Abstract
Background
To increase people’s access to rehabilitation services, particularly in the context of the COVID‐19 pandemic, we need to explore how the delivery of these services can be adapted. This includes the use of home‐based rehabilitation and telerehabilitation. Home‐based rehabilitation services may become frequently used options in the recovery process of patients, not only as a solution to accessibility barriers, but as a complement to the usual in‐person inpatient rehabilitation provision. Telerehabilitation is also becoming more viable as the usability and availability of communication technologies improve.
Objectives
To identify factors that influence the organisation and delivery of in‐person home‐based rehabilitation and home‐based telerehabilitation for people needing rehabilitation.
Search methods
We searched PubMed, Global Health, the VHL Regional Portal, Epistemonikos, Health Systems Evidence, and EBM Reviews as well as preprints, regional repositories, and rehabilitation organisations websites for eligible studies, from database inception to search date in June 2022.
Selection criteria
We included studies that used qualitative methods for data collection and analysis; and that explored patients, caregivers, healthcare providers and other stakeholders’ experiences, perceptions and behaviours about the provision of in‐person home‐based rehabilitation and home‐based telerehabilitation services responding to patients’ needs in different phases of their health conditions.
Data collection and analysis
We used a purposive sampling approach and applied maximum variation sampling in a four‐step sampling frame. We conducted a framework thematic analysis using the CFIR (Consolidated Framework for Implementation Research) framework as our starting point. We assessed our confidence in the findings using the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach.
Main results
We included 223 studies in the review and sampled 53 of these for our analysis. Forty‐five studies were conducted in high‐income countries, and eight in low‐and middle‐income countries. Twenty studies addressed in‐person home‐based rehabilitation, 28 studies addressed home‐based telerehabilitation services, and five studies addressed both modes of delivery. The studies mainly explored the perspectives of healthcare providers, patients with a range of different health conditions, and their informal caregivers and family members.
Based on our GRADE‐CERQual assessments, we had high confidence in eight of the findings, and moderate confidence in five, indicating that it is highly likely or likely respectively that these findings are a reasonable representation of the phenomenon of interest. There were two findings with low confidence.
High and moderate confidence findings
Home‐based rehabilitation services delivered in‐person or through telerehabilitation
Patients experience home‐based services as convenient and less disruptive of their everyday activities. Patients and providers also suggest that these services can encourage patients' self‐management and can make them feel empowered about the rehabilitation process. But patients, family members, and providers describe privacy and confidentiality issues when services are provided at home. These include the increased privacy of being able to exercise at home but also the loss of privacy when one’s home life is visible to others.
Patients and providers also describe other factors that can affect the success of home‐based rehabilitation services. These include support from providers and family members, good communication with providers, the requirements made of patients and their surroundings, and the transition from hospital to home‐based services.
Telerehabilitation specifically
Patients, family members and providers see telerehabilitation as an opportunity to make services more available. But providers point to practical problems when assessing whether patients are performing their exercises correctly. Providers and patients also describe interruptions from family members.
In addition, providers complain of a lack of equipment, infrastructure and maintenance and patients refer to usability issues and frustration with digital technology. Providers have different opinions about whether telerehabilitation is cost‐efficient for them. But many patients see telerehabilitation as affordable and cost‐saving if the equipment and infrastructure have been provided.
Patients and providers suggest that telerehabilitation can change the nature of their relationship. For instance, some patients describe how telerehabilitation leads to easier and more relaxed communication. Other patients describe feeling abandoned when receiving telerehabilitation services.
Patients, family members and providers call for easy‐to‐use technologies and more training and support. They also suggest that at least some in‐person sessions with the provider are necessary. They feel that telerehabilitation services alone can make it difficult to make meaningful connections. They also explain that some services need the provider’s hands. Providers highlight the importance of personalising the services to each person’s needs and circumstances.
Authors' conclusions
This synthesis identified several factors that can influence the successful implementation of in‐person home‐based rehabilitation and telerehabilitation services. These included factors that facilitate implementation, but also factors that can challenge this process. Healthcare providers, program planners and policymakers might benefit from considering these factors when designing and implementing programmes.
Keywords: Humans, Caregivers, COVID-19, Family, Health Personnel, Pandemics
Plain language summary
Factors that influence the provision of home‐ based rehabilitation services for people needing rehabilitation: a qualitative evidence synthesis
The aim of this Cochrane qualitative evidence synthesis was to explore factors that influence rehabilitation services that are delivered in people’s own homes. The synthesis looked at services that were delivered in person as well as services that were delivered through telerehabilitation. To answer this question, we analysed 53 qualitative studies.
Key messages
Home‐based rehabilitation, delivered in‐person or through telerehabilitation, can be experienced as more accessible and more convenient than facility‐based services. Patients, providers and family members also describe how home‐based services can change the nature of their relationships and can have practical and resource implications that can be both positive and negative.
What was studied in this synthesis?
The COVID‐19 pandemic has led to a stronger focus on home‐based healthcare. This includes the delivery of home‐based rehabilitation services delivered in person or using telerehabilitation. Home‐based rehabilitation services may become a common option in the recovery process of patients, either instead of facility‐based services or as a complement to these services. Telerehabilitation is also becoming more common as people’s access to digital technologies increases.
What are the main findings of this synthesis?
We analysed 53 qualitative studies where patients received rehabilitation services in their own homes. In some of the studies, healthcare providers delivered the services in person. In the other studies, providers delivered the services through telerehabilitation using digital technologies. The studies explored the views and experiences of patients, families and healthcare providers. Most of the studies were from high‐income countries.
Our findings highlight several factors that can influence the organisation and delivery of home‐based rehabilitation. We have moderate to high confidence in the following findings.
Home‐based rehabilitation services delivered in‐person or through telerehabilitation
Patients experience home‐based services as convenient and less disruptive of their everyday activities. Patients and providers also suggest that these services can encourage patients' self‐management and can make them feel empowered about the rehabilitation process. But patients, family members, and providers describe privacy and confidentiality issues when services are provided at home. These include the increased privacy of being able to exercise at home but also the loss of privacy when one’s home life is visible to others.
Patients and providers also describe other factors that can affect the success of home‐based rehabilitation services. These include support from providers and family members, good communication with providers, the requirements made of patients and their surroundings, and the transition from hospital to home‐based services.
Telerehabilitation specifically
Patients, family members and providers see telerehabilitation as an opportunity to make services more available. But providers point to practical problems when assessing whether patients are performing their exercises correctly. Providers and patients also describe interruptions from family members.
In addition, providers complain of a lack of equipment, infrastructure and maintenance and patients refer to usability issues and frustration with digital technology. Providers have different opinions about whether telerehabilitation is cost‐efficient for them. But many patients see telerehabilitation as affordable and cost‐saving if the equipment and infrastructure has been provided.
Patients and providers suggest that telerehabilitation can change the nature of their relationship. For instance, some patients describe how telerehabilitation leads to easier and more relaxed communication. Other patients describe feeling abandoned when receiving telerehabilitation services.
Patients, family members and providers call for easy‐to‐use technologies and more training and support. They also suggest that at least some in‐person sessions with the provider are necessary. They feel that telerehabilitation services alone can make it difficult to make meaningful connections. They also explain that some services need the provider’s hands. Providers highlight the importance of personalising the services to each person’s needs and circumstances.
How up to date is this synthesis?
We searched for studies that had been published up to 16 June 2022.
Summary of findings
Summary of findings 1. Summary of qualitative findings.
| Summary of review finding | Studies contributing to the review finding | GRADE‐CERQual assessment of confidence in the evidence | Explanation of GRADE‐CERQual assessment |
| Perceptions about rehabilitation services delivered at patients´ homes through in‐person encounters or via telerehabilitation | |||
| Finding 1. Patients and caregivers receiving and healthcare providers delivering telerehabilitation services perceived at least some in‐person home encounters as necessary. They felt that telerehabilitation services alone lost the rapport of social interaction and the opportunity to make meaningful connections. They also pointed out that some types of services provided with the hands could not be delivered using telerehabilitation (moderate confidence finding). | Brouns 2018; Damhus 2018; Dennett 2020; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; O'Shea 2020; Ownsworth 2020; Palazzo 2016; Pekmezaris 2020; Saywell 2015; Shulver 2016; Van der Meer 2020 | Moderate confidence | Downgraded because we had minor concerns regarding methodological limitations and relevance; no/very minor concerns regarding coherence and adequacy |
| Finding 2. Patients and healthcare providers described how in‐person home‐based rehabilitation and telerehabilitation encouraged patients' self‐management and made them feel empowered about the rehabilitation process. Patients become active contributors and shaped the process and its pace according to their needs. This was seen to facilitate the achievement of final results, whatever the goal that rehabilitation aimed to achieve (high confidence finding). | Argent 2018; Bodker 2015; Dennett 2020; Dinesen 2019; Dubouloz 2004; Edbrooke 2020; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hoaas 2016; Mohd Nordin 2014; Ng 2013; Nordin 2017; O'Shea 2020; Ownsworth 2020; Pekmezaris 2020; Pinto 2014; Ranaldi 2018; Randström 2012; Shulver 2016; Sureshkumar 2016; Tsai 2016; Turner 2011; Van der Meer 2020. | High confidence | We had minor concerns regarding methodological limitations, and no/very minor concerns regarding coherence, adequacy, and relevance |
| Finding 3. Patients and healthcare providers appreciated how in‐person home‐based rehabilitation or telerehabilitation improved patient outcomes related to independence, overall functioning at home, and everyday use of assistive devices, which are facilitated by the interaction with the home environment implicit in these types of services (low confidence finding). | Bodker 2015; Borade 2019; Dennett 2020; Dubouloz 2004; Govender 2019; O'Shea 2020; Pinto 2014; Randstrom 2013 | Low confidence | Downgraded because we had no/very minor concerns regarding methodological limitations, serious concerns regarding coherence, and moderate concerns regarding adequacy and relevance |
| Finding 4. Patients, caregivers and healthcare providers regarded the transition from the hospital to home as a challenging process given the lack of human and infrastructure resources available in the home setting. This may have an impact on the implementation of in‐person home‐based rehabilitation. | Govender 2019; HeydariKhayat 2020; Mohd Nordin 2014; Turner 2011; VanderVeen 2019 | Moderate confidence | Downgraded because we had moderate concerns regarding methodological limitations, minor concerns regarding coherence, and relevance, and no/very minor concerns regarding adequacy |
| Finding 5. Patients and healthcare providers described several factors that might affect patients’ motivation and engagement with telerehabilitation services, including support from healthcare providers or family members and other caregivers during sessions, good communication with the healthcare provider, what the exercise required from the patient and their surroundings, and the presence of comorbidities. | Bodker 2015; Brouns 2018; Dennett 2020; Dinesen 2019; Edbrooke 2020; Folan 2015; Hoaas 2016; Lawson 2020; O'Doherty 2013; O'Shea 2020; Palazzo 2016; Ranaldi 2018; Randström 2014; Saywell 2015; Stark 2019; Stuifbergen 2011; Teriö 2019; Van der Meer 2020; Vik 2009 | Moderate confidence | Downgraded because we had no/very minor concerns regarding methodological limitations and adequacy, moderate concerns regarding coherence, and minor concerns regarding relevance |
| Finding 6. Patients, caregivers, and providers described a number of privacy and confidentiality issues when services were provided at home. These included the increased privacy of being able to exercise at home but also the loss of privacy when elements of one’s home life were visible to others. | Bodker 2015; Brouns 2018; Dennett 2020; Gélinas‐Bronsard 2019; Hoaas 2016; Lawson 2020; Ng 2013; Ownsworth 2020; Oyesanya 2019; Palazzo 2016; Pekmezaris 2020; Randström 2012; Randstrom 2013; Randström 2014;Rietdijk 2020 | High confidence | We had no/very minor concerns regarding methodological limitations and coherence, and minor concerns regarding adequacy and relevance |
| Finding 7. Patients regarded in‐person home‐based rehabilitation and telerehabilitation services as convenient and less disruptive of everyday activities. | Govender 2019; Hale Gallardo 2020; HeydariKhayat 2020; Lawson 2020; Ownsworth 2020; Palmcrantz 2017; Pekmezaris 2020; Pinto 2014; Randström 2012; Randstrom 2013; Shulver 2017; Silveira 2019; Stark 2019; Tsai 2016; Tyagi 2018; Van der Meer 2020 | High confidence | We had no/very minor concerns regarding methodological limitations, coherence, adequacy,and relevance |
| Finding 8. Patients, caregivers, and healthcare providers called for more training in the context of in‐person home‐based rehabilitation. | Govender 2019; O'Doherty 2013; Randström 2014; Schopfer 2020; Umb Carlsson 2019; VanderVeen 2019 | Low confidence | Downgraded because we had no/very minor concerns regarding methodological limitations, minor concerns regarding coherence, serious concerns regarding adequacy, and moderate concerns regarding relevance |
| Perceptions about rehabilitation services delivered at home through telerehabilitation | |||
| Finding 9. Healthcare providers highlighted the importance of personalising the service to each patient’s needs and resources at home. | Bodker 2015; Damhus 2018; Dennett 2020; Edbrooke 2020; Lawson 2020; Ownsworth 2020; Shulver 2017; Silveira 2019; Tsai 2016 | High confidence | We had no/very minor concerns regarding methodological limitations, coherence and adequacy, and minor concerns regarding relevance |
| Finding 10. Patients, caregivers, healthcare providers and other stakeholders described how telerehabilitation changed the nature of the patient‐provider relationship. This included overcoming physical barriers to communication and enabling quick responses to questions, creating a more relaxed environment for communication, and supporting shared decision making. Some patients described how telerehabilitation services allowed them to keep connected with their healthcare provider after being discharged from the hospital. However, other patients felt abandoned when receiving telerehabilitation services. | Argent 2018; Bodker 2015; Brouns 2018; Dennett 2020; Dinesen 2019; Emmerson 2018; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Kamwesiga 2017; Lawson 2020; Malmberg 2018; Nordin 2017; Ownsworth 2020; Palazzo 2016; Palmcrantz 2017; Shulver 2017; Stuifbergen 2011; Tsai 2016; Van der Meer 2020 | High confidence | We had minor concerns regarding methodological limitations and relevance, and no/very minor concerns regarding coherence and adequacy |
| Finding 11. Healthcare providers and patients described some aspects of telerehabilitation services at home as challenging. Healthcare providers described problems in assessing patients, their environment, and whether they were performing exercises correctly. Providers and patients also emphasised the need for a quiet place during telerehabilitation sessions and described challenges tied to interruptions from family members. | Argent 2018; Bodker 2015; Damhus 2018; Lawson 2020; Mendell 2019; Ownsworth 2020; Palazzo 2016; Rietdijk 2020; Shulver 2017; Silveira 2019; Sureshkumar 2016; Tsai 2016; Tyagi 2018 | High confidence | We had no/very minor concerns regarding methodological limitations, coherence and adequacy, and minor concerns regarding relevance |
| Finding 12. Patients, caregivers, healthcare providers and other stakeholders regarded telerehabilitation as an opportunity to make rehabilitation services more accessible. | Argent 2018; Brouns 2018; Damhus 2018; Dennett 2020; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; Malmberg 2018; O'Shea 2020; Ownsworth 2020; Oyesanya 2019; Palmcrantz 2017; Rietdijk 2020; Saywell 2015; Shulver 2017; Tyagi 2018; Van der Meer 2020 | High confidence | We had no/very minor concerns regarding methodological limitations, coherence, adequacy and relevance |
| Finding 13. Healthcare providers and policymakers highlighted the need for adequate equipment, infrastructure and maintenance both on the provider side and the patient side but described how these needs were not always met. They described challenges including a lack of resources and investment, a lack of awareness around the resources needed, and rapid advances in technology that make technology rapidly obsolete. | Bodker 2015; Brouns 2018; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Lawson 2020; Mendell 2019; Ownsworth 2020; Oyesanya 2019; Palmcrantz 2017; Shulver 2016; Teriö 2019; Tyagi 2018; Van der Meer 2020 | Moderate confidence | Downgraded because we had no/very minor concerns regarding methodological limitations, coherence, and adequacy, and moderate concerns regarding relevance |
| Finding 14. Patients and caregivers described many usability issues related to the device, the program or the application; they also emphasised the need for easy‐to‐use technologies that could be adapted to the patient’s individual needs. Patients and caregivers reported a lack of familiarity with, fear of or frustration with digital technology. Patients, caregivers, and healthcare providers called for more training and support in the use of these technologies. | Argent 2018; Bodker 2015; Brouns 2018; Damhus 2018; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; Malmberg 2018; Mendell 2019; O'Shea 2020; Ownsworth 2020; Palazzo 2016; Palmcrantz 2017; Rietdijk 2020; Shulver 2016; Shulver 2017; Silveira 2019; Stuifbergen 2011; Sureshkumar 2016; Teriö 2019; Tsai 2016; Tyagi 2018; Van der Meer 2020 | Moderate confidence | Downgraded because we had minor concerns regarding methodological limitations and coherence, no/very minor concerns regarding adequacy, and moderate concerns regarding relevance |
| Finding 15. Healthcare providers differed in their views about whether telerehabilitation was cost‐efficient for them, but many patients encountered it as affordable and cost‐saving when the equipment and infrastructure have been provided. | Bodker 2015; Brouns 2018; Damhus 2018; Gélinas‐Bronsard 2019; Lawson 2020; Ownsworth 2020; Van der Meer 2020 | High confidence | We had no/very minor concerns regarding methodological limitations, coherence and adequacy, and moderate concerns regarding relevance |
Background
Description of the topic
It is estimated that 15% of the world’s population live with disabilities, and that 2,4 billion people are in need of rehabilitation services (World Health Organization 2011; Negrini 2020a; Cieza 2021). Demographic changes, such as population growth, ageing, increased complexity and chronicity in diseases, and medical advances that preserve life (Gimigliano 2017), indicate that these figures will increase.
These global trends suggest that key indicators of a population’s health will not only be mortality and morbidity, but also functioning (Gimigliano 2017; Negrini 2020b). Healthcare services need to respond to the increased need for long‐term management of disabilities and chronic conditions by strengthening rehabilitation services (Skempes 2021).
Rehabilitation services target mobility, vision, hearing, and cognition, and contribute to optimizing function ability and well‐being across the continuum of acute, subacute, and long‐term care (Van Egmond 2018; EP and RMBA 2018; Gimigliano 2017; Meyer 2014). However, people do not always access the rehabilitation services they need.
According to the International Classification of Functioning, Disability and Health (ICF) (World Health Organization 2001), contextual factors, including the physical, social and attitudinal environment in which people live and conduct their lives, can act as facilitators or barriers for receiving rehabilitation services (Mlenzana 2013; Gutenbrunner 2020b). This includes factors tied to the rehabilitation services themselves, such as users' access to healthcare providers and to information about services, providers’ skills and other attributes, and people’s confidence in these providers; as well as broader factors related to society's lack of awareness about disability and lack of economic resources.
During the 2020 COVID‐19 pandemic, people attempting to access rehabilitation services were facing additional challenges. Rehabilitation has in the present resource scarcity been perceived as ‘non‐essential’, and many have been cancelled or limited, for instance by limiting care to outpatient settings (Negrini 2020b). The lack of services obviously affects the well‐being and quality of life of people living with disabilities and imposes more burdens on a population that is already vulnerable. Some medical conditions can be aggravated by the lack of access to rehabilitation services. Critical situations have been reported for people with acute health conditions (e.g. stroke in adults), other conditions needing specialized inpatient rehabilitation services (e.g. spinal cord injuries, rare diseases, and musculoskeletal conditions) and long‐term assessment (Boldrini 2020; Dorjbal 2019).
To increase people’s access to rehabilitation services, there is a need to explore how the delivery of these services can be adapted, including through the use of home‐based rehabilitation and telerehabilitation (Brennan 2009). These strategies could help avoid the prolonged interruption of services when other modes of service delivery are limited or not possible, for example, due to natural disasters, geographic isolation or pandemics. Home‐based rehabilitation services may become the most frequently used option in the recovery process of patients, not only as an alternative to access barriers, but as a complement to the usual rehabilitation provision.
How the intervention might work
In‐person home‐based rehabilitation refers to the delivery of rehabilitation services with in‐person encounters provided where the patient lives, for instance at home or in nursing homes or long‐term care (Chi 2020). It is often a component of a broader community‐based rehabilitation process (Cobbing 2016), and one of the supportive tools that allow the continuation of care in a familiar living environment.
In‐person home‐based rehabilitation shares the same goals as other types of rehabilitation. It aims to let people resume their activities, improve their quality of life, reduce the burden of caregivers, and prevent complications and secondary conditions (Hotta 2015). Home‐based rehabilitation aims to provide the benefits of effective treatment to people with no access to in‐patient or facility‐based care, or might complement such care (Stolee 2012). In addition, home‐based rehabilitation focuses on improving people's participation in their own care and their ability to evaluate themselves and set goals for their recovery in the context of their own home. It can involve learning strategies for self‐management related to daily activities at home and in the community; receiving exercise training; exploring community services and facilities; dialogue with professionals; and participation in activities aimed at returning to work (Steihaug 2016).
The types of services that in‐person home‐based rehabilitation provides vary according to the person’s needs. These services can include, for instance, assessment of the home and the environment with modification of architectural barriers that may exist as well as the provision of assistive devices; home nursing and education for the person and their caregiver on topics such as hygiene, bladder and bowel management and skin care; social and psychological support for the emotional demands of the person and their family; primary care by general practitioners and therapists with services necessary for the maintenance of health, well‐being and the prevention of complications, as well as transition therapies towards more complex rehabilitation interventions (Rezaei 2019).
Two Cochrane Reviews have found that in‐person home‐based rehabilitation may be as effective as institutional‐based rehabilitation (Anderson 2017; Coupar 2012), while another, for breast cancer survivors, found that in‐person home‐based rehabilitation may be better than usual care for quality of life and may lead to a reduction in fatigue and anxiety, at least in the short term (Cheng 2017). Additionally, another Cochrane Review found that hospitalization at home for people recovering from stroke may lower the risk of living in an institutional setting at six months and may slightly improve patient satisfaction when compared to in‐hospital care (Gonçalves‐Bradley 2017).
Additional benefits of in‐person home‐based rehabilitation that have been reported include keeping people in a familiar environment; expanding access for people who would not otherwise receive care; aligning the rehabilitation process with each patient’s daily activities at their homes (Cobbing 2016; Housley 2016; Steihaug 2016); and reducing the burden and costs of travel, at least for the patient. However, some barriers to implementation have also been described, such as difficulties in patient adherence and requirements in logistics and human resources (Gelaw 2020; Kuo 2019; Widén 1998).
Telerehabilitation has been defined as the delivery of rehabilitation services where the patient lives via information and communication technologies (Brennan 2009). Telerehabilitation can provide many of the same services described for home‐based rehabilitation, thus providing assistance to homebound patients without the physical presence of a therapist or other healthcare provider (Agostini 2015).
Cochrane Reviews assessing the effectiveness of telerehabilitation for a range of conditions show mixed results. Telerehabilitation may be better than traditional in‐person services or standard care for a number of outcomes among people with multiple sclerosis (Khan 2015). For stroke patients, on the other hand, there may be no significant differences between telerehabilitation and standard delivery of rehabilitation (Laver 2020), while for people with chronic low‐back pain, the effects are largely uncertain due to very low‐certainty evidence (Saragiotto 2016).
Home‐based telerehabilitation shares some of the same potential advantages as in‐person home‐based rehabilitation. Both modes of service delivery allow people to stay in a familiar environment and can help align the rehabilitation process with people’s daily activities at home. In addition, home‐based telerehabilitation not only reduces the burden and costs of travel for the patient, but also for the healthcare provider (Kairy 2009; Peretti 2017). It can improve accessibility in remote places, where traditional rehabilitation services may not be easily accessible (Peretti 2017; Tyagi 2018), and can thus increase the frequency and intensity of care provided to patients and consequently to motivate improvements in their own home environment (Agostini 2015). Telerehabilitation programs can also potentially be adjusted to patients’ daily lives since restrictions on time or location are not always imposed, increasing people’s ability to attend work (Knudsen 2019).
However, certain disadvantages of home‐based telerehabilitation have been reported, including skepticism on the part of patients due to remote interaction with their physicians or rehabilitation professionals, equipment setup‐related difficulties, the limited scope of exercises, and the need for proper training and education of people involved (Peretti 2017; Tyagi 2018). Telerehabilitation and other telehealth services also require reliable access to equipment, electricity and internet, which can pose serious challenges, particularly in low resource or remote settings (Odendaal 2020).
Why is it important to do this review?
Many people eligible for rehabilitation experience restricted access to services. The COVID‐19 pandemic has worsened service availability and accordingly introduced growing burdens on patients, families and primary healthcare providers (Bettger 2020; Bittner 2020; Ceravolo 2020a; Negrini 2020b). The restrictions that have been imposed to contain the spread of infection are limiting access to many healthcare services, including rehabilitation. Consequences might be long‐lasting, increasing disabling conditions and hindering illness recovery in the population.
The World Health Organization (WHO) emphasizes the importance of guaranteeing equitable access to quality health services (World Health Organization 2019). As part of this goal, the WHO and the UN have called for the increased use and affordability of information and communication technology (ICT), including telerehabilitation, for people with disabilities. They have also called for more research that can support the quality of rehabilitation services (Clark 2006; World Health Organization 2011).
The identification of factors influencing the organisation and delivery of in‐person home‐based rehabilitation and home‐based telerehabilitation for people in need of rehabilitation in pandemic and non‐pandemic contexts is a relevant issue to investigate. By identifying these factors, we can more easily identify strategies that can improve the provision of these services in ways that are likely to be experienced as acceptable, feasible and equitable by patients, healthcare providers and other stakeholders.
How this review might inform or supplement what is already known in this area
As described above, several systematic reviews have assessed the efficacy and effectiveness of in‐person home‐based rehabilitation and home‐based telerehabilitation services for different patient groups (Anderson 2017; Cheng 2017; Coupar 2012; Gonçalves‐Bradley 2017; Khan 2015; Laver 2020; Saragiotto 2016). In addition, in response to the COVID‐19 pandemic, a series of rapid systematic reviews of the latest scientific literature on rehabilitation have been prepared (Andrenelli 2020; Ceravolo 2020a; Ceravolo 2020b; De Sire 2020). However, these reviews do not aim to explore factors that influence the organisation and delivery of rehabilitation services.
Bettger and colleagues recently published a commentary to describe adjustments to the continuum of rehabilitation services across 12 low‐, middle‐, and high‐income countries in the context of national COVID‐19 preparedness responses. To obtain this information, 20 authors provided reports of rehabilitation practice in their own countries (Argentina, Belgium, Brazil, China, Germany, Guyana, India, Singapore, Spain, Tanzania, the UK,USA) during the COVID‐19 pandemic (Bettger 2020). This commentary describes some of the adaptations and reorganisation of the rehabilitation services carried out in these countries in response to COVID‐19. However, it is not a systematic review and does not have a methodology that allows a formal investigation of the factors that influence the organisation and delivery of rehabilitation services.
We are not aware of any systematic reviews of qualitative research exploring factors that influence the organisation and delivery of in‐person home‐based rehabilitation and home‐based telerehabilitation services, either in pandemic or ‘non‐pandemic’ contexts. Our qualitative evidence synthesis provides information that may be helpful for organising these services and that may also inform the design of future studies and systematic reviews of effectiveness.
Objectives
To identify factors that influence the organisation and delivery of in‐person home‐based rehabilitation for people needing rehabilitation.
To identify factors that influence the organisation and delivery of home‐based telerehabilitation for people needing rehabilitation.
Methods
Criteria for considering studies for this review
Types of studies
We included primary studies applying qualitative designs such as ethnography, phenomenology, case studies, grounded theory studies and qualitative process evaluations. We included studies that used both qualitative methods for data collection (e.g. focus group discussions, individual interviews, observation, diaries, document analysis), and qualitative methods for data analysis (e.g. thematic analysis, framework analysis, grounded theory). We included open‐ended survey questions analysed using a qualitative methodology. We excluded studies that collected data using qualitative methods but did not analyse these data using qualitative analysis methods (e.g. open‐ended survey questions where the response data are analysed using descriptive statistics only).
We included both published and unpublished studies and studies published in any language (see also section on Language translation below).
We included mixed‐methods studies where it was possible to extract the data that were collected and analysed using qualitative methods.
We included studies regardless of whether they were conducted alongside studies of the effectiveness of in‐person home‐based rehabilitation or home‐based telerehabilitation services or not.
We did not exclude studies based on our assessment of methodological limitations. We have used this information about methodological limitations to assess our confidence in the review findings.
Topic of interest
We included studies where the primary focus is experiences, perceptions and behaviours about the provision of in‐person home‐based rehabilitation and home‐based telerehabilitation services responding to patients’ needs in different phases of their health conditions (Gutenbrunner 2020b).
