Abstract
Context
The relationships among different sports, face mask use, and COVID-19 risk among high school athletes remain unknown.
Objective
To evaluate the influence of sport characteristics and face mask use on the COVID-19 incidence among high school athletes.
Design
Descriptive epidemiology study.
Setting
US high school athletic departments.
Patients or Other Participants
Athletic directors.
Main Outcome Measure(s)
Surveys were completed regarding sport reinitiation, COVID-19 cases, and risk-reduction procedures in fall 2020. Separate mixed-effects Poisson regression models were developed to evaluate the associations between the reported COVID-19 incidence and (1) sport characteristics (indoor versus outdoor, individual versus team, contact versus noncontact) and (2) face mask use while playing (yes or no).
Results
A total of 991 schools had restarted fall sports, representing 152 484 athletes on 5854 teams. There were 2565 reported cases of COVID-19, representing a case rate of 1682 cases per 100 000 athletes and an incidence rate of 24.6 cases per 100 000 player-days. The COVID-19 incidence was lower for outdoor versus indoor sports (incidence rate ratio [IRR] = 0.54; 95% CI = 0.49, 0.60; P < .001) and noncontact versus contact sports (IRR = 0.78; 95% CI = 0.70, 0.87; P < .001), but not team versus individual sports (IRR = 0.96; 95% CI = 0.84, 1.1; P = .49). Face mask use was associated with a decreased incidence in girls' volleyball (IRR = 0.53; 95% CI = 0.37, 0.73; P < .001), boys' basketball (IRR = 0.53; 95% CI = 0.33, 0.83; P = .008), and girls' basketball (IRR = 0.36; 95% CI = 0.19, 0.63; P < .001) and approached statistical significance in football (IRR = 0.79; 95% CI = 0.59, 1.04; P = .10) and cheer or dance (IRR = 0.75; 95% CI = 0.53, 1.03; P = .081).
Conclusions
In this nationwide survey of high school athletes, a lower COVID-19 incidence was independently associated with participation in outdoor versus indoor and noncontact versus contact sports but not team versus individual sports. Face mask use was associated with a decreased COVID-19 incidence among indoor sports and may be protective in outdoor sports with prolonged close contact among participants.
Keywords: infection, SARS-CoV-2, adolescents, pediatrics
Key Points
During the fall 2020, the COVID-19 incidence in high school athletes was higher for indoor versus outdoor and contact versus noncontact sports but did not differ between individual and team sports.
Face mask use among athletes while participating in sport was associated with a decreased incidence of COVID-19 in indoor sports and may reduce the incidence in outdoor sports with prolonged, close contact.
Understanding the relative risks associated with different sports and face mask use can help guide decision making regarding risk reduction in youth sports during the COVID-19 pandemic.
To control the spread of the coronavirus disease 2019 (COVID-19) in spring 2020, restrictions were placed on virtually all facets of American society, including the cancellation of school and interscholastic athletics. Early research1–3 suggested that school and sport cancellations during the initial months of the COVID-19 pandemic were associated with decreases in physical activity and worsening of depressive symptoms in children and athletes. Prolonged restriction was projected to contribute significantly to long-term increases in obesity and mental health disorders.4–6 In a nationwide survey of more than 13 000 adolescent athletes in May 2020, 37% reported moderate to severe symptoms of anxiety and 40% reported moderate to severe symptoms of depression.7 Together, these results indicated that isolation and physical inactivity during the COVID-19 restrictions may have represented a substantial threat to physical and mental health in children and adolescents.
Efforts to promote the benefits of youth sports participation were necessarily balanced against the potential risk of COVID-19 transmission. While high school sports restarted in many areas of the United States, they remained shut down in other areas, with a lack of specific evidence to guide decision making. A number of organizations developed risk-reduction protocols in an attempt to mitigate the spread of COVID-19 among youth sport participants, but the limited prior research in sport environments to guide these decisions was widely recognized.8–12 In youth sports, the available evidence was restricted to case reports in adult recreational athletes, media reports of infections among adults and adolescents associated with interscholastic athletics, and a single evaluation of youth soccer in a small-group, physically distanced setting.12–14
Organizations also tried to classify sports in terms of the risk of COVID-19 transmission during participation. These recommendations were based on a number of characteristics but differed among organizations, as evidence derived from sport contexts was lacking.8–11 Two recent publications15,16 on adult professional athletes suggested that transmission among athletes during participation in outdoor sports was rare, although it was unclear whether these findings could be extrapolated to youth sport contexts. In fact, we are aware of no investigators who evaluated the relative risks of COVID-19 among athletes in different sports or with sport characteristics such as indoor versus outdoor, individual versus team, or contact versus noncontact.
