Abstract
Paid sick leave provides workers with paid time-off to receive COVID-19 vaccines and to recover from potential vaccine side effects. We hypothesized that cities with paid sick leave would have higher COVID-19 vaccination coverage and narrower disparities. Using county-level vaccination and paid sick leave data from 37 large US cities in 2021, we estimated the association between city-level paid sick leave policies and vaccination coverage in the working-age population, and repeated the analysis using coverage in the population aged ≥65 as a negative control. We additionally examined associations by neighborhood social vulnerability. Cities with a paid sick leave policy had 17% higher vaccination coverage than cities without a paid sick leave policy. We found stronger associations between paid sick leave and vaccination in the most socially vulnerable neighborhoods compared to the least ones, and no association in the population for the population 65 and under. Paid sick leave policies are associated with higher COVID-19 vaccination coverage and narrower disparities. Increasing access to paid sick leave policies may help increase vaccination and reduce inequities in coverage.
Paid sick leave (PSL) policies provide part or full paid time off from work for caregiving needs or an employee’s own medical needs(1). The United States (US) is one of few wealthy nations lacking a national paid leave program(2). Instead, the US has a patchwork of city, county, and state laws(3) that leave 24% of the civilian workforce without PSL(4). There are wide disparities in access to PSL; low-wage workers and workers of color have substantially lower rates of access to PSL than higher earners and white workers(4).
These gaps in PSL coverage may influence COVID-19 transmission(5). Individuals in frontline occupations, such as service occupations, have the highest rates of exposure to SARS-CoV-2 and the highest morbidity and mortality from COVID-19, while concurrently having the lowest rates of PSL access(4). Among workers who missed work due to being sick or caring for someone with COVID-19, individuals without PSL were disproportionally low-income(6). These same populations with the highest rates of mortality and morbidity from COVID-19 also face inequities in vaccination coverage(7). Inequities in coverage, in large part stem from persistent structural and systemic inequity and racism that contribute to higher COVID-19 rates and present barriers to accessing vaccination(8).
The presence of state PSL policies is associated with lower COVID-19(5) and influenza-like-illness rates(9). PSL mandates increase access to PSL benefits, especially for workers in industries without prior access to PSL(10). Workers are more likely to use paid sick leave when it is more generous(11), and workers are more likely to get vaccines when their employers provide PSL to get vaccinated and recover from side effects(12). PSL may also have a larger impact on more vulnerable neighborhoods, since lower wage workers and more vulnerable populations are less likely to work from home, have less flexible work hours, and are less likely to have employer provided PSL(4). Together, the existing research suggests that the presence of city PSL policies may influence an individual’s ability to get vaccinated, by providing paid time-off to receive vaccines and to recover from potential vaccine side effects, and that city PSL policies may influence city-level vaccination coverage and disparities in vaccinations.
A number of states and cities enacted PSL policies before and during the pandemic(13), and the federal Families First Coronavirus Response Act required certain employers with fewer than 500 employees to provide PSL for COVID-19 related reasons in 2020. However, many of these temporary policies expired by the time vaccines became available, and the federal requirement was replaced with voluntary employer tax credits for providing employees with PSL. In this article we explore the associations of city-level PSL policies with COVID-19 vaccination coverage and disparities in coverage in 37 of the largest US cities in 2021. We hypothesized that vaccination rates would be higher in cities with PSL policies, and that impacts of PSL would be larger in more socially vulnerable neighborhoods.
Methods
Study Setting
We included data from 44 of the largest US cities (see Appendix Exhibit 1(14)). We used cities as our unit of analysis. To explore vaccination coverage disparities, we obtained neighborhood-level vaccination coverage, proxied by zip code tabulation areas (ZCTA), for the 16 cities that had ZCTA-level vaccination data.
Outcome
We used weekly city (county) vaccinations made publicly available by the Centers for Disease Control and Prevention (CDC) and reported from January 1st, 2021 to December 30th, 2021(15). We created three periods, January 1st (federal PSL provisions ended December 31st, 2020) to March 31st(beginning of full 18+ eligibility in all cities), April 1 to October 31st, (beginning of 5-11 eligibility), and November to December 30th. The outcome was full vaccination coverage, defined as the cumulative population share that received two Pfizer/Moderna or one Janssen/Johnson and Johnson vaccine dose by the end of each period. We used data on vaccination coverage for the population aged 18-64 for our main analysis, as this is the working age population, or the population most likely to be employed and therefore impacted by PSL.
For the disparities analysis, we employed ZCTA-level cumulative counts of vaccinated persons compiled by the COVID-19 Health Inequities in Cities dashboard(16) (see Appendix Exhibit 2 for additional outcome information (14)).
