Abstract
Aim
To explore the prevalence and related factors influencing diabetes stigma among Chinese young and middle‐aged patients with type 2 diabetes.
Design
A cross‐sectional, quantitative study was conducted through questionnaires.
Methods
A total of 453 young and middle‐aged patients with type 2 diabetes were recruited. Questionnaire survey was conducted with convenience sampling from September 2019 to December 2020. This included demographic questionnaire, Type 2 Diabetes Stigma Assessment Scale (DSAS‐2) and Connor–Davidson Resilience Scale (CD‐RISC). The STROBE checklist was applied as the reporting guideline for this study.
Results
The scores of diabetes stigma and resilience of patients were 48.18 ± 14.52 and 66.02 ± 7.18, respectively. Diabetes stigma was negatively correlated with resilience, the correlation coefficient was −0.581. The results showed that the complications, diabetes year, monthly income and insulin treatment are important factors affecting stigma. In addition, it is resilience that was a protective factor of diabetes stigma, explaining 27.2% of the variance in diabetes stigma.
Keywords: nursing, resilience, Stigma, type 2 diabetes, young and middle‐aged patients
1. INTRODUCTION
Diabetes mellitus is a group of clinical syndromes with metabolic disorder characterized by hyperglycaemia, among which type 2 diabetes is the most common, accounting for more than 90% of the diabetic population (Li et al., 2020). According to the statistics of the International Health Organization (WHO) (Roglic, 2016), the global prevalence of diabetes (age‐standardized) has nearly doubled since 1980. Also, the prevalence of diabetes in China has increased nearly 20‐fold in the past 30 years, and the prevalence of diabetes over the age of 18 has reached 11.2% (Li et al., 2020). Studies have shown that the onset of diabetes is concentrated in 40–59 years old (Cho et al., 2018), and these patients are the core force of social development and family life, bearing multiple responsibilities and pressures including family and work. The long‐term medical burden caused by diabetes aggravates the burden of self‐perception, leads to the emergence of negative emotions, affects disease control and physical and mental health (Qin & Qing, 2018) and poses a great challenge to the prevention and treatment of diabetes in China (Jialing et al., 2021). At present, more and more attention has been paid to positive psychology. Its research principally includes positive emotional experience, personality traits and other contents that can help individuals enhance their quality of life, which is of great significance to explore the intervention mechanism of negative emotions.
2. BACKGROUND
Diabetes mellitus is incurable and has many complications, which determines that its treatment goal is to avoid diabetes complications, delay the progression of complications and improve the quality of life of patients (Zhang et al., 2020). However, achieving this treatment goal requires patients with diabetes to have strong self‐management ability, so that no deviation can occur in any link in the long‐term self‐management process; otherwise, it will lead to blood glucose fluctuations and even complications. The young and middle‐aged are the core forces of society and the family, and they are under pressure from family and work. The long‐term medical burden brought by diabetes increases their self‐experience burden and forms a long‐term pressure source for individuals. The patient is in a long‐term nervous and out‐of‐control bad state (Coccaro et al., 2021), triggering a stress response, manifested as a fairly common existence including depression, anxiety, stigma and other diabetes‐related psychological problems (Guo et al., 2019; Zhao et al., 2018). Stigma was first defined as “the feature of a person's reputation being greatly tarnished” (Browne et al., 2016), and it is often extended to the psychological stigma of patients due to certain diseases (Kato et al., 2016; Seo & Song, 2019). Diabetes stigma, as a negative emotion, has an adverse effect on the treatment compliance and self‐management ability of patients with type 2 diabetes, thereby reducing the quality of life of patients (Botchway et al., 2021; Kato et al., 2017; Puhl et al., 2020).
In recent years, with the development of positive psychology, researchers gradually began to pay attention to the role of positive emotional experience and personality characteristics in maintaining patients' mental health. Resilience refers to the ability of individuals to make full use of existing resources and adapt to good and positive development in difficult situations when they are under pressure (Kalisch et al., 2017). Resilience can not only improve individuals' negative emotions (Ran et al., 2020; Scarton et al., 2021) but also have a long‐term impact on improving patients' quality of life and physical and mental health (Hsu et al., 2021). For individuals with high resilience level, they are more able to perceive and mobilize available resources to cope with a difficult environment, and they also have stronger adaptability to buffer the bad psychological state of individuals exposed to stressors and promote their physical and mental health.
In China, most studies on resilience focus on the investigation of negative emotions such as anxiety and depression (Hou et al., 2021; Lau, 2022; Song et al., 2021; Zhang et al., 2020). The research on the resilience of patients with diabetes mainly focuses on the related research on mental resilience and quality of life (Luo, Guo, et al., 2021; Mei et al., 2020). There are few reports on the relationship between resilience and stigma among young and middle‐aged patients with type 2 diabetes mellitus. This study will investigate the resilience and stigma of such patients, clarify the correlation between resilience and diabetic stigma and give reference for reducing the level of stigma and reducing the physical and psychological impact of diabetes on patients.
3. THE STUDY
3.1. Aim
We aimed to determine the effect of resilience on diabetes stigma among young and middle‐aged patients with type 2 diabetes after accounting for confounding factors. Therefore, we hypothesized that individuals with higher resilience were more likely to have lower diabetes stigma.