Similarly, the recommendations regarding face mask use during sport participation differed among public health organizations, and the American Academy of Pediatrics recently changed its recommendation to encourage face mask use among youth athletes in most sport contexts.8–10,17 Despite the general consensus in the scientific community that face mask use in community settings could reduce COVID-19 transmission, no specific evidence from youth sport environments regarding its effectiveness and whether any benefit differed by sport or sport characteristic was available. Therefore, the purpose of our study was to determine the associations between COVID-19 risk and specific sports, sport characteristics, and face mask use among US high school athletes.
METHODS
Study Design
All procedures performed in this study were approved by the Institutional Review Board of the University of Wisconsin. In collaboration with the National Federation of State High School Associations, surveys were distributed to all US state high school athletic associations between November 1, 2020, and November 3, 2020. Among states in which fall high school athletics had restarted, surveys were forwarded to the athletic directors of high schools within the state. In addition to the school name and location, athletic directors were asked whether their schools had restarted participation in sports since the initial COVID-19 restrictions in spring 2020. For those schools that had reinitiated sports, athletic directors were asked to provide the specific sports and dates of restarting, number of athletes, number of practices and games, number of COVID-19 cases among athletes, and reported sources of infection (if known) in each sport during the months of August, September, and October 2020. They were also asked about the type of instruction during the fall (virtual, in person) and which restarted sports used face masks for athletes while playing. Schools were included if they had any sport that restarted participation during August, September, or October 2020.
Statistical Analysis
We initially evaluated the data using descriptive statistics, including estimates of central tendency (mean, median) and variability (SD, interquartile range, range) for continuous variables and counts and percentages for categorical variables. Case rates were expressed as the number of reported cases per 100 000 players (cases × 100 000/total number of players) overall and for each sport. The duration of participation for each sport at each school was determined as the difference in days between the date of restarting and October 31, 2020, and player-days were computed as the product of the number of participating players and duration. Incidence rates were expressed as the number of reported cases per 100 000 player-days (cases × 100 000/total number of player-days) overall and for each sport, with CIs calculated using an exact method.
In addition, we determined the number of cases, total population, case rate, and incidence rate during August, September, and October 2020 for each state in which a respondent high school was located from publicly available online information aggregated from the US Centers for Disease Control and Prevention and local health authorities.18 To establish whether background state COVID-19 rates were associated with reported COVID-19 rates among high school athletes, the total number of athletes and COVID-19 cases were aggregated by state. For those states with > 100 athletes, the relationship between COVID-19 case rates among high school athletes and the general population was evaluated with a linear regression model weighted for the number of players from each state.
For those sports with data from ≥50 schools (baseball, boys' and girls' basketball, cheer or dance, cross-country, football, boys' and girls' golf, boys' and girls' soccer, softball, girls' volleyball), the relative risk of each sport was evaluated using a mixed-effects Poisson regression model to predict the number of COVID-19 cases for each team with the state incidence, instructional delivery type (virtual, in person), and sport as fixed effects, school as a random effect, and the log of player-days as an offset, yielding an incidence rate ratio (IRR) with boys' soccer as the reference (because it represented the median unadjusted incidence rate and was typically considered a moderate-risk sport). To assess the independent relationships between COVID-19 cases and sport characteristics, we developed a mixed-effects Poisson regression model to predict the number of cases with the state incidence, instructional delivery type, sport location (indoor, outdoor), sport type (individual, team), and sport contact (contact, noncontact) as fixed effects, school as a random effect, and the log of player-days as an offset including data from all sports reported.
