Abstract
Eosinophilic myocarditis is a rare subtype of myocarditis characterized by myocardial eosinophilic infiltration, and it is potentially lethal if untreated. In its severest form, acute eosinophilic necrotizing myocarditis may lead to cardiac dysfunction and cardiogenic shock. Several cases have been reported after coronavirus disease 2019 (COVID-19) vaccination, but the pathophysiology is still unclear.
We describe a case of acute necrotizing eosinophilic myocarditis complicated by cardiogenic shock in a 33-year-old man after booster dose of mRNA COVID-19 vaccine. The patient was diagnosed with endomyocardial biopsy, successfully treated with steroids, and discharged on Day 20 after admission in stable condition. In short term follow-up, he was asymptomatic with normal left and right ventricular ejection fraction.
Learning objectives
Eosinophilic myocarditis (EM) still has a high morbidity and mortality, so it is crucial to promptly diagnose it and treat as appropriate. Endomyocardial biopsy is the gold standard for the diagnosis of EM. This case highlights the diagnostic work-up, differential diagnosis of hypereosinophilia, and the management of this life-threatening condition.
Introduction
Eosinophilic myocarditis (EM) is a potentially lethal disease characterized by eosinophil infiltration of the myocardium. It may arise from several etiologies, such as hypersensitivity or autoimmune diseases, infections, or neoplasms. In some cases, the etiology remains unknown, and it is defined as idiopathic hypereosinophilic syndrome [1]. Clinical manifestations range from mild symptoms to severe syndromes and its severest form, the acute necrotizing EM, may lead to cardiogenic shock [1]. The definitive diagnosis is made through endomyocardial biopsy, while cardiac magnetic resonance may be helpful after the acute phase to identify the structural changes caused by myocarditis. Treatment includes corticosteroids and, in some cases, anticoagulation together with heart failure therapy and management of cardiac complications [2]. Recently, myocarditis has increasingly emerged as an adverse effect of coronavirus disease 2019 (COVID-19) vaccinations [3]. We present the case of a patient who developed cardiogenic shock due to acute necrotizing EM after mRNA booster dose for COVID-19.
Case report
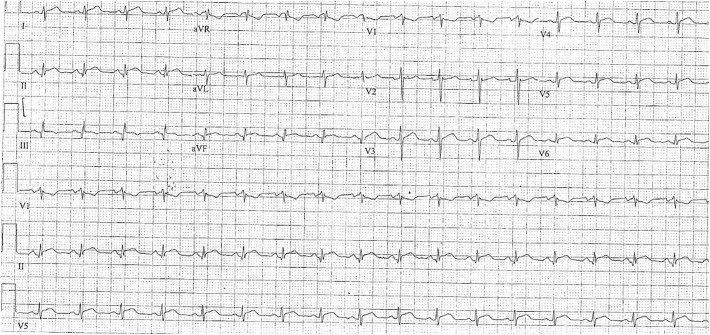
A 33-year-old man was admitted to a peripheral hospital for dyspnea, chest, and abdominal pain. The patient had a history of juvenile epilepsy in pharmacological treatment with valproic acid 500 mg b.i.d.; no history of cardiac disease or cardiovascular risk factors; he received Pfizer-BioNTech COVID-19 booster vaccination 10 days before hospital admission. Recent medical history did not reveal fever and/or recent infections, no overseas travel in the last months, and no history of known allergic diathesis. The clinical examination showed increased jugular pressure, bilateral lung rales, quiet heart sounds, gallop rhythm without peripheral edema. Blood pressure was 90/60 mmHg, heart rate around 100 bpm. Electrocardiogram (ECG) showed sinus tachycardia and diffuse ST-segment elevation with no reciprocal changes (Online Fig. 1); laboratory tests revealed eosinophilic leucocytosis at complete blood count with elevated high-sensitivity troponin I (hs-TnI, 4748 pg/ml) and C-reactive protein levels (CRP, 8.5 mg/dl, upper limit <0.05 mg/dl). The nasopharyngeal swab tested negative for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Echocardiography showed global hypokinesia with reduced left ventricular ejection fraction (LVEF 35 %), normal right heart size and function, no significant valvular diseases, and pericardial effusion with signs of tamponade. Urgent pericardiocentesis was performed draining around 250 ml of citrine fluid and the patient was admitted to the cardiology ward. On the next day, due to the progression of LV dysfunction with haemodynamic instability, the patient was referred to our intensive care unit (ICU).
