Abstract
Black birthing people are twice as likely to experience severe maternal morbidity (SMM) as their white counterparts. Structural racism provides a framework for understanding root causes of perinatal health disparities. Our objective was to investigate associations between measures of structural racism and severe maternal morbidity (SMM) among Black birthing people in the US. We linked delivery hospitalizations for Black birthing people in the National Inpatient Sample (2008–2011) with data from the American Community Survey 2008 5-year estimates and the Vera Institute of Justice Incarceration Trends datasets (2008–2011). Structural racism measures included the Index of Concentration at the Extremes for race and income (i.e., racialized economic segregation) and Black-white incarceration inequality, assessed as quintiles by hospital county. Multilevel logistic regression assessed the relationship between these county-level indicators of structural racism and SMM. Black birthing people delivering in quintiles 5 (concentrated deprivation; OR=1.45, 95% CI = 1.16–1.81) and 3 (OR=1.27, 95% CI = 1.04–1.56) experienced increased odds of SMM compared to those in quintile 1 (concentrated privilege). After adjusting for individual characteristics, obstetric comorbidities, and hospital characteristics the odds of SMM remained elevated for Black birthing people delivering in quintiles 5 (aOR=1.32, 95% CI = 1.02–1.71) and 3 (aOR= 1.24, 95% CI = 1.02–1.51). Delivering in the quintile with the highest incarceration inequality (Q5) was not significantly associated with SMM (aOR=0.95, 95% CI = 0.72–1.25) compared to those delivering in counties with the lowest incarceration inequality (Q1). In this national-level study, racialized economic segregation was associated with SMM among Black birthing people. Our findings highlight the need to promote maternal and perinatal health equity through actionable policies that prioritize investment in communities experiencing deprivation.
Keywords: Structural Racism, Racialized Economic Segregation, Incarceration, Severe Maternal Morbidity, Black Maternal Health, Black Women, Pregnancy Complications
Introduction
Severe maternal morbidity (SMM), defined as highly preventable but unexpected outcomes of labor and birth that result in significant short- and long-term health consequences, has been steadily increasing in the US since 1998 (Callaghan et al., 2012). People with SMM experience severe complications (e.g., cardiac arrest, acute renal failure, eclampsia, sepsis) and/or receive interventions (e.g., assisted ventilation, hysterectomy, blood transfusion) during pregnancy, birth, or postpartum and are at increased risk of death (Centers for Disease Control and Prevention [CDC], 2021a). While increases in SMM have occurred across all racial groups, Black women and birthing people bear a disproportionate share of SMM across all stages of the perinatal continuum, from pregnancy to the postpartum period (CDC, 2021b). The incidence of severe maternal morbidity (SMM) among Black birthing people in the United States is about 231 per 10,000 delivery hospitalizations, two to three times the incidence compared to non-Hispanic white birthing people (Admon et al., 2018). Increasingly, research examining racial disparities in SMM has begun to highlight the role of structural racism in creating and sustaining these disparities (Giurgescu et al., 2022; Janevic et al., 2020; Taylor, 2020).
Structural racism includes the ways in which a society’s culture, institutions, history, ideology, and embedded practices combine to systematically disadvantage, oppress, and exclude historically marginalized racial and ethnic groups, thereby perpetuating inequity (Bailey et al., 2017; Williams & Mohammed, 2013). Structural racism is a root cause of health inequities for Black birthing people in the US where historical and ongoing systems of oppression intersect across race, class, and gender, pervading social and political norms, policies, and institutions (Williams & Mohammed, 2013; Crear-Perry et al., 2021). Ecosocial theory posits that exposure to structural racism impacts the health of Black people across the life course through the embodiment of social and ecological factors that may manifest in biological processes due to accumulated environmental exposures and/or degradations, stress, and social trauma (Krieger, 2012). Structural racism functions across ecosocial levels and operates through intersecting and mutually sustaining societal domains including income, housing, education, criminal justice, political participation, laws and public policy. Exposure to structural racism impacts the health of Black people across the life course through economic suppression that subjects families to the adverse health effects of poverty, racial residential segregation that concentrates poverty and undermines educational quality, lowered educational attainment from poorer quality schools, and racial inequality in the criminal justice system through police brutality and mass incarceration (Williams & Mohammed, 2013).
For this analysis we focus on two key dimensions of structural racism that adversely affect Black maternal, perinatal, and neonatal health outcomes – racialized economic segregation and Black-white incarceration inequality (Chambers et al., 2019; Huynh et al., 2018; Jahn et al., 2020; Janevic et al., 2020; Krieger et al., 2020, Sealy-Jefferson et al., 2020; Sonderlund et al., 2022; Wallace et al., 2015).
First, we examine racialized economic segregation, a measure of structural racism that jointly assesses racial segregation and concentrations of wealth and poverty (Krieger et al., 2016). Racialized economic segregation is driven by historical policies, such as redlining, that have concentrated wealth among white households and systematically excluded Black households from social and economic opportunity (Nardone et al., 2020). Racialized residential segregation and associated concentrations of poverty can create community environments characterized by underfunded and underperforming schools due to low homeownership, less green and pedestrian friendly spaces, food apartheid restricting access to healthy foods, environmental pollution, over policing, fewer health care facilities, and lower quality health care facilities due to underfunding associated with hospitals utilized by patients predominantly covered by public insurance (Krieger, 2012). These neighborhood characteristics become embodied over the lifespan through lowered lifetime earning potential and poverty, diminished access to healthful movement and foods, exposure to pollutants that contribute to chronic disease and inflammatory pathways, and inhibited access to high quality health care.
The Index of Concentration at the Extremes of Race and Income (ICERace-Income) is a measure of racialized economic segregation that has been found to be associated with adverse birth outcomes, cancer, premature and all-cause mortality, and communicable diseases (Sonderlund et al., 2022). The ICERace-Income measure reflects the extent to which an area’s population is concentrated into extremes of deprivation (Black low-income individuals) and privilege (white high-income individuals) (Krieger et al., 2016). While prior research has linked the ICERace-Income measure with poor maternal and perinatal outcomes (Chambers et al., 2019; Krieger et al., 2020), few studies have evaluated relationships between ICERace-Income and SMM (Harden et al., 2022; Janevic et al., 2020). In a 2020 study in New York City, researchers found that birthing people living in neighborhoods with the highest concentration of Black households with low income relative to white households with high income experienced excess SMM risk (Janevic et al., 2020). Another recent investigation found that living in a South Carolina neighborhood with higher concentrated deprivation increased the odds that Black women would reside in an area characterized by high levels of SMM (Harden et al., 2022)
Second, we investigate Black-white jail incarceration inequality, a measure of structural racism that focuses on racial disparities in the criminal justice system. Most individuals incarcerated in jails have not been convicted of a crime and are temporarily detained (Minton & Zheng, 2021). Black individuals are 3.6 times more likely to be incarcerated in jails than white people and this disparity reflects racially disproportionate practices in policing (e.g., search and arrests), prosecution (e.g., charges), and judicial decision-making (e.g., bail) that are often subject to county-level policies (Subramanian et al., 2018). Incarceration has significant community impacts (Dumont et al., 2013) including destabilizing communities via forced migration (Thomas & Torrone, 2011), increasing community stress (Roberts, 2004), decreasing public investment (Golembeski and Fullilove, 2008) and promoting crime as opposed to deterring it (Sampson and Loeffler, 2010). A recent review highlighted the significant and racially disparate adverse health effects of incarceration, including direct effects on the incarcerated person and indirect effects on family and household members of incarcerated people (Wildeman et al., 2017).
There are few investigations that examine the association between Black-white jail incarceration inequality and maternal health. Researchers investigating the association between county-level jail incarceration and preterm birth rates among Black and white women demonstrated that women living in areas with the highest incarceration rates experienced increased odds of preterm birth, with potentially more impact for young mothers (Jahn et al., 2020). However, investigators in one New York state study found that BW incarceration inequality was not significantly associated with SMM (Liu et al., 2019).
It is imperative that researchers develop a better understanding of how structural racism operates as a fundamental determinant of adverse maternal health outcomes, including SMM. Results from previous studies that examine the relationship between measures of structural racism and SMM have been generally limited to the New York area. While they provide important data, they may have limited generalizability. Few national data sources enable linkages between macro-level measures of structural racism and detailed hospital data needed to measure SMM. Here, we capitalize on one of the few data sources that meet these requirements, making this a novel and salient contribution to the literature.
Using linked national administrative data, we investigate how two different measures of county-level structural racism in delivery hospital counties are associated with SMM among Black birthing people in the US. We hypothesized that giving birth in a county with higher racialized economic segregation and a county with higher Black-white incarceration inequality would be associated with higher odds of SMM among Black birthing people.
