Abstract
This case series presents four cases of scapholunate interosseous ligament (SLIL) injury. We discuss the process of early recognition and highlight difficulties encountered in current diagnostic and conservative management strategies. The cases profile interdisciplinary management of four scapholunate (SL) injuries that have different clinical presentations and injury mechanisms. Three sport-related SL injuries were managed conservatively by a sport specialist chiropractor and one sport-related case was self-managed. Management strategies included early wrist immobilization, soft tissue manual therapy, low-level laser therapy, proprioceptive and strengthening exercises, and early orthopedic referral. This case series highlights: (1) the spectrum of SL injuries (2) the importance of early specialty referral, (3) the paucity of literature with respect to conservative management of these injuries and (4) the role of manual therapy and rehabilitation professionals as part of the healthcare team in detecting and helping manage these wrist injuries.
Keywords: scapholunate interosseous ligament, scapholunate instability, scapholunate dissociation, conservative management, rehabilitation, chiropractic
Keywords: ligament interosseux scapho-lunaire, instabilité scapho-lunaire, dissociation scapho-lunaire, gestion conservatrice, réadaptation, chiropratique
Abstract
Cette série de cas présente quatre cas de blessures du ligament interosseux scapho-lunaire (LISL). Nous discutons du processus de reconnaissance précoce et soulignons les difficultés rencontrées dans les stratégies actuelles de diagnostic et de gestion conservatrice. Ces cas illustrent la prise en charge interdisciplinaire de quatre lésions du ligament scapho-lunaire (SL) dont les tableaux cliniques et les mécanismes de blessure sont différents. Trois lésions scapho-lunaires liées au sport ont été prises en charge de manière conservatrice par un chiropraticien spécialiste du sport et un cas lié au sport a été auto-soigné. Les stratégies de prise en charge comprenaient une immobilisation précoce du poignet, une thérapie manuelle des tissus mous, une thérapie par laser à faible niveau, des exercices proprioceptifs et de renforcement, et une demande de consultation d’un orthopédiste le plus tôt possible. Cette série de cas met en évidence : (1) le spectre des lésions du ligament scapho-lunaire, (2) l’importance d’une orientation précoce vers un spécialiste, (3) la rareté des documents scientifiques concernant la gestion conservatrice de ces blessures et (4) le rôle des professionnels de la thérapie manuelle et de la réadaptation en tant que membres de l’équipe de soins de santé dans la détection et la gestion de ces blessures du poignet.
Introduction
Injuries to the hand and wrist can lead to physical impairment and disability resulting in a reduction in quality of life in those whose livelihood rely on the use of the upper extremity.1–3 Hand and wrist injuries are the most expensive injury types when considering health care and productivity costs, with dollar values exceeding $740 million USD annually.4,5 The most common wrist injuries include sprains, strains, fractures, and dislocations, all of which may be encountered by primary care providers and rehabilitation specialists in community, athletic, and teaching settings.4,6,7 When sprains occur, ligamentous structures are injured in isolation or in conjunction with bony and muscular structures.7 At the wrist, ligamentous injury may pose diagnostic and management challenges due to the intricate anatomy and biomechanics. Additionally, variations in inter-carpal articulations and the unique morphology of each individual carpal bone contribute to the difficulties in clinical diagnosis.8–12
The stability and biomechanics of the wrist is largely determined by the summative contributions of the components of the wrist ligamentous complex.13,14 The ligaments provide passive restraint to joint motion but are also rich in mechanoreceptors and sensory nerve endings that contribute an important afferent component to a reflexive muscular stabilization that exists around a joint, often referred to as dynamic stability.15,16 Thus, damage to ligamentous structures may not only impair static stability and carpal biomechanics but may also impair the neuromuscular stabilization process that takes place about the wrist during motion.16–18
The scapholunate interosseous ligament
A sensory-rich articulation at the wrist that is susceptible to injury is the scapholunate (SL) joint.19–21 The scaphoid is the most radially located carpal in the proximal carpal row, whereas the lunate lies between the scaphoid and the medially located triquetrum.22 The scaphoid and the lunate are bridged by a C-shaped intrinsic ligament called the scapholunate interosseous ligament (SLIL), which is anatomically divided into 3 components: the dorsal, volar, and membranous parts10 (Figure 1). The dorsal component is the thickest and strongest and contributes the most to mechanical stability, while the volar component is second strongest. Both of these regions are classified as true ligaments. 19,20 The membranous component is atypical as it is composed of fibrocartilage and does not contribute much to mechanical stability.19,20
Figure 1.
The scapholunate interosseous ligament, with the right scaphoid removed. The lunate is denoted by the asterisk. The dorsal (blue), proximal/membranous (yellow), and volar (green) portions of the SLIL are identified. (Image permissions courtesy of Radsource LLC)61
The SLIL has been shown to act as the primary stabilizer for the SL interval, but also contributes to stabilization of the entire carpal unit during motion.10,19–21 Specifically, the SLIL facilitates static positioning of the scaphoid and the lunate at rest while also checking their limits of motion during wrist flexion, extension, radial and ulnar deviation23,24 – motions highly utilized with occupational and athletic tasks7. The SLIL is surrounded superficially by multiple secondary stabilizers that also play a role in carpal biomechanics and wrist stability.25–27 Isolated disruption of these secondary stabilizers has been found to be insufficient to cause frank carpal instability at rest but may be enough to alter carpal kinematics when under load.10,26,27 In contrast, isolated disruption of the SLIL can result in SL instability – the most common and severe of carpal instabilities.10 These anatomical and biomechanical relationships between the stabilizers that cross the SL interval contribute to the diagnostic and management challenges that are encountered with SL injuries.10,23 Diagnosis is also made challenging due to the extensive differential diagnoses that exist for wrist injuries including scaphoid or distal radius fracture, injury to the distal radioulnar joint or triangular fibrocartilage complex (TFCC) or injury to other ligaments that span the radiocarpal and intercarpal articulations.28,29 It is also essential to consider the presence of co-morbid rheumatological conditions such as rheumatoid arthritis, as synovitis associated with the disease can predispose SLIL weakening and may lead to instability.30,31
The spectrum of scapholunate instability
In 1980, Jack Mayfield25 suggested that ligamentous injuries at the wrist lead to a broad continuum of mechanical dysfunction, with SL instability being the first stage of a predictable four stage pattern of perilunar instability (Table 1). In 1993, orthopedic surgeon Kirk Watson32 further classified SL injury as a spectrum itself, and described three stages of SL instability which included: pre-dynamic, dynamic and static instability (Table 2). The development of these two conceptual frameworks is afforded by an understanding of the aforementioned relationships between the stabilizers and biomechanics of the SL joint and other surrounding inter-carpal joints.
Table 1.
