Abstract
Objective
The COVID-19 pandemic posed new challenges for integrated health care worldwide. Our study aimed to describe newly implemented structures and procedures of psychosocial consultation and liaison (CL) services in Europe and beyond, and to highlight emerging needs for co-operation.
Methods
Cross-sectional online survey from June to October 2021, using a self-developed 25-item questionnaire in four language versions (English, French, Italian, German). Dissemination was via national professional societies, working groups, and heads of CL services.
Results
Of the participating 259 CL services from Europe, Iran, and parts of Canada, 222 reported COVID-19 related psychosocial care (COVID-psyCare) in their hospital. Among these, 86.5% indicated that specific COVID-psyCare co-operation structures had been established. 50.8% provided specific COVID-psyCare for patients, 38.2% for relatives, and 77.0% for staff. Over half of the time resources were invested for patients. About a quarter of the time was used for staff, and these interventions, typically associated with the liaison function of CL services, were reported as most useful. Concerning emerging needs, 58.1% of the CL services providing COVID-psyCare expressed wishes for mutual information exchange and support, and 64.0% suggested specific changes or improvements that they considered essential for the future.
Conclusion
Over 80% of participating CL services established specific structures to provide COVID-psyCare for patients, their relatives, or staff. Mostly, resources were committed to patient care and specific interventions were largely implemented for staff support. Future development of COVID-psyCare warrants intensified intra- and inter-institutional exchange and co-operation.
Keywords: Consultation and liaison psychiatry, COVID-19, Multinational, Mental health care, Psychiatry, Liaison psychiatry, Psychosomatics, Psychology
1. Introduction
The Coronavirus 2019 (COVID-19) pandemic has been associated with significant psychosocial distress for patients and their families [[1], [2], [3]], as well as for hospital staff [4]. COVID-19 related psychosocial distress warrants a special response because of the impact of the pandemic on patients, their relatives, the health care workers, and society in general [5]. None of us have experienced such a pandemic during our lifetimes. More than two years after the World Health Organization (WHO) declared COVID-19 “a Public Health Emergency of International Concern” in February 2020, Europe, Canada and Iran continued to struggle [6], facing a multi-wave incidence pattern. Regarding the COVID-19 pandemic, initial under-preparedness and poor co-ordination between jurisdictions were common across Europe and beyond [7]. As of early 2021, Europe was experiencing a second wave, which peaked in Spring 2021, which ran into a third wave until early Summer 2021, followed by a fourth wave from Autumn 2021. The extent and severity of these waves have varied greatly across Europe, Canada, and Iran, combined with different governmental strategies and vaccination rates [6,8]. This situation has presented considerable challenges for consultation and liaison (CL) mental health services in general hospitals worldwide [9].
During the first wave of the COVID-19 pandemic, the spokespersons of the working group on CL psychosomatics of the German College of Psychosomatic Medicine (DKPM) and the German Society for Psychosomatic Medicine and Medical Psychotherapy (DGPM) entered into discussions on how to support each other. This exchange led to an online survey of psychiatric, psychological, and psychosomatic CL services in Germany (D), Austria (A), and Switzerland (CH) (the “DACH” region), on COVID-19 related psychosocial care (COVID-psyCare), conducted between December 2020 and May 2021 [9]. This research project was communicated via the mailing list of the European Association of Psychosomatic Medicine (EAPM). The feedback received indicated an unmet need for multinational exchange on COVID-psyCare, consistent with a call for action for mental health research efforts for the COVID-19 pandemic [10] and in accordance with the recommendations of the report of the Academy of Consultation-Liaison Psychiatry Task Force on lessons learned from the COVID-19 pandemic [3].
The reported survey across and beyond Europe could build on a substantial history of multinational knowledge sharing between psychosocial CL services. During recent decades, there has been a growing European collaboration to stimulate and support exchange, research, teaching, and training in the areas of Psychosomatic Medicine, CL Psychiatry and Psychosomatics, as well as Integrated Care [11]. In 1955, the first European Conference on Psychosomatic Research (ECPR) was held. In 1998, the European Association of Consultation Liaison Psychiatry and Psychosomatics (EACLPP) was inaugurated, focussing on CL Psychiatry and Psychosomatics as well as Integrated Care [12]. An important step forward was the European Consultation-Liaison Workgroup (ECLW) Collaborative Study [13,14]. In 2005, the European Network on Psychosomatic Medicine (ENPM) was founded as an additional forum to co-ordinate common actions, especially in primary care and specialities [15]. Finally, in 2012, the European Association of Psychosomatic Medicine (EAPM) was founded as a unifying entity in response to reorientation of European psychosomatic development to combine ideas of ECPR, EACLPP, and ENPM. Since that time, the EAPM has been the pre-eminent professional European society to strengthen the collaboration between researchers, practitioners, and teachers in the field.
There are large differences between the health care systems of the participating countries, in particular concerning CL mental health services. The organization and structure of CL mental health care differs widely between countries and often even between hospitals within the same country. CL mental health care is delivered by different mental health disciplines such as Psychiatry, Psychosomatic Medicine, or Psychology. Who delivers CL mental health care depends on the organization of national medical health care services and local hospital structures, and as a result of how these services have organically arisen in different health contexts. In some larger hospitals there may be several CL services of different disciplines providing CL mental health care. This may include services and interventions which depend on patient needs and local service requirements. During the COVID-19 pandemic close collaboration between different services could be helpful. Typically, psychiatric, psychological, and psychosomatic CL services deliver specialized mental health care for patients in a variety of medical settings (e.g., they are mainly situated on wards, but also in emergency units, and in outpatient clinics) and medical departments (e.g., internal medicine, geriatrics, oncology, and surgery) [16]. In line with the bio-psycho-social model [17], they provide a mix of consultation, liaison, specialist psychological interventions, training, and research, provided by multidisciplinary teams [9]. These services are critical in managing the interface between physical and mental health, promoting the integration of mental and physical health care, and in training and supporting general hospital staff [18]. In summary, CL services are structurally heterogeneous and care structures vary between countries [9,19]. All services faced rising and new demands as a consequence of the COVID-19 pandemic, and little is known of their response to this challenge within the framework of their health care system and CL service structure.
The goal of our project was to describe the efforts made in Europe, parts of Canada and Iran in COVID-psyCare in general hospitals, and to learn from the experience gained so far, informing future developments. The objective of this study was to expand the collection of information on three research questions that we previously investigated in the DACH region [9] across and beyond Europe:
-
(1)
“to describe the COVID-psyCare structures implemented by psychosomatic, psychiatric, and psychological CL services,
-
(2)
to review specific services aimed at patients, relatives, and staff, and
-
(3)
to elucidate emerging needs for co-operation, networking, and service development [9].”
2. Materials and methods
2.1. Study design, setting, participants, and ethical approval
We undertook a cross-sectional multinational online survey in eleven European countries (Belgium, Finland, France, Greece, Ireland, Italy, Norway, Poland, Portugal, Spain, and the United Kingdom), Iran, and parts of Canada (Ontario and Quebec). The study was led by a steering group consisting of the spokespersons of the working group consultation and liaison psychosomatics of the German College of Psychosomatic Medicine (DKPM) and the German Society for Psychosomatic Medicine and Medical Psychotherapy (DGPM) (RS, BS, FV) together with representatives from Austria (CF), and Switzerland (CH) in consultation with the EAPM. The interest in participating in the multinational survey was solicited via the EAPM mailing list. There was a significant response across and beyond Europe: 11 European countries outside of the DACH region, Iran, and parts of Canada decided to participate in an extension of the COVID-19 survey among psychosocial CL services [9]. From each participating country, one or two national co-ordinators were nominated. A contact person from the steering group was designated for each country. The survey was reconciled with the respective national professional societies, and relevant working and interest groups (see Table S1). The exact number of CL mental health services was unknown in most countries. Nevertheless, together with the participating professional societies, we aimed to provide an estimate of the number of services to which the survey could be sent out (see Table S1, [43]).
We aimed to contact the heads of all CL mental health services in general hospitals included in these networks via email to ask for their participation. The survey was answered by one main respondent per CL service. No data were collected regarding whether the main respondent was the head of the service or a co-worker of the service. The dissemination of the survey was supported by the national professional societies, and relevant working and interest groups. Emails were sent out via their email distribution lists, complemented by individual email contacts. Three reminder emails were sent via these lists. Each service was asked to nominate a qualified professional to provide the aggregated information once per service. The online survey was open from 11 June 2021 to 3 October 2021. Participation in the online survey was voluntary. Prior to participating in the survey, we obtained written informed consent from each of the participants. Participants had the option to withdraw from the survey at any time and without giving a reason.