Types of participants
We included studies that explore the experiences, perceptions and behaviours of:
adults eligible for rehabilitation, defined as people with either a defined health condition, functioning problem, specific impairment, activity limitations, or participation restriction for which rehabilitation services are provided (Gutenbrunner 2020a);
informal caregivers directly involved in caring for people who are eligible for rehabilitation (often a family member or friend);
rehabilitation healthcare providers; these could include general and specialist physicians, nurses, occupational therapists, physiotherapists, respiratory therapists, psychologists, speech and language therapists, prosthetist and orthotist, community‐based rehabilitation workers, social workers, special educators, and other key professionals and lay health workers who use telerehabilitation to support or provide home‐based care to patients and/or their informal caregivers, or provide in‐person home‐based rehabilitation services;
other stakeholders involved in the commissioning, evaluation, design, and implementation of rehabilitation services. These could include policymakers at the local, national, or supranational level; administrative staff; information technology staff; managerial and supervisory staff at the organisational level; and technical staff who develop and maintain the platforms to provide telerehabilitation services.
Types of intervention
We define rehabilitation as ”a multimodal person‐centred process including functioning interventions, targeting body functions, activities and participation, and the interaction with the environment, aimed at optimising functioning in persons with health conditions, experiencing disability or likely to experience disability” (Negrini 2020c).
1. In‐person home‐based rehabilitation
We included studies of in‐person home‐based rehabilitation, which we defined as the delivery of rehabilitation services with in‐person encounters provided where the patient lives (e.g. home, nursing homes, long‐term care places) (Chi 2020). This can involve a range of services including continuous functioning assessment, prevention, diagnostic, therapy (e.g. nutritional support, dysphagia and swallowing, physical, psychological, cognitive, cardio‐respiratory, language therapy, occupational therapy, and respiratory therapy), monitoring, supervision, education, consultation, counselling, social support, psychological support, home‐based primary care, prescription and provision of assistive technologies (robotic devices, virtual reality devices, games and motion detection tools), home aids, family support, societal integration, home and workplace adaptations, mental support, home nursing and family help, and other methods of healthcare delivery Bittner 2020; Laver 2020; Rezaei 2019).
2. Home‐based telerehabilitation
We also included home‐based telerehabilitation studies, which we defined as the delivery of rehabilitation services where the patient lives using information and communication technologies (Brennan 2009). This can involve the same services as listed above for in‐person, home‐based rehabilitation (Bittner 2020; Laver 2020; Rezaei 2019).
Search methods for identification of studies
Electronic searches
The Information Specialist Paola Andrea Ramírez developed the search strategies in consultation with the review authors, according to the search methods for qualitative synthesis (Booth 2016).
We searched the databases listed below. We did not apply any limits on language or publication date. We included a methodological filter for qualitative studies. See Appendix 1 for all strategies used.
We searched the following databases for primary studies:
PubMed, US National Library of Medicine (NLM) (pubmed.ncbi.nlm.nih.gov/) (searched 16 June 2022);
Global Health, Ovid (https://www.wolterskluwer.com/en/solutions/ovid/global‐health‐30) (searched 23 June 2022);
VHL Regional Portal, BIREME (https://bvsalud.org/) (searched 16 June 2022).
We searched MedXriv via BIREME (https://bvsalud.org/) for pre‐prints(searched 16 June 2022).
We searched the following databases for related systematic reviews that might include eligible primary studies:
Epistemonikos, Epistemonikos Foundation (www.epistemonikos.org/) (searched 16 June 2022);
Health Systems Evidence, McMaster University (www.healthsystemsevidence.org/) (searched 23 June 2022);
EBM Reviews, Ovid (https://www.wolterskluwer.com/en/solutions/ovid/evidencebased‐medicine‐reviews‐ebmr‐904) (searched 23 June 2022).
Searching other resources
We searched international and regional web portals of rehabilitation organisations and associations to identify pertinent studies (searched June 2022).
We reviewed the reference lists of all included studies and key references of systematic reviews. Where necessary, we contacted the authors of included studies to clarify published information and to seek unpublished data. We contacted researchers with expertise relevant to the review topic to request studies that might meet our inclusion criteria.
Data collection, management, and synthesis
Selection of studies
Two review authors from a team of seven (LHL, AMP, DFP, MV, LFM, MAS, KMC) independently assessed the titles and abstracts of the identified records to evaluate eligibility. We retrieved the full text of all the papers identified as potentially relevant by both review authors. Two review authors from a team of nine then assessed these papers independently (LHL, AMP, DFP, MV, CG, LFM, CA, ASR, IL). We resolved disagreements by discussion or, when required, by involving a third review author.
Where the same study, using the same sample and methods, was presented in different reports, we collated these reports so that each study (rather than each report) is the unit of interest in our review.
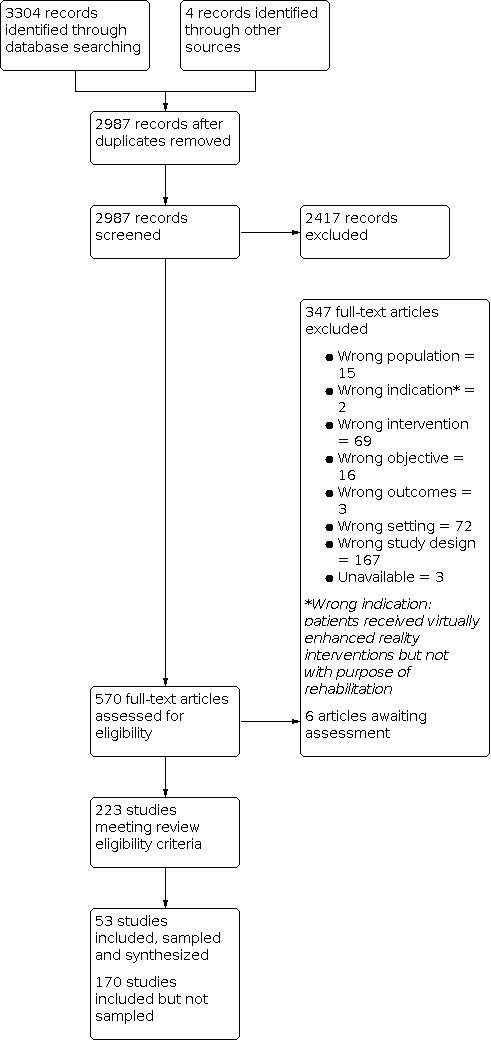
We included a PRISMA flow diagram to show our search results and the process of screening and selecting studies for inclusion (Figure 1).
1.
Language translation
For titles and abstracts that were published in a language that none of the review team are proficient in (i.e. languages other than English, Spanish, Norwegian, Italian, Portuguese, Swedish and Danish), we carried out an initial translation through open‐source software (Google Translate). If this translation indicated inclusion, or if the translation was inadequate to decide, we retrieved the full text of the paper. We then asked members of Cochrane networks or other networks that are proficient in that language to assist us in assessing the full text of the article for inclusion. If this could not be done for a paper in a particular language, the paper was listed under ‘studies awaiting classification,’ to ensure transparency in the review process.
Sampling of studies
Qualitative evidence synthesis aims for variation in concepts rather than an exhaustive sample, and large amounts of study data can impair the quality of the analysis. As we considered that the high number of studies we had included in the review represented a problem for the analysis, we decided to select a sample of these studies for the analysis.
To ensure the broadest possible variation within the studies sampled for analysis, we used a purposive sampling approach and applied maximum variation sampling (Patton 2002). This approach has been successfully implemented in several other qualitative evidence syntheses (Ames 2019; Karimi‐Shahanjarini 2019; McCartan 2020).
To answer our review questions, we decided on four criteria that would enable us to capture rich data from different settings, different types of participants and different health conditions. This became our four‐step sampling frame.
First, we sampled all studies from low‐ and middle‐income country (settings (LMICs), as most studies took place in high‐income country (HIC) settings and we wanted to ensure that findings from LMICs were represented in the synthesis. This gave us seven studies.
Second, we sampled an additional 14 studies that maximized the variation on the types of participants included in the studies (patients and caregivers, healthcare providers, and other stakeholders).
Third, we sampled an additional 23 studies that maximized variation in relation to the type of disability explored in the study (mobility, vision, hearing, or cognition).
Finally, we went through the remaining studies and, for the study data that were relevant to the synthesis objective, assessed the richness of these data. We considered a data‐rich study to be one that provided more detailed descriptions to understand patients', caregivers', healthcare providers' and other stakeholders' experiences and opinions about home‐based rehabilitation. We assessed the richness of these data in relation to our review question as high (i.e. providing perspectives of more than one type of participant‐patients, caregivers, healthcare providers and other stakeholders‐; addressing more than one domain in the Consolidated Framework for Implementation Research (CFIR); and in‐depth data analysis), moderate (i.e., providing perspectives of more than one type of participant or addressing more than one domain in the CFIR framework) or poor (i.e. providing perspectives of one type of participant or addressing only one domain in the CFIR framework ). We then sampled all nine studies that we rated as having moderate or high data richness.
This process gave us a total of 53 sampled studies.
Extraction of information about study characteristics
Two pairs of review authors (AMP, LFM, KMC, MAS) independently extracted information about the study characteristics of the included papers. We extracted information about:
author(s), year, country;
mode of rehabilitation delivery (e.g. home‐based rehabilitation services, home aids, home modifications, home nursing and family help, telerehabilitation);
type of participant (i.e. patient, caregiver, healthcare provider, other stakeholders);
health condition (i.e. physical, vision, hearing, or cognition);
study design, approach for data collection and analysis.
We resolved any differences of opinion about study characteristics by consensus within the pairs of review authors that extracted the information about study characteristics.
Assessing the methodological limitations of included studies
Two review authors [MV, KMC, MAS] independently assessed methodological limitations for each study using the Critical Appraisal Skills Programme (CASP) (Critical Appraisal Skills Programme 2013). We summarised the methodological limitations judgments across different studies for each of the domains listed below.
Was there a clear statement of the aims of the research?
Is a qualitative methodology appropriate?
Was the research design appropriate to address the aims of the research?
Was the recruitment strategy appropriate to the aims of the research?
Were the data collected in a way that addressed the research issue?
Has the relationship between researcher and participants been adequately considered?
Have ethical issues been taken into consideration?
Was the data analysis sufficiently rigorous?
Is there a clear statement of findings?
How valuable is the research? (Determined by assessing the richness of the study data. See section above on 'Sampling of studies' for details).
We resolved disagreements by discussion or, when required, by engaging a third review author. Where any of the review authors were also authors of included studies, they were not involved in the assessment of the study’s methodological limitations.
Data extraction, analysis and synthesis
We considered a number of potentially relevant frameworks for data analysis but chose the CFIR because it provided us with a comprehensive list of factors that could influence intervention implementation (Damschroder 2009). The CFIR has been developed based on different constructs associated with effective implementation; supported by a compilation of publications across 13 scientific disciplines (Damschroder 2009; Means 2020). CFIR facilitates systematic analysis and organisation of findings from implementation studies and, in addition, is adaptable to different settings and scenarios. The CFIR framework is composed of five major domains, each of which may affect an intervention’s implementation (Damschroder 2009; Means 2020).
Intervention characteristics (i.e. key attributes of interventions that influence the success of implementation as their complexity, costs, design, among others).
Inner setting (i.e. features of the implementing organisation as their structural characteristics, networks and communications, culture, and readiness for implementation).
Outer setting (i.e. features of the external context or environment as external policies, incentives, and constraints; patient needs and resources; and peer pressure).
Characteristics of individuals involved in implementation (i.e., individual stage of change, knowledge and beliefs about the intervention, self‐efficacy, and other personal attributes).
Implementation process (i.e. strategies or tactics that might influence implementation, these include strategies for engaging, executing, planning, reflecting and evaluating).
See also Figure 2 for a representation of using the CFIR framework in this review.
2.

Relationship between CFIR Framework and this qualitative evidence synthesis
Extracting and coding the evidence against the CFIR framework: we developed a data extraction form that was based on the CFIR framework and that was piloted on a small number of studies before final approval. Five review authors (MV, LHL, AMP, DP, and LFM) used this data extraction form to extract data on participants’ experiences, perceptions, and behaviours about factors that influence the provision of in‐person home‐based rehabilitation and telerehabilitation services and to code this data against the CFIR framework. A pilot trial of the data extraction form was conducted to check its adequacy, and changes were made when necessary.
Once the five review authors had finished data extraction, four review authors (MV, CG, ASR, and IL) checked this data extraction and verified that all relevant data were extracted. We included data in the form of quotes or field note extracts, as well as authors’ interpretations which could be presented in either the results or discussion sections of the articles.
Once our analyses were finalised, we explored whether any of the factors we had identified were primarily based on studies from high‐, middle‐, or low‐income settings and if they represented only a particular group of patients.
Developing implications for practice
Once we had finished preparing the review findings, we examined each finding, identified factors that could influence the implementation of the intervention/s, and developed prompts for future implementers. These prompts are not intended to be recommendations but are phrased as questions to help implementers consider the implications of the review findings within their context. We sent these prompts to a selection of stakeholders from different countries and professional backgrounds to gather their feedback about the relevance of these prompts and how they are phrased and presented, and then revised the prompts accordingly. These prompts are presented in the "implications for practice" section.
Assessing our confidence in the review findings
Four review authors [MV, LHL, AMP, and DP] used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to assess our confidence in each finding (Lewin 2018). GRADE‐CERQual assesses confidence in the evidence, based on the following four key components.
Methodological limitations of included studies: the extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding.
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data. By cogent, we mean well‐supported or compelling.
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quantity of data supporting a review finding.
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, phenomenon of interest, setting) specified in the review question.
After assessing each of the four components, we developed a ‘Summary of qualitative findings’ table and made a judgment about the overall confidence in the evidence supporting the review finding. We judged confidence as high, moderate, low, or very low. The final assessment was based on consensus among the review authors. All findings started as high confidence and then were graded down if there are important concerns regarding any of the GRADE‐CERQual components.
Summary of Qualitative Findings table(s) and Evidence Profile(s)
We presented summaries of the findings and our assessments of confidence in these findings in a Summary of Qualitative Findings table. We have included detailed descriptions of our confidence assessments in an GRADE‐CERQual Qualitative Evidence Profile (Appendix 2).
Results
Results of the search
The search retrieved 2987 records after duplicates were removed. We reviewed 570 articles in full‐text, 347 were excluded (Additional file) and 223 articles met our inclusion criteria, of which eight were performed in low‐ and middle‐income countries. Eighty‐one studies addressed in‐person home‐based rehabilitation without a telehealth component. One‐hundred‐ten studies addressed home‐based telerehabilitation services. Thirty‐two studies addressed both in‐person home‐based rehabilitation and home‐based telerehabilitation services. Eighty studies presented the perspectives of different types of participants, the remaining studies presented only the perspective of patients (n =105), caregivers (n = 8), healthcare providers (n = 26), and other stakeholders (n = 5). In relation to health conditions, 63 studies focused on rehabilitation services for people who had a stroke. The remaining studies focused on people with cardiovascular diseases (n = 35), musculoskeletal disorders (n = 20), rehabilitation services for elderly people (n = 17), chronic obstructive pulmonary disease (n = 11), cancer (n = 11), brain injury (n = 10), Multiple Sclerosis (n = 10), spinal cord injury, (n = 10), persistent pain (n = 4), intellectual disabilities (n = 3), hearing impairments (n = 1), joint replacements (n = 1), temporomandibular disorders (n = 1), rheumatoid arthritis (n = 1), and burn (n = 1). Six studies did not specify the health condition.
From the 223 studies that met our inclusion criteria, we sampled 53 studies for inclusion in the analysis (Figure 1). All of the sampled studies were published between 2009 and 2020, except for one from 2004 (Dubouloz 2004). All of the studies were published in English. We found six studies that could not be translated and we listed them under the section Characteristics of studies awaiting classification.
Description of the studies
In this section, we describe the studies that we included and sampled. For a more detailed description of 53 studies that were included and sampled see Table 2. For a description of studies that were included but not sampled see Table 3.
1. Characteristics of studies included and sampled.
| Author(s), Year | Country | Mode of rehabilitation delivery | Description of study participants | Health condition or disability addressed by the study/Type of rehabilitation delivered | Study design/ Data collection approach/ Data analysis approach |
| Argent 2018 | Ireland | Home‐based telerehabilitation | Ten healthcare professionals (four physiotherapists, two clinical nurse specialists, two orthopaedic assistants, one occupational therapist and one staff nurse) | Joint replacement/ Exercise therapy |
Qualitative study/ Semi‐structured interviews/ Thematic analysis with a grounded‐theory approach |
| Borade 2019 | India | In‐person home‐based rehabilitation | Twenty‐five patients having mobility related disabilities, who used one or more ads | Mobility restriction/ Activities in daily living (ADL) | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| Brouns 2018 | Netherlands | In‐person + home‐based telerehabilitation | Thirty‐two patients, fifteen caregivers, and thirteen healthcare professionals (physiotherapists, psychologists, occupational therapists, speech therapists, physicians, and managers) | Stroke/ Multidisciplinary | Qualitative study/ Semi‐structured individual and focus group interviews/ Direct content analysis using the implementation model of Grol |
| Bodker 2015 | Denmark | In‐person + home‐based telerehabilitation | Eleven patients with COPD and the therapist of the programme (managing nurse and the physiotherapist) | Chronic Obstructive Pulmonary Disease/ Pulmonary |
Ethnographic/ Observations and semi‐structured interviews/ Analytical concepts developed within STS (Science and Technology Studies) in order to study the taming and unleashing of telecare |
| Damhus 2018 | Denmark | Home‐based telerehabilitation | Twenty‐five healthcare professionals (6 nurses and 19 physiotherapists) | Chronic Obstructive Pulmonary Disease/ Respiratory |
Theoretical domains framework/ Semi‐structured individual and focus group interviews/ Data were triangulated and was used as a coding framework in the analysis |
| Dennett 2020 | England | Home‐based telerehabilitation | Eleven patients with multiple sclerosis | Multiple Sclerosis/ Exercise therapy | Qualitative study/ In‐depth, individual, face‐to‐face interviews/ Thematic analysis |
| Dinesen 2019 | Denmark | Home‐based telerehabilitation | Fourteen cardiac patients, twelve patient spouses/partners, and one son | Cardiac disease/ Cardiac | Descriptive case study/ Documents, participant observation, and interviews/ Thematic analysis |
| Dubouloz 2004 | Canada | In‐person home‐based rehabilitation | Six patients with rheumatoid arthritis | Arthritis/ Activities in daily living (ADL) | Grounded theory study/ Semi‐structured interviews/ Constant comparative analysis |
| Edbrooke 2020 | Australia | In‐person home‐based rehabilitation | Ninety‐two patients with non‐small cell lung cancer | Cancer/ Exercise therapy | Mixed methods study / Semi‐structured interviews, home visits and telephone calls/ Content analysis |
| Emmerson 2018 | Australia | Home‐based telerehabilitation | Ten patients with stroke and upper limb impairment | Stroke/ Exercise therapy | Convergent mixed methods design, based on phenomenology/ Semi‐structured interview in‐depth/ Thematic analysis |
| Folan 2015 | Australia | Home‐based telerehabilitation | Seven patients ( 4 in‐patients and 3 out‐patients) with spinal cord injury | Spinal cord injury/ Activities in daily living (ADL) | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| Govender 2019 | South Africa | In‐person home‐based rehabilitation | Five patients, five family caregivers, five community partners, five clinicians, and five researchers | Elderly/ Multidisciplinary | Exploratory study/ Survey and semi‐structured interviews/ Thematic analysis |
| Gélinas‐Bronsard 2019 | Canada | Home‐based telerehabilitation | Eight patients who had suffered a stroke |
Stroke/ Multidisciplinary | Individual qualitative study/ Semi‐structured interviews/ Content analysis |
| Hale Gallardo 2020 | United States | Home‐based telerehabilitation | Ten stakeholders (medical directors and program managers) | Not specified/ Exercise therapy | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| HeydariKhayat 2020 | Iran | In‐person home‐based rehabilitation | Sixteen burn survivors patients | Burns/ Multidisciplinary | Phenomenological study/ Semi‐structured interviews/ Thematic analysis |
| Hoaas 2016 | Norway | Home‐based telerehabilitation | Ten patients with moderate to severe COPD | Chronic Obstructive Pulmonary Disease /Respiratory | Mixed methods study/ Analysis of logs on the webpage, semi‐structured focus groups, standardised questionnaire and an individual open‐ended questionnaire/ Thematic analysis |
| Kamwesiga 2017 | Uganda | Home‐based telerehabilitation | Eleven patients with stroke and nine family caregivers | Stroke/ Multidisciplinary | Grounded theory study/ Semi‐structured interviews/ Constant comparative analysis |
| Lawson 2020 | Australia | Home‐based telerehabilitation | Twenty‐five patients with stroke and nine healthcare professionals | Stroke/ Cognitive | Qualitative study/ Semi‐structured interviews/ Inductive thematic analysis |
| Malmberg 2018 | Sweden | Home‐based telerehabilitation | Twenty patients that had used Internet interventions for hearing aid | Hearing impairment/ Communication | Qualitative exploratory study/ Semi‐structured telephone interviews/ Content analysis |
| Mendell 2019 | Canada | Home‐based telerehabilitation | Thirty‐eight patients with acute coronary syndrome | Acute coronary syndrome/ Cardiac | Qualitative study/ Chat sessions/ Thematic analysis |
| Mohd Nordin 2014 | Malaysia | In‐person home‐based rehabilitation | Fifteen rehabilitation professionals and eight stroke survivors | Stroke/ Multidisciplinary | Qualitative study/ Focus groups/ Thematic analysis |
| Ng 2013 | Canada | Home‐based telerehabilitation | Three patients and their significant others | Brain Injury/ Cognitive | Case study/ Feedback interviews, therapist´s field notes and session recordings/ Descriptive analysis |
| Nordin 2017 | Sweden | Home‐based telerehabilitation | Nineteen patients with persistent musculoskeletal pain | Persistent Pain/ Multimodal for pain | Qualitative study/ Semi‐structured interviews/ Content analysis |
| O'Doherty 2013 | Ireland | In‐person home‐based rehabilitation | Ten nurses | Elderly/ Nursing in | Qualitative descriptive study/ Semi‐structured interviews/ Thematic analysis |
| O'Shea 2020 | Dublin and Belgium | Home‐based telerehabilitation | Forty‐four patients with cardiovascular disease | Cardiovascular disease/ Cariac | Qualitative study/ Participant debriefs, interviews/ Braun and Clarke framework for thematic analysis |
| Ownsworth 2020 | Australia | Home‐based telerehabilitation | Thirteen multidisciplinary rehabilitation coordinators, nine patients, and eight family caregivers | Brain injury/ Multidisciplinary | Qualitative study/ Semi‐structured interviews/ Inductive analysis |
| Oyesanya 2019 | United States | Home‐based telerehabilitation | Fifteen patients and twelve caregivers | Brain Injury/ Multidisciplinary | Qualitative exploratory study/ Semi‐structured interviews/ Content analysis |
| Palazzo 2016 | France | In‐person + home‐based telerehabilitation | Twenty‐nine patients with chronic low back pain | Chronic low back pain/ Multidisciplinary | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| Palmcrantz 2017 | Sweden | Home‐based telerehabilitation | Fifteen patients who had suffered stroke | Stroke/ Exercise therapy | Qualitative study/ Semi‐structured interviews/ Content analysis |
| Pekmezaris 2020 | United States | In‐person home‐based rehabilitation | Approximately 20 community advisory board members, one‐third were patients and caregivers, one‐third were providers (pulmonologists, researchers, and primary care physicians), and another one‐third were the other stakeholders (such as community‐based organizations) |
Pulmonary diseases/ Respiratory | Qualitative study/ Focus groups/ Content analysis |
| Pinto 2014 | Brazil | In‐person home‐based rehabilitation | Twenty‐three patients with COPD | Chronic Obstructive Pulmonary Disease/ Respiratory | Qualitative study/ Semi‐structured interviews/ Thematic content analysis and contextualized semantic interpretation |
| Ranaldi 2018 | United Kingdom | In‐person home‐based rehabilitation | Four hundred fifty‐seven patients with cardiac disease | Cardiac disease/ Cardiac | Qualitative study/ Questionnaires/ Thematic analysis |
| Randström 2012 | Sweden | In‐person home‐based rehabilitation | Ten older patients | Elderly/ Multidisciplinary | Qualitative study/ Interviews/ Content analysis |
| Randstrom 2013 | Sweden | In‐person home‐based rehabilitation | Six older patients and six family members | Elderly/ Multidisciplinary | Qualitative descriptive study/ Interviews/ Content analysis |
| Randström 2014 | Sweden | In‐person home‐based rehabilitation | Twenty‐eight healthcare providers, six physiotherapists, three occupational therapists, five district nurses, five nurse assistants, one home helper, three home help officers responsible for needs assessment and five home help officers in charge of home help | Elderly/ Multidisciplinary | Qualitative descriptive study/ Focus groups/ Content analysis |
| Rietdijk 2020 | Australia | Home‐based telerehabilitation | Thirty‐six patients and their caregivers | Elderly/ Communication | Mixed methods study/ Skype interview, telephone interview or written questionnaire/ Inductive thematic analysis |
| Rizzo 2019 | United States | In‐person home‐based rehabilitation | Ten patients with orthopaedic diagnoses | Musculoeskeletal/ Exercise therapy | Interpretative study/ Semi‐structured interviews/ Constant comparative analysis |
| Saywell 2015 | New Zealand | Home‐based telerehabilitation | Fifteen patients who had suffered stroke | Stroke/ Exercise therapy | Qualitative descriptive study/ A brief questionnaire was used to gather data on mobile phone ownership/ Inductive analysis |
| Schopfer 2020 | United States | In‐person home‐based rehabilitation | One hundred and seventy one patients with cardiac diseases (acute myocardial infarction, coronary artery bypass graft surgery, obstructive coronary artery disease, stable angina, valve replacement and some outpatients with stable heart failure | Cardiac disease/ Cardiac | Mixed methods study/ Survey, and open‐ended semi‐structured interviews/ Thematic analysis |
| Shulver 2016 | Australia | Home‐based telerehabilitation | Forty‐four health workers (experienced and inexperienced) providing services to older people in the areas of rehabilitation and allied health, residential aged care and palliative care | Elderly/ Multidisciplinary | Qualitative study/ Semi‐structured focus groups/ Thematic analysis |
| Shulver 2017 | Australia | Home‐based telerehabilitation | Thirteen older patients, three spouses and one caregiver | Elderly/ Exercise therapy | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| Silveira 2019 | United States | Home‐based telerehabilitation | Twenty patients with multiple sclerosis who use wheelchairs | Multiple Sclerosis/ Exercise therapy | Qualitative study/ Semi‐structured interviews/ Deductive content analysis |
| Stark 2019 | Germany | In‐person home‐based rehabilitation | Thirteen patients and nine non‐professional coaches (family members) | Stroke/ Exercise therapy | Mixed methods study/ Semi‐structured interviews/ Hermeneutic phenomenological data analysis |
| Stuifbergen 2011 | United States | In‐person + home‐based telerehabilitation | Thirty‐four patients with multiple sclerosis | Multiple Sclerosis/ Cognitive | Qualitative exploratory, descriptive study/ Qualitative data from a questionnaire administered by phone/ Content analysis |
| Sureshkumar 2016 | India | Home‐based telerehabilitation | Sixty patients and their caregivers | Stroke/ Multidisciplinary | Mixed methods study/ Semi‐structured questionnaire/ Framework approach |
| Teriö 2019 | Uganda | Home‐based telerehabilitation | Twelve participants: Four occupational therapists, three researchers, three information technology (IT) specialists and two rehabilitation managers | Stroke/ Activities in daily living (ADL) | Single‐case study/ Semi‐structured interviews/ Framework approach |
| Tsai 2016 | Australia | In‐person + home‐based telerehabilitation | Eleven patients with COPD | Chronic Obstructive Pulmonary Disease/ Respiratory | Mixed methods study/ Semi‐structured interviews/ Thematic descriptive analysis |
| Turner 2011 | Australia | In‐person home‐based rehabilitation | Twenty patients and eighteen family caregivers | Brain Injury/ Multidisciplinary | Qualitative study/ Semi‐structured interviews/ Thematic analysis |
| Tyagi 2018 | Singapore | Home‐based telerehabilitation | Thirty‐seven participants: 13 patient‐caregiver dyads and 11 therapists | Stroke/ Exercise therapy | Qualitative study / Semi‐structured in‐depth interviews and focus group discussions/ Thematic analysis |
| Umb Carlsson 2019 | Sweden | In‐person home‐based rehabilitation | Five residents, six staff members and five rehabilitation professionals | Intellectual disability/ Promotion of healthy lifestyles | Qualitative study/ Semi‐structured interviews/ Content analysis |
| Van der Meer 2020 | Netherlands | Home‐based telerehabilitation | Nine patients and eleven orofacial physical therapists | Temporomandibular Disorders/ Exercise therapy |
Qualitative descriptive study/ Open face‐to‐face interviews/ Thematic analysis |
| VanderVeen 2019 | Netherlands | In‐person home‐based rehabilitation | Fourteen healthcare professionals: two occupational therapists, two physical therapists, two case managers, a psychologist, an elderly advisor, a nurse, a speech therapist, a nursing home manager, a manager in allied healthcare, a general practitioner and a geriatrician. | Stroke/ Multidisciplinary | Qualitative study/ Focus groups and semi‐structured interviews/ Content analysis |
| Vik 2009 | Norway | In‐person home‐based rehabilitation | Three older patients | Elderly/ Nursing in | Case study/ Interviews/ Grounded theory |
