Abstract
Aim
The study aimed to evaluate a tailored reproductive health promotion programme based on the Precaution Adoption Process Model (PAPM) for young adults.
Design
This was a two‐group, non‐blinded randomized controlled trial.
Methods
This study was performed with women aged 18–25 who were not performing reproductive health‐related behaviour from September 2018 to November 2018 in Seoul, South Korea. The participants were stratified by stage of PAPM (1, 2 or 3) and were randomly allocated to the intervention group (n = 30) and the control group (n = 30). Women in the intervention group were given the programme, which was customized according to the stage of PAPM over 8 weeks, such as lectures, giving information, discussions, practical training, Q&A, case experience and counselling. The control group received educational material. The primary outcomes were reproductive‐health‐promoting behaviour and rate of contraception use.
Results
Reproductive‐health‐promoting behaviour was significantly higher in the intervention group than the control group post‐intervention, as were reproductive health beliefs, motivation and self‐efficacy.
Keywords: health behaviour, health promotion, reproductive health, women's health, young adult
1. INTRODUCTION
Recently, reproductive health has emerged as a public health issue due to the interest in healthy pregnancy and childbirth. Although reproductive health in young women is a fundamental element affecting their children's health in the future (Ley et al., 2016), reproductive health in early adulthood could be vulnerable due to increasing sexually risky behaviour (Arnett, 2014; Scott et al., 2011; Tu et al., 2009). Young women in modern society have a longer unmarried time due to demographic changes such as expanding higher education and delayed marriage (Arnett, 2014). This means that young women are more likely than before to be exposed to diverse reproductive health problems before their pregnancy.
Unintended pregnancies and sexually transmitted infections (STIs) are the primary reproductive health problems faced by young women (Braxton et al., 2018; Centers for Disease Control and Prevention [CDC], 2019; Sedgh et al., 2014). Most young people are unaware that unintended pregnancies or STIs will affect their reproductive health (Stephenson et al., 2014). Despite half of STIs being among young people below 25 years (Braxton et al., 2018), young women do not know about STI symptoms or the fact that most STIs will be frequently asymptomatic (Raia‐Barjat et al., 2020). This situation sometimes leads to various complications, such as pelvic infections, ectopic pregnancy and sterility (CDC, 2014; Cunningham & Williams, 2018). Overall pregnancy rates have declined over time; however, about half of pregnancies are still unintended worldwide (Sedgh et al., 2014). Unintended pregnancy is more frequently reported in young people aged 18–29 years (Finer & Zolna, 2016; Sedgh et al., 2014). Most unintended pregnancies are likely to lead to induced abortions, affecting the subsequent pregnancy (Stubblefield et al., 2008).
Young adulthood also lacks preventive actions for sexual and reproductive health compared with people in other age groups (Murray Horwitz et al., 2018) and may have a low medical care access rate due to concerns about the confidential receipt of health services (Loosier et al., 2018). For example, women in early adulthood tend to conceal their reproductive health problems, and they report a low screening rate for STIs as reasons that their parents might find out (Khosropour et al., 2014; Leichliter et al., 2017). In addition, sexual and reproductive knowledge affects reproductive‐health‐related behaviour (Kim et al., 2018); however, young adults' primary source of information about reproductive health is the Internet and social media rather than healthcare providers (Byron et al., 2013; Warzecha et al., 2019). This method of acquisition may give inappropriate information. Consequently, young women's uninformed behaviour about reproductive health may harm potential birth outcomes.
In summary, women can face reproductive health problems without being aware of them, likely affecting their children's health and their own. Therefore, to improve the quality of overall public health, it is necessary to treat reproductive health as an essential health issue among young women who are sexually active but lack preventive health behaviours.
2. BACKGROUND
Many intervention programmes have attempted to promote reproductive health among women in early adulthood (Garzón‐Orjuela et al., 2021; Guse et al., 2012; L'Engle et al., 2016; Salam et al., 2016). Some programmes, including school‐based programmes, focus only on improving knowledge instead of focusing on changes in health behaviour. The result is less effective to change reproductive‐health‐related behaviours (Garzón‐Orjuela et al., 2021). In other programmes, focusing on specific groups (e.g. specific ethnic groups, low‐ and middle‐income countries), it is challenging to generalize their findings due to cultural and environmental differences. As the psychological characteristics of young adults vary, we can find varying knowledge gaps about reproductive health. However, it is not easy to find a programme that considered participants' psychological characteristics and readiness. Thus, tailored interventions that consider these gaps are necessary (Guse et al., 2012).
To effectively promote reproductive health in young women, it is necessary to clarify the stage of their health behaviour and psychological readiness. According to their stage, we should consider factors associated with changes in health behaviour and models that can induce behaviour change. The Precaution Adoption Process Model (PAPM) explains how someone decides on an action and how they transform that decision into action at each stage of behaviour (Weinstein & Sandman, 1992). This study confirmed the reproductive health behaviour of young women via the PAPM and evaluated a reproductive health promotion programme specific to each stage of preventive behaviour.
2.1. Precaution adoption process model
This study used the PAPM model as its framework. This model is suitable to explain an individual's decision‐making process when people take new health‐related actions to protect their health, unlike other behaviour change models. In addition, it is appropriate for application in young people who do not know about sexual and reproductive health by distinguishing stages that are not unaware of the issues.