We obtained written approvals, declarations, or statements from the responsible ethics committee in Basel (Ethics Committee of Northwest and Central Switzerland, EKNZ, Req-2020-00861, update May 20th, 2021), the site of the principal investigator (RS), where the data were stored and processed, and from each of the participating countries (see Table S1). We registered the study on ClinicalTrials.gov (NCT04753242).
2.2. Study questionnaire
A questionnaire on COVID-psyCare provision by mental health CL services was developed based on the relevant literature [10,20], expert experience, and consultation with participating professional societies; the questionnaire was previously used in a survey of mental health CL services in Germany, Austria, and Switzerland [9]. It contains 25 questions on the following structural and process variables [9]:
-
(1)
“Characterization of participating hospitals as well as somatic and psychosocial care structures;
-
(2)
implementation and use of specific services or procedures of COVID-psyCare for the three target groups: patients, their relatives, and hospital staff;
-
(3)
maximum COVID-19 related burden of the psychosocial teams, as well as needs and requests for the future.”
The study questionnaire was translated from German into English, French, and Italian. Language harmonization and cultural adaptation followed a modified committee-based approach informed by the European Social Survey (ESS) Round 9 Translation Guidelines [21]. Methodological details of the translation procedure are provided as supplementary material.
Participants had the option of the language version to reply to. We provide the final English, French, and Italian versions of the survey as supplementary files to this article. In Poland and Portugal, the national co-ordinators prepared auxiliary versions of translations into Polish and Portuguese. Additional translations were sent in a separate file along with an e-mail inviting them to complete the survey. In Iran, the English version of the survey was used; invitation emails and the instructions for the participants were in Farsi.
2.3. Data management
We carried out the data collection with the online survey tool Questback EFS Fall 2019 / license model “Unipark” of Questback GmbH via the University of Basel. Data were stored in the Questback server park in Frankfurt / Main, Germany. This certified data center is subject to high data protection and security requirements according to ISO 27001. It is reliably protected from external access. Subsequently, the pseudonymized data were transferred, processed, and analyzed at the University Hospital Basel. Further processing of the anonymized data and interpretation of the results were carried out in co-operation with the steering group and the national coordinators.
2.4. Statistical methods
We conducted all analyses using the statistical software package IBM SPSS Statistics Version 25. We did not impute missing data. Absolute numbers were used to present categorical data, and means, standard deviation, and range were reported for continuous variables.
3. Results
3.1. Study response
The study flowchart is shown in Fig. 1 . There was an initial set of n = 385 responses from all participating countries. Ninety-three responses were excluded: n = 60 were records consisting only of missing values, indicating that the link was opened, but no questions were answered; n = 33 were filled in twice by the same CL service; in this case, we took the most complete record. A further = 33 records were excluded from the analyses because the structure of the institution did not match the survey, and so filling out the survey was usually terminated during characterization of the service within the first six questions. The final dataset contained n = 259 responses that could be included in the analyses.
Fig. 1.
Study flow chart.
3.2. Characterization of participating hospitals and CL services
The description of the n = 259 participating CL services included in the analyses is shown in Table 1 . Data were available from 28% of CL services based on an estimated denominator of 885 CL services in total. Available data from CL services differed widely between countries from 11% (Spain) to 88% (Norway). Regarding the type of hospital, 116 (45%) were tertiary, 90 (35%) secondary, and 53 (21%) primary hospitals. According to hospital ownership, 237 (91%) of the hospitals were in public, 13 (5%) in private, and 6 (2%) in non-profit ownership. The number of hospital beds was between 250 and 999 beds in 157 (61%), below 250 beds in 52 (20%), and over 1000 beds in 50 (19%) of the hospitals. According to provided data, a psychiatric CL service was available in 225 (87%), a psychological service in 133 (51%), a psychosomatic service in 92 (36%), and other CL services in 25 (10%) hospitals. The professional perspective this survey was answered from was in 198 (76%) of the cases classified as Psychiatry, in 165 (74%) as Psychosomatic Medicine, in 26 (10%) as Psychology, in 20 (8%) as Child and Adolescent Psychiatry, and in 13 (5%) as Medical Psychology.
Table 1.
Sample descriptives.
| Total (n = 259) |
Belgium (n = 17) |
Finland (n = 10) |
France (n = 40) |
Greece (n = 19) |
Ireland (n = 3) |
Italy (n = 15) |
Norway (n = 7) |
Poland (n = 8) |
Portugal (n = 46) |
Spain (n = 12) |
United Kingdom (n = 30) |
Canada (n = 13) |
Iran (n = 39) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated overall number of respective CL services | 925 | 50 (Flanders) | 34 | 84 | 90 | 15 | 101 | 8 | 22 | 126 | 106 | 217 | 27 (Ontario 15 Quebec 12) |
45 |
| Data available from CL services (%) | 28.0 | 34.0 | 29.4 | 47.6 | 21.1 | 20.0 | 14.9 | 87.5 | 36.4 | 36.5 | 11.3 | 13.8 | 48.1 | 86.7 |
| Type of hospital n (%) | ||||||||||||||
| Primary hospital | 53 (20.5) | 5 (29) | 2 (20) | – | 2 (11) | – | 6 (40) | 1 (14) | – | 21 (46) | 2 (17) | 3 (10) | 2 (16) | 4(10) |
| Secondary hospital | 90 (34.7) | 6 (35) | 6 (60) | 8 (20) | 6 (32) | 1 (33) | 8 (53) | 4 (57) | 5 (63) | 17 (37) | 4 (33) | 19 (63) | 2 (15) | 9 (23) |
| Tertiary hospital | 116 (44.8) | 6 (35) | 2 (20) | 32 (80) | 11 (58) | 2 (67) | 1 (7) | 2 (29) | 3 (37) | 8 (17) | 6 (50) | 8 (27) | 9 (69) | 26 (67) |
| Hospital ownership n (%) | ||||||||||||||
| Public providers | 237 (91.1) | 8 (47.1) | 10 (100) | 36 (90.0) | 18 (94.7) | 3 (100) | 15 (100) | 7 (100) | 8 (100) | 41 (89.1) | 11 (91.7) | 30 (100) | 12 (92.3) | 37 (94.9) |
