Abstract
Purpose:
The purpose of this pilot study was to determine the effectiveness and acceptability of an initial module (1.1; active listening skills) of the Simulated Training in Evidence-Based Practice for Stuttering (STEPS) program, a theory-driven, multimodule, content and learning platform designed to advance knowledge and skills in working with culturally and linguistically diverse persons who stutter of all ages.
Method:
Fifteen preservice speech-language pathologists (SLPs) were randomly assigned to complete either the STEPS 1.1 module or a control module. In both conditions, all participants engaged in pre– and post–clinical interviews with a standardized patient portraying a parent of a child who stutters. Prior to participation, all participants provided self-ratings on the Jefferson Scale of Physician Empathy–Health Profession Student. Post participation, trained observers rated all participants' active listening behaviors using the Active Listening Observation Scale–Modified. Post participation, the STEPS 1.1 participants also completed an intervention acceptability questionnaire.
Results:
No differences between groups were found in self-perceived clinical empathy prior to participation. Participants who completed the STEPS 1.1 condition utilized paraphrasing and client-directed eye gaze significantly more frequently at posttest than at pretest and significantly more than the control group at posttest. Quantitative and qualitative responses from the participants who completed STEPS 1.1 indicated high acceptability of its content, structure, duration, and perceived impact.
Conclusion:
Preliminary data from the present pilot study support use of the STEPS 1.1 module to improve preservice SLPs' use of skills that have been shown to predict perceived clinical empathy and increase assessment and treatment effectiveness.
Over the past 3 decades, clinicians have consistently reported a lack of comfort and competence when assessing and treating clients who stutter (Brisk et al., 1997; Cooper & Cooper, 1985, 1996; Gabel, 2014; Kelly et al., 1997, 2020; Klassen & Kroll, 2005; Mallard et al., 1988; St. Louis & Durrenberger, 1993; cf. Crichton-Smith et al., 2003). Several reasons have been offered for the lack of clinician competency in working with persons who stutter, including the overall complexity or long-term nature of the disorder (Cooper & Cooper, 1996; Murphy & Quesal, 2004) and general negative attitudes and stereotypes toward stuttering by speech-language pathologists (SLPs; Brisk et al., 1997). However, the most frequently cited reasons for limited knowledge about stuttering include self-assessed shortages of fluency disorder–based counseling curricula during academic training, limited availability of fluency clients, and decreased emphasis on fluency disorders and counseling skills within clinical practicum (e.g., Coalson et al., 2016; Kelly et al., 1997, 2020; Klassen & Kroll, 2005; Yaruss & Quesal, 2002). This study piloted the effectiveness of the initial module (1.1) of the Simulated Training in Evidence-Based Practice for Stuttering (STEPS) program, an accessible, theory-driven resource designed to improve clinical competency among students and practicing SLPs working with persons who stutter and their families and to enhance client care. Specifically, this study investigated the use of STEPS 1.1 to improve active listening skills among preservice SLPs.
Clinical Training in Stuttering
Individuals who stutter and parents of children who stutter consistently rate clinician competence as a critical element in successful therapy (e.g., Plexico et al., 2010; Yaruss et al., 2002). Despite the increasing number of students entering speech-language pathology over the past decade (American Speech-Language-Hearing Association [ASHA], 2015), a poll by the National Stuttering Association (2009) suggests that clients who stutter continue to be dissatisfied with the services of clinicians who provide treatment for fluency disorders, a finding that mirrors published research (e.g., Yaruss et al., 2002). Client frustration with services is not surprising given that a high percentage of SLPs report insufficient academic or clinical preparation as students (Gabel, 2014). Unfortunately, the quantity and quality of preprofessional training in fluency disorders has been a continued area of concern within the field (e.g., Lee, 2014; Yaruss, 1999; Yaruss & Quesal, 2002). The majority of SLPs report no exposure to fluency clients (e.g., 13%: Gabel, 2014; 43%: Kelly et al., 1997) during graduate or undergraduate training. Access to clinical opportunities is insufficient and may contribute, in part, to limited pursuit of postgraduate specialization in fluency disorders (Coalson et al., 2016; Gabel, 2014; McClure & Olsen, 2010).
In fact, the number of professionals who self-report being competent to treat clients with fluency disorders remains insufficient relative to the size and needs of the clinical population. Among the 153,000+ practicing SLPs in the United States, less than 1% report feeling competent to provide services to the nearly 18 million individuals who stutter, yet 80% (Kelly et al., 2020) to more than 97% (Coalson et al., 2016) of clinicians report having clients who stutter on their caseloads. Additionally, within the field of speech-language pathology, receipt of ASHA's Certificate of Clinical Competence is dependent on the student clinician's understanding of and ability to provide evidence-based practice across client populations. SLPs are also expected to demonstrate counseling competencies to address thoughts, feelings, and life impact associated with communication disorders (ASHA, 2016).
The Role of Counseling in Clinical Practice With Those Who Stutter
Researchers across health care professions (e.g., speech-language pathology, medicine, nursing, dentistry, and pharmacy) have demonstrated that patients, regardless of diagnosis, race, ethnicity, gender, or socioeconomic status, prefer clinicians who are competent in counseling (K. Beck & Kulzer, 2018; Horvath et al., 2011; Lieberman, 2018; Luterman, 2020, 2021). Active listening, one of the most fundamental and trainable counseling skills, is characterized by verbal and nonverbal indicators that the clinician is attending to and listening to the client (K. Beck & Kulzer, 2018; Ivey et al., 1968; Kuntze et al., 2009; Pehrson et al., 2016; Shipley, 1997) and is highly relevant when working with persons who stutter and their parents. Children who stutter as young as 2 years of age report negative communication attitudes, and the emotional consequences of stuttering often intensify with experiences of bullying, discrimination, social rejection, and stigmatization (Blood & Blood, 2016; Boey et al., 2009; Guttormsen et al., 2015; Weidner et al., 2018). Parents of children who stutter report feeling helpless, ashamed, and/or guilty about their children's stuttering, which ultimately influences pediatric treatment outcomes, as well as their own and their children's quality of life (Berquez & Kelman, 2018; Humeniuk & Tarkowski, 2016; Langevin et al., 2010; Nonis et al., 2021; Plexico & Burrus, 2012). These complex emotional reactions to stuttering and their impact on quality-of-life outcomes warrant the use of active listening skills, which have been shown to increase client satisfaction, trust, treatment adherence, perceived clinical empathy, and positive treatment outcomes across a variety of populations (Brugel et al., 2015; Jagosh et al., 2011; Kraft-Todd et al., 2017; Luterman, 2021; Thistle & McNaughton, 2015), including parents of children who stutter (Berquez et al., 2015; Berquez & Kelman, 2018; Croft et al., 2022).
Given the value of utilizing active listening and other counseling skills with persons who stutter and their families, there is a need for both explicit and experiential instruction related to these skills at the undergraduate and graduate training levels (Lieberman, 2018; Luterman, 2020, 2021). In a recent survey examining counseling curricula among accredited communication sciences and disorders graduate programs (Doud et al., 2020), only 40% of programs offered a stand-alone counseling course, signaling a decrease from a previous systematic review investigating counseling curricula among accredited programs (McCarthy et al., 1986). In another survey, 80% of participants (i.e., clinical fellows) reported that their graduate program did not offer a counseling course and that they did not feel comfortable providing clinical counseling (Phillips & Mendel, 2008). However, significant correlations between hours of weekly counseling experience, self-reported comfort with, and self-reported preparedness for counseling were observed, suggesting that opportunities to counsel clients and families may increase comfort and competence. This finding was reinforced by A. R. Beck and Verticchio (2014), who found that 55% of preservice SLPs and 67% of preservice audiologists reported that their lack of counseling competence was due to inexperience. Studies also suggest that self-reported empathy is strongly associated with counseling competence and may facilitate the clinician's interest in and attunement to client needs (Haley et al., 2017; Kelley & Kelley, 2013). Specifically, clinicians with greater empathy may demonstrate an increased use of active listening skills, such as verbally restating client concerns, engaging in client-directed eye gaze, or asking follow-up questions (Haley et al., 2017; Jones & Huggins, 2014).
Previous researchers investigating the effectiveness of counseling intervention on self-reported and observed counseling competence suggested fundamental counseling skills, including active listening, are trainable (e.g., Kaderavek et al., 2004; Thistle & McNaughton, 2015). However, these interventions were conducted over several in-person sessions and employed a variety of resources, such as lecturers and mock role players, which may not be accessible to or feasible for clinical training programs nationwide.
Given the few SLPs who self-report being prepared to serve persons who stutter, the need for experience to improve basic counseling skills, and the limited availability of specialists in fluency disorders postgraduation, the field of speech-language pathology would benefit from an accessible, parsimonious resource providing training in fundamental counseling skills to those who stutter and their families to positively impact professional preparation in the assessment and treatment of stuttering (Coalson et al., 2016; Gabel, 2014; Kelly et al., 2020; Yaruss et al., 2017).
STEPS
As a solution to improving clinical preparation and services for those who stutter, the first author of this study developed the STEPS program, a theory-driven, multimodule, content and learning platform designed to advance knowledge and skills in working with culturally and linguistically diverse persons who stutter of all ages. The STEPS program provides undergraduate and graduate students with an innovative, interactive opportunity to navigate 1,000+ authentic clinical videos of expert clinicians providing assessment and treatment practices to preschoolers, school-age children, older adolescents, and adults who stutter. Ultimately, professors will be able to use STEPS in the classroom as a tool to support translating theory into practice. Practicing SLPs will have the opportunity to expand their clinical skills in stuttering through STEPS. Persons who stutter and their families will also have access to STEPS to broaden their understanding of the nature and treatment of stuttering and to further establish a sense of community.
Both in its early stages and when fully developed, users, including students, SLPs, professors, and persons who stutter and their families, will be able to easily access STEPS on their personal computers or mobile devices to observe and analyze a wide range of clinical scenarios and make complex decisions in the absence of client risk. Users can also access a significant video library of personal journeys with stuttering, client testimonials about specific strategies (e.g., self-disclosure), and perspectives about stuttering by caregivers and family members. For example, through STEPS, users will be able to learn how to identify, discriminate, and analyze speech disfluencies, especially distinguishing stuttered from nonstuttered speech, and identify the prognostic markers that suggest natural recovery versus persistence of stuttering. STEPS also provides users with exposure to multiple complex case profiles that enhance learners' abilities to differentiate stuttering from other clinical fluency disorders (e.g., cluttering) or differences (e.g., increased disfluencies in learners of multiple languages; Byrd et al., 2015, 2020; Eggers et al., 2020). Of particular relevance to this study, the initial STEPS module (i.e., STEPS 1.1) trains users in best practices for active listening and counseling in stuttering assessment and treatment—skills that are critical to increasing client satisfaction, trust, treatment adherence, and clinical effectiveness across individuals with a variety of communication differences and disorders (Croft et al., 2022; Decety et al., 2014; Ebert & Kohnert, 2010; Elliott et al., 2018; Halpern, 2012; Hojat et al., 2011; Kim et al., 2004; Larson & Yao, 2005; Plexico et al., 2010).
Purpose of This Study
The purpose of the present pilot study was to evaluate the effectiveness of one module of STEPS (STEPS 1.1) for improving preservice SLPs' use of active listening skills. The following research questions were addressed:
Research Question 1: Does participation in STEPS 1.1 increase preservice SLPs use of active listening skills when conducting an initial interview with a standardized patient acting as the parent of a child who stutters?
Research Question 2: To what extent is the STEPS 1.1 intervention module acceptable to participants?
Method
Participant Eligibility and Recruitment
Eligible participants included undergraduate students majoring in speech-language pathology (freshman to senior) and leveling students (i.e., postbaccalaureate students completing prerequisite courses in preparation for graduate school) of at least 18 years of age. To prevent participant bias, students who had taken a course with or been supervised by one or more of the researchers of this study were not eligible to participate. Students also needed to be able to complete a survey remotely on the electronic device of their choice and attend a 90-min session (i.e., random assignment to STEPS 1.1 or control condition) at an on-campus clinical research facility. The researchers recruited participants by e-mailing academic advisors, faculty members, and doctoral students in the Department of Speech, Language, and Hearing Sciences, who forwarded the recruitment letter to eligible participants. The recruitment letter stated approval of the study by the university's institutional review board, identified participant eligibility requirements, and provided the researchers' contact information. All participants corresponded with the researchers via e-mail to complete the informed consent document and to schedule the in-person research session.
