Abstract
Although co-stimulation of T cells with agonist antibodies targeting 4-1BB (CD137) improves antitumor immune responses in preclinical studies, clinical development has been hampered by on-target, off-tumor toxicity. Here, we report the development of a tumor-anchored ɑ4-1BB agonist (ɑ4-1BB-LAIR), which consists of an ɑ4-1BB antibody fused to the collagen binding protein LAIR. While combination treatment with an antitumor antibody (TA99) displayed only modest efficacy, simultaneous depletion of CD4+ T cells boosted cure rates to over 90% of mice. We elucidated two mechanisms of action for this synergy: ɑCD4 eliminated tumor draining lymph node Tregs, enhancing priming and activation of CD8+ T cells, and TA99 + ɑ4-1BB-LAIR supported the cytotoxic program of these newly primed CD8+ T cells within the tumor microenvironment. Replacement of ɑCD4 with ɑCTLA-4, a clinically approved antibody that enhances T cell priming, produced equivalent cure rates while additionally generating robust immunological memory against secondary tumor rechallenge.
One Sentence Summary:
Inhibition of nodal Tregs enhances CD8+ T cell priming, improving antitumor responses to collagen-anchored α4-1BB combination therapy.
INTRODUCTION
The use of monoclonal antibodies to perturb immune cell signaling networks and improve anticancer immune responses has gained increased attention in recent years (1). Checkpoint blockade therapy with antagonistic antibodies is safe and efficacious, but agonistic antibodies against targets such as 4-1BB, OX40, GITR, and ICOS have proven to exhibit impractically narrow therapeutic windows due to on-target, off-tumor toxicity (2–5).
4-1BB (also known as CD137 or TNFRSF9) is expressed primarily on activated CD8+ and CD4+ T cells, including CD4+ regulatory T cells (Tregs), and natural killer (NK) cells, and is a promising target for agonist antibodies (6–10). Signaling through 4-1BB in CD8+ T cells leads to proliferation, enhanced survival, cytokine production, improved memory formation, and altered metabolism (11–15). Treating mice with agonist ɑ4-1BB antibodies as a monotherapy or in combination therapies is highly efficacious in several preclinical mouse cancer models (16, 17). However, toxicity has hampered clinical translation of such antibodies, with lethal liver toxicities reported in early phase 2 trials of Urelumab, the first ɑ4-1BB agonistic antibody to enter the clinic (18). At reduced doses which do not elicit dose limiting toxicities (DLTs), little to no clinical efficacy has been reported (18). Utomilumab, the second ɑ4-1BB agonist to enter the clinic, is well tolerated but is a much weaker agonist and has little clinical activity (19, 20). Given the difficulty of uncoupling toxicity from clinical activity with systemically administered agonists, recent development around this target has focused on engineering antibodies with tumor specific activity (21). This includes several bispecific antibodies, with one arm targeting 4-1BB and the other targeting either tumor specific antigens or PD-L1, ɑ4-1BB antibodies that bind only in tumor specific niches, such as high ATP concentrations, or pro-drug ɑ4-1BB antibodies where the binding domain of the antibody is shielded by a peptide “mask” that is cleaved by tumor specific proteases (22–26).
Alternatively, our group and others have demonstrated the utility of using collagen binding strategies to anchor immunotherapy payloads to the tumor microenvironment (27–35). Collagen is a desirable target for localization due to its abundance in the tumor microenvironment (TME) (36). By directly fusing collagen binding domains to cytokines and chemokines or chemical conjugation of collagen binding peptides to ɑCTLA-4 and ɑCD40 antibodies, intratumoral administration of these therapeutic payloads results in prolonged tumor retention, enhanced efficacy, and reduced systemic toxicity.
In this work, we developed a locally retained collagen-anchored ɑ4-1BB agonist, termed ɑ4-1BB-LAIR, by fusing an ɑ4-1BB agonist to the ectodomain of an endogenous collagen binding protein, Leukocyte Associated Immunoglobulin Like Receptor 1 (LAIR1). Tested in combination with an antitumor antibody, TA99, in a fully syngeneic and poorly immunogenic B16F10 murine melanoma model, this combination exhibited little efficacy. Intriguingly, depletion of CD4+ T cells led to long term durable cures in >90% of TA99- + ɑ4-1BB-LAIR-treated animals. However, nearly all of these mice were unable to control a secondary tumor rechallenge. We hypothesized that depletion of Tregs, which comprise a subset of CD4+ T cells, was driving this synergy. Tregs are immunosuppressive CD4+ T cells that express the transcription factor forkhead box P3 (Foxp3) and are critical to maintaining homeostasis and preventing autoimmunity (37, 38). Indeed, Foxp3−/− mice die at a young age from severe lymphoproliferative disease, systemic depletion of Tregs in adult mice leads to rapid lethal autoimmunity, and Foxp3 mutations in humans cause severe immune dysregulation (39–42). Although Tregs play a critical role in curbing autoreactive T cells, they also constrict productive antitumor immune responses through a variety of mechanisms and at various stages of the tumor-immunity cycle (43, 44).
Using flow cytometry and bulk-RNA sequencing, we probed the immunological mechanism of this synergy and found that CD4+ T cell depletion led to an enhanced activation state in the tumor draining lymph node (TdLN), leading to an influx of newly primed CD8+ T cells into the tumor. Local remodeling of the tumor microenvironment by TA99 and ɑ4-1BB-LAIR enhanced the cytotoxicity of these newly primed T cells, leading to tumor cell death and eventual complete tumor regression. Using a Foxp3-DTR mouse model, which allows for selective depletion of Tregs, we confirmed that Treg depletion alone was sufficient for this synergy. Finally, we demonstrated that CD4+ T cell depletion can be replaced with a more clinically relevant agent known to enhance CD8+ T cell priming, ɑCTLA-4, without compromising efficacy. This combination of TA99 + ɑ4-1BB-LAIR + ɑCTLA-4 also resulted in formation of robust immunological memory, enabling rejection of a secondary tumor rechallenge. This work suggests that locally retained 4-1BB agonist and antitumor antibody therapy can be highly efficacious when combined with modalities that enhance T cell priming, which can be restrained by TdLN Tregs.
RESULTS
TA99 + ɑ4-1BB-LAIR synergizes robustly with CD4 compartment depletion
In order to develop a tumor-localized 4-1BB agonist, we leveraged a collagen anchoring strategy previously validated by our lab and others. We recombinantly expressed an ɑ4-1BB antibody (clone LOB12.3, Table S1) as a C-terminal fusion with the ectodomain of murine LAIR1, an endogenous immune cell inhibitory receptor that naturally binds collagen (45–47). We verified that ɑ4-1BB-LAIR expresses without aggregation (Fig. S1A), is able to bind plate bound collagen I via ELISA (Fig. S1B), and that binding to cell-surface expressed 4-1BB is unaffected.
To validate intratumoral retention without confounding target-mediated drug disposition (TMDD) effects, we also generated an ɑFITC-LAIR control antibody as this antibody has no known murine target (Table S1). Fluorescently labeled ɑFITC-LAIR administered intratumorally was preferentially retained in the tumor over unanchored ɑFITC antibody when measured longitudinally with IVIS (Fig. S1D–E).
ɑ4-1BB agonist Urelumab is being clinically tested in combination with antitumor antibodies Rituximab, Cetuximab, and Elotuzumab which target CD20, EGFR, and SLAMF7, respectively (NCT01775631, NCT02110082, NCT02252263). Preliminary data has not been encouraging, with early reports from the Rituximab combination suggesting that Rituximab + Urelumab is no more efficacious than Rituximab monotherapy (48). We sought to evaluate if collagen-anchoring would improve the efficacy of combination ɑ4-1BB agonist + antitumor antibody therapy. Mice were inoculated with B16F10 melanoma flank tumors and treated systemically (intraperitoneally, or i.p.) with TA99, an antitumor antibody that binds to Trp1 expressed on the surface of B16F10 cells, followed by intratumorally (i.t.) administered ɑ4-1BB-LAIR one day later for a total of 4 weekly cycles (This combination of TA99 + ɑ4-1BB-LAIR is referred to collectively as the treatment, or “Tx”, henceforth, Fig. 1A). Although this combination led to a statistically significant growth delay compared to PBS treated mice, nearly all mice eventually succumbed to their tumor burden, with only ~5% of mice achieving a complete response (CR, defined as no palpable tumor at day 100) (Fig. 1B). Notably, this growth delay was only slightly better than the individual components of Tx, although it was the only therapy with any complete responders (Fig. S2A).
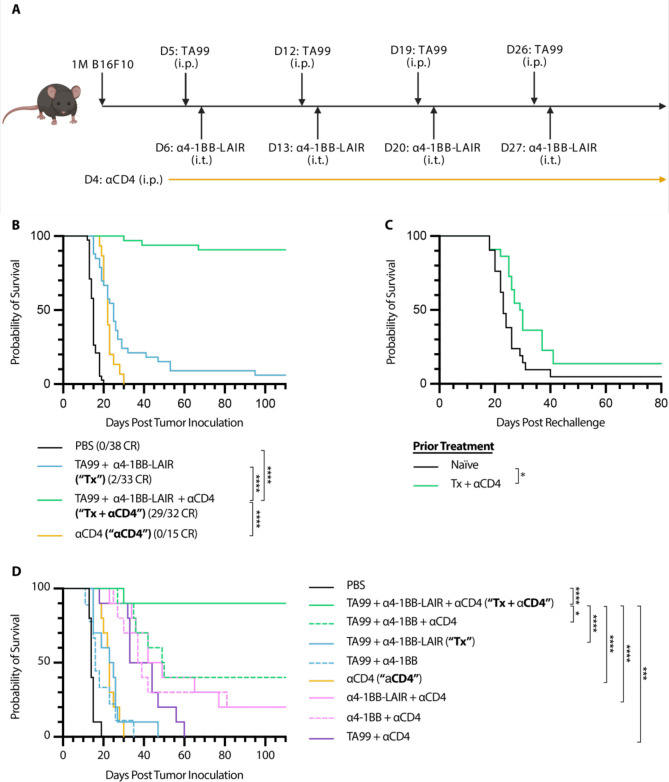
Figure 1. TA99 + α4-1BB-LAIR synergizes robustly with CD4+ T cell depletion.
Mice were inoculated with 1 × 106 B16F10 cells on day 0. (A) Treatment schedule of TA99 + α4-1BB-LAIR + αCD4. Mice were treated with 200 μg of TA99 (i.p.) on days 5, 12, 19, and 26, treated with 36.1 μg α4-1BB-LAIR (i.t.) on days 6, 13, 20, and 27 (molar equivalent to 30 μg α4-1BB), and treated with 400 μg αCD4 (i.p.) every 3 days starting 1 day before the first dose of TA99 and ending one week after the last dose of α4-1BB-LAIR (days 4 to 34). (B) Aggregate survival of mice treated with PBS (n = 38), TA99 + α4-1BB-LAIR (“Tx”) (n = 33), TA99 + α4-1BB-LAIR + αCD4 (“Tx + αCD4”) (n = 32), or αCD4 (n = 15) (eight independent studies). (C) Survival of complete responders to Tx + αCD4 re-challenged on the contralateral flank >100 days after primary tumor inoculation. (D) Overall survival of mice treated with indicated combination variants, demonstrating all components are necessary for maximum efficacy (n = 9–10, two independent experiments). Survival was compared using log-rank Mantel-Cox test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
In an effort to improve this combination therapy, we explored which cell types were critical for response. Surprisingly, we observed that when we also treated these mice with an ɑCD4 antibody that depletes the entire CD4+ T cell compartment, the complete response rate of TA99 + ɑ4-1BB-LAIR improved dramatically, with >90% of mice achieving a complete response (Fig. 1B). However, when long-term survivors were rechallenged on the contralateral flank >100 days after initial tumor inoculation, nearly all mice succumbed to these secondary tumors (Fig. 1C). This was indicative of the inability of these mice to develop robust immune memory to B16F10 tumor cells, likely resulting from the depletion of CD4+ effector T cells.
Growth delay with systemically administered ɑCD4 and ɑ4-1BB has been reported previously, but we find that our specific components were necessary to achieve maximum efficacy, including TA99 (P = .0032) and, notably, retention via collagen anchoring (P = .0289) (Fig. 1D) (49). Consistent with other preclinical reports with this ɑ4-1BB antibody clone, no signs of toxicity were observed for the full therapeutic combination with or without collagen anchoring (Fig. S2B) (50). Although ɑCD4 drastically improved the efficacy of Tx, the lack of immune memory formation and low translational potential of long term ɑCD4 treatment motivated us to understand the mechanism of this synergy and ultimately develop alternative clinically relevant synergistic combinations.