| Private ownership | 13 (5.0) | 6 (35.3) | – | – | – | – | – | – | – | 5 (10.9) | 1 (8.3) | – | 1 (7.7) | |
| Non-profit ownerhip | 6 (2.3) | 2 (11.8) | – | 3 (7.5) | – | – | – | – | – | – | – | – | – | 1 (2.6) |
| Orther ownership | 3 (1.3) | – | – | 1 (2.5) | 1 (5.3) | – | – | – | – | – | – | – | – | 1 (2.6) |
| Number of hospital beds | ||||||||||||||
| Number of beds of the hospitals, mean (min-max, SD, sum) | 654.5 (0–5362, 581.1, 169′515) | 631.9 (0–1200, 319,1, 10′743 | 378.9 (0–1142, 350,3, 3′789) | 1193.9 (150–5362, 1030,1, 47′754) | 451.8 (22–800, 253,3, 8′585) | 560.0 (180–1000, 423,3, 1′680) | 573.3 (0–1213, 482.1, 8′600) | 1026.9 (700–1870, 401,1, 7′188) | 631.1 (88–1161, 399.0, 5′049) | 513.1 (0–1850, 341.8, 23′603) | 715.4 (180–1080, 251.6, 8′585) | 771.9 (0–2500, 509.6, 23′158) | 477.8 (40–800, 224.8, 5′821) | 383,6 (25–1300, 280.6, 14′960) |
| <250 | 52 (20.1) | 2 (11.8) | 4 (40.0) | 2 (5.0) | 5 (26.3) | 1 (33.3) | 6 (40.0) | 1 (12.5) | 9 (19.6) | 1 (8.3) | 3 (10.0) | 2 (15.4) | 16 (41.0) | |
| 250–999 beds | 157 (60.6) | 12 (70.6) | 5 (50.0) | 19 (47.5) | 14 (73.7) | 1 (33.3) | 5 (33.3) | 3 (42.9) | 4 (50.0) | 33 (71.7) | 9 (75.0) | 2 (66.7) | 11 (84.6) | 21 (53.9) |
| ≥ 1′000 beds | 50 (19.3) | 3 (17.8) | 1 (10.0) | 19 (47.5) | – | 1 (33.3) | 4 (26.7) | 4 (57.1) | 3 (37.5) | 4 (8.7) | 2 (16.7) | 7 (23.3) | – | 2 (5.1) |
| Psychosocial services available in the hospital (multiple answers possible) n (%) | ||||||||||||||
| Psychiatric CL service | 225 (86.9) | 16 (94.1) | 9 (90.0) | 37 (92.5) | 19 (100) | – | 13 (86.7) | 6 (85.7) | 8 (100) | 39 (84.8) | 12 (100) | 26 (86.7) | 10 (76.9) | 27 (69.2) |
| Psychological CL service | 133 (51.4) | 10 (58.8) | 3 (30.0) | 6 (15.0) | 12 (63.2) | 2 (66.7) | 10 (66.7) | 3 (42.9) | 6 (75.0) | 41 (89.1) | 6 (50.0) | 13 (43.3) | 3 (23.1) | 18 (46.2) |
| Psychosomatic CL service | 92 (35.5) | 7 (41.2) | 6 (60.0) | 11 (27.5) | 7 (36.8) | 2 (66.7) | 2 (13.3) | 5 (71.4) | 4 (50.0) | 9 (19.6) | 3 (25.0) | 9 (30.0) | 7 (53.8) | 20 (51.3) |
| Other psychosocial services | 25 (9.7) | 1 (5.9) | 1 (10.0) | 10 (25.0) | 1 (5.3) | – | – | 1 (14.3) | 4 (8.7) | – | 4 (13.3) | 2 (15.4) | 1 (2.6) | |
| Professional perspective this survey was answered from (multiple answers possible) n (%) | ||||||||||||||
| Psychiatry | 198 (76.4) | 11(64.7) | 3 (30.0) | 7 (17.5) | 14 (73.7) | – | 12 (80.0) | – | 7 (87.5) | 7 (15.2) | 7 (58.3) | 1 (3.3) | 3 (23.1) | 17 (43.6) |
| Psychosomatic Medicine | 165 (63.7) | 9 (52.9) | 9 (90.0) | 37 (92.5) | 10 (52.6) | 2 (66.7) | 15 (100) | 7 (100) | 5 (62.5) | 17 (37.0) | 9 (75.0) | 28 (93.3) | 10 (76.9) | 22 (56.4) |
| Psychological service / Psychological department | 26 (10.0) | – | – | 1 (2.5) | – | – | 2 (13.3) | – | 3 (37.5) | 15 (32.6) | 2 (16.7) | – | – | 3 (7.7) |
| Child and Adolescent Psychiatry and Psychosomatics | 20 (7.7) | – | – | 5 (12.5) | – | – | 1 (6.7) | – | 1 (12.5) | 7 (15.2) | 2 (16.7) | 1 (3.3) | – | 3 (7.7) |
| Medical Psychology | 13 (5.0) | – | – | 2 (5.0) | – | – | – | – | 3 (37.5) | 6 (13.0) | – | – | – | 2 (5.1) |
| Other | 17 (6.6) | – | – | 3 (7.5) | 1 (5.3) | 1 (33.3) | – | – | – | 5 (10.9) | 2 (16.7) | – | 1 (7.7) | 3 (7.7) |
3.3. Physical care of COVID-19 patients: involvement and structures
Table 2 shows the physical care intensity of COVID-19 patients. The maximum level of involvement of the hospitals in the physical health care of COVID-19 patients since the beginning of the pandemic was strong with a mean of 4.0 on a 6 point Likert scale from 0 = not at all to 5 = very strongly. Most countries reported a mean of at least 4.0. Lower intensities were reported from the three Northern European Countries Finland (1.6), Norway (2.6), and Ireland (3.0). The extent to which the hospitals were maximally occupied regarding the somatic care of COVID-19 patients was high with a mean of the total sample of 4.0 on the same Likert scale. Most countries reported means of around 4, again with the exception of Finland (1.5) and Norway (2.9).
Table 2.
Hospital care provided for COVID-19 patients.
| Total (n = 259) |
Belgium (n = 17) |
Finland (n = 10) |
France (n = 40) |
Greece (n = 19) |
Ireland (n = 3) |
Italy (n = 15) |
Norway (n = 7) |
Poland (n = 8) |
Portugal (n = 46) |
Spain (n = 12) |
United Kingdom (n = 30) |
Canada (n = 13) |
Iran (n = 39) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maximum level of involvement of the hospitals in the somatic care of COVID-19 patients since the beginning of the pandemic (0 = not at all - 5 = very strongly) mean (SD/range) |
4.0 (1.4/ 0–5) |
4.0 (1.6/ 0–5) |
1.6 (1.3/ 0–4) |
4.4 (1.0/ 1–5) |
4.0 (1.3/ 1–5) |
3.0 (2.0/ 1–5) |
4.0 (1.5/ 0–5) |
2.6 (2.0/ 0–5) |
4.3 (0.7/ 3–5) |
4.5 (0.8/ 1–5) |
4.4 (1.0/ 2–5) |
3.9 (1.7/ 0–5) |
4.2 (1.2/ 1–5) |
4.1 (1.3/ 0–5) |
| Extent the hospitals were maximally occupied regarding the somatic care of COVID-19 patients (0 = not at all - 5 = very strongly) mean (SD/ range) |
4.0 (1.3/ 0–5) |
4.2 (0.9/ 1–5) |
1.5 (1.2/ 0–4) |
4.2 (1.2/ 1–5) |
4.0 (1.3/ 1–5) |
4.0 (1.7/ 2–5) |
4.2 (1.5/ 0–5) |
2.9 (1.7/ 1–5) |
3.9 (1.4/ 2–5) |
4.3 (1.0/ 1–5) |
4.4 (0.8/ 3–5) |
3.9 (1.4/ 0–5) |
3.6 (1.7/ 1–5) |
4.0 (1.2/ 1–5) |
| Has any COVID-19 related psychosocial care been provided at your hospital? yes; n (%) | 222 (85.7) | 16 (94.1) | 7 (70.0) | 40 (100) | 14 (73.7) | 3 (100) | 15 (100) | 6 (85.7) | 6 (75.0) | 42 (91.3) | 11 (91.7) | 23 (76.7) | 11 (84.6) | 28 (71.8) |
Fig. S1 shows the structures developed for the physical health care of COVID-19 patients. Regarding hospital wards and units for the treatment of COVID-19 patients (Fig. S1A), 93% of the hospitals reported designated wards for COVID-19 patients, 81% reported specially designated intensive care beds, and 68% reported designated wards for suspected cases. Fig. S1B shows newly established special hospital structures for the somatic care related to COVID-19.
3.4. COVID-psyCare in general hospitals: establishment, structures and burden on the psychosocial teams
222 of the 259 CL services (86%) reported that in their hospital mental health care was provided in connection with COVID-19, while 37 CL services (14%) provided no specific COVID-psyCare (Table 3 ). In all countries, at least 70% of the CL services offered COVID-psyCare. The following information refers to the 222 CL services which did provide COVID-psyCare.
Table 3.
COVID-psyCare in general hospitals: Co-operation structures, maximum burden of the pandemic on the psychosocial teams, and percentage of time utilization for target groups.
