Abstract
Objectives
With increased bicycle use during the COVID-19 pandemic and growing availability of bicycle-sharing programs in Montreal, we hypothesize helmet use has decreased. The aim of this study was to evaluate helmet use and proper fit among Montreal cyclists during the pandemic relative to historical data.
Methods
Nine observers collected data on bike type, gender, helmet use, and ethnicity using the iHelmet© app at 18 locations across the island of Montreal from June to September 2021. Proper helmet wear was assessed at one busy location. Multiple logistic regression was used to identify factors associated with helmet wear and results were compared to a historical study.
Results
Of the 2200 cyclists observed, 1109 (50.4%) wore a helmet. Males (OR = 0.78, 95%CI = 0.65–0.95), young adults (OR = 0.65, 95%CI = 0.51–0.84), visible minorities (OR = 0.38, 95%CI = 0.28–0.53), and bike-share users (OR = 0.21, 95%CI = 0.15–0.28) were less likely to be wearing a helmet, whereas children (OR = 3.92, 95%CI = 2.17–7.08) and cyclists using racing bicycles (OR = 3.84, 95%CI = 2.62–5.62) were more likely to be wearing a helmet. The majority (139/213; 65.3%) of assessed cyclists wore properly fitting helmets. Children had the lowest odds of having a properly fitted helmet (OR = 0.13, 95%CI = 0.04–0.41). Compared to 2011, helmet use during the pandemic increased significantly (1109/2200 (50.4%) vs. 2192/4789 (45.8%); p = 0.032).
Conclusion
Helmet use among Montreal cyclists was associated with age, gender, ethnicity, and type of bicycle. Children were least likely to have a properly fitted helmet. The recent increase in popularity of cycling and expansion of bicycle-sharing programs reinforce the need for bicycle helmet awareness initiatives, legislation, and funding prioritization.
Keywords: Injury prevention, Head injuries, Bicycle helmet, Legislation
Résumé
Objectif
Avec la popularité grandissante du vélo durant la pandémie COVID-19 et l’expansion du vélopartage à Montréal, nous croyons que le port du casque a diminué. L’objectif de cette étude était d’évaluer l’utilisation du casque et le port adéquat parmi les cyclistes montréalais et de comparer nos résultats avec des données historiques.
Méthode
Neuf observateurs, stationnés à 18 emplacements, ont recueilli les informations suivantes en utilisant l’application mobile iHelmet© : type de vélo, sexe, origine ethnique et port du casque. Le port adéquat du casque a été observé à un endroit. L’association de chaque variable avec le port et le port adéquat a été fait par régression multivariable et comparé à des données historiques.
Résultats
Des 2 200 cyclistes observés, 1 109 (50,4 %) portaient un casque. Les enfants (OR = 3,92, IC95% = 2,17–7,08) et les cyclistes de performance (OR = 3,84, IC95% = 2,62–5,62) portaient le casque plus fréquemment tandis que les hommes (OR = 0,78, IC95% = 0,65–0,95), les jeunes adultes (OR = 0,65, IC95% = 0,51–0,84), les minorités visibles (OR = 0,38, IC95% = 0,28–0,53), et les utilisateurs de vélopartage (OR = 0,21, IC95% = 0,15–0,28) le portaient moins. La majorité (139/213; 65,3 %) des casques étaient portés adéquatement. Les enfants étaient plus à risque de porter un casque mal ajusté (OR = 0,13, IC95% = 0,04–0,41). L’utilisation d’un casque chez les cyclistes montréalais a augmenté significativement depuis 2011 (1 109/2 200 (50,4 %) c. 2 192/4 789 (45,8 %); p = 0,032).
Conclusion
Le port du casque à vélo à Montréal est associé à l’âge, le sexe, l’origine ethnique et le type de vélo. Les enfants sont plus à risque de mal porter un casque. Des stratégies de promotion ainsi que la législation peuvent favoriser des comportements sécuritaires à vélo.
Mots-clés: Prévention des accidents, traumatismes crâniens, port du casque à vélo, législation
Introduction
Bicycling is a very popular form of transportation and physical activity on the island of Montreal and has gained significant popularity in recent years. Indeed, according to a report published by Vélo Québec in 2020, the number of bike lanes in Montreal increased by 35% since 2015 (Vélo Québec, 2021) and an additional 327 km of new pedestrian and bike paths were created in the summer of 2020 to provide safe access to different parts of the city (Ville de Montréal, 2020). The utilization of BIXI, a bike-sharing program, also increased by 62% from 2015 to 2019 (Vélo Québec, 2021). Furthermore, as a result of the pandemic, the majority of commuters using public transport to go to and from work felt unsafe doing so and thus, one fifth of those who changed modes of transportation resorted to cycling or walking instead (Statistics Canada, 2020).
Head injuries are among the most severe injuries that cyclists can sustain and represent an important proportion of admissions to the emergency department and deaths following an accident (Rowe et al., 1995; Sack et al., 1991). It is a well-established fact that bike helmet use greatly reduces the risk of traumatic brain injuries (TBIs) (Thompson et al., 2000) and likelihood of admissions for TBIs after a bicycle-related accident (Dagher et al., 2015). In 2011, the proportion of helmet-wearing cyclists on the island of Montreal was 46% with women, youth, and Caucasians being the groups with the highest proportion of helmet wear (Grenier et al., 2013). Additionally, cyclists using a bike-sharing program were significantly less likely to be wearing a helmet (Grenier et al., 2013).