Exposure
Our exposure was city PSL policies, or policies which provide an employee with paid-time-off from work to address their own health needs, and the health and well-being of family members. We excluded laws that only applied to specific employee types or sectors such as police officers, teachers, or service workers. We derived the exposure variable from Temple University’s State and City Earned Sick Leave Laws databases(17, 18), with updates through January, 2022. Our main exposure was a binary variable measuring if cities had or did not have a PSL policy during the study period (see Appendix Exhibit 3 for policies by city and additional information on the exposure classification(14)).
Covariates
We included sociodemographic, political, and public health system covariates that may confound the relationship between PSL and COVID-19 vaccination. We obtained county population information from the 1-year 2019 American Community Survey (ACS). To proxy city political lean, we linked county-level 2020 presidential election results data, obtained from the MIT Election Data + Science Lab(19) and to proxy state political lean, we used the governor’s political party(20). We derived a proxy for state and local (county/city) public health capacity from a dataset produced by Kaiser Health News and Associated Press(21). Our proxy measure includes the proportion of total city (or state) 2017 expenditures spent on public health, behavioral health, medical transportation, and other non-hospital health-related spending such as community outpatient clinics and immunization programs, but excludes hospital and Medicaid spending and financial support of other government health programs. We also adjusted for city social vulnerability using the CDC social vulnerability index (SVI)(22) to adjust for potential compositional differences between cities with and without PSL. For the disparities analysis, we calculated ZCTA level SVI and ranked ZCTAs within cities. We also controlled for the following potential confounders: insurance rate, prioritization of people ≥65 years of age before essential workers(23), and three measures from the COVID-19 Vaccine Coverage Index (CVAC)(24). The CVAC measures represent potential compositional (sociodemographic barriers), and contextual (resource constrained health system, and health care accessibility barriers) confounders(see Appendix Exhibit 4 for further description of potential confounders and direction of associations(14)).
Statistical Analysis
To estimate the association between PSL policies and vaccination coverage, we ran a negative binomial model with cumulative number of vaccinations by period and Huber-White robust standard errors clustered at the state-level. We used a stacked dataset with three observations per city (one per period) and adjusted our models by period. We fitted the main model in two ways: (a) using a log link, that allows for an exploration of multiplicative/relative changes in vaccination coverage; and (b) using an identity link, with the Boshuizen and Feskens model, adapted for a negative binomial model(25), to explore additive/absolute changes in vaccination coverage.
We examined the unadjusted association among the population aged 18-64, using PSL vs no PSL as the main exposure, with population 18-64 as the offset. For our main model we a priori selected the minimum set of covariates necessary to eliminate confounding (minimum confounder set(26)), based on the hypothesized causal model shown in DAG 1 (Appendix Exhibit 4(14)). We controlled for vaccination period, city-level political lean (Swing reference), SVI (continuous), city and state public health capacity (continuous), percent insured (continuous), and prioritization of ≥65 ahead of essential workers (binary). If the association between PSL and vaccination is causal(27), we would expect the association to remain, even after adjusting for these potential confounders.
To estimate the associations between PSL and neighborhood vaccination disparities on a relative and absolute scale, we calculated the Relative Index of Inequality (RII) and Slope Index of Inequality (SII)(25) (28). We estimated the RII and SII using a negative binomial model with neighborhood vaccination count as the outcome and included a PSL vs no PSL dummy variable interacted with SVI (continuous). For the first part of the disparities analysis, we explored whether spatial (neighborhood) disparities in vaccinations were wider or narrower in cities with PSL. We then repeated the model using stratified SVI quintiles to assess the variation in the association between PSL and vaccination coverage for different SVI levels; a larger effect estimate in more vulnerable compared to less vulnerable neighborhoods suggests that PSL was more strongly associated with vaccination coverage in these neighborhoods. For both models we adjusted for city-level political lean, city and state health capacity and insured rate, and included total ZCTA population as the offset, Huber White robust standard errors clustered at the city and state-level.
To further test potential alternative explanations to our findings, we conducted a series of sensitivity analyses. First, we estimated the period-specific association between PSL and COVID-19 vaccination coverage by including an interaction between the PSL policy and period in Model 2 (the adjusted model). Second, we employed a negative control (control populations for which the effect of the exposure is assumed to be limited(29)) by repeating the models above but using vaccination coverage for the population aged ≥65. Less than 20% of the population aged ≥65 is employed(30), so we hypothesized that there would be limited impact of PSL on this population. An IRR (exponentiated PSL variable) of 1 or close to 1, represents no association with PSL for the ≥65 population, which would strengthen our confidence that the association between PSL and vaccination in the 18-64 population is not due to measured or unmeasured confounding factors. Third, based on our DAGs (Appendix Exhibit 4 DAG 2(14)), we included two additional models that correspond to slightly different causal models that could also remove confounding (see Appendix Exhibit 6 (14)). Finally, we repeated the main model using a single period (through December 30th, 2021), to account for potential between period clustering, and included standard errors clustered at the city as well as state level.
