Abstract
Despite guidelines that assert that the vaginal route for benign hysterectomy is preferred as the most minimally invasive approach, rates of vaginal hysterectomy remain very low in the United States. Vaginal natural orifice transluminal endoscopic surgery (vNOTES) might reverse the trend. Potential advantages of vNOTES compared to traditional laparoscopic and robotic approaches include the potential for less pain, decreased operative time, improved cosmesis, and decreased risks. Importantly, vNOTES might allow for the conversion of laparoscopic and robotic routes back to vaginal due to surgeon factors.
Keywords: Minimally invasive gynecologic surgery, vNOTES, Vaginal natural orifice transluminal endoscopic surgery, Vaginal surgery
INTRODUCTION
In the most recent update on nationwide hysterectomy numbers which included inpatient and outpatient all-payer databases, Wright and co-authors describe a concerning trend in the United States over the past two decades.1 The total number of benign hysterectomies declined to 452,226 in 2018, an 8% decrease over two years, and the number of vaginal hysterectomies dropped to 54,219, a 19% decrease over the same period. When looking at hysterectomies done for benign indications, only 12% of hysterectomies were done vaginally; 66% were done laparoscopically or robotically. Unfortunately, the authors could not determine the actual number and proportion of benign vaginal hysterectomies performed for indications other than pelvic organ prolapse (personal communication). They are currently analyzing additional data to answer this question but based on their estimate and our experiences in the field, we suspect the percentage is very low. For all practical purposes, vaginal hysterectomy, except in the setting of pelvic organ prolapse, is extinct. Although all professional gynecologic surgical societies, including the American Congress of Obstetricians and Gynecologists (ACOG), continue to assert that the vaginal route for benign hysterectomy is preferred when feasible, the exact opposite is occurring in current practice.2,3
This paper aims to describe the technique and current surgical landscape of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecology and to explore why and how vNOTES might reverse the decline in vaginal hysterectomy numbers.
What is vNOTES?
Despite its emergence on the surgical scene over a decade ago, most obstetric and gynecologic (OB/GYN) surgeons are not familiar with vNOTES. As multiport laparoscopy and robotics replaced open surgery in most specialties, surgeons started looking for other ways to innovate. As a result, laparoendoscopic single-site surgery (LESS) emerged.4 In LESS, multiple instruments (typically a camera and two or three additional instruments) pass through one port (typically at the umbilicus) with advantages including better cosmesis and potentially less pain. LESS port options include several commercially available products (Figure 1A–C). In low-resource settings, especially in the developing world, where commercially made ports are not available, a self-made port using a surgical glove placed over a small wound retractor is occasionally used, although this off-label use lacks Food and Drug Administration (FDA) approval.5–7 (Figure 2).
Figure 1.

(A) Transabdominal multichannel commercially available single-site port (GelPOINTR Mini) (Applied Medical, Rancho Santa Margarita, CA) placed into the umbilicus. Obtained with permission from Applied Medical, Rancho Santa Margarita, California. (B) Transabdominal multichannel commercially available single-site port (GelPOINT Mini) placed into umbilicus with one additional assist port for laparoscopic myomectomy setup. Obtained with permission from Applied Medical, Rancho Santa Margarita, California. (C) Transabdominal multichannel commercially available single-site port (GelPOINTR Mini) (Applied Medical, Rancho Santa Margarita, CA) placed suprapubically in a multiport laparoscopic surgery setup for general surgery cases. Obtained with permission from Applied Medical, Rancho Santa Margarita, California.
Figure 2.

Self-made two-channel single-site port.7
Learning LESS turned out to be quite challenging for technical reasons, including a limited number of working instruments, restricted movements, clashing of instruments, limited smoke evacuation, loss of triangulation with straight instruments, image reversal with angled instruments, and higher risk of postoperative incisional or umbilical hernias. The difficult learning curve and the narrow margin of benefit over multiport laparoscopy resulted in low utilization.8 Robotic-assisted LESS addressed some of the laparoscopic LESS challenges but still did not reach widespread adoption. One unanticipated consequence of the LESS port use was its adoption for contained morcellation in minimally invasive gynecologic surgery (MIGS). “In-bag” or contained morcellation became standard surgical practice after 2014; a LESS port placed into a mini-laparotomy (2 – 3 cm) abdominal incision used during multiport or robotic surgery was easily converted into an extraction site for contained morcellation at the end of the case.
NOTES emerged as an extension of LESS. The goal of NOTES was to reach the abdominal cavity using natural orifices such as the stomach, esophagus, rectum, bladder, and vagina; however, transvaginal vNOTES emerged as the preferred approach due to the lowest risk of contamination and improved visualization, closure, and healing.9 A self-constructed LESS port (sterile glove fitted over a wound retractor with ports inserted into glove fingers) was initially used by early adopters before a commercial product became available (Figure 3).6 In 2019, the FDA approved a LESS port specifically created for the vNOTES (GelPOINTR V-Path transvaginal access platform, Applied Medical, Rancho Santa Margarita, California) (Figure 4).
Figure 3.

Self-constructed multichannel single-site port device for vaginal natural orifice transluminal endoscopic surgery. Courtesy of Jan Baekeland, MD.
Figure 4.
Commercially available multichannel single-site port device for vaginal natural orifice transluminal endoscopic surgery (GelPOINTR V-Path). Obtained with permission from Applied Medical, Rancho Santa Margarita, California.