However, with the recent increase in commuters cycling to and from work, as well as the increase in popularity of bike-sharing programs, it is unclear whether these historical findings still hold true. Moreover, while proper fit has been previously demonstrated to have a protective role in head injuries, this has not been studied specifically in the Montreal population (Rivara et al., 1999; Ching et al., 1997). Therefore, the aims of this study were (1) to evaluate helmet use and proper fit among Montreal cyclists during the pandemic relative to historical data (Grenier et al., 2013) and (2) to identify factors associated with helmet use and proper fit to help guide future injury prevention initiatives.
Methods
Study design
This cross-sectional cohort study was reported according to the STROBE Guidelines (von Elm et al. 2014) (Appendix 1). Using the McGill University Health Centre Research vs Quality Initiative Screening Tool, this project was deemed to be a quality improvement (QI) project and thus exempt from requiring research ethics board approval.
Participants and setting
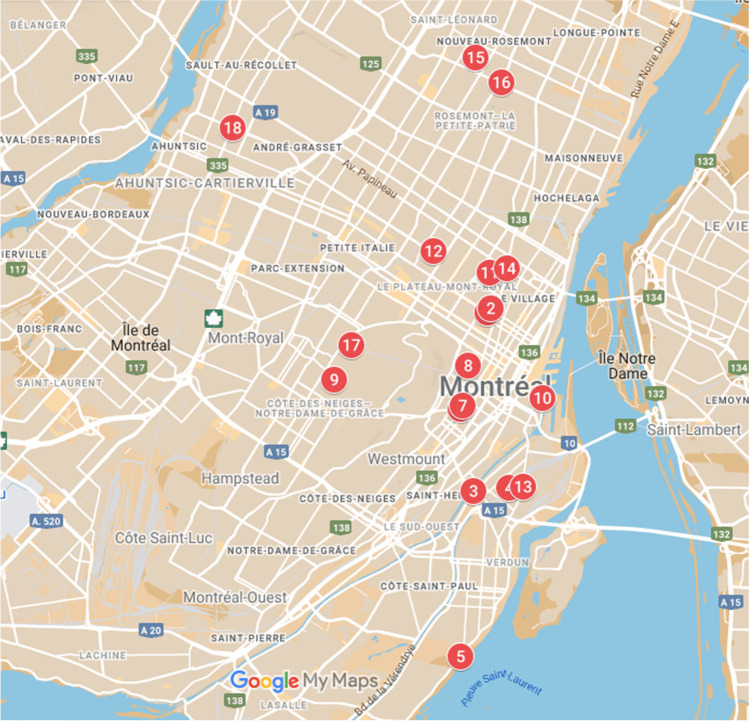
Cyclists of all ages were observed during cumulative 60-min periods, at each of the 18 locations on the island of Montreal during the bike season (specifically from June 15 to September 9, 2021) (Fig. 1). The 60-min observation periods were broken down into one to three intervals. The locations were selected according to a similar study from 2011 according to their proximity to a Level 1 Trauma Centre in Montreal (Montreal General Hospital) and expected high volume of visible cyclists (Grenier et al., 2013). To minimize duplication, data were not recorded at locations where cyclists were doing laps. This was determined by using locations that were not designed for training purposes. Periods of observation took place between 9h00 and 20h00 EST during weekdays and weekends to assure elevated bike traffic and homogeneous inclusion of data. Cyclists were included if they were actively cycling and were counted only once during this single period. Moreover, each cyclist in a group was counted separately. All cyclists observed at an intersection were included, no matter which direction they were headed. Cyclists were excluded if they were not riding their bike. Proper helmet wear was assessed at a single and busy location (Atwater footbridge, number 3 in Fig. 1), on a single weekend day and over a 5-h period, as part of a planned community outreach initiative. A proportion of cyclists observed for proper helmet fit were stopped if they agreed to receive recommendations as part of the community outreach initiative.
Fig. 1.
Eighteen observation locations on the Island of Montreal. (1) Cherrier St./St-Denis St.*; (2) Berri St./Cherrier St.*; (3) Atwater Footbridge North; (4) Hibernia St./Mullins St.; (5) Lasalle Boulevard/Douglas Hospital; (6) Maisonneuve Boul./Mackay St.**; (7) Maisonneuve Boul./Bishop St.**; (8) University St./Milton St.; (9) Édouard-Montpetit St./Louis-Colin St.; (10) De la Commune/McGill Street; (11) Lafontaine Park; (12) Sir Wilfrid Laurier Park; (13) Wellington St./Charron St.; (14) Sherbrooke St./Papineau Ave.; (15) St-Zotique St./41e Ave.; (16) Viau/Rosemont St.; (17) Willowdale Ave./Vincent-d’Indy; (18) Christophe-Colomb Ave./Sauvé St. *Locations 1 and 2 are overlapping on the map. **Locations 6 and 7 are overlapping on the map
Data collection
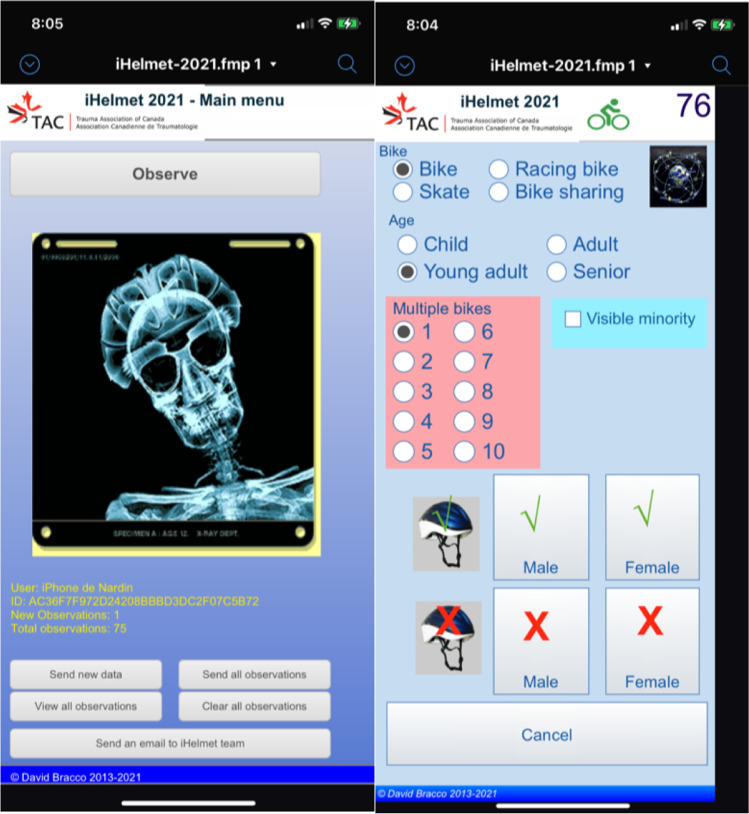
Data on helmet use was collected using the iHelmet© application, developed by the Montreal General Hospital Trauma Centre, specifically for epidemiological surveys of helmet use in the region (Grenier et al., 2013). The iHelmet© app allowed users to collect data on their smartphone in addition to recording the GPS location and time at which data were recorded. The data could then be exported for data analysis.
