Abstract
This study aims to assess the effectiveness of the WIC program at improving children’s dietary quality and to evaluate whether the 2009 food benefit revision further improved the WIC program. A sample of 1,753 children aged between 2 to 4 years from the 2005–2008 and 2011–2016 NHANES was analyzed using a propensity score weighted difference-in-difference approach. Results show that WIC-participating children scored 2.98 points higher (SD: 0.89; P<0.01) in HEI-2015 total scores compared with income-eligible non-participants during 2011–2016. No significant change was observed in the differences of HEI-2015 scores between WIC participants and eligible non-participants from 2005–2008 to 2011–2016.
Keywords: WIC, Children, Nutrition, Dietary Quality, Healthy Eating Index
Introduction
The Special Supplemental Nutrition Program for Women, Infants, and Children, also known as WIC, is a federally funded nutrition assistance program in the US for eligible low-income women, infants, and children up to age five (1). One key goal of the WIC program is to provide free, supplemental food packages with nutritious and balanced dietary support, as maternal and childhood undernutrition negatively impacts children’s physical growth, intellectual development, and a broad range of other key health indicators (2). Although some existing research has shown the effectiveness of WIC for child development (3) and nutritional support (4), evidence has also emerged suggesting that enrolled infants and children did not have better dietary quality than those who were income-eligible but did not enroll. For example, WIC children’s overall diet, measured by Healthy Eating Index (HEI)-2005 total score, did not significantly differ from that of nonparticipating children during the years 1999–2004 (5).
To better address the nutritional needs of lower-income families and to further improve the nutritional value of the food package, the WIC program implemented a comprehensive benefit revision in 2009, the first major change in four decades (6). This modification specifically targeted fresh fruits, vegetables, whole grains, and low-fat dairy while reducing fruit juice, which usually contains excessive added sugar. Such changes were in line with the Institute of Medicine’s dietary recommendations (7). Several national and regional studies found that implementing the 2009 food package revision has increased healthy food access and purchases among WIC-participating families (8–12). A nationwide study using longitudinal consumer data, for example, found that WIC households had seen decreased purchases of refined, high-calorie, or processed foods and increased purchases of fruits and vegetables with the revised food package (11).
With the emerging evidence on the availability of and access to a healthy diet among WIC households, whether the revised food package has improved dietary intake among enrolled children is worth investigating. One study conducted telephone surveys among 3,004 and 2,996 California WIC families in 2009 and 2010, respectively, and confirmed their increased consumption of whole-grain food, lower-fat milk, and fruits and vegetables (13). Another longitudinal study in Chicago comparing 24-hour dietary recalls from 209 WIC households collected in 2009 and 2011 observed a healthier diet after the revision (14). A national study compared the HEI-2010 between 2003–2008 and 2011–2012 and found that the food package revision was associated with significantly higher HEI-2010 total scores among WIC children after the revision (15). However, one limitation of these studies was the short follow-up period after the 2009 WIC food revisions. Notably, the final rule of the WIC revision was implemented in March 2014, which was beyond the follow-up period of these studies (6). Therefore, the long-term impact of this revision on dietary intake is still unknown.
In addition, the existing literature did not address the self-selection bias in WIC participation that might threaten the validity of the evaluations (12,16–19). Self-selection bias arises when factors related to nutritional outcomes influence the likelihood of participation in the WIC program among eligible families. For example, children of more-educated parents may have better nutritional status (20,21). They may also be more likely to participate in WIC if eligible due to the positive correlation between parental education and health-oriented parenting (22). The positive effect of having such WIC participants would inflate nutritional outcomes for the program. The propensity score (PS) method is a common approach to address this concern (23). It accounts for the likelihood of respondents being exposed to a treatment (e.g., WIC participation) in observational data and can better isolate the treatment effect from other potentially overlooked confounders (e.g., parental education). Little work has been done to evaluate the impact of the WIC program’s 2009 food package revision on nutritional outcomes using the PS method to address self-selection bias.
This study evaluates the impact of WIC on children’s dietary quality and assesses the effectiveness of the 2009 WIC food package modification. It makes three contributions to the existing literature that are noteworthy. First, dietary quality was measured using the HEI-2015, an updated and comprehensive metric compared to previously used measures (24). Second, it uses nationally representative data with the post-2009 revision period (2011–2016) that covers the implementation of the final WIC revision rule, which was not done in previous studies. Finally, a propensity score weighted difference-in-difference approach was applied to assess whether the 2009 revision has significantly changed WIC advantages in children’s dietary quality. A major merit of this approach is its ability to effectively control for the self-selection bias commonly seen in observational studies.
Methods
Study Design and Sample
Multiple years of cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) in 2005–2008 and 2011–2016 were pooled for our analyses. As a nationally representative survey of the US civilian population of all ages, NHANES gathers data every two years and adopts a stratified, multistage probability cluster sampling design following standardized protocols for interviews and physical examinations (25). It is listed by the Centers for Disease Control and Prevention (CDC) as a key data source to monitor the US population’s dietary intake and nutritional status (26) and also includes information about households’ participation in federal food assistance programs such as WIC and the Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program (26,27). All NHANES data used in this study were collected by trained interviewers who administered the questionnaires at a participant’s home using a computer-assisted personal interview system (25).
