Abstract
Background
We model the potential impact of relaxing current nicotine vaping product (NVP) restrictions on public health in Australia.
Aims and Methods
A Restricted NVP Scenario was first developed to project current smoking and vaping rates, where a U.S. smoking model was calibrated to recent Australian trends. To model less restrictive NVP policies, a Permissive NVP Scenario applied rates of switching from smoking to vaping, initiation into NVP and cigarette use, and cessation from smoking and vaping based on U.S. trends. The model measures vaping risk relative to the excess mortality rate of smoking. The public health impacts are measured as the difference between smoking- and vaping-attributable deaths (SVADs) and life years lost (LYLs) in the Restricted and Permissive NVP Scenarios. Sensitivity analysis is conducted regarding the NVP excess risk and other factors.
Results
Assuming an NVP excess risk of 5% that of smoking, 104.2 thousand SVADs (7.7% reduction) and 2.05 million LYLs (17.3% reduction) are averted during 2017–2080 in the Permissive NVP Scenario compared to the Restricted NVP Scenario. Assuming 40% NVP excess risk, 70 thousand SVADs and 1.2 million LYLs are averted. The impact is sensitive to the rate at which smokers switch to NVPs and quit smoking, and relatively insensitive to the smoking initiation and NVP initiation and cessation rates.
Conclusions
The model suggests the potential for public health gains to be achieved by relaxing NVP access regulations. However, the model would benefit from better information regarding the impact of NVPs on smoking under a relaxation of current restrictions.
Implications
Australia has implemented a strong array of cigarette-oriented policies, but has restricted access to NVPs. The Smoking and Vaping Model offers a framework for modeling hypothetical policy scenarios. The Australian model shows the potential for public health gains by maintaining cigarette-oriented policies while relaxing the current restrictive NVP policy. Modeling results under a permissive NVP policy are particularly sensitive to the estimated rates of smoking cessation and switching to vaping, which are not well established and will likely depend on past and future cigarette-oriented policies and the specific NVP policies implemented in Australia.
Introduction
Australia has been a leader in tobacco control.1,2 Since the early 1970s, Australia has progressively introduced legislation to reduce the demand for cigarette smoking, including higher cigarette taxes, bans on nearly all forms of tobacco advertising, and prohibiting smoking in indoor workplaces and most public places.3 In addition, Australia was among the first country to implement a national mass media campaign, graphic health warnings (75% of the front and 90% of the back of cigarette packs), and plain packaging for cigarettes.3,4 Australia has one of the world’s highest cigarette tax rates, with annual inflation-adjusted increases of 12.5% from 2013 to 2020, resulting in prices above AUD 40 per pack (~USD 25).4,5 Collectively, these policies have been associated with significant reductions in smoking.6–9 Despite having implemented a strong array of cigarette demand-reduction policies, 12.8% of Australians (ages ≥18) still smoked daily and 14.3% smoked at least weekly in 2019.10 In addition, the relative decline in daily smoking prevalence slowed in recent years11 from 22.9% during 2007–2013 to 14.1% from 2013 to 2019.12
Australia has generally opposed smoking harm reduction policies which would encourage switching from cigarettes to potentially lower-risk alternative products such as oral tobacco and nicotine vaping; in 1991, Australia prohibited the sale of smokeless tobacco13 and access to nicotine vaping products (NVPs) have been strongly restricted since 2012.14,15 Until recently, NVPs were classified by default as “Dangerous Poisons” for nontherapeutic use (making their supply and use illegal without special authorization).16 Nicotine-free vaping products have been subject to similar regulations on public use and marketing as cigarettes.2 However, despite these strong restrictions, over 200 000 Australians were using NVPs (mainly with nicotine) in 2019,17 largely accessing them illegally via under-the-counter sales or personal importation.18 In October 2021, the legal status of NVPs in Australia shifted from dangerous poisons to prescription-only medicines as the default classification.19,20 This change allows Australians to access NVPs via a pharmacy or personal importation with a medical prescription, but harsh penalties apply to sellers for unauthorized sales and consumers who access the products without a prescription.21 Sales of NVPs remain highly restricted compared to cigarettes, which can be bought without a prescription at shops across Australia.
NVPs have been found to increase the success of quit attempts in some clinical trials and observational studies.22 In countries with less restrictive regulatory policies, NVPs have become a popular unapproved smoking cessation aid.23,24 In addition, population-level smoking among youth and young adults has declined rapidly where NVP use has increased.25–27 Studies also indicate that NVPs deliver substantially fewer toxicants than cigarettes.28,29 To the extent that NVPs are less harmful than cigarettes, their use reduces harm when used by people who would have instead initiated smoking or who would have otherwise continued smoking.30 In contrast, vaping increases harm when used by people who would not have otherwise started smoking or who would have otherwise quit smoking by other methods.30
Many countries are grappling with the task of regulating their NVP markets, with some completely banning NVPs, some placing severe restrictions on access, and others placing fewer limits on access.31 The impact of these divergent regulatory approaches on population health is unclear. While simulation modeling has been used to estimate the potential public health outcomes resulting from NVP use,32–40 limited attention has been given to the impact of relaxing restrictions on NVP use. In this paper, we apply the Smoking And Vaping Model (SAVM)38 to Australia to consider the potential public health impact of making NVPs more readily available in a highly restricted market.
Methods
The SAVM simulates the smoking and NVP histories of individual birth-cohorts, allowing for births, deaths, and transitions between smoking and NVP use.30,38 The public health impact of NVP use is estimated by comparing two simulated scenarios. First, the Restricted NVP Scenario projects baseline future cigarette use and associated mortality outcomes in Australia with a continuation of current NVP trends. Then the Permissive NVP Scenario incorporates the less restricted NVP access into cohort trajectories to project smoking and vaping prevalence if NVP products became as widely and legally accessible in Australia as they have been in the United States. Because of limited information on Australia's smoking and vaping transition rates and the mortality rates by smoking status, the Australia SAVM applies the U.S. patterns.38
The Australian SAVM begins in 2017 and tracks all birth cohorts including those born after 2017. Table 1 lists data sources and parameter values used in the Australian SAVM.
Table 1.
Data and Parameters Required for the Australia Smoking and Vaping Model
| Input parameters | Description | Data source or estimate with ranges |
|---|---|---|
| Population | Population by age, gender, and year (2017–2080) | Australian population projections UN41 |
| Mortality rates | Overall mortality rate by age, gender, and year (2017–2080) | Human Mortality Database.42 University of California, Berkeley (USA), and Max Planck Institute for Demographic Research. Exponentially extrapolated future rates using 2007–2017 trends. |
| Expected life years | Life expectancy by age, gender, and year in 2017–2080 | Human Mortality Database.42 University of California, Berkeley (USA), and Max Planck Institute for Demographic Research. Linearly extrapolated the future rates using 2007–2017 trends. |
| Smoking prevalence | Current and former smoking prevalence by age and gender for 2017/18 | Australian Bureau of Statistics, National Health Survey 2017–201812 |
| NVP relative risk multiplier | Excess mortality risk of NVP use measured relative to excess smoking risks | NVP excess mortality risks are estimated at 5%28and 40%. |
| NVP Switching rate | Rate of switching from smoking cigarettes to exclusive NVP use | 4.0% (2.5%) for ages <24, 2.5% (2%) ages 25–34, 2.5% (1.6%) ages 35–44, 1.3% (1.4%) ages 45–54, 1.2% (1.4%) ages 55–64, and 0.6% (1%) ages ≥65 , estimated from 2013 to 2017 PATH. Bounds at 50%–150% of the above rates and a 10% decay rate were considered in sensitivity analysis. |
| Smoking initiation multiplier in thePermissiveNVP Scenario | Ratio of smoking initiation rate in the Permissive NVP Scenario to smoking initiation in the Restricted NVP Scenario | 60% (30%–90%) of the Restricted smoking initiation rate,26,27,51,52as applied to never cigarette and NVP users. |
| NVP initiation multiplier in the Permissive NVP Scenario | Ratio of NVP initiation rate in the Permissive NVP Scenario to smoking initiation in the Restricted NVP Scenario | 75% (50%–200%) of the Restricted NVP smoking initiation rate,53,54as applied to never cigarette and NVP users. |
| Smoking cessation multiplier in thePermissiveNVP Scenario | Ratio of smoking cessation rate in the Permissive NVP Scenario to smoking cessation in the Restricted NVP Scenario | 100% (50%–100%) of the Restricted NVP smoking cessation rate as applied to current NVP users. |
| NVP cessation multiplier in the Permissive NVP Scenario | Ratio of NVP cessation rate in the Permissive NVP Scenario to smoking cessation in the Restricted NVP Scenario | 100% (50%–100%) of the Restricted NVP smoking cessation rate as applied to current smokers. |
NVP = nicotine vaping product; Restricted NVP Scenario refers to values under the current policy where NVP use is restricted; Permissive NVP Scenario refers to values in the assumption of less restricted NVP use.