Experimental Procedure Overview
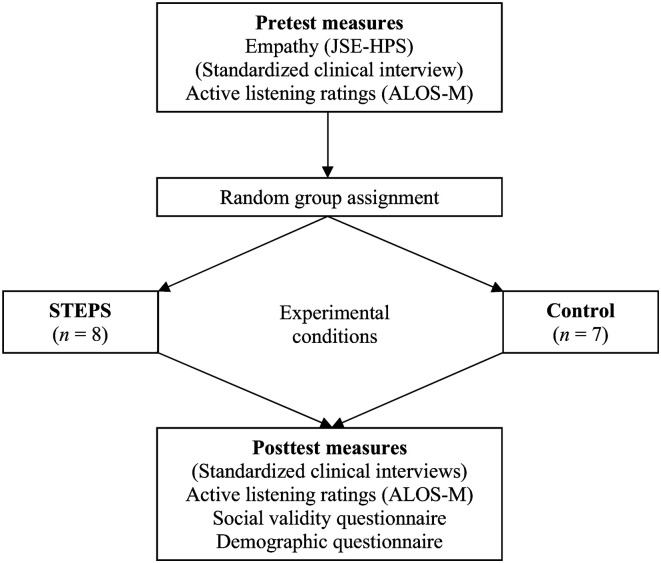
The experimental protocol was developed based on previous research studies implementing pre- and posttests of counseling competence following a training intervention (e.g., Kaderavek et al., 2004; Pehrson et al., 2016; Thistle & McNaughton, 2015). First, all participants completed an informed consent document and pretest measure of empathy (i.e., Jefferson Scale of Physician Empathy–Health Profession Student [JSPE-HPS]; Hojat et al., 2001; Fields et al., 2011) remotely on the electronic device of their choice (Quail et al., 2016). Within 1 week, participants completed a standardized clinical encounter (described in further detail in the next section) with a standardized patient actor portraying a parent of a child who stutters (standardized patient parent [SP Parent]). Participants' use of active listening skills (to be detailed below) during this interaction was video- and audio-recorded and analyzed later by trained coders using the Active Listening Observation Scale–Modified (ALOS-M; Bodie et al., 2014; G. Bodie, personal communication, September 11, 2020) as a measure of active listening skills. Participants were randomly assigned to either a STEPS 1.1 or control group. Following participation in either condition, participants completed a second, standardized clinical encounter as a measure of posttest active listening and provided additional demographic information. Participants in the STEPS 1.1 condition completed an intervention acceptability questionnaire. See Figure 1 for a visual overview of the experimental procedure. Each component of the procedure is described in greater depth in the following sections.
Figure 1.
Overview of the experimental procedure for N = 15 preservice speech-language pathology student participants. JSPE-HPS = Jefferson Scale of Physician Empathy–Health Profession Student; ALOS-M = Active Listening Observation Scale–Modified.
Confidentiality and Informed Consent
All participants received an arbitrary code (e.g., A2) to protect confidentiality throughout the study. Prior to completing any measures, participants read and signed the informed consent document remotely via Qualtrics. This document outlined the general purpose of the study, approval of the study from the university's institutional review board, known associated risks and benefits, the freedom to withdraw from the study at any time, and measures taken to protect the participants' identities and maintain confidentiality. Participants who indicated consent were given instructions for the next steps of the study.
Standardized Clinical Encounter
To provide a pre- and posttest behavioral measure of active listening skills, all participants engaged in two standardized clinical encounters with the SP Parents of a preschooler who stutters. When interacting with participants, both SP Parents were blinded as to whether the preservice SLP participant was in the STEPS 1.1 or control condition and whether the interaction was pre- or posttest. Additionally, participants' interactions with each SP Parent were counterbalanced across pre- and posttests to control for potential order effects. Thus, each student interacted with each SP Parent only once. This standardized clinical encounter was modeled after previous studies (e.g., Marion et al., 2018; Pehrson et al., 2016) and designed to reflect a portion of a typical initial evaluation session with a parent of a child who stutters. Specifically, participants were instructed to ask the SP Parent the following three questions: (a) What brings you here today? (b) What do you think caused your child's stuttering? (c) What, if anything, do you do when your child stutters? Participants could conclude the interaction after obtaining answers to these questions. These pre- and postclinical interactions were video- and audio-recorded for later analysis.
SP Parents
Standardized patients are commonly used with preservice clinicians to allow for student learning in the absence of client risk (K. Beck & Kulzer, 2018; Hill et al., 2010; Kaderavek et al., 2004; Penman et al., 2021; Quail et al., 2016). Moreover, student counseling performance across real and standardized patients has been shown to be comparable (K. Beck & Kulzer, 2018; Schwartz et al., 2015). The standardized patients in this study included two female actors who portrayed the role of a parent of a preschool-age child who stutters. Both actors had extensive experience performing as standardized patients. Each actor demonstrated typical speech and language skills, and appropriate vocal quality and resonance as judged by three certified SLPs who answered “yes” to binary yes/no questions regarding these qualities.
SP Parent Training
The SP Parent training process was modeled after the protocols from Baylor et al. (2017) and Hill et al. (2013). First, the SP Parents were provided with basic information about stuttering (e.g., https://www.asha.org/stuttering/), as well as written excerpts from peer-reviewed, scholarly articles detailing parents' reactions to children's stuttering and coping styles (e.g., Berquez & Kelman, 2018; Humeniuk & Tarkowski, 2016; Millard et al., 2018). Both SP Parents were then given a “profile” outlining their character's name, age, reason for seeking an evaluation for the child, the child's age, stuttering onset and communication attitudes, and scripted responses to learn (see SP Parent Script Development and Preparation below).
Prior to learning the scripts, the SP Parents viewed authentic clinical videos of parents of children who stutter and were provided with observations regarding parent behavior. In each video, an actual parent of a child who stutters was shown answering questions in a diagnostic interview. The researchers highlighted the parent's verbal and nonverbal behavior, such as response content, body position, facial expression, tone, and affect (Baylor et al., 2017). The videos were also used to highlight potential clinician behavior, such as follow-up questions, and parent reactions to clinician behavior (pausing thoughtfully after the clinician asks a question, reactions to clinician interruptions, etc.). Throughout this initial process, SP Parents were encouraged to take notes and share impressions regarding the apparent impact of stuttering on both the parent in the video and the parent's child, consistent with Baylor et al. (2017).
SP Parent Script Development and Preparation
The SP Parents were given a script that provided responses to the three interview questions (i.e., What brings you here today? What do you think caused your child's stuttering? What do you do when your child stutters?). These questions were selected due to their common use in stuttering evaluations and the emotional responses that these questions tend to evoke from parents and caregivers, as indicated by a video analysis of over 50 videos from initial interviews of parents of children who stutter at the first author's clinical research center. These same videos, as well as the first author's 20+ years of experience working with people who stutter and their families, were used to develop two written scripts (one for each SP Parent) to reflect common themes for each of the three questions (e.g., expressing feelings of worry, uncertainty, and guilt). To control for script content while reflecting authentic interview responses, both scripts contained the following components: (a) identification of parent's concern (i.e., child's stuttering), (b) description of child's negative reaction (e.g., frustration), (c) parental self-blame regarding the cause of stuttering, and (d) parental uncertainty regarding what to do. Additionally, the authors gave the SP Parents a list of recorded data so the researchers and SP Parents could review with appropriate responses.
Consistent with Baylor et al. (2017), the SP Parents practiced their script delivery while incorporating the nonverbal behaviors they observed in the training videos. The researchers provided feedback throughout the process regarding naturalness of delivery, affect, and script accuracy. For example, when one SP Parent appeared to be less concerned than the other SP Parent, she was advised to adopt a more concerned tone and to smile less. Each practice session was video- and audio-recorded so the researchers and SP Parents could review and discuss them together.
After this initial practice session, the SP Parents practiced for 1 week at home according to the parameters emphasized in the SP Parent training and which is routine practice for standardized patient preparation protocols, before returning for another in-person practice session. During this session, the SP Parents delivered their scripts five separate times with different communication partners including the second author (a certified SLP), a second SLP with over 5 years of clinical experience working with parents of children who stutter, and three undergraduate student clinicians who did not participate in the study but represented the target participant population. The second author, the additional SLP, and the undergraduate students were then asked whether the SP Parents delivered their responses in a natural-sounding tone (yes/no), appeared to be concerned about their child's stuttering (yes/no), and shared information one might expect a parent of a child who stutters to share during an initial assessment (yes/no). All five communication partners answered “yes” to 100% of these questions across encounters with the SP Parents. These video-recorded practice sessions were then shown to the first author with 20+ years of experience working with persons who stutter and their families, who also endorsed the SP Parents as accurate and believable (i.e., answering “yes” that the SP parent delivered their responses naturally, with a tone of concern, and with relevant content).
Experimental Conditions
STEPS 1.1
Preservice SLP participants in the experimental condition engaged in the STEPS 1.1 intervention module delivered in an online format. First, they were provided with basic information about stuttering (e.g., written descriptions of speech characteristics, prevalence, and potential psychosocial impact on children and parents), as well as video examples of different stuttering types and severities. Next, participants read about effective nonverbal and verbal active listening behaviors. These active listening behaviors reflected those of a Western cultural context (i.e., the cultural context in which the study was conducted). Effective nonverbal behaviors were described as subtle indicators that the clinician is attending to the client, such as engaging in client-directed eye gaze (i.e., looking at the client as they are talking), head nodding, not interrupting, and remaining silent for two full seconds after the client responds to allow for more processing or sharing. Effective verbal behaviors were described as verbally communicating messages back to the speaker to confirm that ideas were understood correctly, such as repeating or rephrasing the client's messages in a clear and succinct manner and/or with an emphasis on their feelings. These behaviors, also known in the counseling literature as counseling “microskills,” were selected due to their trainability in preservice health care professionals with little or no counseling experience (Chandrashekar et al., 2020; Fontaine et al., 2019; Ivey et al., 1968; Levitt, 2002) and their associations with increased client satisfaction and perceived clinician empathy (K. Beck & Kulzer, 2018; Bodie et al., 2012; Croft et al., 2022; Gold, 2018; Ivey et al., 1968; Thistle & McNaughton, 2015; Turnbull et al., 2010). These nonverbal and verbal behaviors parallel those on the ALOS-M used to assess participants' demonstration of active listening in this study (Bodie et al., 2014; Fassaert et al., 2007). The written descriptions of these behaviors were each followed with two video exemplars showing a clinician's effective use of both verbal and nonverbal behaviors. After watching each video exemplar, participants were provided with an explanation of why the clinician's behavior was effective.
The primary portion of STEPS 1.1 guides participants through a series of videos depicting authentic clinical interactions between clinicians and parents of children who stutter. Following the two initial video exemplars and accompanying explanation of the clinician's active listening behaviors, participants watched six videos ranging from 19 to 45 s each. Participants were prompted to watch each video at least twice, with a focus on the clinician's (a) nonverbal and (b) verbal active listening behaviors, respectively. The active listening skills that are assessed on the ALOS-M (i.e., open questions; paraphrasing/verbal reflections; reflection of feelings; check-outs; and other nonverbal indicators of acceptance, congruence empathy, and attendance including open body language, client-directed eye gaze, and back-channeling) were modeled in these training videos. For the STEPS 1.1 module, we targeted exposure to these core active listening skills by asking participants to assess the degree to which the preservice SLPs featured in the videos demonstrated three specific nonverbal behaviors (i.e., client-directed eye gaze, silence, and body orientation) and one specific verbal behavior (i.e., verbal reflections of content and/or feelings) on a Likert scale from 1 (completely disagree) to 7 (completely agree). These rating opportunities allowed participants to focus on global indicators of active listening. Participants completed these four ratings after watching each video and were provided with immediate feedback regarding their ratings, including provision of the authors' own expert ratings of each video, and qualitative rationale. Below is an example of a written explanation of an expert's rating of “1” for a clinician's verbal behavior (i.e., repeating or paraphrasing what the client said in a way that was succinct, concrete, and clear):
The clinician did not reflect or restate the parent's concerns. Instead, she went to the next question. She could improve by summarizing the parent's reason for bringing her son in for the evaluation before moving on. She could have restated the parent's response by saying something like: “Okay, thank you for sharing. If I understand correctly, your son has received speech therapy before, but it was not the best experience. I am so glad that you have come here. What are you hoping to gain from today's evaluation?” Feel free to watch the video again to observe these behaviors in action!