Currently, mainstream vNOTES procedures include hysterectomy, uterosacral ligament suspension,10,11 and adnexal procedures (salpingectomies, oophorectomies, and ovarian cystectomies). Furthermore, several studies have been published describing the use of vNOTES in different settings: large uteri,12 obesity,13 nulliparous patients,14 repeat vNOTES,15 and prior hysterectomy.16 At this time, myomectomies, endometriosis excision,17 lymph node sampling,18,19 and sacrocolpopexies20 are not done routinely via the vNOTES route and remain optimally addressed via laparoscopic and robotic routes.
vNOTES is not a new surgical technique or tool, but rather a new surgical approach that combines and modifies several existing techniques. For example, the traditional vaginal approach, well-established for a hysterectomy, has been used for salpingectomies for sterilization (which are commonly done in the developing world) and uterosacral ligament hysteropexies. As in vaginal hysterectomies, the vNOTES route incorporates the use of bipolar vessel-sealing energy devices to reduce blood loss and operative time, and enables volume reduction techniques such as coring and wedging.21–25 Unlike traditional vaginal surgery; however, vNOTES hysterectomy makes contained tissue extraction possible as the uterus and adnexa can be placed into a containment bag at the end of the case and the specimen does not need to be fragmented to obtain volume reduction. Although the risk of “uncontained” vaginal tissue extraction remains very low during vaginal hysterectomy,26 containment bags can be used during vNOTES surgery where such containment is clinically indicated or desired.
vNOTES Technique
Tips and tricks for technique and instrumentation are described in Table 1. vNOTES hysterectomy begins in the same way as vaginal hysterectomy: a circumferential incision is made and the anterior and posterior colpotomy is performed followed by clamping, cutting, and ligation of the uterosacral ligaments. The vNOTES port is then placed and insufflated. Starting on the patient’s left side, the cervix is pushed medially and cephalad to expose the uterine vessels, which are transected with the bipolar device, followed by the transsection of the broad and round ligaments. Salpingectomy is performed next in case of ovarian conservation, but ovarian attachments (utero-ovarian or infundibulopelvic ligament) are left intact until the right side is detached to stabilize the uterus. Some surgeons prefer to leave round ligaments instead of utero-ovarian or infundibulopelvic ligaments attached (because they prefer to control the blood supply to the uterus). The same steps are repeated on the right side, but this time the adnexa is detached. Finally, the surgeon detaches the remaining attachment on the left, and the pelvis is inspected. After completion of the hysterectomy, the port is disassembled and the specimen is removed. In cases of c-section scar, or limited vaginal access (postmenopausal, nulliparous), the ring can be placed into the posterior cul-de-sac peritoneally but can sit in the anterior fornix (similar to a ring pessary), which then allows for continuing dissection vaginally with laparoscopic instruments until the anterior colpotomy can be safely completed. For adnexal surgery where the uterus is not removed, the vNOTES port is placed into the posterior cul-de-sac, but a smaller ring is utilized.
Table 1.
Technique of Vaginal Natural Orifice Transluminal Endoscopic Surgery Hysterectomy and Concomitant Procedures
| Step of the procedure | Suggestions on technique | Rationale |
|---|---|---|
| Setup | ||
| Draping | Use a drape similar to what is being used for LAVH or TLH | Allows to easy placement of umbilical port in case need to visualize pelvis from above, or in case conversion from vNOTES to the laparoscopic route is needed |
| Preparation | Abdominal and vaginal antiseptic solution (most commonly chlorhexidine), same as what is used for LAVH or TLH | No change in the standard of care in comparison to LAVH or TLH |
| Antibiotics | Same as LAVH or TLH, most commonly cephalosporin and metronidazole | No change in the standard of care in comparison to LAVH or TLH |
| Vaginal hysterectomy instruments | Include a long retractor of choice (right angle, Briesky, Dolen) | Long retractor is used to guide the introducer for the ring |
| Laparoscopic instrumentation | Grasper (atraumatic, “wavy” or a bipolar grasper)A bipolar sealing device with cutting blade | |
| Laparoscopic instrumentation | Laparoscopic suction irrigation is not needed | If suction is needed, use Yankhauer inserted into one of the ports or disassemble LESS port and suction pelvis with ring in place |
| Vaginal entry and ring placement | ||
| Anterior colpotomy | Place an interrupted suture from anterior peritoneum to anterior vaginal mucosa | Assures that ring fits into an anterior cul-de-sac with ease and peritoneum “curtain” is not hanging anteriorly, obstructing the view |
| Stretch anterior perineum after sharp entry with index fingers | Assures enough space for the ring to sit properly in the anterior cul-de-sac | |
| Posterior colpotomy | Place an interrupted suture from the posterior peritoneum to the posterior vaginal mucosa | Assures easy ring placement and decreases chance of it “popping out” |
| Uterosacral ligament ligation | Suture ligate ligaments with double or triple fixation; tag ligaments | Assures secure suture placement, less likely to have to secure ligaments again at the end of the case |
| After ring placement, prior to port assembly | Place a large laparotomy pad into a posterior cul-de-sac | Retracts sigmoid during the case; Aids with sigmoid retraction during uterosacral ligament suspension; Serves as a “backdrop” during adnexectomy to aid with depth perception when looking toward the pelvic brim, decreasing the risk of small and large bowel coming too close to the surgical field |
| Complications | Same approach to management as in vaginal surgery | No change in the standard of care in comparison with vaginal surgery |
| Laparoscopy | ||
| Trandelengerg during laparoscopy | Case-dependent, less than with transabdominal laparoscopy; In case of morbid obesity, can tolerate less Trandelengerg and still get adequate exposure |
Less Trendelenberg improves physiologic parameters and decreases risk |
| Insufflation pressure | Lower than during laparoscopy | Adequate visualization is easier to achieve than in transabdominal laparoscopy |
| Flow rate | Lower than during laparoscopy | Adequate visualization is easier to achieve than in transabdominal laparoscopy |
| Angle of laparoscope | 30-degree angled laparoscope | Less internal instrument and camera collisions |
| Length of laparoscope | Bariatric | Less external instrument and camera collisions |
| Right angle adapter for light source | Less external instrument and camera collisions | |
| Complications | If vaginal or vNOTES repair is not possible, have a low threshold to convert to laparoscopy | |
| Getting started | ||
| Take a hands-on vNOTES course | Includes didactic and hands-on simulation practice | |
| Engage with a colleague (or proctor if not available) who is already doing vNOTES to observe their cases and to have them observe yours | Best practices in surgical education | |
| Chose low- or moderate complexity case as your first case | Best practices in surgical education | |
| Watch vNOTES videos to prepare for your first case | Best practices in surgical education | |
| Record your cases, engage with mentor to do video review | Best practices in surgical education | |
| Low threshold to place umbilical port to visualize pelvis | Best practices in surgical education as adopted to vNOTES | |
| If you are not confident with colpotomy and vaginal part of the procedure, consider asking a colleague who performs vaginal hysterectomies to assist and coach you until you obtain skillset needed | Best practices in surgical education |
Abbreviations: LAVH, laparoscopically assisted vaginal hysterectomy; TLH, total laparoscopic hysterectomy; vNOTES, vaginal natural orifice transluminal endoscopic surgery.
