Abstract
Background:
Hippocampal disturbances are important in the pathophysiology of both schizophrenia and major depressive disorder (MDD). Imaging studies have shown selective volume deficits across hippocampal subfields in both disorders. We aimed to investigate whether these volumetric alterations in hippocampal subfields are shared or divergent across disorders.
Methods:
We searched PubMed and Embase from database inception to May 8, 2021. We identified MRI studies in patients with schizophrenia, MDD or both, in which hippocampal subfield volumes were measured. We excluded nonoriginal, animal or postmortem studies, and studies that used other imaging modalities or overlapping data. We conducted a network meta-analysis to estimate and contrast alterations in subfield volumes in the 2 disorders.
Results:
We identified 45 studies that met the initial criteria for systematic review, of which 15 were eligible for network metaanalysis. Compared to healthy controls, patients with schizophrenia had reduced volumes in the bilateral cornu ammonis (CA) 1, granule cell layer of the dentate gyrus, subiculum, parasubiculum, molecular layer, hippocampal tail and hippocampus–amygdala transition area (HATA); in the left CA4 and presubiculum; and in the right fimbria. Patients with MDD had decreased volumes in the left CA3 and CA4 and increased volumes in the right HATA compared to healthy controls. The bilateral parasubiculum and right HATA were smaller in patients with schizophrenia than in patients with MDD.
Limitations:
We did not investigate medication effects because of limited information. Study heterogeneity was noteworthy in direct comparisons between patients with MDD and healthy controls.
Conclusion:
The volumes of multiple hippocampal subfields are selectively altered in patients with schizophrenia and MDD, with overlap and differentiation in subfield alterations across disorders. Rigorous head-to-head studies are needed to validate our findings.
Introduction
Schizophrenia and major depressive disorder (MDD) are common psychiatric illnesses with overlaps in pathogenesis, symptom presentation and neurobiological features. Epidemiological evidence suggests that both disorders are associated with prenatal maternal adversity, which is a well-established risk factor for pathogenesis.1,2 Large-scale genome-wide association meta-analysis has shown that biological etiology is partially shared in schizophrenia and MDD.3 Clinically, up to 80% of patients with schizophrenia experience depressive episodes in the early stages of illness,4 and people with depression or anxiety disorders may have psychotic symptoms.5 Impulsivity and anhedonia can also be observed in both disorders.6,7 Neurobiological data further reveal a relationship between symptom severity and oxytocin in both disorders,8,9 as well as a genetic correlation between them.10 Overlaps in structural brain alterations have also been found in schizophrenia and MDD,11 including reductions in hippocampal volume.12,13 Because the hippocampus consists of several subfields that relate to cognitive and affective disturbances, abnormalities in its subregions are worthy of investigation. Subfield-level comparisons of volumetric alterations in schizophrenia and MDD would help us to better understand the pathophysiology of both disorders.
Hippocampal subfields are histologically and functionally distinct, including the cornu ammonis (CA) 1 to 4, the dentate gyrus and the subiculum.14 MRI-based segmentation methods in FreeSurfer software (surfer.nmr.mgh.harvard.edu) provide automatic volume measurement of hippocampal subfields with high accuracy.15 These methods have shown favourable performance and have been used widely. For example, Free-Surfer 6.0, employing the atlas of Iglesias and colleagues,15 measures the CA1, CA2/3 and CA4 comparably to histological examinations;16 it also yields higher reproducibility and traces more quickly than manual segmentation.17
Previous MRI studies in schizophrenia and MDD have found selective volume deficits in hippocampal subfields, but the subregions involved have varied across reports. Generally, volume reduction has been identified in the whole hippocampus, CA1, CA2/3, CA4/dentate gyrus and subiculum in patients with schizophrenia,13,18,19 and in the CA1, CA4, molecular layer and hippocampal tail in patients with MDD compared to healthy controls.20,21 Given the partial overlap of subfield volume deficits across disorders, the variability in findings across studies, and the fact that hippocampal subfield volumes have usually been assessed in either schizophrenia or MDD rather than compared directly between them,13,22–24 questions have arisen about the degrees of overlap and differentiation between hippocampal subfield abnormalities in these disorders. Moreover, associated studies have been limited by small and heterogeneous samples and divergent volumetry methods. In this context, a network metaanalysis may be a useful strategy for characterizing similarities and differences in hippocampal alterations, providing a quantitative approach to contrasting hippocampal volumes between schizophrenia and MDD.25,26
We performed a systematic review to summarize the volume alterations in hippocampal subfields in schizophrenia and MDD and a network meta-analysis to quantitatively compare those alterations between disorders. We hypothesized that volume abnormalities in hippocampal subfields would have overlapping features in the CA1 and CA4 in patients with schizophrenia and patients with MDD, and illness-specific features in other subfields.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension statement for the reporting of systematic reviews incorporating network meta-analyses.27 The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42021291470). We did not obtain institutional review board approval, because the included data had been previously published and no individual patient information was involved.
Search strategy, eligibility criteria and study selection
We searched PubMed (www.ncbi.nlm.nih.gov/pubmed) and Embase (www.embase.com) from database inception until May 8, 2021. Details of the search strategy are presented in Appendix 1, Supplementary Methods, available at www.jpn.ca/lookup/doi/10.1503/jpn.220086/tab-related-content. We also manually searched relevant publications for citations that might meet our eligibility criteria.
We included studies in the systematic review if they were MRI studies in patients with schizophrenia, MDD or both; segmented hippocampal subfields and measured volumes; compared patients with schizophrenia or MDD with healthy controls; and were published in English. The exclusion criteria were as follows: nonoriginal studies (e.g., methodological studies, reviews, meta-analyses or case reports); animal or postmortem studies, or studies using imaging modalities other than MRI; studies limited to pediatric or geriatric patients; or studies with identical samples in distinct publications. If studies used partially overlapping samples, we classified the study with the smaller sample size as an overlapping sample and excluded it from the network meta-analysis but included it in the systematic review. In addition to meeting the above inclusion and exclusion criteria, if studies used FreeSurfer with the atlas of Iglesias and colleagues15 and reported bilateral hippocampal subfield volumes as means and standard deviations or errors, we included them in the network meta-analysis.
Two reviewers (S.Y. and H.N.) independently screened and selected the studies. They resolved inconsistencies through discussion, and examples of inconsistencies are provided in Appendix 1, Supplementary Methods. We obtained the full texts of all publications identified as relevant to extract information. We contacted the corresponding authors to obtain unpublished study details, if necessary. Details of study quality assessment are presented in Appendix 1, Supplementary Methods.
Data extraction and summary measures
We obtained data according to 2 analysis plans. First, for studies included in the systematic review, we extracted information about each participant group, including the group category, number of participants, sex ratio, mean age, field strength of the MRI scanner, method of segmentation, study design and main findings. Then, for the studies that met the inclusion criteria for network meta-analysis, we also extracted information about mean age at onset, mean duration of illness, mean number of previous illness episodes, mean symptom ratings, medication status and history of substance use. We extracted mean values and standard deviations of volume measurements for the whole hippocampus and 12 hippocampal subfields, including the CA1, CA3, CA4, granule cell layer of the dentate gyrus, subiculum, presubiculum, parasubiculum, molecular layer, hippocampal tail, fimbria, hippocampal fissure and hippocampus–amygdala transition area (HATA). According to the atlas definition by Iglesias and colleagues,15 CA3 included CA2, and CA4 included the polymorphic layer of the dentate gyrus; the molecular layer consisted of the corresponding layers of the CA and subiculum; and the hippocampal fissure separated the subiculum and the CA from the dentate gyrus as a sulcus.
If only standard errors were reported, we performed conversions to generate standard deviations. If data were reported only graphically, we used WebPlotDigitizer (automeris.io/WebPlotDigitizer) to extract mean values and standard deviations. This tool is a semiautomated, Internet-based application for extracting data from plots, images and maps. For multicentre studies, we treated multiple data sets as separate samples. For studies that divided patient groups into subgroups, we merged the subgroup data (Appendix 1, Supplementary Methods). In the meta-analysis, some studies did not measure smaller hippocampal subfields because of concerns about segmentation reliability; as a result, not all included studies reported every subfield. For each hippocampal subfield, we summarized the number of studies and participants included in the network meta-analysis.
Statistical analysis
In a frequentist framework, we implemented network metaanalysis using R software (version 4.1.3; R Foundation for Statistical Computing) with the metafor and netmeta packages. We obtained direct volume comparisons for patients with schizophrenia versus healthy controls and patients with MDD versus healthy controls by synthesizing the respective original studies. We obtained indirect volume comparisons for patients with schizophrenia versus patients with MDD by synthesizing the studies that compared patients with schizophrenia versus healthy controls and patients with MDD versus healthy controls. To better control for heterogeneity across studies, we selected random-effects models for network meta-analysis. We set a 2-tailed p value of less than 0.05 as statistically significant for the case–control and schizophrenia–MDD contrasts. We used false discovery rate to correct for multiple comparisons. We analyzed 12 hippocampal subfields and the whole hippocampus for each hemisphere, so the number of tests for each analysis was 13.
We evaluated transitivity and inconsistency as the basis of network meta-analysis. We assessed heterogeneity using the I2 statistic,28 with values of 75%, 50% and 25% indicating high, medium and low degrees of heterogeneity, respectively. For each direct comparison with an I2 value greater than 50%, we analyzed the source of the heterogeneity by assessing the potential effects of relevant variables on effect size (mean difference). We performed random univariate effects meta-regression for continuous variables. The dependent variable was effect size (mean difference) between patients and healthy controls for each study. The independent variables were the continuous variables extracted from each study, including age at study, age at onset, illness duration and severity score.
Although only 7 of 15 studies reported intracranial volume (ICV), we reperformed network meta-analysis for these 7 studies to explore the effect of ICV. We did not control for sex effects because no differences in sex ratio were found between patients with schizophrenia and healthy controls (χ2 = 0.10, p = 0.75) or between patients with MDD and healthy controls (χ2 = 1.36, p = 0.24). We also performed direct cross-sectional comparisons between patients with schizophrenia and patients with MDD after controlling for ICV. Details are presented in Appendix 1, Supplementary Methods.
Because of the limited number of included studies, it was not feasible to use funnel plots to detect publication bias.29 Instead, we chose the Egger linear regression test, which quantitatively assesses bias with high detection efficacy for small samples and continuous variables.30 We used comprehensive meta-analysis software (version 3; BioStat) for meta-regression and the assessment of publication bias.