Because our dietary quality measures only apply to individuals aged 2 years or older, we followed a previous study (15) in restricting our sample to 2,126 children between 2 to 4 years old who were age- and income-eligible for WIC. Among them, 584 children had missing information on one or more variables of interest, including 373 children who missed certain dietary recall data to generate HEI-2015 scores and were thus excluded from our analyses. The other 211 respondents had missing data in certain covariates (i.e., nativity, marital status, educational attainment, and SNAP status). These missing values were imputed using a univariate imputation approach with bootstrap so that these respondents were able to be retained in our analyses (28). Specifically, for each one of the four covariates, a multivariate logistic regression model was estimated using information on a child’s age, sex, self-identified race/ethnicity, as well as household income-to-poverty ratio and food security status for the last year. Thus, the final analytical sample included 1,753 WIC-eligible children, divided into four groups, including 496 pre-2009 WIC-participants (pre-exposure), 285 pre-2009 WIC-nonparticipants (pre-comparison), 641 post-2009 WIC-participants (post-exposure), and 331 post-2009 WIC-nonparticipants (post-comparison). Figure 1 illustrates the flow diagram of creating the analytical sample.
Figure 1.
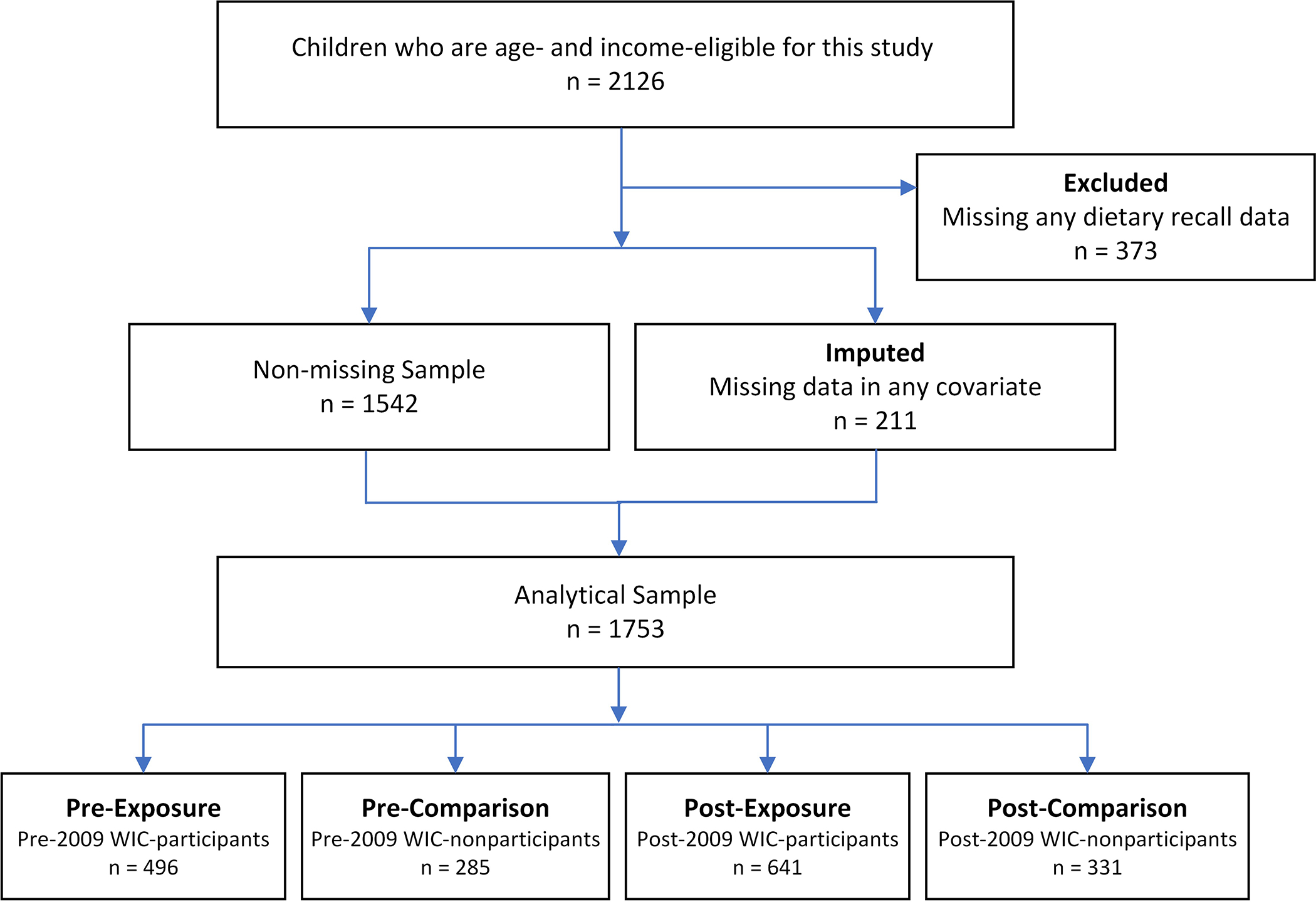
Flow Diagram of Analytical Sample
Measures
The outcome of our main interest, dietary quality, was measured by the 2015 Healthy Eating Index (HEI-2015), a scoring metric that reflects both overall dietary quality and specific dietary components (24). The HEI-2015 scoring standards were jointly developed by the National Cancer Institute (NCI) and the USDA based on the 2015–2020 Dietary Guidelines of Americans (24,29). Specifically, HEI-2015 includes thirteen dietary components: total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and saturated fats. All thirteen component scores are then added to get a total score reflecting the overall diet quality, with a possible range of 0–100 points. A higher value in the total score and each component score indicates better dietary quality. To facilitate research use of the HEI, the NCI and UDSA have developed sample SAS codes that can be applied to food intake data to create HEI-2015 scores (30). For our study, we applied the SAS sample codes to the two days’ 24-hour dietary recall data from NHANES and the Food Patterns Equivalents Database (FPED) from the USDA to create HEI scores for the children in our sample. Note that the FPED is not available to create the HEI-2015 for NHANES data before 2005, and 2015–2016 is the latest wave with complete information for this study (31).
