Abstract
Background:
This study explored whether there are mediated effects of child and family risk in the association between community and organizational risk and obesity among children and adolescents aged 10–17 years using 2017–2018 National Survey of Children's Health (NSCH) data, addressing autism spectrum disorder (ASD) and co-occurring conditions.
Methods:
This cross-sectional study (N = 27,157) used 2017–2018 NSCH data. Frequency distributions and chi-square tests were used to describe participants with and without ASD. Cumulative risk indices were created for child, family, community, and organizational level risk, and mediation analyses were conducted in a two-mediator model (X1: community risk, X2: organizational risk, M1: child risk, M2: family risk) for the dichotomous outcome (Y: obesity). Path analyses were performed using generalized structural equation modeling in Stata 16.0.
Results:
Direct effects for all four risk indices were associated with obesity in single index models (all p < 0.001); only child and family risk indices were associated with obesity in a full model with all four risk indices (both p < 0.001). When child and family risk indices were assessed as mediators, the indirect effects of community and organizational risk were significant (all p < 0.0001). The total effect of community risk on obesity was significant with family risk as a mediator (p = 0.002). The total effect of organizational risk was not significant with either mediator.
Conclusion:
Findings suggest that child and family factors play a strong role in obesity risk and that ASD contributes to this risk. Community risk may be another strong predictor of obesity, mediated by family risk. Additional research on social-ecological risk factors for obesity is needed to identify leverage points to improve obesity risk in children and adolescents with and without ASD.
Keywords: adolescence, ASD, childhood, cross-sectional, structural equation modeling
Introduction
Childhood obesity is a pressing public health concern, with a current estimated prevalence of 18.5% in the United States.1 Children with obesity are more likely to have obesity and chronic diseases such as type 2 diabetes, cardiovascular disease, and certain types of cancer as adults.2,3 Children with autism spectrum disorder (ASD) have an increased risk of having overweight or developing obesity compared with typically developing children, with an estimated obesity prevalence of 22.2% and a 41.1% greater risk of developing obesity compared with typically developing children.4 ASD, characterized by social communication and behavioral challenges, is one of the fasting growing developmental disabilities; the estimated prevalence of ASD in the United States is 23 per 1000 (1 in 44).5 Known risk factors for obesity in children with ASD include unhealthy eating behaviors, increased sedentary behavior, genetic vulnerabilities, and medication use to manage symptoms of ASD and co-occurring conditions.6
As obesity has been associated with various social-ecological determinants,7–12 a useful framework to develop a comprehensive understanding of obesity determinants is the Social Ecological Model (SEM).11,13 Variations of the SEM may include five levels of prevention that interact with each other: individual, such as age, education, and income; interpersonal, including family influences; institutional/organizational, including health care factors; community, such as school, workplace, and neighborhood factors; and policy, including laws and policies.14,15 The Institute of Medicine recommends the SEM to examine determinants of childhood obesity and provide a foundation for intervention research.16 However, there is a lack of integration of studies examining child characteristics with contextual factors of the family, community, and health care-related environment.17,18 Research on obesity in children and adolescents with and without ASD exploring synergistic effects among multiple social-ecological risk factors is limited. Moreover, research on obesity risk factors including ASD diagnosis have focused on child-level factors, rather than family, community, and health care-related factors.6
Research on child, family, community, and organizational factors associated with obesity that includes ASD and co-occurring conditions is warranted. Prior research using 2007–2008 National Survey of Children's Health (NSCH) data has suggested that children with ASD have increased levels of poor neighborhood social capital, greater parental aggravation and difficulty coping, and lower levels of relationship satisfaction and mental health.19 As children with ASD are less likely than other children with special health care needs to receive supportive services, such as occupational therapy and speech therapy,20 health care-related factors, including forgone medical care, should also be examined. Using 2016–2017 NSCH data, previous studies have indicated health insurance may be a protective factor against overweight and obesity in a general population sample of children and adolescents (i.e., most do not have ASD).21 Understanding the social-ecological context for obesity will aid in addressing disparities in life course outcomes present in children and adolescents, and particularly for children and adolescents with ASD and co-occurring conditions as they transition to adult health care.22
There is a need to identify significant independent associations with obesity that could represent potential mediating pathways in the relationship between child and family level risk factors and obesity. The purpose of this study was to examine associations between child, family, community, and organizational risk factors and obesity and to explore whether there are any mediated effects of child and family risk indices in the relationship between community and organizational risk indices and obesity among children and adolescents aged 10–17 years, addressing ASD and co-occurring conditions, using 2017–2018 NSCH data.
Methods
This cross-sectional study used 2017–2018 data from the nationally representative NSCH with a reference population of noninstitutionalized children aged 0–17 years living in the United States.23 Online surveys were completed by a parent or other adult caregiver with knowledge of the child's health and health care. The weighted response rates, which can approximate the proportion of the population for which data are available, were 37.4% and 43.1% for the 2017 and 2018 datasets, respectively.24 For this study, observations for participants aged 10–17 years with and without ASD who had data available for BMI and ASD diagnosis were included, resulting in an unweighted sample size of 27,157 children and adolescents aged 10–17 years (911 children with current ASD diagnosis, weighted n = 1,094,145; 26,246 children without ASD; weighted n = 32,082,679). Missing data were treated with simultaneous imputation methods by the NSCH; race, sex, and ethnicity were imputed using hot-deck imputation, and household income was imputed using regression imputation methods.25 Variables that were missing in error, that is, owing to respondent or system errors, were excluded from analyses. This study was reviewed by the University of South Florida Institutional Review Board and determined exempt.
