Abstract
The point-of-care ultrasound (POCUS) has been effectively used in intensive care units for the management of septic patients. Since it is a time- and cost-effective non-invasive imaging modality, its use in the emergency department (ED) has been advocated for by medical experts. This review summarizes the existing literature regarding the breadth of POCUS as a supplementary tool to the holistic approach of septic patients in the ED setting. A literature search was conducted via PubMed (MEDLINE), Cochrane Library, and Scopus databases, analyzing studies which examined the use of POCUS in the ED for non-traumatic, septic, and/or undifferentiated hypotensive patients, resulting in 26 studies. The first cluster of studies investigates the efficiency of POCUS protocols in the differential diagnosis and its reliability for distributive/septic shock and sepsis management. In the second cluster, POCUS use results in faster sepsis cause identification and improves therapeutic management. The third cluster confirms that POCUS aids in the accurate diagnosis and management, even in rare and complicated cases. The results of the present review support the well-documented utility of POCUS and highlight the importance of POCUS incorporation in the comprehensive management of the septic patient in the ED setting.
Keywords: emergency department, point-of-care ultrasound, sepsis, septic shock
1. Introduction
Sepsis is a medical emergency and a life-threatening disorder, which imposes a major health burden on emergency departments (EDs) and intensive care units (ICUs), accounting for a significant proportion of in-hospital and ICU mortality [1]. In a recent analysis of the Global Burden of Disease, Injuries, and Risk Factors (GBD), sepsis morbidity and mortality is estimated to 48.9 million global cases and 11 million deaths, or 1 in 5 deaths worldwide. Of the 48.9 million cases, 33.1 have occurred in patients with an underlying infectious condition and the remaining 15.8 million in individuals with underlying injuries or non-communicable diseases (NCD) [2]. Although the initial interest on sepsis has been focused in the ICU setting, attention has been gradually shifted towards the ED field, since it has been recognized that the early initiation of treatment in the ED [3], ideally within one hour from the diagnosis of sepsis, is crucial in order to decrease length of stay, morbidity, and mortality [4].
To this end, point-of-care ultrasonography (POCUS) has emerged as an adjunct imaging modality for the management of the septic patient upon arrival to the ED. POCUS allows for fast, real-time assessment of cardiovascular, respiratory, or other acute pathologies. Moreover, as an extension of physical examination and in conjunction with additional testing, it narrows differential diagnosis. In this way, it enhances the initial management plan and it shortens the time to clinical decision-making. Apart from its diagnostic value, POCUS can also provide information regarding a patient’s response to treatment when serially performed [5,6]. Ιn the 1990s, emergency medicine (EM) physicians in the United States of America advocated for the use of POCUS in the ED, so POCUS nowadays is a standard component of EM residency training programs [5]. In light of the recognition of the usefulness of POCUS in EM, several ultrasound protocols have been developed and implemented. The most well-known and widely used protocol for non-traumatic patients is the rapid ultrasound in shock (RUSH) exam, which helps clinicians differentiate various etiologies of shock in a short period of time [6,7,8].
Considering the enormous sepsis-induced burden on health care systems [2], in conjunction with the complex nature of sepsis-associated causes and symptoms, it is obvious that the integration of methods and techniques for early diagnosis and management of sepsis in the ED is not just useful, but also of critical importance. In view of the aforementioned facts, the aim of this manuscript is to review the existing literature regarding the breadth of POCUS use and its contribution to the prompt diagnosis and effective management of septic patients in the ED setting. Specifically, the present review focuses on the existing data with reference to the utility and reliability of multimodal POCUS for non-invasive differential diagnosis of shock, rapid identification of the septic source, and treatment guidance.
2. Materials and Methods
A literature review was conducted using the online databases PubMed (MEDLINE), Cochrane Library, and Scopus. In our search strategy, the publication period under consideration was defined from 2010 to July 2022, excluding all grey literature.
The combinations of medical subject headings that were used in searching included the following: [Sepsis OR Septic Shock OR Septic OR Undifferentiated Shock OR Hypotensive Patient] and [Emergency Department OR ED OR Emergency Room OR Emergency Medicine] or [Point-of-Care OR Bedside OR POCUS] and [Ultrasonography OR US]. In addition to the database search, the cited bibliography of the selected articles was reviewed in order to ensure that no significant relevant research data were missed.
Three reviewers worked independently to review all eligible titles and abstracts, and by using inclusion criteria, defined a priori. These criteria were: publication language (English), time of publication (2010–July 2022), aim (assessment of POCUS use in the ED for non-traumatic, septic, and/or undifferentiated hypotensive patients), and research type, namely randomized clinical trials (RCTs), observational studies (including both prospective and retrospective cohorts), and case reports. After initial selection, the reviewers read the full text to determine whether inclusion criteria were met.
