Abstract
Background:
Previous research suggests that, compared with regional anesthesia, general anesthesia is associated with increased odds of postoperative depressive disorders. No study has specifically evaluated the possible protective effect of neuraxial anesthesia for cesarean delivery on maternal mental health, compared with general anesthesia. This exploratory study was designed to test the hypothesis that general anesthesia for cesarean delivery is associated with increased odds of severe postpartum depression (PPD) requiring hospitalization, compared with neuraxial anesthesia.
Methods:
This retrospective cohort study included cesarean delivery cases performed in New York State hospitals between January 2006 and December 2013. Exclusion criteria were: having more than 1 cesarean delivery during the study period, residing outside of New York State, having a general anesthetic for other surgery or a delivery in the prior year or in the year after the index case. The primary outcome was the occurrence of PPD and the secondary outcomes were: 1) the composite of suicidal ideation or self-inflicted injury (i.e., suicidality), 2) anxiety disorders, and 3) post-traumatic stress disorders (PTSD). Primary and secondary outcomes were identified during the delivery hospitalization and up to 1 year post-delivery. Adjusted odds ratios (aORs) and 95% confidence interval (CIs) of adverse psychiatric outcomes associated with general anesthesia were estimated using propensity score matching.
Results:
Of the 428,204 cesarean delivery cases included, 34,356 had a general anesthetic (8.0%). Severe PPD requiring hospitalization was recorded in 1158 women (2.7 per 1000; 95% CI: 2.5-2.9); of them, 60% were identified during a readmission with a median of 164 days after discharge. Relative to neuraxial anesthesia, general anesthesia in cesarean delivery was associated with a 54% increased odds of PPD (aOR 1.54; 95% CI, 1.21-1.95) and a 91% increased odds of suicidal ideation or self-inflicted injury (aOR 1.91; 95% CI, 1.12-3.25). There was insufficient evidence in these data that general anesthesia was associated with anxiety disorders (aOR 1.37; 95% CI, 0.97-1.95) or PTSD (aOR 1.50; 95% CI, 0.50-4.47).
Conclusion:
General anesthesia for cesarean delivery is associated with increased odds of severe PPD requiring hospitalization, suicidal ideation, and self-inflicted injury. If confirmed, these preliminary findings underscore the need to avoid the use of general anesthesia for cesarean delivery whenever possible and to provide mental health screening, counselling, and other follow-up services to obstetric patients exposed to general anesthesia.
INTRODUCTION
Postpartum depression (PPD) is a serious maternal health issue in the United States. Its reported incidence has increased 7-fold in the past 15 years and it now affects up to 1 in 7 woman.1 PPD is associated with increased odds of severe maternal complications such as suicide and contributes significantly to preventable maternal mortality.2,3 Maternal suicide is the leading cause of direct maternal deaths from 6 weeks postpartum up to one year postpartum in the United Kingdom.4 In 2018, the American College of Obstetricians and Gynecologists (ACOG) released a new recommendation to have all women screened at least once for depression during the perinatal period.5 In 2019, the US Preventive Services Task Force recommended to refer women with at least one risk factor for depression to counseling such as those with a history of depression or certain socioeconomic risk factors (e.g., low income, young or single parenthood).6 To date, the strongest predictor of PPD is a past history of psychopathology and depression during the current pregnancy. However, few of these risk factors are readily modifiable. An additional approach to that of routine perinatal screening for PPD symptoms and interventions for women with known risk factors for PPD would be to identify actionable risk factors for PPD before depressive symptoms occur.
Two recent meta-analyses report that, compared with vaginal delivery, cesarean delivery is associated with an increased risk of PPD.7,8 Possible mechanisms include a delayed first interaction between the mother and her child and delayed first breastfeeding attempt, postpartum pain, and a mismatch between women’s expectations for childbirth and care provided (i.e., mother dissatisfaction).5 However, no study has examined the effect of the mode of anesthesia for cesarean delivery on the risk of PPD. General anesthesia for cesarean delivery might increase the risk of PPD because it is associated with a delayed first skin-to-skin interaction for the maternal-infant dyad, delayed first breastfeeding attempt, increased risk of persistent postoperative pain, and lower maternal satisfaction with anesthesia care.9,10 Therefore, we hypothesized that general anesthesia for cesarean delivery is associated with increased odds of severe postoperative depressive disorders compared with neuraxial anesthesia.
METHODS
The study protocol was granted exemption under 45 Code of Federal Regulation 46 (not human subjects research) by the Institutional Review Board of Columbia University Medical Center. The requirement for written informed consent was waived by the Institutional Review Board. The manuscript is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement and to the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement.
