Abstract
Objective
There is limited information on changes in the patterns of care and outcomes for patients who had vascular procedures after the first wave of the COVID-19 pandemic. The aim of this population based study was to examine the patterns of care and outcomes for vascular lower limb procedures in the UK during the COVID-19 pandemic.
Methods
Lower limb revascularisations and major amputations performed from January 2019 to April 2021 in the UK and entered in the National Vascular Registry were included in the study. The primary outcome was in hospital post-operative death and secondary outcomes were complications and re-interventions. The study was divided into Pre-pandemic (1 January 2019 – 29 February 2020), Wave 1 (1 March – 30 June 2020), Respite (1 July – 31 October 2020), Wave 2/3 (1 November 2020 – 30 April 2021).
Results
The study included 36 938 procedures (7 245 major amputations, 16 712 endovascular, 12 981 open revascularisations), with 15 501 procedures after March 2020, a 27.7% reduction compared with pre-pandemic. The proportion of open surgical procedures performed under general anaesthetic was lower in Wave 1 and after compared with pre-pandemic (76.7% vs. 81.9%, p < .001). Only 4.6% of patients in the cohort had SARS-CoV-2 infection (n = 708), but their in hospital post-operative mortality rate was 25.0% (n = 177), six times higher than patients without SARS-CoV-2 (adjusted odds ratio 5.88; 95% CI 4.80 – 7.21, p < .001). The in hospital mortality rate was higher during the pandemic than pre-pandemic after elective open and endovascular revascularisation (respectively 1.6% vs. 1.1%, p = .033, and 0.9% vs. 0.5%, p = .005) and after major amputations (10.4% during Wave 2/3 vs. 7.7% pre-pandemic, p = .022).
Conclusion
There was excess post-operative mortality rate for patients undergoing lower limb vascular procedures during the pandemic, which was associated with SARS-CoV-2 infections. Further research should be conducted on long term outcomes of patients operated on during the COVID-19 pandemic period.
Keywords: Amputation, COVID-19, Peripheral arterial disease, Revascularisation, United Kingdom Vascular surgery
What this paper adds.
This population based cohort study examined the patterns of care and surgical outcomes for lower limb vascular procedures in the UK during the COVID-19 pandemic. It included 36 938 lower limb revascularisation and major amputation procedures performed from January 2019 to April 2021. Emergency procedures for severe limb ischaemia continued to be performed. The overall in hospital mortality rates after elective revascularisations and major amputations were significantly higher during the pandemic compared with pre-pandemic levels. The excess mortality rate was significantly associated with SARS-CoV-2 infection, after adjusting for changes in the mix of patients undergoing treatment or problems of access to hospital facilities.
Introduction
In March 2020, the World Health Organisation declared a global pandemic in response to the spread of coronavirus SARS-CoV-2.1 The pandemic had a significant impact on the delivery of surgical services worldwide, due to the limited access to critical care and operating facilities as well as staff redeployment. In the UK, a national lockdown was implemented from March to June 2020, followed by two additional lockdowns between November 2020 and February 2021,2 in response to the emergence of a new SARS-CoV-2 variant. For vascular surgery, the National Health Service (NHS) in England and the Vascular Society of Great Britain & Ireland issued guidance recommending the deferral of elective surgery and consideration of therapeutic options with minimal need for post-operative critical care for emergency procedures, in order to preserve healthcare resources and reduce patient exposure to hospital.3 The American College of Surgeons published similar recommendations regarding the review and postponement of elective procedures.4
Changes in the provision of vascular services in response to the pandemic have been documented through surveys of healthcare professionals and institutional reviews.5, 6, 7 Outcomes such as post-operative complications and death after vascular interventions during the COVID-19 pandemic have also been explored in the COvid-19 Vascular sERvice (COVER) Tier 2 multicentre study,8 the COVID-VAS study,9 as well as other single centre and registry studies.10, 11, 12, 13 However, most studies had a small sample of patients and focused on the first wave of the pandemic that started in March 2020, and did not extend to late 2020 and 2021.
The aim of this study was to examine patterns of care and short term outcomes of lower limb vascular procedures performed in the UK during the pandemic compared with a pre-pandemic period.
Materials and Methods
This population based study used data submitted in the National Vascular Registry (NVR), a national clinical audit collecting demographic and clinical information on five major vascular procedures (abdominal aortic aneurysm, carotid endarterectomy, lower limb bypass and endarterectomy, angioplasty, and major amputation) undertaken within NHS hospitals in the UK.14 The NVR captures 81% of open surgical revascularisations, 49% of endovascular revascularisations, and 88% of major amputations in the UK.15 The study involved secondary analysis of existing pseudo-anonymised data and therefore was exempt from NHS Ethics Committee approval. Results are presented in accordance with the Strengthening the Reporting of Observational Studies (STROBE) Statement for cohort studies.16
Study population
The study cohort comprised adult patients who underwent lower limb open or endovascular revascularisation or major amputation procedures, performed in NHS hospitals between 1 January 2019 and 30 April 2021. Open revascularisation procedures consisted of lower limb bypasses and endarterectomies with or without an endovascular component (hybrid), and endovascular procedures included balloon angioplasties with or without stent. If multiple procedures were performed on different dates during a single hospital admission, the first procedure was analysed as the index procedure, and the subsequent procedures were considered re-interventions. Patient records were excluded if data were missing on key variables (age, comorbidities, smoking status, indication for surgery, and procedure details).
