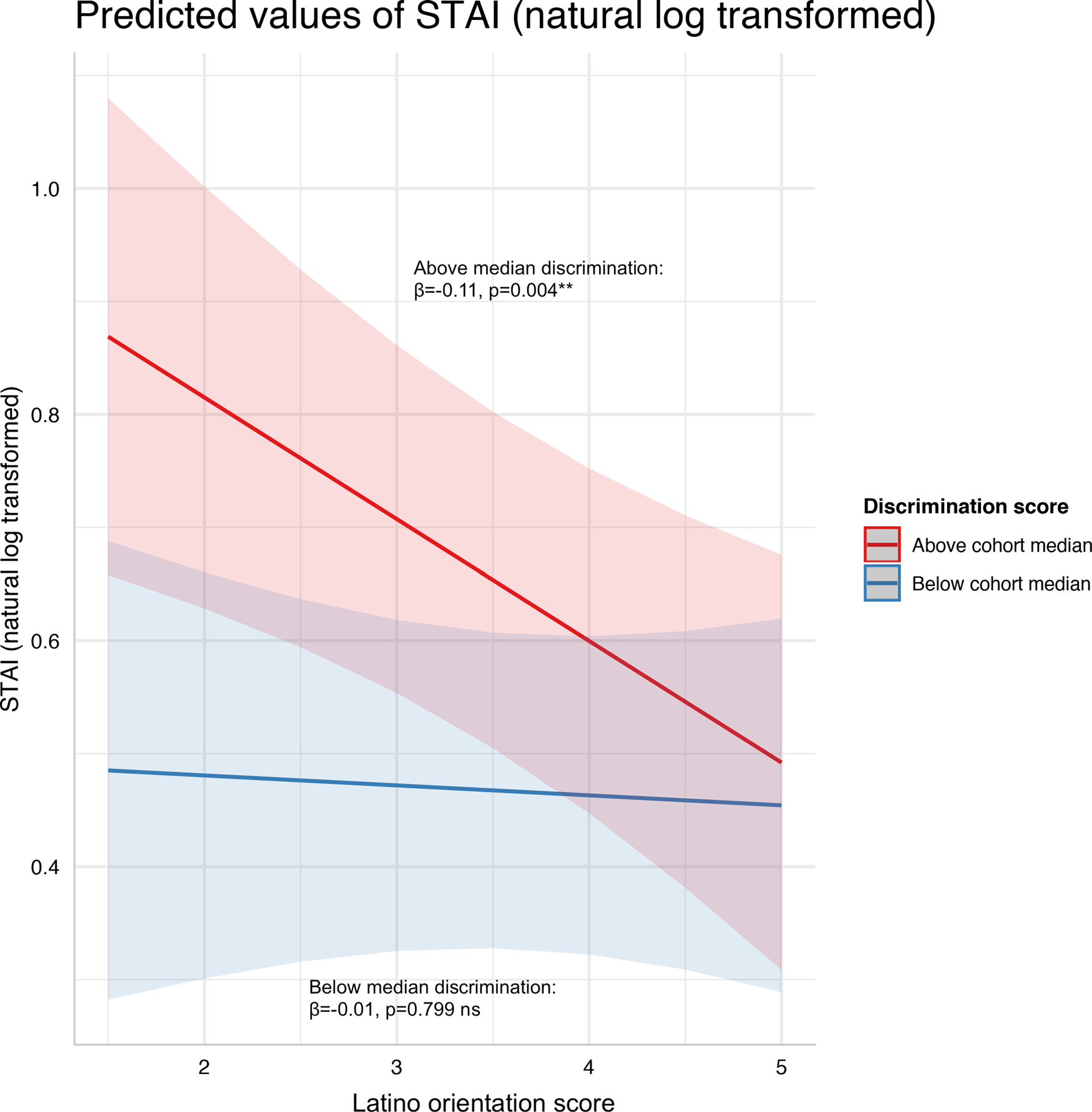
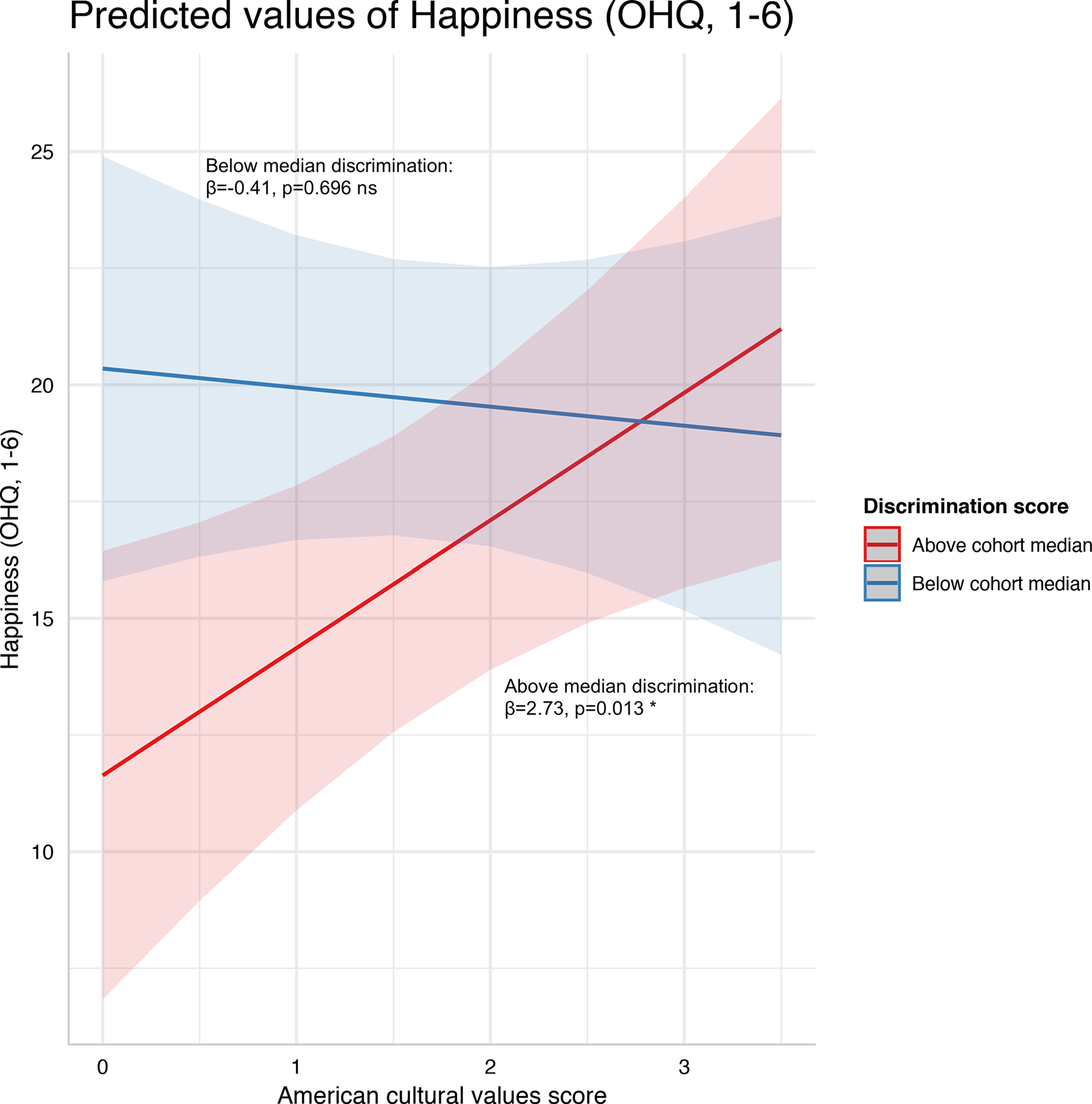
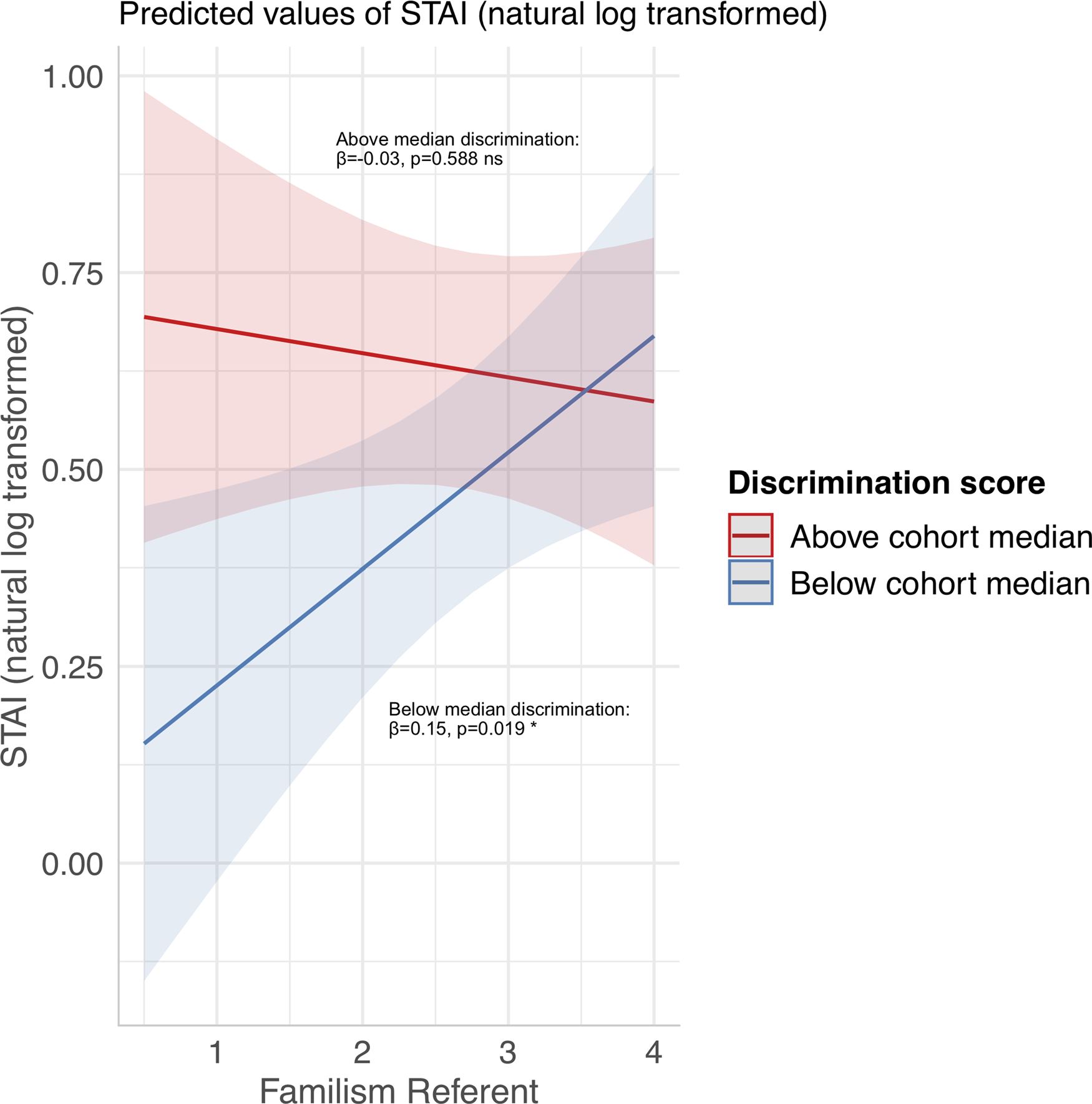
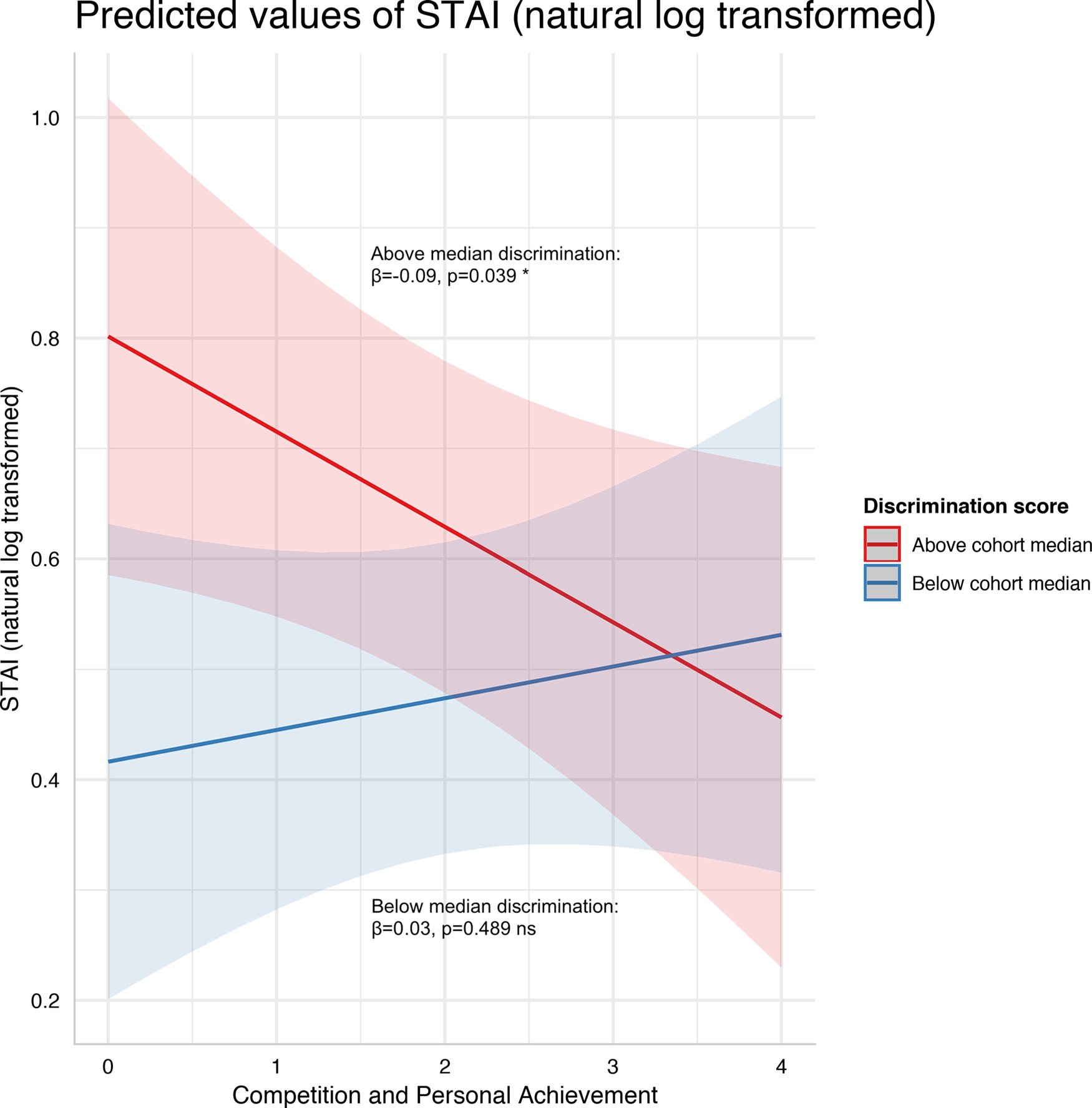
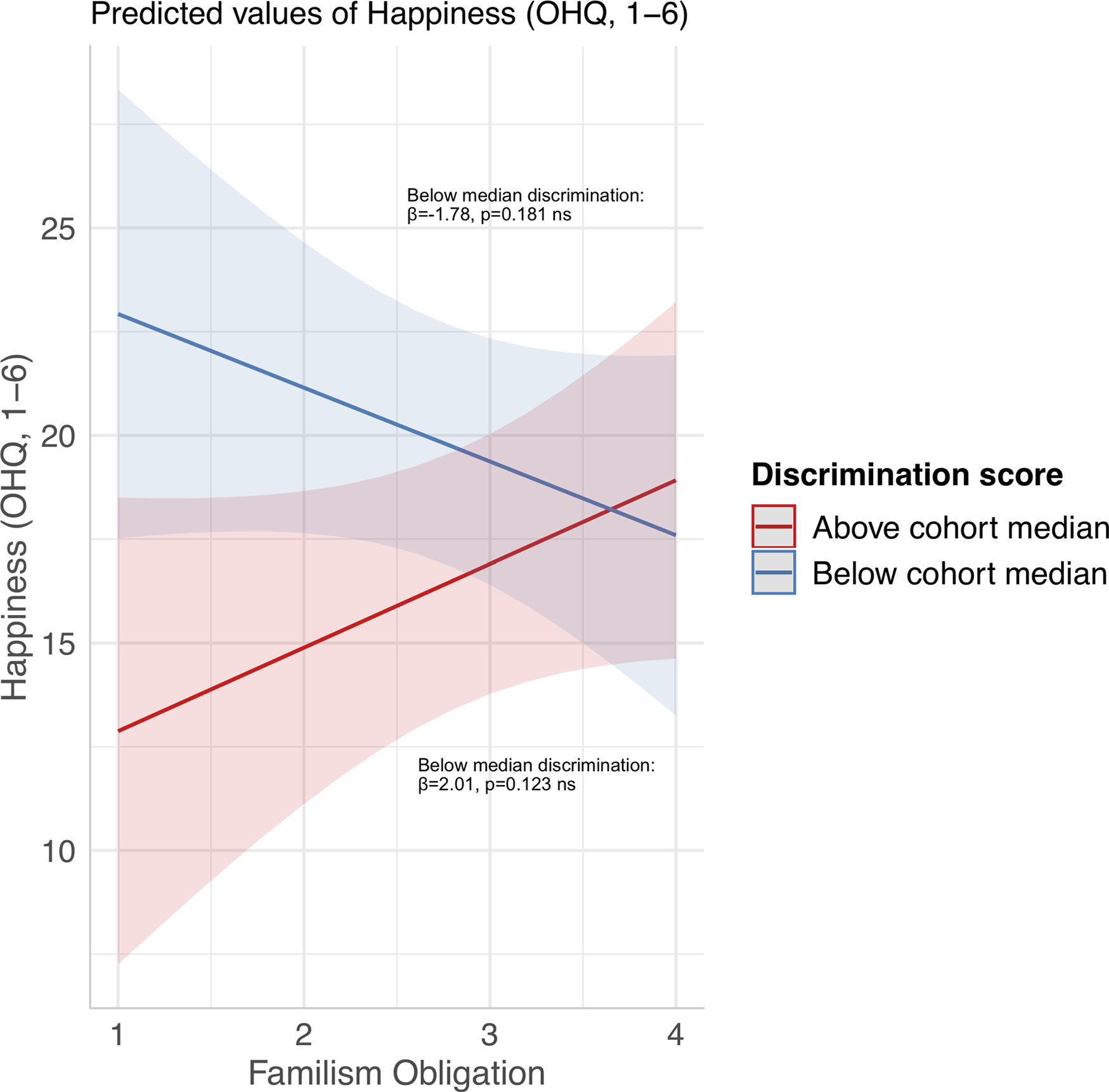
Moderating effects of discrimination. Marginal effect from multiple linear regression models of (A) Latino orientation score on anxiety score, (B) American cultural values score on happiness score,(C) familism referent values score on anxiety score,(D) Competition and personal achievement values score on anxiety score, and (E) familism obligation values score on happiness score. Data subsetted by cohort median discrimination scores. Shading represents 95 percent confidence interval. Simple slope beta coefficients and p-values are noted on the plots. ns: p>0.05 *p<0.05 **p<0.01.