ɑCD4 improves priming in the TdLN
We investigated the chemokine/cytokine profile of the TME following treatments with PBS, Tx, Tx + ɑCD4, or ɑCD4 both 3 and 6 days after ɑ4-1BB-LAIR administration. We dissociated tumors and analyzed the cytokine and chemokine milieu using a multiplexed flow cytometry-based ELISA assay. Although we observed general increases in inflammatory cytokines and chemokines in all treatment groups, only GM-CSF was specifically upregulated in the Tx + ɑCD4 group when compared to Tx or ɑCD4 alone (Fig. S3A). However, neutralization of this cytokine did not abrogate therapeutic efficacy of Tx + ɑCD4, indicating that this spike in GM-CSF was dispensable for therapeutic efficacy (Fig. S3B).
We then used flow cytometry to analyze the tumors and tumor draining lymph nodes (TdLNs) of mice treated with Tx, Tx + ɑCD4, or ɑCD4 again 3 and 6 days after the first ɑ4-1BB-LAIR treatment. As expected, we observed complete depletion of total CD4+ T cells and Tregs (defined as Foxp3+ CD25+ CD4+ T cells) in the tumor (Fig. 2A) and TdLN (Fig. 2B) in both the Tx + ɑCD4 and the ɑCD4 groups.
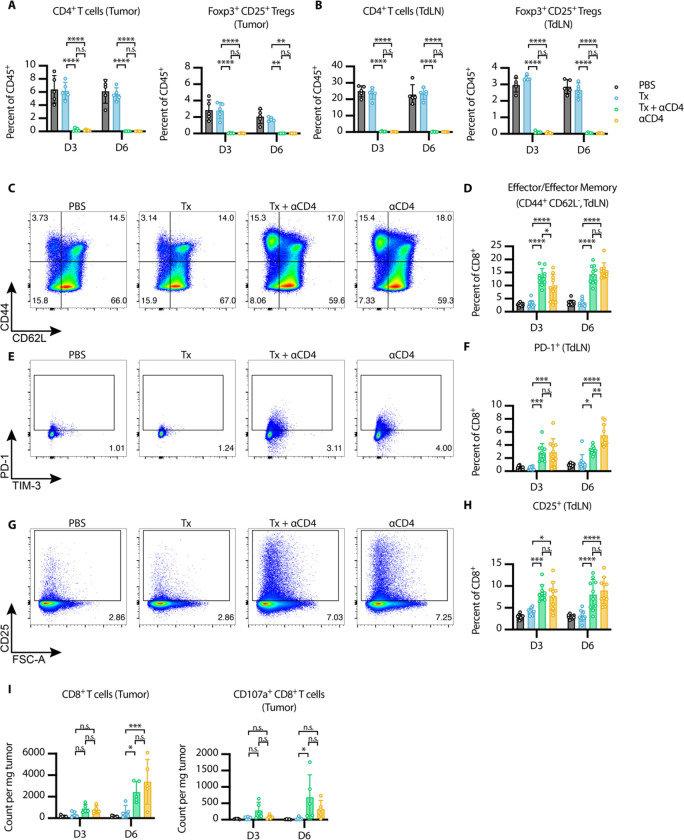
Figure 2. αCD4 leads to new wave of CD8+ T cell priming and Tx supports cytotoxicity of these cells in the tumor.
(A-B) Flow cytometry quantification (mean±SD) of CD4+ T cells (gated on single cell/live/CD45+/CD3+NK1.1−/CD4+) and Tregs (gated on single cell/live/CD45+/CD3+NK1.1−/CD4+/Foxp3+CD25+) in the (A) tumor and (B) TdLN 3 and 6 days after first α4-1BB-LAIR treatment (n = 5). (C) Representative gating on CD44 and CD62L to define effector/effector memory CD8+ T cells in TdLN 6 days after first α4-1BB-LAIR treatment and (D) quantification (mean±SD) of these cell populations 3 and 6 days after first α4-1BB-LAIR treatment (gated on single cell/live/CD45+/CD3+NK1.1−/CD8+/CD44+CD62L−, n = 10, two independent experiments). (E) Representative gating of PD-1+ CD8+ T cells 6 days after first α4-1BB-LAIR treatment and (F) quantification (mean±SD) of these cell populations 3 and 6 days after first α4-1BB-LAIR treatment (gated on single cell/live/CD45+/CD3+NK1.1−/CD8+/PD-1+, n = 10, two independent experiments) (G) Representative gating of CD25+ CD8+ T cells 6 days after first α4-1BB-LAIR treatment and (H) quantification (mean±SD) of these cell populations 3 and 6 days after first α4-1BB-LAIR treatment (gated on single cell/live/CD45+/CD3+NK1.1−/CD8+/CD25+, n = 10, two independent experiments). (I) Flow cytometry quantification (mean±SD) of CD8+ T cells (left) and CD107a+ CD8+ T cells (right) (gated on single cell/live/CD45+/CD3+NK1.1−/CD8+) in the tumor 3 and 6 days after first α4-1BB-LAIR treatment (n = 5). Flow cytometry data was compared using two-way ANOVA with Tukey’s multiple hypothesis testing correction. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Using CD44 and CD62L gating, we divided CD8+ T cells in the TdLN into naive (CD44− CD62L+), effector/effector memory (CD44+ CD62L−), and central memory (CD44+ CD62L+) phenotypes. At both time points, we observed a shift of the CD8+ T cell population towards an effector/effector memory phenotype in the Tx + ɑCD4 and ɑCD4 groups (Fig. 2C–D). Additionally, we observed increases in both PD-1+ CD8+ T cells (Fig. 2E–F) and CD25+ CD8+ T cells (Fig. 2G–H), at both time points in the Tx + ɑCD4 and ɑCD4 groups, both of which are markers of recently activated CD8+ T cells in lymphoid tissue. The magnitude of these changes was equivalent between the Tx + ɑCD4 and ɑCD4 groups, indicating that the ɑCD4 antibody component was driving these changes to the TdLN.
6 days following treatment with either Tx + ɑCD4 or ɑCD4, we observed increased CD8+ T cells infiltrating the tumor (Fig. 2I), which is in agreement with the enhanced activation state observed in the TdLN (Fig. 2E–H). This result is consistent with previous preclinical and clinical studies that have shown treatment with ɑCD4 can enhance T cell priming, leading to increased numbers of tumor reactive CD8+ T cells (51–53). However, only in the Tx + ɑCD4 group, when compared to PBS or Tx alone, do we observe an increase in degranulating CD107a+ CD8+ cytotoxic T cells (Fig. 2I, Fig. S4A). No major differences in 4-1BB expression on CD8+ T cells were detected in the tumor and only minor increases were seen on CD8+ T cells in the TdLN in Tx + ɑCD4 and ɑCD4 treated mice (Fig. S4B–D). These data suggest that ɑCD4 therapy, independent of Tx, induces de novo priming in the TdLN, leading to more CD8+ T cell infiltration in the tumor. However, we hypothesized that Tx supports these newly primed cells and maintains their cytotoxic phenotype within the tumor, leading to eventual tumor regression.
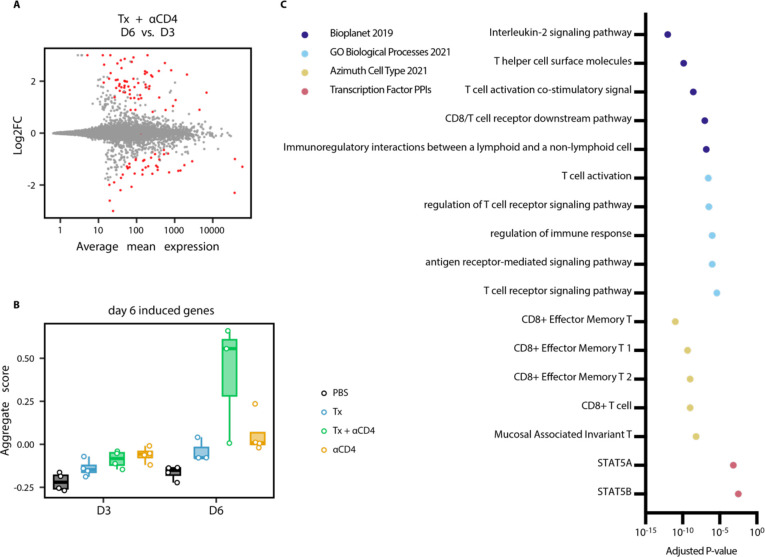
TdLN has increased proliferation and T cell gene signatures by Bulk-RNA sequencing
To further interrogate immunological changes to the TdLN and tumor in an unbiased holistic manner, we performed bulk RNA-sequencing on CD45+ cells from TdLN samples from mice treated with PBS, Tx, Tx + ɑCD4, or ɑCD4 3 and 6 days following ɑ4-1BB-LAIR administration. We generated a UMAP plot of the TdLN samples and found that, at the bulk transcript level, large differences between samples were apparent only at the later time point (Fig. 3A). Additionally, sample clustering at this later time point was driven entirely by ɑCD4, with the ɑCD4 and Tx + ɑCD4 samples clustering separately from the PBS and Tx samples. In fact, we observed almost no differentially expressed genes (DEGs) in the TdLN when comparing Tx + ɑCD4 versus ɑCD4 or Tx versus PBS treated samples (Fig. 3B), indicating that Tx alone had no appreciable change on the transcriptional program in the TdLN.
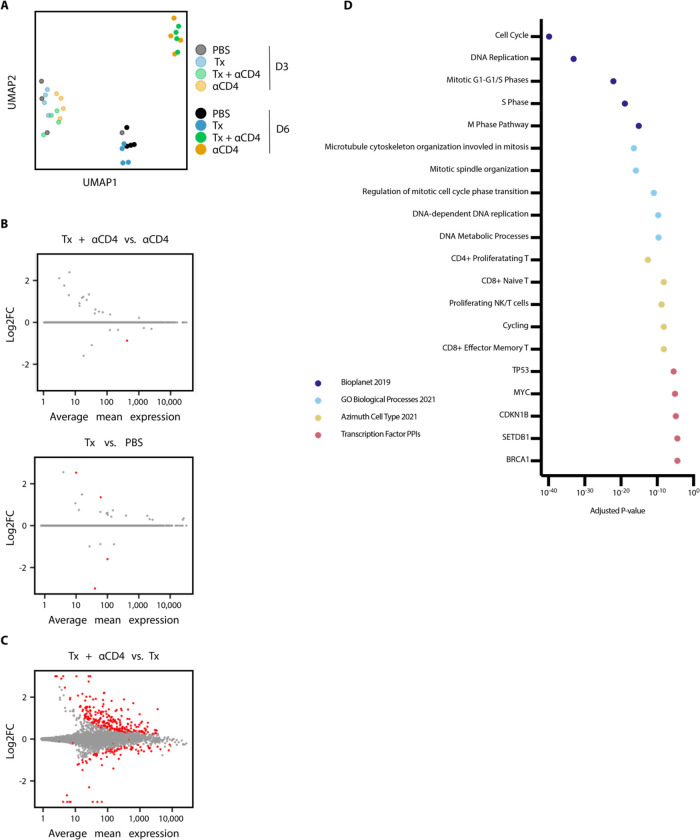
Figure 3. αCD4 drives proliferation in the TdLN.
(A) UMAP plot of TdLN transcriptomes (n = 4 per group) (B) Differential expression testing of Tx + αCD4 vs. αCD4 and Tx vs. PBS TdLN samples 6 days after first α4-1BB-LAIR treatment, with statistically significant hits highlighted in red (FDR ≤ 5%). (C) Differential expression testing of Tx + αCD4 vs. Tx TdLN samples 6 days after to first α4-1BB-LAIR treatment, with statistically significant hits highlighted in red (FDR ≤ 5%). (D) Pathway enrichment analysis of upregulated DEGs identified in (C).
To assess what changes ɑCD4 drove in the TdLN, we examined DEGs between Tx + ɑCD4 and Tx treated samples (Fig. 3B). We found 247 upregulated genes and 82 downregulated genes (FDR ≦5%, Fig. 3C). We used enrichR to determine which pathways these upregulated DEGs were enriched in (54–56). Upregulated genes belonged to pathways involving cell cycling, DNA replication, and Myc related genes, indicative of a highly proliferative state in the TdLN. They were also enriched for both cycling and CD8+ T cell states (Fig. 3D). Overall, the TdLN transcriptional data demonstrated that 1) changes to the TdLN resulted from ɑCD4 treatment, independent of Tx, and 2) these changes led to enhanced proliferation and T cell activation in the TdLN.