Methods
Data source
We used the 2008–2011 National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (Agency for Healthcare Research and Quality, 2021). The 2008–2011 NIS is an all-payer inpatient claims database in the US that includes all discharges from a 20% sample of community hospitals in the US stratified by hospital census region or division, ownership/control, location/teaching, and bed size. Although there are more recent NIS data available, we end our study in 2011 because county-level identifiers, which were needed to link with measures of structural racism, were not included after this year.
Our data sources for measures of structural racism at the county level include the US Census American Community Survey (2007–2011), the Integrated Public Use Microdata Series (IPUMS) (Ruggles et al., n.d.), and the Vera Institute of Justice Incarceration Trends Dataset (Vera Institute of Justice, 2020). Data from these sources were merged with the NIS data using county federal information processing system (FIPS) codes. This study was deemed exempt by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Sample
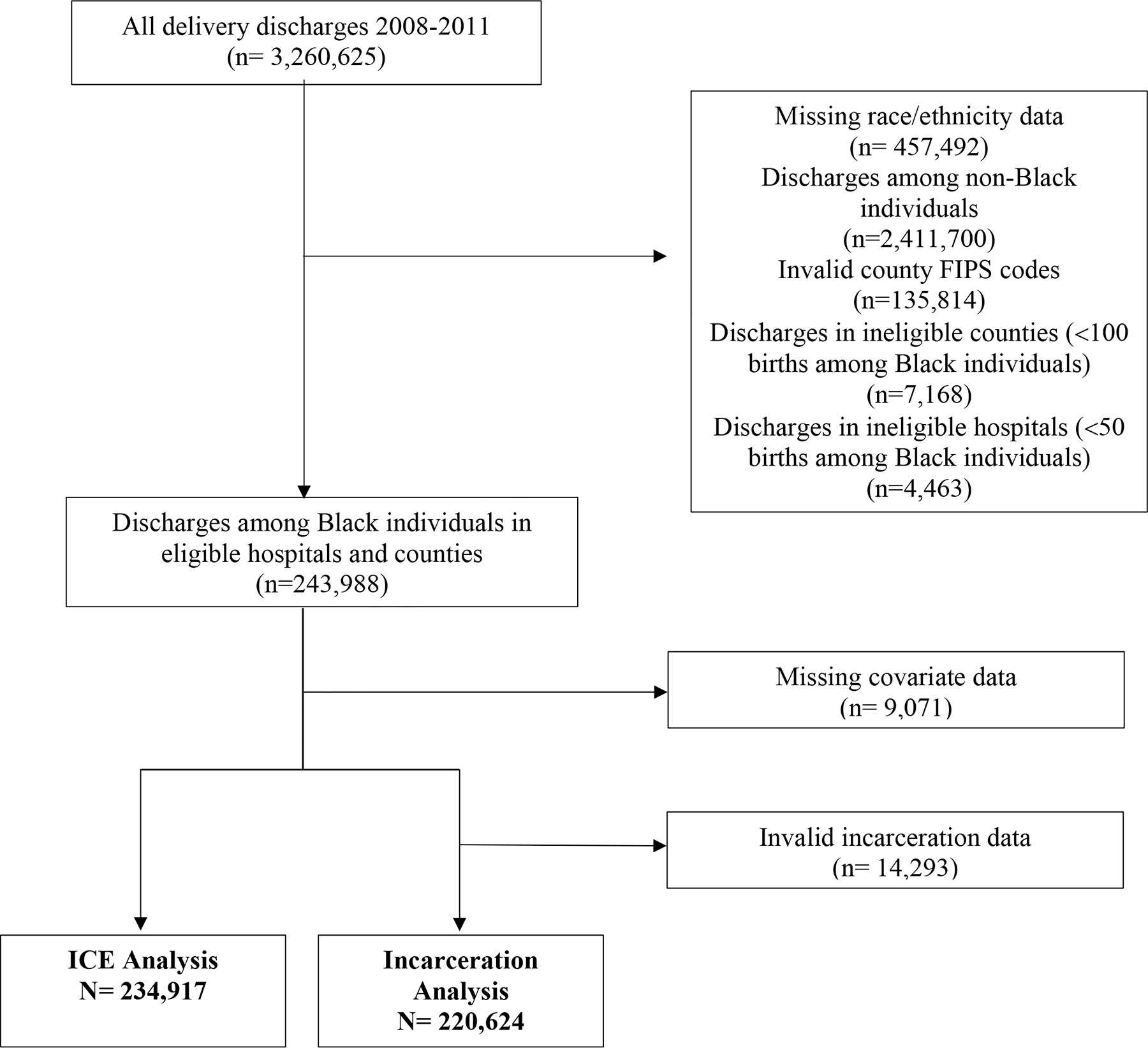
This study included all delivery hospitalizations among non-Hispanic Black people giving birth aged 11–55 years between 2008–2011 recorded in the NIS data. A validated algorithm was used to define delivery hospitalizations using International Classification of Diseases, 9th (ICD-9) procedure codes (Table S1) (Kuklina et al., 2008). Figure 1 depicts a flow diagram of the study sample. Discharges with missing race/ethnicity data were excluded. To obtain accurate standard errors within the multilevel model and ensure reliable SMM estimates, the sample was restricted to delivery discharges in hospitals with at least 50 births to Black birthing people and counties with at least 100 births to Black birthing people over the study period. We excluded discharges with missing county federal information processing system (FIPS) codes. We used two separate samples for each respective analysis because not all counties had similarly complete data for the ICERace-Income and BW incarceration inequality measures.
Figure 1. Flow diagram of study sample (National Inpatient Sample).
Severe maternal morbidity (SMM)
The primary outcome of interest was SMM using the Center for Disease Control and Prevention’s (CDC) index, identified by the presence of one or more ICD-9-CM organ dysfunction diagnosis or procedure codes using a validated algorithm (Table S2; Callaghan et al., 2012; CDC, 2021a). The most recent CDC index includes 21 indicators. One of these indicators, blood transfusion, comprises the majority of SMM cases but prior research indicates that this indicator is non-specific in identifying true obstetric hemorrhage and including it may artificially inflate SMM rates (Callaghan et al., 2012; Main et al., 2016). We conducted our analysis using both the standard SMM index to be comparable to prior studies (Brown et al., 2020; Meeker et al., 2021) and the modified SMM index without the blood transfusion indicator to be consistent with more recent research (Hirai et al., 2022).
Covariates
Demographic variables of interest included maternal age (<19, 20–24, 25–29, 30–34, 35–39, 40–44, and ≥45 years), expected primary payer (private, Medicare/Medicaid, other/uninsured), and quartile of median household income for patient’s ZIP Code (0–25, 26–50, 51–75, 76–100). Comorbidities were identified using a validated Obstetric Comorbidity Index, a weighted algorithm that assigns points for the presence of preexisting comorbidities, substance-related conditions, and pregnancy-related conditions with higher scores corresponding to worse health status (Bateman et al., 2013). In line with prior research, we modified the algorithm to remove ICD-9 codes for sickle cell disease and eclampsia that overlap with CDC SMM indicators (Table S3) (Main et al., 2020). We also removed advanced maternal age from the comorbidity index because we included age as a separate covariate in our model. Hospital characteristics identified by the NIS include urban/teaching status (rural, urban non-teaching, urban teaching), ownership (investor-owned, non-profit, or public), hospital bed size (small, medium, large), and census region (Northeast, South, Midwest, West). We also identified whether the delivery hospital was predominantly Black-serving if it was among the top 10% of hospitals with the highest proportion of Black birthing patients (Jha et al., 2007).
Measures of Structural Racism
Index of Concentration at the Extremes - Race and Income
We derived a modified version of the ICERace-Income measure using American Community Survey 5-year data from 2007–2011 from IPUMS (Ruggles et al., n.d.). The ICERace-Income measure assesses racialized economic segregation in terms of the concentration of Black populations in low-income households to White populations in high-income households. Prior investigators have defined low- and high-income households based on national income thresholds for the 20th and 80th household income percentiles in the US (Krieger et al., 2016). However, we calculated the ICERace-Income measure based on state-specific income thresholds, rather than national thresholds, for the 20th and 80th household income percentiles, similar to other studies (Casey et al., 2017). Using state-specific thresholds allows us to define low- and high-income households based on their local context. Thus, we account for regional differentials in income and cost of living, both of which are subject to local dynamics in labor force participation, unemployment, and educational attainment. The ICERace-Income is measured continuously and ranges from −1 (concentrated deprivation) to 1 (concentrated privilege). We calculated the ICERace-Income scores based on the county where the delivery hospital was located and then categorized scores into quintiles: quintile 1 (concentrated privilege) to quintile 5 (concentrated deprivation).