3.2. Design
A cross‐sectional survey was conducted to select young and middle‐aged patients with type 2 diabetes who were hospitalized or outpatients in the department of endocrinology of a General hospital, Jinzhou city, Liaoning Province, China, from September 2019 to December 2020. The STROBE checklist was used in reporting this study (see Supporting Information).
3.3. Method
3.3.1. Participants
A convenience sample of 453 young and middle‐aged patients with type 2 diabetes from a tertiary hospital in Liaoning, China, was recruited based on the following inclusion criteria: 18–59 years old, being diagnosed with type 2 diabetes, conscious and able to complete the questionnaire independently or with the help of researchers, voluntarily participating in this survey (Figure 1). Patients with combined with other serious physical diseases, combined with neurological diseases or psychiatric history, were excluded.
FIGURE 1.
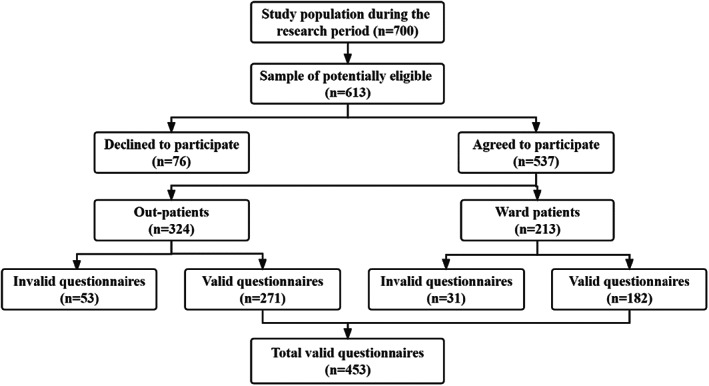
Population flow diagram
3.3.2. Instruments
The questionnaire series includes demographic questionnaire (i.e. gender, age, marital status, education, monthly income, course of illness, etc.) and two mature tools to collect data on diabetes stigma and resilience.
3.3.3. Demographic questionnaire
A thorough literature review was conducted, after which the team designed the demographic questionnaire. Participants were asked to complete 12 self‐reported items, included gender, age, education level, marital status, occupation, monthly income, disease duration, complications, ability to take care of themselves, treatment options, treatment payment methods and the number of hospital admissions.
3.3.4. Diabetes stigma
The Type 2 Diabetes Stigma Assessment Scale (DSAS‐2) was developed by Dr. Browne based on the conceptual model of health‐related diabetes stigma combined with qualitative research on patients with type 2 diabetes (Browne et al., 2016). This study used the Chinese version translated by Yufeng et al. (2017). It includes 19 items to evaluate the stigma of patients with type 2 diabetes in three aspects: the external discriminatory measures against patients with diabetes, the negative stereotypes and evaluations held by the society and the results of stigma caused by the perceived negative attitudes of others. The scale score was measured by Likert grade 5 from extremely inconsistent (1 point) to extremely consistent (5 point). The obtained score ranged from 19–95. The higher the score was, the high the level of the diabetes stigma was. The Cronbach's alpha coefficient of the Chinese version of the DSAS‐2 was verified to be 0.879.
3.3.5. Resilience
The Connor–Davidson Resilience Scale (CD‐RISC) was compiled by American psychologists Connor and Davidson (2003). The scale is widely used to assess the resilience of the general population and clinical patients and has a strong universality. This study used the Chinese vision CD‐RISC which was translated by Xiaonan and Jianxin (2007). There were 25 items from three dimensions in the CD‐RISC, perseverance, self‐reliance and optimism. The scale score was measured by Likert grade 5 from not at all (0 point) to always (4 point). The obtained score ranged from 0–100. The higher the score was, the high the level of resilience was. The Chinese version of the scale has achieved good reliability and validity in the application of patients with diabetes. The Chinese vision of the CD‐RISC Cronbach's alpha coefficient is 0.916 (Yang & Jingping, 2016).
3.4. Data collection
The research team consisted of one diabetes nurse and three graduate students, all of whom had passed uniform training. The researchers distributed questionnaires on site. The patients who met the inclusion criteria signed informed consent forms after explaining the purpose of the survey, requirements and filling methods of the questionnaire. The questionnaires were filled in anonymously and returned on the spot after completion, and the patients were timely informed of any omissions. According to Kendall's (1975) sample calculation method, samples were measured to be 5–10 times the number of scale items with the most items. The Connor–Davidson Resilience Scale consists of 25 items, taking into account a 20% sample loss. As a result, the calculated sample size was at least 150–300. A total of 465 questionnaires with missing data were distributed in this study, and 453 valid questionnaires were recovered, with an effective rate of 97.4%, meeting the sample size requirements.
3.5. Data analysis
SPSS 25.0 statistical analysis software was used for data analysis. Descriptive statistics were calculated to develop descriptive demographic data. Analysis of variance (T/F test) was used for group comparisons. Pearson correlation was used to analyse the relationship between diabetes stigma and resilience. Hierarchical regression analysis was used to identify influencing factors of diabetes stigma (α enter = 0.05, α remove = 0.10). The alpha level for significance in all analyses was determined to be p < .05.