Information on WIC eligibility and WIC participation were used to distinguish WIC participants and WIC-eligible nonparticipants. WIC eligibility was based on a child’s household income-to-poverty ratio, which was defined as the ratio of household income to the federal poverty threshold for the family size and year (32). According to WIC program rules, children with a household income below or equal to 185% of the federal poverty threshold (i.e., income–poverty ratio ≤ 1.85) were eligible for WIC in our analysis (33). WIC participation was based on the interview question asking whether a child had received WIC benefits in the last 12 months. In 2015–2016, this information was no longer available and the household-level variable indicating whether anyone in the household had received WIC benefits in the last 12 months was used to determine a child’s WIC participation status for these two years.
Key sociodemographic covariates in our analysis included children’s age (in years), sex (female and male), self-identified race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and other race/ethnicity), which represents more ethnic designations than a race-only measurement (34), and nativity (whether or not born in the US). Additional variables pertaining to a child’s household characteristics included: parental marital status (married/living with partner, widowed/divorced/separated, and never married), educational attainment of the household reference person (less than high school, high school graduate or GED, some college or AA degree, and college graduate or higher), and household income-to-poverty ratio. Following prior work (15), information on whether a household had received SNAP benefits in the past year was included. Household food security status for the last year was also included (full security, marginal security, low/very low security) and was based on eighteen U.S. Food Security Survey Module questions that were asked of households with children under the age of 18. All these variables were obtained through NHANES questionnaires that were administered by trained interviewers.
Statistical Analysis
Descriptive statistics of children and their households were first calculated for all four groups: pre-exposure, pre-comparison, post-exposure, and post comparison. Total HEI-2015 scores and thirteen subscores were computed. Exposure comparison and pre-post comparison were performed on these scores, using difference-in-difference (DiD) modeling without controlling for confounders. Next, socio-demographics were added to the DiD models as confounders. Finally, propensity score weights were incorporated in the DiD models to account for self-selection biases.
DiD is a common approach in policy evaluation using observational data, because it is able to differentiate out secular trends in the outcome by comparing two groups that are experiencing the same trends over time but one is exposed to the policy change while the other is not (35). In practice, DiD models specify an interaction term between participation status in a program or policy (yes/no) and time period (pre/post) (36). Specific to this study, the differences in dietary quality measured by HEI scores between WIC participants and WIC nonparticipants were compared before-2009 and post-2009. If WIC continued to benefit children’s dietary quality and the 2009 revision was effective, then the benefits should be reflected in higher HEI scores during the post-2009 period relative to the pre-2009 period.
To account for sample selection bias, a threat to validity in observational studies, a propensity score weighting approach was further included in the DiD analysis to assess the impacts of WIC policy revision (37). Specifically, a multinomial logistic regression was first estimated to obtain an individual’s probabilities of being in one of the four subgroups (i.e., pre-treatment, post-treatment, pre-control, post-control) as a function of covariates including age, race/ethnicity, nativity, marital status, education, income–poverty ratio, SNAP status, and food security status. The predicted probabilities of group membership were then used to create a propensity score weight, so the pre-control, pre-treatment, and post-control groups were similar to the post-treatment group in the controlled demographics after applying the weights (37). This approach creates balanced subgroups while retaining a more adequate sample size than other approaches, such as propensity score matching (23). The propensity score weighting approach is more effective in addressing the self-selection bias than in a previous study, which only used the DiD method (15).
The propensity score weights were incorporated as sampling weights in the DiD models to estimate HEI-2015 total scores and component scores, controlling for children’s age, sex, race/ethnicity, and nativity, as well as the caregiver’s marital status, educational attainment, income-to-poverty ratio, SNAP and food security status, and survey years. HEI-2015 scores were created using SAS (38) following the NCI instructions (39) and all other analyses were conducted in Stata 16 (40). P-values that were less than 0.05 were used to determine statistical significance, while those less than 0.1 were considered marginally significant. The study was approved by the Institutional Review Board under federal regulation 45 46.101 (b) CFR. Since this is an exempt study using unidentified secondary data, no informed consent was needed.
Results
Table 1 presents sociodemographic characteristics of WIC-eligible children before and after the 2009 food package revision. Compared with children who were income-eligible but did not enroll in WIC, those who enrolled were slightly younger in age (p < 0.05 for years 2005–2008 and p < 0.01 for years 2011–2016) and were more likely to be US-born (p < 0.001). In regard to household characteristics, the caregivers of WIC-participating children were less educated (p < 0.001) and had lower household incomes (p < 0.001 for years 2005–2008 and p < 0.01 for years 2011–2016). They were also more likely to have received SNAP benefits in the past year (p < 0.001).
Table 1.
