The Veterans Crisis Line (VCL) is an important public health tool to mitigate suicide risk among the Veteran population and connect Veterans in crisis with mental health services. Considering the unique needs and disproportionally high suicide rates among Veterans, many hypothesized that the COVID-19 pandemic could have led to an increase in suicidal behavior and in VCL contact volume [1].
Contrary to these hypotheses, recent literature suggests that the pandemic did not lead to an increase in suicidal behavior in Veterans, nor did it lead to an increase in overall VCL call volume [[2], [3], [4]]. However, there is limited knowledge about whether geographic differences in COVID-19 burden affected the number of unique Veterans who contacted VCL, and whether the pandemic caused a shift in the type of Veterans contacting the crisis line. Understanding COVID-19 related VCL trends is important because, although imperfect, crisis lines can serve as a proxy for measuring community mental health need. Our objective was to explore whether there were changes in the characteristics of Veterans who contacted VCL before and after the pandemic, and whether counties with a higher COVID burden experienced an increase in contact volume with the VCL.
We obtained data from the VCL Medora database on all documented contacts (calls and texts) to the crisis line between June 2, 2018, and June 29, 2021. The final sample included 503,272 calls and texts from 223,378 unique Veterans. Data on county-month level COVID-19 rates among the general population were obtained from the Johns Hopkins Coronavirus Resource Center. COVID-19 pre- and post-periods were defined as before March 2020, and during or after March 2020, respectively. More detail on the data and methodology can be found in Supplement A.
Veterans who contacted VCL during COVID-19 were on average older (mean = 54.24) than those who contacted VCL before the pandemic (mean = 52.49) (Supplement B). This finding is consistent with research showing that loneliness increases with age, social isolation was prevalent during the pandemic, and that older Veterans are significantly more likely to express feeling lonely compared to younger Veterans [5]. Indeed, a mixed-methods study by Krishnamurti and colleagues showed that loneliness, in addition to financial, housing, and mental health concerns, was one of the main reasons for contacting the VCL during the first year of the pandemic, and that the VCL provided much needed support for those in need [6].
Further examination of patient characteristics revealed that Veterans who contacted VCL during COVID-19 had fewer documented behavioral health comorbidities (alcohol and drug abuse, and depression) and were less likely to be homeless relative to Veterans who contacted VCL before the pandemic. However, it is unclear whether the decrease of behavioral health comorbidities is due to a true reduction of these comorbidities, or due to decreased healthcare utilization (and opportunities for diagnosis) during the pandemic. Others have found that the decrease in mental health visits was more prominent among new patients particularly in the beginning of the pandemic [7].
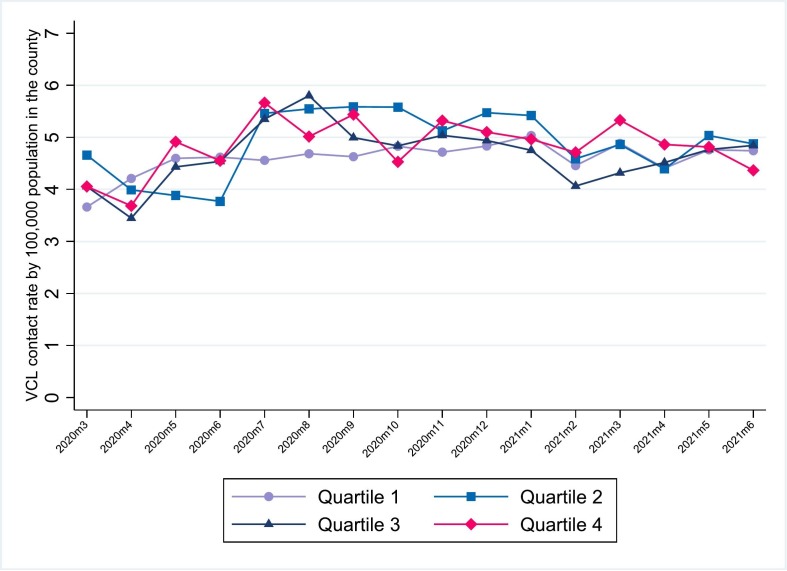
We also examined the changes in the volume of unique and new contacts to the VCL prior to and during the pandemic. While the raw contact volumes increased over time, these trends were not statistically significant after controlling for covariates and quarter fixed effects (Supplement C). Lastly, we did not observe a detectible impact of local COVID-19 burden on VCL contact rates (Fig. 1 ). Our results align with the work of Dichter et al., who did not find evidence of an association between the onset of the COVID-19 pandemic and Veteran VCL call volume [4].