To evaluate the association between the overall COVID-19 incidence and reported face mask use, a mixed-effects Poisson regression model was calculated to predict the number of cases for each team, with the state incidence, instructional delivery type, and face mask use (yes or no) as fixed effects, school as a random effect, and the log of player-days as an offset. Similarly, we created separate models for each sport characteristic (indoor, outdoor, individual, team, contact, noncontact) and each specific sport with > 40 reported cases. Incidence rates and 95% CIs were computed in each sport for those teams reporting face mask use or not and compared descriptively. (Swimming was excluded from the face mask analyses.) Coefficients from Poisson models were exponentiated to represent IRRs for binary variables, and Wald CIs were generated. Given the large number of teams with zero cases, we checked the dispersion to ensure the proper modeling distribution. The significance level was set a priori at the .05 level, and all tests were 2 tailed. All statistical analyses were performed in R (version 4.0.3; The R Foundation).19
RESULTS
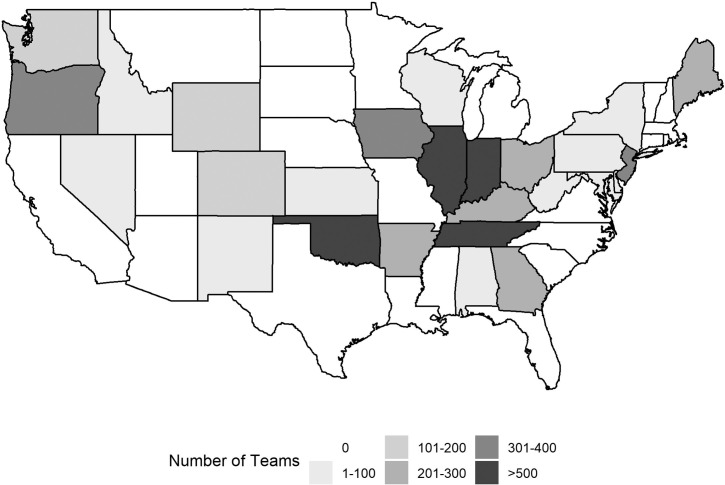
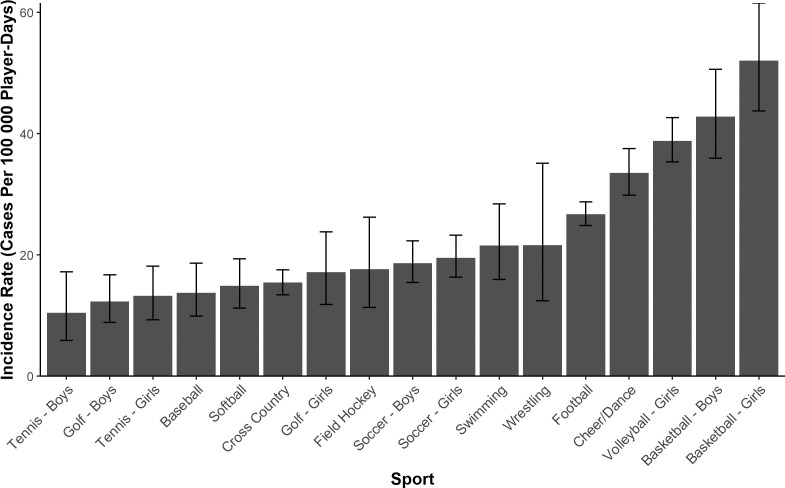
Survey responses were submitted by 1508 schools, of which 991 had restarted a fall sport. These schools represented 152 484 student-athletes on 5854 teams that had participated in 159 947 practices and 48 582 games. The distribution of participating teams by state is shown in Figure 1. A total of 899 (89.7%) schools reported using in-person instruction during fall 2020. Among the schools that had restarted participation, 2565 cases of COVID-19 were reported, yielding a case rate of 1682 cases per 100 000 athletes and an incidence rate of 24.6 (95% CI = 23.7, 25.6) cases per 100 000 player-days. Among 1375 different teams (15%) reporting at least 1 case of COVID-19 during the 3-month study period, 757 (57%) noted a single case and 1336 (97%) noted ≤5 cases (range = 1–16). No reported cases resulted in hospitalization or death. Reported, known-source cases numbered 1494 (58%); of these, 870 (20%) were attributed to household contact, followed by community contact outside sport or school (n = 516, 32%), school contact (n = 115, 4.5%), sport contact (n = 69, 2.7%), and other (n = 24, 0.9%). The unadjusted COVID-19 incidence rate ranged from 10.4 (boys' tennis) to 52.0 cases per 100 000 player-days (girls' basketball), as illustrated in Figure 2.
