Abstract
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare complication of acute pulmonary embolism. It is caused by persistent obstruction of pulmonary arteries by chronic organised fibrotic clots, despite adequate anticoagulation. The pulmonary hypertension is also caused by concomitant microvasculopathy which may progress without timely treatment. Timely and accurate diagnosis requires the combination of imaging and haemodynamic assessment. Optimal therapy should be individualised to each case and determined by an experienced multidisciplinary CTEPH team with the ability to offer all current treatment modalities. This report summarises current knowledge and presents key messages from the International CTEPH Conference, Bad Nauheim, Germany, 2021. Sessions were dedicated to 1) disease definition; 2) pathophysiology, including the impact of the hypertrophied bronchial circulation, right ventricle (dys)function, genetics and inflammation; 3) diagnosis, early after acute pulmonary embolism, using computed tomography and perfusion techniques, and supporting the selection of appropriate therapies; 4) surgical treatment, pulmonary endarterectomy for proximal and distal disease, and peri-operative management; 5) percutaneous approach or balloon pulmonary angioplasty, techniques and complications; and 6) medical treatment, including anticoagulation and pulmonary hypertension drugs, and in combination with interventional treatments. Chronic thromboembolic pulmonary disease without pulmonary hypertension is also discussed in terms of its diagnostic and therapeutic aspects.
Short abstract
This report summarises current knowledge on chronic thromboembolic pulmonary hypertension (CTEPH) and presents key messages from the International CTEPH Conference, Bad Nauheim, Germany, 2021. https://bit.ly/3VJmc2l
New concepts and definitions for patients suffering from chronic organised clots of pulmonary arteries (G. Simonneau)
Chronic thromboembolic pulmonary hypertension (CTEPH) is a disease of patients whose symptoms can be attributed to obstruction of pulmonary arteries by chronic organised fibrotic clots. These patients present mismatched perfusion defects on ventilation/perfusion (V′/Q′) lung scan and specific signs of chronic clots on computed tomography pulmonary angiography (CTPA) or conventional pulmonary angiography (CPA) such as ring-like stenoses, webs/slits, wall irregularities and chronic total occlusions with pouch lesions, these findings being observed after at least 3 months of therapeutic anticoagulation and associated with a pre-capillary pulmonary hypertension (PH) defined as mean pulmonary arterial pressure (mPAP) ≥25 mmHg, mean pulmonary arterial wedge pressure (PAWP) <15 mmHg and pulmonary vascular resistance (PVR) ≥3 WU [1].
Since 2014, cohorts of symptomatic patients have been described showing similar obstructive lesions as in CTEPH without PH at rest (mPAP <25 mmHg and PVR <3 WU) [2, 3]. Their exercise limitation is attributed to a combination of exercise-induced PH and dead space ventilation [4]. These patients may benefit from similar management as for CTEPH, including lifelong effective anticoagulation, surgery (pulmonary endarterectomy (PEA)) and, more recently, balloon pulmonary angioplasty (BPA). Reporting authors proposed the term “chronic thromboembolic disease” (CTED) to characterise this population, which was misleading as it did not specify that the disease was affecting pulmonary arteries. Based on scientific evidence, a decrease in the threshold mPAP defining PH, from 25 to 21 mmHg, was introduced in 2018 at the Sixth World Symposium on Pulmonary Hypertension [5]. In addition, a decrease in the threshold PVR to define pre-capillary PH, from 3 to 2 WU, is proposed in the 2022 European Society of Cardiology/European Respiratory Society guidelines for the diagnosis and treatment of PH [6, 7]. Lowering these threshold values of mPAP and PVR may reclassify former CTED patients as CTEPH patients. To solve this terminological dilemma, Task Force members of the 2021 European Respiratory Society statement on CTEPH proposed the overarching term “chronic thromboembolic pulmonary disease” (CTEPD) to characterise symptomatic patients who present mismatched perfusion defects on V′/Q′ lung scan and specific signs of chronic clots on CTPA or CPA, whether or not they have PH at rest [8]. Some of these patients may still have no PH at rest according to the more recent definition [6, 7]. For patients with PH at rest, the term CTEPH is still of use. Currently, patients without PH at rest represent a minority (<10%) of patients referred to CTEPH centres and their management is not yet well established. The natural history of CTEPD without PH and if it is an early stage of CTEPH is unknown. Clinical experience suggests that some patients with CTEPD and no PH remain stable on lifelong anticoagulation while others experience a rapid deterioration. The cause of this deterioration may be multifactorial, including recurrence of acute pulmonary embolism (PE), development of microvasculopathy or worsening of comorbidities such as chronic lung disease and left heart disease. To answer these questions, a prospective international multicentre registry would be essential.
Pathophysiology
Role of the bronchial circulation and microvasculopathy (E. Fadel)
When a pulmonary artery is occluded, the pulmonary vasculature itself is unable to create collateral vessels bypassing the occlusion, whereas the systemic vasculature will generate bronchial-to-pulmonary artery anastomoses to supply the ischaemic lung region. Enlargement of the bronchial arteries and increased bronchial blood flow have been reported to occur 3 days after left pulmonary artery ligation in piglets, reaching a maximum within 2–4 weeks [9]. The systemic blood flow to the left lung returns to normal within 5 weeks after pulmonary artery reopening and the newly formed systemic vessels undergo partial involution [9]. In CTEPH patients, the cross-sectional area of the bronchial arteries, measured on CTPA 3 months after PEA, is significantly reduced compared with pre-operatively [10] and the pre-operative haemoptysis disappears after PEA [11]. Anastomoses between the enlarged bronchial arteries and pulmonary arteries contribute to the development of microvasculopathy in the occluded lung regions, while high flow induces microvasculopathy in the over-perfused, non-occluded lung regions [12].
Massive haemoptysis requiring bronchial artery embolisation has been reported in 1–4% of CTEPH patients [13, 14]. Only patients with bronchial artery dilation have been shown to be at increased risk of haemoptysis [14]. There is no robust evidence that medical treatment with riociguat may increase the incidence of haemoptysis in CTEPH patients; however, in those experiencing episodes of haemoptysis, the drug is not recommended [15]. No correlations were found between the developed bronchial circulation and other features of CTEPH, such as mosaic perfusion or disease severity [16]. Haemoptysis is one of the most common complications following BPA, occurring in 7–13% of procedures [17, 18]. Neither haemodynamic parameters nor bronchial circulation hypertrophy are associated with this complication, which is attributed to operators and only depends on lesion morphology [19].
Mechanisms of cardiac dysfunction in CTEPH (A. Vonk Noordegraaf)
Right ventricular (RV) failure in CTEPH is a consequence of increased load. RV load can be commonly determined as PVR and arterial compliance. In CTEPH, the RV response to the arterial load is similar to idiopathic pulmonary arterial hypertension (PAH), because the resistor-capacitor time is constant and thus the energy efficacy is the same. However, the impact of mechanical stress, e.g. RV wall tension, is different between CTEPH and idiopathic PAH. RV wall tension is a time-varying load which is imposed on the cardiac muscle, depending on RV volume and pressure based on the Law of Laplace. When RV pressure is augmented at larger RV volume (at earlier maximal systole), RV wall tension increases more markedly. When considering wall tension, the arrival time of reflected pressure waves is identified as an important determinant of RV load [20]. Reflected pressure waves add to forward waves and thus earlier return of reflected waves (at larger RV volume) contributes to more exaggerated RV wall tension. When comparing proximal and distal CTEPH, proximal CTEPH has earlier return of reflected waves due to reflection sites closer to the right ventricle, which contributes to higher RV wall tension and more deteriorated RV function, e.g. lower RV ejection fraction, and larger RV volume and mass, than distal CTEPH [21]. This concept translates to distinguishing differences in RV dysfunction between CTEPH and idiopathic PAH. Compared with idiopathic PAH, the right ventricle is more dilated and stiffer as a consequence of a higher wall tension at a similar load in CTEPH [22]. In CTEPH, the RV load can be uniquely characterised by the early return of reflected waves, which induces high RV wall tension.
Role of genetic studies in CTEPH (M. Toshner)
The study of genetics in disease can elucidate not just underlying pathophysiology but also the understanding of risk prediction and target therapy decision making. There is an open and valid question about how tractable genetic studies are in a rare disease like CTEPH where there is already a confounding or inter-related underlying known disease process (venous thromboembolism (VTE)) for which the genetics are well studied with existing meta-analyses [23]. In the absence of rare mutations with large effects sizes it is probable that the genetics of CTEPH will be moderate to small effect sizes requiring larger numbers of cases. Despite this, we already know from phenotyping and targeted genotyping studies that non-O blood group polymorphisms remain over-represented, although it is not clear if in greater proportions than in VTE/PE [24], and that fibrinogen polymorphisms emerged as associated with CTEPH before VTE [25]. International collaborative studies at scale are the only tractable way to clarify if there is a shared or differing genetic architecture of CTEPH to VTE. These efforts are likely to meaningfully contribute to our underlying understanding of disease aetiology.