Data system
Hospital discharge records of the State Inpatient Database for New York were analyzed. State Inpatient Databases are part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality. They capture all inpatient discharges from non-federal acute care community hospitals, including tertiary and academic centers. They do not capture outpatient or emergency department visits. For each discharge, the New York State Inpatient Database indicates the type of anesthesia provided, one hospital identifier, and patient diagnoses and procedures performed defined in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). They do not contain information on the neonate and do not allow linkage with the neonate record. Furthermore, it provides a variable indicating whether an ICD-9-CM diagnosis code was present on admission or not. This variable allows distinguishing a preexisting condition from a complication arising during hospitalization. Last, for patients with multiple hospitalizations, it also provides a unique readmission identifier (variable VisitLink) that allows tracking patient readmission across hospitals and years. For these patients, a second variable is provided (variable DaysToEvent) that allows calculating the number of days elapsed between readmissions. Hospital characteristics were calculated using the State Inpatient Database or abstracted from the American Hospital Association Annual Survey Database.
Definition of exposure
Exposure of our primary interest was the use of general anesthesia for cesarean delivery. New York State Inpatient Database is the only HCUP participating state providing information on anesthesia care (variable ANESTH). Anesthesia type is reported as a categorical variable with values corresponding to general, regional, other, local, none, and missing. Each discharge record contains a maximum of one value for anesthesia type and woman who received general anesthesia for cesarean delivery because of a failed epidural catheter would be coded as general anesthesia. For the purpose of the study, the variable was categorized as general anesthesia, regional (neuraxial) anesthesia, and missing.
Definition of the study sample
The study sample included all records of discharges after cesarean delivery performed in New York State hospitals between January 1, 2006 and December 31, 2013. Cesarean deliveries were identified with a combination of ICD-9-CM diagnosis and procedure codes as previously described. 11 In case that a woman had more than one cesarean delivery during the study period, only the first cesarean delivery was included in the study. Discharges were also excluded if 1) the patient ZIP code of residence was not located in New York State or missing, 2) information on the type of anesthesia provided was missing, 3) the patient had undergone a general anesthetic in the year before or in the year after the index cesarean delivery case, and 4) the patient had another delivery in the year before or in the year after the index cesarean delivery case.
Definition of the primary and secondary outcomes
The primary outcome was new onset depression during the cesarean delivery hospitalization or during a readmission in a woman with or without a previous history of depression (Supplemental Figure 1). Depression was defined using an ICD-9-CM algorithm, adapted from Savitz, Zhong, and Guglielminotti (Supplemental Table 1). 12-14 A history of depression was defined as a diagnosis of depression recorded during the year preceding the cesarean delivery hospitalization or present on admission of the cesarean delivery hospitalization. New onset depression during the cesarean delivery hospitalization corresponded to a diagnosis of depression recorded during the delivery hospitalization but not present on admission. A new onset depression during a readmission corresponded to a diagnosis of depression recorded during a readmission within one-year postdelivery, but not present during the index delivery hospitalization.
The three secondary outcomes were new onset of 1) suicidal ideation or self-inflicted injury (i.e., suicidality), 2) anxiety disorders, and 3) post-traumatic stress disorder recorded during the initial delivery hospitalization or a readmission in a woman with or without a history of the examined psychiatric outcome.
Obstetrical and hospital characteristics
The following maternal characteristics were recorded directly from the State Inpatient Database: age, race and ethnicity (categorized as non-Hispanics White or non-White), insurance type (categorized as Medicaid-Medicare or non-Medicaid-Medicare), admission for delivery during a weekend, and admission type (categorized as elective or non-elective).