| Total (n = 222) |
Belgium (n = 16) |
Finland (n = 7) |
France (n = 40) |
Greece (n = 14) |
Ireland (n = 3) |
Italy (n = 15) |
Norway (n = 6) |
Poland (n = 6) |
Portugal (n = 42) |
Spain (n = 11) |
United Kingdom (n = 23) |
Canada (n = 11) |
Iran (n = 28) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Establishment of co-operation structures for psychosocial support; yes; n (%) | 192 (86.5) | 13 (81.3) | 5 (71.4) | 35 (87.5) | 11 (78.6) | 2 (66.7) | 12 (80.0) | 5 (83.3) | 6 (100) | 38 (90.5) | 10 (90.9) | 21 (91.3) | 8 (72.7) | 26 (92.9) |
| Clinical psychology | 134 (60.4) | 10 (62.5) | – | 20 (50.0) | 9 (64.3) | 2 (66.7) | 12 (80.0) | 3 (50.0) | 5 (83.3) | 33 (78.6) | 7 (63.6) | 14 (60.9) | 5 (45.5) | 14 (50.0) |
| Psychiatry (community and/or inpatient) | 123 (55.5) | 7 (43.8) | 3 (42.9) | 17 (42.5) | 8 (57.1) | 2 (66.7) | 10 (66.7) | 3 (50.0) | 4 (66.7) | 32 (76.2) | 7 (63.6) | 6 (26.1) | 5 (45.5) | 19 (67.9) |
| Psychosomatic Medicine / CL Psychiatry |
121 (54.5) | 8 (50.0) | 4 (57.1) | 28 (70.0) | 6 (42.9) | 2 (66.7) | – | 3 (50.0) | 4 (66.7) | 19 (45.2) | 7 (63.6) | 17 (73.9) | 6 (54.5) | 17 (60.7) |
| Nursing team | 81 (36.5) | 4 (25.0) | – | 11 (27.5) | 5 (35.7) | 2 (66.7) | 5 (33.3) | 3 (50.0) | 3 (50.0) | 11 (26.2) | 5 (45.5) | 11 (47.8) | 6 (%4.5) | 15 (53.6) |
| Social services | 69 (31.1) | 6 (37.5) | – | 6 (15.0) | 6 (42.9) | 1 (33.3) | 5 (33.3) | 3 (50.0) | 1 (16.7) | 16 (38.1) | 7 (63.6) | 4 (17.4) | 6 (54.5) | 8 (28.6) |
| Spiritual care | 42 (18.9) | 4 (25.0) | – | 4 (10.0) | 1 (7.1) | 1 (33.3) | 1 (6.7) | 3 (50.0) | 2 (33.3) | 7 (16.7) | 1 (9.1) | 11 (47.8) | 5 (45.5) | 3 (10.7) |
| Palliative care | 41 (18.5) | 2 (12.5) | – | 11 (27.5) | – | – | 1 (6.7) | 2 (33.3) | 1 (16.7) | 6 (14.3) | 1 (9.1) | 8 (34.8) | 2 (18.2) | 7 (25.0) |
| Psycho-oncology | 26 (11.7) | – | – | 7 (17.5) | 2 (14.3) | – | 1 (6.7) | 1 (16.7) | 1 (16.7) | 6 (14.3) | 2 (18.2) | 2 (8.7) | 1 (9.1) | 3 (10.7) |
| Has the pandemic task force of your hospital included psychosocial representation? yes; n (%) |
123 (55.4) | 9 (56.3) | 3 (42.9) | 16 (40.0) | 6 (42.9) | 1 (33.3) | 9 (60.0) | 4 (66.7) | 4 (66.7) | 25 (59.5) | 9 (81.8) | 8 (34.8) | 7 (63.6) | 22 (78.6) |
| Maximum burden of the COVID-19 pandemic on the psychosocial teams; (1 = not at all stressed - 10 = extremely stressed) mean (SD) |
7.0 (2.4) | 6.1 (2.0) | 4.3 (3.0) | 6.6 (2.8) | 7.0 (2.2) | 7.7 (0.6) | 7.5 (2.6) | 3.5 (2.1) | 6.5 (1.9) | 7.2 (2.5) | 8.0 (1.3) | 8.4 (1.3) | 7.5 (2.6) | 7.2 (2.1) |
| Percentage of time utilization for target groups; mean (SD; min - max) |
||||||||||||||
| Patients | 56.3 (27.1, 0–100) | 55.0 (22.3, 20–90) |
90.0 (14.1, 70–100) | 59.6 (23.0, 0–100) | 60.4 (23.3, 15–90) | 76.3 (24.7, 50–99) | 52.2 (29.8), 0–95 | 45.8 (40,3, 0–90) | 58.8 (15.5, 45–80) | 44.5 (27.9, 0–100) | 59.5 (6.9, 50–75) | 58.8 (31.3, 0–100) | 71.5 (23.8, 20–100) | 54.7 (26.5, 0–100) |
| Relatives | 14.6 (13.3, 0–60) | 19.7 (10.9, 0–40) |
3.0 (4.5, 0–10) |
14.7 (13.3, 0–50) | 17.1 (9.6, 2–30) | 13.3 (23.1, 0–40) | 19.9 (16.7, 0–50 | 11.8 (12.0, 0–30) | 15.0 (13.5, 5–35) | 16.5 (15.1, 0–50) | 19.5 (8.3, 10–30) | 7.6 (11.8, 0–50) | 9.0 (9.1, 0–20) |
13.5 (13.8, 0–60) |
| Staff members | 23.7 (20.8, 0–100) | 25.3 (20,9, 5–70) | 7.0 (10.1, 0–25) | 25–8 (20.4, 0–100) | 22.5 (19.0, 0–70) | 10.3 (9.5 (1−20) |
20.2 (18.2, 0–70) | 25.7 (32.1, 0–80) | 28.3 (11.1, 15–40) | 26.5 (22.1, 0–100) | 21.0 (8.4, 5–30) | 24.0 (27.2, 0–100) | 19.5 (17.9, 0–60) |
24.0 (21.0, 0–70) |
In these 222 CL services, 192 (87%) reported that additional co-operation structures had been implemented within the hospital for psychosocial support in the context of the COVID-19 pandemic. The partners involved in these co-operative structures were (for the whole sample) in descending order: Clinical Psychology (60%), Psychiatry (community and/or inpatient) (56%), Psychosomatic Medicine/CL Psychiatry (55%), the Nursing team (37%), Social services (31%), Spiritual care (19%), Palliative care (19%), and Psycho-oncology (12%).
123 (55%) of all CL services reported that the COVID-19 task force of the hospital included at least one mental health professional. This was the case in the task force, in descending order, in more than half of the hospitals in Spain, Iran, Norway, Poland, Italy, and Belgium, and in less than half of the hospitals in Greece, Finland, France, United Kingdom, and Ireland.
The maximum burden of the COVID-19 pandemic on the psychosocial teams in the individual countries was reported by the main respondent of the survey like all other data in the survey. This burden can be grouped into three severity levels. In descending order, this burden was high in the United Kingdom, Spain, Ireland, Italy, Canada, Iran, and Greece, and it was reported as medium in France, Poland, and Belgium, low in Finland, and Norway.
Regarding the established structures (multiple answers possible), 136 (61%) of the 222 CL services providing COVID-psyCare responded that existing care structures were refined, 99 (45%) had instituted new care structures, and 35 (16%) reported that their care structure had remained unchanged (Fig. S2A; see Table. 4 for detailed information concerning specific COVID-19 related care structures). Fig. S2B shows the maximum availability of psychosocial care for COVID-19 patients in terms of time (multiple answers possible).
Table 4.
Specific activities offered by the CL services providing COVID-psyCare (n = 222).
| Specific activities … |
Extent to which these activities have proven successful (0 = not at all to 5 = very strongly) |
|
|---|---|---|
| n (%) | mean (SD)1 | |
| … for patients | 135 (60.8) | |
| Liaison staff on COVID wards | 97 (43.7) | 3.6 (1.4) |
| Specific protocols / SOPs4 for common questions | 93 (41.9) | 3.3 (1.3) |
| COVID-19 telephone hotline | 91 (41.0) | 3.5 (1.5) |
| Consultation staff specifically for COVID-19 referrals | 84 (37.8) | 3.6 (1.3) |
| Aftercare services for patients with post-COVID syndrome | 74 (33.3) | 3.0 (1.5) |
| Psychosocial COVID-19 Care Team | 73 (32.9) | 3.3 (1.4) |
| COVID-19 outpatient clinic | 64 (28.8) | 2.9 (1.6) |
| Others | 24 (10.8) | 2.5 (1.8) |
| … for relatives | 85 (38.3) | |
| COVID-19 telephone hotline also for relatives | 64 (28.8) | 3.6 (1.4) |
| Specific counseling for relatives | 59 (26.6) | 3.6 (1.1) |
| Specific protocols / SOPs4 for supporting relatives | 52 (23.4) | 3.4 (1.4) |
| Others | 11 (5.0) | 3.6 (1.2)2 |
| … for staff | 171 (77.0) | |
| Consultation hours / counseling for staff | 132 (59.5) | 3.5 (1.3)3 |
| COVID-19 telephone hotline for staff | 112 (50.5) | 3.4 (1.4) |
| Case discussions on patient-related stressful situations | 103 (46.4) | 3.5 (1.3) |
| Team supervision / facilitated group exchange on how the corona situation is experienced as staff and in the team | 101 (45.5) | 3.5 (1.3) |
| Targeted work with team leaders/supervisors on helpful support measures for staff/teams | 78 (35.1) | 3.4 (1.2) |
| Creating relaxation opportunities for teams under high stress levels | 74 (33.3) | 3.1 (1.5) |
| Training in dealing with psychosocial stress of patients and relatives (recognition, communication, management) | 74 (33.3) | 2.9 (1.1) |
| Workshops to strengthen the resilience of staff (e.g. self-care / resource activation) | 73 (32.9) | 3.4 (1.4) |
| Others | 13 (5.9) | 2.8 (1.8) |
Generally range 0–5; 2 range 2–5; 3 range 1–5; 4 Standard operating procedures.