Tx + ɑCD4 leads to cytotoxic CD8+ T cell program in the tumor
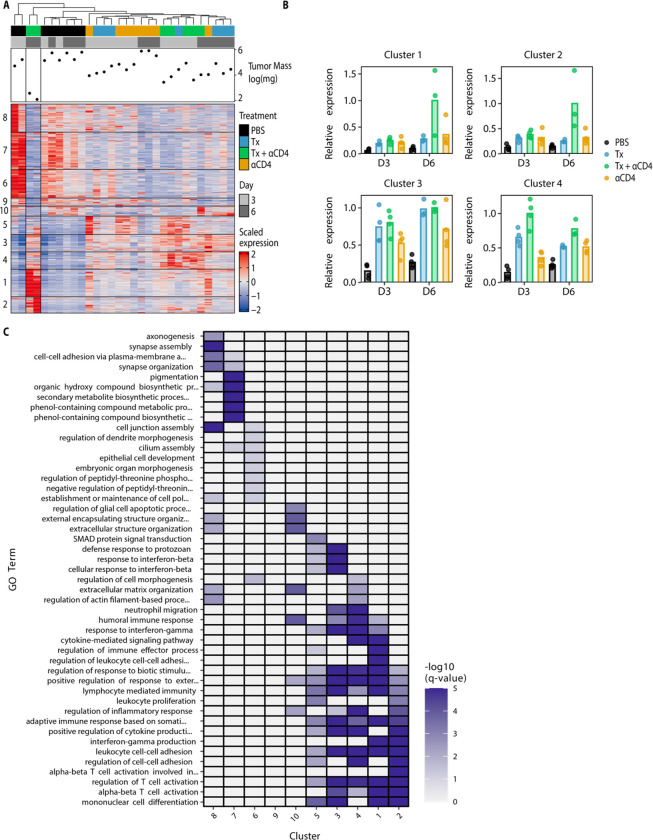
We similarly used bulk-RNA sequencing to examine immune cell gene expression programs within the tumor. We performed hierarchical clustering of the tumor samples while also independently clustering all significant DEGs (with a log 2-fold change ≥2 or ≤−2 and p-adj ≤ 0.05) using k-means clustering. This clustering identified 10 distinct gene clusters of co-expressed genes. Samples clustered imperfectly by treatment type, with two of the three Tx + ɑCD4 day 6 samples showing distinct transcriptional programs (Fig. 4A–B, Fig. S5). These two samples had the smallest tumor size at time of necropsy, indicating they were already robustly responding to therapy at this time point. We next performed pathway enrichment analysis on the individual gene clusters. Of particular interest were cluster 1 and 2 (and to a lesser extent cluster 4), which were upregulated specifically in the Tx + ɑCD4 groups, and cluster 3, which contains genes upregulated in both the Tx + ɑCD4 and Tx groups and representing a Tx-specific transcriptional program (Fig. 4B). These clusters are enriched for a range of GO terms associated with productive cellular immune responses (regulation of T cell activation, alpha-beta T cell activation, lymphocyte mediated immunity, etc.). However, only clusters 1 and 2 were enriched for genes associated with interferon gamma production, suggesting that Tx alone is not sufficient to drive IFNγ production (Fig. 4C). Notably, because Tx + ɑCD4 and ɑCD4 drive similar levels of increased CD8+ T cell counts (Fig. 2F), but cytotoxic genes are only enriched in Tx + ɑCD4, we can conclude that this cytotoxic signature is not an artifact of increased CD8+ T cell counts. Cluster 7, which is highly expressed in PBS samples, contained genes enriched for, among others, pigmentation gene programs, likely representing increased CD45− tumor cells in this sample (Fig. 4C).
Figure 4. Tx + αCD4 upregulated gene clusters enriched for CD8+ effector programs.
(A) Heatmap of k-means clustered DEGs (absolute value lfc ≥ 2, FDR ≤ 10%) and tumor samples hierarchically clustered (n = 3–4) (B) Normalized expression of select individual gene clusters identified in (A) for each experimental condition. (C) Pathway enrichment analysis for each gene cluster identified in (A).
To further assess changes to the tumor microenvironment, we looked at DEGs between Tx + ɑCD4 tumor samples 3 and 6 days following ɑ4-1BB-LAIR. 63 genes were upregulated, and 43 genes downregulated between these two time points (FDR ≤ 5%, Fig. 5A). We used the upregulated DEGs to establish a “response” signature for Tx + ɑCD4. We then asked if this gene signature was expressed in any other treatment conditions/time points. Indeed, this signature was highly expressed only in the Tx + ɑCD4 late time point, indicating this was a bona fide response signature unique to Tx + ɑCD4 treated mice (Fig. 5B). We then performed pathway enrichment analysis to determine what pathways these genes were associated with. Confirming our previous flow data, we saw effector and effector memory T cell signatures. Additionally, we saw genes associated with TCR signaling, interleukin-2 (IL-2) signaling and Stat5a activity (Fig. 5C). Recent literature has highlighted a role for IL-2, or more broadly Stat5a activity, in amplifying T cell populations that drive responses to checkpoint blockade (57–59). Taken together, the tumor transcriptional data support the notion that Tx + ɑCD4 drives a robust cytotoxic T cell program leading to tumor rejection.
Figure 5. Tx + αCD4 associated with cytotoxic T cell signature in the tumor.
(A) Differential expression testing of Tx + αCD4 on day 3 vs. day 6 tumor samples relative to first α4-1BB-LAIR treatment, with statistically significant hits highlighted in red (FDR ≤ 5%). (B) Average expression level of significantly upregulated DEGs identified in (A) across all treatment groups. (C) Pathway enrichment analysis of upregulated DEGs identified in (A).
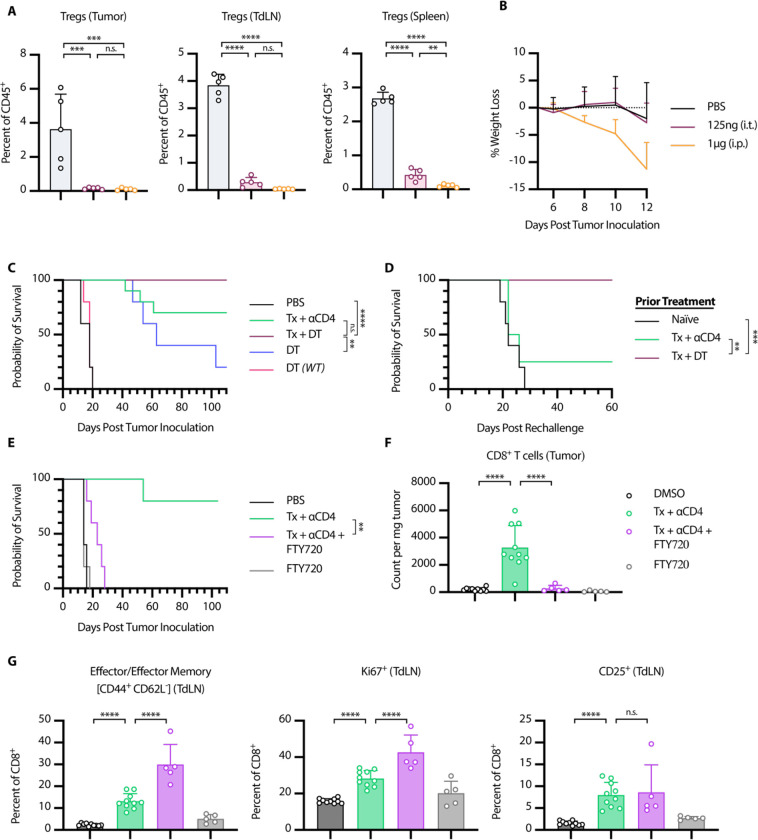
Treg depletion results in equivalent efficacy as whole CD4 compartment depletion
We hypothesized that Treg depletion was the primary functional consequence of ɑCD4 therapy, and that Treg specific elimination would lead to similar efficacy in combination with Tx. To test this hypothesis, we turned to Foxp3-DTR mice, which express the diphtheria toxin receptor (DTR) and GFP under control of the Foxp3 promoter. In these mice, all Foxp3+ cells are also DTR+, and thus susceptible to diphtheria toxin (DT) mediated cell death. Systemic administration of DT to these mice leads to rapid and complete depletion of nearly all Foxp3+ Tregs. However, with repeat dosing these mice succumb to lethal autoimmunity within 10–20 days of DT administration (39). In order to facilitate long term depletion of Tregs in the tumor and TdLN without inducing lethal autoimmunity, we developed a low dose, intratumoral diphtheria regimen. Every other day intratumoral dosing of 75ng or 125ng of DT depleted tumor and TdLN to similar levels as 1μg of systemically administered DT, with reduced impacts on splenic Treg populations (Fig. 6A, S6A). Additionally, we did not observe signs of toxicity, as measured by weight loss, with intratumoral low dose DT, while mice receiving systemic DT showed trends of weight loss at time of euthanasia (Fig. 6B, S6B). Thus, we felt confident that low dose intratumoral DT was a safe and effective model system to achieve long term intratumoral and intranodal Treg depletion
Figure 6. Tx + αCD4 is Treg dependent and requires de novo priming for efficacy.
(A-D) Foxp3-DTR Mice were inoculated with 1 × 106 B16F10 cells on day 0. (A) Mice were treated on days 6, 8, and 10 with either 125 ng DT (i.t.) or 1 μg DT (i.p.). Flow cytometry quantification (mean±SD) of Tregs in tumor, TdLN, or spleen on day 12 (gated on single cell/live/CD45+/CD3+NK1.1−/CD4+/GFP(Foxp3)+, n = 5). (B) Weight loss (mean+SD) of mice from (A). (C) Survival of Foxp3-DTR mice treated with PBS (n = 5), Tx + αCD4 (n = 10), Tx + DT (n = 10), DT (n = 5), WT mice treated with DT (n = 5). Mice were treated with the same relative dose/dose schedule as in Fig. 1A, but treatment initiation was delayed two days. DT treated mice received 125 ng DT (i.t.) every other day from day 6 to day 36. (D) Survival of complete responders to Tx + αCD4 or Tx + DT re-challenged on the contralateral flank >100 days after primary tumor inoculation. (E-G) WT mice were inoculated with 1 × 106 B16F10 cells on day 0. (E) Overall survival of mice treated with PBS/DMSO (n = 5), Tx + αCD4 (n = 5), Tx + αCD4 + FTY720 (n = 5), or FTY720 (n = 5). Mice were treated with the same relative dose/dose schedule as in Fig. 1A, but treatment initiation was delayed two days. Mice were treated with 30 μg of FTY720 (i.p.) every other day from days 6 to 36. (F) Flow cytometry quantification (mean±SD) of CD8+ T cell counts in tumor 6 days after first α4-1BB-LAIR treatment. (gated on single cell/Live/CD45+/CD3+NK1.1−/CD8+, n = 5–10, two independent experiments). (G) Flow cytometry quantification (mean±SD) of effector/effector memory (CD44+ CD62L−), CD25+, and Ki67+ CD8+ T cells in the TdLN 6 days after α4-1BB-LAIR treatment (gated on single cell/live/CD45+/CD3+NK1.1−/CD8+, n = 5–10, two independent experiments). Flow cytometry data was compared using one-way ANOVA with Tukey’s multiple hypothesis testing correction. Survival was compared using log-rank Mantel-Cox test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
B16F10 tumor-bearing Foxp3-DTR mice were treated with Tx + ɑCD4, Tx + DT, or DT alone. To allow for lesions of sufficient size for intratumoral administration of DT, the absolute timing of therapy administration was delayed two days for all groups (such that DT and ɑCD4 were initiated on day 6). Mice receiving Tx + DT responded equally as well as mice receiving Tx + ɑCD4, with a trend (but not statistically significant) towards a higher complete response rate in the Tx + DT group (Fig. 6C). Interestingly, DT on its own also resulted in significant growth delay, but ultimately almost all mice succumbed to their tumor burden. To confirm that the effect of DT was purely a result of Treg depletion, we treated WT mice with DT, which resulted in no different growth kinetics over PBS treated mice. No signs of toxicity, as assessed by weight loss, were observed throughout the course of treatment (Fig. S6C). A previously published study demonstrated that transient DT given with systemic ɑ4-1BB agonist therapy led to severe immune related adverse events (irAEs) in MC38 tumor bearing mice, further highlighting the advantages of our collagen-anchored ɑ4-1BB agonists (60). Notably, when cured mice were rechallenged >100 days after their primary tumor inoculation, the majority of the Tx + ɑCD4 cured mice did not reject rechallenge, consistent with previous results, while 100% of mice cured with Tx + DT rejected this rechallenge, demonstrating that these mice had developed robust immunological memory against B16F10 tumor antigens (Fig. 6D). This result demonstrated that 1) elimination of Tregs is sufficient to boost the efficacy of Tx and 2) elimination of Tregs alone while maintaining the CD4+ effector population allows for the proper formation of long-term immune memory.