The exact indications for general anesthesia (e.g., maternal request) are not explicitly recorded in the State Inpatient Database. The possible indications for general anesthesia were therefore estimated using ICD-9-CM codes and were categorized into three groups: contraindications to neuraxial anesthesia, obstetrical indications, and maternal indications (Supplemental Table 2).15 Possible contraindications to neuraxial anesthesia included: coagulation factor deficit and Von Willebrand disease, thrombocytopenia, sepsis and septic shock, chorioamnionitis. Possible obstetrical indications for general anesthesia included: abnormality fetal heart rate, fetal distress, abruptio placenta, uterine rupture, umbilical cord prolapse, postpartum hemorrhage, blood transfusion, placenta praevia, and placenta accreta. Presence of severe maternal comorbidities can be an indication for general anesthesia (maternal indication). Maternal comorbidities were summarized using the Charlson comorbidity index (with a threshold value of 1) and the comorbidity index for obstetric patients (with a threshold of 2). The two comorbidity indexes were calculated using previously described ICD-9-CM algorithms.16,17
The following hospital characteristics were calculated for each year of the study period using the State Inpatient Database data: volume of delivery, cesarean delivery rate, percent neuraxial anesthesia in vaginal deliveries, percent admission for delivery during a weekend, percent non-White (including Hispanics) in deliveries, percent Medicaid/care beneficiaries in deliveries, percent women with a Charlson comorbidity index ≥ 1 in deliveries, percent women with a comorbidity index for obstetric patients ≥ 2 in deliveries, and intensity of coding. For each hospital, the annual intensity of coding was calculated as the mean number of diagnosis and procedure codes, including E-codes, reported per discharge.18
The following hospital characteristics were obtained from the American Hospital Association Annual Survey Database: hospital location (rural or urban), teaching status, neonatal level-of-care designation (1, 2 or 3), physician-to-bed ratio, resident-to-bed ratio, and nurse-to-bed ratio. Rural hospital location included micropolitan or rural areas based on the Core Based Statistical Areas. A teaching hospital had an affiliation to a medical school or residency training accreditation. Neonatal level-of-care 1 hospitals provide basic neonatal level of care, level 2 specialty neonatal care (e.g., care of preterm infants with birth weight ≥1500 g), and level 3 subspecialty neonatal intensive care (e.g., mechanical ventilation ≥ 24 hour).
Statistical analysis
Statistical analysis was performed with R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and specific packages (mice for multiple imputations, lme4 for mixed-effect models, and Matching for propensity score matching).
Descriptive statistics
Results are expressed as median (interquartile range) or count (% or per 1000). Univariate comparisons used Chi-squared or Fisher exact tests for categorical variables and Wilcoxon test for continuous variables. Missing values were estimated using multiple imputations using the R package mice (Multivariate Imputation by Chained Equations) with 5 iterations and five imputed datasets created (Supplemental Table 3).
Odds of new onset psychiatric outcomes
Unadjusted odds ratios for the 4 psychiatric outcomes associated with exposure to general anesthesia were calculated using univariate logistic regression. Adjusted odds ratio were calculated using propensity score matching.
The propensity score (i.e., individual probability of receiving general anesthesia) was estimated using a mixed-effect logistic regression model. In this model, the random effect was the hospital identifier (normally distributed intercept and constant slope); the fixed-effects were the 39 patient and hospital characteristics described in Supplemental Table 4, along with the year of delivery. Both the fixed and random effects were used to calculate the propensity score. Performance of the model was assessed with the c-index. Each general anesthesia case was matched without replacement to 6 controls using the nearest neighbor approach and a caliper of 0.2. Balance in propensity score matched patients was considered achieved when the standardized mean difference was less than 0.1.
In propensity score matched patients, the odds of new onset psychiatric outcome associated with general anesthesia was quantified with the odds ratio from a mixed-effect logistic regression. In this model, the outcome was the occurrence of the examined outcome, the random effect was the hospital identifier, and the fixed effect was the exposure to general anesthesia.
To assess potential bias due to unmeasured confounder (e.g., emergent cesarean delivery), we calculated the E-value associated with the adjusted odds ratio of adverse outcome. The E-value estimates how strong an unmeasured confounder (i.e., an unknown factor associated with both general anesthesia and the complication examined) would need to be to explain away the observed association between general anesthesia and the complication.19 The lowest possible E-value is 1 and indicates that no unmeasured confounding is needed to explain away the observed association. The higher the E-value, the stronger the confounder association must be to explain away the observed association.
Sensitivity analyses
We performed two sets of sensitivity analysis. First, we assessed the effect of a history of the psychiatric outcome on the odds of a new onset for this outcome by adding the variable “history” as a fixed-effect in the mixed-effect model in propensity score matched patients. Second, we limited the identification of new onset psychiatric outcomes during a readmission to the first and second diagnosis codes. In the main analysis, new onset psychiatric outcomes during readmissions were identified among up to 25 possible diagnosis codes. They may therefore indicate preexisting conditions and not complications leading to the readmission. New onset psychiatric outcomes identified in the first or second diagnosis codes are more likely to represent the reason for readmission than a preexisting condition.