Black-white Incarceration Inequality
We extracted county-level jail incarceration data from the Vera Institute of Justice Incarceration Trends Dataset (Vera Institute of Justice, 2020). The Vera Institute of Justice collected and compiled incarceration data from the Census of Jails and the Annual Survey of Jails by the Bureau of Justice Statistics to generate annual county-level rates per 100,000 residents aged 15–64 years. We calculated the annual ratio of Black residents’ jail incarceration rate to that of white residents’ for each county where the delivery hospital was located and categorized the average of this rate ratio for the years 2008–2011 into quintiles: quintile 1 (low inequality) to quintile 5 (high inequality).
Unit of Analysis
In this study, we investigate the associations between SMM and racialized economic segregation and incarceration inequity at the county level. Counties are important geographic units of analysis given that many public and health policies are implemented at the county-level. Most jails are operated by counties and are subject to county-specific laws, policing norms, and criminal justice policies and practices (Subramanian et al., 2018). While there is some evidence that the ICERace-Income measure yields stronger associations at the smallest geographic units (e.g., census tracts), the measure is a consistent predictor of adverse maternal health outcomes at larger geographic units (e.g., county, zip code, state) (Chambers et al., 2018; Hunyh et al., 2018; Krieger et al., 2020; Thoma et al., 2019).
Statistical Analysis
We conducted descriptive statistics and bivariate analyses separately using samples specific to each structural racism measure for all individual-level, hospital-level, and structural racism variables to characterize the study population, the prevalence of SMM, and the distribution of structural racism. We applied individual discharge sampling weights and sampling strata to account for the NIS sample design.
We conducted three-level multilevel logistic regression models to assess the relationship between each county-level measure of structural racism and SMM with individuals nested within hospitals and hospitals nested within counties. A separate analysis was performed for each structural racism measure. We modeled the relationship between our structural racism measures and SMM using sequential nested models, an approach commonly used in the social sciences (Hayward et al., 2004; Leonard et al., 2019). In this approach, we first estimate a baseline model with no covariates and then sequentially add theoretically-based covariate groupings in nested models. This approach allowed us to see whether adjusting for covariates, which could be on the causal pathway between structural racism and SMM, attenuate the association between each structural racism measure and SMM. Model 1 assessed the crude association between each measure of structural racism and SMM. Model 2 adds individual-level characteristics, such as age and insurance status. Model 3 adds a measure of comorbid obstetric conditions, and Model 4, our final and fully adjusted model, adds hospital characteristics.
We calculated the intraclass correlation coefficient for our multilevel logistic regression models. The intraclass correlation coefficients for the null model for the ICE analysis was 7.0% and 4.0% for SMM and non-transfusion SMM, respectively. The intraclass coefficients for the null model for the incarceration inequality analysis was 7.0% and 3.4% for SMM and non-transfusion SMM, respectively. Given the low intraclass correlations, we also ran 1-level logistic regression models. The results between the two models were not substantially different but given the clustered organization of the data we display the results of the multilevel models. We considered p values <0.05 to be statistically significant. All statistical analyses were performed in Stata 17/BE.
Results
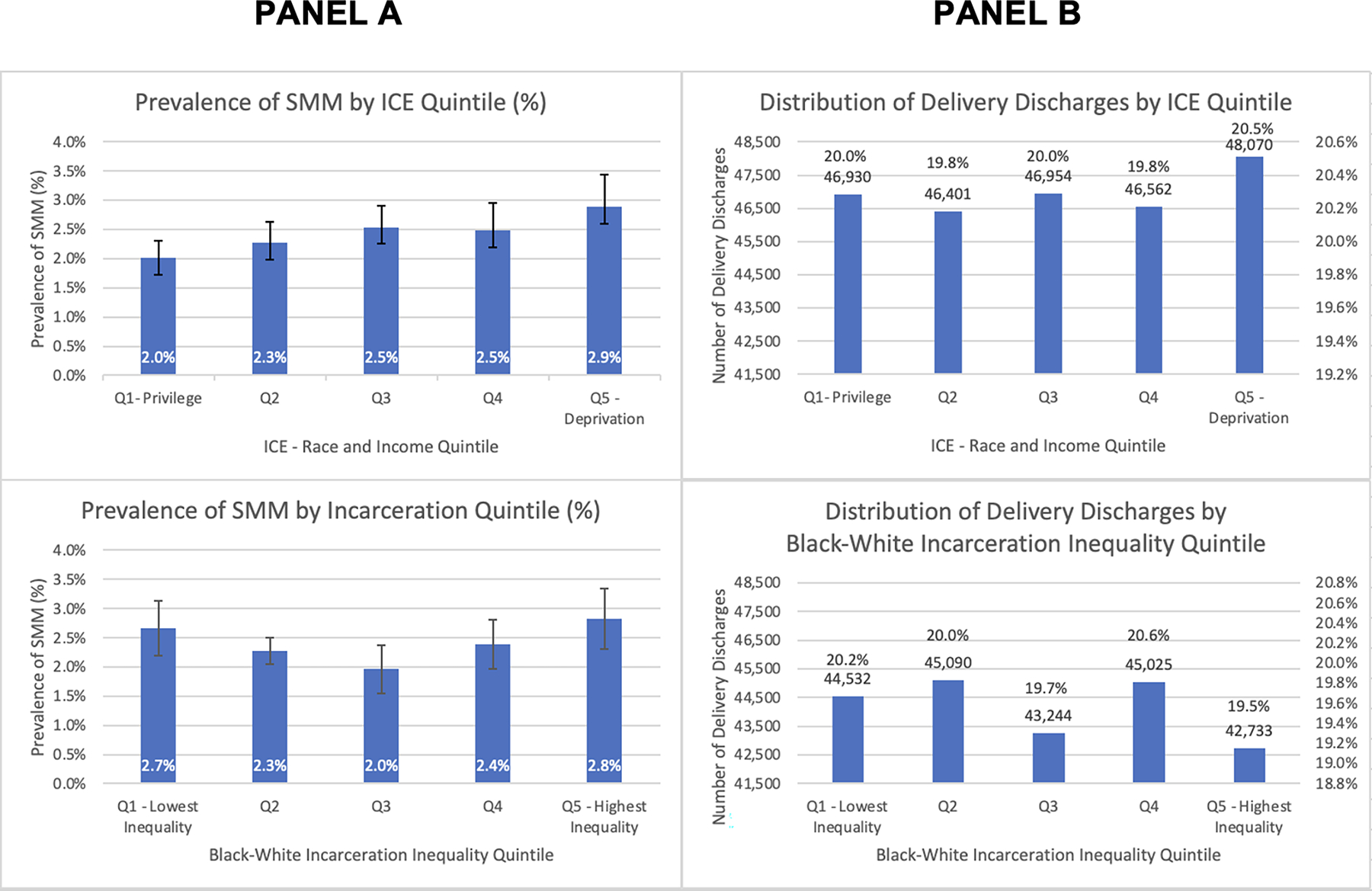
The study samples included 234,917 deliveries in the ICERace-Income analysis and 220,624 deliveries in the BW Incarceration Inequality analysis. Overall, 2.4% of all discharges among Black birthing people in both samples experienced SMM between 2008–2011. In ICERace-Income quintile 1 (concentrated privilege), 2.0 percent of the sample experienced SMM. This rate generally increased across quintiles with 2.9 percent of Black birthing people in quintile 5 (concentrated deprivation) experiencing SMM (see Figure 2). We observed a U-shaped pattern between the BW Incarceration measure and SMM. SMM prevalence was highest in quintile 5 (highest inequality; 2.8%) and quintile 1 (lowest inequality; 2.7%) and lowest in quintile 3 (2.0%).
Figure 2. Panel A - Distribution of Delivery Charges of Black Birthing People by Quintile. Panel B- Prevalence of SMM among Black Birthing People by Structural Racism Measure Quintile.
Sociodemographic and hospital characteristics of the overall samples and by the lowest and highest quintile of each structural racism measure are displayed in Table 1. The overall distribution of characteristics was similar across both structural racism measures. The majority of both samples were less than 35 years old, utilized public insurance as the expected primary payer, and had household income levels in the bottom two quartiles for their zip code. Over 40% of both samples had one or more comorbidities. Most births in both samples occurred in hospitals designated as urban teaching hospitals, with nonprofit ownership, large bed size, and located in the US Census South region. Approximately one-third of each sample gave birth in a predominantly Black-serving hospital.
Table 1.
