Abstract
Background: Prehospital trauma triage tools are not tailored to identify severely injured older adults. Our trauma triage protocol based on a three-tier trauma severity grading system (A, B, and C) has never been studied in this population. The objective was to assess its accuracy in predicting in-hospital mortality among older adults (≥65 years) and to compare it to younger patients. Methods: A retrospective multicenter cohort study, from 2011 to 2021. Consecutive adult trauma patients managed by a mobile medical team were prospectively graded A, B, or C according to the initial seriousness of their injuries. Accuracy was evaluated using sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios. Results: 8888 patients were included (14.1% were ≥65 years). Overall, 10.1% were labeled Grade A (15.2% vs. 9.3% among older and younger adults, respectively), 21.9% Grade B (27.9% vs. 20.9%), and 68.0% Grade C (56.9% vs. 69.8%). In-hospital mortality was 7.1% and was significantly higher among older adults regardless of severity grade. Grade A showed lower sensitivity (50.5 (43.7; 57.2) vs. 74.6 (69.8; 79.1), p < 0.0001) for predicting mortality among older adults compared to their younger counterparts. Similarly, Grade B was associated with lower sensitivity (89.5 (84.7; 93.3) vs. 97.2 (94.8; 98.60), p = 0.0003) and specificity (69.4 (66.3; 72.4) vs. 74.6 (73.6; 75.7], p = 0.001) among older adults. Conclusions: Our prehospital trauma triage protocol offers high sensitivity for predicting in-hospital mortality including older adults.
Keywords: trauma, emergency medical services, triage, older adults
1. Introduction
Older adults represent an expanding segment of the trauma population within developing countries’ healthcare systems; their proportion has increased from 18% in 2005 to 30% in 2015 in the US [1], with a similar trend in Europe [2,3]. Despite this trend, advanced age has been consistently associated with higher proportions of undertriage in the prehospital setting [4,5,6,7]. Although undertriage rates vary across studies, it can reach 50% [8] and patients older than 75 with an injury severity score (ISS) of more than 15 have been found to be 50% less likely to be triaged to a major trauma center compared to their younger counterparts [9]. The American College of Surgeons Committee on Trauma (ACSCOT) has emphasized a need for senior-tailored care [10], but much of that focus has concerned their care once they reach the hospital. Indeed, the identification of older adults with severe trauma as well as the setup of direct access to specialized trauma centers remain suboptimal [11,12,13]. However, the importance of prehospital triage in trauma care cannot be overstated. An accurate prehospital protocol is the cornerstone of a mature trauma system and transport to the most suitable center with a high level of trauma care designation is often regarded as the best option since such centers are associated with a lower risk of death and reduced morbidity [14,15,16]. Undertriage may be partially attributable to the inaccurate recognition of seriously traumatized older adults. Indeed, two recent systematic reviews suggested that current prehospital trauma triage tools may be at fault, as they do not accurately identify older patients with serious injuries, and undertriage is still an ongoing issue [13,17]. This is a critical concern because admission of severely injured older adults to healthcare facilities with higher levels of trauma care designation is associated with gains in the probability of survival [18]. Therefore, the crucial need to focus future research on the development of specific silver triage criteria has been recently highlighted [19,20,21].
Within the French emergency medical services (EMS) system, prehospital triage is performed by physicians, and in some regions, the triage protocol is based on a three-tier severity grading system that integrates clinical evaluation, response to prehospital resuscitation, and trauma circumstances as a surrogate for trauma severity [22]. A recent meta-analysis found that this protocol had high accuracy in predicting an ISS of more than 15, mortality within 30 days, or admission to intensive care unit (ICU) [23]. However, the accuracy of this triage protocol in specifically identifying severely injured older adults has never been evaluated.
Hence, we aimed to evaluate the accuracy of this triage protocol in predicting mortality among older adults (≥65 years) and compare it to younger patients. The secondary objective was to evaluate its accuracy in predicting severe trauma cases.
2. Materials and Methods
2.1. Study Design and Setting
This retrospective multicenter cohort study used data from the Réseau des Urgences de la Vallée du Rhône (RESUVal) Trauma Registry. The registry covers an area of approximately 3 million inhabitants and includes 3 level-I (one pediatric trauma), 1 level-II, and 5 level-III trauma centers. RESUVal prospectively collects pre- and in-hospital information (trauma room, emergency department (ED), and intensive care unit (ICU) if applicable) on all consecutive trauma patients managed by a mobile medical team (MMT).
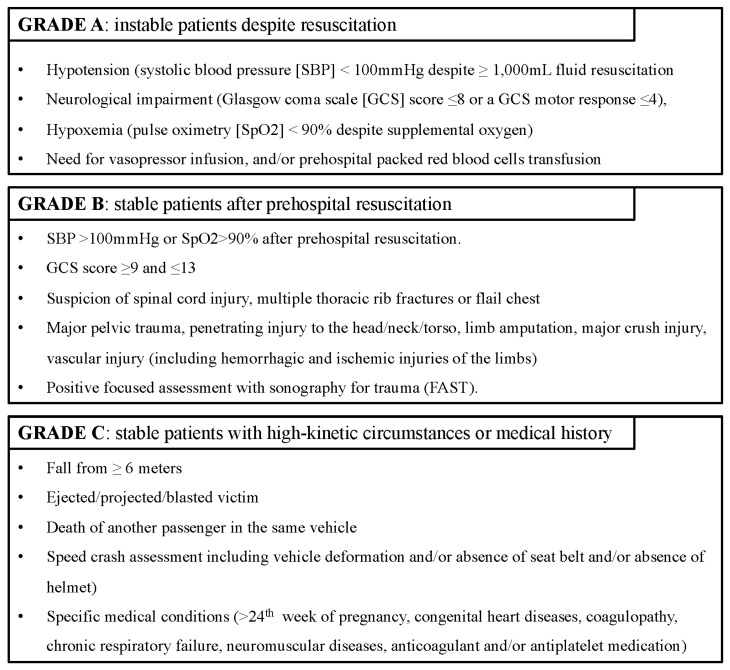
The French prehospital EMS has been described previously [7,24,25,26]. Briefly, it is a 24 h physician-led system, and out-of-hospital suspected severe life-threatening trauma situations are managed by the Service d’Aide Médicale d’Urgence (SAMU). Country-wide 24/7 access to the SAMU is provided by a single national telephone number (15) where a dispatching physician assesses the situation and can activate either a helicopter or ground MMT in suspected critical cases. The MMT is composed of a physician, a nurse, an ambulance driver, and a medical resident (in academic centers). Patient orientation depends on a regional triage protocol (Figure S1) based on a 3-tier grading system. It evaluates the seriousness of patient injuries at presentation on scene and the response to treatment during prehospital resuscitation, and integrates physiological information, trauma circumstances, and comorbidities. A patient is prospectively labeled by the on-scene physician as a Grade A (unstable despite resuscitation), B (stabilized after prehospital resuscitation), or C (stable with high-kinetic circumstances or specific medical conditions) major trauma (Figure 1).
