Abstract
Simple Summary
Based on the latest research progresses, application of immune checkpoint inhibitors (ICIs) has shown promise in treating breast cancer. Moreover, novel ICIs based combined therapy has been sought to further enhance the curative effect. This review brings up a whole new conception of combined strategy by adding miRNA therapy into immune checkpoint blockade (ICB), based on the fact that miRNAs targeting multiple immune checkpoint molecules are believed to enhance the efficacy of ICB by mimicking combination therapy. Potential miRNAs have been summarized in this study. We also discussed the potential side-effects and solutions of applying such method. To thoroughly evaluate the role of miRNAs with multiple immune checkpoint molecules to act as a novel additive therapy for ICB in cancer treatment in future study, may further improve the clinical benefit of cancer immunotherapy.
Abstract
Breast cancer is the most common cancer type and the leading cause of cancer-associated mortality in women worldwide. In recent years, immune checkpoint inhibitors (ICIs) have made significant progress in the treatment of breast cancer, yet there are still a considerable number of patients who are unable to gain lasting and ideal clinical benefits by immunotherapy alone, which leads to the development of a combination regimen as a novel research hotspot. Furthermore, one miRNA can target several checkpoint molecules, mimicking the therapeutic effect of a combined immune checkpoint blockade (ICB), which means that the miRNA therapy has been considered to increase the efficiency of ICIs. In this review, we summarized potential miRNA therapeutics candidates which can affect multiple targets of immune checkpoints in breast cancer with more therapeutic potential, and the obstacles to applying miRNA therapeutically through the analyses of the resources available from a drug target perspective. We also included the content of “too many targets for miRNA effect” (TMTME), combined with applying TargetScan database, to discuss adverse events. This review aims to ignite enthusiasm to explore the application of miRNAs with multiple targets of immune checkpoint molecules, in combination with ICIs for treating breast cancer.
Keywords: microRNA, multiple immune checkpoints blockade, sensitizer, breast cancer, TMTME
1. Introduction
Breast cancer, as one of the most common malignant tumors in women, also accounts for a huge part of cancer-associated deaths world widely. It undoubtedly has become the top killer, severely threatening women’s health [1]. As reported by the International Agency for Research on Cancer (IARC), the disease has already surpassed lung cancer as the leading cause incidence, which made breast cancer the top cancer in 2020 [2]. Moreover, triple-negative breast cancer (TNBC), as a special subtype, can bring even worse prognosis, mortality, and a higher relapse for patients [3]. Therefore, a massive effort has been made for improving the outcome of breast cancer treatment globally. In recent years, as one of the most significant advances, the application of immune checkpoint inhibitors (ICIs) has been considered to possess a promising potential in breast cancer treatment (including TNBC) [4,5]. However, although many immune checkpoint inhibitors (ICIs) have manifested compelling clinical effectiveness for breast cancer, the stable and ideal clinical benefits were still hard to gain (such as the results from the IMpassion050 Trial) [6,7,8], which makes it a global research hotspot how to refine the combination of ICIs to enhance the therapeutic effect.
Interestingly, targeting multiple immune checkpoints has been demonstrated to be a more effective approach to activate anti-tumor immune responses than single immune checkpoint-specific monotherapy [4], which makes the combinations, such as CTLA-4 (cytotoxic T lymphocyte-associated protein-4) blocker plus PD-1/PD-L1 (programmed cell death protein-1/programmed death-ligand 1) blocker, a very promising anti-cancer therapeutic strategy, including against breast cancer [4,9]. Based on that, agents which may further improve the therapeutic effect of multiple immune checkpoints blockade are being explored [9]. For instance, T-DM1 (ado-trastuzumab emtansine) has been found to enhance the curative effect of CTLA-4/PD-1 blockades for breast cancer [9]. Moreover, the approval of cadonilimab has officially opened up a new era for multiple immune checkpoint inhibitors’ application in solid cancers, which also brings a greater opportunity for treating breast cancer [10].
MiRNAs (MicroRNAs) are a class of non-coding RNAs that plays an important role in the post-transcriptionally controlling the expression of messenger RNA (mRNA) translating into protein [11]. One single miRNA has been found to regulate nearly a hundred mRNAs (messenger RNAs); therefore, robust biological responses can be created by simultaneous stimulation on multiple gene networks [11,12,13]. Extracellular miRNAs have also been found to mediate cell–cell communication as chemical messengers [14]. MicroRNA (miRNA)-based therapeutics can be divided into miRNA mimics and inhibitors of miRNAs (antimiRs) [15]. The miRNA mimics are synthetic small RNA molecules which can target and combine the corresponding miRNA sequence for replenishing the lost miRNA expression in certain diseases [15]; meanwhile, miRNA inhibitors have been applied to block the expression of certain oncogenic microRNAs [16]. This miRNA-based therapy has been considered as a potential candidate for cancer treatment, since abnormal expressions of certain genes were found to have inevitable connection with tumorigenesis and cancer development [12,13,15].
Notably, a single miRNA has been shown to target multiple checkpoint molecules, mimicking the therapeutic effect of a combined immune checkpoint blockade (ICB) [17]. As a result, microRNA therapy combined with ICB can potentially increase the efficacy of the established mono-therapeutic approach [18]. In actuality, not only is the ORR (objective response rate) induced by ICIs highly restricted, but the number and severity of adverse effects caused by combinations of immune checkpoint inhibitors are frustrating. Consequently, it is of the utmost importance to investigate novel ways to improve the situation. MiRNAs, particularly those that can target multiple immune checkpoints simultaneously, simulating a multi-checkpoint blockade, have been deemed suitable for enhancing the efficacy of immune checkpoint inhibitors. This strategy is believed to positively modulate the immune response to the treatment and convert non-responders into responders [18]. Even though such a combination approach has not yet reached the stage of clinical trials, there is growing preclinical evidence of potential synergistic interactions between immune checkpoint blockade and microRNAs [19,20] For example, PD-L1 and CD80 expression negatively correlated with miR-424 in ovarian cancer cells. Mimetics of miR-424 are believed to increase the therapeutic efficacy of immunotherapy [21]. In the context of ICB, MiR-138, which can regulate the expression of PD-1 and CTLA-4 in gliomas, has also been deemed to possess a significant therapeutic potential [22]. The intertwined signal networks between miRNAs and immune checkpoint molecules are robust and intricate, resulting in numerous inevitable and formidable obstacles to applying such synergy [23]. Therefore, we are here to summarize potential miRNAs, which can target multiple immune checkpoints to ignite the enthusiasm of exploring the possibilities of such miRNAs combined with ICIs in breast cancer treatment. We also summarized the potential side effects of such synergism and possible solutions to preliminarily construct an overall prospect for such a novel therapeutic strategy in breast cancer treatment.
2. Method
The TargetScan database (https://www.targetscan.org/vert_80/, accessed on 29 November 2022) (TargetScan Release 8.0) was applied to predict the potential targets of selected miRNAs.
3. Results
As displayed by the analyses performed using the TargetScan platform, the number of predicted targets of selected miRNAs ranges from 59 to 7852. For details, miR-149-3p has been found to possess 7852 transcripts with binding sites, containing a total of 17186 sites. The miR-195/miR-497 has 1515 transcripts with conserved sites, including 1769 conserved sites and 687 poorly conserved sites. The miR-93 has 1385 transcripts with conserved sites, containing a total of 1647 conserved sites and 914 poorly conserved sites. As for miR-5119, the number of transcripts with sites binding is 2537, containing a total of 3078 binding sites. The number of transcripts with conserved sites of miR-340 are 1393, containing a total of 1624 conserved sites and 1722 poorly conserved sites. The miR-21 possesses 384 transcripts with conserved sites, including 414 conserved sites and 138 poorly conserved sites. For miR-138, 704 transcripts with conserved sites were predicted (including 787 conserved sites and 306 poorly conserved sites). The miR-100 has been predicted to have 59 transcripts with conserved sites, containing 60 conserved sites and 2 poorly conserved sites, and the predicted counterparts for miR-200a are 905, 1027, and 566, respectively. The miR-4443 has been predicted to possess 4481 transcripts with binding sites, containing a total of 6052 sites (Table 1).
Table 1.
Studies of selected miRNAs targeting multiple immune checkpoints and the total number of potential targets of selected miRNAs.
| MiRNA | Targeted Immune Checkpoints |
Tumor Type | Experimental Setting | Functional Mechanisms | References | Number of Predicted Targets | Conserved Sites and Poorly Conserved Sites |
|---|---|---|---|---|---|---|---|
| MiR-93-5p | B7-H6, PD-L1, PD-L2 |
Breast cancer, lung cancer, colorectal cancer | Database, in vitro, human sample |
Reducing the expression of PD-1, PD-L1, PD-L2, and B7-H6 | [24,25,26] | 1385 | 2561 |
| MiR-149-3p | PD-1, TIM-3, BTLA |
Breast cancer | In vitro | Downregulating mRNAs for PD-1, TIM-3, and BTLA | [27] | 7852 | 17186 |
| MiR-195/MiR-497 | PD-L1, B7-H6 |
Breast cancer, diffuse large B cell lymphoma | Database, in vitro |
Reducing the expression of PD-L1, PD-L2, and B7-H6 | [25,28] | 1515 | 2456 |
| MiR-5119 | PD-L1, IDO2 |
Breast cancer | In vivo, in vitro |
Downregulating the expression of PD-L1 and IDO2 | [29] | 3078 | 2537 |
| MiR-138-5p | PD-L1, PD-1, CTLA-4 |
Breast cancer, oral squamous cell carcinoma | In vitro | Direct anti-tumoral effects and immunostimulatory effects by targeting PD-1 and CTLA-4 | [30,31] | 704 | 1093 |
| MiR-100-5p | PD-L1, PD-1 PD-L2 |
Breast cancer, bladder cancer | Database, human sample |
Downregulating the expression of PD-1, PD-L1, and PD-L2 | [32,33] | 59 | 62 |
| MiR-200a | PD-L1, PD-1 |
Breast cancer, gastrointestinal cancer | Database, in vitro |
Targeting PD-L1, PD-1, and CD86 | [33,34] | 905 | 1593 |
| MiR-21-5p | PD-L1, PD-1, CTLA-4,LAG3 |
Breast cancer, head and neck squamous cell carcinoma | Database, in vitro |
Upregulating PD-L1, PD-1, CTLA-4, and LAG3 | [33,35] | 384 | 552 |
| MiR-4443 | TIGIT, CTLA-4 |
Lung cancer | In vivo, In vitro, database |
Targeting TIGIT and CTLA-4 | [36,37] | 4481 | 6052 |
4. Discussion
4.1. Existing and Potential Immune Checkpoints in Breast Cancer
In recent years, a great progression has been witnessed in the application of ICIs in cancer treatment, including against breast cancer [38]. For instance, it has been presented by the IMpassion130 study that the therapeutic strategy of atezolizumab (a PD-1/PD-L1 inhibitor) plus albumin paclitaxel as the first-line therapy has improved the overall survival (OS) by 7.5 months and reduced the risk of death by 33%, compared with the placebo plus albumin paclitaxel group, for advanced TNBC patients with PD-L1 positive, marking the beginning of the immunotherapy for breast cancer [39]. Consequently, selecting proper immune checkpoint as an effective therapeutic target is a fundamental and crucial aspect of immunotherapy. We now have presented some potential candidates which may act as therapeutic targets in multiple immune checkpoint targeted miRNA therapy (Table 2 and Figure 1).
Table 2.
Application of selected immune checkpoint blockade therapy in cancer treatment.
| Ligand | Expression Location | Roles in Tumor Immunity | Potential Mechanisms |
Approved Drugs or Candidates | Reference | ||
|---|---|---|---|---|---|---|---|
| Targeting Receptors |
Targeting Ligands |
||||||
| PD-1 | PD-L1/PD-L2 | Lymphocytes including T, B, and NK/NKT cells | Suppressing T cell activation and proliferation in late phase; inducing T cell apoptosis. | Phosphorylated PD-1-ITIM/SHP2/SAP signaling; TCR signaling inhibition | Pembrolizumab (approved); pucotenlimab (approved); RAPA-201 (phase I/II); nivolumab+ ipilimumab (phase II); ATRC-101-A01 +pembrolizumab (phase I) |
Atezolizumab (Approved); Durvalumab (Approved); ATRC-101-A01 + Pembrolizumab (Phase I); DKY709 + PDR001 (Phase I) |
[40,41,42,43] |
| CTLA-4 | CD80/CD86 | Activated T cells | Inhibiting T cell activation in early phase | Phosphorylated CTLA4-YVKM/SHP2/RAS signaling; TGF-β/IDO inducing | Ipilimumab (approved); tremelimumab (approved); RAPA-201 (phase I/II); Nivolumab+ Ipilimumab (phase II) |
NA | [44,45,46] |
| TIM-3 | Galactin-9, CEACAM-1, HMGB1, PS | Tumor-infiltrating T cells, Tregs, DCs, monocytes, NK cells | Exhausting tumor-infiltrated T cells | Glycosylated TIM3/AKT/mTOR signaling; phosphorylated TIM3/NFAT/Bat signaling | Sabatolimab (phase III); MAS825 (phase III) RAPA-201 (phase I/II) |
NA | [47,48] |
| LAG-3 | MHC-II, galectin-3, LSECtin | Activated T cells, B, NK cells, DCs | Preventing CD4-MHC-II interaction; inhibiting CD4-dependent T cell function | Phosphorylated LAG-3-KIEELE/mediated reduction in calcium influx impairs TCR signaling | Relatlimab (approved); RAPA-201 (phase I/II) |
NA | [46,49] |
| BTLA | HVEM | T, B, NK cells, macrophages, DCs | Holding back T cell over-activation | Phosphorylated BTLA-ITIM/ITSM/SHP2; inhibiting both TCR and CD28 signaling | Icatolimab (phase II) |
NA | [50,51,52] |
| IDO1/2 | AhR | Tumor cells, stromal cells, and immune cells in TME | Inhibiting the function of effector T cell and promoting Tregs; inducing T cell apoptosis | Catalyzing the oxidative cleavage of tryptophan; producing metabolite kynurenic acid | Epacadostat (phase II); epacadostat and pembrolizumab (phase I/II) |
NA | [53,54,55] |
| TIGIT | CD155, CD112, CD113 | T cells, Tregs, NKT cells | Inhibiting NK/CD8+ T cell-mediated tumor killing; affecting CD8+ T cell priming and differentiation; inducing immunosuppressive DCs | TIGIT/PVR/IL-10 and TGF-β signaling; TIGIT/CD155 ERK signaling | Tiragolumab (phase III); vibostolimab (phase III); ociperlimab (phase III) |
NA | [56,57] |
| B7-H6 | NKp30 | Tumor cells | Regulating the T cell-mediated immune response | Helping NK cells to recognize abnormal cells | NA | NA | [58] |
Abbreviation—NA, not available.