Individual and Hospital Characteristics among Delivery Discharges of Black Birthing People by Structural Racism Measure, United States (2008–2011)
| ICE Quintile | Black-white Incarceration Quintile | |||||
|---|---|---|---|---|---|---|
| Total No., (%) (ICE) | Quintile 1 (Concentrated Privilege) % |
Quintile 5 (Concentrated Deprivation) % |
Total No., (%) (INC) | Quintile 1 (Low Inequality) % |
Quintile 5 (High Inequality) % |
|
| N=234,917 | (n=46,930) | (n=48,070) | N=220,624 | (n=44,532) | (n=42,733) | |
|
| ||||||
| SMM (% of total births) | 5,714 (2.4%) | 2.0% | 2.9% | 5,332 (2.4%) | 2.8% | 2.7% |
| Non-Transfusion SMM (% of total births) | 2,272 (1.0%) | 0.8% | 1.1% | 2,146 (0.9%) | 2.1% | 1.9% |
| Individual-level characteristics (column %) | ||||||
| Age | ||||||
| <20 | 33,932 (14.5) | 14.1% | 16.7% | 32,214 (14.6) | 14.7% | 15.7% |
| 20–24 | 70,769 (30.1) | 29.1% | 32.5% | 67,077 (30.4) | 31.3% | 29.4% |
| 25–29 | 59,278 (25.2) | 25.2% | 24.7% | 55,482 (25.1) | 25.6% | 24.5% |
| 30–34 | 42,412 (18.1) | 18.7% | 15.8% | 39,491 (17.9) | 17.3% | 17.9% |
| 35–39 | 22,188 (9.5) | 10.0% | 7.9% | 20,545 (9.3) | 8.8% | 9.6% |
| 40–44 | 5,886 (2.5) | 2.7% | 2.2% | 5,408 (2.5) | 2.3% | 2.6% |
| >=45 | 452 (0.2) | 0.3% | 0.2% | 407 (0.2) | 0.2% | 0.2% |
| Household Income Quartile by Patient’s Zip Code | ||||||
| Quartile 1 - Highest income | 37,425 (15.9) | 23.9% | 5.3% | 36,409 (16.5) | 8.6% | 13.9% |
| Quartile 2 | 45,513 (19.3) | 17.8% | 14.1% | 42,858 (19.4) | 16.2% | 19.2% |
| Quartile 3 | 50,563 (21.5) | 22.1% | 16.5% | 48,505 (21.9) | 23.9% | 23.1% |
| Quartile 4 - Lowest income | 101,416 (43.3) | 36.1% | 64.2% | 92,852 (42.2) | 51.2% | 43.8% |
| Payer | ||||||
| Private | 81,110 (34.5) | 34.3% | 23.1% | 77,163 (34.9) | 28.9% | 37.0% |
| Public | 143,570 (61.2) | 61.7% | 71.5% | 133,949 (60.8) | 65.4% | 58.4% |
| Other | 10,237 (4.3) | 4.1% | 5.5% | 9,512 (4.3) | 5.8% | 4.5% |
| Comorbidity | ||||||
| 0 | 135,681 (57.7) | 58.5% | 56.4% | 127,432 (57.8) | 59.2% | 56.9% |
| 1 | 53,886 (22.9) | 22.9% | 22.9% | 50,626 (22.9) | 22.8% | 22.8% |
| 2 or more | 45,350 (19.3) | 18.6% | 20.7% | 42,56 (19.3) | 18.1% | 20.3% |
| Hospital-level characteristics (column %) | ||||||
| Hospital Location/Teaching | ||||||
| Rural | 11,668 (4.8) | 4.4% | 10.3% | 11,668 (5.1) | 9.4% | 0.8% |
| Urban - nonteaching | 74,483 (31.8) | 39.1% | 12.5% | 73,772 (33.5) | 44.2% | 21.4% |
| Urban - teaching | 148,766 (63.4) | 56.5% | 77.2% | 135,184 (61.4) | 46.5% | 77.8% |
| Hospital Ownership | ||||||
| Private - Investor Owned | 25,900 (11.5) | 6.1% | 16.6% | 25,900 (12.2) | 20.2% | 2.9% |
| Private - Nonprofit | 173,302 (73.7) | 79.2% | 61.6% | 160,168 (72.5) | 46.4% | 85.3% |
| Public | 35,715 (14.9) | 14.7% | 21.9% | 34,556 (15.3) | 33.4% | 11.8% |
| Hospital Bed Size | ||||||
| Small | 19,523 (7.5) | 8.1% | 7.7% | 17,883 (7.3) | 7.6% | 11.6% |
| Medium | 56,958 (24.2) | 24.6% | 14.8% | 51,773 (23.4) | 15.1% | 28.5% |
| Large | 158,436 (68.3) | 77.5% | 77.5% | 150,968 (69.3) | 77.4% | 59.9% |
| Hospital Region | ||||||
| Northeast | 60,281 (26.4) | 38.2% | 39.3% | 46,137 (21.7) | 0.0% | 37.0% |
| Midwest | 22,228 (9.5) | 9.7% | 0.0% | 22,228 (10.1) | 0.0% | 38.1% |
| South | 119,748 (50.4) | 39.8% | 60.8% | 119,599 (53.7) | 94.6% | 21.8% |
| West | 32,660 (13.6) | 12.2% | 0.0% | 32,660 (14.5) | 5.4% | 3.1% |
| Predominantly Black Serving | ||||||
| No | 156,710 (84.4) | 100.0% | 50.2% | 146,295 (65.9) | 87.6% | 79.5% |
| Yes | 78,207 (15.6) | 0.0% | 49.8% | 74,329 (34.1) | 12.4% | 20.5% |
Relationship between ICERace-Income and SMM
Table 2 presents the results of our logistic regression models using ICERace-Income as the main independent variable. In the unadjusted model (model 1), Black birthing people in ICERace-Income quintile 5 (most deprived) experienced 1.5 times the odds of SMM compared to those in quintile 1 (OR = 1.45, 95% CI = 1.16–1.81). Black birthing people in quintile 3 were 1.27 times as likely to experience SMM compared to Black birthing people in quintile 1 (OR = 1.27, 95% CI = 1.04–1.56). Those in quintiles 2 and 4 also had elevated odds but these were not significant at p<0.05.
Table 2.
Odds ratios and 95% confidence interval for the association between severe maternal morbidity and ICERace-Income
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | |
| OR (CI) | OR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | |
|
| ||||||||
| ICE Quintile | ||||||||
| Q1 – Concentrated Privilege | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Q2 | 1.13 (0.93–1.39) | 1.28 (1.04–1.56)* | 1.15 (0.94–1.40) | 1.28 (1.05–1.56)* | 1.14 (.94–1.39) | 1.28 (1.06–1.53)* | 1.13 (0.92–1.38) | 1.24 (1.03–1.49)* |
| Q3 | 1.27 (1.04–1.56)* | 1.22 (0.99–1.48) | 1.28 (1.05–1.56)* | 1.22 (1.00–1.48)* | 1.26 (1.04–1.53)* | 1.19 (0.99–1.42) | 1.24 (1.02–1.51)* | 1.11 (0.93–1.33) |
| Q4 | 1.14 (0.93–1.42) | 1.03 (0.83–1.27) | 1.16 (0.94–1.43) | 1.04 (0.85–1.28) | 1.13 (0.92–1.39) | 1.02 (0.84–1.23) | 1.11 (0.90–1.38) | 0.98 (0.81–1.20) |
| Q5 – Concentrated Deprivation | 1.45 (1.16–1.81)** | 1.31 (1.06–1.62)* | 1.45 (1.16–1.80)* | 1.36 (1.10–1.68)* | 1.42 (1.14–1.76)** | 1.31 (1.08–1.59)* | 1.32 (1.02–1.71)* | 1.21 (0.97–1.52) |
| Individual-level characteristics | ||||||||
| Age | ||||||||
| <20 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| 20–24 | 1.03 (0.94–1.13) | 1.04 (0.89–1.21) | 0.95 (0.87–1.05) | 0.98 (0.84–1.14) | 0.95 (0.87–1.05) | 0.97 (0.83–1.14) | ||
| 25–29 | 1.17 (1.06–1.28)** | 1.29 (1.10–1.50)*** | 0.99 (0.90–1.09) | 1.12 (0.95–1.30) | 0.99 (0.90–1.09) | 1.11 (0.95–1.30) | ||