Patient characteristics
The NVR dataset contained demographic (patient age at surgery, sex, comorbidities, smoking status) and clinical information (indication for intervention, Fontaine score, date of admission, admission method, date and type of intervention, anaesthetic type), as well as post-operative in hospital patient outcomes. Information on comorbidities included the presence of diabetes mellitus, chronic obstructive pulmonary disease (COPD), ischaemic heart disease (IHD), chronic heart failure (CHF), chronic kidney disease (CKD), and stroke. It also included the patient’s SARS-CoV-2 status (positive polymerase chain reaction or lateral flow test pre- or post-operatively, COVID-19 symptoms, which were added as data items in April 2020). Patients were considered to have SARS-CoV-2 infection if they had a positive test at any point during the admission or a clinical diagnosis was made based on COVID-19 symptoms.
Indications for intervention included chronic limb ischaemia (CLI), acute limb ischaemia, uncontrolled infection, trauma, and aneurysm. CLI was further divided into moderate (Fontaine I and II), if the patient was asymptomatic or had intermittent claudication, and severe (Fontaine III and IV), if the patient had rest pain or tissue loss. The type of anaesthetic was categorised as general or locoregional (including blocks).
Outcomes
The primary outcome was in hospital death after a vascular lower limb procedure. The secondary outcomes were respiratory, cardiac, renal, and cerebrovascular complications, post-operative limb ischaemia, and re-interventions (angioplasty, bypass, major amputation, minor amputation).
Statistical analysis
The study was based on a complete case analysis. Revascularisation procedures with open and endovascular elements (hybrid) were analysed as surgical procedures. Revascularisation procedures were also split into elective and non-elective; major amputations were treated as one group. Changes over time were examined by dividing the time period into pre-pandemic (1 January 2019 – 29 February 2020) and pandemic sections (1 March 2020 – 30 April 2021) with the pandemic section consisting of three segments: Wave 1 (1 March – 30 June 2020), Respite (1 July – 30 October 2020), Wave 2/3 (1 November 2020 – 30 April 2021). Patterns over time were inspected graphically using smoothing splines.
Continuous variables were summarised using the median and interquartile range, and categorical variables using frequencies and proportions. To test the significance of changes over time, the Pearson’s chi square test was used for categorical variables and the Mann–Whitney U test for continuous variables. Poisson regression and logistic regression were used to evaluate differences in procedure volume across time periods and differences in the proportion of procedures performed under general anaesthetic, respectively.
Four multivariable logistic regression models were developed to estimate the impact of SARS-CoV-2 infection and other demographic and clinical characteristics on in hospital post-operative death. The first model included only the time period when the procedure was performed. The second incorporated the procedure type, anaesthetic type, and indication for surgery in addition to the time period. The third model included the previous variables as well as patient age, sex, and comorbidities (diabetes mellitus, chronic obstructive pulmonary disease [COPD], ischaemic heart disease [IHD], chronic heart failure [CHF], chronic kidney disease [CKD]). The peri-operative SARS-CoV-2 status was added as an explanatory variable in the final model, in addition to all the previously included variables. All statistical tests were two sided and p < .05 was considered statistically significant. All analyses were performed using STATA 15.1 (StataCorp, College Station, TX, USA).
Results
The inclusion criteria were fulfilled by 37 393 procedures performed during the study period and 455 were excluded due to missing data on key variables (age, comorbidities, smoking status, indication for surgery, and procedure details). The study analysed information on 36 938 lower limb procedures, comprising of 7 245 (19.6%) major amputations, 16 712 (45.3%) endovascular, and 12 981 (35.1%) open revascularisations.
Procedures in each time period
There were 15 501 procedures performed during the 14 months of the pandemic (March 2020 – April 2021) compared with 21 437 in the 14 months pre-pandemic (January 2019 – February 2020), representing a 27.7% reduction in total procedures.
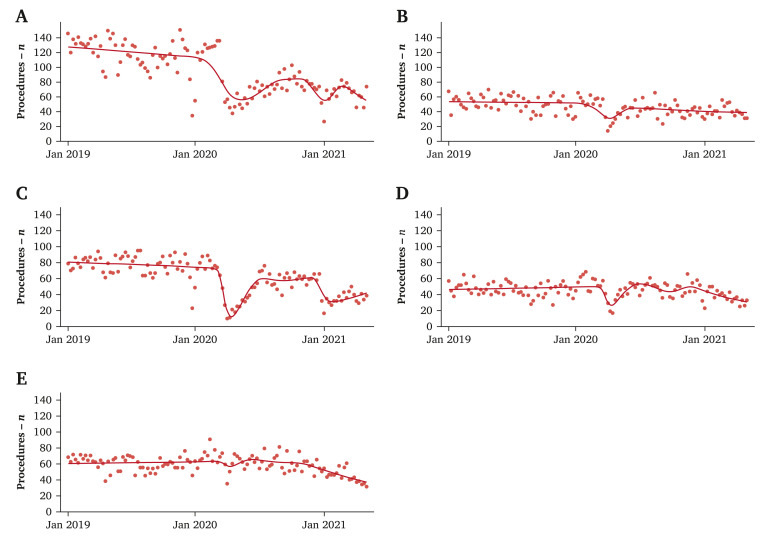
The mix of lower limb vascular procedures performed during the pandemic was significantly different compared with the previous year (p < .001) (Fig. 1 ). There was a decrease in all procedures, especially during the peaks of the pandemic (Wave 1, Wave 2/3) and this reduction was greatest for elective revascularisation procedures (Table 1 ).