New insights into CTEPH pathogenesis: role of neutrophil extracellular traps (I.M. Lang)
Inflammatory conditions, particularly infection of the thrombus, have been associated with clinical cases of CTEPH [26]. Because neutrophils are crucial in sequestering pathogens, the role of neutrophils and neutrophil extracellular traps (NETs), which are nuclear DNA strands expelled upon neutrophil stimulation, was investigated. In the murine inferior vena cava ligation model, staphylococcal infection led to larger thrombi containing more neutrophils and NETs, with less resolution. Neutrophils, markers of neutrophil activation and NET formation were increased in plasma of CTEPH patients. NETs promoted the differentiation of monocytes to activated fibroblasts carrying the same cellular phenotype as fibroblasts from CTEPH vascular occlusions. RNA sequencing of fibroblasts isolated from PEA specimens and pulmonary artery biopsies revealed transforming growth factor (TGF)-β as the central regulator, a phenotype which was replicated in mice with fibroblast-specific TGF-β overactivity. These experiments uncover a role of NETs in fibrotic thrombus remodelling [27]. They support the observation that CTEPH-associated conditions such as staphylococcal infection of transvenous leads [28, 29], inflammatory bowel disease [30], Behçet's disease [31], cancer [28] and familial Mediterranean fever [32] are NET-driven diseases. Thrombus NETs may serve as targets for the treatment of thrombosis and its sequelae.
Diagnosis and imaging
Early diagnosis of CTEPH after acute PE (F.A. Klok)
The primary aim of the diagnostic approach to post-PE syndrome, defined by the combination of persistent dyspnoea, impaired exercise capacity and/or decreased health-related quality of life [33], is to rule out CTEPH, because diagnostic delay is associated with poor outcome, lower quality of life and higher risk of death [8, 34, 35]. Several clues pointing to CTEPH can be identified on imaging tests performed to diagnose and prognosticate acute PE. First, high estimated systolic PAP (>50–60 mmHg) is a clear indicator of underlying PH, since acute PE, even with high clot burden, usually does not lead to such pressures [8]. Second, CTPA that was used to confirm acute PE has been repeatedly reported to show clot morphology consistent with chronicity (e.g. webs, bands and tapered vessels) and signs of chronic PH (e.g. RV hypertrophy and dilated bronchial arteries) in those patients that were ultimately diagnosed with CTEPH [8, 36, 37]. Hence, both persistent dyspnoea after PE as well as echocardiographic or CTPA signs of CTEPH at the time of a PE diagnosis should trigger targeted CTEPH diagnostic testing, starting with echocardiography [8]. The optimal timing for this diagnostic work-up is after 3 months of follow-up unless patients develop severe progressive dyspnoea and/or signs of RV failure before that time. Current diagnostic delay of CTEPH illustrates poor disease awareness [34, 38]. Education of PE caretakers, improved implementation of PE guidelines, which recommend systematic follow-up 3–6 months after acute PE and further evaluation in patients with persistent or new-onset dyspnoea/exercise limitation or with risk factors for CTEPH [39], and expert support for vascular imaging including artificial intelligence tools will all help to diagnose CTEPH earlier.
While CTEPD without PH is not a potentially fatal disease, symptomatic patients should be referred to a CTEPH centre as well since some of them may benefit from similar treatment approaches [8]. Patients with CTEPD may be identified during the work-up of CTEPH, if right heart catheterisation rules out abnormal mPAP and PVR, and if cardiopulmonary exercise testing (CPET) is suggestive, after exclusion of ventilatory limitation, deconditioning and hyperventilation syndrome. Routinely performing CTPA or perfusion imaging in PE survivors with persistent symptoms is not recommended, mostly because persistent clots correlated poorly to functional status or symptom burden.
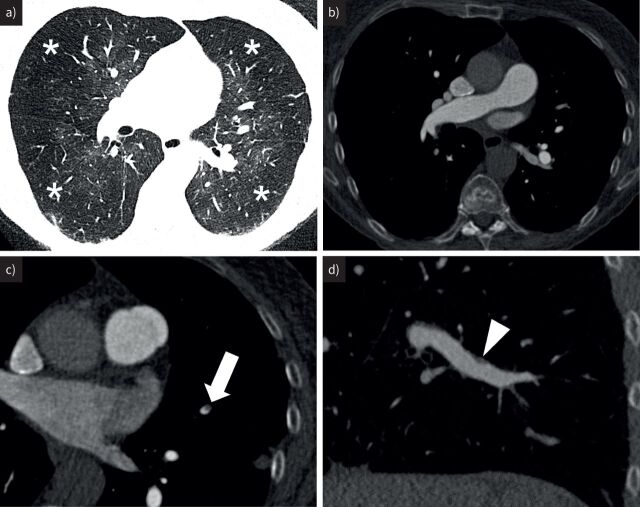
Radiological diagnosis of CTEPH (M.C. McInnis)
Key to the radiological diagnosis of CTEPH is a robust CTPA protocol to produce diagnostic images of high quality. Although CTPA is reported as highly sensitive and specific at expert centres, and the CT level of disease correlates well with operative findings, there are many pitfalls to CT interpretation in real clinical practice [40–42]. Among the most important factors to consider for CTPA in CTEPH is the reconstruction slice thickness. Chronic PE, especially webs and eccentric thickening, routinely measures 1–2 mm in thickness (figure 1). Therefore, multiplanar reformats of a slice thickness ≤1 mm are preferred. The addition of an advanced imaging technique, such as dual-energy CT or lung subtraction iodine mapping, may further improve sensitivity, particularly for segmental/subsegmental lesions [43, 44]. The signs of CTEPH on CTPA can be divided into those of PH (RV enlargement and hypertrophy or main pulmonary artery dilatation), chronic PE (pulmonary artery slits/webs, eccentric thickening, and pouch defects and occlusions), lung perfusion abnormalities (mosaic lung attenuation and peripheral scars) and collateral perfusion, most commonly bronchial artery hypertrophy [45]. Recently added to this list was a highly reproducible sign of abnormal pulmonary venous filling, the “pulmonary vein sign”. Gopalan et al. [46] reported a sensitivity and specificity for CTEPH of 78% and 85%, respectively, among three control groups (CTEPH, acute PE and non-thromboembolic disease). In addition to the diagnosis of CTEPH, the role of CTPA after PEA is unclear. Indeed, Braams et al. [47] report that residual segmental/subsegmental lesions are common after PEA, present in 20% of patients, but residual lesions were not significantly associated with residual PH. As an alternative to CTPA, magnetic resonance (MR) angiography suffers from limitations in spatial resolution and respiratory motion at the subsegmental level. MR perfusion, however, is a potential screening alternative to V′/Q′ imaging (further discussed by N. Screaton in the following section “Beyond V′/Q′ scan: cutting-edge imaging modalities”). Importantly, CPA is still used to assess treatment options when CTPA is inconclusive.
FIGURE 1.
Radiological diagnosis. Computed tomography pulmonary angiography in a 71-year-old woman with progressive shortness of breath, a positive ventilation/perfusion study (not shown) and a mean pulmonary arterial pressure of 38 mmHg. a) Lung windows demonstrate striking mosaic lung attenuation with alternating areas of normal density perihilar lung and hypodense peripheral lung (asterisks). b) Despite this, there is no chronic pulmonary embolism evident in the proximal vasculature. c) Thin sections are critical to identify subtle pulmonary artery filling defects as seen here in the inferior lingula (arrow) and d) sagittal multiplanar reformats are key in revealing subtle eccentric wall thickening in the right lower lobe (arrowhead).
Beyond V′/Q′ scan: cutting-edge imaging modalities (N. Screaton)
Imaging of the pulmonary vasculature is key to the diagnosis and management of PH. This may take the form of morphological imaging of the macroscopic vasculature or imaging of perfusion in the microvasculature. Traditionally, V′/Q′ scintigraphy has been considered the reference standard to differentiate CTEPH from PAH, its high sensitivity leading to it becoming embedded in PH imaging algorithms. In 2007, Tunariu et al. [48] demonstrated that the sensitivity of V′/Q′ scan in CTEPH was >95%, while CT with 4–8-slice scanners had a sensitivity of only 51%. Rapid developments in CT and MR imaging (MRI) have improved morphological imaging, which with 64-slice CT scanners reports a sensitivity of >95%. Importantly, developments in CT technology with spectral CT and subtraction CT permit generation of regional iodine density maps (a surrogate for perfusion) in addition to conventional CTPA. There is excellent concordance between perfusion defects on dual-energy CT and V′/Q′ scan [49], and the use of dual-energy perfusion maps improved detection of disease segments in CTEPH by >25% [50]. In CTEPH as opposed to acute PE, delayed imaging can show reperfusion of the defects by the hypertrophied bronchial collaterals [51]. Dynamic contrast-enhanced MRI also enables detection of perfusion defects and carried comparable sensitivity to perfusion scintigraphy [52]. While absolute regional quantification of perfusion parameters is feasible with MRI, typically qualitative assessment is performed with both CT and MRI. While V′/Q′ scintigraphy continues to be considered the reference standard to rule out chronic thromboembolism, the growing evidence supporting perfusion CT (using spectral imaging) and with MR perfusion means that many centres with the relevant technology are modifying their diagnostic approach.