Regardless of whether the participants' ratings were correct or incorrect, they could watch each video as many times as they preferred and review the expert ratings and qualitative rationales. For each of the last two videos, participants were prompted to type in their own hypothetical verbal restatement to the client prior to seeing the answer key, which contained a written example of an acceptable verbal restatement. The answer key was provided immediately after participants submitted their hypothetical response. Participants could compare their written, hypothetical verbal response to that on the answer key to assess accuracy. Following completion of STEPS 1.1., each participant engaged in a second (posttraining) clinical interview with SP Parents.
Control condition
The control condition task was designed to promote a similar level of cognitive engagement as experienced by the STEPS 1.1 group and to take a similar amount of time (i.e., 45 min to 1 hr). Participants in this condition viewed informational videos about the university's speech, language, and hearing department and rated each video's effectiveness (e.g., “This video was informative regarding academic opportunities at [the university]”) using a 1 (completely disagree) to 7 (completely agree) Likert scale. Participants were also asked to share comments regarding why each video was effective or ineffective in providing information about the university's department. Following completion of the viewings and ratings, each participant from the control group engaged in a second (posttraining) clinical interview with SP Parents.
Piloting the Experimental Protocol
Prior to this study, the experimental protocols for the STEPS 1.1 and control conditions were piloted with six graduate students studying audiology to ensure smooth and feasible implementation, identify optimal camera angles for the standardized clinical interactions, and provide the SP Parents with an opportunity to engage in repeated encounters while maintaining fidelity to their roles. The piloting process demonstrated that the STEPS 1.1 and control interventions took a similar amount of time (i.e., 45 min to 1 hr)—two cameras were needed to capture both the SP Parent and the student's behavior—and confirmed other intervention logistics (e.g., allowing participants to adjust computer volume, asking participants to leave phones and backpacks in waiting room, etc.) were feasible and consistently implementable across participants.
Settings and Materials
When participating in their respective conditions (i.e., on the computer engaging in the STEPS 1.1 or control condition), participants were alone in an office within the clinical research center. During the study, participants only interacted with either the researcher or the SP Parents. All instructions were given individually to each participant in their designated office; therefore, participants were not in the presence of and did not talk with one another at any point before, during, or immediately after engaging in the experimental conditions. All offices contained an iMac desktop, keyboard, and mouse. Each iMac contained the Qualtrics link to the assigned online condition. When watching videos as part of the experimental conditions, participants were able and encouraged to control the computer volume independently. Given that participants were asked to leave their phones and backpacks in the lobby, no extraneous items, apart from a water bottle if desired, were present.
The standardized clinical encounter was conducted in the clinical research facility's therapy rooms, where evaluation and treatment sessions with people who stutter are typically held. Thus, the clinical interaction setting resembled an authentic clinical environment. Therapy rooms contained a table and chairs. Prior to engaging in the standardized clinical encounter, all participants were provided with a clipboard, pen, and piece of paper containing the interview questions. These materials are those typically used during a clinical assessment. All participants were video- and audio-recorded using a Cannon Vixia HFM500 with a Sennheiser AVS Wireless Lavalier microphone. Separate cameras were used to capture each participant from two angles: (a) a frontal view and (b) a profile view. The frontal angle was used to analyze each participant's verbal and nonverbal behavior, whereas the profile angle was used to analyze the SP Parent's behavior for the ongoing fidelity assessment. The authors viewed each video and determined whether the SP Parents delivered the script naturally (yes/no), with a tone of concern (yes/no), and according to how it was written (yes/no), confirming the presence of all three elements by SP Parents for every video. The SP Parents were observed to maintain accuracy in script content and delivery with no significant deviation over the course of the study.
Measures
Pretest measures included a quantitative measure of self-reported empathy by preservice SLPs and ratings by trained observers of the participants' active listening behaviors during the preexperimental standardized clinical encounter. Posttest measures included ratings, by trained observers, of participants' active listening behaviors during a second standardized clinical encounter. Participants in the STEPS 1.1 group also completed post-intervention demographic and acceptability questionnaires. Measures are described in more detail below.
Clinical Empathy
Given that self-reported empathy can influence use of active listening skills (Haley et al., 2017; Kelley & Kelley, 2013), and to control for this variable across the two participant groups, the JSPE-HPS, a 20-item scale designed to measure self-reported empathy in health care professional students, was used to examine participants' self-reported clinical empathy prior to participation in the study (Fields et al., 2011; Hojat et al., 2001). Responses are provided on a Likert scale from 1 (strongly disagree) to 7 (strongly agree). This measure was developed as an adaptation of the JSPE (Hojat et al., 2001), which measures physicians' and medical students' empathy, defined as an “uncritical understanding of the patient's experiences, emotions and feelings” (p. 355). In the adapted version for health care professions students, the word “physician” was replaced with “health care professional.” For the purposes of this study, the term speech-language pathologist (abbreviated as “SLP”) was used instead. The JSPE-HPS previously has been used to measure empathy among students in dentistry (Sherman & Cramer, 2005), nursing (Fields et al., 2004), and speech-language pathology (Quail et al., 2016). Across these studies, the measure has demonstrated adequate construct validity, internal consistency, and test–retest reliability. To calculate a total score, negatively worded items are reverse-scored before summing the item response scores. A higher total sum reflects higher levels of self-reported empathy. This measure was presented electronically via the Qualtrics platform.
Pre- and Posttest Ratings of Active Listening Skills
ALOS
The ALOS-M (Bodie et al., 2014; Fassaert et al., 2007) was used to measure preservice SLPs' active listening behaviors in the standardized clinical encounters before and after participation in the STEPS 1.1 or control condition. The ALOS-M was selected for use in this study because it includes all the basic active listening skills emphasized and modeled in the STEPS 1.1 intervention module and is recommended for use by active listening experts (G. Bodie, personal communication, September 11, 2020). Although many active listening or communication coding systems commonly used in research include more advanced counseling skills, such as making interpretations or providing information (e.g., Bylund & Makoul, 2005; Chamberlain & Ray, 1988), the ALOS-M emphasizes the fundamental active listening skills of primary interest in this study.
The ALOS-M, developed by Bodie et al. (2014), focuses on ratings of the participant's use of four specific active listening behaviors: (a) open questions (open-ended questions that encourage the client to continue talking), (b) paraphrasing (restating the client's message in the client's own words), (c) reflection of feelings (making statements that capture the overall feelings the client expressed), and (d) check-outs (short questions to assure accurate understanding of the client's responses; G. Bodie, personal communication, September 11, 2020). Additionally, raters provide a fifth global rating of the participant's use of nonverbal and verbal behaviors to communicate acceptance, congruence, and empathy, including assessment of the speaker's tone, attendance (e.g., open body language and client-directed eye gaze), and use of back-channeling (e.g., “Yeah” and “Uh huh”; G. Bodie, personal communication, September 11, 2020). As mentioned previously, these active listening skills were modeled in the STEPS 1.1 module.
When assessing participants for their use of active listening skills, raters (see section below) provided Likert scale scores from 0 (never) to 4 (always) for each of the five active listening items. In a previous study, this five-item active listening scale demonstrated high internal consistency and divergent validity, thus supporting its psychometric properties (Bodie et al., 2014). An additional adaptation expanded the length of the scale from five to 10 items to allow for ratings of the participant's active listening skills, on the same items, in both the first and second halves of the clinical interaction (G. Bodie, personal communication, September 11, 2020). This 10-item scale is referred to as the ALOS-M in this study. Quantitative ratings of the participants' use of open questions, paraphrasing, reflection of feelings, check-outs, global empathy, and overall active listening skills were calculated by averaging the scores from the first and second halves of the clinical interaction. Higher average ratings reflect more frequent use of active listening skills.
Client-directed eye gaze
The participants' use of client-directed eye gaze was defined by the amount of time the participant looked at the SP Parent while the SP Parent was talking (Brugel et al., 2015; Dijkstra et al., 2013). Consistent with previous studies investigating active listening skills among nurses (Caris-Verhallen et al., 1999, 2000) and pharmacy students (Thakur et al., 2019), client-directed eye gaze was calculated by dividing the number of seconds that the participant looked at the SP Parent's face by the duration of the total participant–SP Parent interaction (i.e., first word spoken to last word spoken). The final proportion was multiplied by 100 to obtain a percentage of time that the participant engaged in client-directed eye gaze. This percentage was calculated for participants' pre- and posttest SP Parent interactions.
ALOS-M and Client-Directed Eye Gaze Raters and Interrater Reliability
To ensure valid and reliable measurement of participants' pre- and posttest active listening skills, two raters, including the second author and a research assistant who was otherwise uninvolved and unfamiliar with the study's purpose, research questions, and experimental conditions (i.e., a neutral rater), completed the ALOS-M ratings and client-directed eye gaze calculations for this study. Two different neutral raters completed the ALOS-M ratings and the client-directed eye gaze calculations, respectively. Interrater reliability training and analyses were then conducted to ensure valid and reliable measurement of participants' pre- and posttest active listening skills.
For the ALOS-M ratings, the second author and neutral rater reviewed the ALOS-M coding manual (G. Bodie, personal communication, September 11, 2020) and completed three practice video ratings together. Per the manual, the coding process included the following core components: (a) noting the start and end times of the interaction, (b) determining the interaction midpoint, (c) rating the participant's active listening skills (i.e., use of open questions, paraphrasing, reflecting feelings, check-outs, demonstration of acceptance, empathy, and congruence) for the first half of the interaction, and (d) rating the participant's active listening skills for the second half of the interaction. Raters could view the video as many times as they needed to be satisfied with their ratings and were encouraged to use the coding sheet to take notes about the active listening behaviors they observed (e.g., providing time markers corresponding to use of paraphrasing, open questions, etc.).
Recall that participants were instructed to ask the standardized patient actor three open-ended questions typical of a diagnostic interview; thus, the raters did not code or include these questions as part of the participants' active listening behaviors. Rater discrepancies were addressed and resolved during this training period through discussion among the raters and by contacting the author of the manual for clarification (G. Bodie, personal communication, October 11, 2020). Eighty percent agreement among raters was achieved prior to discussions, and 100% agreement was achieved after discussion, at which point raters began viewing the experimental videos.
Modeled after the protocol from Byrd et al. (2021), videos were presented in a randomized order to the trained research assistant who was blinded as to whether the participant was in the STEPS 1.1 or control group and whether they were viewing the pre- or posttest interaction. Additionally, the pre- and posttest videos were counterbalanced across both the STEPS 1.1 and control groups such that 50% of participants' pretest and 50% of participants' posttest videos were rated first. Only one of each participant's videos was rated in the first 50% of videos viewed, ensuring that no participants' two videos were rated consecutively. Each of the two raters viewed and rated 100% of the videos over a period of 7 weeks. The raters maintained an interrater reliability of .924, as determined by Cohen's kappa for two raters, prior to resolving discrepancies. Discrepancies were resolved, and the raters achieved 100% agreement through discussion (i.e., at times, one of the raters chose to change their rating to align with that of the other rater, or if not, an average of both ratings was used) prior to analyzing the data.
For client-directed eye gaze, the second author and the neutral rater began by reviewing the client-directed eye gaze calculation procedure and completed three practice videos together. Next, the second author calculated client-directed eye gaze for 100% of the videos, and the research assistant, who was blind to the study's purpose, hypotheses, and experimental conditions, completed calculations for 50% of the videos. At least 80% agreement was maintained throughout the calculation process. Discrepancies in agreement regarding the percentage of client-directed eye gaze in each interaction were resolved by viewing the video together and coming to a mutual agreement prior to analyzing the data.
Intervention Acceptability
A social validity measure based on the Kirkpatrick model (Hutchinson, 1999) and adapted from Pehrson et al. (2016) and Thistle and McNaughton (2015) was used to determine participants' perceptions of the acceptability of STEPS 1.1 and satisfaction with the experience. Specifically, participants provided responses on a scale from 1 (extremely disagree) to 7 (extremely agree) for five statements asking about STEPS 1.1's effectiveness for increasing clinical confidence and competence, ease of use, enjoyment, and value (e.g., “Participating in STEPS 1.1 increased my confidence related to counseling individuals with communication disorders”). After rating each statement, participants could provide additional comments in a text box. Additionally, four open-ended questions asked participants what they liked about STEPS 1.1, what they disliked about STEPS 1.1, their perceptions of the duration of STEPS 1.1, and any additional comments related to their experience.
Demographic Questionnaire
All participants reported the following demographic information: age, gender, classification (freshman, sophomore, etc.), previous or current clinical experience or practicum with individuals with communication disorders, coursework related to stuttering and/or counseling, and previous interactions with persons who stutter. If participants indicated previous or current clinical practicum with any clinical population, they also were asked to indicate the number of months they were engaged in that experience.