The Restricted NVP Scenario
The Restricted NVP Scenario of the Australia SAVM first applies age- and gender-specific Australian data on yearly population for 2017–208041 and mortality rates and expected life years for 2006–2018.42 Future mortality rates and expected life years by age and gender for 2019–2080 are extrapolated based on their trends from 2007 to 2018. The mortality rate declines over time at an average annual rate of 1.88% for males and 1.64% for females at all ages. Expected life-years increase linearly with an annual male (female) growth rate, which decreases from 0.21 (0.15) at age 0 to 0.18 (0.13) at age 30, and 0.02 (0.01) at age 99.
Because Australia is in a similar stage of the tobacco epidemic as the United States,43 we use U.S. smoking initiation (scaled) and cessation rates to maintain SAVM’s age-period-cohort structure, but use Australian data to initialize and calibrate the model to recent Australian trends in smoking prevalence. Age- and gender-specific current and former smoking prevalence were obtained from 2017 to 2018 nationally-representative Australian National Health Survey (NHS),12 with a final sample size of 21 315 after removing missing data. Smoking includes cigarette, cigar, and pipe smoking. We include only daily smoking, to exclude the less stable category of infrequent (weekly or less) smoking. Among all people who smoke tobacco, 84% smoke daily at ages 18–24 increasing to 94% for ages 45 and above.
The Restricted NVP Scenario projects age- and gender- and year-specific smoking prevalence based on the Australia prevalence by smoking status in the initial year and the scaled U.S. smoking initiation and cessation rates. The U.S. rates (by single age 0–99, gender, and single year 2017–2100) were estimated by an age-period-cohort statistical model developed by the Cancer Intervention and Surveillance Modeling Network (CISNET).44–46 To reflect future trends in the absence of NVPs, these rates are based on data from the U.S. National Health Interview Surveys (NHIS) through the year 2012, before NVP use became more widespread in the United States.38 We applied CISNET initiation and cessation rates matched to the years of the Australian model beginning in 2017. Rather than distinguishing former smoking by years quit, permanent cessation is measured in terms of having quit for at least two years to reflect cessation net of relapse.
To initially scale U.S. CISNET initiation and cessation rates to Australia, we use the ratio of gender- and age-specific 2017 U.S. NHIS44 to Australian NHS12 estimates at age 15–24 (87% for males, 71% for females) for initiation and the corresponding ratio at age 25–64 to scale (119% for males, 132% for females) the cessation. The U.S. mortality rates are distinguished by smoking status after age 4047 using measures developed by the CISNET.48 We apply the ratio of the Australian and U.S. overall mortality rates to scale U.S. mortality rates by smoking status.
Past smoking prevalence trends were similar in the United States and Australia during the pre-vaping period, but we further calibrated the model to ensure that projected future trends in Australia were consistent with past Australian smoking prevalence trends. We calibrated projected trends from the model to age and gender-specific smoking prevalence rates from the nationally representative Australian National Drug Strategy Household Survey (NDSHS)17 over the time period 2001–2019. As described in Supplementary Material 1, SAVM prevalence rates for both genders fell less rapidly before age 34 and for females aged 45–54 and 55–64 and males aged 45–54, which fell more rapidly than NDSHS trends. We reduced the prevalence ratio for initiation rates to 60% for males and 50% for females before the age of 40. We applied unadjusted U.S. cessation rates for males at all ages and females before age 45, while female cessation rates at ages ≥45 were adjusted downward.
To incorporate current Australian NVP use17 despite the ban on use without a prescription, the Restricted NVP Scenario incorporates NVP use obtained from the 2019 NDSHS (see Supplementary Material 2). For ages 14 and above, the overall NVP at least weekly (daily) use was 0.3% (0.2%) among people who never smoked, and 2.7% (2.2%) and 6.2% (3.2%) among people who previously and currently smoked (respectively), with rates declining by age. Dual use is not distinguished from smoking to simplifying the model, implying comparable risks to exclusive smoking.49,50 Since SAVM treats daily smoking while using NVPs as smoking, we incorporate at least weekly exclusive NVP use among people who never and previously daily smoked: 0.4% and 4% for ages 18–24, 0.2% and 2% for those ages 25–44 and 0.1% and 1% for those aged 45–64. NVP use by people aged under 35 who previously smoked is considered NVP use and never smoking. Our measure of current NVP use under the restricted case is likely conservative, since dual use of NVPs and cigarettes encompasses 6.3% of the smoking population compared to overall NVP use in 1.7% of the total population.17 Absent information on trends, the 2019 NVP rates are assumed to stay constant for all years.
The Permissive NVP Scenario
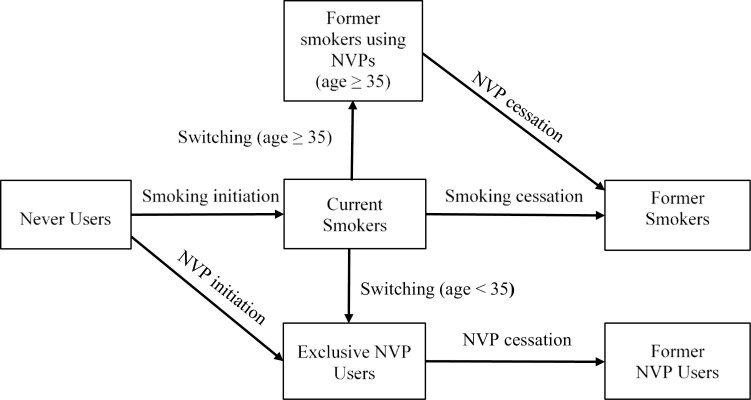
As shown in Figure 1, the Permissive NVP Scenario includes direct switching from cigarettes to exclusive NVP use, initiation into vaping and smoking, and cessation from vaping and smoking. The transition rates are primarily based on U.S. rates through 2018,38 implying a relatively unrestricted approach to NVPs. We consider transition from Australia moving from the Restricted Scenario to the Permissive NVP Scenario in 2022. As above, the transitions are to regular use.
Figure 1.
Transitions between Smoking and nicotine vaping product (NVP) Use States in the Permissive NVP Scenario.
The smoking and vaping initiation rates are both modeled using multipliers relative to the age- and gender-specific smoking initiation rates in the Restricted NVP Scenario, thus implying an age and gender pattern for initiation like those in the Restricted NVP scenario subject to a constant scaler (multiplier). A smoking initiation multiplier greater than 100% implies that smoking initiation with NVP availability is above smoking initiation in the absence of NVPs (i.e. gateway into smoking) and lesser than 100% implies being diverted away from smoking initiation. Trends in youth and young adult smoking in the United States26,27,51,52 indicate that smoking has fallen by at least 60% since 2013, when vaping became more widespread. Therefore, the smoking initiation parameter is set at 60% of the U.S. No-NVP smoking rates with a range of 30%–90%.
The NVP initiation rate multiplier converts net smoking initiation patterns into regular NVP use. Based on recent regular NVP prevalence among U.S. youth and young adults in 2017–2019,53,54 the U.S. NVP initiation has been set at 75% of smoking initiation. We keep the same multiplier for Australia's NVP initiation rates. With overall smoking prevalence by age 18 in the Restricted Scenario at about 8%, the 75% multiplier implies vaping rates of about 6%. However, we also consider a range of 50%–200%, where the upper value reflects the increases in youth vaping rates in 2017–2019 in the United States55,56 and a daily vaping rate of 5.8% in 2020/2021 in New Zealand.57
In the Permissive NVP Scenario, individuals may quit smoking and switch to exclusive NVP use. Applying prospective data from the U.S. PATH survey over 2013–2017, we estimate male (female) switching rates as 4.0% (2.5%) per year for ages under 24, 2.5% (2%) for ages 25–34, 2.5% (1.6%) for ages 35–44, 1.3% (1.4%) for ages 45–54, 1.2% (1.4%) for ages 55–64, and 0.6% (1%) for ages 65 and above. These rates are applied each year. Sensitivity analysis is conducted with a 10% annual relative decline and with rates 50% lower and 50% higher than baseline estimates.