3.6. Ethics
After being informed of the purpose of the study, data collection methods and ethical principles such as confidentiality, anonymity and voluntary opt‐out, all participants agreed in writing to participate voluntarily. In accordance with the Declaration of Helsinki, the study was approved by the Ethical Research Committee of Jinzhou Medical University (JZMULL2022009).
4. RESULTS
4.1. Background characteristics
Table 1 shows the detailed demographic characteristics of 453 patients, including 204 male and 249 female; the mean age was 43.11 ± 11.26; 331 (73.1%) were married. Most of them (219 cases, 36.2%) had a monthly income of less than 3,000 yuan. Median duration was 10 years (P25 = 5, P75 = 18), with a range of 1–26 years. One‐hundred and seventy‐five patients had complications of diabetes. Most patients had normal self‐care ability (363 cases, 38.6%). Three‐hundred forty‐four patients received insulin treatment; Among medical payment methods, urban/employee medical insurance accounted for 383 cases (84.6%); the median number of admissions was 2 (P25 = 1, P75 = 4), with a range of 0–15.
TABLE 1.
Participants' Characteristics (n = 453)
| Variables | n | % |
|---|---|---|
| Gender | ||
| Male | 204 | 45.0 |
| Female | 249 | 55.0 |
| Education background | ||
| Primary and below | 57 | 12.6 |
| Junior high school | 130 | 28.7 |
| Senior high school | 136 | 30.0 |
| College degree or above | 130 | 28.7 |
| Marital status | ||
| Married | 337 | 73.1 |
| Unmarried | 116 | 26.9 |
| Occupation | ||
| Civil servants | 72 | 15.9 |
| Staffer | 63 | 13.9 |
| Worker | 191 | 42.2 |
| Farmer | 88 | 19.4 |
| Freelance | 19 | 8.6 |
| Self‐care ability | ||
| Fully care | 363 | 38.6 |
| Partial dependency | 69 | 15.7 |
| Full dependency | 21 | 11.5 |
| Monthly income (yuan) | ||
| Less than 3,000 | 219 | 48.3 |
| 3,001–4,999 | 164 | 36.2 |
| More than 5,000 | 70 | 15.5 |
| Diabetes year | ||
| 1 | 83 | 18.3 |
| 2–10 | 187 | 41.3 |
| 11–20 | 145 | 32.0 |
| ≥21 | 38 | 8.4 |
| The occurrence of complications | ||
| Yes | 175 | 38.6 |
| No | 278 | 61.4 |
| Insulin treatment | ||
| Yes | 344 | 75.9 |
| No | 109 | 24.1 |
| Medical payment method | ||
| Free medical care | 16 | 3.5 |
| Urban/employee medical insurance | 383 | 84.5 |
| New Rural Cooperative Medical System (NCMS) | 54 | 11.9 |
4.2. Diabetes stigma and resilience among young and middle‐aged patients with type 2 diabetes mellitus
The total score of diabetes stigma among young and middle‐aged patients with type 2 diabetes was (48.18 ± 14.52), in which the scores of different dimensions were (16.83 ± 5.59), (15.60 ± 5.31) and (15.75 ± 5.16). The total score of resilience in young and middle‐aged patients with type 2 diabetes was (66.02 ± 7.18), in which the scores of various dimensions were: tenacity (35.47 ± 4.94), self‐improvement (21.15 ± 2.12), optimism (10.40 ± 1.22). See Table 2 for details.
TABLE 2.
Current status of diabetes stigma and resilience among young and middle‐aged patients with type 2 diabetes (, n = 453)
| Variables | Total average score | Item average score |
|---|---|---|
| Diabetes stigma | 48.18 ± 14.52 | 2.54 ± 0.76 |
| Treated differently | 16.83 ± 5.59 | 2.40 ± 0.80 |
| Blame and judgement | 15.60 ± 5.31 | 2.60 ± 0.89 |
| Self‐diabetes stigma | 15.75 ± 5.16 | 2.62 ± 0.86 |
4.3. Single‐factor analysis of diabetes stigma among young and middle‐aged patients with type 2 diabetes mellitus
Table 3 shows the diabetes stigma score distribution of young and middle‐aged patients with type 2 diabetes mellitus. There were significant differences between the diabetes stigma scores of patients education level, marital status, complications, monthly income, course of the disease, self‐care ability and insulin treatment (p < .05).
TABLE 3.