Together, these results suggest that different cultural orientations predict differential mental health outcomes, and the relationships with anxiety were moderated by discrimination. Results leave open the question of what it is about acculturation status that is connected to mental health in a way that may sometimes be altered by discrimination. The role of cultural values is addressed in the next set of models.
Cultural Value Systems and Mental Health
Separate multiple regression models were fitted to measure how cultural values systems relate to each of the four mental health outcomes, all of which were significant after Bonferroni correction (Table 3; Figure 1, Panel B). In the perceived stress model, no variables of interest contributed significant effects to the model fitting. In the state anxiety model, only discrimination contributed a significantly positive predictive effect after adjusting for the effects of the other predictors (β = 0.452, p = 0.022). In the depression model, only American cultural values was a significantly positive predictor after adjusting for the effects of the other predictors (β = 0.131, p = 0.04) and Latino cultural values contributed a borderline significant effect in the negative direction (β = −0.127, p = 0.093).
TABLE 3.
Multiple regression models reflecting how cultural values systems relate to mental health outcomes
| Stress (PSS) |
Anxiety (STAI) |
Depression (EPDS) |
Happiness (OHQ) |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictor | β | p | β | p | β | p | β | p |
|
| ||||||||
| Intercept | 5.821 | <0.0001 **** | 0.582 | <0.0001 **** | 1.979 | <0.0001 **** | 12.958 | <0.0001 **** |
| American cultural values | 0.537 | 0.167 | 0.016 | 0.749 | 0.131 | 0.04 * | −0.408 | 0.696 |
| Latino cultural values | −0.247 | 0.593 | −0.038 | 0.519 | −0.127 | 0.093 • | 2.077 | 0.096 • |
| Discrimination = Above cohort median | 1.855 | 0.232 | 0.452 | 0.022 * | 0.342 | 0.177 | −6.391 | 0.127 |
| SES | −0.28 | 0.296 | −0.018 | 0.589 | −0.04 | 0.36 | 1.085 | 0.133 |
| In a romantic relationship = Yes | −0.83 | 0.087 • | −0.048 | 0.433 | −0.124 | 0.117 | 1.826 | 0.162 |
| Which discrimination scale = EDS | −0.406 | 0.309 | −0.051 | 0.314 | −0.068 | 0.297 | 2.516 | 0.02 * |
| American cultural values : Discrimination (interaction) | −0.17 | 0.763 | −0.018 | 0.797 | −0.102 | 0.267 | 3.141 | 0.039 * |
| Latino cultural values : Discrimination (interaction) | −0.08 | 0.899 | −0.096 | 0.231 | 0.055 | 0.594 | −0.858 | 0.614 |
Caption: Model fitting statistics: PSS model: Multiple R2=0.09, F(8.0, 270.0)=3.47, p=0.0008 ***, Bonferroni adjusted p=0.0032 **
STAI model: Multiple R2=0.09, F(8.0, 270.0)=3.30, p=0.0013 **, Bonferroni adjusted p=0.0052 **
EPDS model: Multiple R2=0.16, F(8.0, 270.0)=6.29, p=<0.0001 ****, Bonferroni adjusted p=<0.0001 ****
OHQ model: Multiple R2=0.13, F(8.0, 270.0)=4.97, p=<0.0001 ****, Bonferroni adjusted p=<0.0001 ****
For happiness, only Latino cultural values contributed a borderline significant positive effect (β = 2.077, p = 0.096). Additionally, there was evidence of interaction between American cultural values and discrimination (p = 0.039). A plot of the marginal effects helps visualize how American cultural values was associated with greater happiness only for the cohort subset above median discrimination, whereas there was no apparent relationship between American cultural values and happiness for the cohort subset below median discrimination (Figure 2, Panel B; Table S4).
To contextualize the magnitude of these effects, among cohorts of Mexican American adolescents, Berkel et al. (2010) found in their structural equation model that Latino cultural values was significantly associated with externalizing (β = −0.20) and internalizing symptoms (β = −0.11) (Diagnostic Interview Schedule for Children).
Cultural Value Items and Mental Health
Separate multiple regression models were fitted to measure how cultural values items related to each of the four mental health outcomes, all of which were significant after Bonferroni correction (Table 4; Figure 1, Panel C). In the perceived stress model, only traditional gender roles values was a significantly positive predictor after adjusting for the effects of the other predictors (β = 0.814, p = 0.008), and two other values contributed borderline significant effects. In the state anxiety model, familism obligation was associated with less state anxiety (β = −0.129, p = 0.046) and familism referent was associated with greater state anxiety (β = 0.148, p = 0.019). Also, there was a significant interaction between familism referent and discrimination (β = −0.179, p = 0.035) and a borderline significant interaction of competition and personal achievement with discrimination (β = −0.115, p = 0.052). In the depression model, two predictors had borderline significant positive effects: independence and self-reliance (β = 0.093, p = 0.076) and discrimination above cohort median (β = 0.564, p = 0.082). In the happiness model, more-traditional gender roles values was associated with lower happiness (β = −1.915, p = 0.018), and there was a significant interaction of familism obligation with discrimination (β = 3.792, p = 0.043). To contextualize the magnitude of these effects, among a cohort of Mexican American adolescents, Gonzales et al. (2008) found the Externalizing Behaviors subscale of the Youth Self Report Scale was significantly correlated with MACVS subscales familism support (r = −0.18), familism obligation (r = 0.11), and religious values (r = −0.08).
Plots of the marginal effects help visually clarify the interactions. For state anxiety, familism referent values was associated with greater anxiety only for the cohort subset below median discrimination, whereas there did not appear to be an effect for the subset above median discrimination (Figure 2, Panel C; Table S5). Also for state anxiety, competition and personal achievement values was associated with lower state anxiety only for the cohort subset above median discrimination (Figure 2, Panel D; Table S5). For happiness, familism obligation values appears to exert opposite effects, associated with greater happiness for the cohort subset above median discrimination and less happiness for the cohort subset below median discrimination, although these effects were not significant (Figure 2, Panel E; Table S6).
DISCUSSION
Acculturation and Cultural Values
In our cohort, acculturation status exhibited associations with mental health such that both American and Latino cultural orientations were linked with certain benefits. American cultural orientation was associated with lower perceived stress and greater happiness. Latino cultural orientation was borderline associated with greater happiness and was associated with lower anxiety for the cohort subset above median discrimination. These observations are partially consistent with previous studies of Latina pregnant women that found Latino cultural orientation (ARSMA-II MOS) correlated with lower stress (PSS) but greater pregnancy anxiety (Campos et al. 2007) and that bicultural orientation (Psychological Acculturation Scale) was associated with lower state anxiety (STAI) (Barcelona de Mendoza et al. 2016). Our results contrast with previous studies of pregnant Latina women that observed American cultural orientation was correlated with greater stress (PSS) (Campos et al. 2007; Ruiz, Dolbier, and Fleschler 2006), anxiety (STAI) (Barcelona de Mendoza et al. 2016), and depression (Beck Depression Inventory) (Walker et al. 2012) (CES-D) (Heilemann et al. 2004; Martinez-Schallmoser, Telleen, and Macmullen 2003). Others observed no correlations between acculturation and depression among pregnant (D’Anna-Hernandez, Aleman, and Flores 2015) or anxiety among pregnant up to five-years-postpartum (Cordero and Kurz 2006) Latina women, the former using the ARSMA-II and CES-D and the latter using the Short Acculturation Scale for Hispanics and the Patient Health Questionnaire.