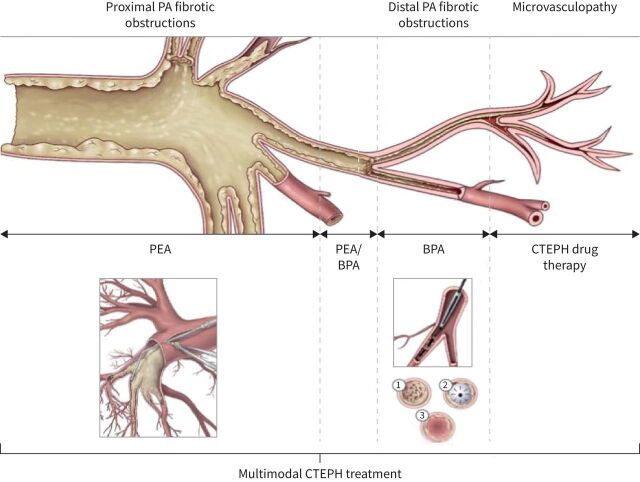
How to select treatment modalities: PEA versus BPA? (E. Mayer)
Two mechanical treatment options have been established for CTEPH patients: surgical PEA and interventional BPA. PEA is recommended for operable patients [53], but operability is subjective and a “grey zone” between PEA and BPA is obvious despite a lack of any evidence (figure 2) [8]. Individual treatment recommendations by a multidisciplinary CTEPH team are mainly based on the localisation of pulmonary artery obstructions at pre-operative imaging. Country and centre experience and practice with PEA and/or BPA seem to be important variables with regard to final CTEPH treatment (table 1) [54]. Even in experienced centres there is no consensus regarding the relevance of severity of PH, comorbidity and age for PEA versus BPA treatment decision making. Individualised multimodality treatment including surgery, intervention and medical therapy is currently recommended for CTEPH, and further discussed by C.B. Wiedenroth in the later section “Multimodal interventions”.
FIGURE 2.
Multimodal chronic thromboembolic pulmonary hypertension (CTEPH) treatment. PA: pulmonary artery; PEA: pulmonary endarterectomy; BPA: balloon pulmonary angioplasty.
TABLE 1.
Pulmonary endarterectomy versus balloon pulmonary angioplasty “grey zone” defined by the proximal end of obstructive material, according to chronic thromboembolic pulmonary hypertension centres surveyed in November 2021
| Centre | Proximal segmental PA | Distal segmental PA | Subsegmental PA | No “grey zone” |
| Okayama | + | + | ||
| Osaka | + | |||
| San Diego | + | |||
| Cambridge | + | |||
| Vienna | + | |||
| Leuven | + | + | ||
| Paris | + | |||
| Hannover | + | |||
| Bad Nauheim | + | + |
This survey illustrates the different approaches to operability between Japan and the rest of the world, and the difficulty to agree on the best therapeutic approach for segmental/subsegmental lesions. PA: pulmonary artery.
Pulmonary endarterectomy
Segmental/subsegmental endarterectomy (M.M. Madani)
PEA, by means of complete resection of organised thrombi within the pulmonary vascular tree, is the preferred treatment for CTEPH. Over the last several decades, the techniques of the procedure and short- and long-term outcomes have become well established. There is little debate that PEA is the preferred approach and treatment when there is disease within the main and lobar pulmonary arteries. However, endarterectomy for disease limited to segmental/subsegmental branches is technically demanding, and the efficacy and long-term outcomes are being challenged by other means of therapy, in particular by BPA with or without combination PH drugs. Using newly revised surgical instruments to allow access into these distal branches, experienced surgeons are now able to perform complete resection even when the disease is limited only to segmental/subsegmental branches, i.e. “distal disease”. In such patients, the endarterectomy plane is started proximally within the normal pulmonary artery at the level of the lobar and proximal segmental branches. The intima and, on occasion, the media is dissected free in a circumferential manner and moved distally to eventually engage and resect the more distal and firm chronic thrombotic material. This facilitates the removal of the entire material to its distal “tail”. Fragmentation of the specimen at this level prevents a complete endarterectomy from being achieved. In some patients with favourable anatomy, visualisation is adequate so that the plane of endarterectomy can be started at the segmental and/or subsegmental branches. In such patients, typically a web, wall thickening or a pouch defect can be appreciated and the plane of dissection can then be carefully started at this distal level. However, in these patients, each individual branch needs careful and thorough examination, and the plane of dissection needs to be developed and established separately.
Using a more contemporary surgical classification to accurately define the location of disease within the pulmonary vasculature (table 2) [53], the University California-San Diego group analysed approximately 800 patients over the previous 4 years and looked at pre-operative patients’ characteristics and short-term outcomes for proximal (level I and II) versus distal (level III and IV) disease. Patients with exclusive bilateral segmental and/or subsegmental disease had similar pre-operative characteristics; however, they seemed to be slightly older, and had more common history of indwelling catheters, pacemaker leads and splenectomy. Both groups had significant and similar improvements in their haemodynamics, although patients with segmental/subsegmental disease had lower mortality (0.8% versus 3.2%) and lower incidence of airway haemorrhage (3.0% versus 6.6%). Not surprisingly, given the technical challenges, the distal endarterectomy group had longer deep hypothermic circulatory arrest (DHCA) times (56 versus 40 min).
TABLE 2.
University California-San Diego chronic thromboembolic disease (CTED) surgical classification
| Level 0 | No evidence of CTED in either lung |
| Level I | CTED starting in the main pulmonary arteries |
| Level IC | Complete occlusion of one main pulmonary artery with CTED |
| Level II | CTED starting at the level of lobar arteries, or in the main descending pulmonary arteries |
| Level III | CTED starting at the level of the segmental arteries |
| Level IV | CTED starting at the level of the subsegmental arteries |
Classification based on the most proximal disease identified. Information from [53].
In conclusion, in experienced centres, segmental/subsegmental PEA is technically feasible and results in favourable haemodynamic outcomes without increased risk of mortality or complications.
PEA: peri-operative management, peri-operative complications and intensive care challenges (G. Martinez, K. Salaunkey and D.P. Jenkins)
Patients’ preparation for PEA should focus on fluid balance optimisation, screening for anaemia and haemoglobinopathies, and a tailored peri-operative anticoagulation plan [55]. The majority of patients present to surgery with a dilated right ventricle. This makes patients vulnerable to systemic hypotension during general anaesthesia; thus, maintaining normal aortic root pressure to ensure good coronary flow to the right ventricle is essential. Intra-operative trans-oesophageal echocardiography is useful to assess the right ventricle, the presence of tricuspid regurgitation and the presence of patent foramen ovale, which can contribute to hypoxaemia [56]. Although up to 80% of patients show moderate to severe tricuspid regurgitation, most resolve after surgery once the PVR decreases [57]. DHCA is required to perform PEA surgery. The general anaesthetic set-up for DHCA does not differ significantly from other complex surgery, and it must include meticulous heparinisation, gradual (slow) institution of hypothermia and external head cooling to avoid re-warming during DHCA [58, 59]. Although steroids are commonly used for DHCA, there is no evidence that they provide additional neuroprotection or show a risk reduction in reperfusion injury after PEA surgery [60].
Serious intra- and peri-operative complications of PEA are frequent, and include lung reperfusion injury, haemoptysis and residual PH with RV failure [61]. Lung reperfusion injury and haemoptysis are usually mild, and they can be managed with conservative measures such as protective ventilation and intermittent airway suction, but in around 2–3% of cases the bleeding rate or parenchymal oedema can be severe and cause life-threatening hypoxaemia. In this context, placement of a bronchial blocker to isolate the area or diversion of blood with extracorporeal membrane oxygenation support is a safe strategy to bridge to recovery [62]. RV failure is less common and normally the consequence of poor surgical clearance with residual PH. It remains a leading cause of in-hospital mortality, with post-operative PVR in the intensive care unit of >500 or <500 dyn·s·cm−5 differentiating mortality of 10.3% versus 0.9% [63].