2. Studies that met our inclusion criteria but were not sampled for analysis.
| Author / year | Country | Health condition | Mode of rehabilitation delivery |
| Alary Gauvreau 2019 | Canada | Aphasia | Telerehabilitation |
| Ando 2019 | United Kingdom | Motor neurone disease | Telerehabilitation |
| Banner 2015 | Canada | Heart disease | Telerehabilitation |
| Barclay 2020 | Australia | Spinal cord injury | Home‐based + telerehabilitation |
| Bendelin 2018 | Sweden | Chronic pain | Home‐based + telerehabilitation |
| Birkeland 2017 | Norway | No specific health condition described | Home‐based rehabilitation |
| Boland 2018 | New Zealand | Stroke | Home‐based rehabilitation |
| Booth 2007 | Australia | Spinal cord injury | Home‐based rehabilitation |
| Brennan 2020 | Ireland | Cancer | Home‐based + telerehabilitation |
| Brewer 2017 | United States | Heart disease | Telerehabilitation |
| Buimer 2017 | Netherlands | Cancer | Telerehabilitation |
| Burkow 2015 | Norway | Pulmonary diseases | Home‐based + telerehabilitation |
| Caughlin 2020 | Canada | Stroke | Telerehabilitation |
| Chen 2019a | China | Elderly | Home‐based rehabilitation |
| Chen 2019b | United States | Stroke | Telerehabilitation |
| Cherry 2017 | United States | Stroke | Telerehabilitation |
| Choularia 2014 | United Kingdom | Stroke | Home‐based rehabilitation |
| Clark 2013 | Australia | Heart disease | Telerehabilitation |
| Cobley 2013 | United Kingdom | Stroke | Home‐based rehabilitation |
| Constantinescu 2017 | Canada | Cancer | Home‐based + telerehabilitation |
| Conti 2015 | Italy | Spinal cord injury | Home‐based rehabilitation |
| Cottrell 2017 | Australia | Musculoeskeletal | Telerehabilitation |
| Davoody 2016 | Sweden | Stroke | Home‐based + telerehabilitation |
| Davoody 2014 | Sweden | Stroke | Telerehabilitation |
| DeVries 2017 | Netherlands | Arthritis | Home‐based + telerehabilitation |
| Deighan 2017 | United Kingdom | Heart disease | Telerehabilitation |
| Delmar 2009 | Denmark | Musculoeskeletal | Home‐based rehabilitation |
| Demain 2013 | United Kingdom | Stroke | Home‐based + telerehabilitation |
| Dimaguila 2019 | Australia | Stroke | Telerehabilitation |
| Dinesen 2011 | Denmark | Pulmonary diseases | Telerehabilitation |
| Dinesen 2013 | Denmark | Pulmonary diseases | Telerehabilitation |
| Dinesen 2018 | Denmark | Heart disease | Telerehabilitation |
| Dithmer 2016 | Denmark | Heart disease | Telerehabilitation |
| Dobson 2019 | New Zealand | Pulmonary diseases | Telerehabilitation |
| Doig 2009 | Australia | Traumatic brain injury | Home‐based rehabilitation |
| Donoso Brown 2015 | United States | Stroke | Home‐based + telerehabilitation |
| Dow 2007 | Australia | Stroke, cancer, brain tumour, amputation, Parkinson's and musculoskeletal | Home‐based rehabilitation |
| Duggan 2013 | United Kingdom | Chronic pain | Home‐based + telerehabilitation |
| Eliassen 2018 | Norway | Musculoeskeletal and Stroke | Home‐based rehabilitation |
| Eriksson 2011 | Sweden | Musculoeskeletal | Home‐based + telerehabilitation |
| Essery 2017 | United Kingdom | Vestibular dysfunction | Telerehabilitation |
| Feinberg 2018 | United States | Heart disease | Home‐based rehabilitation |
| Forman 2014 | United States | Heart disease | Telerehabilitation |
| Forsberg 2014 | Sweden | Multiple sclerosis | Telerehabilitation |
| Frohmader 2017 | Australia | Heart disease | Telerehabilitation |
| Frohmader 2015 | Australia | Heart disease | Telerehabilitation |
| Frost 2019 | United Kingdom | Heart disease | Home‐based + telerehabilitation |
| Galvin 2014 | Ireland | Stroke | Home‐based rehabilitation |
| Gell 2019 | United States | Cancer | Telerehabilitation |
| Giesbrecht 2014 | Canada | Elderly | Telerehabilitation |
| Gilbert 2019 | United Kingdom | Musculoeskeletal | Telerehabilitation |
| Giunti 2018 | Switzerland | Multiple sclerosis | Telerehabilitation |
| Gustafsson 2019 | Sweden | Elderly | Home‐based rehabilitation |
| Gustafsson 2014a | Australia | Stroke | Home‐based rehabilitation |
| Gustafsson 2014b | Australia | Stroke | Home‐based rehabilitation |
| Hale 2005 | New Zealand | Stroke | Home‐based rehabilitation |
| Harder 2017 | United Kingdom | Cancer | Telerehabilitation |
| Hathiramani 2019 | United Kingdom | Cancer | Home‐based rehabilitation |
| Hayward 2015 | Australia | Stroke | Home‐based + telerehabilitation |
| Herber 2017 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Heron 2019 | United Kingdom | Stroke | Telerehabilitation |
| Higgins 2017 | Australia | Heart disease | Telerehabilitation |
| Hill 2016 | Australia | Aphasia | Telerehabilitation |
| Hines 2017 | Australia | Traumatic brain injury | Telerehabilitation |
| Hjelle 2017 | Norway | Elderly | Home‐based rehabilitation |
| Hoffman 2017 | United States | Cancer | Telerehabilitation |
| Hwang 2017 | Australia | Heart disease | Telerehabilitation |
| Inskip 2018 | Canada | Pulmonary diseases | Telerehabilitation |
| Jakobsen 2018 | Norway | Elderly | Home‐based rehabilitation |
| James 2018 | Australia | Motor neurone disease | Home‐based + telerehabilitation |
| Jansen‐Kosterink 2019 | Netherlands | Chronic diseases | Telerehabilitation |
| Jäppinen 2017 | Finland | Musculoeskeletal | Home‐based rehabilitation |
| Jelin 2012 | Norway | Chronic pain | Telerehabilitation |
| Jones 2017 | United Kingdom | Stroke | Home‐based rehabilitation |
| Jones 2007 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Jullamate 2007 | Thailand | Stroke | Home‐based rehabilitation |
| Kairy 2014 | Canada | Traumatic brain injury | Telerehabilitation |
| Kairy 2013 | Canada | Musculoeskeletal | Telerehabilitation |
| Kingston 2014 | Australia | Musculoeskeletal | Telerehabilitation |
| Knudsen 2019 | Denmark | Heart disease | Telerehabilitation |
| Krishnan 2018 | United States | Stroke | Telerehabilitation |
| Lahham 2017 | Australia | Pulmonary diseases | Home‐based + telerehabilitation |
| Lai 2019 | United States | Disability | Telerehabilitation |
| Lawford 2018a | Australia | Musculoeskeletal | Telerehabilitation |
| Lawford 2018b | Australia | Musculoeskeletal | Telerehabilitation |
| Learmonth 2019 | Australia | Multiple sclerosis | Home‐based rehabilitation |
| Lee 2009 | Canada | Heart disease | Home‐based rehabilitation |
| Letts 2011 | Canada | Spinal cord injury | Telerehabilitation |
| Lindblom 2020 | Sweden | Stroke | Home‐based rehabilitation |
| Lou 2017 | Denmark | Stroke | Home‐based rehabilitation |
| Lovo Grona 2017 | Canada | Musculoeskeletal | Telerehabilitation |
| Lovo 2019 | Canada | Musculoeskeletal | Telerehabilitation |
| Lutz 2009 | United States | Stroke | Telerehabilitation |
| Lykke 2019 | Denmark | Elderly | Home‐based rehabilitation |
| Madden 2010 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Magne 2020 | Norway | Elderly | Home‐based rehabilitation |
| Markle‐Reid 2020 | Canada | Stroke | Home‐based + telerehabilitation |
| Martin 2018 | United Kingdom | Traumatic brain injury | Telerehabilitation |
| Martinez 2017 | United States | Traumatic brain injury | Telerehabilitation |
| Marwaa 2020 | Denmark | Stroke | Telerehabilitation |
| Mawson 2016 | United Kingdom | Stroke | Telerehabilitation |
| Mawson 2014 | United Kingdom | Stroke | Home‐based + telerehabilitation |
| Moe 2017 | Norway | Theres is no a health condition | Home‐based rehabilitation |
| Moe 2016 | Norway | Elderly | Home‐based rehabilitation |
| Moraal 2013 | Netherlands | Musculoeskeletal | Telerehabilitation |
| Muller 2014 | United Kingdom | Vestibular dysfunction | Telerehabilitation |
| Nanninga 2015 | Netherlands | Stroke | Home‐based rehabilitation |
| Nasr 2015 | United Kingdom | Stroke | Home‐based + telerehabilitation |
| Nordin 2015 | Sweden | Stroke | Home‐based rehabilitation |
| O'Hara 2015 | Australia | Other neurologic conditions | Telerehabilitation |
| Ouegnin 2018 | United States | Musculoeskeletal | Home‐based + telerehabilitation |
| Palacios‐Ceña 2016 | Spain | Multiple sclerosis | Home‐based + telerehabilitation |
| Pancer 2019 | Canada | Spinal cord injury | Home‐based + telerehabilitation |
| Pani 2016 | Italy | Arthritis | Home‐based + telerehabilitation |
| Parker 2020 | United States | Heart disease | Telerehabilitation |
| Parker 2014 | United Kingdom | Stroke | Home‐based rehabilitation |
| Parsons 2018 | United Kingdom | Stroke | Home‐based rehabilitation |
| Pasipanodya 2020 | United States | Spinal cord injury | Telerehabilitation |
| Paul 2014 | United Kingdom | Multiple sclerosis | Telerehabilitation |
| Pauwels 2018 | France | Elderly | Home‐based rehabilitation |
| Pearson 2016 | United Kingdom | Chronic pain | Telerehabilitation |
| Pettersson 2010 | Sweden | Stroke | Telerehabilitation |
| PfaeffliDale 2015 | New Zealand | Heart disease | Telerehabilitation |
| Pfaeffli 2012 | New Zealand | Heart disease | Home‐based + telerehabilitation |
| Pierce 2015 | United States | Stroke | Telerehabilitation |
| Pierce 2004 | United States | Stroke | Telerehabilitation |
| Pierce 2006 | United States | Stroke | Telerehabilitation |
| Plow 2013 | United States | Multiple sclerosis | Telerehabilitation |
| Randall 2008 | Canada | Theres is no a health condition | Home‐based rehabilitation |
| Rayce 2020 | Denmark | Pulmonary diseases | Home‐based rehabilitation |
| Reunanen 2016 | Finland | Stroke | Home‐based rehabilitation |
| Rothgangel 2017 | Netherlands | Musculoeskeletal | Telerehabilitation |
| Sankaran 2019 | Belgium | Heart disease | Telerehabilitation |
| Serpanou 2019 | Greece | Spinal cord injury | Home‐based rehabilitation |
| Shirai 2020 | Canada | Spinal cord injury | Telerehabilitation |
| Silver 2012 | United States | Spinal cord injury | Home‐based rehabilitation |
| Sivan 2014 | United Kingdom | Stroke | Home‐based rehabilitation |
| Smaerup 2017 | Denmark | Vestibular dysfunction | Telerehabilitation |
| Sørensen 2019 | Denmark | Pulmonary diseases | Home‐based rehabilitation |
| Spasić 2015 | United Kingdom | Musculoeskeletal | Telerehabilitation |
| Standen 2015 | United Kingdom | Stroke | Home‐based + telerehabilitation |
| Steihaug 2014 | Norway | Stroke | Home‐based rehabilitation |
| Steihaug 2016 | Norway | Theres is no a health condition | Home‐based rehabilitation |
| Sturkenboom 2016 | Netherlands | Parkinson | Home‐based rehabilitation |
| Tamm 1996 | Sweden | Stroke, musculoskeletal and disability | Home‐based rehabilitation |
| Taule 2014 | Norway | Stroke | Home‐based rehabilitation |
| Taylor 2015 | Australia | Palliative care patients | Home‐based + telerehabilitation |
| Taylor 2016 | Australia | Palliative care patients | Telerehabilitation |
| Thirumalai 2018 | United States | Multiple sclerosis | Telerehabilitation |
| Thorup 2016 | Denmark | Heart disease | Telerehabilitation |
| Timmerman 2017 | Netherlands | Cancer | Home‐based + telerehabilitation |
| Townsend 2013 | Canada | Arthritis | Telerehabilitation |
| Tung 2012 | Australia | Musculoeskeletal | Home‐based rehabilitation |
| Valdés 2018 | Canada | Motor neurone disease | Home‐based + telerehabilitation |
| VanEngen‐Verheul 2017 | Netherlands | Heart disease | Telerehabilitation |
| VanVelsen 2016 | Netherlands | Stroke, Chronic pain and Cerebral infarction | Telerehabilitation |
| Vloothuis 2020 | Netherlands | Stroke | Home‐based rehabilitation |
| VonKoch 1998 | Sweden | Stroke | Home‐based rehabilitation |
| VonKoch 2000 | Sweden | Stroke | Home‐based rehabilitation |
| Wade 2016 | Australia | Palliative care patients and older people | Telerehabilitation |
| Wakefield 2019 | United States | Heart disease | Home‐based rehabilitation |
| Wade 2016 | Australia | Cancer | Telerehabilitation |
| Walsh 2018 | Ireland | Heart disease | Telerehabilitation |
| Wentink 2019 | Netherlands | Stroke | Telerehabilitation |
| Wilms 2020 | Denmark | Disability | Home‐based rehabilitation |
| Wingham 2006 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Wingham 2014 | United Kingdom | Stroke | Telerehabilitation |
| Wingham 2015 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Wingham 2019 | United Kingdom | Heart disease | Home‐based rehabilitation |
| Wottrich 2007 | Sweden | Stroke | Home‐based rehabilitation |
* Based on our strategy for sampling, the reason for not sampling was the same for all of these studies: i.e., the study setting/population/mode of rehabilitation and type of rehabilitation provided in the study was already covered in many of the other sampled studies or the study was assessed to not provide sufficiently rich data.
Twenty of the 53 sampled studies addressed in‐person home‐based rehabilitation without a telehealth component. Twenty‐eight of the studies addressed home‐based telerehabilitation services. Five of the studies addressed both in‐person home‐based rehabilitation and home‐based telerehabilitation services.
Settings
Most of the studies were undertaken in high‐income countries (45/53): Australia (n = 10), the USA (n = 7), Canada (n = 4), Denmark (n = 3), Sweden (n = 7), UK (n = 2), France (n = 1), Ireland (n = 2), the Netherlands (n = 3), New Zealand (n = 1), Norway (n = 2), Singapore (n = 1), Germany (n = 1), and Belgium and Ireland (n = 1). Eight studies were conducted in low‐ and middle‐income countries, including Uganda (n = 2), India (n = 2), Brazil (n = 1), Iran (n = 1), South Africa (n = 1), and Malaysia (n = 1).
Participants
Seven studies presented the perspective of healthcare providers, 26 studies presented the perspective of patients, and one study presented the perspective of other stakeholders (i.e. administrators in the veteran health system of the USA). Nineteen studies presented the perspectives of different types of participants, including the perspectives of informal/family caregivers in eleven of these studies.
Health condition
Twelve studies focused on rehabilitation services for people who had had a stroke and eight studies on rehabilitation services for elderly people. The remaining studies focused on people with chronic obstructive pulmonary disease (six studies), cardiovascular diseases (five studies), brain injury (five studies), Multiple Sclerosis (three studies), musculoskeletal disorders (two studies), hearing impairments (one study), joint replacements (one study), spinal cord injury, (one study), persistent pain (one study), temporomandibular disorders (one study), intellectual disabilities (one study), rheumatoid arthritis (one study), lung cancer (one study), and burn (one study). Two studies did not specify the health condition.
Type of rehabilitation intervention
The interventions were multi‐component in 29 studies and single component in 24 of the studies. The multi‐component interventions were multidisciplinary rehabilitation (n = 16 studies), pulmonary rehabilitation (n = 6), cardiac rehabilitation (n = 5), multimodal pain rehabilitation (n = 1) and promotion of healthy lifestyles (n = 1). Single component rehabilitation interventions were exercises (n = 13 studies), increase functioning in activities in daily living (ADL) (n = 4), cognitive rehabilitation ( n = 3), nursing rehabilitation (n = 2), and communication rehabilitation (n = 2 studies).
Methodological limitations of the studies
All of the sampled studies gave some description, even if very brief, of the context, participants, sampling, methods, and analysis. However, in general, there was poor reporting of how study participants were recruited, making it difficult to establish whether the strategies used by the study authors were appropriate to the aims of the research. We also found poor reporting of researcher reflexivity across many of the studies, which limited transparency regarding the role of the researcher. Details of the methodological limitations assessments for each study are provided in Table 4.
3. Methodological assessments of included and sampled studies.
| Author(s), Year | Was there a clear statement of the aims of the research? | Is a qualitative method appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been considered? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? (Richness of the study data) | Overall assessment of method limitations |
| Argent 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Borade 2019 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Brouns 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | High | Minor concerns |
| Bodker 2015 | Yes | Yes | Yes | Unclear | No | No | Yes | Yes | Yes | High | Moderate concerns |
| Damhus 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Dennett 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High | None concerns |
| Dinesen 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Moderate | Minor concerns |
| Dubouloz 2004 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Unclear | Moderate | Minor concerns |
| Edbrooke 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Moderate | Minor concerns |
| Emmerson 2018 | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Moderate | Minor concerns |
| Folan 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Govender 2019 | Yes | Yes | Unclear | Unclear | Yes | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Gélinas‐Bronsard 2019 | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Moderate | Minor concerns |
| Hale Gallardo 2020 | No | Yes | Unclear | No | Yes | No | No | Yes | Yes | Moderate | Major concerns |
| HeydariKhayat 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High | None concerns |
| Hoaas 2016 | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Kamwesiga 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Poor | Minor concerns |
| Lawson 2020 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Yes | Yes | High | Minor concerns |
| Malmberg 2018 | Yes | Yes | Yes | Unclear | Yes | No | No | Yes | Yes | Moderate | Moderate concerns |
| Mendell 2019 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Mohd Nordin 2014 | Yes | Unclear | Yes | Unclear | Yes | No | Yes | Yes | Yes | Poor | Moderate concerns |
| Ng 2013 | No | No | Yes | Unclear | No | No | Yes | Yes | No | Poor | Major concerns |
| Nordin 2017 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| O'Doherty 2013 | Yes | Yes | Yes | No | Yes | No | Yes | No | Unclear | Moderate | Moderate concerns |
| O'Shea 2020 | Yes | Unclear | No | Yes | Yes | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Ownsworth 2020 | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | No | High | Minor concerns |
| Oyesanya 2019 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | High | Minor concerns |
| Palazzo 2016 | Yes | Yes | Unclear | Yes | Yes | No | Yes | Yes | No | High | Moderate concerns |
| Palmcrantz 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | High | Minor concerns |
| Pekmezaris 2020 | Yes | No | Yes | Yes | Unclear | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Pinto 2014 | Yes | Unclear | Yes | Unclear | Yes | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Ranaldi 2018 | Yes | No | Unclear | Unclear | Yes | No | Yes | Yes | Yes | Poor | Moderate concerns |
| Randström 2012 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Randstrom 2013 | Yes | Yes | Unclear | Yes | Unclear | No | Yes | Yes | Yes | High | Moderate concerns |
| Randström 2014 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | High | Minor concerns |
| Rietdijk 2020 | Yes | Yes | Yes | Yes | Unclear | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Rizzo 2019 | Yes | Yes | Unclear | Unclear | Yes | No | Yes | Yes | Unclear | Poor | Moderate concerns |
| Saywell 2015 | Yes | Yes | Yes | Yes | Unclear | No | Yes | Yes | Yes | Poor | Minor concerns |
| Schopfer 2020 | Yes | Yes | Unclear | Unclear | Yes | No | Yes | Yes | Yes | Moderate | Moderate concerns |
| Shulver 2016 | Yes | Unclear | Yes | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Shulver 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | High | Minor concerns |
| Silveira 2019 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Moderate | Minor concerns |
| Stark 2019 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| Stuifbergen 2011 | Yes | Yes | No | No | Unclear | No | No | Yes | Yes | Moderate | Major concerns |
| Sureshkumar 2016 | Yes | Unclear | Yes | Yes | Yes | No | Yes | Yes | No | Moderate | Moderate concerns |
| Teriö 2019 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Yes | Yes | Poor | Minor concerns |
| Tsai 2016 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Moderate | Minor concerns |
| Turner 2011 | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Moderate | Minor concerns |
| Tyagi 2018 | Yes | Yes | Yes | No | Yes | No | No | Yes | Yes | High | Moderate concerns |
| Umb Carlsson 2019 | Yes | Yes | Yes | Yes | Unclear | No | Yes | Yes | Unclear | Moderate | Moderate concerns |
| Van der Meer 2020 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
| VanderVeen 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Unclear | Moderate | Minor concerns |
| Vik 2009 | Yes | Yes | Unclear | Yes | Yes | No | Yes | Yes | Yes | Moderate | Minor concerns |
Confidence in the review findings
Based on our CERQual assessments, we had moderate confidence in five of our 15 findings and high confidence in eight of the findings, indicating that it is likely or highly likely that these findings are a reasonable representation of the phenomenon of interest. We had two findings where we had low confidence, indicating that it is possible that those are not a reasonable representation of the phenomenon of interest. Our explanation of the GRADE‐CERQual assessment for each review finding is shown in the Evidence Profiles (Appendix 2).
Review findings
Findings and categories identified in the data
Our findings described a range of factors that could influence the provision of home‐based rehabilitation, either through in‐person delivery or through telerehabilitation services. We used the CFIR framework to organise these findings into factors associated with (see Figure 3):
3.

Relationship between CFIR Framework and findings of this qualitative evidence synthesis
the characteristics of the intervention,
the inner setting and outer setting (i.e. features of both the implementing organisation and the external context or environment),
characteristics of individuals involved in implementation,
the implementation process (i.e. strategies or tactics that might influence implementation).
As we show in Figure 3, some findings refer simultaneously to the inner and outer settings because they have features of both the implementing organisation and the external context. The inner setting refers to the implementing organisation, which we defined in this review as the hospital or healthcare institution responsible for the rehabilitation services. The outer setting refers to the external context or environment, in which we included the patient’s home. The delivery of home‐based rehabilitation requires a continuum between the hospital or health institution and the patient’s home, and therefore there it is challenging to draw a clear line between the inner and outer settings in our findings.
We have presented the findings in two main categories. In the first category, we have presented findings that were common to both in‐person and telerehabilitation services. In the second category, we focus on those findings that were specific to telerehabilitation.
Unless specifically addressed in the detailed finding, the data were not specific to in high‐income country (HIC) or low‐ and middle‐income country LMIC) settings or to specific patient groups. For a description of the context and patients in each study contributing to a finding, please refer to Table 2 (Characteristics of included studies).
Category 1: Perceptions about rehabilitation services delivered at patients´ homes through in‐person encounters or via telerehabilitation
Finding 1. Patients and caregivers receiving and healthcare providers delivering telerehabilitation services perceived at least some in‐person home encounters as necessary. They felt that telerehabilitation services alone lost the rapport of social interaction and the opportunity to make meaningful connections. They also pointed out that some types of services provided with the hands could not be delivered using telerehabilitation (moderate‐confidence finding).
Despite generally positive perceptions about telerehabilitation, there were strong views from patients, caregivers and healthcare providers that telerehabilitation consultations cannot entirely negate the need or desire for in‐person encounters (Shulver 2016; Pekmezaris 2020). Healthcare providers, caregivers and patients that participated in telerehabilitation services argued that if the option is available, they would prefer at least one in‐person encounter, and if possible, more frequent opportunities to discuss experiences and challenges with these services (Hoaas 2016; Lawson 2020; O'Shea 2020; Brouns 2018; Damhus 2018; Gélinas‐Bronsard 2019). Some patients considered that in‐person follow‐up would maintain their motivation with the service (Palazzo 2016).
Patients, caregivers and healthcare providers did not perceive telerehabilitation as an appropriate substitute for human contact because they did not see it as providing meaningful connections (Brouns 2018; Hale Gallardo 2020; Ownsworth 2020; Shulver 2016; Saywell 2015; Van der Meer 2020). They argued that patients need in‐person home encounters with healthcare providers and benefit from peer contact in the rehabilitation setting (Brouns 2018; Dennett 2020). Other healthcare providers believed that it is essential to choose the right group of patients for telerehabilitation, and to be aware that this delivery mode is not suitable for all patients or situations (Damhus 2018).
Healthcare providers were concerned that rehabilitation services traditionally provided with the hands could not be delivered through this mode of rehabilitation delivery (e.g. some services provided by chiropractors, physical therapists, occupational therapists, and kinesiologists) (Hale Gallardo 2020; Shulver 2016).
Finding 2. Patients and healthcare providers described how in‐person home‐based rehabilitation and telerehabilitation encouraged patients' self‐management and made them feel empowered about the rehabilitation process. Patients become active contributors and shaped the process and its pace according to their needs. This was seen to facilitate the achievement of final results, whatever the goal that rehabilitation aimed to achieve (high‐confidence finding).
Patients described feeling empowered by the telerehabilitation services. Patients perceived that they could make their own decisions about the pace of their exercises, stop when tired or make more efforts when encouraged to accomplish a goal. In some studies, authors described a sense of self‐reflection among patients receiving telerehabilitation services, which seemed connected to having a better sense of control over their lives (Folan 2015; Hoaas 2016; Nordin 2017).
These feelings of empowerment and self‐reflection in patients seem to be related to having better access and control over their rehabilitation programs. Patients described how telerehabilitation platforms helped them to plan appointments and remember those appointments (Folan 2015; Ownsworth 2020), remember and check progress with exercises (Emmerson 2018; Ng 2013), share with family members and caregivers how to perform the exercises (Emmerson 2018), acquire more knowledge about self‐management of their condition (Sureshkumar 2016), register their symptoms (Argent 2018; Hoaas 2016), and decide when to push hard or take it easy according to their current condition (Bodker 2015; Hoaas 2016; Tsai 2016; O'Shea 2020; Van der Meer 2020). Patients who used wearable devices felt that tracking their own data and analysing their results was beneficial for their rehabilitation process (Argent 2018; Dinesen 2019; Shulver 2016; Dennett 2020; Pekmezaris 2020).
Caregivers that accessed platforms for telerehabilitation felt that those gave them more information and a clear understanding of the patient’s goals (Dinesen 2019). Some of them also suggested that improvements in patients' self‐efficacy could lead to a decrease in caregiver burden (Gélinas‐Bronsard 2019).
Similar feelings of empowerment and improved self‐management were highlighted in the in‐person home‐based rehabilitation studies (Dubouloz 2004). In‐person home‐based services helped patients feel that they had a normal life and feel less like a patient, and helped them to overcome their fears and to gain control over their bodies and their lives (Edbrooke 2020; Pinto 2014). In Pekmezaris 2020, patients who completed the in‐person home‐based program commented that they were able to see improvements from the exercise and use what they had learned outside of the program (Pekmezaris 2020).
Patients also mentioned that reciprocal interactions between patient and therapist, clear self‐training instructions and the establishment of clear goals, were important to a better understanding of the in‐person home‐based rehabilitation program. These factors also contributed to patients’ self‐confidence, motivation and persistence in training over time (Mohd Nordin 2014; Randstrom 2013; Turner 2011).
Finding 3. Patients and healthcare providers appreciated how in‐person home‐based rehabilitation or telerehabilitation improved patient outcomes related to independence, overall functioning at home, and everyday use of assistive devices, which are facilitated by the interaction with the home environment implicit in these types of services (low confidence finding).
Some patients and healthcare providers described how telerehabilitation services and in‐person home‐based rehabilitation led to an increase in patients´ daily physical activity levels, independence, and also gave them a sense of the importance of self‐care (Bodker 2015; Dennett 2020; Dubouloz 2004; Govender 2019; O'Shea 2020; Pinto 2014). One patient described the following: quote: “Even with obvious limitations, little‐by‐little, you gain control over your life again! No more depending on anybody. I was totally destroyed but now I’m so happy on a physical and mental level! I’m more motivated" (Pinto 2014). Patients perceived exercises as positive and meaningful if they led to improved performance or if the exercises were linked to a meaningful activity of daily life.