The Latino paradox describes how Latino Americans exhibit health outcomes better than expected based on SES (Fox et al. 2015), and the Latina paradox describes the same issue focused on birth outcomes (Fleuriet and Sunil 2015). Our ability to address these paradoxes is limited because we do not compare Latinos with other ethnic groups. However, our results suggest evidence of cultural resilience, discussed below, which could help explain better Latino mental health despite social adversity.
The Latino acculturation paradox describes how first-generation Latino Americans exhibit better health than subsequent generations, particularly for mental health, birth outcomes, obesity, and type 2 diabetes. The prevailing explanation for this trend has been that acculturation endues toxic effects on health via the loss of protective traditional Latino values and behaviors and the adoption of unhealthy American values and behaviors. Consistent with our observation that Latino cultural orientation was linked with mental health benefits but contrary to our observation that American cultural orientation was also linked with mental health benefits, previous studies among nonpregnant Latino cohorts report that acculturation is generally associated with greater psychological stress, eating disorder symptoms, and depression, reviewed elsewhere (Abraído-Lanza et al. 2006; Koneru et al. 2007).
Cultural values systems have been suggested as a partial explanation for acculturation’s effect on mental health (Umaña-Taylor, Updegraff, and Gonzales-Backen 2011). We found that the American cultural values system was positively correlated with depression and the Latino cultural values system was borderline correlated negatively with depression and positively with happiness, consistent with the possibility of an explanatory mechanism linking acculturation with depression, although we did not observe a relationship with acculturation in our cohort. We did not find relationships between cultural values systems and perceived stress or state anxiety. However, particular cultural values items exhibited significant relationships with stress and anxiety. Specifically, we observed that more-traditional gender roles were associated with greater perceived stress and lower happiness and that familism obligation was associated with less and familism referent with greater state anxiety.
Previous studies of cultural values and depression among pregnant and postpartum Latina populations can lend context to our results. Among a cohort of first-trimester pregnant Mexican American women, D’Anna-Hernandez, Aleman, and Flores (2015) found that none of the nine MACVS cultural values items were correlated with depression (CES-D). However, similar to our finding that the Latino cultural values system was borderline correlated negatively with depression, D’Anna-Hernandez, Aleman, and Flores found that the traditionally Latino cultural value of respect was negatively correlated with depression, but only among those who exhibited high levels of acculturative stress. Similar to our finding that the American cultural values system (significantly) and independence and self-reliance (borderline) were positively correlated with depression, D’Anna-Hernandez, Aleman, and Flores found that independence and self-reliance were positively correlated with depression, but only among those who exhibited low levels of acculturative stress. Heilemann et al. (2004) found that a composite variable that included independence and self-reliance was negatively correlated with depression (CES-D) among postpartum Mexican American women and exhibited no significant relation to depression among the pregnant group.
Familism is an aspect of cultural values that should be highlighted for its relevance during pregnancy and postpartum, its prevalence in Latino cultures, and its importance in our findings. Familism is a construct that reflects loyalty and attachment toward kin and reliance on kin for support (Marín and Gamba 2003). Based on their focus group analysis, Knight et al. (2010) deconstructed Latino familism into three subscales that reflect the desire to have close emotional relationships with kin as familism support, valuing tangible support to kin as familism obligation, and behaving in ways that are consistent with expectations of kin and defining oneself communally with kin as familism referent.
Previous studies in nonpregnant Latino populations found benefits of familism values for many behavioral and mental health outcomes, reviewed elsewhere (Katiria Perez and Cruess 2014). Familism values may provide social resources to help individuals cope with stressors (Corona et al. 2017). Interestingly, some evidence suggests that the beneficial effects of familism on mental health may be stronger for females than males among Latino populations (Corona et al. 2017; Lorenzo-Blanco et al. 2012; Morcillo et al. 2011).
Familism has exceptional relevance during the perinatal life phase given the physical, financial, and logistical reliance a woman may have on her family during pregnancy and postpartum. Previous studies have demonstrated that aspects of familism can induce both beneficial and harmful influences on maternal mental health and childrearing among Latina mothers (Calzada, Tamis-LeMonda, and Yoshikawa 2013), aligned with our observations of both positive and negative relationships with mental health outcomes. A qualitative study found bi-directional effects of familism related to financial assistance/strain, parenting assistance/conflict, and emotional protections/pressures (Calzada, Tamis-LeMonda, and Yoshikawa 2013).
We observed familism referent correlated with greater state anxiety. Converse to our finding of mental health detriment, one study found that familism referent was correlated with less depression (CES-D) among Mexican American adolescents (Zeiders et al. 2013). Other studies demonstrate that in the context of family strife, familism may be harmful for mental health (Hernández, Ramírez García, and Flynn 2010). While we did not find an effect for familism support, others have found benefits of familism support for mental health in Latino cohorts, e.g., depression (CES-D) (Zeiders et al. 2013), anxiety, and perceived stress (Depression, Anxiety, and Stress Scale) (Corona et al. 2017).
Our results indicated that familism obligation was associated with lower state anxiety. It is plausible that family obligation reaps benefits during this phase, with families that exhibit high levels of obligation toward each other more likely to provide the needed tangible support. We only found this benefit for anxiety, which would be consistent with the possibility that worries about tangible and logistical needs are alleviated by familism obligation values. Conversely, previous studies generally observe mental health detriments associated with familism obligation. A study among adolescent Latina and African American girls who experienced negative life events found that familism obligation was associated with greater post-traumatic stress disorder and depression (Adolescent Psychopathology Scale) (Milan and Wortel 2015), a study among white and African American adult caregivers found that familism obligation was associated with greater avoidant coping (Sayegh and Knight 2010), and a study among Spanish caregivers found that familism obligation was associated with greater depression (CES-D) and dysfunctional thoughts (Losada et al. 2010).
Gender-role beliefs are another aspect of cultural values that should be highlighted for their relevance during pregnancy and postpartum, unique manifestation in Latino cultures, and importance in our findings. In Latino culture, traditional gender roles include both values that might be expected to have deleterious effects on maternal mental health, such as subservience to males, and values that might be expected to have beneficial effects on maternal mental health, such as importance of motherhood (Galanti 2003). The MACVS subscale includes items reflecting both of these elements (e.g., “Men should earn most of the money for the family so women can stay home and take care of the children and the home.”) Therefore, we did not have a priori predictions about the directionality of relationships between traditional gender roles and maternal mental health.
Our results indicated that more-traditional gender roles were associated with greater perceived stress and lower happiness. Our observed negative relationships with mental health are compatible with a qualitative study of pregnant Latina women in California: the urban cohort subset expressed progressive gender role ideologies aligned with the structure of their surroundings that allow for childcare options outside the home and women’s equal participation in wage labor (Guendelman et al. 2001). Potentially, traditional gender preferences in conflict with these local norms could lead to psychological distress, as we observed. Our results are consistent with previous studies in nonpregnant Latino populations. For example, Latina adolescents exhibited positive correlations between traditional gender role values and depression (Kessler Psychological Distress Scale) (Piña-Watson et al. 2013) (Reynolds Adolescent Depression Scale-2) (Céspedes and Huey 2008). However, in opposition to our findings, traditional gender role values have also been demonstrated to be protective against marital conflict among Mexican American families (Flores et al. 2004).
Discrimination
It is important to understand the complex role of discrimination in altering relationships between sociocultural contexts and the psychological pathway toward embodiment in order to appreciate how social inequality may be transmitted across generations (Gravlee 2009). Among the cohort subset above median discrimination, Latino cultural orientation was associated with lower state anxiety. Because our discrimination questionnaire inquired specifically about experiences related to the participant’s race or ethnicity, the moderating effect of discrimination suggests, potentially, that being more oriented toward Latino identity only benefits mental health if a person is suffering negative consequences of that identity. Torres, Driscoll, and Voell (2012) found that only among low Anglo-oriented individuals, acculturative stress mediated the relationship between discrimination and psychological distress. Together, our results with theirs underscore how the interplay between cultural orientation and discrimination may alter the sociocultural instigators of psychological distress.
Among the cohort subset above median discrimination, American cultural values was associated with greater happiness, and competition and personal achievement values was associated with lower state anxiety. Potentially, these effects could be explained such that, in the context of denigration by American communities, having more American cultural values could benefit self-esteem by encouraging affinity with the denigrators. Another possible explanation is that American cultural values (e.g., competition and personal achievement) engender resilience to the negative mental health consequences of discrimination.
We also observed that for the cohort subset below median discrimination, familism obligation was associated with lower happiness, while for the cohort subset above median discrimination, familism obligation was associated with greater happiness (although not significantly). It is possible that in the absence of cultural stressors (e.g., low discrimination), the pressures of family obligations and expectations undermine psychological well-being, but in the presence of such stressors (e.g., high discrimination), tangible support between family members garners more-useful benefits.