Smoking cessation multipliers reflect those who smoke that quit both smoking and NVP use. With NVP availability, smoking cessation rates of those who do not continue to regularly vape or who quit smoking without vaping are set at 100% of the Restricted NVP smoking cessation rates with a range of 50%–150%. The NVP cessation rate measures the rate at which regular vapers quit vaping, and is set at 100% of the Restricted NVP smoking cessation rates with a range of 50%–150%.
Public Health Impacts
The public health impact of Permissive NVP use is evaluated as the difference in projected smoking- and vaping-attributable deaths (SVADs) and life-years lost (LYLs) between the Restricted and Permissive NVP Scenario. Based on previous approaches,58,59 SVADs are calculated by multiplying the number of people who currently (formerly) smoked and vaped by their excess mortality rate, measured by the current (former) smoking and vaping minus never smoking mortality rates. LYLs are calculated by multiplying the number of SVADs by the remaining life years of someone who never smoked at the same age. NVP-attributable deaths are evaluated at 5% of the excess mortality risks of smoking, based on estimates from a multi-criteria decision analysis60 and an independent review.28 People who quit smoking but currently vape are accorded the risk of former smoking plus the NVP risk multiplied by the difference in risk between current and former smokers. To reflect uncertainty around this estimate,61–63 we also consider NVP relative risks within the range of 2.5%–50% that of smoking excess risks. We also conduct sensitivity analysis of other smoking and vaping multipliers in the Permissive Scenario at fixed NVP relative risks of 5% and 40%.
Results
Comparison of Restricted NVP Scenario and Permissive NVP Scenario for All Cohorts
Table 2 presents the results by gender for all cohorts in 2017 and those born after 2017 with NVP risk at 5% of excess smoking mortality risk. We present outcomes for the short-term in 2026 and the long-term (by 2080).
Table 2.
The Australian Smoking and Vaping Model, Restricted NVP Versus Permissive NVP Scenario, 5% NVP Risks, All Cohorts With New Births, Ages 18–99, 2017–2080
| Scenario | Year | 2017 | 2021 | 2026 | 2040 | 2060 | 2080 | Cumulative* |
|---|---|---|---|---|---|---|---|---|
| Male | ||||||||
| Restricted NVP Scenario | Smokers (%) | 16.1 | 14.5% | 12.9% | 9.9% | 8.1% | 7.6% | — |
| NVP users (%) | 0.25% | 0.20% | 0.16% | 0.14% | 0.14% | 0.15% | — | |
| FS-NVP users (%) | 0.33% | 0.33% | 0.33% | 0.25% | 0.17% | 0.11% | — | |
| SVADs | 17 197 | 16 970 | 17 508 | 18 185 | 14 254 | 8922 | 986 793 | |
| LYLs | 179 806 | 181 739 | 181 506 | 162 751 | 117 637 | 72 276 | 8 882 810 | |
| Permissive NVP Scenario*** | Smokers (%) | 16.1% | 14.5% | 11.1% | 5.3% | 2.6% | 2.2% | — |
| NVP users (%) | 0.2% | 0.2% | 1.6% | 4.5% | 6.5% | 7.1% | — | |
| FS-NVP users (%) | 0.3% | 0.3% | 0.9% | 1.6% | 1.2% | 0.7% | — | |
| SVADs | 17 197 | 16 970 | 17,251 | 17 207 | 12 690 | 6670 | 913 219 | |
| LYLs | 179 806 | 181 739 | 175,831 | 142 023 | 84 073 | 32 209 | 7 356 119 | |
| Difference**** | Smokers averted(%) | — | — | 13% | 46% | 68% | 71% | — |
| SVADs averted | — | — | 258 | 978 | 1564 | 2252 | 73 574 | |
| LYLs averted | — | — | 5675 | 20 727 | 33 564 | 40 066 | 1 526 691 | |
| Female` | ||||||||
| Restricted NVP Scenario | Smokers (%) | 10.8% | 9.8% | 8.7% | 6.5% | 5.2% | 4.8% | — |
| NVP users (%) | 0.23% | 0.20% | 0.16% | 0.14% | 0.15% | 0.15% | — | |
| FS-NVP users (%) | 0.24% | 0.24% | 0.25% | 0.20% | 0.12% | 0.07% | — | |
| SVADs | 5593 | 5306 | 5497 | 6499 | 5885 | 3721 | 362 420 | |
| LYLs | 58 176 | 59 626 | 60 960 | 56 404 | 39 855 | 24 999 | 3 016 399 | |
| Permissive NVP Scenario | Smokers (%) | 10.8% | 9.8% | 7.8% | 4.0% | 2.1% | 1.7% | — |
| NVP users (%) | 0.2% | 0.2% | 0.9% | 2.5% | 3.8% | 4.2% | — | |
| FS-NVP users (%) | 0.2% | 0.2% | 0.6% | 1.0% | 0.7% | 0.5% | — | |
| SVADs | 5593 | 5306 | 5344 | 6027 | 5237 | 2949 | 331 749 | |
| LYLs | 58 176 | 59 626 | 58 248 | 48 309 | 28 594 | 12 622 | 2 488 185 | |
| Difference | Smokers averted (%) | — | — | 11% | 38% | 59% | 64% | — |
| SVADs averted | — | — | 153 | 473 | 648 | 772 | 30 671 | |
| LYLs averted | — | — | 2712 | 8096 | 11 262 | 12 378 | 528 213 | |
| Both genders | ||||||||
| Difference | SVADs averted | — | — | 411 | 1,451 | 2212 | 3023 | 104 245 |
| LYLs averted | — | — | 8387 | 28 823 | 44 826 | 52 444 | 2 054 904 | |
| SVADs averted (%) | — | — | 1.8% | 5.9% | 11.0% | 23.9% | 7.7% | |
| LYLs averted (%) | — | — | 3.5% | 13.2% | 28.5% | 53.9% | 17.3% | |
Abbreviations: NVP = nicotine vaping product, LYL = Life years lost, SVADs = smoking and vaping attributable deaths.
*Cumulative results include the deaths and life-years lost, which are the sum of attributable deaths or life-years lost over the years 2017–2080.
**Restricted NVP Scenario refers to values in the assumption of restricted NVP use.
***Permissive NVP Scenario refers to values relative to less restricted NVP use.
****Difference between the Restricted NVP Scenario and Permissive NVP Scenario includes the percent averted smokers (measured by the relative reduction in the smoking prevalence each year) by gender, averted SVADs, and LYLs for males, females, and both genders. The relative differences (%) of averted SVADs and LYLs are also available for both genders by using formulas:
SVADs averted (%) = SVAD averted/SVADRestricted NVP; LYLs averted (%) = LYL averted/LYLRestricted NVP.
In the Restricted NVP Scenario, adult male smoking prevalence is projected to decline from 16.1% in 2017 to 12.9% in 2026 and 7.6% in 2080. Female smoking prevalence declines from 10.8% in 2017 to 8.7% in 2026 and 4.8% in 2080. Male and female exclusive NVP use and former smokers using NVPs remain under 0.3% of the population. From 2017 to 2080, SAVM projects 0.99 (0.36) million male (female) SVADs with 8.9 (3.0) million male (female) LYLs due to smoking and vaping.
In the Permissive NVP Scenario, male smoking prevalence declines to 11.1% by 2026, a relative decline of 13% below that of the Restricted NVP Scenario, while female rates over the same period decline to 7.8%, an 11% relative decline. By 2080, male smoking declines to 2.2%, a 71% relative decline while female smoking declines to 1.7%, a 64% relative decline. Exclusive NVP prevalence for males and females increases to 1.6% and 0.9% in 2026 and to 7.1% and 4.2% in 2080, with similar percentages of those who were newly initiated and those who switched from current smoking before age 36. Prevalence of current vaping among people who quit smoking remains low, for example, from 0.3% in 2017 to 0.7% in 2080 for males, since most people quit smoking before age 35 and thus are classified as never smoking because of the reduced mortality risk. From 2017 to 2080, a total of 0.91 million male and 0.33 million female SVADs and 7.4 male and 2.5 million females LYLs are projected.