Figure 1.
Weekly volumes of vascular lower limb procedures performed from January 2019 to April 2021 in UK by admission method and procedure type (scatterplot) with a smoothed regression line (red line): (A) elective endovascular revascularisation, (B) non-elective endovascular revascularisation, (C) elective open revascularisation, (D) non-elective open revascularisation, and (E) major lower limb amputation.
Table 1.
Monthly average vascular lower limb procedural volume, proportion of procedures performed under general anaesthetic, and proportion of patients with suspected or confirmed SARS-CoV-2 infection by type and time period of procedure, as observed and relative to 2019 pre-pandemic figures.
| Procedure | Procedures, monthly average – n |
General anaesthetic – % |
SARS-CoV-2 infection – % |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-pandemic | Wave 1 | Respite | Wave 2/3 | Pre-pandemic | Wave 1 | Respite | Wave 2/3 | Pre-pandemic | Wave 1 | Respite | Wave 2/3 | |
| Major amputation | ||||||||||||
| Observed | 270 | 273 | 276 | 213∗ | 71.2 | 64.3∗ | 67.0∗ | 66.5∗ | n/a | 10.5 | 5.8 | 14.2 |
| Relative to 2019 | 101.1 | 102.2 | 78.9 | 90.3 | 94.1 | 93.4 | ||||||
| Elective bypass | ||||||||||||
| Observed | 334 | 160∗ | 264∗ | 181∗ | 86.2 | 81.1∗ | 81.9∗ | 83.3∗ | n/a | 2.3 | 0.9 | 1.9 |
| Relative to 2019 | 47.9 | 79.0 | 54.2 | 94.1 | 95.0 | 96.6 | ||||||
| Non-elective bypass | ||||||||||||
| Observed | 207 | 184 | 209 | 176∗ | 88.9 | 83.8∗ | 85.8∗ | 85.5∗ | n/a | 6.2 | 2.5 | 8.0 |
| Relative to 2019 | 88.9 | 101.0 | 85.0 | 94.3 | 96.5 | 96.2 | ||||||
| Elective endovascular | ||||||||||||
| Observed | 512 | 295∗ | 348∗ | 288∗ | 6.0 | 6.2 | 6.5 | 6.7 | n/a | 0.6 | 0.3 | 1.0 |
| Relative to 2019 | 57.6 | 68.0 | 56.3 | 103.3 | 108.3 | 111.7 | ||||||
| Non-elective endovascular | ||||||||||||
| Observed | 208 | 160∗ | 180∗ | 162∗ | 10.3 | 9.9 | 10.7 | 13.1∗ | n/a | 5.9 | 2.2 | 7.0 |
| Relative to 2019 | 76.9 | 86.5 | 77.9 | 96.1 | 103.9 | 127.2 | ||||||
Statistically significantly different (p < .05) compared with pre-pandemic period. n/a = not available.
Did the characteristics of patients having procedures change?
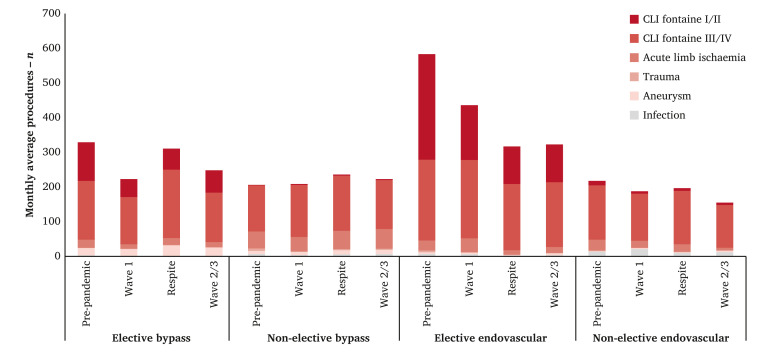
The indication for surgery across the four revascularisation procedures is summarised in Fig. 2 . Among patients who had a major amputation or non-elective revascularisation, the distribution of the indications did not change during the three pandemic time periods compared with the distribution observed in 2019. However, there was a distinct change in the pattern among the patients who had elective revascularisation, with a dramatic drop in the number of procedures performed for moderate disease (Fontaine score I or II) (p < .001). The number of patients treated for trauma, aneurysms, and infection remained stable over time.
Figure 2.
Monthly average number of procedures by indication for surgery in each time period and by procedure type. CLI = chronic limb ischaemia.
Patient and procedure characteristics stratified by time period and procedure type are summarised in Supplementary Table S1. Regarding comorbidities, a significantly higher proportion of patients who underwent elective endovascular revascularisation had diabetes (p < .001), COPD (p = .024), chronic heart failure (p < .001), and CKD (p < .001).