Contraindications to vNOTES include patients with conditions that are likely to scar or obliterate the posterior cul-de-sac, such as low colorectal surgery, pelvic radiation, severe pelvic inflammatory disease, and endometriosis.5,27 Surgeons vary in their comfort level with the vaginal colpotomy (steps before laparoscopic portion), which can become the rate-limiting step for successful vNOTES surgery on patients with limited vaginal access (such as low parity, obesity, prior c-sections, lack of descent, large and bulky uterus). Cervical and lower uterine segment myomas may increase case complexity due to ring placement.
Benefits and Challenges of vNOTES
A potential advantage of vNOTES compared to open and transabdominal multiport and LESS laparoscopic and robotic approaches include the potential for less pain, decreased operative time, improved cosmesis, and decreased risks related to abdominal entry and port placement, especially in patients with multiple prior abdominal surgeries, such as visceral and abdominal wall injuries, port site hernias, and nerve entrapments.
From a technical standpoint, several advantage of vNOTES over transabdominal LESS include a larger and less rigid opening after vNOTES colpotomy compared to minilaparotomy or transabdominal incisions. In addition, the target tissue is closer to the port, significantly decreasing restricted movements and clashing of instruments, and the uterus is used as another point for triangulation that is closer to the instruments and scope. Furthermore, the smoke plume disseminates into the upper abdomen, making it less likely to obstruct the view, and the camera and instruments are less likely to collide with each other (commonly referred to as “sword fighting”) with the use of bariatric scopes, a 30-degree lens, and an angled adapter for the light source.
For obese and morbidly obese, vNOTES also allows for significantly less Trendelenburg (laparotomy packs can be used to pack away the bowel), compared to traditional laparoscopy and robotics, allowing the use of lower insufflation pressures, and translating to shorter operative times.
Another potential benefit unique to vNOTES includes the use of fewer surgical assistants. The assistant to the primary surgeon drives the camera, and the primary surgeon operates alone, similar to robotics but without the need for a skilled and expensive bedside assistant. Additionally, a benefit of the “bottom-up” compared to the “top-down” approach is that the camera provides superior visualization much closer to the target tissue including the ureter at the level of the infundibular ligaments or uterine arteries and uterosacral ligaments at the time of apical suspension.
Describing this procedure in a novel way, vNOTES allows for a different approach to the target organs. For example, when tackling bladder adhesions from prior c-sections during a hysterectomy, one common laparoscopic technique is to skeletonize and seal the uterine arteries first. Then the vesicovaginal space is approached from lateral to medial, which lateralizes the bladder and ureters, and mobilizes them caudally, away from the scar, minimizing the risk of injury and bleeding. With vNOTES (as with traditional vaginal hysterectomy), the vesicovaginal space is typically developed first, then the uterine arteries are sealed before addressing the remaining scar—the same approach is performed in a different order, tackling the easier dissections before the more difficult one. Another example relates to patients with severe mid and upper abdominal adhesions from prior surgeries where the vNOTES approach may eliminate the need for extensive adhesiolysis, which would have been necessary with the transabdominal laparoscopic or robotic approaches. Moreover, when tackling hysterectomies for enlarged uteri (large fibroids, adenomyosis), instead of moving down deeper into the pelvis in transabdominal laparoscopy, the surgeon performing vNOTES moves the uterus cephalad, further into the abdomen, creating more space to operate and controlling the uterine blood supply at the beginning of the case.5
When an apical suspension is needed, there is potential for improved visualization and more precise and higher apical suture placement to reduce the risk of ureteral kinking with vNOTES. While we do not have data on ureteral injury and kinking rates with vNOTES uterosacral ligament suspensions yet, we do know that route may play a role from studies done on vaginal and laparoscopic approaches.28–30 Adnexectomy may also be completed more easily with vNOTES compared to straightforward transvaginal surgery (e.g. in cases such as bilateral salpingo-oophorectomy for breast cancer and transgender patients). The lack of visible laparoscopy scars is an important cosmetic advantage for transgender patients undergoing hysterectomies or other patients who want to conceal salpingectomies for sterilization or hysterectomies for personal or cultural reasons.
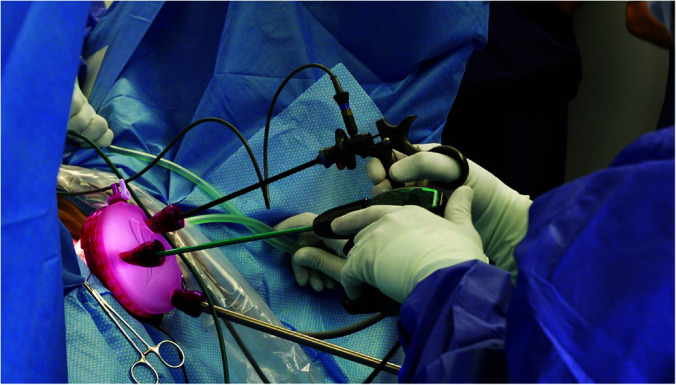
vNOTES represents a potential ergonomic advantage as more awareness of work-related musculoskeletal disorders (WRMDs) and workplace injuries with a focus on prevention, early recognition, treatment, and research gains prominence. Unlike laparoscopy and vaginal surgery, where the surgeon remains in a nonneutral, constrained position for prolonged periods of time,31,32 the vNOTES surgeon could likely operate in a neutral position seated or standing, and unlike robotics, not static at the console for prolonged periods of time (Figure 4). Furthermore, the mechanics and ergonomics of vNOTES are potentially more favorable compared to unassisted transvaginal surgery due to surgeon mechanics.