Statistical Analyses
Data in this study did not meet assumptions of normality and homogeneity of variance needed for parametric statistics. Thus, nonparametric and descriptive statistics were used to analyze results. First, Mann–Whitney–Wilcoxon tests were conducted to ensure nonsignificant, between-groups differences in previous clinical experience and empathy, each of which has been shown to be positively associated with increased use of active listening skills (Haley et al., 2017; Yang et al., 2021). The Mann–Whitney–Wilcoxon test was also used to compare the STEPS 1.1 and control groups' use of active listening skills before and after intervention. The Wilcoxon signed-ranks test was used to identify within-group active listening differences following participation in either the STEPS 1.1 or control condition. We also reported medians, standard deviations, and ranges of participants' active listening scores using descriptive statistics, as well as results from the social validity measure.
Results
Participant Corpus
The participant corpus included 15 preservice SLPs, with eight participants in the STEPS 1.1 group and seven participants in the control group. All 15 participants completed the study in its entirety. These sample sizes resemble those from previous studies exploring the effectiveness and/or acceptability of pilot interventions (de Blok et al., 2006; DiIorio et al., 2003) including active listening interventions (e.g., Levitt, 2002; Newman et al., 2022) and other pilot interventions in the field of communication sciences and disorders (e.g., Nicholson et al., 2015; Pitt et al., 2017). Participants ranged from 18 to 31 years of age and reported a range of academic and clinical experiences. Groups did not significantly differ in months of previous clinical experience (p = .844) or empathy (p = .908), as measured using the JSPE-HPS. See Table 1 for additional data regarding participant demographics, empathy scores, and academic and clinical experiences.
Table 1.
Participant demographics, academic, and clinical experiences (N = 15 preservice speech-language pathology students).
| ID | Group | Age (years) | Gender | Classification | Previous clinical experience (no. of months) | Learned about stuttering in academic coursework | Learned about counseling in academic coursework | Previous interaction with persons who stutter | Empathy score (JSPE-HPS) |
|---|---|---|---|---|---|---|---|---|---|
| A2 | STEPS | 19 | Female | Sophomore | No (0) | Yes | No | Yes | 116 |
| A4 | STEPS | 19 | Female | Junior | No (0) | Yes | No | Yes | 123 |
| A6 | STEPS | 31 | Female | Leveling | Yes (12) | Yes | Yes | No | 137 |
| B4 | STEPS | 20 | Female | Junior | No (0) | No | No | No | 103 |
| C1 | STEPS | 20 | Female | Junior | Yes (12) | Yes | Yes | Yes | 124 |
| C2 | STEPS | 21 | Female | Junior | Yes (4) | Yes | Yes | Yes | 116 |
| D4 | STEPS | 19 | Female | Junior | No (0) | Yes | No | Yes | 129 |
| D2 | STEPS | 21 | Female | Junior | No (0) | Yes | No | No | 121 |
| A3 | Control | 20 | Female | Sophomore | Yes (1) | Yes | No | No | 121 |
| A5 | Control | 19 | Female | Junior | Yes (12) | Yes | No | Yes | 112 |
| B1 | Control | 19 | Female | Sophomore | No (0) | Yes | No | Yes | 128 |
| B3 | Control | 21 | Female | Senior | Yes (36 | Yes | Yes | Yes | 129 |
| B5 | Control | 18 | Female | Freshman | No (0) | Yes | Yes | No | 103 |
| B6 | Control | 18 | Female | Junior | No (0) | Yes | Yes | Yes | 118 |
| D3 | Control | 21 | Female | Junior | No (0) | Yes | Yes | No | 125 |
Note. JSPE-HPS = Jefferson Scale of Physician Empathy–Health Profession Student; STEPS = Simulated Training in Evidence-Based Practice for Stuttering.
Active Listening Skill Differences Between Groups
Mann–Whitney–Wilcoxon tests indicated that the STEPS 1.1 and control groups were not significantly different in their pretest use of open questions (p = .752); paraphrasing (p = .372); reflection of feelings (p = .423); check-outs (p = .350); or demonstration of empathy, acceptance, and congruence (p = .905). Participants also demonstrated similar percentages of client-directed eye gaze, as demonstrated by nonsignificant differences between groups (p = .536).
Posttest analyses revealed significant group differences in use of paraphrasing, U = 55, p = .002. Specifically, the STEPS 1.1 group (Mdn = 2.625) paraphrased significantly more often than the control group (Mdn = 0.000). Analyses also indicated significant differences in use of client-directed eye gaze, U = 55, p = .001, with the STEPS 1.1 group demonstrating a significantly higher percentage of client-directed eye gaze (Mdn = 74.78) than the control group (Mdn = 41.40). No significant, between-groups differences were found for use of open questions (p = .631); reflection of feelings (p = 1.00); check-outs (p = .922); or demonstration of empathy, acceptance, and congruence (p = .261). See Table 2 for medians, means, standard deviations, and ranges of participants' pre- and posttest active listening behaviors according to the ALOS-M and use of client-directed eye gaze, respectively.
Table 2.
Means, medians, standard deviations, and ranges of participants' pre- and posttest active listening behaviors for N = 15 participants.
| Behavior | Pretest |
Posttest |
||
|---|---|---|---|---|
| Mdn | M (SD; range) | Mdn | M (SD; range) | |
| Open questions | ||||
| STEPS | 0 | 0.41 (0.65; 0–1.75) | 0.5 | 0.78 (1.06; 0–3) |
| Control | 0.5 | 0.39 (0.38; 0–.75) | 0.5 | 1.10 (1.17; 0–3) |
| Total | 0 | 0.4 (0.52; 0–1.75) | .5 | 0.93 (1.08; 0–3) |
| Paraphrasing | ||||
| STEPS | 0 | 0.78 (1.38; 0–3.75) | 2.63 | 2.84 (0.84; 2–4)* |
| Control | 0 | 0.29 (0.76; 0–2) | 0 | 0.43 (0.79; 0–2) |
| Total | 0 | 0.55 (1.13; 0–3.75) | 2 | 1.72 (1.48; 0–4) |
| Reflection of feelings | ||||
| STEPS | 0 | 0.06 (0.18; 0–.5) | 0 | 0.25 (0.71; 0–2) |
| Control | 0 | 0 | 0 | 0.14 (0.38; 0–1) |
| Total | 0 | 0.03 (0.13; 0–.5) | 0 | 0.2 (0.56; 0–2) |
| Check-outs | ||||
| STEPS | 0 | 0 | 0 | 0.16 (0.44; 0–1.25) |
| Control | 0 | 0.29 (0.76; 0–2) | 0 | 0.57 (1.51; 0–4) |
| Total | 0 | 0.13 (0.52; 0–2) | 0 | 0.35 (1.06; 0–4) |
| Acceptance, congruence, and empathy | ||||
| STEPS | 2 | 1.72 (0.75; .75–3) | 2 | 2.22 (0.41; 1.75–3) |
| Control | 1.5 | 0.78 (0.78; 1–3) | 1.86 | 1.86 (0.79; 1–3) |
| Total | 2 | 1.73 (0.73; .75–3) | 2 | 2.05 (0.(0.62; 1–3) |
| Client-directed eye gaze | ||||
| STEPS | 51.07% | 51.23% (14.18; 26.43–69.3) | 74.78% | 74.96% (12.22; 55–91.95)* |
| Control | 49.23% | 45.3% (11.23; 24.46–54.22) | 41.41% | 40.8% (16.05; 18.5–65.9) |
| Total | 50% | 48.46% (12.8; 24.46–69.3) | 65.9% | 59.01% (22.28; 18.5–91.95) |
Note. Open questions; paraphrasing; reflection of feelings; check-outs; and acceptance, congruence, and empathy were measured using the Active Listening Observation Scale–Modified (Bodie et al., 2014) on a scale from 0 (never) to 4 (always). Client-directed eye gaze values reflect the percentage of time eye gaze was maintained. STEPS = Simulated Training in Evidence-Based Practice for Stuttering.
Significant difference within and between groups at posttest (p < .01).
Active Listening Skill Differences Within Groups
Within the STEPS 1.1 group, Wilcoxon signed-ranks tests indicated significant differences in use of paraphrasing (p = .034) from pre- to posttest. Specifically, participants paraphrased significantly more often after participating in STEPS 1.1 (Mdn = 2.625) compared to pretest (Mdn = 0.000). A significant increase in use of client-directed eye gaze (p = .008) was also observed from pretest (Mdn = 51.07) to posttest (Mdn = 74.78). The STEPS 1.1 group did not demonstrate within-group, pre- to posttest differences in use of open questions (p = .098); reflection of feelings (p = 1.00); check-outs (p = 1.00); or demonstration of empathy, acceptance, and congruence (p = .073).
Within the control group, results indicated nonsignificant pre- to posttest differences across variables including use of open questions (p = .100); paraphrasing, reflection of feelings (p = 1.00); check-outs (p = 1.00); and demonstration of empathy, acceptance, and congruence (p = 1), as well as nonsignificant differences in client-directed eye gaze (p = .688). Table 2 reports the within-group means/medians, standard deviations, and ranges of participants' pre- and posttest active listening behaviors according to the ALOS-M and use of client-directed eye gaze, respectively.
Social Validity and Acceptability
In response to the five-item social validity and acceptability measure, all eight STEPS 1.1 participants reported participating in STEPS 1.1 active listening training increased their counseling confidence (M = 6.78, SD = 0.44) and competence (M = 6.33, SD = 0.87). Participants also reported that the STEPS 1.1 platform was easy to use (M = 7.00, SD = 0.00), enjoyable (M = 7.00, SD = 0.00), and worth their time (M = 7.00, SD = 0.00).
Participants' qualitative responses revealed a high level of satisfaction with and acceptability of the initial module of the STEPS 1.1 intervention program. Specifically, participants reported that participating in STEPS 1.1 increased their awareness of effective versus ineffective counseling behaviors, as well as their confidence using these behaviors with the parent of a preschooler who stutters. Participants reportedly appreciated the opportunity to view the videos multiple times, were satisfied with the program duration, and felt that participating was worth their time. With regard to suggestions for improvement, participants suggested having the videos depict a broader range of client behavior during counseling interactions with parents of preschoolers who stutter and provide examples of questions and comments that encourage parents to share their feelings about their child's stuttering and provide additional opportunities to practice paraphrasing within the initial STEPS 1.1 module. Qualitative responses detailing participants' acceptability of and perceptions of the content of STEPS 1.1 are reported in Table 3.
Table 3.
Social validity and acceptability questionnaire responses for n = 8 participants in the STEPS 1.1 group.
| Item | M (SD; range) | Representative quote(s) |
|---|---|---|
| 1. Participating in STEPS increased my counseling confidence. | 6.78 (0.44; 6–7) | “STEPS showed me how effective rephrasing what the client says is at making them feel important and understood.” (D4) “Even after watching a few videos, I felt much more relaxed and open, though certainly not the best at counseling. I was also more aware of my actions and the actions/words of the client.” (B4) |
| 2. Participating in STEPS increased my counseling competence (i.e., my ability or skill level). | 6.33 (0.87; 5–7) | “I felt much more comfortable in the second evaluation than I did in the first, and believe I was able to gain more knowledge from the client the second time around.” (D2) “My skill level in counseling parents of individuals with CSD has definitely increased. I do not know if my ability to counsel the individuals themselves (with CSD) has increased. For instance, are these techniques still applicable when interviewing a child who stutters?” (A6) |
| 3. STEPS was easy to use. | 7 | “I liked being able to replay the video as many times as I needed, and I felt like I learned something from the computer portion of STEPS.” (A6) |
| 4. I enjoyed participating in STEPS. | 7 | “I am hoping to specialize in fluency disorders in grad school and I am so glad I had the opportunity to participate in this and start getting some knowledge on what exactly stuttering entails and how to handle initial evaluations!” (A4) “It felt way more personal than my day-to-day classwork, and that personal experience with clients is what drew me to becoming an SLP in the first place.” (A6) |
| 5. Participating in STEPS was worth my time. | 7 | “I truly feel more prepared to counsel clients than before the STEPS program.” (A6) |
| 6. What did you like about STEPS? | “What I like about it is that I am only a second year SLP major and was able to have this experience that really opened my eyes.” (A2) “I like that it offered both written/module-type lessons to prepare me and make me think about things I wouldn't have noticed myself and later it allowed me to apply it to a real-life scenario.” (B4) “I enjoyed getting multiple opportunities to exhibit what I learned here.” (C1) “I really liked all of the videos varying in good and bad.” (C2) “I liked how many video examples it provided. This really helped me understand what effective and ineffective listening looks like.” (D4) |
|
| 7. What did you dislike about STEPS? What would you change for future users? | “Include a different module for counseling the clients who stutter, since this module seemed focused on counseling the parents of clients who stutter. I would love to participate in something like that!” (A6) “Perhaps some more variety in examples of how different clients behave in counseling.” (B4) “I think that adding some short videos about what types of questions to ask clients to get them to talk more about their feelings would be helpful. Also, videos about common stuttering myths and how to explain to the client that they are false would be great.” (D4) “I don't think I disliked anything, but I would maybe allow for a second submission of a modified response to the client after seeing the efficient response. This could make for good practice on what open ended questions could look like.” (D2) |
|
| 8. Please share your comments regarding the duration of STEPS (i.e., the length of STEPS as a whole). | “The program was the perfect amount of time in my opinion.” (C1) “I thought the length was perfect. It was long enough that I easily remembered the information but not too long that I got bored.” (D4) |
|
| 9. Additional feedback | “I'm impressed with how much I gained from this experience, which only lasted about 1 hour! I certainly feel like I've gotten more valuable information than I would have gotten from an average hour of class.” (A6) “Absolutely loved having the opportunity to participate in STEPS! I feel like this is going to be very beneficial for my future as an SLP and it gave me so much excitement for the next few years I will spend continuing to learn more about this field!” (A4) “Thank you so much for this experience. I believe I am walking away with a lot more knowledge and confidence.” (D2) |
Note. Items were based on Pehrson et al. (2016) and Thistle and McNaughton (2015). Responses were provided on a Likert scale from 1 (extremely disagree) to 7 (extremely agree). When a single representative quote is presented, that was the only qualitative feedback for that item. The letter–number combinations (e.g., A6) represent each participant's anonymous code. STEPS = Simulated Training in Evidence-Based Practice for Stuttering; SLP = speech-language pathologist.