All patients need intensive care for the first 24–48 h after PEA, but patients with immediate complications may require an extended critical care stay. The analgesic requirements are low after PEA and morphine is not routinely administered post-operatively to facilitate early awakening [64]. Vasoactive drug use is guided by pulmonary haemodynamics and femoral blood pressure measurements. Inflation of the pulmonary artery catheter balloon is disabled, preventing wedging. Measurement of extravascular lung water might predict the development of reperfusion lung injury [65]. A net negative fluid balance using a continuous furosemide infusion and low threshold to initiate continuous venovenous hemofiltration to treat acute kidney injury are recommended. Systemic anticoagulation with viscoelastic monitoring is started as soon as feasible [66].
Balloon pulmonary angioplasty
State-of-the-art techniques and complication management (H. Matsubara)
BPA has emerged as a treatment option for inoperable CTEPH patients and global experience is growing. Improvements of mPAP and cardiac output of about 25% and 10%, respectively, with a very low 30-day mortality were reported [67]. However, the technical aspects of BPA have not yet been standardised. The only similarities in BPA techniques across centres are the femoral vein approach and the use of balloons smaller than the vessel diameter. Most BPA complications are caused by pulmonary vascular injuries [68], which can be avoided by using soft-tip wires and by keeping the procedure as simple as possible. Most BPA centres have abandoned the routine use of intravascular imaging techniques. The treatment goal of BPA also varies between centres. Since the main symptom of CTEPH patients is shortness of breath caused by a combination of low cardiac output and V′/Q′ mismatch, improvements of both haemodynamics and gas exchange should be targeted. Total reperfusion of all segmental arteries is the ultimate goal of BPA; currently, even total occlusions are treatment targets.
The incidence of lung injury complicating BPA was 60% in early BPA reports but has decreased significantly with technical refinements of the procedure [67]. The severity of lung injury correlates with the level of pre-procedural mPAP [68]. Pre-treatment with riociguat can be used to minimise the risk of lung injury [69]. In addition, oxygen therapy decreases mPAP by approximately 10%, regardless of the use of riociguat [70]. To prevent the occurrence of lung injury, it is essential to treat vascular injury during the procedure by reversal of anticoagulation and temporal occlusion of pulmonary arteries proximal to the injured site. In case of severe bleeding, gelatine embolisation is preferred to coil embolisation, because gelatine is absorbed within a few weeks and patency of the target vessel is restored [71].
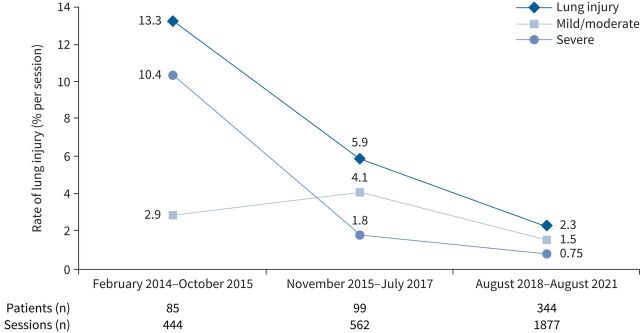
BPA learning curve: the French experience (P. Brénot)
The evolution of the safety and efficacy of BPA over time has been evaluated in a high-volume centre, comparing two periods in which, respectively, 184 and 344 patients were treated (first period: February 2014 to July 2017 [17]; second period: August 2017 to August 2021). The main indication for BPA was clot inaccessibility for surgery. The second period was characterised by an increase in the proportion of patients with residual PH after PEA (17.7% versus 8.2%) and by a new multimodality approach (BPA on one side followed by PEA on the other side; 10%). Compared with the first period, patients had a less severe haemodynamic profile and a higher proportion were receiving PH drugs, including dual combination therapy. The safety analysis highlighted a drastic decrease in the incidence of lung injury, especially severe lung injury (from 20% to 4% per patient; 10.4% to <1% per session) (figure 3). Per-patient multivariate analysis revealed that mPAP and BPA programme experience were the most significant factors related to lung injury. Four peri-procedural deaths occurred among the 528 treated patients (0.75%), all in the first period. No death was observed during the last 5 years. The authors observed a more important reduction in mPAP and PVR (−30% and −49% versus −22% and −37%, respectively) during the second half of the first period [17], which was confirmed in the second period (−31.5% and −45.4%, respectively). The French data show a steep learning curve and that high-volume experience results in a drastic reduction in severe lung injury and in an improvement in BPA effectiveness.
FIGURE 3.
Evolution of the rate of lung injury (% per session) over time.
Medical and multimodal therapy
Anticoagulant options in CTEPH (M.M. Hoeper)
Based on pathogenetic considerations, indefinite anticoagulation is recommended for almost all CTEPH patients [1, 53]. Historically, this has been the domain of vitamin K antagonists (VKAs), but non-VKA oral anticoagulants (NOACs) are increasingly used in this patient population [55, 72]. There are no prospective, randomised studies comparing VKAs and NOACs in CTEPH patients, but concerns have been raised about the safety and efficacy of NOACs in this group of patients. A retrospective study from the UK found a similar rate of bleeding events but a larger risk of recurrent VTE in patients receiving NOACs (n=206) compared with patients receiving VKAs (n=794) [55]. Comparable results were reported from the EXPERT registry, where the rate of recurrent VTE was higher in patients receiving NOACs (n=198) than in patients receiving VKAs (n=683), while the rate of bleeding events was similar [73]. Survival rates up to 3 years were identical in both groups [73]. The use of NOACs in CTEPH patients is covered by their label as they are used to prevent recurrent VTE. The available data are insufficient to make firm conclusions on the safety and efficacy of NOACs versus VKAs in this patient population. When NOACs are used in patients with CTEPH, they are usually administered at their initial maintenance doses, e.g. rivaroxaban 20 mg once daily or apixaban 5 mg twice daily.
Role of medical therapy in CTEPH (H.A. Ghofrani)
While the central and intermediate pulmonary vascular compartments are the targets for surgical and/or interventional therapies, the microvasculopathy of the pre-capillary pulmonary arterial resistance vessels is amenable to medical therapy. The first successfully tested medical therapy for patients with inoperable CTEPH was riociguat, an oral stimulator of soluble guanylate cyclase, which showed efficacy (26 m increase in 6-min walk distance and 31% reduction in PVR, at 16 weeks) and safety in the randomised, double-blinded, placebo-controlled CHEST-1 and extension CHEST-2 studies [74, 75]. Consequently, riociguat became the first approved treatment for these patients. Subsequent studies investigated other PAH targeted drugs, such as the subcutaneously administered prostanoid treprostinil and the oral endothelin receptor antagonist macitentan. Treprostinil, based on the results of the CTREPH study, was recently approved by the European Medicines Agency for the treatment of inoperable CTEPH [76]. Macitentan was successfully tested in a phase II randomised controlled trial [77] and is currently being investigated in phase III. Combinations or sequential utilisation of different treatment modalities are under investigation. In particular, the value of pre-treating patients who are scheduled for BPA with medical therapy was recently described by two independent studies from France (RACE) [69] and Japan (MR BPA) [78]. Those studies showed good efficacy for both treatment modalities, with stronger immediate haemodynamic benefits for BPA, while the safety of this procedure could be substantially improved if patients were pre-treated with riociguat prior to BPA according to the RACE study.
Medical versus BPA treatment in non-operable patients (X. Jaïs)
The RACE study investigated the safety and efficacy of riociguat versus BPA in newly diagnosed, treatment-naïve, non-operable CTEPH patients with PVR >4 WU [69]. The primary end-point was PVR at week 26 expressed as a percentage of the baseline value. From 2016 to 2019, 105 patients were enrolled with 53 randomly assigned to riociguat and 52 to BPA. At week 26, geometric mean PVR decreased to 40% of baseline in the BPA group and to 67% in the riociguat group (geometric mean ratio 0.6, 95% CI 0.52–0.69; p<0.0001). However, treatment-related serious adverse events were more frequent with BPA than with riociguat (42% and 9% of patients, respectively). Patients completing the RACE trial were included in an extended 26-week follow-up study and those remaining symptomatic with PVR >4 WU were offered to receive add-on therapy with riociguat for those assigned to BPA and vice versa. At week 52, there was no significant difference between first-line BPA and riociguat for change in PVR. By contrast, a lower incidence of serious adverse events related to BPA was observed when patients had received a 26-week treatment with riociguat prior to BPA. Riociguat initiated before BPA may improve the safety of BPA by optimising pre-BPA haemodynamics.
In conclusion, medical therapies are one essential cornerstone in the multimodal treatment armamentarium for CTEPH patients. They exert therapeutic effects on their own, but also qualify as effective combination partners with other treatment modalities.