Distribution of diabetes stigma score with different demographic characteristics (, n = 453)
| Items | Diabetes stigma | F/t | p‐value |
|---|---|---|---|
| Gender | 1.106 | .269 | |
| Male | 49.01 ± 14.48 | ||
| Female | 47.50 ± 14.55 | ||
| Education level | 3.908 | .009 | |
| Primary and below | 49.82 ± 18.20 | ||
| Junior high school | 51.11 ± 15.15 | ||
| Senior high school | 45.34 ± 11.51 | ||
| College degree or above | 47.51 ± 14.44 | ||
| Marital status | −2.093 | .037 | |
| Married | 47.32 ± 14.02 | ||
| Unmarried | 50.52 ± 15.62 | ||
| Occupation | 1.726 | .071 | |
| Civil servants | 46.19 ± 14.01 | ||
| Staffer | 45.00 ± 11.04 | ||
| Worker | 50.04 ± 15.41 | ||
| Farmer | 49.00 ± 16.07 | ||
| Freelance | 46.05 ± 10.76 | ||
| Self‐care ability | 12.441 | .001 | |
| Fully care | 46.79 ± 13.81 | ||
| Partial dependency | 51.57 ± 15.46 | ||
| Full dependency | 61.10 ± 15.81 | ||
| Monthly income (yuan) | 3.697 | .026 | |
| Less than 3,000 | 49.66 ± 15.23 | ||
| 3,001–4,999 | 47.86 ± 14.00 | ||
| More than 5,000 | 44.31 ± 12.78 | ||
| Diabetes year | 4.723 | .008 | |
| 1 | 50.89 ± 15.09 | ||
| 2–10 | 49.69 ± 14.91 | ||
| 11–20 | 45.12 ± 12.79 | ||
| ≥21 | 46.50 ± 15.83 | ||
| The occurrence of complications | 5.582 | .001 | |
| Yes | 52.83 ± 16.33 | ||
| No | 45.26 ± 12.43 | ||
| Insulin treatment | 3.445 | .001 | |
| Yes | 49.49 ± 14.38 | ||
| No | 44.06 ± 14.25 | ||
| Medical payment method | 0.601 | .549 | |
| Free medical care | 45.31 ± 13.59 | ||
| Medical insurance in urban areas | 48.09 ± 14.16 | ||
| New Rural Cooperative Medical System (NCMS) | 49.67 ± 17.23 |
4.4. The correlations between diabetes stigma and resilience
Table 4 shows the correlation between diabetes stigma and resilience among young and middle‐aged patients with type 2 diabetes. The total score and dimensions of stigma were significantly negatively correlated with the total score and dimensions of resilience scale (r = −.431 ~ −.581, p < .001).
TABLE 4.
Correlation between diabetes stigma and resilience among young and middle‐aged patients with type 2 diabetes (r‐value, n = 453)
| Diabetes stigma | Treated differently | Blame and judgement | Self‐stigma | |
|---|---|---|---|---|
| Resilience | −0.581** | −0.514** | −0.522** | −0.540** |
| Tenacity | −0.493** | −0.437** | −0.444** | −0.458** |
| Strength | −0.532** | −0.468** | −0.484** | −0.494** |
| Optimism | −0.490** | −0.441** | −0.431** | −0.458** |
p < .001.
4.5. Multivariate stratified linear regression analysis of diabetes stigma among young and middle‐aged patients with type 2 diabetes mellitus
Table 5 shows multivariate stratified linear regression analysis was used to explore the influence factors of diabetes stigma, stigma the young and middle‐aged patients with type 2 diabetes disease score as the dependent variable, the model 1 in marital status, income, diabetes year, complications, self‐care ability and insulin treatment as independent variables, model 2 into the correlation analysis with statistical significance in resilience scores as independent variables, resilience could independently explain 27.2% of the variance of diabetes stigma (p < .05) (Table 6).
TABLE 5.
Multivariate stratified linear regression analysis of influencing factors of diabetes stigma (n = 453)
| Variables | B | SE | β | t | p | 95% CI |
|---|---|---|---|---|---|---|
| Model 1 | ||||||
| The occurrence of complications | −7.82 | 1.40 | −0.26 | −5.61 | <.001 | −10.56 ~ −5.08 |
| Diabetes year | −3.04 | 0.77 | −0.11 | −3.97 | <.001 | −4.72 ~ −1.74 |
| Monthly income | −2.25 | 0.88 | −0.11 | −2.18 | .011 | −3.98 ~ −0.51 |
| Insulin treatment | −3.39 | 1.56 | −0.10 | −2.18 | .030 | −6.45 ~ −0.33 |
| Model 2 | ||||||
| The occurrence of complications | −5.23 | 1.18 | −0.18 | −4.46 | <.001 | −7.54 ~ −2.92 |
| Diabetes year | −1.92 | 0.64 | −0.11 | −3.01 | .003 | −3.17 ~ −0.37 |
| Monthly income | −1.81 | 0.74 | −0.09 | −2.46 | .014 | −3.25 ~ −0.37 |
| Insulin treatment | −2.95 | 1.30 | −0.09 | −2.28 | .023 | −5.50 ~ −0.40 |
| Resilience | −1.08 | 0.08 | −0.53 | −14.17 | <.001 | −1.23 ~ −0.93 |
Abbreviations: CI, confidence interval; SE, standard error.
TABLE 6.
Summary results of the hierarchical regression analysis model
| Model | R | R 2 | Adjusted R 2 | F | p |
|---|---|---|---|---|---|
| 1 | 0.352 | 0.124 | 0.116 | 15.807 | <.001 |
| 2 | 0.629 | 0.395 | 0.388 | 58.409 | <.001 |
5. DISCUSSION
5.1. Current status of diabetes stigma among young and middle‐aged patients with type 2 diabetes
This study showed that the total score of diabetes stigma among young and middle‐aged patients with type 2 diabetes was 48.18 ± 14.52, which was at a medium level and lower than that reported by Wei et al. (2020) and Zhaofang et al. (2020). Diabetes has a long course and many comorbidities. When patients face long‐term and tedious self‐care, they have psychological pressure, which makes patients prone to suffering and other psychological experience. China has a long‐standing stereotype that diabetes is equal to a disease of wealth (Jaacks et al., 2015). Patients with diabetes are usually considered to lack restraint, lazy and irresponsible for their own health. These negative social evaluations of the disease and patients can easily lead to and increase the stigma of the disease. Diabetes stigma is essentially rooted in social relationships and is affected by social economy and culture (Weiwei et al., 2021). When suffering from the negative impact of stigma in life, good social support for young and middle‐aged patients with diabetes can buffer the patient's acute stress state, which can alleviate the stigma of young and middle‐aged patients to a certain extent.