Therapy induced de novo priming is necessary for therapeutic efficacy
Our data suggest that ɑCD4 mediates an increase in CD8+ T cell priming in the TdLN, which then leads to accumulation of newly primed CD8+ T cells in the tumor. However, an alternative explanation is that endogenous T cells already in the tumor locally proliferate and expand after ɑCD4 treatment. To test this hypothesis and assess if this intratumoral T cell expansion is critical to therapeutic efficacy, we treated tumor bearing mice with FTY720 concurrent with Tx + ɑCD4. FTY720 is a small molecule S1PR antagonist that prevents lymphocyte egress from lymphoid tissues, thus blocking any contributions from therapy-induced de novo priming to efficacy (61). FTY720 was initiated concurrently with the start of ɑCD4 treatment. To give sufficient time for the endogenous T cell response to develop before FTY720 initiation, treatment initiation was delayed two days (such that ɑCD4 and FTY720 were initiated on day 6 following tumor inoculation).
The addition of FTY720 to Tx + ɑCD4 abrogated therapeutic efficacy, with no complete responders and only minor tumor growth delay in this treatment cohort (Fig. 6E). Indeed, when we examined the tumor compartment via flow cytometry, addition of FTY720 to Tx + ɑCD4 dropped CD8+ T cell counts back to baseline (PBS/DMSO) levels (Fig. 6F). This confirmed that increases in CD8+ T cells in the tumor after Tx + ɑCD4 were due to de novo priming and trafficking from the TdLN and not local proliferation of T cells already in the tumor. The increased activation and proliferation in the TdLN (as measured by increased Ki67+ CD8+ T cells, increased CD25+ CD8+ T cells, and a shift to an effector/effector memory phenotype in the CD8+ T cell population) was preserved with the addition of FTY720, confirming that FTY720 prevented trafficking of these newly primed T cells to the tumor (Fig. 6G, Fig. 7A). Indeed, beginning ɑCD4 therapy 8 days before tumor inoculation maintained some efficacy of the combination; however, delaying initiation of ɑCD4 therapy to day 10 abrogated efficacy (Fig. S7B), consistent with ɑCD4’s role in priming (Fig. S7B).
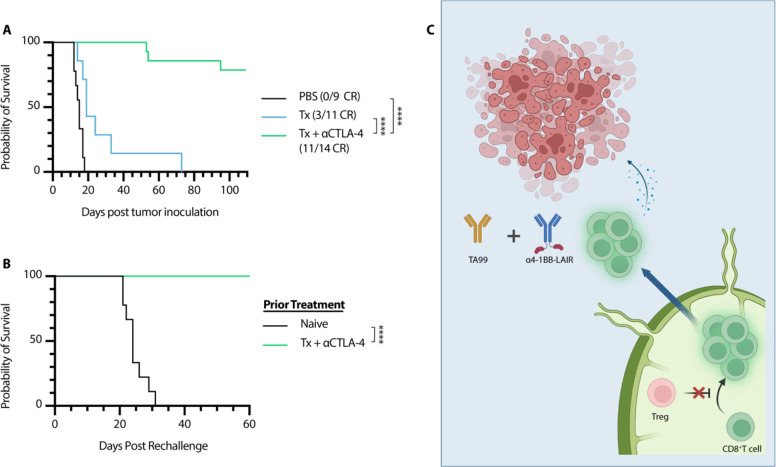
Figure 7. αCTLA-4 can replace αCD4 while maintaining efficacy and rescuing memory formation.
Mice were inoculated with 1 × 106 B16F10 cells on day 0. (A) Overall survival of mice treated either with PBS (n = 9, two independent studies), Tx (n = 7), or Tx + αCTLA-4 (n = 14, two independent studies). Mice were treated with the same dose/dose schedule as in Fig. 1A with 200 μg αCTLA-4 (i.p.) given on days 6, 9, 13, 16, 20, 23, and 27. (B) Survival of complete responders to Tx + αCTLA-4 re-challenged on the contralateral flank >100 days after primary tumor inoculation. (C) Graphical Abstract of proposed mechanism of action. Tregs in the TdLN constrain proper priming of tumor reactive CD8+ T cells, and inhibition or depletion of these cells results in a wave of newly primed CD8+ T cells entering the tumor, where their cytotoxic program is supported by TA99 and collagen-anchored α4-1BB-LAIR. Survival was compared using log-rank Mantel-Cox test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Interestingly, if initiation of FTY720 therapy was delayed just two days (concurrent with ɑ4-1BB-LAIR), therapeutic efficacy of this combination was restored and T cell counts in the tumor were restored to the same levels as Tx + ɑCD4 (Fig. S7C–E). For all FTY720 dosing schemes, blood T cell levels were significantly reduced compared to untreated mice, confirming that FTY720 was functioning as expected after treatment initiation (Fig. S7F). These data suggest that only a single priming wave is sufficient for efficacy of Tx + ɑCD4, and this priming wave occurs in a narrow time frame of two days following ɑCD4 initiation.
ɑCTLA-4 therapy also synergizes with TA99 + ɑ4-1BB-LAIR
Based on the presented data, we concluded that ɑCD4 synergizes with Tx by initiating a wave of de novo priming, that these new tumor-infiltrating T cells are supported by the local ɑ4-1BB-LAIR agonist and TA99, and that this two-step process ultimately drives therapeutic efficacy. We therefore hypothesized that other modalities capable of improving priming, such as ɑCTLA-4, would also synergize well with TA99 + ɑ4-1BB-LAIR. Although the dominant mechanism of ɑCTLA-4 is contested, literature supports that treatment with ɑCTLA-4 improves T cell priming and infiltration into the tumor (62). We therefore treated B16F10-bearing mice with Tx + ɑCTLA-4, and found that this combination was also highly efficacious, with an ~80% complete response rate (Fig. 7A, Fig. S8). We hypothesized that mice cured with Tx + ɑCTLA-4 would also generate robust immune memory and reject rechallenge as their CD4+ effector T cell pool remained intact. In agreement with this hypothesis, 100% of survivors rechallenged >100 days after initial tumor inoculation rejected this secondary tumor rechallenge (Fig. 7B).
DISCUSSION
ɑ4-1BB agonist antibodies have demonstrated robust efficacy as both a monotherapy and in combination with other immunotherapy agents in preclinical mouse models but have so far failed in the clinic due to dose-limiting toxicities. In this work, we set out to develop ɑ4-1BB antibodies with tumor-restricted activity via collagen anchoring. We have previously demonstrated that fusion of collagen binding proteins lumican or LAIR to extended half-life versions of IL-2 and IL-12 improves efficacy and limits toxicities when directly injected into tumors, even in relatively collagen-sparse B16F10 melanoma tumors, such as those used in this study (27, 28, 36).
To generate collagen anchored ɑ4-1BB antibodies, we fused murine LAIR1 to the C-terminus of the heavy chain of an ɑ4-1BB agonist antibody. We tested this agonist combination with a systemic antitumor antibody, TA99. We chose this combination because 1) ɑ4-1BB agonist Urelumab is currently being tested in combination with antitumor antibodies Cetuximab, Rituximab, and Elotuzumab and 2) a wide range of other antitumor antibodies which recognize antigens expressed on tumor cells are currently in the clinic (63). Antitumor antibodies have been demonstrated to improve antitumor immune responses by both generating antigenic cell debris to enhance T cell priming and also by reprogramming myeloid cells in the tumor through Fc:FcγR interactions (64). In agreement with preliminary phase 1 data, this combination did not result in robust efficacy in our hands, with only minor growth delay and complete responses in ~5% of treated mice (48). However, we unexpectedly discovered that depletion of the entire CD4+ T cell compartment throughout the course of this combination therapy dramatically improved response rates, with >90% of mice achieving durable complete responses. A similarly efficacious combination (systemic ɑ4-1BB + ɑCD4) has been reported in the literature, although durable responses were not seen, with all mice succumbing to their tumors between day 70–80 (49). To our knowledge, this is the highest complete response rate seen of any ɑ4-1BB agonist antibody therapy in the poorly immunogenic B16F10 melanoma tumor model.
As Tregs comprise a sizable portion of the CD4+ T cell compartment, we tested Treg depletion in lieu of whole CD4+ T cell depletion using Foxp3-DTR mice in combination with TA99 + ɑ4-1BB-LAIR and observed equivalent efficacy. While Tregs play a crucial role in preventing autoimmunity, they also constrain productive antitumor immune responses. Intratumoral Treg infiltration is correlated with poor prognosis across many different tumor types and there is evidence that intranodal Tregs infiltration is a better predictor of survival than blood or intratumoral Tregs in certain contexts (65–68). Tregs exert their effects through multiple different pathways, including secretion of immunosuppressive cytokines such as IL-10, Transforming Growth Factor-beta (TGF-β), and IL-35, acting as a sink for IL-2 due to their high expression of the IL-2 high affinity receptor CD25, generation of immunosuppressive adenosine through expression of CD39, and expression of inhibitory receptors such as CTLA-4 and LAG-3 (43, 44).
Tregs are a major contributor to the immunosuppressive environment of the tumor, but they can also interfere with CD8+ T cell priming in lymphoid tissues (69, 70). Even prior to the identification of the transcription factor Foxp3 as the canonical driver of Tregs, seminal work found that depletion of CD25+ T cells (a subset of which are Tregs) before tumor implantation can lead to enhanced antitumor immune responses and eventual spontaneous tumor rejection (71). Although how Tregs constrain priming is multifaceted, it is well established that CTLA-4 expressed on Tregs can transendocytose CD80 and CD86 off the surface of dendritic cells, hampering their ability to provide proper co-stimulation and prime CD8+ T cells (72–74). Blocking this transendocytosis is thought to at least partially explain the mechanism of how ɑCTLA-4 therapy functions to improve priming. Indeed, we show ɑCTLA-4 synergized as well as complete CD4+ T cell or Treg specific depletion with TA99 + ɑ4-1BB-LAIR. Our work supports the notion that intranodal Tregs dampen antitumor immune responses by constraining proper priming, and that relieving this constraint can bolster the magnitude of the antitumor T cell response and synergize robustly with T cell directed agonist immunotherapies, particularly in immunologically cold tumors such as the one used in this study.
Although long-term CD4+ T cell compartment depletion leads to obvious defects in both T and B cell adaptive immune responses, transient CD4+ T cell depletion has been clinically tested in cancer and other disease states using an ɑCD4 antibody. Transient ɑCD4 depletion resulted in similar increases in de novo priming and CD8+ T cell infiltration in the tumor, consistent with our own data (52, 53). However, although no adverse events have been reported in these small phase 1 trials, these patients are still at risk of severe and possibly fatal infections if exposed to pathogens while devoid of their CD4+ compartment. Additionally, although ɑCD4 depletion therapy synergized well with TA99 + ɑ4-1BB-LAIR, mice failed to form immunological memory, which can be important for long term tumor control and control of distant metastases. In patients, the presence of memory T cells corresponds with breast cancer survival and memory T cells have been reported to persist in survivors of melanoma treated with immunotherapy for at least 9 years (75, 76). With this in mind, we set out to understand the mechanism of how CD4+ T cell compartment depletion synergized with TA99 + ɑ4-1BB-LAIR and develop new combination therapies with higher translational potential. Our data demonstrated that CD4+ T cell depletion eliminated Tregs in the TdLN, removing immunosuppressive constraints on proper CD8+ T cell priming, and induced a wave of freshly primed T cells to enter the TME. The combination of TA99 + ɑ4-1BB-LAIR is able to reprogram the TME into a more supportive environment for these newly primed T cells, allowing them to maintain their cytotoxic phenotype, leading to tumor regression and clearance (Fig. 7C). Indeed, recent data has suggested a two-step model for CD8+ T cell activation in cancer, with initial activation in the TdLN and effector differentiation occurring with co-stimulation in the tumor (77). The two components of our therapy mirror this paradigm, with ɑCD4 increasing activation in the TdLN and TA99 + ɑ4-1BB-LAIR enhancing effector functions of these newly activated CD8+ T cells directly in the tumor.
This localized therapy is reliant on intratumoral administration of the ɑ4-1BB-LAIR component, which is clinically feasible with advances in interventional radiology (78–80). Indeed, the oncolytic virus therapy talimogene laherparepvec (T-vec) has been approved since 2015 and is routinely injected into cutaneous and subcutaneous unresectable melanoma lesions (81, 82). Preclinical and clinical development around intratumorally administered therapies have been steadily on the rise.