To collect data in a standardized fashion, observers were trained to use the iHelmet© app and variables were predefined among the 9 observers prior to data collection. The iHelmet© app allows to record information about the following variables: age group (child, young adult, adult and senior), type of bike (commuter bike, racing bike, bike-sharing), helmet usage (yes or no), visible minority (yes or no), and gender (male or female) (Fig. 2). To optimize interrater reliability, observers collected data using predefined visible characteristics defined in Table 1.
Fig. 2.
iHelmet© app interface. The app allows for the user to record data on the following variables: bike type (bike, racing bike, skate, bike sharing), age (child, young adult, adult, senior), number of bikes, visible minority (yes or no), helmet use (yes or no), and gender (male or female)
Table 1.
Predefined visible characteristics for Montreal cyclists
| Variable | Value | Description |
|---|---|---|
| Age group | Child | Prepubescent |
| Young adult | Young-looking, pubescent | |
| Adult | Mature-looking | |
| Senior | Person with traits associated with older age (e.g., grey hair, fat wasting, wrinkles) | |
| Type of bike | Commuter bike | Includes vintage-like bikes (e.g., older bike models with curved handlebars), bikes with travelling bags; excludes bicycles from bike-sharing programs |
| Racing bike | Bicycles with curved handlebar and/or performance bikes, known high-performance bikes, and cyclists wearing performance attire | |
| Bike sharing | Standard bicycles labelled with known bike-sharing program logos | |
| Visible minority | Yes | Non-Caucasian, darker skin colour |
| Gender | Male | Secondary male sex characteristics such as increased muscle mass, facial hair, and increased body hair |
| Female | Secondary female sex characteristics such as no facial hair, fine facial features, and lighter muscle mass |
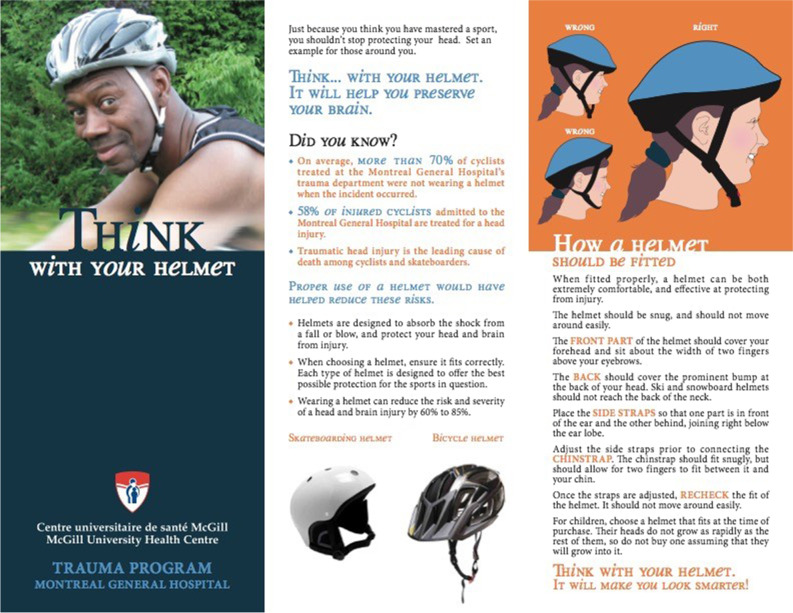
Data on proper helmet fit were collected on paper and we observed the following variables, as defined previously: gender (male or female), visible minority (yes or no), age group (senior, adult, young adult, and children), and proper helmet fit (yes or no). Proper helmet fit was defined based on previous evidence-based recommendations developed by the Montreal General Hospital safety brochure (Trauma Program Montreal General Hospital, 2010) (see Appendix 2, Fig. 3). These recommendations include 4 criteria for proper helmet fit: front part covering the forehead and within 2 fingerbreadths above the eyebrows, adequate coverage of the occipital region of the head, side straps joining at the bottom of the ear lobe and forming a “V” around the ear, and adequate fit of the chinstrap (Trauma Program Montreal General Hospital, 2010).