Measures
Obesity
Using the BMI categories included in the NSCH dataset, obesity was coded as obesity vs. nonobesity (overweight, healthy weight, or underweight). The NSCH calculates BMI based on parent-reported height and weight (“What is this child's current height?” and “How much does this child currently weigh?”) for the selected child and determines obesity status based on the CDC growth chart, as it defines BMI-for-age at 95th percentile or greater as obesity.26
Autism spectrum disorder
Children were classified as having ASD based on “yes” responses to the questions: (1) “Has a doctor or other health care provider ever told you that this child has Autism or Autism Spectrum Disorder (ASD)? (Including diagnoses of Asperger's Disorder or Pervasive Developmental Disorder (PDD)” and (2) “If yes, does (child) currently have the condition?” Participants were excluded from the analysis to minimize misclassification if the response to the first question was “yes” but the response to the second question was “no.” Because question (2) is not based on the clinical evaluation, but rather based on the parents' self-report, we could not clearly verify whether the participants had a child with ASD or without ASD at the time of NSCH data collection.
Social-ecological risk indices
Four separate risk indices (child, family, community, and organizational) were developed based on chi-square tests for dichotomous variables and t-tests for continuous variables that indicated significant associations with obesity. Table 1 provides the characteristics used for each index. To allow equal weights for all variables in the indices, continuous variables were recoded on a 0–1 scale. The child risk index (0–6 points) included ASD diagnosis (current diagnosis vs. never diagnosed), co-occurring conditions [current diagnosis of one or more co-occurring conditions that were significantly associated with obesity (intellectual disability, learning disability, speech problems, developmental delay, depression, or anxiety) vs. never diagnosed with any co-occurring conditions], male sex (vs. female), Black race (vs. non-Black race), Hispanic ethnicity (vs. non-Hispanic ethnicity), and low household income (coded continuously from 0 to 1). Age, low birth weight, premature birth, and urbanicity were also examined and found not to be significantly associated with obesity.
Table 1.
Prevalence of Child, Family, Community, and Organizational Characteristics in Adolescents 10–17 Years with and without Obesity
|
Obesity
|
|
Without obesity
|
|
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| n | Weighted n | % | n | Weighted n | % | Test statistica | Degrees of freedom | p | |
| Child risk | |||||||||
| ASD diagnosis | 12.68 | 26,001 | 0.0004** | ||||||
| Currently diagnosed with ASD | 194 | 255,069 | 5.3 | 674 | 761,662 | 2.9 | |||
| Not diagnosed with ASD | 3242 | 4,528,289 | 94.7 | 21,993 | 25,781,719 | 97.1 | |||
| Co-occurring conditionsb | 17.77 | 26,164 | <0.0001*** | ||||||
| Has one or more co-occurring conditions | 977 | 1,118,209 | 23.3 | 4549 | 4,612,311 | 17.3 | |||
| Does not have any co-occurring conditions | 2487 | 3,689,625 | 76.7 | 18,253 | 22,094,662 | 82.7 | |||
| Age, years | 1.81 | 26,164 | 0.1789 | ||||||
| 10–13 | 1592 | 2,496,840 | 51.9 | 9802 | 13,125,508 | 50.9 | |||
| 14–17 | 1872 | 2,310,994 | 48.1 | 13,000 | 13,581,465 | 49.1 | |||
| Gender | 4.12 | 26,164 | 0.0424* | ||||||
| Male | 2088 | 2,632,165 | 54.7 | 11,563 | 13,493,693 | 50.5 | |||
| Female | 1376 | 2,175,668 | 45.3 | 11,239 | 13,213,280 | 49.5 | |||
| Race | 24.03 | 26,164 | <0.0001*** | ||||||
| Black | 378 | 981,974 | 20.4 | 1344 | 3,450,424 | 12.9 | |||
| Non-Black | 3086 | 3,825,858 | 79.6 | 21,458 | 23,256,548 | 87.1 | |||
| Ethnicity | 11.89 | 26,164 | 0.0006** | ||||||
| Hispanic | 525 | 1,531,092 | 31.8 | 2418 | 6,525,655 | 24.4 | |||
| Non-Hispanic | 2939 | 3,276,741 | 68.2 | 20,384 | 20,181,318 | 75.6 | |||
| Low birth weight | 0.23 | 25,166 | 0.6303 | ||||||
| Born with a low birth weight | 265 | 443,917 | 9.7 | 1842 | 2,333,044 | 9.2 | |||
| Did not have a low birth weight | 3043 | 4,123,045 | 90.3 | 20,118 | 23,144,385 | 90.8 | |||
| Premature birth | 1.86 | 25,778 | 0.1725 | ||||||