Results
Study selection
The search strategy identified 840 records, of which 45 studies16,20,21,23,31–71 were included in the systematic review. Appendix 1, Figure S1, shows the flowchart for literature screening and eligibility assessment. A total of 2624 patients with schizophrenia (1767 males and 857 females; mean age 34.4 years), 1417 patients with MDD (523 males and 894 females; mean age 37.6 years) and 4788 healthy controls (2516 males and 2272 females; mean age 33.9 years) were included. Of the 45 studies, 17 compared volumetric metrics between patients with schizophrenia and healthy controls, 27 compared volumetric metrics between patients with MDD and healthy controls and 1 compared volumetric metrics among patients with schizophrenia, patients with MDD and healthy controls. The magnetic field strengths of MRI scanners were 7 T (3 studies), 4.7 T (3 studies), 3 T (33 studies), 1.5 T (4 studies) and both 1.5 T and 3 T (1 study); the remaining study did not report magnetic field strength. Forty-one studies segmented the hippocampus along the transverse axis, and 4 studies62,65–67 employed a more detailed segmentation method (e.g., further dividing certain subfields into heads and bodies). The main characteristics of each study are summarized in Table 1. Several studies reported findings with overlapping samples.21,41,42,47,61,62,63,67
Table 1.
Characteristics of studies included in the systematic review (part 1 of 3)
| Author (year) | Participants, n (% female, mean age) | MRI scanner | Segmentation method | Study design | Main findings |
|---|---|---|---|---|---|
| Alnæs et al.42 (2019)*† | Schizophrenia, 1151 (31%, 34 y) Healthy controls, 2010 (44%, 33 y) |
1.5 T and 3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort, multisite; genes | Smaller volume in all subfields; larger left and right hippocampal fissure |
| Brown et al.43 (2019) | MDD, 24 (38%, 40 y) Healthy controls, 20 (25%, 40 y) |
7.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort | No significant difference |
| Cao et al.44 (2018) | MDD, 24 (58%, 31 y) Healthy controls, 15 (66%, 33 y) |
3.0 T | Automatic (FreeSurfer 5.3¶) | Longitudinal design, case–control; ECT | Baseline: no significant difference Longitudinal changes: increased left CA2/3, left and right CA4, left and right granule cell layer of the dentate gyrus, left subiculum |
| Cao et al.31 (2017) | MDD, 86 (70%, 41 y) Healthy controls, 152 (63%, 35 y) |
1.5 T | Automatic (FreeSurfer 5.3¶) | Cross-sectional design, case–control | No significant difference |
| Doolin et al.32 (2018) | MDD, 74 (64%, 33 y) Healthy controls, 37 (51%, 31 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort | Smaller left CA1, left and right CA2/3, right CA4 |
| du Plessis et al.33 (2020) | First-episode schizophrenia, 79 (27%, 23 y) Healthy controls, 82 (43 %, 23) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort | Statistical analysis between 2 groups was not available |
| Frodl et al.45 (2014) | MDD, 43 (60%, 41 y) Healthy controls, 43 (60%, 37 y) |
3.0 T | Automatic (FreeSurfer**) | Cross-sectional design, case–control; genes | Smaller CA1, CA2/3, CA4/dentate gyrus, subiculum |
| Frodl et al.46 (2014) | MDD, 38 (66%, 41 y) Healthy controls, 44 (61%, 36 y) |
3.0 T | Automatic (FreeSurfer**) | Cross-sectional design, case–control; genes | Smaller left CA2/3, left CA4/dentate gyrus |
| Han et al.21 (2019)‡ | MDD, 102 (59%, 36 y) Healthy controls, 135 (58%, 36 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Smaller left and right whole hippocampus, left and right CA1, left CA2/3, left and right CA4, left and right granule cell layer of the dentate gyrus, right subiculum, right presubiculum, left and right molecular layer |
| Han et al.47 (2017)‡ | MDD, 105 (82%, 43 y) Healthy controls, 85 (71%, 40 y) |
3.0 T | Automatic (FreeSurfer 5.3¶) | Cross-sectional design, case–control; genes | No significant difference |
| Han et al.48 (2016) | MDD, 20 (100%, 42 y) Healthy controls, 21 (100%, 42 y) |
1.5 T | Automatic (FreeSurfer 5.3**) | Cross-sectional design, case–control | Smaller left whole hippocampus, left CA2/3, left CA4/dentate gyrus, left and right subiculum |
| Harel et al.49 (2016) | MDD, 15 (53%, 36 y) Healthy controls, 15 (47%, 37 y) |
3.0 T | Automatic (FreeSurfer 5.3**) | Cross-sectional design, case–control | Smaller right whole hippocampus, right CA1, right CA2/3, right CA4/dentate gyrus |
| Ho et al.16 (2017) | Schizophrenia, 155 (32%, 32 y) Healthy controls, 79 (35%, 31 y) |
3.0 T | Automatic (FreeSurfer 5.3¶) | Cross-sectional design, case–control; longitudinal design in a subcohort; multisite | Schizophrenia: smaller left and right whole hippocampus, left CA1 Early-course schizophrenia: smaller left and right whole hippocampus, left and right CA1, right granule cell layer of the dentate gyrus Longitudinal changes: decreased left and right CA1, right CA2/3, left and right granule cell layer of the dentate gyrus, right molecular layer |
| Schizophrenia, 46 (22%, 43 y) Healthy controls, 46 (22%, 42 y) |
Smaller left and right whole hippocampus, left and right CA1, left and right CA2/3, left and right CA4, left and right granule cell layer of the dentate gyrus, left and right subiculum, left and right molecular layer, left and right hippocampal tail | ||||
| Hu et al.66 (2020) | Never-treated long-term schizophrenia, 29 (55%, 46 y) Treated long-term schizophrenia, 40 (55%, 48 y) Healthy controls, 40 (55%, 48 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Never-treated long-term schizophrenia: smaller left and right whole hippocampus, right CA1 (body), left and right CA2/3 (head), right CA2/3 (body), left and right CA4 (head), left and right CA4 (body), left and right granule cell layer of the dentate gyrus (head), left and right granule cell layer of the dentate gyrus (body), left and right subiculum (body), left and right molecular layer (body), left and right hippocampal tail Treated long-term schizophrenia: smaller left and right whole hippocampus, left CA4 (body), left granule cell layer of the dentate gyrus (body), left and right subiculum (body), left and right molecular layer (body), left and right hippocampal tail |
| Hu et al.50 (2019) | Nonresponding MDD, 13 (38%, 36 y) Early responding MDD, 25 (44%, 36 y) Healthy controls, 55 (62%, 36 y) |
3.0 T | Automatic (FreeSurfer 5.3**) | Cross-sectional design, case–control, cohort | MDD: no significant difference Nonresponding MDD: larger left and right CA1, left CA2/3, left CA4/dentate gyrus, left and right subiculum |
| Huang et al.67 (2013)§ | Unmedicated MDD, 9 (44%, 33 y) Medicated MDD, 11 (55%, 37 y) Healthy controls, 27 (70%, 33 y) |
4.7 T | Manual | Cross-sectional design, case–control | Unmedicated MDD: smaller CA1–3 (body), dentate gyrus |
| Hýža et al.51 (2016) | First-episode schizophrenia, 58 (0%, 23 y) Healthy controls, 58 (0%, 24 y) |
1.5 T | Automatic (FreeSurfer 5.2**) | Cross-sectional design, case–control | Larger left CA1 |
| Jiang et al.52 (2019) | Schizophrenia with symptom remission after ECT, 10 (50%, 30 y) Schizophrenia without symptom remission after ECT, 11 (55%, 28 y) Schizophrenia treated by ECT (with and without symptom remission), 21 (52%, 29 y) Schizophrenia with symptom remission after antipsychotic medication, 12 (75%, 31 y) Schizophrenia without symptom remission after antipsychotic medication, 9 (33%, 30 y) Schizophrenia treated by antipsychotic medication (with and without symptom remission), 21 (57%, 31 y) Healthy controls, 23 (52%, 31 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Longitudinal design, cohort; ECT | Longitudinal changes: schizophrenia treated by ECT (with and without symptom remission), increased left and right whole hippocampus |
| Kakeda et al.53 (2018) | First-episode MDD, 40 (50%, 47 y) Healthy controls, 47 (28%, 41 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | No significant difference |
| Kawano et al.68 (2015) | First-episode schizophrenia, 19 (53%, 25 y) Subchronic schizophrenia, 6 (50%, 22 y) Chronic schizophrenia, 9 (33%, 37 y) Healthy controls, 15 (33%, 25 y) |
1.5 T | Automatic (FreeSurfer 5.1**) | Cross-sectional design, case–control; longitudinal design in a subcohort | Baseline: first-episode schizophrenia, smaller left CA2/3, left CA4/ dentate gyrus Subchronic schizophrenia: smaller left whole hippocampus, left CA2/3, left CA4/ dentate gyrus Chronic schizophrenia: smaller left whole hippocampus, left CA2/3, left CA4/ dentate gyrus |
| Kraus et al.54 (2019) | Acute MDD, 20 (70%, 31 y) Remitted MDD, 28 (57%, 27 y) Healthy controls, 22 (55%, 26 y) |
7 T | Automatic (FreeSurfer 6.0¶) | Longitudinal design, open-label trial | Time 1: remitted MDD, larger right hippocampal fissure Longitudinal changes: no significant difference Time 2: remitted MDD, larger right HATA |
| Li et al.55 (2018) | First-episode schizophrenia, 41 (59%, 24 y) Healthy controls, 39 (51%, 24 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control; longitudinal design; antipsychotics | Baseline: larger left and right CA4, left and right granule cell layer of the dentate gyrus, left and right molecular layer Longitudinal changes: decreased left and right whole hippocampus, left CA1, left CA2/3, left and right CA4, left and right granule cell layer of the dentate gyrus, left and right molecular layer, left and right hippocampal tail, left fimbria After treatment: larger left and right CA4 |
| Maller et al.20 (2018) | MDD, 182 (52%, 33 y) Healthy controls, 68 (50%, 30 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Open-label trial | Baseline: larger hippocampal tail |
| Mathew et al.69 (2014) | Schizophrenia, 219 (34%, 35 y) Healthy controls, 337 (55%, 37 y) |
Unknown | Automatic (FreeSurfer 5.1**) | Cross-sectional design, case–control, multisite | Smaller left and right whole hippocampus, left and right CA1, left and right CA2/3, left and right CA4/dentate gyrus, left and right subiculum, left and right presubiculum |
| Mikolas et al.56 (2019) | MDD, 85 (67%, 39 y) Healthy controls, 67 (67%, 36 y) |
3.0 T | Automatic (FreeSurfer 5.3¶) | Cross-sectional design, case–control; genes | Smaller whole hippocampus, CA1, CA2/3, CA4, granule cell layer of the dentate gyrus, molecular layer |
| Na et al.57 (2014) | MDD, 45 (76%, 42 y) Healthy controls, 72 (71%, 41 y) |
3.0 T | Automatic (FreeSurfer 5.0**) | Cross-sectional design, case–control; genes | No significant difference |
| Na et al.34 (2018) | MDD, 47 (100%, 45 y) Healthy controls, 30 (100%, 43 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control; genes | No significant difference |