These observations and potential explanations may add nuance to the prevailing theory and observations that traditional Latino cultural values, particularly familism, engender resilience to stressors against anxiety (Corona et al. 2017) and other mental health problems (Katiria Perez and Cruess 2014). It may be the case that in facing discrimination stress, certain American cultural values (e.g., competition and personal achievement) and certain traditional Latino cultural values (e.g., familism obligation) can enhance mental health, even if these values do not provide benefits in the absence of discrimination.
Reproductive Habitus
The emphasis on a distinctive “reproductive habitus” was proposed by Smith-Oka (2012) to highlight how institutions, environments, and social interactions may influence women’s bodies during reproductive experiences, such as pregnancy. This concept was developed and has been thus far exclusively implemented in studies of Mexican American pregnant women (Fleuriet and Sunil 2015; Smith-Oka 2012). Our results in a similar cohort speak to this stream of scholarship by exploring how cultural values, family, and experiences of discrimination interact to potentially affect the reproductive habitus, as well as elucidate the psychological pathways by which these perturbations may occur. Upon such influence on women’s bodies, there is potential for impact on the biochemical signals to which a developing fetus is exposed. For example, different psychological states during pregnancy may correspond to alterations to the hormonal milieu, inflammatory balance, or oxidative stress in the intrauterine environment. These biochemical environments guide fetal development, shaping phenotypes (Fall 2013; Kuzawa and Gravlee 2016). Thus, an individual’s health and disease risk may be, in part, attributable to the mother’s experiences during and before pregnancy—that is, the concept of fetal programming. Our study follows calls to investigate developmental processes and intergenerational transmission of health disparities (Gravlee 2009). Here, we explored one step in this pathway (namely, how environments and experiences relate to maternal psychology), and future research should continue to elucidate the other parts of this chain of events, as well as establish timing and causality.
Resilience
Our inclusion of not only risk factors but also resilience factors in both positive and negative psychology follows calls to increase attention to resilience and examine how it is related to culture (Panter-Brick 2014). Our study cohort faces various adversities related to the interpersonal and structural challenges associated with minority ethnicity as well as pregnancy and low SES. We found that certain personal cultural resources may lend resilience, such that the Latino cultural values system had borderline evidence of resilience against depression and the familism obligation value had evidence of resilience against state anxiety. In the face of social adversity—that is, the cohort subset above median discrimination—competition and personal achievement value had evidence of resilience against state anxiety. Additionally, resilience reflects not only the absence of psychopathology but also the presence of positive outcomes in the context of adversity. We found for the cohort subset above median discrimination, American cultural values and familism obligation were associated with greater happiness.
Evolution and Maternal Psychological Adjustment
Improved understanding of how social context affects women’s psychological risk during pregnancy is crucial for elucidating the adaptation of the maternal brain in the context of humans as a cooperatively breeding species. While there is broad recognition of pregnancy as a period of developmental plasticity for the offspring, much less attention has been paid to the fact that, simultaneously, pregnancy represents a period of developmental plasticity for the mother. Particularly, maternal affective, cognitive, and social functions undergo considerable reorganization, with both short-term and long-term consequences. This phenomenon has been most extensively documented in nonhuman mammals, especially rodents, evincing the deep evolutionary roots of this system. This period of psychological reorganization comes with one of the highest risks of psychopathology onset compared to other life-history phases (Glynn, Howland, and Fox 2018). Thus, pregnancy is a period of transformation for the maternal brain during which psychological adjustment and psychopathology risk and resilience should be investigated, as we have done here. Our failure to replicate findings from nonpregnant populations—e.g., we observed benefits related to American cultural values and familism obligation, whereas studies of nonpregnant Latino populations have observed the opposite—suggests that biopsychosocial systems may respond in unique ways during pregnancy.
Social support improves mother–infant outcomes and reproductive success. This has been appreciated by evolutionary models that emphasize how “helpers at the nest” support women’s motherhood needs—that is, cooperative breeding. However, little is known about the socially contextual instigators of maternal brain adaptation and failure to enact adaptive changes. Evolutionary anthropology high-lights how maternal psychology during and after pregnancy may involve adaptations that promote the mother’s reproductive success and could help explain human vulnerability to psychopathology during this phase (Leckman and Herman 2002). Human psychological adaptations are often context-dependent (Griskevicius et al. 2009); therefore, given different cultural and social environments and access to resources, women may exhibit different facultative strategies. Our observation that tangible but not emotional support from kin was associated with reduced maternal anxiety could suggest that costly precautionary attitudes are necessary when tangible kin support is lacking.
Limitations
Our study was limited to self-report data, inherently vulnerable to bias or inaccuracy (Van de Mortel 2008). Cross-sectional data are unable to gauge change over time or child developmental outcomes. We only asked about discrimination related to ethnicity or race; thus, we cannot speak to the intersectional social identities of participants who may face discrimination due to gender, pregnancy, or other reasons. Our cohort only included women age eighteen and older and was mostly (88.2 percent) of Mexican heritage, so further research is needed to understand relevant effects in the context of adolescent pregnancy and among other subsets of the diverse Latino population. Although we did not find significant differences in mental health outcomes between pregnancy and postpartum (Table S2), other studies found differences over this period among Latinas (Luis Sanchez, Urbina, and D’Anna-Hernandez 2020; Preciado and D’Anna-Hernandez 2017). This study did not involve clinician assessments of mental health outcomes, and we used short-form versions of questionnaire instruments whenever possible in order to minimize participation fatigue, at the expense of more comprehensive assessments. Future studies should improve upon our psychological assessment techniques.
CONCLUSION
This study examined how cultural orientations and values interact with perceived discrimination to influence depression, state anxiety, perceived stress, and happiness in a cohort of Latina pregnant and postpartum women. Our results may inform understandings of how the interplay between identity, culture, and context affects human psychology. It is uniquely important to understand these processes among Latina pregnant and postpartum women because this is an underserved community facing substantial social adversity, and biopsychosocial pathways function differently during pregnancy and postpartum, so we cannot assume that research findings from Latino populations in other life-history phases can be applied to the Latina reproductive habitus. Our findings add nuance to assumptions about the health benefits and detriments of mainstream and traditional cultures and how discrimination could affect intergenerational health. This information not only could help the Latino community but also could provide a parallel example that generates research and outreach ideas for other underserved minority communities.
Supplementary Material
Acknowledgements.
The author deeply thanks the study participants and their families. The author thanks the students and volunteers of the Mothers’ Cultural Experiences Study, Kristine Chua, Delaney Knorr, and Kotrina Kajokaite. The author gratefully acknowledges Maridet Ibanez and the team at Women’s Infants and Children in Santa Ana CA, Celia Bernstein and the team at Westside Family Health Center, Lirona Katzir and the team at Olive View-UCLA Medical Center, and Yvette Bojorquez and the team at MOMS Orange County, as well as Patricia Greenfield, Gail Greendale, Rachel Brook, Janet P. Pregler, Laura M. Glynn, Curt A. Sandman, and Chris Dunkel Schetter. The author thanks the editors and anonymous reviewers for their insights and effort towards this manuscript. This study was funded by NIH National Institute of Diabetes and Digestive and Kidney Diseases K01 DK105110 and R03 DK125524 to M.F., and UCLA Center for the Study of Women Faculty Research Grant to M.F.