| Born premature | 439 | 631,068 | 13.4 | 2525 | 3,075,886 | 11.7 | |||
| Not born premature | 2973 | 4,092,318 | 86.6 | 19,943 | 23,266,240 | 88.3 | |||
| Urbanicity | 0.90 | 26,164 | 0.3418 | ||||||
| Lives in an urban areac | 2352 | 4,012,560 | 83.5 | 15,366 | 22,556,139 | 84.5 | |||
| Does not live in an urban area | 1112 | 795,273 | 16.5 | 7436 | 4,150,834 | 15.5 | |||
| Low household incomec | 0.54 | 0.41 | −9.46 | 26,164 | <0.0001*** | ||||
| Family risk | |||||||||
| Mother's health | 47.27 | 23,140 | <0.0001*** | ||||||
| Mother has excellent physical and mental health | 1503 | 1,961,968 | 49.5 | 13,519 | 14,864,679 | 64.0 | |||
| One or both of mother's physical and mental health is not excellent | 1476 | 1,999,265 | 50.5 | 6744 | 8,363,643 | 36.0 | |||
| Father's health | 24.88 | 20,025 | <0.0001*** | ||||||
| Father has excellent physical and mental health | 1304 | 1,618,920 | 55.8 | 12,140 | 13,218,412 | 67.3 | |||
| One or both of father's physical and mental health is not excellent | 1067 | 1,282,682 | 44.2 | 5616 | 6,415,330 | 32.7 | |||
| Household smoking | 33.82 | 25,795 | <0.0001*** | ||||||
| Someone in the household smokes | 790 | 1,025,316 | 21.8 | 3165 | 3,742,693 | 14.3 | |||
| No one in the household smokes | 2616 | 3,673,987 | 78.2 | 19,326 | 22,461,392 | 85.7 | |||
| Working poor | 13.38 | 25,692 | 0.0003** | ||||||
| Working poor household | 377 | 845,110 | 18.3 | 1658 | 3,275,018 | 12.6 | |||
| Not a working poor household | 3012 | 3,785,084 | 81.7 | 20,747 | 22,740,356 | 87.4 | |||
| Food insufficiency | 62.32 | 25,729 | <0.0001*** | ||||||
| Could always afford nutritious meals | 1972 | 2,527,108 | 54.3 | 17,003 | 18,275,911 | 69.9 | |||
| Could not always afford nutritious meals | 1425 | 2,130,303 | 45.7 | 5431 | 7,866,552 | 30.1 | |||
| Emotional support | −0.26 | 20,333 | 0.2851 | ||||||
| Parents have emotional support | 2616 | 3,357,648 | 71.0 | 18,073 | 19,251,184 | 73.2 | |||
| Parents do not have emotional support | 800 | 1,373,477 | 29.0 | 4481 | 7,061,095 | 26.8 | |||
| Family adversityc | 0.23 | 0.20 | −2.16 | 25,512 | 0.031* | ||||
| Lack of parent copingc | 0.12 | 0.13 | 0.85 | 26,050 | 0.396 | ||||
| Parental aggravationc | 0.19 | 0.18 | 2.48 | 25,785 | 0.013* | ||||
| Lack of parent educationc | 0.43 | 0.30 | −8.35 | 26,266 | <0.0001*** | ||||
| ACE countd | 1.35 | 0.97 | −6.71 | 25,936 | <0.0001*** | ||||
| Community risk | |||||||||
| Lack of neighborhood supportc | 0.28 | 0.25 | −3.16 | 25,490 | 0.002** | ||||
| Lack of school safetyc | 0.13 | 0.11 | −2.75 | 25,534 | 0.006** | ||||
| Lack of neighborhood amenitiesc | 0.37 | 0.33 | −2.98 | 25,432 | 0.003** | ||||
| Lack of neighborhood safetyc | 0.86 | 0.87 | 1.18 | 25,776 | 0.0237* | ||||
| Neighborhood detracting elementsc | 0.12 | 0.086 | 3.91 | 25,558 | <0.0001*** | ||||
| Organizational risk | |||||||||
| Forgone care | 8.17 | 26,089 | 0.0043** | ||||||
| Forgone health care | 167 | 321,385 | 6.7 | 618 | 961,668 | 3.6 | |||
| No forgone health care | 3287 | 4,442,913 | 93.3 | 22,119 | 25,623,161 | 96.4 | |||
| Special education | 8.94 | 26,056 | 0.0028** | ||||||
| Receives special education or early intervention plan | 512 | 609,216 | 12.7 | 2247 | 2,483,144 | 9.4 | |||
| Does not receive special education or early intervention plan | 2935 | 4,169,375 | 87.3 | 20,464 | 24,073,543 | 90.6 | |||
| Special services | 11.52 | 25,886 | 0.0007** | ||||||
| Receives special services | 319 | 426,805 | 9.0 | 1285 | 1,520,893 | 5.8 | |||
| Does not receive special services | 3114 | 4,317,723 | 91.0 | 21,270 | 24,860,583 | 94.2 | |||
| Medical home | 21.78 | 26,161 | <0.0001*** | ||||||
| Health care meets medical home criteria | 1644 | 1,899,156 | 39.6 | 12,045 | 12,987,582 | 48.6 | |||
| Health care does not meet medical home criteria | 1819 | 2,901,085 | 60.4 | 10,395 | 13,713,911 | 51.4 | |||
| Insurance | 0.076 | 26,092 | 0.7829 | ||||||
| Adequate health insurance | 2206 | 3,046,823 | 63.8 | 14,764 | 17,084,812 | 64.3 | |||
| Not adequate health insurance | 1245 | 1,729,705 | 36.2 | 7979 | 9,468,212 | 35.7 | |||
Chi-square tests and t-tests were conducted to identify associations with obesity (vs. nonobesity).
