Abstract
Introduction
This study aimed to identify the common barriers leading to delayed initial management, microbiological diagnosis, and appropriate empirical antimicrobial treatment in sepsis.
Patients and methods
A cross-sectional study was performed by the application of a population-based survey. Four different surveys were designed, targeting the healthcare personnel located in main hospital areas [emergency department (SEMES); infectious diseases and clinical microbiology-micro-biological diagnosis (SEIMC-M); intensive care and infectious diseases, (SEMICYUC-GTEIS); and infectious diseases and clinical microbiology-clinical diagnosis, (SEIMC-C)].
Results
A total of 700 valid surveys were collected from June to November 2019: 380 (54.3%) of SEMES, 127 (18.1%) of SEIMC-M, 97 (13.9%) de SEMICYUC-GTEIS and 96 (13.7%) of SEIMC-C, in 270 hospitals of all levels of care. The qSOFA score was used as a screening tool. The most used biomarker was procalcitonin (n=92, 39.8%). The sepsis code was implemented in 157 of 235 participating centers (66.2%), particularly in tertiary level hospitals. The mean frequency of contaminated blood cultures was 8.9% (8.7). In 85 (78.7%) centers, positive results of blood cultures were available within the first 72 hours and were communicated to the treating physician effectively by phone or e-mail in 76 (81.7%) cases. The main reason for escalating treatment was clinical deterioration, and the reason for de-escalating antimicrobials was significantly different between the specialties. Quality indicators were not frequently monitored among the different participating centers.
Conclusion
There are significant barriers that hinder adequate management processes in sepsis in Spanish hospitals.
Keywords: Sepsis management, Sepsis Code, quality indicators
Abstract
Introducción
Este estudio tuvo como objetivo identificar las barreras comunes que conducen al retraso en el manejo inicial, el diagnóstico microbiológico y el tratamiento antimicrobiano empírico adecuado en la sepsis.
Pacientes y métodos
Se realizó un estudio transversal mediante la aplicación de una encuesta de base poblacional. Se diseñaron cuatro encuestas diferentes, dirigidas al personal de salud ubicado en las principales áreas hospitalarias [urgencias (SEMES); enfermedades infecciosas y microbiología clínica-diagnóstico microbiológico (SEIMC-M); cuidados intensivos y enfermedades infecciosas (SEMICYUC-GTEIS); y enfermedades infecciosas y microbiología clínica-diagnóstico clínico, (SEIMC-C)].
Resultados
Se recogieron un total de 700 encuestas válidas de junio a noviembre de 2019: 380 (54,3%) de SEMES, 127 (18,1%) de SEIMC-M, 97 (13,9%) de SEMICYUC-GTEIS y 96 (13,7%) de la SEIMC-C, en 270 hospitales de todos los niveles de atención. El qSOFA se utilizó principalmente como herramienta de detección. El biomarcador más utilizado fue la procalcitonina (n=92, 39,8%). El código sepsis estaba implementado en 157 de 235 centros participantes (66,2%), particularmente en hospitales de tercer nivel. La frecuencia media de hemocultivos contaminados fue del 8,9% (8,7). En 85 (78,7%) de los centros, los resultados de los hemocultivos positivos estuvieron disponibles en las primeras 72 horas y se comunicaron al médico responsable del paciente por teléfono o correo electrónico en 76 casos (81,7%). El motivo principal de la escalada del tratamiento fue el deterioro clínico y el motivo de la desescalada de los antimicrobianos fue significativamente diferente entre las especialidades. Los indicadores de calidad no se monitorizaban con frecuencia en los diferentes centros.
Conclusión
Existen importantes barreras que dificultan los procesos de manejo adecuado de la sepsis en los hospitales españoles.
Palabras clave: Sepsis, Código Sepsis, indicadores de calidad
INTRODUCTION
Sepsis is a frequent condition associated with increased mortality and high morbidity burden for patients. Therefore, protocolized management of sepsis is time-critical for adequate antimicrobial therapy, source control, and hemodynamic resuscitation [1]. Delayed antimicrobial treatment is an independent risk factor for mortality and organ dysfunction, particularly in patients with septic shock [2,3]. Still, there are significant barriers to materializing international guidelines’ recommendations regarding the early management of sepsis in daily clinical practice [4,5].
There are no comprehensive data on the global processes for sepsis care in Spanish hospitals, including organization standards, coordination, and usual care practices of all professionals involved in managing sepsis patients. This study aimed to identify the common barriers leading to delayed initial management, microbiological diagnosis, and appropriate empirical antimicrobial treatment in sepsis in Spanish hospitals. Data on quality of assistance will aid the development of future quality improvements for the practical implementations of stand-of-care interventions.