3.5. Target group specific services or procedures of COVID-psyCare
The specific activities of COVID-psyCare for the three target groups are shown in Tables 3, 4 and S2. Of the 222 CL services providing COVID-psyCare, 135 (61%) reported interventions for COVID-19 patients, 85 (38%) reported services for relatives of COVID-19 patients, and 171 (77%) reported additional COVID-19 related services for hospital staff (see Table S2). In regard to the percentage of time spent by the CL mental health team for COVID-psyCare, 56% (SD 27%) of the time was used for patient care, 15% (SD 13%) for relatives, and 24% (SD 20%) for staff (see Table 3). Table 4 shows in descending order the extent to which these target group specific services or procedures have proven successful. Table S2 shows the specific activities undertaken for the different target groups for the total sample, as well as for the single countries.
Table S3 shows the methods of communication with the different target groups about the COVID-psyCare services.
3.6. Needs and requests for the future development of COVID-psyCare
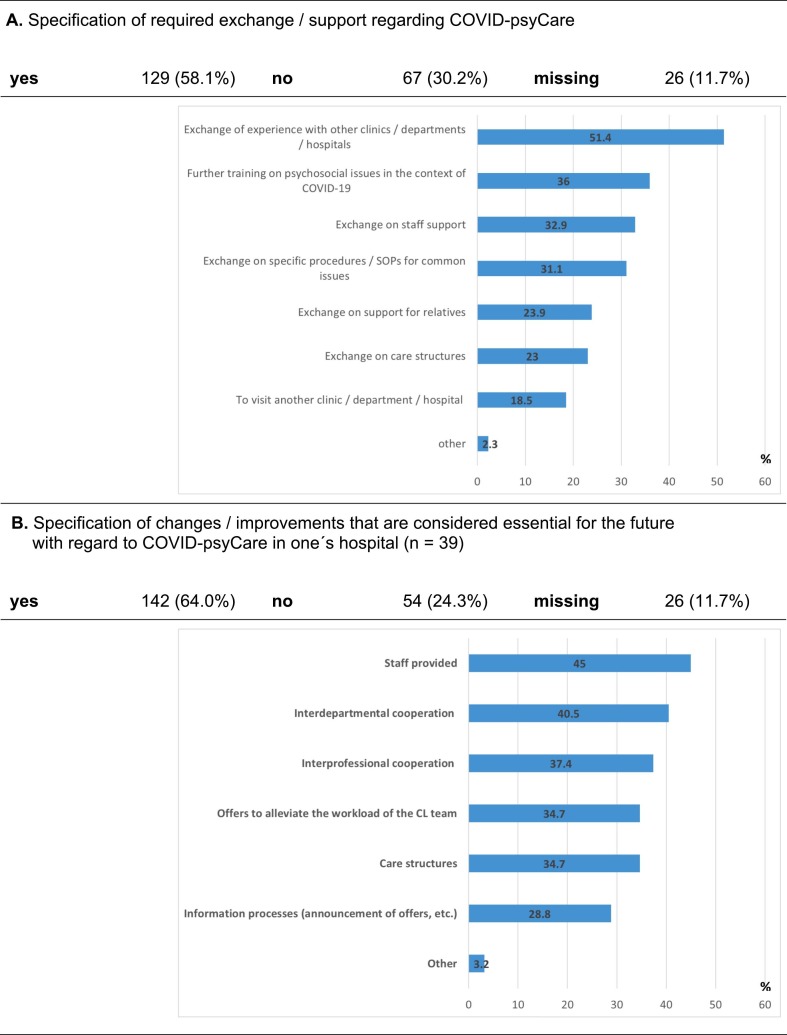
Needs and requests for the future of COVID-psyCare are depicted in Fig. 2 . Among the 222 CL services providing COVID-psyCare, 129 (58%) requested exchange/ support (Fig. 2A), 142 (64%) proposed changes/ improvements that they considered crucial for the future (Fig. 2B).
Fig. 2.
Needs and requests for the future.
4. Discussion
4.1. Key results
To our knowledge, this is the first multicenter CL services study across Europe, Iran, and parts of Canada, reporting on adaptations to mental health care as a reaction to a global health threat. Until now, little is known on how CL mental health services in general hospitals organized and provided psychosocial support and collaboration during the COVID-19 pandemic. Our multinational online survey of such services provided the following key results, referring to our three study objectives:
-
(1)
Health care in the COVID-19 pandemic in Europe, Iran and parts of Canada required the development of additional collaborative structures to meet the need of intensified interdisciplinary and interprofessional co-operation.
-
(2)
Out of 259 participating CL mental health services, 222 (86%) provided COVID-psyCare. Among them, 135 (61%) offered specific interventions for patients, 85 (38%) for relatives, and 171 (77%) for staff. In Europe, Iran, Ontario, and Quebec, COVID-19 drew attention to the hospital staff's psychosocial burden. However, regarding time resources appointed to COVID-psyCare, most of the time (56%) was used for psychosocial support of COVID-19 patients, corresponding to the core emphasis of CL services on patient care.
-
(3)
In Europe, Iran, Ontario, and Quebec, there is a high demand for exchange of information and experiences between CL services and for advances in mental health services in general hospitals in order to optimize present and future pandemic response.
4.2. Study response and characterization of participating hospitals and CL services
Across participating countries the need to quantify the number of existing mental health CL services became apparent: this number depends on the size of the country. The estimated number of mental health CL services and the observed response rates varied widely between 113% (Spain) and 88% (Norway) with a figure of 28% for the total sample. The study respondents showed heterogeneous characteristics, and the reported psychosocial care structures were diverse. In the participating countries health care systems and hospitals have developed a broad and heterogeneous landscape of psychosocial care structures. Mental health CL services available in the hospitals were mainly (87%) psychiatric, followed by psychological (51%), and psychosomatic (36%) CL services. Irrespective of this, the self-understanding of the participating CL services differed between the countries: a predominantly psychiatric self-understanding was reported by Poland and Greece; a more psychosomatic self-understanding by Norway, the United Kingdom, France, Finland, Canada, Spain, and Ireland; a psychiatric as well as psychosomatic by Belgium, Italy, and Iran; an additionally also psychological by Portugal.
4.3. Somatic care of COVID-19 patients
The involvement of the hospitals in mental health care of COVID-19 patients was high in most countries, with the exception of Finland, Norway, and Ireland. Notably, peak occupation of hospitals related to somatic health care of COVID-19 patients was lowest in Finland and Norway, in line with Finland and Norway experiencing rather modest relative numbers of COVID-19 infections and deaths, as compared to other European countries, along with mostly manageable burden of COVID-19 on the hospitals. In contrast, this burden was particularly high in the southern European countries of Italy, Portugal, and Spain, as well as in France and in the United Kingdom. In all these countries, hospitals developed new structures for the mental health care of COVID-19 patients.
4.4. Provision of COVID-psyCare in the general hospital
Up to the fourth wave of the COVID-19 pandemic, provision of COVID-psyCare was reported by 86% of participating CL services. Among these CL services, 87% stated that additional co-operation structures were established within the hospital for COVID-psyCare. These numbers are higher than those reported from the DACH-region (79% of the CL services provided psychosocial care in connection with COVID-19, 61% had established additional co-operation structures), indicating presumably on the one side a higher burden of the pandemic, on the other side more time passed since its beginning [9]. We emphasize that all results of the survey in the DACH region are difficult to compare with the results in this paper because the COVID pandemic has gone through multiple waves and these have required different responses.
The partners involved in the established co-operation structures were in descending order of frequency: Clinical Psychology, Psychiatry (community and/or inpatient), Psychosomatic Medicine/CL Psychiatry, the Nursing team, Social services, Spiritual care, Palliative care, and Psycho-oncology. This differs in particular from Germany, where there is a separate discipline and accordingly a more important role of Psychosomatic Medicine and Psychotherapy [9]. Generally, the findings emphasize that in dealing with the COVID-19 pandemic, interdisciplinary and interprofessional work has been intensified.