5.2. Influencing factors of diabetes stigma of type 2 diabetes mellitus among young and middle‐aged patients
This study showed that young and middle‐aged patients with type 2 diabetes who had complications, a short diabetes year, low monthly income and received insulin treatment had a higher level of diabetes stigma (p < .05). Young and middle‐aged patients with type 2 diabetes with complications have a higher degree of diabetes stigma, which is consistent with previous studies (Smith‐Miller et al., 2017). People around you will understand the cause of diabetes‐related complications as the lack of self‐management ability of patients, and patients will also attribute it to self‐factors, resulting in inherent stigma. In addition, the patient's heavy burden of disease treatment has also led to increased psychological pressure and aggravated diabetes stigma. Young and middle‐aged patients with type 2 diabetes who have a shorter diabetes year have a stronger sense of diabetes stigma. (Hansen et al., 2020). Young and middle‐aged patients with type 2 diabetes with shorter diabetes year have insufficient knowledge of the disease, fear and anxiety about the complications caused by poor disease control and worry that the cost of life‐long treatment will bring an economic burden to the family economy. When the cause of the disease occurs, it is easily affected by the actual stigma in the surrounding environment and feels self‐blame for the bad living habits before the diagnosis, which causes the patient to have an internal stigma and a strong diabetes stigma. Middle‐aged and young patients with type 2 diabetes who received insulin treatment had a higher level of diabetes stigma, which was consistent with previous studies (Holmes‐Truscott et al., 2018; Liu et al., 2017). In the course of long‐term insulin treatment, some patients, in order to conceal their condition, reduce or refuse group activities by avoiding and hiding, which affects the social activities and work of the patients. In addition, the long‐term use of insulin treatment affects the daily life of patients to a certain extent, aggravates the psychological burden of patients and causes aggravation of patients' diabetes stigma. The lower the monthly income, the more severe the diabetes stigma of the patient. The limited monthly income prevents the patient from having sufficient financial conditions to support him to obtain more medical resources and disease‐related knowledge. In addition, the economic burden of the patient due to disease treatment and daily life is relatively higher. This is consistent with related studies (Jing et al., 2020; Whittle et al., 2017).
This study focused on how young and middle‐aged patients with type 2 diabetes deal with diabetes stigma and explored its influence on stigma from the perspective of resilience. Our study showed that the three dimensions of resilience, tenacity, self‐reliance and optimism, are all related to stigma, that is, resilience is an important protective factor for the occurrence of stigma among young and middle‐aged patients with type 2 diabetes, and the stronger the individual's resilience, the lower the degree of stigma. Individuals with strong psychological resilience have higher confidence level and emotional function when facing pressure, which can prevent and reduce the impact of negative emotions (Dubois et al., 2020; Luo, Gu, et al., 2021), which is consistent with our research results. Therefore, when there is a higher resilience, patients can effectively buffer the negative impact of stressful life events, avoid negative emotions and relieve patients' stigma by integrating the ability of goal setting, behaviour control and decision‐making. This study suggests that patients should pay more attention to their psychological status, encourage patients to share difficulties, guide patients to actively seek help from medical staff and family, improve their coping ability and recovery ability, so that they can effectively resist stigma.
5.3. Strategies for coping with diabetes stigma among young and middle‐aged patients with type 2 diabetes
Diabetes stigma among young and middle‐aged patients with type 2 diabetes poses a serious threat to their physical and mental condition and quality of life, increasing the risk of poor prognosis (Kato et al., 2016). First of all, medical staff can combine “mindfulness‐based cognitive behavioural therapy” (Christopher et al., 2018), peer support (Pillen & Ward, 2021) and other intervention methods to help patients improve their resilience, actively adjust their psychological state and stress coping styles and relieve their diabetes stigma. Second, the nursing staff can strengthen related to young and middle‐aged patients with disease treatment and management of information communication and emotional communication, to improve patients' diabetes stigma related to cognition and response ability, help patients set up the confidence of the disease management, guiding the correct response to negative emotions, reduce the stress associated with disease, to alleviate the disease stigma. Finally, medical staff and social media can popularize diabetes knowledge to the public, break the stereotype of insulin treatment and avoid discrimination. By setting up “diabetes management rooms” in public areas, patients can avoid the embarrassment of managing blood glucose in front of people, increase the sense of privacy of insulin injection and then alleviate the diabetes stigma.