Jack Mayfield’s four stages of perilunar instability (SL = scapholunate)
| Stages of perilunar instability | Description |
|---|---|
| Stage I perilunar instability: Scapholunate dissociation | Disruption of the SL ligament with widening of the SL interval. Exacerbated on clenched fist radiograph. |
| Stage II perilunar instability: Perilunate dislocation | Lunate remains normally aligned, and capitate bone is dislocated (typically dorsally). Capitolunate joint is disrupted. This stage may be associated with a scaphoid fracture. |
| Stage III perilunar instability: Mid-carpal dislocation | SL and lunotriquetral ligament disruption, and capitolunate dislocation |
| Stage IV perilunar instability: Lunate dislocation | Stage III plus a ruptured dorsal radiocarpal ligament resulting in volar dislocation of the lunate into the carpal tunnel |
Table 2.
Table adapted from original 1993 paper by Kirk Watson and colleagues. (SL = scapholunate)
| Scapholunate Instability Classification | Diagnostic description |
|---|---|
| Pre-dynamic instability | Rotary subluxation of the scaphoid only identifiable on physical examination (e.g., positive Watson’s scaphoid shift test). No SL widening on static or stress-view wrist radiographs. |
| Dynamic instability | Rotary subluxation identified during physical exam, and SL widening identified on stress radiographs (e.g., clenched fist or ulnar deviation views) or other special studies (e.g., fluoroscopy). |
| Static instability | Rotary subluxation identified during physical exam, and SL widening on static wrist radiographs. Radiographic findings include, foreshortening of the scaphoid, “ring sign”, SL diastasis, overlapping of the scaphoid and the capitate, and increased SL angle on the lateral view. |
Recognition of Watson’s SLIL injury spectrum may further assist the astute clinician in the early detection of such injuries, particularly in those without obvious static radiographic instability. This may subsequently influence the initiation of prompt management. Unfortunately, current literature is lacking with respect to how to best manage SLIL injuries.21,33,34 For example, for acute and complete tears surgery may be required in attempts to restore articular congruency, stability, and biomechanics.21 However, there is insufficient evidence to declare a gold standard procedure as surgical outcomes are inconsistent. 21,33,34 For chronic instabilities, response to surgery is also mixed.21
For incomplete tears without radiographic evidence of instability, non-surgical management may have some benefit.10,35 Case reports have described implementing neuromuscular rehabilitation of the dynamic stabilizers of the wrist that are thought to be “SL joint friendly”.28,35,36 These include the flexor carpi radialis, extensor carpi radialis longus, flexor carpi ulnaris and the abductor pollicis longus and although these muscles’ tendons do not directly attach to the proximal carpal row, they are thought to contribute to normal intercarpal kinematics while maintaining appropriate positioning of the scaphoid and the lunate when the SLIL is incompetent on its own.15,36 Additionally, the use of an arch of motion called the dart-thrower’s motion (DTM, Figure 2a–c) in rehabilitation has been described, as it has been shown to place minimal strain on the SLIL and is a commonly used application in post-surgical SLIL rehabilitation.28,36–39 These approaches have been extrapolated from basic science literature, rehabilitation concepts that exist for other anatomical locations, and biomechanical research of the wrist. However, there is limited evidence to describe the efficacy of these applications. 17,18,40 Also, to our knowledge there are no randomized clinical trials or guidelines to suggest the ideal conservative rehabilitative strategies for SLIL injuries.
Figure 2.
The different positions of the dart thrower’s motion (DTM). The beginning stage starts in a position of radial-extension (a), transitioning through neutral (b) and finishing in a position of ulnar-flexion (c).
While considering the paucity of literature, it is still inevitable that rehabilitation clinicians will attend to patients who have sustained SLIL injuries. For example, primary care providers such as chiropractors or other manual therapy and rehabilitation professionals may be the first health care provider to assess an injury to the wrist, as many therapists work directly with athletes and working-class populations.41–43 As experts in the diagnosis and conservative management for ailments of the musculoskeletal system, these professionals are well positioned to recognize and initiate management for such injuries. We present four cases that highlight the manual therapy and rehabilitation professionals’ role in the diagnosis and initiation of interdisciplinary conservative management for confirmed sport-related injuries to the SLIL.
Case 1 presentation
An 18-year-old elite male international level gymnast presented to a sports specialist chiropractor with a four-day history of right wrist pain. The wrist pain began following vaulting practice during which he planted and twisted hands-first on the vault. This maneuver resulted in loaded wrist extension combined with ulnar deviation. During the moment of injury, the patient reported that he felt “one of his bones pop out of place”. Following this incident, training ceased due to immediate pain and swelling located at the right dorsoradial wrist. The athlete reported that he was unable to perform any degree of active wrist range of motion in all directions immediately following the injury, including an inability to actively hold a cellular device. The patient did not report any subjective neurological symptom descriptors in the upper extremity. Past health history was unremarkable for any underlying connective tissue or rheumatological conditions in the athlete or his immediate family. There was no history of previous injury to the affected right wrist.
Physical examination revealed mild swelling located over the dorsal SL interval of the right wrist with no visible bruising. Active and passive wrist ranges of motion were limited to 25 degrees in flexion and extension (normal ranges: 75 degrees flexion, 70 degrees extension44), 0 degrees ulnar deviation, and 15 degrees radial deviation (normal ranges: 30 degrees ulnar deviation, 20 degrees radial deviation44). Peripheral vascular examination revealed adequate peripheral perfusion and pulses at both radial and ulnar arteries. Give-way 4/5 weakness due to pain was elicited with resisted wrist flexion and extension. There was mild hypoesthesia over the right dorsal wrist in a non-dermatomal distribution. Carpal ballottement (Figure 3) over the scaphoid and lunate recreated the patient’s chief complaint. Palpation of the dorsal and volar distal radioulnar joint was tender. Watson’s scaphoid shift test (Figure 4) was painful but negative for a palpable “clunk” on the right, and negative on the uninjured left side. Triangular fibrocartilage complex provocation tests (Figure 5) were negative bilaterally.
Figure 3.
The scapholunate ballottement test. The examiner uses a pinch grip to stabilize the lunate on the volar and dorsal side of the wrist. While stabilizing, the examiner applies an alternating volar-to-dorsal shearing motion at the adjacent scaphoid to assess the integrity of the SLIL. A positive tests results in excess intercarpal motion, typically in the presence of pain.
Figure 4.
Watson’s scaphoid shift test. The examiner places a volar-to-dorsal pressure on the scaphoid tubercle with their thumb (*) beginning with the affected wrist in ulnar-extension (a). While maintaining pressure, the wrist is brought through the neutral position (b) and into radialflexion (c) where the examiner then removes their thumb pressure. A positive test results in a palpable “clunk” with or without pain, as the scaphoid relocates from a dorsally subluxated position.
Figure 5.