Figure 1.
Major trauma grading system.
2.2. Study Population
All consecutive trauma patients aged 18 years or older managed by a prehospital MMT from January 2011 to December 2021 were considered for analyses. Those who died in the prehospital setting (either at the scene or during transportation) or with missing data pertaining to age, trauma grade, and/or ISS were excluded. Older adults were defined as those aged ≥65 years. Analyses were also performed within three subgroups among older adults (65–74, 75–84, and ≥85 years).
2.3. Data Collection
Prehospital, ED, and ICU data are collected by the physician in charge of the patient, while research technicians provide continuous monitoring of the completeness and correctness of the registry. They also collected patient outcomes at hospital discharge. Data management and analyses are performed by a data-manager-statistician (CC), from RESUVal. MMT physicians are asked to fill out a standardized case report form for any trauma patient with at least one Vittel criterion corresponding to effective or suspected seriously injured patients [27], and a research assistant reviews patients’ medical records in case of an incomplete case report form.
2.4. Study Data
The following prehospital variables were prospectively recorded: sociodemographic and trauma characteristics, first physiological parameters measured by the MMT (including point-of-care (POC) capillary hemoglobin concentration), and data pertaining to prehospital MMT advanced life support (ALS) procedures. The Abbreviated Injury Scale (AIS, based on the 1998 version) and ISS were calculated after anatomical and physiological assessments were completed.
2.5. Outcome Measures
The main outcome was the accuracy of the triage tool in predicting in-hospital mortality. Accuracy metrics were the sensitivity (Se), specificity (Sp), negative (NPV) and positive predictive value (PPV), and negative (NLR) and positive (PLR) likelihood ratio. The secondary outcome tested was the accuracy in predicting severe trauma cases defined as those with an ISS >15.
2.6. Statistics
Categorical data were described by frequencies and proportions (%), and continuous data were described by medians and interquartile ranges (IQR), first and third quartiles]. Univariable statistical comparisons of continuous data were performed using the nonparametric Wilcoxon rank sum test for two-group comparisons and the Kruskal–Wallis rank sum test for three-group comparisons. The Pearson chi-squared test was used for categorical data. For each outcome, Se, Sp, NPV, PPV, NLR, and PLR were computed using the epiR library [28].
Considering that all patients were graded A, B, or C, we did not test grade C accuracy as it would have led to 100% sensitivity. Consequently, Grade A and Grade B were considered thresholds for the different outcomes. Because the triage protocol is expected to predict severe trauma cases to avoid undertriage, we focused on presenting Se and NPV. The comparisons of accuracy metrics between groups were realized using the Pearson chi-squared test. Missing data were not imputed. We conventionally accepted a p value less than 0.05 as statistically significant. Statistical analyses were performed by a statistician (CC) using R® software (version 4.1.2).
2.7. Ethics Approval and Consent to Participate
All patients received written information on their information being used for research and could oppose the use of their data. Given that the study was retrospective in nature and that patient information was anonymized before the analysis, the need for an ethics committee as well as written consent was waived according to French law. The study received approval from the national data protection agency (Commission Nationale de l’Informatique et des Libertés, CNIL; DE-2012-059) and the Advisory Committee on the Treatment of Research Information (Comité consultatif sur le traitement de l’information en matière de recherche, CCTIRS). All methods were performed in accordance with the Declaration of Helsinki.
3. Results
3.1. Patient Characteristics
During the study period, a total of 8888 patients were included (Figure S2), of whom 1250 (14.1%) were aged ≥65 years. Older adults were less frequently male than younger adults (63.6% vs. 77.4%, p < 0.0001), and the main trauma mechanism was a road traffic accident in both age groups (49.2% and 64.0%, p < 0.0001). At MMT arrival in the prehospital setting, the proportion of patients with hypoxia (SpO2 < 95%; 29.3% vs. 14.4%), anemia (hemoglobin < 9 g/dL; 4.3% vs. 2.0%), or decreased level of consciousness (GCS ≤ 8; 19.0% vs. 11.9%) was higher among older adults (p < 0.0001). Table S1 reports patient characteristics in the subgroups of patients aged 65–74, 75–84, and ≥85 years.
A total of 10.1% of patients were labeled Grade A (15.2% vs. 9.3% among older and younger adults, respectively), 21.9% were Grade B (27.9% vs. 20.9%), and 68.0% were Grade C (56.9% vs. 69.8%). Overall, most patients were admitted to a level-I trauma center. The median (IQR) ISS was higher among older adults (17 (9–25) vs. 11 (5–22), p < 0.0001, Table 1).
Table 1.