5.4. Limitations
It must be noted that the limitations of this study are convenience sampling, and all data are collected through self‐report, which is not conducive to the generalization of results. The participants in our study were all from Liaoning Province, China, which is a geographical limitation, and future studies could examine this relationship based on more typical samples from multiple regions and seek to collect data from multiple sources, such as caregivers, to make the results more representative. It should also be noted that cross‐sectional studies cannot discern causal relationships between variables and only allow the identification of some relationships without causal effects. This conclusion needs to be further verified in future longitudinal follow‐up studies.
Theoretically, through exploring the influencing factors of stigma among young and middle‐aged patients with type 2 diabetes, this study found the protective factors of resilience on stigma, which enriched the knowledge of previous studies and helped to further understand the relationship between diabetes stigma and resilience. These findings are crucial for maintaining the physical and mental health of young and middle‐aged patients with type 2 diabetes.
6. CONCLUSION
The diabetes stigma of young and middle‐aged patients with type 2 diabetes was at a moderate level. Healthcare providers should explore appropriate psychological intervention modes to improve resilience, reduce diabetes stigma and promote patients' recovery.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
In accordance with the Declaration of Helsinki, the study was approved by the Ethical Research Committee of Jinzhou Medical University. All participants or their authorized agents agreed in writing to participate voluntarily after being informed of the purpose of the study, data collection methods and ethical principles such as confidentiality, anonymity and voluntary opt‐out.
Supporting information
STROBE Checklist
ACKNOWLEDGEMENTS
Thanks to the patients who participated in this study and also to the head nurse for her strong support of sample collection.
Zhang, Y.‐B. , Yang, Z. , Zhang, H.‐J. , Xu, C.‐Q. , & Liu, T. (2023). The role of resilience in diabetes stigma among young and middle‐aged patients with type 2 diabetes. Nursing Open, 10, 1776–1784. 10.1002/nop2.1436
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Botchway, M. , Davis, R. E. , Merchant, A. T. , Appiah, L. T. , & Moore, S. (2021). Diabetes‐related stigma and its influence on social networks, social support, and HbA1c in Ghana. Ethnicity & Disease, 31(1), 57–66. 10.18865/ed.31.1.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne, J. L. , Ventura, A. D. , Mosely, K. , & Speight, J. (2016). Measuring the stigma surrounding type 2 diabetes: Development and validation of the type 2 Diabetes Stigma Assessment Scale (DSAS‐2). Diabetes Care, 39(12), 2141–2148. 10.2337/dc16-0117 [DOI] [PubMed] [Google Scholar]
- Cho, N. H. , Shaw, J. E. , Karuranga, S. , Huang, Y. , da Rocha Fernandes, J. D. , Ohlrogge, A. W. , & Malanda, B. (2018). IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice, 138, 271–281. 10.1016/j.diabres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- Christopher, M. S. , Hunsinger, M. , Goerling, L. R. J. , Bowen, S. , Rogers, B. S. , Gross, C. R. , Dapolonia, E. , & Pruessner, J. C. (2018). Mindfulness‐based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psychiatry Research, 264, 104–115. 10.1016/j.psychres.2018.03.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro, E. F. , Lazarus, S. , Joseph, J. , Wyne, K. , Drossos, T. , Phillipson, L. , & de Groot, M. (2021). Emotional regulation and diabetes distress in adults with type 1 and type 2 diabetes. Diabetes Care, 44(1), 20–25. 10.2337/dc20-1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor, K. M. , & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor‐Davidson Resilience Scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Dubois, S. K. , Lehrer, H. M. , Whyne, E. Z. , & Steinhardt, M. A. (2020). A resilience intervention for adults with type 2 diabetes: Proof‐of‐concept in community health centers. International Journal of Behavioral Medicine, 27(5), 565–575. 10.1007/s12529-020-09894-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, J. , Yang, J. , Wiley, J. , Ou, X. , Zhou, Z. , & Whittemore, R. (2019). Perceived stress and self‐efficacy are associated with diabetes self‐management among adolescents with type 1 diabetes: A moderated mediation analysis. Journal of Advanced Nursing, 75(12), 3544–3553. 10.1111/jan.14179 [DOI] [PubMed] [Google Scholar]
- Hansen, U. M. , Olesen, K. , & Willaing, I. (2020). Diabetes stigma and its association with diabetes outcomes: A cross‐sectional study of adults with type 1 diabetes. Scandinavian Journal of Public Health, 1403494819862941, 855–861. 10.1177/1403494819862941 [DOI] [PubMed] [Google Scholar]