LIMITATIONS
While our study sequentially rules out alternative non causal explanations for the association between PSL and vaccination coverage, and the associations are consistent across covariate sets and sensitivity analysis, we cannot rule out other unmeasured sources of bias. For example, prior vaccination coverage, local vaccine policies, or primary care use may act as confounders, in addition to mediators, of the relationship between PSL policies and COVID-19 vaccination. Access to care and political lean are also both potential confounders that may be imperfectly controlled in the models, may be subject to exposure misclassification, and may be more salient for working-age adults than retired older adults. Additionally, though our analysis includes longitudinal data, no cities enacted PSL in 2021 ruling out potential quasi-experimental designs comparing vaccination rates before and after enactment. New Mexico has a PSL law that was implemented in July 2022(31), creating opportunities for future analysis using alternative robust study designs.
We measured PSL policies at the city-level and vaccination coverage at the county-level because of data availability. However, all cities but one (Minneapolis) accounted for more than 50 percent of the county population, or the city and county shared the same exposure (both with or without PSL). We repeated the main analysis, dropping Minneapolis, to account for this potential exposure misclassification. It is also possible that there may be some spillover effects, if people who work in a city with/without the policy were vaccinated in a city with the opposite policy. However, the treatment and comparison cities are not geographically proximate, limiting the potential of this bias. Our study did not include any cities that voted Republican in 2020, which may limit generalizability of the findings. Though the analysis measures association between city-level PSL mandates and vaccination, some employers may also provide PSL as an employment benefit, and some cities may have sector specific PSL policies, which may bias our estimates towards the null if there is differential access to sector specific or employer provided PSL in cities without PSL policies.
RESULTS
Our main analysis included 37 cities (35 counties) across 25 states. These cities account for over 66 million individuals or nearly 20% of the total US population. A total of 31,115,517 individuals aged 18-64 were fully vaccinated between January 1st and December 30th, 2021 in our cities. Exhibit 1 displays descriptive statistics for cities with PSL policies, compared to cities without PSL. There were 22 cities with PSL policies and 15 cities without PSL. The average population was substantially larger and average SVI was slightly higher in PSL cities compared to cities without PSL. The median percent vaccinated among the population aged 18-64 was 73.2% and 66.5% in cities with and without PSL, respectively.
Exhibit 1:
Descriptive statistics for 37 large US cities by paid-sick leave status, 2021
| Variable | PSL policy | No PSL Policy |
|---|---|---|
| Number of Cities | 22 | 15 |
| Social Vulnerability Index (SVI): Mean | 0.5 | 0.4 |
| City Political Lean (2020 presidential election) | ||
| Republican | 0 | 0 |
| Democratic | 15 | 9 |
| Mixed | 5 | 6 |
| State Politics (Governor’s Party) | ||
| Republican | 4 | 10 |
| Democratic | 16 | 5 |
| Vaccine Prioritization | ||
| ≥65 prioritized ahead of essential workers | 15 | 12 |
| ≥65 NOT prioritized ahead of essential workers | 5 | 3 |
| Population Size | ||
| Median | 1,627,697 | 945,726 |
| Inter-quartile range | 9,69,713, 2,534,619 | 734,884, 1,087,147 |
| City % Insured | ||
| Median | 93% | 89.90% |
| Inter-quartile range | 91.5, 95.3 | 88.3, 92.4 |
| State % Expenditures on Public Health | ||
| Median | 1.30% | 1.90% |
| Inter-quartile range | 0.4, 2,1 | 1.4, 2.8 |
| City % Expenditures on Public Health | ||
| Median | 3.20% | 1.50% |
| Inter-quartile range | 1.0, 5.2 | 1.1, 3.1 |
| City Resource Constrained Health System | ||
| Median | 0.29 | 0.37 |
| Inter-quartile range | 0.16, 0.37 | 0.28,0.47 |
| State Resource Constrained Health System | ||
| Median | 0.76 | 0.62 |
| Inter-quartile range | 0.33, 0.80 | 0.52, 0.84 |
| City Health Accessibility Barriers | ||
| Median | 0.49 | 0.67 |
| Inter-quartile range | 0.34, 0.54 | 0.49, 0.70 |
| City Sociodemographic Barriers | ||
| Median | 0.38 | 0.37 |
| Inter-quartile range | 0.24,0.52 | 0.31, 0.66 |
| % Vaccinated 18-64 | ||
| Median | 73.20% | 66.50% |
| Inter-quartile range | 67.4, 82.3 | 60.8, 68.7 |
| % Vaccinated ≥65 | ||
| Median | 86.70% | 87.30% |
| Inter-quartile range | 82.4, 91.9 | 92.9, 89.0 |
SOURCE: Author’s analyses of 2019 American Community Survey data, MIT Election Data + Science Lab data, Kaiser Health News and the Associated Press data, CDC Social Vulnerability Index, the COVID-19 US state policy database data, and the COVID-19 Vaccine Coverage Index. We combined cities that share the same county (Long Beach and Los Angeles California, and Phoenix and Mesa Arizona) in analyses.