4.5. Target groups of COVID-psyCare for CL services
Regarding target groups of COVID-psyCare, in the multinational survey presented in this manuscript, as compared to the survey we previously conducted in the DACH region [9], considerably more CL services reported seeing patients (61% vs. 34%), relatives (38% vs. 25%), and staff (77% vs. 60%), while both surveys reported similar percentages of time utilization for patients (56% vs. 61%), relatives (15% vs. 12%), and staff (24% vs. 27%). The differences could be related to the different time points of the surveys and waves of the pandemic but to different health system structures, too. In both surveys, successful interventions for patients, their relatives, and for hospital staff members, which were perceived as highly beneficial, point to a broad scope of these services which may have increasingly emerged during the COVID-19 pandemic [3]. Furthermore, telepsychiatry options including telephone hotlines have gained importance during the pandemic [[22], [23], [24], [25]].
4.6. Specific services of COVID-psyCare for patients
In hospitalized COVID-19 patients, a high incidence of psychological distress, and neuropsychiatric symptoms have been reported [3,5,26]. Specific COVID-psyCare services for patients identified in our international survey were in descending order of frequency: liaison staff on COVID-19 wards, specific procedures/standard operating procedures (SOPs) for common questions, telephone hotlines, consultation staff specifically for COVID-19 referrals, aftercare services for patients with post-COVID syndrome, and a psychosocial COVID-19 care team. Most of these services were perceived as highly successful.
4.7. Specific services of COVID-psyCare for relatives of COVID-19 infected patients
In relatives of COVID-19 patients, illness-related, psychosocial, and hospital-related characteristics have been demonstrated to be risk factors for clinically relevant psychological distress: resilience was negatively correlated with anxiety, depression, and PTSD in relatives [1]. Specific COVID-psyCare services for relatives reported in our survey were in descending order: telephone hotlines, specific counseling, and specific procedures for supporting relatives. Generally, all services offered for relatives were perceived as highly successful.
4.8. Specific services of COVID-psyCare for hospital staff
On average 24% of the time committed to COVID-psyCare was directed towards staff. Specific services for hospital staff were reported by 77% of CL services providing COVID-psyCare. This is consistent with recent studies on the psychosocial burden, including increased depressive symptoms, anxiety, psychological distress, and poor sleep quality in hospital staff [5,20,[27], [28], [29]]. As a result, health care organizations implemented procedures to support institutional and individual resilience. It has been discussed that there might be concerns about a conflict of interest if mental health staff are seeing other staff members in a clinician/client relationship while also working as colleagues. Hence, it seems to be possible to find appropriate, mindful and acceptable ways of dealing with these concerns: According to the reports of respected consultation-liaison psychiatric organizations [3] and experts [4], as well as according to our own experiences, psychosocial CL services have been largely involved in the support of hospital staff. Based on our survey, CL services appear to be suitable structures for providing adequate support to hospital staff, especially during times of crisis.
Specific services of COVID-psyCare for hospital staff reported in our survey were in descending order: counseling for staff, telephone hotlines for staff, case discussions on patient-related stressful situations, team supervision/facilitated group exchange on experience of the pandemic, work with team leaders on helpful support measures for staff/teams, creating relaxation opportunities for high-stress teams, training in dealing with psychosocial stress of patients and relatives, and workshops to strengthen resilience. All of these were reported as successful. Ideally, a stepped and integrated continuum of institutional and individual staff support should be established [25,[30], [31], [32]]. Due to positive effects on absenteeism and turnover, such coordinated programs may be cost-effective [33,34]. In some systems, problems may arise due to time spent on staff support not being chargeable. Although such services have low utilization rates - physicians use them less than nurses - informal contact with CL staff may increase interest in using them [3]. Furthermore, it could be expected that information about such services could have a positive impact on HCWs' mental health through the implicit acknowledgement of job stress it conveys. To establish the greatest foundation for healthy and productive work, measures need to be adapted to the demands of various categories of HCWs (e.g. gender, age, family and living situation, migrant background, frontline workers) [35].
Many of the same problems that apply to other HCWs are likely to apply to CL professionals as well: fear of becoming infected or of infecting others, traumatizing experiences during CL work, and burnout [3,9,36,37]. On a scale of 1 (“not at all stressed”) to 10 (“extremely stressed”), this study reported a substantial mean score of 7.0 for the greatest impact of the COVID-19 pandemic on psychosocial teams [9]. In descending order, this burden was high in the United Kingdom, Spain, Ireland, Italy, Canada, Iran, and Greece, medium in France, Poland, and Belgium, low in Finland, and Norway. This may reflect the impact of the COVID-19 pandemic on the different countries.
4.9. Need for further exchange, requests for the future, and research implications
In our multinational study more CL services expressed wishes for mutual exchange and support regarding COVID-psyCare (58%), as well as suggestions for future changes or improvements that they considered essential (64%). This underlines the high international need for communication on COVID-psyCare in general hospitals across psychiatric, psychological, and psychosomatic CL services.
The following are the key issues raised for this exchange of experience with other clinics/departments/hospitals: exchange on further training on psychosocial issues in the context of COVID-19; exchange on staff support; on specific procedures/SOPs for common issues; on support for relatives; on care structures; and finally to visit another clinic/department/hospital.
In the context of COVID-19, the following improvements were considered essential in descending order for the future, with regard to CL services: the provision of more staff for psychosocial CL services, interdepartmental and interprofessional co-operation, offers to alleviate the workload of the CL team, better care structures, improvement of information processes.
Further studies should evaluate the use of mental health professionals on COVID-19 cohort wards and specially designated ICU units/beds.
In addition, post-acute COVID-19 symptoms, frequently referred to as ‘long COVID’, raise new challenges for CL services regarding the integration of psychosocial care in the management of these persistent symptoms [[38], [39], [40]].
4.10. Strengths and limitations
A strength of our study is that it provides naturalistic health services research data. However, it has several limitations. First, due to significant heterogeneity of health care systems and organizational models of CL mental health services, comparability between these services between countries is limited. Second, when interpreting the findings of this study, a selection bias must be considered: since the invitation to the study had been made via the EAPM mailing list, more psychosomatically oriented colleagues may have been reached as compared to psychiatric and psychological CL services despite structured efforts to reach as many psychiatric, psychosomatic and psychological CL services as possible. Third, when interpreting the fact that approximately 86% of participating CL services have reported the provision of specific COVID-psyCare whereas approximately 14% did not provide such care, it needs to be considered that there were also differences between the hospitals regarding the reported level of involvement in the somatic care of COVID-19 patients. Fourth, it became clear that accurate national denominators on the number of CL services per country are not available and that obtaining an estimate was difficult; it is often unknown what catchment areas are served by the CL services; thus the relation with the population served is not always clear; furthermore, the structure and form of organized CL mental health services is heterogeneous and the level and features of organization of the CL networks and scientific societies is different between countries (e.g. [41,42]): this results in a varying accuracy of the estimated number of CL services per country as well as of the achieved response rates. Fifth, the response rate of our study was limited at 28% of surveyed CL services; this is a good percentage for mail surveys, but nevertheless is a limitation as it means that overall, the CL services that could be reached with our survey may not fully represent the entire field; thus, the generalizability of our results may be restricted [9]. Sixth, only one representative of the respective CL service answered the questionnaire as per study design, and this might have brought subjective bias to the response [9]. Seventh, data quality was affected by missing answers. Eighth, the specific models of care substantially varied across and even within countries, so that a country specific, thorough description would have gone beyond the scope of this manuscript. Ninth, our survey period from 06/2021 to 10/2021 met a similar 4-wave incidence pattern, yet still somewhat different situation of COVID-19 infections in the different countries which may have influenced study results (a comparison of COVID-19 infection numbers and death rates during the different waves of the pandemic within the survey period can be for example found in: https://coronavirus.jhu.edu/map.html) [8]. Services might also have been further modified and optimized after the end of this survey in October 2021 [9]. Finally, one of the strengths of this study also implies a limitation: The number of respondents within Europe and the possibility for participants to be compared in the same snapshot in time seems particularly useful for the European context. However, despite the additional participation of Iran and parts of Canada, the conclusions from this study cannot be generalized to other countries and other regions in the world where experiences with COVID-19 in the general hospital setting may have been vastly different.
5. Conclusion
The COVID-19 pandemic has highlighted and exposed shortcomings in our health care systems. This study gives a cross sectional snapshot of the services being offered by CL mental health teams in Europe, Iran and parts of Canada. It provides self-reported information on success of newly implemented service procedures and COVID-19 related burden of the CL teams. The findings of this multinational survey may stimulate CL mental health services considering an integrated and comprehensive health care approach to address challenges of the COVID-19 and potential future pandemics in general hospitals. Eighty-six percent of participating CL services provided COVID-psyCare for patients, their relatives or staff. In particular, those interventions that are typically associated with the liaison function of CL services seemed to be perceived as most useful. With health care personnel reporting higher levels of psychosocial strain, focusing on staff support will be of increasing relevance. Future development of COVID-psyCare internationally warrants intensified intra- and inter-institutional exchange and co-operation.