With regard to cost and efficiency, more studies are needed, but the following should be considered. Excluding operative time and robotics (the latter of which would also need to factor in the cost of skilled bedside assistants and the additional robotic equipment), the vNOTES setup compared to laparoscopy has the potential for cost savings. With vNOTES, no accessory ports, no laparoscopic suction, no barbed suture for cuff closure, nor suture or skin glue for fascia and skin closure are needed. In addition, fewer instruments are needed and equipment management is easier for the nursing and operating room staff. While the added cost of the commercially available vNOTES port (GelPOINTR V-Path transvaginal access platform, Applied Medical, Rancho Santa Margarita, California) compared to unassisted vaginal surgery will be greater, these costs will have to be balanced against the operative time and recovery room stay, risk of surgeon musculoskeletal injury, patient perceptions of surgery experience, and potential for greater efficiency and decreased risk of complications.
vNOTES also presents unique challenges. Most importantly, the surgeon must be able to perform an anterior and posterior colpotomy, which appears to be a rate-limiting step in vNOTES adoption. In higher-complexity cases with difficult vaginal access such as a narrowed introitus and vaginal canal, limited descent, narrow pubic arch, and conditions such as obesity, nulliparity, postmenopausal atrophy, testosterone use in transgender patients, colpotomies are more difficult and require skills to address them. One potential solution to this obstacle would be for urogynecologists and vaginal surgeons to partner up with surgeons who are on their vNOTES learning curves. With such a setup, an experienced surgeon can guide their colleagues through the colpotomies. Notably, in a large series (over 1000 hysterectomy cases) by high-volume surgeons, cystotomy rates were low at 1.2%.33 In addition, surgeons have to think differently about case selection. For example, endometriosis excision is still best done from “above” (transabdominal laparoscopy or robotics). In addition, while the “bottom-up view” is advantageous as described above, it can also be limiting because the surgeon may not be able to see potential pathology (for example, middle and upper abdominal bowel adhesions to a large fibroid uterus) which may require surgeons to have a lower threshold or higher conversion rate to laparoscopy. While conversions are quality metrics we generally try to avoid, converting from vNOTES to a laparoscopic route is generally considered a reversion to a default approach. The role of pre-operative imaging in vNOTES is not clear at this time and high-quality transvaginal ultrasound or magnetic resonance imaging might be beneficial in select cases.
To address this, innovation continues as a novel robotic system was developed recently which combines a vNOTES LESS port for instrumentation with a transabdominal LESS port for camera and accessory trocar insertion.34 A new robotic platform, Hominis Arms™ (Memic Innovative Surgery Ltd., Or Yehuda, Israel), approved by the FDA in 2021 for hysterectomy and adnexectomy, combines a transabdominal laparoscopic view from “above” via a separately inserted laparoscope with the vaginal LESS approach using wristed robotic instruments placed through the posterior cul-de-sac.34,35
Robotic platforms are also being explored in the setting of vNOTES. Xiaoming Guan and colleagues published a small comparative feasibility study of traditional laparoscopic and robotic-assisted vNOTES hysterectomies.36 Robotic-assisted vNOTES publications currently consist of case reports and series describing hysterectomies,37,38 sacrocolpopexies,39,40 bowel deep infiltrating endometriosis,17 and myomectomy,41 mostly by two surgical teams (Dr. Xiaoming Guan in Baylor, Texas and Dr. Chyi-Long Lee in Taiwan). Single site Xi da Vinci robotic system (Intuitive Surgical, Sunnyvale, CA) via vaginal LESS port to treat endometriosis is considered experimental at this time, with only one single institution retrospective review of 33 published cases.42
History and Introduction of vNOTES in the United States
vNOTES approach was first reported in general surgery for appendectomies and cholecystectomies.43,44 In 2012, Chyi-Long, a MIGS surgeon in Taiwan, and this team were the first to describe vNOTES for adnexal surgery in gynecology,45 and around the same time, the first feasibility study describing vNOTES hysterectomies was published, utilizing self-made LESS ports (Figures 2 and 3).46 Jan Baekeland, a gynecologic oncologist in Belgium, was an early adapter of this technique6 in Europe, and used a multichannel commercially available transabdominal single-site port (GelPOINTR Mini) (Applied Medical, Rancho Santa Margarita, CA) in vNOTES, although this use remains off-label (Figure 1). A group of gynecologic surgeons from the United States (Alexander Burnett, Grover May) traveled to Belgium in 2017 to train and brought this technique to the United States. Since then, over 550 surgeons have taken the Applied Medical vNOTES course at the time of writing of this manuscript with monthly courses occurring (personal communication). Finally, in 2019, the FDA approved a multichannel single-site port device for vNOTES (GelPOINTR V-Path transvaginal access platform, Applied Medical, Rancho Santa Margarita, California), specifically designed for the transvaginal route.
Tracking vNOTES cases and outcomes is a challenge similar to other gynecologic surgical procedures, but it is especially problematic given that no current procedural terminology code exists for this route. Most surgeons use laparoscopically assisted vaginal hysterectomy codes for vNOTES hysterectomy when billing, which complicates tracking. International NOTES Society (iNOTESs) is managing a voluntary case registry, but this data is not available for public use.47
What is the Evidence?