3. Results
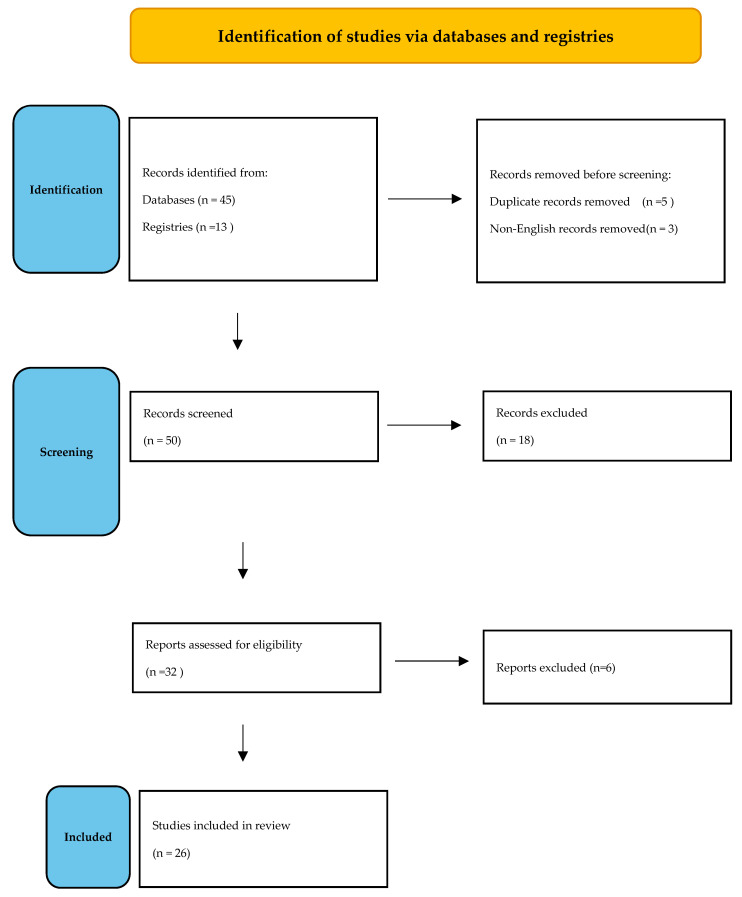
Initial search resulted in a total of 58 articles, with 32 being eligible for review. After reading the full text, 6 more articles not meeting inclusion criteria were excluded. Eventually, 26 articles [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] were included in the final analysis (Figure 1).
Figure 1.
Search flow diagram.
Out of 26 articles, 11 were prospective observational studies, 2 were RCTs, 1 was a retrospective cohort trial, and 12 were case reports. All but two ([10,14]) were single-center studies. Except for the case reports, the remaining 13 articles were divided into two categories based on their main purpose: the first cluster comprised 9 articles [9,10,11,12,13,14,15,16,17] which studied the contribution of POCUS to the diagnosis of undifferentiated hypotensive/critically ill, non-traumatic patients (Table 1); the second cluster consisted of 5 articles [18,19,20,21,22] which studied the utility of POCUS in determining sepsis cause and managing those patients (Table 2). The main results of the 12 case reports [23,24,25,26,27,28,29,30,31,32,33,34] are presented in Table 3.
Table 1.
Studies examining the contribution of POCUS to the diagnosis of undifferentiated hypotensive/critically ill patients *.
| 1st Author, Year, Country, Design, Setting | POCUS Protocol (If Any) | Aim | Patient Number/Age | Main Results |
|---|---|---|---|---|
| Ahn et al., 2017, Korea, POS, single- center ED [9] | SEARCH 8E’s | “SEARCH 8E’s” protocol vs. final diagnosis | 308/>18 yo |
|
| Atkinson et al., 2018, international (N. America & S. Africa), RCT, multicenter (n = 6) [10] | Μulti-organ POCUS based on ACES & RUSH protocols | POCUS protocol vs. standard care without POCUS |
273/>19 yo |
|
| Bagheri-Hariri et al., 2015, Iran, POS pilot, single-center ED [11] | RUSH | RUSH-based shock type diagnosis vs. final diagnosis |
25/N/A |
|
| Ghane et al., 2015, Iran, POS, single- center ED [12] | RUSH | Accuracy of early RUSH protocol performed by emergency physicians to predict shock type in critically ill patients |
52/>18 yo |
|
| Javali et al., 2020, India, POS, single—center ED, 18-month period [13] | Multi-organ POCUS protocol | Multi-organ POCUS to improve accuracy, narrow differential diagnosis, test effectiveness of EGDT |
100/>18 yo |
|
| Mosier et al., 2019, USA, ROS (cohort), 2-center EDs [14] | Impact of POCUS on care processes and outcomes in critically ill nontraumatic patients Method: 3 patient cohorts: no POCUS (cohort 1 = 4165), POCUS prior to key intervention (cohort 2 = 614), and POCUS after key intervention (cohort 3 = 662). Primary outcome: in-hospital mortality |
5441/> 18 yo |
|
|
| Sasmaz et al., 2017, Turkey, POS, single-center ED [15] | RUSH | Effect of POCUS on clinical decision, by comparing diagnosis before and after POCUS with the definitive diagnosis |
180/>18 yo |
|
| Shokoohi et al., 2015, USA, POS, single-center ED, 32-month period [16] | US hypotensionprotocol (FOCUS, RV, IVC, abdominal & transthoracic scans) | Impact of protocol on diagnostic certainty & ability, treatment, and resource utilization |
118/>18 yo |
|
| Volpicelli et al., 2013, Italy, POS, single-center ED [17] | Multi-organ POCUS protocol | Efficacy of protocol, for diagnostic process of symptomatic, hypotensive patients in the ED Assessment of decisive role of included lung scan |
108/N/A |
|