This study has the potential for immediate translational impact. Since both antitumor antibodies and ɑCTLA-4 antagonists are approved and routinely used in clinically, they could easily be combined with clinical stage localized ɑ4-1BB agonists. Indeed, our data demonstrated that even non-collagen anchored ɑ4-1BB agonists synergize fairly well with antitumor antibodies in combination with ɑCTLA-4 therapy, identifying a potential triple combination therapy whose individual components are all already in clinical use.
In conclusion, we found that effective TA99 + ɑ4-1BB-LAIR therapy requires a wave of de novo CD8+ T cell priming to achieve maximum efficacy. In this study, we generated this enhanced priming wave through whole CD4+ T cell compartment depletion with an ɑCD4 depleting antibody, Treg specific ablation using Foxp3-DTR mice, or treatment with ɑCTLA-4, a modality known to increase priming. These combinations resulted in high levels of primary tumor efficacy, with ~80–100% complete response rates. However, only in the latter two strategies, which preserved CD4+ effector T cells, did mice also develop robust long-term immunological memory, with 100% of cured mice rejecting secondary tumor rechallenge. Our data demonstrate that at baseline, proper CD8+ T cell priming is constrained by Tregs present in the TdLN. All three priming enhancing strategies are directed towards Tregs, either depleting them completely (ɑCD4 and DT), or blocking their immunosuppressive pathways (ɑCTLA-4). This provides strong rationale for development of Treg-directed therapies that modulate Treg function in the TdLN which, in combination with proper immune agonists, can drive high levels of efficacy even in immunologically cold tumors.
MATERIALS AND METHODS
Study Design
The purpose of this study was to (i) evaluate the efficacy and safety of collagen anchoring ɑ4-1BB-LAIR and subsequently to (ii) understand the mechanism driving synergy between TA99 + ɑ4-1BB-LAIR and ɑCD4 and finally to (iii) identity more clinically relevant therapies that synergize with TA99 + ɑ4-1BB-LAIR. We used the syngeneic murine melanoma line B16F10 for all studies. Mice were randomized before beginning treatment to ensure equal tumor size in all groups and were monitored for tumor size and weight loss until euthanasia or until complete tumor regression. Investigators were not blinded during the studies. In all studies there were at least 5 mice per experimental group, except for the bulk RNA-sequencing experiment which had 3–4 mice per group. No data/experiments were excluded unless there were technical issues with the experiment, and outliers were not excluded. Many experiments were repeated twice, and number of mice per group, number of experimental repeats, and statistical methods are noted in figure legends.
Mice
C57Bl/6 (C57Bl/6NTac) mice were purchased from Taconic. C57Bl/6 albino (B6(Cg)-Tyrc−2J/J) mice were purchased from The Jackson Laboratory. C57Bl/6 Foxp3-DTR(B6.129(Cg)-Foxp3tm3(DTR/GFP)Ayr/J) mice were a gift from the Spranger lab (MIT). B6 Foxp3-DTR mice were bred in house and genotyped using Transnetyx. All animal work was conducted under the approval of the Massachusetts Institute of Technology Committee on Animal Care in accordance with federal, state, and local guidelines.
Cells
B16F10 cells were purchased from ATCC. Apigmented B16F10 cells used for imaging were generated by genetic deletion of Tyrosinase-related-protein-2 (TRP2), referred to as B16F10-Trp2 KO cells (83). Tumor cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM, ATCC) supplemented with 10% Fetal Bovine Serum (FBS, Gibco). FreeStyle 293-F cells and Expi293 cells were purchased from Invitrogen and cultured in FreeStyle expression medium (Gibco) and Expi293 expression medium (Gibco), respectively. CHO DG44 cells were cultured in ProCHO5 (Lonza) supplemented with 4 mM L-glutamine, 0.1 mM hypoxanthine, and 16 μM thymidine. Tumor cells were maintained at 37°C and 5% CO2 and FreeStyle 293-F cells, Expi293 cells, and CHO DG44 cells were maintained at 37°C and 8% CO2. All cells tested negative for mycoplasma contamination.
Tumor Inoculation and Treatment
Mice were aged six to twelve weeks before tumor inoculations. 1 × 106 B16F10 or B16F10-Trp2KO cells were suspended in 50uL sterile PBS (Corning) and injected subcutaneously on the right flank.
Mice were randomized before beginning treatment to ensure equal tumor size in all groups. TA99 was administered intraperitoneally (i.p) at a dose of 200 μg in 200 μL sterile PBS (Corning). ɑ4-1BB or ɑ4-1BB-LAIR was administered intratumorally (i.t.) in 20 μL of sterile PBS (Corning) at a dose of 30 μg or 36.1 μg (molar equivalents), respectively. ɑCD4 (Clone GK1.5, Bioxcell) was administered i.p. at a dose of 400 μg in 100 μL sterile PBS (Corning). ɑCTLA-4 (Clone 9D9, mIgG2c isotype) was administered i.p. at a dose of 200 μg in 100 μL of sterile PBS (Corning). Diphtheria Toxin (DT, Sigma Aldrich) was administered i.p. at a dose of 1 μg in 100 μL sterile PBS (Corning) or i.t. at a dose of 75 ng or 125 ng in 20 μL sterile PBS (Corning). Stock solutions of FTY720 (Sigma Aldrich) were resuspended at 10 mg/mL in DMSO and diluted to a dose of 30 μg in sterile PBS (Corning) to a final volume of 150 μL and administered i.p.
TA99 was dosed on days 5, 12, 19, and 26 and ɑ4-1BB and ɑ4-1BB-LAIR were administered on days 6, 13, 20, and 27. ɑCD4 was administered starting on day 4 and continued every three days until day 37 (Fig. 1A). For some studies, therapy initiation was delayed by 2 days to allow for larger tumors at time of analysis (flow cytometry, chemokine/cytokine analysis, and bulk-RNA-sequencing), sufficiently sized tumors for intratumoral DT administration (DT survival studies), or to avoid interfering with the endogenous T cell response (FTY720 studies, except Fig. S7C which followed Fig. 1A dosing scheme). DT was administered every other day starting on day 6 and continued until day 36. FTY720 was administered starting concurrently with ɑCD4 and continued every other day until one week after final ɑ4-1BB-LAIR dose. “Delayed” FTY720 was administered starting concurrently with ɑ4-1BB-LAIR and continued every other day until one week after final ɑ4-1BB-LAIR dose. ɑCTLA-4 was given on days 6, 9, 13, 16, 20, 23, and 27.
During all tumor studies, mice were monitored continuously for tumor growth and weight change. Tumor growth was assessed by direct measurement with calipers and mice were euthanized when their tumor area (length × width) reached 100 mm2 or mice lost more than 20% of their body weight. Mice that were cured of their primary tumor but later euthanized due to overgrooming related dermatitis were still classified as complete responders and included in analysis.
For rechallenge studies, mice that rejected their primary tumors were inoculated with 1 × 105 B16F10 tumor cells on the left, or contralateral, flank 100–110 days after primary tumor inoculation and monitored for tumor outgrowth. Age matched naïve mice were used as controls in these studies
Flow Cytometry
Tumors were excised, weighed, and mechanically dissociated before being enzymatically digested using a gentleMACS Octo Dissociator with Heaters (Miltenyi Biotec) in gentleMACS C tubes (Miltenyi Biotec) and enzymes from the Mouse Tumor Dissociation Kit (Miltenyi Biotec). Tumors were digested using the 37C_m_TDK_1 program for soft tumors. Following digestion, tumors were filtered through a 40 μm filter and transferred to a V-bottom 96 well plate for staining. TdLN and spleens were excised, weighed, and mechanically dissociated through a 70 μm filter. Spleen samples were resuspended with 5 mL of ACK Lysis buffer (Gibco) to lyse red blood cells before being re-filtered through a 70 μm filter. TdLN and spleen samples were then transferred to a V-bottom 96 well plate for staining. Blood samples were collected via cardiac puncture into K3 EDTA coated tubes (MiniCollect). 200 μL of blood was mixed with 1 mL of ACK lysis buffer (Gibco) to lyse red blood cells before being transferred to a V-bottom 96 well plate for staining. Precision Counting Beads (Biolegend) were added to each well to account for sample loss during processing and obtain accurate counts. Cells were washed once with PBS and then resuspended in Zombie UV Fixable Viability Dye (Biolegend) to stain dead cells for 30 minutes at RT in the dark. Cells were then washed with FACS buffer (PBS (Corning) + 0.1% BSA (Sigma Aldrich) + 2mM EDTA (Gibco)) and blocked with αCD16/CD32 antibody (Clone 93, eBioscience) for 20 minutes on ice in the dark and then stained for extracellular markers for 30 minutes on ice in the dark. Samples not requiring intracellular staining were washed with FACS buffer and fixed with BD Cytofix (BD Biosciences) for 30 minutes at RT in the dark. Cells were then washed and resuspended in FACS buffer. For samples requiring intracellular staining, cells were washed after extracellular staining, fixed and permeabilized with the Foxp3/Transcription Factor Staining Buffer Set (eBiosciences), and stained for 30 minutes at RT in the dark, before being washed and resuspended in FACS buffer. Samples were analyzed with a BD FACS Symphony A3 (BD Biosciences) and data was processed and analyzed with FlowJo V10. See Figure S9 for example gates.
Tumor and TdLN samples in Figures 2 and S4 were stained with αCD45-BUV395 (30-F11, BD Biosciences), αCD4-BUV563 (RM4-4, BD Biosciences), αCD8ɑ-BUV737 (53–6.7 BD Biosciences), αCD62L-BUV805 (MEL-14, BD Biosciences), αCD44-BV421 (1M7, Biolegend), αKi67-BV605 (16A8, Biolegend), αCD3-BV711 (17A2, Biolegend), αTIM-3-BV785 (RMT3-23, Biolegend), αTCF1/TCF7-AF488 (C63D9, Cell Signaling Technology), αPD-1-PerCp/Cy5.5 (29F.1A12, Biolegend), αFoxp3-PE (FJK-16s, Invitrogen), αCD25-PE-Cy5 (PC61, Biolegend), αNK1.1-PE-Cy7 (PK126, Biolegend), α4-1BB-APC (17B5, Biolegend), αCD107a-APC-Cy7 (1D4B, Biolegend).
Tumor, TdLN, and spleen samples in Figure 5A and S6 were stained with αCD45-BUV395 (30F-11, BD Bioscience), αCD8a-BUV737 (53–6.7, BD Biosciences), αCD3-BV785 (17A2, Biolegend), αNK1.1-PE-Cy7 (PK-136, Biolegend), αCD4-APC-Cy7 (GK1.5, Biolegend), and Foxp3+ cells were identified using the GFP reporter expressed under the Foxp3 locus in Foxp3-DTR mice.
Tumor, TdLN and blood samples in Figures 5F–G and S7 were stained with αCD45-BUV395 (30-F11, BD Biosciences), αCD4-BUV563 (RM4-4, BD Biosciences), αCD44-BUV737 (1M7 BD Biosciences), αKi67-BV421 (16A8, Biolegend), αCD3-BV711 (17A2, Biolegend), αCD8a-FITC (53–6.7, Biolegend) αFoxp3-PE (FJK-16s, Invitrogen), αCD25-PE-Cy5 (PC61, Biolegend), αNK1.1-PE-Cy7 (PK126, Biolegend), αCD62L-APC (MEL-14, Biolegend), αCD107a-APC-Cy7 (1D4B, Biolegend).
RNA extraction for Sequencing
Tumor samples were processed as previously described. Samples were enriched for CD45+ cells using an EasySep Mouse TIL (CD45) Positive Selection kit (STEMCELL) and RNA was extracted with an RNeasy Plus Mini Kit (Qiagen). TdLN samples were processed as previously described. Samples were again enriched for CD45+ cells using an EasySep Mouse CD45 Positive Selection kit (STEMCELL) and RNA was extracted with an RNeasy Plus Mini Kit (Qiagen). RNA was stored at −80°C until further processing.
RNA-seq Library Preparation and Sequencing
RNA-sequencing was performed by the BioMicro Center at MIT using a modified version of the SCRB-seq protocol (84). Libraries were sequenced on a NextSeq 500 using a 75-cycle kit.