Fig. 1.
Average rate of contact with the VCL, stratified by local COVID-19 burden quartiles.
Our findings may be partially explained by a pre-existing telehealth structure at the VHA that was rapidly expanded during the pandemic [8]. In fact, Veterans saw only a slight reduction in VHA mental health utilization during the pandemic – from an average of 2.55 mental health visits between October 2019 and February 2020, to 2.36 visits between April and June 2020 [9]. Future research should examine the relationship between VHA mental health clinic and telehealth service capacity and crisis line call volume.
Although the composition of Veterans who contacted the crisis line changed after the onset of the COVID-19 pandemic, we did not observe evidence of an increase in unique and new contacts with the VCL or a clear relationship between local COVID-19 burden and VCL contact rates during the initial year of the COVID-19 pandemic. These results can help VCL better direct resources to those who need it most and identify callers who might benefit from additional follow-up services. For example, as more older Veterans contact the VCL, responders need to be trained in age-related themes that may come up, including physical health problems and loneliness [10].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2023.02.001.
Appendix A. Supplementary data
Supplement A: Methods and Limitations
Supplement B: Table1
Supplement C: Figure 1
Data availability
The authors do not have permission to share data.
References
- 1.Straus E., Norman S.B., Tripp J.C., et al. Behavioral epidemic of loneliness in older US military veterans: results from the 2019-2020 national health and resilience in veterans study. Am J Geriatr Psychiatry. 2022;30(3):297–310. doi: 10.1016/j.jagp.2021.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Doran N., Gress-Smith J., Raja P., et al. Suicide risk among military veterans in the southwestern United States before and during the COVID-19 pandemic. Mil Med. 2022 doi: 10.1093/milmed/usac303. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nichter B., Hill M.L., Na P.J., et al. Prevalence and trends in suicidal behavior among US military veterans during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(11):1218–1227. doi: 10.1001/jamapsychiatry.2021.2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dichter M.E., Chhatre S., Hoffmire C., Bellamy S., Montgomery A.E., McCoy I. Variation in call volume to the veterans crisis line by women and men veterans prior to and following onset of the COVID-19 pandemic. J Psychiatr Res. 2022;151:561–563. doi: 10.1016/j.jpsychires.2022.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brülhart M., Klotzbücher V., Lalive R., Reich S.K. Mental health concerns during the COVID-19 pandemic as revealed by helpline calls. Nature. 2021;600(7887):121–126. doi: 10.1038/s41586-021-04099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnamurti L.S., Agha A., Iverson K.M., Monteith L.L., Dichter M.E. Outreach to the veterans crisis line during the COVID-19 pandemic: a mixed-methods analysis. Psychiatr Serv. 2022;74(2):142–147. doi: 10.1176/appi.ps.202200044. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J., Boden M., Trafton J. Mental health treatment and the role of tele-mental health at the veterans health administration during the COVID-19 pandemic. Psychol Serv. 2022;19(2):375. doi: 10.1037/ser0000530. [DOI] [PubMed] [Google Scholar]
- 8.Connolly S.L., Stolzmann K.L., Heyworth L., Weaver K.R., Bauer M.S., Miller C.J. Rapid increase in telemental health within the Department of Veterans Affairs during the COVID-19 pandemic. Telemed e-Health. 2021;27(4):454–458. doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- 9.Rosen C.S., Morland L.A., Glassman L.H., et al. Virtual mental health care in the veterans health Administration’s immediate response to coronavirus disease-19. Am Psychol. 2021;76(1):26. doi: 10.1037/amp0000751. [DOI] [PubMed] [Google Scholar]
- 10.Rasmussen K.A., King D.A., Gould M.S., et al. Concerns of older veteran callers to the veterans crisis line. Suicide Life Threat Behav. 2017;47(4):387–397. doi: 10.1111/sltb.12313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement A: Methods and Limitations
Supplement B: Table1
Supplement C: Figure 1
Data Availability Statement
The authors do not have permission to share data.