Triangular fibrocartilage complex (TFCC) provocation tests. The triangular fibrocartilage complex compression test (a) is performed with the patient’s affected limb placed on a flat surface with the elbow flexed such that the forearm is perpendicular to the floor. While stabilizing the affected limb proximal to the radiocarpal joint, the examiner grasps the hand and places the wrist in ulnar deviation and applies an axial load with or without a shearing motion. Ulnar sided wrist pain is considered a positive test. The ulnomeniscaltriquetral dorsal glide test (b, c) is performed with the patient’s wrist placed on a flat surface in the pronated position. With the examiner placing a thumb contact on the dorsal ulna (b) a dorsal counter force is applied by contacting the volar pisotriquetral complex using the distal phalanx of the index finger (c). Ulnar sided wrist pain and/or laxity is considered a positive test.
The constellation of clinical findings suggested an acute SLIL injury with a differential diagnosis of a scaphoid fracture or other carpal instability. Wrist radiographs including anterior-posterior, lateral, oblique, and bilateral clenched fist stress views were obtained. The radiographs did not reveal any signs of bony injury or SL interval widening and thus no signs of a dynamic or static SL instability. Despite a negative imaging report, the athlete was referred to a sports medicine physician the same day in hopes of obtaining advanced imaging due to the potential presence of a traumatic pre-dynamic instability. He was also instructed to purchase an over-the-counter wrist support to immobilize the wrist until further investigation was completed. A standard wrist brace with dorsal and volar metal stays was purchased and the patient adhered to the immobilization recommendations.
An MRI was obtained four-days following the initial consult (eight days after injury) and revealed disruption of the volar aspect of the SLIL, however the dorsal component was intact. The surrounding dorsal extrinsic ligament complex revealed enhanced signal, suggestive of mild sprain. At this time, the sports medicine physician instructed the athlete to halt training, continue to immobilize the wrist and to begin conservative therapy while awaiting consultation with a hand and wrist specialist. The conservative management was provided by a sports specialist chiropractor two times per week and began with wrist/forearm isometric strengthening exercises, low-level laser therapy (LLLT) over the dorsal and volar scapholunate interval, and static myofascial therapy to the forearm musculature for symptomatic relief. The athlete was also instructed to temporarily modify his training in such a way as to not to load the wrist in any degree of extension.
Consultation with the hand and wrist specialist occurred three weeks following the MRI. At this time active right wrist range of motion had improved and was near full. The hand and wrist specialist concluded that based on the physical examination, absence of detectable instability on radiographs, but presence of partial SLIL tear on MRI that the athlete continue to be managed conservatively, as a case of pre-dynamic SL instability due to an “acute on chronic” ligament irritation was suspected. Conservative care continued and proprioceptive and strengthening exercises gradually progressed from isometric to isotonic exercises using pain, range of motion and self-reported function as a guide. A graduated exposure and reintegration into sport specific activity that involved loaded wrist extension was permitted with the aid of supportive wrist taping using zinc-oxide athletic tape. The athlete occasionally encountered some aggravation during pommel horse competition, but it did not prevent the athlete from competing. This pain remained dependent on the volume of pommel horse training and competition. The athlete was lost to follow-up as he moved back to his home country and to our knowledge, he is still competing at a high level.
Case 2 presentation
A 23-year-old female chiropractic student presented to a chiropractic teaching clinic in January 2018 with sharp pain and stiffness in her right wrist following a kick-boxing session involving repetitive axial loading of the wrist while using a punching bag and performing repetitive burpee exercises. The wrist pain began one day after the exercise session with a pain rating of 3/10 at rest and 8/10 with movement as measured by the numeric pain rating scale (NPRS). Aggravating movements included wrist flexion and extension with pain located at the dorsoradial wrist. Grasping objects and resisting wrist motion in radial and ulnar deviation also reproduced the chief complaint. There was no subjective report of clicking, locking, or grinding at the time of presentation. Importantly, prior to this kickboxing incident, the patient had been self-managing fluctuating bilateral diffuse wrist discomfort, which was aggravated during activities involving loaded wrist extension, including chiropractic technique practice. Her medical history revealed no known connective tissue or rheumatologic disorders in the patient or her immediate family.
Physical examination revealed minor edema over the dorsal SL interval, with no bruising. Active and passive right wrist ranges of motion were limited due to pain to 10 degrees in radial deviation, and 50 degrees in flexion and extension. All other ranges of motion were maintained. Active and passive combined wrist flexion and radial deviation recreated the chief complaint of dorsoradial wrist pain. Resisted ranges of motion with the wrist in neutral position was graded as 5/5 with no pain, however isolated resisted finger flexion of digits 1 to 3 reproduced dorsal wrist pain on the affected right side. Carpal ballottement over the right SL interval reproduced the patient’s chief complaint. Watson’s scaphoid shift test was positive on the right for pain and a palpable clunk, but negative on the left. Triangular fibrocartilage complex provocation tests were negative bilaterally. Upper extremity neurovascular examination was normal bilaterally. Notably, the Beighton Score for generalized joint hypermobility was scored as 7/9, indicating generalized joint hypermobility (GJH).45 The only components the patient was unable to perform were the forward bend test and right sided thumb apposition, with the latter limited due to pain.
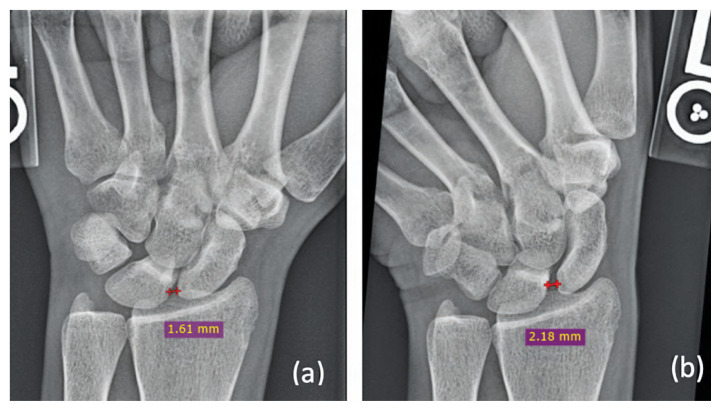
Due to suspicion of a SLIL injury, wrist radiographs were obtained. Figure 6 identifies widening of the SL interval of the right wrist compared to the asymptomatic left wrist. Measurements were obtained during a clenched fist stress view, indicating a dynamic SL instability. The patient was referred to a hand specialist immediately where she was instructed to begin conservative management, as her injury was deemed to be non-surgical. Conservative management included immobilization of the affected wrist for six weeks, followed by wrist flexor/extensor isometric strengthening, LLLT over the dorsal and volar scapholunate interval, and gradual implementation of proprioceptive exercises including the DTM (Figure 2a–c). Treatment was prescribed at a frequency of two times per week for eight weeks following immobilization, including daily at-home exercises, however compliance to the prescribed rehabilitation was inconsistent.
Figure 6.
