Abstract
Objective:
To test the feasibility and preliminary efficacy of a couple-based communication intervention for advanced GI cancer delivered via videoconference.
Methods:
32 couples were randomly assigned to either couples communication skills training (CCST) or an education comparison intervention, both delivered via videoconference. Participation was limited to couples who reported communication difficulties at screening. Patients and partners completed measures of relationship functioning and individual functioning at baseline and post-intervention.
Results:
88% of randomized dyads completed all six sessions and reported high levels of satisfaction with the intervention. Between-group effect sizes suggested that the CCST intervention led to improvements in relationship satisfaction for patients and partners, and to improvements in intimacy and communication for patients.
Conclusions:
A couples-based communication intervention delivered via videoconference is feasible and acceptable in the context of advanced cancer. Preliminary findings suggest that the intervention shows promise in contributing to enhanced relationship functioning.
Keywords: gastrointestinal cancer, communication, couples, psychosocial intervention, videoconference
Background
There is increasing recognition of the impact of cancer not only on patients but on their spouses/intimate partners and on the patient-partner relationship. Accumulating evidence suggests that couples’ ability to communicate effectively plays a major role in the psychological adjustment of both patients and partners, the quality of their relationship, and their ability to cope with the effects of cancer and its treatment.[1] Specifically, patients and partners who have difficulty talking about their cancer-related concerns report higher levels of individual psychological distress and poorer relationship functioning. [2] This has been found among couples coping with both early stage [3, 4] and advanced disease [5, 6].
Many couples experience difficulty communicating about cancer-related issues, even in the context of satisfying relationships.[7, 8] This may occur for multiple reasons: Patients may be overwhelmed with medical decisions, treatment side effects, and emotional distress. Partners may also be overwhelmed as they face multiple and competing demands, including providing support to the patient and dealing with their own fears and emotions.[9] Second, both patients and partners often have the misconception that it is harmful for patients to discuss their cancer or any negative aspects of the situation. Some partners believe they need to cheer the patient up and should always be optimistic.[10] Finally, patients and partners often avoid discussing sensitive issues such as sexual functioning or disease progression.[5, 11]
The impact of cancer on both members of the couple and on their relationship has led to increasing interest in couple-based interventions. A recent review and meta-analysis of couple-based interventions to improve patient and partner adaptation to cancer identified 23 studies and found that the interventions had small but beneficial effects on patient and partner individual and relationship functioning.[14] However, most interventions tested multimodal treatment packages, of which communication skills training was but one component. Thus, it is difficult if not impossible to evaluate the unique effects of training couples in communication skills.
In addition, most studies focused on patients with early stage disease. It may be particularly important to target interventions to couples facing advanced cancer for several reasons. First, patients with advanced disease are often coping with higher levels of symptom burden and disability which can impact their partners and their relationships.[6][13] These couples are also dealing with anticipatory grief and struggling to make meaning of their lives and relationships. In addition, research indicates that attending to family relationships is vitally important to patients and their family members at end of life.[12] Thus, couple-based interventions may be particularly relevant during this time.
Recently, we conducted a study testing the efficacy of a partner-assisted emotional disclosure intervention among 130 patients with gastrointestinal (GI) cancer (88% with advanced disease) and their spouses.[15, 16] The intervention trained couples in communication skills to help patients disclose cancer-related feelings and concerns and partners to listen supportively. Compared to an education comparison condition, the intervention led to significant improvements in relationship quality and intimacy in couples in which the patient reported high baseline levels of holding back (e.g., active inhibition of expression of cancer-related concerns ones’ partner).
While promising, this study had a number of limitations. First, the intervention’s application of communication skills was narrow in focus (i.e., patient disclosure to partner without opportunities for the partner to disclose). Second, we did not screen participants for inclusion based on communication difficulties. There is increasing recognition that psychosocial interventions for cancer, including couple-based interventions, should be targeted to those at risk for poor outcomes without intervention.[17, 18] Finally, like most couple-based intervention studies, we relied on an in-person treatment delivery format. For couples facing advanced cancer in particular, there are numerous barriers to attending face-to-face intervention sessions (e.g., problems with mobility, fatigue, and costs of travel). Thus, it is critical to develop couple-based interventions that are easily accessible.
Videoconferencing is increasingly utilized in health care (e.g.,[19, 20]), including for delivery of mental health services, and is associated with high levels of patient satisfaction and efficacy.[19] However, to date there have been no studies of videoconference-based interventions for couples facing advanced cancer. It is important to conduct pilot feasibility studies in order to understand and address technical challenges posed by videoconferencing, and to assess the preliminary efficacy of interventions delivered in this manner.
We therefore conducted a pilot feasibility study of a Couples Communication Skills Training (CCST) intervention delivered via videoconference for patients with advanced GI cancer and their partners. The intervention focused solely on communication skills training and explicitly encouraged both patients and partners to share their concerns with each other. We targeted couples who reported difficulties communicating about cancer-related concerns, a subgroup that our previous research identified to be at risk for poor adjustment. [5, 16] All couples in the study received tablet computers with cellular data plans to use during the study for videoconferencing.
There were two aims: (1) To determine the feasibility and acceptability of the CCST intervention; and (2) to provide preliminary data on the effects of CCST compared to an educational comparison condition on measures of couples’ relationship and individual functioning.