| Nakahara et al.35 (2020) | Schizophrenia, 176 (25%, 39 y) Healthy controls, 173 (29%, 38 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, multisite | Smaller CA1, CA4, granule cell layer of the dentate gyrus, molecular layer, hippocampal tail; larger hippocampal fissure |
| Nguyen et al.58 (2019) | First-episode MDD, 38 (47%, 47 y) Healthy controls, 39 (28%, 41 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control; genes | No significant difference |
| Ohi et al.36 (2021) | Schizophrenia, 138 (60%, 42 y) Healthy controls, 162 (33%, 37 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Smaller right HATA; larger right hippocampal fissure |
| Orfei et al.59 (2017) | Schizophrenia, 45 (33%, 40 y) Healthy controls, 45 (33%, 40 y) |
3.0 T | Automatic (FreeSurfer**) | Cross-sectional design, case–control | Smaller left and right whole hippocampus, left and right CA1, left and right CA2/3, left and right CA4/dentate gyrus, left subiculum, left and right presubiculum, left and right hippocampal fissure |
| Ota et al.23 (2017) | Schizophrenia, 20 (25%, 37 y) MDD, 36 (47%, 38 y) Healthy controls, 35 (46%, 39 y) |
3.0 T | Automatic (ASHS) | Cross-sectional design, case–control | Schizophrenia: smaller whole hippocampus, CA1, dentate gyrus than healthy controls, smaller whole hippocampus, dentate gyrus than MDD without medication MDD: no significant difference |
| Otsuka et al.60 (2019) | First-episode MDD, 27 (41%, 46 y); Healthy controls, 42 (26%, 41 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control; genes | No significant difference |
| Roddy et al.70 (2019) | MDD, 80 (71%, 35 y) Healthy controls, 83 (59%, 32 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Smaller left CA1, left and right CA2/3, left and right CA4, left and right granule cell layer of the dentate gyrus, left and right subiculum, left hippocampal tail; larger right molecular layer |
| Sasabayashi et al.37 (2021) | Schizophrenia, 77 (49%, 29 y) Healthy controls, 87 (47%, 26 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort | Smaller left and right CA1, left and right molecular layer, left hippocampal tail |
| Tannous et al.71 (2020) | MDD, 71 (55%, 32 y) Healthy controls, 46 (54%, 32 y) |
7.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort | No significant difference |
| Tesli et al.61 (2020)† | Schizophrenia with a history of violence, 24 (4%, 34 y) Schizophrenia with no history of violence, 51 (2%, 29 y) Healthy controls, 90 (3%, 33 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control, cohort, multisite | Schizophrenia with a history of violence: smaller whole hippocampus, CA1, molecular layer, fimbria, HATA; larger hippocampal fissure Schizophrenia with no history of violence: no significant difference |
| Travis et al.62 (2015)§ | MDD, 15 (80%, 38 y) Healthy controls, 15 (67%, 35 y) |
4.7 T | Manual | Cross-sectional design, case–control, cohort | Smaller dentate gyrus (body) |
| Travis et al.63 (2016)§ | MDD, 14 (64%, 36 y) Healthy controls, 14 (71%, 33 y) |
4.7 T | Manual | Cross-sectional design, case–control, cohort | No significant difference |
| Vargas et al.64 (2018) | Schizophrenia, 91 (26%, 38 y) Healthy controls, 70 (56%, 18 y) |
3.0 T | Automatic (FreeSurfer 5.3**) | Cross-sectional design, case–control | Smaller left and right whole hippocampus, right CA1, left and right CA2/3, left and right CA4/dentate gyrus, left and right subiculum, left and right presubiculum |
| Xiu et al.38 (2021) | First-episode schizophrenia, 39 (59%, 29 y) Healthy controls, 30 (57%, 28 y) |
3.0 T | Automatic (FreeSurfer 5.3¶) | Cross-sectional design, case–control | No significant difference |
| Xu et al.39 (2018) | MDD, 15 (100%, 35 y) Healthy controls, 12 (100%, 34 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Smaller left fimbria |
| Yuan et al.40 (2020) | MDD, 41 (59%, 35 y) Healthy controls, 44 (59%, 33 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | No significant difference |
| Zheng et al.41 (2019)* | Schizophrenia, 69 (16%, 38 y) Healthy controls, 72 (29%, 36 y) |
3.0 T | Automatic (FreeSurfer 6.0¶) | Cross-sectional design, case–control | Smaller left and right whole hippocampus, left CA1, left subiculum, left and right presubiculum, right parasubiculum, left and right molecular layer, left hippocampal tail |
| Zhou et al.65 (2020) | MDD, 44 (64%, 35 y) Healthy controls, 45 (53%, 33 y) | 3.0 T | Automatic (FreeSurfer 6.0¶) | Longitudinal design; ketamine treatment | Baseline: smaller left and right whole hippocampus Longitudinal changes: increased right whole hippocampus, right CA4 (head), left CA4 (body), left granule cell layer of the dentate gyrus (body), right molecular layer (head) |
ASHS = Automatic Segmentation of Hippocampal Subfields; CA = cornu ammonis; ECT = electroconvulsive therapy; HATA = hippocampus–amygdala transition area; MDD = major depressive disorder.
Overlapped data.
Overlapped data.
Overlapped data.
Overlapped data.
Atlas by van Leemput and colleagues.72
Atlas by Iglesias and colleagues.15
For the network meta-analysis, 15 eligible studies did not have overlapping samples.16,20,21,31–41,70 The main characteristics of these individual studies are shown in Table 2. The total sample size was 2698 (ranging from 27 to 349 per study; 47.6% female), including 779 patients with schizophrenia, 627 patients with MDD and 1292 healthy controls. The mean age of the participants varied from 23.0 to 45.3 years, and the mean age at onset ranged from 18.3 to 40.6 years. The mean duration of illness was 0.64 to 18.2 years. Table 3 and Table 4 characterize the statistical heterogeneities among these studies. Means and standard deviations for the hippocampal subfield volumes are listed and summarized in Appendix 2, available at www.jpn.ca/lookup/doi/10.1503/jpn.220086/tab-related-content. In terms of study quality, all studies in the network meta-analysis achieved Newcastle–Ottawa Scale scores of 6 to 7 points, indicating moderate to high quality (Appendix 1, Table S2). Of the 15 studies included in the network meta-analysis, 3 used FreeSurfer 5.3 for data preprocessing16,31,38 and all used the atlas of Iglesias and colleagues15 for segmentation of hippocampal subfields, generating consistent boundaries for each hippocampal subfield.
Table 2:
Main characteristics of the studies included in the network meta-analysis (part 1 of 2)
| Author (year) | No. participants (female) | Participant age, y | Age at onset, y | Illness duration, y | Mean no. of episodes | Score of severity (scale type) | Medication status | Substance misuse | MRI field strength, subfield segmentation | Study design | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Patients | Healthy controls | p for sex | Patients | Healthy controls | p for age | |||||||||
| Ho et al.16 (2017) | 155 (49) | 79 (28) | 0.66 | 32.5 | 31.2 | 0.30 | 25.9 | 6.6 | NA | 40.6 (PANSS) | CPZ-eq: 212.32 ± 191.25 mg/d | No substance misuse 3 mo preceding the study | 3.0 T, automatic (FreeSurfer 5.3) | Cross-sectional design; case–control; longitudinal in a subcohort; multisite |
| 46 (10) | 46 (10) | > 0.99 | 42.9 | 41.9 | 0.61 | 24.5 | 18.2 | NA | 81.6 (PANSS) | CPZ-eq: 532.45 ± 447.16 mg/d | ||||
| Zheng et al.41 (2019) | 69 (11) | 72 (21) | 0.06 | 37.7 | 35.9 | 0.046 | NA | NA | NA | NA | NA | NA | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
| du Plessis et al.33 (2020) | 79 (21) | 82 (35) | 0.03 | 23.0 | 23.0 | 0.97 | 22.36* | 0.64 | First-episode schizophrenia | 91.27 (PANSS) | Treated ≤ 1 mo | First-episode schizophrenia: 35 (44%) Controls: 22 (27%) |
3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control; cohort |
| Nakahara et al.35 (2020) | 176 (44) | 173 (50) | 0.39 | 38.9 | 37.6 | 0.27 | 21.9 | 17.1 | NA | 57.9 (PANSS) | CPZ-eq: 372 ± 390 mg/d (n = 144) | None | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control; multisite |
| Ohi et al.36 (2021) | 138 (83) | 162 (54) | < 0.05† | 42.0 | 36.7 | < 0.05† | 26.2 | 16.3 | NA | 33.9 (PANSS positive symptoms and PANSS negative symptoms) | CPZ-eq: 519.0 ± 524.0 mg/d | NA | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
| Sasabayashi et al.37 (2021) | 77 (38) | 87 (41) | > 0.05† | 28.8 | 26.3 | < 0.05† | 22.8 | 5.6 | NA | 68.7 (PANSS) | HPD-eq: 10.6 ± 8.3 mg/d (n = 65) | None | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control; cohort |
| Xiu et al.38 (2021) | 39 (23) | 30 (17) | 0.85 | 28.9 | 27.5 | 0.54 | 26.95* | 1.95 | First-episode schizophrenia | 44.5 (MCCB) | All naive | None | 3.0 T, automatic (FreeSurfer 5.3) | Cross-sectional design; case–control |
| Cao et al.31 (2017) | 86 (60) | 152 (96) | > 0.05† | 41.2 | 35.4 | < 0.05† | 32.3* | 8.9 | 3‡ | 10.5 (HDRS-17) | On medication: 4 | Drug use disorder < 10 | 1.5 T, automatic (FreeSurfer 5.3) | Cross-sectional design; case–control |
| Doolin et al.32 (2018) | 74 (47) | 37 (19) | > 0.05 | 32.9 | 30.9 | > 0.05 | NA | NA | First-episode MDD (n = 39) > 1 (n = 35) | 23.46 (HDRS-17) | On medication: 47 Medication-free: 27 | NA | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control; cohort; |
| Maller et al.20 (2018) | 182 (95) | 68 (34) | > 0.05 | 33.0 | 29.6 | 0.048 | 22.2* | 10.8 | 9.6 | 21.36 (HDRS-17) | All naive or with a washout period ≥ 5 half-lives | NA | 3.0 T, automatic (FreeSurfer 6.0) | Open-label trial |
| Na et al.34 (2018) | 47 (47) | 30 (30) | > 0.05 | 45.3 | 43.0 | 0.41 | 40.6* | 4.7 | NA | 12.9 (HDRS-17) | On medication: 35 | NA | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control; genes |
| Xu et al.39 (2018) | 15 (15) | 12 (12) | > 0.05 | 34.6 | 34.1 | 0.51 | NA | NA | NA | 33.13 (HDRS-24) | NA | None | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
| Han et al.21 (2019) | 102 (60) | 135 (78) | > 0.05† | 36.0 | 36.0 | > 0.05† | 32.3* | 3.7 | First-episode MDD (n = 25) > 1 (n = 77) | 13.93 (HDRS-17) | On medication: most | None | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
| Roddy et al.70 (2019) | 80 (57) | 83 (49) | 0.14 | 34.5 | 31.5 | 0.13 | 32.1* | 2.4 | First-episode MDD (n = 43) > 1 (n = 37) | 22.2 (HDRS-17) | NA | None | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
| Yuan et al.40 (2020) | 41 (24) | 44 (26) | 0.96 | 34.8 | 33.3 | 0.54 | 18.3* | 16.5§ | < 3 (n = 18), ≥ 3 (n = 13)¶ | 18.3 (HDRS-17) | Naive: 16 Untreated ≥ 3 w: 25 | MDD with drug use disorder: 17 MDD without drug use disorder: 24 | 3.0 T, automatic (FreeSurfer 6.0) | Cross-sectional design; case–control |
CPZ-eq = chlorpromazine equivalent; HDRS-17 or -24 = 17- or 24-item Hamilton Depression Rating Scale; HPD-eq = haloperidol equivalent; MCCB = MATRICS Consensus Cognitive Battery; MDD = major depressive disorder; NA = not available; PANSS = Positive and Negative Syndrome Scale.