Jan Baekeland and his colleagues described complication rates in vNOTES hysterectomies in a large series,33 followed by two noninferiority randomized controlled trials (RCT) comparing vNOTES to the transabdominal laparoscopic approach. One is HALON (Hysterectomy by transAbdominal Laparoscopy Or Natural orifice transluminal endoscopic surgery), a noninferiority blinded RCT powered for conversions. The authors randomized 70 patients to vNOTES hysterectomy with sham skin incisions or laparoscopic hysterectomy (ClinicalTrials.gov NCT02631837).48 The authors concluded that vNOTES hysterectomy was noninferior to laparoscopic hysterectomy; the vNOTES arm had a shorter length of stay and lower rates of complications. Similarly, vNOTES was not inferior to laparoscopy in the NOTABLE trial (transvaginal Natural orifice Transluminal endoscopic Adnexectomy for Benign pathology compared with Laparoscopic Excision) (ClinicalTrials.gov NCT02630329). In addition, the vNOTES group had lower pain scores and shorter operative times but a nonsignificant trend toward higher complications, mostly due to bleeding.49
A systematic review and meta-analysis comparing vNOTES to laparoscopic hysterectomy published in 2020 included one RCT and five retrospective cohort trials.50
Authors found that vNOTES had shorter operative times, shorter length of stay, and lower estimated blood loss with no difference in complications, readmissions, and pain scores.
Reasons for Declining Rates of Vaginal Hysterectomy
The reasons behind the near disappearance of vaginal hysterectomy from the surgical repertoire (except for vaginal hysterectomy for prolapse) are worth exploring. While the decline in total hysterectomy numbers might be related to improved medical therapies, expansion of uterine-preserving procedures, and changing attitudes toward hysterectomy,1 the reasons for the declining rate of vaginal hysterectomy is a complicated topic with multiple potential causes.51,52 While some individual surgeons maintain high vaginal hysterectomy rates (up to 30%), most do not. In 2016, Dr. Andrew Walter, who was leading initiatives to increase MIGS and vaginal hysterectomy rates at Kaiser Permanente, proposed a goal rate of vaginal hysterectomy of at least 40%.52 Along those lines, institutional and local efforts have shown it is feasible to achieve rates as high as 90%.53,54 Furthermore, high-volume vaginal surgeons deliver the most value overall due to lower complication rates and shorter operative times.55
Recent attempts to implement initiatives to increase vaginal hysterectomy rates included ACOG regional cadaveric courses and annual hands-on cadaver courses organized by the vaginal surgery special interest group at the American Association of Gynecologic Laparoscopists. Neither has resulted in a significant uptick in vaginal hysterectomy rates.
With the emergence of laparoscopic hysterectomy, more open surgeries were converted to laparoscopic over vaginal, even though it was harder to learn and do. For many, the laparoscopic route was easier for surgeons compared to the vaginal because of the global view even with the most skillful retraction in vaginal surgery. Patients do nearly as well with laparoscopic recovery as with vaginal. Finally, the emergence of the science of surgical ergonomics and increased recognition of surgeon WRMD may have led many to abandon vaginal surgery for laparoscopy and laparoscopy for robotic surgery.31
According to the Accreditation Council for Graduate Medical Education (ACGME), OB/GYN residents are required to log 85 total hysterectomies to graduate, with a 15-case minimum in the vaginal hysterectomy category. However, work by Jelovsek and colleagues showed that when resident performance is objectively measured in the operating room with standardized tools, minimal competency cut-off requires residents to perform at least 27 vaginal hysterectomies.56 As such, ACGME level of surgical exposure in residency does not approach proficiency, and recent surveys suggest that residents feel more comfortable with laparoscopic compared to vaginal hysterectomy (only 28% of residents felt comfortable with the vaginal approach).57 Except for female pelvic medicine and reconstructive surgery and few MIGS fellowships that offer vaginal hysterectomy training, there are few training opportunities after residency which only accelerates the decline of the transvaginal technique.
How Does vNOTES Fit into the Current Surgical Landscape in Gynecology?
Let’s consider a few clinical scenarios concerning case selection as surgeons go through their vNOTES learning curves. First, the goal would be to convert less complex laparoscopic hysterectomies such as for abnormal uterine bleeding, adenomyosis, and fibroids. to vNOTES. The next step would be to convert laparoscopic and robotic cases to vNOTES, such as hysterectomies with prior c-sections, mid- and upper-abdominal surgeries, and more distorted uterine anatomy (larger fibroids, more difficult locations). Since urogynecologists are the primary vaginal hysterectomy teachers for residents and fellows, the desired consequence of converting vaginal uterosacral ligament suspensions to vNOTES due to improved technique (as above), would be the training of the next generation of residents and fellows. Those new vNOTES-trained surgeons will be more likely to adopt vNOTES into their practice, and in turn, train others. In addition, once vNOTES becomes more commonplace, salpingectomies (for sterilization), prophylactic bilateral salpingo-ophorectomies, uterosacral ligament hysteropexies, and transgender hysterectomies will be converted from laparoscopic/robotic to vNOTES route.
We suspect that with vNOTES, the vaginal route can be easily attained in 30% – 50% of all hysterectomies across different skill sets and practice settings. Conversely, this rate might be higher for surgeons who handle lower complexity cases, and less applicable to MIGS practices that get more endometriosis and pelvic pain referrals.
Surgeons in Practice: Past, Present, and Future
The emergence of laparoscopy initiated the decline of vaginal surgery, with robotics putting an additional dent in vaginal surgery rates. Despite the increased cost and a significant learning curve,58–62 laparoscopic surgery became more prevalent. With improved visualization and the development of laparoscopic techniques that were not possible via open and vaginal routes, some surgeons who abandoned vaginal surgery for laparoscopic and robotic routes. Newly trained fellows and residents were not getting vaginal training as a result.
vNOTES might be a unique technique that serves the younger generation of surgeons who will adopt it because they are used to laparoscopic techniques. Older surgeons who feel left out of robotics and laparoscopy might use it as a way to learn new laparoscopic skills and pass down vaginal skills. The common goal would be to build a community of practice and provide short- and long-term support. Surgical coaching models might be of benefit in this endeavor.63 It is our prediction and hope that vNOTES will bring vaginal surgery back and lead to future innovation and advances.