Design-based F statistic for chi-square tests and t statistic for t-tests.
Intellectual disability, learning disability, speech problems, developmental delay, depression, or anxiety.
Comparison of means for variables weighted on a 0–1 scale.
Count of ACEs (0–9).
p < 0.05; **p < 0.01; ***p < 0.001.
ACE, adverse childhood experience; ASD, autism spectrum disorder.
The family risk index (0–16 points) included poor/average overall health of mother (excellent physical and mental health vs. one or both not excellent), poor/average overall health of father (excellent physical and mental health vs. one or both not excellent), household smoking (vs. no household smoking), working poor (vs. not working poor), food insufficiency (“We could always afford to eat good nutritious meals” vs. “We could always afford enough to eat but not always the kinds of food we should eat,” “Sometime we could afford enough to eat,” or “Often we could not afford enough to eat”),27 family adversity (coded continuously from 0 to 1), parental aggravation (coded continuously from 0–1), lack of parent education (coded continuously from 0 to 1), and adverse childhood experiences (ACEs) count (coded continuously from 0 to 9). Based on the NSCH, “working poor” households have someone employed for 50 weeks in the past year and a total household income <100% federal poverty level (FPL). Family adversity was derived from four reverse-coded questions about family members talking about what to do when faced with problems, working together to solve problems, knowing they have strength to draw on when faced with problems, and staying hopeful in difficult times when faced with problems. Parental aggravation was derived from three questions about parents feeling, during the past month: their child was harder than most to care for, their child did things that bothered them, and angry with their child. Lack of parent education was based on the “Highest education of adult in household” variable (“Less than high school,” “High school degree or GED,” “Some college or technical school,” “College degree or higher”). ACEs were derived from a count of nine ACEs. Emotional support and lack of parent coping were also examined and found not to be significantly associated with obesity.
The community risk index (0–4 points) included four variables that were coded continuously from 0 to 1: lack of neighborhood support, lack of school safety, lack of neighborhood amenities, and neighborhood detracting elements. Lack of neighborhood support was derived from three reverse-coded questions about people in the neighborhood: helping each other out, watching out for each other's children, and knowing where to go for help. Lack of school safety was derived from reverse-coded Likert scale responses regarding parents perceiving that their children are safe at school. Lack of neighborhood amenities was derived from four questions about the neighborhood: not containing sidewalks or walking paths; not containing a park or playground area; not containing a recreation center, community center or Boys’/Girls' Club; not containing a library or bookmobile. Neighborhood detracting elements was derived from three questions about the neighborhood: having litter or garbage on sidewalks and streets, having poorly kept or dilapidated housing, and having broken windows or graffiti. Lack of neighborhood safety was also examined and found not to be significantly associated with obesity.
The organizational risk index (0–4 points) included: forgone care (“Yes” vs. “No” response to “During the past 12 months, was there any time when this child needed health care but it was not received?”), special education (currently receives special education or early intervention plan vs. does not currently receive special education or early intervention plan), special services (currently receives special services to meet child's developmental needs vs. does not currently receive special services to meet child's developmental needs), and lack of medical home (health care does not meet medical home criteria vs. health care meets medical home criteria), were all coded as dichotomous variables. The NSCH measures the presence of a medical home28 based on 16 items from 5 domains: personal doctor or nurse, usual source for sick case, family-centered care, problems getting needed referrals, and effective care coordination when needed. Insurance was also examined and found not to be significantly associated with obesity.
Demographic characteristics
Age was measured as a numerical value from 10 to 17. Sex was a dichotomous variable including male and female. Race/ethnicity was a categorical variable including Hispanic; White, non-Hispanic; Black, non-Hispanic; and Multiracial/Other. Household income was a categorical variable including: 0%–99% FPL, 100%–199% FPL, 200%–399% FPL, and 400% FPL or greater. Household income refers to the combined annual income of all members in the household. FPL is the poverty threshold set forth by the US Census Bureau to estimate the number of Americans in poverty.
Statistical Analysis
Analyses were performed in STATA/SE 16.29 Analyses were weighted to account for selection and nonresponse bias. An a priori conceptual model was designed based on the social-ecological framework (i.e., having individual, interpersonal, community, and organizational levels) using risk indices and their corresponding indicators. The study sample was described for participants with and without ASD using frequency distributions and chi-square tests to identify bivariate associations for the development of risk indices and to describe demographic characteristics of children and adolescents with and without ASD. Variables that were not associated with the outcome of obesity were excluded from the risk indices and subsequent analyses.