Online Fig. 1.
Electrocardiogram showing sinus tachycardia and diffuse ST-segment elevation with no reciprocal changes
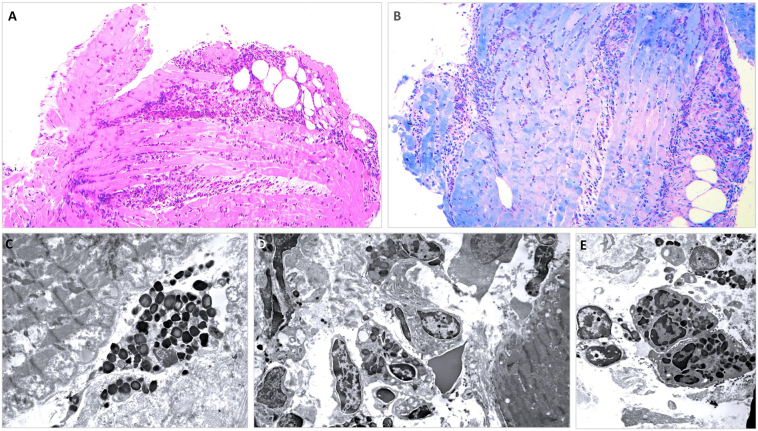
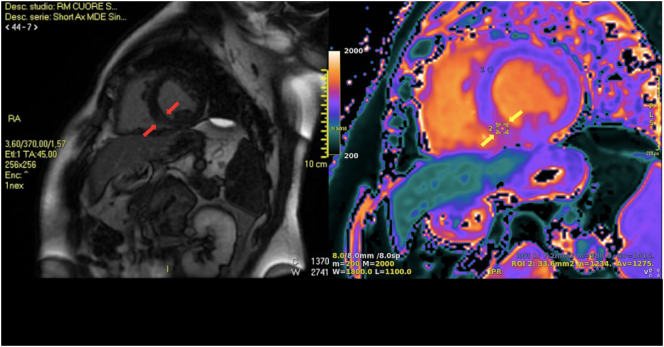
The differential diagnosis included acute coronary syndrome, fulminant myocarditis, and septic shock. COVID-19 was excluded through the SARS-CoV-2 polymerase chain reaction (PCR) test. ECG showed non-ischemic abnormalities, troponin was elevated, and echocardiogram findings together with leukocytosis and elevated CRP, oriented to differential diagnosis between peri-myocarditis or septic shock. Blood and urine cultures were unrevealing and chest X-ray showed bilateral pleural effusion, ruling out the infective status hypothesis. Pericardial exudate demonstrated inflammatory cells but was negative for malignant cells, acid-fast bacilli stain, and tuberculosis PCR. Moreover, the presence of remarkable eosinophilia at presentation and the recent vaccination raised concern for possible drug-induced eosinophilia versus hypereosinophilic syndrome (HES), eosinophilic granulomatosis with polyangiitis (EGPA), and myeloproliferative disorders. Transthoracic echocardiography performed at ICU revealed a LV with normal dimensions, thickened walls, global hypokinesia with severe systolic dysfunction (LVEF 20 %), normal right heart size and function, and no significant valvular diseases (Online Video 1). Considering the hemodynamic deterioration without a definite cause, an endomyocardial biopsy (EMB) was performed urgently (n. 11 biopsy specimens were obtained from right ventricle para-apical region, infundibulum, and anterior septum) and the sample confirmed diffuse infiltrations of eosinophils into the myocardium; PCR did not reveal SARS-CoV-2 RNA and antigens in cardiac samples, nor viral particles were observed in myocytes and/or endothelia (Fig. 1A-E). Subsequently, the diagnosis of myocarditis was confirmed by cardiac magnetic resonance (CMR) performed on day 10 with evidence of myocardial edema at the level of the middle inferior septum in the T2-weighted sequences, intramyocardial late gadolinium enhancement (LGE) at the level of the middle inferior septum (non-ischemic pattern), and an increased native T1 value