Footnotes
Acknowledgements: none.
Funding sources: none.
Disclosure: VL is a consultant for Applied Medical. GM is a consultant for Applied Medical.
Conflict of interests: none.
Informed consent: Dr. Veronica Lerner declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Veronica T. Lerner, Department of Obstetrics & Gynecology, Lenox Hill Hospital, Northwell Health, New York, NY..
Grover May, Department of OB/GYN, ETSU College of Medicine, Department of OBGYN, Johnson City, TN..
Cheryl B. Iglesia, Departments of Obstetrics and Gynecology and Urology, Georgetown University, Washington, DC..
References:
- 1.Wright JD, Huang Y, Li AH, Melamed A, Hershman DL. Nationwide estimates of annual inpatient and outpatient hysterectomies performed in the United States. Obstet Gynecol. 2022;139(3):446–448. [DOI] [PubMed] [Google Scholar]
- 2.Committee Opinion No. 701 Summary: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017;129(6):1149–1150. [DOI] [PubMed] [Google Scholar]
- 3.Moen M, Walter A, Harmanli O, et al. Considerations to improve the evidence-based use of vaginal hysterectomy in benign gynecology. Obstet Gynecol. 2014;124(3):585–588. [DOI] [PubMed] [Google Scholar]
- 4.Georgiou AN, Rassweiler J, Herrmann TR, et al. Evolution and simplified terminology of natural orifice transluminal endoscopic surgery (NOTES), laparoendoscopic single-site surgery (LESS), and mini-laparoscopy (ML). World J Urol. 2012;30(5):573–580. [DOI] [PubMed] [Google Scholar]
- 5.Burnett AF, Rojo MO. Vaginal natural orifice transluminal endoscopic surgery for gynecologic and gynecologic oncology procedures. In: Marchand G., editor. Single Port Gynecologic Laparoscopic and Robotic-Assisted Surgery. London: Intech Open; 2021. Accessed: May 26, 2022. Available from: https://www.intechopen.com/chapters/76497. [Google Scholar]
- 6.Baekelandt J. Total vaginal NOTES hysterectomy: a new approach to hysterectomy. J Minim Invasive Gynecol. 2015;22(6):1088–1094. [DOI] [PubMed] [Google Scholar]
- 7.Chen YJ, Wang PH, Ocampo EJ, Twu NF, Yen MS, Chao KC. Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2011;117(4):906–912. [DOI] [PubMed] [Google Scholar]
- 8.Greaves N, Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011;93(6):437–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santos BF, Hungness ES. Natural orifice translumenal endoscopic surgery: progress in humans since white paper. World J Gastroenterol. 2011;17(13):1655–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aharoni S, Matanes E, Lauterbach R, Mor O, Weiner Z, Lowenstein L. Transvaginal natural orifice transluminal endoscopic versus conventional vaginal hysterectomy with uterosacral ligament suspension for apical compartment prolapse. Eur J Obstet Gynecol Reprod Biol. 2021;260:203–207. [DOI] [PubMed] [Google Scholar]
- 11.Lowenstein L, Baekelandt J, Paz Y, Lauterbach R, Matanes E. Transvaginal natural orifice transluminal endoscopic hysterectomy and apical suspension of the vaginal cuff to the uterosacral ligament. J Minim Invasive Gynecol. 2019;26(6):1015. [DOI] [PubMed] [Google Scholar]
- 12.Nulens K, Bosteels J, De Rop C, Baekelandt J. vNOTES hysterectomy for large uteri: a retrospective cohort study of 114 patients. J Minim Invasive Gynecol. 2021;28(7):1351–1356. [DOI] [PubMed] [Google Scholar]
- 13.Kaya C, Yıldız Ş, Alay İ, Aslan Ö, Aydıner İE, Yaşar L. The comparison of surgical outcomes following laparoscopic hysterectomy and vNOTES hysterectomy in obese patients. J Invest Surg. 2022;35(4):862–867. [DOI] [PubMed] [Google Scholar]
- 14.Nulens K, Kempenaers R, Baekelandt J. Hysterectomy via vaginal natural orifice transluminal endoscopic surgery in virgin patients: a first feasibility study. J Obstet Gynaecol. 2022;42(1):116–121. [DOI] [PubMed] [Google Scholar]
- 15.Nulens K, Van Genechten I, Baekelandt J. Repeat vaginal natural orifice transluminal endoscopic surgery: a first feasibility study. Gynecol Obstet Invest. 2021;86(1–2):117–122. [DOI] [PubMed] [Google Scholar]
- 16.Vanhooren E, Baekelandt J. Vaginal NOTES surgery in patients with prior hysterectomy: a first case series. Asian J Endosc Surg. 2021;14(4):811–815. [DOI] [PubMed] [Google Scholar]
- 17.Guan X, Welch JR, Wu G. Robotic transvaginal natural orifice transluminal endoscopic surgery for resection of parametrial and bowel deeply infiltrated endometriosis. J Minim Invasive Gynecol. 2022;29(3):341–342. [DOI] [PubMed] [Google Scholar]
- 18.Baekelandt JF. New retroperitoneal transvaginal natural orifice transluminal endoscopic surgery approach to sentinel node for endometrial cancer: a demonstration video. J Minim Invasive Gynecol. 2019;26(7):1231–1232. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Deng L, Tang S, et al. vNOTES hysterectomy with sentinel lymph node mapping for endometrial cancer: description of technique and perioperative outcomes. J Minim Invasive Gynecol. 2021;28(6):1254–1261. [DOI] [PubMed] [Google Scholar]