Case 2: Initial stress radiographs (e.g., clenched fist view) of the bilateral wrists taken in January 2018 demonstrate mild widening of the right scapholunate interval when compared to the asymptomatic left side. A normal SL interval in adults should be <2mm.
In April 2019 (15 months later), the patient presented with worsening right wrist pain and concern about the implications on her future career due to pain while performing chiropractic therapeutic procedures. There was no new injury to trigger this second consultation. During evaluation, dorsal wrist swelling remained consistent with that of the initial consultation. Active and passive wrist flexion and extension remained limited to 60 degrees with pain. Radial and ulnar deviations were now both reduced and painful. Pronation and supination did not reproduce pain. Watson’s scaphoid shift test and SL ballottement remained positive on the right. Grip strength remained full, graded as 5/5, however reproduced pain over the dorsal right wrist. Due to worsening pain and loss of function, the patient was sent for follow-up radiographs (Figure 7), which revealed increased widening of the SL interval during bilateral clenched fist wrist views. Importantly, there was also an increase in the size of the SL interval in the currently asymptomatic left wrist. These findings confirmed a dynamic SL injury on the right. At this point, she was immediately re-referred to the hand and wrist specialist, instructed to immobilize the wrist while waiting for an appointment, and informed to modify her athletic activities and chiropractic training, so as to not place her wrist into positions of forceful extension. Her pain at rest eventually resolved at the end of the six-week immobilization period. The consultation with the hand and wrist specialist occurred in June 2019 where the injury was deemed to still be non-surgical. At this time, she was instructed to monitor her symptoms and continue conservative care, which included the same treatment approach, frequency and duration as previously described. Compliance to the treatment recommendations and at-home exercises remained inconsistent.
Figure 7.
Case 2: Follow-up stress radiographs taken in April 2019 demonstrating progression of the right scapholunate interval widening. Note the additional presence of widening of the scapholunate interval in the newly symptomatic left wrist.
In November 2019 the patient presented for a third time with continued right wrist pain, and new onset left wrist pain. The right wrist was described as sharp pain over the dorsal SL interval and aggravated with the same maneuvers described above. The left wrist pain originated while exercising where she began experiencing feeling a “clunk” during maneuvers that involved axially loaded wrist extension. The patient reported she had been compensating with the left wrist due to the right-sided wrist pain. Watson’s scaphoid shift test on the left was negative but mildly painful. Wrist flexion combined with ulnar deviation reproduced the chief complaint on the left. Triangular fibrocartilage complex provocation tests on the left were positive for ulnar sided wrist pain. The left wrist was subsequently diagnosed with a suspected TFCC injury with a suspicion of a clinically relevant dynamic SL instability.
At this time the patient became compliant with a bi-weekly conservative management strategy for eight weeks. During the eight weeks, isometric wrist strengthening was progressed to isotonic strengthening. Proprioceptive exercises included the use of the DTM that were eventually progressed to DTM while holding light weight (e.g., 1 kilogram). After eight weeks, she continued with at-home wrist strengthening exercises using pain and function as a guide for further progression, while also modifying her athletic and chiropractic activities. In February 2020 she reported a 90% improvement in right wrist discomfort in all ranges of motion except for loaded wrist extension, which still produced sharp dorsal wrist pain. This pain was described as transient and did not persist upon removal of this provocative movement.
In March 2021 the patient returned for a re-evaluation. Her chief complaint remained as wrist pain that was aggravated with loaded wrist extension. Both right and left wrists exhibited a positive Watson’s scaphoid shift test, with pain present only on the right. Palpable clunking was now present during bilateral SL ballottement. As of late 2021, the patient still reported pain when performing certain chiropractic therapeutic procedures, and as such was instructed to continue to use technique modifications that did not produce pain (e.g., using supine thoracic spinal manipulative therapy instead of prone procedures). She is continuing to perform at-home strengthening and proprioceptive exercises and is still occasionally managed conservatively by a sports specialist chiropractor which she describes as being beneficial for the reduction of pain during periods of exacerbation. No further hand specialist consultation has taken place as of this writing.
Case 3 presentation
A 26-year-old male chiropractic student noticed severe left wrist pain the morning after a round of golf. There was no identifiable trauma that occurred during the golf round; however, he described the wrist as being so painful that he “couldn’t even lift his comforter off himself.” There was reported redness and generalized swelling at the dorsoradial wrist that was painful to self-palpation. Suspecting an osseous or ligamentous injury, the patient began to self-manage by applying an over-the-counter rigid brace for two weeks, combined with 500mg of acetaminophen daily for three days. Due to a successful reduction in pain, he continued to self-manage for five weeks which included a combination of gentle active range of motion exercises and isometric strengthening of the wrist in neutral position. He also modified his daily activities by refraining from golf and avoiding all chiropractic training procedures that involved loaded wrist extension.
Approximately seven weeks after the onset of wrist pain, the patient presented to a chiropractic teaching clinic for an examination as there was remaining pain with loaded wrist flexion and extension. History revealed no previous wrist trauma, however mild wrist discomfort had been identified in years past while playing golf and during certain chiropractic training procedures that involved loaded wrist extension. At the time of presentation, chiropractic technique training remained as the chief aggravating factor for his wrist pain. Remaining personal and family health history was unremarkable for any connective tissue or rheumatologic disorders.
Physical examination revealed full pain-free active and passive wrist ranges of motion, that produced a pain-free “click and snap” perceived by the patient at the dorsal wrist. Physical tests including Watson’s scaphoid shift test and TFCC provocation tests were negative bilaterally. Neurovascular examination of the upper extremity was normal bilaterally. Due to suspicion of a golf-related SLIL injury, left wrist radiographs were obtained. SL interval widening was identified on static PA projection (Figure 8a), which subsequently worsened during an ulnar deviation stress view (Figure 8b). The diagnosis of a static SL instability resulted in a prompt referral to a hand and wrist specialist who subsequently ordered an MRI that revealed fluid signal within an intact dorsal SLIL suggestive of previous injury, and the presence of a dorsal ganglion cyst that was continuous with the SL joint (Figure 9a). Although a static instability was identified on radiograph the hand and wrist specialist deemed the findings on advanced imaging to be non-surgical, and the patient was instructed to continue with his current approach of wrist strengthening.
Figure 8.
Figure 8a–b. Case 3: Widening of the scapholunate interval on PA projection (a) that increases with ulnar deviation stress view (b).
Figure 8c–d.
Case 3: The capitolunate angle is normal (c). The scapholunate angle is measured at 70 degrees, the upper limits of normal (d).
Figure 9.
Case 3: Axial PD FS (a) demonstrates high signal within the intact scapholunate ligament (curved arrow) and dorsal ganglion cyst with fluid signal continuous to the scapholunate joint (blue arrow). Sagittal PD (b) through the capitolunate joint demonstrates a normal capitolunate angle of 28.6 degrees (normal = <30 degrees).