The PAPM focuses on an individual's psychological process to predict preventive behaviour and describes seven stages of preventive behaviour, from “unaware of the issue” to “maintaining acting” (Glanz et al., 2008). For example, people in Stage 1 are unaware of the health problem. Even though those in Stage 2 are aware of the issue, they are unengaged in the issue. In Stage 3, people are undecided about what action to take. Stages 4 and 5 refer to people deciding how to act. Those who choose to take action are classified in Stage 5; those who do not take action are categorized in Stage 4. People in stage 6 begin preventive behaviours, and the individual in Stage 7 maintains those behaviours. Because people at each stage behave differently, different information and strategies might be needed stage‐wise to promote action (Weinstein & Sandman, 1992).
Therefore, this study hypothesized that different strategies would be required at each stage to promote reproductive health in young women. Accordingly, intervention in each stage was given using Information–Motivation–Behavioural Skills (IMB) components as determinants of behaviour change (Fisher & Fisher, 1992). We assumed that women were at different levels of IMB model constructs according to their stage of the PAPM on reproductive health. Thus, to successfully change reproductive health behaviour, we designed a tailored programme for each stage of the PAPM using constructs of the IMB model. Among the seven stages of the PAPM, this programme targeted women in Stages 1, 2 and 3, before they make decisions about their actions.
2.2. Aim
This study aimed to assess the reproductive health behaviour of young women via the PAPM and to verify the effectiveness of a reproductive health promotion programme specific to each stage of preventive behaviour.
3. METHODS
3.1. Design
This study used a two‐group, non‐blinded and randomized controlled trial design to examine the programme's effectiveness. The programme was conducted from September 2018 to November 2018 in Seoul, South Korea. The study was registered in the ISRCTN registry (ISRCTN No.12556383). The present study conforms with the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.
3.2. Setting and participants
We conducted an online survey to identify the stages of PAPM in young women on reproductive health before our trials and develop a tailored reproductive health promotion programme on that basis. The participants were recruited through convenience sampling using the online community notice boards of eight universities (including six women's universities) in Seoul, Korea. A total of 508 young women completed an online survey from December 2017 to April 2018. Among them, the present study included 60 eligible participants who met our inclusion criteria and indicated their desire to participate in this programme. The inclusion criteria were: (1) young women aged 18–25 years, (2) who had had coitus in the previous 3 months and had partners and (3) women in Stages 1, 2 or 3 of the PAPM on reproductive health.
3.3. Sample size and randomization
The required sample size was estimated using G*Power Version 3.1.9.2. The standardized effect size in Cohen (1988) was used to calculate this study. To calculate the sample size for repeated‐measures ANOVA, we used the following settings: effect size (f) of .40, significance level (α) of .05, power (1‐β) of .95 and three measurements. As a result, 58 subjects were calculated, 29 per study group. Considering the expected dropout rate, we included 60 participants.
After completing the baseline measurement, the participants were randomly assigned in a 1:1 ratio to the intervention group and the control group using stratified block randomization. First, the participants were stratified by stage of PAPM (1, 2, or 3), and then random allocation was conducted using a computer‐generated randomization sequence (https://www.randomizer.org/). The block size was adjusted according to number of participants by PAPM stage. Consequently, we allocated 30 participants to the intervention group (17 in Stage 1, 8 in Stage 2, 5 in Stage 3) and 30 to the control group (18 in Stage 1, 7 in Stage 2, 5 in Stage 3; Figure 1). The randomization process in this study was performed independently by one of the researchers (I.C.), and the allocation sequence was concealed to participants until the completion of the assignment. Also, after completion of allocation, participants could not change their group.
FIGURE 1.
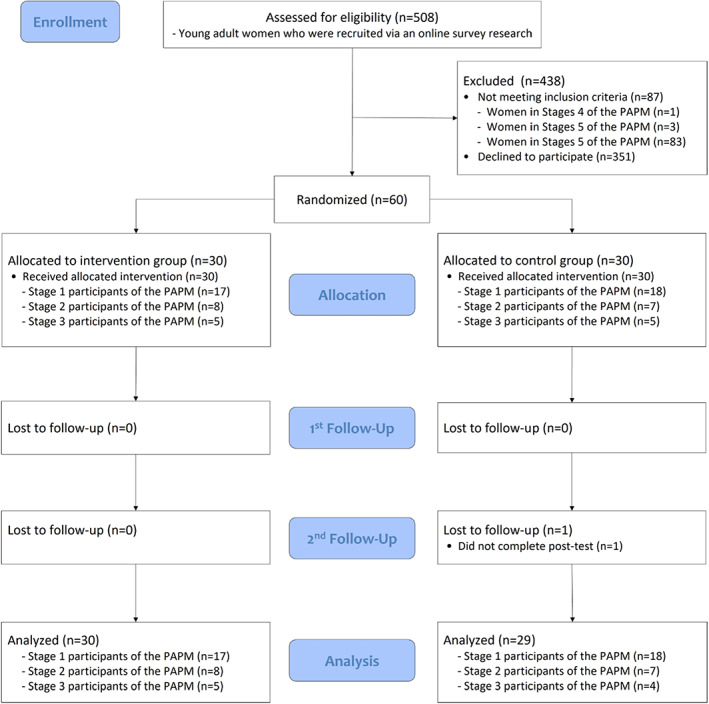
Flow diagram of the study
3.4. Blinding
The intervention allocation was not possible to mask to participants due to the nature of the programme, as participants in the intervention group attended a seminar and were given counselling. Thus, participants were aware of their allocation. Data collection was conducted through an online survey, measurement consisted of a self‐reported questionnaire. Researchers who analysed the data were not masked.