Multimodal interventions (C.B. Wiedenroth)
As shown in the previous sections, treatment modalities are available for each compartment of the affected pulmonary arteries: PEA for proximal vessels, BPA for distal vessels and PH drugs for the microcirculation. Several combinations of these modalities are possible, but the evidence for these combinations is often scarce. In carefully selected patients with severe PH and operable lesions on one side, but predominantly peripheral changes on the opposite side, a combined procedure of PEA with the possibility of intra-operative BPA can be considered. BPA was performed under extracorporeal circulation in the warming phase after PEA [79]. Pre-operative BPA followed by PEA is another option for those patients (unpublished data, Paris). For treatment decision making, the cause of residual or recurrent PH after PEA should be considered. The anticoagulation needs to be re-evaluated, redo surgical treatment must be considered and PH medication is indicated. In addition, BPA may be considered [80–82]. Finally, the multimodal approach with medical treatment before/after surgical or interventional therapy is common practice with limited evidence. Besides the already presented data showing a lower complication rate for BPA after drug pre-treatment [69], pre-PEA medical treatment, although widely used, is not based on evidence.
In conclusion, multidisciplinary CTEPH teams are mandatory for complex multimodal treatment recommendations and individual long-term follow-up and therapy.
CTEPD without PH: exercise haemodynamics and treatment evidence (S. Guth)
CTEPD without PH has been coined for symptomatic patients with pulmonary vascular obstructions and no PH at rest. During exercise, mPAP increases in excess relative to the increase in cardiac output. Normally, this results in a mPAP/cardiac output slope >3 mmHg·L−1·min [83]. Patients with this condition have no symptoms at rest but complain of exertional dyspnoea; therefore, physical exercise is limited. Caution should be taken to exclude cardiopulmonary comorbidities as potential causes of dyspnoea before envisioning specific therapy.
There are now five small case series describing the beneficial effect of surgery in these patients regarding improvements in exercise capacity and quality of life [2, 84–87]. Significant improvements are shown for mPAP, mPAP/cardiac output slope and CPET. These surgical series did not experience early mortality, but complication rates ranged between 0% and 40%.
In conclusion, PEA in these patients is an effective treatment with significant improvement of functionality and exercise capacity without in-hospital mortality. There is, however, no evidence if surgery avoids long-term deterioration to CTEPH and provides a survival advantage. Additionally, two small series reported significant clinical and haemodynamic improvements in patients with CTEPD without PH undergoing BPA with a low rate of complications [88, 89].
Key messages
CTEPH is associated with persistent obstruction of pulmonary arteries by chronic organised fibrotic clots. Preliminary genome-wide association studies showed shared and differing genetic architecture of CTEPH to VTE. Inflammatory conditions, specifically neutrophils and NETs, contribute to CTEPH aetiology. Anastomoses between the enlarged bronchial arteries and pulmonary arteries contribute to the development of microvasculopathy in the occluded lung regions, while high flow induces microvasculopathy in the over-perfused, non-occluded lung regions. Improved understanding of cardiac dysfunction translates to distinguishing differences in the right ventricle between CTEPH and idiopathic PAH. Compared with idiopathic PAH, the right ventricle is more dilated and stiffer when arterial load increases in CTEPH.
Progress in non-invasive imaging of intravascular and perfusion changes allows for better localisation of abnormalities and allocation of appropriate modality of management. While V′/Q′ scintigraphy continues to be the reference standard to rule out chronic thromboembolism, there is growing evidence supporting perfusion CT (using spectral imaging) and MR perfusion. There is continuous improvement in peri-operative care and, as a result, in long-term outcomes for patients treated surgically, therefore PEA remains as the treatment of choice. BPA and medical therapy are now well established for non-operable patients either as individual modalities or in combination. Combining medical and interventional (BPA) therapies is improving the safety of the procedure and long-term outcomes of CTEPH patients. In conclusion, multidisciplinary CTEPH teams are mandatory for complex multimodal treatment recommendations and individual long-term follow-up and therapy.
Increased awareness of post-PE syndrome has improved our understanding of CTEPD without PH. Clinical experience suggests that some of these patients remain stable on lifelong anticoagulation while others experience a rapid deterioration.
Points for clinical practice
CTEPH is caused by obstruction of pulmonary arteries by chronic organised fibrotic clots in addition to varying degrees of microvasculopathy contributing to PH.
It is defined by the combination of pre-capillary PH, mismatched perfusion defects on V′/Q′ lung scan and specific signs of chronic clots on CTPA or CPA after at least 3 months of therapeutic anticoagulation.
CTEPD, which includes CTEPH, can also be observed without PH.
PEA is the treatment of choice for CTEPH.
In experienced centres, segmental/subsegmental CTEPD without PH can be treated surgically with similar outcomes to more proximal disease.
BPA is a safe and effective alternative for patients with inaccessible disease.
mPAP and operator experience are the best predictors of BPA complications.
Medical therapy is recommended in inoperable patients, alone or in combination with BPA.
PEA, BPA and medical therapy are complementary.
All CTEPH patients should be evaluated by a CTEPH team, including at least a PEA surgeon, a PH physician (pneumologist/cardiologist) and an interventional cardiologist/radiologist.
Acknowledgements
The International CTEPH Congress 2021 was organised by the International CTEPH Association, an independent organisation of physicians, surgeons and other medically qualified professionals committed to advancing the diagnosis and treatment of CTEPH, and coordinated by Sonja Mariotti and Simone Lerch (International CTEPH Association, Basel, Switzerland). It was endorsed by the European Reference Network (ERN)-LUNG and the World Symposium on Pulmonary Hypertension Association, among others.
Provenance: Commissioned article, peer reviewed.
This article has an editorial commentary: https://doi.org/10.1183/16000617.0006-2023
Number 1 in the Series “The world of rare lung diseases” Edited by Michael Kreuter, Marc Humbert, Thomas Wagner and Marlies Wijsenbeek
Conflict of interest: E. Fadel, G. Martinez, G. Simonneau, K. Salaunkey, N. Screaton and P. Brénot have no conflicts of interest to declare. A. Vonk Noordegraaf is supported by the Netherlands CardioVascular Research Initiative (CVON-2012–08 PHAEDRA, CVON-2017-10 DOLPHIN-GENESIS) and the Netherlands Organization for Scientific Research (NWO-VICI: 918.16.610); his institute received speakers fees from Johnson & Johnson, MSD, Actelion, Bayer and Ferrer in the past 3 years; and he served as a member of the scientific advisory boards of Morphogen-X, Ferrer, Gossamer Bio Services Inc. and Johnson & Johnson. C.B. Wiedenroth has received speaker fees and/or consultant honoraria from Actelion, AOP Orphan Pharmaceuticals AG, Bayer AG, BTG, MSD and Pfizer. D.P. Jenkins is on the adjudication committees for the SELECT and Maciteph studies (Actelion), and has received fees for lectures on CTEPH from Actelion. E. Mayer has received speaker or consulting fees from Actelion/Janssen, Bayer and MSD. F.A. Klok has received research support from Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, MSD, Leo Pharma, Actelion, the Netherlands Organisation for Health Research and Development, the Dutch Thrombosis Association, the Dutch Heart Foundation and the Horizon Europe Program, unrelated to the current work and paid to his institution. H.A. Ghofrani has received grants/research support from Actelion, Janssen, Bayer, Gossamer, Acceleron; honoraria or consultation fees from Actelion, Janssen, Bayer, Gossamer, Acceleron, Pfizer, Novartis and MSD; and participated in a company sponsored speaker's bureau for Actelion, Janssen, Bayer, Gossamer, Pfizer, Novartis and MSD. H. Matsubara has received honoraria for lectures from Janssen Pharmaceutical KK, Bayer Yakuhin Ltd, Nippon Shinyaku Co Ltd, Mochida Pharmaceutical Co. Ltd and Kaneka Medix Corporation. I.M. Lang has a financial interest with Actelion/Janssen, AOP Orphan, Medtronic, Daiichi Sankyo, Neutrolis, United Therapeutics and Ferrer that could be perceived as a real or apparent conflict of interest in the context of the subject of this article. J. Pepke-Zaba has received speaker or consulting fees from Actelion/Janssen, Bayer, MSD and Ferrer, and a research grant from MSD, all outside submitted work. M.C. McInnis reports honoraria from Bayer and Boehringer Ingelheim, unrelated to the current work. M. Delcroix reports research grants from Actelion/Janssen, speaker and consultant fees from Altavant, Acceleron, AOP, Daiichi Sankyo, Bayer, Ferrer, Gossamer and MSD, outside the submitted work, and all paid to her institution. She is holder of the Janssen Chair for Pulmonary Hypertension at KU Leuven. M.M. Hoeper reports fees for lectures and/or consultations from Acceleron, Actelion, Bayer, GSK, Janssen, MSD and Pfizer. M.M. Madani is a consultant for Actelion. M. Toshner reports grants and personal fees from Bayer, personal fees from MSD, grants and personal fees from Actelion, and personal fees from GSK within the last 5 years. N.H. Kim has served as consultant for Bayer, Janssen, Merck and United Therapeutics. S. Guth has received speaker fees and/or consultant honoraria from Actelion, Bayer, GSK, MSD and Pfizer. X. Jaïs reports grants from the French Ministry of Health and Bayer Healthcare, during the conduct of the study; grants from Acceleron, Janssen and MSD; personal fees from Janssen and MSD; and non-financial support from Janssen.