Determined based on the difference between patient mean age and illness duration.
Inferred based on the results of the corresponding analysis of variance or χ2 test.
Median.
One participant lacked information on illness duration.
Ten participants lacked information on number of prior episodes.
Table 3.
Direct volume comparisons between patients with schizophrenia and healthy controls
| Region of interest | Mean difference (95% CI), mm3 | p value* | I 2 , % | No. of studies | No. of patients with schizophrenia | No. of healthy controls |
|---|---|---|---|---|---|---|
| Left whole hippocampus† | −127.840 (−209.381 to −46.298) | 0.005 | 49 | 6 | 700 | 649 |
| Left CA1† | −21.721 (−36.328 to −7.113) | 0.006 | 0 | 7 | 779 | 731 |
| Left CA3 | −4.555 (−9.580 to 0.471) | 0.08 | 42 | 7 | 779 | 731 |
| Left CA4† | −6.875 (−11.728 to −2.021) | 0.008 | 45 | 7 | 779 | 731 |
| Left granule cell layer of the dentate gyrus† | −8.430 (−14.089 to −2.771) | 0.006 | 44 | 7 | 779 | 731 |
| Left subiculum† | −10.245 (−18.124 to −2.366) | 0.01 | 36 | 7 | 779 | 731 |
| Left presubiculum† | −7.667 (−14.219 to −1.116) | 0.03 | 2 | 6 | 578 | 606 |
| Left parasubiculum† | −3.041 (−4.531 to −1.551) | < 0.001 | 0 | 5 | 539 | 576 |
| Left molecular layer† | −17.412 (−27.110 to −7.714) | 0.002 | 0 | 7 | 779 | 731 |
| Left hippocampal tail† | −24.456 (−40.346 to −8.566) | 0.006 | 74 | 7 | 779 | 731 |
| Left fimbria | −2.008 (−5.401 to 1.385) | 0.25 | 20 | 5 | 539 | 576 |
| Left hippocampal fissure† | 4.941 (1.953 to 7.930) | 0.004 | 0 | 5 | 539 | 576 |
| Left HATA† | −2.044 (−3.156 to −0.932) | 0.002 | 23 | 5 | 539 | 576 |
| Right whole hippocampus† | −108.803 (−182.105 to −35.500) | 0.01 | 35 | 6 | 700 | 649 |
| Right CA1† | −16.337 (−29.533 to −3.140) | 0.02 | 32 | 7 | 779 | 731 |
| Right CA3 | −2.776 (−7.850 to 2.299) | 0.28 | 30 | 7 | 779 | 731 |
| Right CA4 | −4.929 (−10.152 to 0.293) | 0.07 | 47 | 7 | 779 | 731 |
| Right granule cell layer of the dentate gyrus† | −6.657 (−11.976 to −1.338) | 0.02 | 38 | 7 | 779 | 731 |
| Right subiculum† | −8.764 (−17.057 to −0.472) | 0.049 | 8 | 7 | 779 | 731 |
| Right presubiculum | −7.051 (−14.077 to −0.024) | 0.06 | 0 | 6 | 578 | 606 |
| Right parasubiculum† | −2.899 (−4.797 to −1.001) | 0.01 | 27 | 5 | 539 | 576 |
| Right molecular layer† | −13.845 (−25.233 to −2.457) | 0.02 | 23 | 7 | 779 | 731 |
| Right hippocampal tail† | −17.221 (−31.208 to −3.234) | 0.02 | 18 | 7 | 779 | 731 |
| Right fimbria† | −4.201 (−6.586 to −1.816) | 0.003 | 0 | 5 | 539 | 576 |
| Right hippocampal fissure† | 9.849 (6.728 to 12.970) | < 0.001 | 0 | 5 | 539 | 576 |
| Right HATA† | −2.727 (−3.787 to −1.667) | < 0.001 | 0 | 5 | 539 | 576 |
CA = cornu ammonis; CI = confidence interval; HATA = hippocampus–amygdala transition area.
Adjusted.
Statistically significant difference.
Table 4.
Direct volume comparisons between patients with MDD and healthy controls
| Region of interest | Mean difference (95% CI), mm3 | p value* | I 2 , % | No. of studies | No. of patients with MDD | No. of healthy controls |
|---|---|---|---|---|---|---|
| Left whole hippocampus | −74.998 (−175.651 to 25.656) | 0.26 | 88 | 5 | 422 | 325 |
| Left CA1 | −13.373 (−28.894 to 2.147) | 0.24 | 83 | 8 | 598 | 546 |
| Left CA3† | −7.491 (−12.873 to −2.109) | 0.04 | 71 | 8 | 598 | 544 |
| Left CA4† | −8.137 (−13.724 to −2.549) | 0.04 | 69 | 7 | 557 | 504 |
| Left granule cell layer of the dentate gyrus | −6.711 (−13.427 to 0.005) | 0.22 | 74 | 6 | 535 | 508 |
| Left subiculum | −7.580 (−16.215 to 1.055) | 0.24 | 66 | 8 | 596 | 546 |
| Left presubiculum | 0.247 (−6.656 to 7.150) | 0.94 | 72 | 5 | 494 | 466 |
| Left parasubiculum | 0.465 (−1.220 to 2.151) | 0.77 | 40 | 4 | 347 | 222 |
| Left molecular layer | −2.925 (−15.559 to 9.710) | 0.77 | 81 | 5 | 493 | 464 |
| Left hippocampal tail | −3.943 (−25.319 to 17.433) | 0.78 | 88 | 4 | 445 | 436 |
| Left fimbria | −4.641 (−10.825 to 1.543) | 0.26 | 74 | 2 | 91 | 92 |
| Left hippocampal fissure | 4.000 (−1.544 to 9.544) | 0.26 | NA | 1 | 75 | 79 |
| Left HATA | 0.628 (−1.139 to 2.396) | 0.70 | 0 | 2 | 258 | 149 |
| Right whole hippocampus | −39.031 (−127.489 to 49.426) | 0.50 | 84 | 5 | 421 | 325 |
| Right CA1 | −9.269 (−22.842 to 4.303) | 0.29 | 71 | 8 | 598 | 547 |
| Right CA3 | −4.766 (−10.052 to 0.520) | 0.17 | 66 | 8 | 598 | 548 |
| Right CA4 | −7.333 (−13.175 to −1.491) | 0.09 | 68 | 7 | 557 | 502 |
| Right granule cell layer of the dentate gyrus | −6.295 (−12.299 to −0.292) | 0.17 | 62 | 6 | 535 | 508 |
| Right subiculum | −8.339 (−17.172 to 0.495) | 0.17 | 77 | 8 | 597 | 547 |
| Right presubiculum | 2.210 (−4.963 to 9.384) | 0.65 | 80 | 5 | 495 | 466 |
| Right parasubiculum | 1.117 (−1.101 to 3.335) | 0.47 | 63 | 4 | 348 | 223 |
| Right molecular layer | 1.735 (−12.626 to 16.095) | 0.81 | 84 | 5 | 495 | 466 |
| Right hippocampal tail | 2.729 (−15.585 to 21.042) | 0.81 | 89 | 4 | 448 | 436 |
| Right fimbria | −4.211 (−9.167 to 0.745) | 0.18 | 0 | 2 | 92 | 92 |
| Right hippocampal fissure | 5.000 (−0.544 to 10.544) | 0.17 | NA | 1 | 78 | 81 |
| Right HATA† | 2.413 (0.958 to 3.868) | 0.01 | 27 | 2 | 260 | 149 |
CA = cornu ammonis; CI = confidence interval; HATA = hippocampus–amygdala transition area; MDD = major depressive disorder; NA, not available.
Adjusted.
Statistically significant difference.