3.5. Intervention
3.5.1. Intervention group
This programme was performed for 8 weeks and was customized for reproductive health according to the stage of PAPM, using components of the IMB model (Table 1).
TABLE 1.
Constructs and strategies of the programme
| IMB | Detailed constructs | Strategies | PAPM | ||
|---|---|---|---|---|---|
| Stage 1 (Unaware) | Stage 2 (Unengaged) | Stage 3 (Undecided) | |||
| Information |
|
Lecture | ✓ | ✓ | ✓ |
| Providing periodic information | ✓ | ✓ | ✓ | ||
| Providing information tailored to individuals' needs | ✓ | ||||
| Motivation |
|
Small group discussions | ✓ | ✓ | ✓ |
| Q&A | ✓ | ✓ | ✓ | ||
| Individual counselling using the 5A's | ✓ | ||||
| Individual counselling using the 5R's | ✓ | ||||
| Case experience using videos | ✓ | ||||
| Behavioural skills |
|
Practical training | ✓ | ✓ | ✓ |
Abbreviations: IMB, Information‐Motivation‐Behavioural Skill model; PAPM, Precaution Adoption Process Model; Q&A, question and answer sessions.
For Stage 1 participants, who were mostly not aware of reproductive health matters, the programme composed strategies including lectures, giving periodic information, small group discussions, practical training, giving periodic information and Q&A. We implemented the lectures, small group discussions and practical training as 1‐day seminars for 4 hours in a conference room in Seoul. Two nurse researchers participated in the seminar, and only one researcher was aware of participants' group allocation. The lectures were conducted on four topics (“Menstruation”, “Genital infections and sexually transmitted diseases”, “Contraception”, “Preconception Care”). The small group discussion consisted of four to five people to share their experiences on the subject (“The meaning of reproductive health to me”). Practical training was given on the contraception method, including condoms, to ensure that the correct usage method was applied. Periodic information was given every 2 weeks through a mobile‐based social networking service (SNS) channel that only participants had access to. The participant could engage in Q&A sessions via this channel and could receive answers immediately.
The participants in Stage 2 knew the health risks but were not interested in reproductive health behaviours. The tailored programme in Stage 2 was designed for participants who tended to have personal invulnerability or optimism. The programme in Stage 2 included tailored strategies for the participants of Stage 2, along with the strategies of Stage 1. The tailored strategy consisted of case experience using videos and individual counselling using the 5 R's. We produced three interview videos of 1–2 min each about a young woman with reproductive health problems, to reduce the optimistic bias of the participants through surrogate experience. The video was distributed every 2 weeks to the participants in Stage 2. The individual counselling was designed to strengthen participants' motivation through the 5 R's counselling strategies: “Relevance”, “Risks”, “Rewards”, “Roadblocks” and “Repetition” (Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff, 2008). Trained nurses who completed sexual health education and counselling expert training gave individual counselling over the phone. Counselling was carried out once every video distribution for 15–20 min; hence, counselling per participant was given three times during the study.
Our programme added tailored strategies for Stage 3 with the strategies of Stage 1. These tailored strategies included providing tailored information and individual counselling using the 5 A's (“Assess”, “Advice”, “Agree”, “Assist” and “Arrange”). The participants in Stage 3 considered whether preventive behaviours could perform but did not determine action. We aimed that they could practice reproductive‐health‐promoting behaviour. Before the programme, we asked what they needed to improve reproductive health and what they could practice behaviour for reproductive health. According to the participant's response, we offered tailored information to support their behaviour change. The individual counselling using the 5 A's was applied to those willing to change their behaviour and was conducted to support behaviour change (Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff, 2008; Whitlock et al., 2002). It was performed by a trained nurse over the phone during the study, three to four times per participant. It took an average of 20 min each time.
3.5.2. Control group
The participants assigned to the control group received educational material once. This educational material consisted of the content of the lecture, given using Google Drive.
3.6. Data collection
We obtained data at three time points. T0 indicates the baseline, T1 indicates after the completion of the seminar (2 weeks after baseline), and T2 indicates after completion of the interventions (8 weeks after baseline).
Data collection was conducted through an online questionnaire. All measurements were performed using the same questionnaire as at baseline, except for general characteristics, for both the intervention and control groups.
3.7. Outcomes
In this study, the primary outcome variables were reproductive‐health‐promoting behaviour and rate of contraception use. The secondary outcome variables were reproductive health knowledge, beliefs, motivation and self‐efficacy.
3.8. Measurements
3.8.1. Primary outcomes
Reproductive‐health‐promoting behaviours were measured using the scale to measure reproductive health‐promoting behaviour developed by Jo et al. (2014). The scale contains 18 questions that query safe sexual acts (4 items), gender responsibility (4 items), reproductive health care (4 items), preventing STIs (3 items) and reproductive hygiene management (3 items). Each question was scored on a four‐point Likert scale. Scores ranged from 18–72, and higher scores indicated better reproductive‐health‐promoting behaviours. Cronbach's alpha reliability coefficient was .88 at the time of development and .96 in this study.
We measured the rate of contraception use during sexual intercourse with the opposite sex. Participants were asked to confirm their degree of contraception use per sexual activity, from 0%–100%, in the past month. Considering the period of intervention, we measured this at baseline (T0) and at the second measurement point (T2).