The authors of one study emphasised how in‐person home‐based rehabilitation could increase patient awareness of adopting a healthy behaviour, engage them in positive lifestyle changes, improve their diet, and increase their levels of exercise (Ranaldi 2018). Patients reported a greater understanding of their condition and of potential risk factors and said that the programme increased their understanding by addressing misconceptions and managing their expectations of recovery. Medication, exercise, and coping strategies were frequently referred to by patients as areas in which they felt their knowledge had improved (Ranaldi 2018).
For patients, assistive devices at home were also important to improving their independence. For instance, orthotics services and assistive devices for bathing, transfers from beds, personal indoor and outdoor mobility and transportation, wheelchairs, and walkers, were highly appreciated. Patients also recognized healthcare providers directly involved with the fitting of optimal assistive devices as important to promoting independence and facilitating patient participation in meaningful activities (Borade 2019; Govender 2019; Randström 2012).
Finding 4. Patients, caregivers and healthcare providers regarded the transition from the hospital to home as a challenging process given the lack of human and infrastructure resources available in the home setting. This may have an impact on the implementation of in‐person home‐based rehabilitation (moderate confidence finding).
The studies highlighted how the planning of in‐person home‐based rehabilitation programs may need to consider the challenges faced by patients, caregivers and healthcare providers in the transition from the hospital to home. Patients experienced a lack of follow‐up after being discharged from the hospital. As stated in Govender 2019, quote: "No one [in the hospital] prepared me to go home. When I was at home it was even harder for me because I was very weak at that time and none knew how to take care of me"’, another patient in the same study mentioned: quote: "After coming back from the hospital, I didn’t know how to do most things; my family did not know anything" (Govender 2019).
This view was shared by healthcare providers who stated that the transition from the hospital to the home environment created some challenges for patients and caregivers and for the rehabilitation process. These challenges were related to the gap between the human and infrastructure resources that were available to take care of people in hospitals and the lack of these resources in the home setting. When patients returned home, they faced challenges with the architecture of their homes, and also relied on caregivers without training (VanderVeen 2019).
In addition, the process of organising home or community support was not included within the discharge process and this responsibility was often left to patients or their caregivers (Turner 2011; VanderVeen 2019). This situation created difficulties for the continuity of services and delayed the start of the outpatient rehabilitation process (Turner 2011).
The continuity of rehabilitation services after discharge was also challenging where there were long distances between the hospital and the patients’ residence, and by the lack of communication between the healthcare provider at the institution and the home‐based or community‐based healthcare provider. This situation was stated by a healthcare provider in Malaysia as quote: “I agree; the continuity of the programme outside there [the hospital] is very lacking. I don’t know who monitors them or if they get improved in that way, maybe there’s continuity. So, hospital‐based, healthcare‐based, and then what…..?” (Mohd Nordin 2014).
Financial barriers were also mentioned as a challenge during this transition phase. Turner 2011 found that privately funded participants commonly experienced greater access to post‐discharge rehabilitation services, which meant more therapy with less time constraints (Turner 2011).
In contrast to these challenges, one study highlighted how well‐established follow‐up home rehabilitation programs were fundamental to the recovery of patients. HeydariKhayat 2020 described how a follow‐up rehabilitation program for burn survivors played a vital role in their recovery and improvement (HeydariKhayat 2020).
Finding 5. Patients and healthcare providers described several factors that might affect patients’ motivation and engagement with telerehabilitation services, including support from healthcare providers or family members and other caregivers during sessions, good communication with the healthcare provider, what the exercise required from the patient and their surroundings, and the presence of comorbidities (moderate confidence finding).
Maintenance of motivation was seen by patients as a highly relevant challenge in long‐term telerehabilitation services (Hoaas 2016). But even in short telerehabilitation services, patients felt that the support offered by healthcare providers in this delivery mode was insufficient or not humanized, disengaging them from the rehabilitation process\9 (Brouns 2018; Dennett 2020; Palazzo 2016; Saywell 2015). Healthcare providers noted that patients receiving telerehabilitation services might not be very accountable for doing the clinician's exercises. In Lawson 2020, a healthcare provider quoted: "I wondered if not having to prepare in advance to make the trip to an appointment meant that it was easier for it to slip their mind” (Lawson 2020). In contrast, other patients experienced the encouragement from the provider as particularly meaningful and felt motivated to stick to the therapy over the four‐week course. One of them said: “I’m the type of person who does things better when someone else is there and knows what he/she is doing and tells me what to do. Then I’ll do it. Sometimes I don’t have the, I wouldn’t say motivation, but, well, then I think: Just let it be. It’s not good, […] but that’s the way humans are” (Stark 2019).
Some patients described how they appreciated the support and encouragement they received from families and non‐professional coaches when rehabilitation was offered at home (Stark 2019; Randstrom 2013). The positive influence that family members had on the rehabilitation process of patients was also noted in long‐term care facilities (O'Doherty 2013). However, there were patients who reported that their caregivers had not given them the support they had hoped for. For example, in Stark 2019, one patient was somewhat disappointed as their family seemed not to understand the importance of the therapy and did not support them in the way they hoped for (Stark 2019).
Patients noted that good communication with the healthcare provider was a crucial factor for gaining confidence to continue with therapy. This included efforts to make sure that the instructions were clear to them as well as the provision of information and encouragement, (Edbrooke 2020; Vik 2009).
Patients described how telerehabilitation services had led to an increase in their daily physical activity levels (Bodker 2015; Dennett 2020; O'Shea 2020). However, some patients expressed that with long and intense sessions it was difficult to sustain concentration and very easy to lose motivation, mainly when their own expectations were not met (Folan 2015; Lawson 2020; O'Shea 2020; Stuifbergen 2011). Caregivers also described how they took too much responsibility for the rehabilitation process and pushed the patient too hard in relation to exercises (Dinesen 2019). In contrast, other patients expressed that if exercises were too easy, they did not see additional value in using a telerehabilitation application and might also lose motivation (Van der Meer 2020). Healthcare providers highlighted the importance of discussing expectations, real achievable goals of exercise and its potential benefits, particularly for those whose condition was deteriorating (Dennett 2020; Teriö 2019.
For some patients, their comorbidities and other conditions limited their progress and engagement in the rehabilitation process at home (Ranaldi 2018). In stroke patients, caregivers perceived it as difficult to motivate patients to use the affected arm more often in everyday life (Stark 2019).
Finally, for some patients, adherence and engagement to home rehabilitation were enhanced when the activities did not require an excessive amount of time, equipment or physical space and when they could be adapted to personal exercises routines like walking or running (Edbrooke 2020; Rizzo 2019).
Finding 6. Patients, caregivers, and providers described a number of privacy and confidentiality issues when services were provided at home. These included the increased privacy of being able to exercise at home but also the loss of privacy when elements of one’s home life were visible to others (high confidence finding).
Home‐based services, delivered either through in‐person visits or through telerehabilitation, allow healthcare providers to see inside patients’ homes. For some healthcare providers, older patients and their caregivers, the number of persons (or colleagues in the case of healthcare providers) providing rehabilitation services in the home created feelings of anxiety and discomfort (Randström 2012; Randstrom 2013; Randström 2014). In Randstrom 2013, a family caregiver described this as follows: quote: “There are so many people coming here, and there are always new ones. You feel like you have lost your home, even though I get out of the way when they come”.
Similar privacy issues were reported for telerehabilitation services. Healthcare providers were favourable to telerehabilitation services that allowed them to see into their patients' homes as this provided them with information about the environment where patients function that could be used to plan individualized services (Lawson 2020; Ownsworth 2020). Patients also preferred to exercise in the privacy and comfort of their own home, avoiding the stigma or embarrassment of exercising in front of others (Dennett 2020; Hoaas 2016; Pekmezaris 2020; Rietdijk 2020). In Dennett 2020, a patient described this as follows quote: "If I was doing it in a group session, I would be conscious of being clumsy and messing up and something like that. At least at home, I am more comfortable at doing it at my own pace and my own way and then monitoring it. So, I feel better doing it that way". However, other healthcare providers pointed out that group sessions could make elements of patients' personal lives visible to other participants (Bodker 2015), and suggested that privacy and confidentiality issues should be considered when planning these services (Brouns 2018; Gélinas‐Bronsard 2019; Ng 2013).
Patients receiving telerehabilitation services that used monitoring devices were also uncomfortable with the idea that these devices observed their movements and were concerned that this personal information could be sent to other people without their consent (Oyesanya 2019). Patients that received services that involved digital social networks expressed concerns about confidentiality and the subsequent consequences of sharing personal medical information (Palazzo 2016). However, other patients described devices as less intrusive than home visits and noted that these gave them more control over when to mute or switch off the camera (Ownsworth 2020).
Finding 7. Patients regarded in‐person home‐based rehabilitation and telerehabilitation services as convenient and less disruptive of everyday activities (high confidence finding).
In many studies, patients regarded telerehabilitation and in‐person home‐based rehabilitation services as suitable to their everyday routines and explained that exercises can be done anywhere (Dennett 2020; Malmberg 2018; Ownsworth 2020; Palmcrantz 2017; Pinto 2014; Tyagi 2018; Van der Meer 2020). Patients commented that they were able to perform and repeat those exercises that felt most effective as many times and at any moment that was convenient for them (Nordin 2017; O'Shea 2020; Tyagi 2018). Patients believed that homecare enabled them to receive the rehabilitation service with no disruption to their daily life processes (HeydariKhayat 2020; Pekmezaris 2020).
Patients felt more comfortable performing the exercises in their homes (Lawson 2020; Ownsworth 2020; Silveira 2019). They described how telerehabilitation reduces the fatigue associated with driving, and saved costs related to the journey and parking at the hospital (Govender 2019; Ownsworth 2020; Palmcrantz 2017; Shulver 2017; Tsai 2016). This last element was more relevant for patients with frequent appointments (Hale Gallardo 2020; Tsai 2016). In‐person home‐based rehabilitation was also considered as optimal for chronically ill patients who could not drive and depended on public transportation (Pinto 2014). It was also considered optimal for older people (Randström 2014), and for residents of distant rural areas. One patient expressed the following idea, quote: “It was really nice that you came to our place. On the one hand, coming to the hospital was a reminder of difficult days and on the other hand, my husband was working in the farm so he did not have enough time for follow‐up visits in the hospital” (Stark 2019).
Finding 8. Patients, caregivers, and healthcare providers called for more training in the context of in‐person home‐based rehabilitation (low confidence finding).
Patients mentioned that they and their caregivers required more training and information to better carry over the rehabilitation program during the transition from the hospital to the home or the community (Govender 2019; Schopfer 2020; VanderVeen 2019). Healthcare providers also called for better instructions, information and continued support for patients and their caregivers to prepare them for the transition to home. As noted by one healthcare provider quote: “They [the client and caregiver] hear: “It was a stroke”, and the next second they are home again. Caregivers are not included at all” (VanderVeen 2019). In the context of home‐based rehabilitation of older people, there is also a need for better information for patients and caregivers on how to perform the exercises and use assistive devices at home (Randstrom 2013).
In addition, patients, caregivers and healthcare providers mentioned the need for better training of nurses and residents of long‐term care facilities regarding home‐based rehabilitation services (O'Doherty 2013; Umb Carlsson 2019).
Category 2: Perceptions about rehabilitation services delivered at home through telerehabilitation
Finding 9. Healthcare providers highlighted the importance of personalising the service to each patient’s needs and resources at home (high confidence finding).
Healthcare providers highlighted the importance of conducting home visits as part of the planning of the telerehabilitation service (Shulver 2017). Other providers suggested that home visits might provide a good picture of the kinds of training that the patient can do at home (Bodker 2015).
Healthcare providers appreciated telerehabilitation services that allowed them to create personalised services based on patients' experiences, family interactions and individual needs (Lawson 2020). This included the value placed on having an easily accessed, portable and flexible individualized rehabilitation program (Bodker 2015; Damhus 2018; Dennett 2020; Silveira 2019). In Bodker 2015, one physiotherapist said the following: "Okay, at Margaret's, she has those challenges, and there is a coffee table there, so maybe she can't walk so much in the living room, but she has a dinner table where she can do stand‐up‐sit‐down exercises from".
Patients also expressed a feeling of confidence and enthusiasm with services or strategies that were specifically designed for their needs (Edbrooke 2020; Tsai 2016), as well as in using the resources in their own home to perform the exercises (Bodker 2015).
Healthcare providers pointed out that group sessions might not be suitable for patients who need a personalized plan and considered it necessary to assess whether an individual or group session fitted better with the patient's needs (Lawson 2020). Healthcare providers also highlighted the limitations that digital technologies placed on group interaction as only one participant can speak at a time. When two or more participants talk simultaneously, it is difficult to hear and understand what is happening, and health providers described how this led to frustration and disengagement (Bodker 2015; Ownsworth 2020).
Finding 10. Patients, caregivers, healthcare providers and other stakeholders described how telerehabilitation changed the nature of the patient‐provider relationship. This included overcoming physical barriers to communication and enabling quick responses to questions, creating a more relaxed environment for communication, and supporting shared decision‐making. Some patients described how telerehabilitation services allowed them to keep connected with their healthcare provider after being discharged from the hospital. However, other patients felt abandoned when receiving telerehabilitation services (high confidence finding).
In several studies, healthcare providers and patients described how telerehabilitation services could overcome physical barriers to participating in rehabilitation (Bodker 2015; Dinesen 2019; Hale Gallardo 2020; Lawson 2020; Nordin 2017). They described how telerehabilitation could facilitate communication with the clinician (Gélinas‐Bronsard 2019; Lawson 2020; Nordin 2017; Ownsworth 2020; Palmcrantz 2017; Shulver 2017; Tsai 2016). For example, in Lawson 2020, the study authors highlighted that for some healthcare providers, telerehabilitation sessions made them and their patients feel more relaxed than in‐person sessions. For example, a healthcare provider expressed the following, quote:: “[stroke survivors] probably felt a little bit more relaxed and comfortable because they were just logging in from their kitchen. It felt at times that it wasn’t as clinical as sitting opposite someone in a clinic room.” In studies where patients with aphasia were involved, they also expressed that telerehabilitation services improved their communication with the healthcare provider (Emmerson 2018; Kamwesiga 2017; Lawson 2020; Ownsworth 2020).
Patients, healthcare providers and policymakers highlighted that telerehabilitation can enable rapid contact between patient and healthcare provider, principally when digital platforms are available and patients can send messages, ask questions, or connect with the provider in case of questions (Bodker 2015; Gélinas‐Bronsard 2019; Malmberg 2018). In Gélinas‐Bronsard 2019, an occupational therapist also expressed that he could solve situations more quickly than following the route of an in‐person appointment: “sometimes we realize very quickly it could have been effectively solved remotely without an appointment. I give the example of an upside‐down cushion that can create a lot of discomfort”. These digital platforms allowed healthcare providers and policymakers to make quick decisions that could improve the rehabilitation process, prevent complaints reoccurring, and decrease treatment frequency and needs (Argent 2018; Bodker 2015; Gélinas‐Bronsard 2019; VanderVeen 2019).
Patients emphasised the importance of receiving feedback from healthcare providers about their rehabilitation progress and whether they were doing their exercises correctly (Argent 2018; Malmberg 2018; Palmcrantz 2017; Stuifbergen 2011). Some of the telerehabilitation services allowed for personalized or computerized feedback to patients Argent 2018; Palazzo 2016; Palmcrantz 2017), which was considered by patients as an essential advantage of this mode of rehabilitation delivery (Palmcrantz 2017; Van der Meer 2020). Healthcare providers perceived that telerehabilitation services gave more opportunities for shared decision‐making and shared responsibility about quality and safety with patients. This was not because they considered patients receiving telerehabilitation to be more qualified than patients receiving hospital‐based rehabilitation. Rather this was simply because shared responsibility became a pragmatic solution to the challenges emerging with the use of information technologies and remote connection, giving patients the opportunity to freely propose and discuss solutions (Bodker 2015; Nordin 2017). In Nordin 2017, a patient described this: “my own thinking about my situation was confirmed by the content in the web‐program (Web‐BCPA)”...this made me feel safe to share those thoughts (with the health care professionals) to acquire new knowledge that I can use in meetings with people that are involved in my rehabilitation...I was equipped with putting words on my thinking”. However, healthcare providers recognized that such shifting of tasks and responsibilities requires training as well as re‐calibration of skill sets between healthcare providers and patients and caregivers (Shulver 2017).
Patients who received telerehabilitation services after being discharged from a rehabilitation centre felt that continuing with a plan of exercises at home helped them feel less abandoned (Brouns 2018). This perception of having someone who was keeping an eye on them was also expressed by some patients who received only telerehabilitation services (Dennett 2020; Tsai 2016). However, for other patients who received telerehabilitation instead of in‐person rehabilitation, this delivery mode led to a feeling of abandonment (Palazzo 2016).
Finding 11. Healthcare providers and patients described some aspects of telerehabilitation services at home as challenging. Healthcare providers described problems in assessing patients, their environment, and whether they were performing exercises correctly. Providers and patients also emphasised the need for a quiet place during telerehabilitation sessions and described challenges tied to interruptions from family members (high confidence finding).
Healthcare providers delivering telerehabilitation services described challenges in assessing patients' immediate environments, for instance identifying whether furniture or other elements might represent a risk for falls (Ownsworth 2020). In several studies healthcare providers also described difficulties in seeing the whole patient's body and what he or she was doing, interpreting non‐verbal cues that give information about how the person is feeling physically or emotionally, and managing other problems or risks (Bodker 2015; Damhus 2018; Lawson 2020; Rietdijk 2020; Shulver 2017; Silveira 2019). In Bodker 2015, one healthcare provider described the following situation, quote: "if they move far enough away, so that we can see their whole body, well, then, we can't see their face. I'm thinking that I would rather see their face than I would see them falling off a chair five metres back in the room, because I couldn't see that they were feeling bad".
Additional challenges emerged when technical problems occurred, for example, if the screen froze, preventing them from assessing what the patient was doing (Tsai 2016). When patients are performing exercises, it is not easy to know if patients have the correct position or motion (Palazzo 2016); many times, healthcare providers have not had the opportunity of demonstrating the exercises to patients (Mendell 2019). Healthcare providers described how it was impossible to physically test muscle strength, gait, or balance in telerehabilitation (Argent 2018; Tyagi 2018).
Healthcare providers and patients highlighted the need for a quiet place in the home during telerehabilitation sessions. Interruptions and distractions created by family members in the background at the patient's home (Lawson 2020; Sureshkumar 2016), as well as patients that interrupted each other when speaking during online group rehabilitation sessions (Bodker 2015; Damhus 2018), were described as frequent challenges. Some healthcare providers suggested a planning meeting with patients and caregivers for explaining the optimal conditions for developing the telerehabilitation session (Ng 2013; Ownsworth 2020).
Finding 12. Patients, caregivers, healthcare providers and other stakeholders regarded telerehabilitation as an opportunity to make rehabilitation services more accessible (high confidence finding).
Patients, caregivers, healthcare providers, policymakers and IT engineers agreed that telerehabilitation services, including assistive, wearable, and mobile technology, represent new opportunities for healthcare delivery (Argent 2018; Dennett 2020; Emmerson 2018; Folan 2015; O'Shea 2020; Shulver 2017). Study authors explained that these opportunities are made possible by the fact that digital technology is becoming increasingly accessible, and many people use it on a regular basis (Argent 2018; Gélinas‐Bronsard 2019; Ownsworth 2020; Oyesanya 2019; Palazzo 2016; Van der Meer 2020). In addition, the study authors described how digital/technological rehabilitation software that was specifically designed for these specific populations had also improved access (Ownsworth 2020; Palmcrantz 2017).
Patients, caregivers, healthcare providers and other stakeholders pointed out that telerehabilitation can increase access to healthcare for patients in distant, rural, or underserved areas (Hoaas 2016; Lawson 2020; Malmberg 2018; Ownsworth 2020; Shulver 2017) and for patients with difficulties in attending in‐person rehabilitation centres (Damhus 2018; Hale Gallardo 2020; Rietdijk 2020; Tyagi 2018). In one study (Saywell 2015), which included the views of 15 patients who had experienced a stroke, participants described how the technology really helped with ‘‘keeping connected’’. Patients also noted that a program, including text messaging and phone contact and ensuring a very clear timetable of contact with the healthcare provider, could help the transition from acute care to living independently. In addition, such programs could reduce the shock and disappointment that frequently accompanies discharge from the hospital.
Finding 13. Healthcare providers and policymakers highlighted the need for adequate equipment, infrastructure and maintenance both on the provider side and the patient side but described how these needs were not always met. They described challenges including a lack of resources and investment, a lack of awareness around the resources needed, and rapid advances in technology that make technology quickly obsolete (moderate confidence finding).
Some authors emphasised how telerehabilitation is dependent on an infrastructure that requires financial investment and extensive and continuous maintenance (Bodker 2015). However, healthcare providers were concerned about the quality and range of the telerehabilitation infrastructure currently available to them and the limitations that this placed on what could be done via telehealth (Shulver 2017). Healthcare providers and policymakers had concerns regarding the lack of proper and sufficient equipment in healthcare institutions such as up‐to‐date computers and software, bandwidth capacity, and protections regarding the ensuing risk for security and confidentiality of data, especially with videoconferences (Brouns 2018; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Ownsworth 2020).
Other healthcare providers were concerned that part‐time clinicians or healthcare providers with a private practice might not have the appropriate space or the capacity to invest in adequate technology to provide telerehabilitation services (Hale Gallardo 2020). In Hale Gallardo 2020, one participant expressed these concerns as follows: "Most of the providers are not going to become full‐time tele‐rehab providers, so it is challenging to get space and equipment that can be used on a rotating basis". However, depending on the kind of telerehabilitation service provided, healthcare providers felt that they require fewer resources than in‐person sessions. The provider only needs a room and a computer (Lawson 2020).
Program coordinators believed that managers were unaware of the organisational and technological resources required (Ownsworth 2020). Others pointed out that lack of investment in infrastructure and maintenance could be one of the factors that explain why telecare often fails to make the provision of healthcare services more efficient and, hence, less costly (Bodker 2015). Healthcare providers also described how rapid and ongoing advances in technology could also pose challenges for maintaining effective telerehabilitation networks (Shulver 2017).
Healthcare providers and policymakers pointed out that to participate in telerehabilitation services, patients need appropriate equipment, enough bandwidth capacity in their home network, and devices and programs that are compatible with those used by healthcare providers (Brouns 2018; Hale Gallardo 2020; Ownsworth 2020; Palmcrantz 2017; Tyagi 2018).
Authors indicated that patients in rural or underserved areas might have the worst internet connectivity, or may not have any connectivity, which implies the provision of telerehabilitation through telephone or other strategies (Mendell 2019). In low‐income settings, patients and caregivers described high technology costs as a barrier, pointing out the necessity for low‐ or no‐cost technology (Oyesanya 2019; Van der Meer 2020). Other patients saw the use of tablets as impractical due to the risk of being robbed in public spaces (Teriö 2019). Still others described how they were unable to participate in the telerehabilitation session because another member of the family that was handling the phones travelled away, which also complicated follow‐up (Teriö 2019).
Finding 14. Patients and caregivers described many usability issues related to the device, the program or the application; they also emphasised the need for easy‐to‐use technologies that could be adapted to the patient’s individual needs. Patients and caregivers reported a lack of familiarity with, fear of or frustration with digital technology. Patients, caregivers, and healthcare providers called for more training and support in the use of these technologies (moderate confidence finding).
While patients and caregivers were generally enthusiastic about using the telerehabilitation technology, they highlighted many usability issues. Some issues were related to the device (Hoaas 2016; Palazzo 2016; Shulver 2016), others to the program or application (Brouns 2018; Hoaas 2016; Van der Meer 2020), and others to the interaction between a patient with a disability and the technology (Teriö 2019). Patients and caregivers gave great importance to devices and programs that were simple and easy to use and navigate and fit the needs of the patient (Brouns 2018; Malmberg 2018; Palazzo 2016). According to Argent 2018, the usability of any technology was associated with the patient's engagement and motivation to participate in telerehabilitation services (Argent 2018).
In many studies patients reported a lack of familiarity with digital technology in general, and with telerehabilitation technology specifically (Damhus 2018; Emmerson 2018; Gélinas‐Bronsard 2019; Hoaas 2016; Lawson 2020; Mendell 2019; O'Shea 2020; Ownsworth 2020; Shulver 2016; Van der Meer 2020). This meant that some patients relied on a caregiver or family member to help them with the telerehabilitation devices (Brouns 2018; Hale Gallardo 2020; Lawson 2020; Shulver 2017; Tyagi 2018).
Patients and caregivers of different ages expressed being afraid of using technology or felt anxious with the use of devices and programs (Emmerson 2018; Hale Gallardo 2020); some healthcare providers indicated that those feelings prevent patients to the use and success of the telerehabilitation service (Hale Gallardo 2020). However, some patients expressed that they were able to overcome their anxiety and get along with the telerehabilitation service (Emmerson 2018). For example, patients and caregivers described feelings of anxiety or frustration when they were not able to connect to the devices and therefore could not participate in the telerehabilitation session as planned (Damhus 2018; Folan 2015; Hoaas 2016; Ownsworth 2020; Stuifbergen 2011). As described by the authors in Folan 2015: "The word "frustrating" was commonly used to describe the challenges experienced. Other words were used such as "slow", "hate", "annoying" and "mind‐blowing" to describe their initial feelings towards computer use." Some healthcare providers reported that the time invested in solving problems with digital systems did not leave much room for the actual rehabilitation care of the patient or represented an extra workload (Brouns 2018; Damhus 2018; Gélinas‐Bronsard 2019; Ownsworth 2020; Van der Meer 2020). Problems related to IT systems and patients feelings of frustration sometimes discouraged them from participating in telerehabilitation services, even precluding this mode of delivery for some patients (Bodker 2015; Brouns 2018; Emmerson 2018; Folan 2015; Hoaas 2016; O'Shea 2020; Ownsworth 2020; Palmcrantz 2017; Stuifbergen 2011; Sureshkumar 2016; Tsai 2016). In Hoaas 2016 a patient said quote: "I had many difficulties during a videoconference with the physiotherapist. Sometimes we saw each other but could not speak. Sometimes we could speak, but we could not see each other. It has been a slight nightmare at times" (patient). Some caregivers also described frustrations with technology performance problems or connectivity problems (Ownsworth 2020).
For some healthcare providers, the problems with IT systems did not affect the performance or delivery of the service and were regarded as a minor problem easily solved (Lawson 2020; Rietdijk 2020; Tyagi 2018). Some healthcare providers suggested planning backups for appointments when IT system problems appear (Ownsworth 2020).
In several studies, patients and caregivers perceived that in order to feel sufficiently comfortable with the technology, they needed more support and information, and also sufficient time to practice these new technology skills (Folan 2015; Hoaas 2016; Palmcrantz 2017; Sureshkumar 2016; Teriö 2019; Tyagi 2018). Patients and healthcare providers proposed providing step‐by‐step guidelines (Ownsworth 2020), meetings to discuss optimal conditions for use (Ownsworth 2020), demonstrations (Stuifbergen 2011), a section of "Frequently Asked Question" (Van der Meer 2020), and video tutorials (Ownsworth 2020; Silveira 2019). Healthcare providers pointed out that it is crucial that they receive education and training to communicate and plan telerehabilitation services before performing in real‐time (Damhus 2018; Hale Gallardo 2020).
Finding 15. Healthcare providers differed in their views about whether telerehabilitation was cost‐efficient for them, but many patients encountered it as affordable and cost‐saving, when the equipment and infrastructure were provided by the health services, (high confidence finding).
Healthcare providers and program coordinators had varying views about the resources required for telerehabilitation services. Some healthcare providers felt that telerehabilitation required more time than in‐person sessions (Bodker 2015; Brouns 2018; Damhus 2018; Gélinas‐Bronsard 2019; Lawson 2020; Ownsworth 2020; Van der Meer 2020). Some healthcare providers explained that the administrative load of emailing patients ahead of appointments to set up telerehabilitation sessions required more organisation and resources and was less convenient than in‐person sessions (Lawson 2020). Others argued that problems with internet connections, speed, and issues with "lagging" or "drop‐out" led to concerns that the time spent on actual rehabilitation would instead be spent trying to guide patients through the technology and establish or re‐establish the connection during sessions (Damhus 2018; Ownsworth 2020). However, other healthcare providers felt that clinicians' administrative demands for in‐person and telerehabilitation sessions were comparable (Lawson 2020).
Some authors highlighted concerns regarding the investment in infrastructure and continuous maintenance and updating. As we explained in finding 13, this investment might be underestimated and affect the cost‐efficiency of this mode of rehabilitation delivery (Bodker 2015; Ownsworth 2020). Healthcare providers and other stakeholders (i.e. information technology specialists and rehabilitation managers) pointed out concerns about the capacity to invest in infrastructure and maintenance, which were more relevant in low‐ and middle‐income countries (Teriö 2019).