at middle inferior septum (Fig. 2). Screening for hematologic causes of peripheral eosinophilia was negative; the autoimmunity panel including anti-neutrophil cytoplasmic autoantibody was unremarkable. Testing for infectious diseases was negative. Total-body computed tomography did not reveal malignancies. All tests are summarized in Table 1. Upon admission to the ICU, the patient underwent orotracheal intubation, cardiogenic shock was treated with adrenaline 0.05 μg/kg/min and levosimendan titrated up to 0.2 μg/kg/min and, as soon as perfusion was restored, furosemide 5 mg/h was started. After histological analysis, methylprednisolone i.v. 1 g/day was administered for three days and then tapered, followed by a decreased eosinophilic count. Anticoagulation with unfractionated heparin was also provided. The patient was discharged after 20 days on prednisone 60 mg/die with a slow taper over a period of 28 days and heart failure drugs; at last follow-up, LVEF recovered to 50 % with normal wall thickness. After 2 weeks the patient reported complete relief of symptoms; echocardiography showed a preserved LVEF with mildly reduced longitudinal strain in mid-segment of the inferior interventricular septum. Eosinophilic count moved from 3.0 × 109/l (13.4 %) at admission to 0.72 × 109/l (3.1 %) at day 3 and 0.12 × 109/l (1.4 %) at discharge (day 20). hs-TnI moved from a peak of 4748.70 ng/l at admission to 2179 ng/l at day 3 and negative values at discharge. CRP decreased from 8.5 mg/dl towards negative values.
Fig. 1.
Light (A and B) and electron microscopy (C-E) views of endomyocardial biopsy samples. Massive interstitial inflammatory infiltration, burdened by eosinophilic granulocytes (A: hematoxylin and eosin; B: Giemsa stain). Panel (C) shows a partially degranulated eosinophilic granulocyte close to a myocyte that shows non-specific myofibrillar lysis. Although the inflammatory cells were mixed (D), most infiltrates were constituted of eosinophilic granulocytes (E).
Fig. 2.
Short-axis late gadolinium enhancement imaging demonstrated intramyocardial fibrosis at middle inferior septum (red arrows); at the same level, T1 mapping showed an increased native T1 value (yellow arrows).
Table 1.
Diagnostic tests.