* All studies excluded traumatic patients and/or hypotension due to obvious cause. Abbreviations: ACES = Abdominal and cardiac evaluation with sonography in shock; APACHE II = Acute physiology and chronic health evaluation II; CI = Confidence interval; CT = Computerized tomography; ED = Emergency department; CVP = Central venous pressure; EGDT = Early goal-directed therapy; FOCUS = Focused echocardiography; IVC = Inferior vena cava; k = Kappa coefficient; LOS = Length of stay; LV = Left ventricle; LVEF = Left ventricular ejection fraction; N/A = Not available; NPV = Negative predictive value; OR = Odds ratio; POCUS = Point-of-care ultrasound; POS = Prospective observational study; PPV = Positive predictive value; RCT = Randomized controlled trial; ROS = Retrospective observational study; RUSH = rapid ultrasound in shock; RV = Right ventricle; US = Ultrasound; SEARCH 8E’s = Sonographic evaluation of etiology of respiratory difficulty, chest pain and hypotension using “8 Es’”: empty thorax, edematous lung, extended focused assessment with sonography for trauma (E-FAST), effusion, equality (left to right ventricular ejection fraction ratio), exit (aorta), entrance (IVC) and endocardial movement [8]; vs. = Versus; yo = Years old.
Table 2.
Studies examining the utility of POCUS in identifying the source of sepsis, as well as guiding and managing septic patients *.
| 1st Author, Year, Country, Design, Setting | POCUS Protocol (If Any) | Aim | Patient Number/Age and Main Inclusion Criteria | Main Results |
|---|---|---|---|---|
| Cortellaro et al., 2017, Italy, POS, single-center ED [18] | Comparison of standard diagnostic work-up vs. early POCUS use regarding speed of diagnosis and accuracy in identification of the infectious source | 200/>18 yo |
|
|
| Devia Jaramillo et al., 2021, Colombia, POS cohort, single-center ED [19] | USER | US-based protocol for fluid administration and initiation of vasopressors in septic shock. | 83/>18 yo in septic shock |
|
| Haydar et al., 2012, USA, POS, single-center ED [20] | Protocol consisting of 3 main POCUS measures | Effect of 3 POCUS measures on clinical decision-making | 74/>18 yo |
|
| Musikatavorn et al., 2020, RCT, single-center ED [21] |
IVC assessment | Effect of UGFM strategy on 30-d mortality in patients with septic shock or sepsis-indued hypoperfusion vs. standard care. | 202/>18 yo |
|
| Lafon et al., 2020, France, POS, single-center ED [22] | FOCUS | FOCUS-based evaluation of early hemodynamic profile in patients presenting with ACF | 100/>18 yo presenting with ACF |
Sepsis cohort: 55 patients, Non-Sepsis: 45 patients. FOCUS was performed after administration of 500 mL of crystalloids Patients with sepsis had qSOFA score ≥ 2 points on ED admission and:
|
* All studies included non-traumatic septic patients. Abbreviations: ACF = Acute circulatory failure; CNS = Central nervous system; ED = Emergency department; FOCUS = Focused echocardiography; IVC = Inferior vena cava; LV = Left ventricle; MAP = Mean arterial pressure; POCUS = Point-of-care ultrasound; POS = Prospective observational study; qSOFA = quick Sequential organ failure assessment; SIRS = Systemic inflammatory response syndrome; US = Ultrasound; USER = Ultrasound for emergency room; VAS = Visual analog scale; vs. = Versus; yo = Years old.
Table 3.
Case reports depicting POCUS contribution to the diagnosis and management of septic patients.