METHODS
A cross-sectional study was performed by the application of a population-based survey to assess health care professionals’ opinions and usual practices (Supplementary material). Numbers were described as n (%). Given that no patient data was obtained from this study, the Research Ethics Committee approval was waived. Four different surveys were designed, targeting the healthcare personnel located in main hospital areas involved in the initial management processes of sepsis patients. The surveys, which included between 21-27 questions, were implemented by using the web platform www.surveymonkey.com. The surveys were distributed by e-mail to all members of the Spanish Society of Emergencies (SEMES), the Spanish Working group of Infectious diseases and Sepsis (GTEIS), the Spanish Society of Intensive Care Medicine and Coronary Units (SEMICYUC), and The Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC), who received one survey to assess clinical diagnosis (SEIMC-C), and other to evaluate microbiological diagnosis (SEIMC-M). Surveys collected data on clinical suspicion of sepsis, microbiological diagnosis, empirical antimicrobial treatment, targeted treatment, and treatment withdrawal. The availability, compliance with recommendations, and performance of the Sepsis Code were assessed among non-intensivists.
RESULTS
A total of 700 valid surveys were collected from June to November 2019: 380 (54.3%) of SEMES, 127 (18.1%) of SEIMC-M, 97 (13.9%) de SEMICYUC-GTEIS and 96 (13.7%) of SEIMC-C. These surveys were fulfilled by healthcare professionals in 270 hospitals (supplementary table 1). Most centers were public (n=225; 81.2%), or university (n=164; 59.2%) hospitals, with < 300 beds (n=125; 45.1%). Most hospitals were secondary level (n=117; 42.2%) or tertiary level (n=87; 31.4%) hospitals. Two-hundred and forty-five (88.4%) of all participating hospitals had general laboratory services running 24 hours a day, seven days a week. Only 127 (45.8%) centers have a microbiology laboratory available 24 hours, seven days a week, and 31 (11.7%) had no microbiology laboratory available onsite. Two hundred and thirty (83%) hospitals had intensive care departments. Among the participating emergency services (206), 168 (81.6%) used an emergency department triage classification system such as the Manchester Triage System.
Among the 476 specialists (SEMES and SEIMC-C) who fulfilled the survey, 375 (75%) mainly used qSOFA as a screening tool (supplementary table 2). Regarding the tools for confirmation of diagnosis, 265 (57%) participants considered the presence of systemic inflammatory response syndrome + documented or suspected infection. The most used biomarker was procalcitonin (n=92, 39.8%) (supplementary table 3).
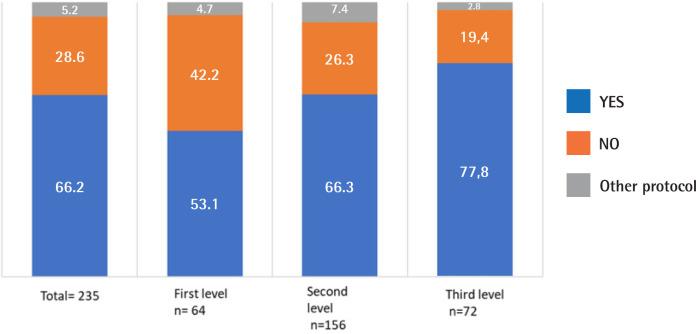
The sepsis code was implemented in 157 of 235 participating centers (66.2%), particularly in tertiary hospitals. Only 92 (30.2%) of sepsis code activations involved the application of a management bundle (e.g., obtaining cultures, initiation of appropriate empirical antimicrobials, hemodynamic resuscitation, and seeking ICU consultation) (supplementary table 4). Among the 380 SEMES responses regarding the obtention of cultures, only 320 (84.2%) of participants urged for their rapid blood extraction, and 68.3% asked for the obtention of two separate sets of blood cultures by venipuncture. Empirical antimicrobials were prescribed following institutional protocols in 72.3% of the participating centers. Of note, administration of the antimicrobials in the emergency department was limited by administrative distribution issues or insufficient stock onsite in 38.3% of centers.