Figure 1.
Heat map demonstrating the number of responding teams from US high schools by state.
Figure 2.
Unadjusted incidence rates of COVID-19 among US high school sports during fall 2020. The incidence rate is shown as reported cases per 100 000 player-days for those sports with > 50 schools reporting reinitiation.
When aggregated by state, the overall COVID-19 case rates for athletes were highly correlated with the case rates for each respective state's general population (β = 1.09 ± 0.16, r = 0.81, P < .001; see Figure 3). The reported COVID-19 IRRs for specific sports, adjusted for the state COVID-19 incidence, instruction delivery type, and school repeated measures, are provided in Figure 4. After adjusting for state COVID-19 incidence, reported COVID-19 incidence among high school athletes was significantly and independently lower for outdoor versus indoor sports (IRR = 0.54; 95% CI = 0.49, 0.60; P < .001), noncontact versus contact sports (IRR = 0.78; 95% CI = 0.70, 0.87; P < .001), and virtual versus in-person instructional delivery (IRR = 0.70; 95% CI = 0.51, 0.97; P = .029); no association was identified with respect to team versus individual sports (IRR = 0.96; 95% CI = 0.84, 1.1; P = .49).
Figure 3.
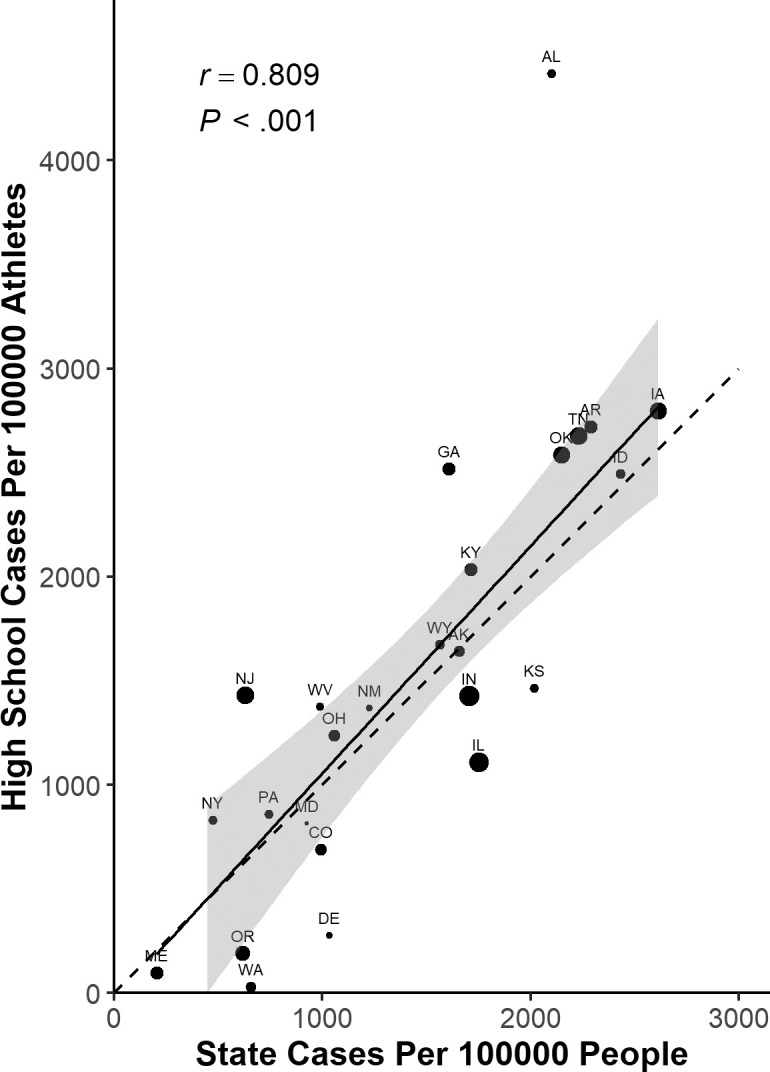
Reported COVID-19 case rates for high school athletes and the general populations of their respective states during fall 2020. The size of the point is scaled to the number of players from each state, and the dashed line represents a line of equality. The solid line and shaded area represent the regression line and 95% CI from the linear model weighted for the number of players from each state. Abbreviation: r = correlation coefficient.