In Exhibit 2 we plot the percent of the population vaccinated by month in cities with PSL policies vs cities without policies. The figure shows higher percent vaccinated over time in PSL cities than cities without PSL, for the 18-64 population, beginning in February and widening through August. For the population aged ≥65, vaccination coverage was similar in both groups, with slightly higher vaccination in cities without PSL from January to March, and slightly higher vaccination in PSL cities in March through September.
EXHIBIT 2: Monthly vaccination coverage by PSL policy in 37 US cities for the population aged 18-64 and ≥65 during 2021.
Source/notes: SOURCE: Authors’ analysis of CDC vaccination data.
We found a statistically significant association between PSL policies and vaccination coverage for the population aged 18-64. Vaccination coverage was 17% higher (IRR: 1.17; 95% Confidence Interval (CI): 1.09, 1.25), or 4.15 percentage points higher (IRD 4.15%, CI: 2.15, 6.15), in cities with PSL compared to cities without a PSL policy for the population aged 18-64, after adjustment (Exhibit 3, Model 1(14)). This association was consistent, though slightly attenuated, using alternative adjustment sets (Appendix Exhibit 6(14)). The association between PSL and vaccination became stronger over time in the additive model and weaker in the multiplicative one (Appendix Exhibit 5(14)).
Exhibit 3:
Estimates of the association between paid sick leave policies and vaccination rates, comparing cities with and without paid sick leave, 37 US cities, 2021
| Population 18 to 64 | Negative Control Population ≥65 |
|||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Multiplicative model (Incidence Rate Ratio) | ||||
| No Paid Sick Leave | Ref. | Ref. | Ref. | Ref. |
| Paid Sick Leave | 1.14 | 1.17 **** | 1.02 | 1.01 |
| (0.91, 1.41) | (1.09, 1.25) | (0.92, 1.13) | (0.95,1.07) | |
| Additive model (Incidence Rate Difference) | ||||
| No Paid Sick Leave | Ref. | Ref. | Ref. | Ref. |
| Paid Sick Leave | 5.59 | 4.15**** | 0.7 | −0.032 |
| (−7.12, 18.3) | (2.15, 6.15) | (−7.59, 8.99) | (−4.98, 4.92) | |
SOURCE Authors’ analysis of CDC vaccination data. NOTES “Ref.” = reference. Value for reference group is 1 for the incidence rate ratios and 0 for the incidence rate differences. 95% confidence intervals shown below the Incidence Rate Ratios and Differences.
p < 0.1
p < 0.05
p < 0.01
p < 0.001
Model results come from a negative binomial model with city population aged 18-64 as the offset, and Huber-White standard errors clustered at the state level. The negative control includes only the population aged ≥65, with population aged ≥65 as the offset. By exponentiating the coefficient for the PSL variable in the multiplicative model we obtained the incidence rate ratio (IRR) representing the association between vaccination coverage and having a PSL policy compared to having no PSL policy. The coefficient for the PSL variable in the additive model represents the incidence rate difference (IRD) representing the absolute (percentage point) difference in vaccination coverage in cities with a PSL minus cities without a PSL policy. Model 1 is unadjusted; Model 2 adjusts for vaccination period, city-level political lean, SVI, city and state public health capacity, percent insured, and prioritization of ≥65 ahead of essential workers.
We tested alternative explanations for our findings. First, we found no association between PSL and vaccination coverage for the population aged ≥65 (IRR: 1.01,95%CI: 0.95,1.07; IRD:−0.03;95%CI: −4.98, 4.92;Exhibit 3). In a formal test we rejected the null that the association in the two groups were the same (exponentiated 95% CI for the interaction between age group [using age 65+ as the reference] and PSL policy:1.02, 1.24), suggesting the policy associations significantly differed between the working age and 65+ groups. Our sensitivity analysis removing various cities (Indianapolis, Washington DC, smaller BCHC cities) did not substantively impact the estimates or confidence intervals, though the estimate was slightly attenuated after removing the non BCHC cities (Appendix Exhibit 7(14)). The confidence intervals were slightly wider and estimates slightly attenuated in the model addressing potential between period clustering (IRR: 1.13, CI: 1.03, 1.23) but unchanged in the model clustering standard errors on city as well as state.