| 1st Author, Year, Country | Patient’ s Symptoms/Clinical Status on ED Presentation | Management and POCUS Findings | Final Diagnosis |
|---|---|---|---|
| Alhabashy, 2018, Egypt [23] | 63 yo female with CAP |
|
AHFREF with severe aortic stenosis and mitral regurgitation |
| Alonso et al., 2017, UK [24] | 60-yo female, 3-day left leg pain, treated for suspected cellulitis |
|
Necrotizing fasciitis |
| Alonso et al., 2019, UK [25] | 70-yo female with diarrhea, vomiting for 1 week |
|
Obstructive stone causing moderate right-sided hydronephrosis |
| Cohen et al., 2020, USA [26] | 26-yo female, intravenous drug user, agitated |
|
Myocardial infarction caused by endocarditis-related septic embolization |
| Derr et al., 2012, USA [27] | 69-yo male, hematemesis |
|
Esophageal perforation |
| Gibbons et al., 2018, USA [28] | 40-yo female in severe sepsis, flank pain |
|
Xanthogranulomatous pyelonephritis |
| Hill et al., 2021, USA [29] | 5-yo male, 2 days febrile, cough, rhinorrhea, pruritus, decreased appetite |
|
Ruptured pulmonary hydatid cyst |
| Kinas et al., 2018, USA [30] | 34-yo male, after smoking crystal methamphetamine Symptoms: palpitations, dyspnea, cough with one episode of hemoptysis |
|
Methamphetamine-associated cardiomyopathy |
| Kotlarsky et al., 2016, Israel [31] | ROS included pediatric patients with septic arthritis of the hip joint |
|
Septic arthritis of the hip joint |
| Perez et al., 2021, USA [32] | 79-yo male, with a medical history of DM, hypertension, CAD, febrile, mild dyspnea, chills, myalgias, arthralgias for the past 2 days. |
|
Glenohumeral joint septic arthritis and subdeltoid septic bursitis |
| Romano et al., 2016, Canada [33] | 61-yo female with rheumatoid arthritis, Sjogren syndrome, presented with confusion, decreased LOC, 2 weeks of productive cough, fatigue, mild dyspnea in the last 24 h |
|
(Unsuspected) empyema in a patient being treated for CAP |
| Varela et al., 2019, Portugal [34] | 77-yo male suffering from acute dyspnea, 1 week of malaise, nausea, vomiting |
|
Liver abscess |
Abbreviations: AHFREF = Acute heart failure with reduced ejection fraction; CAD = Coronary artery disease; CAP = Community-acquired pneumonia; CXR = Chest x-ray; DM = Diabetes mellitus; ECG = Electrocardiogram; ECHO = Echocardiography; ED = Emergency department; IV = Intravenous; IVC = Inferior vena cava; LOC = Level of consciousness; LV = Left ventricle; LVEF = Left ventricular ejection fraction; MRSA = Methicillin-resistant Staphylococcus aureus; MSK = Musculoskeletal; POCUS = Point-of-care ultrasound; ROS = Retrospective observational study; RUSH = rapid ultrasound in shock; STEMI = ST-elevation myocardial infarction; US = Ultrasound; yo = Years old.
4. Discussion
Although sepsis represents one of the main causes of ED admission, its incidence remains underestimated because it constitutes an intermediate and not a primary cause of illness and death [2]. In the present review, the studies included in the first cluster demonstrate that the incidence of sepsis remains high, yet widely variable. Specifically, three [9,11,12] out of nine studies present the frequency of septic shock in the ED (3.6%, 12%, and 13.5%, respectively), while four [10,13,15,17] report the overall incidence of in-hospital sepsis (52%, 32%, 22.2%, and 55.5%, respectively). All these studies emphasize the importance of recognizing sepsis early in the clinical course, while consistently adopting a systematic evidence-based bundle of care and implementing it in a timely manner. Indeed, this approach is corroborated by recent sepsis guidelines [4].
Almost all studies from the first cluster conclude that the use of POCUS contributes to the early differential diagnosis, either of the cause of hypotension, or the cause of signs and symptoms that are suggestive of shock regardless of systolic blood pressure. This notion is even supported by Atkinson et al. [10], although their RCT failed to demonstrate any survival benefit conveyed by the use of POCUS in ED patients with shock and undifferentiated hypotension. In addition, in four out of nine studies, the addition of POCUS to standard ED care yielded a narrower and more accurate list of possible causes of nontraumatic undifferentiated hypotension, as evidenced by the reliability indices displaying agreement between the initial working diagnosis (based on combined clinical and POCUS evaluation) and the final diagnosis. Indeed, with regard to distributive shock, the combined clinical and POCUS diagnosis demonstrates high agreement with the final diagnosis (as measured by Kappa coefficient—k, ranging from 0.71 to 1.00), while it shows very good sensitivity (63.6–75%), as well as excellent specificity (99.7–100%), positive predictive value (87.5–100%), and negative predictive value (86.1–100%) [9,11,12,13] (Table 4). Two key points of these studies are worth mentioning. First, when implementing RUSH protocol, serial examinations are needed in cases of suspected septic shock [12]. Second, sepsis is a form of distributive shock that can be promptly diagnosed through identification of the sepsis source with the use of POCUS; multimodal POCUS can reveal multiple “foci of sepsis”, such as consolidation, air bronchogram, gallbladder wall thickening, limb cellulitis, hypoechoic pancreas, and vegetations [13]. Furthermore, Sasmaz et al. [15] and Volpicelli et al. [17] have reported perfect total agreement between the preliminary (ultrasonography-based) and final diagnosis (k = 0.82 and k = 0.838 respectively, p < 0.001 in both). In the latter study, ultrasonography-based diagnosis for distributive shock was accurate in 35 of 40 patients (87.5%). In conclusion, the contribution of POCUS to the early diagnosis of nontraumatic undifferentiated hypotension in ED patients is almost indisputable. Even in the sole study with contradictory results, which reports that POCUS use in the ED prior to a key intervention was associated with a higher mortality rate in critically ill patients [14], the authors admit potential sources of bias against POCUS. In fact, their registry does not include patients who were resuscitated in the ED. On top of that, the proportion of patients with diagnostic uncertainty, who were eventually identified as critically ill with the use of POCUS, is not taken into account.