Statistical analysis
Data were reported as frequencies with proportions, means with standard deviations, or medians with interquartile ranges (Q1 to Q3), as appropriate. A regression analysis was conducted to calculate unadjusted and adjusted odds ratios (aORs) for covariates associated with helmet use, as well as proper helmet fit. The aORs and 95% confidence ratios from this study were compared to those from previously available data collected in 2011 in order to identify significant changes since the COVID pandemic. The χ2 test was used to compare the proportion of helmet wearers from this study and 2011. A p-value less than 0.05 was considered statistically significant. Statistical analyses were performed using R statistical software version 3.5.3 (R Project for Statistical Computing) (R Core Team, 2013).
Results
Helmet wear
From June to September 2021, a total of 2200 cyclists were observed and 1109 (50.4%) were wearing a helmet. Cyclist demographics are reported in Table 2. Helmet use increased significantly (1109/2200 (50.4%) vs. 2192/4789 (45.8%); p = 0.032) as compared to the historical cohort of 2011. After adjusting for age, ethnicity, and bike type, females were found to have higher odds of bike helmet wear compared to males (aOR 1.28, 95% CI 1.05–1.54). In the adjusted model, young adults were less likely to be wearing a helmet (aOR 0.65, 95% CI 0.51–0.84) while the odds of children wearing a helmet were nearly fourfold greater than those of adults (aOR 3.92, 95% CI 2.17–7.08). Visible minorities (aOR 0.38, 95% CI 0.28–0.53) and bike-sharing program users (aOR 0.21, 95% CI 0.15–0.28) were also less likely to be wearing a helmet. Cyclists using a racing bike had higher odds of bike helmet wear compared to cyclists on commuter bikes (aOR 3.84, 95% CI 2.62–5.62) and the odds of bike-sharing program users wearing a helmet were significantly lower than those of commuter cyclists (aOR 0.21, 95% CI 0.15–0.28).
Table 2.
Factors associated with bike helmet use
| Variable | Helmet use n/N* (%) | OR (unadjusted) | 95% CI | OR (adjusted)** | 95% CI |
|---|---|---|---|---|---|
| Overall | 1109/2200 (50.4) | ||||
| Gender | |||||
| Male | 696/1433 (48.6) | Ref | Ref | Ref | Ref |
| Female | 413/767 (53.8) | 1.24 | 1.03–1.47 | 1.28 | 1.05–1.54 |
| Age group | |||||
| Adult | 774/1578 (49.0) | Ref | Ref | Ref | Ref |
| Child | 66/80 (82.5) | 4.85 | 2.78–9.09 | 3.92 | 2.17–7.08 |
| Young adult | 157/342 (45.9) | 0.88 | 0.70–1.11 | 0.65 | 0.51–0.84 |
| Senior | 112/200 (56.0) | 1.32 | 0.98–1.78 | 1.09 | 0.80–1.49 |
| Ethnicity | |||||
| Caucasian | 1046/1955 (53.5) | Ref | Ref | Ref | Ref |
| Visible minority | 63/245 (25.7) | 0.30 | 0.22–0.40 | 0.38 | 0.28–0.53 |
| Type of bicycle | |||||
| Commuter bike | 899/1671 (53.8) | Ref | Ref | Ref | Ref |
| Racing bike | 149/185 (80.5) | 3.54 | 2.46–5.23 | 3.84 | 2.62–5.62 |
| Bike sharing | 61/344 (17.7) | 0.19 | 0.14–0.25 | 0.21 | 0.15–0.28 |
*Excluded N = 72 from total due to incomplete data (n = 50) and skaters (n = 22). **Adjusts for gender, age, ethnicity, and bike type
Helmet fit
Helmet fit was observed in 213 cyclists and 139 (65.3%) were found to be wearing a properly fitted helmet. Demographics for cyclists assessed for helmet fit are reported in Table 3. After adjusting for age and ethnicity, there was a trend for males (aOR 0.73, 95% CI 0.40–1.34) to have less properly fitted helmets. There was also a trend for visible minorities (aOR 0.74, 95% CI 0.33–1.65) to less often have properly fitted helmets as compared to Caucasians. After adjusting for ethnicity and gender, children were found to have significantly lower odds of wearing a properly fitted helmet compared to adults (aOR 0.13, 95% CI 0.04–0.41).
Table 3.
Proper helmet fit in Montreal cyclists
| Variable | Proper fit n/N* (%) | OR (unadjusted) | 95% CI | OR (adjusted)** | 95% CI |
|---|---|---|---|---|---|
| Overall | 139/213 (65.3) | ||||
| Gender | |||||
| Male | 69/113 (61.1) | Ref | Ref | Ref | Ref |
| Female | 70/100 (70.0) | 1.49 | 0.84–2.63 | 1.37 | 0.75–2.50 |
| Age group | |||||
| Adult*** | 97/142 (68.3) | Ref | Ref | Ref | Ref |
| Child | 4/19 (21.1) | 0.13 | 0.03–0.38 | 0.13 | 0.04–0.41 |
| Senior | 38/52 (73.1) | 1.25 | 0.62–2.62 | 1.23 | 0.58–2.57 |
| Ethnicity | |||||
| Caucasian | 119/178 (67.0) | Ref | Ref | Ref | Ref |
| Visible minority | 20/35 (57.1) | 0.66 | 0.32–1.41 | 0.74 | 0.33–1.65 |
*18 excluded due to incomplete data. **Adjusts for sex, age, and ethnicity. ***Includes “young adults”
Discussion
To our knowledge, this is the first study to perform an objective assessment of proper helmet fit on the island of Montreal and is the only observational study looking at bicycle helmet use in Montreal since 2011 (Grenier et al. 2013). Contrary to our initial hypothesis, despite the increase in bike-sharing programs, helmet use has increased significantly since 2011. In keeping with previous findings, Montreal cyclists who are young adults, of male gender, a visible minority, and bike-sharing program users are less likely to wear a helmet. While children were the most likely to wear a helmet among all age groups, they were significantly less likely to have a properly fitting helmet.