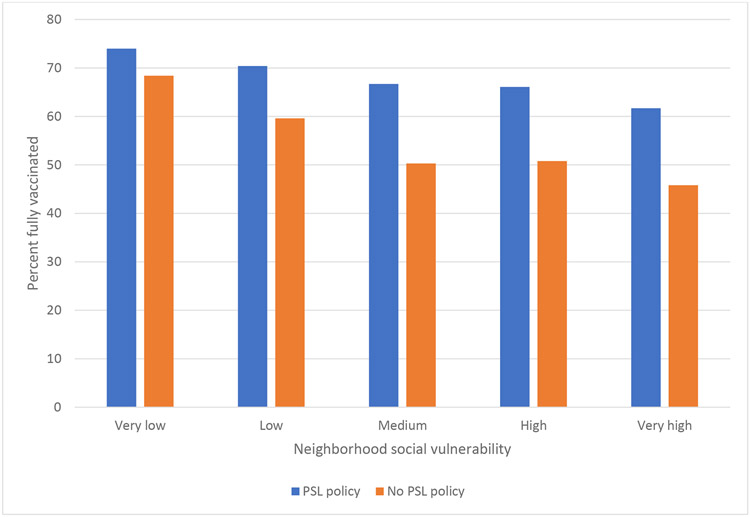
In the analysis examining if disparities in vaccination coverage between neighborhoods were narrower in cities with PSL, we found that after adjustment, cities with PSL had narrower spatial disparities in vaccination. Specifically, in cities with PSL, vaccination coverage in the least vulnerable areas was 29% (RII: 1.29, 95% CI: 1.23, 1.36), or 17.2 percentage points (SII: 17.2, 95% CI: 13.8, 20.5), higher than the most vulnerable areas. In cities without PSL, vaccination coverage in the least vulnerable areas was 72% (RII: 1.72, 95% CI: 1.52, 1.94),or 28.2 percentage points (SII: 28.2, 95% CI:22.0,34.3), higher than the most vulnerable areas(Appendix Exhibit 8(14)). We also found that the association between PSL and vaccination coverage varied by neighborhood vulnerability. Specifically, we found stronger associations between PSL and vaccination coverage in the most vulnerable compared to the least vulnerable neighborhoods (Most vulnerable IRR:1.36, 95%CI:1.28, 1.46; Least vulnerable IRR:1.08, 95%CI: 1.02, 1.16) (Appendix Exhibit 9(14) and found that vaccination coverage was higher across vulnerability levels in cities with PSL (Exhibit 4).
Exhibit 4: Vaccine coverage percent by neighborhood social vulnerability and paid-sick leave status, 37 US cities, 2021.
Source/notes: SOURCE: Authors’ analysis of CDC vaccination data
DISCUSSION
The US lacks universal PSL, leaving nearly a quarter of American workers without access to paid time off for sickness, vaccination, or medical care(32). In our analysis comparing COVID-19 vaccination coverage in cities with and without PSL, we found three key results. First, we found a statistically significant 17% higher vaccination coverage in cities with PSL compared to cities without PSL. This association remained after controlling for various potential confounding sociodemographic characteristics, city and state political factors, health spending and health system vaccine barriers, and vaccine prioritization strategies. This association was robust to different model specifications. Second, we found no association for individuals aged ≥65, who are less likely to be employed and therefore may be less affected by a PSL policy. And third, we found that cities with PSL had narrower disparities in vaccination coverage, and that the association between PSL and vaccination coverage was strongest in the most vulnerable neighborhoods.
PSL policies may be one tool to reduce COVID-19 vaccination barriers and help prevent severe COVID-19, as vaccination dramatically reduces the risk of hospitalization and death from COVID-19(33). Having PSL benefits was associated with a higher likelihood of influenza vaccination(34), and federal PSL coverage reduced COVID-19 case rates(5), but research had not examined the relationship between PSL and COVID-19 vaccination. Lack of PSL may act as a structural barrier to vaccination, and PSL policies may help close gaps in vaccination. For example, early in the vaccine rollout, 64% of unvaccinated Hispanic and 55% of unvaccinated Black adults were worried about missing work because of vaccine side effects(35). And, more than a quarter of employed adults who were not yet ready to get vaccinated said they would be more likely to do so if given paid time off for vaccination and recovery from side effects(35).