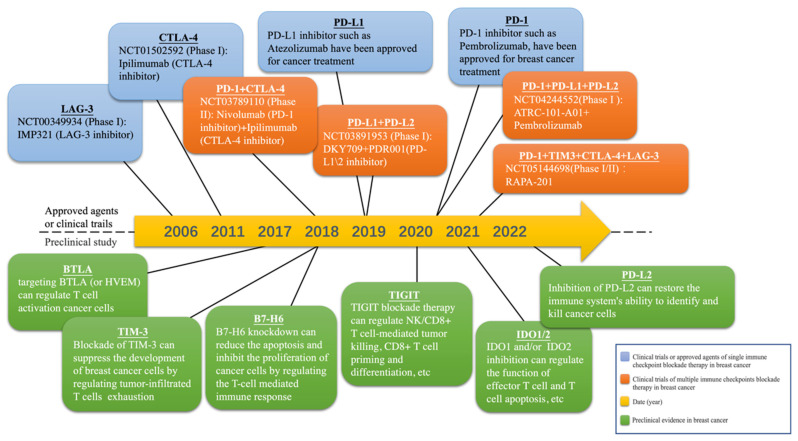
Figure 1.
Milestones of selected immune checkpoint blockade therapy utilized in treating breast cancer. Currently, four clinical trials are testing different multiple immune checkpoint blockade therapy in breast cancer. The therapeutic value of seven novel immune checkpoint suppression methods in breast cancer treatment has been reported by preclinical studies.
4.1.1. PD-1/PD-L1
PD-1, or differentiated cluster 279 (CD279), is an important immunosuppressive molecule. As a cell surface receptor and a member of the CD28 family, this molecule is expressed in lymphocytes, such as T cells, B cells, natural killer (NK) cells, and myeloid cells [59]. PD-L1 (CD274), a ligand for PD-1, is a type 1 transmembrane protein. PD-L1 can be glycosylated by N-linked glycoproteins in the endoplasmic reticulum and Golgi apparatus, and then transported to the cell membrane as a ligand for PD-1. There is evidence that PD-L1 is highly expressed in some breast cancers, and the positive rate of PD-L1 in triple-negative breast cancer can reach 20% [60,61]. In addition, it has been discovered that the binding of PD-L1 to PD-1 inhibits T cell proliferation and activation, resulting in immunosuppression. Based on this fact, inhibitors of PD-1 or PD-L1have then been developed for cancer treatment (including breast cancer), by restoring anti-cancer immunology [43]. These PD-1/PD-L1 inhibitors, such as atezolizumab and pembrolizumab, have already been approved for application in breast cancer treatment [43]. However, the therapeutic effect of PD-1/PD-L1 inhibitor monotherapy for breast cancer is limited, resulting in more attention on the multiple immune checkpoint blockade therapeutic strategy [62,63]. For instance, a phase I/II study (NCT05187338) is currently testing the triplex CTLA4/PD1/PDL1 inhibitors combination therapy for advanced solid tumors (including breast cancer).
4.1.2. CTLA-4
CTLA-4, known as CD152, is a leukocyte differentiation antigen. Such a protein is a transmembrane receptor on T cells that shares the B7 ligand with CD28, which participate in the negative regulation of immune response [64]. Furthermore, CTLA-4 has been proven to act as an efficient therapeutic target in cancer treatment. For instance, ipilimumab was the first CTLA-4 inhibitor for treating metastatic melanoma approved by U.S. Food and Drug Administration (FDA) in 2011 [65]. Its application has now been expanded to renal cell carcinoma, hepatocellular carcinoma, and colorectal cancer [66,67,68]. Moreover, research has further shown that preoperative cryoablation and single-dose ipilimumab are safe for use in monotherapy or in combination while treating early-stage breast cancer [69]. Another CTLA-4 inhibitor, tremelimumab, has also displayed therapeutic potential for treating breast cancer according to recent clinical evidence [70]. An ongoing phase II study is also evaluating the combination therapy of nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4) in patients with breast cancer (NCT03789110).
4.1.3. TIM-3
T cell immunoglobulin and mucin domain 3 (TIM-3) (or CD366), also named as hepatitis A virus cellular receptor 2 (HAVCR2), is also a transmembrane protein. Ligands of TIM3 include galactin-9 (Gal-9), carcinoembryonic antigen cell adhesion molecule-1 (CEACAM-1), high mobility group protein B1 (HMGB1), and phosphatidylserine (PS) [71]. The TIM-3/Gal-9 axis has been found to modulate tumor immunity by negatively regulating T cell immunity [71]. Evidence showed that the blockade of TIM-3 can inhibit the proliferation, migration, and invasion of breast cancer cells, indicating that TIM-3 is an effective therapeutic target [72]. Several TIM-3 inhibitors, as novel ICIs, including sabatolimab and cobolimab, have been evaluating by certain ongoing clinical trials [73,74]. Moreover, RAPA-201 therapy, which has been thought to block the expression of PD-1, CTLA-4, TIM-3, and LAG3, thereby improving the immune suppressive tumor microenvironment, is currently being trialed in a phase I/II study for patients with solid cancer (including breast cancer) (NCT05144698). However, the clinical application of TIM-3 inhibitor in breast cancer treatment still requires more supportive evidence.
4.1.4. LAG-3
Lymphocyte-activation gene 3 (LAG-3) is a type I transmembrane protein which mainly expressed in activated T cells, NK cells, B cells, and plasma cell dendritic cells [75]. Such an immune checkpoint has been found to regulate the activity of T cells by binding to the major histocompatibility complex II (MHC-II) and other ligands [76]. Evidence showed that the low expression of LAG-3 was substantially linked to longer relapse-free and overall survival times, making relatlimab, which acts as a LAG3 inhibitor, a promising anti-cancer agent [77]. For details, in 2022, the U.S. FDA approved the combination therapy of relatlimab and nivolumab for adults and children 12 years of age and older with unresectable or metastatic melanoma, setting the milestone for the application of LAG-3 inhibitors, as a novel ICI, in cancer treatment [78]. Currently, more LAG-3 immune checkpoint inhibitors (including tebotelimab, relatlimab, IMP321, etc.) have been trialed and presented strong efficacy against solid tumors including melanoma, breast cancer, NSCLC, and gastric cancer [79,80,81,82,83]. Such an agent has also displayed a good anti-tumor synergistic effect for PD-1/PD-L1 inhibitor in clinical trials [79,80,81,82,83].
4.1.5. BTLA
BTLA (B and T lymphocyte attenuator, CD272) belongs to the CD28 family and is an important immune checkpoint molecule which is expressed in activated T and B lymphocytes [84]. Herpesvirus entry mediator (HVEM), which is widely expressed in various cell types (including in breast cancer) and participates in immune homeostasis, is the ligand of BTLA [85,86]. Evidence has also indicated that targeting BTLA (or HVEM) is a very promising novel immunotherapy for breast cancer treatment [85,86]. As a potential therapeutic target for cancer immunotherapy, BTLA is similar to PD-1 and CTLA-4, but possesses different functions [87]. Icatolimab (TAB004/JS004), as the first BTLA monoclonal antibody, is currently being tested in different clinical trials for cancer treatment (such as studies NCT04278859, NCT04137900, and NCT04477772) [88]. So far, icatolimab monotherapy, or in combination with triprilimab, was well tolerated and showed initial clinical efficacy in the treatment of relapsed/refractory lymphoma, [89].
4.1.6. IDO1, 2
Indoleamine-2,3-dioxygenase (IDO)1 and IDO2 are two catabolizing enzymes which are closely related to tryptophan; they are induced under inflammatory conditions and have been found to regulate immune responses. The IDO1 is widely expressed in both immune and non-immune tissues, while IDO2 is restrictively expressed in liver, kidney, and antigen-presenting cells (dendritic cells and B cells). They have been discovered to catalyze the metabolism of tryptophan through the canine urine pathway, along with the unrelated enzyme tryptophan dioxygenase (TDO) [90]. Moreover, IDO1 and IDO2 have been considered to possess different abilities in anti-cancer immunity regulation [91]. Additionally, IDO1 and IDO2 are upregulated in many tumors, including breast cancer, and the overexpression of IDO1 has been found to be associated with poor prognosis [92]. As reported by a phase I/II trial (NCT02178722), a novel combined therapy of epacadostat (IDO1 inhibitor) and pembrolizumab (PD-1 inhibitor) was well tolerated and showed antitumor activity in patients with triple-negative breast cancer [55]. Consequently, in 2017, IDO1 inhibitor was then praised as the next hot research spot for cancer immunotherapy by the American Society of Clinical Oncology [93]. Furthermore, recent evidence from a wet-lab has further shown that the IDO1/2 dual-target inhibitor 4t has a superior antitumor efficacy compared to epacadostat [94], indicating that such a therapeutic strategy is worthy of further research and development investment.
4.1.7. TIGIT
TIGIT (T cell immunoglobulin and ITIM domain), also named as WUCAM, Vstm3, and VSIG9, has been reported to possess the ability of suppressing both T cell-driven inflammation and T cell and NK cell-dependent anti-tumor immunity, as a coinhibitory receptor and a novel immune checkpoint [95,96]. Its expression can be upregulated by activated T cells, natural killer cells, and regulatory T cells. In addition, TIGIT has been found to bind three ligands, namely CD155 (PVR), CD112 (PVRL2, nectin-2), and CD113 (PVRL3), which are expressed by tumor cells, antigen-presenting cells, and also T-lymphocytes in the tumor microenvironment [95,96,97]. Furthermore, TIGIT has been found to affect innate and adaptive immunity through a variety of mechanisms. For instance, the binding of TIGIT and CD155 can cause the CD155-expressing dendritic cells to be tolerogenic and reduce the production of cytokines IL-12 and IL-10; additionally, TIGIT can also inhibit the degranulation of NK cells, the production of cytokine, and NK cell-mediated tumor cytotoxicity [98]. Based on those findings, TIGIT monoclonal antibodies (such as tiragolumab, vibostolimab, ociperlimab) and multiple immune checkpoint blockade therapies (including PD-1/TIGIT, and PD-1/TIGIT/LAG-3), have all been developed for cancer treatment, and some are currently in ongoing clinical trials [56,57,99,100,101,102]. In particular, high-frequency PD-1−TIGIT + CD8+ tumor-infiltrating lymphocytes (TILs) were observed in TNBC cells, making the strategy of dual PD-1/TIGIT blockade a promising therapeutic approach via increasing CD8+ TIL function in TNBC, which may further improve the immunotherapy for breast cancer [103].
4.1.8. PD-L2
Programmed cell death ligand-2 (PD-L2) (known as CD273), is a member of the B7 family, and is another important ligand of PD-1 and, therefore, to affect the function of immune cells [104]. Furthermore, PD-L2 can competitively bind to PD-1 with a stronger affinity than PD-L1 to PD-1, thereby inhibiting the immune activation of T cells through downstream signal pathways which are related to tyrosine phosphatase 2 (SHP-2), lymphocyte-specific protein tyrosine kinase (LcK), phosphatidylinositol 3 (PI3K), and mitogen-activated protein kinase (MAPK) [105]. Additionally, PD-L2 has also been considered as a promising biomarker for risk assessment in patients with TNBC [105]. Moreover, agents which can selectively block dual targets, namely PD-L1 and PD-L2, have been intended to be developed for the treatment of a variety of advanced solid tumors, based on the fact that inhibition of PD-L2 can restore the ability of the immune system to recognize and kill cancer cells [106,107]. For instance, the combination therapy of DKY709 and PDR001 (a humanized IgG4 monoclonal antibody directed against PD-1 that blocks the binding of PD-L1 and PD-L2) is being tested in patients with triple-negative breast cancer in an ongoing phase I trial (NCT03891953). The combination therapy of ATRC-101-A01 and pembrolizumab is also being trialed in patients with breast cancer in a phase I study (NCT04244552).
4.1.9. B7-H6
Natural killer cell cytotoxicity receptor 3 ligand 1 (NCR3LG1, also known as B7-H6) is a member of the B7 family which can regulate the T cell-mediated immune response [58]. It has been reported that, in TNBC cells (MDA-MB-231), B7-H6 knockdown can induce apoptosis and inhibit the proliferation of cancer cells, leading to the suppression of tumor development by regulating the T cell-mediated immune response, which indicated that B7-H6 possesses the potential to play a significant role in the treatment of TNBC [108].