3.8.2. Secondary outcomes
Knowledge was measured on the reproductive health knowledge scale developed by Park and Choi (2014). It composes 34 items including the structure and function of the genital organs (6 items), pregnancy and childbirth (11 items), contraceptives and STIs (12 items) and genital cancer (5 items). One point was awarded if the correct answer was chosen. Scores ranged from 0–34, and higher scores indicated higher reproductive health knowledge. Cronbach's alpha was .79 in Park and Choi (2014) and .88 in this study.
Reproductive health beliefs, motivation and health self‐efficacy were measured using the Korean version of Champion's Health Belief Model Scale (K‐CHBMS; Lee et al., 2002). The questionnaire consists of 27 items, each of which is assessed via a five‐point Likert scale, evaluating susceptibility (5 items), seriousness (6 items), benefits (4 items), barriers (6 items), self‐efficacy (3 items) and motivation (3 items). Scores ranged from 27–135, and higher scores indicated greater health belief in each area. The reliability of the K‐CHBMS was 0.72–0.92. In our study, Cronbach's alpha was .88 for reproductive health belief, .89 for reproductive health motivation and .82 for reproductive health self‐efficacy.
3.9. Ethical considerations
This study was approved by the institutional review board of the university to which the researcher belongs (IRB no. 1040548‐KU‐IRB‐17‐169‐A‐3). We explained to potential participants about the purpose, procedures, methods, randomization, benefits and risks of participation in the study and the right to withdraw participation at any time without disadvantages. After explaining about this study, written consent was signed voluntarily by each participant.
3.10. Data analysis
Data were analysed using SPSS (SPSS Statistics 25). Analysis followed the per‐protocol principle. General characteristics were described using descriptive statistics, such as frequency, percentage, mean and standard deviation. Differences between groups were analysed using the t‐test, Chi‐square test, Fisher's exact test and the Mann–Whitney U test. The hypothesis about the effectiveness of this programme was assessed using repeated measures ANOVA and t‐tests. For post‐hoc analysis, Bonferroni correction was used. Additionally, to examine the effectiveness of the programme for each stage of the PAPM, Friedman's test and the Wilcoxon rank‐sum test were used. The reliability of the measurements used in this study was verified by calculating Cronbach's alpha. In this study, p < 0.05 was considered statistically significant, and all tests were two‐sided.
4. RESULTS
Comparison of the outcome variables between groups using repeated‐measures ANOVA is shown in Figure 2 and the Supporting Information in Addendum 1.
FIGURE 2.
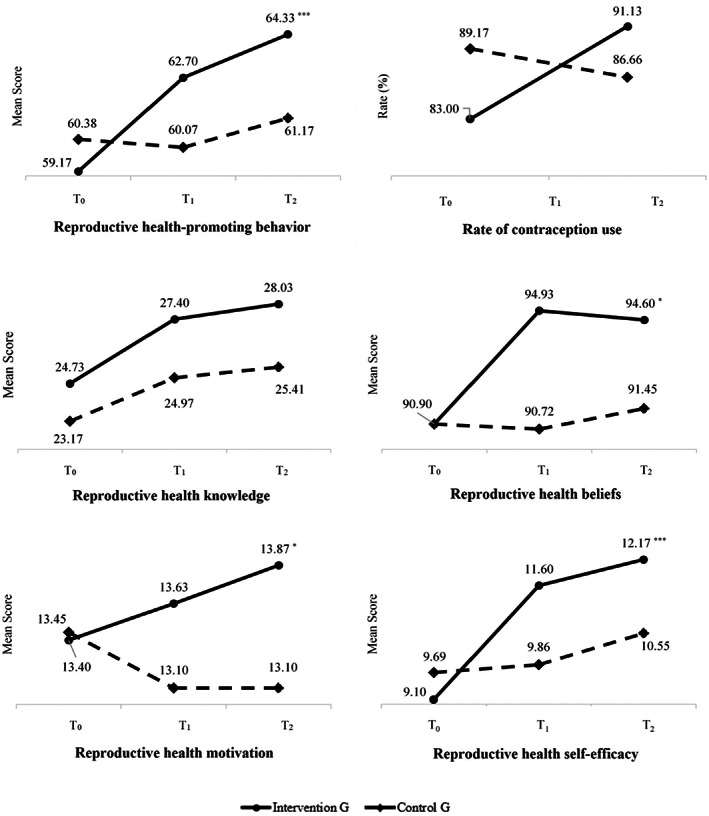
Comparison of primary and secondary outcome variables between groups over time by repeated‐measures ANOVA (N = 59)
4.1. Participant characteristics
In this study, 60 participants were enrolled, with the final analysis considering 30 in the intervention group (17 in Stage 1, 8 in Stage 2 and 5 in Stage 3) and 29 in the control group (18 in Stage 1, 7 in Stage 2 and 4 in Stage 3). No statistically significant differences were found between groups, except for average age (Table 2).
TABLE 2.