We found narrower vaccination disparities in cities with PSL and found the largest benefits of PSL in the most vulnerable neighborhoods. As with other studies(36, 37), we also found decreasing vaccination with increasing vulnerability. These dual findings suggest that PSL may reduce disparities by potentially increasing vaccination in the most vulnerable neighborhoods. There are wide disparities in access to PSL across socio-economic and racial/ethnic groups(4). Among people who missed work due to COVID-19 in 2020, those without PSL were more likely to be low-income(6). This additional benefit of PSL policies is likely because higher income individuals and people living in less vulnerable areas are more likely to already have access to PSL from employers or be able to work from home(4), concentrating benefits among those populations without prior access. Therefore, though PSL is a universal city/state policy, the scale and intensity of impact are proportionate to the level of disadvantage. For this reason, in the US context a PSL mandate could be considered a form of targeted universalism, which has been hypothesized to have the strongest disparities reduction effects(38).
However, even in places with PSL policies, there are often disparities in PSL use. For example, low-wage workers experience additional structural barriers to accessing PSL benefits when they are eligible(39), and part-time and foreign-born workers reported limited knowledge of emergency sick leave availability in 2020(40). While our analysis only examined presence of a PSL policy, future work should examine how features of PSL policies-differences in populations eligible, accrual process, covered employees, permitted uses, and posting and alerting employees to PSL- impact vaccination coverage and inequities.
Many states have declined to enact PSL policies, and even where cities want to provide paid time off to workers and their families, states often preempt them and prohibit them from doing so(3). For example, Austin, San Antonio, and Dallas all passed paid sick leave ordinances, but in 2020, months into the COVID-19 pandemic, the Texas supreme court blocked the ordinances from being enacted(41). While the attempted federal OSHA rule, announced in November 2021, required employers with more than 100 employees to provide time off to get vaccinated and recover from side effects(42), the rule was struck down by the supreme court (43). The 2022 national COVID-19 plan includes continued emphasis on vaccination, along with increasing masking and testing availability and access, and “calls on employers” to provide paid time off to employees(44). However, this plan does not include concrete proposals or policies to enforce this “call”(44). The Build Back Better legislation included four weeks of PSL but appears stalled in Congress, and the Healthy Families Act, paid sick day legislation, was reintroduced in April 2021 and remains in committee in the House of Representatives(45).
Conclusions
The United States continues to lag other wealthy nations in vaccination coverage and does not guarantee universal access to paid leave for all workers. In our analysis of 37 of the largest cities in the US, we found higher vaccine coverage and narrower vaccine disparities in cities with PSL policies. This study suggests that lack of paid sick leave may act as a structural barrier to vaccination uptake, particularly in the most vulnerable neighborhoods. To encourage vaccination, reduce disparities in vaccination, and prevent further morbidity and mortality due to COVID-19, Congress and the president should approve legislation to provide PSL to all workers. Absent federal policies, states should retract their preemptions of local PSL policies, while cities and states without PSL policies should consider enacting their own PSL polices.
Supplementary Material
Funding Information:
This work was partially funded by the Robert Wood Johnson Foundation under grant RWJF 77644 and 78325. UB, PM, and ASM were supported by the Office of the Director of the National Institutes of Health under award number DP5OD26429; ASM was supported by the National Institute of Allergy and Infectious Diseases under award number K01AI168579-01; PM was supported by the Cotswold Postdoctoral Fellowship award number 284134; JR and AS were supported by the National Institute of Mental Health K01 MH116817 and Robert Wood Johnson Foundation award number 77922. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of interest:
The authors declare no conflict of interest
References
- 1.United States, Library of Congress, Paid Family and Medical Leave in the United States Congressional Research Service; by Donovan Sarah A., Washington DC: 2020. R44385. Updated, 13 June, 2022. Available from: https://crsreports.congress.gov/product/pdf/R/R448352 [Google Scholar]