Direct, indirect, and total effects were assessed using the mediation analysis framework proposed by Baron and Kenny.30 A mediator is a variable that is part of the causal pathway between an exposure and outcome. Mediation quantifies the causal relationship between an exposure, mediator, and outcome. The total effect of an exposure on the outcome can be broken down into the exposure's direct effect and indirect effect. The direct effect is the remaining effect from the exposure on the outcome after considering the mediator in the model. The indirect effect is the product of the effect of exposure on the mediator and the effect of the mediator on the outcome.
Based on analysis of direct effects of child, family, community, and organizational risk on obesity using separate models for each risk index, child and family level factors were identified as possible mediators, and community and organizational factors were identified as distal factors. Mediation analyses were conducted in a two-mediator model (X1: community risk, X2: organizational risk, M1: child risk, M2: family risk) for the dichotomous outcome (Y: obesity). Variables included in the risk indices are given in Table 1. As it was hypothesized that there would be a relationship between child and family risk indices, two plausible models were tested: one with and one without covariance between error variables for child and family risk indices. The model with covariance between the error variables was selected owing to a smaller Bayesian information criterion value. Path analyses were performed to examine indirect and total effects of community and organizational risk with child and family risk as mediators using generalized structural equation modeling (GSEM). Parameter estimation was performed with the maximum likelihood estimation method. The Bernoulli likelihood and logit link function were applied to the outcome variable of obesity. Unstandardized beta coefficients are reported owing to constraints of GSEM procedures in STATA.
Results
Obesity prevalence was 25.1% in children and adolescents with ASD and 14.9% in those without ASD (p = 0.0004). Children and adolescents with ASD were more likely to be male (75.3% vs. 50.3%, p < 0.0001), have lower household income (45.6% at 200% of the FPL or greater vs. 58.5%, p = 0.0231). Children and adolescents with ASD were 75.3% male, 47% non-Hispanic White, 33.7% Hispanic, 12.6% non-Hispanic Black, and 6.8% non-Hispanic Multiracial/Other. Children and adolescents without ASD were 50.3% male, 49.7% non-Hispanic White, 25.6% Hispanic, 14.8% non-Hispanic Black, and 9.9% non-Hispanic Multiracial/Other. Full demographic characteristics for children and adolescents with and without ASD are given in Table 2.
Table 2.
Demographic Characteristics in Adolescents 10–17 Years with and without Autism Spectrum Disorder
|
ASD
|
Without ASD
|
|
|
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| N | Weighted n | % | n | Weighted n | % | F statistic | Degrees of freedom | p | |
| Obesity | 12.68 | 26,001 | 0.0004*** | ||||||
| Obesity | 194 | 255,069 | 25.1 | 3242 | 4,528,289 | 14.9 | |||
| Nonobesity | 674 | 761,662 | 74.9 | 21,993 | 25,781,719 | 85.1 | |||
| Age, years | 0.034 | 27,055 | 0.8548 | ||||||
| 10–13 | 397 | 557,998 | 51.0 | 11,500 | 16,105,515 | 50.2 | |||
| 14–17 | 514 | 536,147 | 49.0 | 14,746 | 15,977,165 | 49.8 | |||
| Sex | 26.62 | 27,055 | <0.0001*** | ||||||
| Male | 710 | 823,791 | 75.3 | 13,388 | 16,130,743 | 50.3 | |||
| Female | 201 | 270,354 | 24.7 | 12,858 | 15,951,936 | 49.7 | |||
| Race/ethnicity | 2.052 | 27,055 | 0.1288 | ||||||
| Hispanic | 109 | 368,362 | 33.7 | 2997 | 8,220,393 | 25.6 | |||
| White, non-Hispanic | 639 | 513,805 | 47.0 | 18,290 | 15,938,460 | 49.7 | |||
| Black, non-Hispanic | 58 | 137,597 | 12.6 | 1785 | 4,736,533 | 14.8 | |||
| Multiracial/Other, non-Hispanic | 105 | 74,382 | 6.8 | 3174 | 3,187,294 | 9.9 | |||
| Household income | 3.52 | 27,055 | 0.0231* | ||||||
| 0%–99% FPL | 137 | 260,151 | 23.8 | 3067 | 6,403,188 | 20.0 | |||
| 100%–199% FPL | 194 | 335,184 | 30.6 | 4061 | 6,886,056 | 21.5 | |||
| 200%–399% FPL | 268 | 245,549 | 22.4 | 7794 | 8,676,192 | 27.0 | |||
| 400% FPL or greater | 312 | 253,260 | 23.2 | 11,324 | 10,117,243 | 31.5 | |||
Chi-square tests were conducted to examine differences between adolescents with and without ASD.
*p < 0.05; ***p < 0.001.
FPL, federal poverty level.