Patient characteristics.
| All Patients n = 8888 |
18–64 Years n = 7638 |
≥65 Years n = 1250 |
p Value | |
|---|---|---|---|---|
| Age | 38 (26–55) | 34 (24–48) | 74 (69–82) | <0.0001 |
| Sex, male, n = 8857 | 6681 (75.4) | 5890 (77.4) | 791 (63.6) | <0.0001 |
| Type of trauma, n = 8797 | 0.0227 | |||
| Blunt | 7959 (90.5) | 6823 (90.2) | 1136 (92.3) | |
| Penetrating | 838 (9.5) | 743 (9.8) | 95 (7.7) | |
| Mechanism, n = 8807 | ||||
| Road collision | 5452 (61.9) | 4844 (64.0) | 608 (49.2) | <0.0001 |
| Fall | 1930 (21.9) | 1486 (19.6) | 444 (36.0) | <0.0001 |
| Gunshot, stab | 680 (7.7) | 609 (8.0) | 71 (5.8) | 0.004 |
| Other | 745 (8.5) | 633 (8.4) | 112 (9.1) | 0.44 |
| Delays | ||||
| On-scene time, n = 6891 | 33 (25–45) | 33 (24–45) | 35 (25–46) | 0.0245 |
| Total prehospital time a, n = 5668 | 80 (60–105) | 79 (60–104) | 85 (65–111) | 0.0001 |
| Prehospital medical evaluation | ||||
| Systolic blood pressure, n = 8140 | 129 (113–143) | 127 (112–140) | 140 (120–163) | <0.0001 |
| Heart rate, n = 8190 | 88 (75–101) | 89 (76–103) | 82 (70–96) | <0.0001 |
| SpO2 <95%, n = 7427 | 1219 (16.4) | 920 (14.4) | 299 (29.3) | <0.0001 |
| Hemoglobin <9 g/dL, n = 7378 | 172 (2.3) | 129 (2.0) | 43 (4.3) | <0.0001 |
| Shock index >1, n = 7903 | 764 (9.7) | 691 (10.2) | 73 (6.6) | 0.0003 |
| GCS score ≤8, n = 8155 | 1051 (12.9) | 834 (11.9) | 217 (19.0) | <0.0001 |
| Prehospital ALS procedures | ||||
| Mechanical ventilation, n = 7899 | 1738 (22.0) | 1431 (21.0) | 307 (28.0) | <0.0001 |
| Thoracostomy, n = 7841 | 90 (1.2) | 81 (1.2) | 9 (0.8) | 0.3628 |
| Packed red blood cell transfusion, n = 8022 | 128 (1.6) | 107 (1.6) | 21 (1.9) | 0.4826 |
| Fluid resuscitation, n = 8066 | 6366 (78.9) | 5500 (79.2) | 866 (77.4) | 0.1883 |
| Vasopressor infusion, n = 8030 | 707 (8.8) | 567 (8.2) | 140 (12.6) | <0.0001 |
| Tranexamic acid, n = 6882 | 3569 (51.9) | 3048 (51.5) | 521 (53.8) | 0.1993 |
| Pelvic binder, n = 7843 | 1279 (16.3) | 1154 (17.1) | 125 (11.5) | <0.0001 |
| FAST, n = 7770 | 2626 (33.8) | 2331 (34.8) | 295 (27.5) | <0.0001 |
| Anticoagulant and/or antiplatelet medication | 636 (7.7) | 199 (2.8) | 437 (37.1) | <0.0001 |
| Severity grade | <0.0001 | |||
| A | 898 (10.1) | 708 (9.3) | 190 (15.2) | |
| B | 1944 (21.9) | 1595 (20.9) | 349 (27.9) | |
| C | 6046 (68.0) | 5335 (69.8) | 711 (56.9) | |
| Trauma center admission level | 0.3113 | |||
| I | 7529 (84.7) | 6483 (84.9) | 1046 (83.7) | |
| II | 756 (8.5) | 633 (8.3) | 123 (9.8) | |
| III | 602 (6.8) | 521 (6.8) | 81 (6.5) | |
| Compliance to the field triage protocol b | 8823 (99.3) | 7587 (99.3) | 1236 (98.9) | 0.1186 |
| ISS | 13 (5–24) | 11 (5–22) | 17 (9–25) | <0.0001 |
| In-hospital trauma procedures c | ||||
| Packed red blood cell transfusion | 897 (10.1) | 704 (9.2) | 193 (15.4) | <0.0001 |
| Vasopressor infusion | 1187 (13.4) | 943 (12.4) | 244 (19.5) | <0.0001 |
| Surgery, n = 8836 | 2587 (29.3) | 2322 (30.6) | 265 (21.3) | <0.0001 |
| Angioembolization, n = 8834 | 270 (3.1) | 220 (2.9) | 50 (4.0) | 0.0396 |
| Chest tube drainage | 495 (5.6) | 435 (5.7) | 60 (4.8) | 0.2252 |
| ICU admission, n = 8711 | 4008 (46.0) | 3248 (43.4) | 760 (62.0) | <0.0001 |
Data are presented as median (IQR) or n (%); proportions (%) were calculated among those with data. a From call to hospital arrival, expressed in minutes. b Defined as the proportion of patients admitted to a trauma center whose level of care is in accordance with the triage protocol. c Within the first 24 h. ALS: Advanced life support; FAST: Focused assessment with sonography for trauma; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation measured by pulse oximetry.
3.2. Accuracy of the Triage Protocol in Predicting In-Hospital Mortality
A total of 7.1% (n = 571) of patients died (19.8% vs. 5.0% among older and younger adults, respectively, p < 0.0001). Mortality was significantly higher among older adults at all severity grades (Grade A: 65.3% vs. 40.6%, Grade B: 28.7% vs. 5.7%, and Grade C: 3.6% vs. 0.2, p < 0.0001, Table 2).
Table 2.