The patient continued to self-manage using isometric and eventually isotonic strengthening exercises for the wrist and forearm muscles. Weight bearing activities at the wrist, including push-ups, were slowly implemented using pain as a guide for self-progression. Eighteen months later, the patient reported the ability to still recreate a “click and pop” in the left dorsoradial wrist during maximum wrist flexion and extension, that remained painless. Previously aggravating positions such as loaded wrist extension was no longer bothersome (e.g., push-ups and chiropractic technique training) and the patient was able to return to golf with no limitations. No bracing or taping to provide additional stability was required. He is currently training for golf season one to two times per week in an indoor practice facility with no reported functional limitations or discomfort during or after the activity. He continues to use prophylactic activity modifications during his chiropractic training to limit his exposure to loaded wrist extension (e.g., using a forearm contact instead of loaded wrist extension during side posture lumbar manipulation procedures).
Case 4 presentation
A 34-year-old female yoga instructor and chiropractic student presented to a chiropractic teaching clinic in September 2021 with left dorsoradial wrist pain. The wrist pain began three years prior following pregnancy, where the patient described repetitively supporting herself in an axially loaded wrist position while breast feeding. The wrist pain that developed was significantly worsened during a subsequent increase in physical training and yoga instruction.
Minimal pain was reported at rest, but pain was aggravated with maximal wrist flexion and extension, particularly loaded wrist extension. Examples of provoking positions included the push-up or downward-dog yoga positions and manual therapy training during her chiropractic curricula. Her pain was reported as sharp and rated as 6–7/10 on the NPRS during these activities and was located at the anatomical snuffbox and dorsoradial wrist. A sensation of “clicking and popping” during active pronation and supination of the wrist was reported to be non-painful. Since the onset of wrist pain, the patient described using modified wrist positions during sport and recreational activities, such as performing push-ups on her fists, which was moderately effective in preventing pain. Her past medical history revealed no personal or family history of connective tissue or rheumatologic disorders.
Approximately two months prior to the consultation in September 2021, the patient had seen a different chiropractor for the same wrist complaint. The chiropractor administered LLLT to the dorsal and volar wrist surfaces, and applied intercarpal high velocity, low amplitude adjustments. The patient reported that the adjustments exacerbated her pain.
Physical examination in September 2021 revealed no swelling or bruising. Passive range of motion of the affected wrist was pain-free in all directions, however resisted supination and loaded wrist extension both reproduced the chief complaint. Tenderness was located near the snuffbox and the dorsal SL interval. There was surrounding wrist extensor muscle hypertonicity. Watson’s scaphoid shift test was positive with a painful clunk on the left and negative on the right. Triangular fibrocartilage complex provocation tests were also positive on the affected left wrist.
Due to the suspicion of a SLIL injury, left wrist radiographs were ordered which revealed widening of the SL interval with the ulnar deviation stress view (Figure 10b), but not the static posterior-anterior (PA) view (Figure 10a). An increase in the capitolunate angle was also identified on the lateral view (Figure 10d). These findings led to a diagnosis of a dynamic SL instability and conservative care began immediately.
Figure 10a–b.
Case 4: Radiographic examination of the left wrist demonstrating a normal scapholunate interval in the PA view (a), with an increase in the interval measurement with ulnar deviation stress view (b).
Figure 10c–d.
Case 4: Radiographic examination of the left wrist demonstrates a normal scapholunate angle (c) and a widened capitolunate lunate angle (d).
Conservative management was prescribed one time per week for eight weeks and included manual and instrument assisted soft tissue therapy of the wrist flexors and extensors and LLLT to the dorsal and volar SL interval. However, the focus of management was active rehabilitation that included isometric strengthening of the wrist flexors and extensors and dynamic wrist stabilizers within pain free ranges. During management, the patient reported the greatest pain reduction from the active care portion of the management plan. As wrist function and tolerance to load improved, rehabilitation progressed to include isotonic strengthening and proprioceptive exercises that included external perturbation from the treating practitioner. This included providing an unexpected force to the wrist and hand in different planes of motion to challenge the dynamic stabilizers of the wrist. Additionally, the DTM was incorporated into rehabilitation with the intent of minimizing stress to the SLIL during active strengthening.
By the sixth week of conservative management, the patient reported that her wrist was “feeling great”. She was now able to use 3 lbs weights during the DTM exercises and progressed to perform some weightbearing activities with her wrist approaching 40–50 degrees of extension, including the downward-dog and upward-dog yoga postures. She continued to perform push-ups on clenched fists prophylactically and reported no pain during or after these exercises. She was also instructed to modify some of the therapeutic procedures she is learning during her chiropractic training in attempts to limit maximal wrist extension as this position remained painful. Currently, the patient is continuing with conservative management and gradual progression of her at-home rehabilitative exercises.
Discussion
Scapholunate interosseous ligament injuries can pose both diagnostic and management challenges. The featured cases illustrate the variability in how these injuries may present and the varying degrees of activity limitation that may result.
In studying these four cases, we identified a lack of consistent relationship between severity of pain and extent of ligamentous injury when investigated via stress radiographs and advanced imaging. In cases 1, 2 and 4 none of the patients presented with identifiable instabilities on static radiographs. Not until stress radiographs or advanced imaging was obtained were injuries to the SLIL confirmed. Additionally, these three cases had very different injury mechanisms, initial pain levels and degrees of dysfunction, suggesting that these factors may not be accurate predictors of injury severity on their own.
Case 2 highlights the progression of a dynamic SL instability in a hypermobile individual who was not compliant to initial management recommendations. It is difficult to construe a direct effect of poor compliance or GJH with respect to the outcomes of this case, even considering the well-established relationship between ligamentous laxity in GJH and joint pain at other regions in the body.46,47 Case 4 highlights a successful implementation of an active rehabilitation plan resulting in a meaningful reduction of pain that allowed for a return to modified yoga activity. In this case, the atraumatic onset of wrist pain was in close temporal proximity to pregnancy. It is well-known that pregnancy can induce ligamentous laxity due to increases in the levels of certain hormones such as relaxin and progesterone.48,49 Musculoskeletal disorders, including those of the hand and wrist, are common during pregnancy49 and there are case reports to suggest pregnancy-induced laxity of the SLIL can present as a dynamic SL instability50. These concepts raise suspicion as to the potential contribution of pregnancy-induced hormonal changes to the eventual repetitive use mechanism of SLIL injury that was observed in Case 4. In the context of Cases 2 and 4, further studies investigating the potential relationships between GJH or pregnancy-induced ligamentous laxity and injury to the SLIL should be conducted. Establishing a better understanding of these potential relationships may be particularly important when there is suspicion of an SLIL injury in the absence of an identifiable acute trauma.
Case 3 highlights a successful implementation of immobilization with respect to pain reduction. Multiple sources suggest the use of wrist immobilization after acute SLIL injury10,21, however empirical evidence is lacking specific criteria with respect to the ideal duration and type of brace to use. It is difficult to determine if the early bracing strategy improved the prognosis for the individual or helped facilitate a full return to sport, however, early suspicion of injury permitted immediate intervention and early resolution of pain, which ultimately allowed for progression of self-prescribed isometric and isotonic wrist strengthening exercises.