Figure 4.
COVID-19 incidence rate ratios during fall 2020 for US high school sports, adjusted for the state COVID-19 incidence, instructional delivery type, and repeated measures from the same school. Includes those sports with > 50 schools reporting participation, with boys' soccer as reference. a P < .05.
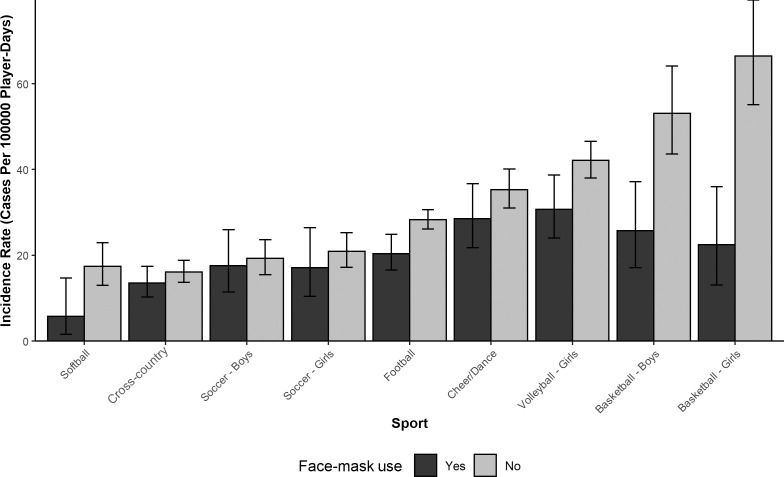
Face mask use by athletes at 284 schools (28%) while playing certain sports was reported, representing 1677 (28.6%) of all teams participating during the study period. Overall, teams reporting face mask use did not have a lower incidence of COVID-19 among players (IRR = 0.94; 95% CI = 0.75, 1.16; P = .55). However, COVID-19 incidence was lower with face mask use in players participating in indoor sports (Table 1). Differences in COVID-19 incidences between teams that did and those that did not use face masks in each sport are shown in Figure 5 for those sports with > 40 reported cases. Face mask use was also associated with a decreased COVID-19 incidence in boys' basketball, girls' basketball, and girls' volleyball and approached significance in football and cheer or dance, but no association was identified in other sports (Table 2).
Table 1.
Association of Reported Face Mask Use With the COVID-19 Incidence by Each Sport Characteristic Among US High School Athletes During Fall 2020a
| Sport Characteristic |
No. (%) |
Incidence Rate Ratio (95% CI) |
P Value |
| Indoor | 305 (23.5) | 0.44 (0.29, 0.66) | <.001 |
| Outdoor | 773 (18.4) | 1.02 (0.80, 1.31) | .88 |
| Individual | 441 (17.7) | 0.89 (0.64, 1.25) | .50 |
| Team | 637 (21.2) | 0.92 (0.70, 1.20) | .52 |
| Contact | 452 (20.9) | 0.86 (0.63, 1.18) | .36 |
| Noncontact | 626 (18.8) | 0.88 (0.66, 1.16) | .36 |
Incidence rate ratios and Wald CIs from separate, mixed-effects Poisson models for each sport characteristic to predict COVID-19 cases with local incidence and face mask use (yes or no) as fixed effects, school as a random effect, and log (player-days) as an offset.
Figure 5.
COVID-19 incidence rate ratios in each sport for those teams reporting the use of face masks or not among US high schools during fall 2020. Includes those sports with > 40 reported cases.
Table 2.