Systematic review
A total of 18 studies compared hippocampal subfield volumes between patients with schizophrenia and healthy controls. Specifically, 15 studies reported smaller hippocampal subfields in patients with schizophrenia than in healthy controls, and 2 studies in patients with first-episode schizophrenia found larger subfields involving the left CA151 and bilateral CA4, the granule cell layer of the dentate gyrus and the molecular layer.55 One study found no volume differences between patients with first-episode schizophrenia and healthy controls.38
Longitudinal changes in hippocampal subfield volumes were also observed in patients with schizophrenia. Ho and colleagues16 showed volume reductions in the bilateral CA1 and granule cell layer of the dentate gyrus, the right CA2/3 and the right molecular layer at an average follow-up of 4.5 years. Jiang and colleagues52 reported that 4-week electroconvulsive therapy induced volume increases in the bilateral hippocampus in patients with schizophrenia relative to drug treatment. In patients with first-episode schizophrenia after short-term drug treatment, Kawano and colleagues68 found volume increases in the left CA4/dentate gyrus, and Li and colleagues55 reported volume decreases in the bilateral whole hippocampus, CA4, granule cell layer of the dentate gyrus, molecular layer, hippocampal tail, left CA1, CA2/3 and fimbria.
In 28 studies, hippocampal subfield volumes were compared between patients with MDD and healthy controls. Of those, 14 studies found no volume differences between groups, and 12 studies reported smaller volumes in patients with MDD, including all subfields except the parasubiculum and HATA. Four studies reported larger hippocampal subfields in patients with MDD compared to healthy controls: Hu and colleagues50 reported larger volumes in the bilateral CA1 and subiculum and left CA2/3 and CA4/ dentate gyrus in patients who did not respond to antidepressants; Kraus and colleagues54 found larger volumes in the right HATA in remitted patients with MDD; and Maller and colleagues20 and Roddy and colleagues70 identified a larger hippocampal tail and a larger right molecular layer, respectively.
In terms of longitudinal changes in patients with MDD, Cao and colleagues44 found that electroconvulsive therapy induced volume increases in the bilateral CA4 and granule cell layer of the dentate gyrus, and in the left CA3 and subiculum. Zhou and colleagues65 reported increased volumes after ketamine treatment in the right hippocampus, CA4 (head) and molecular layer (head), and in the left CA4 (body) and granule cell layer of the dentate gyrus (body). Kraus and colleagues54 did not detect antidepressant-related changes in subfield volumes in patients with MDD.
Network meta-analysis
Because 12 hippocampal subfields and the whole hippocampus were considered in each hemisphere, we performed network meta-analyses 26 times in total. We performed direct comparisons between patients with schizophrenia and healthy controls and between patients with MDD and healthy controls; we also performed indirect comparisons between patients with schizophrenia and patients with MDD (because the comparison was not based on a direct group comparison in the same study). Subfield volumes were measured in the CA1, CA3 and subiculum by 15 studies; in the CA4 by 14 studies; in the granule cell layer of the dentate gyrus by 13 studies; in the molecular layer by 12 studies; in the whole hippocampus, presubiculum and hippocampal tail by 11 studies; in the parasubiculum by 9 studies; in the fimbria and HATA by 7 studies; and in the hippocampal fissure by 6 studies. For each hippocampal subfield, Table 3 and Table 4 show the number of studies and participants included in the network meta-analysis.
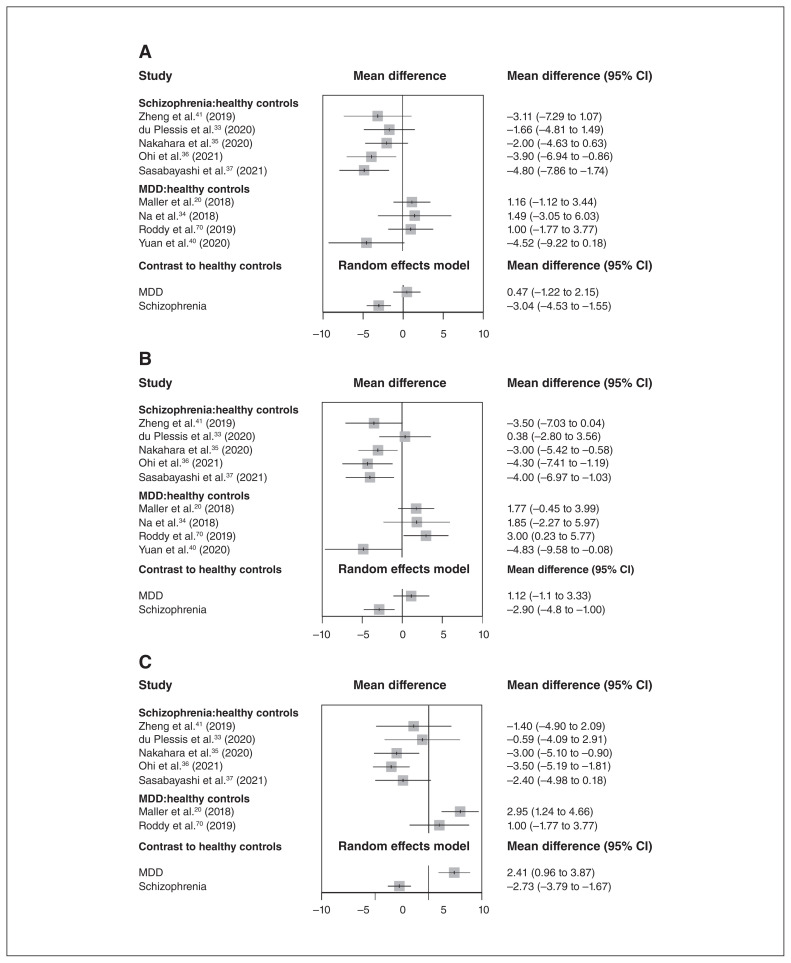
We found volume differences in the bilateral parasubiculum and right HATA between patients with schizophrenia and patients with MDD in the network meta-analysis; forest plots for these subfields are shown in Figure 1. We found no volume differences in other hippocampal subfields between patients with schizophrenia and patients with MDD; related forest plots are shown in the Supplementary Materials (Appendix 1, Figure S2).
Figure 1.
(A) Forest plot for the left parasubiculum. (B) Forest plot for the right parasubiculum. (C) Forest plot for the right HATA. CI = confidence interval; HATA = hippocampus–amygdala transition area; MDD = major depressive disorder.
Through direct volume comparisons with healthy controls, we determined that patients with schizophrenia had smaller volumes in the whole hippocampus bilaterally and in 17 of 24 hippocampal subfields, including the bilateral CA1, granule cell layer of the dentate gyrus, subiculum, parasubiculum, molecular layer, hippocampal tail and HATA; the left CA4 and presubiculum; and the right fimbria. No hippocampal subfields were larger in patients with schizophrenia than in healthy controls (Table 3). Patients with MDD had smaller volumes in the left CA3 and CA4 than healthy controls. Patients with MDD had larger volumes in the right HATA than healthy controls (Table 4). Through indirect comparisons, we found that patients with schizophrenia had smaller subfields than patients with MDD in the bilateral parasubiculum and the right HATA. No hippocampal subfields were larger in patients with schizophrenia than in patients with MDD (Table 5).
Table 5.
Indirect volume comparisons between patients with schizophrenia and patients with MDD
| Region of interest | Mean difference (95% CI), mm3 | p value* |
|---|---|---|
| Left whole hippocampus | −52.842 (−182.380 to 76.696) | 0.67 |
| Left CA1 | −8.347 (−29.661 to 12.966) | 0.67 |
| Left CA3 | 2.936 (−4.428 to 10.300) | 0.67 |
| Left CA4 | 1.262 (−6.139 to 8.663) | 0.77 |
| Left granule cell layer of the dentate gyrus | −1.719 (−10.501 to 7.063) | 0.77 |
| Left subiculum | −2.665 (−14.354 to 9.025) | 0.77 |
| Left presubiculum | −7.914 (−17.431 to 1.602) | 0.34 |
| Left parasubiculum† | −3.506 (−5.755 to −1.256) | 0.03 |
| Left molecular layer | −14.488 (−30.416 to 1.440) | 0.32 |
| Left hippocampal tail | −20.513 (−47.148 to 6.122) | 0.34 |
| Left fimbria | 2.633 (−4.420 to 9.687) | 0.67 |
| Left hippocampal fissure | 0.941 (−5.357 to 7.239) | 0.77 |
| Left HATA | −2.672 (−4.761 to −0.584) | 0.08 |
| Right whole hippocampus | −69.772 (−184.654 to 45.111) | 0.43 |
| Right CA1 | −7.067 (−25.997 to 11.863) | 0.75 |
| Right CA3 | 1.990 (−5.337 to 9.317) | 0.77 |
| Right CA4 | 2.404 (−5.432 to 10.240) | 0.77 |
| Right granule cell layer of the dentate gyrus | −0.362 (−8.383 to 7.659) | 1.00 |
| Right subiculum | −0.426 (−12.542 to 11.691) | 1.00 |
| Right presubiculum | −9.261 (−19.302 to 0.780) | 0.25 |
| Right parasubiculum† | −4.016 (−6.935 to −1.097) | 0.046 |
| Right molecular layer | −15.580 (−33.907 to 2.748) | 0.25 |
| Right hippocampal tail | −19.950 (−42.993 to 3.094) | 0.25 |
| Right fimbria | 0.011 (−5.489 to 5.510) | 1.00 |
| Right hippocampal fissure | 4.849 (−1.513 to 11.211) | 0.29 |
| Right HATA† | −5.140 (−6.940 to −3.340) | < 0.001 |
CA = cornu ammonis; CI = confidence interval; HATA = hippocampus–amygdala transition area; MDD = major depressive disorder.
Adjusted.
Statistically significant difference.
The results of network meta-analysis of 7 studies that reported ICV were not completely consistent with the results from the 15 studies reported above. Through direct comparisons, we found that patients with schizophrenia had smaller volumes in the whole hippocampus bilaterally and in 15 of 24 hippocampal subfields (bilateral CA1, CA4, granule cell layer of the dentate gyrus, subiculum and molecular layer; left hippocampal tail; and right CA3, parasubiculum, fimbria and HATA). No hippocampal subfields were larger in patients with schizophrenia than in healthy controls (Appendix 1, Table S3). Patients with MDD had larger volumes in the right HATA than healthy controls. No hippocampal subfields were smaller in patients with MDD than in healthy controls (Appendix 1, Table S4). Through indirect comparisons, we found that patients with schizophrenia had smaller volumes in the right HATA than patients with MDD. No hippocampal subfields were larger in patients with schizophrenia than in patients with MDD (Appendix 1, Table S5).