4.2. Selected MicroRNA Targeted Multiple Immune Checkpoints in Breast Cancer
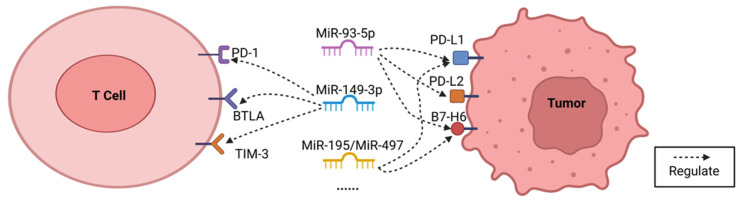
Based on the existing evidence, miRNAs which may regulate more than one immune checkpoint in breast cancer cells have been selected for potential immunotherapy application, as shown below (Table 1 and Figure 2).
Figure 2.
Selected miRNAs which can regulate multiple immune checkpoints, such as miR-93-5p, which can potentially affect the expression of PD-L1, PD-L2, and B7-H6; miR-149-3p, which can regulate the expression of PD-1, TIM-3, and BTLA. Furthermore, the expression of PD-L1 and B7-H6 can be modulated by miR-195/miR-497.
4.2.1. MiR-93-5p
MiR-93-5p is a small noncoding RNA which acts as a gene regulator in numerous cancers [26]. It has been reported that overexpressed miR-93-5p can reduce the expression of PD-L1 and suppress the growth of MDA-MB-231 cells [26]. Moreover, miR-93-5p has also been shown to potentially regulate the immune evasion of breast cancer cells by targeting PD-L1, PD-L2, and B7-H6, based on a data analysis [25]. In colorectal cancer cells, miR-93-5p has been proven to downregulate the expression of PD-L1 by binding to the 3′-UTR region of PD-L1, and also to decrease the migration, invasion, and the immune evasion of cancer cells [24]. Therefore, miR-93-5p, as a circulating miRNA with multiple targets of immune checkpoints (including PD-L1, PD-L2, and B7-H6), has been considered to possess the potential in breast cancer immunotherapy, by a possible mechanism of reducing the expression of PD-L1, PD-L2, and B7-H6. However, additional research is still required for its application in cancer immunotherapy (Figure 2).
4.2.2. MiR-149-3p
As a cancer suppressor gene the overexpression of miR-149-3p, has also been reported to decrease proliferation, migration, and invasion, and to trigger apoptosis in cells in different cancers (including breast cancer) [109]. Moreover, evidence has displayed that miR-149-3p can regulate the expression of PD-1, TIM-3, and BTLA by binding to the 3′UTRs of their mRNAs, thereby preventing tumor immune escape [27]. In addition, overexpressed miR-149-3p has been found to decrease T cell apoptosis and to weaken the miRNA markers of T cell exhaustion, which increased CD8+ T cells’ ability to destroy 4T1 breast cancer cells [27]. Thus, miR-149-3p may also be applied in breast cancer immunotherapy via regulating the expression of PD-1, TIM-3, and BTLA (Figure 2).
4.2.3. MiR-195/MiR-497
As reported in previous studies, the expression of miR-195/miR-497 differs in normal and breast cancer tissues, making miR-195/miR-497 a potential biomarker for breast cancer treatment [110,111]. Further bioinformatic analysis indicated that miR-195/miR-497 can potentially regulate the immune evasion of breast cancer cells by targeting PD-L1 and B7-H6 [25]. For instance, miR-195/miR-497 mimicking transfection has been found to dramatically decrease the mRNA (messenger RNA) and protein expression of PD-L1 in MDA-MB-231 cells [25]. Additionally, the transfection of miR-195 has also been reported to downregulate the mRNA and protein expression of PD-L1, therefore reducing the proliferation and migration of OCI-Ly10 cells (diffuse large B cell lymphoma), and also preventing OCI-Ly10 cells from immune escape while raising apoptotic ratio in those cells [28]. Additionally, it has also been demonstrated that miR-195/miR-497 may target PD-L1 and B7-H6 after analyzing the transcriptome profiling (microRNA expression quantification) data from the TCGA database [25]. Thus, miR-195/miR-497 has been recommended as a potential candidate for multiple immune checkpoint blockade therapy in breast cancer by regulating the expression of PD-L1 and B7-H6. However, more research investment is still required for revealing its potential mechanisms and functions (Figure 2).
4.2.4. MiR-5119
MiR-5119 has been reported to act as a regulator for anti-tumor immunity in breast cancer [29]. It has been found that engineering DCs (dendritic cells) and miR-5119, when employed as a novel combined therapeutic strategy, can simultaneously suppress multiple negative regulatory molecules, including IR (inhibitory receptor) ligands, such as PD-L1 and IDO2, in DCs, thereby improving anti-tumor immune response, upregulating cytokine production, and reducing the apoptosis of T cells in breast cancer cells [29]. Furthermore, MiR-5119 can also act as a potential regulator of PD-L1 in immune tolerance of tissue transplants [112]. Briefly, miR-5119 may target specific sequences in the 3′ UTRs of PD-L1 and IDO2 genes, therefore, suppressing the synthesis of both proteins [29]. As shown in a dual-luciferase reporter assay, miR-5119 mimic can reduce luciferase activity compared to the control miRNA, indicating that miR-5119 can directly bind and influence the expression of the PD-L1 gene [29]. Hence, miR-5119 has also been considered as a promising sensitizer for ICIs-based immunotherapy, even though further research work should be performed before its clinical application.
4.2.5. MiR-138-5p
As a tumor suppressor miRNA, miR-138-5p has already been reported to suppress the metastasis, proliferation, and epithelial–mesenchymal transmission in different types of cancer cells [113,114]. Recently, many researches have also indicated that miR-138-5p can regulate the expression of certain immune checkpoints [115]. For instance, in breast cancer MDA-MB-231 cells, it has been reported that PD-L1 expression can be reduced by miRNA-138-5p transfection, and then the suppressed PD-L1 expression can further restrain the exhaustion of T cells, which inhibits proliferation, cloning, and migration of cancer cells [31]. Evidence has also found that miR-138-5p can exert multiple anti-tumor effects and immunostimulatory effects by targeting PD-1 and CTLA-4 in oral squamous cell carcinoma [30]. However, a similar function of miR-138-5p has not yet been confirmed in breast cancer.
4.2.6. MiR-100-5p
MiR-100-5p is a member of the miR-100 family and is aberrantly expressed in different cancers [116,117]. Similar to miR-138-5p, miR-100-5p has also been proven to be a tumor suppressor by regulating cell death, the cell cycle, cell differentiation, proliferation, invasion, and migration of cancer cells [116]. For breast cancer, it has also been found that miR-100-5p transfection can promote cell death while impairing cell proliferation, migration, and invasion [116]. Furthermore, recent evidence has preliminarily revealed that the targets of miR-100-5p are possibly enriched in PD-1 and PD-L1 pathways, indicating the potential regulatory functions of miR-100-5p on PD-1 and PD-L1 [33]. Moreover, the expression of miR-100-5p has been reported to be negatively correlated with the expressions of PD-L1 and PD-L2 in bladder cancer, indicating a potential regulatory loop involving miR-100-5p, PD-L1, and PD-L2 [32]. Hence, miR-100-5p may also possess the potential to regulate the expression of PD-1, PD-L1, and PD-L2 in breast cancer.
4.2.7. MiR-200a
MiR-200a is a member of miR-200 family and is abnormally overexpressed in breast cancer tissues [33]. Stomach cancer patients who have a higher expression level of miR-200a have a better prognosis compared to those who have lower expression level of miR-200a, indicating its important role in prognostic prediction [34]. Furthermore, miR-200a has also been found to be negatively associated with CD86 in gastrointestinal cancer as a potential therapeutic targets [34]. As for breast cancer, the excellent diagnostic and therapeutic performance held by the microRNA has also been reported [118,119]. Moreover, as for breast cancer, recent evidence has preliminarily displayed that the genes potentially targeted by miR-200a are enriched in the PD-1 and PD-L1 pathways, indicating the potential ability of miR-200a to regulate those immune checkpoints [33].
4.2.8. MiR-21-5p
As the most common and strongly upregulated miRNA in glioblastoma, miR-21-5p has also been found to be abnormally overexpressed in different cancers including breast cancer [120]. Evidence has showed that suppression of miR-21-5p expression can reduce the migration, proliferation, and invasion of breast cancer cells [121]. In addition, potential pathways of miR-21-5p were predicted to mainly focus on PD-L1 and PD-1 immune checkpoints in breast cancer [33]. Moreover, transfection of miR-21-5p has also been reported to significantly elevate the expression levels of CTLA-4 and LAG3 miRNA in head and neck squamous cell carcinoma [35]. Therefore, the potential ability of miR-21-5p to target multiple immune checkpoints has been preliminarily displayed, and awaits further exploration.
4.2.9. MiR-4443
In lung cancer patients, miR-4443 has been shown to potentially affect the expression of CTLA-4 and TIGIT, and the overall survival of patients by regulating the ZC3H12D-hsa-miR-4443-ENST00000630242 axis [36]. Therefore, miR-4443 was chosen as a potential candidate. However, its effects on breast cancer require further investigation.
4.3. Oncogenice or Tumor Suppressor Roles of Selected MicroRNAs
The miRNAs involved in cancer have been classified as two groups, one of which is the onco-miRNAs (oncoMiRs) which have been found to induce tumorigenesis and tumor progression, and these genes are abnormally and highly expressed in cancer cells. The other group is onco-suppressor miRNAs. This group of genes is frequently downregulated in cancer cells and can inhibit the cancer-related phenotype of cells [122]. Therefore, immune checkpoint targeting miRNAs which have already been classified may provide a more specific and clearer perspective in their application in cancer treatment.
For instance, overexpression of miR-93-5p has been found to diminish PD-L1 expression and inhibit MDA-MB-231 cell proliferation [26]. Furthermore, miR-93-5p can also control breast cancer cell migration by inhibiting the epithelial–mesenchymal transition (EMT) of the cells [123]. Thus, miR-93-5p is a promising onco-suppressor miRNA for the treatment of breast cancer.
Evidence also reported that overexpression of miR-149-3p can reduce proliferation, migration, and invasion, and can induce death in cancer cells (including breast cancer), indicating the potential of miR-149-3p as an onco-suppressor miRNA in breast cancer [109].
As for miR-100-5p, overexpression of such an onco-suppressor miRNA has been found to promote cell death and reduce proliferation, migration, and invasion of breast cancer cells [116]. Furthermore, it has been proved that miR-100-5p can suppress the migration and invasion of MDA-MB-231 breast cancer cells by targeting FZD-8 and inhibiting the Wnt/beta-catenin pathway [124]. As we presented above, miR-100-5p possesses the potential to regulate the expression of PD-1 and PD-L1, thus, exerting anti-tumor effects [33]. Therefore, miR-100-5p may hold multiple anti-cancer effects in breast cancer treatment.
In addition, the miR-200 family has been reported to regulate the transition between breast cancer-stem-cell-like and non-stem-cell-like phenotypes, and also modulate cellular plasticity and tumor suppression in breast cancer [125]. Furthermore, evidence has also shown that the expression of the miR-200b/200a/429 cluster can significantly inhibit the proliferation in the murine claudin-low mammary tumor cell line [126]. Furthermore, in breast cancer cells, miR-200a/b has been proven to inhibit the epithelial–mesenchymal transition and tumor metastasis via association with p73 as a tumor suppressor [127]. More specifically, evidence has shown that miR-200a can exert the anti-cancer effect on triple-negative breast cancer cells by direct repression of the EPHA2 oncogene [128]. As mentioned above, miR-200a can also potentially regulate the expression of PD-1 and PD-L1 and, therefore, enhances the therapeutic effect of an immune checkpoint blockade [33]. Thus, miR-200a may exert multiple anti-cancer effects as a potential sensitizer for ICIs in breast cancer treatment.
Evidence also found that knockdown of miR-21-5p can reduce the cell growth and increase the apoptosis level of MCF-7 cells [121,129]. However, the potential pathways of miR-21-5p have been predicted to mainly focus on PD-L1 and PD-1 immune checkpoints [121]. Therefore, miR-21, as a oncoMiR, may also become an effective anti-tumor immunity regulator with extra effects in regulating cancer development.
As for the other IC-targeting miRNAs mentioned above, such as miR-195/miR-497, miR-5119, miR-138-5p, and miR-4443, their roles of being oncoMiRs or onco-suppressor miRNAs in breast cancer are still not yet confirmed [25,29,31,36]. Therefore, more research exploration is recommended in this field.
4.4. Side Effect and Solutions
One of the main limitations of the ICI therapy is the appearance of immune-related adverse events (irAEs), which often leads to the interruption of the treatment. These irAEs are related side effects caused by the intervention of checkpoint inhibitors which can stimulate the immune system to raise up a series of intense immunoreactions not just against cancer cells, but also self normal tissues. For example, PD-1 inhibitors can cause pneumonitis, arthralgia, and hypothyroidism. Colitis, hypophysitis and rash were common in patients treated with CTLA4 inhibitors [130]. The incidence of irAEs can further increase if two immune checkpoint inhibitors are combined [18,131]. For instance, evidence has shown that CTLA4 inhibitors combined with PD-1 or PD-L1 agents can bring about higher incidence and severity of irAEs, such as the combination of ipilimumab and nivolumab, irrespective of the primary cancer treated [132,133,134]. Furthermore, immune-related adverse events could also be triggered by miRNA-based therapeutics [135,136,137]. That was the main reason why only 10 obtainable miRNA drugs have been in clinical trials with none undergoing phase III, while over 60 siRNA drugs are in complete clinical trial progression, including two approvals (patisiran and givosiran) [135,136,137]. For instance, MRX34 (a miR-34a mimic) in a phase I clinical trial led to tested objects undergoing five serious immune-related adverse events, therefore, terminating the project [138]. Additionally, RG-101, an anti-miR-122 drug, succeeded in phase I but was discontinued in phase II due to the occurrence of a few cases of hyperbilirubinemia [139].