Methods
Participants
Patients were eligible if they were: (a) married or in a committed intimate relationship (whether or not they were cohabitating), (b) diagnosed with Stage 3 or 4 GI cancer, and (c) had a life expectancy of ≥ 6 months as estimated by their treating oncologist. Both members of the couple had to be age ≥ 18 and able to speak and read English. Patients with a diagnosis of active psychosis or dementia were excluded.
Because we wanted to focus on couples with difficulty communicating about cancer-related concerns, we administered the Holding Back subscale of the Emotional Disclosure Scale [5, 7] which measures active inhibition of expression of cancer-related concerns to one’s partner. It has been used in numerous studies of patients with cancer and demonstrated excellent psychometric properties [5, 16, 21, 22]. The range is 0 to 4, with reported mean scores ranging from 0.82 [16] to 1.23 [5]. Higher scores have been consistently associated with poorer psychological and relationship functioning.[5, 7, 21, 22] The study coordinator administered the measure by telephone. Typically, the patient was contacted and screened first; if s/he scored ≥ 1.0 (the median score in our previous study with this population [16]), the couple was invited to participate. If the patient scored below the cutoff, the study coordinator asked for permission to contact the partner and screen him/her. Among the 22 couples in which both the patient and partner completed the holding back measure, in 16 cases both partners met the criteria, in 3 cases the patient but not the partner met the criteria, and in 3 cases the partner but not the patient met the criteria.
Procedures
All study procedures were approved by the Institutional Review Board at Duke University Medical Center. Participants were recruited between September, 2012 and May, 2014 from the outpatient cancer clinic. After completing informed consent, participants completed pretreatment measures and were then randomly assigned with 1:1 allocation to either Couples Communication Skills Training (CCST) or an education comparison condition (Healthy Lifestyle Information; HLI). Randomization was stratified by patient sex and cancer stage (3 versus 4). Within the four strata, a random number generator was used to assign treatment order with a block size of two. Except for the study statistician (M.O.), all study personnel were blinded to block size and randomization sequence. Assignments were concealed in envelopes that were opened by the study coordinator after both members of the couple completed their pre-treatment evaluation. After completing the intervention, participants completed post-treatment measures. Evaluations were mailed to participants who were instructed to complete the questionnaires independently and return them by mail; separate envelopes were provided. It was intended that post measures be completed 2–3 weeks following the final intervention session, to allow time for mailing; the average number of days was 18 (SD=14, range=5–62). Each participant was reimbursed $50 ($25 for each evaluation).
Measures
Demographic information was collected from patients and partners, and medical information was collected via medical record review. Both members of the couple completed the following self-report questionnaires at baseline and post-treatment. Scale ranges and alphas are presented in Tables 2 and 3.
Table 2.
Means, standard deviations, and effect sizes of screening and outcome variables for patients
| Patients | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| CCST | HLI | ||||||||
|
| |||||||||
| Scale Range | Alpha | N | Pre M (SD) | Post M(SD) | N | Pre M (SD) | Post M (SD) | Effect Size | |
| Screening: Holding back | 0–4 | .78 | 8 | 1.21 (0.80) | -- | 14 | 1.83 (0.86) | -- | -- |
| Relationship functioning | |||||||||
| Relationship satisfaction | 0–42 | .86 | 11 | 28.0 (5.6) | 29.2 (5.9) | 17 | 29.6 (7.5) | 28.4 (8.5) | .30 |
| Intimacy | 0–10 | .94 | 12 | 8.0 (0.9) | 8.4 (0.9) | 17 | 8.0 (1.3) | 7.8 (1.6) | .63 |
| Affective communicationa | 0–13 | .89 | 12 | 3.4 (3.0) | 2.4 (3.4) | 17 | 4.5 (3.9) | 4.2 (3.7) | −.35 |
| Problem solving communicationa | 0–19 | .88 | 12 | 7.3 (4.4) | 5.2 (3.6) | 17 | 9.0 (5.8) | 8.7 (6.0) | −.50 |
| Individual functioning | |||||||||
| Cancer-related distress | 0–4 | .71 | 12 | 2.5 (0.5) | 2.4(0.6) | 17 | 2.6 (0.6) | 2.5 (0.6) | .11 |
| Self-efficacy | 10–100 | .97 | 12 | 66.4 (22.7) | 68.7 (19.8) | 16 | 62.6 (21.3) | 69.1 (19.2) | −.22 |
| PTGIb Total | 0–105 | .93 | 11 | 63.4 (21.6) | 62.6 (15.8) | 17 | 71.1 (16.9) | 71.6 (17.4) | .02 |
| PTGIb Relating to Others | 0–30 | .82 | 11 | 19.3 (5.8) | 19.4 (5.5) | 17 | 20.6 (5.0) | 21.3 (4.8) | −.06 |
| PTGIb New Possibilities | 0–25 | .70 | 11 | 12.3 (5.3) | 10.8 (4.1) | 17 | 14.5 (4.9) | 14.9 (4.9) | −.37 |
| PTGIb Personal Strength | 0–20 | .74 | 11 | 12.2 (5.5) | 13.3 (3.7) | 16 | 13.2 (3.8) | 12.9 (4.1) | .36 |
| PTGIb Spiritual Change | 0–10 | .90 | 11 | 5.2 (3.8) | 5.4 (4.4) | 17 | 6.8 (2.8) | 7.1 (3.0) | .03 |
| PTGIb Appreciation of Life | 0–15 | .84 | 11 | 11.2 (2.8) | 10.7 (3.8) | 14 | 12.5 (2.6) | 11.8 (2.7) | .02 |
Notes:
For Affective communication and Problem solving communication, lower scores are indicative of more effective communication.