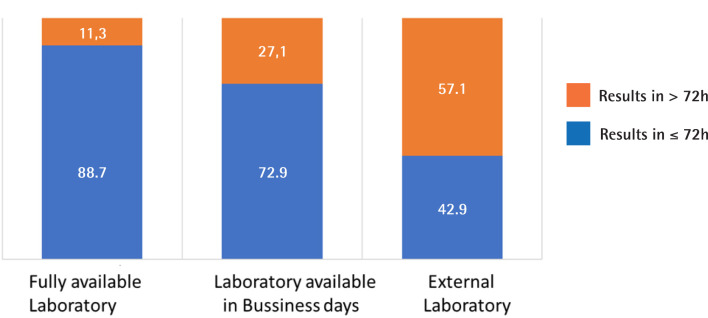
Regarding microbiological diagnosis (supplementary table 5), prioritization of blood cultures samples of sepsis code patients was infrequent (35 of 93 centers, 37.6%), due to the absence of a specific protocol to handle samples or the lack of a communication network between health care professionals responsible for activating Sepsis Code and the microbiological laboratory. The mean frequency of contaminated blood cultures was 8.9% (8.7). Only 17 (18.3%) of laboratories perform the rapid antimicrobial susceptibility testing recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST). In 85 (78.7%) centers, positive results of blood cultures were available within the first 72 hours and were communicated to the treating physician effectively by phone or e-mail in 76 (81.7%) cases (Figure 1).
Figure 1.
The time to obtain positive blood culture results depends on the availability of a microbiology laboratory.
The numbers represent the proportion of hospitals. There were significant differences in time to results according to the availability of microbiology laboratory (p=0.012)
Antimicrobial stewardship processes (Supplementary Figure 1) were indagated in 95 SEMYCYUC-GTEIS specialists and 95 SEIMC-C specialists (supplementary table 1). The main reason for escalating treatment was clinical deterioration (e.g., shock or organ dysfunction) (79.4% of SEMICYUC-GTEIS specialists and 87.4% of SEIMC-C). However, the reason for de-escalating antimicrobials was significantly different between the two specialties (table 1).
Table 1.
Decision criteria for antimicrobial therapy modification.
| Total n= 192 |
SEMICYUC-GTEIS n= 97 |
SEIMC-Clinical n= 95 |
|
|---|---|---|---|
| Escalate Treatment | |||
| ICU admission | 5 (2.6) | 5 (5.2) | 0 (0) |
| Clinical deterioration | 160 (83.3) | 77 (79.4) | 83 (87.4) |
| Microbiological results | 16 (8.3) | 11 (13.4) | 3 (3.2) |
| Abnormalities of laboratory values | 11 (5.7) | 2 (2.1) | 9 (9.5) |
| De-escalate Treatment | |||
| Clinical Improvement | 41 (21.6) | 20 (21.1) | 21 (21.1) |
| Microbiological results | 87 (45.8) | 61 (62.4) | 26 (27.4) |
| Antimicrobial Stewardship Program | 62 (32.6) | 14 (14.7) | 48 (50.5) |
Values are depicted as totals (n)(%). Significant differences in the decision for escalation and de-escalation of treatment (p<0,001). SEMICYUC denotes Spanish Society of Intensive Care Medicine and Coronary Units, GTEIS Spanish Working group of Infectious diseases and Sepsis, SEIMC Spanish Society of Infectious Diseases and Clinical Microbiology receiving one survey to assess clinical diagnosis (SEIMC-C), PROA Antimicrobial stewardship Optimization program.
Quality indicators were not registered by 76 of 206 SEMES, 32 of 66 (48.5%) SEMICYUC-GTEIS, 61 of 94 (64.9%) SEIMC-M, and 54 of 74 (73%) SEIMC-C specialists. Additional results are detailed in the Supplementary Material.
DISCUSSION
This study describes the results of the first multidiscipli-nary survey in Spain evaluating the processes for the identification and initial management of sepsis. Substantial barriers to appropriate sepsis management were identified. Outstandingly, the implementation of the Sepsis Code is limited to some institutions, and there are significant delays in the notification of blood culture results since the availability of microbiology laboratories 24 hours a day is not widely extended. The limited use of rapid identification techniques for microbiological diagnosis, barriers to the prompt administration of appropriate antimicrobials, and differences in antimicrobial stewardship among specialties are significant. Simplified systems that aid the rapid implementation of recommendations, such as the “Sepsis Six” (United Kingdom), have had notable contributions to the improvement of clinical outcomes (e.g., reduced the number of ICU admissions, hospital length of stay, and in-hospital mortality [6]. In a previous study performed in our geographical area, improved clinical outcomes were observed among patients who were managed following the activation of the Sepsis Code protocol in the emergency department [7]. In the present study, only two-thirds of participating centers currently implement Sepsis Code in their institutional protocols, and 40% of activations involve all the interventions recommended in the sepsis bundles (Figure 2). The qSOFA score has been widely used as a screening tool, and SIRS in the context of infection as criteria for confirming the diagnosis. The use of biomarkers is limited, despite their benefits for the early recognition of sepsis, risk stratification, and antimicrobial de-escalation [8,9].