Case 1 also responded favourably to partial wrist immobilization. Supportive athletic wrist taping was used to prevent provocative ranges of motion during gymnastics and served as an exogenous form of stabilization, although in a more dynamic environment when compared to Case 3. Importantly, taping the wrist permitted the athlete in Case 1 to tolerate load with the wrist in an extended position that was otherwise too painful to perform without the tape. This ultimately assisted the athlete in returning to sport.
In addition to providing an extrinsic support to the wrist, other physiological mechanisms may explain the response to taping that we observed. Proposed mechanisms include but are not limited to: improvement of local strength and proprioception51 and local pain inhibition of the injured joint that was taped52,53. It is important to note that these mechanisms remain controversial and to our knowledge have not been demonstrated at the SL joint, specifically. Due to limited evidence supporting rigid bracing and athletic taping for SLIL injuries, we recommend that efficacy studies be performed to determine the best approach and timing for wrist immobilization following SLIL injury. We also recommend that studies continue to investigate the mechanisms of action for various types of taping which may inform our clinical applications for both athletes and non-athletes.
Within our series, three cases included early referral to hand and wrist specialists which facilitated advanced imaging, confirmed the diagnosis, and determined that the cases were non-surgical, despite the presence of ligamentous injury. Without interdisciplinary collaboration in the diagnostic process, there may have been greater uncertainty surrounding the most appropriate care. The recommendations from the hand and wrist specialists to proceed with conservative management may have been due to the lack of consensus on gold standard surgical procedures to treat more subtle instabilities, combined with the mixed outcomes and overall unpredictable prognosis found within the existing surgical literature.21,33 Additionally, surgery is typically only considered in the presence of static SL instability or significant arthritis (e.g., scapholunate advanced collapse [SLAC]), combined with significant pain and disability.21,33 Thus, the recommendation for non-invasive methods of management including immobilization for a period of six to eight weeks with gradual implementation of range of motion, strength, and proprioceptive exercises, seems reasonable.
Additionally, implementing LLLT seemed appropriate in our cases as it has been shown to be safe54,55 and there is preliminary evidence to suggest mild pain reduction in various disorders of the elbow, wrist, and hand56,57. The mechanisms of action for LLLT include changes in local tissue mitochondrial metabolism, which in turn may have a positive influence on local blood flow, clearance of metabolic by-products, and reduction of proinflammatory neuropeptides that accumulate at the location of injury. 58,59
We recognize that certain conservative management recommendations were made in the absence of high quality literature addressing the efficacy of these interventions for SLIL injuries10, emphasizing the need for future research to investigate the efficacy of these applications for SLIL injuries, specifically.
Case 4 highlights a successful implementation of active rehabilitation using concepts of motor control15,18, conscious proprioception15,17,18, and biomechanics10,23. We extrapolated findings from kinematic and orthopedic literature which led to the use of the DTM during rehabilitation to reduce SLIL stress while maintaining ranges of motion and strengthening dynamic stabilizers.15,37–39 Kinematic studies have identified that the arch of motion from wrist radial-extension to ulnar-flexion (e.g., like that of throwing a dart), places the least amount of strain on the SLIL.37–39 This movement is the only exception to the complex intercarpal motion that occurs during all wrist movement as the DTM results in null movement of the proximal carpal row, with nearly all motion taking place at the mid-carpal joint.37–39 It is important to recognize this inherent stability in the proximal carpal row during the DTM, as multiple every-day activities and sporting tasks require this arch of motion. For example, activities such as hammering a nail, pouring a pitcher of water, throwing a javelin, and holding a golf club all require combinations of radial-extension and ulnar-flexion.37,39 Since the identification of this kinematic relationship, dart-thrower’s orthoses have been prescribed post-surgically to reduce strain at the repaired SLIL while permitting safe and early rehabilitation.37,39 Actively using this arch of motion also utilizes musculature that is thought to be “SL joint friendly”.15,36 Thus, utilizing this motion in conservative therapies in the absence of surgery may be an avenue to implement greater degrees of motion without placing the SLIL at risk of further injury. Extrapolating what exists within the surgical, biomechanical, and basic science literature was necessary during our approach to the conservative management of the four cases presented, as empirical evidence remains limited.
It is also important to recognize that the individuals included in this series had active lifestyles that required extensive use of their hands and upper extremity in sport and their healthcare training. Considering this, we provided advice to modify certain activities in attempts to limit exposure to aggravating wrist positions. This advice was a staple of our conservative management, and in collaboration with each patient, we were able to identify reasonable ways to modify their activities. Cases 2, 3 and 4 provide examples of successful activity modification that was implemented during their chiropractic training to avoid positions of loaded wrist extension. An example of these modifications includes using supine thoracic spinal manipulative procedures instead of prone procedures. The patient in Case 3 reported that he continues to use this strategy in a prophylactic manner to avoid further injury. We also assisted Case 4 in identifying ways to perform certain yoga positions to facilitate a return to instruction. For example, substituting positions that typically involved extended wrists and fingers with closed fists with the wrists in a neutral position (e.g., during downward and upward dog postures).
The role of manual therapy and rehabilitation professionals
As manual therapists we may often consider our handson therapeutic skills as our largest asset. However, when presented with wrist pain we must consider the underlying etiology and question whether joint manipulation is the best strategy to treat a given condition. A negative response to carpal manipulation was reported in Case 4, however we do not have enough information to draw conclusions as to why. One hypothesis includes the challenge of applying therapeutic forces across the extremely small articulations of the wrist without influencing other nearby structures. More importantly, it is already understood that the presence of an identifiable instability is a contraindication to manipulation at other regions in the body.60 Thus, before attempting to manipulate joints at the wrist it may be prudent to ask ourselves if an individual who is presenting with wrist pain is suffering from “just a sprain”, or if there may be a mild but clinically relevant instability that warrants further investigation?2 If this is the case, it is reasonable to believe that facilitating motion beyond a joint’s physiological end range may not be favourable in an already hypermobile or dynamically unstable joint. Therefore, it is our opinion that having a better understanding of carpal biomechanics is essential. This may decrease the likelihood of performing procedures that may not be helpful for a given condition, while also helping inform our clinical decision-making during the diagnostic process, as illustrated in the cases above.