The phenomenon of “too many targets for miRNA effect” (TMTME) has been considered to answer the main adverse events from the miRNA therapeutics [140]. Evidence has shown that one single miRNA can targets hundreds of genes [140]. Therefore, TMTME has been considered as an inevitable consequence caused by miRNA treatment. In other words, unlike most approved drugs with limited targets (including ICIs and siRNA drugs), a miRNA has far more target sequences to bind and cause incomplete complementation (including circRNAs, long non-coding RNAs, protein-coding genes, etc.) [140]. Hence, numerous chain reactions which might further lead to physiological dysfunction or other diseases (including irAEs) could happen after the introduction or removal of miRNA in humans [135]. Some of those changes are unknown and unpredictable, which brings huge obstacle to miRNA multiple target treatment [135]. Furthermore, as shown in our analyses performed using the TargetScan platform, the total amount of predicted targets of selected miRNAs ranges from 59 to 7852, which theoretically can trigger massive chain reactions by regulating multiple signal pathways, therefore, making TMTME an inevitable issue.
Of course, efforts have been made to eliminate or weaken the existing obstacles that were caused by TMTME. One of the potential solutions is the application of a safe and targeted drug delivery system which is a pattern of specifically designed carriers, largely based on nanomedicine [141,142]. Such a nanoparticle system has been considered to weaken the obstacles caused by TMTME by decreasing systemic drug concentration and effective doses [135]. Those nanoparticles were built to encapsulate and deliver miRNAs to specific lesion sites with enhanced solubility and efficacy of drugs, and reduced interaction with untargeted tissues [141,142,143]. Thus, potentially, the number of unnecessary targets that are supposed to be affected by delivered miRNAs could also be reduced [141,142,143]. Certain miRNA delivery systems were also developed for breast cancer treatment. For instance, in triple-negative breast cancer treatment, hyaluronic acid–chitosan was built to deliver miR-34a mimics [144], and RNA-NPs (nanoparticles) decorated with EGFR-targeting aptamer, which was used to carry a miR-21 inhibitor [145]. A novel fabricated nano-complex, namely gold–nanoparticles (AuNPs), was developed for miR-206 for the treatment of breast cancer [146]. However, as a potential approach for dealing with the TMTME issue, more research and still required to further evaluate the relevant effects of nanoparticle systems. The application of a delivery system also has disadvantages. For example, such an approach will undoubtedly increase the cost, and the storage could become more difficult due to the crystallization process, which might cause drug expulsion from the nanoparticles [147,148,149,150]. Another promising technique is the embodiment of miRNA therapeutics into a biodegradable 3D matrix [151]. Such an approach can reduce the side effects by directly implantation into a local lesion as part of a surgical intervention. Briefly, it has been proved that an implanted 3D matrix can locally trigger a continuous, tissue-related, and comparatively moderate release of miRNA-based curatives [152,153]. In addition, ex vivo miRNA-based therapeutics have also been regarded as a potential option which may provide more immediate clinical effect without going through complicated metabolic processes [151,152]. Such a technique has been shown to improve the effectiveness of adoptive immune cell transfer approaches, including potentiating adoptive T cell treatments, by regulating genes involved in T cell activation and fitness [151,152]. Moreover, based on the potential curative effect possessed by certain miRNAs originated from medically relevant plant sources, a novel concept of oral administration of miRNA-based therapeutics that stem from plants has been provided as a potential solution [154]. However, many problems, such as the bioavailability of miRNAs contained in plant food and the regulatory capacity of plant miRNAs in mammalian cells, are still unclear [155,156]. Therefore, massive investigations are required before any related therapeutic application can be implemented. Approaches, such as topical, periocular, and systemic corticosteroids administration have also been developing for controlling related side effects [157,158,159]. Indeed, the selection of qualified and proper miRNA is most crucial. However, to achieve this goal, significant research is required, since it is a novel and innovative field.
Another potential solution is to introduce the application of miRNAs that can predict the response to an immune checkpoint blockade [160]. Recent evidence has found that some miRNAs, as complex regulators of gene expression which reflect immune status and activity, can be used to predict the potential clinical benefit of ICI therapy (shown in Supplementary File S1) [160]. For instance, in patients with non-small cell lung cancer (NSCLC), certain miRNAs (miR-215-5p, miR-411-3p, miR-493-5p, miR-494-3p, miR-495-3p, miR-548j-5p, and miR-93-3p) have been found to be expressed differently between the “good responders” (overall survival, OS > 6 months) and the “poor responders” (OS < 6 months), and showed a promising predictive value for ICIs therapy [161]. Furthermore, in esophageal squamous cell carcinoma patients, after nivolumab treatment, low expression levels of miR-6885-5p, miR-4698, and miR-128-2-5p assisted in separating responders from non-responders [162,163]. It has been concluded that targeting and regulating the immune checkpoint proteins is a potential mechanism for miRNAs to predict the response to ICIs and the therapeutic effect. Furthermore, readily accessible pretreatment blood miRNAs may provide a more convenient way to perform the prediction, making miRNA-based prediction very crucial for cancer immunotherapy [160]. However, to the best of our knowledge, miRNAs for predicting ICIs therapy in breast cancer have not yet been reported. Therefore, more research investment is strongly required in this field [164].
Additionally, alternatives to miRNAs, as sensitizers for ICI-based treatment, also require investment in research. Angiogenesis blockade, for example, has been found to exert a better therapeutic effect when applied with an immune checkpoint inhibitor in solid cancers [165]. Evidence also reported that an appropriate angiogenesis inhibitor can alleviate immunosuppression and enhance immunity by pruning blood vessels that are pivotal for tumor progression, and by blocking negative immune signals via decreasing the level at immune checkpoints, thereby increasing the anti-/pro-tumor immune subset ratio and alleviating hypoxia by normalizing tumor vasculature. Furthermore, the efficacy of anti-angiogenic therapies can also be improved by ICIs via recruiting immune cell subtypes with an angio-modulatory function [165]. Moreover, recent evidence has reported that histone deacetylases 2 (HDAC2) blockade can regulate the level of T lymphocyte subsets, inhibit tumor immune suppression and, consequently, enhance the efficacy of PD-1/PD-L1 inhibitors by regulating the progress of membranal PD-L1 nuclear translocation, improving anti-cancer immunity [143,166,167]. Thus, HDAC2 inhibitors, as a novel type of anticancer drug, have also displayed their potential as a sensitizer for cancer immunotherapy [166]. Furthermore, CAXII (carbonic anhydrase XII) inhibitor is also considered as a potential sensitizer which has been reported to reduce the immunosuppressive stress mediated by hypoxic/acidic metabolism, to modulate the expression of CCL8, and to affect the functions of monocytes and macrophages, thereby improving anti-tumor immunity and enhancing the therapeutic effect of PD-1 inhibitors in solid cancer [168,169,170,171,172]. Other approaches from alternative medicine, such as human biofield therapy, have also been mentioned [173,174]. Certainly, the combination strategy of multiple ICI sensitizers may also provide a novel perspective for the future study of cancer treatments.
5. Conclusions
The application of ICI monotherapy and combined ICIs has shown promise in treating a variety of malignancies. However, many patients, including breast cancer patients, cannot obtain an ideal and long-lasting curative effect from such a therapeutic approach. Based on the regulating effect of miRNAs on the transcription of immune checkpoints, a strategy combining miRNA with ICIs has been considered as a very novel and exciting way to enhance the potency of immune checkpoint-specific monotherapy. The miRNAs targeting multiple immune checkpoint molecules are believed to enhance the efficacy of ICI by mimicking combination therapy. Nonetheless, risks, such as irAEs, may also come along with such promising but innovative therapeutic synergism. Therefore, this review not only selected potential microRNAs for further exploration, but also discussed the risks associated with applying such a therapeutic strategy and the potential solutions to those risks. This may realize a whole new possible form of cancer immunotherapy by applying miRNAs with multiple immune checkpoint molecules as a novel additive therapy for ICI.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15030824/s1. File S1: Some miRNAs [175,176,177,178].
Author Contributions
R.H. created the original concept of this paper; R.H. and H.Z. wrote the manuscript; W.J. helped to complete the figures and tables; R.H. and L.L. revised the manuscript. All authors reviewed the manuscript; All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interests.
Funding Statement
This research was supported by “National Natural Science Foundation of China Youth Fund (82204864)” project (to Rui Han).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Gomez-Puerto D., Llop-Guevara A., Cruellas M., Torres-Esquius S., De La Torre J., Peg V., Balmaña J., Pimentel I. Genetic and functional homologous repair deficiency as biomarkers for platinum sensitivity in TNBC: A case report. Front. Oncol. 2022;12:963728. doi: 10.3389/fonc.2022.963728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotte A. Combination of CTLA-4 and PD-1 blockers for treatment of cancer. J. Exp. Clin. Cancer Res. 2019;38:255. doi: 10.1186/s13046-019-1259-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qureshi S., Chan N., George M., Ganesan S., Toppmeyer D., Omene C. Immune Checkpoint Inhibitors in Triple Negative Breast Cancer: The Search for the Optimal Biomarker. Biomark. Insights. 2022;17:11772719221078774. doi: 10.1177/11772719221078774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meng Z., Zhang R., Wu X., Zhang M., Jin T. PD-L1 mediates triple-negative breast cancer evolution via the regulation of TAM/M2 polarization. Int. J. Oncol. 2022;61:150. doi: 10.3892/ijo.2022.5440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge X., Yost S.E., Lee J.S., Frankel P.H., Ruel C., Cui Y., Murga M., Tang A., Martinez N., Chung S., et al. Phase II Study Combining Pembrolizumab with Aromatase Inhibitor in Patients with Metastatic Hormone Receptor Positive Breast Cancer. Cancers. 2022;14:4279. doi: 10.3390/cancers14174279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huober J., Barrios C.H., Niikura N., Jarząb M., Chang Y.-C., Huggins-Puhalla S.L., Pedrini J., Zhukova L., Graupner V., Eiger D., et al. Atezolizumab with Neoadjuvant Anti–Human Epidermal Growth Factor Receptor 2 Therapy and Chemotherapy in Human Epidermal Growth Factor Receptor 2–Positive Early Breast Cancer: Primary Results of the Randomized Phase III IMpassion050 Trial. J. Clin. Oncol. 2022;40:2946–2956. doi: 10.1200/JCO.21.02772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Müller P., Kreuzaler M., Khan T., Thommen D.S., Martin K., Glatz K., Savic S., Harbeck N., Nitz U., Gluz O., et al. Trastuzumab emtansine (T-DM1) renders HER2 + breast cancer highly susceptible to CTLA-4/PD-1 blockade. Sci. Transl. Med. 2015;7:315ra188. doi: 10.1126/scitranslmed.aac4925. [DOI] [PubMed] [Google Scholar]