There was also a significant increase in the proportion of current smokers undergoing amputation (34.7% during the pandemic vs. 31.7% pre-pandemic, p = .007), elective (35.4% vs. 31.4%, p < .001), and non-elective (44.9% vs. 40.4%, p = .001) surgical revascularisation.
Was there a change in the type of anaesthetic used during the pandemic?
The proportion of amputation procedures performed under general anaesthetic was 66.0% during the pandemic compared with 71.2% in the pre-pandemic period (p < .001). This reduction was also observed in elective (82.2% vs. 86.2%, p < .001) and non-elective (85.1% vs. 88.9%, p < .001) surgical revascularisation procedures. There was no change in the anaesthetic type for endovascular procedures (Table 1).
How many patients were reported as having SARS-CoV-2 infection?
Only a small proportion of patients who had vascular procedures had suspected or confirmed SARS-CoV-2 infection during their admission (4.6%, n = 708). The rate of SARS-CoV-2 infection for procedures performed during the pandemic was highest for patients having amputation (9.1%, n = 361), followed by non-elective bypass (5.1%, n = 152) and non-elective endovascular revascularisation (4.7%, n = 122), while it was less than 1% for elective revascularisation procedures. The infection rate was higher in the Wave 2/3 period than in Wave 1 (Table 1).
Did the time that patients spent in hospital change?
The median time from admission to procedure was shorter by one day during the pandemic compared with the pre-pandemic period for amputations and non-elective revascularisation procedures (Supplementary Figure S1). Median length of stay was also significantly shorter during the pandemic for amputations (18 days vs. 22 days pre-pandemic), non-elective open surgical revascularisation (12.5 days vs. 15 days pre-pandemic), and endovascular revascularisation (11 days vs. 12 days pre-pandemic) (Supplementary Figure S1).
Complications and re-interventions
There was a significant increase in respiratory complications after amputation and non-elective revascularisation procedures, while no change was observed after elective procedures (Table 2 ). Additionally, rates of cardiac and renal complications, stroke, and surgical site infections remained stable during the pandemic for all procedures (Supplementary Table S2).
Table 2.
In hospital mortality rate and rate of respiratory complications by type and time period of vascular lower limb procedure
| Procedure | Pre-pandemic | Wave 1 | Respite | Wave 2/3 |
|---|---|---|---|---|
| In hospital mortality | ||||
| Amputation | 7.7 (6.9–8.6) | 7.8 (6.3–9.5) | 8.1 (6.5–9.8) | 10.4 (8.8–12.2) |
| Elective bypass | 1.1 (0.8–1.4) | 2.0 (1.1–3.5) | 1.9 (1.2–2.9) | 1.1 (0.6–1.9) |
| Non-elective bypass | 4.2 (3.5–5.0) | 4.4 (3.0–6.1) | 5.1 (3.7–6.9) | 6.0 (4.6–7.6) |
| Elective endovascular | 0.5 (0.3–0.7) | 1.1 (0.6–1.9) | 0.6 (0.3–1.2) | 1.0 (0.6–1.6) |
| Non-elective endovascular | 4.2 (3.5–5.0) | 5.5 (3.9–7.5) | 4.5 (3.1–6.2) | 5.7 (4.3–7.3) |
| Respiratory complication rate | ||||
| Amputation | 8.6 (7.7–9.5) | 11.3 (9.5–13.3) | 7.1 (5.6–8.8) | 11.9 (10.2–13.8) |
| Elective bypass | 2.9 (2.4–3.4) | 4.1 (2.7–5.9) | 2.6 (1.7–3.7) | 1.9 (1.2–2.9) |
| Non-elective bypass | 5.1 (4.4–6.0) | 8.3 (6.4–10.5) | 5.0 (3.6–6.7) | 7.8 (6.2–9.5) |
| Elective endovascular | 0.2 (0.1–0.3) | 0.6 (0.2–1.2) | 0.4 (0.1–0.8) | 0.4 (0.2–0.8) |
| Non-elective endovascular | 3.2 (2.5–3.9) | 5.8 (4.1–7.9) | 2.1 (1.2–3.4) | 5.5 (4.1–7.1) |
Data are presented as % (95% confidence interval).
Regarding re-interventions after the primary procedure during an admission, bypass and major amputation rates following elective open revascularisation were increased compared with the pre-pandemic period, but not for the other categories of revascularisation procedure. There was a significant increase in the proportion of non-elective angioplasty procedures that were followed by an unplanned bypass during the second and third wave compared with the pre-pandemic period (Supplementary Table S2).