Conclusion
In conclusion, this case series highlights several important considerations and clinical decisions with respect to the recognition and management of SLIL injuries including the value of stress radiographs and advanced imaging to identify subtle injuries to the SLIL. As members of the healthcare community, manual therapists and rehabilitation professionals must acknowledge when collaboration is necessary to aid in accurate diagnosis while keeping patient-centeredness in mind. As identified in the cases presented, there may be value in implementing conservative management strategies including bracing/immobilization, activity modification, and a rehabilitation program that considers the stability and biomechanics of the SL articulation. It must be emphasized that this was permitted by extrapolating and synthesizing information from basic science, biomechanical and orthopedic literature, suggesting that more research in controlled environments is necessary to be more confident in our conservative approaches. Future investigations should aim to identify the appropriate frequency, duration and type of bracing and exercise that is most effective for these injuries and how these parameters may change with differing severities of injury.
Acknowledgements
The authors of this paper would like to acknowledge Dr. Chris deGraauw for his assistance in reviewing our manuscript for content and readability. The lead author would also like to acknowledge the Foundation of the Royal College of Chiropractic Sports Sciences (Canada) for the formal recognition of this case series as a contribution to sports chiropractic literature.
Footnotes
The authors have no disclaimers, competing interests, funding, or sources of support to report in preparation of this manuscript. All patients included in this case series provided written consent for case publication.
References
- 1.Capkin S, Cavit A, Yilmaz K, Erdogan E, Kaleli T. Associations between initial injury severity in acute hand, wrist or forearm injuries and disability ratings and time to return to work. Ulus Travma Acil Cerrahi Derg. 2020;26(3):453–461. doi: 10.14744/tjtes.2019.40524. [DOI] [PubMed] [Google Scholar]
- 2.Jones W. Beware the sprained wrist. J Bone Joint Surg Br. 1988;70B:293–297. doi: 10.1302/0301-620X.70B2.3346308. [DOI] [PubMed] [Google Scholar]
- 3.MacIntyre N, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29(2):136–145. doi: 10.1016/j.jht.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Gil JA, Weiss A-PC. The weekend warrior: common hand and wrist injuries in athletes. R I Med. 2020:49–53. [PubMed] [Google Scholar]
- 5.de Putter CE, Selles RW, Polinder S, Panneman MJ, Hovius SE, van Beeck EF. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94(9):e56. doi: 10.2106/JBJS.K.00561. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson R, Riley ND, Wijendra A, Thurley N, Carr AJ, Bjf D. Wrist pain: a systematic review of prevalence and risk factors-what is the role of occupation and activity? BMC Musculoskelet Disord. 2019;20(1):542. doi: 10.1186/s12891-019-2902-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pulos N, Kakar S. Hand and wrist injuries: common problems and solutions. Clin Sports Med. 2018;37(2):217–243. doi: 10.1016/j.csm.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Taleisnik J. The ligaments of the wrist. J Hand Surg. 1976;1(2):110–118. doi: 10.1016/s0363-5023(76)80004-4. [DOI] [PubMed] [Google Scholar]
- 9.Lau S, Swarna SS, Tamvakopoulos GS. Scapholunate dissociation: an overview of the clinical entity and current treatment options. Eur J Orthop Surg Traumatol. 2009;19(6):377–385. [Google Scholar]
- 10.Kitay A, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2012;37(10):2175–2196. doi: 10.1016/j.jhsa.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 11.Crisco JJ, Coburn JC, Moore DC, Upal MA. Carpal bone size and scaling in men versus in women. J Hand Surg Am. 2005;30(1):35–42. doi: 10.1016/j.jhsa.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Prosser R, Harvey L, LaStayo P, Hargreaves I, Scougall P, Herbert RD. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother. 2011;57(4):247–253. doi: 10.1016/S1836-9553(11)70055-8. [DOI] [PubMed] [Google Scholar]
- 13.MG-E Kinetic analysis of carpal stability during grip. Hand Clin. 1997;13(1):151–158. [PubMed] [Google Scholar]
- 14.Patterson RM, Yazaki N, Andersen CR, SFV Prediction of ligament length and carpal diastasis during wrist flexion-extension and after simulated scapholunate instability. J Hand Surg Am. 2013;38(3):509–518. doi: 10.1016/j.jhsa.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salva-Coll G, Garcia-Elias M, Hagert E. Scapholunate instability: proprioception and neuromuscular control. J Wrist Surg. 2013;2(2):136–140. doi: 10.1055/s-0033-1341960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mataliotakis G, Doukas M, Kostas I, Lykissas M, Batistatou A, Beris A. Sensory innervation of the subregions of the scapholunate interosseous ligament in relation to their structural composition. J Hand Surg Am. 2009;34(8):1413–1421. doi: 10.1016/j.jhsa.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Wolff AL, Wolfe SW. Rehabilitation for scapholunate injury: application of scientific and clinical evidence to practice. J Hand Ther. 2016;29(2):146–153. doi: 10.1016/j.jht.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Karagiannopoulos C, Michlovitz S. Rehabilitation strategies for wrist sensorimotor control impairment: from theory to practice. J Hand Ther. 2016;29(2):154–165. doi: 10.1016/j.jht.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg. 1996;21A:170–178. doi: 10.1016/S0363-5023(96)80096-7. [DOI] [PubMed] [Google Scholar]
- 20.Berger RA, Imeada T, Berglund L, An K-N. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg. 1999;24A:953–962. doi: 10.1053/jhsu.1999.0953. [DOI] [PubMed] [Google Scholar]
- 21.Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017;2(9):382–393. doi: 10.1302/2058-5241.2.170016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eschweiler J, Li J, Quack V, Rath B, Baroncini A, Hildebrand F, et al. Anatomy, biomechanics, and loads of the wrist joint. Life (Basel) 2022;12(2) doi: 10.3390/life12020188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajan PV, Day CS. Scapholunate interosseous ligament anatomy and biomechanics. J Hand Surg Am. 2015;40(8):1692–1702. doi: 10.1016/j.jhsa.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 24.Marras WS, Schoenmarklin RW. Wrist motions in industry. Ergonomics. 1993;36(4):341–351. doi: 10.1080/00140139308967891. [DOI] [PubMed] [Google Scholar]