| Infections | |
| Urine cultures | Negative |
| Blood cultures | Negative |
| Pericardial fluid | Negative |
| HCV, HBV, HSV, VZV, CMV, HHV-6, EBV, parvovirus B19, adenovirus, Coxsackie virus, HTLV1–2 | Negative |
| Toxoplasmosis, Toxocara spp., Entamoeba histolytica, Strongyloides stercoralis; parasitological stool test | Negative |
| Immunology | |
| Total IgE | 60 KU/l (n.v. 0–87) |
| Total IgA | 1.15 g/dl (n.v. 0.80–5.30) |
| Total Ig M | 2.38 g/dl (n.v.0.50–2.00) |
| IgG4 | 270,7 mg/l (n.v. 39,2-864,0) |
| Complement C3 | 1.10 g/dl (n.v.0.79–1.52) |
| Complement C4 | 0.13 g/dl (n.v. 0.16–0.38) |
| Autoimmunity | |
| c-ANCA; p-ANCA, ANA, AMA, ENA, nDNA-Ab | Negative |
| Coronavirus | |
| SARS-CoV2 PCR testing | Negative |
| RBD–SARS–CoV2 Ab | Positive (28,925 U/ml) |
| Total SARS-CoV2-Ab | Positive |
| Hematology | |
| BCR/ABL, PDGFR/TEL; FIPIL1/PDGFRA | Negative |
HCV, hepatitis C virus; HBV, hepatitis B virus; HSV, herpes simplex virus; VZV, varicella-zoster virus; HHV-6, human herpesvirus 6; EBV, Epstein-Barr virus; HTLV 1–2, human T-lymphotropic virus type 1–2; IgE, immunoglobulin E; IgA, immunoglobulin A; IgM, immunoglobulin M; IgG4, immunoglobulin G4; c-ANCA, p-ANCA, anti-neutrophil cytoplasmic antibodies targeting proteinase 3 and myeloperoxidase respectively; ANA, anti-nuclear antibody; AMA, anti-mitochondrial antibody; ENA, extractable nuclear antigen; nDNA-Ab, anti-native DNA antibody; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; RBD-SARS-CoV-2 Ab, anti-SARS-CoV-2 spike protein receptor binding domain. BCR/ABL, PDGFR/TEL; FIPL1/PDGFRA gene transcripts.
Discussion
Myocarditis is one of the major recognized adverse reactions to the COVID-19 mRNA vaccine. EM is a hypereosinophilic syndrome with cardiac involvement and, about in 20 % of cases, persistent peripheral eosinophilia [4]. Myocarditis is a major cause of morbidity and mortality. Eosinophil-mediated cardiac damage evolves through 3 phases and many cases are fatal in the first stage: an acute necrotic phase, an intermediate stage with hypercoagulability and risk of thrombotic development, and, if not promptly diagnosed and treated, a fibrotic stage that may result in restrictive cardiomyopathy [5]. The histological findings obtained by EMB were characterized by prevalent eosinophilic infiltrates associated with the degranulation of crystalloids (Fig. 1). Early diagnosis and treatment with high-dose steroids have however resulted in complete cardiac recovery in the majority of individuals [2]: our patient, immediately treated with systemic steroids, had shown a fast recovery, thus not requiring any mechanical support. In a systematic revision of all published histologically proven cases of EM [2], 36 % of cases had not a definite cause, 34 % of patients had hypersensitivity myocarditis traced to a drug, EGPA accounted for 13 %, and HES 8 %. In the remaining 9 %, there were a variety of causes including parasites and malignancies. The diagnosis of HES requires the presence of 1500 peripheral eosinophils/μl, no alternative etiologies, and organ damage due to hypereosinophilia [6]. In our case, EGPA was excluded for the absence of atopy history and negative immunological screening; Loeffler's endomyocarditis was excluded by echocardiographic and CMR findings. Infectious diseases and malignancies were also excluded. Thus, we hypothesized hypersensitivity (i.e. vaccine-related) or idiopathic EM. Myocarditis is a rare complication of vaccination against viruses and has previously been linked only to smallpox vaccination [7]. A recent meta-analysis showed that the overall incidence of myopericarditis from 22 studies was 33.3 cases per million vaccine doses and did not significantly differ between people who received COVID-19 vaccines and those who received non-COVID-19 vaccines. However, among people who received COVID-19 vaccines, the incidence of myopericarditis was significantly higher in males, in people younger than 30 years, after receiving an mRNA vaccine, and after the second dose of vaccine (vs. a first or a third dose) [3]. More recently, EM has been described as a possible adverse reaction to the mRNA COVID-19 vaccine, suggesting a possible hypersensitivity to some component of the vaccine that may act as a hapten: the first case has been reported in a previously well 57-year-old woman after the first Pfizer-BioNTech vaccine [8], and three cases were described within a period of two weeks after the second dose of the same vaccine in patients with known allergic disorders [9]. Furthermore, the presence of eosinophils in myocardial infiltrates has already been described in previous reports of post-COVID-19 vaccine myocarditis undergoing EMB or autopsy studies [10]. In conclusion, in our case, EMB was essential to make the diagnosis and start immunosuppressive treatment. Although a definite cause was not identified, the recent vaccination supports the hypothesis of a possible role of mRNA vaccine in the pathogenic mechanisms. Myocarditis is increasingly being reported in young adults after vaccination for COVID-19, predominantly in young males after their second dose of vaccination [3]. Temporal association does not prove causation, but the brief timespan between vaccination and myocarditis onset together with recent evidence lend support to a possible relationship that deserves further investigations.