The public health impact in terms of averted SADs (LYL) increases from about 1500 (29 000) in 2040 to 2200 (45 000) in 2060 to 3000 (52 400) in 2080. From 2021 to 2080, approximately 104.2 thousand SVADs are averted and 2.1 million life years are gained in the Permissive compared to the Restricted NVP Scenario, representing relative reductions of 7.7% in SVADs and 17.3% in LYLs.
Applying the same transition parameters, the results with the NVP risk set at 40% of excess smoking risks are shown in Supplementary Material 3. The prevalence of cigarette and NVP use changes imperceptibly even in the Permissive NVP Scenario, since the primary effect is through the deaths of NVP users who like those who smoke die at later ages. However, relative to the Restricted NVP Scenario with the same risks, public health gains decline by 5.1% to 69 700 SVADs averted and by 10% to 1.2 million LYL averted.
Sensitivity Analysis
Sensitivity analyses are shown in Table 3 for SVADs and LYLs for both genders combined for the Permissive NVP period 2021–2080, with estimates in terms of relative changes from the baseline scenario. To gauge the sensitivity to specific parameters, we show the absolute and relative difference in SVADs and LYLs, as compared to the baseline cases in the previous section.
Table 3.
Australian Smoking and Vaping Model, Averted Smoking- and Vaping-Attributable Deaths and Life Year Lost, Sensitivity Analysis, 5% Versus 40% NVP Risks, Ages 18–99, 2021–2080
| SVADs for both genders in different scenarios | |||||
|---|---|---|---|---|---|
| Scenario and parameter change | 5% NVP risk multiplier | 40% NVP risk multiplier | |||
| Restricted NVP Scenario* | Cumulative SVADs*** | Cumulative SVADs*** | – | ||
| 1 282 061 | 1 297 562 | – | |||
| Permissive NVP Scenario** | Averted SVADs | Relative Difference from best estimate**** | Averted SVADs | Relative Difference from best estimate**** | Relative Reduction % (5% vs. 40% risk) |
| Best estimate (initial) | 104 245 | 0.0% | 69 680 | 0.0% | −33.2 |
| 50% of switch rate, no decay | 69 061 | −33.8% | 48 414 | −30.5% | −29.9 |
| 150% of switch rate, no decay | 129 702 | 24.4% | 85 027 | 22.0% | −34.4 |
| 100% of switch rate, 10% decay | 53 104 | −49.1% | 38 630 | −44.6% | −27.3 |
| 30% smoking initiation multiplier | 109 249 | 4.8% | 76 883 | 10.3% | −29.6 |
| 90% smoking initiation multiplier | 99 423 | −4.6% | 62 739 | −10.0% | −36.9 |
| 50% NVP initiation multiplier | 104 570 | 0.3% | 73 275 | 5.2% | −29.9 |
| 100% NVP initiation multiplier | 103 932 | −0.3% | 66 197 | −5.0% | −36.3 |
| 200% NVP initiation multiplier | 102 782 | −1.4% | 53 308 | −23.5% | −48.1 |
| 50% smoking cessation multiplier | 7501 | −92.8% | −35 843 | −151.4% | −577.8 |
| 150% smoking cessation multiplier | 155 355 | 49.0% | 126 510 | 81.6% | −18.6 |
| 50% NVP cessation multiplier | 100 166 | −3.9% | 39 597 | −43.2% | −60.5 |
| 150% NVP cessation multiplier | 106 376 | 2.0% | 85 629 | 22.9% | −19.5 |
| LYLs for both genders in different scenarios | |||||
| Scenario and parameter change | 5% NVP risk multiplier | 40% NVP risk multiplier | |||
| Restricted NVP Scenario* | Total LYLs | Total LYLs | – | ||
| 11 181 138 | 11 301 585 | – | |||
| Permissive NVP Scenario** with parameter changes from baseline | Averted LYLs | Relative Difference from best estimate**** | Averted LYLs | Relative Difference from best estimate**** | Relative Change % (5% risk vs. 40% risk) |
| Best estimate (initial) | 2 054 904 | 0.0% | 1 200 952 | 0.0% | −41.6 |
| 50% of switch rate, no decay | 1 416 983 | −31.0% | 805 227 | −33.0% | −43.2 |
| 150% of switch rate, no decay | 2 507 408 | 22.0% | 1 481 418 | 23.4% | −40.9 |
| 100% of switch rate, 10% decay | 1 107 582 | −46.1% | 611 860 | −49.1% | −44.8 |
| 30% smoking initiation multiplier | 2 196 320 | 6.9% | 1 409 124 | 17.3% | −35.8 |
| 90% smoking initiation multiplier | 1 919 347 | −6.6% | 1 001 312 | −16.6% | −47.8 |
| 50% NVP initiation multiplier | 2 063 920 | 0.4% | 1 305 893 | 8.7% | −36.7 |
| 100% NVP initiation multiplier | 2 046 240 | −0.4% | 1 099 627 | −8.4% | −46.3 |
| 200% NVP initiation multiplier | 2,014 839 | −1.9% | 727,948 | −39.4% | −63.9 |
| 50% smoking cessation multiplier | 1 027 310 | −50.0% | 61 274 | −94.9% | −94.0 |
| 150% smoking cessation multiplier | 2 708 277 | 31.8% | 1 937 095 | 61.3% | −28.5 |
| 50% NVP cessation multiplier | 2 000 669 | −2.6% | 780 074 | −35.0% | −61.0 |
| 150% NVP cessation multiplier | 2 088 479 | 1.6% | 1 462 870 | 21.8% | −30.0 |
Abbreviations: NVP = nicotine vaping product, LYLs = Life years lost, SVADs = smoking and vaping attributable deaths.
*Restricted NVP Scenario refers to values under the current situation with restricted NVP use.
**Permissive NVP Scenario refers to a hypothetical future scenario with more permissive policies towards NVPs. For switching rates, the sensitivity analyses are conducted as a percent of the initial switching rates from cigarette to NVP use. For the smoking and NVP initiation and cessation rates, sensitivity analyses are conducted through constant value multipliers that are applied directly to the respective smoking initiation and cessation rates in the Restricted NVP Scenario.
***Cumulative results include the deaths and life-years lost, which are the sum of attributable deaths or life-years lost over the years at age ≥18 in 2017–2080.
****Difference between the Restricted NVP Scenario and Permissive NVP Scenario includes the percent averted smokers (measured by the relative reduction in the smoking prevalence each year) by gender, averted SVADs and LYLs for males, females, and both genders. The relative differences (%) for averted SVADs and LYLs are calculated for both genders by using the formulas:.
SVADs averted (%) = SVAD averted/SVADRestricted NVP; LYLs averted (%) = LYL averted/LYLRestricted NVP.
With the NVP risk at 5% of the excess smoking risk, increasing the base case smoking initiation rate from a 60% to 90% multiplier reduces averted SVADs by 4.6% and averted LYLs by 6.6%, while a 30% multiplier increases averted SVADs by 4.8% and averted LYLs by 6.9%. Changing the NVP initiation multiplier from 75% to either 50% or 100% yields small changes in averted SVADs (0.3%) and averted LYLs (0.4%). Even with the NVP initiation multiplier at 200% (i.e., twice the smoking rate in the Restricted NVP Scenario), the percentage change in SVADs and in LYLs was still less than 2%.
Unlike the smoking and NVP initiation and NVP cessation parameters, which yield changes in SVADs and LYLs later in life, the results are sensitive to the smoking cessation multiplier and the switching rate, which change smoking behavior at all ages. A 50% increase from the 100% multiplier yields 49.0% higher averted SVADs and 31.8% higher LYLs, while reducing by 50% reduces averted SVADs by 92.8% and averted LYLs by 50.0%. A 50% reduction in the baseline switching rates reduces averted SVADs by 33.8% and averted LYLs by 31.0%, while increasing the switching rate by 50% increases averted SVADs by 24.4% and averted LYLs by 22.0%. With a 10% annual decline in switching rates, SVADs are reduced by 49.1% and averted LYLs by 46.1%. However, changes in the NVP cessation multiplier yield relatively small changes (<4%) in averted SVADs and LYLs, because of the lower risks of NVPs relative to smoking. Table 3 also provides estimates of averted SVADs and LYLs with the NVP relative risk multiplier at 40%. Increasing NVP risks from 5% to 40% leads to greater sensitivity of SVADs and LYLs to changes to each of the parameters. Public health gains are projected for all the above scenarios, except at the lower bound of the smoking cessation multiplier.
