Abstract
Previous reports on cardiac intervention in cases with antithrombin deficiency are extremely limited. We report a case of acute coronary syndrome with antithrombin deficiency in a 62-year-old man with multiple histories of thrombosis. He had worsening chest pain, and laboratory data showed an elevated level of troponin T, suggesting acute myocardial infarction. Currently, there is no fixed anticoagulation strategy for coronary intervention in patients with antithrombin deficiency. In this case, we performed coronary intervention with heparin in addition to antithrombin concentrate. The intervention was successfully performed without thrombosis or bleeding complications.
Learning objective
Antithrombin deficiency is a rare disorder and data about coronary intervention for cases with antithrombin deficiency are limited. We successfully performed intervention with our anticoagulant management and it would be beneficial for future reference.
Keywords: Antithrombin deficiency, Acute coronary syndrome
Introduction
Antithrombin deficiency is a rare autosomal dominant disorder, and patients have a higher risk of developing thromboembolism [1]. Heparin exhibits an anticoagulant effect by forming a complex with antithrombin, so antithrombin deficiency weakens the activity of heparin as an anticoagulant. Previous reports on cardiac interventions in cases with antithrombin deficiency are extremely limited. Herein, we report the case of a 62-year-old man with antithrombin deficiency, presenting with acute coronary syndrome.
Case report
A 62-year-old man visited our hospital due to worsening chest pain. He had a history of thrombosis including left deep venous thrombosis at the age of 39 years and acute limb ischemia at the age of 40 years. For this thrombosis history, direct oral anticoagulant (edoxaban) was continuously prescribed. He smoked about 50 cigarettes per day from age 16–40 years. He had a family history of arteriosclerosis and thromboembolism.
On admission, vital signs included blood pressure of 116/59 mm Hg and pulse rate of 93 beats per minute in a regular rhythm. Physical examination was unremarkable. Laboratory data showed an elevated level of troponin T (208 ng/L, normal range within 14 ng/L). Creatine kinase (CK) and CK-MB levels were within the normal range. The N-terminal pro-brain natriuretic peptide and D-dimer levels were 1819 pg/mL and 0.6 mg/L, respectively. The chest radiography showed no lung congestion and cardiomegaly. The electrocardiogram showed sinus rhythm, first-degree atrioventricular block, complete right bundle branch block, and no ST-segment change (Fig. 1). The echocardiography showed hypokinesis of the lateral and inferior walls with an ejection fraction of 56 %.
Fig. 1.
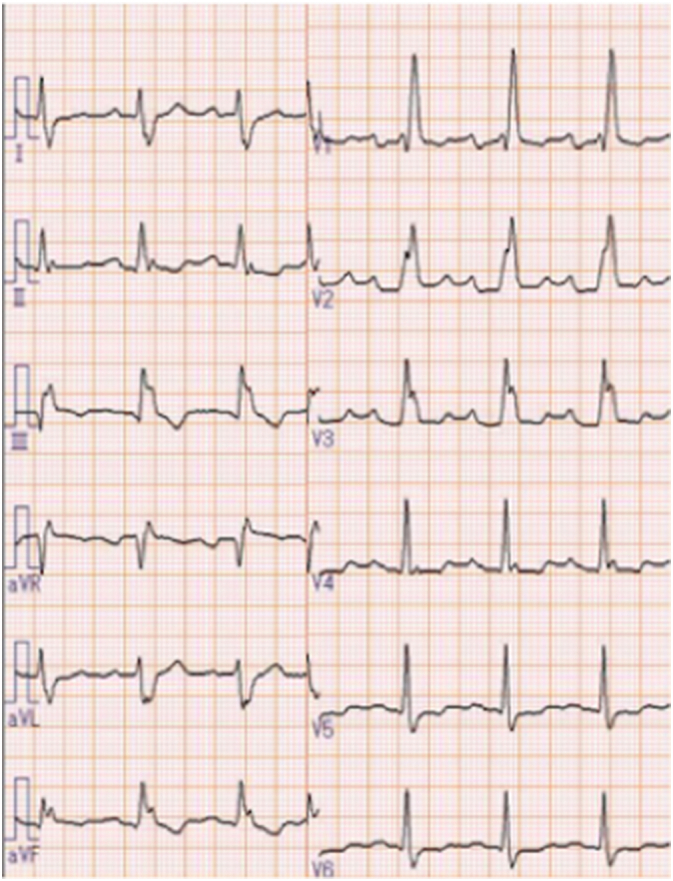
Electrocardiogram showing sinus rhythm, first-degree atrioventricular block, and complete right bundle branch block.
Before urgent coronary angiography, we suspected that he had thrombophilia based on his multiple histories of thrombosis and submitted serological tests related to thrombophilia. The result revealed a decrease in antithrombin activity of 41.0 % (normal range, 80.0 %–130.0 %), suspecting antithrombin deficiency. We had to develop an anticoagulant strategy because heparin could not exhibit enough anticoagulant effects under low antithrombin activity.