- 20.Alay I, Kaya C, Cengiz H, et al. Apical pelvic organ prolapse repair via vaginal-assisted natural orifice transluminal endoscopic surgery: initial experience from a tertiary care hospital. Asian J Endosc Surg. 2021;14(3):346–352. [DOI] [PubMed] [Google Scholar]
- 21.Levy B, Emery L. Randomized trial of suture versus electrosurgical bipolar vessel sealing in vaginal hysterectomy. Obstet Gynecol. 2003;102(1):147–151. [DOI] [PubMed] [Google Scholar]
- 22.Magos A, Bournas N, Sinha R, Richardson RE, O'Connor H. Vaginal hysterectomy for the large uterus. Br J Obstet Gynaecol. 1996;103(3):246–251. [DOI] [PubMed] [Google Scholar]
- 23.Wong WS, Lee TC, Lim CE. Novel vaginal “paper roll” uterine morcellation technique for removal of large (>500 g) uterus. J Minim Invasive Gynecol. 2010;17(3):374–378. [DOI] [PubMed] [Google Scholar]
- 24.Pelosi MA, Pelosi MA. The Pryor technique of uterine morcellation. Int J Gynaecol Obstet. 1997;58(3):299–303. [DOI] [PubMed] [Google Scholar]
- 25.Günthert AR, Christmann C, Kostov P, Mueller MD. Safe vaginal uterine morcellation following total laparoscopic hysterectomy. Am J Obstet Gynecol. 2015;212(4):546.e1-4–546.e4. [DOI] [PubMed] [Google Scholar]
- 26.Wasson M, Magtibay P, Magtibay P, Magrina J. Incidence of occult uterine malignancy following vaginal hysterectomy with morcellation. J Minim Invasive Gynecol. 2017;24(4):665–669. [DOI] [PubMed] [Google Scholar]
- 27.Kapurubandara S, Lowenstein L, Salvay H, Herijgers A, King J, Baekelandt J. Consensus on safe implementation of vaginal natural orifice transluminal endoscopic surgery (vNOTES). Eur J Obstet Gynecol Reprod Biol. 2021;263:216–222. [DOI] [PubMed] [Google Scholar]
- 28.Unger CA, Walters MD, Ridgeway B, Jelovsek JE, Barber MD, Paraiso MF. Incidence of adverse events after uterosacral colpopexy for uterovaginal and posthysterectomy vault prolapse. Am J Obstet Gynecol. 2015;212(5):.e1-7–603.e7. [DOI] [PubMed] [Google Scholar]
- 29.Houlihan S, Kim-Fine S, Birch C, Tang S, Brennand EA. Uterosacral vault suspension (USLS) at the time of hysterectomy: laparoscopic versus vaginal approach. Int Urogynecol J. 2019;30(4):611–621. [DOI] [PubMed] [Google Scholar]
- 30.Barber MD, Visco AG, Weidner AC, Amundsen CL, Bump RC. Bilateral uterosacral ligament vaginal vault suspension with site-specific endopelvic fascia defect repair for treatment of pelvic organ prolapse. Am J Obstet Gynecol. 2000;183(6):1402, discussion 1410-1411. [DOI] [PubMed] [Google Scholar]
- 31.Yurteri-Kaplan LA, Zhu X, Iglesia CB, et al. Differences in postural loading between primary and assistant surgeons during vaginal surgery. Int J Ind Ergon. 2018;65:60–67. [Google Scholar]
- 32.Catanzarite T, Tan-Kim J, Menefee SA. Ergonomics in gynecologic surgery. Curr Opin Obstet Gynecol. 2018;30(6):432–440. [DOI] [PubMed] [Google Scholar]
- 33.Baekelandt J, Kapurubandara S. Benign gynaecological procedures by vaginal natural orifice transluminal endoscopic surgery (vNOTES): complication data from a series of 1000 patients. Eur J Obstet Gynecol Reprod Biol. 2021;256:221–224. [DOI] [PubMed] [Google Scholar]
- 34.Lowenstein L, Mor O, Matanes E, et al. Robotic vaginal natural orifice transluminal endoscopic hysterectomy for benign indications. J Minim Invasive Gynecol. 2021;28(5):1101–1106. [DOI] [PubMed] [Google Scholar]
- 35.Lowenstein L, Matanes E, Weiner Z, Baekelandt J. Robotic transvaginal natural orifice transluminal endoscopic surgery for bilateral salpingo oophorectomy. Eur J Obstet Gynecol Reprod Biol X. 2020;7:100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koythong T, Thigpen B, Sunkara S, Erfani H, Delgado S, Guan X. Surgical outcomes of hysterectomy via robot-assisted versus traditional transvaginal natural orifice Transluminal Endoscopic Surgery. J Minim Invasive Gynecol. 2021;28(12):2028–2035. [DOI] [PubMed] [Google Scholar]
- 37.Lee CL, Wu KY, Su H, Han CM, Huang CY, Yen CF. Robot-assisted natural orifice transluminal endoscopic surgery for hysterectomy. Taiwan J Obstet Gynecol. 2015;54(6):761–765. [DOI] [PubMed] [Google Scholar]
- 38.Yang YS. Robotic natural orifice transluminal endoscopic surgery (NOTES) hysterectomy as a scarless and gasless surgery. Surg Endosc. 2020;34(1):492–500. [DOI] [PubMed] [Google Scholar]
- 39.Guan X, Guan Z, Koythong T, Liu J. Robot-assisted transvaginal single-site sacrocolpopexy for pelvic organ prolapse. J Minim Invasive Gynecol. 2021;28(6):1141. [DOI] [PubMed] [Google Scholar]
- 40.Guan X, Guan Z, Koythong T, Liu J, Delgado S, Wang Q. Integration of a robotic platform for sacrocolpopexy in transvaginal natural orifice transluminal endoscopic surgery: a novel surgical technique. Urology. 2021;154:109–114. [DOI] [PubMed] [Google Scholar]