- 10.Keam S.J. Cadonilimab: First Approval. Drugs. 2022;82:1333–1339. doi: 10.1007/s40265-022-01761-9. [DOI] [PubMed] [Google Scholar]
- 11.Beavers K.R., Nelson C.E., Duvall C.L. MiRNA inhibition in tissue engineering and regenerative medicine. Adv. Drug Deliv. Rev. 2015;88:123–137. doi: 10.1016/j.addr.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han R., Chen X., Li Y., Zhang S., Li R., Lu L. MicroRNA-34a suppresses aggressiveness of hepatocellular carcinoma by modulating E2F1, E2F3, and Caspase-3. Cancer Manag. Res. 2019;11:2963–2976. doi: 10.2147/CMAR.S202664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han R., Zhao J., Lu L. MicroRNA-34a expression affects breast cancer invasion in vitro and patient survival via downregulation of E2F1 and E2F3 expression. Oncol. Rep. 2020;43:2062–2072. doi: 10.3892/or.2020.7549. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rupaimoole R., Slack F.J. MicroRNA therapeutics: Towards a new era for the management of cancer and other diseases. Nat. Rev. Drug Discov. 2017;16:203–222. doi: 10.1038/nrd.2016.246. [DOI] [PubMed] [Google Scholar]
- 16.Ling H., Fabbri M., Calin G.A. MicroRNAs and other non-coding RNAs as targets for anticancer drug development. Nat. Rev. Drug Discov. 2013;12:847–865. doi: 10.1038/nrd4140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smolle M.A., Calin H.N., Pichler M., Calin G.A. Noncoding RNAs and immune checkpoints-clinical implications as cancer therapeutics. FEBS J. 2017;284:1952–1966. doi: 10.1111/febs.14030. [DOI] [PubMed] [Google Scholar]
- 18.Dragomir M., Chen B., Fu X., Calin G.A. Key questions about the checkpoint blockade-are microRNAs an answer? Cancer Biol. Med. 2018;15:103–115. doi: 10.20892/j.issn.2095-3941.2018.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei Q., Zhu R., Zhu J., Zhao R., Li M. E2-Induced Activation of the NLRP3 Inflammasome Triggers Pyroptosis and Inhibits Autophagy in HCC Cells. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2019;27:827–834. doi: 10.3727/096504018X15462920753012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Martino M., Riillo C., Scionti F., Grillone K., Polerà N., Caracciolo D., Arbitrio M., Tagliaferri P., Tassone P. miRNAs and lncRNAs as Novel Therapeutic Targets to Improve Cancer Immunotherapy. Cancers. 2021;13:1587. doi: 10.3390/cancers13071587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu S., Tao Z., Hai B., Liang H., Shi Y., Wang T., Song W., Chen Y., OuYang J., Chen J., et al. miR-424(322) reverses chemoresistance via T-cell immune response activation by blocking the PD-L1 immune checkpoint. Nat. Commun. 2016;7:11406. doi: 10.1038/ncomms11406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao L., Yu H., Yi S., Peng X., Su P., Xiao Z., Liu R., Tang A., Li X., Liu F., et al. The tumor suppressor miR-138-5p targets PD-L1 in colorectal cancer. Oncotarget. 2016;7:45370–45384. doi: 10.18632/oncotarget.9659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nygren M.K., Tekle C., Ingebrigtsen V.A., Makela R., Krohn M., Aure M.R., Nunes-Xavier C.E., Perala M., Tramm T., Alsner J., et al. Identifying microRNAs regulating B7-H3 in breast cancer: The clinical impact of microRNA-29c. Br. J. Cancer. 2014;110:2072–2080. doi: 10.1038/bjc.2014.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y., Wang G., Lin B., Huang J. MicroRNA-93-5p expression in tumor tissue and its tumor suppressor function via targeting programmed death ligand-1 in colorectal cancer. Cell Biol. Int. 2020;44:1224–1236. doi: 10.1002/cbin.11323. [DOI] [PubMed] [Google Scholar]
- 25.Yang L., Cai Y., Zhang D., Sun J., Xu C., Zhao W., Jiang W., Pan C. miR-195/miR-497 Regulate CD274 Expression of Immune Regulatory Ligands in Triple-Negative Breast Cancer. J. Breast Cancer. 2018;21:371–381. doi: 10.4048/jbc.2018.21.e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang M., Xiao R., Wang X., Xiong Y., Duan Z., Li D., Kan Q. MiR-93-5p regulates tumorigenesis and tumor immunity by targeting PD-L1/CCND1 in breast cancer. Ann. Transl. Med. 2022;10:203. doi: 10.21037/atm-22-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang M., Gao D., Shi Y., Wang Y., Joshi R., Yu Q., Liu D., Alotaibi F., Zhang Y., Wang H., et al. miR-149-3p reverses CD8 + T-cell exhaustion by reducing inhibitory receptors and promoting cytokine secretion in breast cancer cells. Open Biol. 2019;9:190061. doi: 10.1098/rsob.190061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Q.-M., Lian G.-Y., Song Y., Huang Y.-F., Gong Y. LncRNA MALAT1 promotes tumorigenesis and immune escape of diffuse large B cell lymphoma by sponging miR-195. Life Sci. 2019;231:116335. doi: 10.1016/j.lfs.2019.03.040. [DOI] [PubMed] [Google Scholar]
- 29.Zhang M., Shi Y., Zhang Y., Wang Y., Alotaibi F., Qiu L., Wang H., Peng S., Liu Y., Li Q., et al. miRNA-5119 regulates immune checkpoints in dendritic cells to enhance breast cancer immunotherapy. Cancer Immunol. Immunother. 2020;69:951–967. doi: 10.1007/s00262-020-02507-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li L., Lu S., Liang X., Cao B., Wang S., Jiang J., Luo H., He S., Lang J., Zhu G. γδTDEs: An Efficient Delivery System for miR-138 with Anti-tumoral and Immunostimulatory Roles on Oral Squamous Cell Carcinoma. Mol. Ther. Nucleic Acids. 2019;14:101–113. doi: 10.1016/j.omtn.2018.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rasoolnezhad M., Safaralizadeh R., Hosseinpourfeizi M.A., Banan-Khojasteh S.M., Baradaran B. MiRNA-138–5p: A strong tumor suppressor targeting PD-L-1 inhibits proliferation and motility of breast cancer cells and induces apoptosis. Eur. J. Pharmacol. 2021;896:173933. doi: 10.1016/j.ejphar.2021.173933. [DOI] [PubMed] [Google Scholar]
- 32.El Ahanidi H., El Azzouzi M., Hafidi Alaoui C., Tetou M., Bensaid M., Chaoui I., Benbacer L., Hassan I., Oukabli M., Michaud K., et al. Immune Checkpoint and Telomerase Crosstalk Is Mediated by miRNA-138 in Bladder Cancer. Front. Oncol. 2022;11:5774. doi: 10.3389/fonc.2021.795242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim J. Identification of MicroRNAs as Diagnostic Biomarkers for Breast Cancer Based on the Cancer Genome Atlas. Diagnostics. 2021;11:107. doi: 10.3390/diagnostics11010107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang H., Li M., Kaboli P.J., Ji H., Du F., Wu X., Zhao Y., Shen J., Wan L., Yi T., et al. Identification of cluster of differentiation molecule-associated microRNAs as potential therapeutic targets for gastrointestinal cancer immunotherapy. Int. J. Biol. Markers. 2021;36:22–32. doi: 10.1177/17246008211005473. [DOI] [PubMed] [Google Scholar]
- 35.Zheng Y., Song A., Zhou Y., Zhong Y., Zhang W., Wang C., Ding X., Du Y., Li G., Wu H., et al. Identification of extracellular vesicles-transported miRNAs in Erlotinib-resistant head and neck squamous cell carcinoma. J. Cell Commun. Signal. 2020;14:389–402. doi: 10.1007/s12079-020-00546-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen W., Guo Z., Wu J., Lin G., Chen S., Lin Q., Yang J., Xu Y., Zeng Y. Identification of a ZC3H12D-regulated competing endogenous RNA network for prognosis of lung adenocarcinoma at single-cell level. BMC Cancer. 2022;22:115. doi: 10.1186/s12885-021-08992-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J., Liu X., Hao C., Lu Y., Duan X., Liang R., Gao G., Zhang T. MEG3 modulates TIGIT expression and CD4 + T cell activation through absorbing miR-23a. Mol. Cell. Biochem. 2019;454:67–76. doi: 10.1007/s11010-018-3453-2. [DOI] [PubMed] [Google Scholar]
- 38.Gaynor N., Crown J., Collins D.M. Immune checkpoint inhibitors: Key trials and an emerging role in breast cancer. Semin. Cancer Biol. 2022;79:44–57. doi: 10.1016/j.semcancer.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 39.Schmid P., Rugo H.S., Adams S., Schneeweiss A., Barrios C.H., Iwata H., Diéras V., Henschel V., Molinero L., Chui S.Y., et al. Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): Updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21:44–59. doi: 10.1016/S1470-2045(19)30689-8. [DOI] [PubMed] [Google Scholar]
- 40.Ameri A., Tavakoli-Far B., Rostami M., Kiasari B.A., Sakhaei D., Ahmed O.S., Forouzani F., Fazli Y. Recent advances in atezolizumab-based programmed death-ligand 1 (PD-L1) blockade therapy for breast cancer. Int. Immunopharmacol. 2022;113:109334. doi: 10.1016/j.intimp.2022.109334. [DOI] [PubMed] [Google Scholar]
- 41.Dhillon S. Pucotenlimab: First Approval. Drugs. 2022;82:1557–1564. doi: 10.1007/s40265-022-01787-z. [DOI] [PubMed] [Google Scholar]
- 42.Giannopoulos S., Bozkus C.C., Zografos E., Athanasiou A., Bongiovanni A.M., Doulaveris G., Bakoyiannis C.N., Theodoropoulos G.E., Zografos G.C., Witkin S.S., et al. Targeting Both Autophagy and Immunotherapy in Breast Cancer Treatment. Metabolites. 2022;12:966. doi: 10.3390/metabo12100966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.He R., Yuan X., Chen Z., Zheng Y. Combined immunotherapy for metastatic triple-negative breast cancer based on PD-1/PD-L1 immune checkpoint blocking. Int. Immunopharmacol. 2022;113:109444. doi: 10.1016/j.intimp.2022.109444. [DOI] [PubMed] [Google Scholar]
- 44.Qiu D., Zhang G., Yan X., Xiao X., Ma X., Lin S., Wu J., Li X., Wang W., Liu J., et al. Prospects of Immunotherapy for Triple-Negative Breast Cancer. Front. Oncol. 2021;11:797092. doi: 10.3389/fonc.2021.797092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Santa-Maria C.A., Dunn S.A., Ho A.Y. Immunotherapy Combined with Radiation Therapy in Breast Cancer: A Rapidly Evolving Landscape. Semin. Radiat. Oncol. 2022;32:291–297. doi: 10.1016/j.semradonc.2022.01.001. [DOI] [PubMed] [Google Scholar]
- 46.Luo L., Wei Q., Xu C., Dong M., Zhao W. Immune landscape and risk prediction based on pyroptosis-related molecular subtypes in triple-negative breast cancer. Front. Immunol. 2022;13:933703. doi: 10.3389/fimmu.2022.933703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gardner A., Pulido D.M., Hänggi K., Bazargan S., Onimus A., Kasprzak A., Conejo-Garcia J.R., Rejniak K.A., Ruffell B. TIM-3 blockade enhances IL-12-dependent antitumor immunity by promoting CD8+ T cell and XCR1+ dendritic cell spatial co-localization. J. Immunother. Cancer. 2022;10:e003571. doi: 10.1136/jitc-2021-003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhu C., Dixon K.O., Newcomer K., Gu G., Xiao S., Zaghouani S., Schramm M.A., Wang C., Zhang H., Goto K., et al. Tim-3 adaptor protein Bat3 is a molecular checkpoint of T cell terminal differentiation and exhaustion. Sci. Adv. 2021;7:eabd2710. doi: 10.1126/sciadv.abd2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qian W., Zhao M., Wang R., Li H. Fibrinogen-like protein 1 (FGL1): The next immune checkpoint target. J. Hematol. Oncol. 2021;14:147. doi: 10.1186/s13045-021-01161-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Battin C., Leitner J., Waidhofer-Söllner P., Grabmeier-Pfistershammer K., Olive D., Steinberger P. BTLA inhibition has a dominant role in the cis-complex of BTLA and HVEM. Front. Immunol. 2022;13:956694. doi: 10.3389/fimmu.2022.956694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu W., Chou T.-F., Garrett-Thomson S.C., Seo G.-Y., Fedorov E., Ramagopal U.A., Bonanno J.B., Wang Q., Kim K., Garforth S.J., et al. HVEM structures and mutants reveal distinct functions of binding to LIGHT and BTLA/CD160. J. Exp. Med. 2021;218:e20211112. doi: 10.1084/jem.20211112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Murphy T.L., Murphy K.M. Slow Down and Survive: Enigmatic Immunoregulation by BTLA and HVEM. Annu. Rev. Immunol. 2010;28:389–411. doi: 10.1146/annurev-immunol-030409-101202. [DOI] [PubMed] [Google Scholar]
- 53.Dill E.A., Dillon P.M., Bullock T.N., Mills A.M. IDO expression in breast cancer: An assessment of 281 primary and metastatic cases with comparison to PD-L1. Mod. Pathol. 2018;31:1513–1522. doi: 10.1038/s41379-018-0061-3. [DOI] [PubMed] [Google Scholar]