A priori effect size calculation
Based on our previous research, we expected to have 645,000 cesarean deliveries cases in New York State between 2006 and 2013 and a general anesthesia rate of about 7%.15 With a rate of new onset depression of 0.25% in women who received neuraxial anesthesia, a proportion of discharges with exclusion criteria of 35%, an alpha of 5%, a power of 80%, and a two-sided test, we will be able to demonstrate a 35% or greater relative increase in the rate of new onset depression in women who received general anesthesia (rate of 0.34% or greater) compared with neuraxial anesthesia.13
RESULTS
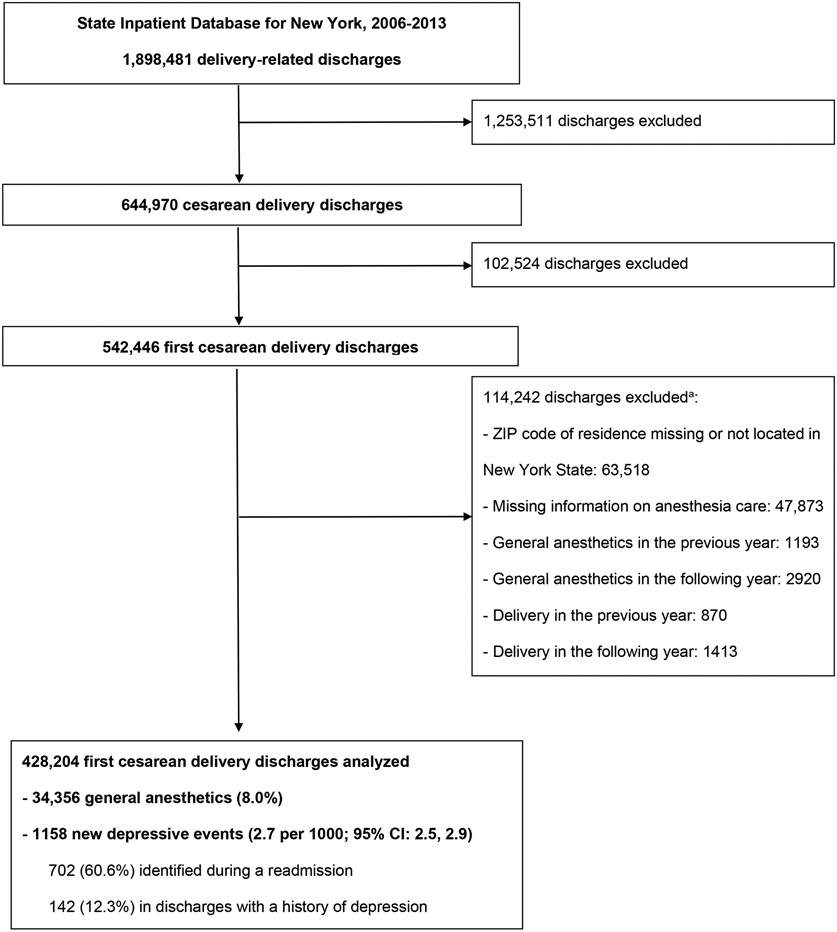
The study sample included 428,204 cesarean delivery cases meeting the inclusion criteria (Figure 1). Among the included cases, 34,356 had a general anesthetic (8.0%; 95% confidence interval (CI): 7.9-8.1). Compared with women undergoing cesarean delivery under neuraxial anesthesia, women undergoing cesarean delivery under general anesthesia were older and more often non-White or Medicaid/Medicare beneficiary (Supplemental Table 4). They had higher comorbidity indexes values and delivered more often in a neonatal level-of-care 3 hospital. Comparison of included and excluded cesarean delivery cases is presented in the Supplemental Table 5.
Figure 1.
Flowchart of the study (a total does not round up because reasons for exclusion are not mutually exclusive)
New onset depressive disorder was recorded in 1158 women (2.70 per 1000; 95% CI: 2.55-2.86); of them, 702 (60.6%) were identified during a readmission with a median of 128 days after discharge (interquartile range 38-247). Among women with a new onset depressive disorder, 12.3% had a history of depression (95% CI, 10.4-14.3). Suicidal ideation or self-inflicted injury was recorded in 214 women (0.50 per 1000; 95% CI: 0.44-0.57); of them, 123 (57.5%) were also diagnosed with new onset depression. The incidence of the 4 outcomes examined in the general and neuraxial anesthesia groups, the proportion of cases identified during a readmission, and the time-to-readmission are presented in Tables 1 and 2.
Table 1.
Incidence of adverse psychiatric maternal outcomes associated with general anesthesia for cesarean delivery in the State Inpatient Database for New York, 2006-2013.
| Neuraxial anesthesia (N = 393,848) |
General anesthesia (N = 34,356) |
|||||
|---|---|---|---|---|---|---|
| Number | Incidence (Per 1000) | 95% CI | Number | Incidence (Per 1000) | 95% CI | |
| Depression | 1034 | 2.62 | 2.47-2.79 | 124 | 3.61 | 3.00-4.30 |
| Suicidal ideation or self-inflicted injury | 182 | 0.46 | 0.40-0.53 | 32 | 0.93 | 0.64-1.31 |
| Anxiety | 636 | 1.61 | 1.49-1.74 | 50 | 1.45 | 1.08-1.92 |
| Post-traumatic stress disorder | 52 | 0.13 | 0.10-0.17 | - a | - a | 0.06-0.38 |
Abbreviations: CI: confidence interval.