Sociodemographic Characteristics of WIC-Eligible Participating and Nonparticipating Children, NHANES 2005–2008 and 2011–20161
| 2005–20082 |
2011–20162 |
|||||
|---|---|---|---|---|---|---|
| Non-WIC | WIC | P-value 4 | Non-WIC | WIC | P-value 4 | |
|
|
|
|||||
| Child Characteristics | ||||||
| Age in Years | 2.94 (0.86) | 2.82 (0.84) | 0.049 | 3.00 (0.83) | 2.84 (0.83) | 0.003 |
| Female | 49.8% | 47.4% | 0.510 | 51.96% | 50.08% | 0.577 |
| Race/Ethnicity | 0.002 | < 0.001 | ||||
| Non-Hispanic White | 34.04% | 21.77% | 27.49% | 16.07% | ||
| Non-Hispanic Black | 21.75% | 22.78% | 32.33% | 31.98% | ||
| Mexican American | 30.53% | 39.72% | 18.43% | 26.05% | ||
| Other Hispanic | 7.02% | 10.08% | 9.06% | 15.29% | ||
| Other race3 | 6.67% | 5.65% | 12.69% | 10.61% | ||
| US Born | 93.68% | 98.59% | < 0.001 | 95.77% | 99.22% | < 0.001 |
| Household Characteristics | ||||||
| Marital Status | 0.012 | 0.493 | ||||
| Married/Living with partner | 71.58% | 62.70% | 60.42% | 64.12% | ||
| Widowed/Divorced/Separated | 15.44% | 16.13% | 17.82% | 15.44% | ||
| Never married | 12.98% | 21.17% | 21.75% | 20.44% | ||
| Educational Attainment | < 0.001 | < 0.001 | ||||
| Less than high school | 34.74% | 53.23% | 25.38% | 38.69% | ||
| High school graduate/GED | 31.58% | 21.57% | 29.31% | 27.93% | ||
| Some college/AA degree | 24.91% | 21.37% | 35.05% | 27.61% | ||
| College graduate or higher | 8.77% | 3.83% | 10.27% | 5.77% | ||
| Income-Poverty Ratio | 1.01 (0.46) | 0.82 (0.42) | < 0.001 | 0.95 (0.47) | 0.85 (0.47) | 0.002 |
| Received SNAP | 36.84% | 57.46% | < 0.001 | 54.98% | 70.51% | < 0.001 |
| Food Security | 0.104 | 0.020 | ||||
| Full security | 52.28% | 44.56% | 46.22% | 36.97% | ||
| Marginal security | 16.84% | 18.35% | 19.03% | 22.15% | ||
| Low/Very low security | 30.88% | 37.10% | 34.74% | 40.87% | ||
|
| ||||||
| Observations | 285 | 496 | 331 | 641 | ||
Data shown are means or percentages.
Standard deviations are in parentheses.
Other race also includes multi-racial individuals.
Statistically significant p-values are bold (p < 0.05).
Table 2 presents children’s unadjusted HEI-2015 total scores and all component scores in specific food groups from DiD analyses. WIC-participating children in 2011–2016 had significantly higher HEI-2015 total scores (55.81) than nonparticipants (53.61) (p < 0.01). Similar patterns of WIC-participating children’s diet advantage over nonparticipants also emerged in certain component scores during 2011–2016, such as seafood and plant proteins, fatty acids, and saturated fats (p < 0.05). The only exception was total fruits, in which WIC-participating children’s advantage disappeared from 2005–2008 to 2011–2016. DiD analyses revealed little change in WIC impact between the two periods, with one exception. WIC participants had better scores in the fatty acid category during the post-2009 period, but not during the pre-2009 period, and this difference is statistically significant (p < 0.05). Table 3 presents predicted HEI-2015 total scores and component scores using DiD analysis adjusted for child and household characteristics but without propensity score adjustments. The results are similar to those shown in Table 2 from the unadjusted DiD analyses.
Table 2.
Predicted HEI-2015 Scores from Unadjusted Difference-in-Difference Analysis without Propensity Score Weighting, NHANES 2005–2008 and 2011–2016
|
2005–2008
|
2011–2016
|
Difference-in-Difference 1 | |||||
|---|---|---|---|---|---|---|---|
| HEI-2015 Scores | Non-WIC | WIC | Difference1 | Non-WIC | WIC | Difference1 | |
|
|
|
||||||
| Total Score | 52.37 | 53.89 | 1.52 (0.84)+ | 53.61 | 55.81 | 2.20 (0.76)** | 0.68 (1.13) |
| Total Fruits | 3.55 | 3.86 | 0.31 (0.12)* | 3.64 | 3.77 | 0.13 (0.11) | −0.18 (0.17) |
| Whole Fruits | 3.19 | 3.24 | 0.05 (0.15) | 3.27 | 3.23 | −0.04 (0.14) | −0.09 (0.21) |
| Total Vegetables | 2.21 | 2.27 | 0.07 (0.10) | 2.06 | 2.22 | 0.16 (0.09)+ | 0.09 (0.13) |
| Greens and Beans | 1.06 | 1.21 | 0.16 (0.14) | 1.14 | 1.36 | 0.22 (0.13)+ | 0.06 (0.19) |
| Whole Grains | 2.01 | 1.81 | −0.20 (0.19) | 2.99 | 2.84 | −0.15 (0.18) | 0.05 (0.26) |
| Dairy | 8.25 | 8.41 | 0.16 (0.19) | 7.73 | 7.80 | 0.07 (0.18) | −0.08 (0.26) |
| Total Protein Foods | 3.78 | 3.91 | 0.13 (0.10) | 3.71 | 3.78 | 0.07 (0.07) | −0.07 (0.13) |
| Seafood and Plant Proteins | 1.98 | 1.93 | −0.04 (0.15) | 1.71 | 1.99 | 0.29 (0.14)* | 0.33 (0.20) |
| Fatty Acids | 2.74 | 2.54 | −0.20 (0.22) | 3.47 | 3.91 | 0.44 (0.20)* | 0.64 (0.30)* |
| Refined Grains | 6.33 | 6.61 | 0.29 (0.24) | 5.90 | 5.93 | 0.03 (0.22) | −0.26 (0.32) |
| Sodium | 6.04 | 6.19 | 0.15 (0.23) | 5.48 | 5.54 | 0.06 (0.20) | −0.10 (0.30) |
| Added Sugars | 6.17 | 6.86 | 0.69 (0.21)** | 6.98 | 7.47 | 0.48 (0.19)* | −0.21 (0.28) |
| Saturated Fats | 5.06 | 5.03 | −0.04 (0.22) | 5.53 | 5.98 | 0.45 (0.20)* | 0.49 (0.30) |
|
| |||||||
| Observations | 285 | 496 | 331 | 641 | 1,753 | ||
Standard errors are in parenthesis.
p < 0.1
p < 0.05
p < 0.01
p < 0.001
Table 3.