- 2.Khan MS. Paid family leave and children health outcomes in OECD countries. Children Youth Serv Rev.2020;116:10529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pomeranz JL, Silver D, Lieff SA, Pagán JA. State Paid Sick Leave and Paid Sick-Leave Preemption Laws Across 50 US States, 2009–2020. Am J Prev Med.2022;62:688–95. [DOI] [PubMed] [Google Scholar]
- 4.Bureau of Labor Statistics (BLS), National Compensation Survey: Employee Benefits in the United States, Washington DC: 2021. Available from:https://www.bls.gov/ncs/ebs/benefits/2021/home.html [Google Scholar]
- 5.Pichler S, Wen K, Ziebarth NR. COVID-19 Emergency Sick Leave Has Helped Flatten The Curve In The United States. Health Aff(Millwood).2020;39(12):2197–204. [DOI] [PubMed] [Google Scholar]
- 6.Raifman JR, Raderman W, Skinner A, Hamad R. Paid Sick Leave Policies Can Help Keep Businesses Open and Food on Workers' Tables. Health Affairs blog on the internet, 25 October, 2021. Available from:https://www.healthaffairs.org/do/10.1377/hblog20211021.197121/full/ [Google Scholar]
- 7.Barry V, Dasgupta S, Weller DL, Kriss JL, Cadwell BL, Rose C, et al. Patterns in COVID-19 Vaccination Coverage, by Social Vulnerability and Urbanicity–United States, December 14, 2020–May 1, 2021.MMWR Morbid Mortal W.2021;70(22):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bilal U, Mullachery P, Schnake-Mahl A, Rollins H, McCulley E, Kolker J, et al. Heterogeneity in the Spatial Inequities in COVID-19 Vaccination in across 16 Large US Cities. Am J Epidemiol, 2022. 191(9): 1546–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pichler S, Wen K, Ziebarth NR. Positive health externalities of mandating paid sick leave.J Policy Anal Manage.2021;40(3):715–43. [Google Scholar]
- 10.Callison K, Pesko MF. The effect of paid sick leave mandates on coverage, work absences, and presenteeism.J Human Resour.2020:1017–9124R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maclean JC, Pichler S, Ziebarth NR. Mandated sick pay: Coverage, utilization, and welfare effects: NBER; 2020. Available from:https://www.nber.org/papers/w2683213. [Google Scholar]
- 12.Kaiser Family Foundation. Workers Are More Likely to Get a COVID-19 Vaccine When Their Employers Encourage It and Provide Paid Sick Leave, Though Most Workers Don't Want Their Employers to Require It[serial on the internet]: 2021. June 30[cited 2022 Aug 3]:Available from:https://www.kff.org/coronavirus-covid-19/press-release/workers-are-more-likely-to-get-a-covid-19-vaccine-when-their-employers-encourage-it-and-provide-paid-sick-leave-though-most-workers-dont-want-their-employers-to-require-it/ [Google Scholar]
- 13.Peters HEP, Marotta J, Bramhall E. State Preemption of Local Paid Sick Days Ordinances: Lessons from a Pandemic: Urban Institute;29 October, 2020. Available from:https://www.urban.org/research/publication/state-preemption-local-paid-sick-days-ordinances [Google Scholar]
- 14.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 15.Centers for Disease Control and Prevention. COVID-19 vaccinations in the United States, jurisdiction[serial on the internet]:2021[cited Aug 3, 2022]. Available from:https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-Jurisdi/unsk-b7fc [Google Scholar]
- 16.Diez Roux A, Kolker J, Barber S, Bilal U, Mullachery P, Schnake-Mahl A, et al. COVID-19 Health Inequities In Cities Dashboard [internet]. Drexel University, Urban Health Collaborative: 2021. [cited 2022 Aug 3].Available from: https://www.covid-inequities.info/ [Google Scholar]
- 17.Policy Surveillance Program Staff, Earned Sick Leave Laws[internet].In: Law Atlas, editor. Philadelphia: Center for Public Health Law Research, Beasley School of Law, Temple University; 2021. [cited 2022 Aug 3]. Available from:https://lawatlas.org/datasets/earned-sick-leave-laws [Google Scholar]
- 18.Center for Public Health Law Research. 2021. Earned Sick Leave Data[internet].Cityhealth. Available from:https://www.cityhealth.org/our-policy-package/earned-sick-leave/. [Google Scholar]
- 19.MIT Election Data and Science Lab. County Presidential Election Returns 2000–2020. In: Dataverse H, editor; 2018. [cited 2022 Aug 3].Available from: 10.7910/DVN/VOQCHQ [DOI] [Google Scholar]
- 20.Civil Services. United States Governors. Gihub[serial on the internet].2021. [cited 2022 Aug 3]. Available from:https://github.com/CivilServiceUSA/us-governors [Google Scholar]
- 21.Kaiser Health News. Underfunded Under Threat Data: 03, county and local government spending. Github[serial on the internet].2020[cited 2022 Aug 3]. Available from:https://github.com/khnews/2020-underfunded-under-threat-data [Google Scholar]
- 22.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homel Securt Emerg.2011;8(1). [Google Scholar]
- 23.Raifman J, Nocha K, Jones D, Bor J, Lipson S, Jay J, et al. COVID-19 US state policy database[Internet].2020[cited 2022 Aug 3]. Available from:https://statepolicies.com/ [Google Scholar]