Discrimination as a Moderator of the Effects of Acculturation and Cultural Values on Mental Health among Pregnant and Postpartum Latina Women
Footnotes
REFERENCES CITED
- Abraído-Lanza Ana F., Armbrister Adria N., Flórez Karen R., and Aguirre Alejandra N.. 2006. “Toward a Theory-Driven Model of Acculturation in Public Health Research.” American Journal of Public Health 96 (8): 1342–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo Beverly Y., and Borrell Luisa N.. 2006. “Understanding the Link between Discrimination, Mental Health Outcomes, and Life Chances among Latinos.” Hispanic Journal of Behavioral Sciences 28 (2): 245–66. [Google Scholar]
- Barcelona de Mendoza Veronica, Harville Emily, Theall Katherine, Buekens Pierre, and Lisa Chasan-Taber. 2016. “Effects of Acculturation on Prenatal Anxiety among Latina Women.” Archives of Women’s Mental Health 19 (4): 635–44. 10.1007/s00737-016-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck Cheryl Tatano, Froman Robin D., and Bernal Henrietta. 2005. “Acculturation Level and Postpartum Depression in Hispanic Mothers.” MCN: The American Journal of Maternal/Child Nursing 30 (5): 299–304. [DOI] [PubMed] [Google Scholar]
- Berkel Cady, Knight George P., Zeiders Katharine H., Tein Jenn-Yun, Roosa Mark W., Gonzales Nancy A., and Saenz Delia. 2010. “Discrimination and Adjustment for Mexican American Adolescents: A Prospective Examination of the Benefits of Culturally Related Values.” Journal of Research on Adolescence 20 (4): 893–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry John W. 2003. “Conceptual Approaches to Acculturation.” In Acculturation: Advances in Theory, Measurement, and Applied Research, edited by Chun Kevin M, Organista Pamela Balls, and Gerardo Marín, 17–37. Washington, DC: American Psychological Association. [Google Scholar]
- Brondolo Elizabeth, Kelly Kim P., Coakley Vonetta, Gordon Tamar, Thompson Shola, Levy Erika, Cassells Andrea, Tobin Jonathan N., Sweeney Monica, and Contrada Richard J.. 2005. “The Perceived Ethnic Discrimination Questionnaire: Development and Preliminary Validation of a Community Version 1.”Journal of Applied Social Psychology 35 (2): 335–65. [Google Scholar]
- Calzada Esther J., Tamis-LeMonda Catherine S., and Hirokazu Yoshikawa. 2013. “Familismo in Mexican and Dominican Families from Low-Income, Urban Communities.” Journal of Family Issues 34 (12): 1696–724. [Google Scholar]
- Campos Belinda, Schetter Christine Dunkel, Walsh Julia A., and Schenker Marc. 2007. “Sharpening the Focus on Acculturative Change: ARSMA-II, Stress, Pregnancy Anxiety, and Infant Birthweight in Recently Immigrated Latinas.” Hispanic Journal of Behavioral Sciences 29 (2): 209–24. [Google Scholar]
- Cervantes Richard C., Gattamorta Karina A., and Jodi Berger-Cardoso. 2019. “Examining Difference in Immigration Stress, Acculturation Stress and Mental Health Outcomes in Six Hispanic/Latino Nativity and Regional Groups.” Journal of Immigrant and Minority Health 21 (1): 14–20. [DOI] [PubMed] [Google Scholar]
- Céspedes Yolanda M., and Huey Stanley J. Jr. 2008. “Depression in Latino Adolescents: A Cultural Discrepancy Perspective.” Cultural Diversity and Ethnic Minority Psychology 14 (2): 168–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobas Jose A., Balcazar Hector, Benin Mary B., Keith Verna M., and Chong Yinong. 1996. “Acculturation and Low-Birthweight Infants among Latino Women: A Reanalysis of HHANES Data with Structural Equation Models.” American Journal of Public Health 86 (3): 394–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon, Kamarck Tom, and Mermelstein Robin. 1983. “A Global Measure of Perceived Stress.” Journal of Health and Social Behavior 24 (4): 385–96. [PubMed] [Google Scholar]
- Constantine Madonna G., Alleyne Vanessa L., Wallace Barbara C., and Franklin-Jackson Deidre C.. 2006. “Africentric Cultural Values: Their Relation to Positive Mental Health in African American Adolescent Girls.” Journal of Black Psychology 32 (2): 141–54. [Google Scholar]
- Cordero Antonia, and Kurz Brenda. 2006. “Acculturation and the Mental Health of Latina Women in the Women, Infant, and Children Program.” Affilia 21 (1): 46–58. [Google Scholar]
- Corona Rosalie, Rodríguez Vivian M., McDonald Shelby E., Efren Velazquez, Adriana Rodríguez, and Fuentes Vanessa E.. 2017. “Associations between Cultural Stressors, Cultural Values, and Latina/O College Students’ Mental Health.” Journal of Youth and Adolescence 46 (1): 63–77. [DOI] [PubMed] [Google Scholar]
- Cox John L., Holden Jeni M, and Ruth Sagovsky. 1987. “Detection of Postnatal Depression:Development of the 10-Item Edinburgh Postnatal Depression Scale.” The British Journal of Psychiatry 150 (6): 782–86. [DOI] [PubMed] [Google Scholar]
- Cruise Sharon Mary, Lewis Christopher Alan, and Conor McGuckin. 2006. “Internal Consistency, Reliability, and Temporal Stability of the Oxford Happiness Questionnaire Short-Form: Test-Retest Data over Two Weeks.” Social Behavior and Personality: An International Journal 34 (2): 123–26. [Google Scholar]
- Csordas Thomas J. 1994. Embodiment and Experience: The Existential Ground of Culture and Self. Volume 2. Cambridge: Cambridge University Press. [Google Scholar]
- Cuellar Israel, Arnold Bill, and Maldonado Roberto. 1995. “Acculturation Rating Scale for Mexican Americans-II: A Revision of the Original ARSMA Scale.”Hispanic Journal of Behavioral Sciences 17 (3): 275–304. [Google Scholar]
- D’Anna-Hernandez Kimberly L., Aleman Brenda, and Flores Ana-Mercedes. 2015. “Acculturative Stress Negatively Impacts Maternal Depressive Symptoms in Mexican-American Women during Pregnancy.” Journal of Affective Disorders 176: 35–42. 10.1016/j.jad.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiPietro Janet A., Novak Matthew F. S. X., Costigan Kathleen A., Atella Lara D., and Reusing Sarah P.. 2006. “Maternal Psychological Distress during Pregnancy in Relation to Child Development at Age Two.” Child Development 77 (3): 573–87. 10.1111/j.1467-8624.2006.00891.x. [DOI] [PubMed] [Google Scholar]
- Doucerain Marina M. 2019. “Moving Forward in Acculturation Research by Integrating Insights from Cultural Psychology.” International Journal of Intercultural Relations 73:11–24. [Google Scholar]
- Dunkel-Schetter Christine. 1998. “Maternal Stress and Preterm Delivery.” Prenatal and Neonatal Medicine 3:39–42. [Google Scholar]
- Dunkel-Schetter C, and Glynn LM. 2011. “The Handbook of Stress Science: Biology, Psychology, and Health.” In Handbook of Stress Science: Biology, Psychology, and Health, edited by Contrada Rand Baum A, 321–43. New York: Springer Publishing Company. [Google Scholar]
- Engel George L. 1977. “The Need for a New Medical Model: A Challenge for Biomedicine.” Science 196 (4286): 129–36. [DOI] [PubMed] [Google Scholar]
- Fall Caroline H.D. 2013. “Fetal Programming and the Risk of Non-communicable Disease.” The Indian Journal of Pediatrics 80 (1): 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch Brian Karl, Frank Reanne, and Vega William A.. 2004. “Acculturation and Acculturation Stress: A Social-Epidemiological Approach to Mexican Migrant Farmworkers’ Health1.” International Migration Review 38 (1): 236–62. 10.1111/j.1747-7379.2004.tb00195.x. [DOI] [Google Scholar]
- Finch Brian Karl, Kolody Bohdan, and Vega William A.. 2000. “Perceived Discrimination and Depression among Mexican-Origin Adults in California.” Journal of Health and Social Behavior 41: 295–313. [PubMed] [Google Scholar]
- Flaskerud Jacquelyn H., and Uman Gwen. 1996. “Acculturation and Its Effects on Self-Esteem among Immigrant Latina Women.” Behavioral Medicine 22 (3): 123–33. 10.1080/08964289.1996.9933773. [DOI] [PubMed] [Google Scholar]
- Fleuriet K. Jill, and Sunil TS. 2015. “Reproductive Habitus, Psychosocial Health, and Birth Weight Variation in Mexican Immigrant and Mexican American Women in South Texas.” Social Science & Medicine 138:102–09. [DOI] [PubMed] [Google Scholar]
- Flores Elena, Tschann Jeanne M., Marin Barbara VanOss, and Philip Pantoja. 2004. “Marital Conflict and Acculturation among Mexican American Husbands and Wives.” Cultural Diversity and Ethnic Minority Psychology 10 (1): 39. [DOI] [PubMed] [Google Scholar]
- Flores Elena, Tschann Jeanne M., Dimas Juanita M., Bachen Elizabeth A., Pasch Lauri A., and de Groat Cynthia L.. 2008. “Perceived Discrimination, Perceived Stress, and Mental and Physical Health among Mexican-Origin Adults.” Hispanic Journal of Behavioral Sciences 30 (4): 401–24. [Google Scholar]