References
- 1.Galiè N, Humbert M, Vachiery J-L, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 2015; 46: 903–975. doi: 10.1183/13993003.01032-2015 [DOI] [PubMed] [Google Scholar]
- 2.Taboada D, Pepke-Zaba J, Jenkins DP, et al. Outcome of pulmonary endarterectomy in symptomatic chronic thromboembolic disease. Eur Respir J 2014; 44: 1635–1645. doi: 10.1183/09031936.00050114 [DOI] [PubMed] [Google Scholar]
- 3.de Perrot M, Mayer E. Chronic thromboembolic pulmonary hypertension: do we need a new definition? Eur Respir J 2014; 44: 1401–1403. doi: 10.1183/09031936.00177514 [DOI] [PubMed] [Google Scholar]
- 4.Claeys M, Claessen G, Gerche AL, et al. Impaired cardiac reserve and abnormal vascular load limit exercise capacity in chronic thromboembolic disease. JACC Cardiovasc Imaging 2019; 12: 1444–1456. doi: 10.1016/j.jcmg.2018.07.021 [DOI] [PubMed] [Google Scholar]
- 5.Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019; 53: 1801913. doi: 10.1183/13993003.01913-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2023; 61: 2200879. doi: 10.1183/13993003.00879-2022 [DOI] [PubMed] [Google Scholar]
- 7.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2022; 43: 3618–3731. doi: 10.1093/eurheartj/ehac237 [DOI] [PubMed] [Google Scholar]
- 8.Delcroix M, Torbicki A, Gopalan D, et al. ERS statement on chronic thromboembolic pulmonary hypertension. Eur Respir J 2021; 57: 2002828. doi: 10.1183/13993003.02828-2020 [DOI] [PubMed] [Google Scholar]
- 9.Fadel E, Wijtenburg E, Michel R, et al. Regression of the systemic vasculature to the lung after removal of pulmonary artery obstruction. Am J Respir Crit Care Med 2006; 173: 345–349. doi: 10.1164/rccm.200506-894OC [DOI] [PubMed] [Google Scholar]
- 10.Shimizu H, Tanabe N, Terada J, et al. Dilatation of bronchial arteries correlates with extent of central disease in patients with chronic thromboembolic pulmonary hypertension. Circ J 2008; 72: 1136–1141. doi: 10.1253/circj.72.1136 [DOI] [PubMed] [Google Scholar]
- 11.Dartevelle P, Fadel E, Chapelier A, et al. Angioscopic video-assisted pulmonary endarterectomy for post-embolic pulmonary hypertension. Eur J Cardiothorac Surg 1999; 16: 38–43. doi: 10.1016/S1010-7940(99)00116-5 [DOI] [PubMed] [Google Scholar]
- 12.Dorfmüller P, Günther S, Ghigna M-R, et al. Microvascular disease in chronic thromboembolic pulmonary hypertension: a role for pulmonary veins and systemic vasculature. Eur Respir J 2014; 44: 1275–1288. doi: 10.1183/09031936.00169113 [DOI] [PubMed] [Google Scholar]
- 13.Reesink HJ, van Delden OM, Kloek JJ, et al. Embolization for hemoptysis in chronic thromboembolic pulmonary hypertension: report of two cases and a review of the literature. Cardiovasc Intervent Radiol 2007; 30: 136–139. doi: 10.1007/s00270-005-0382-8 [DOI] [PubMed] [Google Scholar]
- 14.Clements W, Venn G, McGiffin D, et al. Chronic thromboembolic pulmonary hypertension (CTEPH) and massive hemoptysis: the rationale for bronchial artery embolization. Respir Med 2022; 195: 106784. doi: 10.1016/j.rmed.2022.106784 [DOI] [PubMed] [Google Scholar]
- 15.European Medicines Agency . Adempas: EPAR – product information. 2015. www.ema.europa.eu/en/documents/product-information/adempas-epar-product-information_en.pdf Date last accessed: 3 July 2022.
- 16.Remy-Jardin M, Duhamel A, Deken V, et al. Systemic collateral supply in patients with chronic thromboembolic and primary pulmonary hypertension: assessment with multi-detector row helical CT angiography. Radiology 2005; 235: 274–281. doi: 10.1148/radiol.2351040335 [DOI] [PubMed] [Google Scholar]
- 17.Brenot P, Jais X, Taniguchi Y, et al. French experience of balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Eur Respir J 2019; 53: 1802095. doi: 10.1183/13993003.02095-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saito S, Ikeda N, Iijima R, et al. Evaluation of the effect of nitric oxide inhalation in the patients with chronic thromboembolic pulmonary hypertension or pulmonary disease during balloon pulmonary angioplasty. Pulm Circ 2022; 12: e12032. doi: 10.1002/pul2.12032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ikeda N, Kubota S, Okazaki T, et al. The predictors of complications in balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Catheter Cardiovasc Interv 2019; 93: E349–E356. doi: 10.1002/ccd.28133 [DOI] [PubMed] [Google Scholar]
- 20.Fukumitsu M, Groeneveldt JA, Braams NJ, et al. When right ventricular pressure meets volume: the impact of arrival time of reflected waves on right ventricle load in pulmonary arterial hypertension. J Physiol 2022; 600: 2327–2344. doi: 10.1113/JP282422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fukumitsu M, Westerhof BE, Ruigrok D, et al. Early return of reflected waves increases right ventricular wall stress in chronic thromboembolic pulmonary hypertension. Am J Physiol Heart Circ 2020; 319: H1438–H1450. doi: 10.1152/ajpheart.00442.2020 [DOI] [PubMed] [Google Scholar]
- 22.Braams NJ, van Leeuwen JW, Vonk Noordegraaf A, et al. Right ventricular adaptation to pressure-overload: differences between chronic thromboembolic pulmonary hypertension and idiopathic pulmonary arterial hypertension. J Heart Lung Transplant 2021; 40: 458–466. doi: 10.1016/j.healun.2021.02.018 [DOI] [PubMed] [Google Scholar]
- 23.Germain M, Chasman DI, de Haan H, et al. Meta-analysis of 65,734 individuals identifies TSPAN15 and SLC44A2 as two susceptibility loci for venous thromboembolism. Am J Hum Genet 2015; 96: 532–542. doi: 10.1016/j.ajhg.2015.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pepke-Zaba J, Delcroix M, Lang I, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation 2011; 124: 1973–1981. doi: 10.1161/CIRCULATIONAHA.110.015008 [DOI] [PubMed] [Google Scholar]
- 25.Suntharalingam J, Goldsmith K, van Marion V, et al. Fibrinogen Aα Thr312Ala polymorphism is associated with chronic thromboembolic pulmonary hypertension. Eur Respir J 2008; 31: 736–741. doi: 10.1183/09031936.00055107 [DOI] [PubMed] [Google Scholar]
- 26.Bonderman D, Jakowitsch J, Redwan B, et al. Role for staphylococci in misguided thrombus resolution of chronic thromboembolic pulmonary hypertension. Arterioscler Thromb Vasc Biol 2008; 28: 678–684. doi: 10.1161/ATVBAHA.107.156000 [DOI] [PubMed] [Google Scholar]
- 27.Sharma S, Hofbauer TM, Ondracek AS, et al. Neutrophil extracellular traps promote fibrous vascular occlusions in chronic thrombosis. Blood 2021; 137: 1104–1116. doi: 10.1182/blood.2020005861 [DOI] [PubMed] [Google Scholar]
- 28.Bonderman D, Jakowitsch J, Adlbrecht C, et al. Medical conditions increasing the risk of chronic thromboembolic pulmonary hypertension. Thromb Haemost 2005; 93: 512–516. doi: 10.1160/TH04-10-0657 [DOI] [PubMed] [Google Scholar]
- 29.Jevnikar M, Montani D, Savale L, et al. Chronic thromboembolic pulmonary hypertension and totally implantable central venous access systems. Eur Respir J 2020; 57: 2002208. doi: 10.1183/13993003.02208-2020 [DOI] [PubMed] [Google Scholar]
- 30.Angelidou I, Chrysanthopoulou A, Mitsios A, et al. REDD1/autophagy pathway is associated with neutrophil-driven IL-1β inflammatory response in active ulcerative colitis. J Immunol 2018; 200: 3950–3961. doi: 10.4049/jimmunol.1701643 [DOI] [PubMed] [Google Scholar]
- 31.Joncour AL, Martos R, Loyau S, et al. Critical role of neutrophil extracellular traps (NETs) in patients with Behcet's disease. Ann Rheum Dis 2019; 78: 1274. doi: 10.1136/annrheumdis-2018-214335 [DOI] [PubMed] [Google Scholar]
- 32.Apostolidou E, Skendros P, Kambas K, et al. Neutrophil extracellular traps regulate IL-1β-mediated inflammation in familial Mediterranean fever. Ann Rheum Dis 2016; 75: 269–277. doi: 10.1136/annrheumdis-2014-205958 [DOI] [PubMed] [Google Scholar]