Because of HCUP data use agreement restrictions on small cell size, the number of observed cases and exact proportions are not presented.
Table 2.
Proportion of adverse psychiatric maternal outcomes identified during readmissions and time elapsed between hospital discharge and readmission in the State Inpatient Database for New York, 2006-2013.
| Neuraxial anesthesia (N = 393,848) |
General anesthesia (N = 34,356) |
|||
|---|---|---|---|---|
| Outcome | Proportion | Time-to-readmission (days)a |
Proportion | Time-to-readmission (days)a |
| Depression | 626/1034 (60%) | 125 (35-242) | 76/124 (61%) | 164 (64-261) |
| Suicidal ideation or self-inflicted injury | 150/182 (82%) | 180 (87-255) | 21/32 (66%) | 209 (127-300) |
| Anxiety | 281/636 (44%) | 140 (45-249) | 22/50 (44%) | 156 (27-256) |
| Post-traumatic stress disorder | 51/52 (98%) | 174 (66-283) | --b (≈ 83 %) | 108 (92-276) |
Time-to-readmission is expressed as median (interquartile range)
Because of HCUP data use agreement restrictions on small cell size, the number of observed cases and exact proportions are not presented.
The c-statistic of the mixed-effect model used to estimate the propensity score was 0.897 (95% CI: 0.895, 0.898) and the coefficient of determination (r-squared) was 51%. After propensity score matching, 16,477 cases were matched to 98,862 controls. The standardized mean difference was less than 0.1 for all the 39 patient- and hospital-level characteristics examined and for the year of delivery (Supplemental Table 4). In matched patients, general anesthesia was associated with 54% increased odds of PPD (adjusted OR (aOR) 1.54; 95% CI, 1.21-1.95) and 91% increased odds of suicidal ideation or self-inflicted injury (aOR 1.91; 95% CI, 1.12-3.25) (Table 3). The E-value for PPD was 2.45 (lower limit of the 95% CI, 1.71) and for suicidal ideation or self-inflicted injury 3.23 (lower limit of the 95% CI, 1.49). General anesthesia was not associated with a significantly increased odds of anxiety or PTSD. Results from the sensitivity analyses were generally consistent with the findings from the main analyses (Supplemental Tables 6 and 7).
Table 3:
Crude and adjusted odds ratio for the risk of adverse psychiatric maternal outcomes associated with general anesthesia for cesarean delivery in the State Inpatient Database for New York, 2006-2013.
| Outcome | Crude OR | 95% CI | Adjusted OR a | 95% CI | E-value (lower limit of the 95% CI) b |
|---|---|---|---|---|---|
| Depression | 1.38 | 1.14-1.66 | 1.54 | 1.21-1.95 | 2.45 (1.71) |
| Suicidal ideation or self-inflicted injury | 2.02 | 1.38-2.94 | 1.91 | 1.12-3.25 | 3.23 (1.49) |
| Anxiety | 0.90 | 0.68-1.20 | 1.37 | 0.97-1.95 | -- |
| Post-traumatic stress disorder | 1.32 | 0.57-3.08 | 1.50 | 0.50-4.47 | -- |
Abbreviations: CI: confidence interval; OR: odds ratio.
Using propensity score matching
The E-value estimates how strong an unmeasured confounder would need to be to explain away the association observed between general anesthesia and the complication. The lowest possible E-value is 1 and indicates that no unmeasured confounding is needed to explain away the observed association. The higher the E-value, the stronger the confounder association must be to explain away the observed association.
DISCUSSION
Using data from cesarean deliveries performed in New York State hospitals between 2006 and 2013, we report increased odds of severe PPD requiring hospitalization, suicidal ideation, and self-inflicted injury in women who had a cesarean delivery performed under general anesthesia compared with neuraxial anesthesia. These findings are robust when adjusted for history of depressive disorders, the strongest predictor of PPD.