Direct comparisons between patients with schizophrenia and patients with MDD
Through direct cross-sectional volume comparisons between patients with schizophrenia and patients with MDD, we found that patients with schizophrenia had larger volumes in the whole hippocampus bilaterally and in 19 of 24 hippocampal subfields (bilateral CA1, CA3, CA4, granule cell layer of the dentate gyrus, subiculum, presubiculum, parasubiculum, molecular layer and hippocampal tail; and right HATA). Patients with schizophrenia had smaller volumes in the left HATA than patients with MDD (Appendix 1, Table S6). We did not perform direct comparisons for the bilateral fimbria and hippocampal fissure because few studies measured all of the subfields.
Meta-regression
The results of the preplanned meta-regression are presented in Appendix 1, Table S7. Corresponding meta-regression graphs are shown in Appendix 1, Figure S3.
For the direct comparison between patients with schizophrenia and healthy controls, heterogeneity in results for the left hippocampal tail was related to age, illness duration and scores on the Positive and Negative Syndrome Scale.
For the direct comparison between patients with MDD and healthy controls, heterogeneity in results for the left CA3 and CA4 was related to age and scores on the Hamilton Depression Rating Scale. Heterogeneity in results for the left granule cell layer of the dentate gyrus was related to age. Heterogeneity in results for the right CA3 and CA4 could be explained by scores on the Hamilton Depression Rating Scale. For these comparisons, all results were initially significant but did not survive false discovery rate correction.
For the direct comparison between patients with MDD and healthy controls, we did not perform meta-regression for the whole hippocampus, parasubiculum, hippocampal tail or left fimbria because few studies measured all subfields. For the remaining hippocampal subfields with I2 greater than 50%, we did not identify any source of heterogeneity.
Heterogeneity, transitivity, inconsistency and publication bias
We evaluated heterogeneity using the I2 statistic; findings are presented in Table 3 and Table 4. From the results of direct meta-analysis, we found evidence for statistical heterogeneity, most notably in pair-wise comparisons between patients with MDD and healthy controls. Because not all included studies consistently reported potential effect modifiers, we could not statistically assess transitivity. Therefore, we evaluated transitivity by comparing the main participant characteristics for the included studies. Because we lacked a direct comparison between patients with schizophrenia and patients with MDD, we did not directly estimate inconsistency. The results of the Egger linear regression test indicated no publication bias in network meta-analysis except for the right HATA in the comparisons between patients with schizophrenia and healthy controls (Appendix 1, Table S8).
Discussion
In this systematic review and network meta-analysis, we investigated the common and specific features in volume abnormalities of hippocampal subfields based on MRI studies in patients with schizophrenia and patients with MDD. The systematic review found that patients with schizophrenia had more extensive hippocampal subfields with volume reduction. We also compared the whole hippocampus and 12 hippocampal subfields in each hemisphere using network meta-analysis. Through direct comparisons with healthy controls, we observed volume abnormalities (increases, decreases or both) in 17 subfields in patients with schizophrenia and in 3 subfields in patients with MDD; only the left CA4 was smaller in both groups compared to healthy controls. Indirect comparisons between patient groups showed that the bilateral parasubiculum and right HATA were smaller in patients with schizophrenia compared to patients with MDD. These findings indicate common and distinct hippocampal volume abnormalities at the subfield level in patients with schizophrenia and patients with MDD. The left CA4 was the only shared hippocampal subfield that showed a volume reduction in both.
Direct comparisons between patients with schizophrenia and healthy controls demonstrated widespread volume deficits across hippocampal subfields in patients with schizophrenia.16,69,73,74 Our findings partially echoed the findings of a study that compared patients with schizophrenia, patients with MDD and healthy controls simultaneously. This study found volume reductions not only in the CA1 and dentate gyrus in patients with schizophrenia compared to healthy controls, but also in the dentate gyrus in patients with schizophrenia compared to patients with MDD.23 Notably, this study used Automatic Segmentation of Hippocampal Subfields (ASHS) as the segmentation tool, rather than FreeSurfer. According to the segmentation protocol,15,75 the dentate gyrus traced by ASHS is roughly equivalent to the combined area of the CA4 and the granule cell layer of the dentate gyrus parcellated by the atlas of Iglesias and colleagues.15 Some original studies in patients with schizophrenia that used a previous segmentation method of FreeSurfer72 also found extensive volume reductions in hippocampal subfields compared to healthy controls, involving the CA1, CA2/3, CA4/dentate gyrus, subiculum and presubiculum.59,64,69 Their results were generally consistent with our findings in these subfields. Although we did not detect a significant difference in CA2/3 volume, the left CA2/3 did show a tendency toward volume decrease. A meta-analysis of postmortem studies in patients with schizophrenia also reported fewer neurons in the CA1, CA2/3 and subiculum76 compared to healthy controls, which was concordant with our findings in the CA1 and subiculum.
Relative to healthy controls, we found fewer hippocampal subfields with volume alterations in patients with MDD than in patients with schizophrenia. A 4.7 T MRI study using manual segmentation found that medication-naive or unmedicated patients with MDD had smaller volumes in the dentate gyrus and CA1 to 3 than healthy controls,67 and this finding was compatible with our direct comparison evidence of a smaller CA2/3. Our findings related to CA2/3 and CA4 also replicated those of studies45,46,48,49 that used a previous segmentation method in FreeSurfer.72 An open-label trial found that patients with remitted MDD had larger volumes in the right HATA, in line with our findings.54 Nevertheless, our findings did not replicate those of the study that used ASHS.23 A large sample study showed a larger hippocampal tail in patients with MDD than in healthy controls,20 and a 7 T MRI study failed to detect any volume abnormalities in hippocampal subfields.71 These inconsistencies in the results may be because of the heterogeneity inherent in mood disorders (related to illness duration and treatment effects) probably along with less robust and more limited findings of hippocampal alterations in patients with MDD.
Greater hippocampal atrophy in the parasubiculum and HATA in patients with schizophrenia relative to patients with MDD may contribute to the distinct clinical presentations associated with the 2 disorders. The parasubiculum is a major input structure of the medial entorhinal cortex77 and is involved in scene-based cognitive and spatial processing.77 A study found that the performance of scene processing was significantly impaired in patients with schizophrenia compared to patients with depression.78 The parasubiculum is also associated with the integration of hippocampal and cortical information processing,79 which has been found to be impaired in patients with schizophrenia.80 The HATA, closely connected with amygdala nuclei that pertain to the hippocampal–amygdala network, is related to fear regulation and situational learning.81,82 A previous study that measured skin conductance response to interpersonal stimuli found that patients with schizophrenia exhibited poorer fear conditioning than patients with depression.83 Thus, in aggregate, differences between schizophrenia and MDD in terms of parasubiculum and HATA volumetric alterations might contribute to the distinct cognitive impairments and emotional dysregulation seen in the 2 disorders. However, considering the publication bias we found in relation to findings for the right HATA in patients with schizophrenia, these findings should be interpreted with caution and warrant further study.
The deficient CA4 (including the polymorphic layer of the dentate gyrus in our study) in patients with schizophrenia and patients with MDD suggests a common structural feature of the disorders. The CA4/dentate gyrus is the initial hippocampal substructure along the trisynaptic pathway, and it acts as the input gate for the dentate gyrus–CA3–CA1–subiculum circuit.84 As proposed in a pathophysiological model of schizophrenia,85 disruptions in the CA4/dentate gyrus may weaken glutamate transmission to the CA3, which in turn promotes local neuronal hypersensitivity to stimuli via hippocampal plasticity. It has been proposed that this mechanism strengthens information processing and contributes to the generation of inappropriate associations and psychotic memory constructions.86 Negative psychotic symptoms, including anhedonia and apathy, have been associated with volume reductions in the C4/dentate gyrus in clinical studies.68,73 An animal study of MDD proposed that reduced expression of brain-derived neurotrophic factor in the dentate gyrus reduces neurogenesis and affects behaviour associated with depression.87 The CA4/dentate gyrus has also been found to be vulnerable to childhood trauma and stress,88 which are risk factors for MDD. Furthermore, some molecular alterations in the CA4 have been reported in patients with schizophrenia and patients with MDD. These involved fibroblast growth factor receptor mRNA and glutamic acid decarboxylase mRNA,89,90 which are related to normal hippocampal synaptology, signal transmission, plasticity and circuitry. Therefore, the overlap in CA4/dentate gyrus volume deficits may be considered a shared neurobiological feature that underlies the 2 disorders. It is of note that the volumetric reductions in the CA4 or CA4/dentate gyrus mentioned above were reported across the entire hippocampus.
Limitations
Our study had several limitations that need to be considered. Previous medication exposure and substance use might have influenced our findings. For example, postmortem evidence has suggested an association between antidepressant treatment and a larger dentate gyrus in patients with MDD.91 Short-term antipsychotic treatment may reduce the volumes of previously enlarged subfields in antipsychotic-naive patients with first-episode schizophrenia.55 Inversely, long-term use of certain antipsychotics may protect hippocampal substructures in patients with schizophrenia.66 However, limited information in the primary literature makes it difficult to control for these confounders.
We performed cross-sectional comparisons only in subfield volumes. Longitudinal research from the early course of illness is needed to understand developmental trajectories and potential differences in hippocampal subfield volumes between schizophrenia and MDD.
Study heterogeneity was more noteworthy in the direct comparison of patients with MDD and healthy controls. Because heterogeneity in the results for the right parasubiculum was higher in the comparison of patients with MDD and healthy controls, the related results should be interpreted with caution. To control for heterogeneity, we used random-effects models in all analyses, and the source analysis highlighted age, illness duration and symptom severity as potential contributors to heterogeneity. Another contributor could be insufficient disclosure of some subfield features in the primary literature.
Limited by inconsistent volumetry and uneven reports of hippocampal subfields in the original studies, our statistical power to detect group differences was lower in some subfields.
We did not control for the confounding effects of ICV in the network meta-analysis. Only 7 of the 15 studies reported ICV, and the results obtained from the 7 studies were slightly different from those obtained from the 15 studies. Such insufficient stability may have been because of the relatively small sample size of 7 studies, the confounding effects of ICV or both. The results of direct comparisons between patients with schizophrenia and patients with MDD after controlling for ICV should be interpreted with caution because of the demographic differences between patients.
Hippocampal subfields might not be uniformly affected along the longitudinal axis (i.e., head, body and tail in sequence) in psychotic disorders.92 However, few studies have investigated such detailed anatomy, so it was not feasible to distinguish more subtle alterations within each subfield.