Outcomes.
| All Patients n = 8888 |
18–64 Years n = 7638 |
≥65 Years n = 1250 |
|
|---|---|---|---|
| Severe trauma as per the composite definition | 4294 (48.3) | 3477 (45.5) | 817 (65.4) |
| Grade A | 888/898 (98.9) | 701/708 (99.0) | 187/190 (98.4) |
| Grade B | 1739/1944 (89.5) | 1407/1595 (88.2) | 332/349 (95.1) |
| Grade C | 3293/6046 (54.5) | 2839/5335 (53.2) | 454/711 (63.9) |
| ISS >15 | 3785 (42.6) | 3073 (40.2) | 712 (57.0) |
| Grade A | 803/898 (89.4) | 636/708 (89.8) | 167/190 (87.9) |
| Grade B | 1339/1944 (68.9) | 1078/1595 (67.6) | 261/349 (74.8) |
| Grade C | 1643/6046 (27.2) | 1359/5335 (25.5) | 284/711 (39.9) |
| In-hospital urgent and specialized trauma care a | 5554 (62.5) | 4639 (60.7) | 915 (73.2) |
| Grade A | 877/908 (96.6) | 694/708 (98.0) | 183/200 (96.3) |
| Grade B | 1687/1944 (86.8) | 1363/1595 (85.5) | 324/349 (92.8) |
| Grade C | 2990/6046 (49.5) | 2582/5335 (48.4) | 408/711 (57.4) |
| In-hospital mortality | 571 (7.1) | 351 (5.0) | 220 (19.8) |
| Grade A | 373/816 (45.7) | 262/646 (40.6) | 111/170 (65.3) |
| Grade B | 165/1673 (9.9) | 79/1373 (5.7) | 86/300 (28.7) |
| Grade C | 33/5593 (0.6) | 10/4950 (0.2) | 23/643 (3.6) |
Data are presented as n (%); proportions (%) were calculated among those with data. ISS: Injury severity score. a Includes the need for ≥1 of the following urgent and specialized in-hospital trauma care: surgery and/or angioembolization within 24 h after admission, chest tube drainage, endotracheal intubation with mechanical ventilation, vasopressor infusion, packed red blood cell transfusion, and/or ICU admission.
Grade A sensitivity (%) (CI95%) in predicting mortality was significantly lower in the group of older adults (50.5 (43.7; 57.2) vs. 74.6 (69.8; 79.1), p < 0.0001). Similarly, Grade A NPV (%) (CI95%) was lower among older adults (88.4 (86.2; 90.4) vs. 98.6 (98.3; 98.9), p < 0.0001). Grade B was associated with higher sensitivity than Grade A but was still lower among older adults (89.5 (84.7; 93.3) vs. 97.2 (94.8; 98.6), p = 0.0003). Similarly, NPV was lower in older adults labeled grade B (96.4 (94.7; 97.7) vs. 99.8 (99.6; 99.9), p < 0.0001, Table 3).
Table 3.
Performance of the grading system to predict in-hospital mortality.
| In-Hospital Mortality | ||||
|---|---|---|---|---|
| 18–64 Years | ≥65 Years | p Value | ||
| Grade A | Se | 74.6 (69.8; 79.1) | 50.5 (43.7; 57.2) | <0.0001 |
| Sp | 94.2 (93.6; 94.7) | 93.4 (91.6; 94.9) | 0.3776 | |
| PPV | 40.6 (36.7; 44.5) | 65.3 (57.6; 72.4) | <0.0001 | |
| NPV | 98.6 (98.3; 98.9) | 88.4 (86.2; 90.4) | <0.0001 | |
| PLR | 12.9 (11.5; 14.4) | 7.6 (5.8; 10.1) | 0.00007 | |
| NLR | 0.27 (0.22; 0.32) | 0.53 (0.46; 0.61) | <0.0001 | |
| Grade B | Se | 97.2 (94.8; 98.6) | 89.5 (84.7; 93.3) | 0.0003 |
| Sp | 74.6 (73.6; 75.7) | 69.4 (66.3; 72.4) | 0.001 | |
| PPV | 16.9 (15.3; 18.6) | 41.9 (37.4; 46.5) | <0.0001 | |
| NPV | 99.8 (99.6; 99.9) | 96.4 (94.7; 97.7) | <0.0001 | |
| PLR | 3.8 (3.7; 4.0) | 2.9 (2.6; 3.3) | <0.0001 | |
| NLR | 0.04 (0.02; 0.07) | 0.15 (0.10; 0.22) | 0.00002 | |
Se: Sensibility, Sp: Specificity, PPV: Positive predictive value, NPV: Negative predictive value, PLR: Positive likelihood ratio, NLR: Negative likelihood ratio.
Grade A and B accuracy among the group of older adults (65–74, 75–84, and ≥85 years) are presented in Table S2.
3.3. Accuracy of the Triage Protocol in Predicting Patients with an ISS >15
Overall, 42.6% (n = 3785) of patients had an ISS >15 (57.0% vs. 40.2% among older and younger adults, respectively, p < 0.0001). The proportion of patients with an ISS >15 was not significantly different between Grade A older and younger adults (87.9% vs. 89.8%, p = 0.27). Conversely, it was higher among older adults in the two other severity groups (Grade B: 74.8% vs. 67.6%, p = 0.01 and Grade C: 39.9% vs. 25.5%, p < 0.0001, Table 2).
Grade A sensitivity in predicting patients with an ISS >15 was not significantly different between the two age groups (23.5 (20.4; 26.7) vs. 20.7 (19.3; 22.2), p = 0.1161), but its NPV was significantly lower among older adults (48.6 (45.5; 51.6) vs. 64.8 (63.7; 66.0), p < 0.0001). Grade B showed higher sensitivity than Grade A, and it was significantly higher among older adults (60.1 (56.4; 63.7) vs. 55.8 (54.0; 57.5), p = 0.0393). Conversely, NPV associated with Grade B was significantly lower among older adults (60.1 (56.4;63.7) vs. 74.5 (73.3; 75.7), p < 0.0001; Table 3). Grade A and B accuracy among the group of older adults (65–74, 75–84, and ≥85 years) are presented in Additional file 4.
4. Discussion
The A/B/C prehospital triage tool showed high sensitivity in predicting in-hospital mortality across all age groups but performed less well for older adults. A nonnegligible proportion of Grade C patients, those with an initial reassuring clinical exam but high-kinetic trauma circumstances or specific medical conditions, were found to be severe trauma cases, but very few of them died.