Table 4.
Reliability indices (Sensitivity, Specificity, Positive and Negative Predictive Value) and Kappa coefficient showing degree of agreement between initial diagnosis (based on combined clinical and POCUS evaluation) and final diagnosis of distributive/septic shock.
| 1st Author (Year) | Shock Type | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Kappa | p |
|---|---|---|---|---|---|---|---|
| Ahn et al. (2017) [9] | Sepsis (distributive shock) | 63.6 | 99.7 | 87.5 | 98.7 | 0.729 | <0.001 |
| Bagheri-Hariri et al. (2015) [11] | Distributive | 75 | 100 | 100 | 95.5 | 0.83 | 0.002 |
| Hypovolemic Distributive | 100 | 100 | 100 | 100 | 1.00 | 0.003 | |
| Ghane et al. (2015) [12] | Distributive (RUSH Protocol) | 75 | 100 | 100 | 94.9 | 0.83 | 0.000 |
| Javali et al. (2020) [13] | Distributive (POCUS alone) | 15 | 100 | 100 | 71.5 | N/A | N/A |
| Distributive (combined clinical and POCUS evaluation) | 73.68 | 100 | 100 | 86.11 | 0.717 | <0.001 |
The second cluster of studies [18,19,20,21,22] acknowledge the contributing role of POCUS in determining the source and guiding the management of sepsis. Considering the complex nature of sepsis, the results are really promising. According to a study by Cortellaro et al., in 89% of the cases, POCUS enhanced emergency physicians’ (EP) ability to identify the cause of sepsis; moreover, POCUS-based diagnosis was achieved in an expedited manner (10min), with great accuracy (75%) and sensitivity (73%) [18]. Furthermore, the use of POCUS has been shown to be beneficial in terms of guiding fluid administration and achieving hemodynamic improvement in 97.4% of ED patients with septic shock [19]. In the study of Haydar et al., it was demonstrated that the use of POCUS facilitated clinical decision-making by increasing EPs’ certainty in 71% of the cases and by leading to the revision of overall treatment plans in 53% of the cases (change of the presumed cause in 17% and modification of the procedural intervention plans in 27%) [20]. However, a recent RCT assessed the effect of ultrasound-guided fluid management (UGFM) in patients with septic shock and showed no significant difference in 30-day mortality between patients receiving usual care and patients of the UGFM group, even though the latter group were administered less amount of resuscitation fluid [21]. Finally, the fourth study of this cluster [22] pointed out the high prevalence of sepsis in ED patients with acute circulatory failure (ACF) and verifies the preponderance of hypovolemia and vasoplegia in septic patients. This study showed that focused cardiac ultrasounds (FOCUS) could promptly identify left or right ventricular systolic failure in 31% of septic patients. Additionally, the study depicted that, even recently trained in ultrasounds, EPs were able to properly identify ACF mechanisms, achieving high agreement with the interpretation of ultrasound findings by ICU experts. Therefore, early FOCUS assessment can serve as a guide to fluid resuscitation in septic patients presenting to the ED with ACF.
Similar promising results have emerged from the third cluster of studies, which included case reports. POCUS was found to be a supportive tool for early and accurate diagnosis and overall management in complex septic cases. Three of the POCUS-based diagnoses involved the cardiovascular system (acute heart failure with reduced ejection fraction, severe aortic stenosis, and mitral regurgitation [23]; myocardial infarction caused by endocarditis-related septic embolization [26]; methamphetamine-associated cardiomyopathy [30]). In the latter case, POCUS set the diagnosis, dictated the appropriate restriction in the administration of intravenous fluids, and guided proper consultation. Two cases involved the respiratory system. Τhe first one was a ruptured pulmonary hydatid cyst, in which case POCUS directed EPs towards a timely and proper diagnosis, hence enabling appropriate management of the underlying septic and anaphylactic shock while prompting definitive surgical intervention [29]. The second one was an unexpected empyema revealed by POCUS in a patient being treated for community-acquired pneumonia [33]. Both of these cases confirm the utility of POCUS, not only in diagnosing pneumonia, but also in identifying associated complications, such as pleural effusions or empyema. Accordingly, POCUS is proposed as a valuable tool in the ED setting for patients with undifferentiated dyspnea and sepsis. Four cases dealt with various other clinical entities, namely esophageal perforation [27], obstructive uropathy causing moderate kidney hydronephrosis [25], xanthogranulomatous pyelonephritis [28], and liver abscess [34]. Regarding esophageal perforation, deterioration and death due to sepsis can occur within hours of presentation. Likewise, obstructive pyonephrosis has a mortality rate of 40% if not addressed in a timely manner, while pyogenic liver abscess is also accompanied by high mortality if not diagnosed promptly. In all previous four cases, POCUS imaging played a pivotal role in the accurate diagnosis of the sepsis cause. Finally, two case reports and a retrospective case series analysis involved the musculoskeletal system: necrotizing fasciitis of the left inner thigh, diagnosed via RUSH protocol [24]; glenohumeral joint septic arthritis and subdeltoid septic bursitis, in which case musculoskeletal POCUS was diagnostic through ultrasound-guided needle aspiration [32]; and septic arthritis of the hip diagnosed via POCUS and treated with aspiration in the ED in a series of 17 children [31].