Results from Adjusted Difference-in-Difference Analysis without Propensity Score Weighting, NHANES 2005–2008 and 2011–20161
| 2005–2008 |
2011–2016 |
Difference-in-Difference2 | |||||
|---|---|---|---|---|---|---|---|
| HEI-2015 Scores | Non-WIC | WIC | Difference2 | Non-WIC | WIC | Difference2 | |
|
|
|
||||||
| Total Score | 56.80 | 59.01 | 2.21 (0.85)** | 63.60 | 65.96 | 2.36 (0.77)** | 0.15 (1.12) |
| Total Fruits | 3.65 | 4.02 | 0.37 (0.13)** | 4.15 | 4.31 | 0.16 (0.12) | −0.21 (0.17) |
| Whole Fruits | 3.20 | 3.43 | 0.23 (0.16) | 3.75 | 3.80 | 0.05 (0.14) | −0.18 (0.21) |
| Total Vegetables | 2.07 | 2.15 | 0.09 (0.10) | 1.96 | 2.13 | 0.18 (0.09)+ | 0.09 (0.13) |
| Greens and Beans | 1.59 | 1.77 | 0.17 (0.14) | 1.79 | 1.99 | 0.20 (0.13) | 0.02 (0.19) |
| Whole Grains | 1.47 | 1.47 | 0.00 (0.20) | 2.50 | 2.50 | 0.00 (0.18) | 0.01 (0.26) |
| Dairy | 9.52 | 9.76 | 0.24 (0.19) | 9.99 | 10.01 | 0.02 (0.18) | −0.22 (0.26) |
| Total Protein Foods | 3.72 | 3.80 | 0.08 (0.10) | 3.77 | 3.82 | 0.05 (0.09) | −0.03 (0.13) |
| Seafood and Plant Proteins | 3.29 | 3.32 | 0.03 (0.15) | 3.66 | 3.95 | 0.29 (0.14)* | 0.26 (0.20) |
| Fatty Acids | 1.53 | 1.25 | −0.28 (0.22) | 2.59 | 3.03 | 0.44 (0.20)* | 0.72 (0.29)* |
| Refined Grains | 8.16 | 8.49 | 0.34 (0.24) | 9.06 | 9.07 | 0.01 (0.22) | −0.33 (0.32) |
| Sodium | 7.95 | 8.20 | 0.25 (0.23) | 8.55 | 8.54 | −0.01 (0.21) | −0.26 (0.30) |
| Added Sugars | 5.46 | 6.18 | 0.72 (0.21)** | 5.39 | 5.91 | 0.52 (0.19)** | −0.20 (0.28) |
| Saturated Fats | 5.17 | 5.15 | −0.02 (0.23) | 6.42 | 6.87 | 0.46 (0.21)* | 0.48 (0.30) |
|
| |||||||
| Observations | 285 | 496 | 331 | 641 | 1,753 | ||
All models adjusted for age, sex, race, nativity, marital status, education, income–poverty ratio, SNAP status, food security status, and survey year.
Standard errors are in parenthesis.
p < 0.1
p < 0.05
p < 0.01
p < 0.001
Table 4 shows the results from the propensity score-weighted DiD analysis. Consistent with earlier findings, WIC-participating children had better HEI-2015 total scores than nonparticipants (p < 0.01) in both 2005–2008 and 2011–2016, but these advantages did not differ significantly between the two periods. Specific to the thirteen dietary components in HEI-2015, during 2005–2008, WIC-participating children were better off in terms of total fruits (p < 0.05) and reduced consumption of added sugars (p < 0.01). During the post-revision period of 2011–2016, besides added sugars (p < 0.01), WIC-participating children had gained advantages over nonparticipants in fatty acids (p < 0.05) and saturated fats (p < 0.05). However, DiD estimates did not show significant improvements in these food groups from 2005–2008 to 2011–2016. The significant post-2009 improvement in fatty acids observed from previous models became weaker and reached marginal significance level (p = 0.075).
Table 4.