- 54.Lu J., Liu X., Liao Y.-P., Wang X., Ahmed A., Jiang W., Ji Y., Meng H., Nel A.E. Breast Cancer Chemo-immunotherapy through Liposomal Delivery of an Immunogenic Cell Death Stimulus Plus Interference in the IDO-1 Pathway. ACS Nano. 2018;12:11041–11061. doi: 10.1021/acsnano.8b05189. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 55.Spira A.I., Hamid O., Bauer T.M., Borges V.F., Wasser J.S., Smith D.C., Clark A.S., Schmidt E.V., Zhao Y., Maleski J.E., et al. Efficacy/safety of epacadostat plus pembrolizumab in triple-negative breast cancer and ovarian cancer: Phase I/II ECHO-202 study. J. Clin. Oncol. 2017;35:1103. doi: 10.1200/JCO.2017.35.15_suppl.1103. [DOI] [Google Scholar]
- 56.Shen X., Fu W., Wei Y., Zhu J., Yu Y., Lei C., Zhao J., Hu S. TIGIT-Fc Promotes Antitumor Immunity. Cancer Immunol. Res. 2021;9:1088–1097. doi: 10.1158/2326-6066.CIR-20-0986. [DOI] [PubMed] [Google Scholar]
- 57.Chen C., Guo Q., Fu H., Yu J., Wang L., Sun Y., Zhang J., Duan Y. Asynchronous blockade of PD-L1 and CD155 by polymeric nanoparticles inhibits triple-negative breast cancer progression and metastasis. Biomaterials. 2021;275:120988. doi: 10.1016/j.biomaterials.2021.120988. [DOI] [PubMed] [Google Scholar]
- 58.Chen Y., Mo J., Jia X., He Y. The B7 Family Member B7-H6: A New Bane of Tumor. Pathol. Oncol. Res. 2018;24:717–721. doi: 10.1007/s12253-017-0357-5. [DOI] [PubMed] [Google Scholar]
- 59.Han Y.Y., Liu D.D., Li L.H. PD-1/PD-L1 pathway: Current researches in cancer. Am. J. Cancer Res. 2020;10:727–742. [PMC free article] [PubMed] [Google Scholar]
- 60.Mittendorf E.A., Philips A.V., Meric-Bernstam F., Qiao N., Wu Y., Harrington S., Su X., Wang Y., Gonzalez-Angulo A.M., Akcakanat A., et al. PD-L1 Expression in Triple-Negative Breast Cancer. Cancer Immunol. Res. 2014;2:361–370. doi: 10.1158/2326-6066.CIR-13-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thomas R., Al-Khadairi G., Decock J. Immune Checkpoint Inhibitors in Triple Negative Breast Cancer Treatment: Promising Future Prospects. Front. Oncol. 2020;10:600573. doi: 10.3389/fonc.2020.600573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Loi S., Giobbie-Hurder A., Gombos A., Bachelot T., Hui R., Curigliano G., Campone M., Biganzoli L., Bonnefoi H., Jerusalem G., et al. Pembrolizumab plus trastuzumab in trastuzumab-resistant, advanced, HER2-positive breast cancer (PANACEA): A single-arm, multicentre, phase 1b–2 trial. Lancet Oncol. 2019;20:371–382. doi: 10.1016/S1470-2045(18)30812-X. [DOI] [PubMed] [Google Scholar]
- 63.Schmid P., Cortes J., Pusztai L., McArthur H., Kümmel S., Bergh J., Denkert C., Park Y.H., Hui R., Harbeck N., et al. Pembrolizumab for Early Triple-Negative Breast Cancer. N. Engl. J. Med. 2020;382:810–821. doi: 10.1056/NEJMoa1910549. [DOI] [PubMed] [Google Scholar]
- 64.Zhang H., Dai Z., Wu W., Wang Z., Zhang N., Zhang L., Zeng W.-J., Liu Z., Cheng Q. Regulatory mechanisms of immune checkpoints PD-L1 and CTLA-4 in cancer. J. Exp. Clin. Cancer Res. 2021;40:184. doi: 10.1186/s13046-021-01987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lipson E.J., Drake C.G. Ipilimumab: An Anti-CTLA-4 Antibody for Metastatic Melanoma. Clin. Cancer Res. 2011;17:6958–6962. doi: 10.1158/1078-0432.CCR-11-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baas P., Scherpereel A., Nowak A.K., Fujimoto N., Peters S., Tsao A.S., Mansfield A.S., Popat S., Jahan T., Antonia S., et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): A multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;397:375–386. doi: 10.1016/S0140-6736(20)32714-8. [DOI] [PubMed] [Google Scholar]
- 67.Larkin J., Chiarion-Sileni V., Gonzalez R., Grob J.-J., Cowey C.L., Lao C.D., Schadendorf D., Dummer R., Smylie M., Rutkowski P., et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N. Engl. J. Med. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Motzer R.J., Tannir N.M., McDermott D.F., Aren Frontera O., Melichar B., Choueiri T.K., Plimack E.R., Barthélémy P., Porta C., George S., et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2018;378:1277–1290. doi: 10.1056/NEJMoa1712126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McArthur H.L., Diab A., Page D.B., Yuan J., Solomon S.B., Sacchini V., Comstock C., Durack J.C., Maybody M., Sung J., et al. A Pilot Study of Preoperative Single-Dose Ipilimumab and/or Cryoablation in Women with Early-Stage Breast Cancer with Comprehensive Immune Profiling. Clin. Cancer Res. 2016;22:5729–5737. doi: 10.1158/1078-0432.CCR-16-0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Page D.B., Beal K., Linch S.N., Spinelli K.J., Rodine M., Halpenny D., Modi S., Patil S., Young R.J., Kaley T., et al. Brain radiotherapy, tremelimumab-mediated CTLA-4-directed blockade +/− trastuzumab in patients with breast cancer brain metastases. NPJ Breast Cancer. 2022;8:50. doi: 10.1038/s41523-022-00404-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Anderson A.C. Tim-3: An Emerging Target in the Cancer Immunotherapy Landscape. Cancer Immunol. Res. 2014;2:393–398. doi: 10.1158/2326-6066.CIR-14-0039. [DOI] [PubMed] [Google Scholar]
- 72.Cheng S., Han F., Xu Y., Qu T., Ju Y. Expression of Tim-3 in breast cancer tissue promotes tumor progression. Int. J. Clin. Exp. Pathol. 2018;11:1157–1166. [PMC free article] [PubMed] [Google Scholar]
- 73.Kim H., Gridelli C., Kapur D., Tufman A., Felip E., Velcheti V., Kim Y., Goetze T., Lopez P.G., Corre R., et al. Cobolimab with Dostarlimab and Docetaxel in Patients with Advanced Non-small Cell Lung Cancer (NSCLC): COSTAR Lung. J. Thorac. Oncol. 2022;17:S109–S110. doi: 10.1016/j.jtho.2022.07.183. [DOI] [Google Scholar]
- 74.Murthy G.G., Atallah E. Targeting TIM-3 as a new strategy in immunotherapy: Focus on sabatolimab. Drugs Future. 2021;46:901–905. doi: 10.1358/dof.2021.46.11.3343951. [DOI] [Google Scholar]
- 75.Chocarro L., Blanco E., Zuazo M., Arasanz H., Bocanegra A., Fernández-Rubio L., Morente P., Fernández-Hinojal G., Echaide M., Garnica M., et al. Understanding LAG-3 Signaling. Int. J. Mol. Sci. 2021;22:5282. doi: 10.3390/ijms22105282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goldberg M.V., Drake C.G. LAG-3 in Cancer Immunotherapy. In: Dranoff G., editor. Cancer Immunology and Immunotherapy. Volume 344. Springer; Berlin/Heidelberg, Germany: 2011. pp. 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stovgaard E.S., Kümler I.M., List-Jensen K., Roslind A.M., Christensen I.J.M., Høgdall E.P., Nielsen D.P., Balslev E. Prognostic and Clinicopathologic Associations of LAG-3 Expression in Triple-negative Breast Cancer. Appl. Immunohistochem. Mol. Morphol. 2021;30:62–71. doi: 10.1097/PAI.0000000000000954. [DOI] [PubMed] [Google Scholar]
- 78.Tawbi H.A., Schadendorf D., Lipson E.J., Ascierto P.A., Matamala L., Gutiérrez E.C., Rutkowski P., Gogas H.J., Lao C.D., De Menezes J.J., et al. Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. N. Engl. J. Med. 2022;386:24–34. doi: 10.1056/NEJMoa2109970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chocarro L., Blanco E., Arasanz H., Fernández-Rubio L., Bocanegra A., Echaide M., Garnica M., Ramos P., Fernández-Hinojal G., Vera R., et al. Clinical landscape of LAG-3-targeted therapy. Immunooncol. Technol. 2022;14:100079. doi: 10.1016/j.iotech.2022.100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kakish H.H., Ahmed F.A., Elshami M., Loftus A.W., Hoehn R.S., Ammori J.B., Ocuin L.M., Winter J.M., Bordeaux J.S., Mangla A., et al. Trends in Melanoma Phase 3 Clinical Trials since 2010: Is there Hope for Advanced Melanoma Therapies beyond Approved Treatment Mechanisms? Cancers. 2022;14:5184. doi: 10.3390/cancers14215184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhao B.-W., Zhang F.-Y., Wang Y., Chen G.-M., Nie M., Zhao Z.-K., Chen X.-J., Jiang K.-M., Nie R.-C., Chen Y.-B. LAG3-PD1 or CTLA4-PD1 Inhibition in Advanced Melanoma: Indirect Cross Comparisons of the CheckMate-067 and RELATIVITY-047 Trials. Cancers. 2022;14:4975. doi: 10.3390/cancers14204975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shi A.-P., Tang X.-Y., Xiong Y.-L., Zheng K.-F., Liu Y.-J., Shi X.-G., Lv Y., Jiang T., Ma N., Zhao J.-B. Immune Checkpoint LAG3 and Its Ligand FGL1 in Cancer. Front. Immunol. 2021;12:785091. doi: 10.3389/fimmu.2021.785091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barshidi A., Karpisheh V., Noukabadi F.K., Kiani F.K., Mohammadi M., Afsharimanesh N., Ebrahimi F., Kiaie S.H., Navashenaq J.G., Hojjat-Farsangi M., et al. Dual Blockade of PD-1 and LAG3 Immune Checkpoints Increases Dendritic Cell Vaccine Mediated T Cell Responses in Breast Cancer Model. Pharm. Res. 2022;39:1851–1866. doi: 10.1007/s11095-022-03297-9. [DOI] [PubMed] [Google Scholar]
- 84.Kraehenbuehl L., Weng C.-H., Eghbali S., Wolchok J.D., Merghoub T. Enhancing immunotherapy in cancer by targeting emerging immunomodulatory pathways. Nat. Rev. Clin. Oncol. 2022;19:37–50. doi: 10.1038/s41571-021-00552-7. [DOI] [PubMed] [Google Scholar]
- 85.Tsang J.Y.S., Chan K.-W., Ni Y.-B., Hlaing T., Hu J., Cheung S.-Y., Tse G.M. Expression and Clinical Significance of Herpes Virus Entry Mediator (HVEM) in Breast Cancer. Ann. Surg. Oncol. 2017;24:4042–4050. doi: 10.1245/s10434-017-5924-1. [DOI] [PubMed] [Google Scholar]
- 86.Li D., Fu Z., Chen S., Yuan W., Liu Y., Li L., Pang D., Li D. HVEM Gene Polymorphisms Are Associated with Sporadic Breast Cancer in Chinese Women. PLoS ONE. 2013;8:e71040. doi: 10.1371/journal.pone.0071040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xu Z., Shen J., Wang M.H., Yi T., Yu Y., Zhu Y., Chen B., Chen J., Li L., Li M., et al. Comprehensive molecular profiling of the B7 family of immune-regulatory ligands in breast cancer. Oncoimmunology. 2016;5:e1207841. doi: 10.1080/2162402X.2016.1207841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schilder R.J., Powderly J.D., Park H., Bilen M.A., McKean M., May R., Feng H., Yao S., Keegan P., Naing A. Phase Ia dose-escalation study of the anti-BTLA antibody icatolimab as a monotherapy in patients with advanced solid tumor. J. Clin. Oncol. 2022;40:2643. doi: 10.1200/JCO.2022.40.16_suppl.2643. [DOI] [Google Scholar]
- 89.Ma J., Xie Y., Zhang H., Song Y., Zhao W., Pan Y., Ran F., Feng H., Yao S., Keegan P., et al. Phase I study of the anti-BTLA antibody icatolimab as a single agent or in combination with toripalimab in relapsed/refractory lymphomas. J. Clin. Oncol. 2022;40:7578. doi: 10.1200/JCO.2022.40.16_suppl.7578. [DOI] [Google Scholar]
- 90.Ball H.J., Fedelis F.F., Bakmiwewa S.M., Hunt N.H., Yuasa H.J. Tryptophan-Catabolizing Enzymes—Party of Three. Front. Immunol. 2014;5:485. doi: 10.3389/fimmu.2014.00485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Li P., Xu W., Liu F., Zhu H., Zhang L., Ding Z., Liang H., Song J. The emerging roles of IDO2 in cancer and its potential as a therapeutic target. Biomed. Pharmacother. 2021;137:111295. doi: 10.1016/j.biopha.2021.111295. [DOI] [PubMed] [Google Scholar]
- 92.Mondanelli G., Mandarano M., Belladonna M.L., Suvieri C., Pelliccia C., Bellezza G., Sidoni A., Carvalho A., Grohmann U., Volpi C. Current Challenges for IDO2 as Target in Cancer Immunotherapy. Front. Immunol. 2021;12:679953. doi: 10.3389/fimmu.2021.679953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tang K., Wu Y.-H., Song Y., Yu B. Indoleamine 2,3-dioxygenase 1 (IDO1) inhibitors in clinical trials for cancer immunotherapy. J. Hematol. Oncol. 2021;14:68. doi: 10.1186/s13045-021-01080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.He X., He G., Chu Z., Wu H., Wang J., Ge Y., Shen H., Zhang S., Shan J., Peng K., et al. Discovery of the First Potent IDO1/IDO2 Dual Inhibitors: A Promising Strategy for Cancer Immunotherapy. J. Med. Chem. 2021;64:17950–17968. doi: 10.1021/acs.jmedchem.1c01305. [DOI] [PubMed] [Google Scholar]