It has been well documented that head injuries represent one of the most fatal types of bicycling injury (Sosin et al., 1996; Shafi et al., 1998) and cyclists who wear helmets tend to sustain less severe head injuries such as skull fractures (Shafi et al., 1998). A retrospective study by Dagher et al. (2015) looked at patients admitted to the Montreal General Hospital following a cycling accident between 2007 and 2011. Their group demonstrated that cyclists who were not wearing a helmet suffered more serious TBIs, required a longer intensive care unit stay, and underwent more neurosurgical interventions. In addition to helmet use and in assessing a helmet’s degree of protection during a bicycle-related accident, the maximum protection relies on proper helmet fit (Romanow et al., 2014). In a review of fatal pediatric bicycle accidents, 89% of “unsurvivable” injuries were head injuries (Spence et al., 1993) and patients who self-reported poor helmet fit were at a 1.96-fold increased risk of head injury following a cycling crash compared to those who self-reported proper helmet fit (Rivara et al., 1999). The latter is likely an underestimate due to recall bias. Similarly, a more recent case–control study conducted in Calgary, Canada, looking at injured cyclists recruited from 7 emergency departments (EDs) by scanning their Information System and reviewing ED charts daily over a 2-year period, showed that a helmet that came off during a crash increased the odds of facial injury threefold and that wearing a helmet that tilted back increased the odds of facial injury almost fivefold (Romanow et al., 2014). These findings highlight the importance of including proper helmet fit as a covariate when studying the association between helmet wear and head injury and explain, at least in part, why previous studies which exclusively looked at helmet wear (and not fit) have not demonstrated as strong an association (Romanow et al., 2014). Furthermore, proper helmet fit also needs to be a vital part of children’s education in part through positive modelling from caregivers. There is a strong correlation between adults’ non-wear or improper helmet wear and children’s non-wear or improper helmet wear (Twomey et al., 2001). Indeed, a study observed that children travelling with adults who were either not wearing a helmet or wearing a helmet that was not properly fitted were less likely to have a properly fitted helmet compared to those who traveled with adults wearing a properly fitted helmet (Twomey et al., 2001). Therefore, future interventions targeting proper helmet fit in the pediatric population should also include adult populations.
Although we documented an increase in helmet use over time, there is still much room for improvement. Legislation to make helmet wear mandatory has long been advocated for by different medical societies, including the Canadian Pediatric Society, as an intervention to increase helmet use and decrease the incidence of bicycle head-related injuries (Hagel and Yanchar, 2013). However, in the last 10 years and since the first iteration of this observational study, neither the province of Quebec nor the city of Montreal has mandated helmet wear for cyclists using a non-electric bike, despite the clear evidence for its utility for risk reduction when it comes to bike accidents (Hagel and Yanchar, 2013; Shafi et al., 1998). Based on the results of our study, legislation mandating helmet use for cyclists, including bike-sharing users, could be beneficial. However, although multiple studies have demonstrated that the institution of penalties for not wearing a helmet can significantly increase helmet wear among all age groups, particularly among children (Karkhaneh et al., 2011; Parkin et al., 2003), legislative measures may not have been implemented due to other potential consequences.
In fact, legislation could be detrimental to vulnerable social groups, as it could widen the gap between different socioeconomic classes if not implemented with concomitant targeted public health initiatives. For example, a study by Parkin et al. (2003) in Metropolitan Toronto compared the proportion of helmet wear among children living in low- and middle-income areas with that of children in high-income areas before and after the implementation of legislation. Despite the significant increase in helmet wear in both groups, children living in high-income areas consistently had a higher proportion of helmet wear. Another study by Williams et al. (2018) in Illinois looked at children under 18 admitted for a bicycle crash and compared the proportion of helmet use between communities with and those without legislation. Results demonstrated that poorer, non-Hispanic Black and Hispanic children were less likely to wear helmets, and there was no significant change in helmet use over time. This study also demonstrated that helmet use was significantly higher in high-income areas, regardless of legislation, emphasizing that disparity could stem from income differences. Furthermore, legislation may unintentionally lead to an overall decrease in bicycle use. For example, a study by Robinson (1996) in Australia demonstrated that despite a significant increase in proportion of helmet wearers after the implementation of legislation, there was an overall reduction in child cyclists.
Therefore, legislation could have unintended consequences on certain disadvantaged socioeconomic groups if implemented without additional interventions. The addition of social initiatives, such as targeted educational programs and the distribution of free helmets, could play a role in bridging this gap for marginalized communities. For example, in light of the findings from our study, these programs should pay particular attention to ethnic minority communities. Several research groups have looked into comprehensive regional- and community-based efforts to support and strengthen helmet wear. One option could be to subsidize the purchase of helmets or provide free helmets in conjunction with a school-based educational program. In a study by Ederer et al. (2016) in Cambodia, helmets were distributed to children in nine schools where the majority commuted using a bicycle or on a motorcycle and lived in a location at risk (lack of street signs, high traffic density, and multiple recorded road traffic accidents). In schools that received the intervention, helmet wear increased by more than 80% (from 0.46% to 86.5%), while the proportion of helmet wear in the four control schools remained as low as 0.35%. Another study by Watts et al. (1997) found similar results in a higher-income setting, in the United States. In this study, children who participated in a safety bicycle program and received a free helmet were significantly more likely to wear a helmet than those who participated in the program but did not receive a helmet. This may also represent an impactful intervention to target bike-sharing users given the findings of our study. The distribution of free helmets with membership or at the very least providing access to low-cost helmets at rental sites may be worthwhile initiatives in the future.