- Holmes‐Truscott, E. , Browne, J. L. , Ventura, A. D. , Pouwer, F. , & Speight, J. (2018). Diabetes stigma is associated with negative treatment appraisals among adults with insulin‐treated Type 2 diabetes: Results from the second Diabetes MILES – Australia (MILES‐2) survey. Diabetic Medicine, 35(5), 658–662. 10.1111/dme.13598 [DOI] [PubMed] [Google Scholar]
- Hou, W. K. , Tong, H. , Liang, L. , Li, T. W. , Liu, H. , Ben‐Ezra, M. , Goodwin, R. , & Lee, T. M. (2021). Probable anxiety and components of psychological resilience amid COVID‐19: A population‐based study. Journal of Affective Disorders, 282, 594–601. 10.1016/j.jad.2020.12.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, H. C. , Chen, S. Y. , Lee, Y. J. , Chen, W. Y. , & Wang, R. H. (2021). Pathways of diabetes distress, decisional balance, self‐efficacy and resilience to quality of life in insulin‐treated patients with type 2 diabetes: A 9‐month prospective study. Journal of Clinical Nursing, 30(7–8), 1070–1078. 10.1111/jocn.15652 [DOI] [PubMed] [Google Scholar]
- Jaacks, L. M. , Liu, W. , Ji, L. , & Mayer‐Davis, E. J. (2015). Type 1 diabetes stigma in China: A call to end the devaluation of individuals living with a manageable chronic disease. Diabetes Research and Clinical Practice, 107(2), 306–307. 10.1016/j.diabres.2014.12.002 [DOI] [PubMed] [Google Scholar]
- Jialing, X. , Shuqin, J. , Lili, Z. , Yan, W. , Yu, L. , & Xiaowan, W. (2021). Visual analysis of the status quo and hot spots of diabetes distress research at homeand abroad from 2010 to 2020. Nursing Journal of Chinese People's Liberation Army, 38(12), 57–60. 10.3969/j.issn.1008-9993.2021.12.015 [DOI] [Google Scholar]
- Jing, Y. , Honghua, G. , Minxiang, L. , & Caihong, Z. (2020). Prevalence and influencing factors of diabetic‐related stigma. Nursing Journal of Chinese People's Liberation Army, 37(7), 20–23, 28. [Google Scholar]
- Kalisch, R. , Baker, D. G. , Basten, U. , Boks, M. P. , Bonanno, G. A. , Brummelman, E. , Chmitorz, A. , Fernàndez, G. , Fiebach, C. J. , Galatzer‐Levy, I. , Geuze, E. , Groppa, S. , Helmreich, I. , Hendler, T. , Hermans, E. J. , Jovanovic, T. , Kubiak, T. , Lieb, K. , Lutz, B. , … Kleim, B. (2017). The resilience framework as a strategy to combat stress‐related disorders. Nature Human Behaviour, 1(11), 784–790. 10.1038/s41562-017-0200-8 [DOI] [PubMed] [Google Scholar]
- Kato, A. , Fujimaki, Y. , Fujimori, S. , Isogawa, A. , Onishi, Y. , Suzuki, R. , Yamauchi, T. , Ueki, K. , Kadowaki, T. , & Hashimoto, H. (2017). Psychological and behavioural patterns of stigma among patients with type 2 diabetes: A cross‐sectional study. BMJ Open, 7(3), e013425. 10.1136/bmjopen-2016-013425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato, A. , Fujimaki, Y. , Fujimori, S. , Izumida, Y. , Suzuki, R. , Ueki, K. , Kadowaki, T. , & Hashimoto, H. (2016). A qualitative study on the impact of internalized stigma on type 2 diabetes self‐management. Patient Education and Counseling, 99(7), 1233–1239. 10.1016/j.pec.2016.02.002 [DOI] [PubMed] [Google Scholar]
- Kendall, M. (1975). Multivariate analysis. Charles Griffin. [Google Scholar]
- Lau, W. K. W. (2022). The role of resilience in depression and anxiety symptoms: A three‐wave cross‐lagged study. Stress and Health, 38, 804–812. 10.1002/smi.3136 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Teng, D. , Shi, X. , Qin, G. , Qin, Y. , Quan, H. , Shi, B. , Sun, H. , Ba, J. , Chen, B. , Du, J. , He, L. , Lai, X. , Li, Y. , Chi, H. , Liao, E. , Liu, C. , Liu, L. , Tang, X. , … Shan, Z. (2020). Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: National cross sectional study. BMJ, 369, m997. 10.1136/bmj.m997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, N. F. , Brown, A. S. , Folias, A. E. , Younge, M. F. , Guzman, S. J. , Close, K. L. , & Wood, R. (2017). Stigma in people with type 1 or type 2 diabetes. Clinical Diabetes, 35(1), 27–34. 10.2337/cd16-0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, D. , Gu, W. , Bao, Y. , Cai, X. , Lu, Y. , Li, R. , Wang, Y. , & Li, M. (2021). Resilience outstrips the negative effect of caregiver burden on quality of life among parents of children with type 1 diabetes: An Application of Johnson‐Neyman Analysis. Journal of Clinical Nursing, 30(13–14), 1884–1892. 10.1111/jocn.15739 [DOI] [PubMed] [Google Scholar]
- Luo, J. , Guo, J. , Yang, J. , Ou, X. , & Grey, M. (2021). Parent‐child relationship quality as a mediator of the association between perceived stress and diabetes self‐management in adolescents with type 1 diabetes. Journal of Family Nursing, 27(1), 73–82. 10.1177/1074840720971584 [DOI] [PubMed] [Google Scholar]
- Mei, H. , Yuanyuan, L. , Shuping, L. , & Lu, X. (2020). The mediating role of psychological elasticity in the relationship between perceived stress and quality of life in patients with diabetes. Chinese Preventive Medicine, 21(11), 1193–1197. 10.16506/j.1009-6639.2020.11.007 [DOI] [Google Scholar]