Results from Adjusted Difference-in-Difference Analysis with Propensity Score Weighting, NHANES 2005–2008 and 2011–20161
| 2005–2008 |
2011–2016 |
Difference-in-Difference2 | |||||
|---|---|---|---|---|---|---|---|
| HEI-2015 Scores | Non-WIC | WIC | Difference2 | Non-WIC | WIC | Difference2 | |
|
|
|
||||||
| Total Score | 57.83 | 60.96 | 3.13 (1.02)** | 64.84 | 67.82 | 2.98 (0.89)** | −0.15 (1.33) |
| Total Fruits | 3.79 | 4.20 | 0.42 (0.17)* | 4.25 | 4.42 | 0.17 (0.14) | −0.25 (0.22) |
| Whole Fruits | 3.29 | 3.66 | 0.37 (0.21)+ | 3.79 | 3.91 | 0.11 (0.16) | −0.26 (0.26) |
| Total Vegetables | 2.34 | 2.51 | 0.17 (0.13) | 2.53 | 2.69 | 0.16 (0.10) | −0.01 (0.17) |
| Greens and Beans | 2.44 | 2.57 | 0.14 (0.17) | 3.00 | 3.16 | 0.16 (0.15) | 0.03 (0.22) |
| Whole Grains | 0.70 | 0.82 | 0.12 (0.19) | 1.84 | 1.92 | 0.09 (0.22) | −0.03 (0.29) |
| Dairy | 9.53 | 9.74 | 0.21 (0.25) | 10.30 | 10.25 | −0.05 (0.21) | −0.26 (0.33) |
| Total Protein Foods | 4.06 | 4.07 | 0.01 (0.11) | 4.08 | 4.13 | 0.05 (0.10) | 0.04 (0.15) |
| Seafood and Plant Proteins | 3.52 | 3.45 | −0.07 (0.20) | 3.92 | 4.15 | 0.23 (0.16) | 0.30 (0.25) |
| Fatty Acids | 2.07 | 2.04 | −0.03 (0.26) | 2.92 | 3.52 | 0.60 (0.24)* | 0.64 (0.36)+ |
| Refined Grains | 8.08 | 8.41 | 0.33 (0.29) | 8.94 | 9.06 | 0.13 (0.27) | −0.20 (0.40) |
| Sodium | 5.69 | 5.96 | 0.28 (0.28) | 5.12 | 5.20 | 0.08 (0.24) | −0.19 (0.37) |
| Added Sugars | 6.72 | 7.63 | 0.91 (0.28)** | 7.42 | 8.02 | 0.61 (0.22)** | −0.30 (0.35) |
| Saturated Fats | 5.59 | 5.89 | 0.30 (0.31) | 6.74 | 7.38 | 0.64 (0.24)** | 0.34 (0.39) |
|
| |||||||
| Observations | 285 | 496 | 331 | 641 | 1,753 | ||
All models adjusted for age, sex, race, nativity, marital status, education, income–poverty ratio, SNAP status, food security status, and survey year.
Standard errors are in parenthesis.
p < 0.1
p < 0.05
p < 0.01
p < 0.001
Discussion
The 2009 WIC revision was the major milestone for WIC’s food package changes in the last four decades. The revision process was finally completed in 2014, at which point the USDA implemented the final rule. The primary goal of the 2009 WIC food package revision was to promote healthy eating and to improve dietary quality among US children (6). Previous studies have produced mixed results regarding the effectiveness of WIC’s 2009 food package revision (16). Several national studies support the overall effectiveness of WIC’s 2009 revision (11,15,41,42), but results from a few local studies have shown inconsistent results (14,43,44). Much of the existing research evaluated the revision in a short time after 2009, which may not have captured the full impact of the 2014 completion of the revisions. Moreover, few studies have addressed self-selection bias, which was evident in social welfare program participation such as WIC. This undoubtedly posed an obstacle to achieving better causal inference in observational studies on WIC effectiveness (45). Even among study designs using DiD analysis, a key underlying assumption is that the two comparison groups (i.e., those who experienced the policy change vs. those who did not experience it) are exchangeable, which may not be substantiated in the WIC program (36). We aimed to address these issues by using a longer period of post-revision data and using a propensity score weighting approach, which helped generate more balanced comparisons between the exposure groups (WIC participants) and the control group (nonparticipants). Results from this study did not offer support for the 2009 revision’s significant effectiveness in enlarging the WIC advantage in overall dietary quality. As shown, both WIC participants and nonparticipants had similar improvements in HEI-2015 total scores during 2011–2016 compared to 2005–2008, at the descriptive level, after controlling for sociodemographic variables and after using propensity score weighting to correct for selection bias.
Compared with other nationwide studies reporting benefits of the WIC 2009 food package revision (15,42), the current study took advantage of an updated diet quality measure and a longer period of post-WIC-revision data, which helped better capture the policy impact as it took time to roll out in its entirety. To the best of our knowledge, it is one of the first studies to use a propensity score weighted difference-in-difference design to aid in reducing selection bias in WIC participation. Results showed that, while WIC-participating children had maintained their advantages over nonparticipants in overall dietary quality, as measured by HEI-2015 total scores, they did not have an increased advantage due to the 2009 WIC policy modification. Specific to several dietary components being targeted in this revision (6), WIC-participating children did not have increased advantages in fruits, vegetables, and whole grains. While WIC-participating children had better diets when it came to added sugars and saturated fats during the post-revision period, such advantages did not seem to be attributable to the food package revision according to the covariate-adjusted and propensity score weighted difference-in-difference analysis. Therefore, this study made an important novel contribution to the literature by providing more null results about the effectiveness of the 2009 WIC revision, which are needed to design future WIC food package revisions.
A few study limitations should be acknowledged. First, because the dietary quality measures are based on self-reported data, recall bias is thus inevitable (46). Although using both days of self-reported dietary data can reduce such bias, they still do not perfectly reflect respondents’ usual dietary intake. Second, while the propensity score method can overcome the limitations of cross-sectional data in drawing causal inferences and the current study included confounders, given data availability, the estimates may still be subject to bias if these confounders were insufficient. Specific to dietary quality, households’ decisions to enroll in WIC can be influenced by many other factors, such as WIC program characteristics, state policies, or local food prices, none of which were available in the data. Furthermore, this study used a measure of whether children had participated in WIC in the last 12 months, which may not be able to capture the “WIC effect” from a holistic view. For example, besides a binary indicator of WIC participation status, length of participation and the purchase of WIC foods could also make a difference in nutritional outcomes among young children (47,48). Due to the limited information related to state identifiers and various policies regarding WIC enrollment, this study did not consider adjunct WIC eligibility, e.g., participating in Medicaid making one automatically eligible for WIC.