| 30–34 | 1.49 (1.35–1.64) *** | 1.79 (1.53–2.09) *** | 1.17 (1.05–1.29)** | 1.42 (1.21–1.68)*** | 1.17 (1.06–1.29)** | 1.41 (1.20–1.65)*** | ||
| 35–39 | 1.83 (1.65–2.05) *** | 2.28 (1.92–2.70)*** | 1.33 (1.19–1.48)*** | 1.67 (1.40–1.98)*** | 1.33 (1.18–1.48)*** | 1.65 (1.38–1.96)*** | ||
| 40–44 | 2.48 (2.14–2.88) *** | 3.08 (2.46–3.85)*** | 1.68 (1.45–1.95)*** | 2.08 (1.67–2.61)*** | 1.67 (1.44–1.95)*** | 2.05 (1.63–2.57)*** | ||
| >=45 | 2.90 (1.90–4.42) *** | 2.27 (1.06–4.86)** | 1.77 (1.16–2.72) | 1.34 (0.62–2.88) | 1.77 (1.15–2.71)** | 1.32 (0.61–2.83) | ||
| Income Quartile by Zip Code | ||||||||
| Quartile 1 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Quartile 2 | 0.95 (0.86–1.05) | 0.93 (0.80–1.07) | 0.94 (0.85–1.04) | 0.91 (0.79–1.05) | 0.94 (0.85–1.03) | 0.91 (0.79–1.05) | ||
| Quartile 3 | 1.03 (0.93–1.15) | 0.96 (0.82–1.11) | 1.00 (0.90–1.11) | 0.92 (0.80–1.07) | 1.00 (0.90–1.11) | 0.92 (0.79–1.07) | ||
| Quartile 4 | 1.06 (0.95–1.17) | 0.93 (0.81–1.08) | 1.00 (0.90–1.10) | 0.87 (0.76–1.00) | 0.99 (0.90–1.10) | 0.86 (0.74–0.99) | ||
| Payer | ||||||||
| Private | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Public | 1.25 (1.17–1.33)*** | 1.12 (1.01–1.23)* | 1.18 (1.10–1.25)*** | 1.05 (0.95–1.15) | 1.17 (1.10–1.25)*** | 1.03 (0.94–1.14) | ||
| Other | 1.20 (1.05–1.37)** | 1.08 (0.87–1.33) | 1.18 (1.02–1.35)* | 1.04 (0.85–1.28) | 1.17 (1.03–1.34)** | 1.03 (0.84–1.27) | ||
| Comorbidity | ||||||||
| 0 | Ref. | Ref. | Ref. | Ref. | ||||
| 1 | 1.90 (1.77–2.04)*** | 1.47 (1.30–1.65)*** | 1.90 (1.77–2.04)*** | 1.46 (1.30–1.65)*** | ||||
| 2 or more | 4.77 (4.48–5.08)*** | 5.26 (4.79–5.79)*** | 4.75 (4.46–5.06)*** | 5.16 (4.69–5.68)*** | ||||
| Hospital-level characteristics | ||||||||
| Hospital Location/Teaching | ||||||||
| Rural | Ref. | Ref. | ||||||
| Urban - nonteaching | 1.21 (0.94–1.56) | 1.09 (0.83–1.43) | ||||||
| Urban - teaching | 1.31 (1.01–1.69) | 1.50 (1.15–1.97)** | ||||||
| Hospital Ownership | ||||||||
| Private - Investor Owned | Ref. | Ref. | ||||||
| Private - Nonprofit | 1.02 (0.85–1.23) | 1.04 (0.86–1.26) | ||||||
| Government | 1.06 (0.85–1.33) | 1.06 (0.85–1.32) | ||||||
| Hospital Bed Size | ||||||||
| Small | Ref. | Ref. | ||||||
| Medium | 1.27 (1.02–1.59)*** | 1.45 (1.15–1.82)** | ||||||
| Large | 1.46 (1.19–1.79)*** | 1.63 (1.31–2.01)*** | ||||||
| Hospital Region | ||||||||
| Northeast | Ref. | Ref. | ||||||
| Midwest | 0.95 (0.73–1.24) | 0.99 (0.75–1.30) | ||||||
| South | 0.98 (0.82–1.18) | 1.20 (1.03–1.40)** | ||||||
| West | 0.90 (0.72–1.12) | 1.19 (0.98–1.45) | ||||||
| Predominantly Black Serving | ||||||||
| No | Ref. | Ref. | ||||||
| Yes | 1.11 (0.93–1.33) | 1.05 (0.89–1.22) | ||||||
Notes:
p<0.05
p<0.01
p<0.001
Adjusting for individual characteristics (model 2), ICERace-Income remained significantly associated with SMM for birthing people who gave birth in both quintile 3 (aOR = 1.28, 95% CI = 1.05–1.56) and quintile 5 (aOR = 1.45, 95% CI = 1.16–1.80). After adjusting for individual characteristics and obstetric comorbidities (model 3), Black birthing people who gave birth in quintile 3 (aOR = 1.26, 95% CI = 1.04–1.53) and quintile 5 (aOR = 1.42, 95% CI = 1.14–1.76) continued to experience elevated odds of SMM. In model 4, which adjusted for individual characteristics, obstetric comorbidities, and hospital characteristics, Black birthing people who gave birth in quintiles 3 (aOR = 1.24, 95% CI = 1.02–1.51) and 5 (aOR = 1.32; 95%CI = 1.02–1.71) had significantly higher odds of SMM compared to Black birthing people who gave birth in quintile 1; odds ratios for quintiles 2 and 4 also indicated increased odds of SMM compared to quintile 1, but were non-significant.
Similar patterns were observed in the association between ICERace-Income and non-transfusion SMM. In an unadjusted model (model 1), Black birthing people who gave birth in ICERace-Income quintile 2 (OR = 1.28, 95% CI = 1.04–1.56) and quintile 5 (OR = 1.31, 95% CI = 1.06–1.62) were at increased odds of experiencing non-transfusion SMM compared to Black birthing people who gave birth in quintile 1. When adjusting for individual characteristics, birthing people who gave birth in quintiles 2 (aOR = 1.28, 95% CI = 1.05–1.56), 3 (aOR = 1.22, 95% CI = 1.00–1.48), and 5 (aOR = 1.36, 95% CI = 1.10–1.68) were at increased odds of experiencing non-transfusion SMM compared to birthing people who gave birth in quintile 1. Adjusting for individual characteristics and obstetric comorbidities, birthing people who gave birth in quintiles 2 (aOR = 1.28, 95% CI = 1.06–1.53) and 5 (aOR = 1.31, 95% CI = 1.08–1.59) were at increased odds of experiencing non-transfusion SMM compared to those in quintile 1. However, these relationships partially attenuated after adjustment for hospital characteristics (model 4); Black birthing people who gave birth in quintile 2 (aOR=1.24; 95% CI = 1.03–1.49) were at increased odds of experiencing non-transfusion SMM compared to those who gave birth in quintile 1.
Relationship between Black-white Incarceration Inequality and SMM
Table 3 presents the results of our logistic regression models using BW incarceration inequality as the main independent variable. In the crude model, Black birthing people in all quintiles exhibited decreased odds of SMM. These relationships were not significant at p<0.05. Adjusting for individual characteristics in model 2, individual characteristics and obstetric comorbidities in model 3, and hospital characteristics in model 4 produced similar results. There were no significant associations between Black-white incarceration inequality and non-transfusion SMM.
Table 3.