PTGI=post-traumatic growth inventory.
Table 3.
Means, standard deviations, and effect sizes of screening and outcome variables for partners.
| Partners | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| CCST | HLI | ||||||||
|
| |||||||||
| Scale Range | Alpha | N | Pre M (SD) | Post M(SD) | N | Pre M (SD) | Post M (SD) | Effect Size | |
| Screening: Holding Back | 0–4 | .84 | 12 | 2.40 (1.36) | -- | 17 | 2.00 (1.0) | -- | -- |
| Relationship functioning | |||||||||
| Relationship satisfaction | 0–42 | .91 | 12 | 26.6 (6.0) | 26.9 (8.2) | 16 | 30.6 (6.0) | 28.8 (7.7) | .34 |
| Intimacy | 0–10 | .92 | 12 | 8.0 (1.0) | 8.0 (1.3) | 17 | 8.4 (1.4) | 8.4 (1.6) | −.07 |
| Affective communicationa | 0–13 | .88 | 11 | 3.7 (2.8) | 3.3 (3.4) | 17 | 3.8 (3.8) | 3.4 (4.1) | −.14 |
| Problem solving communicationa | 0–19 | .89 | 12 | 7.8 (5.2) | 7.4 (5.2) | 17 | 7.1 (5.1) | 6.9 (6.0) | −.07 |
| Individual functioning | |||||||||
| Cancer-related distress | 0–4 | .83 | 12 | 2.1 (0.6) | 2.3 (0.7) | 17 | 2.2 (0.7) | 2.5 (0.6) | −.14 |
| Self-efficacy | 10–100 | .96 | 10 | 57.9 (20.2) | 61.0 (23.2) | 16 | 65.7 (19.3) | 70.1 (17.7) | −.25 |
| PTGIb Total | 0–105 | .95 | 10 | 38.3 (20.2) | 48.0 (29.4) | 17 | 63.7 (21.8) | 69.5 (20.9) | .18 |
| PTGIb Relating to Others | 0–30 | .88 | 10 | 10.2 (4.9) | 13.9 (9.5) | 17 | 18.3 (6.5) | 19.3 (6.8) | .49 |
| PTGIb New Possibilities | 0–25 | .80 | 9 | 5.9 (4.6) | 9.8 (6.5) | 17 | 13.0 (6.1) | 15.0 (5.4) | .07 |
| PTGIb Personal Strength | 0–20 | .88 | 9 | 7.6 (5.7) | 8.5 (6.0) | 16 | 12.1 (5.1) | 14.1 (5.4) | −.14 |
| PTGIb Spiritual Change | 0–10 | .91 | 10 | 3.3 (4.1) | 3.5 (3.7) | 17 | 5.7 (3.6) | 6.2 (3.7) | .05 |
| PTGIb Appreciation of Life | 0–15 | .63 | 11 | 7.7 (4.0) | 8.9 (4.1) | 16 | 10.8 (3.0) | 12.0 (2.0) | −.10 |
Notes:
For Affective communication and Problem solving communication, lower scores are indicative of more effective communication.
PTGI=post-traumatic growth inventory.
Acceptability was measured using the Client Satisfaction Questionnaire (CSQ-8[23]) which assesses effectiveness of/satisfaction with services received. This scale was administered at post-treatment only. Cronbach’s alphas were .86 and .83 for patients and partners, respectively. Additional questions were added to assess the convenience of the videoconference format, preference for format (videoconference, telephone, or in person), and comments regarding aspects of the intervention that they found most and least helpful (open ended).
Relationship Satisfaction was measured with the Revised Dyadic Adjustment Scale (RDAS)[24], a standardized and validated measure widely used to evaluate relationship satisfaction. The reliability and validity of the RDAS has been established in cancer populations.[25]
Intimacy was measured with the Miller Social Intimacy Scale (MSIS)[26] which assesses the degree of intimacy, closeness, and trust that an individual feels in a relationship toward his or her partner. The MSIS has demonstrated adequate reliability and validity.[26]
Communication was measured using two subscales of the Marital Satisfaction Inventory-Revised,[27] Problem Solving Communication (PSC) and Affective Communication (AFC). The PSC assesses difficulty resolving minor differences, lack of problem solving skills, and inability to discuss sensitive issues. The AFC assesses lack of support and affection and limited disclosure of feelings or lack of understanding. The MSI-R and its subscales have been extensively validated.[27]
Cancer-related Distress was assessed using the 8-item version of the Impact of Events Scale (IES).[28] This scale has been found to reliably assess intrusive thoughts about stressful events and conscious avoidance of feelings and ideas about the events.[29] Internal consistency for the shortened version has been found to be as good as the longer version.[30]
Psychological Growth was measured with the Posttraumatic Growth Inventory (PTGI)[31] which assesses how patients and partners feel that they have changed as a result of the patient’s illness and focuses on positive outcomes. There is a total score and five subscales: Relating to Others, New Possibilities, Personal Strength, Spiritual Change, and Appreciation of Life.