Direct Effects
The direct effects of child, family, community, and organizational risk indices on obesity were examined through separate models by social-ecological level and a full model with all four levels. In separate single index models, child, family, community, and organizational risk indices (all p < 0.0001) were associated with obesity. The direct effects of community and organizational risk were no longer significant, indicating child and family risk mediate most of the effects of community and organization risks on obesity. The results for direct effects are given in Table 3.
Table 3.
Direct Effects of Child, Family, Community, and Organizational Risk Indices on Obesity in Adolescents Aged 10–17 Years
| Separate models (path coefficient, p -value) | Full model (path coefficient, p -value) | |
|---|---|---|
| Child risk | 0.40, p < 0.0001*** | 0.26, p < 0.0001*** |
| Family risk | 0.18, p < 0.0001*** | 0.14, p < 0.0001*** |
| Community risk | 0.42, p < 0.0001*** | 0.082, p = 0.343 |
| Organizational risk | 0.29, p < 0.0001*** | −0.016, p = 0.827 |
Path analyses were performed separately for each risk index and for the full model using generalized structural equation modeling.
p < 0.001.
Indirect and Total Effects
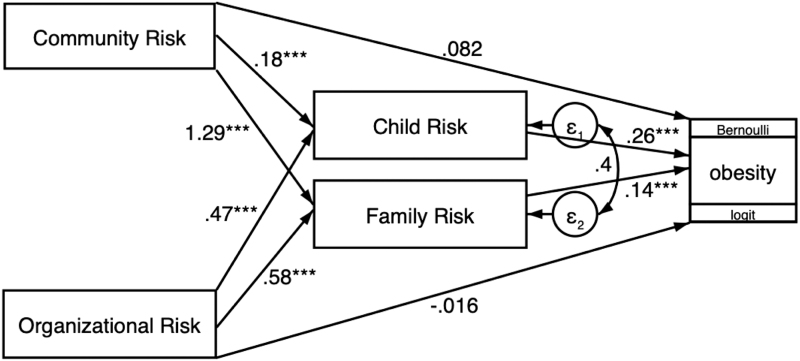
When child risk and family risk were separately analyzed as mediators, the indirect effects of community risk (β = 0.046 and β = 0.18, respectively) and organizational risk (β = 0.12 and β = 0.081, respectively) were significant (all p < 0.0001). In the full model, the total effect of community risk on obesity was significant when family risk was analyzed as the mediator (β = 0.26, p = 0.002). The other three total effects examined were not significant. Indirect and total effects of community and organizational risk indices on obesity are given in Table 4, and the full model summarizing indirect and direct effects of community and organizational risk indices on obesity is given in Figure 1.
Table 4.
Indirect and Total Effects of Community and Organizational Risk Indices on Obesity in Adolescents Aged 10–17 Years in the Full Model with Child, Family, Community, and Organizational Risk Indices
| Indirect effect (coefficient, p -value) | Total effect (coefficient, p -value) | |
|---|---|---|
| Child risk | ||
| Community risk | 0.046, p < 0.0001*** | 0.13, p = 0.138 |
| Organizational risk | 0.12, p < 0.0001*** | 0.11, p = 0.113 |
| Family risk | ||
| Community risk | 0.18, p < 0.0001*** | 0.26, p = 0.002** |
| Organizational risk | 0.081, p < 0.0001*** | 0.065, p = 0.357 |
Path analyses were performed to examine indirect and total effects of community and organizational risk with child and family risk as mediators using generalized structural equation modeling.
p < 0.01; ***p < 0.001.
Figure 1.
Full mediation model including child, family, community, and organizational risk indices. aValues represent unstandardized beta coefficients for indirect and direct effects. ***p < 0.001.
Discussion
This study investigated associations between ASD and other child, family, community/neighborhood, and organizational risk factors and obesity and examined whether there were mediated effects of child and family risk indices in the associations between community and organizational risk indices and obesity among children and adolescents aged 10–17 years using 2017–2018 NSCH data. Several factors from child, family, community, and organizational levels were associated with obesity, and each of the risk indices was independently associated with obesity, indicating multilevel obesity risk factors in addition to ASD and co-occurring conditions. Although the indirect effects of community and organizational risk were significant with child and family risk as mediators, total effect was only significant for the relationship between community risk and obesity, mediated by family risk.
The results suggested that community risk may be a strong predictor of obesity (β = 0.26), mediated by family risk. These factors include important indicators such as neighborhood support, safety, amenities, and distracting elements, as well as school safety. As ASD was included in the child risk index along with co-occurring conditions, gender, race, ethnicity, and income, the finding that the relationship between community risk and obesity may be mediated by family risk is applicable to all children and adolescents. The community risk index may be a strong predictor for obesity owing to the inclusion of both school and neighborhood components.31,32 Previous research has also suggested that community factors, including neighborhood characteristics, parent perceptions of neighborhood characteristics,11 and the school environment33 were associated with children's overweight/obesity status.