The association between exposure to surgery and general anesthesia in adults and the risk of postoperative depression has not been well established and none of the previous studies were conducted in obstetric patients.20,21 In the present study, we report that cesarean delivery under general anesthesia is associated with increased odds of PPD, suicidal ideation, and self-inflicted injury. Similar to PPD, suicidal ideation is also increasingly recognized as a concern for maternal mental health in the United States. A recent study reports a prevalence of suicidal ideation of 19% in women screened positive using the Edinburgh Postnatal Depression Scale and suicidal ideation is a predictor of later suicide attempt and completion.22 General anesthesia for cesarean delivery might increase the risk of PPD because it is associated with delayed first skin-to-skin interaction for the maternal-infant dyad, delayed first breastfeeding attempt, an increased risk of persistent postpartum pain, and decreased maternal satisfaction with anesthesia care.9,10 Delays in first interaction between the mother and her child and in initiation of breastfeeding have been linked to increased risk of PPD.23,24 The World Health Organization recommends that breastfeeding is initiated within the first hour of neonatal delivery. General anesthesia for cesarean delivery or abdominal hysterectomy is associated with increased risks of severe acute postoperative pain, prolonged postoperative recovery, and persistent chronic pain.10,25 Moreover, the intensity of acute postpartum pain has been linked to increased risk of PPD; compared to women with mild postpartum pain, women with severe postpartum pain have a 3.0-fold increased risk of depression at 8 weeks postpartum.26 Two studies conducted in obstetric patients also suggest an increased risk of PPD associated with poor pain control using labor neuraxial analgesia and parturient dissatisfaction with analgesia care provided.27,28
Our findings should be interpreted in the context of several limitations. First, our study is based on observational data. The reported association between exposure to general anesthesia and the risk of postpartum depression and suicidality does not necessarily represent a causal relationship. Second, confounding by indication and residual confounding could explain the observed associations between general anesthesia and postpartum mood disorders. Indeed, the exact indication for general anesthesia cannot be accurately identified in administrative data and the propensity score used to estimate the odds of receiving general anesthesia includes only known confounders or available confounders. Furthermore, we have no information on whether the cesarean delivery was emergent or not, and no information on neonatal outcomes. Emergent cesarean delivery and adverse neonatal outcomes may constitute a traumatic childbirth experience, which has been associated with the subsequent development of mood disorders. 29,30 To assess the impact of emergent cesarean delivery on our results, we calculated the E-value associated with the adjusted odds ratio for the risk of PPD and suicidality. This relatively new metric takes into consideration two associations: 1) that between the confounder (emergent cesarean delivery) and the outcome (postpartum depression); and 2) the association between the confounder (emergent cesarean delivery) and the exposure (general anesthesia). An E-value of 1.7 for the unmeasured confounder emergent cesarean delivery indicates that to explain away the association between general anesthesia and depression, either: 1) emergent cesarean delivery increases the risk of depression by at least 70%; or 2) emergent cesarean delivery is at least 70% more prevalent among general anesthesia than among neuraxial anesthesia. Either association is clinically plausible. Third, the identification of PPD was limited to the delivery hospitalization or to a hospital readmission. Data on outpatient visits or emergency department visits were not included. We may have therefore identified only severe PPD and underestimated the true incidence of PPD. The incidence of PPD (0.27%) identified in the current study aligns with previous research on PPD requiring hospitalization13. Fourth, there is no specific code to identify PPD and we used a previously published ICD-9-CM algorithm.13,14,31 This algorithm has a high specificity but a low sensitivity.32 Inclusion of at least one antidepressant prescription may have increased the sensitivity of this algorithm to identify depressive disorders but prescription drugs are not available in hospital discharge records. Last, this study was limited to New York State and its results may not be generalizable to other states given the marked variations across states in both the utilization of general anesthesia for cesarean delivery and in the incidence of PPD. 1,33
If confirmed, our findings can have important implications for obstetric anesthesia practice, maternal health, and healthcare policy. First, general anesthesia is a potentially modifiable risk factor for PPD. This finding provides further supporting evidence favoring neuraxial over general anesthesia in cesarean delivery whenever possible. Although general anesthesia is associated with the shortest decision-to-delivery interval in case of an emergent cesarean delivery, there is no evidence that it improves outcomes for neonates and mounting evidence that it is associated with adverse consequences for mothers.34 Second, the use of general anesthesia for cesarean delivery identifies a high-risk population for postpartum mental health disorders. This population is likely to benefit from mental health screening, counseling and other follow-up services as recommended by the 2018 US Preventive Services Task Force.6
In conclusion, our study indicates that exposure to general anesthesia in cesarean delivery is associated with significantly increased odds of severe PPD requiring hospitalization and suicidal ideation or self-inflicted injury. If confirmed, these preliminary findings underscore the need to reduce the use of general anesthesia in cesarean delivery whenever possible and enhance postpartum care and counseling services for women who underwent cesarean delivery under general anesthesia.