Odds ratios and 95% confidence interval for the association between severe maternal morbidity and Black–white Incarceration Inequality
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | SMM | Non-Transfusion SMM | |
| OR (CI) | OR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | AOR (CI) | |
|
| ||||||||
| Black white Incarceration Inequality | ||||||||
| Q1- Lowest inequality | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Q2 | 0.89 (.71–1.12) | 0.94 (0.75–1.19) | 0.91 (0.72–1.14) | 0.95 (0.76–1.20) | 0.86 (0.69–1.08) | 0.90 (0.73–1.10) | 0.87 (0.70–1.10) | 0.89 (0.72–1.09) |
| Q3 | 0.86 (0.68–1.08) | 0.98 (0.78–1.24) | 0.87 (0.69–1.10) | 0.97 (0.78–1.22) | 0.82 (0.66–1.03) | 0.92 (0.75–1.13) | 0.85 (0.67–1.08) | 0.93 (0.75–1.15) |
| Q4 | 0.95 (0.74–1.20) | 1.06 (0.84–1.33) | 0.94 (0.74–1.20) | 1.01 (0.80–1.27) | 0.88 (0.70–1.10) | 0.94 (0.77–1.16) | 0.86 (0.66–1.12) | 0.93 (0.74–1.17) |
| Q5- Highest Inequality | 0.98 (0.78–1.22) | 1.03 (0.82–1.29) | 0.98 (0.78–1.22) | 0.99 (0.79–1.24) | 0.93 (0.75–1.15) | 0.93 (0.76–1.14) | 0.95 (0.72–1.25) | 0.99 (0.78–1.27) |
| Individual-level characteristics | ||||||||
| Age | ||||||||
| <20 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| 20–24 | 1.01 (0.92–1.11) | 1.01 (0.87–1.18) | 0.94 (0.85–1.03) | 0.95 (0.81–1.11) | 0.93 (0.85–1.03) | 0.94 (0.89–1.10) | ||
| 25–29 | 1.13 (1.03–1.25)** | 1.25 (1.07–1.29)** | 0.96 (0.87–1.06) | 1.08 (0.93–1.27) | 0.96 (0.87–1.06) | 1.08 (0.92–1.26) | ||
| 30–34 | 1.45 (1.31–1.61)*** | 1.77 (1.51–2.08)*** | 1.14 (1.03–1.26)** | 1.40 (1.19–1.65)*** | 1.13 (1.02–1.26)** | 1.39 (1.18–1.63)*** | ||
| 35–39 | 1.78 (1.59–1.99)*** | 2.23 (1.87–2.65)*** | 1.28 (1.15–1.44)*** | 1.63 (1.36–1.94)*** | 1.28 ((1.14–1.44)*** | 1.60 (1.34–1.91)*** | ||
| 40–44 | 2.49 (2.14–2.91)*** | 3.07 (2.43–3.86)*** | 1.68 (1.44–1.96)*** | 2.07 (1.64–2.61)*** | 1.67 (1.43–1.96) *** | 2.03 (1.61–2.57)*** | ||
| >=45 | 2.93 (1.89–4.56)*** | 2.09 (0.92–4.75) | 1.77 (1.13–2.77)** | 1.22 (0.54–2.79) | 1.77 (1.13–2.77) | 1.19 (0.53–2.73) | ||
| Income Quartile by Zip Code | ||||||||
| Quartile 1 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Quartile 2 | 0.92 (0.83–1.01) | 0.92 (0.79–1.06) | 0.90 (0.82–1.00) | 0.90 (0.78–1.04) | 0.90 (0.82–0.99)* | 0.90 (0.77–1.04) | ||
| Quartile 3 | 1.01 (0.91–1.12) | 0.95 (0.82–1.11) | 0.98 (0.88–1.09) | 0.92 (0.79–1.07) | 0.97 (0.87–1.08) | 0.91 (0.78–1.06) | ||
| Quartile 4 | 1.05 (0.94–1.16) | 0.94 (0.81–1.09) | 0.98 (0.89–1.09) | 0.87 (0.75–1.01) | 0.97 (0.88–1.08) | 0.85 (0.74–0.99)** | ||
| Payer | ||||||||
| Private | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Public | 1.25 (1.17–1.34)*** | 1.12 (01.01–1.24)* | 1.18 (1.10–1.26)*** | 1.05 (0.95–1.16) | 1.18 (1.10–1.26) | 1.04 (0.94–1.15) | ||
| Other | 1.21 (1.06–1.39)* | 1.08 (0.87–1.34) | 1.19 (1.03–1.36)** | 1.05 (0.85–1.30) | 1.19 (1.03–1.36) | 1.04 (0.85–1.30) | ||
| Comorbidity | ||||||||
| 0 | Ref. | Ref. | Ref. | Ref. | ||||
| 1 | 1.88 (1.75–2.03)*** | 1.44 (1.27–1.63)*** | 1.88 (1.75–2.03)*** | 1.43 (1.27–1.62)*** | ||||
| 2 or more | 4.73 (4.43–5.05)*** | 5.19 (4.70–5.72)*** | 4.72 (4.42–5.03)*** | 5.08 (4.61–5.61)*** | ||||
| Hospital-level characteristics | ||||||||
| Hospital Location/Teaching | ||||||||
| Rural | Ref. | Ref. | ||||||
| Urban - nonteaching | 1.20 (0.93–1.50) | 1.07 (0.82–1.41) | ||||||
| Urban - teaching | 1.32 (1.02–1.71) | 1.52 (1.16–2.00)** | ||||||
| Hospital Ownership | ||||||||
| Private - Investor Owned | Ref. | Ref. | ||||||
| Private - Nonprofit | 1.02 (0.84–1.24) | 1.03 (0.85–1.24) | ||||||
| Public | 1.04 (0.82–1.30) | 1.00 (0.80–1.25) | ||||||
| Hospital Bed Size | ||||||||
| Small | Ref. | Ref. | ||||||
| Medium | 1.23 (0.97–1.55) | 1.37 (1.08–1.74) | ||||||
| Large | 1.39 (1.12–1.72) | 1.56 (1.25–1.94)*** | ||||||
| Hospital Region | ||||||||
| Northeast | Ref. | Ref. | ||||||
| Midwest | 0.90 (0.68–1.18) | 0.87 (0.65–1.16) | ||||||
| South | 1.00 (0.79–1.26) | 1.23 (1.01–1.50)* | ||||||
| West | 0.95 (0.74–1.21) | 1.18 (0.94–1.48) | ||||||
| Predominantly Black Serving | ||||||||
| No | Ref. | Ref. | ||||||
| Yes | 1.20 (1.02–1.42) | 1.06 (0.92–1.22) | ||||||
Notes:
p<0.05
p<0.01
p<0.001
Discussion and Conclusions
Researchers are increasingly investigating the role of structural racism as a root cause of poor perinatal health outcomes among Black birthing people (Chambers et al., 2019; Chambers et al., 2018; Liu et al., 2019). Our study contributes to this growing body of research by testing the association between SMM and two measures of county-level structural racism– the Index of Concentration at the Extremes of Race and Income and Black-white incarceration inequality in a national sample.
Black birthing people who gave birth in a county with higher levels of concentrated deprivation (ICERace-Income quintiles 5 and 3) had higher odds of experiencing SMM than those giving birth in a county with concentrated privilege (ICERace-Income quintile 1), even after adjusting for individual characteristics, obstetric comorbidities, and hospital characteristics. We also found that Black birthing people who gave birth in a county with higher levels of concentrated deprivation (ICERace-Income quintiles 5 and 2) had higher odds of experiencing non-transfusion SMM than those giving birth in a county with concentrated privilege (ICERace-Income quintile 1), even after adjusting for individual characteristics and obstetric characteristics. Adjusting for hospital-level characteristics (urban/teaching status, ownership, and hospital bed size and census region) partially attenuates this relationship. These results support the role of structural racism in predicting poor perinatal health outcomes for Black birthing people. Our findings are consistent with previous findings from state-based studies that find a relationship between ICERace-Income and SMM, preterm birth, infant mortality, and maternal death (Chambers et al., 2019; Hunyh et al., 2018, Janevic et al., 2020; Krieger at al., 2020). Our study expands the evidence by estimating the association between racialized economic segregation with SMM in a large population-based sample of Black delivery discharges in the US, which to our knowledge had not been evaluated in prior research.
Our findings suggest that hospital-level characteristics may mediate the relationship between racialized economic segregation and non-transfusion SMM among Black birthing people. This result is important to consider given recent research by Janevic and colleagues in which they demonstrated that the delivery hospital was responsible for at least 35% of the difference between Black and white SMM rates in New York City (2020) and suggest that the hospital is a potential pathway through which structural racism creates racial disparities in very preterm birth (2021). Hospital quality is a product of various systems of structural racism such as redlining, carceral system and law enforcement exposure. This may constrain access to high-quality healthcare throughout the perinatal continuum for Black birthing people (Adkins-Jackson et al., 2021; Mendez et al., 2011). Community-level structural racism may result in under-resourced hospitals with staffing and infrastructure constraints, lack of proactive transferring, limited 24-hour on-site anesthesiology, and high hospital volume (Howell et al., 2016). While measurement efforts around structural racism continue to grow, it is critical to expand macro-level assessments of hospital quality at county, community, and facility levels, including quality metrics reported by race and ethnicity (Crear-Perry et al., 2020), to better understand drivers of lower care quality and worse maternity outcomes in facilities serving Black birthing people. These assessments are critical to inform place-based interventions to tackle the segregation of birthing care, as well as better support Black-serving hospitals.
We found no significant relationship between BW incarceration inequality and SMM. Although our results differ from prior studies that found a positive association between county-level incarceration and preterm birth (Dyer et al., 2019; Jahn et al., 2020), they are consistent with studies that demonstrate no significant relationship between the measure of BW incarceration inequality and SMM (Liu et al., 2019) and BW prison incarceration and infant mortality (Wallace et al., 2017). However, recent research supports the idea that a unidimensional measure of racial inequality in incarceration may be an insufficient proxy for structural racism (Wallace et al., 2015). Wallace and colleagues (2015) found that women living in areas with both high racial inequality in incarceration and income inequality were at higher risk of having a small for gestational birth, though this increased risk was not observed among women living in areas with high incarceration inequality but low-income inequality. Another potential explanation for our findings may be due to poor validity of the measure. The validity of the measure may have been affected by limited area-level variation in ratios in Black-white incarceration inequality (Sealy-Jefferson et al., 2020) or inaccurate measurement of race among individuals incarcerated in jails (Subramanian et al., 2018). Moreover, although Black individuals bear the burden of persistent racial disparities in jail incarceration, the incarceration of white individuals has been increasing steadily since 2000, which could impact the measure’s validity (Subramanian et al., 2018). Taken together, these considerations suggest that further development of a measure of structural racism that incorporates racial inequality in incarceration is warranted.