Conclusions
This study makes a unique contribution to assessing the impact of the 2009 WIC food package revision on children’s dietary quality by using an updated dietary quality measure based on more recent data and addressing program participation selection bias. Results from this study suggest that the 2009 WIC food package revision was not as effective as thought in previous literature in terms of improving WIC children’s dietary quality. The findings suggest that more significant food package changes might be needed in future WIC revisions. For example, the cash value benefits significantly increased during the COVID-19 pandemic, which allowed WIC participants to buy more fruits and vegetables (49). Future research is needed to examine whether the temporary increase in these benefits improved the participants’ dietary quality. If confirmed, similar package changes can be proposed in the next round of the WIC food package review.
References
- 1.USDA Economic Research Service. WIC Program. https://www.ers.usda.gov/topics/food-nutrition-assistance/wic-program/. Published 2021. Accessed September 10, 2021.
- 2.Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Mathers C, Rivera J. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–260. [DOI] [PubMed] [Google Scholar]
- 3.Guan A, Hamad R, Batra A, Bush NR, Tylavsky FA, LeWinn KZ. The Revised WIC Food Package and Child Development: A Quasi-Experimental Study. Pediatrics. 2021;147(2):e20201853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siega-Riz AM, Kranz S, Blanchette D, Haines PS, Guilkey DK, Popkin BM. The effect of participation in the WIC program on preschoolers’ diets. J Pediatr. 2004;144:229–234. [DOI] [PubMed] [Google Scholar]
- 5.Cole N, Fox MK. Diet Quality of American Young Children by WIC Participation Status: Data from the National Health and Nutrition Examination Survey, 1999–2004. US Department of Agriculture; 2008. http://www.usda.gov/wps/portal/usdahome. Accessed July 19, 2020. [Google Scholar]
- 6.USDA Food and Nutrition Service. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC Food Packages; Final Rule. Vol 79.; 2014:1–74. https://www.federalregister.gov/documents/2007/12/06/E7-23033/special-supplemental-nutrition-program-for-women-infants-and-children-wic-revisions-in-the-wic-food. Accessed September 10, 2021. [Google Scholar]
- 7.WIC Food Packages. WIC Food Packages: Time for a Change. Washington, D.C.: National Academies Press; 2005. http://www.nap.edu/catalog/11280. Accessed September 10, 2021. [Google Scholar]
- 8.Schultz DJ, Byker Shanks C, Houghtaling B. The Impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children Food Package Revisions on Participants: A Systematic Review. J Acad Nutr Diet. 2015;115(11):1832- [DOI] [PubMed] [Google Scholar]
- 9.Zenk SN, Odoms-Young A, Powell LM, Campbell RT, Block D, Chavez N, Krauss RC, Strode S, Armbruster J. Fruit and vegetable availability and selection: Federal food package revisions, 2009. Am J Prev Med. 2012;43(4):423–428. [DOI] [PubMed] [Google Scholar]
- 10.Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive Influence of the Revised Special Supplemental Nutrition Program for Women, Infants, and Children Food Packages on Access to Healthy Foods. J Acad Nutr Diet. 2012;112(6):850–858. [DOI] [PubMed] [Google Scholar]
- 11.Ng SW, Hollingsworth BA, Busey EA, Wandell JL, Miles DR, Poti JM. Federal Nutrition Program Revisions Impact Low-income Households’ Food Purchases. Am J Prev Med. 2018;54(3):403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oh M, Jensen HH, Rahkovsky I. Did revisions to the WIC program affect household expenditures on whole grains? Appl Econ Perspect Policy. 2016;38:578–598. [Google Scholar]
- 13.Whaley SE, Ritchie LD, Spector P, Gomez J. Revised WIC Food Package Improves Diets of WIC Families. J Nutr Educ Behav. 2012;44(3):204–209. [DOI] [PubMed] [Google Scholar]
- 14.Kong A, Odoms-Young AM, Schiffer LA, Kim Y, Berbaum ML, Porter SJ, Blumstein LB, Bess SL, Fitzgibbon ML. The 18-month impact of special supplemental nutrition program for women, infants, and children food package revisions on diets of recipient families. Am J Prev Med. 2014;46(6):543–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tester JM, Leung CW, Crawford PB. Revised WIC Food Package and Children’s Diet Quality. Pediatrics. 2016;137(5):e20153557–e20153557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Q, Alsuliman MA, Wright M, Wang Y, Cheng X. Fruit and Vegetable Purchases and Consumption among WIC Participants after the 2009 WIC Food Package Revision: A Systematic Review. Adv Nutr. 2020;1(6):1646–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Q, Zhang J, Park K, Tang C. App Usage Associated With Full Redemption of WIC Food Benefits: A Propensity Score Approach. J Nutr Educ Behav. 2021;53:779–786. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Q, Chen C, Xue H, Park K, Wang Y. Revisiting the relationship between WIC participation and breastfeeding among low-income children in the U.S. after the 2009 WIC food package revision. Food Policy. 2021;101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sonchak L The Impact of WIC on Birth Outcomes: New Evidence from South Carolina. Matern Child Health J. 2016;20:1518–1525. [DOI] [PubMed] [Google Scholar]
- 20.Rodenburg G, Oenema A, Kremers SPJ, van de Mheen D. Parental and child fruit consumption in the context of general parenting, parental education and ethnic background. Appetite. 2012;58(1):364–372. [DOI] [PubMed] [Google Scholar]
- 21.Cribb VL, Jones LR, Rogers IS, Ness AR, Emmett PM. Is maternal education level associated with diet in 10-year-old children? Public Health Nutr. 2011;14(11):2037–2048. [DOI] [PubMed] [Google Scholar]
- 22.Mekonnen T, Havdal HH, Lien N, O’Halloran SA, Arah OA, Papadopoulou E, Gebremariam MK. Mediators of socioeconomic inequalities in dietary behaviours among youth: A systematic review. Obes Rev. 2020;21(7). [DOI] [PubMed] [Google Scholar]
- 23.Guo S, Fraser MW. Propensity score analysis: Statistical methods and applications. 2nd ed. Thousand Oaks: Sage Publications; 2015. [Google Scholar]
- 24.Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, Wilson MM, Reedy J. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Center for Health Statistics. NHANES Survey Methods and Analytic Guidelines. 2018. Available from: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx. Accessed September 10, 2021.