Patients and caregivers described telerehabilitation services as affordable and even cost‐saving. Some of them pointed out that they do not have to spend time or money on travel to the rehabilitation centre, paying for parking, or getting a replacement at work (Ownsworth 2020; Palmcrantz 2017; Shulver 2017; Tsai 2016; Tyagi 2018; Van der Meer 2020). However, if the health system did not provide the necessary technology or if was not already available in the patient's home, some patients and caregivers considered that purchasing devices or paying for application could be a barrier to effective use of telerehabilitation services (Oyesanya 2019; Van der Meer 2020).
Review author reflexivity
In keeping with quality standards for reflexivity within qualitative research, we maintained a reflexive stance throughout all stages of the review process, from study selection to data synthesis. Throughout the review process, we discussed with each other how our backgrounds and positions, views and beliefs could influence the choices we were making in terms of the scope of the review, our review methods, and our interpretation of the data.
Eleven members of the review team have clinical backgrounds in medicine, including specialists in rehabilitation (MV, LHL, AMP, LFM, SN, CK, KMC, MAS, ASR,IL); four have training and experience in qualitative research (MV, LHL, DP, CG); three (CG, IL, ASR) are researchers based at a rehabilitation hospital in Norway, three are researchers based at a rehabilitation hospital in Colombia (AMP, LFM, KMC), and two have experience in rehabilitation and health systems methodology and research (CK, SN). Our research team was composed of people with different types of exposure to the rehabilitation field and of people from both high‐ and middle‐income countries. We, therefore, have different experiences about the organisation, availability and accessibility of health services in general and rehabilitation in particular. However, all members of the review author team believe that people with disabilities should have equitable access to healthcare without discrimination.
At the beginning of this review process, some of the review authors had concerns about the use of digital health services because of challenges in implementing these in an equitable, reliable and sustainable manner. Some review authors also had questions about the extent to which home‐based rehabilitation could represent a sufficient substitute for in‐patient rehabilitation services. However, we also believed that home‐based rehabilitation and telerehabilitation had the potential to help people access appropriate healthcare during the COVID‐19 pandemic and in other circumstances where access to in‐patient services was challenging. One of the authors (SN) noted how, during the COVID‐19 lockdown in his country, he had become suddenly aware of the need for telerehabilitation to continue following up chronic outpatients (Negrini 2020d; Romano 2021) (please also see CN's CoI in the appropriate section of the declarations of interest).
Our concerns about the challenges of implementing telerehabilitation services, including the many technical challenges tied to usability and access, were confirmed in our review findings. However, our work on this review has also led us to recognise to a greater extent that home‐based services have features and advantages that in‐patient services may not be able to provide, and we increasingly view home‐based rehabilitation as more than simply a substitute for in‐patient services when these are unavailable.
Discussion
This review was conceived in response to the COVID‐19 pandemic and the need to explore alternative solutions where facility‐based services were suspended or severely limited. This situation has been part of a broader, global phenomenon where the pandemic has forced activities in all sectors of society to relocate to people’s homes. The findings in this review suggest, however, that home‐based services are not necessarily only a ‘second‐best’ solution. In fact, the findings point to several possible advantages. These include the potential for increased convenience, independence and empowerment for patients receiving services at home and for less disruption of everyday activities. In addition, the review suggests that telerehabilitation in particular has the potential to increase patient‐provider communication and shared decision‐making. At the same time, the review points to challenges, including privacy and confidentiality issues when providers have access to people’s homes, either digitally or in‐person. Home‐based telerehabilitation also brings with it a range of technical, usability and cost challenges for both providers and patients as well as challenges for providers attempting to assess patients through digital channels.
This review has increased our acknowledgement of home‐based care as a different type of service with its own advantages and disadvantages rather than a service driven primarily by necessity. This also reflects broader social discourses around the organisation of society post‐pandemic (Grundstein 2021) and an increasing realization that we may not want to return to pre‐pandemic circumstances. Instead, there is a growing interest in exploring how rehabilitation providers can maintain the advantages of home‐based activities including home‐based rehabilitation services while addressing the many challenges.
In the ‘Implications for practice’ section of this review, we have drawn on our review findings to suggest issues that programme planners and implementers could consider in order to help address some of these challenges with implementing home‐based rehabilitation services. This section also reiterates the needs and desires expressed by patients, family members and other caregivers and healthcare providers; including the need for more training, the importance of personalising services to each patient’s needs and resources in the home, and the need to prepare patients for the transition from institution‐based to home‐based care.
Agreements and disagreements with other studies or reviews
The review team identified two Cochrane qualitative evidence syntheses that had a similar scope to this review (Ames 2019; Odendaal 2020). Ames 2019 explored affecting patients’ and other healthcare users’ perceptions and experiences of targeted digital communication via mobile devices on topics related to reproductive, maternal, newborn, child, or adolescent health. Odendaal 2020 explored health workers' perceptions and experiences of using mHealth technologies to deliver primary healthcare services. The findings from these two reviews and our own review point to many of the same topics and we have highlighted two.
First, the reviews all suggest that digital services can influence the relationships of the people involved. In all three reviews, healthcare users, patients and providers describe how digital services change the nature of the patient‐provider relationship. Patients in our own review describe improved patient‐provider communication, while healthcare users in Ames 2019 refer to increased feelings of support and connectedness with providers, and providers in Odendaal 2020 state that communicating with patients by mobile phone has improved their relationships with patients. However, some patients in our own review also describe feelings of abandonment. In addition, providers and patients in our own review and providers in the Odendaal review argue that some patients need in‐person contact.
Similarly, both our own review and the Ames 2019 review suggest that these types of digital services can change the nature of the patient’s relationship with their families. Healthcare users in Ames 2019 describe how they share information from digital messages with family and friends while our own review points to the increased involvement of family when services are home‐based.
In Odendaal 2020, providers also describe the impact of digital health on the provider‐provider relationship. Some providers appreciate being more connected to colleagues and think this improves coordination and quality of care. However, others describe problems and prefer face‐to‐face contact with colleagues. This particular issue was not identified in our own review, probably because our focus was on the provision of home‐based rehabilitation rather than on communication between providers located in the community and the hospital.
A second topic identified by patients and providers in all three reviews is tied to internet access, access to functioning and affordable devices, and a need for training in the use of these digital systems. All of these are factors that might challenge or influence the provision of digital services.
We identified several reviews of intervention effectiveness that might complement this QES. Three of these reviews focused on telerehabilitation services for persons with multiple sclerosis (Khan 2015), patients with stroke (Laver 2020), and patients with chronic respiratory disease (Cox 2021), and were broadly similar in terms of population groups, type of rehabilitation, mode of delivery, setting, and publication date to our review.
Overall, these reviews found low‐certainty evidence that telerehabilitation leads to similar or better outcomes for these patient groups when compared to traditional in‐person, facility‐based rehabilitation services. This suggests that telerehabilitation is not inferior for patients with stroke (Laver 2020), or for patients with chronic respiratory disease (Cox 2021)
We also identified two effectiveness reviews addressing and comparing the provision of home‐based cardiac rehabilitation versus centre‐based (Anderson 2017), and another review comparing care home versus hospital and own home environments for rehabilitation of older people (Ward 2008). The Ward review had insufficient evidence to make any conclusions about the effectiveness of home‐based rehabilitation. However, the Anderson 2017 review found low‐certainty evidence that home‐based rehabilitation leads to similar outcomes as centre‐based care.
All the effectiveness reviews discussed here suggest that home‐based telerehabilitation and in‐person home‐based rehabilitations are suitable alternatives for the provision of rehabilitation services. However, the findings from our own and other qualitative evidence syntheses (Ames 2019; Odendaal 2020) suggest that the success of these services can be influenced by a range of implementation considerations. These considerations need to be taken into account by those making decisions regarding the provision of these services.
Overall completeness and applicability of the evidence and limitations of the evidence
In this review, we included 53 studies sampled from a group of 224 eligible studies. Twenty of the studies addressed in‐person home‐based rehabilitation, 28 of the studies addressed home‐based telerehabilitation services, and five of the studies addressed both in‐person home‐based rehabilitation and home‐based telerehabilitation services. We included the experiences and perceptions of patients, caregivers, healthcare providers and other stakeholders, covering different types of rehabilitation for a range of patients with different conditions, including elderly people and people with stroke, chronic obstructive pulmonary disease and cardiovascular diseases.
People’s views and experiences of home‐based services are likely to be influenced by whether these are their only alternatives or something they have chosen instead of in‐patient rehabilitation services. For instance, people who have actively chosen this option may be more likely to be positive towards it. In some studies, it was clear that the focus was on the provision of rehabilitation services in rural or underserved areas, where home‐based rehabilitation was likely to be the only alternative. However, most of the studies did not explain whether the services were provided instead of available in‐patient services or as a continuity of in‐patient services.
There are five main limitations to the evidence we have presented. First, we did not find studies that evaluated people’s experiences, perceptions and behaviours regarding home‐based rehabilitation in long‐term programmes. These could be important since many conditions that cause disability have a chronic evolution. Second, we did not identify studies about some health conditions, for example, Parkinson´s disease or amputations, although these are important conditions for rehabilitation interventions. Third, we did not find many studies from low‐ or middle‐income countries. It is possible that the availability and organisation of home‐based and facility‐based services in these settings are not comparable to those found in the settings of the studies included. Fourth, we decided not to search CINAHL database based the rationale that research focused on the nursing and allied health professions might be captured in the general search; however, it is possible that some relevant studies may have been missed. Finally, we were not able to translate six studies that are listed in the Studies awaiting classification section. However, we do not think this small number of studies would have important impacts on sampling or on the review findings.
Authors' conclusions
Implications for practice
Below are a set of questions that may help health system or programme managers when implementing or planning for home‐based services, delivered either face‐to‐face or through telerehabilitation. For an overview of the links between the review findings and these implications for practice, please see Appendix 3.
1. Have you considered who may benefit the most and opt for telerehabilitation and other home‐based services (including telerehabilitation)?
For instance, where there is a choice, have you considered offering these services to:
people who express a preference for home‐based services;
people with frequent appointments;
People who depend on public transportation;
people living in rural areas and remote areas
people who depend on a caregiver to transfer to an institution;
people with financial constraints.
2. Have you considered how you must organise home‐based services in a way that they can be adapted fully to suit each individual’s needs, accessibility, availability and home environment?
Are exercises adapted to the amount of time, equipment and space the patient has at home? For instance, does the patient have a quiet space to exercise without interruptions from other family members?
When considering providing telerehabilitation services, can you provide these services including at least one in‐person home visit where patients and providers can meet each other and where providers can assess the home environment and develop exercise programmes that are tailored to the individual’s situation and needs?
Before considering providing telerehabilitation services to a patient, have you discussed with them whether individual or group sessions fits their needs and preferences best?
Are the home‐based and telerehabilitation services more accessible for patients, caregivers and healthcare providers than outpatient services?
3. Have you considered how you can support patients’ motivation and ability to carry out their exercises at home?
Does the patient always receive clear instructions from the provider?
Does the patient receive encouragement from the provider and from family members and other caregivers?
Do the provider, patient and caregivers interact together to establish common expectations and goals?
Are providers able to ascertain that patients are performing exercises safely and correctly?
When considering providing telerehabilitation services, are providers able to monitor whether patients are performing exercises safely and correctly?
When considering providing telerehabilitation services, are there established procedures ready to be applied to support patients and providers when problems occur during sessions?
4. Have you used the advantages that home‐based rehabilitation services offer to give patients more control over their own rehabilitation?
Are the programs flexible? Do patients have a choice to select among the sessions and their frequency?
Can they plan their own appointments, access information about their condition and how to perform exercises, and track their own progress?
Can they easily involve family members and caregivers in the rehabilitation process?
5. Do you systematically plan the transition from hospital to home‐based rehabilitation to ensure continuity of care so as to ensure that the outpatient rehabilitation process is not delayed?
Is planning for this transition systematically included in the discharge process?
Are there well‐established channels of communication between hospital‐based healthcare providers and the community‐based providers delivering services in the home?
6. Do you have a realistic overview of the resources and costs home‐based services require?
Have you considered the amount of time required for administrative tasks such as setting up making appointments, travel and parking, and work absence?
When considering providing telerehabilitation, have you taken into account the amount of time required for introducing patients to the technology employed, the exercises to be performed, and establishing or re‐establishing connections during sessions?
When considering providing telerehabilitation, have you taken into account the initial costs of setting up the technology (including servers, computers, screens, mobile devices and other related technologies), as well as running costs for airtime, IT support, and maintenance of hardware and software?
When considering providing telerehabilitation, have you taken into account who will pay for patients’ computers, screens, or other devices, the maintenance and repairs?
7. Are systems in place to protect the privacy and confidentiality of patients and families when providers enter their homes, either in‐person or through digital devices?
For in‐person visits, can you limit the number of providers that visit the home to the minimum needed?
Can you ensure training of the providers in ethical, privacy and confidentiality issues, especially the do’s and dont’s?
Have you catered for the job description of the provider at home and provided the same to the patient and caregivers?
Is there a system for complaint reporting or redressal of grievances?
When considering providing telerehabilitation services, do patients have full control over muting or switching off their digital devices? And are there systems in place to ensure data privacy for information gathered through these devices?
8. For telerehabilitation services, do all patients, caregivers and providers have the necessary equipment, training and technical support?
Is the necessary infrastructure in place, both in the facility and in the home? This includes reliable internet connectivity, updated computers and software, and systems to repair or replace these when needed.
Do patients and providers have access to devices and programs that are easy to use and that can be tailored to the needs of the individual?
Do patients and providers have access to technical support when problems occur during sessions?
Have patients, caregivers and providers received sufficient training in the use of the relevant technologies and platforms? Patients and providers in this review suggest step‐by‐step guidelines, meetings to discuss optimal conditions for use, demonstrations, a section of "Frequently Asked Questions", and video tutorials.
Has this training been adapted to meet the individual’s digital skills?
Have providers received training in how to communicate and plan digital sessions?
Are patients specifically trained to practice with the equipment which will be used at home before the transition from hospital to home? Do they learn beforehand the exercises to be performed at home? Do they have sufficient time to practice before going home?
9. Have you considered how telerehabilitation must be used to improve the patient‐provider relationship and avoid the patient feeling abandoned?
For instance, does the system:
enable quick and easy contact between patient and provider, allowing patients and caregivers to send messages and ask questions that will be replied to quickly?
give patients the opportunity to share their thoughts, discuss solutions and reach shared decisions with the provider?
enable patients to communicate orally or audio‐visually with the rehabilitation professionals of the telerehabilitation providing centre?
allow the provider to give quick feedback to patients about their progress and whether they are doing their exercises correctly?
give patients and caregivers the opportunity to incorporate their preferences and views about how the telerehabilitation service can be improved?
give patients opportunities to interact with other patients?
Implications for future research
Researchers carrying out future qualitative and mixed‐methods research about factors that influence home‐based rehabilitation services should report their research methods transparently, particularly around participant recruitment strategies, data collection strategies and ethical issues. They should be more explicit about how their own values, experiences and opinions might have influenced their collection and interpretation of the data.
We need more primary research in low‐ and middle‐income settings that further examines the factors that we identify in our review. Most of the studies included in this review were conducted in high‐income settings, and it is possible that studies from low‐and‐middle‐income settings may change some of the findings, particularly those findings relating to the need for and availability of easy‐to‐use technologies, appropriate investment, adequate equipment, infrastructure, maintenance, training and support.
Our review points to a number of topics that future qualitative or mixed‐methods research could explore. This includes an assessment of how home‐based rehabilitation services are perceived when provided after finalizing in‐hospital rehabilitation (continuity of services) compared to services provided as a substitute for in‐hospital rehabilitation (alternative mode of delivery). In addition, this research could explore patients’ perceptions of home‐based services that are provided as the only available option, for instance, for patients in remote geographical areas as compared to patients in urban and well‐served regions that can attend in‐hospital services.
Future research could also assess health system factors that facilitate or hinder the transition from hospital to home‐based rehabilitation services, as well as the training and education needs of patients, caregivers, and providers when using telerehabilitation technologies and platforms. Future effectiveness research, including randomized trials, should explore if home‐based rehabilitation can maintain the same motivation and outcomes in the short and long terms as in‐patient rehabilitation. This review suggests that it is important to focus on outcomes such as empowerment, self‐management, independence, patients' control over their bodies and their lives, achieving healthier behaviours and lifestyles and improving the participation of people with disabilities.
Acknowledgements
We would like to acknowledge the contributions of Paola Andrea Ramírez for the support in designing and developing the searching of studies, as well as the contribution of Juan‐Carlos Velásquez for the support in data collection and data management.
Cochrane Effective Practice and Organisation of Care supported the authors in the development of this review.
The following people conducted the editorial process for this article.
Sign‐off Editor (final editorial decision): Simon Lewin, Norwegian University of Science and Technology;
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Elizabeth Paulsen, Norwegian Institute of Public Health;
Copy Editor (copy editing and production): Elizabeth Royle and the Copy Edit Support Team;
Peer‐reviewers (provided comments and recommended an editorial decision): Mira Palonen, Janet Bettger, and Rod Taylor (clinical/content review), Jane Noyes (methods review), Marit Johansen, Norwegian Institute of Public Health (search review).
When preparing this protocol/review, we used EPOC’s Protocol and Review Template for Qualitative Evidence Synthesis (Glenton C, Bohren MA, Downe S, Paulsen EJ, Lewin S, on behalf of Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Synthesis: Protocol and review template. Version 1.1. EPOC Resources for review authors. Oslo: Norwegian Institute of Public Health; 2020. Available at: https://zenodo.org/record/5973704#.Y0lx2XZBwuU.
Appendices
Appendix 1. Search strategies
Epistemonikos, Epistemonikos Foundation ‐ using Advanced search (searched 16 June 2022)
| Part 1. (Title) rehabilitation AND (Title/Abstract) "ambulatory care" OR "home care" OR outpatient AND (Title/Abstract) qualitative OR "Grounded Theory" OR "mixed methods" OR interview OR ethnography OR "case study" OR "content analysis" OR "participant observation" OR interpretative OR "participatory action" OR "thematic analysis" Part 2. (Title) rehabilitation AND (Title/Abstract) telemedicine OR ehealth OR mhealth OR internet OR web AND (Title/Abstract) qualitative OR "Grounded Theory" OR "mixed methods" OR interview OR ethnography OR "case study" OR "content analysis" OR "participant observation" OR interpretative OR "participatory action" OR "thematic analysis" Part 3 (Title/abstract) telerehabilitation AND (Title/Abstract) qualitative OR "Grounded Theory" OR "mixed methods" OR interview OR ethnography OR "case study" OR "content analysis" OR "participant observation" OR interpretative OR "participatory action" OR "thematic analysis" |
Health Systems Evidence, McMaster University (searched 22 July 2022)
rehabilitation AND telemedicine AND (qualitative OR "Grounded Theory" OR "participatory action")
No filters added
EBM Reviews, Ovid (searched 23 June 2022)
| 1 rehabilitation.de. or rehabilitation.ab. or rehabilitation.ti. (42931) 2 home.ab. or home.ti. or outpatient.ti. or outpatient.ab. or ambulatory care.de. or "ambulatory care".ab. or "ambulatory care".ti. (135062) 3 1 and 2 (6647) 4 qualitative.ab. or qualitative.ti. or "grounded theory".ti. or "grounded theory".ab. or Grounded Theory.de. or "mixed methods".ab. or "mixed methods".ti. or interview.ab. or interview.ti. or ethnography.ab. or ethnography.ti. or "case study".ab. or "case study".ti. or "content analysis".ab. or "content analysis".ti. or "participant observation".ab. or "participant observation".ti. or interpretat*.ab. or interpretat*.ti. or "participatory action".ab. or "participatory action".ti. or "thematic analysis".ab. or "thematic analysis".ti. or Qualitative Research.de. (170708) 5 3 and 4 (517) 6 telemedicine.ab. or telemedicine.ti. or telehealth.ti. or telehealth.ab. or telemedicine.de. or ehealth.ab. or ehealth.ti. or "Mobile Health".ab. or "Mobile Health".ti. or mhealth.ab. or mhealth.ti. or telecare.ab. or telecare.ti. or telenursing.ab. or telenursing.ti. or telemonitor*.ab. or telemonitor*.ti. or teleconsult*.ab. or teleconsult*.ti. or telecounsel*.ab. or telecounsel*.ti. or telecoach*.ab. or telecoach*.ti. or internet.ab. or internet.ti. or web.ab. or web.ti. (52824) 7 1 and 6 (1086) 8 4 and 7 (124) 9 5 or 8 (586) |
PubMed, NLM (searched 16 June 2022)
| ("rehabilitation"[Title/Abstract] AND ((("home"[Title/Abstract] OR "Outpatient"[Title/Abstract]) OR "ambulatory care"[Title/Abstract]) OR "out‐patient"[Title/Abstract])) AND (((((((((("qualitative"[Title/Abstract] OR "Grounded Theory"[Title/Abstract]) OR "mixed methods"[Title/Abstract]) OR "interview"[Title/Abstract]) OR "ethnography"[Title/Abstract]) OR "case stud*"[Title/Abstract]) OR "content analysis"[Title/Abstract]) OR "participant observation"[Title/Abstract]) OR "interpretat*"[Title/Abstract]) OR "participatory action"[Title/Abstract]) OR "thematic analysis"[Title/Abstract]) OR ((((((((((((((((((((("telemedicine"[MeSH Terms] OR "telemedicine"[Title/Abstract]) OR "telehealth"[Title/Abstract]) OR "ehealth"[Title/Abstract]) OR "e‐health"[Title/Abstract]) OR "Mobile Health"[Title/Abstract]) OR "mhealth"[Title/Abstract]) OR "m‐health"[Title/Abstract]) OR "telecare"[Title/Abstract]) OR "telenursing"[Title/Abstract]) OR "tele‐nursing"[Title/Abstract]) OR "telemonitor*"[Title/Abstract]) OR "tele monitor*"[Title/Abstract]) OR "teleconsult*"[Title/Abstract]) OR "tele consult*"[Title/Abstract]) OR "telecounsel*"[Title/Abstract]) OR "telecoach*"[Title/Abstract]) OR "tele coach*"[Title/Abstract]) OR "internet"[Title/Abstract]) OR "web"[Title/Abstract]) AND "rehabilitation"[Title/Abstract]) OR (((("telerehabilitation"[MeSH Terms] OR "telerehabilitation"[Title/Abstract]) OR "Tele‐rehabilitation"[Title/Abstract]) OR "virtual rehabilitation"[Title/Abstract]) OR "remote rehabilitation"[Title/Abstract])) AND ((((((((((((("Qualitative Research"[MeSH Terms] OR "qualitative"[Title/Abstract]) OR "Grounded Theory"[MeSH Terms]) OR "Grounded Theory"[Title/Abstract]) OR "mixed methods"[Title/Abstract]) OR "interview"[Title/Abstract]) OR "ethnography"[Title/Abstract]) OR "case stud*"[Title/Abstract]) OR "content analysis"[Title/Abstract]) OR "participant observation"[Title/Abstract]) OR "participatory action"[Title/Abstract]) OR "focus group"[Title/Abstract]) OR "interpretat*"[Title/Abstract]) OR "thematic analysis"[Title/Abstract]) |
Global Health, Ovid (searched 23 June 2022)
We used the same strategy as for EBM Reviews, Ovid
VHL Regional Portal, BIREME (including MedRxiv) (searched 16 June 2022)
| rehabilitation AND (home OR outpatient OR "ambulatory care" OR telerehabilitation OR telemedicine OR telehealth OR telecare OR ehealth OR mhealth OR telenursing OR internet OR web) AND (qualitative OR "Grounded Theory" OR "mixed methods" OR interview OR ethnography OR "case study" OR "content analysis" OR "participant observation" OR interpretative OR "participatory action" OR "thematic analysis") Limited to the following databases: "LILACS" OR "IBECS" OR "BDENF" OR "CUMED" OR INDEXPSI" OR "MedCarib" OR "MedRxiv" OR "BINACIS" OR "LIS" OR "PAHOIRIS" |
The following websites were searched using the terms: telemedicine, telerehabilitation, home‐based rehabilitation, home‐based care, e‐health, mobile health, telecare
United Nations, World Health Organization, European Association of Service providers for Persons with Disabilities, International Telecommunications Union, the Organization of American States,International Labour Organization, the International Federation of Red Cross and Red Crescent, International Committee of the Red Cross, United Nations Human Rights, Economic Commission for Latin American and the Caribbean, Economic and Social Commission for Asia and the Pacific, United Nations Office for the Coordination of Humanitarian Affairs, the United Nations Educational, Scientific and Cultural Organization, Economic and Social Commission for Western Asia, UNICEF, Human Rights Watch, International Covenant on Economic, Social and Cultural Rights.