Figure 2.
Centers implementing Sepsis Code protocols.
Numbers represent the proportion of participating centers. Significant differences are observed in the availability of Sepsis Code among participating centers according to the level of care (p=0.024)
Though frequently overlooked, transferring blood cultures to the microbiology laboratory for analysis and early notification of results to the treating clinician is crucial to effective antimicrobial stewardship during the management of severe infections. Thus, it is worrying that only 46% of participating centers have a full-time available microbiology laboratory, leading to delays in laboratory results determining subsequent inappropriate antimicrobial stewardship decisions. Our results prove that in centers with available laboratories only in business days (27% of centers), blood culture results are delayed more than 72 hours. This proportion doubles in the case of centers that depend on external microbiology laboratories to send, often during working hours, and process samples. Using satellite blood culture incubators onsite could significantly reduce the times for incubation of blood cultures in the emergency department and ICU [10]. Also, adequate communication processes between laboratory and clinicians determine management.
Regarding the quality of blood culture testing, less than 20% of centers perform the rapid antimicrobial susceptibility testing recommended by the EUCAST. Although obtaining a second set of blood cultures improves the sensitivity for the detection of bacteriemia, only two-thirds of the centers perform two sets of blood cultures by peripheral venipuncture [11]. The proportion of contaminated blood cultures is consistent with another tertiary center in our geographical area [12] and triples the recommended rate by the SEIMC [13]. According to its current recommendations, quality improvement programs on the importance of the blood culture aseptic technique, the use of the same needle for extraction and inoculation, and optimal antiseptics for use before obtaining samples should be reinforced. The current Nursing Working Group Guideline recommends appropriate antiseptic technique for skin prior to venipuncture, using 2% chlorhexidine. Blood culture specimens should be drawn using either a needle and syringe or a vacuum extraction blood-sampling system that draws blood into vacuum-sealed test bottles [14].
Antimicrobial stewardship varies depending on the specialty of the treating physician. Only a minority of specialists (8.3%) escalated treatment according to microbiology results, maintaining initial broad-spectrum empirical antimicrobial treatment. Of note, there are significant differences between intensivists and microbiologists regarding antimicrobial stew-ardship practices. Sixty-three percent of SEMYCIUC specialists modified or de-escalated treatments according to culture results, which contrasts with the 99% of modified treatments when GTEIS specialists were in charge. SEIMC-C specialists based their criteria for de-escalating treatment on antimicrobial optimization programs, while SEMYCIUC-GTEIS specialists mainly base their decisions on culture results.
Finally, the registration of quality indicators that evaluate and optimize antimicrobial stewardship processes is limited in most participating centers. Implementation and monitoring of quality indicators would give more information on sepsis care processes and establish quality improvement programs focused on protocolizing processes and adequate follow-up.
This study has some limitations. First, subjective impressions of participants may modify data on the quality-of-care processes. Second, including other front-line professionals, such as nurses, was not possible due to difficulties in reaching a representative number of participants. Although the previously mentioned limitations, this study contributes to identifying barriers and areas for improvement during the management process of sepsis. In some regions of our country, the development of protocols has enhanced appropriate management practices [15]. However, we believe that other Spanish Societies involved in developing quality improvement programs should make specific recommendations that culminate in specific interventions to improve and monitor quality indicators.
ACKNOWLEDGEMENTS
All members of SEMES, SEIMC, SEMICYUC-GTEIS and teamworks who participated in the diffusion and response to the survey.
FUNDING
This research has received an unrestricted grant Beckton, Dickinson and Company (BD), S.A.
CONFLICTS OF INTEREST
MNL has participated as a speaker at scientific meetings sponsored by Accelerate Diagnostics and bioMérieux.