- 26.Centers for Disease Control and Prevention. Surveillance Systems. https://www.cdc.gov/obesity/data/surveillance.html. Accessed September 10, 2021.
- 27.National Academies of Sciences, Engineering, and Medicine. Review of WIC Food Packages: Improving Balance and Choice: Final Report. Washington, D.C.: National Academies Press; 2017. [PubMed] [Google Scholar]
- 28.Little RJA, Rubin DB. Statistical Analysis with Missing Data. Wiley; 2014. [Google Scholar]
- 29.DeSalvo KB, Olson R, Casavale KO. Dietary Guidelines for Americans. JAMA. 2016;315(5):457–458. [DOI] [PubMed] [Google Scholar]
- 30.Kirkpatrick SI, Reedy J, Krebs-Smith SM, Pannucci TRE, Subar AF, Wilson MM, Lerman JL, Tooze JA. Applications of the Healthy Eating Index for Surveillance, Epidemiology, and Intervention Research: Considerations and Caveats. J Acad Nutr Diet. 2018;118(9):1603–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Department of Agriculture. Overview of Food Patterns Equivalents Database. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview. Accessed September 10, 2021.
- 32.US Census Bureau. How the Census Bureau Measures Poverty. https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html. Accessed June 4, 2021.
- 33.USDA Food and Nutrition Service. WIC Eligibility Requirements. https://www.fns.usda.gov/wic/wic-eligibility-requirements. Accessed September 10, 2021.
- 34.Duggan CP, Kurpad A, Stanford FC, Sunguya B, Wells JC. Race, ethnicity, and racism in the nutrition literature: An update for 2020. Am J Clin Nutr. 2020;112(6):1409–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: The difference-in-differences approach. JAMA. 2014;312(22):2401–2402. [DOI] [PubMed] [Google Scholar]
- 36.Strumpf EC, Harper S, Kaufman J. Fixed effects and difference in differences. In: Oakes JM, Kaufman JS, editors. Methods in social epidemiology. Jossey-Bass; 2017. [Google Scholar]
- 37.Stuart EA, Huskamp HA, Duckworth K, Simmons J, Song Z, Chernew ME, Barry CL. Using propensity scores in difference-in-differences models to estimate the effects of a policy change. Heal Serv Outcomes Res Methodol. 2014;14:166–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SAS Institute. SAS Version 9.4. Cary, NC: SAS Institute Inc; 2017. [Google Scholar]
- 39.National Cancer Institute. Overview & Background of Healthy Eating Index (HEI). https://epi.grants.cancer.gov/hei/. Accessed September 10, 2021.
- 40.StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 41.Jun S, Catellier DJ, Eldridge AL, Dwyer JT, Eicher-Miller HA, Bailey RL. Usual nutrient intakes from the diets of US children by WIC participation and income: Findings from the feeding infants and toddlers study (FITS) 2016. J Nutr. 2018;148(9):1567S–1574S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guthrie JF, Anater AS, Hampton JC, Catellier DJ, Eldridge AL, Johnson WL, Quann EE. The Special Supplemental Nutrition Program for Women, Infants, and Children is Associated with Several Changes in Nutrient Intakes and Food Consumption Patterns of Participating Infants and Young Children, 2008 Compared with 2016. J Nutr October 2020. doi: 10.1093/jn/nxaa265 [DOI] [PubMed] [Google Scholar]
- 43.Reat AM, Crixell SH, Friedman BJ, Von Bank JA. Comparison of Food Intake Among Infants and Toddlers Participating in a South Central Texas WIC Program Reveals Some Improvements After WIC Package Changes. Matern Child Health J. 2015; 19(8): 1834–1841. [DOI] [PubMed] [Google Scholar]
- 44.Odoms-Young AM, Kong A, Schiffer LA, Porter SJ, Blumstein L, Bess S, Berbaum ML, Fitzgibbon ML. Evaluating the initial impact of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food packages on dietary intake and home food availability in African-American and Hispanic families. Public Health Nutr. 2014;17(01):83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li K, Wen M, Reynolds M, Zhang Q. WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach. Int J Environ Res Public Health. 2019;16(15):2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thompson FE, Subar AF. Dietary Assessment Methodology. In: Nutrition in the Prevention and Treatment of Disease. Academic Press; 2017:5–48. [Google Scholar]
- 47.Weinfield NS, Borger C, Au LE, Whaley SE, Berman D, Ritchie LD. Longer Participation in WIC Is Associated with Better Diet Quality in 24-Month-Old Children. J Acad Nutr Diet. 2020;120(6):963–971. [DOI] [PubMed] [Google Scholar]
- 48.Au LE, Paolicelli C, Gurzo K, Ritchie LD, Weinfield NS, Plank KR, Whaley SE. Contribution of WIC-Eligible Foods to the Overall Diet of 13- and 24-Month-Old Toddlers in the WIC Infant and Toddler Feeding Practices Study-2. J Acad Nutr Diet. 2019;119(3):435–448. [DOI] [PubMed] [Google Scholar]
- 49.USDA Food and Nutrition Service. Extending the Temporary Increase in the Cash-Value Voucher/Benefit. 2022; Available from: https://www.fns.usda.gov/wic/policy-memo-2022-2-extending-temporary-increase-cash-value-voucher-benefit. Accessed March 18, 2022.