Appendix 2. GRADE‐CERQual qualitative evidence profiles
[Enter text here]
| Finding 1. Patients and caregivers receiving and healthcare providers delivering telerehabilitation services perceived at least some in‐person home encounters as necessary. They felt that telerehabilitation services alone lost the rapport of social interaction and the opportunity to make meaningful connections. They also pointed out that some types of services provided with the hands could not be delivered using telerehabilitation. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns about the possibility of cognitive bias as the researchers were describing what they interpreted from interviews and focus groups with a lack of reflexivity on how their own values, experiences and opinions might have influenced their collection and interpretation of the data. |
| Coherence | No/Very minor concerns |
| Relevance | Minor concerns regarding relevance because all the studies were from high‐income settings; however, we consider that studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Brouns 2018; Damhus 2018; Dennett 2020; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; O'Shea 2020; Ownsworth 2020; Palazzo 2016; Pekmezaris 2020; Saywell 2015; Shulver 2016; Van der Meer 2020 | |
| Finding 2. Patients and healthcare providers described how in‐person home‐based rehabilitation and telerehabilitation encouraged patients' self‐management and made them feel empowered about the rehabilitation process. Patients become active contributors and shaped the process and its pace according to their needs. This was seen to facilitate the achievement of final results, whatever the goal that rehabilitation aimed to achieve. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns about the possibility of cognitive bias as the researchers were describing what they interpreted from interviews and focus groups with a lack of reflexivity on how their own values, experiences and opinions might have influenced their collection and interpretation of the data. |
| Coherence | No/Very minor concerns |
| Relevance | No/Very minor concerns |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | Minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and No/Very minor concerns regarding relevance |
| Contributing studies | |
| Argent 2018; Bodker 2015; Dennett 2020; Dinesen 2019; Dubouloz 2004; Edbrooke 2020; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hoaas 2016; Mohd Nordin 2014; Ng 2013; Nordin 2017; O'Shea 2020; Ownsworth 2020; Pekmezaris 2020; Pinto 2014; Ranaldi 2018; Randström 2012; Shulver 2016; Sureshkumar 2016; Tsai 2016; Turner 2011; Van der Meer 2020. | |
| Finding 3. Patients and healthcare providers appreciated how in‐person home‐based rehabilitation or telerehabilitation improved patient outcomes related to independence, overall functioning at home, and everyday use of assistive devices, which are facilitated by the interaction with the home environment implicit in these types of services. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | Serious concerns regarding coherence because it’s not clear if some of the underlying data support the review finding, specifically regarding the use of assistive devices. We have also concerns because many studies lack an explanation about how in‐person home‐based rehabilitation or telerehabilitation improves patients’ functioning and independence. |
| Relevance | Moderate concerns regarding relevance because all the studies were from high‐income settings; we consider that studies from low‐and‐middle‐income settings would change the finding regarding the use of assistive devices given that those are no easily accessible in those countries. |
| Adequacy | Moderate concerns regarding adequacy because of low richness and quantity of data supporting that in‐person home‐based rehabilitation and telerehabilitation improve the use of assistive devices. |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | No/Very minor concerns regarding methodological limitations, Serious concerns regarding coherence, Moderate concerns regarding adequacy, and Moderate concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Borade 2019; Dennett 2020; Dubouloz 2004; Govender 2019; O'Shea 2020; Pinto 2014; Randstrom 2013 | |
| Finding 4. Patients, caregivers and healthcare providers regarded the transition from the hospital to home as a challenging process given the lack of human and infrastructure resources available in the home setting. This may have an impact on the implementation of in‐person home‐based rehabilitation. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Moderate concerns about the possibility of cognitive bias as the researchers were describing what they interpreted from interviews and focus groups with lack of reflexivity on how their own values, experiences and opinions might have influenced their collection and interpretation of the data. |
| Coherence | Minor concerns regarding coherence because of contradictory findings between studies. Some studies might be describing challenges related to transitioning from in‐patient to out‐patient rehabilitation, and not particularly related to in‐person home‐based rehabilitation mode of service delivery. |
| Relevance | Minor concerns regarding relevance because all the studies were from high‐income settings; however, we consider that studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Moderate concerns regarding methodological limitations, Minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Govender 2019; HeydariKhayat 2020; Mohd Nordin 2014; Turner 2011; VanderVeen 2019 | |
| Finding 5. Patients and healthcare providers described several factors that might affect patients’ motivation and engagement with telerehabilitation services, including support from healthcare providers or family members and other caregivers during sessions, good communication with the healthcare provider, what the exercise required from the patient and their surroundings, and the presence of comorbidities. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | Moderate concerns regarding coherence because of contradictory findings between studies. |
| Relevance | Minor concerns regarding relevance because 19/20 studies were from high‐income settings; however, we consider that studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | No/Very minor concerns regarding methodological limitations, Moderate concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Brouns 2018; Dennett 2020; Dinesen 2019; Edbrooke 2020; Folan 2015; Hoaas 2016; Lawson 2020; O'Doherty 2013; O'Shea 2020; Palazzo 2016; Ranaldi 2018; Randström 2014; Saywell 2015; Stark 2019; Stuifbergen 2011; Teriö 2019; Van der Meer 2020; Vik 2009 | |
| Finding 6. Patients, caregivers, and providers described a number of privacy and confidentiality issues when services were provided at home. These included the increased privacy of being able to exercise at home but also the loss of privacy when elements of one’s home life were visible to others. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Minor concerns regarding relevance because all studies were from high‐income settings; however, we consider that studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, Minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Brouns 2018; Dennett 2020; Gélinas‐Bronsard 2019; Hoaas 2016; Lawson 2020; Ng 2013; Ownsworth 2020; Oyesanya 2019; Palazzo 2016; Pekmezaris 2020; Randström 2012; Randstrom 2013; Randström 2014; Rietdijk 2020 | |
| Finding 7. Many patients regarded in‐person home‐based rehabilitation and telerehabilitation services as convenient and less disruptive of everyday activities. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | No/Very minor concerns |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and No/Very minor concerns regarding relevance |
| Contributing studies | |
| Govender 2019; Hale Gallardo 2020; HeydariKhayat 2020; Lawson 2020; Ownsworth 2020; Palmcrantz 2017; Pekmezaris 2020; Pinto 2014; Randström 2012; Randstrom 2013; Shulver 2017; Silveira 2019; Stark 2019; Tsai 2016; Tyagi 2018; Van der Meer 2020 | |
| Finding 8. Patients, caregivers, and healthcare providers called for more training in the context of in‐person home‐based rehabilitation. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | Minor concerns regarding coherence because there are differences about needs of training |
| Relevance | Moderate concerns regarding relevance because 5/6 studies were from high‐income settings and not all primary studies supported the finding. |
| Adequacy | Serious concerns about adequacy due to thin data from a small number of studies. |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | No/Very minor concerns regarding methodological limitations, Minor concerns regarding coherence, Serious concerns regarding adequacy, and Moderate concerns regarding relevance |
| Contributing studies | |
| Govender 2019; O'Doherty 2013; Randström 2014; Schopfer 2020; Umb Carlsson 2019; VanderVeen 2019 | |
| Finding 9. Healthcare providers highlighted the importance to personalise the service to each patient's needs and resource at home. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Minor concerns regarding relevance because all studies were from high‐income settings; however, we consider that more studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Damhus 2018; Dennett 2020; Edbrooke 2020; Lawson 2020; Ownsworth 2020; Shulver 2017; Silveira 2019; Tsai 2016 | |
| Finding 10. Patients, caregivers, healthcare providers and other stakeholders described how telerehabilitation changed the nature of the patient‐provider relationship. This included overcoming physical barriers to communication and enabling quick responses to questions, creating a more relaxed environment for communication, and supporting shared decision making. Some patients described how telerehabilitation services allowed them to keep connected with their healthcare provider after being discharged from the hospital. However, other patients felt abandoned when receiving telerehabilitation services. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns regarding methodological limitations because possibility of cognitive bias as the researchers were describing what they interpreted from interviews and focus groups with lack of reflexivity on how their own values, experiences and opinions might have influenced their collection and interpretation of the data. |
| Coherence | No/Very minor concerns |
| Relevance | Minor concerns regarding relevance because 18/19 studies were from high‐income settings; however, we consider that studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence |
Explanation: Minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Argent 2018; Bodker 2015; Brouns 2018; Dennett 2020; Dinesen 2019; Emmerson 2018; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Kamwesiga 2017; Lawson 2020; Malmberg 2018; Nordin 2017; Ownsworth 2020; Palazzo 2016; Palmcrantz 2017; Shulver 2017; Stuifbergen 2011; Tsai 2016; Van der Meer 2020 | |
| Finding 11. Healthcare providers and patients described as challenging some conditions for delivering telerehabilitation services at home, such as ensuring that patients have a safe environment, the need for a quiet place for performing the telerehabilitation session, ensuring that patient performed exercises correctly and challenges tied to interruptions from family members. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Minor concerns regarding relevance because 12/13 studies were from high‐income settings; however, we consider that more studies from low‐and‐middle‐income settings would not substantially change the finding. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Minor concerns regarding relevance |
| Contributing studies | |
| Argent 2018; Bodker 2015; Damhus 2018; Lawson 2020; Mendell 2019; Ownsworth 2020; Palazzo 2016; Rietdijk 2020; Shulver 2017; Silveira 2019; Sureshkumar 2016; Tsai 2016; Tyagi 2018 | |
| Finding 12. Patients, caregivers, healthcare providers and other stakeholders regarded telerehabilitation as an opportunity to make rehabilitation services more accessible. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | No/Very minor concerns |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence |
No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and No/Very minor concerns regarding relevance |
| Contributing studies | |
| Argent 2018; Brouns 2018; Damhus 2018; Dennett 2020; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; Malmberg 2018; O'Shea 2020; Ownsworth 2020; Oyesanya 2019; Palmcrantz 2017; Rietdijk 2020; Saywell 2015; Shulver 2017; Tyagi 2018; Van der Meer 2020 | |
| Finding 13. Healthcare providers and decision‐makers highlighted the need for adequate equipment, infrastructure and maintenance, but described how these needs were not always met. They described challenges including a lack of investment, a lack of awareness around the resources needed, and rapid advances in technology that make technology rapidly obsolete. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Moderate concerns regarding relevance because 12/13 studies were from high‐income settings, and is likely that in low‐ and middle‐income settings needs for infrastructure are an important barrier for providing telerehabilitation services. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence |
No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Moderate concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Brouns 2018; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Lawson 2020; Mendell 2019; Ownsworth 2020; Oyesanya 2019; Palmcrantz 2017; Shulver 2016; Teriö 2019; Tyagi 2018; Van der Meer 2020 | |
| Finding 14. Patients and caregivers described many usability issues related to the device, the program or the application; they also emphasised the need for easy‐to‐use technologies that could be adapted to the patient’s individual needs. Patients and caregivers reported a lack of familiarity with, fear of or frustration with digital technology. Patients, caregivers, and healthcare providers called for more training and support in the use of these technologies. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Moderate concerns regarding relevance because 24/26 studies were from high‐income settings. It is likely that in low‐ and middle‐income settings the lack of technology and devices´ availability is a challenge. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence |
No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Moderate concerns regarding relevance. |
| Contributing studies | |
| Argent 2018; Bodker 2015; Brouns 2018; Damhus 2018; Emmerson 2018; Folan 2015; Gélinas‐Bronsard 2019; Hale Gallardo 2020; Hoaas 2016; Lawson 2020; Malmberg 2018; Mendell 2019; O'Shea 2020; Ownsworth 2020; Palazzo 2016; Palmcrantz 2017; Rietdijk 2020; Shulver 2016; Shulver 2017; Silveira 2019; Stuifbergen 2011; Sureshkumar 2016; Teriö 2019; Tsai 2016; Tyagi 2018; Van der Meer 2020 | |
| Finding 15. Healthcare providers differed in their views about whether telerehabilitation was cost‐efficient for them, but many patients encountered it as affordable and cost‐saving when the equipment and infrastructure have been provided. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | No/Very minor concerns |
| Coherence | No/Very minor concerns |
| Relevance | Moderate concerns regarding relevance because all the studies were from high‐income settings. It is likely that experiences in low‐ and middle‐income settings are different. |
| Adequacy | No/Very minor concerns |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence |
No/Very minor concerns regarding methodological limitations, No/Very minor concerns regarding coherence, No/Very minor concerns regarding adequacy, and Moderate concerns regarding relevance |
| Contributing studies | |
| Bodker 2015; Brouns 2018; Damhus 2018; Gélinas‐Bronsard 2019; Lawson 2020; Ownsworth 2020; Van der Meer 2020 | |
Appendix 3. Moving from the review findings to implications for practice
| Synthesis finding | Implications for practice (IP) |
| Finding 1. Patients, caregivers and healthcare providers receiving telerehabilitation services perceived at least some in‐person home encounters as necessary. They felt that telerehabilitation services alone lost the rapport of social interaction and the opportunity to make meaningful connections and also pointed out that some types of services provided with the hands were not eligible for telerehabilitation (moderate‐confidence finding). | Have you considered how you can adapt home based services to suit each individual’s needs and their home environments?
|
| Finding 2. Patients and healthcare providers described how in‐person home‐based rehabilitation and telerehabilitation encouraged patients' self‐management and made them feel empowered about the rehabilitation process. In telerehabilitation, those feelings were related to having better access and control over the rehabilitation program. In the in‐person home‐based programs, those feelings were related to achieving a normal life, gaining control over their lives and having reciprocal interactions between patient and health care provider (high‐confidence finding). | Have you used the opportunities that home‐based rehabilitation services offer to give patients more control over their own rehabilitation? For instance:
|
| Finding 3. Patients and healthcare providers appreciated how in‐person home‐based rehabilitation or telerehabilitation improved patients’ functioning, independence and the use of assistive devices (low‐confidence finding). | Have patients’ options for improve functioning and independence when providing services in‐person home‐based rehabilitation considered? |
| Finding 4. Patients, caregivers and healthcare providers regarded the transition from the hospital to home as a challenging process given the lack of human and infrastructure resources available in the home setting. This may have an impact on the implementation of in‐person home‐based rehabilitation (moderate‐confidence finding). | Have you planned the transition from hospital to home‐based rehabilitation to ensure continuity of care and ensure that the outpatient rehabilitation process is not delayed? For instance:
|
| Finding 5. Patients and healthcare providers described several factors that might affect patients’ motivation and engagement with telerehabilitation services, including support from healthcare providers or family members and other caregivers during sessions, good communication with the healthcare provider, what the exercise required from the patient and their surroundings, and the presence of comorbidities (moderate‐confidence finding). | Have you considered how you can support patients’ motivation and ability to carry out their exercises at home?
Have you considered how you can adapt home‐based services to suit each individual’s needs and their home environments?
For telerehabilitation services, do both patients, caregivers and providers have the necessary equipment, training and support?
|
| Finding 6. Patients, caregivers, and providers described a number of privacy and confidentiality issues when services were provided at home. These included the increased privacy of being able to exercise at home but also the loss of privacy when elements of one’s home life was visible to others (high confidence finding). | Are systems in place to protect the privacy and confidentiality of patients and families when providers enter their homes, either in‐person or through digital devices? For instance:
|
| Finding 7. Patients regarded telerehabilitation and in‐person home‐based rehabilitation services as convenient and less disruptive of everyday activities (high confidence finding). | Have you considered who may benefit the most and who may prefer telerehabilitation and other home‐based services? services? For instance, where this a choice have you considered offering these services to:
|
| Finding 8. Patients, caregivers, and healthcare providers called for more training in the context of in‐person home‐based rehabilitation (low confidence finding). | For telerehabilitation services, do both patients, caregivers and providers have the necessary equipment, training and support?
|
| Finding 9. Healthcare providers highlighted the importance of personalising the service to each patient’s needs and resources at home (high confidence finding). | Have you considered how you can adapt home based services to suit each individual’s needs and their home environments?
|
| Finding 10. Patients, caregivers, healthcare providers and other stakeholders described how telerehabilitation changed the nature of the patient‐provider relationship. This included overcoming physical barriers to communication and enabling quick responses to questions, creating a more relaxed environment for communication, and supporting shared decision making. Some patients described how telerehabilitation services allowed them to keep connected with their healthcare provider after being discharged from the hospital. However, other patients felt abandoned when receiving telerehabilitation services (high confidence finding). | Have you considered how telerehabilitation can be used to improve the patient‐provider relationship and can avoid the patient feeling abandoned? For instance, does the system:
|
| Finding 11. Healthcare providers and patients described some aspects of telerehabilitation services at home as challenging. Healthcare providers described problems in assessing patients, their environment, and whether they were performing exercises correctly. Providers and patients also emphasised the need for a quiet place during telerehabilitation sessions and described challenges tied to interruptions from family members (high confidence finding). | Have you considered how you can adapt home‐based services to suit each individual’s needs and their home environments?
|
| Finding 12. Patients, caregivers, healthcare providers and other stakeholders regarded telerehabilitation as an opportunity to make rehabilitation services more accessible (high confidence finding). | |
| Finding 13. Healthcare providers and policymakers highlighted the need for adequate equipment, infrastructure and maintenance both on the provider side and the patient side but described how these needs were not always met. They described challenges including a lack of investment, a lack of awareness around the resources needed, and rapid advances in technology that make technology rapidly obsolete (moderate confidence finding). | For telerehabilitation services, do both patients, caregivers and providers have the necessary equipment, training and support?
|
| Finding 14. Patients and caregivers described many usability issues related to the device, the program or the application; they also emphasised the need for easy‐to‐use technologies that could be adapted to the patient’s individual needs. Patients and caregivers reported a lack of familiarity with, fear of or frustration with digital technology. Patients, caregivers, and healthcare providers called for more training and support in the use of these technologies (moderate confidence finding). | For telerehabilitation services, do both patients, caregivers and providers have the necessary equipment, training and support?
|
| Finding 15. Healthcare providers differed in their views about whether telerehabilitation was cost‐efficient for them, but many patients encountered it as affordable and cost‐saving when the equipment and infrastructure have been provided (high confidence finding). | Do you have a realistic overview of the resources and costs home‐based services may require?
|
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alary Gauvreau 2019.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To describe the components and evaluate a Communities of practice (CoPs) for speech‐language pathologists about participation and aphasia rehabilitation" | |
| participant´s description | Thirteen speech‐language pathologists | |
| Health condition | Aphasia | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Recordings and logbooks/ Thematic analysis and interpretation of descriptive statistics | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Ando 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To examine the experiences of using telemonitoring in patients with MND (motor neurone disease) on noninvasive ventilation (NIV)" | |
| participant´s description | Seven patients with MND and five caregivers | |
| Health condition | Motor neurone disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Argent 2018.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | Quote: "To perform an exploration of the opportunities and challenges of using wearable technology in rehabilitation after joint replacement surgery. Following this, clinicians were provided with a demonstration of an exemplar wearable exercise biofeedback system, and their perceptions of its potential use in the clinical setting were evaluated while incorporating the healthcare professional in the user‐centred design process" | |
| participant´s description | Ten clinicians from a multidisciplinary team of healthcare professionals, including four physiotherapists, two clinical nurse specialists, two orthopaedic assistants, one occupational therapist and one staff nurse, from a hospital in Dublin | |
| Health condition | Joint replacement | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis with a grounded‐theory approach | |
| Funding sources for the study / Conflict of interest | Quote: "This project forms part of the CHESS (Connected Health Early Stage Researcher Support System) Innovation Training Network and has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska‐Curie grant agreement no. 67620" Quote: "Competing interests: None declared" |
|
| Notes | Study purposively sampled | |
Banner 2015.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "This paper examines the qualitative findings from a 16‐month mixed methods randomized controlled trial examining the impact of a virtual CRP (vCRP)" | |
| participant´s description | Twenty‐two adults in‐patients with acute coronary syndrome or following a revascularization procedure from two rurally located hospitals | |
| Health condition | Acute Coronary Syndrome | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Barclay 2020.
| Study characteristics | ||
| Country / Income of the Country | Australia, USA, Canada, New Zealand, UK, Sweden and Norway (HICs) | |
| Objective of study | Quote: "To describe and compare models of service delivery intended to support community integration in the immediate period following inpatient rehabilitation for SCI, and describe the characteristics of these models or approaches" | |
| participant´s description | Ten managers of spinal services: two from USA, two from Canada, two from Australia, one from each of New Zealand, UK, Sweden and Norway | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Open‐ended and semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Bendelin 2018.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To describe how chronic pain patients work in an Internet‐delivered cognitive behavioraltherapy (ICBT) program, through their descriptions of what is important when they initiate behavior change in aftercare and their descriptions of what is important for ongoing practice of selfmanagement skills in aftercare" | |
| participant´s description | Twenty‐nine patients | |
| Health condition | Chronic pain | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ patient´s written diaries/ Latent content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Birkeland 2017.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To elucidate how the interdisciplinary collaboration in reablement worked in a Norwegian context" | |
| participant´s description | Thirty‐three healthcare providers (nine physiotherapists, nine nurses, seven occupational therapists, four social educators, three auxiliary nurses and one social worker) from seven municipalities | |
| Health condition | NA | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups interviews/ Hermeneutic approach | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Bodker 2015.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"Telecare promises to deliver healthcare services more efficiently while, at the same time, improving the quality of care. The purpose of this paper is to challenge these promises by analysing the implications of introducing telecare in the rehabilitation of patients suffering from chronic obstructive pulmonary disease" | |
| participant´s description | Eleven patients with Chronic Obstructive Pulmonary Disease (COPD) and the therapist of the programme (managing nurse and the physiotherapist) from a Danish hospital | |
| Health condition | COPD | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Respiratory and in ativities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Ethnographic study/ Observations and semi‐structured interviews/ Analytical concepts developed within STS (Science and Technology Studies) | |
| Funding sources for the study / Conflict of interest | "No information on funding provided" Quote: "No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Boland 2018.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote: "To identify the Adaptive equipment that people typically use after a stroke and the outcomes achieved as a result, and to explore people’s experiences obtaining and using Adaptive equipment, to inform both practice and policy in this field." | |
| participant´s description | Two hundred and fifty‐eight people responded to the initial questionnaire. A sampling of respondents were interviewed | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Postal questionnaire followed by semi‐structured interviews/ Grounded theory | |
| Funding sources for the study / Conflict of interest | Not sampled | |
| Notes | This study was eligible but not sampled given that the data werenot as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Booth 2007.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To identify the factors influencing participation and outline the benefits and challenges of providing transitional rehabilitation for people with spinal cord injury (SCI) from rural and regional locations." | |
| participant´s description | Records of 40 patients | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Grounded Theory/ Program records and policy and service documents/ Open and axial coding | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Borade 2019.
| Study characteristics | ||
| Country / Income of the Country | India (LMIC) | |
| Objective of study | Quote: "To gain insight into the lived experiences of people using assistive devices with specific reference to mobility related disability in India" | |
| participant´s description | Twenty‐five individuals having mobility related disabilities, who used one or more ads for minimum 48 weeks | |
| Health condition | Mobility restriction | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative inquiry design/ Qualitative interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: "No information on funding provided" Quote: ''No potential conflict of interest was reported by the authors'' |
|
| Notes | Study purposively sampled | |
Brennan 2020.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | Quote: "To explore the experiences and unmet needs of women during home rehabilitation following surgery for breast cancer and to gather survivors’ perspectives on and requirements from mHealth technology for postoperative breast cancer rehabilitation." | |
| participant´s description | Ten women | |
| Health condition | Breast Cancer Surgery | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Brewer 2017.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To assess the feasibility and acceptability of a VW‐based CR program as an extension to medical center‐based CR. Our goal is to apply the study results toward the design of a patient‐centered VW platform prototype with high usability, understandability, and credibility" | |
| participant´s description | Patients recently enrolled in outpatient Cardiovascular Rehabilitation | |
| Health condition | Acute coronary syndrome (ACS), heart valve replacement, elective percutaneous coronary intervention (PCI), and stable angina | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed method/ Survey through both closed and open‐ended questions/ Ethnomethodology and structural narrative analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Brouns 2018.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Acute coronary syndrome (ACS),"To explore which factors influence the uptake of eRehabilitation in stroke rehabilitation, among stroke patients, informal caregivers, and healthcare professionals" | |
| participant´s description | Thirty‐two patients, fifteen informal caregivers, and13 healthcare professionals (physiotherapists, psychologists, occupational therapists, speech therapists, physicians, and managers) | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''Stichting Innovatie Alliantie supported this project financially (Grant 2014‐046PRO)'' Quote:''The authors declare that they have no competing interests'' |
|
| Notes | Study purposively sampled | |
Buimer 2017.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To explore the determinants of patient adherence to a blended care rehabilitation program, which includes a Web portal, from a patient's perspective." | |
| participant´s description | Twelve patients participated in interviews. Furthermore, portal usage data was analyzed of 31 patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Burkow 2015.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To assess patient acceptability of the delivery mode and components of a comprehensive pulmonary rehabilitation programme for any stage of COPD, as well as the technology usability, patient outcomes and economic aspects." | |
| participant´s description | Ten patients | |
| Health condition | Chronic obstructive pulmonary disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Mixed method/ Semi‐structured interviews/ Descriptive interpretation | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Caughlin 2020.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To summarize the facilitators and barriers to the implementation oftelerehabilitation services within a research context." | |
| participant´s description | Other stakeholders (researchers) | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Narrative review/ Interviews/ Descriptive | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Chen 2019a.
| Study characteristics | ||
| Country / Income of the Country | China (LMIC) | |
| Objective of study | Quote:"to assess the efficacy, safety, and acceptability of the addition of the BESMILE‐HF program to usual medications for patients with chronic heart failure". | |
| participant´s description | Aged 18 years or above, diagnosed with chronic heart failure, Clinically stable, defined as symptoms/signs that have remained generally unchanged for ≥ 1 month | |
| Health condition | Chronic heart failure | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Chen 2019b.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | " To investigate patient perceived benefits of and barriers to using the telerehabilitation system at home" | |
| participant´s description | Thirteen patients with stroke who were enrolled in a clinical trial of arm motor rehabilitation therapy | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Cherry 2017.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To determine participants’ general impressions about the benefits and barriers of using robotic therapy devices for inhome rehabilitation." | |
| participant´s description | Ten patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Ethnographic/ Direct observation of the in‐home environment and in‐depth semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Choularia 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To explore the perspectives of healthcare professionals and commissioners working with a stroke Early Supported Discharge service" | |
| participant´s description | Thirty‐five key informants including practitioners, managers and commissioners | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Cross‐sectional qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Clark 2013.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To evaluate the feasibility and utility of an Internet‐based, electronic Outpatient Cardiac Rehabilitation (eOCR) program in rural primary care." | |
| participant´s description | Sixteen health professionals (cardiologists, general practitioners, nurses and allied health) and 24 patients participated in the project | |
| Health condition | Cardiac disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Pilot study used a mixed methods design | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Cobley 2013.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To investigate patients’ and carers’ experiences of Early Supported Discharge services and inform future Early Supported Discharge service development and provision" | |
| participant´s description | Twenty‐seven stroke patients and fifteen15 carers in the Nottinghamshire region | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Constantinescu 2017.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To identify self‐reported factors that influence adherence to conventional home therapy without a mobile device in HNC patients" | |
| participant´s description | Ten patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Conti 2015.
| Study characteristics | ||
| Country / Income of the Country | Italy (HIC) | |
| Objective of study | Quote:"To explore the situation of informal caregivers of persons with SCI when discharged home from a SCI Unit, in relation to needs, emotional experiences, difficulties and subsequent reactions to discharge." | |
| participant´s description | Eleven caregivers | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Phenomenological/ Semi‐structured interviews/ Giorgi method for analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Cottrell 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia | |
| Objective of study | Quote:"To evaluate service provider’s views on current barriers to patients’ accessing Neurosurgical & Orthopaedic Physiotherapy Screening Clinic and Multidisciplinary Service" | |
| participant´s description | Physiotherapists | |
| Health condition | Neurosurgical and orthopaedic conditions | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Damhus 2018.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To examine the barriers and enablers of health professionals to online exercisebased telerehabilitation "TR" in patients with Chronic obstructive pulmonary disease "COPD", to support a successful implementation process" | |
| participant´s description | Twenty‐five health professionals (6 nurses and 19 physiotherapists (24 to 57 years) from hospitals or municipalities | |
| Health condition | Chronic Obstructive Pulmonary Disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Theoretical domains framework/ Semi‐structured interviews and focus groups/ Framework analysis | |
| Funding sources for the study / Conflict of interest | "No information on funding provided" Quote:''The authors report no conflicts of interest in this work'' |
|
| Notes | Study purposively sampled | |
Davoody 2014.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore current processes in post‐discharge stroke care, to describe current information exchange and interaction points, and to analyse their implications for design of supportive electronic tools." | |
| participant´s description | The care professionals at the primary care centre and the neuro team | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and non‐participatory observations/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Davoody 2016.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore post‐discharge stroke patients’ information needs using patient journey mapping and to use patients’ perceived needs to propose eHealth services that can support them throughout their care and rehabilitation processes." | |
| participant´s description | Twelve participants with mild physical, cognitive and/or psychosocial disabilities | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL), exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Deighan 2017.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To assess the acceptability, accessibility and usability of the ‘Digital Heart Manual (D‐HM) prototype to patients and cardiac nurses to optimise the intervention and user engagement." | |
| participant´s description | Twenty‐eight people participated; patient representatives (PR) and health professionals (HP) | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured questionnaires and telephone interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Delmar 2009.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To identify older persons’ (‡75 years of age) experiences of the rehabilitation process after total hip replacement" | |
| participant´s description | Nine patients | |
| Health condition | Hip replacement | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Phenomenological/ Interviews/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Demain 2013.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To identify current assistive technology knowledge and service provision and the barriers and opportunities for evidence based assistive technologies to be used in stroke upper limb rehabilitation practice, as perceived by stroke survivors, family caregivers and healthcare professionals." | |
| participant´s description | Thirty‐one healthcare providers; 32 patients and/or family caregivers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dennett 2020.
| Study characteristics | ||
| Country / Income of the Country | England (HIC) | |
| Objective of study | Quote:"To explore the user experience of a webbased intervention which was part of a multi‐centre randomized controlled feasibility trial of web‐based physiotherapy ""WEBPaMS" and specifically, whether or not users perceived that it had impacted on their ability to increase and sustain engagement in physical activity" | |
| participant´s description | Eleven patients from Plymouth site | |
| Health condition | Multiple sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Face‐to‐face interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:"No information on funding provided" ''No potential conflict of interest was reported by the authors'' |
|
| Notes | Study purposively sampled | |
DeVries 2017.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To explore which patient‐, intervention‐, and environment‐related factors are determinants of adherence to the online component of e‐Exercise, a 12‐week blended intervention for patients with hip and/or knee osteoarthritis." | |
| participant´s description | Ten patients | |
| Health condition | Hip and/or knee osteoarthritis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐srtructured interviews/ Constant comparison analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dimaguila 2019.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To present the perceptions of stroke survivors, on the effects of PGHD from a poststroke simulated rehabilitation technology in order to refine a Patient Reported outcome measures(PROM) ‐ person‐generated health data (PGHD) that has wider relevance and application." | |
| participant´s description | Ten patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups and semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dinesen 2011.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | "To discuss the obstacles that arise in the co‐innovation process of developing an integrated technique for tele‐rehabilitation of COPD patients." | |
| participant´s description | Representatives from district nursing, hospital, healthcare center, GP and firms; managerial staff from the pulmonary medical ward at the hospital, district nursing and healthcare center; and principal participants from the IT‐ and administration in the municipality and region | |
| Health condition | Chronic obstructive pulmonary disease ‐COPD | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Documents, participant observation and qualitative interviews/ Inductive and deductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data was not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dinesen 2013.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | "To describe patients’ attitudes towards tele‐rehabilitation in the Danish TELEKAT (for Telehomecare, Chronic Patients and the Integrated Healthcare System) project, in order to better understand patients’ behavior when performing tele‐rehabilitation activities in home surroundings." | |
| participant´s description | Twenty‐two patients | |
| Health condition | Chronic obstructive pulmonary disease ‐COPD | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Case study/ Document analysis, participant observation, and qualitative interviews/ Inductive and deductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data was not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dinesen 2018.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To assess the interorganizational cooperation between health care professionals across sectors (hospitals, municipal health care centers) in a cardiac telerehabilitation program." | |
| participant´s description | Healthcare professionals (nurses, a physician, and physiotherapist) | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Case study/ Documents, participant observation, and qualitative interviews/ Inductive and deductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dinesen 2019.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: " To explore the experiences of cardiac patients and their partners of participating in the Teledialog Telerehabilitation Program "TTP"" | |
| participant´s description | Fourteen cardiac patients, twelve patient spouses/partners, and 1 son | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Case study/ Documents, participant observation, and interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: " "No information on funding provided" Quote: ''Conflicts of Interest: None declared'' |
|
| Notes | Study purposively sampled | |
Dithmer 2016.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To describe the development and testing of a prototype application (“The Heart Game”) using gamification principles to assist heart patients in their telerehabilitation process in the Teledialog project." | |
| participant´s description | Ten patients and 3 healthcare providers | |
| Health condition | Heart failure, myocardial infarction, or angina pectoris | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews, participant observations, focus group interviews, and workshop/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dobson 2019.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote: "To understand the needs, preferences, and priorities of end users for the development of an adaptive mobile PR (mPR) support program." | |
| participant´s description | Twenty‐nine clinicians | |
| Health condition | COPD, bronchiectasis and interstitial lung disorders | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ A survey, ethnographicsemistructured interviews and key informant interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Doig 2009.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To examine the experiences of clients, family members, and therapists involved in client‐centered, goal‐directed therapy" | |
| participant´s description | Twelve patients, ten significant others, and three occupational therapists | |
| Health condition | Traumatic Brain Injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cognitive | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Donoso Brown 2015.