There are some limitations to note. We used delivery data from 2008–2011, though we note that there are no national-level data sources that include data after 2011 that would allow us to examine relationships between structural racism and SMM. Future research could leverage more recent claims data from specific populations (e.g., Medicaid claims data or private insurance claims data) to further evaluate this important research question. Given that the NIS is an administrative dataset intended for billing purposes, it lacks detailed information on individual and hospital characteristics, clinical severity of SMM conditions, and obstetric history (e.g., parity, prior cesareans). Because 14% of the NIS delivery hospitalization records in our study do not include information on race/ethnicity, we may not have captured all deliveries among Black individuals, and it is possible that these data could be missing for systematic reasons. Additionally, prior to 2015, the NIS organizes “race” and “Hispanic” ethnicity as mutually exclusive categories. Hispanic ethnicity takes precedence over race in NIS data coding, so we were unable to include births among Black Hispanic birthing people in our analysis. The NIS also does not include information about nativity status (i.e., foreign-born vs. US-born), thus limiting our ability to examine heterogeneity in the associations between structural racism and SMM among Black birthing people. Other than median household income in the patient’s zip code, we did not have key contextual information on the individuals’ neighborhood (e.g., racial residential segregation, economic inequality, or incarceration), thus limiting our ability to understand the contextual interplay between where individuals live and where they give birth in determining their SMM risk. Notably, we also did not have data on technical or experiential quality of care to assess relationships between hospital county-level structural racism and hospital quality of care experiences.
Another potential limitation is that although our findings suggest a possible mediating effect by hospital characteristics, we did not conduct a causal mediation analysis. Nonetheless, there is strong evidence for the role of hospital characteristics in mediating the relationship between structural racism and maternal health outcomes (Janevic et al., 2020; Janevic et al., 2021). Future research is needed to further investigate these relationships. Additionally, in conducting our analyses at the county-level, it is possible we are missing some salient variation in the ICE and incarceration measures that may be captured in smaller geographical units, as has been found in recent research relating ICE and disparities in child health (Krieger et al., 2018). Finally, while our study focused on two individual measures of structural racism, a small but growing number of researchers (Alvarez, 2022; Chantarat et al., 2021; Dougherty et al., 2020) are testing novel multidimensional measures that better capture the interconnectedness and mutual reinforcement that define structural racism. We did not have access to publicly available multidimensional measures, but this will be an important area for future inquiry.
The US maternal health crisis cannot be addressed without achieving maternal health equity. Previous efforts to address longstanding racial disparities in perinatal health have largely focused on individual risk behaviors, yet these approaches fail to account for structural determinants that shape access to health-promoting resources over the life course (Crear-Perry et al., 2020). The results of our study suggest that investing in communities with persistent racial and economic segregation could positively impact Black maternal and perinatal health by deconcentrating poverty. Policy solutions should focus on improving the quality of job opportunities, increasing employment compensation, generating affordable housing, enforcing housing anti-discrimination laws, promoting Black homeownership, improving school funding and quality including decoupling from homeowner tax, and facilitating mobility and integration of lower-income families into higher-opportunity areas (Ray et al., 2022). Furthermore, providing targeted investment to support hospitals that operate in areas experiencing chronic deprivation could further promote positive Black maternal health outcomes. Although these solutions require overcoming political, economic, and institutional challenges, they offer a promising avenue for ultimately closing the health equity gap among current and future generations.
Supplementary Material
Highlights.
Where Black birthing people give birth matters.
National delivery discharge data linked to county-level structural racism measures.
Racialized economic segregation increases SMM risk for Black birthing people
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adkins-Jackson PB, Chantarat T, Bailey ZD, & Ponce NA (2021). Measuring structural racism: A guide for epidemiologists and other health researchers. American Journal of Epidemiology, 191(4), 539–547. 10.1093/aje/kwab239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, & Dalton VK (2018). Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012–2015. Obstetrics & Gynecology, 132(5), 1158–1166. 10.1097/AOG.0000000000002937 [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. (2021). HCUP NIS database documentation. Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp [Google Scholar]
- Alvarez CH (2022). Structural Racism as an Environmental Justice Issue: A multilevel analysis of the state racism index and environmental health risk from air toxics. Journal of Racial and Ethnic Health Disparities. 10.1007/s40615-021-01215-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z, Krieger N, Agénor M, Graves J, Linos N, & Bassett M (2017). Structural racism and health inequities in the USA: Evidence and interventions. The Lancet, 389(10047), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Bateman BT, Mhyre JM, Hernandez-Diaz S, Huybrechts KF, Fischer MA, Creanga AA, Callaghan WM, & Gagne JJ (2013). Development of a comorbidity index for use in obstetric patients. Obstetrics and Gynecology, 122(5), 10.1097/AOG.0b013e3182a603bb. 10.1097/AOG.0b013e3182a603bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CC, Adams CE, George KE, & Moore JE (2020). Associations between comorbidities and severe maternal morbidity. Obstetrics & Gynecology, 136(5), 892–901. 10.1097/AOG.0000000000004057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris HH, Passarella M, Handley SC, Srinivas SK, & Lorch SA (2021). Black-White disparities in maternal in-hospital mortality according to teaching and Black-serving hospital status. American Journal of Obstetrics and Gynecology, 225(1), 83.e1–83.e9. 10.1016/j.ajog.2021.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan WM, Creanga AA, & Kuklina EV (2012). Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics & Gynecology, 120(5), 1029–1036. 10.1097/AOG.0b013e31826d60c5 [DOI] [PubMed] [Google Scholar]
- Casey JA, James P, Cushing L, Jesdale BM, & Morello-Frosch R (2017). Race, ethnicity, income concentration and 10-year change in urban greenness in the United States. International Journal of Environmental Research and Public Health, 14(12), 1–15. 10.3390/ijerph14121546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021a). How does CDC identify serve maternal morbidity. centers for disease control and prevention, US Department of Health and Human Services. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm [Google Scholar]
- Centers for Disease Control and Prevention. (2021b). Severe maternal morbidity in the United States. Centers for Disease Control and Prevention, US Department of Health and Human Services. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html [Google Scholar]
- Chambers BD, Baer RJ, McLemore MR, & Jelliffe-Pawlowski LL (2019). Using Index of Concentration at the Extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality—California, 2011–2012. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 96(2), 159–170. 10.1007/s11524-018-0272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers BD, Erausquin JT, Tanner AE, Nichols TR, & Brown-Jeffy S (2018). Testing the association between traditional and novel indicators of county-level structural racism and birth outcomes among Black and White women. Journal of Racial and Ethnic Health Disparities, 5(5), 966–977. 10.1007/s40615-017-0444-z [DOI] [PubMed] [Google Scholar]
- Chantarat T, Van Riper DC, & Hardeman RR (2021). The intricacy of structural racism measurement: A pilot development of a latent-class multidimensional measure. EClinicalMedicine, 40, 1–7. 10.1016/j.eclinm.2021.101092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, & Wallace M (2020). Social and structural determinants of health inequities in maternal health. Journal of Women’s Health, 30(2), 230–235. 10.1089/jwh.2020.8882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty GB, Golden SH, Gross AL, Colantuoni E, & Dean LT (2020). Measuring structural racism and its association with BMI. American Journal of Preventive Medicine, 59(4), 530–537. 10.1016/j.amepre.2020.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont DM, Allen SA, Brockmann BW, Alexander NE, & Rich JD (2013). Incarceration, community health, and racial disparities. Journal of Health Care for the Poor and Underserved, 24(1), 78–88. 10.1353/hpu.2013.0000 [DOI] [PubMed] [Google Scholar]