Discussion
Researchers have repeatedly demonstrated SLPs self-report having low competence and confidence when assessing and treating persons who stutter (Kelly et al., 1997, 2020; Tellis et al., 2008) and express discomfort with using the word “stuttering” during stuttering assessments (Byrd et al., 2020). These self-reports of clinical un- or underpreparedness may contribute, at least in part, to client reports of dissatisfaction, with persons who stutter and/or their families perceiving SLPs as not understanding or adequately attending to their concerns (Manning, 2004; Yaruss et al., 2002). The lack of preservice clinical training opportunities specific to stuttering and counseling likely plays a role in clients' dissatisfaction with services and feelings of unreadiness among SLPs (Yaruss et al., 2017). The purpose of this pilot study was to determine the effectiveness and acceptability of STEPS 1.1, the first module of an accessible, cost-effective, theory-driven content and learning platform, for improving active listening skills in one target group—preservice SLPs—during initial assessment interviews of parents of young children who stutter. Findings have implications for improving training for SLPs working with persons who stutter and their families, increasing accessibility to and feasibility of clinical training and improving stuttering assessment and treatment effectiveness.
The Use of STEPS 1.1 to Improve Active Listening Skills
Findings from this study suggest that participation in STEPS 1.1 increases preservice SLPs' use of some active listening skills compared to pretest and to a control group when conducting a brief initial interview with an SP Parent of a child who stutters. Specifically, preservice SLPs who engaged in STEPS 1.1 utilized paraphrasing and client-directed eye gaze significantly more frequently at posttest than at pretest (and more at posttest than participants who did not participate in STEPS 1.1). Significant pre- to posttest differences were not observed for use of open questions; reflection of feelings; check-outs; or global ratings of acceptance, congruence, and empathy across the STEPS 1.1 or control groups.
There are several reasons why participants demonstrated the greatest improvements in paraphrasing and client-directed eye gaze following participation in STEPS 1.1 compared to other active listening behaviors. First, as previously indicated, videos provided through STEPS 1.1 were relatively brief (i.e., 19–45 s each), and the STEPS 1.1 training module used in this study lasted approximately 45 min. Previous studies citing broader improvement in active listening skills following intervention were longer in duration, with interventions lasting several hours (Kaderavek et al., 2004), lasting several weeks (Newman et al., 2022), or occurring over the course of a semester (Kuntze et al., 2009; Levitt, 2002). The duration of this study was purposefully brief to provide initial data about the method and outcome of STEPS 1.1 in preparation for future, expanded research. Our pilot study supports use of even a brief active listening intervention to achieve improvement in client-directed eye gaze and use of paraphrasing; however, it is possible that other active listening skills, such as the use of check-outs, may require longer exposures to clinician behavior and repeated opportunities for practice before improvement is observed.
Second, although STEPS 1.1 participants observed video exemplars of clinicians demonstrating each of the active listening behaviors that subsequently were assessed (e.g., reflection of feeling, check-outs, and demonstration of empathy), they were only asked to rate and were provided corrective feedback for the clinician's use of client-directed eye gaze, silence, body orientation, and verbal reflections/paraphrasing of content and/or feelings. Therefore, participants did improve use of two of the behaviors—client-directed eye gaze and paraphrasing—they explicitly identified, but not other active listening skills. It should be noted that body orientation was largely determined by the arrangement of the interview room (i.e., placement of the chairs, table, and cameras). Previous studies also have shown that the use of silence (e.g., pausing) is particularly challenging for learners (Back et al., 2009; Levitt, 2002). Thus, increasing the use of silence may require longer, more explicit training (an empirical question for further investigation). In general, our findings suggest that engaged and intentional practice of specific targets, rather than passive observation, seems to be most effective for improving preservice SLPs' use of active listening skills.
Acceptability of STEPS 1.1
Quantitative and qualitative responses from the eight participants who completed STEPS 1.1 indicate that the initial active listening module of the STEPS 1.1 program was highly acceptable in its content, structure, duration, and impact, as reflected by quantitative ratings ranging from 5 to 7 across each social validity domain. Participants' qualitative responses provide valuable insight into which specific components of STEPS 1.1 were most effective and those that should be adjusted in future iterations. For example, for self-perceived increases in counseling competence following the STEPS 1.1 intervention, participants reported a mean average rating of 6.33 on the Likert scale of 1 (extremely disagree) to 7 (extremely agree). As illustrated in Table 3, one participant noted being able to collect more information from the SP Parent during the second clinical interaction, suggesting that training students in active listening skills through STEPS 1.1 may increase their perceived abilities to collect information during a diagnostic interview. Another participant shared uncertainty regarding whether the active listening skills learned through STEPS 1.1 would apply in a different but related clinical context, for example, when interviewing a child who stutters. Future studies should determine the degree to which STEPS 1.1 (and subsequent modules) improve preservice SLPs' active listening and other clinical skills with children, teens, and adults who stutter; parents and other caregivers; and practicing SLPs across varying clinical scenarios.
Importantly, STEPS 1.1 also appears to be feasible and acceptable for implementation. All eight participants who started the STEPS 1.1 intervention voluntarily completed it, and all participants “extremely agreed” that STEPS 1.1 was easy to use, enjoyable, and worth their time. Participants independently accessed and navigated the STEPS 1.1 active listening module without needing help from the researcher, supporting the feasibility of its use among preservice SLPs in a university setting and either in person (as in this study) or online.
Participants' responses regarding what they liked about STEPS 1.1 revealed components that were particularly salient or meaningful, such as the number and variety of video exemplars, as well as exposure to “real-life” clinical situations even at an early stage in their education in the field. The value of exposure to stuttering at the pregraduate level is supported, in part, by previous researchers who have found that increased exposure to fluency disorders at the undergraduate and graduate levels is associated with an increased likelihood of specializing in fluency disorders postgraduation, suggesting opportunities for the development of even more advanced skills and expanded clinical experience (Coalson et al., 2016). Findings from this study suggest that STEPS 1.1 is a brief, effective, and viable method for providing students with increased exposure to stuttering even at the undergraduate level and that students recognize and appreciate this opportunity.
Participants also provided critical insights about how STEPS 1.1 should be modified for maximum effectiveness and engagement. For example, one participant suggested allowance of more opportunities for users to type in hypothetical verbal responses after observing the expert clinician to obtain more practice and, presumably, increase confidence and competency. Participants also suggested inclusion of videos providing exposure to persons who stutter themselves and depicting a wider variety of client behavior. Participants also suggested that STEPS 1.1 could provide guidance on how to elicit thoughts and feelings from clients and how to counsel clients regarding myths and facts about stuttering. Finally, participants shared their satisfaction regarding how much they gained from STEPS 1.1 despite the brevity of the intervention and, in comparison to classroom instruction, implicating the role of STEPS 1.1 for improving clinical training.
Future Expansion of STEPS
In future studies, examination of STEPS 1.1 in terms of optimal number and types of practice opportunities and types of video exemplars necessary to achieve competency in active listening skills is needed. STEPS also is being expanded to target training across the diverse elements of stuttering assessment and treatment. As noted in the introduction, another module focused on identifying stuttering behaviors currently is being tested. Other future expansions of STEPS will include training modules that target differential diagnosis (e.g., stuttering vs. cluttering); comprehensive assessment of the affective; behavioral and cognitive components of stuttering; acquiring knowledge about the genetic, developmental, and epigenetic contributions to stuttering; and evidence-based methods of advancing clinical care (self-disclosure, voluntary stuttering, communication effectiveness, etc.). Expansions of STEPS may also target increased understanding of stuttering among teachers, university professors, interdisciplinary health care professionals, and the general population to reduce misconceptions and stigmatization of stuttering.
Implications for Clinical Training and Practice
Results from this study are encouraging in that even brief participation in an intervention that targets effective use of active listening in a stuttering assessment, such as STEPS 1.1, can increase preservice SLPs' use of paraphrasing and client-directed eye gaze. Arguably, these two behaviors can begin to enhance the quality of clinical assessment and treatment of persons who stutter and all client populations SLPs serve (Croft et al., 2022). Findings also echo those of previous studies in medicine, nursing, and psychotherapy citing improvement in use of active listening and other counseling skills following participation in an online intervention (Kemper et al., 2008; Lockwood et al., 2018; Pehrson et al., 2016; Schönrock-Adema et al., 2009) and signal exciting directions for training in speech-language pathology. Specifically, to help students improve use of active listening skills (e.g., client-directed eye gaze and paraphrasing), instructors and clinical supervisors could utilize training methods that allow for observation, application, corrective feedback, and repeated practice, as included in STEPS. Given its cost-effectiveness and accessibility, this training method could be used to supplement classroom instruction and/or provided to students as an additional opportunity for learning and clinical exposure.
Improving preservice SLPs' use of active listening skills also has positive implications for consumers of our clinical practice. Perceived clinical empathy is highly associated with greater client satisfaction and enhanced treatment outcomes (Elliott et al., 2011, 2018) and has been highlighted as a key contributor to effective provision of clinical services for persons who stutter (Manning, 2004; Plexico et al., 2010). These positive outcomes are particularly relevant when working with parents of children who stutter who often report strong, negative emotional responses to their child's stuttering (Berquez & Kelman, 2018; Croft et al., 2022; Humeniuk & Tarkowski, 2016; Langevin et al., 2010; Nonis et al., 2021; Plexico & Burrus, 2012). Equipping preservice SLPs with active listening training may promote their use of these skills as practicing SLPs across client populations and, more specifically, as applicable to STEPS, to foster more personalized, empathic care for persons who stutter and their families.
Additional Considerations and Future Directions
Findings from this pilot study should be interpreted with the following considerations in mind. First, given the exploratory nature of this study, the sample size was relatively small (i.e., 15 participants total) and homogeneous (e.g., all female participants and from the same university). Participants' pre- and posttest behaviors and acceptability measures may differ within a larger and more diverse sample. Future studies should recruit a larger participant sample that reflects greater diversity in gender and career stage (e.g., preservice vs. practicing SLPs) to determine whether these factors influence the effectiveness and acceptability of STEPS 1.1 for improving active listening skills. It should also be considered that all participants in this study elected to enroll and had learned about stuttering in their coursework and thus might reflect a more motivated group of preservice SLPs than those from a randomly selected sample. It should also be noted that several acceptability questions were posed in an affirmative manner (e.g., “Participating in STEPS 1.1 increased my confidence…”), which might have affected participants' responses. Participants' self-reported acceptability may differ with more neutral item wording. In contrast, the four open-ended questions allowed for the full range of comments and suggestions.