Funding
No external funding was received for this study.
Authors' contribution
-
•
RS, BS, CF, CH, FV, and GM contributed to the conception and design of the study.
-
•
RS, BS, CF, CH, FV, GM, and NR contributed to the development of the survey questionnaire.
-
•
RS, BS, CF, CH, FV, GM, VL, NR, SF, TDM, and CFC contributed to the translation of the survey.
-
•
GM, RS, and FV ensured clarifications on data protection. CFC contributed.
-
•
RS, CF, FV, CFC, VL, CL, MS, AMD, and WL took care of the necessary ethical approvals.
-
•
RS and CH arranged study registration.
-
•
GM and NR programmed the online survey. FV shared the invitation to participate in the study with national representatives and managed communication via the EAPM mailing list.
-
•
RS, BB, BS, CF, CH, FV, SS, CL, CFC, WL, GMDL, VL, AMD, MS, and UH contributed to the dissemination of the survey.
-
•
NR, GM, and BS organized the database.
-
•
BS performed the statistical analysis.
-
•
RS wrote the first draft of the manuscript.
-
•
WL and CFC advised on survey design and methods, WL contributed the UK denominator data.
-
•
CH wrote sections of the manuscript.
-
•
All authors contributed to the interpretation of the data, manuscript revision, read, and approved the final manuscript.
Declaration of Competing Interest
All other authors declare that they have no competing financial interests related to this study.
Acknowledgements
The authors thank the EAPM for creating and maintaining the network for international exchange facilitating the formation of the consortium that has carried out the present study. Furthermore, the authors would like to express their gratitude to the professional societies who participated. Many thanks to Sabrina Elia, Roger Moser-Starck, Jean-Claude Bertrand, André Lelièvre, Chantale Montigny, Rahel Ghiorgis-Wolde, and Pierre Verrier for proofreading the translation of the survey into French and Italian as CL experts. Thank you very much to Tabea Rocco for her assistance in editing the manuscript. We are very grateful to all participating colleagues and CL services.
Glossary of abbreviations and acronyms
- CL services
Consultation and liaison services
- COVID-19
Coronavirus disease 2019
- COVID-psyCare
COVID-19 related psychosocial care
- DGPM
German Society for Psychosomatic Medicine and Medical Psychotherapy
- DKPM
German College for Psychosomatic Medicine
- EACLPP
European Association of Consultation Liaison Psychiatry and Psychosomatics
- EAPM
European Association of Psychosomatic Medicine
- ECLW
European Consultation-Liaison Workgroup
- ECPR
European Conference on Psychosomatic Research
- EKNZ
Ethikkommission Nordwest- und Zentralschweiz (Ethics Committee of Northwest and Central Switzerland)
- HCW
Health care worker
- ICU
Intensive care unit
- PPE
Personal protection equipment
- PTSD
Posttraumatic stress disorder
- SD
Standard deviation
- SOP
Standard operation procedure
- UK
United Kingdom
- WHO
World Health Organization
- 95% CI
95% Confidence interval
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychores.2023.111183.
Appendix A. Supplementary data
Supplementary Tables and Figures
Study information and survey questionnaire in English
Study information and survey questionnaire in French
Study information and survey questionnaire in Italian
Methodological details of the translation procedure
References
- 1.Vincent A., Beck K., Becker C., Zumbrunn S., Ramin-Wright M., Urben T., Quinto A., Schaefert R., Meinlschmidt G., Gaab J., Reinhardt T., Bassetti S., Schuetz P., Hunziker S. Psychological burden in patients with COVID-19 and their relatives 90 days after hospitalization: a prospective observational cohort study. J. Psychosom. Res. 2021;147 doi: 10.1016/j.jpsychores.2021.110526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck K., Vincent A., Becker C., Keller A., Cam H., Schaefert R., Reinhardt T., Sutter R., Tisljar K., Bassetti S., Schuetz P., Hunziker S. Prevalence and factors associated with psychological burden in COVID-19 patients and their relatives: a prospective observational cohort study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapiro P.A., Brahmbhatt K., Caravella R., Erickson J., Everly G., Giles K., Gopalan P., Greenspan H., Huijón R.M., Key R.G., Kroll D., Prince E., Rabinowitz T., Saad-Pendergrass D., Shalev D. Report of the academy of consultation-liaison psychiatry task force on lessons learned from the COVID-19 pandemic: executive summary. J. Acad. Consult. Liaison Psychiatry. 2021;62:377–386. doi: 10.1016/j.jaclp.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horn M., Granon B., Vaiva G., Fovet T., Amad A. Role and importance of consultation-liaison psychiatry during the Covid-19 epidemic. J. Psychosom. Res. 2020;137 doi: 10.1016/j.jpsychores.2020.110214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iftekhar E.N., Priesemann V., Balling R., Bauer S., Beutels P., Valdez A. Calero, Cuschieri S., Czypionka T., Dumpis U., Glaab E., Grill E., Hanson C., Hotulainen P., Klimek P., Kretzschmar M., Krüger T., Krutzinna J., Low N., Machado H., Martins C., McKee M., Mohr S.B., Nassehi A., Perc M., Petelos E., Pickersgill M., Prainsack B., Rocklöv J., Schernhammer E., Staines A., Szczurek E., Tsiodras S., Van Gucht S., Willeit P. A look into the future of the COVID-19 pandemic in Europe: an expert consultation. Lancet Reg. Health Eur. 2021;8 doi: 10.1016/j.lanepe.2021.100185. 100185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carroll W.D., Strenger V., Eber E., Porcaro F., Cutrera R., Fitzgerald D.A., Balfour-Lynn I.M. European and United Kingdom COVID-19 pandemic experience: the same but different. Paediatr. Respir. Rev. 2020;35:50–56. doi: 10.1016/j.prrv.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johns Hopkins University & Medicine Johns Hopkins Coronavirus Resource Center. 2022. https://coronavirus.jhu.edu (accessed 7 April 2022)
- 9.Schaefert R., Stein B., Meinlschmidt G., Roemmel N., Huber C., Hepp U., Saillant S., Fazekas C., Vitinius F. COVID-19-related psychosocial care in general hospitals: results of an online survey of psychosomatic, psychiatric, and psychological consultation and liaison services in Germany, Austria, and Switzerland. Front. Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.870984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science, lancet. Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deter H.C., Orth-Gomér K., Wasilewski B., Verissimo R. The European Network on Psychosomatic Medicine (ENPM) – history and future directions. Biopsychosoc. Med. 2017;11:3. doi: 10.1186/s13030-016-0086-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leentjens A.F.G., Rundell J.R., Diefenbacher A., Kathol R., Guthrie E. Psychosomatic medicine and consultation-liaison psychiatry: scope of practice, processes, and competencies for psychiatrists working in the field of CL psychiatry or psychosomatics. [corrected] A consensus statement of the European Association of Consultation-Liaison Psychiatry and Psychosomatics (EACLPP) and [corrected] the Academy of Psychosomatic Medicine (APM). [corrected] Psychosomatics. 2011;52:19–25. doi: 10.1016/j.psym.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 13.Huyse F.J., Herzog T., Lobo A., Malt U.F., Opmeer B.C., Stein B., Creed F., Crespo M.D., Gardoso G., Guimaraes-Lopes R., Mayou R., van Moffaert M., Rigatelli M., Sakkas P., Tienari P. European consultation-liaison psychiatric services: the ECLW collaborative study. Acta Psychiatr. Scand. 2000;101:360–366. doi: 10.1034/j.1600-0447.2000.101005360.x. [DOI] [PubMed] [Google Scholar]
- 14.Huyse F.J., Herzog T., Lobo A., Malt U.F., Opmeer B.C., Stein B., de Jonge P., van Dijck R., Creed F., Crespo M.D., Cardoso G., Guimaraes-Lopes R., Mayou R., van Moffaert M., Rigatelli M., Sakkas P., Tienari P. Consultation-liaison psychiatric service delivery: results from a European study. Gen. Hosp. Psychiatry. 2001;23:124–132. doi: 10.1016/s0163-8343(01)00139-6. [DOI] [PubMed] [Google Scholar]
- 15.Deter H.C. Impressions from the 7th conference of the European Association of Psychosomatic Medicine (EAPM) - 7 years later, after the unification of European network of psychosomatic medicine (ENPM) and the European Association for Consultation Liaison Psychiatry and Psychosomatics (EACLPP) Psychother. Psychosom. Med. Psychol. 2020;70:46–48. doi: 10.1055/a-1080-3450. [DOI] [PubMed] [Google Scholar]