Association of Reported Face Mask Use With the COVID-19 Incidence in Each Sport Among US High School Athletes During Fall 2020a
| Sport |
No. (%) |
Incidence Rate Ratio (95% CI) |
P Value |
| Baseball | 39 (26.4) | 1.2 (0.44, 2.93) | .69 |
| Boys' basketball | 74 (25.7) | 0.53 (0.33, 0.83) | .008 |
| Girls' basketball | 78 (22.6) | 0.36 (0.19, 0.63) | <.001 |
| Cheer or dance | 96 (18.3) | 0.75 (0.53, 1.03) | .081 |
| Cross-country | 123 (15.7) | 0.86 (0.53, 1.31) | .5 |
| Football | 94 (14.0) | 0.79 (0.59, 1.04) | .10 |
| Boys' golf | 69 (18.9) | 0.57 (0.17, 1.42) | .28 |
| Boys' soccer | 74 (24.5) | 1.1 (0.65, 1.71) | .77 |
| Girls' soccer | 70 (20.5) | 1.3 (0.76, 2.18) | .3 |
| Softball | 39 (17.3) | 0.53 (0.12, 1.71) | .34 |
| Girls' volleyball | 120 (22.0) | 0.53 (0.37, 0.73) | <.001 |
Incidence rate ratios and Wald CIs from separate, mixed-effects Poisson models in each sport to predict COVID-19 cases with local incidence, school instruction type, and face mask use (yes or no) as fixed effects, school as a random effect, and log (player-days) as an offset,
DISCUSSION
These findings suggested that the incidence of COVID-19 among US high school athletes in fall 2020 differed by sport and sport characteristics. Although only a small proportion of the cases with a reported source were attributed to sport contact, indoor location and contact were independently associated with an increased incidence rate of COVID-19. This was the first evidence we were aware of that was derived specifically from a high school sport context, but it agreed with prior research and recommendations from various public health organizations that indicated COVID-19 was most likely to be transmitted among individuals in close proximity for prolonged periods and may have been more easily transmissible indoors than outdoors.8–10 Specifically, indoor versus outdoor sport participation appeared to have the strongest influence on COVID-19 incidence in our group of athletes, while contact had an independent yet weaker relationship. We did not find an independent association between COVID-19 incidence and team versus individual sport participation, suggesting that this effect was minimal after accounting for the influences of location and contact. This information appeared to be consistent with recent evidence from youth and professional sports that demonstrated minimal transmission of COVID-19 during outdoor sport participation.12,15,15,20,21 Although limited to case reports, our data were consistent with prior evidence suggesting that transmission may have occurred during participation in indoor sports with prolonged close contact.13,22
Public health organizations and sport governing bodies attempted to classify sports based on the expected risk of COVID-19 transmission8–11; however, we were aware of no earlier evidence that evaluated these within sport environments. With respect to the risk categories offered for high school athletics by the National Federation of State High School Associations,10 our findings agreed with the suggestion that outdoor, noncontact sports had the lowest COVID-19 incidence. These data also aligned with the indication that sports with close, sustained contact may have carried a relatively increased risk but that an indoor location may have had the strongest influence on the COVID-19 risk. Still, it should be noted that wrestling displayed an intermediate risk despite being an indoor sport with prolonged, close contact between participants. Why this would be the case is unclear, though the sample size in this sport was relatively small and, consequently, the CIs were relatively wide, making it difficult to confidently classify the risk associated with wrestling.
Participation was not reported in all sports during the same timeframe and, therefore, sports may have had different background COVID-19 incidences during their respective seasons. Nationwide COVID-19 cases decreased in 2020 through August and were relatively stable during September until they began increasing in October.23 Although we tried to account for differences in the state COVID-19 disease burden within our adjusted models by including state COVID-19 rates during the fall months, we could not exclude the possibility that the higher incidence among traditional winter sports may have been partly due to higher local COVID-19 incidences later in the study period when these sports began participation.
We found that face mask use was associated with a decreased incidence of COVID-19 in specific sports. In general, those sports with the highest incidence of COVID-19 also displayed the greatest benefit from reported face mask use. Specifically, the COVID-19 incidence was lower among indoor sports in which face masks were reportedly used when evaluated collectively, but this was also true in boys' basketball, girls' basketball, and volleyball when evaluated individually. Importantly, the reported COVID-19 incidence for indoor team sports (basketball, volleyball) when athletes used face masks appeared comparable with the incidence for outdoor team sports, suggesting that the increased risk associated with being indoors may be reduced considerably by face mask use. Face mask use also appeared to be associated with a decreased COVID-19 incidence in football and cheer or dance, even though this did not reach statistical significance. This finding may be attributable to the relatively small proportion of the teams in these sports that reported face mask use; a larger sample of teams using face masks in these sports might have revealed a significant association.