- Fox Molly, Entringer Sonja, Buss Claudia, Jessica DeHaene, and Wadhwa Pathik D.. 2015. “Intergenerational Transmission of the Effects of Acculturation on Health in Hispanic Americans: A Fetal Programming Perspective.” American Journal of Public Health 105 (S3): S409–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox Molly, Thayer Zaneta M., Ramos Isabel F., Meskal Sarah J., and Wadhwa Pathik D.. 2018. “Prenatal and Postnatal Mother-to-Child Transmission of Acculturation’s Health Effects in Hispanic Americans.” Journal of Women’s Health 27 (8): 1054–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox Molly, Thayer Zaneta M., and Wadhwa Pathik D.. 2017a. “Acculturation and Health: the Moderating Role of Sociocultural Context.” American Anthropologist 119 (3): 405–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox Molly, Thayer Zaneta M., and Wadhwa Pathik D.. 2017b. “Assessment of Acculturation in Minority Health Research.” Social Science & Medicine 176:123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanti Geri-Ann. 2003. “The Hispanic Family and Male-Female Relationships: An Overview.” Journal of Transcultural Nursing 14 (3): 180–85. 10.1177/1043659603014003004. [DOI] [PubMed] [Google Scholar]
- Glynn Laura M., Howland Mariann A., and Fox Molly. 2018. “Maternal Programming: Application of a Developmental Psychopathology Perspective.” Development and Psychopathology 30 (3): 905–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn Laura M., Christine Dunkel-Schetter Calvin J. Hobel, and Sandman Curt A.. 2008. “Pattern of Perceived Stress and Anxiety in Pregnancy Predicts Preterm Birth.” Health Psychology 27 (1): 43–51. 10.1037/0278-6133.27.1.43. [DOI] [PubMed] [Google Scholar]
- Gonzales Nancy A., Miguelina Germán Su Yeong Kim, George Preethy, Fabrett Fairlee C., Millsap Roger, and Dumka Larry E.. 2008. “Mexican American Adolescents’ Cultural Orientation, Externalizing Behavior and Academic Engagement: The Role of Traditional Cultural Values.” American Journal of Community Psychology 41 (1–2): 151–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravlee Clarence C. 2009. “How Race becomes Biology: Embodiment of Social Inequality.” American Journal of Physical Anthropology 139 (1): 47–57. [DOI] [PubMed] [Google Scholar]
- Griskevicius Vladas, Tybur Joshua M., Gangestad Steven W., Perea Elaine F., Shapiro Jenessa R., and Kenrick Douglas T.. 2009. “Aggress to Impress: Hostility as an Evolved Context-Dependent Strategy.” Journal of Personality and Social Psychology 96 (5): 980. [DOI] [PubMed] [Google Scholar]
- Guendelman Sylvia, Malin Christina, Barbara Herr-Harthorn, and Patricia Noemi Vargas. 2001. “Orientations to Motherhood and Male Partner Support among Women in Mexico and Mexican-Origin Women in the United States.” Social Science & Medicine 52 (12): 1805–13. [DOI] [PubMed] [Google Scholar]
- Gurven Michael, Stieglitz Jonathan, Trumble Benjamin, Blackwell Aaron D., Beheim Bret, Davis Helen, Hooper Paul, and Kaplan Hillard. 2017. “The Tsimane Health and Life History Project: Integrating Anthropology and Biomedicine.” Evolutionary Anthropology: Issues, News, and Reviews 26 (2): 54–73. 10.1002/evan.21515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn Robert A., and Inhorn Marcia Claire. 2009. “Introduction.” In Anthropology and Public Health: Bridging Differences in Culture and Society, edited by Robert A Hahn and Marcia Claire Inhorn. New York: Oxford University Press. [Google Scholar]
- Hamilton Brady E., Martin Joyce A., Osterman Michelle J. K., and Rossen Lauren M.. 2019. Births: Provisional Data for 2018. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Heilemann MarySue, Frutos Lisa, Lee Kathyrn, and Kury Felix Salvador. 2004. “Protective Strength Factors, Resources, and Risks in Relation to Depressive Symptoms among Childbearing Women of Mexican Descent.” Health Care for Women International 25 (1): 88–106. [DOI] [PubMed] [Google Scholar]
- Hernández Brenda, Ramírez García Jorge I., and Megan Flynn. 2010. “The Role of Familism in the Relation between Parent–Child Discord and Psychological Distress among Emerging Adults of Mexican Descent.” Journal of Family Psychology 24 (2): 105–14. 10.1037/a0019140. [DOI] [PubMed] [Google Scholar]
- Hertzman Clyde. 1999. “The Biological Embedding of Early Experience and Its Effects on Health in Adulthood.” Annals of the New York Academy of Sciences 896 (1): 85–95. [DOI] [PubMed] [Google Scholar]
- Hills Peter, and Argyle Michael. 2002. “The Oxford Happiness Questionnaire: A Compact Scale for the Measurement of Psychological Well-Being.” Personality and Individual Differences 33 (7): 1073–82. 10.1016/S0191-8869(01)00213-6. [DOI] [Google Scholar]
- Hoffman M. Camille, Mazzoni Sara E., Wagner Brandie D., and Laudenslager Mark L.. 2016. “Measures of Maternal Stress and Mood in Relation to Preterm Birth.” Obstetrics and Gynecology 127 (3): 545–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey Joseph D., Kim Sheena E., and Seligman Laura D.. 2006. “The Influences of Cultural Values, Ethnic Identity, and Language Use on the Mental Health of Korean American College Students.” The Journal of Psychology 140 (5): 499–511. [DOI] [PubMed] [Google Scholar]
- Hwang Wei-Chin, and Goto Sharon. 2008. “The Impact of Perceived Racial Discrimination on the Mental Health of Asian American and Latino College Students.” Cultural Diversity and Ethnic Minority Psychology 14 (4): 326–35. [DOI] [PubMed] [Google Scholar]
- Jayasvasti Kanthika, and Kanchanatawan Buranee. 2005. “Happiness and Related Factors in Pregnant Women.” Journal of the Medical Association of Thailand 88:S220–25. [PubMed] [Google Scholar]
- Joiner Thomas E., Jr Marisol Perez, Karen Dineen Wagner Abbey Berenson, and Marquina Graciela S.. 2001. “On Fatalism, Pessimism, and Depressive Symptoms among Mexican-American and Other Adolescents Attending an Obstetrics-Gynecology Clinic.” Behaviour Research and Therapy 39 (8): 887–96. [DOI] [PubMed] [Google Scholar]
- Kagawa Singer M, Dressler W, George S, and the NIH Expert Panel. 2016. “Culture: The Missing Link in Health Research.” Social Science & Medicine 170:237–46. [DOI] [PubMed] [Google Scholar]
- Karam Fatiha, Anick Bérard, Odile Sheehy, Huneau Marie-Claude, Briggs Gerald, Chambers Christina, Einarson Adrienne, et al. 2012. “Reliability and Validity of the 4-Item Perceived Stress Scale among Pregnant Women: Results from the OTIS Antidepressants Study.” Research in Nursing & Health 35 (4): 363–75. 10.1002/nur.21482. [DOI] [PubMed] [Google Scholar]
- Katiria Perez Giselle, and Dean Cruess. 2014. “The Impact of Familism on Physical and Mental Health among Hispanics in the United States.” Health Psychology Review 8 (1): 95–127. 10.1080/17437199.2011.569936. [DOI] [PubMed] [Google Scholar]
- Knight George P., Gonzales Nancy A., Saenz Delia S., Bonds Darya D., Miguelina Germán, Julianna Deardorff, Roosa Mark W., and Updegraff Kimberly A.. 2010. “The Mexican American Cultural Values Scales for Adolescents and Adults.” Journal of Early Adolescence 30 (3): 444–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koneru Vamsi K., de Mamani Amy G. Weisman, Flynn Patricia M., and Hector Betancourt. 2007. “Acculturation and Mental Health: Current Findings and Recommendations for Future Research.” Applied and Preventive Psychology 12 (2): 76–96. 10.1016/j.appsy.2007.07.016. [DOI] [Google Scholar]
- Krieger Nancy, Smith Kevin, Naishadham Deepa, Hartman Cathy, and Barbeau Elizabeth M.. 2005. “Experiences of Discrimination: Validity and Reliability of a Self-Report Measure for Population Health Research on Racism and Health.” Social Science & Medicine 61 (7): 1576–96. [DOI] [PubMed] [Google Scholar]
- Kuzawa Christopher W., and Gravlee Clarence C.. 2016. “Beyond Genetic Race: Biocultural Insights into the Causes of Racial Health Disparities.” In New Directions in Biocultural Anthropology, edited by Zuckerman Molly K. and Martin Debra L., 89–105. Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Lara-Cinisomo Sandraluz, Arianna Di Florio McKenney, and Samantha Meltzer-Brody. 2017. “Associations between Postpartum Depression, Breastfeeding, and Oxytocin Levels in Latina Mothers.” Breastfeeding Medicine 12 (7): 436–42. 10.1089/bfm.2016.0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Cinisomo Sandraluz, Girdler Susan S., Grewen Karen, and Samantha Meltzer-Brody. 2016. “A Biopsychosocial Conceptual Framework of Postpartum Depression Risk in Immigrant and U.S.-born Latina Mothers in the United States.” Women’s Health Issues 26 (3): 336–43. 10.1016/j.whi.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leckman James F., and Herman Amy E.. 2002. “Maternal Behavior and Developmental Psychopathology.” Biological Psychiatry 51 (1): 27–43. 10.1016/S0006-3223(01)01277-X. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Blanco Elma I., Unger Jennifer B., Baezconde-Garbanati Lourdes, Ritt-Olson Anamara, and Soto Daniel. 2012. “Acculturation, Enculturation, and Symptoms of Depression in Hispanic Youth: The Roles of Gender, Hispanic Cultural Values, and Family Functioning.” Journal of Youth and Adolescence 41 (10): 1350–65. 10.1007/s10964-012-9774-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada Andrés, Márquez-González María, Knight Bob G., Yanguas Javier, Sayegh Philip, and Rosa Romero-Moreno. 2010. “Psychosocial Factors and Caregivers’ Distress: Effects of Familism and Dysfunctional Thoughts.” Aging & Mental Health 14 (2):193–202. 10.1080/13607860903167838. [DOI] [PubMed] [Google Scholar]