Self-efficacy for managing symptoms was assessed with a modified version of a standard self-efficacy scale.[32] Items assess one’s perceived ability to manage a variety of cancer symptoms (patient version) or help the patient manage symptoms (partner version). Prior studies using this instrument with cancer patients and caregivers have demonstrated evidence of its validity [33, 34].
Interventions
General factors.
The six, 60-minute sessions were conducted with via videoconference. Therapists were two master’s level social workers. Sessions for both treatment conditions included both didactic and experiential components, and information was summarized in handouts given to the couple. Several steps were taken to ensure that the treatment protocols and delivery were uniform. First, therapists received training in the protocols by the study PI (L.S.P.). Both therapists had prior training in couple therapy and experience delivering similar interventions to couples coping with advanced cancer, thus training was conducted in one four-hour workshop consisting of an overview of the goals and treatment strategies for each protocol, a review of the treatment manual, and role-plays of commons scenarios. Therapists then role-played each session and these were reviewed to ensure adherence and quality. Therapists followed treatment manuals for each session. All sessions were audio recorded, reviewed by the study PI, and discussed with the therapists in biweekly supervision sessions.
The Couples Communication Skills Training (CCST) protocol systematically trained couples in two communication skills to help patients and their partners (a) disclose their thoughts and feelings related to the cancer experience to each other, and (b) make decisions about cancer-related issues. The intervention emphasized the importance of both patients and partners having the opportunity to address their concerns and be heard by the other person. Following each session, the couple was given home practice assignments focusing on ways to incorporate material from the session into daily life.
In the first session, couples learned communication skills for disclosing thoughts and feelings about cancer, along with strategies for accepting and affirming the other person’s feelings and perspectives.[35]. They were instructed to share their thoughts and feelings regarding a topic related to the patient’s cancer. A list of possible topics was provided (e.g., disruptions to life caused by the illness; talking to family or friends; plans for the future; fears or worried about death), but couples were encouraged to talk about something of personal concern. They were encouraged to discuss both negative feelings (i.e., fears, frustrations, concerns) and positive feelings (i.e. hope, gratitude, affection) associated with these topics.
Session 2 focused on training couples in communication skills for joint decision making.[36]. In this session, they were instructed to think of a problem that they would like to solve or a decision that they would like to make that involves the patient’s cancer. They were told that they did not necessarily need to come to a final decision or solution, but if they did they were encouraged to implement it and to review the outcomes in subsequent sessions.
In sessions 3–6, the patient and partner each had the opportunity to select a topic to discuss and specified whether they wanted to focus exclusively on expressing their concerns, or if they also wanted to make a decision about the issue. The last session included discussions of the couple’s progress during treatment and future issues the couple anticipated addressing relative to communicating about cancer. Sessions were audio recorded for quality assurance.
The Healthy Lifestyle Information (HLI) intervention provided couples with health information relevant to cancer in a supportive environment. Sessions focused on the following topics: fatigue, sleep disturbance, nutrition, physical activity, survivorship care plans, and palliative care. Patients and partners in this condition were invited to discuss their experiences around the session topics with the therapist and ask questions about the information presented. However, they did not receive training in communication skills, nor were they encouraged to disclose emotions or problem solve with each other. Following each session, the couple was encouraged to review the session handouts and utilize the information provided as appropriate.
Statistical Analyses
Descriptive analyses examined recruitment rates, pre/post means on outcome measures for the two study conditions, and feasibility and acceptability measures. Due to the small sample size, for primary analyses significance tests were not calculated for between-group comparisons of pre-post change, and only complete data (i.e., data from participants available at both pre/post-treatment) were used. Using procedures employed in other small psychosocial intervention studies [37, 38], pre- to post-treatment change scores were calculated for each person. Between-group effect sizes were then calculated (group-wise difference in mean change scores/pooled change score SD) [37]. Effect sizes were classified as large (≥.80), medium (.30-.60), and small (.20-.30).[39] Analyses were conducted using SAS Version 9.2 (Cary, NC).
Results
Participants
Baseline demographic and medical data for participants are presented in Table 1. Patients were mostly male, Caucasian, and highly educated. Partners were all opposite-sex, and all couples were cohabitating. Baseline scores on the RDAS indicate that, on average, participants were highly satisfied in their relationships.
Table 1.