Given that motivation can influence trainees' use of active listening skills (Nemec et al., 2017), future studies should determine the effectiveness of active listening skills training when participants are randomly selected. Future studies should also investigate additional contributors to individual differences in use of active listening skills in a stuttering assessment, such as self-reported empathy, anxiety, confidence, previous clinical experience, previous interaction with persons who stutter or as a person who stutters, and time since stuttering and/or counseling course enrollment and/or clinical training experience in stuttering. Each of these factors may influence participants' presenting levels of comfort, confidence, and counseling competence, as well as the necessary intervention dosage needed to achieve competence (Chan et al., 1998; Jin et al., 2019; Kelley & Kelley, 2013; Levitt, 2002; Schlair et al., 2012). Moreover, given the experimental design of this study, it is unknown whether gains in active listening observed in the STEPS 1.1 group (i.e., increased use of paraphrasing and client-directed eye gaze) were maintained. It is critical to determine whether participants in STEPS 1.1 maintain improvements in active listening skills over time and how much exposure to STEPS 1.1 is necessary for maximum and long-lasting effectiveness.
For clinical training, it would be interesting to identify the influence of clinical exposure to persons who stutter through interactive video modules, such as in STEPS, on participants' clinical confidence and self-perceived competence when working with persons who stutter, particularly given the literature citing low self-reported confidence and competence among SLPs with this population (Byrd et al., 2020; Gabel, 2014; Kelly et al., 2020; Tellis et al., 2008). It would also be helpful to compare the use of counseling microskills following STEPS 1.1 to simple instruction in a classroom setting in relation to both demonstration and self-perceptions of comfort and confidence in implementing these skills. The influence of opportunities such as STEPS on participants' decisions to work with those who stutter, and even specialize in stuttering later in their career, should also be examined. Coalson et al. (2016) reported that extensive exposure to child or adult fluency clients (i.e., five clients or more) predicted later self-reported specialization in fluency disorders. However, it is unknown whether simulated exposure, such as that provided through STEPS, is as effective as in-person exposure. Future studies should investigate the influence of STEPS (1.1. and additional modules) on clinicians' postgraduation specialization in fluency disorders, with an emphasis on the appropriate dosage needed to significantly increase participants' desires to provide services to those who stutter, or even specialize in stuttering.
Additionally, future studies should investigate the use of the STEPS training approach for improving more advanced counseling skills, such as information giving, relaying a diagnosis of stuttering, counseling persons who stutter on avoidance behaviors, and rectifying common misconceptions about stuttering. The effectiveness of STEPS for improving these skills should be examined not only immediately following intervention but also over time.
Conclusions
This study provides pilot data supporting the use of brief intervention via the STEPS 1.1 program to improve preservice SLPS' use of client-directed eye gaze and paraphrasing and active listening skills that have been shown to predict perceived clinical empathy and increase assessment and treatment effectiveness. Future studies should determine whether gains following participation in STEPS 1.1 are maintained over time, recruit larger and more diverse participant samples, test other modules of STEPS, and identify the effectiveness of STEPS 1.1 and all of STEPS' components across critical competencies related to assessing and treating persons who stutter.
Data Availability Statement
The authors are actively collaborating with our institution's department of research data services to develop a publicly available website for the Arthur M. Blank Center for Stuttering Education and Research, the expressed purpose of which will be to share (a) data sets, (b) published articles, and (c) professional posters and presentations. A prototype of this website may be found at https://moody.utexas.edu/centers/lang-stuttering-institute/stuttering-research-resources, with a more full-scale rollout of the website targeted for January 1, 2023.
Acknowledgments
This project was completed with support from the Malcolm Fraser Foundation and the Blank Foundation Legacy Grant awarded to the first author, as well as the National Institute on Deafness and Other Communication Disorders Award F31DC020117-01 to the second author. The authors thank Michael Mahometa for his help with the statistical analyses, as well Phoebe Fertig and Marlo Levey for their assistance with interrater reliability. This study would not have been possible without each preservice speech-language pathologist participant who gave their time, insight, and feedback during the study. Thank you for helping to advance clinical training for speech-language pathologists working with persons who stutter and their families worldwide.
Funding Statement
This project was completed with support from the Malcolm Fraser Foundation and the Blank Foundation Legacy Grant awarded to the first author, as well as the National Institute on Deafness and Other Communication Disorders Award F31DC020117-01 to the second author. The authors thank Michael Mahometa for his help with the statistical analyses, as well Phoebe Fertig and Marlo Levey for their assistance with interrater reliability. This study would not have been possible without each preservice speech-language pathologist participant who gave their time, insight, and feedback during the study.
References
- American Speech-Language-Hearing Association. (2015). Highlights and trends: Member and affiliate counts, year-end 2015. http://www.asha.org/research/memberdata/
- American Speech-Language-Hearing Association. (2016). Scope of practice in speech-language pathology [Scope of practice]. http://www.asha.org/policy/
- Back, A. L. , Bauer-Wu, S. M. , Rushton, C. H. , & Halifax, J. (2009). Compassionate silence in the patient-clinician encounter: A contemplative approach. Journal of Palliative Medicine, 12(12), 1113–1117. https://doi.org/10.1089/jpm.2009.0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Burns, M. I. , Struijk, J. , Herron, L. , Mach, H. , & Yorkston, K. (2017). Assessing the believability of standardized patients trained to portray communication disorders. American Journal of Speech-Language Pathology, 26(3), 791–805. https://doi.org/10.1044/2017_AJSLP-16-0068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. R. , & Verticchio, H. (2014). Facilitating speech-language pathology graduate students' ability to manage stress: A pilot study. Contemporary Issues in Communication Science and Disorders, 41(Spring), 24–38. https://doi.org/10.1044/cicsd_41_S_24 [Google Scholar]
- Beck, K. , & Kulzer, J. (2018). Teaching counseling microskills to audiology students: Recommendations from professional counseling educators. Seminars in Hearing, 39(1), 91–106. https://doi.org/10.1055/s-0037-1613709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berquez, A. , Hertsberg, N. , Hollister, J. , Zebrowski, P. , & Millard, S. (2015). What do children who stutter and their parents expect from therapy and are their hopes aligned? Procedia—Social and Behavioral Sciences, 193, 25–36. https://doi.org/10.1016/j.sbspro.2015.03.241 [Google Scholar]
- Berquez, A. , & Kelman, E. (2018). Methods in stuttering therapy for desensitizing parents of children who stutter. American Journal of Speech-Language Pathology, 27(3S), 1124–1138. https://doi.org/10.1044/2018_AJSLP-ODC11-17-0183 [DOI] [PubMed] [Google Scholar]
- Blood, G. W. , & Blood, I. M. (2016). Long-term consequences of childhood bullying in adults who stutter: Social anxiety, fear of negative evaluation, self-esteem, and satisfaction with life. Journal of Fluency Disorders, 50, 72–84. https://doi.org/10.1016/j.jfludis.2016.10.002 [DOI] [PubMed] [Google Scholar]
- Bodie, G. D. , Jones, S. M. , Vickery, A. J. , Hatcher, L. , & Cannava, K. (2014). Examining the construct validity of enacted support: A multitrait–multimethod analysis of three perspectives for judging immediacy and listening behaviors. Communication Monographs, 81(4), 495–523. https://doi.org/10.1080/03637751.2014.957223 [Google Scholar]
- Bodie, G. D. , St. Cyr, K. , Pence, M. , Rold, M. , & Honeycutt, J. (2012). Listening competence in initial interactions I: Distinguishing between what listening is and what listeners do. International Journal of Listening, 26(1), 1–28. https://doi.org/10.1080/10904018.2012.639645 [Google Scholar]
- Boey, R. A. , van de Heyning, P. H. , Wuyts, F. L. , Heylen, L. , Stoop, R. , & de Bodt, M. S. (2009). Awareness and reactions of young stuttering children aged 2–7 years old towards their speech disfluency. Journal of Communication Disorders, 42(5), 334–346. https://doi.org/10.1016/j.jcomdis.2009.03.002 [DOI] [PubMed] [Google Scholar]
- Brisk, D. J. , Healey, E. C. , & Hux, K. A. (1997). Clinicians' training and confidence associated with treating school-age children who stutter. Language, Speech, and Hearing Services in Schools, 28(2), 164–176. https://doi.org/10.1044/0161-1461.2802.164 [Google Scholar]
- Brugel, S. , Postma-Nilsenová, M. , & Tates, K. (2015). The link between perception of clinical empathy and nonverbal behavior: The effect of a doctor's gaze and body orientation. Patient Education and Counseling, 98(10), 1260–1265. https://doi.org/10.1016/j.pec.2015.08.007 [DOI] [PubMed] [Google Scholar]
- Bylund, C. L. , & Makoul, G. (2005). Examining empathy in medical encounters: An observational study using the empathic communication coding system. Health Communication, 18(2), 123–140. https://doi.org/10.1207/s15327027hc1802_2 [DOI] [PubMed] [Google Scholar]
- Byrd, C. T. , Bedore, L. M. , & Ramos, D. (2015). The disfluent speech of bilingual Spanish–English children: Considerations for differential diagnosis of stuttering. Language, Speech, and Hearing Services in Schools, 46(1), 30–43. https://doi.org/10.1044/2014_LSHSS-14-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd, C. T. , Werle, D. , & St. Louis, K. O. (2020). Speech-language pathologists' comfort level with use of term “stuttering” during evaluations. American Journal of Speech-Language Pathology, 29(2), 841–850. https://doi.org/10.1044/2020_AJSLP-19-00081 [DOI] [PubMed] [Google Scholar]
- Byrd, C. T. , Winters, K. L. , Young, M. , Werle, D. , Croft, R. L. , Hampton, E. , Coalson, G. , White, A. , & Gkalitsiou, Z. (2021). The communication benefits of participation in camp dream. Speak. Live.: An extension and replication. Seminars in Speech and Language, 42(02), 117–135. https://doi.org/10.1055/s-0041-1723843 [DOI] [PubMed] [Google Scholar]
- Caris-Verhallen, W. M. , Kerkstra, A. , & Bensing, J. M. (1999). Non-verbal behaviour in nurse–elderly patient communication. Journal of Advanced Nursing, 29(4), 808–818. https://doi.org/10.1046/j.1365-2648.1999.00965.x [DOI] [PubMed] [Google Scholar]
- Caris-Verhallen, W. M. , Kerkstra, A. , Bensing, J. M. , & Grypdonck, M. H. (2000). Effects of video interaction analysis training on nurse-patient communication in the care of the elderly. Patient Education and Counseling, 39(1), 91–103. https://doi.org/10.1016/S0738-3991(99)00094-4 [DOI] [PubMed] [Google Scholar]
- Chamberlain, P. , & Ray, J. (1988). The therapy process code: A multidimensional system for observing therapist and client interactions in family treatment. Advances in Behavioral Assessment of Children and Families, 4, 189–217. [Google Scholar]
- Chan, F. , Leahy, M. , Chan, C. , Lam, C. S. , Hilburger, J. , Jones, J. , & Kamnetz, B. (1998). Training needs of rehabilitation counselors in the emerging mental health/managed care environment. Rehabilitation Education, 12(4), 333–345. [Google Scholar]