Awareness campaigns also play a significant role in increasing helmet use. For example, a program conducted in Miami, where physical education teachers were trained to deliver an educational curriculum to grades 6–8 youths on bike helmet use and proper helmet fit, has been shown to significantly improve overall knowledge following pre- and post-training tests of students from 6 different schools (Hooshmand et al., 2014). Cusimano et al. (2013) also demonstrated the success of a similar program where material on bicycle helmet safety was provided in 24 kindergarten classes in Prince Edward Island, Canada. Implementing such a program could reach many children without significant use of resources (Hooshmand et al., 2014). In another study conducted by Ryan et al. (2020), parent–child dyads were recruited at a primary care clinic in Baltimore to receive educational material on bike safety. In addition, the youths received a free helmet, a fitting demonstration, and a flyer on helmet use. Despite the small sample size of participants (n = 20), post-intervention helmet use was 100% among the youths who reported bike-riding at the 1-month follow-up. In fact, there is further evidence that multi-pronged approaches appear most successful. For example, the Swedish Bike Helmet Initiative, through the distribution of brochures, videos, and flyers, the organization of seminars and conferences, and community-led efforts, increased helmet wear among all age groups over a decade (Svanström et al., 2002). The initiative group organized presentations as part of injury prevention conferences, as well as participated in international events where they not only shared their experience but also learned from others’ experiences. A collaboration between the initiative group and national authorities allowed the design and distribution of information supply in the form of videos and flyers across the country. Another study by Lucke-Wold et al. (2020) conducted at the University of Florida breaking down their Helmet Initiative demonstrates its successful implementation by combining an awareness campaign driven by local stakeholders and public health champions, free helmet distribution, and disciplinary action for those not wearing a helmet.
In summary, the island of Montreal has taken the first steps in protecting its cyclists through increased cycling infrastructures and public health campaigns in the last few years. Strengthening its community outreach initiatives, as well as establishing mandatory helmet wear, could further contribute to increasing safety and decreasing the number and severity of TBIs.
Limitations
This study has several limitations. First, it relied on the categorization of ethnicity, gender, and age of cyclists based on visible characteristics. The authors fully acknowledge the complexity of these concepts; however, due to the observational nature of the study, these assumptions were necessary. Furthermore, the small sample size of the cohort assessed for proper helmet fit is another limitation, making it difficult to reach significant differences between the different groups observed and limiting the generalizability of the cohort. Larger studies with helmet fit assessments that would include observation at multiple locations and longer periods of evaluation are needed to strengthen the data. Similarly, due to the small sample size, subgroup analyses of helmet use for the different age and ethnicity groups by gender were not performed. Missing data were also a limitation and may have introduced a component of bias, although unlikely. Given that our only reference was a previous study from 2011, it is difficult to differentiate the effects of the pandemic from other factors affecting helmet use over time; therefore, a causal relationship between our findings and the pandemic cannot be established.
Despite these limitations, this is the first study, to our knowledge, to have performed an objective assessment of proper helmet fit in real time on the island of Montreal and provides an overview of factors associated with helmet use and proper fit to guide future injury prevention initiatives.
Conclusion
Helmet use among Montreal cyclists during the COVID-19 pandemic increased as compared to 2011 and was associated with children, female gender, Caucasian ethnicity, and non-sharing bikes. However, children were less likely to have properly fitted helmets. The recent increase in popularity of cycling and expansion of bike-sharing programs reinforce the need for bicycle helmet awareness initiatives, education about proper helmet fit, legislation, and funding priorities of the City of Montreal, especially for our vulnerable populations. This study’s findings can help these programs better target their future initiatives.
Contributions to knowledge
What does this study add to existing knowledge?
Helmet use among cyclists significantly increased in comparison to 2011 despite the increase in bike-sharing programs where helmet use is limited.
Cyclists of female gender, Caucasian ethnicity, or younger age, and non-bike sharing users are significantly more likely to wear a helmet.
Children are significantly less likely to have a properly fitted helmet compared to adults.
What are the key implications for public health interventions, practice, or policy?
Given the expansion of cycling infrastructures on the island of Montreal and the low proportion of helmet wear among certain groups, legislation could play an important role in increasing helmet wear.
Given the lower proportion of helmet wear among young adults, males, visible minorities, and bike-sharing users, concomitant targeted public health initiatives such as subsidized bike helmets or targeted injury prevention programs could play a role in bridging the gap.
Increased targeted education in a variety of settings is needed to raise awareness about the importance of proper helmet fit among children and their caregivers.
Acknowledgements
We would like to acknowledge all the volunteers who participated in the data collection process and those who participated in the different outreach activities.