Supplementary Material
Key Points.
Question:
Is general anesthesia for cesarean delivery associated with increased odds of maternal psychiatric complications?
Findings:
In women who received general anesthesia for cesarean delivery in New York State hospitals between 2006 and 2013, general anesthesia was associated with significantly increased odds of severe postpartum depression requiring hospitalization, suicidal ideation, and self-inflicted injury.
Meaning:
If confirmed, these preliminary findings underscore the need to avoid general anesthesia for cesarean delivery whenever possible.
Acknowledgments
The authors would like to thank Dr. Ruth Landau (MD, Department of Anesthesiology, Columbia University College of Physicians and Surgeons, New York, NY, USA.) for her invaluable help during the preparation of the manuscript.
Sources of financial support:
Jean Guglielminotti is supported by an R03 from the Agency for Healthcare Research and Quality (1 R03 HS025787-01).
Glossary of terms
- ACOG
American College of Obstetricians and Gynecologists
- CI
Confidence interval
- ICD-9-CM
International Classification of Diseases, ninth revision, Clinical Modification
- HCUP
Healthcare Cost and Utilization Project
- OR
Odds ratio
- POA
Present on admission
- PPD
Postpartum depression
- PTSD
Post-traumatic stress disorder
- RECORD
REporting of studies Conducted using Observational Routinely-collected health Data
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology statement
- US
United States
- ZIP
Zone Improvement Plan
Footnotes
Competing interests: The authors declare no competing interests.
Previous presentation: This work was presented as an oral communication at the 51st annual meeting of the Society for Obstetric Anesthesia and Perinatology (SOAP) in Phoenix, AZ (May 1-5, 2019).
REFERENCES
- 1.Haight SC, Byatt N, Moore Simas TA, Robbins CL, Ko JY. Recorded diagnoses of depression during delivery hospitalizations in the United States, 2000-2015. Obstet Gynecol 2019;133:1216–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johannsen BM, Larsen JT, Laursen TM, Bergink V, Meltzer-Brody S, Munk-Olsen T. All-cause mortality in women with severe postpartum psychiatric disorders. Am J Psychiatry 2016;173:635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MMRCs. Report from nine maternal mortality review committees. Available at: https://stacks.cdc.gov/view/cdc/51660. Last accessed: October 23, 2019.
- 4.Knight M, Bunch K, Tuffnell D, Jayakody H, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ, on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2014-16: National Perinatal Epidemiology Unit, University of Oxford, 2018. [Google Scholar]
- 5.ACOG. ACOG Committee Opinion No. 757: Screening for Perinatal Depression. Obstet Gynecol 2018;132:e208–e12. [DOI] [PubMed] [Google Scholar]
- 6.USPSTF, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW Jr., Grossman DC, Kemper AR, Kubik M, Landefeld CS, Mangione CM, Silverstein M, Simon MA, Tseng CW, Wong JB. Interventions to prevent perinatal depression: US Preventive Services Task Force Recommendation Statement. JAMA 2019;321:580–7. [DOI] [PubMed] [Google Scholar]
- 7.Xu H, Ding Y, Ma Y, Xin X, Zhang D. Cesarean section and risk of postpartum depression: A meta-analysis. J Psychosom Res 2017;97:118–26. [DOI] [PubMed] [Google Scholar]
- 8.Moameri H, Ostadghaderi M, Khatooni E, Doosti-Irani A. Association of postpartum depression and cesarean section: A systematic review and meta-analysis. Clin Epidemiol Glob Health 2019;7:41–480. [Google Scholar]
- 9.Yurashevich M, Carvalho B, Butwick AJ, Ando K, Flood PD. Determinants of women's dissatisfaction with anaesthesia care in labour and delivery. Anaesthesia 2019;74:1112–20. [DOI] [PubMed] [Google Scholar]
- 10.Nikolajsen L, Sorensen HC, Jensen TS, Kehlet H. Chronic pain following caesarean section. Acta Anaesthesiol Scand 2004;48:111–6. [DOI] [PubMed] [Google Scholar]
- 11.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, Marchbanks PA. An enhanced method for identifying obstetric deliveries: Implications for estimating maternal morbidity. Matern Child Health J 2008;12:469–77. [DOI] [PubMed] [Google Scholar]