- Chandrashekar, B. R. , Chako, T. V. , Anand, K. M. , Suvetha, K. , Jaishankar, H. P. , & Suma, S. (2020). Enhancing identification and counseling skills of dental undergraduate students using a customized Tobacco Counseling Training Module (TCTM)—A piloting of the process using ADDIE framework. Indian Journal of Cancer, 57(3), 296–310. https://doi.org/10.4103/ijc.IJC_229_19 [DOI] [PubMed] [Google Scholar]
- Coalson, G. A. , Byrd, C. T. , & Rives, E. (2016). Academic, clinical, and educational experiences of self-identified fluency specialists. Perspectives of the ASHA Special Interest Groups, 1(4), 16–43. https://doi.org/10.1044/persp1.SIG4.16 [Google Scholar]
- Cooper, E. B. , & Cooper, C. S. (1985). Clinician attitudes toward stuttering: A decade of change (1973–1983). Journal of Fluency Disorders, 10(1), 19–33. https://doi.org/10.1016/0094-730X(85)90003-8 [Google Scholar]
- Cooper, E. B. , & Cooper, C. S. (1996). Clinician attitudes towards stuttering: Two decades of change. Journal of Fluency Disorders, 21(2), 119–135. https://doi.org/10.1016/0094-730X(96)00018-6 [Google Scholar]
- Crichton-Smith, I. , Wright, J. , & Stackhouse, J. (2003). Attitudes of speech and language therapists towards stammering: 1985 and 2000. International Journal of Language and Communication Disorders, 38(3), 213–234. https://doi.org/10.1080/1368282031000086282 [DOI] [PubMed] [Google Scholar]
- Croft, R. L. , Byrd, C. T. , & Kelly, E. M. (2022). The influence of active listening on parents' perceptions of clinical empathy in a stuttering assessment: A preliminary study. Journal of Communication Disorders, 100, Article 106274. https://doi.org/10.1016/j.jcomdis.2022.106274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Blok, B. M. , de Greef, M. H. , ten Hacken, N. H. , Sprenger, S. R. , Postema, K. , & Wempe, J. B. (2006). The effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: A pilot study. Patient Education and Counseling, 61(1), 48–55. https://doi.org/10.1016/j.pec.2005.02.005 [DOI] [PubMed] [Google Scholar]
- Decety, J. , Smith, K. E. , Norman, G. J. , & Halpern, J. (2014). A social neuroscience perspective on clinical empathy. World Psychiatry: Official Journal of the World Psychiatric Association, 13(3), 233–237. https://doi.org/10.1002/wps.20146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiIorio, C. , Resnicow, K. , McDonnell, M. , Soet, J. , McCarty, F. , & Yeager, K. (2003). Using motivational interviewing to promote adherence to antiretroviral medications: A pilot study. Journal of the Association of Nurses in AIDS Care, 14(2), 52–62. https://doi.org/10.1177/1055329002250996 [DOI] [PubMed] [Google Scholar]
- Dijkstra, H. , Albada, A. , Klöckner Cronauer, C. , Ausems, M. G. , & van Dulmen, S. (2013). Nonverbal communication and conversational contribution in breast cancer genetic counseling: Are counselors' nonverbal communication and conversational contribution associated with counselees' satisfaction, needs fulfillment and state anxiety in breast cancer genetic counseling? Patient Education and Counseling, 93(2), 216–223. https://doi.org/10.1016/j.pec.2013.05.014 [DOI] [PubMed] [Google Scholar]
- Doud, A. K. , Hoepner, J. K. , & Holland, A. L. (2020). A survey of counseling curricula among accredited communication sciences and disorders graduate student programs. American Journal of Speech-Language Pathology, 29(2), 789–803. https://doi.org/10.1044/2020_AJSLP-19-00042 [DOI] [PubMed] [Google Scholar]
- Ebert, K. D. , & Kohnert, K. (2010). Common factors in speech-language treatment: An exploratory study of effective clinicians. Journal of Communication Disorders, 43(2), 133–147. https://doi.org/10.1016/j.jcomdis.2009.12.002 [DOI] [PubMed] [Google Scholar]
- Eggers, K. , Van Eerdenbrugh, S. , & Byrd, C. (2020). Speech disfluencies in bilingual Yiddish-Dutch speaking children. Clinical Linguistics & Phonetics, 34(6), 576–592. https://doi.org/10.1080/02699206.2019.1678670 [DOI] [PubMed] [Google Scholar]
- Elliott, R. , Bohart, A. C. , Watson, J. C. , & Greenberg, L. S. (2011). Empathy. Psychotherapy, 48(1), 43–49. https://doi.org/10.1037/a0022187 [DOI] [PubMed] [Google Scholar]
- Elliott, R. , Bohart, A. C. , Watson, J. C. , & Murphy, D. (2018). Therapist empathy and client outcome: An updated meta-analysis. Psychotherapy (Chicago, Ill.), 55(4), 399–410. https://doi.org/10.1037/pst0000175 [DOI] [PubMed] [Google Scholar]
- Fassaert, T. , van Dulmen, S. , Schellevis, F. , & Bensing, J. (2007). Active listening in medical consultations: Development of the Active Listening Observation Scale (ALOS-global). Patient Education and Counseling, 68(3), 258–264. https://doi.org/10.1016/j.pec.2007.06.011 [DOI] [PubMed] [Google Scholar]
- Fields, S. K. , Hojat, M. , Gonnella, J. S. , Mangione, S. , Kane, G. , & Magee, M. (2004). Comparisons of nurses and physicians on an operational measure of empathy. Evaluation & the Health Professions, 27(1), 80–94. https://doi.org/10.1177/0163278703261206 [DOI] [PubMed] [Google Scholar]
- Fields, S. K. , Mahan, P. , Tillman, P. , Harris, J. , Maxwell, K. , & Hojat, M. (2011). Measuring empathy in healthcare profession students using the Jefferson Scale of Physician Empathy: Health Provider–Student version. Journal of Interprofessional Care, 25(4), 287–293. https://doi.org/10.3109/13561820.2011.566648 [DOI] [PubMed] [Google Scholar]
- Fontaine, G. , Cossette, S. , Maheu-Cadotte, M. A. , Mailhot, T. , Heppell, S. , Roussy, C. , Côté, J. , Gagnon, M. P. , & Dubé, V. (2019). Behavior change counseling training programs for nurses and nursing students: A systematic descriptive review. Nurse Education Today, 82, 37–50. https://doi.org/10.1016/j.nedt.2019.08.007 [DOI] [PubMed] [Google Scholar]
- Gabel, R. M. (2014). School speech-language pathologists' experiences with stuttering: An Ohio survey. eHearsay, 3(3), 5–29. [Google Scholar]
- Gold, J. M. (2018). Recognizing and resolving ethical issues: In counseling stepfamilies. The Family Journal, 26(1), 73–76. https://doi.org/10.1177/1066480718754768 [Google Scholar]
- Guttormsen, L. S. , Kefalianos, E. , & Næss, K. A. (2015). Communication attitudes in children who stutter: A meta-analytic review. Journal of Fluency Disorders, 46, 1–14. https://doi.org/10.1016/j.jfludis.2015.08.001 [DOI] [PubMed] [Google Scholar]
- Haley, B. , Heo, S. , Wright, P. , Barone, C. , Rettiganti, M. R. , & Anders, M. (2017). Relationships among active listening, self-awareness, empathy, and patient-centered care in associate and baccalaureate degree nursing students. NursingPlus Open, 3, 11–16. https://doi.org/10.1016/j.npls.2017.05.001 [Google Scholar]
- Halpern, J. (2012). Clinical empathy in medical care. In J. Decety (Ed.), Empathy: From bench to bedside (pp. 229–244). MIT Press. https://doi.org/10.7551/mitpress/9780262016612.003.0013 [Google Scholar]
- Hill, A. E. , Davidson, B. J. , & Theodoros, D. G. (2010). A review of standardized patients in clinical education: Implications for speech-language pathology programs. International Journal of Speech-Language Pathology, 12(3), 259–270. https://doi.org/10.3109/17549500903082445 [DOI] [PubMed] [Google Scholar]
- Hill, A. E. , Davidson, B. J. , & Theodoros, D. G. (2013). The performance of standardized patients in portraying clinical scenarios in speech-language therapy. International Journal of Language & Communication Disorders, 48(6), 613–624. https://doi.org/10.1111/1460-6984.12034 [DOI] [PubMed] [Google Scholar]
- Hojat, M. , Louis, D. Z. , Markham, F. W. , Wender, R. , Rabinowitz, C. , & Gonnella, J. S. (2011). Physicians' empathy and clinical outcomes for diabetic patients. Academic Medicine, 86(3), 359–364. https://doi.org/10.1097/ACM.0b013e3182086fe1 [DOI] [PubMed] [Google Scholar]
- Hojat, M. , Mangione, S. , Nasca, T. J. , Cohen, M. J. M. , Gonnella, J. S. , Erdmann, J. B. , Veloski, J. , & Magee, M. (2001). The Jefferson Scale of Physician Empathy: Development and preliminary psychometric data. Educational and Psychological Measurement, 61(2), 349–365. https://doi.org/10.1177/00131640121971158 [Google Scholar]
- Horvath, A. O. , Del Re, A. C. , Flückiger, C. , & Symonds, D. (2011). Alliance in individual psychotherapy. Psychotherapy, 48(1), 9–16. https://doi.org/10.1037/a0022186 [DOI] [PubMed] [Google Scholar]
- Humeniuk, E. , & Tarkowski, Z. (2016). Parents' reactions to children's stuttering and style of coping with stress. Journal of Fluency Disorders, 49, 51–60. https://doi.org/10.1016/j.jfludis.2016.08.002 [DOI] [PubMed] [Google Scholar]
- Hutchinson, L. (1999). Evaluating and researching the effectiveness of educational interventions. BMJ, 318(7193), 1267–1269. https://doi.org/10.1136/bmj.318.7193.1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivey, A. E. , Normington, C. J. , Miller, C. D. , Morrill, W. H. , & Haase, R. F. (1968). Microcounseling and attending behavior: An approach to prepracticum counselor training. Journal of Counseling Psychology, 15(5, Pt.2), 1–12. https://doi.org/10.1037/h0026129 [Google Scholar]
- Jagosh, J. , Donald Boudreau, J. , Steinart, Y. , Macdonald, M. E. , & Ingram, L. (2011). The importance of physician listening from the patients' perspective: Enhancing diagnosis, healing, and the doctor-patient relationship. Patient Education and Counseling, 85(3), 369–374. https://doi.org/10.1016/j.pec.2011.01.028 [DOI] [PubMed] [Google Scholar]
- Jin, H. K. , Park, S. H. , Kang, J. E. , Choi, K. S. , Kim, H. A. , Jeon, M. S. , & Rhie, S. J. (2019). The influence of a patient counseling training session on pharmacy students' self-perceived communication skills, confidence levels, and attitudes about communication skills training. BMC Medical Education, 19(1), 172. https://doi.org/10.1186/s12909-019-1607-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, L. M. , & Huggins, T. J. (2014). Empathy in the dentist-patient relationship: Review and application. The New Zealand Dental Journal, 110(3), 98–104. [PubMed] [Google Scholar]
- Kaderavek, J. N. , Laux, J. M. , & Hills, N. H. (2004). A counseling training module for students in speech-language pathology training programs. Contemporary Issues in Communication Science and Disorders, 31(Fall), 153–161. https://doi.org/10.1044/cicsd_31_F_153 [Google Scholar]
- Kelley, K. J. , & Kelley, M. F. (2013). Teaching empathy and other compassion-based communication skills. Journal for Nurses in Professional Development, 29(6), 321–324. https://doi.org/10.1097/01.NND.0000436794.24434.90 [DOI] [PubMed] [Google Scholar]
- Kelly, E. M. , Martin, J. S. , Baker, K. E. , Rivera, N. I. , Bishop, J. E. , Krizizke, C. B. , Stettler, D. , & Stealy, J. M. (1997). Academic and clinical preparation and practices of school speech-language pathologists with people who stutter. Language, Speech, and Hearing Services in Schools, 28(3), 195–212. https://doi.org/10.1044/0161-1461.2803.195 [Google Scholar]
- Kelly, E. M. , Singer, C. M. , Henderson, J. K. , & Shaw, K. O. (2020). Stuttering practice self-assessment by school speech-language practitioners. Language, Speech, and Hearing Services in Schools, 51(4), 1156–1171. https://doi.org/10.1044/2020_LSHSS-20-00028 [DOI] [PubMed] [Google Scholar]
- Kemper, K. J. , Foy, J. M. , Wissow, L. , & Shore, S. (2008). Enhancing communication skills for pediatric visits through on-line training using video demonstrations. BMC Medical Education, 8(1), Article number 8. https://doi.org/10.1186/1472-6920-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. S. , Kaplowitz, S. , & Johnston, M. V. (2004). The effects of physician empathy on patient satisfaction and compliance. Evaluation & the Health Professions, 27(3), 237–251. https://doi.org/10.1177/0163278704267037 [DOI] [PubMed] [Google Scholar]
- Klassen, T. R. , & Kroll, R. M. (2005). Opinions on stuttering and its treatment: A follow-up survey and cross-cultural comparison. Journal of Speech Language and Audiology, 29(2), 73–82. [Google Scholar]