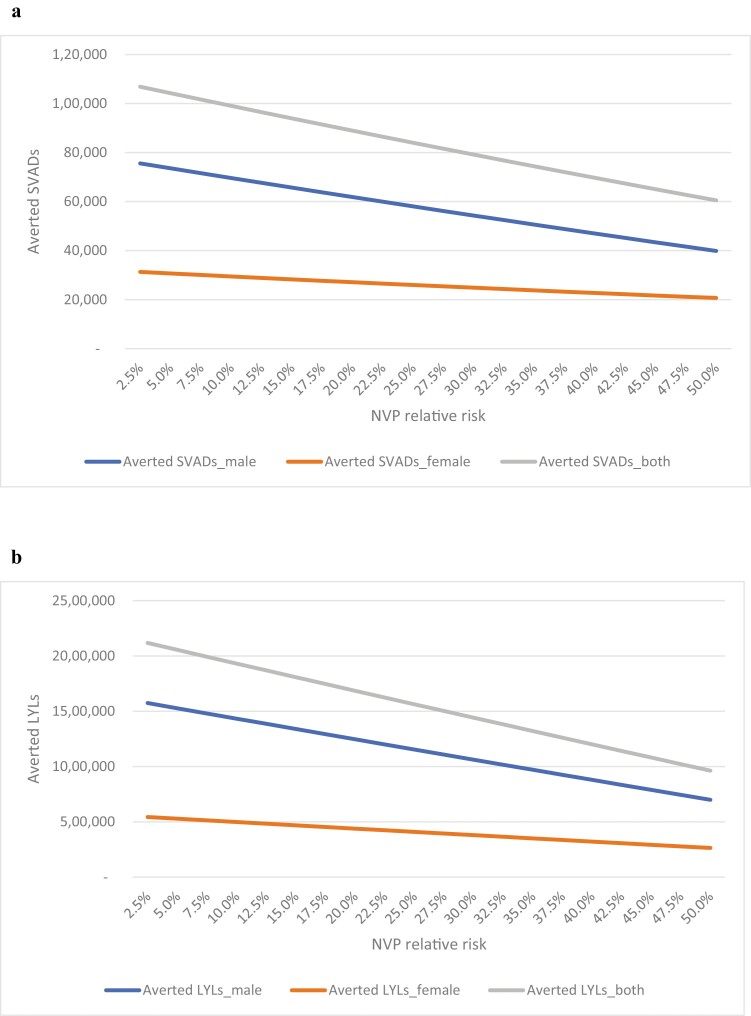
To further examine the impact of NVP relative risks, we conducted a separate sensitivity analysis that focus on NVP risks ranging from 2.5% to 50.0% (Figure 2a and b) Total averted SVADs declined from 106 872 with 2.5% NVP risk to 88 942 with 20% risk, 60 503 with 50% risk, a 43% relative reduction from the lower to upper bound. Total averted LYLs declined from 2 117 069 with 2.5% NVP risk to 1 685 236 with 20% risk, and 962 378 with 50% risk, a 55% relative reduction from the lower to upper bound.
Figure 2. (.
a) Averted smoking- and vaping-attributable deaths (SVADs) and life years lost (LYLs) with nicotine vaping product (NVP) relative risks [2.5%−50.0%] by gender and both genders, ages 18−99, 2021−2080. (b) Averted LYLs with NVP Relative Risks [2.5%−50.0%] by gender and both genders, ages 18−99, 2021−2080.
Discussion
The results of our modeling suggest that relaxing NVP access restrictions in Australia are likely to yield a net public health benefit. The estimated number of averted deaths because of the relaxed policy is sensitive to assumptions about the presumed relative risks of NVP use compared to smoking and estimates of switching from cigarettes to NVPs. Another modeling study64 also found likely public health benefits from reducing NVP restrictions in New Zealand, while other modeling studies also indicate that NVPs are likely to increase public health.29,32–39 Indeed, since NVP use became more widespread in the United States and England, smoking prevalence has substantially declined, particularly among young adults,26,27,51,52,65,66 while during the same years smoking prevalence showed only modest change in Australia.11 In New Zealand, a decline in adult path-month smoking prevalence from 11.9% in 2019/2020 to 9.4% in 2020/2021 coincided with an increase in adult daily vaping prevalence from 3.5% to 6.2%57
In our baseline Permissive Scenario, male smoking prevalence fell from 16% in 2017 to 11% by 2026 (a 13% drop relative to the baseline scenario) and to 2.2% (a 71% relative drop) by 2080. In terms of meeting the Australian government’s goal of lesser than 5% adult smoking prevalence by 2030,67 smoking prevalence is projected to reach 5% for males in 2042 and for females in 2036, indicating that additional policies will be needed to reach less than 5% by 2030. In the Restricted NVP Scenario, smoking prevalence is 7.5% in 2080 for males and the 5% goal is only reached in 2064 for females. The impact of permissive NVP policies compares favorably to the impact of other tobacco control policies. For example, based on recent elasticity estimates,4,68,69 a tax increase equal to about 65% of the current cigarette price (including previous taxes) would be needed to obtain a short-run reduction in smoking prevalence of 12%, which would increase to 24% over the long-run. Nevertheless, with Australian prices as high as AUD 48.70 per pack of 25 cigarettes in 2020,4 the effects of such an increase are highly uncertain and the political acceptability of such an increase is questionable.
The analyses are based on transitions observed in the United States, and thus the Australian Permissive Scenario estimates assume these same patterns would develop in Australia if NVP policies were relaxed to achieve a similar level of consumer access to nicotine-containing e-cigarettes as in the United States. However, our Permissive NVP Scenario switching and cessation parameters using U.S. data from 2013 to 2017, before nicotine-salt pod devices became popular.38 In addition, future technological improvements may increase the substitutability of NVPs for cigarettes over time,70,71 leading to a faster transition to vaping products than suggested by our model.
Our analyses also depend on smoking and vaping initiation parameters. Although some studies find that NVPs may be a gateway to trying smoking,72,73 a systematic review suggested that these results may be large because of confounding74 and population-level studies indicate that increased NVP use is associated with substantially less smoking, especially daily smoking, among youth and young adults than suggested by our model.26,27,53,75–77 U.S. youth NVP rates increased substantially in 201955,56 with the popularity of Juul, but then fell substantially in 2020.55 The New Zealand youth (15–17 years) daily smoking prevalence also fell substantially between 2019/2020 (3.1%) and 2020/2021 (1.1%).57 At the same time, youth daily vaping prevalence rose from 2.3% to 5.8%,57 consistent with our 200% NVP multiplier. Unlike the smoking cessation and switching rate and the NVP risk parameters, public health outcomes in the Permissive NVP Scenario were relatively insensitive to the impact of NVPs on smoking and NVP initiation rates, except at the upper end of NVP excess mortality risks.
In modeling the impact of a more permissive policy, we did not consider differences in past NVP-oriented and cigarette-oriented policies in Australia compared to the United States. The negative government and health organization messaging and history of restrictive NVP policies15,78 may reduce the impact of more permissive NVP policies, for example, because of perceptions of disproportionately large NVP health risks relative to cigarettes. However, the current stringent Australian cigarette-oriented policies may instead heighten the impact of more relaxed NVP policies. For example, with cigarette prices at exceptionally high levels and other strong cigarette-oriented policies in Australia, consumers may be especially motivated to switch to NVPs in the absence of comparable NVP excise taxes. Indeed, demand studies79–82 indicate that NVPs are a substitute for cigarettes, and cessation studies23,83 indicate that NVPs are often used successfully for quitting by those who have had limited success with traditional cessation treatments. Thus, consumers may be especially likely to switch to NVPs and use NVPs to quit smoking because of the currently strong cigarette-oriented policies in Australia.