Given that identification of trauma severity at the scene directly influences patient triage and orientation, which may impact trauma-related mortality, having efficient triage protocols remains a cornerstone of any mature trauma system. This is particularly true for older adults. Early identification of major injuries in this population has been defined as the first decision-making step in managing older patients with injuries [20]. The triage protocol used herein demonstrated great accuracy in identifying the most severe cases, those who died during their in-hospital stay, regardless of age. Nevertheless, it was less efficient in identifying patients with an ISS >15. In another similar French prehospital trauma setting, using the same triage protocol, Bouzat et al. uniformly found a total of 89% of patients with an ISS >15 among Grade A (vs. 89.4% herein), 64% (vs. 68.9%) among Grade B, and 31% (vs. 27.2%) among Grade C patients [22]. The study neither provided diagnostic performance data, nor performed age stratification. In Canada, Coulombe et al. specifically assessed the accuracy of a five-step paramedic-led prehospital trauma triage protocol to identify the need for advanced trauma care in the older adults. They concluded that there was insufficient sensitivity (65.8% (95% CI: 48.7–80.4%)) when combining the five steps for patients aged ≥65 years, and this sensitivity was even lower among the oldest adults [29]. In the Netherlands, Voskens et al. assessed the performance of the national triage protocol, regardless of the actual destination facility, and reported an undertriage of 63.8% 95% CI (59.2–68.1%) [30]. More generally, it has been reported that almost all protocols have a low sensitivity, thereby failing to identify severely injured patients [31]. Nevertheless, sensitivity and specificity are incidence-dependent; therefore, the comparison of metric characteristics between studies should be interpreted with caution. Interestingly, Nishijima et al. assessed the performance of the US field triage guidelines for specifically identifying traumatic intracranial hemorrhage among older adults. They reported a very low sensitivity of 19.8% 95% CI (5.5–51.2%) [32]. These findings suggest that prehospital EMS should develop and use age-specific trauma triage criteria that should focus on the premorbid status of the individual as suggested before [21].
Despite the good performance of the grading system, the present study raises a serious point of concern. Among the group of adults graded C, mortality was less than 1%. However, a nonnegligible proportion of those patients who presented with an ISS >15 (more than one in four cases) and/or required advanced trauma interventions; these proportions were even higher in the group of older adults. Therefore, these findings invite in-hospital clinicians of level-III trauma centers to remain vigilant for Grade C patients. Indeed, based on our triage protocol, those potentially severely injured patients may be assigned to level-III healthcare facilities although fewer trauma care resources are available. Avenues to improve the diagnostic performance of Grade C and better identify and triage severely injured patients could be to consider removing high energy transfer criteria from the list. Accordingly, Cassignol et al. reported that no criterion related to kinetic elements was significantly correlated with an ISS >15, mortality within 30 days, or admission to the ICU [33]. Another possibility to improve the on-field identification of severe trauma cases among Grade C patients would be to add easy-to-use and quickly measurable clinical variables such as the shock index, which may help to improve the identification of severe cases. As such, substituting the criterion of SBP <90 mm Hg in the American National Trauma Triage Protocol with a shock index >1 resulted in a considerable reduction in undertriage (−5.9%) without a substantial rise in overtriage (+1.3%) [34]. Technologies such as capillary hemoglobin concentration measurement at the scene to screen for occult anemia are also an easy-to-use tool for physicians as well as paramedics in their daily routine and could be of help in discriminating severe cases. Some authors showed that hemoglobin variation (measured with a POC device) was able to predict significant hemorrhage [35]. Elsewhere, it has been suggested that integrating prehospital serum lactate measurement may improve the prediction of in-hospital mortality, emergent surgery, and multiple organ dysfunction syndrome [36,37]. More specifically, St John et al. showed that prehospital lactate was predictive of the need for resuscitative care among normotensive trauma patients [38], which could be of noteworthy help within the group of patients meeting only the high-kinetic trauma circumstances red flag. Although the current data showed feasibility, further research is still needed to establish whether lactate might truly provide meaningful guidance during prehospital triage [39]. Another insufficiently explored track would be to evaluate the accuracy of physician judgment regarding trauma severity when facing a hemodynamically stable patient presenting with only high-kinetic trauma circumstances. Indeed, although it has been shown elsewhere that the judgment of nonphysician EMS providers was useful in identifying high-risk patients missed by other criteria [40], the accuracy of physician judgment has never been investigated for this older adult trauma population.
Among the specific group of older adults, the accuracy of field triage protocols could be improved by integrating geriatric-specific criteria. For instance, adding preinjury comorbidities and geriatric-specific physiological measures has shown high sensitivity improvement at the cost of a decrement in specificity in identifying severe trauma (ISS ≥16 or need for major nonorthopedic surgery) [41].
A major strength of this study is that it was conducted in a wide area, including urban as well as rural zones, and patients were included over a large period, reducing selection bias, and assuring a high level of generalizability to comparable settings. Another strength is that the trauma registry captures most severe trauma cases given that very few patients are directly admitted to an ED by relatives or bystanders. However, the study suffers from some limitations. First, due to the observational retrospective nature of the study, potential confounding factors may have impacted comparisons between the two age groups. For instance, data concerning the decision to withhold and terminate resuscitation were not collected, which could have influenced the results related to grade performance, especially those regarding in-hospital mortality. Second, we do not have all data on the appropriateness of severity grade category assignment (e.g., some clinical findings pertaining to Grade B category or details on trauma mechanism pertaining to Grade C category were not collected in the registry). Third, it must also be acknowledged that the limited sample size of the very old patient groups can affect the interpretation of our results. Fourth, given that this study was conducted in a physician-staffed prehospital EMS, this limits the opportunity to compare the findings to other prehospital EMS, which are paramedic-led in most EMS [42].
Future research is warranted to identify the underlying reasons for the disparity in accuracy performance between the two age groups and to adjust the grading system criteria to population-specific characteristics of older adults to optimize the identification of high-risk patients. Another avenue for future studies based on large cohorts would be to integrate machine learning to enhance triage accuracy. Some authors have already developed an artificial-intelligence-based method for predicting various outcomes including shock, major surgery, and early massive transfusion in patients with truncal gunshot wounds [43]. Such a strategy may greatly help clinicians in facilitating patient risk assessment and triaging and optimize resource use. Elsewhere, machine-learning-based models predicted the need for urgent neurosurgery [44] or trauma mortality [45]. The potential clinical benefits of such models as decision-making and triage tools deserve further assessment in the prehospital environment. In addition, these models were built a posteriori. Therefore, computerization of prehospital EMS would be required to integrate such AI-based tools into daily healthcare professionals’ routines.