- Pillen, H. , & Ward, P. R. (2021). How might diabetes organisations address diabetes‐related stigma? Findings from a deliberative democratic case study. Health expectations, 1–10. 10.1111/hex.13398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl, R. M. , Himmelstein, M. S. , Hateley‐Browne, J. L. , & Speight, J. (2020). Weight stigma and diabetes stigma in U.S. adults with type 2 diabetes: Associations with diabetes self‐care behaviors and perceptions of health care. Diabetes Research and Clinical Practice, 168, 108387. 10.1016/j.diabres.2020.108387 [DOI] [PubMed] [Google Scholar]
- Qin, C. , & Qing, F. (2018). Stigma in young and middle‐aged diabetic patients: Qualitative study. Nursing Journal of Chinese People's Liberation Army, 35(23), 12–16. 10.3969/j.issn.1008-9993.2018.23.003 [DOI] [Google Scholar]
- Ran, L. , Wang, W. , Ai, M. , Kong, Y. , Chen, J. , & Kuang, L. (2020). Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID‐19: A study of the general population in China at the peak of its epidemic. Social Science & Medicine, 262, 113261. 10.1016/j.socscimed.2020.113261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roglic, G. (2016). WHO Global report on diabetes: A summary. International Journal of Noncommunicable Diseases, 1, 3. 10.4103/2468-8827.184853 [DOI] [Google Scholar]
- Scarton, L. , Hebert, L. E. , Goins, R. T. , Umans, J. G. , Jiang, L. , Comiford, A. , Chen, S. , White, A. , Ritter, T. , & Manson, S. M. (2021). Diabetes and health‐related quality of life among American Indians: The role of psychosocial factors. Quality of Life Research, 30(9), 2497–2507. 10.1007/s11136-021-02830-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo, K. , & Song, Y. (2019). Self‐stigma among Korean patients with diabetes: A concept analysis. Journal of Clinical Nursing, 28(9–10), 1794–1807. 10.1111/jocn.14789 [DOI] [PubMed] [Google Scholar]
- Smith‐Miller, C. A. , Berry, D. C. , & Miller, C. T. (2017). Diabetes affects everything: Type 2 diabetes self‐management among Spanish‐speaking hispanic immigrants. Research in Nursing & Health, 40(6), 541–554. 10.1002/nur.21817 [DOI] [PubMed] [Google Scholar]
- Song, H. , Zhang, M. , Wang, Y. , Yang, L. , Wang, Y. , & Li, Y. (2021). The impact of resilience on anxiety and depression among grass‐roots civil servants in China. BMC Public Health, 21(1), 710. 10.1186/s12889-021-10710-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei, W. , Junmei, Z. , Jie, W. , Wenzhen, H. , Li, L. , & Yinghua, L. (2020). Relationship among stigma, depression and glucose control among patients with type 2 diabetes mellitus. Journal of Nursing Science, 35(12), 75–78. [Google Scholar]
- Weiwei, X. , Peiru, Z. , Qing, Y. , Shuyin, L. , & Yanfen, L. (2021). Status quo of the relationship between stigma and psychological insulin resistance in diabetics and its influencing factors. Nursing Journal of Chinese People's Liberation Army, 38(6), 22–26. [Google Scholar]
- Whittle, H. J. , Palar, K. , Ranadive, N. A. , Turan, J. M. , Kushel, M. , & Weiser, S. D. (2017). “The land of the sick and the land of the healthy”: Disability, bureaucracy, and stigma among people living with poverty and chronic illness in the United States. Social Science & Medicine, 190, 181–189. 10.1016/j.socscimed.2017.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiaonan, Y. , & Jianxin, Z. (2007). A comparison between the Chinese version of Ego‐Rsiliency Scale and Connor‐Davidson Resilience Scale. Psychological Science, 5(35), 1169–1171. [Google Scholar]
- Yang, L. , & Jingping, Z. (2016). Reliability and validity of the Chinese version of Connor‐ Davidson Resilience Scale among diabetes patients. Chinese General Practice, 19(10), 1188–1193. 10.3969/j.issn.1007-9572.2016.10.017 [DOI] [Google Scholar]
- Yufeng, L. , Hongwen, M. , Renan, H. , Jaclyn, C. , & Changde, J. (2017). Reliability and validity of the Chinese version of the Type 2 Diabetes Stigma Assessment Scale. Chinese Journal of Practical Nursing, 33(30), 2343–2347. 10.3760/cma.j.issn.1672-7088.2017.30.006 [DOI] [Google Scholar]
- Zhang, J. , Yang, Z. , Wang, X. , Li, J. , Dong, L. , Wang, F. , Li, Y. , Wei, R. , & Zhang, J. (2020). The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID‐19 in China: A cross‐sectional study. Journal of Clinical Nursing, 29(21–22), 4020–4029. 10.1111/jocn.15425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, F. F. , Suhonen, R. , Katajisto, J. , & Leino‐Kilpi, H. (2018). The association of diabetes‐related self‐care activities with perceived stress, anxiety, and fatigue: A cross‐sectional study. Patient Preference and Adherence, 12, 1677–1686. 10.2147/PPA.S169826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhaofang, Y. , Cong, W. , & Qingmei, J. (2020). Stigma and its influencing factors in young patients with type 2 diabetes mellitus. Preventive Medicine, 32(12), 1246–1249. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
STROBE Checklist
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