References
- 1.Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-247. DOI: 10.1007/s00134-021-06506-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rüddel H, Thomas-Rüddel DO, Reinhart K, Bach F, Gerlach H, Lind-ner M, et al. Adverse effects of delayed antimicrobial treatment and surgical source control in adults with sepsis: results of a planned secondary analysis of a cluster-randomized controlled trial. Crit Care. 2022;26(1):51. DOI: 10.1186/s13054-022-03901-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mensa J, Barberán J, Ferrer R, Borges M, Rascado P, Maseda E, et al. Recommendations for antibiotic selection for severe nosocomial infections. Rev Esp Quimioter. 2021;34(5):511-24. DOI: 10.37201/req/126.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlbom DJ, Rubenfeld GD. Barriers to implementing protocol-based sepsis resuscitation in the emergency department--results of a national survey. Crit Care Med. 2007;35(11):2525-32. DOI: 10.1097/01.ccm.0000298122.49245.d7 [DOI] [PubMed] [Google Scholar]
- 5.Simmonds M, Hutchinson A, Chikhani M, Bewick T, Meyer J, Davies SR, et al. Surviving Sepsis beyond Intensive Care: A Retrospective Cohort Study of Compliance with the International Guidelines. Journal of the Intensive Care Society. 2008;9:124-7. [Google Scholar]
- 6.Lin Y. Effectiveness of the sepsis six bundle in the management of acute adult sepsis in the UK. Emerg Nurse. 2021;29(2):26-9. DOI: 10.7748/en.2020.e2064 [DOI] [PubMed] [Google Scholar]
- 7.Robert Boter N, Modol Deltell JM, Casas Garcia I, Rocamora Blanch G, Llados Beltran G, Carreres Molas A. Activation of a code sepsis in the emergency department is associated with a decrease in mortality. Med Clin (Barc). 2019;152(7):255-60. DOI: 10.1016/j.medcli.2018.02.013 [DOI] [PubMed] [Google Scholar]
- 8.Schuetz P, Beishuizen A, Broyles M, Ferrer R, Gavazzi G, Gluck EH, et al. Procalcitonin (PCT)-guided antibiotic stewardship: an international experts consensus on optimized clinical use. Clin Chem Lab Med. 2019;57(9):1308-18. DOI: 10.1515/cclm-2018-1181 [DOI] [PubMed] [Google Scholar]
- 9.Baldira J, Ruiz-Rodriguez JC, Wilson DC, Ruiz-Sanmartin A, Cortes A, Chiscano L, et al. Biomarkers and clinical scores to aid the identification of disease severity and intensive care requirement following activation of an in-hospital sepsis code. Ann Intensive Care. 2020;10(1):7. DOI: 10.1186/s13613-020-0625-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orellana MA, Chaves F, Delgado R. Improved blood culture work-flow in the time to detection of microorganisms placing incubators systems outside of microbiology laboratory. Braz J Microbiol. 2020;51(3):1103-8. DOI: 10.1007/s42770-020-00298-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coburn B, Morris AM, Tomlinson G, Detsky AS. Does this adult patient with suspected bacteremia require blood cultures? Jama. 2012;308(5):502-11. DOI: 10.1001/jama.2012.8262 [DOI] [PubMed] [Google Scholar]
- 12.Pinilla Rello A, Huarte Lacunza R, Magallón Martínez A, Marrón Time to decision in sepsis Tundidor R, Martínez Álvarez R, Bustamante Rodríguez E, et al. [Assessment of outcomes of implementing the Sepsis Code in the emergency department of a tertiary hospital]. J Healthc Qual Res. 2020;35(5):281-90. DOI: 10.1016/j.jhqr.2020.06.008 [DOI] [PubMed] [Google Scholar]
- 13.Rodríguez Díaz JC, Guna Serrano MR, Larrosa Escartín N, and Marín Arriaza M. Diagnóstico microbiológico de la bacteriemia y la fungemia: hemocultivos y métodos moleculares. 2017. 62. Procedimientos en Microbiología Clínica. Cercenado Mansilla E, Cantón Moreno R (editores). Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC). 2017. https://seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimientomicrobiologia62.pdf. [DOI] [PubMed] [Google Scholar]
- 14.Grupo de trabajo de la Guía de Práctica Clínica Enfermera sobre Hemocultivos . 2020. Guía de Práctica Clínica Enfermera sobre Hemocultivos. Instituto Español de Investigación Enfermera, 2020. Guías de Práctica Clínica Enfermera en el Instituto Español de Investigación Enfermera: Madrid n.º 2020/01., [Google Scholar]
- 15.Yebenes JC, Lorencio C, Esteban E, Espinosa L, Badia JM, Capdevila JA, et al. Interhospital Sepsis Code in Catalonia (Spain): Territorial model for initial care of patients with sepsis. Med Intensiva. 2020;44(1):36-45. DOI: 10.1016/j.medin.2019.05.008 [DOI] [PubMed] [Google Scholar]