The availability of an acceptable substitute for cigarettes may also increase the public acceptability of even stronger cigarette-oriented policies. For example, combining access to non-combusted nicotine products with the policy of reducing the nicotine content of cigarettes to nonaddictive levels has been previously proposed84–86 and will be adopted in New Zealand.87 Implementing a very low nicotine product standard while allowing consumers to switch to NVPs may assist countries to more quickly reach a very low smoking prevalence, although it could also maintain nicotine addiction through vaping. It is notable that while an Australian study88 found that a majority of participants who smoke indicated they were interested in switching to a reduced-risk nicotine substitute, most also expressed negative sentiments towards maintaining nicotine addiction. A higher prevalence of NVP use, particularly among youth and young adults may also be publicly and politically unacceptable.
Our results also depend on other model assumptions and parameters. The NVP model does not distinguish dual use from exclusive smoking. Dual use is assumed to have the same cessation and switching patterns as exclusive smoking in the Permissive NVP Scenario and to have the same health risks.49,50 While some studies indicate stable levels of dual use,89,90 other studies indicate dual use is an unstable use state with high rates of transition to exclusive NVP use or cigarette smoking.91–95 To the extent that dual use transitions into exclusive NVP use, smoking will be further reduced in the Permissive NVP Scenario. In addition, our study focused on daily smoking, due to the relatively high percentage of smoking that is done on a daily basis. However, with relaxed restrictions on NVPs, daily smoking may reduce to non-daily smoking with vaping instead of quitting. However, non-daily smoking is associated with higher quit rates96,97 and lower health risks than daily smoking.98
The results also depend on how the Restricted and Permissive NVP Scenarios were constructed. The Restricted NVP Scenario applies initiation and cessation rate parameters based on the well-validated U.S. age-period-cohort smoking analysis.44–46 In applying the U.S. parameters, however, we scaled initiation using the ratio of U.S. to Australian smoking prevalence at the relevant ages to the U.S. age-period-cohort parameters. A similar age-period-cohort analysis could be applied to Australia in future analyses to bolster the results presented here. However, given the similarity in historical smoking prevalence trends in the United States and Australia, we expect that applying an age-period-cohort analysis of Australian data rather than scaled prevalence data would not substantively affect the results. We also calibrated to Australian trends, dampening the recent reductions in Australian age 18–24 rates and the flattening of older female smoking rates at older ages (see Supplementary Material 1). These modifications reduced the recent decline in Australian young adult smoking rates. If, however, recent trends continue, then the impact of a relaxed NVP restriction would be less than our predictions.
Our analysis did not consider the impact of the most recent changes in laws regarding NVP use in Australia, in which the legal status of NVPs in Australia shifted as the default classification of the products from dangerous poisons to prescription-only medicines.19,20 Making NVPs prescription only may provide consumers greater confidence in using them as a smoking cessation aid, but the need to get a prescription may be viewed as a greater impediment than just buying an illegal substance and may be unattractive to those who reject a medical model of smoking cessation.99 The impact of this policy is not yet known, but merits consideration in evaluating the impact of more relaxed restrictions on NVPs.
In conclusion, results from the Australia SAVM suggest greater access to NVPs can create the potential for major reductions in smoking, and the replacement of smoking with vaping. Nevertheless, the results are subject to the assumptions of the model and uncertainty about the impact of countries switching from a more to a less restrictive NVP regime and how the impacts depend on cigarette-oriented policies already in place. The model would benefit from better information regarding the impact of NVPs on smoking under a relaxation of current restrictions.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgments
We would like to thank the participants of talks given to the International Tobacco Control Policy Evaluation Project. We especially thank Shannon Gravely and Andrew Hyland for their very useful comments on a previous draft.
Contributor Information
David T Levy, Lombardi Comprehensive Cancer Center, Georgetown University, Washington DC, USA.
Coral Gartner, School of Public Health, Faculty of Medicine, University of Queensland, Queensland, Australia.
Alex C Liber, Lombardi Comprehensive Cancer Center, Georgetown University, Washington DC, USA.
Luz Maria Sánchez-Romero, Lombardi Comprehensive Cancer Center, Georgetown University, Washington DC, USA.
Zhe Yuan, Lombardi Comprehensive Cancer Center, Georgetown University, Washington DC, USA.
Yameng Li, Lombardi Comprehensive Cancer Center, Georgetown University, Washington DC, USA.
K Michael Cummings, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, USA.
Ron Borland, Melbourne Centre for Behaviour Change, School of Psychological Sciences, University of Melbourne, Melbourne, Australia.
Funding
Drs. Borland, Cummings, Levy, Liber, and Sanchez-Romero received funding from National Cancer Institute ITC grant, P01CA200512. Dr. Gartner received funding from National Health and Medical Research Council grant GNT1198301.
Declaration of Interests
None reported.
Authors’ Contributions
DTL wrote the original manuscript, DTL, YL, ZY, and LMSR developed the initial model, YL and ZY conducted the analyses, edited the Methods section, and wrote the original Results section. RB, CG, KMC, DTL, YL, ZY, AL, and LMSR edited the paper and helped frame the analysis.
Data Availability
The model will be made available to all requestors.
References
- 1. Studlar DT. The Political dynamics of tobacco control in Australia and New Zealand: explaining policy problems, instruments, and patterns of adoption. Aust J Polit Sci. 2006;40(2):255–274. [Google Scholar]
- 2. Chapman S, Wakefield M.. Tobacco control advocacy in Australia: reflections on 30 years of progress. Health Educ Behav. 2001;28(3):274–289. [DOI] [PubMed] [Google Scholar]
- 3. Australian Government DoH. Smoking and Tobacco Laws in Australia. health.gov.au/health-topics/smoking-and-tobacco/about-smoking-and-tobacco/smoking-and-tobacco-laws-in-australia#review. Published 2020. Accessed September 20, 2020.
- 4. Greenhalgh E, Scollo M, Winstanley M.. Tobacco in Australia: Facts and Issues. Melbourne: Cancer Council Victoria.www.TobaccoInAustralia.org.au. Published 2020. Accessed July10, 2021. [Google Scholar]
- 5. Hirono KT, Smith KE.. Australia’s $40 per pack cigarette tax plans: the need to consider equity. Tob Control. 2018;27(2):229–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wakefield MA, Coomber K, Durkin SJ, et al. Time series analysis of the impact of tobacco control policies on smoking prevalence among Australian adults, 2001-2011. Bull World Health Organ. 2014;92(6):413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98(8):1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilkinson AL, Scollo MM, Wakefield MA, et al. Smoking prevalence following tobacco tax increases in Australia between 2001 and 2017: an interrupted time-series analysis. Lancet Public Health. 2019;4(12):e618–e627. [DOI] [PubMed] [Google Scholar]
- 9. Miller CL, Hill DJ, Quester PG, Hiller JE.. Response of mass media, tobacco industry and smokers to the introduction of graphic cigarette pack warnings in Australia. Eur J Public Health. 2009;19(6):644–649. [DOI] [PubMed] [Google Scholar]
- 10. Greenhalgh, EM., Bayly, M., Scollo M.. 1.3 Prevalence of smoking—adults. In: Tobacco in Australia: Facts and Issue. Melbourne: Cancer Council Victoria. Available from http://www.tobaccoinaustralia.org.au/chapter-1-prevalence/1-3-prevalence-of-smoking-adults. Web site. http://www.tobaccoinaustralia.org.au/chapter-1-prevalence/1-3-prevalence-of-smoking-adults. Published 2921. Accessed October 30, 2021. [Google Scholar]
- 11. Mendelsohn C, Hall W, Borland R.. Could vaping help lower smoking rates in Australia? Drug Alcohol Rev. 2020;39(4):415–418. [DOI] [PubMed] [Google Scholar]
- 12. Australian Bureau of Statistics. 4364.0.55.001 – National Health Survey: First Results. Australia Bureau of Statistics. Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release. Published 2020. Accessed Oct 10, 2020.
- 13. Greenhalgh EM, Gartner C, Scollo MM.. InDepth 18A: Smokeless tobacco. In: Scollo, MM and Winstanley, MH, eds. Tobacco in Australia: Facts and Issues. Melbourne: Cancer Council Victoria; 2016. Available from: http://www.tobaccoinaustralia.org.au/chapter-18-harm-reduction/indepth-18a-smokeless-tobacco. Accessed December 1, 2021. [Google Scholar]
- 14. Australian Bureau of Statistics. 4364.0.55.001 – National Health Survey: First Results, 2017-18 . https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019. Published 2018. Accessed October 10, 2020.