Although the organizational risk index was associated with obesity in a single index model (p < 0.0001), and the indirect effects were significant when both child and family risk indices were assessed as mediators, the total effects of organizational risk were not significant with either mediator. As only four variables (forgone care, special education, special services, and lack of medical home) were included in the organizational risk index, there may be a need for additional variables related to health care and service utilization. Among children and adolescents with ASD, unmet care needs may include information on services, family support, and respite care.34 In the general population, prior research has found associations between health care access variables, such as having a usual source of care provider, well-child visits, and preventative dental use, and obesity among children,35 but there is a lack of research using multivariable risk indices or latent variables to investigate health care or other organizational level risk factors or obesity among children and adolescents with or without ASD.
This study was limited by the cross-sectional methodology of the NSCH. There were no data on age of onset for the obesity outcome, so directionality of associations cannot be determined. Moreover, national-level data for children and adolescents with ASD or nationally representative data with ASD-specific weights are needed to conduct mediation analyses in samples of children and adolescents with ASD. In addition, risk indices for this study were created by applying weights to differences in scales such that continuous variables were coded 0–1.
Future research may improve upon this methodology by taking into account regression coefficients or otherwise standardizing values. This study was further limited by the fact that our risk indices included general variables for each level of the SEM model. Future analyses may define more specific family-level risk indices including variables such as family screen time and family eating meals together. Furthermore, as the study relies on self-report for all measures, there may be information bias, particularly for key variables including ASD diagnosis and BMI.
Nevertheless, this research provides insight into pathways for obesity risk in children and adolescents aged 10–17 years by applying the SEM to understand ASD and other risk factors using a large, nationally representative dataset. Twenty-five risk factors, including ASD, were included in four separate risk indices. Our findings buttress past research by elucidating pathways between these risk indices and including ASD and co-occurring conditions. A conceptual model will aid in directing coordinated care among health care providers by delineating evidence-based interaction among multiple levels of the SEM and potential pathways for intervention.
The pathways involving the child risk index highlight the significance of ASD in obesity risk, whereas the pathways involving the family risk index point to the importance of family, community, and organizational risk factors among all children and adolescents. The community risk index in particular emerged as a strong predictor of obesity. As the family risk index included nine variables (mother's health, father's health, household smoking, working poor, food insufficiency, family adversity, parental aggravation, lack of parent education, and count of ACEs), future research should investigate how these factors work together to influence obesity risk among children and adolescents.
The findings of this study may help to identify leverage points for advancing best practices to improve the physical and behavioral health of children and adolescents with and without ASD. For example, parents and families may support their children's healthy lifestyle behaviors through positive role modeling, and providers may encourage family involvement in promoting these behaviors for children and adolescents. Moreover, community stakeholders may be identified to help create healthy school and neighborhood environments. Investing in and increasing the availability of inclusive sports and recreation programs for children and adolescents may also be leveraged. Further research on social-ecological risk factors for obesity is needed to inform children and adolescents, parents, care providers, and policy makers alike36 on key pathways for action. The risk indices used in this study can be used as a guiding framework for research and practice. Future research should investigate and define community and organizational level risk factors among children and adolescents, and obesity prevention interventions should target the community environment, including school and neighborhood safety and access to nutrient-dense food and physical activity opportunities in children and adolescents with and without ASD. Future studies may also include behavioral variables that have been established in the literature as obesity risk factors, such as physical activity, for a more comprehensive social-ecological analysis.
Disclaimer
This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by Health Resources and Services Administration (HRSA), Health and Human Services (HHS), or the U.S. Government.
Funding Information
This project is supported by the HRSA of the U.S. Department of HHS under Grant No. R41MC39340 and R40 Maternal and Child Health Field-initiated Innovative Research Studies Program. A.W.B. is currently supported by the National Cancer Institute Behavioral Oncology Education and Career Development Grant (T32CA090314, MPIs Vadaparampil/Brandon).
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief 2017;1–8. [PubMed] [Google Scholar]
- 2. Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes Rev 2016;17:56–67. [DOI] [PubMed] [Google Scholar]
- 3. Sahoo K, Sahoo B, Choudhury AK, et al. Childhood obesity: Causes and consequences. J Family Med Prim Care 2015;4:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kahathuduwa CN, West BD, Blume J, et al. The risk of overweight and obesity in children with autism spectrum disorders: A systematic review and meta-analysis. Obes Rev 2019;20:1667–1679. [DOI] [PubMed] [Google Scholar]
- 5. Maenner MJ, Shaw KA, Bakian AV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. Morb Mortal Wkly Rep 2021;70:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dhaliwal KK, Orsso CE, Richard C, et al. Risk factors for unhealthy weight gain and obesity among children with autism spectrum disorder. Int J Mol Sci 2019;20:3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Granich J, Lin A, Hunt A, et al. Obesity and associated factors in youth with an autism spectrum disorder. Autism Int J Res Pract 2016;20:916–926. [DOI] [PubMed] [Google Scholar]
- 8. Gurnani M, Birken C, Hamilton J. Childhood obesity: Causes, consequences, and management. Pediatr Clin North Am 2015;62:821–840. [DOI] [PubMed] [Google Scholar]
- 9. Nichols M, Nemeth LS, Magwood G, et al. Exploring the contextual factors of adolescent obesity in an underserved population through photovoice. Fam Community Health 2016;39:301–309. [DOI] [PubMed] [Google Scholar]
- 10. Ohri-Vachaspati P, Lloyd K, Delia D, et al. A closer examination of the relationship between children's weight status and the food and physical activity environment. Prev Med 2013;57:162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ohri-Vachaspati P, DeLia D, DeWeese RS, et al. The relative contribution of layers of the Social Ecological Model to childhood obesity. Public Health Nutr 2015;18:2055–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stark CM, Devine CM, Dollahite JS. Characteristics associated with the application of an ecological approach to preventing childhood obesity. Public Health Nutr 2017;20:174–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol 1977;32:513–531. [Google Scholar]
- 14. Pereira MMCE, Padez CMP, Nogueira HG da SM. Describing studies on childhood obesity determinants by Socio-Ecological Model level: A scoping review to identify gaps and provide guidance for future research. Int J Obes (Lond) 2019;43:1883–1890. [DOI] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention. The social-ecological model: A framework for prevention. January 29, 2021. https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html (Last accessed September 22, 2021).