RNA-seq Alignment, Quantification, and Quality Control
Data preprocessing and count matrix construction were performed using the Smart-seq2 Multi-Sample v2.2.0 Pipeline (RRID:SCR_018920) on Terra. For each cell in the batch, single-end FASTQ files were first processed with the Smart-seq2 Single Sample v5.1.1 Pipeline (RRID:SCR_021228). Reads were aligned to the GENCODE mouse (M21) reference genome using HISAT2 v2.1.0 with default parameters in addition to --k 10 options. Metrics were collected and duplicate reads marked using the Picard v.2.10.10 CollectMultipleMetrics and CollectRnaSeqMetrics, and MarkDuplicates functions with validation_stringency=silent. For transcriptome quantification, reads were aligned to the GENCODE transcriptome using HISAT2 v2.1.0 with --k 10 --no-mixed --no-softclip --no-discordant --rdg 99999999,99999999 --rfg 99999999,99999999 --no-spliced-alignment options. Gene expression was calculated using RSEM v1.3.0’s rsem-calculate-expression --calc-pme --single-cell-prior. QC metrics, RSEM TPMs and RSEM estimated counts were exported to a single Loom file for each sample. All individual Loom files for the entire batch were aggregated into a single Loom file for downstream processing. The final output included the unfiltered Loom and the tagged, unfiltered individual BAM files.
RNA-Seq Analysis
Samples with less than 10,000 genes detected were excluded from analysis. This led to exclusion of two tumor samples, one from the Tx + ɑCD4 group and one from the ɑCD4 group at the day 6 time point (Fig. S10). UMAP embedding of TdLN samples was generated from the top 5 principal components and top 3000 variable features. DEseq2 was used to conduct differential expression testing and apeglm was used for effect size estimation (85, 86). Pathways enrichment analysis for statistically significant upregulated genes was performed using enrichR to query the databases indicated in the text (54–56). A score for the derived response gene signature was calculated for each experimental cohort using Seurat (AddModuleScore) (87). Differential expression testing was performed as described above comparing all tumor sample cohorts to the D3 PBS, D6 PBS, D3 Tx + aCD4, and D6 Tx + aCD4 cohorts. All statistically significant hits (p-adj ≦5 with absolute value log2 fold-change ≥ 2 were included for further analysis. Gene clusters were defined using k-means clustering and the complexHeatmap package was used to generate expression heatmaps for these genes (88). Relative expression profiles of these gene clusters were generated by summarizing the percent expression using Seurat (PercentageFeatureSet) per sample and dividing by the highest average percent per condition (87). Gene sets were obtained from MSigDB and enrichment of genes from each cluster in these gene sets was calculated using the enrichGO package (89).
Statistical Methods
Statistics were computed in GraphPad Prism v9 as indicated in figure captions. Survival studies were compared using the log-rank (Mantel-Cox) test. Flow data and tumor supernatant cytokine/chemokine data were compared using one- or two-way ANOVA with Tukey’s multiple comparison correction. Differential expression analysis using DESeq2 models counts for each gene using a negative binomial model and tests for significance using Wald tests (86). Gene set enrichment is calculated by the Fisher’s exact test. P values are corrected for multiple hypothesis testing using the Benjamini-Hochberg procedure for all RNA-sequencing analysis. Sample size and P-value cutoffs are indicated in figure captions.
Supplementary Material
Acknowledgement:
We thank the Koch Institute’s Robert A. Swanson (1969) Biotechnology Center (National Cancer Institute Grant P30-CA14051) for technical support, specifically the Flow Cytometry Core Facility and the BioMicro Center. We thank the Spranger lab for the gift of the Foxp3-DTR breeding pair. We thank the Protein Production and Structure Core Facility at the École polytechnique fédérale de Lausanne for the development of the 9D9 stable line. Figures partially created with biorender.com.
Funding:
NCI CA271243, NIBIB EB031082
NSF Graduate Research Fellowship Program (JRP, BML, LS, EAL)
Ludwig Center at MIT Graduate Fellowship (LRD)
Footnotes
Competing Interest:
JRP and KDW are inventors on U.S. Provisional Patent application no. 62/738,981 regarding the aforementioned collagen-anchoring immunomodulatory molecules and methods thereof. Cullinan Oncology is the assignee of this patent application. KDW is a consultant/advisor for Cullinan Oncology. All other authors declare that they have no competing interests.
Data and materials availability:
All raw data or materials are available upon request. Sequencing data can be found in the GEO database under accession GSE223087.
References
- 1.Scott A. M., Wolchok J. D., Old L. J., Antibody therapy of cancer. Nat Rev Cancer. 12, 278–287 (2012). [DOI] [PubMed] [Google Scholar]
- 2.Jhajj H. S., Lwo T. S., Yao E. L., Tessier P. M., Unlocking the potential of agonist antibodies for treating cancer using antibody engineering. Trends Mol Med. 29, 48–60 (2023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayes P. A., Hance K. W., Hoos A., The promise and challenges of immune agonist antibody development in cancer. Nat Rev Drug Discov. 17, 509–527 (2018). [DOI] [PubMed] [Google Scholar]
- 4.Borghaei H., Gettinger S., Vokes E. E., Chow L. Q. M., Burgio M. A., Carpeno J. de C., Pluzanski A., Arrieta O., Frontera O. A., Chiari R., Butts C., Wójcik-Tomaszewska J., Coudert B., Garassino M. C., Ready N., Felip E., García M. A., Waterhouse D., Domine M., Barlesi F., Antonia S., Wohlleber M., Gerber D. E., Czyzewicz G., Spigel D. R., Crino L., Eberhardt W. E. E., Li A., Marimuthu S., Brahmer J., Five-Year Outcomes From the Randomized, Phase III Trials CheckMate 017 and 057: Nivolumab Versus Docetaxel in Previously Treated Non–Small-Cell Lung Cancer. J Clin Oncol. 39, 723–733 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolchok J. D., Chiarion-Sileni V., Gonzalez R., Grob J.-J., Rutkowski P., Lao C. D., Cowey C. L., Schadendorf D., Wagstaff J., Dummer R., Ferrucci P. F., Smylie M., Butler M. O., Hill A., Márquez-Rodas I., Haanen J. B. A. G., Guidoboni M., Maio M., Schöffski P., Carlino M. S., Lebbé C., McArthur G., Ascierto P. A., Daniels G. A., Long G. V., Bas T., Ritchings C., Larkin J., Hodi F. S., Long-Term Outcomes With Nivolumab Plus Ipilimumab or Nivolumab Alone Versus Ipilimumab in Patients With Advanced Melanoma. J Clin Oncol. 40, 127–137 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vinay D. S., Kwon B. S., 4-1BB signaling beyond T cells. Cell Mol Immunol. 8, 281–284 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drenkard D., Becke F. M., Langstein J., Spruss T., Kunz-Schughart L. A., Tan T. E., Lim Y. C., Schwarz H., CD137 is expressed on blood vessel walls at sites of inflammation and enhances monocyte migratory activity. FASEB J. 21, 456–463 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Teijeira Á., Palazón A., Garasa S., Marré D., Aubá C., Rogel A., Murillo O., Martínez-Forero I., Lang F., Melero I., Rouzaut A., CD137 on inflamed lymphatic endothelial cells enhances CCL21-guided migration of dendritic cells. FASEB J. 26, 3380–3392 (2012). [DOI] [PubMed] [Google Scholar]
- 9.Watts T. H., TNF/TNFR family members in costimulation of T cell responses. Annu Rev Immunol. 23, 23–68 (2005). [DOI] [PubMed] [Google Scholar]
- 10.Kwon B. S., Weissman S. M., cDNA sequences of two inducible T-cell genes. Proc National Acad Sci. 86, 1963–1967 (1989). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi B. K., Lee D. Y., Lee D. G., Kim Y. H., Kim S.-H., Oh H. S., Han C., Kwon B. S., 4-1BB signaling activates glucose and fatty acid metabolism to enhance CD8+ T cell proliferation. Cell Mol Immunol. 14, 748–757 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee H., Nam K., Park S., Kwon B. S., 4-1BB enhances CD8+ T cell expansion by regulating cell cycle progression through changes in expression of cyclins D and E and cyclin-dependent kinase inhibitor p27kip1. Eur J Immunol. 33, 2133–2141 (2003). [DOI] [PubMed] [Google Scholar]
- 13.Lee H.-W., Park S.-J., Choi B. K., Kim H. H., Nam K.-O., Kwon B. S., 4-1BB Promotes the Survival of CD8+ T Lymphocytes by Increasing Expression of Bcl-xL and Bfl-1. J Immunol. 169, 4882–4888 (2002). [DOI] [PubMed] [Google Scholar]
- 14.Willoughby J. E., Kerr J. P., Rogel A., Taraban V. Y., Buchan S. L., Johnson P. W. M., Al-Shamkhani A., Differential Impact of CD27 and 4-1BB Costimulation on Effector and Memory CD8 T Cell Generation following Peptide Immunization. J Immunol. 193, 244–251 (2014). [DOI] [PubMed] [Google Scholar]
- 15.Shuford W. W., Klussman K., Tritchler D. D., Loo D. T., Chalupny J., Siadak A. W., Brown T. J., Emswiler J., Raecho H., Larsen C. P., Pearson T. C., Ledbetter J. A., Aruffo A., Mittler R. S., 4-1BB Costimulatory Signals Preferentially Induce CD8+ T Cell Proliferation and Lead to the Amplification In Vivo of Cytotoxic T Cell Responses. J Exp Med. 186, 47–55 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melero I., Shuford W. W., Newby S. A., Aruffo A., Ledbetter J. A., Hellström K. E., Mittler R. S., Chen L., Monoclonal antibodies against the 4-1BB T-cell activation molecule eradicate established tumors. Nat Med. 3, 682–685 (1997). [DOI] [PubMed] [Google Scholar]
- 17.Melero I., Sanmamed M. F., Glez-Vaz J., Luri-Rey C., Wang J., Chen L., CD137 (4-1BB)-Based Cancer Immunotherapy on Its 25th Anniversary. Cancer Discov, OF1–OF19 (2022). [DOI] [PubMed] [Google Scholar]
- 18.Segal N. H., Logan T. F., Hodi F. S., McDermott D., Melero I., Hamid O., Schmidt H., Robert C., Chiarion-Sileni V., Ascierto P. A., Maio M., Urba W. J., Gangadhar T. C., Suryawanshi S., Neely J., Jure-Kunkel M., Krishnan S., Kohrt H., Sznol M., Levy R., Results from an Integrated Safety Analysis of Urelumab, an Agonist Anti-CD137 Monoclonal Antibody. Clin Cancer Res. 23, 1929–1936 (2017). [DOI] [PubMed] [Google Scholar]
- 19.Chin S. M., Kimberlin C. R., Roe-Zurz Z., Zhang P., Xu A., Liao-Chan S., Sen D., Nager A. R., Oakdale N. S., Brown C., Wang F., Yang Y., Lindquist K., Yeung Y. A., Salek-Ardakani S., Chaparro-Riggers J., Structure of the 4-1BB/4-1BBL complex and distinct binding and functional properties of utomilumab and urelumab. Nat Commun. 9, 4679 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segal N. H., He A. R., Doi T., Levy R., Bhatia S., Pishvaian M. J., Cesari R., Chen Y., Davis C. B., Huang B., Thall A. D., Gopal A. K., Phase I Study of Single-Agent Utomilumab (PF-05082566), a 4-1BB/CD137 Agonist, in Patients with Advanced Cancer. Clin Cancer Res. 24, 1816–1823 (2018). [DOI] [PubMed] [Google Scholar]
- 21.Etxeberria I., Glez-Vaz J., Teijeira Á., Melero I., New emerging targets in cancer immunotherapy: CD137/4-1BB costimulatory axis. ESMO Open. 4, e000733 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Etxeberria I., Bolaños E., Teijeira A., Garasa S., Yanguas A., Azpilikueta A., Kavanaugh W. M., Vasiljeva O., Belvin M., Howng B., Irving B., Tipton K., West J., Mei L., Korman A. J., Sega E., Olivera I., Cirella A., Ochoa M. C., Rodriguez M. E., Melero A., Sanmamed M. F., Engelhardt J. J., Melero I., Antitumor efficacy and reduced toxicity using an anti-CD137 Probody therapeutic. Proc National Acad Sci. 118, e2025930118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hinner M. J., Aiba R. S. B., Jaquin T. J., Berger S., Dürr M. C., Schlosser C., Allersdorfer A., Wiedenmann A., Matschiner G., Schüler J., Moebius U., Rothe C., Matis L., Olwill S. A., Tumor-Localized Costimulatory T-Cell Engagement by the 4-1BB/HER2 Bispecific Antibody-Anticalin Fusion PRS-343. Clin Cancer Res. 25, 5878–5889 (2019). [DOI] [PubMed] [Google Scholar]