Referring to an article on the strategy for cardiovascular surgery in antithrombin deficiency cases [2], our strategy was as follows: the antithrombin concentrate was administered to achieve antithrombin activity of ≥120 % before transferring the patient to the catheter room after the administration of dual antiplatelet therapy (DAPT; aspirin and prasugrel). The activated clotting time (ACT) was confirmed to be ≥200 s during the coronary angiography and ≥300 s during the percutaneous coronary intervention (PCI). When these ACT targets were not achieved after heparin administration, argatroban was used as the alternative anticoagulant.
He received 3000 IU of antithrombin concentrate which was empirically determined, and antithrombin activity reached 124.4 %, which was over 120 %. In the catheter room, 4500 IU (50 IU/body weight) of heparin was injected, and 10 min later, the ACT reached 235 s. The angiography revealed total occlusion in the proximal right coronary artery, 99 % stenosis in the posterolateral branch of the left circumflex artery (LCX) with thrombolysis in myocardial infarction (TIMI) II flow, and 75 % stenosis in the proximal left anterior descending artery (Fig. 2). Therefore, PCI for LCX was subsequently performed. We administered 4500 IU of heparin, and 10 min later, the ACT was 262 s, not enough for the target (≥300 s). Therefore, 2000 IU of heparin was injected, and the ACT reached 336 s. During the intervention, the ACT was checked every 15 min to keep it ≥300 s. After all, the ACT targets were achieved only with heparin, so argatroban was not used.
Fig. 2.
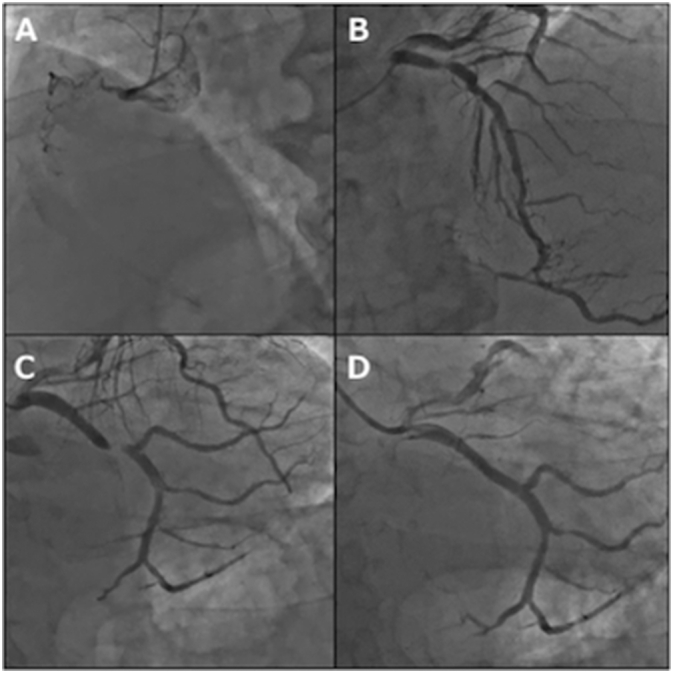
Coronary angiogram showing the total occlusion of the right coronary artery (A), 75 % stenosis of the proximal left anterior descending artery (B), 99 % stenosis of the posterolateral branch (#13) of the left circumflex artery (C), and final angiogram following stent implantation (D).
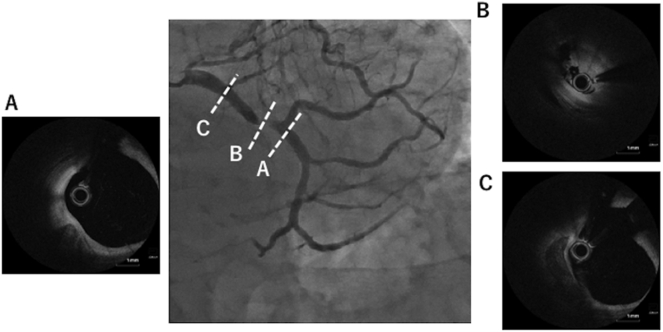
Optical coherence tomography showed attenuated plaque with platelet thrombus at the culprit lesion and the calcified plaque was detected around the culprit (Fig. 3). The LCX lesion was pre-dilated with a 2.0 × 15 mm semi-compliant balloon, and a 4.0 × 15 mm Xience Skypoint stent (Abbott Vascular, Santa Clara, CA, USA) was placed. The final angiogram showed TIMI III flow in the LCX.
Fig. 3.
Optical coherence tomography showing attenuated plaque with platelet thrombus at the culprit lesion (B), and calcified plaque around the lesion (A and C).
Following the coronary intervention, DAPT was continued, and warfarin was also administered as an anticoagulant therapy. He was stable without chest pain and discharged after 2 weeks.
Discussion
Antithrombin is an anticoagulant produced in the liver that inactivates the intrinsic coagulant pathway. Antithrombin deficiency is a rare autosomal dominant disorder that was first reported by Egeberg in 1965 [3], and the estimated prevalence in the general population is between 0.05 and 5 per 1000 [4]. Patients with antithrombin deficiency are at increased risk for thromboembolism mainly in the venous circulation, such as deep venous thrombosis. The relationship seemed unclear between antithrombin deficiency and arterial embolism.