- 16.Stein B., Müller M.M., Meyer L.K., Söllner W. CL guidelines working group, psychiatric and psychosomatic consultation-liaison Services in General Hospitals: a systematic review and Meta-analysis of effects on symptoms of depression and anxiety. Psychother. Psychosom. 2020;89:6–16. doi: 10.1159/000503177. [DOI] [PubMed] [Google Scholar]
- 17.Engel G.L. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 18.Aitken P., Robens S., Emmens T. Strategic Clinical Network for Mental Health: Dementia and Neurological Conditions South West, England. first ed. 2014. Developing models for liaison psychiatry services-guidance. [Google Scholar]
- 19.Hopkins J., Cullum S., Sundram F. The state of play – the first national survey of consultation-liaison psychiatry services in New Zealand, Australas. Psychiatry. 2020;28:448–453. doi: 10.1177/1039856220908174. [DOI] [PubMed] [Google Scholar]
- 20.Weilenmann S., Ernst J., Petry H., Pfaltz M.C., Sazpinar O., Gehrke S., Paolercio F., von Känel R., Spiller T.R. Health care Workers’ mental health during the first weeks of the SARS-CoV-2 pandemic in Switzerland—a cross-sectional study. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.594340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harkness J.A. In: Cross-Cultural Survey Methods. Harkness J.A., van de Vijver F.J.R., Mohler P.Ph., editors. John Wiley & Sons; New York: 2003. Questionnaire translation; pp. 35–56. [Google Scholar]
- 22.Beran C., Sowa N.A. Adaptation of an academic inpatient consultation-liaison psychiatry service during the SARS-CoV-2 pandemic: effects on clinical practice and trainee supervision. J. Acad. Consult. Liaison Psychiatry. 2021;62:186–192. doi: 10.1016/j.psym.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funk M.C., Beach S.R., Shah S.B., Boland R. Consultation-liaison psychiatry in the age of COVID-19: reaffirming ourselves and our worth. Psychosomatics. 2020;61:571–572. doi: 10.1016/j.psym.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sánchez-González M.Á. The role of consultation-liaison psychiatry in the COVID-19 Pandemic. Prim. Care Companion CNS Disord. 2020;22 doi: 10.4088/PCC.20com02669. 20com02669. [DOI] [PubMed] [Google Scholar]
- 25.Bäuerle A., Jahre L., Teufel M., Jansen C., Musche V., Schweda A., Fink M., Dinse H., Weismüller B., Dörrie N., Junne F., Graf J., Skoda E.-M. Evaluation of the E-mental health mindfulness-based and skills-based “CoPE it” intervention to reduce psychological distress in times of COVID-19: results of a Bicentre longitudinal study. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.768132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.López-Atanes M., González-Briceño J.P., Abeal-Adham A., Fuertes-Soriano S., Cabezas-Garduño J., Peña-Rotella Á., Sáenz-Herrero M. Liaison psychiatry during the peak of the coronavirus pandemic: a description of referrals and interventions. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.555080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gainer D.M., Nahhas R.W., Bhatt N.V., Merrill A., McCormack J. Association between proportion of workday treating COVID-19 and depression, anxiety, and PTSD outcomes in US physicians. J. Occup. Environ. Med. 2021;63:89–97. doi: 10.1097/JOM.0000000000002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan N., Palepu A., Dodek P., Salmon A., Leitch H., Ruzycki S., Townson A., Lacaille D. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider J.N., Hiebel N., Kriegsmann-Rabe M., Schmuck J., Erim Y., Morawa E., Jerg-Bretzke L., Beschoner P., Albus C., Hannemann J., Weidner K., Steudte-Schmiedgen S., Radbruch L., Brunsch H., Geiser F. Moral distress in hospitals during the first wave of the COVID-19 pandemic: a web-based survey among 3,293 healthcare workers within the German network university medicine. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.775204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Everly G.S. Psychological first aid to support healthcare professionals. J. Patient Saf. Risk Manag. 2020;25:159–162. doi: 10.1177/2516043520944637. [DOI] [Google Scholar]
- 31.Everly G.S., Wu A.W., Cumpsty-Fowler C.J., Dang D., Potash J.B. Leadership principles to decrease psychological casualties in COVID-19 and other disasters of uncertainty. Disaster Med. Public Health Prep. 2020:767–769. doi: 10.1017/dmp.2020.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu A.W., Connors C., Everly G.S. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann. Intern. Med. 2020;172:822–823. doi: 10.7326/M20-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moran D., Wu A.W., Connors C., Chappidi M.R., Sreedhara S.K., Selter J.H., Padula W.V. Cost-benefit analysis of a support program for nursing staff. J. Patient Saf. 2020;16:e250–e254. doi: 10.1097/PTS.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 34.Sheppard K.N., Runk B.G., Maduro R.S., Fancher M., Mayo A.N., Wilmoth D.D., Morgan M.K., Zimbro K.S. Nursing moral distress and intent to leave employment during the COVID-19 pandemic. J. Nurs. Care Qual. 2022;37:28–34. doi: 10.1097/NCQ.0000000000000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jerg-Bretzke L., Kempf M., Jarczok M.N., Weimer K., Hirning C., Gündel H., Erim Y., Morawa E., Geiser F., Hiebel N., Weidner K., Albus C., Beschoner P. Psychosocial impact of the COVID-19 pandemic on healthcare workers and initial areas of action for intervention and prevention—the egePan/VOICE study. Int. J. Environ. Res. Public Health. 2021;18:10531. doi: 10.3390/ijerph181910531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Unützer J., Kimmel R.J., Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. 2020;19:130–131. doi: 10.1002/wps.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., Claassen J., Cornelius T., Derby L., Dong M., Givens R.C., Hochman B., Homma S., Kronish I.M., Lee S.A.J., Manzano W., Mayer L.E.S., McMurry C.L., Moitra V., Pham P., Rabbani L., Rivera R.R., Schwartz A., Schwartz J.E., Shapiro P.A., Shaw K., Sullivan A.M., Vose C., Wasson L., Edmondson D., Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bottemanne H., Gouraud C., Hulot J.-S., Blanchard A., Ranque B., Lahlou-Laforêt K., Limosin F., Günther S., Lebeaux D., Lemogne C. Do anxiety and depression predict persistent physical symptoms after a severe COVID-19 episode? A prospective study. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.757685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horn M., Fovet T., Vaiva G., D’Hondt F., Amad A. Somatic symptom disorders and long COVID: a critical but overlooked topic. Gen. Hosp. Psychiatry. 2021;72:149–150. doi: 10.1016/j.genhosppsych.2021.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sancak B., Ozer Agirbas U., Kilic C. Long COVID and its psychiatric aspects. J. Acad. Consult. Liaison Psychiatry. 2021;62:480–481. doi: 10.1016/j.jaclp.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrari S., Rigatelli M. General hospital psychiatry in Italy: an update. J. Psychosom. Res. 2006;60:217–218. doi: 10.1016/j.jpsychores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 42.Lobo A., Rabanaque I., Blanch J., Campos R., Ezquiaga E., Farré J.M., Gómez-Reino I., Marco C., Navío M., Ochoa E., Parramón G., Ventura T., Aguilar E.J., Artal J., Cuesta M., Devolx V.M., Espárrago G., Franco M.A., Hernández Fleta J.L., Martínez Jambrina J.J., Ortega M.Á., Palomo J., Pérez Costillas L., Roca M. The development of psychosomatic and liaison psychiatry units in Spain: a national enquiry. J. Psychosom. Res. 2019;125 doi: 10.1016/j.jpsychores.2019.109784. 109784. [DOI] [PubMed] [Google Scholar]
- 43.Lanvin V., Lemogne C. In: Psychosomatics during the Pandemic - 8th Annual Conference of EAPM. The European Association of Psychosomatic Medicine and CL Psychiatry, editor. 2021. Report of the first national survey of consultation-liaison psychiatry in France, Poster; p. 141. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Tables and Figures
Study information and survey questionnaire in English
Study information and survey questionnaire in French
Study information and survey questionnaire in Italian
Methodological details of the translation procedure