- 24.Claus C., Ferrara C., Xu W., Sam J., Lang S., Uhlenbrock F., Albrecht R., Herter S., Schlenker R., Hüsser T., Diggelmann S., Challier J., Mössner E., Hosse R. J., Hofer T., Brünker P., Joseph C., Benz J., Ringler P., Stahlberg H., Lauer M., Perro M., Chen S., Küttel C., Mohan P. L. B., Nicolini V., Birk M. C., Ongaro A., Prince C., Gianotti R., Dugan G., Whitlow C. T., Sai K. K. S., Caudell D. L., Burgos-Rodriguez A. G., Cline J. M., Hettich M., Ceppi M., Giusti A. M., Crameri F., Driessen W., Morcos P. N., Freimoser-Grundschober A., Levitsky V., Amann M., Grau-Richards S., von Hirschheydt T., Tournaviti S., Mølhøj M., Fauti T., Heinzelmann-Schwarz V., Teichgräber V., Colombetti S., Bacac M., Zippelius A., Klein C., Umaña P., Tumor-targeted 4-1BB agonists for combination with T cell bispecific antibodies as off-the-shelf therapy. Sci Transl Med. 11, eaav5989 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kamata-Sakurai M., Narita Y., Hori Y., Nemoto T., Uchikawa R., Honda M., Hironiwa N., Taniguchi K., Shida-Kawazoe M., Metsugi S., Miyazaki T., Wada N. A., Ohte Y., Shimizu S., Mikami H., Tachibana T., Ono N., Adachi K., Sakiyama T., Matsushita T., Kadono S., Komatsu S., Sakamoto A., Horikawa S., Hirako A., Hamada K., Naoi S., Savory N., Satoh Y., Sato M., Noguchi Y., Shinozuka J., Kuroi H., Ito A., Wakabayashi T., Kamimura M., Isomura F., Tomii Y., Sawada N., Kato A., Ueda O., Nakanishi Y., Endo M., Jishage K., Kawabe Y., Kitazawa T., Igawa T., Antibody to CD137 Activated by Extracellular Adenosine Triphosphate Is Tumor Selective and Broadly Effective In Vivo without Systemic Immune Activation. Cancer Discov. 11, 158–175 (2021). [DOI] [PubMed] [Google Scholar]
- 26.Muik A., Garralda E., Altintas I., Gieseke F., Geva R., Ben-Ami E., Maurice-Dror C., Calvo E., LoRusso P. M., Alonso G., Rodriguez-Ruiz M. E., Schoedel K. B., Blum J. M., Sänger B., Salcedo T. W., Burm S. M., Stanganello E., Verzijl D., Vascotto F., Sette A., Quinkhardt J., Plantinga T. S., Toker A., van den Brink E. N., Fereshteh M., Diken M., Satijn D., Kreiter S., Breij E. C. W., Bajaj G., Lagkadinou E., Sasser K., Türeci Ö., Forssmann U., Ahmadi T., Şahin U., Jure-Kunkel M., Melero I., Preclinical Characterization and Phase I Trial Results of a Bispecific Antibody Targeting PD-L1 and 4-1BB (GEN1046) in Patients with Advanced Refractory Solid Tumors (GEN1046), a Bispecific Antibody Targeting PD-L1 and 4-1BB. Cancer Discov. 12, 1248–1265 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Momin N., Mehta N. K., Bennett N. R., Ma L., Palmeri J. R., Chinn M. M., Lutz E. A., Kang B., Irvine D. J., Spranger S., Wittrup K. D., Anchoring of intratumorally administered cytokines to collagen safely potentiates systemic cancer immunotherapy. Sci Transl Med. 11, eaaw2614 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Momin N., Palmeri J. R., Lutz E. A., Jailkhani N., Mak H., Tabet A., Chinn M. M., Kang B. H., Spanoudaki V., Hynes R. O., Wittrup K. D., Maximizing response to intratumoral immunotherapy in mice by tuning local retention. Nat Commun. 13, 109 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mansurov A., Ishihara J., Hosseinchi P., Potin L., Marchell T. M., Ishihara A., Williford J.-M., Alpar A. T., Raczy M. M., Gray L. T., Swartz M. A., Hubbell J. A., Collagen-binding IL-12 enhances tumour inflammation and drives the complete remission of established immunologically cold mouse tumours. Nat Biomed Eng. 4, 531–543 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ishihara J., Ishihara A., Potin L., Hosseinchi P., Fukunaga K., Damo M., Gajewski T. F., Swartz M. A., Hubbell J. A., Improving Efficacy and Safetty of Agonistic Anti-CD40 Antibody Through Extracellular Matrix Affinity. Mol Cancer Ther. 17, 2399–2411 (2018) [DOI] [PubMed] [Google Scholar]
- 31.Ishihara J., Fukunaga K., Ishihara A., Larsson H. M., Potin L., Hosseinchi P., Galliverti G., Swartz M. A., Hubbell J. A., Matrix-binding checkpoint immunotherapies enhance antitumor efficacy and reduce adverse events. Sci Transl Med. 9, eaan0401 (2017). [DOI] [PubMed] [Google Scholar]
- 32.Mansurov A., Hosseinchi P., Chang K., Lauterbach A. L., Gray L. T., Alpar A. T., Budina E., Slezak A. J., Kang S., Cao S., Solanki A., Gomes S., Williford J.-M., Swartz M. A., Mendoza J. L., Ishihara J., Hubbell J. A., Masking the immunotoxicity of interleukin-12 by fusing it with a domain of its receptor via a tumour-protease-cleavable linker. Nat Biomed Eng, 7, 819–829 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williford J.-M., Ishihara J., Ishihara A., Mansurov A., Hosseinchi P., Marchell T. M., Potin L., Swartz M. A., Hubbell J. A., Recruitment of CD103+ dendritic cells via tumor-targeted chemokine delivery enhances efficacy of checkpoint inhibitor immunotherapy. Sci Adv. 5, eaay1357 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ishihara J., Ishihara A., Sasaki K., Lee S. S.-Y., Williford J.-M., Yasui M., Abe H., Potin L., Hosseinchi P., Fukunaga K., Raczy M. M., Gray L. T., Mansurov A., Katsumata K., Fukayama M., Kron S. J., Swartz M. A., Hubbell J. A., Targeted antibody and cytokine cancer immunotherapies through collagen affinity. Sci Transl Med. 11, eaau3259 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Y., Su Z., Zhao W., Zhang X., Momin N., Zhang C., Wittrup K. D., Dong Y., Irvine D. J., Weiss R., Multifunctional oncolytic nanoparticles deliver self-replicating IL-12 RNA to eliminate established tumors and prime systemic immunity. Nat Cancer. 1, 882–893 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riegler J., Labyed Y., Rosenzweig S., Javinal V., Castiglioni A., Dominguez C. X., Long J. E., Li Q., Sandoval W., Junttila M. R., Turley S. J., Schartner J. M., Carano R., Tumor Elastography and Its Association with Collagen and the Tumor Microenvironment. Clin Cancer Res. 24, 4455–4467 (2018) [DOI] [PubMed] [Google Scholar]
- 37.Hori S., Nomura T., Sakaguchi S., Control of Regulatory T Cell Development by the Transcription Factor Foxp3. Science. 299, 1057–1061 (2003). [DOI] [PubMed] [Google Scholar]
- 38.Fontenot J. D., Gavin M. A., Rudensky A. Y., Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 4, 330–336 (2003). [DOI] [PubMed] [Google Scholar]
- 39.Kim J. M., Rasmussen J. P., Rudensky A. Y., Regulatory T cells prevent catastrophic autoimmunity throughout the lifespan of mice. Nat Immunol. 8, 191–197 (2007). [DOI] [PubMed] [Google Scholar]
- 40.Lahl K., Loddenkemper C., Drouin C., Freyer J., Arnason J., Eberl G., Hamann A., Wagner H., Huehn J., Sparwasser T., Selective depletion of Foxp3+ regulatory T cells induces a scurfy-like disease. J Exp Med. 204, 57–63 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brunkow M. E., Jeffery E. W., Hjerrild K. A., Paeper B., Clark L. B., Yasayko S.-A., Wilkinson J. E., Galas D., Ziegler S. F., Ramsdell F., Disruption of a new forkhead/winged-helix protein, scurfin, results in the fatal lymphoproliferative disorder of the scurfy mouse. Nat Genet. 27, 68–73 (2001). [DOI] [PubMed] [Google Scholar]
- 42.Bennett C. L., Christie J., Ramsdell F., Brunkow M. E., Ferguson P. J., Whitesell L., Kelly T. E., Saulsbury F. T., Chance P. F., Ochs H. D., The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet. 27, 20–21 (2001). [DOI] [PubMed] [Google Scholar]
- 43.Lucca L. E., Dominguez-Villar M., Modulation of regulatory T cell function and stability by co-inhibitory receptors. Nat Rev Immunol. 20, 680–693 (2020). [DOI] [PubMed] [Google Scholar]
- 44.Scott E. N., Gocher A. M., Workman C. J., Vignali D. A. A., Regulatory T Cells: Barriers of Immune Infiltration Into the Tumor Microenvironment. Front Immunol. 12, 702726 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lebbink R. J., de Ruiter T., Kaptijn G. J. A., Bihan D. G., Jansen C. A., Lenting P. J., Meyaard L., Mouse leukocyte-associated Ig-like receptor-1 (mLAIR-1) functions as an inhibitory collagen-binding receptor on immune cells. Int Immunol. 19, 1011–1019 (2007). [DOI] [PubMed] [Google Scholar]
- 46.Meyaard L., Adema G. J., Chang C., Woollatt E., Sutherland G. R., Lanier L. L., Phillips J. H., LAIR-1, a Novel Inhibitory Receptor Expressed on Human Mononuclear Leukocytes. Immunity. 7, 283–290 (1997). [DOI] [PubMed] [Google Scholar]
- 47.Taraban V. Y., Rowley T. F., O’Brien L., Chan H. T. C., Haswell L. E., Green M. H. A., Tutt A. L., Glennie M. J., Al-Shamkhani A., Expression and costimulatory effects of the TNF receptor superfamily members CD134 (OX40) and CD137 (4-1BB), and their role in the generation of anti-tumor immune responses. Eur. J. Immunol. 32, 3617–3627 (2002). [DOI] [PubMed] [Google Scholar]
- 48.Timmerman J., Herbaux C., Ribrag V., Zelenetz A. D., Houot R., Neelapu S. S., Logan T., Lossos I. S., Urba W., Salles G., Ramchandren R., Jacobson C., Godwin J., Carpio C., Lathers D., Liu Y., Neely J., Suryawanshi S., Koguchi Y., Levy R., Urelumab alone or in combination with rituximab in patients with relapsed or refractory B-cell lymphoma. Am. J. Hematol. 95, 510–520 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choi B. K., Kim Y. H., Kang W. J., Lee S. K., Kim K. H., Shin S. M., Yokoyama W. M., Kim T. Y., Kwon B. S., Mechanisms Involved in Synergistic Anticancer Immunity of Anti-4-1BB and Anti-CD4 Therapy. Cancer Res. 67, 8891–8899 (2007). [DOI] [PubMed] [Google Scholar]
- 50.Qi X., Li F., Wu Y., Cheng C., Han P., Wang J., Yang X., Optimization of 4-1BB antibody for cancer immunotherapy by balancing agonistic strength with FcγR affinity. Nat Commun. 10, 2141 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aoki H., Ueha S., Shichino S., Ogiwara H., Hashimoto S., Kakimi K., Ito S., Matsushima K., TCR Repertoire Analysis Reveals Mobilization of Novel CD8+ T Cell Clones Into the Cancer-Immunity Cycle Following Anti-CD4 Antibody Administration. Front Immunol. 9, 3185 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shitara K., Ueha S., Shichino S., Aoki H., Ogiwara H., Nakatsura T., Suzuki T., Shimomura M., Yoshikawa T., Shoda K., Kitano S., Yamashita M., Nakayama T., Sato A., Kuroda S., Wakabayashi M., Nomura S., Yokochi S., Ito S., Matsushima K., Doi T., First-in-human phase 1 study of IT1208, a defucosylated humanized anti-CD4 depleting antibody, in patients with advanced solid tumors. J Immunother Cancer. 7, 195 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aoki H., Ueha S., Shichino S., Ogiwara H., Shitara K., Shimomura M., Suzuki T., Nakatsura T., Yamashita M., Kitano S., Kuroda S., Wakabayashi M., Kurachi M., Ito S., Doi T., Matsushima K., Transient Depletion of CD4+ Cells Induces Remodeling of the TCR Repertoire in Gastrointestinal Cancer. Cancer Immunol Res. 9, 624–636 (2021). [DOI] [PubMed] [Google Scholar]