- 33.Klok FA, van der Hulle T, den Exter PL, et al. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev 2014; 28: 221–226. doi: 10.1016/j.blre.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 34.Klok FA, Barco S, Konstantinides SV, et al. Determinants of diagnostic delay in chronic thromboembolic pulmonary hypertension: results from the European CTEPH Registry. Eur Respir J 2018; 52: 1801687. doi: 10.1183/13993003.01687-2018 [DOI] [PubMed] [Google Scholar]
- 35.Boon GJAM, van den Hout WB, Barco S, et al. A model for estimating the health economic impact of earlier diagnosis of chronic thromboembolic pulmonary hypertension. ERJ Open Res 2021; 7: 00719-2020. doi: 10.1183/23120541.00719-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guérin L, Couturaud F, Parent F, et al. Prevalence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Thromb Haemostasis 2014; 112: 598–605. doi: 10.1160/TH13-07-0538 [DOI] [PubMed] [Google Scholar]
- 37.Ende-Verhaar YM, Meijboom LJ, Kroft LJM, et al. Usefulness of standard computed tomography pulmonary angiography performed for acute pulmonary embolism for identification of chronic thromboembolic pulmonary hypertension: results of the InShape III study. J Heart Lung Transplant 2019; 38: 731–738. doi: 10.1016/j.healun.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 38.Ende-Verhaar YM, Hout WB, Bogaard HJ, et al. Healthcare utilization in chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. J Thromb Haemost 2018; 16: 2168–2174. doi: 10.1111/jth.14266 [DOI] [PubMed] [Google Scholar]
- 39.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Respir J 2019; 54: 1901647. doi: 10.1183/13993003.01647-2019 [DOI] [PubMed] [Google Scholar]
- 40.Dong C, Zhou M, Liu D, et al. Diagnostic accuracy of computed tomography for chronic thromboembolic pulmonary hypertension: a systematic review and meta-analysis. PLoS One 2015; 10: e0126985. doi: 10.1371/journal.pone.0126985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rogberg AN, Gopalan D, Westerlund E, et al. Do radiologists detect chronic thromboembolic disease on computed tomography? Acta Radiol 2019; 60: 1576–1583. doi: 10.1177/0284185119836232 [DOI] [PubMed] [Google Scholar]
- 42.McInnis MC, Wang D, Donahoe L, et al. Importance of computed tomography in defining segmental disease in chronic thromboembolic pulmonary hypertension. ERJ Open Res 2020; 6: 00461-2020. doi: 10.1183/23120541.00461-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tamura M, Yamada Y, Kawakami T, et al. Diagnostic accuracy of lung subtraction iodine mapping CT for the evaluation of pulmonary perfusion in patients with chronic thromboembolic pulmonary hypertension: correlation with perfusion SPECT/CT. Int J Cardiol 2017; 243: 538–543. doi: 10.1016/j.ijcard.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 44.Dournes G, Verdier D, Montaudon M, et al. Dual-energy CT perfusion and angiography in chronic thromboembolic pulmonary hypertension: diagnostic accuracy and concordance with radionuclide scintigraphy. Eur Radiol 2014; 24: 42–51. doi: 10.1007/s00330-013-2975-y [DOI] [PubMed] [Google Scholar]
- 45.Grosse A, Grosse C, Lang I. Evaluation of the CT imaging findings in patients newly diagnosed with chronic thromboembolic pulmonary hypertension. PLoS One 2018; 13: e0201468. doi: 10.1371/journal.pone.0201468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gopalan D, Nordgren-Rogberg A, Le EPV, et al. Abnormal pulmonary venous filling: an adjunct feature in the computed tomography pulmonary angiogram assessment of chronic thromboembolic pulmonary hypertension. J Am Heart Assoc 2020; 9: e018075. doi: 10.1161/JAHA.120.018075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Braams NJ, Ruigrok D, Schokker MGM, et al. Pulmonary vascular imaging characteristics after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant 2020; 39: 248–256. doi: 10.1016/j.healun.2019.11.020 [DOI] [PubMed] [Google Scholar]
- 48.Tunariu N, Gibbs SJR, Win Z, et al. Ventilation–perfusion scintigraphy is more sensitive than multidetector CTPA in detecting chronic thromboembolic pulmonary disease as a treatable cause of pulmonary hypertension. J Nucl Med 2007; 48: 680–684. doi: 10.2967/jnumed.106.039438 [DOI] [PubMed] [Google Scholar]
- 49.Giordano J, Khung S, Duhamel A, et al. Lung perfusion characteristics in pulmonary arterial hypertension (PAH) and peripheral forms of chronic thromboembolic pulmonary hypertension (pCTEPH): dual-energy CT experience in 31 patients. Eur Radiol 2017; 27: 1631–1639. doi: 10.1007/s00330-016-4500-6 [DOI] [PubMed] [Google Scholar]
- 50.Faivre JL, Duhamel A, Khung S, et al. Impact of CT perfusion imaging on the assessment of peripheral chronic pulmonary thromboembolism: clinical experience in 62 patients. Eur Radiol 2016; 26: 4011–4020. doi: 10.1007/s00330-016-4262-1 [DOI] [PubMed] [Google Scholar]
- 51.Hong YJ, Kim JY, Choe KO, et al. Different perfusion pattern between acute and chronic pulmonary thromboembolism: evaluation with two-phase dual-energy perfusion CT. AJR Am J Roentgenol 2013; 200: 812–817. doi: 10.2214/AJR.12.8697 [DOI] [PubMed] [Google Scholar]
- 52.Rajaram S, Rajaram S, Swift AJ, et al. 3D contrast-enhanced lung perfusion MRI is an effective screening tool for chronic thromboembolic pulmonary hypertension: results from the ASPIRE Registry. Thorax 2013; 68: 677–678. doi: 10.1136/thoraxjnl-2012-203020 [DOI] [PubMed] [Google Scholar]
- 53.Kim NH, Delcroix M, Jais X, et al. Chronic thromboembolic pulmonary hypertension. Eur Respir J 2019; 53: 1801915. doi: 10.1183/13993003.01915-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guth S, D'Armini AM, Delcroix M, et al. Current strategies for managing chronic thromboembolic pulmonary hypertension: results of the worldwide prospective CTEPH Registry. ERJ Open Res 2021; 7: 00850-2020. doi: 10.1183/23120541.00850-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bunclark K, Newnham M, Chiu Y, et al. A multicenter study of anticoagulation in operable chronic thromboembolic pulmonary hypertension. J Thromb Haemost 2020; 18: 114–122. doi: 10.1111/jth.14649 [DOI] [PubMed] [Google Scholar]
- 56.Vandenheuvel M, Bouchez S, Wouters P, et al. Assessing right ventricular function in the perioperative setting, Part I: echo-based measurements. Anesthesiol Clin 2019; 37: 675–695. doi: 10.1016/j.anclin.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 57.Zhen Y, Zhang J, Liu X, et al. Impact of pulmonary thromboendarterectomy on tricuspid regurgitation in patients with chronic thromboembolic pulmonary hypertension: a single-center prospective cohort experience. J Thorac Dis 2020; 12: 758–764. doi: 10.21037/jtd.2019.12.99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Veerhoek D, van Barneveld LJ, Haumann RG, et al. Anticoagulation management during pulmonary endarterectomy with cardiopulmonary bypass and deep hypothermic circulatory arrest. Perfusion 2021; 36: 87–96. doi: 10.1177/0267659120928682 [DOI] [PubMed] [Google Scholar]
- 59.O'Neill B, Bilal H, Mahmood S, et al. Is it worth packing the head with ice in patients undergoing deep hypothermic circulatory arrest? Interact Cardiov Thorac Surg 2012; 15: 696–701. doi: 10.1093/icvts/ivs247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kerr KM, Auger WR, Marsh JJ, et al. Efficacy of methylprednisolone in preventing lung injury following pulmonary thromboendarterectomy. Chest 2012; 141: 27–35. doi: 10.1378/chest.10-2639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mayer E, Jenkins D, Lindner J, et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. J Thorac Cardiovasc Surg 2011; 141: 702–710. doi: 10.1016/j.jtcvs.2010.11.024 [DOI] [PubMed] [Google Scholar]