| Study characteristics | ||
| Country / Income of the Country | SA (HIC) | |
| Objective of study | Quote: "To qualitatively describe 1) upper extremity use at home, 2) previous home exercise or activity programs, and 3) the acceptability of a novel upper extremity home program, NeuroGame Therapy (NGT), that combines surface electromyography (sEMG) biofeedback and a commercial computer game." | |
| participant´s description | Ten patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dow 2007.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | surface electromyography (sEMG) "To explain how is the role of the carer constructedin rehabilitation‐in‐the home (RITH) programs? | |
| participant´s description | Twenty‐four carers | |
| Health condition | Not specific | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content and thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Dubouloz 2004.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: (sEMG) "To explore the transformation of meaning perspectives among clients undergoing occupational therapy treatment for rheumatoid arthritis" | |
| participant´s description | Six patients, five women and one man | |
| Health condition | Arthritis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Grounded theory/ Qualitative interviews, semi‐structured interviews and suggested prompts/ Constant comparative method | |
| Funding sources for the study / Conflict of interest | Quote: ''This study was funded by a research grant from the Canadian Occupational Therapy Foundation and The Arthritis Society'' Quote: "No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Duggan 2013.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To describe an evaluation of SMART2, a personalised selfmanagement system incorporating activity planning and review, feedback on behaviour‐ and acceptance‐based therapeutic exercises." | |
| participant´s description | Ten patients | |
| Health condition | Chronic pain | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Edbrooke 2020.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To characterise the views and experiences of participants with inoperable lung cancer who completed a home‐based rehabilitation program" | |
| participant´s description | Ninety‐two patients were recruited (45 intervention group, 47 usual care) | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews, home visits and telephone calls/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: "This research was funded through a National Health and Medical Research Council project grant (APP1060484). Lara Edbrooke is the recipient of a Victorian Government Olivia Newton John Cancer Wellness and Research Centre Supportive Care PhD scholarship, through the Victorian Cancer Agency (ONJ16010)" Quote: "The authors declare that they have no conflict of interest" |
|
| Notes | Study purposively sampled | |
Eliassen 2018.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | The aim of this study was to explore how the home trainers follow up instructions and supervision by PTs in reablement. | |
| participant´s description | Twenty‐five patients | |
| Health condition | Not pecific condition | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Video recordings, semistructured interviews and an observation guide/ No analysis specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Emmerson 2018.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the lived experience of patients utilising touch screen tablets to support an upper limb home exercise program post stroke" | |
| participant´s description | Ten patients from a community rehabilitation program in a large metropolitan health service | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This study was supported by the Eastern Health Foun dation, 2013'' Quote: ''The authors declare no conflict of interest related to this work. The authors alone are responsible for the content and writing of this article'' |
|
| Notes | Study purposively sampled | |
Eriksson 2011.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: " To evaluate effects and experiences of patients who had undergone a shoulder joint replacement and participated in physiotherapy at home via video communication in real time" | |
| participant´s description | Twenty‐two patients | |
| Health condition | Shoulder joint replacement | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Essery 2017.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To gain a greater understanding of: how older adults experience internet‐based VR" | |
| participant´s description | Eighteen adults aged 50and over | |
| Health condition | Neurologialc conditions | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Vestibular rehabilitation | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Feinberg 2018.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To evaluate the Home Heart Health program, an adapted CR model for the home care setting, by exploring the programs’ feasibility and acceptability" | |
| participant´s description | Twenty‐eight patients | |
| Health condition | Heart failure, coronary artery disease, surgical aftercare following circulatory system surgery, atrial fibrillation | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Folan 2015.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To gain an understanding of the experiences of clients with tetraplegia trialing assistive technologies for computer access during different stages in a public rehabilitation service" | |
| participant´s description | Three outpatient and four in patient from the Victorian Spinal Cord Service (VSCS), Royal Talbot Rehabilitation Centre (RTRC) in Melbourne | |
| Health condition | Spinal cord injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: "No information on funding provided" Quote: ''The authors declare no conflict of interest'' |
|
| Notes | Study purposively sampled | |
Forman 2014.
| Study characteristics | ||
| Country / Income of the Country | SA (HIC) | |
| Objective of study | Quote: "To overcome logistic obstacles and increase efficiencies of learning, behavior modification, and exercise surveillance may increase Cardiac Rehabilitation participation." | |
| participant´s description | Twenty‐six patients | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Observational study/ Staff considerations/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Forsberg 2014.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To describe experiences of using Nintendo Wii Fit for balance exercise, from the perspectives of patients with multiple sclerosis (MS) and their physiotherapists (PT)." | |
| participant´s description | Fifteen patients and nine physiotherapists | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Frohmader 2015.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore and describe long‐term thoughts and perceptions of the Aussie Heart Guide Programme including the role of the mentor, held by patients recovering from myocardial infarction" | |
| participant´s description | Thirteen patients | |
| Health condition | Myocardial infarction | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Telephone interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Frohmader 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | "To explore nurse mentor perceptions of their role in the delivery of a home‐based CR program for rural patients unable to attend a hospital or outpatient Cardiac Rehabilitation program. " | |
| participant´s description | Seven nurse mentors | |
| Health condition | Myocardial infarction | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Interpretive study/ Survey open‐ended questions/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data was not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Frost 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To identify and explore change processes explaining the effects of the Rehabilitation Enablement in Chronic Heart Failure (REACH‐HF) intervention taking account of reach, amount of intervention received, delivery fidelity and patient and caregiver perspectives" | |
| participant´s description | Patients and caregivers | |
| Health condition | Heart failure | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Interviews/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Galvin 2014.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | " To explore the impact of family involvement in exercise delivery after stroke from the perspective of the individual with stroke and his or her family member" | |
| participant´s description | Fifteen designated “family” members | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Phenomenological theoretical framework and a grounded theory/ In‐depth semi‐structured interviews/ Framework analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Gélinas‐Bronsard 2019.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To identify older assistive technology users and family caregivers’ needs related to assistive technology procurement, and to explore how to offer remote support through an Internet‐based intervention" | |
| participant´s description | Ten patients and ten family caregivers, health workers, other stakeholders (decision‐makers, community partners and researchers) | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ''This work was financed by AGEWELL NCE [CRP 2015‐WP2.2] and the Initiative for the development of new technologies and innovative practices in Rehabilitation (INSPIRE) research program (Ahmed) [010228]. The authors acknowledge salary support from Fonds de recherche en sante du Quebec (Auger, Ahmed) [32988,33084] and Canadian Institutes of Health Research (Mortenson) [360820]'' Quote: ''No potential conflict of interest was reported by the authors'' |
|
| Notes | Study purposively sampled | |
Gell 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To examine female cancer survivor perspectives on remote monitoring and communication to support independent, physical activity maintenance after completing a structured, facility‐based program" | |
| participant´s description | Nineteen patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Giesbrecht 2014.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To develop a prototype Wheelchair Skills Training Program that could be delivered as a home program using a computer tablet, entitled Enhancing Participation in the Community by Improving Wheelchair Skills or EPIC Wheels." | |
| participant´s description | Ten patients | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Participatory action design/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Gilbert 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To understant what is the acceptability of Videoconferencing (VC) between clinicians and patients for a follow‐up consultation for atraumatic shoulder instability?" | |
| participant´s description | Sixteen patients and nine clinicians | |
| Health condition | Atraumatic shoulder instability | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Giunti 2018.
| Study characteristics | ||
| Country / Income of the Country | Switzerland (HIC) | |
| Objective of study | Quote: "To explore Multiple Sclerosis‐specific needs for MS mHealth solutions for Physical Activity" | |
| participant´s description | Patients and physicians, physio‐, occupational, and sports therapists | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews and focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Govender 2019.
| Study characteristics | ||
| Country / Income of the Country | South Africa (LMIC) | |
| Objective of study | Quote: "To explore community reintegration experiences of CVA survivors in a peri‐urban area in KwaZulu‐Natal and the factors that facilitate or hinder this reintegration" | |
| participant´s description | Eight patients who had suffered a stroke, residing in the KwaDabeka community (five male and three females, ranging from 38 to 79 years) | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative exploratory study/ Biographical surveys and semistructured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article'' | |
| Notes | Study purposively sampled | |
Gustafsson 2014a.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To trial Stroke Rehabilitation Enhancing and Guiding Transition Home (STRENGTH), an approach to rehabilitation" | |
| participant´s description | Nine participants, comprising 3 occupational therapists, 4 physiotherapists, and 2 speech pathologists | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Survey and focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Gustafsson 2014b.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To investigate the experiences and expectations of people with stroke, during their transition from hospital to home, after participating in a novel inpatient outreach program, entitled STRENGTH" | |
| participant´s description | Seven patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Gustafsson 2019.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To illuminate older adults’ perceptions of multi proffesional team’s caring skills as success factors for health support in the short‐term goal directed reablement" | |
| participant´s description | Twenty‐three older persons | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Not specified | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Phenomenographic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hale 2005.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote: "To address the paucity of information on the content of home interventions for people with stroke by reporting on the practice of physiotherapeutic home‐based stroke rehabilitation in New Zealand." | |
| participant´s description | Twenty physiotherapists | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Grounded Theory/ Semi‐structured interviews/ Grounded theory analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hale Gallardo 2020.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "This study investigated barriers and facilitators to the implementation of a national TeleRehabilitation program to meet the needs of rural Veterans Health Administration "VHA" patients" | |
| participant´s description | Ten stakeholders (medical directors and program managers) | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | N/A | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''Inc. Funding was provided by the Office of Rural Health, U.S. Department of Veterans Affairs'' Quote: ''The authors report no conflicts of interest in this work'' |
|
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Harder 2017.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To develop a mobile application (app) supported by user preferences to optimise selfmanagement of arm and shoulder exercises for upper‐limb dysfunction (ULD) after breast cancer treatment." | |
| participant´s description | Patients | |
| Health condition | upper‐limb dysfunction (ULD) after breast cancer treatment | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hathiramani 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To explore the experience of a sample of lymphoma survivors participating in a home‐based intervention following chemotherapy" | |
| participant´s description | Thirty‐five patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Open‐ended questionnaire/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hayward 2015.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the feasibility of self‐administered, home‐based SMART Arm training for one person with stroke who has severe and chronic upper‐limb disability" | |
| participant´s description | A 57‐year‐old man with severe upper‐limb disability | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Pretest post‐test follow‐up/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Herber 2017.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To explore what reasons do nonattenders and noncompleters give for their patterns of participation or nonparticipation in cardiac rehabilitation programmes and how future uptake could be enhanced." | |
| participant´s description | Twenty‐five patients | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Heron 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To conduct a pilot trial of the effectiveness of a revised version of The Healthy Brain Rehabilitation Manual during the acute period following a first Transient Isquemic Attack (TIA) or ‘minor’ stroke." | |
| participant´s description | Four patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cognitive | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
HeydariKhayat 2020.
| Study characteristics | ||
| Country / Income of the Country | Iran (LMIC) | |
| Objective of study | Quote:"To explore the lived experiences of burn survivors after a six‐month period of home care following hospital discharge" | |
| participant´s description | Sixteen burn survivors from a university hospital in kermanshah province (10 female and 6 male burn survivors) | |
| Health condition | Burns | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Phenomenological study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:"No information on funding provided" Quote:''There was no conflict of interest'' |
|
| Notes | Study purposively sampled | |
Higgins 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To translate the existing Beating Heart Problems group program into an online format, Help Yourself Online, and second, to pilot test the Help Yourself Online program with a sample of cardiac patients" | |
| participant´s description | Fifteen patients | |
| Health condition | Acute cardiac event | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hill 2016.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To explore the usability and acceptability of eSALT from the perspective of participants with aphasia and speech‐language pathologists" | |
| participant´s description | Five patients and three clinicians | |
| Health condition | Aphasia | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Usability study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hines 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore health professionals’ experiences of, and attitudes towards eHealth technologies to support interdisciplinary practice within rehabilitation for people after TBI." | |
| participant´s description | health professionals (n = 17) | |
| Health condition | Traumatic brain injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Interpretive qualitative study/ Interviews and focus groups/ Narrative analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hjelle 2017.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To describe how older adults in Norway experience participation in reablement" | |
| participant´s description | Eight older adults | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Nursing in | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hoaas 2016.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To explore COPD patients’ adherence and experiences in long‐term telerehabilitation to understand factors affecting satisfaction and potential for service improvements" | |
| participant´s description | Ten patients with moderate to severe Chronic Obstructive Pulmonary Disease (COPD) | |
| Health condition | COPD | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Focus groups and questionnaires/Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''The study was funded by the Northern Norway Regional Health Authority (grant number HST1014‐11)'' Quote: ''The authors declare that they have no competing interests'' |
|
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hoffman 2017.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To provide evidence on the acceptability of an effective postsurgical exercise intervention targeting the self‐management of cancer‐related fatigue" | |
| participant´s description | Thirty‐seven patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Open‐ended questionary/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Hwang 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To describe patient experiences and perspectives of a group‐based heart failure (HF) telerehabilitation program delivered to the homes via online video‐conferencing." | |
| participant´s description | Seventeen participants | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Inskip 2018.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To identify the necessary features of pulmonary telerehabilitation (P‐TR) from the perspectives of individuals living with chronic lung disease and health care professionals (HCPs) who deliver pulmonary rehabilitation (PR)" | |
| participant´s description | Fifty‐two patients | |
| Health condition | COPD, asthma, and interstitial lung disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Questionnaires and focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jakobsen 2018.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To describe health professionals’ perspectives of next of kin in the context of reablement." | |
| participant´s description | Forty‐nine health professionals from different organizational levels. Registered nurses, health workers, student nurses, social educators, and occupational therapists. | |
| Health condition | n/A | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Grounded Theory/ Focus groups/ Comparative analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
James 2018.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the views of people with motor neurone disease (MND) on the barriers, facilitators and potential benefits of using home‐based e‐Health service delivery (telehealth) to access MND multidisciplinary clinic care." | |
| participant´s description | Twelve patients from three MND multidisciplinary clinics and an MND support association group | |
| Health condition | Motor neurone disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative multimethod approach/ Surveys and semi‐structured interviews/ Inductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jansen‐Kosterink 2019.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | To look beyond the common theoretical approaches towards end‐user acceptance (like the Technology Acceptance Model and the Unified Theory of Acceptance and Use of Technology), and to explore the factors that contribute to or hinder the acceptance of a telemedicine service for rehabilitation care by patients with a chronic disease. | |
| participant´s description | One hundred eighty‐eight patients | |
| Health condition | Chronic diseases | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jäppinen 2017.
| Study characteristics | ||
| Country / Income of the Country | Finland (HIC) | |
| Objective of study | Quote: " To explore postoperative patient education in physiotherapy from total hip arthroplasty (THA) patients’ perspectives, which has been a little‐studied area of research. " | |
| participant´s description | Ten patients | |
| Health condition | Total hip arthroplasty | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Individual interviews/ Phenomenographic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jelin 2012.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To explore female patients’ experiences of participating in a 4‐week web‐based home intervention after in‐house multidimensional rehabilitation" | |
| participant´s description | Seven patients | |
| Health condition | Fibromyalgia | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Systematic text condensation | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jones 2007.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To explore patients’ reasons for non‐participation in or non‐adherence to a home‐ or hospital‐based CR programme." | |
| participant´s description | Forty‐nine patients, eleven aged 70 years or over, fifteen from ethnic minority groups | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Charting analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jones 2017.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To show the extent to which experiences from stroke survivors receiving rehabilitation in control (usual care) and intervention (integrated self‐management) sites reflected the differences in rehabilitation received and whether their understandings aligned with the self‐management approach employed." | |
| participant´s description | Twenty‐two patients, twelve from integrated self‐management sites and ten from usual care sites | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Jullamate 2007.
| Study characteristics | ||
| Country / Income of the Country | Thailand (HIC) | |
| Objective of study | Quote: "To Identify the reasons for the provision of informal rehabilitation services at home to stroke relatives by Thai caregivers" | |
| participant´s description | Twenty primary informal caregivers to stroke survivors | |
| Health condition | ||
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Kairy 2013.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To explore patients’ perceptions regarding telerehabilitation services received post total knee replacement" | |
| participant´s description | Five patients who had previously received in‐home telerehabilitation post total knee arthroplasty | |
| Health condition | Knee arthroplasty | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Case study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Kairy 2014.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "This study aimed at exploring patients’ perceptions regarding telerehabilitation services received post total knee replacement" | |
| participant´s description | Sixteen Health Practicioners (including three clinical coordinators) | |
| Health condition | Traumatic brain injury and spinal cord injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Case study/ Focus groups and semi‐structured interviews/ Intergroup analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Kamwesiga 2017.
| Study characteristics | ||
| Country / Income of the Country | Uganda (LMIC) | |
| Objective of study | Quote: "To describe the experiences and meaning of using mobile phones in everyday life after stroke, among persons with stroke and their family members" | |
| participant´s description | Eleven patients and nine family members | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Grounded theory/ Semi‐structured interviews/ Constant comparative method | |
| Funding sources for the study / Conflict of interest | ''The financial support for this study was provided by the Swedish Research Council, Developmental Research [grant number 2014‐28‐63]'' Quote: ''The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article'' |
|
| Notes | Study purposively sampled | |
Kingston 2014.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the experience of receiving medical and rehabilitation intervention for rural and remote residents in North Queensland" | |
| participant´s description | Fifteen patients living in rural areas | |
| Health condition | Traumatic hand injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Interpretive phenomenological study/ In‐depth semi‐structured interviews/ Inductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Knudsen 2019.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To explore patients’ experiences of tele‐rehabilitation and the perceived gains of taking part in the program." | |
| participant´s description | Eight patients | |
| Health condition | Ischemic heart disease and heart valve surgery | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Phenomenological‐hermeneutic study/ Interviews/ Theory of Paul Ricoeur analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Krishnan 2018.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To explore the mobility‐related preferences among stroke survivors and caregivers following post‐acute rehabilitation at inpatient or skilled nursing facilities." | |
| participant´s description | Thirty‐nine patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Cross‐sectional study/ Semi‐structured interviews/ Comparative content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lahham 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To document the perspective of patients with chronic obstructive pulmonary disease (COPD) who underwent home‐based pulmonary rehabilitation (HBPR) in a clinical trial." | |
| participant´s description | Thirteen patients | |
| Health condition | Chronic obstructive pulmonary disease ‐COPD | |
| Mode of rehabilitation delivery | Respiratory | |
| Type of rehabilitation provided | In‐person home‐based rehabilitation and telerehabilitation | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lai 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To examine the usability of a mobile exercise app in People with physical disabilities (PWD)" | |
| participant´s description | Twelve patients | |
| Health condition | Physical disabilities | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Usability testing and interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lawford 2018a.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore physiotherapists’ perceptions before and after delivering exercise advice via telephone to patients with knee osteoarthritis (OA)." | |
| participant´s description | Eight physiotherapists | |
| Health condition | Knee osteoarthritis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lawford 2018b.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore peoples’ perceptions of 26 exercise therapy delivered by physiotherapists via telephone for their knee osteo arthrosis (OA)" | |
| participant´s description | Twenty patients | |
| Health condition | Knee osteoarthritis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lawson 2020.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the issue of acceptability by characterizing the experience of telerehabilitation for service providers and consumers of a memory rehabilitation program" | |
| participant´s description | Twenty‐five patients and nine health workers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This work was supported by National Stroke Foundation: [Grant Number SPG1712]; Turner Institute for Brain and Mental Health: [Grant Number Seed Grant]'' Quote: ''No potential conflict of interest was reported by the author(s)'' |
|
| Notes | Study purposively sampled | |
Learmonth 2019.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To understand experiences of persons with Multiple Sclerosis who participated in a feasibility research study of a home‐based exercise intervention" | |
| participant´s description | Eighteen patients | |
| Health condition | Multiple sclerosis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and questionnaires/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lee 2009.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To evaluate and to decribe ARDS (acute respiratory distress syndrome) survivors' support needs" | |
| participant´s description | Twenty‐five patients | |
| Health condition | Acute respiratory distress syndrome ‐ARDS | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Framework analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Letts 2011.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To explore the perceptions of people with spinal cord injury (SCI) regarding preferred messengers and methods for obtaining physical activity (PA) information. " | |
| participant´s description | Sixteen community‐dwelling adults | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Phenomenological study/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lindblom 2020.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To explore the transition process between hospital and the home with continued rehabilitation in the home environment." | |
| participant´s description | Patients, caregivers and healthcare professionals | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Grounded Theory/ Semi‐structured interviews/ Grounded Theory analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lou 2017.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To investigate how mild stroke patients’ and their partners’ experience and manage everyday life in a context of Early supported discharge. " | |
| participant´s description | Patients and their partners | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lovo 2019.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To investigate the experiences of practitioners and patients during a novel interprofessional model of assessment where an urban‐based physical therapist used videoconferencing to virtually join a rural nurse practitioner and a rural patient with chronic back disorders." | |
| participant´s description | Nineteen patients | |
| Health condition | Low back and/or leg‐related pain | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and surveys/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lovo Grona 2017.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To evaluate the delivery of an inter‐professional (IP) spinal triage management approach to chronic back disorders using remote presence robotic technology as an innovative form of telerehabilitation in a northern Saskatchewan community. " | |
| participant´s description | One patient, a local nurse practitioner (NP) and a physical therapist in an urban centre | |
| Health condition | Chronic Back pain | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Case report/ Semi‐structured interviews and survey/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lutz 2009.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To implement a stroke‐specific, care coordination home telehealth (CCHT) programme for US veterans with stroke and their family caregivers." | |
| participant´s description | Nine veterans and six caregivers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis and constant comparison | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Lykke 2019.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To describe and interpret perspectives of older adults with disabilities and their health are professionals (HCPs) on experienced loneliness during home‐based rehabilitation." | |
| participant´s description | Seven older adults and three health care professionals | |
| Health condition | Older Adults With Disabilities | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Interpretive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Madden 2010.
| Study characteristics | ||
| Country / Income of the Country | England (HIC) | |
| Objective of study | Quote: "To describe the choices patients make when offered home‐based or hospital‐based cardiac rehabilitation." | |
| participant´s description | Staff members and thirty‐five patients | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Magne 2020.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To describe how older adults engage in daily activities within the context of reablement and to explore participation in daily activities." | |
| participant´s description | Ten older adults age 70 to 94 years old | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews/ Text condensation | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Malmberg 2018.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To explore participants’ experiences of an Internet‐based aural rehabilitation "IAR" program for HAusers, and to explore the possible subjective benefits of such a program" | |
| participant´s description | Twenty patients | |
| Health condition | Hearing impairment | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Qualitative exploratory study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: "This work was supported by Research and Technology Development, Habilitation & Health, Region Vastra Gotaland. It also was supported in part by a program grant from the Swedish Council for Wealth, Working Life and Welfare (FORTE) under grant number [2009‐0055]" Quote: "The authors report no conflict of interest'" |
|
| Notes | Study purposively sampled | |
Markle‐Reid 2020.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To investigate the feasibility of a larger RCT to examine the effectiveness of this integrated TC intervention for community‐living older adults with stroke and multimorbidity newly discharged from hospital and referred to an outpatient stroke rehabilitation setting." | |
| participant´s description | Patients | |
| Health condition | Stroke and multimorbidity | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Focus groups and interviews | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Martin 2018.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To to understand what the therapists considered to be important in terms of the challenges of living with a Traumatic Brain Injury" | |
| participant´s description | Therapists include both occupational therapists (OTs) and speech and language therapists (SLTs) | |
| Health condition | Traumatic Brain Injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | User‐centered approach/ Semi‐structured questions/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | ||
Martinez 2017.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To examine the perspectives of Veterans Health Administration health care providers on implementing clinical video telehealth technology for the assessment and treatment of mild traumatic brain injury among veterans " | |
| participant´s description | Twenty‐six providers | |
| Health condition | Traumatic Brain Injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Marwaa 2020.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote: "To explore significant others’ perspectives on how information and communication technology can support the rehabilitation process after stroke and facilitate participation in everyday life." | |
| participant´s description | A significant other of a stroke survivors | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Grounded theory study/ Focus groups/ Grounded theory analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Mawson 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: " To develop and evaluate an information and communication technology (ICT) solution for a post‐stroke Personalised Self‐Managed Rehabilitation System (PSMrS)." | |
| participant´s description | Patients, family caregivers and healthcare professionals | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | User‐centred design/ Home visits, focus groups, in‐depth interviews, cultural probes and technology biographies/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Mawson 2016.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To understand the conditions under which this technology‐based rehabilitation solution would most likely have an impact on the motor behavior of the user, what would work for whom, in what context, and how." | |
| participant´s description | Five patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Mendell 2019.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "The current investigation has reviewed the online chat sessions between participants and healthcare providers to describe the content of discussions during the virtual Cardiac rehabilitation programs "vCRP" intervention. The current investigation focuses on participants randomized to the intervention arm; the vCRP" | |
| participant´s description | Thirty‐eight patients from a tertiary care hospital in Vancouver and a regional hospital serving Northern British Columbia | |
| Health condition | Acute coronary syndrome | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Chat sessions/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''Funding for this study was provided by the Heart and Stroke foundation of BC and Yukon and Canada Health Infoway. Dr. Lear holds the Pfizer/Heart and Stroke Foundation Chair in Cardiovascular Prevention Research'' Quote: ''No competing financial interests exist'' |
|
| Notes | Study purposively sampled | |
Moe 2016.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To gain knowledge about employees’ experiences with establishing a new multidisciplinary team and developing a team‐based work model." | |
| participant´s description | An occupational therapist, two care workers with further education in rehabilitation, a nurse, a physiotherapist, and a project leader | |
| Health condition | Not an specific illness | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Moe 2017.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote: "To generate a grounded theory of practitioners’ patterns of action when establishing reablement in a community setting" | |
| participant´s description | An occupational therapist, physiotherapist, nurse and care workers with training in rehabilitation | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ SFocus groups and interviews/ Theoretical coding | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Mohd Nordin 2014.