Participant demographic and medical characteristics
| Patients M (SD) | Partners M (SD) | |
|---|---|---|
| Age | 54.7 (10.4) | 52.3 (10.1) |
| Length of marriage/relationship (years) | 18.8 (14.0) | 18.8 (14.0) |
| Education (years) | 15.8 (2.9) | 14.8 (2.7) |
|
| ||
| n (%) | n (%) | |
|
| ||
| Gender (%male) | 22 (68.8) | 10 (31.2) |
| Race/ethnicity | ||
| White | 28 (87.5) | 28 (87.5) |
| Hispanic | 1 (3.1) | 0 (0) |
| Cancer site | ||
| Colorectal | 14 (43.8) | |
| Pancreatic | 8 (25.0) | |
| Esophageal | 4 (12.5) | |
| Other | 6 (18.8) | |
| Cancer stage | ||
| Stage IV | 23 (71.9) | |
Feasibility and Acceptability
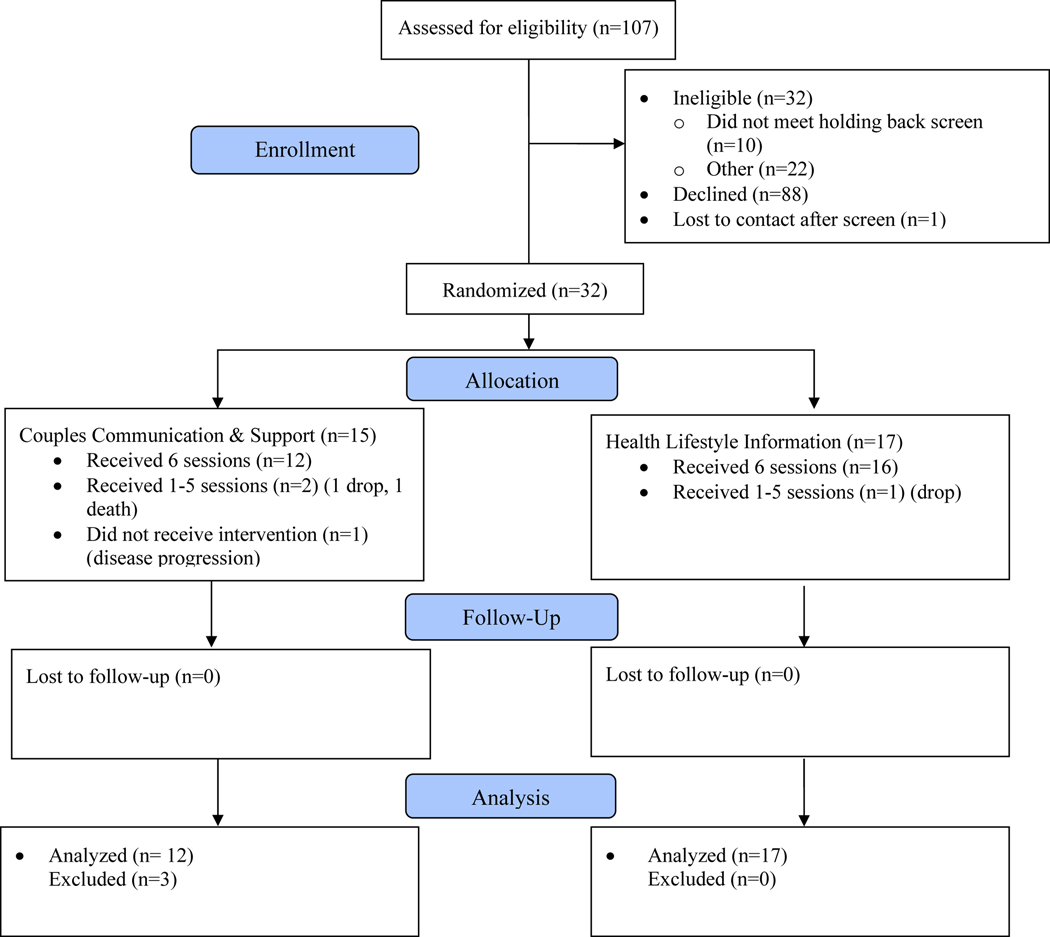
Study Enrollment and Participation (see Figure 1).
Figure 1.
Study consort diagram
Of 153 patients screened, 32 (21%) were excluded, 10 because neither the patient nor partner met criteria on the Holding Back screen. Of 121 eligible patients, 34 (28%) agreed to participate. Reasons for refusal included lack of patient or partner interest (n=56); lack of time (n=21); feeling too ill (n=6); and concerns about privacy (n=4). Thirty-four couples were consented and 32 were randomized; one partner changed her mind prior to completing baseline questionnaires, and one couple was unresponsive to multiple contact attempts. 29 couples completed the study. Three couples in the CCST group dropped out; one because the patient died and two because of declining health. One couple in the HLI group discontinued the treatment sessions but completed post-treatment surveys. All analyses are based on the 29 couples who provided both baseline and post-test data.
Acceptability.
Among patients, those in CCST reported mean satisfaction ratings of 3.63 (SD=0.40) while those in HLI reported mean satisfaction ratings of 3.19 (SD=0.48). Among partners, the mean satisfaction ratings were 3.43 (SD=0.46) for CCST and 3.18 (SD=0.61) for HLI. Responses to the question on the satisfaction survey regarding the videoconference format indicated high satisfaction with this format, with a mean rating of 3.7 (SD=.79). When queried about their preference for format, 77% chose videoconference compared to 20% who chose in person and 3% telephone.
In response to the open-ended question, participants in the both treatment conditions commented favorably on having the opportunity to discuss cancer-related issues with a skilled, empathic moderator, and on the flexibility and convenience of the videoconference format. Several participants in both conditions noted that the intervention would have been more helpful closer to the time of diagnosis. Among participants in the CCST condition, many reported that the training in communication skills, particularly in listening, was very helpful. One partner noted that it would have been helpful to have more guidance regarding specific topics to work on.
Preliminary Efficacy
Effect Sizes for Patients (see Table 2).
For measures of relationship functioning, medium effects were found in favor of CCST for relationship satisfaction, intimacy, affective communication, and problem-solving communication. For measures of individual functioning, a medium effect size in favor of CCST was found for the PTGI Personal Strength subscale, while small to medium effects in favor of HLI were found for self-efficacy and PTGI New Possibilities.