It should be noted that the number of cases attributed to transmission during sports was small, and it was difficult to fully assign differences in COVID-19 incidences between teams that did and those that did not use face masks to face mask use itself, as other behaviors that influenced risk may have confounded this relationship. For example, differences in the COVID-19 incidences between those who did and did not use face masks could have been attributed to concomitant risk-reduction policies at those schools. To attempt to address this, we included both school and instructional delivery method as covariates within the models to specifically try to account for the influence that school-specific factors may have had on the COVID-19 incidence. Nonetheless, the relationship between face mask use and the COVID-19 incidence persisted for certain types of sports, particularly indoor sports. Recent research in school settings indicated that in-school transmission was low when risk-reduction procedures were in place24 but that face mask use in schools was nonetheless associated with a reduced incidence of COVID-19.25 Therefore, while the influence of face masks on transmission was minimal in settings with an already low likelihood of transmission (eg, outdoor sports and those with low background levels of disease), face masks may have offered some protection in settings with a higher risk of transmission.
We were unable to identify publicly available, state-specific, adolescent case rates during the fall months for many of the represented states in our sample, yet we nonetheless noted a strong relationship between reported COVID-19 case rates in our high school athletes and the COVID-19 case rates among the general populations in their respective states. In addition, most cases with a reported source were attributed to household and community contact, with a much smaller proportion attributed to school or sport contact. This might suggest that the COVID-19 incidence in adolescent athletes largely reflected background COVID-19 rates in their community. The overwhelming majority of schools reported in-person instruction, making it difficult to fully evaluate the role of in-person school instruction in the COVID-19 incidence among high school athletes. Even so, we included school instruction type within our adjusted models to account for the confounding role this could have played in comparing groups.
Limitations
This study had several limitations. The information was self-reported by the athletic directors at each school and could not be directly verified through medical records or another independent source. Ideally, state-level, daily COVID-19 case data for adolescents would have been available, but because this was not publicly accessible in many cases, our adjusted models could only account for the population-level background incidence in each state. However, reported case rates in our sample and the state general populations were highly related. As mentioned earlier, the incidence of COVID-19 was likely not stable throughout the fall in many areas, and those sports that initiated play during periods of increased background incidence (winter sports in October, for example) may have been biased toward a higher incidence that was not directly attributable to the sport itself. We would have preferred to use individual-level case data with formal contact tracing by public health authorities. Unfortunately, these were not available, and sources of infection were provided by the schools themselves. It is possible that behaviors outside of sport that could have influenced COVID-19 risk were related to participation in certain sports or face mask use, and we could not account for these. We also could not directly account for the possibility of transmission among players that went unidentified. Finally, although these data represented information regarding a large number of male and female high school athletes from a nationwide sample, whether this sample was sufficiently heterogeneous with respect to characteristics such as geography or socioeconomic status as to be generalizable to all high school athletes is unknown. In addition, they may not be generalizable to older or younger athlete populations.
CONCLUSIONS
Our results suggested that certain high school sports and sport characteristics could have a greater relative risk of COVID-19 and that face mask use could help to reduce the risk of COVID-19 among adolescent athletes in sports with higher risks. Specifically, indoor sports appeared to have a greater risk of COVID-19 infection among participants, whereas outdoor, noncontact sports had the lowest risk. However, use of face masks was associated with a decreased incidence of COVID-19 in indoor sports, and this appeared to mitigate a large portion of the increased risk. Given the general lack of information regarding the COVID-19 risk among youth sport participants, this information may help guide decision making to reduce the risk of COVID-19 transmission while facilitating the wide-ranging physical and mental health benefits of sport participation.
REFERENCES
- 1.Bates LC, Zieff G, Stanford K, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children (Basel) . 2020;7(9):138. doi: 10.3390/children7090138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health . 2020;20(1):1351. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gouttebarge V, Ahmad I, Mountjoy M, Rice S, Kerkhoffs G. Anxiety and depressive symptoms during the COVID-19 emergency period: a comparative cross-sectional study in professional football. Clin J Sport Med . 2020;32(1):21–27. doi: 10.1097/JSM.0000000000000886. [DOI] [PubMed] [Google Scholar]
- 4.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci . 2020;9(4):302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr . 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res . 2020;293:113429. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGuine TA, Biese KM, Petrovska L, et al. Changes in the health of adolescent athletes: a comparison of health measures collected before and during the COVID-19 pandemic. J Athl Train . 2021;56(8):836–844. doi: 10.4085/1062-6050-0739.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coronavirus disease 2019 (COVID-19). Considerations for youth sports. Centers for Disease Control and Prevention. Reviewed May 19, 2020. Accessed December 21, 2020. https://stacks.cdc.gov/view/cdc/88186.