Our literature search revealed a few case reports of acute coronary syndrome with antithrombin deficiency [5], [6], [7]. In all three cases, the patients were in their 20s or 30s without coronary risks. Peovska et al. reported myocardial reinfarction in a 24-year-old man with congenital antithrombin deficiency [7]. After the first event, the anticoagulant therapy was stopped in 6 months, the patient was readmitted with severe chest pain, and balloon dilation was performed for in-stent occlusion. These cases are referable, but they provided little information on the anticoagulants used in the procedure. Above all, it has not been revealed before the procedure that antithrombin activity is lower than the usual cases.
Heparin is the most frequently used anticoagulant agent in cardiac catheterization. Its anticoagulant effect is exhibited by forming a complex with antithrombin, and in the case of antithrombin deficiency, the anticoagulant activity is assumed insufficient. We chose argatroban hydrate as a second-line agent because antithrombin was not involved in the anticoagulant effect of argatroban, a direct thrombin inhibitor. The lack of antagonist for argatroban is a negative point, but it is an issue for future investigation whether argatoroban is effective in coronary intervention for cases with antithrombin deficiency.
In a surgical report, Nishimura et al. included five cardiovascular surgical cases with antithrombin deficiency [2]. Their protocol suggested the method of administering antithrombin concentrate and ACT control management. The surgical report included five cases, and the perioperative outcomes were all satisfactory. A notable case was a dialysis patient with aortic valve stenosis. Aortic valve replacement was performed with the bioprosthetic valve, and because of valve deterioration, re-operation was necessary 9 months after initial replacement. The cause was assumed to be the discontinuation of warfarin therapy due to bleeding at the vascular access site, resulting in multiple thrombi formed on the leaflets. The current case and the aforementioned case with in-stent occlusion suggest that anticoagulant therapy was key management. Warfarin has been accepted as an effective anticoagulant for decades, but clinical evidence of direct oral anticoagulants for antithrombin deficiency is lacking [8]. In the current case, the bleeding risk was relatively low, and a longer duration of triple therapy (DAPT and warfarin) might be beneficial to decrease thrombotic events. We assume the desirable duration of the triple therapy is 1 to 6 months which depends on the bleeding risk, although definite evidence is lacking.
Conclusion
We experienced a case of acute coronary syndrome with antithrombin deficiency. The current case was managed with antithrombin concentrate, and the procedure was successfully performed using heparin as an anticoagulant agent without thrombus or bleeding complications.
Conflict of interest
Kengo Tanabe received honoraria from Abbott Medical, Boston Scientific, Japan Lifeline, Kaneka, Orbusneich, Daiichi Sankyo, and Bayer. The other authors declare that they have no conflicts of interest to disclose.
Footnotes
Drs Kitamura and Komiyama contributed equally to this work.
References
- 1.Patnaik M.M., Moll S. Inherited antithrombin deficiency: a review. Haemophilia. 2008;14:1229–1239. doi: 10.1111/j.1365-2516.2008.01830.x. [DOI] [PubMed] [Google Scholar]
- 2.Nishimura Y., Takagi Y. Strategy for cardiovascular surgery in patients with antithrombin III deficiency. Ann Thorac Cardiovasc Surg. 2018;24:187–192. doi: 10.5761/atcs.oa.18-00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egeberg O. Inherited antithrombin deficiency causing thrombophilia. Thromb Diath Haemorrh. 1965;13:516–530. doi: 10.1055/s-0038-1656297. [DOI] [PubMed] [Google Scholar]
- 4.Wells P.S., Blajchman M.A., Henderson P., Wells M.J., Demers C., Bourque R., McAvoy A. Prevalence of antithrombin deficiency in healthy blood donors: a cross-sectional study. Am J Hematol. 1994;45:321–324. doi: 10.1002/ajh.2830450409. [DOI] [PubMed] [Google Scholar]
- 5.Fennich N., Salwa A., Nadia B., Latifa O., Jamila Z., Mohamed C. Acute coronary syndrome in a young woman with antithrombin III deficiency. J Cardiol Cases. 2013;7:e101–e103. doi: 10.1016/j.jccase.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tu C.M., Hsueg C.H., Chu K.M., Cheng S.M., Tsao T.P. Simultaneous thromboses of double coronary arteries in a young male with antithrombin III deficiency. Am J Emerg Med. 2009;27(1169):e3–e6. doi: 10.1016/j.ajem.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Peovska I., Maksimovic J., Kalpak O., Pejkov H., Bosevski M. Recurrent myocardial infarction in a young football player with antithrombin III deficiency. Cardiol J. 2008;15:463–466. [PubMed] [Google Scholar]
- 8.Pabinger I., Thaler J. How I treat patients with hereditary antithrombin deficiency. Blood. 2019;134:2346–2353. doi: 10.1182/blood.2019002927. [DOI] [PubMed] [Google Scholar]