Demographic characteristics of the participants in two groups (N = 59)
| Variables | Categories | Intervention Group (n = 30) | Control Group (n = 29) | t | p |
|---|---|---|---|---|---|
| n (%) or mean ± SD | |||||
| Age (years) | 23.00 ± 1.88 | 22.03 ± 1.52 | 2.17 | .034 | |
| Perceived economic level | High | 2 (6.7) | 3 (10.3) | 0.59 a | .753 |
| Middle | 23 (76.7) | 20 (69.0) | |||
| Low | 5 (16.7) | 6 (20.7) | |||
| Socioeconomic status | Undergraduate student | 27 (90.0) | 27 (93.1) | 1.12 a | .802 |
| Graduate student | 2 (6.7) | 2 (6.9) | |||
| Job applicants | 1 (3.3) | 0 (0.0) | |||
| Contraception use in the last month | All the time | 19 (63.3) | 23 (79.3) | 2.69 a | .673 |
| More than half | 4 (13.3) | 3 (10.3) | |||
| Half | 3 (10.0) | 1 (3.4) | |||
| Less than half | 3 (10.0) | 2 (6.9) | |||
| Not using at all | 1 (3.3) | 0 (0.0) | |||
| Contraception method | Male condom | 27 (49.1) | 27 (50.0) | 1.38 | .927 |
| Oral pills | 5 (9.1) | 7 (13.0) | |||
| Withdrawal | 13 (23.6) | 13 (24.0) | |||
| Fertility awareness | 9 (16.4) | 6 (11.1) | |||
| Emergency contraception | 1 (1.8) | 1 (1.9) | |||
| Gynaecology clinics visit history | Yes | 24 (80.0) | 25(86.2) | 0.40 a | .525 |
| No | 6 (20.0) | 4(13.8) | |||
Fisher's exact test.
4.2. Primary outcomes
The mean scores for reproductive‐health‐promoting behaviour increased over time in the intervention group (T0 = 59.10, T1 = 62.70, T2 = 64.33) and were higher than those of the control group (T0 = 60.38, T1 = 60.07, T2 = 61.17). There was a statistically significant group × time interaction (F = 8.12, p = .001). The rate of contraception used in the intervention group varied from 83.00%–91.13%, whereas that of the control group changed from 89.17%–86.66%. However, no statistically significant differences between groups were found (Z = −0.47, p = .641).
4.3. Secondary outcomes
Figure 2 shows that the mean scores of all secondary outcome variables in the intervention group increased over time. Reproductive health knowledge exhibited no statistically significant group × time interaction (F = 1.40, p = .252). However, there was a statistically significant group × time interaction for reproductive health belief (F = 4.13, p = .019), reproductive health motivation (F = 3.27, p = .042) and reproductive health self‐efficacy (F = 12.71, p < .001).
4.4. Effect of programme for each stage of PAPM
The effect of the programme for each stage of PAPM is reported in Addendum 2. In the intervention group, the mean scores of reproductive‐health‐promoting behaviour, knowledge and self‐efficacy in Stage 1 participants significantly increased over time (reproductive‐health‐promoting behaviour: χ 2 = 13.23, p = .001; reproductive health knowledge: χ 2 = 25.01, p < .001; reproductive health self‐efficacy: χ 2 = 24.90, p < .001), as did scores among Stage 2 participants (reproductive‐health‐promoting behaviour: χ 2 = 11.14, p = .004; reproductive health beliefs: χ 2 = 7.55, p = .019; reproductive health motivation: χ 2 = 6.42, p = .045; reproductive health self‐efficacy: χ 2 = 11.27, p = .001). In Stage 3, only the mean scores of reproductive health self‐efficacy significantly increased over time (reproductive health self‐efficacy: χ 2 = 9.33, p = .003).
In the control group, only the mean scores of reproductive health knowledge in Stage 1 significantly increased over time (reproductive health knowledge: χ 2 = 7.85, p = .018). Furthermore, the mean scores of reproductive health motivation in Stage 2 significantly decreased over time (reproductive health motivation: χ 2 = 6.50, p = .037).
5. DISCUSSION
The tailored programme in the present study was designed to promote reproductive health in young women who are not performing precautionary behaviours (PAPM Stages 1, 2 and 3). We applied a differentiated strategy depending on individuals' psychological readiness and motivation in the PAPM stage to facilitate the participant's behaviours. This study confirmed that reproductive‐health‐promoting behaviour, reproductive health beliefs, motivation and self‐efficacy improved post‐intervention, excluding knowledge and rate of contraception use.
Many previous interventions have attempted to change women's perspectives and behaviours in early adulthood on sexual and reproductive health. One review that identified the effectiveness of sexual and reproductive intervention in early adulthood recommended randomization to recognize any meaningful behavioural changes (Salam et al., 2016). However, most studies carried out used poor methodological quality, and the results have low validity (Cowan, 2002). Our finding could be notable in that the study was conducted as RCTs, and young women facilitated their reproductive‐health‐promoting behaviour.
Arguments continue about practical and feasible approaches in sexual and reproductive health for young women (Chandra‐Mouli et al., 2015). Intervention based on traditional sexual and reproductive health education can change their knowledge; however, participants' behaviours can be more challenging to affect (Chandra‐Mouli et al., 2015; Cowan, 2002). Also, single‐focus prevention intervention has been criticized in adolescent and young adult health interventions (Catalano et al., 2012). In this context, this study is noteworthy in that it that tried to influence individual behaviour patterns using different, effective approaches per stage, beyond traditional education. Likewise, it was meaningful that we focus on comprehensive precautionary behaviours, not single behaviours such as delaying sexual engagement and contraceptive method use.
The result of our programme was similar to those of previous studies, which applied the stages of the change model to promote reproductive health behaviour. Lee and Yen (2007) used the transtheoretical model to conduct tailored sexual health education programmes according to participants' learning preparedness. After the programme, sexual self‐efficacy increased significantly, with improved knowledge and attitude scores in the intervention group; however, these changes were insufficient to explain whether the programme led to behavioural change for contraceptive behaviour. Their subsequent research (Lee et al., 2011) showed significant increases in contraceptive self‐efficacy and the choice of effective contraceptive behaviour; however, application of these findings might be limited owing to the fact that participants of the programme were postpartum women. Therefore, our findings are encouraging because the tailored programme according to the PAPM stage was effective to promote reproductive‐health‐promoting behaviour for young women.