- 15. Gartner C, Bromberg M.. One Does not Simply Sell E-cigarettes in Australia: An Overview of Australian E-cigarette Regulations. The regulation of e-cigarettes: international, European and national challenges. Cheltenham, UK: Edward Elgar Publishing; 2019. [Google Scholar]
- 16. Australian Government DoH, Therapeutics Goods Administration. The Poison Standard. tga.gov.au/publikcations/poisons-standard-susmp. Published 2020. Accessed October 10, 2020.
- 17. Australian Institute of Health and Welfare. National Drug Strategy Household Survey (NDSHS) 2019 Key Findings Data Tables AIHW . https://www.aihw.gov.au/reports/children-youth/alcohol-tobacco-and-other-drugs. Published 2017. Accessed July 10, 2020.
- 18. Chan G, Morphett K, Gartner C, et al. Predicting vaping uptake, vaping frequency and ongoing vaping among daily smokers using longitudinal data from the International Tobacco Control (ITC) Four Country Surveys. Addiction. 2019;114(suppl 1):61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Australian Government Department of Health Therapeutic Goods Administration. Nicotine Scheduling Regulation Impact Statement (RIS). https://www.tga.gov.au/sites/default/files/nicotine-scheduling-regulation-impact-statement-ris.pdf.. Published 2020. Accessed October 18, 2021.
- 20. Australian Government Department of Health Therapeutic Goods Administration. Nicotine Vaping Product Access. Therapeutic Goods Administration (TGA). Australian Government Department of Health. https://www.tga.gov.au/nicotine-vaping-product-access. Published 2021. Accessed October 5, 2021.
- 21. Australian Government Department of Health Therapeutic Goods Administration. Notice of an Interim Decision to Amend the Current Poisons Standard . https://www.tga.gov.au/sites/default/files/notice-interim-decision-amend-current-poisons-standard-joint-acms-accs-25-june-2020.pdf. Published 2020. Accessed October 10 2020.
- 22. Hartmann-Boyce J, McRobbie H, Lindson N, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2021;4:CD010216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA.. Quit Methods Used by US Adult Cigarette Smokers, 2014-2016. Prev Chronic Dis. 2017;14:E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Giovenco DP, Delnevo CD.. Prevalence of population smoking cessation by electronic cigarette use status in a national sample of recent smokers. Addict Behav. 2018;76:129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sun T, Lim CCW, Stjepanovic D, et al. Has increased youth e-cigarette use in the USA, between 2014 and 2020, changed conventional smoking behaviors, future intentions to smoke and perceived smoking harms? Addict Behav. 2021;123:107073. [DOI] [PubMed] [Google Scholar]
- 26. Meza R, Jimenez-Mendoza E, Levy DT.. Trends in tobacco use among adolescents by grade, sex, and race, 1991-2019. JAMA Netw Open. 2020;3(12):e2027465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Levy DT, Warner KE, Cummings KM, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob Control. 2019;28(6):629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McNeill A, Brose L, Calder R, Bauld L, Robson D.. Evidence Review of E-cigarettes and Heated Tobacco Products 2018. A Report Commissioned by Public Health England. London: Public Health England, 2018. [Google Scholar]
- 29. National Academy of Sciences EaM. Public Health Consequences of E-cigarettes. In. Washington, DC: The National Acadamies Press; 2018. [Google Scholar]
- 30. Levy DT, Cummings KM, Villanti AC, et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction. 2017;112(1):8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Institute for Global Tobacco Control. E-Cigarette Policy Scan . Institute for Global Tobacco Control, Johns Hopkins Unversity.https://www.globaltobaccocontrol.org/e-cigarette/country-laws/view. Published 2019. Accessed December 9, 2019.
- 32. Cherng ST, Tam J, Christine PJ, Meza R.. Modeling the effects of e-cigarettes on smoking behavior: implications for future adult smoking prevalence. Epidemiology. 2016;27(6):819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Levy DT, Yuan Z, Li Y, Alberg AJ, Cummings KM.. A modeling approach to gauging the effects of nicotine vaping product use on cessation from cigarettes: what do we know, what do we need to know? Addiction. 2019;114(suppl 1):86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Niaura R, Rich I, Johnson AL, et al. Young adult tobacco and e-cigarette use transitions: examining stability using multistate modeling. Nicotine Tob Res. 2020;22(5):647–654. [DOI] [PubMed] [Google Scholar]
- 35. Levy DT, Borland R, Lindblom EN, et al. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob Control. 2018;27(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bachand AM, Sulsky SI, Curtin GM.. Assessing the likelihood and magnitude of a population health benefit following the market introduction of a modified-risk tobacco product: enhancements to the dynamic population modeler, DPM(+1). Risk Anal. 2018;38(1):151–162. [DOI] [PubMed] [Google Scholar]
- 37. Levy DT, Sanchez-Romero LM, Li Y, et al. England SimSmoke: the impact of nicotine vaping on smoking prevalence and smoking-attributable deaths in England. Addiction. 2021;116(5):1196–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Levy DT, Tam J, Sanchez-Romero LM, et al. Public health implications of vaping in the USA: the smoking and vaping simulation model. Popul Health Metr. 2021;19(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mendez D, Warner KE.. A magic bullet? The potential impact of e-cigarettes on the toll of cigarette smoking. Nicotine Tob Res. 2021;23(4):654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Levy DT, Sanchez-Romero LM, Travis N, et al. US nicotine vaping product simsmoke simulation model: the effect of vaping and tobacco control policies on smoking prevalence and smoking-attributable deaths. Int J Environ Res Public Health. 2021;18(9):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. United Nations Department of Economic and Social Affairs Population Division. Population Data. https://population.un.org/wpp/Download/Standard/Interpolated/. Published 2020. Accessed May 20, 2020.
- 42. University of California BU, and Max Planck Institute for Demographic Research (Germany). Human Mortality Database. https://www.mortality.org/cgi-bin/hmd/country.php?cntr=AUS&level=1. Published 2019. Accessed September 12, 2021.
- 43. Thun M, Peto R, Boreham J, Lopez AD.. Stages of the cigarette epidemic on entering its second century. Tob Control. 2012;21(2):96–101. [DOI] [PubMed] [Google Scholar]
- 44. Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort-specific smoking histories, 1965-2009. Am J Prev Med. 2014;46(2):e31–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Jeon J, Holford TR, Levy DT, et al. Smoking and lung cancer mortality in the united states from 2015 to 2065: a comparative modeling approach. Ann Intern Med. 2018;169(10):684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. CISNET. Smoking Histories. https://resources.cisnet.cancer.gov/projects/. Published 2016. Accessed December 20, 2019.
- 47. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. [DOI] [PubMed] [Google Scholar]
- 48. Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA. 2014;311(2):164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Czoli CD, Fong GT, Goniewicz ML, Hammond D.. Biomarkers of exposure among “dual users” of tobacco cigarettes and electronic cigarettes in Canada. Nicotine Tob Res. 2019;21(9):1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Shahab L, Goniewicz ML, Blount BC, et al. Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: a cross-sectional study. Ann Intern Med. 2017;166(6):390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. National Center for Health Statistics. Percentage of Adults Aged 18–24 Years Who Currently Smoke Cigarettes or Who Currently Use Electronic Cigarettes, by Year — National Health Interview Survey, United States, 2014–2018. https://www.cdc.gov/mmwr/volumes/68/wr/mm6839a6.htm. Published 2019. Accessed December 8, 2018.
- 52. Foxon F, Selya AS.. Electronic cigarettes, nicotine use trends and use initiation ages among US adolescents from 1999 to 2018. Addiction. 2020;115(12):2369–2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME.. Trends in adolescent vaping, 2017-2019. N Engl J Med. 2019;381(15):1490–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gentzke AS, Wang TW, Jamal A, et al. Tobacco product use among middle and high school students - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and associated factors among middle and high school students - United States, 2019. MMWR Surveill Summ. 2019;68(12):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Edwards R, Ball J, Hoek J, Wilson N, Waa A.. Key Findings on Smoking and E-cigarette Use Prevalence and Trends in the 2020/21 NZ Health Survey. https://blogs.otago.ac.nz/pubhealthexpert/key-findings-on-smoking-and-e-cigarette-use-prevalence-and-trends-in-the-2020-21-nz-health-survey/. Published 2021. Accessed August 7, 2022.