Appendix 1
| Section and item | Item no | Recommendation | Reported on page no |
|---|---|---|---|
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | 1 |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | 3–4 | ||
| Introduction | |||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 5 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | 5 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper | 5 |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 6 (Fig. 1) |
| Participants | 6 | (a) Cohort study—Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up | N/A |
| Case–control study—Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls | N/A | ||
| Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants | 5–6 | ||
| (b) Cohort study—For matched studies, give matching criteria and number of exposed and unexposed | N/A | ||
| Case–control study—For matched studies, give matching criteria and the number of controls per case | N/A | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 6–7 (Table 1) |
| Data sources/measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 6–7 (Table 1 and Fig. 2) |
| Bias | 9 | Describe any efforts to address potential sources of bias | 6 |
| Study size | 10 | Explain how the study size was arrived at | 6 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 7 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 7 |
| (b) Describe any methods used to examine subgroups and interactions | 7 | ||
| (c) Explain how missing data were addressed | Tables 2 and 3 | ||
| (d) Cohort study—If applicable, explain how loss to follow-up was addressed | N/A | ||
| Case–control study—If applicable, explain how matching of cases and controls was addressed | N/A | ||
| Cross-sectional study—If applicable, describe analytical methods taking account of sampling strategy | N/A | ||
| (e) Describe any sensitivity analyses | N/A | ||
| Results | |||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed | 7–8 (Tables 2 and 3) |
| (b) Give reasons for non-participation at each stage | N/A | ||
| (c) Consider use of a flow diagram | N/A | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders | 7–8 (Tables 1, 2, and 3) |
| (b) Indicate number of participants with missing data for each variable of interest | Tables 2 and 3 | ||
| (c) Cohort study—Summarize follow-up time (e.g., average and total amount) | N/A | ||
| Outcome data | 15* | Cohort study—Report numbers of outcome events or summary measures over time | N/A |
| Case–control study—Report numbers in each exposure category, or summary measures of exposure | N/A | ||
| Cross-sectional study—Report numbers of outcome events or summary measures | 7–8 (Tables 2 and 3) | ||
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95% confidence interval). Make clear which confounders were adjusted for and why they were included | 7–8 (Tables 2 and 3) |
| (b) Report category boundaries when continuous variables were categorized | N/A | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | N/A | ||
| Other analyses | 17 | Report other analyses done—e.g., analyses of subgroups and interactions, and sensitivity analyses | N/A |
| Discussion | |||
| Key results | 18 | Summarize key results with reference to study objectives | 8 |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | 11–12 |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 8–12 |
| Generalizability | 21 | Discuss the generalizability (external validity) of the study results | 12 |
| Other information | |||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | 1 |
Appendix 2
Fig. 3.
Montreal General Hospital Safety Brochure (Trauma Program Montreal General Hospital, 2010)
Author contributions
Conception and design: NF, AG, EGW
Analysis and interpretation: All authors
Data collection: NF, AG, AAB
Writing the article: NF, AG, NGC, EGW
Critical revision of the article: All authors
Final approval of the article: All authors
Statistical analysis: AAB, NGC
Obtained funding: EGW
Overall responsibility: All authors
Funding
Molson Brothers Award in Trauma – Montreal General Hospital Foundation.
Availability of data and material
N/A
Code availability
N/A
Declarations
Ethical approval
Using the McGill University Health Centre Research vs Quality Initiative Screening Tool, this project was deemed to be a quality improvement (QI) project and thus exempt from requiring research ethics board approval.
Consent to participate
Verbal consent was obtained from all individual participants during helmet verification kiosks.
Consent for publication
N/A
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ching RP, Thompson DC, Thompson RS, Thomas DJ, Chilcott WC, Rivara FP. Damage to bicycle helmets involved with crashes. Accident; Analysis and Prevention. 1997;29(5):555–562. doi: 10.1016/S0001-4575(97)00008-0. [DOI] [PubMed] [Google Scholar]
- Cusimano MD, Faress A, Luong WP, Lockhart S, Amin K, Garland RJ, Russell K. Evaluation of a bicycle helmet safety program for children. Canadian Journal of Neurological Sciences. 2013;40(5):710–716. doi: 10.1017/S0317167100014967. [DOI] [PubMed] [Google Scholar]
- Dagher JH, Costa C, Lamoureux J, de Guise E, Feyz M. Comparative outcomes of traumatic brain injury from biking accidents with or without helmet use. Canadian Journal of Neurological Sciences. 2015;43(1):56–64. doi: 10.1017/cjn.2015.281. [DOI] [PubMed] [Google Scholar]
- Ederer DJ, Bui TV, Parker EM, Roehler DR, Sidik M, Florian MJ, Kim P, Sim S, Ballesteros MF. Helmets for kids: Evaluation of a school-based helmet intervention in Cambodia. Injury Prevention: Journal of the International Society for Child and Adolescent Injury Prevention. 2016;22(1):52–58. doi: 10.1136/injuryprev-2014-041434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenier T, Deckelbaum DL, Boulva K, Drudi L, Feyz M, Rodrigue N, Tze N, Fata P, Khaja K, Chughtai T, Razek T. A descriptive study of bicycle helmet use in Montreal, 2011. Revue Canadienne De Santé Publique. 2013;104(5):400–404. doi: 10.17269/cjph.104.3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagel BE, Yanchar NL. Bicycle helmet use in Canada: The need for legislation to reduce the risk of head injury. Paediatrics & Child Health. 2013;18(9):475–480. doi: 10.1093/pch/18.9.475. [DOI] [Google Scholar]