Most previous reproductive health promotion programmes and related studies assessed contraceptive behavioural changes to confirm the programme's effectiveness. A meta‐analysis showed that theory‐based programmes effectively promote the use of effective contraception methods, condom use after the programme and overlapping contraception methods (Lopez et al., 2016). Meanwhile, Peipert et al. (2011) conducted a programme (Project PROTECT) using a transtheoretical model to promote the use of double contraception, with a 24‐month follow‐up period to confirm compliance among female participants of childbearing age; however, it was confirmed that these customized programmes increased the initiation of double contraceptive use but did not change STI incidence or the number of unplanned pregnancies. As per the above results, it was a meaningful finding that the reproductive health promotion programme developed in this study was strategically applied to each stage, which positively affected reproductive health beliefs, reproductive health motivation and reproductive health self‐efficacy; this led to reproductive health promotion behaviour. However, the rate of contraception use was not significantly different between groups, versus the significant increase in reproductive‐health‐promoting behaviour scores. Because the period between the T0 and T2 surveys, which confirmed the rate of contraception use, was short, this might not accurately reflect whether the participants were practising contraception. Thus, it is necessary to conduct further studies with a sufficient follow‐up period.
5.1. Limitations
This study has several limitations. First, since the potential participants recruited through an online survey were 358 in Stage 1, 48 in Stage 2 and 15 in Stage 3, the number of our programme's participants in Stages 2 and 3 was less than 10. As such, although a tailored programme according to each stage of the PAPM was effective, generalizability of the findings is limited. Second, the intervention period was relatively short to affect long‐term behaviour. In addition, the retention and persistence of behaviour changes since completion of this programme have not been confirmed with follow‐up investigations. Third, in this programme, only the correct use of the contraceptive tool was included as the practical training. To improve the reproductive health knowledge and contraceptive use rate, various educational content should be used to promote behavioural skills related to reproductive health promotion activities, including appropriate education strategies for young women. Finally, the second and third stages in this study used personalized strategies that focused on individuals through individual counselling. Individual counselling using the 5 A's and the 5 R's was a brief and effective evidence‐based approach. However, it was ineffective in terms of time and cost because of the individual consultations. Further studies are necessary to supplement individual counselling, such as counselling using digital devices or web‐based programmes. Thus, subsequent reproductive health promotion programmes based on PAPM for young women need to be repeated to supplement these limitations.
6. CONCLUSION
In this study, we strategically applied a tailored programme to each stage of the PAPM (Stages 1, 2 and 3) for young women who are not performing precautionary behaviours. As a result, this programme effectively induced reproductive‐health‐promoting behaviour in young women. Thus, the programme may be considered adequate for improving reproductive health. Also, our findings suggest that tailoring messages and approaches according to individuals' psychological readiness and motivation is necessary to promote reproductive‐health‐promoting behaviour. Overall, our programme is feasible and effective for young women, addressing limitations of time and cost.
AUTHOR CONTRIBUTIONS
Conceptualization: Young‐Joo Park and Inhae Cho; Data curation: Inhae Cho; Formal analysis: Inhae Cho; Funding acquisition: Inhae Cho; Investigation: Inhae Cho; Methodology: Young‐Joo Park and Inhae Cho; Project administration: Inhae Cho; Resources: Young‐Joo Park and Inhae Cho; Software: Inhae Cho; Supervision: Young‐Joo Park; Validation: Young‐Joo Park; Visualization: Inhae Cho; Roles, writing original draft: Inhae Cho; Writing, review & editing: Young‐Joo Park.
All authors have agreed on the final version and meet at least one of the following criteria [recommended bythe ICMJE (http://www.icmje.org/recommendations/)]:
• substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
• drafting the article or revising it critically for important intellectual content.
FUNDING INFORMATION
This study was supported by the Health Fellowship Foundation in Korea. The funding source was not involved in the research conducted or preparation of the article.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest.
ETHICS STATEMENTS
This study obtained ethical approval from the institutional review board of Korea University (1040548‐KU‐IRB‐17‐169‐A‐3).
CLINICAL TRIAL REGISTRATION NUMBER
ISRCTN registry number (ISRCTN12556383).
Supporting information
Appendix S1
ACKNOWLEDGEMENT
The authors wish to express appreciation to the participants of this study.