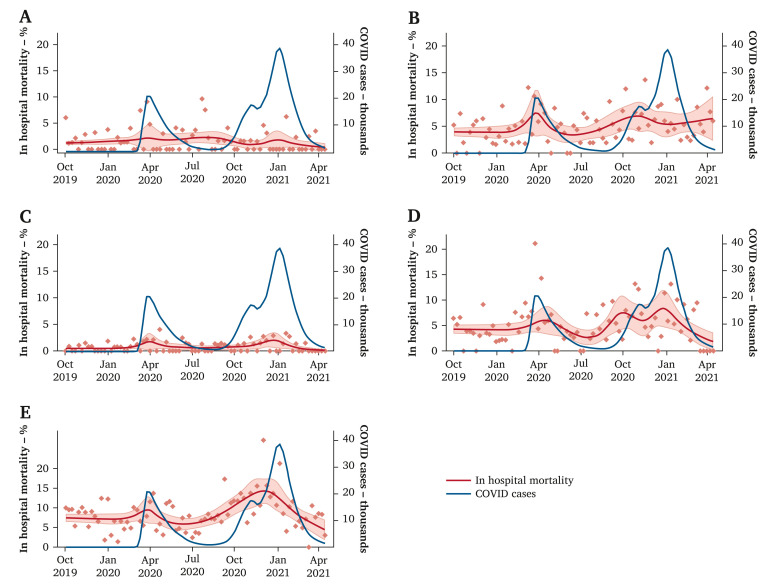
In hospital post-operative death
The in hospital mortality rates after elective open and endovascular revascularisation were 1.6% and 0.9% overall during the pandemic period and were slightly higher than observed in the pre-pandemic period (1.6% vs. 1.1%, p = .033; and 0.9% vs. 0.5%, p = .005, respectively). Figure 3 illustrates that the increased mortality rate was associated with the COVID waves. For elective open revascularisation procedures, the mortality rate doubled during the first months of the pandemic (Table 2). In hospital death after major amputations was greatest during the Wave 2/3 period, reaching 10.4% (95% CI 8.8 – 12.2) compared with 7.7% (95% CI 6.9 – 8.6) in the pre-pandemic period (p = .022) (Fig. 3). The post-operative mortality rate did not change significantly after open and endovascular non-elective revascularisation procedures.
Figure 3.
Weekly average in hospital mortality over time from October 2019 to April 2021 by vascular lower limb procedure type (red dots), with a smoothed regression line for mortality (red line) and 95% confidence intervals (light red band). The blue line indicates the number of national cases of COVID-19 in the UK: (A) elective bypass, (B) non-elective bypass, (C) elective endovascular, (D) non-elective endovascular, and (E) major lower limb amputation.
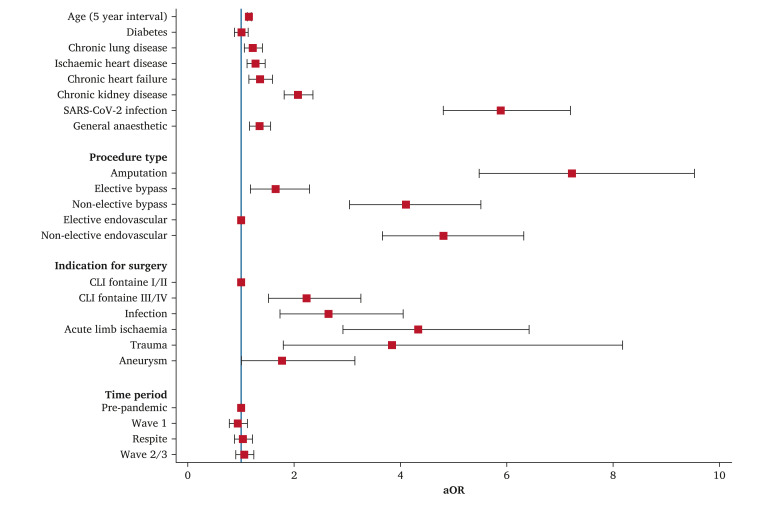
The impact of patient and clinical factors on in hospital mortality from the four regression models are shown in Supplementary Table S3. As indicated by Model 1, procedures during the COVID-19 pandemic period were associated with an excess mortality rate (adjusted odds ratio [aOR] 1.45, 95% CI 1.23 – 1.71 for Wave 1; aOR 1.61, 95% CI 1.39 – 1.86] for Wave 2/3). Adding procedural factors (Model 2) demonstrates that some of the excess mortality was associated with a change in the mix of procedures performed, even though there is still evidence of excess mortality in Wave 2/3 (Model 2, aOR 1.38, 95% CI 1.19 – 1.59). The increased mortality in Wave 2/3 persisted after further adjustment for patient age, sex, and comorbidities, indicating that the excess mortality was not associated with treating patients with worse general health (Model 3, aOR 1.43, 95% CI 1.23 – 1.66). Finally, after the inclusion of the SARS-CoV-2 infection variable in the model (Model 4), the time period of the procedure was no longer associated with a significant effect on mortality (Fig. 4 ). This suggests the excess mortality in the population of lower limb procedures performed during the pandemic is predominantly attributable to SARS-CoV-2 infections among individuals. Compared with patients without SARS-CoV-2 infection, the SARS-CoV-2 positive patients had six times higher in hospital mortality rate, after adjusting for age, sex, comorbidities, indication for surgery, type of procedure, type of anaesthetic, and time period of procedure (aOR 5.88, 95% CI 4.80 – 7.21, p < .001). The overall mortality rate among those with SARS-CoV-2 infection was 25.0% (n = 177).
Figure 4.
Coefficients plot of the adjusted odds ratio (aOR) and 95% confidence intervals for in hospital death after lower limb vascular procedures. The blue line indicates aOR of 1. SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; CLI = chronic limb ischaemia.