All the aforementioned studies emphasize the utility of POCUS in the ED, highlighting its role as a time- and cost-effective, accurate, and non-invasive diagnostic imaging modality. With the focus on septic patients and their complex pathology, a systematic effort is warranted in order to develop integrated protocols [8,9], algorithms [25], and guidelines. The objective is to facilitate the rapid and holistic assessment οf patients in the ED, readily identify the source of sepsis or the cause of undifferentiated hypotension, and further guide the resuscitation process. A recent review summarizes the application of an integrated bedside ultrasound multiorgan approach in septic patients as an adjunctive tool to clinical examination and laboratory studies. Its use is not only supported for the diagnosis of septic shock and for the identification of the culprit infection, but also for the assessment of fluid responsiveness, resuscitation effectiveness, and guidance of diagnostic procedures and infectious source control [35].
This review depicts the limited number of studies regarding the use of POCUS in ED septic patients when compared with similar studies in the ICU setting, which is the main limitation of the study. These available studies have shown diversity in terms of cohort size and characteristics, POCUS parameters evaluated, and outcome elements that have been measured. However, even though POCUS is an established imaging modality in the ED for multiple time-sensitive, critical diseases such as trauma or cardiac arrest and it is already incorporated in universal guidelines, it seems that there is a delay in the integration of POCUS in international sepsis guidelines.
5. Conclusions
The results of the present review support the well-documented utility of POCUS and highlight the importance of POCUS incorporation in the comprehensive management of the septic patient in the ED setting. At the same time, literature remains limited in terms of large scale, multi-center studies focused only in septic patients presented to the ED. Further development of research studies, alongside with integration of POCUS use in sepsis guidelines, will strengthen and extend its use in everyday clinical practice.
Author Contributions
E.P. conceived, designed and coordinated the study; D.M., S.B. and C.V. contributed to the data acquisition, analysis and interpretation; C.V. drafted the manuscript and contributed to the final layout of the tables and figure; E.P. and I.V. provided fundamental guidance; J.P. and I.V. performed editing and critical revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
Verras, Ventoulis, Bezati, Matsiras and Polyzogopoulou have no conflicts of interest or financial ties to disclose. Parissis received honoraria for lectures from Orion pharma, Pfizer, Servier, Astra, AO Orphan and Roche Diagnostics.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cecconi M., Evans L., Levy M., Rhodes A. Sepsis and Septic Shock. Lancet. 2018;392:75–87. doi: 10.1016/S0140-6736(18)30696-2. [DOI] [PubMed] [Google Scholar]
- 2.Rudd K.E., Johnson S.C., Agesa K.M., Shackelford K.A., Tsoi D., Kievlan D.R., Colombara D.V., Ikuta K.S., Kissoon N., Finfer S., et al. Global, Regional, and National Sepsis Incidence and Mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–211. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macdonald S.P., Williams J.M., Shetty A., Bellomo R., Finfer S., Shapiro N., Keijzers G. Review Article: Sepsis in the Emergency Department—Part 1: Definitions and Outcomes. Emerg. Med. Australas. 2017;29:619–625. doi: 10.1111/1742-6723.12886. [DOI] [PubMed] [Google Scholar]
- 4.Evans L., Rhodes A., Alhazzani W., Antonelli M., Coopersmith C.M., French C., Machado F.R., Mcintyre L., Ostermann M., Prescott H.C., et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Intensive Care Med. 2021;47:1181–1247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitson M.R., Mayo P.H. Ultrasonography in the Emergency Department. Crit Care. 2016;20:227. doi: 10.1186/s13054-016-1399-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rice J.A., Brewer J., Speaks T., Choi C., Lahsaei P., Romito B.T. The POCUS Consult: How Point of Care Ultrasound Helps Guide Medical Decision Making. Int. J. Gen. Med. 2021;14:9789–9806. doi: 10.2147/IJGM.S339476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ultrasound Guidelines: Emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Ann. Emerg. Med. 2017;69:e27–e54. doi: 10.1016/j.annemergmed.2016.08.457. [DOI] [PubMed] [Google Scholar]