Cho, I. , & Park, Y.‐J. (2023). The effectiveness of a tailored programme to promote reproductive‐health‐promoting behaviour in young women based on the Precaution Adoption Process Model: A randomized controlled trial. Nursing Open, 10, 1704–1714. 10.1002/nop2.1425
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Arnett, J. J. (2014). Emerging adulthood: The winding road from the late teens through the twenties. Oxford University Press. [Google Scholar]
- Braxton, J. , Davis, D. W. , Emerson, B. , Flagg, E. W. , Grey, J. , Grier, L. , Harvey, A. , Kidd, S. , Kreisel, K. , Llata, E. , Presley, M. K. R. , Ramirez, V. , Shapiro, S. , St. Cyr, S. , Stenger, M. , Torrone, E. , Weinstock, H. , Weston, E. , & Womack, N. (2018). Sexually transmitted disease surveillance, 2017. Centers for Disease Control and Prevention. 10.15620/cdc.59237 [DOI] [Google Scholar]
- Byron, P. , Albury, K. , & Evers, C. (2013). “It would be weird to have that on Facebook”: Young people's use of social media and the risk of sharing sexual health information. Reproductive Health Matters, 21(41), 35–44. 10.1016/S0968-8080(13)41686-5 [DOI] [PubMed] [Google Scholar]
- Catalano, R. F. , Fagan, A. A. , Gavin, L. E. , Greenberg, M. T. , Irwin, C. E., Jr. , Ross, D. A. , & Shek, D. T. (2012). Worldwide application of prevention science in adolescent health. The Lancet, 379(9826), 1653–1664. 10.1016/S0140-6736(12)60238-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] . (2014). Recommendations for the laboratory‐based detection of Chlamydia trachomatis and Neisseria gonorrhoeae—2014. Recommendations and Reports, 63(RR‐02), 1–19. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] . (2019). Sexually transmitted disease surveillance, 2018. 10.15620/cdc.79370 [DOI]
- Chandra‐Mouli, V. , Lane, C. , & Wong, S. (2015). What does not work in adolescent sexual and reproductive health: A review of evidence on interventions commonly accepted as best practices. Global Health: Science and Practice, 3(3), 333–340. 10.9745/GHSP-D-15-00126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff . (2008). A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. American Journal of Preventive Medicine, 35(2), 158–176. 10.1016/j.amepre.2008.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Academic. [Google Scholar]
- Cowan, F. M. (2002). Adolescent reproductive health interventions. Sexually Transmitted Infections, 78, 315–318. 10.1136/sti.78.5.315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, F. G. , & Williams, J. W. (2018). Williams obstetrics (25th ed.). McGraw‐Hill Education. [Google Scholar]
- Finer, L. B. , & Zolna, M. R. (2016). Declines in unintended pregnancy in the United States, 2008–2011. The New England Journal of Medicine, 374(9), 843–852. 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, J. D. , & Fisher, W. A. (1992). Changing AIDS‐risk behavior. Psychological Bulletin, 111(3), 455–474. 10.1037/0033-2909.111.3.455 [DOI] [PubMed] [Google Scholar]
- Garzón‐Orjuela, N. , Samacá‐Samacá, D. , Moreno‐Chaparro, J. , Ballesteros‐Cabrera, M. D. P. , & Eslava‐Schmalbach, J. (2021). Effectiveness of sex education interventions in adolescents: An overview. Comprehensive child and adolescent nursing, 44(1), 15–48. 10.1080/24694193.2020.1713251 [DOI] [PubMed] [Google Scholar]
- Glanz, K. , Rimer, B. K. , & Viswanath, K. (2008). Health behavior and health education: Theory, research, and practice. John Wiley & Sons. [Google Scholar]
- Guse, K. , Levine, D. , Martins, S. , Lira, A. , Gaarde, J. , Westmorland, W. , & Gilliam, M. (2012). Interventions using new digital media to improve adolescent sexual health: A systematic review. Journal of Adolescent Health, 51(6), 535–543. 10.1016/j.jadohealth.2012.03.014 [DOI] [PubMed] [Google Scholar]
- Jo, H. Y. , Kim, Y. H. , & Son, H. M. (2014). Development of a scale to measure reproductive health promoting behavior of undergraduates. Korean Journal of Health Education and Promotion, 31(5), 29–43. 10.14367/kjhep.2014.31.5.29 [DOI] [Google Scholar]
- Khosropour, C. M. , Broad, J. M. , Scholes, D. , Saint‐Johnson, J. , Manhart, L. E. , & Golden. (2014). Estimating chlamydia screening coverage: A comparison of self‐report and Healthcare Effectiveness Data and Information Set (HEDIS) measures. Sexually Transmitted Diseases, 41(11), 665–670. 10.1097/OLQ.0000000000000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, H. Y. , Park, M. , & Lee, E. (2018). A cross‐sectional survey of relationships between sexual knowledge, sexual attitudes, and reproductive health behaviour among female university students. Contemporary Nurse, 54(6), 640–650. 10.1080/10376178.2018.1556104 [DOI] [PubMed] [Google Scholar]
- Lee, E.‐H. , Kim, J.‐S. , & Song, M. S. (2002). Translation and validation of champion's health belief model scale with Korean women. Cancer Nursing, 25(5), 391–395. 10.1097/00002820-200210000-00010 [DOI] [PubMed] [Google Scholar]
- Lee, J. T. , Tsai, J. L. , Tsou, T. S. , & Chen, M. C. (2011). Effectiveness of a theory‐based postpartum sexual health education program on women's contraceptive use: A randomized controlled trial. Contraception, 84(1), 48–56. 10.1016/j.contraception.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Lee, J. T. , & Yen, H.‐W. (2007). Randomized controlled evaluation of a theory‐based postpartum sexual health education programme. Journal of Advanced Nursing, 60(4), 389–401. 10.1111/j.1365-2648.2007.04395.x [DOI] [PubMed] [Google Scholar]