Finally, the automatic segmentation algorithm of Iglesias and colleagues15 is based on previous and visible features, possibly ignoring individual variations in hippocampal subfield anatomy.93 The developers of this algorithm acknowledged that volumes of internal subfields, such as the CA4, the granule cell layer of the dentate gyrus and the molecular layer, must be interpreted with caution (surfer.nmr.mgh.harvard.edu/fswiki/HippocampalSubfields).
Conclusion
Patients with schizophrenia and patients with MDD had overlapping and distinct volume abnormalities in hippocampal subfields. The 2 disorders showed a common lower volume in the left CA4. Inter-disorder differences included greater volume reductions in the bilateral parasubiculum and right HATA in patients with schizophrenia compared to patients with MDD. This combination of similarities and differences may help us to better understand the pathophysiology of both disorders.
Supplementary Material
Footnotes
Competing interests: J. Sweeney consults with VeraSci. No other competing interests were declared.
Contributors: Y. Sun, N. Hu, J. Sweeney, Q. Gong, C. Qiu and S. Lui designed the study. Y. Sun acquired the data, which Y. Sun, N. Hu, M. Wang, L. Lu, C. Luo, B. Tang and C. Yao analyzed. Y. Sun and N. Hu wrote the article, which M. Wang, L. Lu, C. Luo, B. Tang, C. Yao, J. Sweeney, Q. Gong, C. Qiu and S. Lui reviewed. All authors approved the final version to be published, agree to be accountable for all aspects of the work and can certify that no other individuals not listed as authors have made substantial contributions to the paper. See: https://creativecommons.org/licenses/by-nc-nd/4.0/
Funding: This study was supported by the National Natural Science Foundation of China (82102000, 82120108014, 82071908 and 81621003), the Sichuan Science and Technology Program (2022NSFSC1496 and 2021JDTD0002), the National Key R&D Program of China (2022YFC2009901 and 2022YFC2009900), the CAMS Innovation Fund for Medical Sciences (2021-I2M-C&T-A-022) and the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYYC08001 and ZYJC18020). Dr. Su Lui acknowledges support from the Humboldt Foundation Friedrich Wilhelm Bessel Research Award and Chang Jiang Scholars (T2019069). J. Sweeney acknowledges support from the University of Cincinnati Schizophrenia Research Fund.
References
- 1.Gilman SE, Hornig M, Ghassabian A, et al. Socioeconomic disadvantage, gestational immune activity, and neurodevelopment in early childhood. Proc Natl Acad Sci U S A 2017;114:6728–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet 2014;384:1800–19. [DOI] [PubMed] [Google Scholar]
- 3.Wray NR, Ripke S, Mattheisen M, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet 2018;50:668–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Upthegrove R, Birchwood M, Ross K, et al. The evolution of depression and suicidality in first episode psychosis. Acta Psychiatr Scand 2010;122:211–8. [DOI] [PubMed] [Google Scholar]
- 5.Wigman JT, van Nierop M, Vollebergh WA, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity — implications for diagnosis and ultra-high risk research. Schizophr Bull 2012; 38:247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iancu I, Bodner E, Roitman S, et al. Impulsivity, aggression and suicide risk among male schizophrenia patients. Psychopathology 2010;43:223–9. [DOI] [PubMed] [Google Scholar]
- 7.Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci 2012;35:68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubin LH, Carter CS, Drogos L, et al. Peripheral oxytocin is associated with reduced symptom severity in schizophrenia. Schizophr Res 2010;124:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scantamburlo G, Hansenne M, Fuchs S, et al. Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology 2007;32:407–10. [DOI] [PubMed] [Google Scholar]
- 10.Lee SH, Ripke S, Neale BM, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet 2013;45:984–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang M, Womer FY, Edmiston EK, et al. Neurobiological commonalities and distinctions among three major psychiatric diagnostic categories: a structural MRI study. Schizophr Bull 2018;44:65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmaal L, Veltman DJ, van Erp TG, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. Mol Psychiatry 2016;21:806–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu N, Luo C, Zhang W, et al. Hippocampal subfield alterations in schizophrenia: a selective review of structural MRI studies. Biomarkers Neuropsychiatry 2020;3:100026. [Google Scholar]
- 14.Duvernoy HM, Cattin F, Risold P-Y. The human hippocampus: functional anatomy, vascularization and serial sections with MRI. 4th ed. Berlin: Springer; 2013. [Google Scholar]
- 15.Iglesias JE, Augustinack JC, Nguyen K, et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: application to adaptive segmentation of in vivo MRI. Neuroimage 2015;115:117–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho NF, Iglesias JE, Sum MY, et al. Progression from selective to general involvement of hippocampal subfields in schizophrenia. Mol Psychiatry 2017;22:142–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cover KS, van Schijndel RA, Bosco P, et al. Can measuring hippocampal atrophy with a fully automatic method be substantially less noisy than manual segmentation over both 1 and 3 years? Psychiatry Res Neuroimaging 2018;280:39–47. [DOI] [PubMed] [Google Scholar]
- 18.Arnold SJ, Ivleva EI, Gopal TA, et al. Hippocampal volume is reduced in schizophrenia and schizoaffective disorder but not in psychotic bipolar I disorder demonstrated by both manual tracing and automated parcellation (FreeSurfer). Schizophr Bull 2015;41: 233–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McHugo M, Armstrong K, Roeske MJ, et al. Hippocampal volume in early psychosis: a 2-year longitudinal study. Transl Psychiatry 2020;10:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maller JJ, Broadhouse K, Rush AJ, et al. Increased hippocampal tail volume predicts depression status and remission to antidepressant medications in major depression. Mol Psychiatry 2018;23:1737–44. [DOI] [PubMed] [Google Scholar]
- 21.Han KM, Kim A, Kang W, et al. Hippocampal subfield volumes in major depressive disorder and bipolar disorder. Eur Psychiatry 2019; 57:70–7. [DOI] [PubMed] [Google Scholar]
- 22.Malykhin NV, Coupland NJ. Hippocampal neuroplasticity in major depressive disorder. Neuroscience 2015;309:200–13. [DOI] [PubMed] [Google Scholar]
- 23.Ota M, Sato N, Hidese S, et al. Structural differences in hippocampal subfields among schizophrenia patients, major depressive disorder patients, and healthy subjects. Psychiatry Res Neuroimaging 2017;259:54–9. [DOI] [PubMed] [Google Scholar]
- 24.Maller JJ, Daskalakis ZJ, Thomson RH, et al. Hippocampal volumetrics in treatment-resistant depression and schizophrenia: the devil’s in de-tail. Hippocampus 2012;22:9–16. [DOI] [PubMed] [Google Scholar]
- 25.Dias S, Caldwell DM. Network meta-analysis explained. Arch Dis Child Fetal Neonatal Ed 2019;104:F8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med 2017;12:103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG.Quantifying heterogeneity in a metaanalysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- 29.He Y, Zhong J, Zhou W, et al. Four surgical strategies for the treatment of cesarean scar defect: a systematic review and network meta-analysis. J Minim Invasive Gynecol 2020;27:593–602. [DOI] [PubMed] [Google Scholar]
- 30.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao B, Passos IC, Mwangi B, et al. Hippocampal subfield volumes in mood disorders. Mol Psychiatry 2017;22:1352–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doolin K, Allers KA, Pleiner S, et al. Altered tryptophan catabolite concentrations in major depressive disorder and associated changes in hippocampal subfield volumes. Psychoneuroendocrinology 2018;95:8–17. [DOI] [PubMed] [Google Scholar]
- 33.du Plessis S, Scheffler F, Luckhoff H, et al. Childhood trauma and hippocampal subfield volumes in first-episode schizophrenia and healthy controls. Schizophr Res 2020;215:308–13. [DOI] [PubMed] [Google Scholar]
- 34.Na KS, Won E, Kang J, et al. Interaction effects of oxytocin receptor gene polymorphism and depression on hippocampal volume. Psychiatry Res Neuroimaging 2018;282:18–23. [DOI] [PubMed] [Google Scholar]
- 35.Nakahara S, Turner JA, Calhoun VD, et al. Dentate gyrus volume deficit in schizophrenia. Psychol Med 2020;50:1267–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ohi K, Nemoto K, Kataoka Y, et al. Alterations in hippocampal subfield volumes among schizophrenia patients, their first-degree relatives and healthy subjects. Prog Neuropsychopharmacol Biol Psychiatry 2021;110:110291. [DOI] [PubMed] [Google Scholar]
- 37.Sasabayashi D, Yoshimura R, Takahashi T, et al. Reduced hippocampal subfield volume in schizophrenia and clinical high-risk state for psychosis. Front Psychiatry 2021;12:642048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiu MH, Lang X, Chen DC, et al. Cognitive deficits and clinical symptoms with hippocampal subfields in first-episode and never-treated patients with schizophrenia. Cerebral Cortex 2021;31:89–96. [DOI] [PubMed] [Google Scholar]
- 39.Xu J, Tang Y, Cecilio Baro C, et al. Left fimbria atrophy is associated with hippocampal metabolism in female major depressive disorder patients. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. 2018 July 18–21; Honolulu (HI). New York: IEEE; 2018:1136–9. [DOI] [PubMed] [Google Scholar]
- 40.Yuan M, Rubin-Falcone H, Lin X, et al. Smaller left hippocampal subfield CA1 volume is associated with reported childhood physical and/or sexual abuse in major depression: a pilot study. J Affect Disord 2020;272:348–54. [DOI] [PubMed] [Google Scholar]
- 41.Zheng F, Li C, Zhang D, et al. Study on the sub-regions volume of hippocampus and amygdala in schizophrenia. Quant Imaging Med Surg 2019;9:1025–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alnæs D, Kaufmann T, Van Der Meer D, et al. Brain heterogeneity in schizophrenia and its association with polygenic risk. JAMA Psychiatry 2019;76:739–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown SSG, Rutland JW, Verma G, et al. Structural MRI at 7T reveals amygdala nuclei and hippocampal subfield volumetric association with major depressive disorder symptom severity. Sci Rep 2019;9:10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cao B, Luo Q, Fu Y, et al. Predicting individual responses to the electroconvulsive therapy with hippocampal subfield volumes in major depression disorder. Sci Rep 2018;8:5434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frodl T, Carballedo A, Frey EM, et al. Expression of glucocorticoid inducible genes is associated with reductions in cornu ammonis and dentate gyrus volumes in patients with major depressive disorder. Dev Psychopathol 2014;26:1209–17. [DOI] [PubMed] [Google Scholar]