- Dyer L, Hardeman R, Vilda D, Theall K, & Wallace M (2019). Mass incarceration and public health: The association between black jail incarceration and adverse birth outcomes among black women in Louisiana. BMC Pregnancy and Childbirth, 19(1), 525. 10.1186/s12884-019-2690-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giurgescu C, & Misra DP (2022). Structural racism and maternal morbidity among Black women. Western Journal of Nursing Research, 44(1), 3–4. 10.1177/01939459211043942 [DOI] [PubMed] [Google Scholar]
- Golembeski C, & Fullilove R (2008). Criminal (in)justice in the city and its associated health consequences. American Journal of Public Health, 98(Supplement_1), S185–S190. 10.2105/AJPH.98.Supplement_1.S185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden SR, Runkle JD, & Sugg MM (2022). An Exploratory Spatiotemporal Analysis of Socio-Environmental Patterns in Severe Maternal Morbidity. Maternal and Child Health Journal. 10.1007/s10995-021-03330-0 [DOI] [PubMed] [Google Scholar]
- Hayward MD, & Gorman BK (2004). The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography, 41(1), 87–107. 10.1353/dem.2004.0005 [DOI] [PubMed] [Google Scholar]
- Hirai AH, Owens PL, Reid LD, Vladutiu CJ, & Main EK (2022). Trends in severe maternal morbidity in the US across the transition to ICD-10-CM/PCS from 2012–2019. JAMA Network Open, 5(7), e2222966. 10.1001/jamanetworkopen.2022.22966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Egorova N, Balbierz A, Zeitlin J, & Hebert PL (2016). Black-white differences in severe maternal morbidity and site of care. American Journal of Obstetrics and Gynecology, 214(1), 122.e1–7. 10.1016/j.ajog.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh M, Spasojevic J, Li W, Maduro G, Van Wye G, Waterman PD, & Krieger N (2018). Spatial social polarization and birth outcomes: Preterm birth and infant mortality – New York City, 2010–14. Scandinavian Journal of Public Health, 46(1), 157–166. 10.1177/1403494817701566 [DOI] [PubMed] [Google Scholar]
- Jahn JL, Chen JT, Agénor M, & Krieger N (2020). County-level jail incarceration and preterm birth among non-Hispanic Black and white U.S. women, 1999–2015. Social Science & Medicine, 250, 1–8. 10.1016/j.socscimed.2020.112856 [DOI] [PubMed] [Google Scholar]
- Janevic T, Zeitlin J, Egorova N, Hebert PL, Balbierz A, & Howell EA (2020). Neighborhood racial and economic polarization, hospital of delivery, and severe maternal morbidity. Health Affairs, 39(5), 768–776. 10.1377/hlthaff.2019.00735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janevic T, Zeitlin J, Egorova NN, Hebert P, Balbierz A, Stroustrup AM, & Howell EA (2021). Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm. The Journal of Pediatrics, 235, 116–123. 10.1016/j.jpeds.2021.03.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Li Z, & Epstein AM (2007). Concentration and quality of hospitals that care for elderly black patients. Archives of Internal Medicine, 167(11), 1177–1182. 10.1001/archinte.167.11.1177 [DOI] [PubMed] [Google Scholar]
- Krieger N (2012). Methods for the scientific study of discrimination and health: An ecosocial approach. American Journal of Public Health, 102(5), 936–944. 10.2105/AJPH.2011.300544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Kim R, Feldman J, & Waterman PD (2018). Using the Index of Concentration at the Extremes at multiple geographical levels to monitor health inequities in an era of growing spatial social polarization: Massachusetts, USA (2010–14). International Journal of Epidemiology, 47(3), 788–819. 10.1093/ije/dyy004 [DOI] [PubMed] [Google Scholar]
- Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, Gwynn RC, Barbot O, & Bassett MT (2020). Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. American Journal of Public Health, 110(7), 1046–1053. 10.2105/AJPH.2020.305656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, & Van Wye G (2016). Public health monitoring of privilege and deprivation with the Index of Concentration at the Extremes. American Journal of Public Health, 106(2), 256–263. 10.2105/AJPH.2015.302955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, & Marchbanks PA (2008). An enhanced method for identifying obstetric deliveries: Implications for estimating maternal morbidity. Maternal and Child Health Journal, 12(4), 469–477. 10.1007/s10995-007-0256-6 [DOI] [PubMed] [Google Scholar]
- Leonard SA, Main EK, & Carmichael SL (2019). The contribution of maternal characteristics and cesarean delivery to an increasing trend of severe maternal morbidity. BMC Pregnancy and Childbirth, 19(1), 16. 10.1186/s12884-018-2169-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SY, Fiorentini C, Bailey Z, Huynh M, McVeigh K, & Kaplan D (2019). Structural racism and severe maternal morbidity in New York state. Clinical Medicine Insights: Women’s Health, 12, 1–8. 10.1177/1179562X19854778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main EK, Abreo A, McNulty J, Gilbert W, McNally C, Poeltler D, Lanner-Cusin K, Fenton D, Gipps T, Melsop K, Greene N, Gould JB, & Kilpatrick S (2016). Measuring severe maternal morbidity: Validation of potential measures. American Journal of Obstetrics and Gynecology, 214(5), 643.e1–643.e10. 10.1016/j.ajog.2015.11.004 [DOI] [PubMed] [Google Scholar]
- Main EK, Leonard SA, & Menard MK (2020). Association of maternal comorbidity with severe maternal morbidity: A cohort study of California mothers delivering between 1997 and 2014. Annals of Internal Medicine, 173(11_Supplement), S11–S18. 10.7326/M19-3253 [DOI] [PubMed] [Google Scholar]
- Meeker JR, Canelón SP, Bai R, Levine LD, & Boland MR (2021). Individual-level and neighborhood-level risk factors for severe maternal morbidity. Obstetrics & Gynecology, 137(5), 847–854. 10.1097/AOG.0000000000004343 [DOI] [PubMed] [Google Scholar]
- Mendez DD, Hogan VK, & Culhane J (2011). Institutional racism and pregnancy health: Using home mortgage disclosure act data to develop an index for mortgage discrimination at the community level. Public Health Reports, 126(3_suppl), 102–114. 10.1177/00333549111260S315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minton TD (2020). Jail Inmates in 2020 – Statistical Tables. Bureau of Justice Statistics, 27. [Google Scholar]
- Nardone AL, Casey JA, Rudolph KE, Karasek D, Mujahid M, & Morello-Frosch R (2020). Associations between historical redlining and birth outcomes from 2006 through 2015 in California. PLOS ONE, 15(8), e0237241. 10.1371/journal.pone.0237241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R, Perry AM, Harshbarger D, Elizondo S, & Gibbons A (2021, September 1). Homeownership, racial segregation, and policy solutions to racial wealth equity. Brookings. https://www.brookings.edu/essay/homeownership-racial-segregation-and-policies-for-racial-wealth-equity/ [Google Scholar]
- Roberts DE (2004). The social and moral cost of mass incarceration in African American communities. Faculty Scholarship at Penn Carey Law, 36, 1271–1305. https://scholarship.law.upenn.edu/faculty_scholarship/583 [Google Scholar]
- Ruggles S, Flood S, Foster S, Goeken R, Pacas J, Schouweiler M, & Sobek M (n.d.). IPUMS USA: Version 11.0 [dataset]. IPUMS. 10.18128/D010.V11.0 [DOI] [Google Scholar]
- Sampson RJ, & Loeffler C (2010). Punishment’s place: The local concentration of mass incarceration. Daedalus, 139(3), 20–31. 10.1162/DAED_a_00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sealy-Jefferson S, Butler B, Price-Spratlen T, Dailey RK, & Misra DP (2020). Neighborhood-level mass incarceration and future preterm birth risk among African American Women. Journal of Urban Health, 97(2), 271–278. 10.1007/s11524-020-00426-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonderlund AL, Charifson M, Schoenthaler A, Carson T, & Williams NJ (2022). Racialized economic segregation and health outcomes: A systematic review of studies that use the Index of Concentration at the Extremes for race, income, and their interaction. PLOS ONE, 17(1), e0262962. 10.1371/journal.pone.0262962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian R, Riley K, & Mai C (2018). Divided Justice: Trends in Black and White Jail Incarceration, 1990–2013. 1–48. https://www.vera.org/downloads/publications/Divided-Justice-full-report.pdf [Google Scholar]
- Taylor JK (2020). Structural racism and maternal health among Black women. Journal of Law, Medicine & Ethics, 48(3), 506–517. 10.1177/1073110520958875 [DOI] [PubMed] [Google Scholar]
- Thoma ME, Drew LB, Hirai AH, Kim TY, Fenelon A, & Shenassa ED (2019). Black-white disparities in preterm birth: Geographic, social, and health determinants. American Journal of Preventive Medicine, 57(5), 675–686. 10.1016/j.amepre.2019.07.007 [DOI] [PubMed] [Google Scholar]
- Thomas JC, & Torrone E (2008). Incarceration as Forced Migration: Effects on Selected Community Health Outcomes. American Journal of Public Health, 98(Supplement_1), S181–S184. 10.2105/AJPH.98.Supplement_1.S181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera Institute of Justice. (2020). Incarceration Trends [Dataset]. Vera Institute of Justice. https://github.com/vera-institute/incarceration-trends [Google Scholar]
- Wallace M, Crear-Perry J, Richardson L, Tarver M, & Theall K (2017). Separate and unequal: Structural racism and infant mortality in the US. Health & Place, 45, 140–144. 10.1016/j.healthplace.2017.03.012 [DOI] [PubMed] [Google Scholar]
- Wallace ME, Mendola P, Liu D, & Grantz KL (2015). Joint effects of structural racism and income inequality on small-for-gestational-age birth. American Journal of Public Health, 105(8), 1681–1688. 10.2105/AJPH.2015.302613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, & Wang EA (2017). Mass incarceration, public health, and widening inequality in the USA. The Lancet, 389(10077), 1464–1474. 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57(8), 1152–1173. 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