The following are the supplementary data related to this article.
Transthoracic echocardiogram: four-chamber view showing normal left ventricular dimensions, thickened walls, global hypokinesia with severe systolic dysfunction, normal right heart size andfunction, and no significant valvular diseases
Funding
Not funded.
Declaration of competing interest
The authors declare that there is no conflict of interest.
Acknowledgments
NA.
References
- 1.Kuchynka P., Palecek T., Masek M., Cerny V., Lambert L., Vitkova I., Linhart A. Current diagnostic and therapeutic aspects of eosinophilic myocarditis. Biomed Res Int. 2016;2016 doi: 10.1155/2016/2829583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brambatti M., Matassini M.V., Adler E.D., Klingel K., Camici P.G., Ammirati E. Eosinophilic myocarditis: characteristics, treatment, and outcomes. J Am Coll Cardiol. 2017;70:2363–2375. doi: 10.1016/j.jacc.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 3.Ling R.R., Ramanathan K., Tan F.L., Tai B.C., Somani J., Fisher D., MacLaren G. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med. 2022;10:679–688. doi: 10.1016/S2213-2600(22)00059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kassem K.M., Souka A., Harris D.M., Parajuli S., Cook J.L. Eosinophilic myocarditis: classic presentation of elusive disease. Circ Cardiovasc Imaging. 2019;12:10–12. doi: 10.1161/CIRCIMAGING.119.009487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogbogu P.U., Rosing D.R., Horne M.K., III Cardiovascular manifestations of hypereosinophilic syndromes. Immunol Allergy Clin North Am. 2007;27:457–475. doi: 10.1016/j.iac.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kahn J.E., Groh M., Lefèvre G. (A critical appraisal of) classification of hypereosinophilic disorders. Front Med (Lausanne) 2017;4:216. doi: 10.3389/fmed.2017.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dudley M.Z., Halsey N.A., Omer S.B., Orenstein W.A., O'Leary S.T., Limaye R.J., Salmon D.A. The state of vaccine safety science: systematic reviews of the evidence. Lancet Infect Dis. 2020;20:e80–e89. doi: 10.1016/S1473-3099(20)30130-4. [DOI] [PubMed] [Google Scholar]
- 8.Ameratunga R., Woon S.T., Sheppard M.N., Garland J., Ondruschka B., Wong C.X., Stewart R.A.H., Tatley M., Stables S.R., Tse R.D. First identified case of fatal fulminant necrotizing eosinophilic myocarditis following the initial dose of the Pfizer-BioNTech mRNA COVID-19 vaccine (BNT162b2, Comirnaty): an extremely rare idiosyncratic hypersensitivity reaction. J Clin Immunol. 2022;42:441–447. doi: 10.1007/s10875-021-01187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frustaci A., Verardo R., Galea N., Lavalle C., Bagnato G., Scialla R., Chimenti C. Hypersensitivity myocarditis after COVID-19 mRNA vaccination. J Clin Med. 2022;11:1660. doi: 10.3390/jcm11061660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verma A.K., Lavine K.J., Lin C.Y. Myocarditis after Covid-19 mRNA vaccination. N Engl J Med. 2021;385:1332–1334. doi: 10.1056/NEJMc2109975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiogram: four-chamber view showing normal left ventricular dimensions, thickened walls, global hypokinesia with severe systolic dysfunction, normal right heart size andfunction, and no significant valvular diseases