Effect Sizes for Partners (see Table 3).
For measures of relationship functioning, there was a medium effect in favor of CCST for relationship satisfaction, but no effects for intimacy or communication. For measures of individual functioning, there was a medium effect in favor of CCST for PTGI Relating to Others, and a small effect in favor of HLI for self-efficacy.
Conclusions
The primary aim of this study was to determine the feasibility and acceptability of a couples communication intervention delivered via videoconference to patients with advanced GI cancer and their partners. To a large degree, findings supported the feasibility and acceptability of this approach. Retention was excellent, with 91% of randomized couples randomized providing post-test data; this is in contrast to a 22% attrition rate among patients with advanced cancer and their partners reported in a recent review of couple-based interventions. [40] Treatment completion rates were also excellent with 88% of randomized couples receiving all six sessions. These are considerable improvements on retention and treatment completion rates in our previous couple-based intervention study which consisted of four in-person sessions; in that study, 79% of couples provided post-test data, and only 56% received all four sessions. One likely reason for these improvements is the convenience and flexibility afforded by the videoconference format. This was particularly important for patients dealing with fatigue and other cancer symptoms and treatment-related side effects, but it was also helpful for couples with childcare and work responsibilities, and for those who lived at a distance from the medical center.
From therapist and participant report, the home-based sessions via videoconference also appeared to enhance participant-therapist rapport. Participants frequently used the videoconference to share personal aspects of their home life with the therapist (e.g., introducing a pet, or showing the therapist a favorite part of their house). Some participants noted that they felt it less intimidating to discuss sensitive issues over videoconference compared to in person. Therapists reported that they felt levels of rapport were as high as, or higher than, in-person sessions. Technological problems were limited almost exclusively to poor reception via the cellular data plan. If the couple was not able to connect through videoconference, the session was conducted by telephone. This occurred in approximately 20% of the sessions, most of which were early in the study. It is likely that the geographic area covered by cellular data plan increased over the course of the study, and will continue to increase in the future, making videoconferencing increasingly accessible to more participants.
Another important feature of the study was the focus on couples who reported having difficulty communicating about cancer-related issues. Interestingly, only 10 couples were excluded from the study because neither member scored highly enough on the Holding Back scale. Thus, the use of the screening questionnaire did not unduly hinder recruitment. However, most couples who declined to participate did so prior to completing screening. Thus, it is not known whether couples with communication difficulties are more or less likely to participate in a study focused on enhancing communication. We observed that, in the first session of the communication intervention, most couples admitted to challenges in talking about cancer-related issues and thought the content of the intervention would be helpful for them. This is in contrast to our previous intervention study in which many couples said at the outset that they thought they communicated relatively well. Thus, it is possible that limiting participation to couples based on the Holding Back screen increased the relevance of the intervention for them and might also have contributed to the high treatment completion rate.
Acceptability ratings were high among participants in both treatment arms, albeit somewhat higher in the communication intervention versus the comparison condition. Another indication of acceptability is the uptake, or percent of eligible couples who agree to participate in the study. The uptake in this study (28%) was lower than we had hoped, although similar to that in our previous couple-based intervention study with the same population (25%). As we and others have noted [40, 41], recruitment of couples into psychosocial treatment studies is particularly challenging. While travel to attend intervention sessions is one salient barrier that can be overcome using technology such as videoconferencing, research is needed to more precisely identify and overcome other barriers to participation, such as perceptions of stigma associated with psychosocial care. [40] Integration of psychosocial assessment and treatment into routine clinical care may help legitimize participation in psychosocial treatment studies, as would maximizing involvement by patients’ physicians during the recruitment process. [40, 41] Oncologists are viewed as highly credible by their patients, and their endorsement of the value of psychosocial treatment studies may play a key role in patients’ and partners’ willingness to participate.
Regarding the efficacy of the intervention, the small sample size makes it difficult to interpret the outcome data. However, the between-group effect sizes suggest that the CCST intervention led to improvements in relationship functioning, particularly for patients. Both patients and partners in the CCST arm reported greater improvements in relationship satisfaction than did couples in the comparison condition. In addition, patients in CCST reported improvements in intimacy with their partner, and in their communication. Notably, these effects were obtained in the context of a study design that used a comparison condition that equated for time and attention given to couples. Thus, these findings suggest that it is not simply attending sessions with one’s partner in a supportive environment that leads to improvements in relationship functioning. Rather, training couples in communication skills and giving them the opportunity to share their thoughts and feelings and problem solve about cancer-related concerns appears to be the active ingredient.
The limited number of findings for partners is somewhat surprising given that, in our previous study, findings were consistent between patients and partners. In addition, unlike our previous intervention which focused exclusively on patient disclosure, the current intervention encouraged both patients and partners to talk about their cancer-related concerns to each other. Despite this more balanced approach, patients seemed to benefit more than partners, at least in the short-term. One possible explanation is that partners may have felt uncomfortable focusing on their own concerns in addition to the patients’. The fact that, at baseline, partners reported higher levels of holding back than patients supports this possibility. It is also possible that partners may report more benefits of the intervention over time as they continue to use the communication skills in their conversations with their partners (the patients).