- 12.Zhong QY, Gelaye B, Smoller JW, Avillach P, Cai T, Williams MA. Adverse obstetric outcomes during delivery hospitalizations complicated by suicidal behavior among US pregnant women. PLoS One 2018;13:e0192943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savitz DA, Stein CR, Ye F, Kellerman L, Silverman M. The epidemiology of hospitalized postpartum depression in New York State, 1995-2004. Ann Epidemiol 2011;21:399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guglielminotti J, Landau R, Li G. Major neurologic complications associated with post-dural puncture headache in obstetrics: A retrospective cohort study. Anesth Analg 2019;129:1328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guglielminotti J, Landau R, Li G. Adverse events and factors associated with potentially avoidable use of general anesthesia in cesarean deliveries. Anesthesiology 2019;130:912–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bateman BT, Mhyre JM, Hernandez-Diaz S, Huybrechts KF, Fischer MA, Creanga AA, Callaghan WM, Gagne JJ. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol 2013;122:957–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–82. [DOI] [PubMed] [Google Scholar]
- 18.Guglielminotti J, Deneux-Tharaux C, Wong CA, Li G. Hospital-level factors associated with anesthesia-related adverse events in cesarean deliveries, New York State, 2009-2011. Anesth Analg 2016;122:1947–56. [DOI] [PubMed] [Google Scholar]
- 19.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: Introducing the E-Value. Ann Intern Med 2017;167:268–74. [DOI] [PubMed] [Google Scholar]
- 20.Wilson L, Bekeris J, Fiasconaro M, Liu J, Poeran J, Kim DH, Gonzalez Della Valle A, Memtsoudis SG. Risk factors for new-onset depression or anxiety following total joint arthroplasty: The role of chronic opioid use. Reg Anesth Pain Med 2019. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien H, Scarlett S, O'Hare C, Bhriain SN, Kenny RA. Hospitalisation and surgery: Is exposure associated with increased subsequent depressive symptoms? Evidence from The Irish Longitudinal Study on Ageing (TILDA). Int J Geriatr Psychiatry 2018;33:1105–13. [DOI] [PubMed] [Google Scholar]
- 22.Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013;70:490–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehler K, Hucklenbruch-Rother E, Trautmann-Villalba P, Becker I, Roth B, Kribs A. Delivery room skin-to-skin contact for preterm infants. A randomized clinical trial. Acta Paediatr 2019. [DOI] [PubMed] [Google Scholar]
- 24.Watkins S, Meltzer-Brody S, Zolnoun D, Stuebe A. Early breastfeeding experiences and postpartum depression. Obstet Gynecol 2011;118:214–21. [DOI] [PubMed] [Google Scholar]
- 25.Catro-Alves LJ, De Azevedo VL, De Freitas Braga TF, Goncalves AC, De Oliveira GSJ. The effect of neuraxial versus general anesthesia techniques on postoperative quality of recovery and analgesia after abdominal hysterectomy: A prospective, randomized, controlled trial. Anesth Analg 2011;113:1480–6. [DOI] [PubMed] [Google Scholar]
- 26.Eisenach JC, Pan PH, Smiley R, Lavand'homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain 2008;140:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lim G, Farrell LM, Facco FL, Gold MS, Wasan AD. Labor analgesia as a predictor for reduced postpartum depression scores: A retrospective observational study. Anesth Analg 2018;126:1598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orbach-Zinger S, Landau R, Harousch AB, Ovad O, Caspi L, Kornilov E, Ioscovich A, Bracco D, Davis A, Fireman S, Hoshen M, Eidelman LA. The relationship between women's intention to request a labor epidural analgesia, actually delivering with labor epidural analgesia, and postpartum depression at 6 weeks: A prospective observational study. Anesth Analg 2018;126:1590–7. [DOI] [PubMed] [Google Scholar]
- 29.Creedy DK, Shochet IM, Horsfall J. Childbirth and the development of acute trauma symptoms: Incidence and contributing factors. Birth 2000;27:104–11. [DOI] [PubMed] [Google Scholar]
- 30.Soet JE, Brack GA, Dilorio C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth 2003;30:36–46. [DOI] [PubMed] [Google Scholar]
- 31.Wu YM, McArthur E, Dixon S, Dirk JS, Welk BK. Association between intrapartum epidural use and maternal postpartum depression presenting for medical care: A population-based, matched cohort study. Int J Obstet Anesth 2018;35:10–6. [DOI] [PubMed] [Google Scholar]
- 32.Fiest KM, Jette N, Quan H, St Germaine-Smith C, Metcalfe A, Patten SB, Beck CA. Systematic review and assessment of validated case definitions for depression in administrative data. BMC Psychiatry 2014;14:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N. United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open 2018;1:e186567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmer E, Ciechanowicz S, Reeve A, Harris S, Wong DJN, Sultan P. Operating room-to-incision interval and neonatal outcome in emergency caesarean section: a retrospective 5-year cohort study. Anaesthesia 2018;73:825–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.