- Kraft-Todd, G. T. , Reinero, D. A. , Kelley, J. M. , Heberlein, A. S. , Baer, L. , & Riess, H. (2017). Empathic nonverbal behavior increases ratings of both warmth and competence in a medical context. PLOS ONE, 12(5), e0177758. https://doi.org/10.1371/journal.pone.0177758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntze, J. , Molen, H. T. , & Born, M. P. (2009). Increase in counselling communication skills after basic and advanced microskills training. British Journal of Educational Psychology, 79(1), 175–188. https://doi.org/10.1348/000709908X313758 [DOI] [PubMed] [Google Scholar]
- Langevin, M. , Packman, A. , & Onslow, M. (2010). Parent perceptions of the impact of stuttering on their preschoolers and themselves. Journal of Communication Disorders, 43(5), 407–423. https://doi.org/10.1016/j.jcomdis.2010.05.003 [DOI] [PubMed] [Google Scholar]
- Larson, E. B. , & Yao, X. (2005). Clinical empathy as emotional labor in the patient–physician relationship. JAMA, 293(9), 1100–1106. https://doi.org/10.1001/jama.293.9.1100 [DOI] [PubMed] [Google Scholar]
- Lee, J. (2014). Update on didactic and clinical education in fluency disorders: 2013–2014 [Unpublished master's thesis] . University of Pittsburgh. [DOI] [PubMed] [Google Scholar]
- Levitt, D. H. (2002). Active listening and counselor self-efficacy. The Clinical Supervisor, 20(2), 101–115. https://doi.org/10.1300/J001v20n02_09 [Google Scholar]
- Lieberman, A. (2018). Counseling issues: Addressing behavioral and emotional considerations in the treatment of communication disorders. American Journal of Speech-Language Pathology, 27(1), 13–23. https://doi.org/10.1044/2017_AJSLP-16-0149 [DOI] [PubMed] [Google Scholar]
- Lockwood, S. N. , Compton, S. M. , Green, J. L. , & Rasmussen, K. (2018). Dental hygiene students' clinical skill acquisition: Activity theory and the use of videos. Journal of Dental Hygiene, 92(2), 15–21. [PubMed] [Google Scholar]
- Luterman, D. (2020). On teaching counseling: Getting beyond informational counseling. American Journal of Speech-Language Pathology, 29(2), 903–908. https://doi.org/10.1044/2019_AJSLP-19-00013 [DOI] [PubMed] [Google Scholar]
- Luterman, D. (2021). Counseling parents at the time of diagnosis: Moving toward client-centered practice. American Journal of Audiology, 30(1), 226–230. https://doi.org/10.1044/2020_AJA-20-00122 [DOI] [PubMed] [Google Scholar]
- Mallard, A. R. , Gardner, L. S. , & Downey, C. S. (1988). Clinical training in stuttering for school clinicians. Journal of Fluency Disorders, 13(4), 253–259. https://doi.org/10.1016/0094-730X(88)90016-2 [Google Scholar]
- Manning, W. (2004). How can you understand? You don't stutter. Contemporary Issues in Communication Science and Disorders, 31(Spring), 58–68. https://doi.org/10.1044/cicsd_31_S_58 [Google Scholar]
- Marion, G. S. , Hairston, J. M. , Davis, S. W. , & Kirk, J. K. (2018). Using standardized patient assessments to evaluate a health literacy curriculum. Family Medicine, 50(1), 52–57. https://doi.org/10.22454/FamMed.2018.539107 [DOI] [PubMed] [Google Scholar]
- McCarthy, P. , Culpepper, N. B. , & Lucks, L. (1986). Variability in counseling experiences and training among ESB-accredited programs. ASHA, 28(9), 49–52. [PubMed] [Google Scholar]
- McClure, J. A. , & Olsen, C. (2010). Specialty recognition in fluency disorders: Challenges for the second decade. SIG 4 Perspectives on Fluency and Fluency Disorders, 20(1), 15–19. https://doi.org/10.1044/ffd20.1.15 [Google Scholar]
- Millard, S. K. , Zebrowski, P. , & Kelman, E. (2018). Palin parent–child interaction therapy: The bigger picture. American Journal of Speech-Language Pathology, 27(3S), 1211–1223. https://doi.org/10.1044/2018_AJSLP-ODC11-17-0199 [DOI] [PubMed] [Google Scholar]
- Murphy, W. P. , & Quesal, R. W. (2004). Best practices for preparing students to work with people who stutter. Contemporary Issues in Communication Science and Disorders, 31(Spring), 25–39. https://doi.org/10.1044/cicsd_31_S_25 [Google Scholar]
- National Stuttering Association. (2009, May). The experience of people who stutter: A survey by the National Stuttering Association. Executive summary. https://westutter.org/what-is-stuttering/experience-people-stutter/
- Nemec, P. B. , Spagnolo, A. C. , & Soydan, A. S. (2017). Can you hear me now? Teaching listening skills. Psychiatric Rehabilitation Journal, 40(4), 415–417. https://doi.org/10.1037/prj0000287 [DOI] [PubMed] [Google Scholar]
- Newman, D. S. , Gerrard, M. K. , Villarreal, J. N. , & Kaiser, L. T. (2022). Deliberate practice of consultation microskills: An exploratory study of training. Training and Education in Professional Psychology, 16(3), 263–271. https://doi.org/10.1037/tep0000368 [Google Scholar]
- Nicholson, N. , Martin, P. F. , & Munoz, K. (2015). Satisfaction with communication using remote face-to-face language interpretation services with Spanish-speaking parents: A pilot study. SIG 9 Perspectives on Hearing and Hearing Disorders in Childhood, 25(2), 70–82. https://doi.org/10.1044/hhdc25.2.70 [Google Scholar]
- Nonis, D. , Unicomb, R. , & Hewat, S. (2021). Parental perceptions of stuttering in children: A systematic review of the literature. Speech, Language and Hearing. https://doi.org/10.1080/2050571X.2021.191329970 [Google Scholar]
- Pehrson, C. , Banerjee, S. C. , Manna, R. , Shen, M. J. , Hammonds, S. , Coyle, N. , Krueger, C. A. , Maloney, E. , Zaider, T. , & Bylund, C. L. (2016). Responding empathically to patients: Development, implementation, and evaluation of a communication skills training module for oncology nurses. Patient Education and Counseling, 99(4), 610–616. https://doi.org/10.1016/j.pec.2015.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penman, A. , Hill, A. E. , Hewat, S. , & Scarinci, N. (2021). Does a simulation-based learning programme assist with the development of speech–language pathology students' clinical skills in stuttering management? International Journal of Language & Communication Disorders, 56(6), 1334–1346. https://doi.org/10.1111/1460-6984.12670 [DOI] [PubMed] [Google Scholar]
- Phillips, D. T. , & Mendel, L. L. (2008). Counseling training in communication disorders: A survey of clinical fellows. Contemporary Issues in Communication Science and Disorders, 35(Spring), 44–53. https://doi.org/10.1044/cicsd_35_S_44 [Google Scholar]
- Pitt, R. , Theodoros, D. , Hill, A. J. , Rodriguez, A. D. , & Russell, T. (2017). The feasibility of delivering constraint-induced language therapy via the Internet. Digital Health, 3, 205520761771876. https://doi.org/10.1177/2055207617718767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plexico, L. W. , & Burrus, E. (2012). Coping with a child who stutters: A phenomenological analysis. Journal of Fluency Disorders, 37(4), 275–288. https://doi.org/10.1016/j.jfludis.2012.06.002 [DOI] [PubMed] [Google Scholar]
- Plexico, L. W. , Manning, W. H. , & DiLollo, A. (2010). Client perceptions of effective and ineffective therapeutic alliances during treatment for stuttering. Journal of Fluency Disorders, 35(4), 333–354. https://doi.org/10.1016/j.jfludis.2010.07.001 [DOI] [PubMed] [Google Scholar]
- Quail, M. , Brundage, S. B. , Spitalnick, J. , Allen, P. J. , & Beilby, J. (2016). Student self-reported communication skills, knowledge and confidence across standardised patient, virtual and traditional clinical learning environments. BMC Medical Education, 16(1), 73. https://doi.org/10.1186/s12909-016-0577-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlair, S. , Hanley, K. , Gillespie, C. , Disney, L. , Kalet, A. , Darby, P. C. , Frank, E. , Spencer, E. , Harris, J. , & Jay, M. (2012). How medical students' behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. Journal of Nutrition Education and Behavior, 44(6), 653–657. https://doi.org/10.1016/j.jneb.2011.08.006 [DOI] [PubMed] [Google Scholar]
- Schönrock-Adema, J. , Van der Molen, H. T. , & van der Zee, K. I. (2009). Effectiveness of a self-instruction program for microcounseling skills training. Teaching of Psychology, 36(4), 246–252. https://doi.org/10.1080/00986280903173132 [Google Scholar]
- Schwartz, V. S. , Rothpletz-Puglia, P. , Denmark, R. , & Byham-Gray, L. (2015). Comparison of standardized patients and real patients as an experiential teaching strategy in a nutrition counseling course for dietetic students. Patient Education and Counseling, 98(2), 168–173. https://doi.org/10.1016/j.pec.2014.11.009 [DOI] [PubMed] [Google Scholar]
- Sherman, J. J. , & Cramer, A. (2005). Measurement of changes in empathy during dental school. Journal of Dental Education, 69(3), 338–345. https://doi.org/10.1002/j.0022-0337.2005.69.3.tb03920.x [PubMed] [Google Scholar]
- Shipley, K. G. (1997). Interviewing and counseling in communicative disorders: Principles and procedures. Allyn & Bacon. [Google Scholar]
- St. Louis, K. O. , & Durrenberger, C. H. (1993). What communication disorders do experienced clinicians prefer to manage? ASHA, 35(12), 23–35. [PubMed] [Google Scholar]
- Tellis, G. M. , Bressler, L. , & Emerick, K. (2008). An exploration of clinicians views about assessment and treatment of stuttering. SIG 4 Perspectives on Fluency and Fluency Disorders, 18(1), 16–23. https://doi.org/10.1044/ffd18.1.16 [Google Scholar]
- Thakur, T. , Frey, M. , & Chewning, B. (2019). Evaluating pharmacy student consultations with standardized patients on opioid medication use and opioid-specific risks. American Journal of Pharmaceutical Education, 83(10), 7494. https://doi.org/10.5688/ajpe7494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thistle, J. J. , & McNaughton, D. (2015). Teaching active listening skills to pre-service speech-language pathologists: A first step in supporting collaboration with parents of young children who require AAC. Language, Speech, and Hearing Services in Schools, 46(1), 44–55. https://doi.org/10.1044/2014_LSHSS-14-0001 [DOI] [PubMed] [Google Scholar]
- Turnbull, A. P. , Turnbull, R. , Erwin, E. J. , Soodak, L. , & Shogren, K. A. (2010). Families, professionals, and exceptionality. Positive outcomes through partnership and trust (6th ed.). Merrill Prentice Hall. [Google Scholar]
- Weidner, M. E. , St. Louis, K. O. , & Glover, H. L. (2018). Changing nonstuttering preschool children's stuttering attitudes. American Journal of Speech-Language Pathology, 27(4), 1445–1457. https://doi.org/10.1044/2018_AJSLP-18-0019 [DOI] [PubMed] [Google Scholar]
- Yang, Y. S. , Liu, P. C. , Lin, Y. K. , Lin, C. D. , Chen, D. Y. , & Lin, B. Y. (2021). Medical students' preclinical service-learning experience and its effects on empathy in clinical training. BMC Medical Education, 21(1), 301. https://doi.org/10.1186/s12909-021-02739-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaruss, J. S. (1999). Current status of academic and clinical education in fluency disorders at ASHA-accredited training programs. Journal of Fluency Disorders, 24(3), 169–183. https://doi.org/10.1016/S0094-730X(99)00013-3 [Google Scholar]
- Yaruss, J. S. , Lee, J. , Kikani, K. , Leslie, P. , Herring, C. , Ramachandar, S. , Tichenor, S. , Quesal, R. , & McNeil, M. (2017). Update on didactic and clinical education in fluency disorders: 2013–2014. American Journal of Speech-Language Pathology, 26(1), 124–137. https://doi.org/10.1044/2016_AJSLP-15-0154 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S. , & Quesal, R. W. (2002). Academic and clinical education in fluency disorders: An update. Journal of Fluency Disorders, 27(1), 43–63. https://doi.org/10.1016/S0094-730X(01)00112-7 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S. , Quesal, R. W. , Reeves, L. , Molt, L. F. , Kluetz, B. , Caruso, A. J. , McClure, J. A. , & Lewis, F. (2002). Speech treatment and support group experiences of people who participate in the National Stuttering Association. Journal of Fluency Disorders, 27(2), 115–134. https://doi.org/10.1016/S0094-730X(02)00114-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are actively collaborating with our institution's department of research data services to develop a publicly available website for the Arthur M. Blank Center for Stuttering Education and Research, the expressed purpose of which will be to share (a) data sets, (b) published articles, and (c) professional posters and presentations. A prototype of this website may be found at https://moody.utexas.edu/centers/lang-stuttering-institute/stuttering-research-resources, with a more full-scale rollout of the website targeted for January 1, 2023.