- 16. Institute of Medicine (US) Committee on Prevention of Obesity in Children and Youth; Koplan JP, Liverman CT, Kraak VI (eds). Preventing Childhood Obesity: Health in the Balance. Atlanta, GA: National Academies Press (US), 2005. [PubMed] [Google Scholar]
- 17. Fein D, Helt M. Facilitating autism research. J Int Neuropsychol Soc 2017;23:903–915. [DOI] [PubMed] [Google Scholar]
- 18. Happé F, Ronald A. The “fractionable autism triad”: A review of evidence from behavioural, genetic, cognitive and neural research. Neuropsychol Rev 2008;18:287–304. [DOI] [PubMed] [Google Scholar]
- 19. Hock R, Ahmedani BK. Parent perceptions of autism severity: Exploring the social ecological context. Disabil Health J 2012;5:298–304. [DOI] [PubMed] [Google Scholar]
- 20. Benevides TW, Carretta HJ, Lane SJ. Unmet need for therapy among children with autism spectrum disorder: Results from the 2005-2006 and 2009-2010 National Survey of Children with special health care needs. Matern Child Health J 2016;20:878–888. [DOI] [PubMed] [Google Scholar]
- 21. Yusuf ZI, Dongarwar D, Yusuf RA, et al. Social determinants of overweight and obesity among children in the United States. Int J MCH AIDS 2020;9:22–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Acharya K, Meza R, Msall ME. Disparities in life course outcomes for transition-aged youth with disabilities. Pediatr Ann 2017;46:e371–e376. [DOI] [PubMed] [Google Scholar]
- 23. Child and Adolescent Health Measurement Initiative (CAHMI). The 2017-2018 National Survey of Children's Health (2 years combined data set), STATA Indicator Data Set. 2019. www.childhealthdata.org (Last accessed September 13, 2020).
- 24. Child and Adolescent Health Measurement Initiative. Fast Facts: 2017-2018 National Survey of Children's Health. Data Resource Center for Child and Adolescent Health, supported by Cooperative Agreement U59MC27866 from the U.S. Department of Health and Human Services, Health Resources and Services Administration's Maternal and Child Health Bureau (HRSA MCHB). www.childhealthdata.org (Last accessed March 15, 2022).
- 25. U.S. Census Bureau. 2018 National Survey of Children's Health: Methodology Report. 2019. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2018-NSCH-Methodology-Report.pdf (Last accessed March 15, 2022).
- 26. Centers for Disease Control and Preventio, National Center for Health Statisticsn. CDC Growth Charts: United States. 2000. www.cdc.gov/growthcharts (Last accessed March 15, 2022).
- 27. Sonik RA, Coleman-Jensen A, Parish SL. Household food insufficiency, health status, and emergency healthcare utilization among children with and without special health care needs. Public Health Nutr 2020;23:3204–3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Medical Home Initiatives for Children with special needs Project Advisory Committee. The Medical Home. Pediatrics 2002;110:184–186.12093969 [Google Scholar]
- 29. StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC, 2019. [Google Scholar]
- 30. Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 31. Gray HL, Buro AW, Barrera Ikan J, et al. School-level factors associated with obesity: A systematic review of longitudinal studies. Obes Rev 2019;20:1016–1032. [DOI] [PubMed] [Google Scholar]
- 32. Suglia SF, Shelton RC, Hsiao A, et al. Why the neighborhood social environment is critical in obesity prevention. J Urban Health 2016;93:206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Noh K, Min JJ. Understanding school-aged childhood obesity of Body Mass Index: Application of the social-ecological framework. Children (Basel) 2020;7:E134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hodgetts S, Zwaigenbaum L, Nicholas D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism 2015;19:673–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Berdahl T, Biener A, McCormick MC, et al. Annual Report on Children's Healthcare: Healthcare access and utilization by obesity status in the United States. Acad Pediatr 2020;20:175–187. [DOI] [PubMed] [Google Scholar]
- 36. Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet 2015;385:2410–2421. [DOI] [PubMed] [Google Scholar]