- Hooshmand J, Hotz G, Neilson V, Chandler L. BikeSafe: Evaluating a bicycle safety program for middle school aged children. Accident; Analysis and Prevention. 2014;66:182–186. doi: 10.1016/j.aap.2014.01.011. [DOI] [PubMed] [Google Scholar]
- Karkhaneh M, Rowe BH, Saunders LD, Voaklander DC, Hagel BE. Bicycle helmet use four years after the introduction of helmet legislation in Alberta, Canada. Accident; Analysis and Prevention. 2011;43(3):788–796. doi: 10.1016/j.aap.2010.10.026. [DOI] [PubMed] [Google Scholar]
- Lucke-Wold B, Pierre K, Dawoud F, Guttierez M. Changing the culture: Improving helmet utilization to prevent traumatic brain injury. Journal of Emergency Medicine Forecast. 2020;3(1):1020. [PMC free article] [PubMed] [Google Scholar]
- Parkin PC, Khambalia A, Kmet L, Macarthur C. Influence of socioeconomic status on the effectiveness of bicycle helmet legislation for children: A prospective observational study. Pediatrics. 2003;112(3 Pt 1):e192–e196. doi: 10.1542/peds.112.3.e192. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Astley SJ, Clarren SK, Thompson DC, Thompson RS. Fit of bicycle safety helmets and risk of head injuries in children. Injury Prevention: Journal of the International Society for Child and Adolescent Injury Prevention. 1999;5(3):194–197. doi: 10.1136/ip.5.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DL. Head injuries and bicycle helmet laws. Accident; Analysis and Prevention. 1996;28(4):463–475. doi: 10.1016/0001-4575(96)00016-4. [DOI] [PubMed] [Google Scholar]
- Romanow NR, Hagel BE, Williamson J, Rowe BH. Cyclist head and facial injury risk in relation to helmet fit: A case-control study. Chronic Diseases and Injuries in Canada. 2014;34(1):1–7. doi: 10.24095/hpcdp.34.1.01. [DOI] [PubMed] [Google Scholar]
- Rowe, B. H., Rowe, A. M., & Bota, G. W. (1995). Bicyclist and environmental factors associated with fatal bicycle-related trauma in Ontario. CMAJ, 152(1), 45–53. [PMC free article] [PubMed]
- Ryan LM, Solomon BS, Ziegfeld S, Gielen A, Malloy L, Foster D, McDonald E. Evaluation of a culturally tailored educational video intervention to promote bike helmet safety for urban children: A pilot study. Health Promotion Practice. 2020;21(6):872–876. doi: 10.1177/1524839920920304. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. http://www.R-project.org/. Accessed 27 June 2022.
- Sacks, J. J., Holmgreen, P., Smith, S. M., & Sosin, D. M. (1991). Bicycle-associated head injuries and deaths in the United States from 1984 through 1988. How many are preventable? JAMA, 266(21), 3016–3018. [PubMed]
- Shafi, S., Gilbert, J. C., Loghmanee, F., Allen, J. E., Caty, M. G., Glick, P. L., & Azizkhan, R. G. (1998). Impact of bicycle helmet safety legislation on children admitted to a regional pediatric trauma center. Journal of Pediatric Surgery, 33(2), 317–321. [DOI] [PubMed]
- Sosin DM, Sacks JJ, Webb KW. Pediatric head injuries and deaths from bicycling in the United States. Pediatrics. 1996;98(5):868–870. doi: 10.1542/peds.98.5.868. [DOI] [PubMed] [Google Scholar]
- Spence LJ, Dykes EH, Bohn DJ, Wesson DE. Fatal bicycle accidents in children: A plea for prevention. Journal of Pediatric Surgery. 1993;28(2):214–216. doi: 10.1016/S0022-3468(05)80278-7. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2020, 10 August). More commuters now walk or bike to work than take public transit. https://www150.statcan.gc.ca/n1/daily-quotidien/200810/dq200810a-eng.htm. Accessed 27 June 2022.
- Svanström L, Welander G, Ekman R, Schelp L. Development of a Swedish bicycle helmet promotion programme–One decade of experiences. Health Promotion International. 2002;17(2):161–169. doi: 10.1093/heapro/17.2.161. [DOI] [PubMed] [Google Scholar]
- Thompson, D. C., Rivara, F. P., & Thompson, R. (2000). Helmets for preventing head and facial injuries in bicyclists. The Cochrane Database of Systematic Reviews, 1999(2), CD001855. [DOI] [PMC free article] [PubMed]
- Trauma Program Montreal General Hospital. (2010). Think with your Helmet. Resource flyer. McGill University Health Centre. https://codetrauma.s3.us-east-2.amazonaws.com/2019/12/HelmetFlyerSummerREV2_July2010.pdf. Accessed 27 May 2022.
- Twomey, J. G., Bevis, M. C., & McGibbon, C. A. (2001). Associations between adult and child bicycle helmet use. MCN. The American Journal of Maternal Child Nursing, 26(5), 272–277. [DOI] [PubMed]
- Vélo Québec. (2021, 8 June). L’état du vélo au Québec en 2020. https://www.velo.qc.ca/salle-de-presse/etat-du-velo/letat-du-velo-au-quebec-en-2020/. Accessed 27 June 2022.
- Ville de Montréal. (2020, 15 May). COVID-19 : Montréal to offer safe active transportation circuit this summer. http://ville.montreal.qc.ca/portal/page?_pageid=5977,43117560&_dad=portal&_schema=PORTAL&id=32662. Accessed 27 June 2022.
- von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., & STROBE Initiative. (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. International Journal of Surgery (London, England), 12(12), 1495–1499. [DOI] [PubMed]
- Watts D, O’Shea N, Flynn E, Trask A, Kelleher D. Effect of a bicycle safety program and free bicycle helmet distribution on the use of bicycle helmets by elementary school children. Journal of Emergency Nursing. 1997;23(5):417–419. doi: 10.1016/S0099-1767(97)90134-3. [DOI] [PubMed] [Google Scholar]
- Williams C, Weston R, Feinglass J, Crandall M. Pediatric bicycle helmet legislation and crash-related traumatic brain injury in Illinois, 1999–2009. The Journal of Surgical Research. 2018;222:231–237. doi: 10.1016/j.jss.2017.11.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A
N/A