- 54.Chen E. Y., Tan C. M., Kou Y., Duan Q., Wang Z., Meirelles G. V., Clark N. R., Ma’ayan A., Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics. 14, 128 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kuleshov M. V., Jones M. R., Rouillard A. D., Fernandez N. F., Duan Q., Wang Z., Koplev S., Jenkins S. L., Jagodnik K. M., Lachmann A., McDermott M. G., Monteiro C. D., Gundersen G. W., Ma’ayan A., Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 44, W90–W97 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xie Z., Bailey A., Kuleshov M. V., Clarke D. J. B., Evangelista J. E., Jenkins S. L., Lachmann A., Wojciechowicz M. L., Kropiwnicki E., Jagodnik K. M., Jeon M., Ma’ayan A., Gene Set Knowledge Discovery with Enrichr. Curr Protoc. 1, e90 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beltra J. C., Abdel-Hakeem M. S., Manne S., Zhang Z., Huang H., Kurachi M., Su L., Picton L., Muroyama Y., Casella V., Huang Y. J., Giles J. R., Mathew D., Belman J., Klapholz M., Decaluwe H., Huang A. C., Berger S. L., Garcia C. K., Wherry J. E., Enhanced STAT5a activation rewires exhausted CD8 T cells during chronic stimulation to acquire a hybrid durable effector like state. BioRxiv (2022), doi: 10.1101/2022.10.03.509766. [DOI] [Google Scholar]
- 58.Hashimoto M., Araki K., Cardenas M. A., Li P., Jadhav R. R., Kissick H. T., Hudson W. H., McGuire D. J., Obeng R. C., Wieland A., Lee J., McManus D. T., Ross J. L., Im S. J., Lee J., Lin J.-X., Hu B., West E. E., Scharer C. D., Freeman G. J., Sharpe A. H., Ramalingam S. S., Pellerin A., Teichgräber V., Greenleaf W. J., Klein C., Goronzy J. J., Umaña P., Leonard W. J., Smith K. A., Ahmed R., PD-1 combination therapy with IL-2 modifies CD8+ T cell exhaustion program. Nature, 610 173–181 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deak L. C., Nicolini V., Hashimoto M., Karagianni M., Schwalie P. C., Lauener L., Varypataki E. M., Richard M., Bommer E., Sam J., Joller S., Perro M., Cremasco F., Kunz L., Yanguez E., Hüsser T., Schlenker R., Mariani M., Tosevski V., Herter S., Bacac M., Waldhauer I., Colombetti S., Gueripel X., Wullschleger S., Tichet M., Hanahan D., Kissick H. T., Leclair S., Freimoser-Grundschober A., Seeber S., Teichgräber V., Ahmed R., Klein C., Umaña P., PD-1-cis IL-2R agonism yields better effectors from stem-like CD8+ T cells. Nature, 1–12 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu J., Blake S. J., Harjunpää H., Fairfax K. A., Yong M. C. R., Allen S., Kohrt H. E., Takeda K., Smyth M. J., Teng M. W. L., Assessing Immune-Related Adverse Events of Efficacious Combination Immunotherapies in Preclinical Models of Cancer. Cancer Res. 76, 5288–5301 (2016). [DOI] [PubMed] [Google Scholar]
- 61.Brinkmann V., Billich A., Baumruker T., Heining P., Schmouder R., Francis G., Aradhye S., Burtin P., Fingolimod (FTY720): discovery and development of an oral drug to treat multiple sclerosis. Nat Rev Drug Discov. 9, 883–897 (2010). [DOI] [PubMed] [Google Scholar]
- 62.Sotomayor E. M., Borrello I., Tubb E., Allison J. P., Levitsky H. I., In vivo blockade of CTLA-4 enhances the priming of responsive T cells but fails to prevent the induction of tumor antigen-specific tolerance. Proc National Acad Sci. 96, 11476–11481 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tsao L., Force J., Hartman Z. C., Mechanisms of Therapeutic Antitumor Monoclonal Antibodies. Cancer Res, 81, 4641–4651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wittrup K. D., Antitumor Antibodies Can Drive Therapeutic T Cell Responses. Trends Cancer. 3, 615–620 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Deng L., Zhang H., Luan Y., Zhang J., Xing Q., Dong S., Wu X., Liu M., Wang S., Accumulation of Foxp3+ T Regulatory Cells in Draining Lymph Nodes Correlates with Disease Progression and Immune Suppression in Colorectal Cancer Patients. Clin Cancer Res. 16, 4105–4112 (2010). [DOI] [PubMed] [Google Scholar]
- 66.Devi-Marulkar P., Fastenackels S., Karapentiantz P., Goc J., Germain C., Kaplon H., Knockaert S., Olive D., Panouillot M., Validire P., Damotte D., Alifano M., Murris J., Katsahian S., Lawand M., Dieu-Nosjean M.-C., Regulatory T cells infiltrate the tumor-induced tertiary lymphoïd structures and are associated with poor clinical outcome in NSCLC. Commun Biology. 5, 1416 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Curiel T. J., Coukos G., Zou L., Alvarez X., Cheng P., Mottram P., Evdemon-Hogan M., Conejo-Garcia J. R., Zhang L., Burow M., Zhu Y., Wei S., Kryczek I., Daniel B., Gordon A., Myers L., Lackner A., Disis M. L., Knutson K. L., Chen L., Zou W., Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 10, 942–949 (2004). [DOI] [PubMed] [Google Scholar]
- 68.Shou J., Zhang Z., Lai Y., Chen Z., Huang J., Worse outcome in breast cancer with higher tumor-infiltrating FOXP3+ Tregs : a systematic review and meta-analysis. BMC Cancer. 16, 687 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Joshi N. S., Akama-Garren E. H., Lu Y., Lee D.-Y., Chang G. P., Li A., DuPage M., Tammela T., Kerper N. R., Farago A. F., Robbins R., Crowley D. M., Bronson R. T., Jacks T., Regulatory T Cells in Tumor-Associated Tertiary Lymphoid Structures Suppress Anti-tumor T Cell Responses. Immunity. 43, 579–590 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Boissonnas A., Scholer-Dahirel A., Simon-Blancal V., Pace L., Valet F., Kissenpfennig A., Sparwasser T., Malissen B., Fetler L., Amigorena S., Foxp3+ T Cells Induce Perforin-Dependent Dendritic Cell Death in Tumor-Draining Lymph Nodes. Immunity. 32, 266–278 (2010). [DOI] [PubMed] [Google Scholar]
- 71.Shimizu J., Yamazaki S., Sakaguchi S., Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol. 163, 5211–5218 (1999). [PubMed] [Google Scholar]
- 72.Qureshi O. S., Zheng Y., Nakamura K., Attridge K., Manzotti C., Schmidt E. M., Baker J., Jeffery L. E., Kaur S., Briggs Z., Hou T. Z., Futter C. E., Anderson G., Walker L. S. K., Sansom D. M., Trans-Endocytosis of CD80 and CD86: A Molecular Basis for the Cell-Extrinsic Function of CTLA-4. Science. 332, 600–603 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wing K., Onishi Y., Prieto-Martin P., Yamaguchi T., Miyara M., Fehervari Z., Nomura T., Sakaguchi S., CTLA-4 Control over Foxp3+ Regulatory T Cell Function. Science. 322, 271–275 (2008). [DOI] [PubMed] [Google Scholar]
- 74.Ovcinnikovs V., Ross E. M., Petersone L., Edner N. M., Heuts F., Ntavli E., Kogimtzis A., Kennedy A., Wang C. J., Bennett C. L., Sansom D. M., Walker L. S. K., CTLA-4–mediated transendocytosis of costimulatory molecules primarily targets migratory dendritic cells. Sci Immunol. 4, eaaw0902 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Han J., Zhao Y., Shirai K., Molodtsov A., Kolling F. W., Fisher J. L., Zhang P., Yan S., Searles T. G., Bader J. M., Gui J., Cheng C., Ernstoff M. S., Turk M. J., Angeles C. V., Resident and circulating memory T cells persist for years in melanoma patients with durable responses to immunotherapy. Nat Cancer. 2, 300–311 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Savas P., Virassamy B., Ye C., Salim A., Mintoff C. P., Caramia F., Salgado R., Byrne D. J., Teo Z. L., Dushyanthen S., Byrne A., Wein L., Luen S. J., Poliness C., Nightingale S. S., Skandarajah A. S., Gyorki D. E., Thornton C. M., Beavis P. A., Fox S. B., K. C. F. C. for R. into F. B. C. (kConFab), Darcy P. K, Speed T. P, Mackay L. K, Neeson P. J, Loi S., Single-cell profiling of breast cancer T cells reveals a tissue-resident memory subset associated with improved prognosis. Nat Med. 24, 986–993 (2018). [DOI] [PubMed] [Google Scholar]
- 77.Prokhnevska N., Cardenas M. A., Valanparambil R. M., Sobierajska E., Barwick B. G., Jansen C., Moon A. R., Gregorova P., delBalzo L., Greenwald R., Bilen M. A., Alemozaffar M., Joshi S., Cimmino C., Larsen C., Master V., Sanda M., Kissick H., CD8+ T cell activation in cancer comprises an initial activation phase in lymph nodes followed by effector differentiation within the tumor. Immunity, 56, 107–124 (2022) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marabelle A., Tselikas L., de Baere T., Houot R., Intratumoral immunotherapy: using the tumor as the remedy. Ann Oncol. 28, xii33–xii43 (2017). [DOI] [PubMed] [Google Scholar]
- 79.Melero I., Castanon E., Alvarez M., Champiat S., Marabelle A., Intratumoural administration and tumour tissue targeting of cancer immunotherapies. Nat Rev Clin Oncol, 18, 558–576 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Humeau J., Naour J. L., Galluzzi L., Kroemer G., Pol J. G., Trial watch: intratumoral immunotherapy. Oncoimmunology. 10, 1984677 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rehman H., Silk A. W., Kane M. P., Kaufman H. L., Into the clinic: Talimogene laherparepvec (T-VEC), a first-in-class intratumoral oncolytic viral therapy. J Immunother Cancer. 4, 53 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andtbacka R. H. I., Kaufman H. L., Collichio F., Amatruda T., Senzer N., Chesney J., Delman K. A., Spitler L. E., Puzanov I., Agarwala S. S., Milhem M., Cranmer L., Curti B., Lewis K., Ross M., Guthrie T., Linette G. P., Daniels G. A., Harrington K., Middleton M. R., Jr W. H. M., Zager J. S., Ye Y., Yao B., Li A., Doleman S., VanderWalde A., Gansert J., Coffin R. S., Talimogene Laherparepvec Improves Durable Response Rate in Patients With Advanced Melanoma. J Clin Oncol. 33, 2780–2788 (2015). [DOI] [PubMed] [Google Scholar]
- 83.Moynihan K. D., Opel C. F., Szeto G. L., Tzeng A., Zhu E. F., Engreitz J. M., Williams R. T., Rakhra K., Zhang M. H., Rothschilds A. M., Kumari S., Kelly R. L., Kwan B. H., Abraham W., Hu K., Mehta N. K., Kauke M. J., Suh H., Cochran J. R., Lauffenburger D. A., Wittrup K. D., Irvine D. J., Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses. Nat Med. 22, 1402–1410 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Soumillon M., Cacchiarelli D., Semrau S., van Oudenaarden A., Mikkelsen T. S., Characterization of directed differentiation by high-throughput single-cell RNA-Seq. Biorxiv, 003236 (2014). Doi: 10.1101/003236 [DOI] [Google Scholar]
- 85.Zhu A., Ibrahim J. G., Love M. I., Heavy-tailed prior distributions for sequence count data: removing the noise and preserving large differences. Bioinformatics. 35, 2084–2092 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Love M. I., Huber W., Anders S., Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Butler A., Hoffman P., Smibert P., Papalexi E., Satija R., Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol. 36, 411–420 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gu Z., Eils R., Schlesner M., Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 32, 2847–2849 (2016). [DOI] [PubMed] [Google Scholar]
- 89.Wu T., Hu E., Xu S., Chen M., Guo P., Dai Z., Feng T., Zhou L., Tang W., Zhan L., Fu X., Liu S., Bo X., Yu G., clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation. 2, 100141 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lo M., Kim H. S., Tong R. K., Bainbridge T. W., Vernes J.-M., Zhang Y., Lin Y. L., Chung S., Dennis M. S., Zuchero Y. J. Y., Watts R. J., Couch J. A., Meng Y. G., Atwal J. K., Brezski R. J., Spiess C., Ernst J. A., Effector-attenuating Substitutions That Maintain Antibody Stability and Reduce Toxicity in Mice. J Biol Chem. 292, 3900–3908 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All raw data or materials are available upon request. Sequencing data can be found in the GEO database under accession GSE223087.