- Leichliter, J. S. , Copen, C. , & Dittus, P. J. (2017). Confidentiality issues and use of sexually transmitted disease services among sexually experienced persons aged 15–25 years ‐ United States, 2013–2015. Morbidity and Mortality Weekly Report, 66(9), 237–241. 10.15585/mmwr.mm6609a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- L'Engle, K. L. , Mangone, E. R. , Parcesepe, A. M. , Agarwal, S. , & Ippoliti, N. B. (2016). Mobile phone interventions for adolescent sexual and reproductive health: A systematic review. Pediatrics, 138(3), e20160884. 10.1542/peds.2016-0884 [DOI] [PubMed] [Google Scholar]
- Ley, C. , de la Luz Sanchez, M. , Mathur, A. , Yang, S. , Sundaram, V. , & Parsonnet, J. (2016). Stanford's Outcomes Research in Kids (STORK): A prospective study of healthy pregnant women and their babies in Northern California. BMJ Open, 6(4), e010810. 10.1136/bmjopen-2015-010810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loosier, P. S. , Hsieh, H. , Cramer, R. , & Tao, G. (2018). Young adults' access to insurance through parents: Relationship to receipt of reproductive health services and chlamydia testing, 2007–2014. Journal of Adolescent Health, 63(5), 575–581. 10.1016/j.jadohealth.2018.04.015 [DOI] [PubMed] [Google Scholar]
- Lopez, L. M. , Grey, T. W. , Chen, M. , Tolley, E. E. , & Stockton, L. L. (2016). Theory‐based interventions for contraception. The . Cochrane Database of Systematic Reviews, 11(11), CD007249. 10.1002/14651858.CD007249.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray Horwitz, M. E. , Pace, L. E. , & Ross‐Degnan, D. (2018). Trends and disparities in sexual and reproductive health behaviors and service use among young adult women (aged 18–25 years) in the United States, 2002–2015. American Journal of Public Health, 108(S4), S336–S343. 10.2105/AJPH.2018.304556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, M. N. , & Choi, S. Y. (2014). Development of reproductive health program and identification of effect for married women immigrants. Journal of Korean Academy of Nursing, 44(3), 248–258. 10.4040/jkan.2014.44.3.248 [DOI] [PubMed] [Google Scholar]
- Peipert, J. F. , Zhao, Q. , Meints, L. , Peipert, B. J. , Redding, C. A. , & Allsworth, J. E. (2011). Adherence to dual‐method contraceptive use. Contraception, 84(3), 252–258. 10.1016/j.contraception.2011.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raia‐Barjat, T. , Gannard, I. , Virieux, D. , Del Aguila‐Berthelot, C. , Nekaa, M. , Chauvin, F. , … Gagneux‐Brunon, A. (2020). Health students' knowledge of sexually transmitted infections and risky behaviors before participation to the health promotion program. Medecine et maladies infectieuses, 50(4), 368–371. 10.1016/j.medmal.2020.01.015 [DOI] [PubMed] [Google Scholar]
- Salam, R. A. , Faqqah, A. , Sajjad, N. , Lassi, Z. S. , Das, J. K. , Kaufman, M. , & Bhutta, Z. A. (2016). Improving adolescent sexual and reproductive health: A systematic review of potential interventions. Journal of Adolescent Health, 59(4), S11–S28. 10.1016/j.jadohealth.2016.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott, M. E. , Wildsmith, E. , Welti, K. , Ryan, S. , Schelar, E. , & Steward‐Streng, N. R. (2011). Risky adolescent sexual behaviors and reproductive health in young adulthood. Perspectives on Sexual Reproductive Health, 43(2), 110–118. 10.1363/4311011 [DOI] [PubMed] [Google Scholar]
- Sedgh, G. , Singh, S. , & Hussain, R. (2014). Intended and Unintended Pregnancies Worldwide in 2012 and Recent Trends. Studies in Family Planning, 45, 301–314. 10.1111/j.1728-4465.2014.00393.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson, J. , Patel, D. , Barrett, G. , Howden, B. , Copas, A. , Ojukwu, O. , … Shawe, J. (2014). How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PLoS One, 9(7), e103085. 10.1371/journal.pone.0103085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubblefield, P. G. , Coonrod, D. V. , Reddy, U. M. , Sayegh, R. , Nicholson, W. , Rychlik, D. F. , & Jack, B. W. (2008). The clinical content of preconception care: Reproductive history. American Journal of Obstetrics & Gynecology, 199(6), S373–S383. 10.1016/j.ajog.2008.10.048 [DOI] [PubMed] [Google Scholar]
- Tu, W. , Batteiger, B. E. , Wiehe, S. , Ofner, S. , Van Der Pol, B. , Katz, B. P. , … Fortenberry, J. D. (2009). Time from first intercourse to first sexually transmitted infection diagnosis among adolescent women. Archives of Pediatrics and Adolescent Medicine, 163(12), 1106–1111. 10.1001/archpediatrics.2009.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warzecha, D. , Szymusik, I. , Pietrzak, B. , Kosinska‐Kaczynska, K. , Sierdzinski, J. , Sochacki‐Wojcicka, N. , & Wielgos, M. (2019). Sex education in Poland: A cross‐sectional study evaluating over twenty thousand Polish women's knowledge of reproductive health issues and contraceptive methods. BMC Public Health, 19(1), 1–8. 10.1186/s12889-019-7046-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein, N. D. , & Sandman, P. M. (1992). A model of the precaution adoption process: Evidence from home radon testing. Health Psychology, 11(3), 170–180. 10.1037/0278-6133.11.3.170 [DOI] [PubMed] [Google Scholar]
- Whitlock, E. P. , Orleans, C. T. , Pender, N. , & Allan, J. (2002). Evaluating primary care behavioral counseling interventions: An evidence‐based approach. American Journal of Preventive Medicine, 22(4), 267–284. 10.1016/S0749-3797(02)00415-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