5. Conclusions
This prehospital triage protocol offers high sensitivity in predicting in-hospital mortality including in older adults, which is of great interest for prehospital and in-hospital clinicians, and for emergency service organization. Nevertheless, it needs to be refined to better identify severe trauma cases in the prehospital setting among patients presenting with reassuring initial clinical examinations and high-kinetic trauma circumstances or specific medical conditions.
Acknowledgments
We thank Véréna Landel (DRCI, Hospices Civils de Lyon) for help in the manuscript preparation, as well as the local investigators of the trauma registry: Antoine Blum (Saint Vallier), Djamel Bekka (Privas), Eric Cesareo (Lyon), Patricia Trinquet (Vienne), Stéphane Blain (Ambérieu), Thomas Paita (Bourgoin-Jallieu), Johan Restier (Valence), Olivier Debas (Belley), Raphael Brilland (Tarare), Nicolas Roumestand (Montélimar), Xavier-Jean Taverna (HEH), Jean-Stéphane David (CHLS), Etienne Javouhey (HFME), Loïs Grattier (Valence), Frédéric Verbois (Villefranche-sur-Saone), and Patrice Serre (Bourg-en-Bresse).
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph20031975/s1, Table S1: Older adult characteristics according to age subgroups. Table S2: Performance of the triage protocol to detect patients who died during their in-hospital stay or with a severe trauma among older patient groups. Figure S1: Triage protocol. Figure S2: Flow chart.
Author Contributions
A.B., Concept and Design, Methodology, Writing—original draft; M.E., E.M., M.H., T.G., J.-S.D., P.S.-S. and K.Y., Critical revision of the manuscript; C.C., Concept and Design, Data curation, Methodology, Formal analysis, Writing—review & editing; K.T., Supervision, Validation, Writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and received approval from the national data protection agency (Commission Nationale de l’Informatique et des Libertés, CNIL; DE-2012-059) and the Advisory Committee on the Treatment of Research Information (Comité consultatif sur le traitement de l’information en matière de recherche, CCTIRS).
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated and analyzed in the current study are not publicly available due to ethical restrictions on sharing a dataset because the data contain potentially identifying information. Further description or analysis of data are available from the authors upon reasonable request.
Conflicts of Interest
All authors declare no conflict of interest.
Funding Statement
The trauma registry is funded by the regional health agency (Agence Régionale de Santé Auvergne Rhône-Alpes), which was in no way involved in the design, data collection, or analyses of this study. The study presented herein did not receive any specific grant.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Jiang L., Zheng Z., Zhang M. The incidence of geriatric trauma is increasing and comparison of different scoring tools for the prediction of in-hospital mortality in geriatric trauma patients. World J. Emerg. Surg. 2020;15:59. doi: 10.1186/s13017-020-00340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalbas Y., Lempert M., Ziegenhain F., Scherer J., Neuhaus V., Lefering R., Teuben M., Sprengel K., Pape H.C., Jensen K.O., et al. A retrospective cohort study of 27,049 polytraumatized patients age 60 and above: Identifying changes over 16 years. Eur. Geriatr. Med. 2021;13:233–241. doi: 10.1007/s41999-021-00546-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kehoe A., Smith J.E., Edwards A., Yates D., Lecky F. The changing face of major trauma in the UK. Emerg. Med. J. 2015;32:911–915. doi: 10.1136/emermed-2015-205265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers A., Rogers F.B. Increased mortality with undertriaged patients in a mature trauma center with an aggressive trauma team activation system. Eur. J. Trauma Emerg. Surg. 2013;39:599–603. doi: 10.1007/s00068-013-0289-z. [DOI] [PubMed] [Google Scholar]
- 5.Uribe-Leitz T., Jarman M.P., Sturgeon D.J., Harlow A.F., Lipsitz S.R., Cooper Z., Salim A., Newgard C.D., Haider A.H. National Study of Triage and Access to Trauma Centers for Older Adults. Ann. Emerg. Med. 2020;75:125–135. doi: 10.1016/j.annemergmed.2019.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang D.C., Bass R.R., Cornwell E.E., Mackenzie E.J. Undertriage of elderly trauma patients to state-designated trauma centers. Arch. Surg. 2008;143:776–781; discussion 782. doi: 10.1001/archsurg.143.8.776. [DOI] [PubMed] [Google Scholar]
- 7.Benhamed A., Fraticelli L., Claustre C., Gossiome A., Cesareo E., Heidet M., Emond M., Mercier E., Boucher V., David J.S., et al. Risk factors and mortality associated with undertriage after major trauma in a physician-led prehospital system: A retrospective multicentre cohort study. Eur. J. Trauma Emerg. Surg. 2022 doi: 10.1007/s00068-022-02186-5. online ahead of print . [DOI] [PubMed] [Google Scholar]
- 8.Horst M.A., Morgan M.E., Vernon T.M., Bradburn E.H., Cook A.D., Shtayyeh T., D’Andrea L., Rogers F.B. The geriatric trauma patient: A neglected individual in a mature trauma system. J. Trauma Acute Care Surg. 2020;89:192–198. doi: 10.1097/TA.0000000000002646. [DOI] [PubMed] [Google Scholar]
- 9.Lukin W., Greenslade J.H., Chu K., Lang J., Brown A.F. Triaging older major trauma patients in the emergency department: An observational study. Emerg. Med. J. 2015;32:281–286. doi: 10.1136/emermed-2013-203191. [DOI] [PubMed] [Google Scholar]
- 10.American College of Surgeons Committee on Trauma ACS TQIP Geriatric Trauma Management Guidelines. [(accessed on 10 January 2023)]. Available online: https://www.facs.org/media/314or1oq/geriatric_guidelines.pdf.