- 95.Chauvin J.-M., Zarour H.M. TIGIT in cancer immunotherapy. J. Immunother. Cancer. 2020;8:e000957. doi: 10.1136/jitc-2020-000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rotte A., Sahasranaman S., Budha N. Targeting TIGIT for Immunotherapy of Cancer: Update on Clinical Development. Biomedicines. 2021;9:1277. doi: 10.3390/biomedicines9091277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Devilard E., Xerri L., Dubreuil P., Lopez M., Reymond N. Nectin-3 (CD113) Interacts with Nectin-2 (CD112) to Promote Lymphocyte Transendothelial Migration. PLoS ONE. 2013;8:e77424. doi: 10.1371/journal.pone.0077424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Meggyes M., Nagy D.U., Feik T., Boros A., Polgar B., Szereday L. Examination of the TIGIT-CD226-CD112-CD155 Immune Checkpoint Network during a Healthy Pregnancy. Int. J. Mol. Sci. 2022;23:10776. doi: 10.3390/ijms231810776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shaw G., Cavalcante L., Giles F.J., Taylor A. Elraglusib (9-ING-41), a selective small-molecule inhibitor of glycogen synthase kinase-3 beta, reduces expression of immune checkpoint molecules PD-1, TIGIT and LAG-3 and enhances CD8+ T cell cytolytic killing of melanoma cells. J. Hematol. Oncol. 2022;15:134. doi: 10.1186/s13045-022-01352-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hutten T., Norde W.J., Woestenenk R., Wang R.C., Maas F., Kester M., Falkenburg J.F., Berglund S., Luznik L., Jansen J.H., et al. Increased Coexpression of PD-1, TIGIT, and KLRG-1 on Tumor-Reactive CD8+ T Cells During Relapse after Allogeneic Stem Cell Transplantation. Biol. Blood Marrow Transplant. 2018;24:666–677. doi: 10.1016/j.bbmt.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 101.Liu X., Li M., Wang X., Dang Z., Jiang Y., Wang X., Kong Y., Yang Z. PD-1+ TIGIT+ CD8+ T cells are associated with pathogenesis and progression of patients with hepatitis B virus-related hepatocellular carcinoma. Cancer Immunol. Immunother. 2019;68:2041–2054. doi: 10.1007/s00262-019-02426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Guo Q., Chen C., Wu Z., Zhang W., Wang L., Yu J., Li L., Zhang J., Duan Y. Engineered PD-1/TIGIT dual-activating cell-membrane nanoparticles with dexamethasone act synergistically to shape the effector T cell/Treg balance and alleviate systemic lupus erythematosus. Biomaterials. 2022;285:121517. doi: 10.1016/j.biomaterials.2022.121517. [DOI] [PubMed] [Google Scholar]
- 103.Pandey A.K., Chauvin J.M., Brufsky A., Pagliano O., Ka M., Menna C., McAuliffe P., Zarour H. Targeting TIGIT and PD-1 in triple negative breast cancer. Cancer Res. 2020;80:P5-04-28. doi: 10.1158/1538-7445.SABCS19-P5-04-28. [DOI] [Google Scholar]
- 104.Yearley J.H., Gibson C., Yu N., Moon C., Murphy E., Juco J., Lunceford J., Cheng J., Chow L.Q., Seiwert T.Y., et al. PD-L2 Expression in Human Tumors: Relevance to Anti-PD-1 Therapy in Cancer. Clin. Cancer Res. 2017;23:3158–3167. doi: 10.1158/1078-0432.CCR-16-1761. [DOI] [PubMed] [Google Scholar]
- 105.Hoffmann O., Wormland S., Bittner A.-K., Collenburg M., Horn P.A., Kimmig R., Kasimir-Bauer S., Rebmann V. Programmed death receptor ligand-2 (PD-L2) bearing extracellular vesicles as a new biomarker to identify early triple-negative breast cancer patients at high risk for relapse. J. Cancer Res. Clin. Oncol. 2022:1–16. doi: 10.1007/s00432-022-03980-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shi Y., Wu J., Wang Z., Zhang L., Wang Z., Zhang M., Cen H., Peng Z., Li Y., Fan L., et al. Efficacy and safety of geptanolimab (GB226) for relapsed or refractory peripheral T cell lymphoma: An open-label phase 2 study (Gxplore-002) J. Hematol. Oncol. 2021;14:12. doi: 10.1186/s13045-021-01033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shi Y., Cai Q., Jiang Y., Huang G., Bi M., Wang B., Zhou Y., Wang G., Ying H., Tao Z., et al. Activity and Safety of Geptanolimab (GB226) for Patients with Unresectable, Recurrent, or Metastatic Alveolar Soft Part Sarcoma: A Phase II, Single-arm Study. Clin. Cancer Res. 2020;26:6445–6452. doi: 10.1158/1078-0432.CCR-20-2819. [DOI] [PubMed] [Google Scholar]
- 108.Zhang B., Sun J., Yao X., Li J., Tu Y., Yao F., Sun S. Knockdown of B7H6 inhibits tumor progression in triple-negative breast cancer. Oncol. Lett. 2018;16:91–96. doi: 10.3892/ol.2018.8689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li P., Zeng Y., Chen Y., Huang P., Chen X., Zheng W. LRP11-AS1 promotes the proliferation and migration of triple negative breast cancer cells via the miR-149-3p/NRP2 axis. Cancer Cell Int. 2022;22:116. doi: 10.1186/s12935-022-02536-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li X., Wang Q., Rui Y., Zhang C., Wang W., Gu J., Tang J., Ding Y. HOXC13-AS promotes breast cancer cell growth through regulating miR-497-5p/PTEN axis. J. Cell. Physiol. 2019;234:22343–22351. doi: 10.1002/jcp.28800. [DOI] [PubMed] [Google Scholar]
- 111.Purohit P.K., Edwards R., Tokatlidis K., Saini N. MiR-195 regulates mitochondrial function by targeting mitofusin-2 in breast cancer cells. RNA Biol. 2019;16:918–929. doi: 10.1080/15476286.2019.1600999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang H., Zhang M., Yang Y., Wang Y., Peng S., Joshi R., Shi Y., Liu Y., Zhang Y., Jiang J., et al. miR-5119 inhibitor prolonging allograft survival in heart transplantation by regulation of inhibitory receptor ligands in DCs. Eur. J. Immunol. 2019;49:1507–1508. [Google Scholar]
- 113.Zhang D., Liu X., Zhang Q., Chen X. miR-138-5p inhibits the malignant progression of prostate cancer by targeting FOXC1. Cancer Cell Int. 2020;20:297. doi: 10.1186/s12935-020-01386-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang W., Liao K., Liu D. MiR-138-5p Inhibits the Proliferation of Gastric Cancer Cells by Targeting DEK. Cancer Manag. Res. 2020;12:8137–8147. doi: 10.2147/CMAR.S253777. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 115.Shadbad M., Safaei S., Brunetti O., Derakhshani A., Lotfinejad P., Mokhtarzadeh A., Hemmat N., Racanelli V., Solimando A., Argentiero A., et al. A Systematic Review on the Therapeutic Potentiality of PD-L1-Inhibiting MicroRNAs for Triple-Negative Breast Cancer: Toward Single-Cell Sequencing-Guided Biomimetic Delivery. Genes. 2021;12:1206. doi: 10.3390/genes12081206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li X., Ren Y., Liu D., Yu X., Chen K. Role of miR-100-5p and CDC25A in breast carcinoma cells. PeerJ. 2022;10:e12263. doi: 10.7717/peerj.12263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ma P., Han J. Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8. Open Med. 2022;17:1172–1182. doi: 10.1515/med-2022-0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kim H.-K., Park J.D., Choi S.H., Shin D.J., Hwang S., Jung H.-Y., Park K.-S. Functional Link between miR-200a and ELK3 Regulates the Metastatic Nature of Breast Cancer. Cancers. 2020;12:1225. doi: 10.3390/cancers12051225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zou Q., Zhou E., Xu F., Zhang D., Yi W., Yao J. A TP73-AS1/miR-200a/ZEB1 regulating loop promotes breast cancer cell invasion and migration. J. Cell. Biochem. 2018;119:2189–2199. doi: 10.1002/jcb.26380. [DOI] [PubMed] [Google Scholar]
- 120.Liu M., Mo F., Song X., He Y., Yuan Y., Yan J., Yang Y., Huang J., Zhang S. Exosomal hsa-miR-21-5p is a biomarker for breast cancer diagnosis. PeerJ. 2021;9:e12147. doi: 10.7717/peerj.12147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang Y., Wang Y., Xue J., Liang W., Zhang Z., Yang X., Qiao Z., Jiang Y., Wang J., Cao X., et al. Co-treatment with miR-21-5p inhibitor and Aurora kinase inhibitor reversine suppresses breast cancer progression by targeting sprouty RTK signaling antagonist 2. Bioengineered. 2021;13:455–468. doi: 10.1080/21655979.2021.2009410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Aggarwal T., Wadhwa R., Gupta R., Paudel K.R., Collet T., Chellappan D.K., Gupta G., Perumalsamy H., Mehta M., Satija S., et al. MicroRNAs as Biomarker for Breast Cancer. Endocr. Metab. Immune Disord. Drug Targets. 2020;20:1597–1610. doi: 10.2174/1871530320666200428113051. [DOI] [PubMed] [Google Scholar]
- 123.Xiang Y., Liao X.-H., Yu C.-X., Yao A., Qin H., Li J.-P., Hu P., Li H., Guo W., Gu C.-J., et al. MiR-93-5p inhibits the EMT of breast cancer cells via targeting MKL-1 and STAT3. Exp. Cell Res. 2017;357:135–144. doi: 10.1016/j.yexcr.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 124.Jiang Q., He M., Guan S., Ma M., Wu H., Yu Z., Jiang L., Wang Y., Zong X., Jin F., et al. MicroRNA-100 suppresses the migration and invasion of breast cancer cells by targeting FZD-8 and inhibiting Wnt/β-catenin signaling pathway. Tumor Biol. 2016;37:5001–5011. doi: 10.1007/s13277-015-4342-x. [DOI] [PubMed] [Google Scholar]
- 125.Lim Y.-Y., Wright J.A., Attema J.L., Gregory P.A., Bert A.G., Smith E., Thomas D., Lopez A.F., Drew P.A., Khew-Goodall Y., et al. Epigenetic modulation of the miR-200 family is associated with transition to a breast cancer stem cell-like state. J. Cell Sci. 2013;126:2256–2266. doi: 10.1242/jcs.122275. [DOI] [PubMed] [Google Scholar]
- 126.Watson K.L., Jones R.A., Bruce A., Moorehead R.A. The miR-200b/200a/429 cluster prevents metastasis and induces dormancy in a murine claudin-low mammary tumor cell line. Exp. Cell Res. 2018;369:17–26. doi: 10.1016/j.yexcr.2018.04.024. [DOI] [PubMed] [Google Scholar]
- 127.Lu Z., Jiao D., Qiao J., Yang S., Yan M., Cui S., Liu Z. Restin suppressed epithelial-mesenchymal transition and tumor metastasis in breast cancer cells through upregulating mir-200a/b expression via association with p73. Mol. Cancer. 2015;14:102. doi: 10.1186/s12943-015-0370-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tsouko E., Wang J., Frigo D.E., Aydoğdu E., Williams C. miR-200a inhibits migration of triple-negative breast cancer cells through direct repression of the EPHA2 oncogene. Carcinogenesis. 2015;36:1051–1060. doi: 10.1093/carcin/bgv087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pan X., Wang Z.-X., Wang R. MicroRNA-21: A novel therapeutic target in human cancer. Cancer Biol. Ther. 2010;10:1224–1232. doi: 10.4161/cbt.10.12.14252. [DOI] [PubMed] [Google Scholar]
- 130.Khoja L., Day D., Chen T.W.-W., Siu L.L., Hansen A.R. Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: A systematic review. Ann. Oncol. 2017;28:2377–2385. doi: 10.1093/annonc/mdx286. [DOI] [PubMed] [Google Scholar]
- 131.Chennamadhavuni A., Abushahin L., Jin N., Presley C.J., Manne A. Risk Factors and Biomarkers for Immune-Related Adverse Events: A Practical Guide to Identifying High-Risk Patients and Rechallenging Immune Checkpoint Inhibitors. Front. Immunol. 2022;13:779691. doi: 10.3389/fimmu.2022.779691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wongvibulsin S., Pahalyants V., Kalinich M., Murphy W., Yu K.-H., Wang F., Chen S.T., Reynolds K., Kwatra S.G., Semenov Y.R. Epidemiology and risk factors for the development of cutaneous toxicities in patients treated with immune-checkpoint inhibitors: A United States population-level analysis. J. Am. Acad. Dermatol. 2022;86:563–572. doi: 10.1016/j.jaad.2021.03.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Biewenga M., van der Kooij M.K., Wouters M.W.J.M., Aarts M.J.B., Berkmortel F.W.P.J.V.D., de Groot J.W.B., Boers-Sonderen M.J., Hospers G.A.P., Piersma D., van Rijn R.S., et al. Checkpoint inhibitor induced hepatitis and the relation with liver metastasis and outcome in advanced melanoma patients. Hepatol. Int. 2021;15:510–519. doi: 10.1007/s12072-021-10151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Molina G.E., Zubiri L., Cohen J.V., Durbin S.M., Petrillo L., Allen I.M., Murciano-Goroff Y.R., Dougan M.L., Thomas M.F., Faje A.T., et al. Temporal Trends and Outcomes Among Patients Admitted for Immune-Related Adverse Events: A Single-Center Retrospective Cohort Study from 2011 to 2018. Oncologist. 2021;26:514–522. doi: 10.1002/onco.13740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang S., Cheng Z., Wang Y., Han T. The Risks of miRNA Therapeutics: In a Drug Target Perspective. Drug Des. Dev. Ther. 2021;15:721–733. doi: 10.2147/DDDT.S288859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Quan D., Obici L., Berk J.L., Ando Y., Aldinc E., White M.T., Adams D. Impact of baseline polyneuropathy severity on patisiran treatment outcomes in the APOLLO trial. Amyloid. 2022:1–10. doi: 10.1080/13506129.2022.2118043. [DOI] [PubMed] [Google Scholar]