- 8.Perera P., Mailhot T., Riley D., Mandavia D. The RUSH Exam: Rapid Ultrasound in SHock in the Evaluation of the Critically Lll. Emerg. Med. Clin. N. Am. 2010;28:29–56. doi: 10.1016/j.emc.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Ahn J.H., Jeon J., Toh H.-C., Noble V.E., Kim J.S., Kim Y.S., Do H.H., Ha Y.R. SEARCH 8Es: A Novel Point of Care Ultrasound Protocol for Patients with Chest Pain, Dyspnea or Symptomatic Hypotension in the Emergency Department. PLoS ONE. 2017;12:e0174581. doi: 10.1371/journal.pone.0174581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atkinson P.R., Milne J., Diegelmann L., Lamprecht H., Stander M., Lussier D., Pham C., Henneberry R., Fraser J.M., Howlett M.K., et al. Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients With Undifferentiated Hypotension? An International Randomized Controlled Trial From the SHoC-ED Investigators. Ann. Emerg. Med. 2018;72:478–489. doi: 10.1016/j.annemergmed.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Bagheri-Hariri S., Yekesadat M., Farahmand S., Arbab M., Sedaghat M., Shahlafar N., Takzare A., Seyedhossieni-Davarani S., Nejati A. The Impact of Using RUSH Protocol for Diagnosing the Type of Unknown Shock in the Emergency Department. Emerg. Radiol. 2015;22:517–520. doi: 10.1007/s10140-015-1311-z. [DOI] [PubMed] [Google Scholar]
- 12.Ghane M.R., Gharib M., Ebrahimi A., Saeedi M., Akbari-Kamrani M., Rezaee M., Rasouli H. Accuracy of Early Rapid Ultrasound in Shock (RUSH) Examination Performed by Emergency Physician for Diagnosis of Shock Etiology in Critically Ill Patients. J. Emergencies Trauma Shock. 2015;8:5–10. doi: 10.4103/0974-2700.145406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Javali R.H., Loganathan A., Srinivasarangan M., Patil A., Siddappa G.B., Satyanarayana N., Bheemanna A.S., Jagadeesh S., Betkerur S. Reliability of Emergency Department Diagnosis in Identifying the Etiology of Nontraumatic Undifferentiated Hypotension. Indian J. Crit. Care Med. 2020;24:313–320. doi: 10.5005/jp-journals-10071-23429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mosier J.M., Stolz U., Milligan R., Roy-Chaudhury A., Lutrick K., Hypes C.D., Billheimer D., Cairns C.B. Impact of Point-of-Care Ultrasound in the Emergency Department on Care Processes and Outcomes in Critically Ill Nontraumatic Patients. Crit. Care Explor. 2019;1:e0019. doi: 10.1097/CCE.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sasmaz M.I., Gungor F., Guven R., Akyol K.C., Kozaci N., Kesapli M. Effect of Focused Bedside Ultrasonography in Hypotensive Patients on the Clinical Decision of Emergency Physicians. Emerg. Med. Int. 2017;2017:6248687. doi: 10.1155/2017/6248687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shokoohi H., Boniface K.S., Pourmand A., Liu Y.T., Davison D.L., Hawkins K.D., Buhumaid R.E., Salimian M., Yadav K. Bedside Ultrasound Reduces Diagnostic Uncertainty and Guides Resuscitation in Patients With Undifferentiated Hypotension. Crit. Care Med. 2015;43:2562–2569. doi: 10.1097/CCM.0000000000001285. [DOI] [PubMed] [Google Scholar]
- 17.Volpicelli G., Lamorte A., Tullio M., Cardinale L., Giraudo M., Stefanone V., Boero E., Nazerian P., Pozzi R., Frascisco M.F. Point-of-Care Multiorgan Ultrasonography for the Evaluation of Undifferentiated Hypotension in the Emergency Department. Intensive Care Med. 2013;39:1290–1298. doi: 10.1007/s00134-013-2919-7. [DOI] [PubMed] [Google Scholar]
- 18.Cortellaro F., Ferrari L., Molteni F., Aseni P., Velati M., Guarnieri L., Cazzola K.B., Colombo S., Coen D. Accuracy of Point of Care Ultrasound to Identify the Source of Infection in Septic Patients: A Prospective Study. Intern. Emerg. Med. 2017;12:371–378. doi: 10.1007/s11739-016-1470-2. [DOI] [PubMed] [Google Scholar]