Discussion
This study found an overall 28% reduction in vascular lower limb surgical activity during the COVID-19 pandemic period compared with the previous months, with greater effects observed in elective revascularisation procedures. Even though the proportion of patients with SARS-CoV-2 infection undergoing vascular procedures was only 4.6%, a COVID-19 diagnosis was associated with six times higher mortality rate, even after adjusting for patient and procedure characteristics. The overall complication and re-operation rates were comparable to the previous year, but there was a significant increase in in hospital mortality after elective revascularisation and amputation procedures, mainly related to concomitant SARS-CoV-2 infection.
In this study, a 40% decrease in elective revascularisation procedures was noted during the pandemic. This decline in vascular activity has also been reported for carotid endarterectomies, aortic aneurysm repairs, and lower limb procedures by another UK study during the first wave of the pandemic.17 A similar decrease in elective activity has been recorded in other countries, such as Italy13 and the United States.18 The postponement of non-urgent surgical procedures and the prioritisation of urgent and emergency work was recommended by surgical professional bodies in order to reduce the exposure of patients to hospitals and preserve critical care resources. This decrease in surgical volume stems mainly from the reduction in procedures performed for mild or moderate CLI (Fontaine I/II), while the number of procedures for severe limb ischaemia (Fontaine III/IV) remained stable. This is reassuring, as it indicates that urgent limb saving procedures continued to be performed. A reduction in procedures for claudication was also noted in a report from the Swedish Vascular Registry and Southern Italy.19 , 20 Interestingly, the Swedish report did not identify a significant reduction in vascular procedures overall during 2020 compared with previous years, which may be because no national lockdown was imposed in the country.19
Previous studies from The Netherlands and Italy noted an increase in amputation rates, which was attributed to hospital avoidance and subsequent delayed presentation with severe limb ischaemia.21, 22, 23, 24, 25 However, a significant increase in primary major amputations was not identified. This finding is supported by previously published studies, which are however limited to patients with diabetes.26 , 27
Regarding differences in the patterns of care, patients undergoing elective endovascular revascularisation procedures during the pandemic period had more comorbidities, such as diabetes, COPD, kidney disease, and chronic heart failure. An increase in some of these comorbidities was also noted in a study from the United States.28 There has also been an increase in the proportion of current smokers that underwent amputation and surgical revascularisation, which may be an indication of the impact of lockdown on mental health and change in smoking habits.29 Only a small proportion of patients included in this study had SARS-CoV-2 infection, similar to other studies.20 The infection rate was higher in Wave 2/3 than in Wave 1, which may be related to more and better testing at later stages of the pandemic.
Additionally, an increase in revascularisation procedures performed endovascularly in this study was not identified, even though this has been described by the international COVER study,7 as well as single centre studies from the United States and Portugal.30 These studies may be at risk of selection bias, as they involved units that registered to participate, rather than population level data. Moreover, more open surgical procedures (revascularisation and amputation) were performed under locoregional anaesthesia during the pandemic period compared with pre-pandemic, which has also been described in a study from Portugal.30 This approach may have been chosen where possible in an attempt to preserve critical care resources, avoid the use of anaesthetic equipment and staff, and reduce the risk of pulmonary complications associated with the use of general anaesthetic. Additionally, this practice of performing revascularisations under locoregional anaesthesia is supported by an update of the European Society of Vascular Surgery guidelines for Acute Limb Ischaemia, published in early 2022.31
Both median time from admission to procedure and length of stay were shorter during the pandemic. Due to the high rates of SARS-CoV-2 transmission in hospital, this finding may indicate a conscious effort by healthcare staff to reduce the length of stay in hospital. It may also be related to the fact that there was less pressure on emergency theatre capacity by other specialties, since professional bodies recommended non-operative treatment for acute conditions such as appendicitis.
In hospital death after elective revascularisation procedures and major amputations was higher during the pandemic than the pre-pandemic period. This increase can be explained by the presence of SARS-CoV-2 infection, which was associated with a six times increase in mortality. Patients with SARS-CoV-2 infection had a post-operative mortality rate of 25%, which is comparable with the 30 day mortality rate of 23.8% reported by the multicentre COVIDSurg study32 and two studies of vascular procedures from Lombardy (25% in hospital mortality in patients with COVID-19).10 , 33 It is also lower than the 30 day mortality rate of 37.3% after vascular surgery procedures reported in the COVID-VAS multicentre study from Spain for patients with SARS-CoV-2 infection during the first wave.9 Notably, there was no change in mortality or post-operative complication rates after vascular procedures in the Swedish registry.19
The main strength of this study is the large sample size and the long study period, which included the three waves of the pandemic in the UK. Additionally, historical data allowed the comparison of the pandemic period with pre-pandemic patterns of care and outcomes.
This study has certain limitations. First, due to population based observational study design, there is a possibility that the rate of SARS-CoV-2 infection was under reported during data collection. Another factor that may have contributed to underestimation of the rate of SARS-CoV-2-positive patients is the limited availability of diagnostic tests during the first wave of the pandemic. Second, the case ascertainment of endovascular revascularisation procedures in the National Vascular Registry is lower than open revascularisation procedures.15 Third, procedural volumes may have been impacted by under reporting during the pandemic period, but this would not have an effect on the patterns of care and outcomes that this study presented.