- 41.Sunkara S, Guan X. Robotic vaginal natural orifice transluminal endoscopic myomectomy. Fertil Steril. 2022;118(2):414–416. [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y, Delgado S, Liu J, Guan Z, Guan X. Robot-assisted transvaginal natural orifice transluminal endoscopic surgery for management of endometriosis: a pilot study of 33 cases. J Minim Invasive Gynecol. 2021;28(12):2060–2066. [DOI] [PubMed] [Google Scholar]
- 43.Zorrón R, Filgueiras M, Maggioni LC, Pombo L, Lopes Carvalho G, Lacerda Oliveira A. NOTES. Transvaginal cholecystectomy: report of the first case. Surg Innov. 2007;14(4):279–283. [DOI] [PubMed] [Google Scholar]
- 44.Bernhardt J, Gerber B, Schober HC, Kähler G, Ludwig K. NOTES–case report of a unidirectional flexible appendectomy. Int J Colorectal Dis. 2008;23(5):547–550. [DOI] [PubMed] [Google Scholar]
- 45.Ahn KH, Song JY, Kim SH, Lee KW, Kim T. Transvaginal single-port natural orifice transluminal endoscopic surgery for benign uterine adnexal pathologies. J Minim Invasive Gynecol. 2012;19(5):631–635. [DOI] [PubMed] [Google Scholar]
- 46.Su H, Yen CF, Wu KY, Han CM, Lee CL. Hysterectomy via transvaginal natural orifice transluminal endoscopic surgery (NOTES): feasibility of an innovative approach. Taiwan J Obstet Gynecol. 2012;51(2):217–221. [DOI] [PubMed] [Google Scholar]
- 47.International NOTES Society. iNOTESs website. Available from: https://www.notesurgery.org/. Accessed: May 25, 2022.
- 48.Baekelandt JF, De Mulder PA, Le Roy I, et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: a randomised controlled trial. BJOG. 2019;126(1):105–113. [DOI] [PubMed] [Google Scholar]
- 49.Baekelandt J, De Mulder PA, Le Roy I, et al. Adnexectomy by vaginal natural orifice transluminal endoscopic surgery versus laparoscopy: results of a first randomised controlled trial (NOTABLE trial). BJOG. 2021;128(11):1782–1791. [DOI] [PubMed] [Google Scholar]
- 50.Housmans S, Noori N, Kapurubandara S, et al. Systematic review and meta-analysis on hysterectomy by vaginal natural orifice transluminal endoscopic surgery (vNOTES) compared to laparoscopic hysterectomy for benign indications. JCM. 2020;9(12):3959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Walter A,M. Vaginal hysterectomy is safe and cost-efficient, why aren’t more surgeons perfroming it? Newscope. July-Sept 2014. Available at: https://newsscope.aagl.org/printnewsscope/NewsScope_Jul-Sep_2014.pdf. Accessed: May 25, 2022.
- 52.Walter AJ. Why do we argue about route of hysterectomy? A call for dialogue. Int Urogynecol J. 2017;28(3):339–340. Epub 2016 Dec 26. [DOI] [PubMed] [Google Scholar]
- 53.Kovac SR. Decision-directed hysterectomy: a possible approach to improve medical and economic outcomes. Int J Gynaecol Obstet. 2000;71(2):159–169. [DOI] [PubMed] [Google Scholar]
- 54.Dorsey JH, Steinberg EP, Holtz PM. Clinical indications for hysterectomy route: patient characteristics or physician preference? Am J Obstet Gynecol. 1995;173(5):1452–1460. [DOI] [PubMed] [Google Scholar]
- 55.Rogo-Gupta LJ, Lewin SN, Kim JH, et al. The effect of surgeon volume on outcomes and resource use for vaginal hysterectomy. Obstet Gynecol. 2010;116(6):1341–1347. [DOI] [PubMed] [Google Scholar]
- 56.Jelovsek JE, Walters MD, Korn A, et al. Establishing cutoff scores on assessments of surgical skills to determine surgical competence. Am J Obstet Gynecol. 2010;203(1):81.e1-6–81.e6. [DOI] [PubMed] [Google Scholar]
- 57.Antosh DD, Gutman RE, Iglesia CB, Sokol AI, Park AJ. Resident opinions on vaginal hysterectomy training. Female Pelvic Med Reconstr Surg. 2011;17(6):314–317. [DOI] [PubMed] [Google Scholar]
- 58.Härkki-Siren P, Sjöberg J. Evaluation and the learning curve of the first one hundred laparoscopic hysterectomies. Acta Obstet Gynecol Scand. 1995;74(8):638–641. [DOI] [PubMed] [Google Scholar]
- 59.Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004;104(2):308–313. [DOI] [PubMed] [Google Scholar]
- 60.Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16(7):1473–1478. [DOI] [PubMed] [Google Scholar]
- 61.Bojahr B, Raatz D, Schonleber G, Abri C, Ohlinger R. Perioperative complication rate in 1706 patients after a standardized laparoscopic supracervical hysterectomy technique. J Minim Invasive Gynecol. 2006;13(3):183–189. [DOI] [PubMed] [Google Scholar]
- 62.Woelk JL, Casiano ER, Weaver AL, Gostout BS, Trabuco EC, Gebhart JB. The learning curve of robotic hysterectomy. Obstet Gynecol. 2013;121(1):87–95. [DOI] [PubMed] [Google Scholar]
- 63.Orlando MS, Greenberg CC, Pavuluri Quamme SR, Yee A, Faerber AE, King CR. Surgical coaching in obstetrics and gynecology: an evidence-based strategy to elevate surgical education and promote lifelong learning. Am J Obstet Gynecol. 2022;227(1):51–56. [DOI] [PubMed] [Google Scholar]