- Sanchez Luis, Erika B, Eva Urbina, and D’Anna-Hernandez Kimberly L.. 2020. “Sociocultural Stressors across the Perinatal Period and Risk for Postpartum Depressive Symptoms in Women of Mexican Descent.” Cultural Diversity and Ethnic Minority Psychology 26 (1): 124. [DOI] [PubMed] [Google Scholar]
- MacLachlan Malcolm. 2004. Embodiment: Clinical, Critical and Cultural Perspectives on Health and Illness. Berkshire: McGraw-Hill Education. [Google Scholar]
- Marín G, and Gamba RJ. 2003. “Acculturation and Changes in Cultural Values.” In Acculturation: Advances in Theory, Measurement, and Applied Research, edited by Chun Kevin M, Organista Pamela Balls, and Gerardo Marín, 83–93. Washington, DC: American Psychological Association. [Google Scholar]
- Marteau Theresa M., and Bekker Hilary. 1992. “The Development of a Six-Item Short-Form of the State Scale of the Spielberger State—Trait Anxiety Inventory (STAI).”British Journal of Clinical Psychology 31 (3): 301–06. [DOI] [PubMed] [Google Scholar]
- Martinez-Schallmoser Lucy, Telleen Sharon, and Macmullen Nancy J.. 2003. “The Effect of Social Support and Acculturation on Postpartum Depression in Mexican American Women.” Journal of Transcultural Nursing 14 (4): 329–38. [DOI] [PubMed] [Google Scholar]
- Milan Stephanie, and Wortel Sanne. 2015. “Family Obligation Values as a Protective and Vulnerability Factor among Low-Income Adolescent Girls.” Journal of Youth and Adolescence 44 (6): 1183–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morcillo Carmen, Duarte Cristiane S., Shen Sa, Blanco Carlos, Canino Glorisa, and Bird Hector R.. 2011. “Parental Familism and Antisocial Behaviors: Development, Gender, and Potential Mechanisms.” Journal of the American Academy of Child & Adolescent Psychiatry 50 (5): 471–79. 10.1016/j.jaac.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray Lynne, and Carothers Andrew D.. 1990. “The Validation of the Edinburgh Post-Natal Depression Scale on a Community Sample.” The British Journal of Psychiatry 157 (2): 288–90. [DOI] [PubMed] [Google Scholar]
- Organista Pamela Balls, Organista Kurt C., and Kurasaki Karen. 2003. “The Relationship between Acculturation and Ethnic Minority Health.” In Acculturation: Advancesin Theory, Measurement and Applied Research, edited by Chun KM, Organista PB, and Marín G, 139–61. Washington, DC: American Psychological Association. [Google Scholar]
- Panter-Brick Catherine. 2014. “Health, Risk, and Resilience: Interdisciplinary Concepts and Applications.” Annual Review of Anthropology 43:431–48. [Google Scholar]
- Panter-Brick Catherine, and Eggerman Mark. 2018. “The Field of Medical Anthropology in Social Science & Medicine.” Social Science & Medicine 196:233–39. 10.1016/j.socscimed.2017.10.033. [DOI] [PubMed] [Google Scholar]
- Piña-Watson Brandy, Castillo Linda G., Ojeda Lizette, and Rodriguez Kimberly M.. 2013. “Parent Conflict as a Mediator between Marianismo Beliefs and Depressive Symptoms for Mexican American College Women.” Journal of American College Health 61 (8): 491–96. [DOI] [PubMed] [Google Scholar]
- Preciado Andrea, and D’Anna-Hernandez Kimberly. 2017. “Acculturative Stress Is Associated with Trajectory of Anxiety Symptoms during Pregnancy in Mexican-American Women.” Journal of Anxiety Disorders 48: 28–35. 10.1016/j.janxdis.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayburn William F. 2018. “Pregnancy: An Opportune Time to Evaluate and Treat Mental Health Disorders.” Obstetrics and Gynecology Clinics 45 (3): xiii–xiv. [DOI] [PubMed] [Google Scholar]
- Reeve Bryce B., Willis Gordon, Shariff-Marco Salma N., Nancy Breen, Williams David R., Gee Gilbert C., Margarita Alegria, Takeuchi David T., Martha Stapleton, and Levin Kerry Y.. 2011. “Comparing Cognitive Interviewing and Psychometric Methods to Evaluate a Racial/Ethnic Discrimination Scale.” Field Methods 23 (4): 397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz R. Jeanne, Dolbier Christyn L., and Robin Fleschler. 2006. “The Relationships among Acculturation, Biobehavioral Risk, Stress, Corticotropin-Releasing Hormone, and Poor Birth Outcomes in Hispanic Women.” Ethnicity and Disease 16 (4): 926–32. [PubMed] [Google Scholar]
- Santos Iná S., Matijasevich Alicia, Tavares Beatriz Franck, Barros Aluísio J. D., Botelho Iara Picinini, Catherine Lapolli, da Silva Magalhães Pedro Vieira, et al. 2007. “Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a Sample of Mothers from the 2004 Pelotas Birth Cohort Study.” Cadernos de Saúde Pública 23:2577–88. [DOI] [PubMed] [Google Scholar]
- Sawrikar Pooja, and Hunt Caroline J.. 2005. “The Relationship between Mental Health, Cultural Identity and Cultural Values in Non-English Speaking Background (NESB) Australian Adolescents.” Behaviour Change 22 (2): 97–113. [Google Scholar]
- Sayegh Philip, and Knight Bob G.. 2010. “The Effects of Familism and Cultural Justification on the Mental and Physical Health of Family Caregivers.” The Journals of Gerontology: Series B 66B (1): 3–14. 10.1093/geronb/gbq061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner Richard, and Dwyer James H.. 1989. “Acculturation and Low Birthweight among Latinos in the Hispanic HANES.” American Journal of Public Health 79 (9): 1263–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariff-Marco Salma, Breen Nancy, Landrine Hope, Reeve Bryce B., Krieger Nancy, Gee Gilbert C., Williams David R., et al. 2011. “Measuring Everyday Racial/Ethnic Discrimination in Health Surveys: How Best to Ask the Questions, in One or Two Stages, across Multiple Racial/Ethnic Groups?” Du Bois Review:Social Science Research on Race 8 (1): 159–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Oka Vania. 2012. “Bodies of Risk: Constructing Motherhood in a Mexican Public Hospital.” Social Science & Medicine 75 (12): 2275–82. [DOI] [PubMed] [Google Scholar]
- Spielberger Charles D. 1983. Manual for the State-Trait Anxiety Inventory: STAI (Form Y). Palo Alta, CA: Consulting Psychologists Press. [Google Scholar]
- Torres Lucas, Driscoll Mark W., and Voell Maria. 2012. “Discrimination, Acculturation, Acculturative Stress, and Latino Psychological Distress: A Moderated Mediational Model.” Cultural Diversity and Ethnic Minority Psychology 18 (1): 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Türk Rukiye, Sakar Tuğçe, and Erkaya Reyhan. 2017. “The Effect of Pregnancy on Happiness.” Procedia-Social and Behavioral Sciences 237:1247–53. [Google Scholar]
- Umaña-Taylor Adriana J., Updegraff Kimberly A., and Gonzales-Backen Melinda A.. 2011. “Mexican-Origin Adolescent Mothers’ Stressors and Psychosocial Functioning: Examining Ethnic Identity Affirmation and Familism as Moderators.” Journal of Youth and Adolescence 40 (2): 140–57. [DOI] [PubMed] [Google Scholar]
- Van Buuren S, and Karin Groothuis-Oudshoorn. 2010. “Mice: Multivariate Imputation by Chained Equations in R.” Journal of Statistical Software 45 (3): 1–68. [Google Scholar]
- Van de Mortel Thea F. 2008. “Faking It: Social Desirability Response Bias in Self-Report Research.” Australian Journal of Advanced Nursing 25 (4): 40. [Google Scholar]
- Walker Janiece L., Ruiz R. Jeanne, Chinn Juanita J., Nathan Marti, and Ricks Tiffany N.. 2012. “Discrimination, Acculturation and Other Predictors of Depression Among Pregnant Hispanic Women.” Ethnicity & Disease 22 (4): 497–503. [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Yu Yan, Jackson James S., and Anderson Norman B.. 1997. “Racial Differences in Physical and Mental Health: Socio-Economic Status, Stress and Discrimination.” Journal of Health Psychology 2 (3): 335–51. [DOI] [PubMed] [Google Scholar]
- Zeiders Katharine H., Updegraff Kimberly A., Umaña-Taylor Adriana J., Wheeler Lorey A., Perez-Brena Norma J., and Rodríguez Sue A.. 2013. “Mexican-Origin Youths’ Trajectories of Depressive Symptoms: the Role of Familism Values.” Journal of Adolescent Health 53 (5): 648–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman Molly K., and Martin Debra L.. 2016. “Introduction: The Development of Biocultural Perspectives in Anthropology.” In New Directions in Biocultural Anthropology, edited by Zuckerman Molly K. and Martin Debra L., 7–26. Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