- 62.Guth S, Wiedenroth CB, Wollenschläger M, et al. Short-term venoarterial extracorporeal membrane oxygenation for massive endobronchial hemorrhage after pulmonary endarterectomy. J Thorac Cardiovasc Surg 2018; 155: 643–649. doi: 10.1016/j.jtcvs.2017.09.045 [DOI] [PubMed] [Google Scholar]
- 63.Madani MM, Auger WR, Pretorius V, et al. Pulmonary endarterectomy: recent changes in a single institution's experience of more than 2,700 patients. Ann Thorac Surg 2012; 94: 97–103. doi: 10.1016/j.athoracsur.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 64.Giménez-Milà M, Videla S, Jenkins D, et al. Acute pain and analgesic requirements after pulmonary endarterectomy with deep hypothermic circulatory arrest. J Cardiothor Vasc Anesth 2015; 30: 993–996. doi: 10.1053/j.jvca.2015.11.013 [DOI] [PubMed] [Google Scholar]
- 65.Butchart AG, Zochios V, Villar SS, et al. Measurement of extravascular lung water to diagnose severe reperfusion lung injury following pulmonary endarterectomy: a prospective cohort clinical validation study. Anaesthesia 2019; 74: 1282–1289. doi: 10.1111/anae.14744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Serraino GF, Murphy GJ. Routine use of viscoelastic blood tests for diagnosis and treatment of coagulopathic bleeding in cardiac surgery: updated systematic review and meta-analysis. Br J Anaesth 2017; 118: 823–833. doi: 10.1093/bja/aex100 [DOI] [PubMed] [Google Scholar]
- 67.Shimokawahara H, Ogawa A, Matsubara H. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: advances in patient and lesion selection. Curr Opin Pulm Med 2021; 27: 303–310. doi: 10.1097/MCP.0000000000000797 [DOI] [PubMed] [Google Scholar]
- 68.Ejiri K, Ogawa A, Fujii S, et al. Vascular injury is a major cause of lung injury after balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension. Circ Cardiovasc Interv 2018; 11: e005884. doi: 10.1161/CIRCINTERVENTIONS.117.005884 [DOI] [PubMed] [Google Scholar]
- 69.Jaïs X, Brenot P, Bouvaist H, et al. Balloon pulmonary angioplasty versus riociguat for the treatment of inoperable chronic thromboembolic pulmonary hypertension (RACE): a multicentre, phase 3, open-label, randomised controlled trial and ancillary follow-up study. Lancet Respir Med 2022; 10: 961–971. doi: 10.1016/S2213-2600(22)00214-4 [DOI] [PubMed] [Google Scholar]
- 70.Shigetoshi M, Hatanaka K, Ogawa A, et al. Oxygen inhalation can selectively dilate pulmonary arteries in patients with chronic thromboembolic pulmonary hypertension before balloon angioplasty. J Cardiol 2022; 79: 265–269. doi: 10.1016/j.jjcc.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 71.Inami T, Kataoka M, Shimura N, et al. Incidence, avoidance, and management of pulmonary artery injuries in percutaneous transluminal pulmonary angioplasty. Int J Cardiol 2015; 201: 35–37. doi: 10.1016/j.ijcard.2015.08.052 [DOI] [PubMed] [Google Scholar]
- 72.Kramm T, Wilkens H, Fuge J, et al. Incidence and characteristics of chronic thromboembolic pulmonary hypertension in Germany. Clin Res Cardiol 2018; 107: 548–553. doi: 10.1007/s00392-018-1215-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Humbert M, Simonneau G, Pittrow D, et al. Oral anticoagulants (NOAC and VKA) in chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant 2022; 41: 716–721. doi: 10.1016/j.healun.2022.02.002 [DOI] [PubMed] [Google Scholar]
- 74.Ghofrani H-A, D'Armini AM, Grimminger F, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med 2013; 369: 319–329. doi: 10.1056/NEJMoa1209657 [DOI] [PubMed] [Google Scholar]
- 75.Simonneau G, D'Armini AM, Ghofrani HA, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension: a long-term extension study (CHEST-2). Eur Respir J 2015; 45: 1293–1302. doi: 10.1183/09031936.00087114 [DOI] [PubMed] [Google Scholar]
- 76.Sadushi-Kolici R, Jansa P, Kopec G, et al. Subcutaneous treprostinil for the treatment of severe non-operable chronic thromboembolic pulmonary hypertension (CTREPH): a double-blind, phase 3, randomised controlled trial. Lancet Respir Med 2019; 7: 239–248. doi: 10.1016/S2213-2600(18)30367-9 [DOI] [PubMed] [Google Scholar]
- 77.Ghofrani H-A, Simonneau G, D'Armini AM, et al. Macitentan for the treatment of inoperable chronic thromboembolic pulmonary hypertension (MERIT-1): results from the multicentre, phase 2, randomised, double-blind, placebo-controlled study. Lancet Respir Med 2017; 5: 785–794. doi: 10.1016/S2213-2600(17)30305-3 [DOI] [PubMed] [Google Scholar]
- 78.Kawakami T, Matsubara H, Abe K, et al. Multicentre randomised controlled trial of balloon pulmonary angioplasty and riociguat in patients with chronic thromboembolic pulmonary hypertension: protocol for the MR BPA study. BMJ Open 2020; 10: e028831. doi: 10.1136/bmjopen-2018-028831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wiedenroth CB, Liebetrau C, Breithecker A, et al. Combined pulmonary endarterectomy and balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant 2016; 35: 591–596. doi: 10.1016/j.healun.2015.10.030 [DOI] [PubMed] [Google Scholar]
- 80.Araszkiewicz A, Darocha S, Pietrasik A, et al. Balloon pulmonary angioplasty for the treatment of residual or recurrent pulmonary hypertension after pulmonary endarterectomy. Int J Cardiol 2019; 278: 232–237. doi: 10.1016/j.ijcard.2018.10.066 [DOI] [PubMed] [Google Scholar]
- 81.Shimura N, Kataoka M, Inami T, et al. Additional percutaneous transluminal pulmonary angioplasty for residual or recurrent pulmonary hypertension after pulmonary endarterectomy. Int J Cardiol 2015; 183: 138–142. doi: 10.1016/j.ijcard.2015.01.034 [DOI] [PubMed] [Google Scholar]
- 82.Yanaka K, Nakayama K, Shinke T, et al. Sequential hybrid therapy with pulmonary endarterectomy and additional balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. J Am Heart Assoc 2018; 7: e008838. doi: 10.1161/JAHA.118.008838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kovacs G, Herve P, Barbera JA, et al. An official European Respiratory Society statement: pulmonary haemodynamics during exercise. Eur Respir J 2017; 50: 1700578. doi: 10.1183/13993003.00578-2017 [DOI] [PubMed] [Google Scholar]
- 84.van Kan C, van der Plas MN, Reesink HJ, et al. Hemodynamic and ventilatory responses during exercise in chronic thromboembolic disease. J Thorac Cardiovasc Surg 2016; 152: 763–771. doi: 10.1016/j.jtcvs.2016.05.058 [DOI] [PubMed] [Google Scholar]
- 85.Guth S, Wiedenroth CB, Rieth A, et al. Exercise right heart catheterisation before and after pulmonary endarterectomy in patients with chronic thromboembolic disease. Eur Respir J 2018; 52: 1800458. doi: 10.1183/13993003.00458-2018 [DOI] [PubMed] [Google Scholar]
- 86.Donahoe L, Vanderlaan R, Thenganatt J, et al. Symptoms are more useful than echocardiography in patient selection for pulmonary endarterectomy. Ann Thorac Surg 2017; 104: 1179–1185. doi: 10.1016/j.athoracsur.2017.05.024 [DOI] [PubMed] [Google Scholar]
- 87.Yıldızeli ŞO, Kepez A, Taş S, et al. Pulmonary endarterectomy for patients with chronic thromboembolic disease. Anatol J Cardiol 2018; 19: 273–278. doi: 10.14744/AnatolJCardiol.2018.37929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wiedenroth CB, Olsson KM, Guth S, et al. Balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic disease. Pulm Circ 2018; 8: 2045893217753122. doi: 10.1177/2045893217753122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Inami T, Kataoka M, Kikuchi H, et al. Balloon pulmonary angioplasty for symptomatic chronic thromboembolic disease without pulmonary hypertension at rest. Int J Cardiol 2019; 289: 116–118. doi: 10.1016/j.ijcard.2019.04.080 [DOI] [PubMed] [Google Scholar]