- 58. Institute of Medicine. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington (DC): National Academy of Sciences; 2015. [Google Scholar]
- 59. Tam J, Levy DT, Jeon J, et al. Projecting the effects of tobacco control policies in the USA through microsimulation: a study protocol. BMJ Open. 2018;8(3):e019169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Nutt DJ, Phillips LD, Balfour D, et al. E-cigarettes are less harmful than smoking. Lancet. 2016;387(10024):1160–1162. [DOI] [PubMed] [Google Scholar]
- 61. Eissenberg T, Bhatnagar A, Chapman S, et al. Invalidity of an oft-cited estimate of the relative harms of electronic cigarettes. Am J Public Health. 2020;110(2):161–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Alzahrani T, Pena I, Temesgen N, Glantz SA.. Association between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55(4):455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bhatta DN, Glantz SA.. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med. 2020;58(2):182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Petrović-Van Der Deen FS, Wilson N, Crothers A, et al. Potential country-level health and cost impacts of legalizing domestic sale of vaporized nicotine products. Epidemiology. 2019;30(3):396–404. [DOI] [PubMed] [Google Scholar]
- 65. Beard E, West R, Michie S, Brown J.. Association of prevalence of electronic cigarette use with smoking cessation and cigarette consumption in England: a time-series analysis between 2006 and 2017. Addiction. 2020;115(5):961–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Jackson SE, Beard E, Michie S, et al. Are smokers who are regularly exposed to e-cigarette use by others more or less motivated to stop or to make a quit attempt? A cross-sectional and longitudinal survey. BMC Med. 2018;16(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Australia Government DoH. National Preventive Health Strategy, 2021-2030.https://www.health.gov.au/sites/default/files/documents/2021/12/national-preventive-health-strategy-2021-2030_1.pdf. Published 2022. Accessed May 30, 2022.
- 68. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 69. Levy DT, Tam J, Kuo C, Fong GT, Chaloupka F.. The impact of implementing tobacco control policies: the 2017 tobacco control policy scorecard. J Public Health Manag Pract. 2018;24(5):448–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Abrams DB. Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete? JAMA. 2014;311(2):135–136. [DOI] [PubMed] [Google Scholar]
- 71. Levy D, Lindblom E, Sweanor D, et al. An economic analysis of the pre-deeming us market for nicotine vaping products. Tob Regul Sci. 2019;5(2):169–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Watkins SL, Glantz SA, Chaffee BW.. Association of noncigarette tobacco product use with future cigarette smoking among youth in the Population Assessment of Tobacco and Health (PATH) study, 2013-2015. JAMA Pediatr. 2018;172(2):181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chan GCK, Stjepanović D, Lim C, et al. Gateway or common liability? A systematic review and meta-analysis of studies of adolescent e-cigarette use and future smoking initiation. Addiction. 2021;116(4):743–756. [DOI] [PubMed] [Google Scholar]
- 75. Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of e-cigarette use among U.S. adults: behavioral risk factor surveillance system, 2016. Ann Intern Med. 2018;169(7):429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vallone DM, Cuccia AF, Briggs J, et al. Electronic cigarette and JUUL use among adolescents and young adults. JAMA Pediatr. 2020 Mar 1;174(3):277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Al Rifai M, Merchant AT, Nambi V, et al. Temporal trends in e-cigarette use among U.S. adults: behavioral risk factor surveillance system, 2016 to 2018. Am J Med. 2020;133(9):e508–e511. [DOI] [PubMed] [Google Scholar]
- 78. Gartner C, Bonevski B, Hall W.. Miscommunication about the causes of the US outbreak of lung diseases in vapers by public health authorities and the media. Drug Alcohol Rev. 2020;39(1):3–6. [DOI] [PubMed] [Google Scholar]
- 79. Huang J, Gwarnicki C, Xu X, et al. A comprehensive examination of own- and cross-price elasticities of tobacco and nicotine replacement products in the U.S. Prev Med. 2018;117:107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Pesko MF, Courtemanche CJ, Catherine Maclean J.. The effects of traditional cigarette and e-cigarette tax rates on adult tobacco product use. J Risk Uncertain. 2020;60(3):229–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Zheng Y, Zhen C, Dench D, Nonnemaker JU.. Demand for tobacco products in a system framework. Health Econ. 2017;26(8):1067–1086. [DOI] [PubMed] [Google Scholar]
- 82. Pesko MF, Huang J, Johnston LD, Chaloupka FJ.. E-cigarette price sensitivity among middle- and high-school students: evidence from monitoring the future. Addiction. 2018;113(5):896–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Beard E, West R, Michie S, Brown J.. Association between electronic cigarette use and changes in quit attempts, success of quit attempts, use of smoking cessation pharmacotherapy, and use of stop smoking services in England: time series analysis of population trends. BMJ. 2016;354:i4645. [DOI] [PubMed] [Google Scholar]
- 84. Gottlieb S, Zeller M.. A nicotine-focused framework for public health. N Engl J Med. 2017;377(12):1111–1114. [DOI] [PubMed] [Google Scholar]
- 85. Gray N, Henningfield JE, Benowitz NL, et al. Toward a comprehensive long term nicotine policy. Tob Control. 2005;14(3):161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Donny EC, Walker N, Hatsukami D, Bullen C.. Reducing the nicotine content of combusted tobacco products sold in New Zealand. Tob Control. 2017;26(e1):e37–e42. [DOI] [PubMed] [Google Scholar]
- 87. New Zealand Government. Aotearoa 2025 Action Plan Ministry of Health. https://www.health.govt.nz/system/files/documents/publications/hp7801_-_smoke_free_action_plan_v15_web.pdf. Smokefree. Published 2021. Accessed 2022, May 31.
- 88. Morphett K, Puljevic C, Borland R, et al. Attitudes towards a hypothetical “clean nicotine” product and harm reduction among smokers. Int J Drug Policy. 2021;88:103020. [DOI] [PubMed] [Google Scholar]
- 89. Bandi P, Cahn Z, Goding Sauer A, et al. Trends in e-cigarette use by age group and combustible cigarette smoking histories, U.S. adults, 2014-2018. Am J Prev Med. 2021;60(2):151–158. [DOI] [PubMed] [Google Scholar]
- 90. Owusu D, Huang J, Weaver SR, et al. Patterns and trends of dual use of e-cigarettes and cigarettes among U.S. adults, 2015-2018. Prev Med Rep. 2019;16:101009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Coleman B, Rostron B, Johnson SE, et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013-2015). Tob Control. 2019 Jan;28(1):50–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Azagba S, Shan L, Latham K.. Adolescent dual use classification and its association with nicotine dependence and quit intentions. J Adolesc Health. 2019;65(2):195–201. [DOI] [PubMed] [Google Scholar]
- 93. Robertson L, Hoek J, Blank ML, et al. Dual use of electronic nicotine delivery systems (ENDS) and smoked tobacco: a qualitative analysis. Tob Control. 2019;28(1):13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Borland R, Murray K, Gravely S, et al. A new classification system for describing concurrent use of nicotine vaping products alongside cigarettes (so-called “dual use”): findings from the ITC-4 Country Smoking and Vaping wave 1 Survey. Addiction. 2019;114(suppl 1):24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Brouwer AF, Jeon J, Hirschtick JL, et al. Transitions between cigarette, ENDS and dual use in adults in the PATH study (waves 1-4): multistate transition modelling accounting for complex survey design. Tob Control. 2020. doi:10.1136/tobaccocontrol-220-055967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kotz D, Fidler J, West R.. Very low rate and light smokers: smoking patterns and cessation-related behaviour in England, 2006-11. Addiction. 2012;107(5):995–1002. [DOI] [PubMed] [Google Scholar]
- 97. Arancini L, Borland R, Le Grande M, et al. Age as a predictor of quit attempts and quit success in smoking cessation: findings from the International Tobacco Control Four-Country survey (2002-14). Addiction. 2021;116(9):2509–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Inoue-Choi M, McNeel TS, Hartge P, et al. Non-daily cigarette smokers: mortality risks in the U.S. Am J Prev Med. 2019;56(1):27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Morphett K, Carter A, Hall W, Gartner C.. Medicalisation, smoking and e-cigarettes: evidence and implications. Tob Control. 2017;26(e2):e134–e139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The model will be made available to all requestors.