The findings from this study suggest that elective surgery was markedly reduced during the COVID-19 pandemic and that the observed excess mortality rate was associated with the infection by the virus. This indicates that strategies should be developed to define criteria for priority access to care for patients who need it most and which would limit the excess mortality rate due to delays to treatment. Operational plans should also be in place to enable a rapid return to normal operations while ensuring that the risk of infection for PAD patients is minimised. Examples could be the development of protected operating pathways in dedicated surgical hubs or within larger hospitals, as well as pathways from referral to treatment.
Conflict of Interest
None.
Funding
P.B. and E.A. are supported by a Royal College of Surgeons of England/Circulation Foundation Research Fellowship. This study was undertaken as part of the work of the NVR, which is commissioned by the Healthcare Quality Improvement Partnership (HQIP) and funded by NHS England and the Welsh Government. The funding bodies had no role in the study design, data collection/analysis and manuscript preparation. The authors had complete access to the study data. The data governance arrangements do not allow the authors to redistribute NVR data to other parties. Researchers can apply for access through HQIP’s Data Access Request facility (https://www.hqip.org.uk).
Acknowledgements
The authors acknowledge the support of the vascular specialists and hospital staff who have participated in the NVR and devoted considerable time to data collection.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ejvs.2023.02.002.
Supplementary Material
References
- 1.World Health Organisation WHO announces COVID-19 outbreak a pandemic. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic Available at:
- 2.Institute for Government Timeline of UK government coronavirus lockdowns and restrictions. https://www.instituteforgovernment.org.uk/charts/uk-government-coronavirus-lockdowns Available at:
- 3.The Vascular Society for Great Britain and Ireland COVID-19 Virus and Vascular Surgery. https://www.vascularsociety.org.uk/professionals/news/113/covid19_virus_and_vascular_surgery Available at:
- 4.American College of Surgeons COVID-19: recommendations for management of elective surgical procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at:
- 5.Lee K.S., Ranganathan S., Choong A.M.T.L., Ng J.J. A scoping review on the changes in vascular surgical practice during the early phases of the COVID-19 pandemic. Semin Vasc Surg. 2021;34:63–73. doi: 10.1053/j.semvascsurg.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Natarajan J.P., Mahenthiran A.K., Bertges D.J., Huffman K.M., Eldrup-Jorgensen J., Lemmon G.W. Effects of coronavirus disease 2019 on the Society for Vascular Surgery Vascular Quality Initiative arterial procedure registry. J Vasc Surg. 2021;73:1852–1857. doi: 10.1016/j.jvs.2020.12.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Vascular and Endovascular Research Network (VERN) COVER study collaborative Global impact of the first coronavirus disease 2019 (COVID-19) pandemic wave on vascular services. Br J Surg. 2020;107:1396–1400. doi: 10.1002/bjs.11961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benson R.A., Nandhra S. Outcomes of Vascular and Endovascular Interventions Performed During the Coronavirus Disease 2019 (COVID-19) Pandemic. Ann Surg. 2021;273:630–635. doi: 10.1097/SLA.0000000000004722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.San Norberto E.M., De Haro J., Peña R., Riera L., Fernández-Caballero D., Sesma A., et al. Outcomes after vascular surgery procedures in patients with COVID-19 infection: a national multicenter cohort study (COVID-VAS) Ann Vasc Surg. 2021;73:86–96. doi: 10.1016/j.avsg.2021.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahlberg A., Mascia D., Bellosta R., Attisani L., Pegorer M., Socrate A.M., et al. Vascular surgery during COVID-19 emergency in hub hospitals of Lombardy: experience on 305 patients. Eur J Vasc Endovasc Surg. 2021;61:306–315. doi: 10.1016/j.ejvs.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mascia D., Kahlberg A., Melloni A., Rinaldi E., Melissano G., Chiesa R. Single-center vascular hub experience after 7 weeks of COVID-19 pandemic in Lombardy (Italy) Ann Vasc Surg. 2020;69:90–99. doi: 10.1016/j.avsg.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellosta R., Bissacco D., Rossi G., Pirrelli S., Lanza G., Frigerio D., et al. Differences in hub and spoke vascular units practice during the novel Coronavirus-19 (COVID-19) outbreak in Lombardy, Italy. J Cardiovasc Surg (Torino) 2021;62:71–78. doi: 10.23736/S0021-9509.20.11564-7. [DOI] [PubMed] [Google Scholar]
- 13.Boschetti G.A., Di Gregorio S., Mena Vera J.M., Pane B., Spinella G., Palombo D., et al. COVID-19 impact on vascular surgery practice: experience from an Italian university regional hub center for vascular pathology. Ann Vasc Surg. 2021;74:73–79. doi: 10.1016/j.avsg.2021.01.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Healthcare Quality Improvement Partnership (HQIP) National Vascular Registry (NVR) https://www.hqip.org.uk/a-z-of-nca/national-vascular-registry/#.YgpGo9_P2Ul Available at:
- 15.Waton S., Johal A., Birmpili P., Li Q., Cromwell D., O’Neill R., et al. The Royal College of Surgeons of England; London: 2021. National Vascular Registry: 2021 Annual Report. [Google Scholar]
- 16.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ball S., Banerjee A., Berry C., Boyle J.R., Bray B., Bradlow W., et al. CVD-COVID-UK Consortium Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart. 2020;106:1890–1897. doi: 10.1136/heartjnl-2020-317870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lou J.Y., Kennedy K.F., Menard M.T., Abbott J.D., Secemsky E.A., Goodney P.P., et al. North American lower-extremity revascularization and amputation during COVID-19: observations from the Vascular Quality Initiative. Vasc Med. 2021;26:613–623. doi: 10.1177/1358863X211021918. [DOI] [PubMed] [Google Scholar]
- 19.Björses K., Blomgren L., Holsti M., Jonsson M., Smidfelt K., Mani K. Editor's Choice – The impact of Covid-19 on vascular procedures in Sweden 2020. Eur J Vasc Endovasc Surg. 2021;62:136–137. doi: 10.1016/j.ejvs.2021.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martelli E., Sotgiu G., Saderi L., Martelli A.R., Settembrini A.M. Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula. The impact of the first 11 months of the COVID-19 Pandemic on vascular patients' care and hospitalisation rate in the vascular surgery divisions of southern Italy. Eur J Vasc Endovasc Surg. 2022;64:274–275. doi: 10.1016/j.ejvs.2022.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu C., You J., Zhu W., Chen Y., Li S., Zhu Y., et al. The COVID-19 outbreak negatively affects the delivery of care for patients with diabetic foot ulcers. Diabetes Care. 2020;43:e125–e126. doi: 10.2337/dc20-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schuivens P.M.E., Buijs M., Boonman-de Winter L., Veen E.J., de Groot H.G.W., Buimer T.G., et al. Impact of the COVID-19 lockdown strategy on vascular surgery practice: more major amputations than usual. Ann Vasc Surg. 2020;69:74–79. doi: 10.1016/j.avsg.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caruso P., Longo M., Signoriello S., Gicchino M., Maiorino M.I., Bellastella G., et al. Diabetic foot problems during the COVID-19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care. 2020;43:e123–e124. doi: 10.2337/dc20-1347. [DOI] [PubMed] [Google Scholar]
- 24.Sena G., Gallelli G. An increased severity of peripheral arterial disease in the COVID-19 era. J Vasc Surg. 2020;72:758. doi: 10.1016/j.jvs.2020.04.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ng J.J., Gan T.R.X., Niam J.Y., Menon R.K., Ho P., Dharmaraj R.B., et al. Experience from a Singapore tertiary hospital with restructuring of a vascular surgery practice in response to national and institutional policies during the COVID-19 pandemic. J Vasc Surg. 2020;72:1166–1172. doi: 10.1016/j.jvs.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Mestral C., Gomez D., Wilton A.S., Lee D.S., Albalawi Z., Austin P.C., et al. A population-based analysis of diabetes-related care measures, foot complications, and amputation during the COVID-19 pandemic in Ontario, Canada. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2021.42354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Valabhji J., Barron E., Vamos E.P., Dhatariya K., Game F., Kar P., et al. Temporal trends in lower-limb major and minor amputation and revascularization procedures in people with diabetes in England during the COVID-19 pandemic. Diabetes Care. 2021;44:e133–e135. doi: 10.2337/dc20-2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho V.T., Eberhard A.V., Asch S.M., Leeper N.J., Fukaya E., Arya S., et al. US national trends in vascular surgical practice during the COVID-19 pandemic. JAMA Surg. 2021;156:681–683. doi: 10.1001/jamasurg.2021.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carreras G., Lugo A., Stival C., Amerio A., Odone A., Pacifici R., et al. Impact of COVID-19 lockdown on smoking consumption in a large representative sample of Italian adults. Tob Control. 2022;31:615–622. doi: 10.1136/tobaccocontrol-2020-056440. [DOI] [PubMed] [Google Scholar]
- 30.Duarte A., Gouveia E.M.R., Lopes A., Rato J.P., Valente J., Pedro L.M. Lessons learned from the impact of the COVID-19 pandemic in a vascular surgery department and preparation for future outbreaks. Ann Vasc Surg. 2021;73:97–106. doi: 10.1016/j.avsg.2021.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jongkind V., Earnshaw J.J., Bastos Gonçalves F., Cochennec F., Debus E.S., Hinchliffe R., et al. Editor's Choice – Update of the European Society for Vascular Surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia in light of the COVID-19 pandemic, based on a scoping review of the literature. Eur J Vasc Endovasc Surg. 2022;63:80–89. doi: 10.1016/j.ejvs.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bellosta R., Piffaretti G., Bonardelli S., Castelli P., Chiesa R., Frigerio D., Lanza G., Pirrelli S., Rossi G., Trimarchi S., Lombardy Covid-19 Vascular Study Group Regional survey in Lombardy, northern Italy, on vascular surgery intervention outcomes during the COVID-19 pandemic. Eur J Vasc Endovasc Surg. 2021;61:688–697. doi: 10.1016/j.ejvs.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.