- 46.Frodl T, Skokauskas N, Frey EM, et al. BDNF Val66Met genotype interacts with childhood adversity and influences the formation of hippocampal subfields. Hum Brain Mapp 2014;35:5776–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han KM, Won E, Kang J, et al. TESC gene-regulating genetic variant (rs7294919) affects hippocampal subfield volumes and parahippocampal cingulum white matter integrity in major depressive disorder. J Psychiatr Res 2017;93:20–9. [DOI] [PubMed] [Google Scholar]
- 48.Han KM, Won E, Sim Y, et al. Hippocampal subfield analysis in medication-naïve female patients with major depressive disorder. J Affect Disord 2016;194:21–9. [DOI] [PubMed] [Google Scholar]
- 49.Harel EV, Tennyson RL, Fava M, et al. Linking major depression and the neural substrates of associative processing. Cogn Affect Behav Neurosci 2016;16:1017–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu X, Zhang L, Hu X, et al. Abnormal hippocampal subfields may be potential predictors of worse early response to antidepressant treatment in drug-naïve patients with major depressive disorder. J Magn Reson Imaging 2019;49:1760–8. [DOI] [PubMed] [Google Scholar]
- 51.Hýža M, Kuhn M, Cešková E, et al. Hippocampal volume in first-episode schizophrenia and longitudinal course of the illness. World J Biol Psychiatry 2016;17:429–38. [DOI] [PubMed] [Google Scholar]
- 52.Jiang Y, Xu L, Li X, et al. Common increased hippocampal volume but specific changes in functional connectivity in schizophrenia patients in remission and non-remission following electroconvulsive therapy: a preliminary study. Neuroimage Clin 2019;24:102081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kakeda S, Watanabe K, Katsuki A, et al. Relationship between interleukin (IL)-6 and brain morphology in drug-naïve, first-episode major depressive disorder using surface-based morphometry. Sci Rep 2018;8:10054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kraus C, Seiger R, Pfabigan DM, et al. Hippocampal subfields in acute and remitted depression-an ultra-high field magnetic resonance imaging study. Int J Neuropsychopharmacol 2019;22:513–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li W, Li K, Guan P, et al. Volume alteration of hippocampal subfields in first-episode antipsychotic-naïve schizophrenia patients before and after acute antipsychotic treatment. Neuroimage Clin 2018;20: 169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mikolas P, Tozzi L, Doolin K, et al. Effects of early life adversity and FKBP5 genotype on hippocampal subfields volume in major depression. J Affect Disord 2019;252:152–9. [DOI] [PubMed] [Google Scholar]
- 57.Na KS, Chang HS, Won E, et al. Association between glucocorticoid receptor methylation and hippocampal subfields in major depressive disorder. PLoS One 2014;9:e85425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nguyen L, Kakeda S, Katsuki A, et al. Relationship between VEGF-related gene polymorphisms and brain morphology in treatment-naïve patients with first-episode major depressive disorder. Eur Arch Psychiatry Clin Neurosci 2019;269:785–94. [DOI] [PubMed] [Google Scholar]
- 59.Orfei MD, Piras F, Banaj N, et al. Unrealistic self-overconfidence in schizophrenia is associated with left presubiculum atrophy and impaired episodic memory. Cortex 2017;86:132–9. [DOI] [PubMed] [Google Scholar]
- 60.Otsuka Y, Kakeda S, Sugimoto K, et al. COMT polymorphism regulates the hippocampal subfield volumes in first-episode, drug-naive patients with major depressive disorder. Neuropsychiatr Dis Treat 2019;15:1537–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tesli N, van der Meer D, Rokicki J, et al. Hippocampal subfield and amygdala nuclei volumes in schizophrenia patients with a history of violence. Eur Arch Psychiatry Clin Neurosci 2020;270:771–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Travis S, Coupland NJ, Silversone PH, et al. Dentate gyrus volume and memory performance in major depressive disorder. J Affect Disord 2015;172:159–64. [DOI] [PubMed] [Google Scholar]
- 63.Travis SG, Coupland NJ, Hegadoren K, et al. Effects of cortisol on hippocampal subfields volumes and memory performance in healthy control subjects and patients with major depressive disorder. J Affect Disord 2016;201:34–41. [DOI] [PubMed] [Google Scholar]
- 64.Vargas T, Dean DJ, Osborne KJ, et al. Hippocampal subregions across the psychosis spectrum. Schizophr Bull 2018;44:1091–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhou YL, Wu FC, Liu WJ, et al. Volumetric changes in subcortical structures following repeated ketamine treatment in patients with major depressive disorder: a longitudinal analysis. Transl Psychiatry 2020;10:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hu N, Sun H, Fu G, et al. Anatomic abnormalities of hippocampal subfields in never-treated and antipsychotic-treated patients with long-term schizophrenia. Eur Neuropsychopharmacol 2020;35: 39–48. [DOI] [PubMed] [Google Scholar]
- 67.Huang Y, Coupland NJ, Lebel RM, et al. Structural changes in hippocampal subfields in major depressive disorder: a high-field magnetic resonance imaging study. Biol Psychiatry 2013;74:62–8. [DOI] [PubMed] [Google Scholar]
- 68.Kawano M, Sawada K, Shimodera S, et al. Hippocampal subfield volumes in first episode and chronic schizophrenia. PLoS One 2015;10:e0117785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mathew I, Gardin TM, Tandon N, et al. Medial temporal lobe structures and hippocampal subfields in psychotic disorders: findings from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. JAMA Psychiatry 2014;71:769–77. [DOI] [PubMed] [Google Scholar]
- 70.Roddy DW, Farrell C, Doolin K, et al. The hippocampus in depression: more than the sum of its parts? Advanced hippocampal substructure segmentation in depression. Biol Psychiatry 2019;85:487–97. [DOI] [PubMed] [Google Scholar]
- 71.Tannous J, Godlewska BR, Tirumalaraju V, et al. Stress, inflammation and hippocampal subfields in depression: a 7 Tesla MRI Study. Transl Psychiatry 2020;10:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van Leemput K, Bakkour A, Benner T, et al. Automated segmentation of hippocampal subfields from ultra-high resolution in vivo MRI. Hippocampus 2009;19:549–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haukvik UK, Westlye LT, Mørch-Johnsen L, et al. In vivo hippocampal subfield volumes in schizophrenia and bipolar disorder. Biol Psychiatry 2015;77:581–8. [DOI] [PubMed] [Google Scholar]
- 74.Haukvik UK, Tamnes CK, Söderman E, et al. Neuroimaging hippocampal subfields in schizophrenia and bipolar disorder: a systematic review and meta-analysis. J Psychiatr Res 2018;104:217–26. [DOI] [PubMed] [Google Scholar]
- 75.Yushkevich PA, Wang H, Pluta J, et al. Nearly automatic segmentation of hippocampal subfields in in vivo focal T2-weighted MRI. Neuroimage 2010;53:1208–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roeske MJ, Konradi C, Heckers S, et al. Hippocampal volume and hippocampal neuron density, number and size in schizophrenia: a systematic review and meta-analysis of postmortem studies. Mol Psychiatry 2021;26:3524–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tang Q, Burgalossi A, Ebbesen CL, et al. Functional architecture of the rat parasubiculum. J Neurosci 2016;36:2289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bazin N, Brunet-Gouet E, Bourdet C, et al. Quantitative assessment of attribution of intentions to others in schizophrenia using an ecological video-based task: a comparison with manic and depressed patients. Psychiatry Res 2009;167:28–35. [DOI] [PubMed] [Google Scholar]
- 79.Wang AY, Lohmann KM, Yang CK, et al. Bipolar disorder type 1 and schizophrenia are accompanied by decreased density of parvalbumin-and somatostatin-positive interneurons in the parahippocampal region. Acta Neuropathol 2011;122:615–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weiss AP, Goff D, Schacter DL, et al. Fronto-hippocampal function during temporal context monitoring in schizophrenia. Biol Psychiatry 2006;60:1268–77. [DOI] [PubMed] [Google Scholar]
- 81.Fudge JL, deCampo DM, Becoats KT. Revisiting the hippocampalamygdala pathway in primates: association with immature-appearing neurons. Neuroscience 2012;212:104–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maren S, Phan KL, Liberzon I. The contextual brain: implications for fear conditioning, extinction and psychopathology. Nat Rev Neurosci 2013;14:417–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tani H, Tada M, Maeda T, et al. Comparison of emotional processing assessed with fear conditioning by interpersonal conflicts in patients with depression and schizophrenia. Psychiatry Clin Neurosci 2019;73:116–25. [DOI] [PubMed] [Google Scholar]
- 84.Tamminga CA, Southcott S, Sacco C, et al. Glutamate dysfunction in hippocampus: relevance of dentate gyrus and CA3 signaling. Schizophr Bull 2012;38:927–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tamminga CA, Zukin RS. Schizophrenia: evidence implicating hippocampal GluN2B protein and REST epigenetics in psychosis pathophysiology. Neuroscience 2015;309:233–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tamminga CA, Stan AD, Wagner AD. The hippocampal formation in schizophrenia. Am J Psychiatry 2010;167:1178–93. [DOI] [PubMed] [Google Scholar]
- 87.Taliaz D, Stall N, Dar DE, et al. Knockdown of brain-derived neurotrophic factor in specific brain sites precipitates behaviors associated with depression and reduces neurogenesis. Mol Psychiatry 2010;15: 80–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Teicher MH, Anderson CM, Polcari A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc Natl Acad Sci U S A 2012;109:E563–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gaughran F, Payne J, Sedgwick PM, et al. Hippocampal FGF-2 and FGFR1 mRNA expression in major depression, schizophrenia and bipolar disorder. Brain Res Bull 2006;70:221–7. [DOI] [PubMed] [Google Scholar]
- 90.Thompson Ray M, Weickert CS, Wyatt E, et al. Decreased BDNF, trkB-TK+ and GAD67 mRNA expression in the hippocampus of individuals with schizophrenia and mood disorders. J Psychiatry Neurosci 2011;36:195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Boldrini M, Santiago AN, Hen R, et al. Hippocampal granule neuron number and dentate gyrus volume in antidepressant-treated and untreated major depression. Neuropsychopharmacology 2013;38:1068–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McHugo M, Talati P, Woodward ND, et al. Regionally specific volume deficits along the hippocampal long axis in early and chronic psychosis. Neuroimage Clin 2018;20:1106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wisse LEM, Chételat G, Daugherty AM, et al. Hippocampal subfield volumetry from structural isotropic 1 mm3 MRI scans: a note of caution. Hum Brain Mapp 2021;42:539–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.