- 11.Morris R.S., Karam B.S. Field-Triage, Hospital-Triage and Triage-Assessment: A Literature Review of the Current Phases of Adult Trauma Triage. J. Trauma Acute Care Surg. 2021;90:e138–e145. doi: 10.1097/TA.0000000000003125. [DOI] [PubMed] [Google Scholar]
- 12.Sewalt C.A., Gravesteijn B.Y., Nieboer D., Steyerberg E.W., Den Hartog D., Van Klaveren D. Identifying trauma patients with benefit from direct transportation to Level-1 trauma centers. BMC Emerg. Med. 2021;21:93. doi: 10.1186/s12873-021-00487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alshibani A., Alharbi M., Conroy S. Under-triage of older trauma patients in prehospital care: A systematic review. Eur. Geriatr. Med. 2021;12:903–919. doi: 10.1007/s41999-021-00512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polites S.F., Leonard J.M., Glasgow A.E., Zielinski M.D., Jenkins D.H., Habermann E.B. Undertriage after severe injury among United States trauma centers and the impact on mortality. Am. J. Surg. 2018;216:813–818. doi: 10.1016/j.amjsurg.2018.07.061. [DOI] [PubMed] [Google Scholar]
- 15.Candefjord S., Asker A., Caragounis E.C. Mortality of trauma patients treated at trauma centers compared to non-trauma centers in Sweden: A retrospective study. Eur. J. Trauma Emerg. Surg. 2022;48:525–536. doi: 10.1007/s00068-020-01446-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tignanelli C.J., Vander Kolk W.E., Mikhail J.N., Delano M.J., Hemmila M.R. Noncompliance with American College of Surgeons Committee on Trauma recommended criteria for full trauma team activation is associated with undertriage deaths. J. Trauma Acute Care Surg. 2018;84:287–294. doi: 10.1097/TA.0000000000001745. [DOI] [PubMed] [Google Scholar]
- 17.Fuller G., Pandor A., Essat M., Sabir L., Buckley-Woods H., Chatha H., Holt C., Keating S., Turner J. Diagnostic accuracy of prehospital triage tools for identifying major trauma in elderly injured patients: A systematic review. J. Trauma Acute Care Surg. 2021;90:403–412. doi: 10.1097/TA.0000000000003039. [DOI] [PubMed] [Google Scholar]
- 18.Pracht E.E., Langland-Orban B., Flint L. Survival advantage for elderly trauma patients treated in a designated trauma center. J. Trauma. 2011;71:69–77. doi: 10.1097/TA.0b013e31820e82b7. [DOI] [PubMed] [Google Scholar]
- 19.Alshibani A., Banerjee J., Lecky F., Coats T.J., Prest R., Mitchell A., Laithwaite E., Wensley M., Conroy S. A consensus building exercise to determine research priorities for silver trauma. BMC Emerg. Med. 2020;20:63. doi: 10.1186/s12873-020-00357-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harthi N., Goodacre S., Sampson F., Alharbi R. Research priorities for prehospital care of older patients with injuries: Scoping review. Age Ageing. 2022;51 doi: 10.1093/ageing/afac108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eichinger M., Robb H.D.P., Scurr C., Tucker H., Heschl S., Peck G. Challenges in the PREHOSPITAL emergency management of geriatric trauma patients—A scoping review. Scand. J. Trauma Resusc. Emerg. Med. 2021;29:100. doi: 10.1186/s13049-021-00922-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bouzat P., Ageron F.X., Brun J., Levrat A., Berthet M., Rancurel E., Thouret J.M., Thony F., Arvieux C., Payen J.F., et al. A regional trauma system to optimize the pre-hospital triage of trauma patients. Crit. Care. 2015;19:111. doi: 10.1186/s13054-015-0835-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gianola S., Castellini G., Biffi A., Porcu G., Fabbri A., Ruggieri M.P., Stocchetti N., Napoletano A., Coclite D., D’Angelo D., et al. Accuracy of pre-hospital triage tools for major trauma: A systematic review with meta-analysis and net clinical benefit. World J. Emerg. Surg. 2021;16:31. doi: 10.1186/s13017-021-00372-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.David J.S., Bouzat P., Raux M. Evolution and organisation of trauma systems. Anaesth. Crit. Care Pain Med. 2019;38:161–167. doi: 10.1016/j.accpm.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 25.Gauss T., Ageron F.X., Devaud M.L., Debaty G., Travers S., Garrigue D., Raux M., Harrois A., Bouzat P. Association of Prehospital Time to In-Hospital Trauma Mortality in a Physician-Staffed Emergency Medicine System. JAMA Surg. 2019;154:1117–1124. doi: 10.1001/jamasurg.2019.3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamada S.R., Gauss T., Duchateau F.X., Truchot J., Harrois A., Raux M., Duranteau J., Mantz J., Paugam-Burtz C. Evaluation of the performance of French physician-staffed emergency medical service in the triage of major trauma patients. J. Trauma Acute Care Surg. 2014;76:1476–1483. doi: 10.1097/TA.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 27.Riou B. Le traumatisé grave. Actualités en réanimation préhospitalière. Journées Scientifiques du SAMU de France. Oct 9–11, 2002.
- 28.Stevenson M. epiR: Tools for the Analysis of Epidemiological. Data. R Package Version 2.0.48. 2022. [(accessed on 7 September 2022)]. Available online: https://cran.r-project.org/package=epiR.