- 137.Ricci A., Ventura P. Givosiran for the treatment of acute hepatic porphyria. Expert Rev. Clin. Pharmacol. 2022;15:383–393. doi: 10.1080/17512433.2022.2075848. [DOI] [PubMed] [Google Scholar]
- 138.Zarin D.A., Tse T., Williams R.J., Califf R.M., Ide N.C. The ClinicalTrials.gov Results Database—Update and Key Issues. N. Engl. J. Med. 2011;364:852–860. doi: 10.1056/NEJMsa1012065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tao J., Luo M., Sun H., Zhao H., Sun Q., Huang Z. Overexpression of tripartite motif containing 26 inhibits non-small cell lung cancer cell growth by suppressing PI3K/AKT signaling. Kaohsiung J. Med. Sci. 2020;36:417–422. doi: 10.1002/kjm2.12194. [DOI] [PubMed] [Google Scholar]
- 140.Hansen T.B., Jensen T.I., Clausen B.H., Bramsen J.B., Finsen B., Damgaard C.K., Kjems J. Natural RNA circles function as efficient microRNA sponges. Nature. 2013;495:384–388. doi: 10.1038/nature11993. [DOI] [PubMed] [Google Scholar]
- 141.Agrawal S., Garg A., Varshney V. Recent updates on applications of Lipid-based nanoparticles for site-specific drug delivery. Pharm. Nanotechnol. 2022;10:24–41. doi: 10.2174/2211738510666220304111848. [DOI] [PubMed] [Google Scholar]
- 142.Silva-Cázares M.B., Saavedra-Leos M.Z., Jordan-Alejandre E., Nuñez-Olvera S.I., Cómpean-Martínez I., López-Camarillo C. Lipid-based nanoparticles for the therapeutic delivery of non-coding RNAs in breast cancer (Review) Oncol. Rep. 2020;44:2353–2363. doi: 10.3892/or.2020.7791. [DOI] [PubMed] [Google Scholar]
- 143.Han R., Nusbaum O., Chen X., Zhu Y. Valeric Acid Suppresses Liver Cancer Development by Acting as a Novel HDAC Inhibitor. Mol. Ther. Oncolytics. 2020;19:8–18. doi: 10.1016/j.omto.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Deng X., Cao M., Zhang J., Hu K., Yin Z., Zhou Z., Xiao X., Yang Y., Sheng W., Wu Y., et al. Hyaluronic acid-chitosan nanoparticles for co-delivery of MiR-34a and doxorubicin in therapy against triple negative breast cancer. Biomaterials. 2014;35:4333–4344. doi: 10.1016/j.biomaterials.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 145.Shu D., Li H., Shu Y., Xiong G., Carson W.E., 3rd, Haque F., Xu R., Guo P. Systemic Delivery of Anti-miRNA for Suppression of Triple Negative Breast Cancer Utilizing RNA Nanotechnology. ACS Nano. 2015;9:9731–9740. doi: 10.1021/acsnano.5b02471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chaudhari R., Nasra S., Meghani N., Kumar A. MiR-206 conjugated gold nanoparticle based targeted therapy in breast cancer cells. Sci. Rep. 2022;12:4713. doi: 10.1038/s41598-022-08185-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Botto C., Augello G., Amore E., Emma M.R., Azzolina A., Cavallaro G., Cervello M., Bondì M.L. Cationic Solid Lipid Nanoparticles as Non Viral Vectors for the Inhibition of Hepatocellular Carcinoma Growth by RNA Interference. J. Biomed. Nanotechnol. 2018;14:1009–1016. doi: 10.1166/jbn.2018.2557. [DOI] [PubMed] [Google Scholar]
- 148.Wang X., Yu B., Wu Y., Lee R.J., Lee L.J. Efficient down-regulation of CDK4 by novel lipid nanoparticle-mediated siRNA delivery. Anticancer. Res. 2011;31:1619–1626. [PubMed] [Google Scholar]
- 149.Shoji S., Miura S., Watanabe S., Ohtsubo A., Nozaki K., Saida Y., Ichikawa K., Kondo R., Tanaka T., Koyama K., et al. Phase II study of nanoparticle albumin-bound paclitaxel monotherapy for relapsed non-small cell lung cancer with patient-reported outcomes (NLCTG1302) Transl. Lung Cancer Res. 2022;11:1359–1368. doi: 10.21037/tlcr-22-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Funk F., Flühmann B., Barton A.E. Criticality of Surface Characteristics of Intravenous Iron–Carbohydrate Nanoparticle Complexes: Implications for Pharmacokinetics and Pharmacodynamics. Int. J. Mol. Sci. 2022;23:2140. doi: 10.3390/ijms23042140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Diener C., Keller A., Meese E. Emerging concepts of miRNA therapeutics: From cells to clinic. Trends Genet. 2022;38:613–626. doi: 10.1016/j.tig.2022.02.006. [DOI] [PubMed] [Google Scholar]
- 152.Zhang X., Li Y., Chen Y.E., Chen J., Ma P.X. Cell-free 3D scaffold with two-stage delivery of miRNA-26a to regenerate critical-sized bone defects. Nat. Commun. 2016;7:10376. doi: 10.1038/ncomms10376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Katoh S., Yoshioka H., Senthilkumar R., Preethy S., Abraham S.J. Enhanced miRNA-140 expression of osteoarthritis-affected human chondrocytes cultured in a polymer based three-dimensional (3D) matrix. Life Sci. 2021;278:119553. doi: 10.1016/j.lfs.2021.119553. [DOI] [PubMed] [Google Scholar]
- 154.Shende P., Trivedi R. 3D Printed Bioconstructs: Regenerative Modulation for Genetic Expression. Stem Cell Rev. Rep. 2021;17:1239–1250. doi: 10.1007/s12015-021-10120-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhang L., Hou D., Chen X., Li D., Zhu L., Zhang Y., Li J., Bian Z., Liang X., Cai X., et al. Exogenous plant MIR168a specifically targets mammalian LDLRAP1: Evidence of cross-kingdom regulation by microRNA. Cell Res. 2012;22:107–126. doi: 10.1038/cr.2011.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sanchita, Trivedi R., Asif M.H., Trivedi P.K. Dietary plant miRNAs as an augmented therapy: Cross-kingdom gene regulation. RNA Biol. 2018;15:1433–1439. doi: 10.1080/15476286.2018.1551693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gambichler T., Scheel C., Reuther J., Susok L. Management of immune-related adverse events in anti-PD-1-treated patients with advanced cutaneous squamous cell carcinoma. J. Eur. Acad. Dermatol. Venereol. 2022;36((Suppl. 1)):23–28. doi: 10.1111/jdv.17402. [DOI] [PubMed] [Google Scholar]
- 158.Fortes B.H., Liou H., Dalvin L.A. Ophthalmic adverse effects of immune checkpoint inhibitors: The Mayo Clinic experience. Br. J. Ophthalmol. 2021;105:1263–1271. doi: 10.1136/bjophthalmol-2020-316970. [DOI] [PubMed] [Google Scholar]
- 159.Hong D.S., Kang Y.K., Borad M., Sachdev J., Ejadi S., Lim H.Y., Brenner A.J., Park K., Lee J.L., Kim T.Y., et al. Phase 1 study of MRX34, a liposomal miR-34a mimic, in patients with advanced solid tumours. Br. J. Cancer. 2020;122:1630–1637. doi: 10.1038/s41416-020-0802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Huemer F., Leisch M., Geisberger R., Zaborsky N., Greil R. miRNA-Based Therapeutics in the Era of Immune-Checkpoint Inhibitors. Pharmaceuticals. 2021;14:89. doi: 10.3390/ph14020089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Halvorsen A.R., Sandhu V., Sprauten M., Flote V.G., Kure E.H., Brustugun O.T., Helland Å. Circulating microRNAs associated with prolonged overall survival in lung cancer patients treated with nivolumab. Acta Oncol. 2018;57:1225–1231. doi: 10.1080/0284186X.2018.1465585. [DOI] [PubMed] [Google Scholar]
- 162.Kudo T., Hamamoto Y., Kato K., Ura T., Kojima T., Tsushima T., Hironaka S., Hara H., Satoh T., Iwasa S., et al. Nivolumab treatment for oesophageal squamous-cell carcinoma: An open-label, multicentre, phase 2 trial. Lancet Oncol. 2017;18:631–639. doi: 10.1016/S1470-2045(17)30181-X. [DOI] [PubMed] [Google Scholar]
- 163.Sudo K., Kato K., Matsuzaki J., Takizawa S., Aoki Y., Shoji H., Iwasa S., Honma Y., Takashima A., Sakamoto H., et al. Identification of serum microRNAs predicting the response of esophageal squamous-cell carcinoma to nivolumab. Jpn. J. Clin. Oncol. 2020;50:114–121. doi: 10.1093/jjco/hyz146. [DOI] [PubMed] [Google Scholar]
- 164.Bao S., Zhou T., Yan C., Bao J., Yang F., Chao S., Zhou M., Xu Z. A blood-based miRNA signature for early non-invasive diagnosis of preeclampsia. BMC Med. 2022;20:303. doi: 10.1186/s12916-022-02495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhu L., Yu X., Wang L., Liu J., Qu Z., Zhang H., Li L., Chen J., Zhou Q. Angiogenesis and immune checkpoint dual blockade in combination with radiotherapy for treatment of solid cancers: Opportunities and challenges. Oncogenesis. 2021;10:47. doi: 10.1038/s41389-021-00335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gao Y., Nihira N.T., Bu X., Chu C., Zhang J., Kolodziejczyk A., Fan Y., Chan N.T., Ma L., Liu J., et al. Acetylation-dependent regulation of PD-L1 nuclear translocation dictates the efficacy of anti-PD-1 immunotherapy. Nat. Cell Biol. 2020;22:1064–1075. doi: 10.1038/s41556-020-0562-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Han R., Yang H., Li Y., Ling C., Lu L. Valeric acid acts as a novel HDAC3 inhibitor against prostate cancer. Med Oncol. 2022;39:213. doi: 10.1007/s12032-022-01814-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ning W.-R., Jiang D., Liu X.-C., Huang Y.-F., Peng Z.-P., Jiang Z.-Z., Kang T., Zhuang S.-M., Wu Y., Zheng L. Carbonic anhydrase XII mediates the survival and prometastatic functions of macrophages in human hepatocellular carcinoma. J. Clin. Investig. 2022;132:e153110. doi: 10.1172/JCI153110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Raines L.N., Zhao H., Wang Y., Chen H.-Y., Gallart-Ayala H., Hsueh P.-C., Cao W., Koh Y., Alamonte-Loya A., Liu P.-S., et al. PERK is a critical metabolic hub for immunosuppressive function in macrophages. Nat. Immunol. 2022;23:431–445. doi: 10.1038/s41590-022-01145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Buddingh E.P., Kuijjer M.L., Duim R.A., Bürger H., Agelopoulos K., Myklebost O., Serra M., Mertens F., Hogendoorn P.C., Lankester A.C., et al. Tumor-Infiltrating Macrophages Are Associated with Metastasis Suppression in High-Grade Osteosarcoma: A Rationale for Treatment with Macrophage Activating Agents. Clin. Cancer Res. 2011;17:2110–2119. doi: 10.1158/1078-0432.CCR-10-2047. [DOI] [PubMed] [Google Scholar]
- 171.Han R., Yang H., Lu L., Lin L. Tiliroside as a CAXII inhibitor suppresses liver cancer development and modulates E2Fs/Caspase-3 axis. Sci. Rep. 2021;11:8626. doi: 10.1038/s41598-021-88133-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Han R., Yang H., Ling C., Lu L. Tiliroside suppresses triple-negative breast cancer as a multifunctional CAXII inhibitor. Cancer Cell Int. 2022;22:368. doi: 10.1186/s12935-022-02786-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gronowicz G., Secor E.R., Jr., Flynn J.R., Kuhn L.T. Human biofield therapy does not affect tumor size but modulates immune responses in a mouse model for breast cancer. J. Integr. Med. 2016;14:389–399. doi: 10.1016/S2095-4964(16)60275-3. [DOI] [PubMed] [Google Scholar]
- 174.Oliveira C.R., Spindola D.G., Garcia D.M., Erustes A., Bechara A., Palmeira-Dos-Santos C., Smaili S.S., Pereira G.J., Hinsberger A., Viriato E.P., et al. Medicinal properties of Angelica archangelica root extract: Cytotoxicity in breast cancer cells and its protective effects against in vivo tumor development. J. Integr. Med. 2019;17:132–140. doi: 10.1016/j.joim.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 175.Galore-Haskel G., Nemlich Y., Greenberg E., Ashkenazi S., Hakim M., Itzhaki O., Shoshani N., Shapira-Fromer R., Ben-Ami E., Ofek E., et al. A novel immune resistance mechanism of melanoma cells controlled by the ADAR1 enzyme. Oncotarget. 2015;6:28999–29015. doi: 10.18632/oncotarget.4905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Peng X.X., Yu R.Y., Wu X., Wu S.Y., Pi C., Chen Z.H., Zhang X.C., Gao C.Y., Shao Y., Liu L., et al. Correlation of plasma exosomal microRNAs with the efficacy of immunotherapy in EGFR/ALK wild-type advanced non-small cell lung cancer. J. Immunother. Cancer. 2020;8:e000376. doi: 10.1136/jitc-2019-000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Genova C., Coco S., Rossi G., Longo L., Chiorino G., Ostano P., Guana F., Metro G., Baglivo S., Ludovini V., et al. An exosomal miRNA signature as predictor of benefit from immune checkpoint inhibitors in non-small cell lung cancer. Ann. Oncol. 2020;31:S825–S826. doi: 10.1016/j.annonc.2020.08.1591. [DOI] [Google Scholar]
- 178.Huber V., Vallacchi V., Fleming V., Hu X.Y., Cova A., Dugo M., Shahaj E., Sulsenti R., Vergani E., Filipazzi P., et al. Tumor-derived microRNAs induce myeloid suppressor cells and predict immunotherapy resistance in melanoma. J. Clin. Investig. 2018;128:5505–5516. doi: 10.1172/JCI98060. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.