A qualitative analysis of couples’ conversations during the intervention sessions, including the topics they discussed, who initiated the conversation, and whether the focus was on the patient or partner, may also help shed light on why patients benefited more than partners. We are currently conducting these analyses, but an informal review of the topics discussed suggests that they were quite varied. Examples include: practical day-to-day issues (e.g., the logistics of getting to medical appointments; management of household responsibilities); the emotional toll that cancer was taking on the patient, partner, and their relationship (e.g., feelings of guilt and worry; the desire to foster greater emotional and physical intimacy); their experiences in talking with and receiving support from friends and family; plans for the future (e.g., travel, job transitions); and end-of-life issues such as the preparation of wills and funeral arrangements. While therapists did not explicitly recommend that couples address end-of-life issues, they were attune to the fact that these issues were salient for these couples but also likely to spur avoidance. Thus, if one member of the couple raised such an issue, the therapist encouraged the couple to address it while processing, normalizing, and working through any avoidance. Notably, even many of the seemingly mundane topics that couples discussed were imbued with an additional layer of meaning associated with recognition of the patient’s shortened life expectancy. For example, a discussion regarding whether to get a Christmas tree was driven by competing desires to create lasting memories and to avoid unnecessary hassle given the burdens associated with the patient’s ongoing treatment. Thus, many couples used the sessions as an opportunity to discuss issues related to life completion.
Limitations of the study include the small sample size and the lack of long-term follow up. A larger study would enable examination of dyadic effects, including whether intervention effects differ for patients versus partners, using analytic strategies suited for dyadic data.[42] Ideally, a future study would also (a) utilize a three-group design, comparing the couple-based communication and education interventions to a standard-care control group; (b) examine mechanisms of change to help elucidate differential effects of the two interventions, and (c) include observational measures of couples’ communication skills. A future study might also include patients with other types of advanced cancer, such as prostate and breast cancer which, like GI cancer, are associated with difficulties related to couple communication [7, 21] and focus on enrolling a more diverse sample. Finally, in light of participant comments, it may be helpful to focus on couples closer to the time of the patient’s diagnosis and, in the communication intervention to provide more guidance about specific topics to focus on, perhaps guiding couples to focus on issues related to life completion to assist with transitions at the end of life.
Despite its limitations, this study offers support for the feasibility of a couple-based communication skills training intervention delivered via videoconference. This is the first study to demonstrate that videoconference is a feasible and acceptable mode of delivery for couple-based interventions in the context of advanced cancer that may aid in treatment adherence. This is also the first study to target couples having communication difficulties for inclusion in a couple-based intervention study. While preliminary, findings suggest that the communication intervention shows promise in enhancing couples’ relationship functioning.
Acknowledgements
This study was supported by grant PEP-12–180-01-PCSM from the American Cancer Society. The authors gratefully acknowledge the contributions of Jessyka Glatz, M.A., Emily Patterson, M.S.W., L.C.S.W., and Margaret Falkovic, M.S.W. They also extend their gratitude to all of the study participants for their time and effort.
References
- [1].Baucom DH, Porter LS, Kirby JS, Hudepohl J. Couple-based interventions for medical problems. Behavior Therapy. 2012;43:61–76. [DOI] [PubMed] [Google Scholar]
- [2].Traa MJ, De Vries J, Bodenmann G, Den Oudsten BL. Dyadic coping and relationship functioning in couples coping with cancer: A systematic review. British Journal of Health Psychology. 2015;20:85–114. [DOI] [PubMed] [Google Scholar]
- [3].Kuijer R, Ybema J, Buunk BP, DeJong M. Active engagement, protective buffering, and overprotection. Journal of Social and Clinical Psychology. 2000;19:256–75. [Google Scholar]
- [4].Manne SL, Kissane D, Zaider T, Kashy D, Lee D, Heckman C, et al. Holding back, intimacy, and psychological and relationship outcomes among couples coping with prostate cancer. J Fam Psychol. 2015;29:708–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Porter LS, Keefe FJ, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psychooncology. 2005;14:1030–42. [DOI] [PubMed] [Google Scholar]
- [6].Badr H, Pasipanodya EC, Laurenceau JP. An electronic diary study of the effects of patient avoidance and partner social constraints on patient momentary affect in metastatic breast cancer. Annals of Behavioral Medicine. 2013;45:192–202. [DOI] [PubMed] [Google Scholar]
- [7].Pistrang N, Barker C. The partner relationship in psychological response to breast cancer. Soc Sci Med. 1995;40:789–97. [DOI] [PubMed] [Google Scholar]
- [8].Lichtman RR SET, Wood JV. Social support and marital adjustment after breast cancer. Journal of psychosocial oncology. 1987;5:47–74. [Google Scholar]
- [9].Northouse LL, Mood D, Templin T, Mellon S, George T. Couples’ patterns of adjustment to colon cancer. Social Science and Medicine. 2000;50:271–84. [DOI] [PubMed] [Google Scholar]