- 29.Coulombe P., Tardif P.A., Nadeau A., Beaumont-Boileau R., Malo C., Emond M., Blanchard P.G., Moore L., Mercier E. Accuracy of Prehospital Trauma Triage to Select Older Adults Requiring Urgent and Specialized Trauma Care. J. Surg. Res. 2022;275:281–290. doi: 10.1016/j.jss.2022.02.037. [DOI] [PubMed] [Google Scholar]
- 30.Voskens F.J., van Rein E.A.J., van der Sluijs R., Houwert R.M., Lichtveld R.A., Verleisdonk E.J., Segers M., van Olden G., Dijkgraaf M., Leenen L.P.H., et al. Accuracy of Prehospital Triage in Selecting Severely Injured Trauma Patients. JAMA Surg. 2018;153:322–327. doi: 10.1001/jamasurg.2017.4472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Rein E.A.J., Houwert R.M., Gunning A.C., Lichtveld R.A., Leenen L.P.H., van Heijl M. Accuracy of prehospital triage protocols in selecting severely injured patients: A systematic review. J. Trauma Acute Care Surg. 2017;83:328–339. doi: 10.1097/TA.0000000000001516. [DOI] [PubMed] [Google Scholar]
- 32.Nishijima D.K., Gaona S.D., Waechter T., Maloney R., Blitz A., Elms A.R., Farrales R.D., Montoya J., Bair T., Howard C., et al. The Incidence of Traumatic Intracranial Hemorrhage in Head-Injured Older Adults Transported by EMS with and without Anticoagulant or Antiplatelet Use. J. Neurotrauma. 2018;35:750–759. doi: 10.1089/neu.2017.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cassignol A., Marmin J., Cotte J., Cardinale M., Bordes J., Pauly V., Kerbaul F., Demory D., Meaudre E. Correlation between field triage criteria and the injury severity score of trauma patients in a French inclusive regional trauma system. Scand. J. Trauma Resusc. Emerg. Med. 2019;27:71. doi: 10.1186/s13049-019-0652-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haider A.A., Azim A., Rhee P., Kulvatunyou N., Ibraheem K., Tang A., O’Keeffe T., Iftikhar H., Vercruysse G., Joseph B. Substituting systolic blood pressure with shock index in the National Trauma Triage Protocol. J. Trauma Acute Care Surg. 2016;81:1136–1141. doi: 10.1097/TA.0000000000001205. [DOI] [PubMed] [Google Scholar]
- 35.Figueiredo S., Taconet C., Harrois A., Hamada S., Gauss T., Raux M., Duranteau J., Traumabase G. How useful are hemoglobin concentration and its variations to predict significant hemorrhage in the early phase of trauma? A multicentric cohort study. Ann. Intensive Care. 2018;8:76. doi: 10.1186/s13613-018-0420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fukuma H., Nakada T.A., Shimada T., Shimazui T., Aizimu T., Nakao S., Watanabe H., Mizushima Y., Matsuoka T. Prehospital lactate improves prediction of the need for immediate interventions for hemorrhage after trauma. Sci. Rep. 2019;9:13755. doi: 10.1038/s41598-019-50253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guyette F., Suffoletto B., Castillo J.L., Quintero J., Callaway C., Puyana J.C. Prehospital serum lactate as a predictor of outcomes in trauma patients: A retrospective observational study. J. Trauma. 2011;70:782–786. doi: 10.1097/TA.0b013e318210f5c9. [DOI] [PubMed] [Google Scholar]
- 38.St John A.E., McCoy A.M., Moyes A.G., Guyette F.X., Bulger E.M., Sayre M.R. Prehospital Lactate Predicts Need for Resuscitative Care in Non-hypotensive Trauma Patients. West J. Emerg. Med. 2018;19:224–231. doi: 10.5811/westjem.2017.10.34674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewis C.T., Naumann D.N., Crombie N., Midwinter M.J. Prehospital point-of-care lactate following trauma: A systematic review. J. Trauma Acute Care Surg. 2016;81:748–755. doi: 10.1097/TA.0000000000001192. [DOI] [PubMed] [Google Scholar]
- 40.Newgard C.D., Kampp M., Nelson M., Holmes J.F., Zive D., Rea T., Bulger E.M., Liao M., Sherck J., Hsia R.Y., et al. Deciphering the use and predictive value of “emergency medical services provider judgment” in out-of-hospital trauma triage: A multisite, mixed methods assessment. J. Trauma Acute Care Surg. 2012;72:1239–1248. doi: 10.1097/TA.0b013e3182468b51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Newgard C.D., Lin A., Eckstrom E., Caughey A., Malveau S., Griffiths D., Zive D., Bulger E. Comorbidities, anticoagulants, and geriatric-specific physiology for the field triage of injured older adults. J. Trauma Acute Care Surg. 2019;86:829–837. doi: 10.1097/TA.0000000000002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Rein E.A.J., van der Sluijs R., Houwert R.M., Gunning A.C., Lichtveld R.A., Leenen L.P.H., van Heijl M. Effectiveness of prehospital trauma triage systems in selecting severely injured patients: Is comparative analysis possible? Am. J. Emerg. Med. 2018;36:1060–1069. doi: 10.1016/j.ajem.2018.01.055. [DOI] [PubMed] [Google Scholar]
- 43.Nederpelt C.J., Mokhtari A.K., Alser O., Tsiligkaridis T., Roberts J., Cha M., Fawley J.A., Parks J.J., Mendoza A.E., Fagenholz P.J., et al. Development of a field artificial intelligence triage tool: Confidence in the prediction of shock, transfusion, and definitive surgical therapy in patients with truncal gunshot wounds. J. Trauma Acute Care Surg. 2021;90:1054–1060. doi: 10.1097/TA.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 44.Yoshimatsu Y., Tobino K., Kawabata T., Noguchi N., Sato R., Motomura D., Sueyasu T., Yoshimine K., Nishizawa S., Natori Y. Hemorrhaging from an intramedullary cavernous malformation diagnosed due to recurrent pneumonia and diffuse aspiration bronchiolitis. Intern. Med. 2021;60:1451–1456. doi: 10.2169/internalmedicine.5752-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee S., Kang W.S., Seo S., Kim D.W., Ko H., Kim J., Lee S., Lee J. Model for Predicting In-Hospital Mortality of Physical Trauma Patients Using Artificial Intelligence Techniques: Nationwide Population-Based Study in Korea. J. Med. Internet Res. 2022;24:e43757. doi: 10.2196/43757. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analyzed in the current study are not publicly available due to ethical restrictions on sharing a dataset because the data contain potentially identifying information. Further description or analysis of data are available from the authors upon reasonable request.