- 24.Mishra A, Sutermaster S, Smittenaar P, Stewart N, Sgaier S. COVID-19 Vaccine Coverage Index: Identifying barriers to COVID-19 vaccine uptake across US counties. medRxiv[serial on the internet].2021. June 22[cited 2022 Aug 3].Available from:https://www.medrxiv.org/content/10.1101/2021.06.17.21259116v1 [Google Scholar]
- 25.Boshuizen HC, Feskens EJ. Fitting additive Poisson models. Epidemiol Persp & Innov.2010;7(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tennant PW, Murray EJ, Arnold KF, Berrie L, Fox MP, Gadd SC, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hernán MA. The C-word: scientific euphemisms do not improve causal inference from observational data.AJPH.2018;108(5):616–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moreno-Betancur M, Latouche A, Menvielle G, Kunst AE, Rey G. Relative index of inequality and slope index of inequality: a structured regression framework for estimation.Epidemiology. 2015;26(4):518–27. [DOI] [PubMed] [Google Scholar]
- 29.Lipsitch M, Tchetgen ET, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies.Epidemiology. 2010;21(3):383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bureau of Labor Statistics (BLS). Labor Force Statistics from the Current Population Survey[Internet].2021[cited 2022 Aug 3].Available from:https://www.bls.gov/cps/cpsaat18.html. [Google Scholar]
- 31.Lester NS, Thornton KW. New Mexico Enacts Paid Sick Leave Law. The National Law Review [Internet]. 2021. February 22, 2022. Available from: https://www.natlawreview.com/article/new-mexico-enacts-paid-sick-leave-law. [Google Scholar]
- 32.Bureau of Labor Statistics (BLS). Leave Benefits: Access, Civillian Workers, March 2019 [internet]. US Department of Labor: 2019. Available from:https://www.bls.gov/ncs/ebs/benefits/2019/ownership/civilian/table31a.pdf. [Google Scholar]
- 33.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine.NEJM. 2021;384(5):403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhai Y, Santibanez TA, Kahn KE, Black CL, de Perio MA. Paid sick leave benefits, influenza vaccination, and taking sick days due to influenza-like illness among US workers. Vaccine. 2018;36(48):7316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Artiga S, Hamel L. How Employer Actions Could Facilitate Equity in COVID-19 Vaccinations. Kaiser Family Foundation[serial on the Internet]. 2021. May 17[cited 2022 Aug 3]. Available from:https://www.kff.org/policy-watch/how-employer-actions-could-facilitate-equity-in-covid-19-vaccinations/ [Google Scholar]
- 36.Brown CC, Young SG, Pro GC. COVID-19 vaccination rates vary by community vulnerability: A county-level analysis. Vaccine. 2021;39(1):4245–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hughes MM, Alice Wang, Grossman MK, Pun E, Whiteman A, Deng L, et al. County-Level COVID-19 Vaccination Coverage and Social Vulnerability-United States, December 14, 2020-March 1, 2021.MMWR Morbid Mortal W. 2021;70(12):431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Benach J, Malmusi D, Yasui Y, Martínez JM. A new typology of policies to tackle health inequalities and scenarios of impact based on Rose's population approach.J Epidemiol Comm H. 2013;67(3):286–91. [DOI] [PubMed] [Google Scholar]
- 39.Romig K, Bryant K. A National Paid Leave Program Would Help Workers, Families Should Prioritize Workers of Color and Those with Low Wages: Center on Budget and Policy Priorities[internet]: Center on Budget and Policy Priorities. 2021. April 27[cited 2022 Aug 3].Available from:https://www.cbpp.org/research/economy/a-national-paid-leave-program-would-help-workers-families [Google Scholar]
- 40.Jelliffe E, Pangburn P, Pichler S, Ziebarth NR. Awareness and use of (emergency) sick leave: US employees’ unaddressed sick leave needs in a global pandemic.PNAS. 2021;118(29). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Platoff E Rejecting appeal, Texas Supreme Court blocks Austin's paid sick leave ordinance[serial on the internet]. The Texas Tribune 2020. June 5[cited 2022 Aug 3]. Available from:https://www.texastribune.org/2020/06/05/texas-supreme-court-austin-sick-leave/ [Google Scholar]
- 42.United States Department of Labor (DOL). COVID-19 Healthcare ETS- Frequently Asked Questions[internet]. 2021. Nov 15[cited 2022 Aug 3]; Available from:https://www.osha.gov/coronavirus/ets/faqs. [Google Scholar]
- 43.National Federation of Independent Businesses V Deparment of Labor, Occupational Safety and Health Administration, 595 US; (2022). [Google Scholar]
- 44.The White House. President Biden Announces New Actions to Protect Americans Against the Delta and Omicron Variants as We Battle COVID-19 this Winter[internet].Briefing Room. 2021. Dec 2 [cited 2022 Aug 3]. Available from:https://www.whitehouse.gov/briefing-room/statements-releases/2021/12/02/fact-sheet-president-biden-announces-new-actions-to-protect-americans-against-the-delta-and-omicron-variants-as-we-battle-covid-19-thiswinter/#:~:text=As%20we%20head%20into%20winter,and%20Keep%20Our%20Schools%20Open [Google Scholar]
- 45.Healthy Families Act(2021) S.1195. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.