- 25.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunate instability. J Hand Surg. 1980;5(3):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 26.Short WH, Werner FW, Green JK, Masaoka S. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: Part II. J Hand Surg Am. 2005;30(1):24–34. doi: 10.1016/j.jhsa.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 27.Short WH, Werner FW, Green JK, Sutton LG, Brutus JP. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part III. J Hand Surg Am. 2007;32(3):297–309. doi: 10.1016/j.jhsa.2006.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feehan L, Fraser T. Early controlled mobilization using dart-throwing motion with a twist for the conservative management of an intra-articular distal radius fracture and scapholunate ligament injury: a case report. J Hand Ther. 2016;29(2):191–198. doi: 10.1016/j.jht.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 29.Young D, Papp S, Giachino A. Physical examination of the wrist. Hand Clin. 2010;26(1):21–36. doi: 10.1016/j.hcl.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Flury M, Herren D, Simmen B. Rheumatoid arthritis of the wrist classification related to the natural course. Clin Orthop Relat Res. 1999;366:72–77. [PubMed] [Google Scholar]
- 31.Kushner D, Braunstein E, Buckwalter K, Krohn K, White H. Carpal instability in rheumatoid arthritis. Can Assoc Radiol J. 1993;44(4):291–295. [PubMed] [Google Scholar]
- 32.Watson H, Ottoni I, Pitts E, Handal A. Rotary subluxation of the scaphoid: a spectrum of instability. J Hand Surg. 1993;18B:62–64. doi: 10.1016/0266-7681(93)90199-p. [DOI] [PubMed] [Google Scholar]
- 33.Konopka G, Chim H. Optimal management of scapholunate ligament injuries. Orthop Res Rev. 2018;10:41–54. doi: 10.2147/ORR.S129620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elzinga K, Kamnerdnakta S, Chung K. Concepts and artistry in the treatment of scapholunate ligament injuries. Plast Reconstr Surg. 2018;142(3):322e–333e. doi: 10.1097/PRS.0000000000004690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hessam S, Abbas R, Kasra M. Injury to the scapholunate ligament in sport “a case report”. WJSS. 2012;7(3):154–159. [Google Scholar]
- 36.Kamal R, Moore W, Kakar S. Team approach: management of scapholunate instability. JBJS Rev. 2019;7(2):e2. doi: 10.2106/JBJS.RVW.18.00021. [DOI] [PubMed] [Google Scholar]
- 37.Moritomo H, Apergis EP, Garcia-Elias M, Werner FW, Wolfe SW. International federation of societies for surgery of the hand 2013 committee’s report on wrist dart-throwing motion. J Hand Surg Am. 2014;39(7):1433–1439. doi: 10.1016/j.jhsa.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 38.Werner FW, Green JK, Short WH, Masaoka S. Scaphoid and lunate motion during a wrist dart throw motion. J Hand Surg Am. 2004;29(3):418–422. doi: 10.1016/j.jhsa.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 39.Crisco JJ, Coburn JC, Moore DC, Akelman E, Weiss A-PC, Wolfe SW. In vivo radiocarpal kinematics and the dart thrower’s motion. J Bone Joint Surg. 2005;87-A(8):2729–2739. doi: 10.2106/JBJS.D.03058. [DOI] [PubMed] [Google Scholar]
- 40.Aman JE, Elangovan N, Yeh IL, Konczak J. The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci. 2014;8:1075. doi: 10.3389/fnhum.2014.01075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Konckzak CR. Chiropractic utilization in BMX athletes at the UCI World Championships: a retrospective study. JCCA. 2010;54(4):250–256. [PMC free article] [PubMed] [Google Scholar]
- 42.Nook DD, Nook EC, Nook BC. Utilization of chiropractic care at the World Games 2013. J Manipulative Physiol Ther. 2016;39(9):693–704. doi: 10.1016/j.jmpt.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Theberge N. The integration of chiropractors into healthcare teams: a case study from sport medicine. Sociol Health Illn. 2008;30(1):19–34. doi: 10.1111/j.1467-9566.2007.01026.x. [DOI] [PubMed] [Google Scholar]
- 44.American Academy of Orthopaedic Surgeons. Joint motion: method of measuring and recording. Chicago, IL: American Academy of Orthopaedic Surgeons; 1965. [Google Scholar]
- 45.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011;19(8):463–471. doi: 10.5435/00124635-201108000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Grahame R, Keer R, Hakim A. Hypermobility, fibromyalgia and chronic pain: Elsevier Health Sciences. 2010 [Google Scholar]
- 48.Cherni Y, Desseauve D, Decatoire A, Veit-Rubinc N, Begon M, Pierre F, et al. Evaluation of ligament laxity during pregnancy. J Gynecol Obstet Hum Reprod. 2019;48(5):351–357. doi: 10.1016/j.jogoh.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 49.Afshar A, Tabrizi A. Pregnancy-related Hand and Wrist Problems. Arch Bone Jt Surg. 2021;9(3):345–349. doi: 10.22038/abjs.2020.50995.2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miller EK, Tanaka MJ, LaPorte DM, Humbyrd CJ. Pregnancy-related ligamentous laxity mimicking dynamic scapholunate instability: a case report. JBJS Case Connect. 2017;7(3):e54. doi: 10.2106/JBJS.CC.16.00268. [DOI] [PubMed] [Google Scholar]
- 51.Liu K, Qian J, Gao Q, Ruan B. Effects of kinesio taping of the knee on proprioception, balance, and functional performance in patients with anterior cruciate ligament rupture: a retrospective case series. Medicine (Baltimore) 2019;98(48):e17956. doi: 10.1097/MD.0000000000017956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu K, Yin L, Ma Z, Yu B, Ma Y, Huang L. Effect of different kinesio taping interventions on the local thresholds of current perception and pressure pain in healthy adults. Front Physiol. 2020;11:596159. doi: 10.3389/fphys.2020.596159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu WT, Hong CZ, Chou LW. The kinesio taping method for myofascial pain control. Evid Based Complement Alternat Med. 2015;2015:950519. doi: 10.1155/2015/950519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Sonis ST, Elad S, et al. Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 1: mechanisms of action, dosimetric, and safety considerations. Support Care Cancer. 2016;24(6):2781–2792. doi: 10.1007/s00520-016-3152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bensadoun RJ, Epstein JB, Nair RG, Barasch A, Raber-Durlacher JE, Migliorati C, et al. Safety and efficacy of photobiomodulation therapy in oncology: a systematic review. Cancer Med. 2020;9(22):8279–8300. doi: 10.1002/cam4.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Okuni I, Ushigome N, Harada T, Ohshiro T, Musya Y, Sekiguchi M. Low level laser therapy (LLLT) for chronic joint pain of the elbow, wrist and fingers. Laser Ther. 2012;21(1):33–37. doi: 10.5978/islsm.12-OR-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rayegani SM, Moradi-Joo M, Raeissadat SA, Bahrami MH, Seyed-Nezhad M, Heidari S. Effectiveness of low-level laser therapy compared to ultrasound in patients with carpal tunnel syndrome: a systematic review and meta-analysis. J Lasers Med Sci. 2019;10(Suppl 1):S82–S89. doi: 10.15171/jlms.2019.S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Farivar S, Malekshahabi T, Shiari R. Biological effects of low level laser therapy. Lasers Med Sci. 2014;5(2):58–62. [PMC free article] [PubMed] [Google Scholar]
- 60.Puentedura EJ, March J, Anders J, Perez A, Landers MR, Wallmann HW, et al. Safety of cervical spine manipulation: are adverse events preventable and are manipulations being performed appropriately? a review of 134 case reports. J Man Manip Ther. 2012;20(2):66–74. doi: 10.1179/2042618611Y.0000000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bodor D. SLL tear and DISI deformity. Brentwood, Tennessee: Radsource LLC; 2009. [cited 2022 May 11]. Available from: https://radsource.us/sll-tear-and-disi-deformity/ [Google Scholar]