- [10].Peters-Golden H. Breast cancer: varied perceptions of social support in the illness experience. Social Science and Medicine. 1982;16:483–91. [DOI] [PubMed] [Google Scholar]
- [11].Reese JB, Shelby RA, Keefe FJ, Porter LS, Abernethy AP. Sexual concerns in cancer patients: a comparison of GI and breast cancer patients Support Care Cancer. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–82. [DOI] [PubMed] [Google Scholar]
- [13].McLean LM, Jones JM. A review of distress and its management in couples facing end-of-life cancer. Psychooncology. 2007;16:603–16. [DOI] [PubMed] [Google Scholar]
- [14].Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psycho-oncology. 2012;22:1688–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson ES, et al. Partner-Assisted Emotional Disclosure for Patients with GI Cancer: Eight-week follow up and processes associated with change. Supportive Care in Cancer. in press. [DOI] [PubMed] [Google Scholar]
- [16].Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson E, et al. Partner-assisted emotional disclosure for patients with gastrointestinal cancer: Results from a randomized controlled trial. Cancer. 2009;115(S18):4326–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Schneider S, Moyer A, Knapp-Oliver S, Sohl S, Cannella D, Targhetta V. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: A meta-analysis. Journal of Behavioral Medicine. 2010;33:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jacobsen PB. Lost in translation: The need for clinically relevant research on psychological interventions for distress in cancer patients. Annals of Behavioral Medicine. 2006;32:119–20. [DOI] [PubMed] [Google Scholar]
- [19].Richardson LK, Frueh BC, Grubaugh AL, Egede L, Elhai JD. Current directions in videoconferencing tele-mental health research. Clinical Psychology. 2009;16:323–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lawrence D. Let’s meet onscreen. The use of video is expanding beyond rural areas. Healthc Inform. 2010;27:26–8. [PubMed] [Google Scholar]
- [21].Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship. 2010;4:74–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Figueiredo M, Fries E, Ingram K. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psycho-oncology. 2004;13:96–105. [DOI] [PubMed] [Google Scholar]
- [23].Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and program planning. 1983;6:299–314. [DOI] [PubMed] [Google Scholar]
- [24].Busby DH, Crane DR, Christensen C. A revision of the dyadic adjustment scale for use with distressed and non-distressed couples: construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy. 1995;21:289–308. [Google Scholar]
- [25].Shields CG, Travis LA, Rousseau SL. Marital attachment and adjustment in older couples coping with cancer. Aging and Mental Health 2000;4:223–33. [Google Scholar]
- [26].Miller RS, Lefcourt HM. Miller Social Intimacy Scale. In: Corcoran K, Fischer J, editors. Measures for Clinical Practice: A Sourcebook, 3rd ed. New York, NY: Free Press; 2000. [Google Scholar]
- [27].Snyder DK. Manual for the Marital Satisfaction Inventory. Los Angeles, CA: Western Psychological Services; 1997. [Google Scholar]
- [28].Zilberg NJ, Weiss DS, Horowitz MJ. Impact of Event Scale: a cross-validation study and some empirical evidence supporting a conceptual model of stress response syndromes. Journal of Consulting and Clinical Psychology. 1982;50:407–14. [DOI] [PubMed] [Google Scholar]
- [29].Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–18. [DOI] [PubMed] [Google Scholar]
- [30].McBride CM, Clipp E, Peterson BL, Lipkus IM, Demark-Wahnefried W. Psychological impact of diagnosis and risk reduction among cancer survivors. Psychooncology. 2000;9:418–27. [DOI] [PubMed] [Google Scholar]
- [31].Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Trauma and Stress. 1996;9:455–71. [DOI] [PubMed] [Google Scholar]
- [32].Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. [DOI] [PubMed] [Google Scholar]
- [33].Porter LS, Keefe FJ, Garst J, McBride CM, Baucom DH. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: associations with symptoms and distress. Pain. 2008;137:306–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Keefe FJ, Ahles TA, Sutton L, Dalton J, Baucom DH, Pope MS, et al. Partner-guided pain management at the end of life: a preliminary study. Journal of Pain and Symptom Management. 2005;29:263–72. [DOI] [PubMed] [Google Scholar]
- [35].Epstein N, Baucom DH. Enhanced cognitive-behavioral therapy for couples: A contextual approach. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- [36].Baucom DH, Shoham V, Mueser KT, Daiuto AD, Stickle TR. Empirically supported couples and family therapies for adult problems. Journal of Consulting and Clinical Psychology. 1998;66:53–88. [DOI] [PubMed] [Google Scholar]
- [37].Baucom DH, Porter LS, Kirby JS, Gremore TM, Wiesenthal N, Aldridge W, et al. A couple-based intervention for female breast cancer. Psycho-Oncology. 2009;18:276–83. [DOI] [PubMed] [Google Scholar]
- [38].Reese JB, Porter LS, Regan KR, Keefe FJ, Azad NS, Diaz LA, et al. A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology. 2014;23:1005–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cohen J. Statistical power analysis for the behavioral sciences Second ed. New York: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- [40].Regan T, Lambert SD, Kelly B. Uptake and attrition in couple-based interventions for cancer: perspectives from the literature. Psychooncology. 2013;22:2639–47. [DOI] [PubMed] [Google Scholar]
- [41].Fredman SJ, Baucom DH, Gremore TM, Castellani AM, Kallman TA, Porter LS, et al. Quantifying the recruitment challenges with couple-based interventions for cancer: applications to early-stage breast cancer. Psychooncology. 2009;18:667–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kenny D, Kashy D, Cook W. Dyadic Data Analysis. New York: Guilford; 2006. [Google Scholar]