- 9.COVID-19 interim guidance: return to sports and physical activity. American Academy of Pediatrics. Accessed December 21, 2020. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-interim-guidance-return-to-sports/
- 10.Guidance for opening up high school athletics and activities. National Federation of State High School Associations. Accessed December 21, 2020. https://nfhs.org/media/3812287/2020-nfhs-guidance-for-opening-up-high-school-athletics-and-activities-nfhs-smac-may-15_2020-final.pdf.
- 11.Resocialization of collegiate sport: checklist. National Collegiate Athletics Association. Accessed December 21, 2020. http://www.ncaa.org/sport-science-institute/resocialization-collegiate-sport-checklist.
- 12.Drezner JA, Drezner SM, Magner KN, Ayala JT. COVID-19 surveillance in youth soccer during small group training: a safe return to sports activity. Sports Health . 2021;13(1):15–17. doi: 10.1177/1941738120964458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atubin D, Wiese M, Bohinc B. An outbreak of COVID-19 associated with a recreational hockey game—Florida, June 2020. MMWR Morb Mortal Wkly Rep . 2020;69(41):1492–1493. doi: 10.15585/mmwr.mm6941a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Most school-associated COVID-19 cases in Shelby County are sports-related, officials say. Memphis Commercial Appeal. Published October 22, 2020. Accessed December 21, 2020. https://www.commercialappeal.com/story/news/education/2020/10/22/most-school-associated-covid-19-cases-shelby-county-sports-related-officials-say/3735873001/
- 15.Jones B, Phillips G, Kemp S, et al. SARS-CoV-2 transmission during rugby league matches: do players become infected after participating with SARS-CoV-2 positive players? Br J Sports Med . 2021;55(14):807–813. doi: 10.1136/bjsports-2020-103714. doi: [DOI] [PubMed] [Google Scholar]
- 16.Schumacher YO, Tabben M, Hassoun K, et al. Resuming professional football (soccer) during the COVID-19 pandemic in a country with high infection rates: a prospective cohort study. Br J Sports Med . 2021;55(19):1092–1098. doi: 10.1136/bjsports-2020-103724. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.COVID-19 return-to-sport considerations for secondary school athletic trainers. National Athletic Trainers' Association. Published May 2020. Accessed September 22, 2020. https://www.nata.org/sites/default/files/covid_19_return-to-sport_considerations_for_secondary_school_ats_1.pdf.
- 18.US COVID-19 cases and deaths by state. USAFacts. Accessed January 7 2021. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/
- 19.R Core Team. R: a language and environment for statistical computing. The R Project for Statistical Computing. Accessed February 13, 2019. http://www.R-project.org/
- 20.Sasser P, McGuine T, Haraldsdottir K, et al. Reported COVID-19 incidence in Wisconsin high school athletes in fall 2020. J Athl Train . 2021;57(1):59–64. doi: 10.4085/1062-6050-0185.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watson AM, Haraldsdottir K, Biese KM, Goodavish L, Stevens B, McGuine TA. COVID-19 in US youth soccer athletes during summer 2020. J Athl Train . 2021;56(6):542–547. doi: 10.4085/610-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atherstone C, Siegel M, Schmitt-Matzen E, et al. SARS-CoV-2 transmission associated with high school wrestling tournaments—Florida, December 2020–January 2021. MMWR Morb Mortal Wkly Rep . 2021;70(4):141–143. doi: 10.15585/mmwr.mm7004e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVID data tracker Centers for Disease Control and Prevention. Accessed December 30, 2020. https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
- 24.Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 cases and transmission in 17 K–12 schools—Wood County, Wisconsin, August 31–November 29, 2020. MMWR Morb Mortal Wkly Rep . 2021;70(4):136–140. doi: 10.15585/mmwr.mm7004e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Budzyn SE, Panaggio MJ, Parks SE, et al. Pediatric COVID-19 cases in counties with and without school mask requirements—United States, July 1–September 4, 2021. MMWR Morb Mortal Wkly Rep . 2021;70(39):1377–1378. doi: 10.15585/mmwr.mm7039e3. [DOI] [PMC free article] [PubMed] [Google Scholar]