- 19.Devia Jaramillo G., Menendez Ramirez S. USER Protocol as a Guide to Resuscitation of the Patient with Septic Shock in the Emergency Department. Open Access Emerg. Med. 2021;13:33–43. doi: 10.2147/OAEM.S289148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haydar S.A., Moore E.T., Higgins G.L., Irish C.B., Owens W.B., Strout T.D. Effect of Bedside Ultrasonography on the Certainty of Physician Clinical Decisionmaking for Septic Patients in the Emergency Department. Ann. Emerg. Med. 2012;60:346–358.e4. doi: 10.1016/j.annemergmed.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Musikatavorn K., Plitawanon P., Lumlertgul S., Narajeenron K., Rojanasarntikul D., Tarapan T., Saoraya J. Randomized Controlled Trial of Ultrasound-Guided Fluid Resuscitation of Sepsis-Induced Hypoperfusion and Septic Shock. West J. Emerg. Med. 2021;22:369–378. doi: 10.5811/westjem.2020.11.48571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lafon T., Appert A., Hadj M., Bigrat V., Legarcon V., Claveries P., Goudelin M., Evrard B., Padilla A.C.H., Baisse A., et al. Comparative Early Hemodynamic Profiles in Patients Presenting to the Emergency Department with Septic and Nonseptic Acute Circulatory Failure Using Focused Echocardiography. Shock. 2020;53:695–700. doi: 10.1097/SHK.0000000000001449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alhabashy W.S. Echocardiography guided septic shock management; Proceedings of the Seventh International Conference and Exhibition on Surgery and the Third International Conference on Anesthesia; Dublin, Ireland. 21–23 June 2018; Brussels, Belgium: International Online Medical Council (IOMC); 2018. p. 70. [Google Scholar]
- 24.Valle Alonso J., Lakshmanan G., Saleem Y. Use of POCUS Ultrasound in Sepsis, Bedside Diagnosis of Necrotizing Fasciitis. QJM. 2017;110:687–688. doi: 10.1093/qjmed/hcx137. [DOI] [PubMed] [Google Scholar]
- 25.Alonso J.V., Turpie J., Farhad I., Ruffino G. Protocols for Point-of-Care-Ultrasound (POCUS) in a Patient with Sepsis; An Algorithmic Approach. Bull. Emerg. Trauma. 2019;7:67–71. doi: 10.29252/beat-070110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen S., Ford L., Situ-LaCasse E., Tolby N. Infective Endocarditis Causing Acute Myocardial Infarction. Cureus. 2020;12:e11245. doi: 10.7759/cureus.11245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derr C., Drake J.M. Esophageal Rupture Diagnosed with Bedside Ultrasound. Am. J. Emerg. Med. 2012;30:e1–e3. doi: 10.1016/j.ajem.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 28.Gibbons R., Leonard N., Magee M., Zanaboni A., Patterson J., Costantino T. Xanthogranulomatous Pyelonephritis: A Complicated Febrile Urinary Tract Infection Detected by Point-of-Care Ultrasound in the Emergency Department. J. Emerg. Med. 2018;55:e1–e4. doi: 10.1016/j.jemermed.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 29.Hill A., Guillén M., Martin D., Dreyfuss A. Point-of-Care Ultrasound Diagnosis of Pulmonary Hydatid Cyst Disease Causing Shock: A Case Report. Clin. Pract. Cases Emerg. Med. 2021;5:403–406. doi: 10.5811/cpcem.2021.5.52264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kinas D., Dalley M., Guidry K., Newberry M.A., Farcy D.A. Point-of-Care Ultrasound Identifies Decompensated Heart Failure in a Young Male with Methamphetamine-Associated Cardiomyopathy Presenting in Severe Sepsis to the Emergency Department. Case Rep. Emerg. Med. 2018;2018:2859676. doi: 10.1155/2018/2859676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kotlarsky P., Shavit I., Kassis I., Eidelman M. Treatment of Septic Hip in a Pediatric ED: A Retrospective Case Series Analysis. Am. J. Emerg. Med. 2016;34:602–605. doi: 10.1016/j.ajem.2015.12.090. [DOI] [PubMed] [Google Scholar]
- 32.Perez J., Sorensen S., Rosselli M. Utilisation of Musculoskeletal Ultrasonography for the Evaluation of Septic Arthritis in a Patient Presenting to the Emergency Department with Fever during the Era of COVID-19. BMJ Case Rep. 2021;14:e242370. doi: 10.1136/bcr-2021-242370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romano M., Jelic T., Chenkin J. Simple Pneumonia or Something More?: A Case Report and Discussion of Unexpected Empyema Identified by Point-of-Care Ultrasound. CJEM. 2016;18:391–394. doi: 10.1017/cem.2015.71. [DOI] [PubMed] [Google Scholar]
- 34.Varela M.L., Fernandes R.M., Melão M.L., Moreno J., Granja C. Shedding Light on a Hidden Source of Septic Shock with POCUS. POCUS. 2019;4:15–16. doi: 10.24908/pocus.v4i2.13689. [DOI] [Google Scholar]
- 35.Sweeney D.A., Wiley B.M. Integrated Multiorgan Bedside Ultrasound for the Diagnosis and Management of Sepsis and Septic Shock. Semin. Respir. Crit. Care Med. 2021;42:641–649. doi: 10.1055/s-0041-1733896. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.