| Study characteristics | ||
| Country / Income of the Country | Malaysia (LMIC) | |
| Objective of study | Quote: "To explore perceptions of long term rehabilitation among rehabilitation professionals and people with stroke, and identify strategies for the provision of such services" | |
| participant´s description | Fifteen rehabilitation professionals and eight stroke survivors | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: "No information on funding provided" Quote: ''The authors declare that they have no competing interests'' |
|
| Notes | Study purposively sampled | |
Moraal 2013.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote: "To provide an analysis of bodily experiences of a man with a lower leg amputation who used a virtual rehabilitation program." | |
| participant´s description | One patient, 36 years old Afghanistan veteran | |
| Health condition | Amputee | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Phenomenological exploration/ Semi‐structured interviews/ Phenomenological analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Muller 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To identify communication features that may affect the development of the therapeutic relationship during telephone support sessions for people undertaking self‐directed therapy." | |
| participant´s description | Sixty‐one patients | |
| Health condition | Chronic dizziness | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Neurological | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Telephone sessions/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Nanninga 2015.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote: "To increase understanding of stroke survivor’s needs to successfully re‐establish attachment to meaningful places at home and in the community." | |
| participant´s description | Thirty‐three Stroke survivors | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Inductive and deductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Nasr 2015.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To examine stroke survivors’ experiences of living with stroke and with technology in order to provide technology developers with insight into values, thoughts and feelings of the potential users of a tobe‐designed robotic technology for home‐based rehabilitation of the hand and wrist." | |
| participant´s description | Ten stroke survivors and their family carers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative and user‐centred design/ Interviews, diaries and photography activities/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Ng 2013.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To investigate the feasibility of implementing the Cognitive Orientation to daily Occupational Performance approach "CO‐OP" in a telerehabilitation format and to examine its impact on community integration and executive dysfunction for adults with traumatic brain injury" | |
| participant´s description | Three patients | |
| Health condition | Brain injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Case study/ Fedback interviews, field notes and session recordings/ Descriptive analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''The researchers and organizations involved in this study had no affiliation with Logitech, SkypeTM, or Pamela for SkypeTM. This study was conducted by the primary author while she was an MSc student in the Graduate Department of Rehabilitation Science at the University of Toronto. Personnel funding for her graduate studies was received from the Canadian Occupational Therapy Foundation, the Toronto Rehabilitation Institute and the Ontario Ministry of Health and Long Term Care through the Ontario
Research Coalition of Research Institutes/Centres on Health and Aging. The study was supported by a grant to D. Dawson from the Ontario Neurotrauma Foundation in collaboration with the Quebec Rehabilitation Research Network (ONF‐REPAR) and a grant to D. Dawson from the Ontario Rehabilitation Research Advisory Network'' Quote: ''The authors report no conflicts of interest'' |
|
| Notes | Study purposively sampled | |
Nordin 2015.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To describe patients’ expectations of coming home very early after stroke with support and rehabilitations at home" | |
| participant´s description | Ten participants with mild to moderate stroke symptoms | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Nordin 2017.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To explore patients’ experiences of patient participation in a Web Behavior Change Program for Activity "Web‐BCPA" in combination with multimodal rehabilitation "MMR" among patients with persistent pain in primary health care" | |
| participant´s description | Nineteen patients | |
| Health condition | Chronic pain | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multimodal for pain | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''Financed by the Research project REHSAM (REHabilitering och SAMordning), a co‐operation between the Swedish Social Insurance Agency, the Ministry of Health and Social Affairs, the Swedish Association of Local Authorities and Regions, and the Vårdal Foundation'' Quote: ''Conflicts of Interest none declared'' |
|
| Notes | Study purposively sampled | |
O'Doherty 2013.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | Quote: "To find out how nurses view their role in relation to the rehabilitation of older people within a care‐home environment Our ultimate aim was to develop guidance to improve future practice and to normalise this aspect of nursing care" | |
| participant´s description | Ten nurses working in two long‐term care residences | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | Home‐based rehabilitation | |
| Type of rehabilitation provided | Nursing in | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Semi‐structured interviews/ Data analysis was in accordance with the framework described by burnard (1991) | |
| Funding sources for the study / Conflict of interest | Quote: "No information on funding provided" Quote: "No information on conflict provided" |
|
| Notes | Study purposively sampled | |
O'Hara 2015.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To understand the experiences of the clients, allied health professionals and students in using telehealth in terms of the technology, interaction via videoconferencing, comfort, confidentiality, and the accessibility of expert services, clinical knowledge and skills." | |
| participant´s description | Three allied health professionals and four students, from the disciplines of physiotherapy and occupational therapy. Ten patients | |
| Health condition | Neurological conditions | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Neurologic | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Questionnaires and staff review/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
O'Shea 2020.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | Quote: "To explore participants’ views and experiences of an eHealth phase three cardiac rehabilitation "CR" intervention: Physical Activity Towards Health "PATHway"" | |
| participant´s description | Fourty‐four patients | |
| Health condition | Cardiovascular disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Participant debriefs, interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This project has received funding from the European Union’s Horizon 2020 Framework Programme for Research and Innovation Action under Grant Agreement no. 643491:https://ec. europa.eu/digital‐single‐market/en/policies/ehealth. This was awarded to KM, CW, NM, NMcC, WB, VC, and RB. No the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript'' Quote: ''The authors have declared that no competing interests exist'' |
|
| Notes | Study purposively sampled | |
Ouegnin 2018.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To determine client’s preferred mode of home exercise program delivery when offered a choice between a cellular video and paper handout" | |
| participant´s description | Thirty patients | |
| Health condition | Upper extremity disability | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Cross‐sectional study/ Self‐report patient preference questionnaire/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Ownsworth 2020.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "To explore the perspectives of rehabilitation coordinators, individuals with acquired brain injury, and family caregivers on the usability and acceptability of VC in community based rehabilitation" | |
| participant´s description | Thirteen multidisciplinary rehabilitation coordinators, nine patients, and eight family caregivers | |
| Health condition | Brain injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Inductive analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''The authors acknowledge funding from RECOVER (University of Queensland) and the Menzies Health Institute Queensland (Griffith University). We would also like to thank all participants of the study'' Quote: ''The authors have nothing to disclose'' |
|
| Notes | Study purposively sampled | |
Oyesanya 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To investigate views of technology in the context of managing one’s everyday life from the perspectives of persons with Traumatic Brain Injury and their family caregivers" | |
| participant´s description | Fifteen patients and twelve family caregivers | |
| Health condition | Brain injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative exploratory study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This research was supported by the National Institute for Disability, Independent Living, and Rehabilitation Research, Rehabilitation Engineering Research Center (PI, F. DeRuyter) (Grant # 90RE5023‐01‐00)'' Quote: ''The authors declare no conflicts of interest'' |
|
| Notes | Study purposively sampled | |
Palacios‐Ceña 2016.
| Study characteristics | ||
| Country / Income of the Country | Spain (HIC) | |
| Objective of study | Quote: "To explore the experiences of multiple sclerosis patients who performed a virtual home‐exercise programme using Kinect." | |
| participant´s description | Patients aged between 20 and 60 years | |
| Health condition | Multiples Sclerosis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Unstructured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Palazzo 2016.
| Study characteristics | ||
| Country / Income of the Country | France (HIC) | |
| Objective of study | Quote: "To assess views of patients with chronic low back pain "cLBP" concerning barriers to homebased exercise program adherence and to record expectations regarding new technologies." | |
| participant´s description | Twenty‐nine patients from a tertiary care hospital | |
| Health condition | Chronic low back pain | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote: "No information on funding provided" Quote: ''The authors declare that they have no competing interests'' |
|
| Notes | Study purposively sampled | |
Palmcrantz 2017.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To explore the feasibility and safety of using the DISKO‐tool, customized for interactive stroke rehabilitation in the home setting, in different rehabilitation phases after stroke" | |
| participant´s description | Fifteen patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This project was supported through grants from VINNOVA (2012‐02539), Stockholm County Council (ALF), Västerås Municipality, Västmanland County Administrative Board, Västmanland County Council, Örebro County Council and Örebro Municipality'' Quote: ''The authors declare that they have no competing interests'' |
|
| Notes | Study purposively sampled | |
Pancer 2019.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote: "To identify the preferred features of a Web‐based self‐management physical activity portal through stakeholder engagement with individuals with a spinal cord injury and health care professionals (HCPs)." | |
| participant´s description | Thirteen individuals with an Spinal Cord Injury and nine HealthCare Professionals | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Interpretive phenomenology methodology/ Semi‐structured interviews/ analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pani 2016.
| Study characteristics | ||
| Country / Income of the Country | Italy (HIC) | |
| Objective of study | Quote: "To evaluated patients’ perspectives on the use of a system for home tele‐rehabilitation, designed for subjects with low computer literacy suffering hand impairment due to rheumatic diseases" | |
| participant´s description | Fourty patients, 20 with Rheumatoid arthritis and 20 with systemic sclerosis | |
| Health condition | Rheumatoid arthritis and systemic sclerosis | |
| Mode of rehabilitation delivery | Multimodal for pain | |
| Type of rehabilitation provided | In‐person home‐based rehabilitation and telerehabilitation | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Parker 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To test and refine intervention theories by exploring the complex interactions of contexts, mechanisms and outcomes s that arise from technology deployment in the home." | |
| participant´s description | Five patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Different data collection methods/ Thematic and framework analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Parker 2020.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To evaluate the usability and acceptability of a prototype App to deliver a combined, home‐based behavioural activation and rehabilitation intervention to acute respiratory failure survivors" | |
| participant´s description | An acute respiratory failure survivor and care partner | |
| Health condition | Acute respiratory failure | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Parsons 2018.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: "To investigate stroke rehabilitation clinician’s perceptions of the patient as an active partner in setting goals within stroke rehabilitation and factors that influence patient engagement" | |
| participant´s description | Twenty clinicians | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Inductive analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pasipanodya 2020.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To describe the use of teleSCI to provide care to an individual with SCI in the midst and immediate aftermath of a natural disaster." | |
| participant´s description | An adult who sustained a spinal cord injury | |
| Health condition | Spinal Cord Injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Case study/ Observation/ Analysis not provided | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Paul 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: " To explore the effectiveness and participant experience of web‐based physiotherapy for people moderately affected with Multiple Sclerosis (MS)" | |
| participant´s description | Thirty community dwelling adults | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | A randomised controlled pilot study/ Telephone interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pauwels 2018.
| Study characteristics | ||
| Country / Income of the Country | France (HIC) | |
| Objective of study | Quote: "To assess barriers and facilitators to home‐based cycling in older patients with lumbar spinal stenosis" | |
| participant´s description | Fifteen patients | |
| Health condition | Lumbar spinal stenosis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ / Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pearson 2016.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote: To codesign a Web‐based version of ESCAPE‐pain that people with chronic joint pain find engaging, informative, and useful." | |
| participant´s description | One hundred patients | |
| Health condition | Chronic Knee and Hip Pain | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Focus groups and semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pekmezaris 2020.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To analyze qualitative data from focus groups with key stakeholders to ensure the acceptability and usability of the TM COPD intervention" | |
| participant´s description | Approximately 20 community advisory board members were invited to each meeting, with about one‐third representing patients and caregivers, one‐third representing providers (pulmonologists, researchers, and primary care physicians), and another one‐third representing the other stakeholders (such as community‐based organisations) Cab members included stakeholders, including African American and Hispanic COPD patients; nonprofessional caregivers; experts in health and social disparities; clinicians (geriatrician, pulmonary expert, and a respiratory therapist); and patient advocates | |
| Health condition | Chronic Obstructive Pulmonary Disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote: ''This study was funded through a Patient‐Centered Outcomes Research Institute (PCORI) Award (1511‐33066). The statements presented in this study are solely the responsibility of the author(s) and do not necessarily represent the views of the PCORI, its board of governors, or methodology committee'' ''Conflicts of Interest: None declared'' |
|
| Notes | Study purposively sampled | |
Pettersson 2010.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote: "To explore home care staff experiences in relation to assistive devices and the use of assistive device at work." | |
| participant´s description | Fourteen home care staff: six assistant nurses, six home careers and two personal assistants | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pfaeffli 2012.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote: "To present the content development process for a mHealth (mobile phone and internet‐based) cardiac rehabilitation (CR) exercise intervention." | |
| participant´s description | Thirty‐eight cardiac rehabilitation patients and three cardiac rehabilitation nurses | |
| Health condition | Ischaemic heart disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Focus groups and interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
PfaeffliDale 2015.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote: "To conduct a process evaluation of the HEART intervention to determine what worked and what did not, as well as acceptability and usability." | |
| participant´s description | One hundred seventy‐one adults | |
| Health condition | Ischaemic heart disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pierce 2004.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote: "To test the feasibility of providing Internet‐based education and support intervention to caregivers living in rural settings, including caregivers’ satisfaction with the intervention." | |
| participant´s description | Nine adult caregivers of persons with stroke | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Interviews and e‐mail communications/ Framework analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pierce 2006.
| Study characteristics | ||
| Country / Income of the Country | USa (HIC) | |
| Objective of study | Quote: "To identify perceived problems of new caregivers while caring for persons with stroke during their first 3 months of caregiving in home settings" | |
| participant´s description | Nine adult caregivers new to the role of caring for persons with stroke | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Telephone calls/ Narrative analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pierce 2015.
| Study characteristics | ||
| Country / Income of the Country | United States (HIC) | |
| Objective of study | "To examine a nurse specialist’s responses and advice that she gave in a web‐based supportive intervention for stroke family caregivers" | |
| participant´s description | Family caregivers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Email forum/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data was not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Pinto 2014.
| Study characteristics | ||
| Country / Income of the Country | Brazil (LMIC) | |
| Objective of study | Quote: "Explores the illness experiences, the efficacy of pulmonary rehabilitation as perceived by patients with chronic obstructive pulmonary disease "COPD" and their rational for improvements in health" | |
| participant´s description | Twenty‐three patients with COPD | |
| Health condition | Chronic Obstructive Pulmonary Disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis and semantic interpretation | |
| Funding sources for the study / Conflict of interest | Quote: ''Financial support was provided by the University of Salamanca, the Ministry of Foreign Affairs and Cooperation (J. M. S. Pinto) and CNPq (productivity in science grant #307346/2011‐0 – M. Nations)'' Quote: "No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Plow 2013.
| Study characteristics | ||
| Country / Income of the Country | USa (HIC) | |
| Objective of study | Quote: "To examine the usability of Nintendo Wii Fit to promote physical activity in adults with multiple sclerosis." | |
| participant´s description | Thirty patients with mild to moderate symptoms | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Ranaldi 2018.
| Study characteristics | ||
| Country / Income of the Country | UKingdom (HIC) | |
| Objective of study | Quote: "Explored patient‐reported outcomes of home‐based cardiac rehabilitation in relation to current Scottish, UK and European guidelines" | |
| participant´s description | Four hundred fifty‐seven patiens | |
| Health condition | Cardiovascular disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Questionnaires/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not‐for‐profit sectors'' Quote:''Competing interests: None declared'' |
|
| Notes | Study purposively sampled | |
Randall 2008.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To explore the impact of the managed competition reform on the for‐profit and the not‐for‐profit organisations that provided rehabilitation home‐care services" | |
| participant´s description | Fourty‐nine individuals, including 17 representatives from the community care access centres, 19 representatives from the for‐profit and not‐for‐profit provider agencies and 13 additional representatives from external organisations including government | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | In‐person home‐bases rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Case study/ In‐depth interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Randström 2012.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore older people’s experience of environmental factors that impact on their activity and participation in home rehabilitation" | |
| participant´s description | Ten older patients aged between 68 and 93 years (3 men and 7 women) | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Qualitative interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:"No information on funding provided" Quote:''The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article'' |
|
| Notes | Study purposively sampled | |
Randstrom 2013.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore the experiences of older people and their supporting family members in relation to home rehabilitation, with a focus on activity and participation" | |
| participant´s description | Six older people and six family members | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Qualitative interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This research did not receive any grants from funding agencies in the public, commercial, or not‐for‐profit sectors'' Quote:"No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Randström 2014.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore multidisciplinary teams’ experiences of home rehabilitation for older people" | |
| participant´s description | Twenty‐eight healthcare providers, physiotherapists (n = 6), occupational therapists (n = 3), district nurses (n = 5), nurse assistants (n = 5), home helper (n = 1), home help officers responsible for needs assessment (n = 3) and home help officers in charge of home help (n = 5). The participants´ ages ranged from 28 to 61 years, while time in profession ranged from 3 to 28 years, and time working in home rehabilitation ranged from 2 to 7 years | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This research did not receive any grants from funding agencies in the public, commercial, or not‐for‐profit sectors'' Quote:"No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Rayce 2020.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To explore how home‐based telemediated exercise training offered by a physiotherapist (PT) becomes part of the conduct of everyday lives of patients with very severe COPD" | |
| participant´s description | Patients with very severe COPD and spouses or partners | |
| Health condition | Chronic Obstructive Pulmonary Disease (COPD) | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Ethnographic/ Observations and interviews/ Critical psychology | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Reunanen 2016.
| Study characteristics | ||
| Country / Income of the Country | Finland (HIC) | |
| Objective of study | Quote: To find out what kinds of experiences the clients had of the home‐based intervention and what functions and activities they considered important from the viewpoint of their own reintegration." | |
| participant´s description | Fourteen patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Rietdijk 2020.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote: "Acceptability of telehealth delivery of communication skills training. The research questions relating to acceptability, which are the focus of the present paper, were: 1. Are there differences between telehealth participants and in‐person participants in quantitative measures of acceptability of the social communication skills intervention TBIconneCT? 2. What are the perspectives of people with TBI and their carers regarding acceptability of TBIconneCT telehealth delivery?" | |
| participant´s description | Thirty‐six patients (23 metropolitan and 13 regional) and their caregivers. Fourteen patients/caregivers received in‐person services, and 15 telerehabilitation | |
| Health condition | Brain injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Skype interview, telephone interview or written questionnaires/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The authors disclosed receipt of the following financial sup port for the research, authorship and/or publication of this article: This work was supported by a grant from icare NSW and an Australian Postgraduate Award'' Quote:''The authors declared the following potential conflicts ofinterest with respect to the research, authorship, and/or pub lication of this article: R.R., E.P., M.A. and L.T. are authors of the published training manual for the intervention reported in this paper. The authors do not receive royalties from purchases of this manual'' |
|
| Notes | Study purposively sampled | |
Rizzo 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"Explored orthopedic outpatients mental models of adherence to prescribed home exercise programs and how they related to mental models of adherence to other types of personal regimens" | |
| participant´s description | Ten patients (seven women and three men, mean age was 50.3 years. Orthopaedic diagnoses for the ten participants included three participants each for thoracolumbar/lumbar, foot and ankle, and shoulder dysfunction, and one participant for knee dysfunction | |
| Health condition | Musculoeskeletal disorders | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Interpretive study/ Semi‐structured interviews/ Constant comparative method | |
| Funding sources for the study / Conflict of interest | Quote:"No information on funding provided" Quote:''No potential conflict of interest was reported by the authors'' |
|
| Notes | Study purposively sampled | |
Rothgangel 2017.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To describe the user‐centered approach that guided the design and development of a telerehabilitation platform for patients with phantom limb pain." | |
| participant´s description | Patients | |
| Health condition | Phantom Limb Pain | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Pain | |
| Study design / Data collection approach / Data analysis approach | A User‐Centered Approach/ Questionnaire and interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Sankaran 2019.
| Study characteristics | ||
| Country / Income of the Country | Belgium (HIC) | |
| Objective of study | Quote:"To investigate the impact of the HeartHab app on patients’ overall motivation, increasing physical activities, reaching exercise targets, quality of life, and modifiable risk factors in patients with CAD during telerehabilitation." | |
| participant´s description | Thirty‐two patients | |
| Health condition | Coronary artery disease | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Questionnaires, semi‐structured interviews/ Context analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Saywell 2015.
| Study characteristics | ||
| Country / Income of the Country | New Zealand (HIC) | |
| Objective of study | Quote:"To draw on the insights of people with stroke to assist in the development of a telerehabilitation program, using easily accessible technology to deliver an intervention" | |
| participant´s description | Fifteen patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Questionnaires,/Inductive analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This study was completed using a grant from Physiotherapy New Zealand'' Quote:''The authors report no declarations of interest'' |
|
| Notes | Study purposively sampled | |
Schopfer 2020.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To explore among patients the rationale for declining to participate in cr even when a home‐based cardiac rehabilitation program is available" | |
| participant´s description | Ten patients, all of them male, 40% smokers, 30% had prior coronary artery bypass surgery, and 60% had a recent percutaneous coronary intervention | |
| Health condition | Cardiovascular disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Quantitative survey and open‐ended semi‐structured phone interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This study was supported by a grant from the Department of Veterans Affairs Quality Enhancement Research Initia tive (VA QUERI 1IP1HX002002‐01) and a contract with the Patient Centered Outcomes Research Institute (PCORI IH‐1304‐6787). Dr Schopfer was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under award no. KL2TR000143 and NIH NHLBI K23HL136886. This research is solely the responsibility of the authors and does not necessarily repre sent the offi cial views of the NIH or refl ect the position or policy of the Department of Veterans Affairs'' Quote:''All authors declare no conflicts of interest'' |
|
| Notes | Study purposively sampled | |
Serpanou 2019.
| Study characteristics | ||
| Country / Income of the Country | Greece (HIC) | |
| Objective of study | Quote:"To explore the physical therapists’ perspectives about patients with incomplete post‐traumatic paraplegia adherence to recommended home exercises" | |
| participant´s description | Thirteen registered physical therapists | |
| Health condition | Spinal cord injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Shirai 2020.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To explore the experiences of individuals living with Spinal cord injury/disease on the use of Pressure Ulcer Target (PUT), a mobile educational app for PI prevention and management." | |
| participant´s description | Nine patients | |
| Health condition | Spinal cord injury | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Shulver 2016.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | "To examine healthcare worker views on telehealth, and their implications for implementation to mainstream healthcare services for older people. The study includes a focus on two further dimensions of urban versus rural services and level of clinician experience with telehealth" | |
| participant´s description | Forty‐four health workers (experienced and inexperienced) providing services to older people in the areas of rehabilitation and allied health, residential aged care and palliative care | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This research was supported by a Flinders University, South Australia project ‘Telehealth in the Home: Aged and Palliative Care in South Australia’, an initiative funded by the Australian Government'' Quote:''The authors declare that they have no competing interest'' |
|
| Notes | Study purposively sampled | |
Shulver 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"How do community dwelling older people experience rehabilitation programmes using telehealth technologies? " | |
| participant´s description | Thirteen older patients, three spouses and one caregiver | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This research was supported by a Flinders University, South Australia project ‘Telehealth in the Home: Aged and Palliative Care in South Australia’, an initiative funded by the Australian Government'' Quote:''No conflict of interests to declare'' |
|
| Notes | Study purposively sampled | |
Silveira 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"Investigated the perceptions of persons with multiple sclerosis "MS" who use wheelchairs regarding preferences for the design of exercise programs" | |
| participant´s description | Twenty patients who use wheelchairs | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This work was supported through a training grant from the National Multiple Sclerosis Society (MB 0029)'' Quote:''The authors report no conflicts of interest'' |
|
| Notes | Study purposively sampled | |
Silver 2012.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To identify the barriers encountered by individuals with acute spinal cord injury as they attempt to reintegrate into their community during the challenging first year post inpatient rehabilitation." | |
| participant´s description | Twenty‐six patients | |
| Health condition | Spinal cord injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Self‐reported data Goal Tracking Form (GTF)/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Sivan 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To evaluate whether the International Classification of Functioning, Disability, and Health (ICF) framework provides a useful basis to ensure that key user needs are identified in the development of a home‐based arm rehabilitation system for stroke patients" | |
| participant´s description | Nine patients and six healthcare professionals | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Smaerup 2017.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To identify possible reasons for a modest level of exercise compliance during computer‐assisted training for vestibular rehabilitation" | |
| participant´s description | Seven participants with peripheral, central and/or mixed vestibular dysfunction | |
| Health condition | Vestibular dysfunction | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Neurologic | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Interpretative analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Spasić 2015.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To demonstrate the feasibility of a Web‐based, interactive app, and to conduct a preliminary review of its practicability as part of a complex medical intervention in the rehabilitation of knee disorders. Based on the precognitions of stakeholder expectations, our objective was to examine possible ways of facilitating remote self‐care" | |
| participant´s description | Forty‐four participants: 29 patients and 15 physiotherapists | |
| Health condition | Knee disorders | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Questionnaires/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Standen 2015.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To investigate if effectiveness depends on adherence, so did patients use the intervention to the recommended level" | |
| participant´s description | Seventeen patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) Exercise therapy |
|
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Stark 2019.
| Study characteristics | ||
| Country / Income of the Country | Germany (HIC) | |
| Objective of study | Quote:"To investigate the experiences of chronic stroke patients and non‐professional coaches with home‐based constraint induced movement therapy "homeCIMT"" | |
| participant´s description | Thirteen patients and nine non‐professional coaches (family members) | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Semi‐structured interviews/ Hermeneutic phenomenological analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The study was funded by the German Federal Ministry of Education and Research (Grant No. BMBF 01‐GX‐1003)'' Quote:''The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publica tion of this article'' |
|
| Notes | Study purposively sampled | |
Steihaug 2014.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To use general policy guidelines and staff experience of rehabilitation work in two boroughs in Oslo to develop a model for the organisation of and cooperation on homebased rehabilitation." | |
| participant´s description | Fifiteen employees in the boroughs, five employees in two nursing homes, two in two hospitals and two general practitioners (GPs) | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) Exercise therapy |
|
| Study design / Data collection approach / Data analysis approach | Practice‐oriented study/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Steihaug 2016.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To investigate how rehabilitation work is perceived and carried out by first‐line service providers compared with the guidelines issued by Norway’s health authorities." | |
| participant´s description | Twenty‐four participants: 19 women and five men. Fifteen were employees of the boroughs; five were employees in two nursing homes; two were hospital employees; and two were general practitioners (GPs). Seven of the informants were managers or middle managers | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Practice‐oriented study/ Focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Stuifbergen 2011.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To explore the feasibility of home‐based computer‐assisted training and systematically examine the perceptions of people with MS regarding home use of the program" | |
| participant´s description | Thirty‐four patients (relapse‐free for at least 90 days) | |
| Health condition | Multiple Sclerosis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Cognitive | |
| Study design / Data collection approach / Data analysis approach | Qualitative exploratory study/ Questionnaires/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:'This work was supported by the National Institutes of Health, National Institute of Nursing Research, Grant 1R21NR011076'' Quote:''The authors have no conflicts of interest to disclose'' |
|
| Notes | Study purposively sampled | |
Sturkenboom 2016.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:" To evaluate fidelity, treatment enactment and the experiences of an occupational therapy intervention in Parkinson’s disease, to identify factors that affect intervention delivery and benefits." | |
| participant´s description | One hundred and twenty‐four home‐dwelling Parkinson’s disease patients and their primary caregivers (recipients), and 18 occupational therapists | |
| Health condition | Parkinson's disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Focus groups/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Sureshkumar 2016.
| Study characteristics | ||
| Country / Income of the Country | India (LMIC) | |
| Objective of study | Quote:"To identify operational issues encountered by study participants in using the ‘Care for Stroke’ intervention." | |
| participant´s description | Sixty patients and their caregivers living in Chennai | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Semi‐structured interviews/ Framework approach | |
| Funding sources for the study / Conflict of interest | Quote:''This work was supported by a Wellcome Trust Capacity Strengthening Strategic Award to the Public Health Foundation of India and a consortium of UK universities'' ''Competing interests: None declared'' |
|
| Notes | Study purposively sampled | |
Sørensen 2019.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To develop a theoretical account of the behavioural pattern of adherence to home‐based inspiratory muscle training (IMT) in people with chronic obstructive pulmonary disease (COPD)" | |
| participant´s description | Thirty‐three patients | |
| Health condition | Chronic Obstructive Pulmonary Disease (COPD) | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Grounded Theory( Data collection no clear/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Tamm 1996.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To investigate the ethical dilemmas community‐based occupational therapists report encountering in home settings." | |
| participant´s description | Twenty‐three community‐based occupational therapists | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Dilemmas/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Taule 2014.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To explore experiences of mild‐stroke survivors in the context of early supported discharge. " | |
| participant´s description | Eight patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Text condensation | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Taylor 2015.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To understand the issues encountered during the provision of technology services that supported this trial." | |
| participant´s description | Eight clinical staff (therapists, nurses and doctors) | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Staff observations and documents including job logs, meetings, emails and technology descriptions/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Taylor 2016.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To identify which technical factors influence the quality of video conferencing in the home setting and to assess the impact of these factors on the clinical perceptions and acceptance of video conferencing for health care delivery into the home." | |
| participant´s description | Clinical teams | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Action research/ computer‐based questionnaire/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Teriö 2019.
| Study characteristics | ||
| Country / Income of the Country | Uganda (LMIC) | |
| Objective of study | Quote:"To evaluate the implementation process of a mobile phone‐supported family‐centred rehabilitation intervention and to gain knowledge on the mechanisms of impact as well as the contextual factors that might have affected the implementation process and its outcome" | |
| participant´s description | Twelve participants; four occupational therapists, three researchers, three information technology (IT) specialists and two rehabilitation managers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) | |
| Study design / Data collection approach / Data analysis approach | Single‐case study/ Semi‐structured interviews/ Framework approach | |
| Funding sources for the study / Conflict of interest | Quote:''This study was supported by grant from The Swedish Research Council grant number 2014‐28‐63 that was used for design of the study, interpretation of data and manuscript writing. Further, the study was supported by a Minor Field Studies (MFS), as SIDA (The Swedish International Development Co operation Agency) funded scholarship for field studies with the purpose to give students an opportunity to learn more about low‐ and middle income countries, development issues and to promote internationalization. MFS funded data collection, analysis and interpretation of data and manuscript writing'' Quote:''The authors declare that they have no competing interests'' |
|
| Notes | Study purposively sampled | |
Thirumalai 2018.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To describes the development process of the TEAMS (Tele‐Exercise and Multiple Sclerosis) app, which is being used by people with multiple sclerosis in a large randomized controlled trial to engage in home‐based telerehabilitation." | |
| participant´s description | Twenty‐one patients | |
| Health condition | Multiple sclerosis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Thorup 2016.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"To explore pedometer use and self‐determined motivation for walking during a cardiac telerehabilitation program from patients’ and health professionals’ experiences." | |
| participant´s description | Twelve patients, eleven health professionals, six physiotherapists and five registered nurses | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Observations and interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Timmerman 2017.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:" To evaluate the feasibility of a telehealthcare application for operable lung cancer patients, consisting of ambulant symptom and physical activity monitoring (S&PAM) and a web‐accessible home‐based exercise program (WEP), and identify possible barriers for successful adoption and implementation" | |
| participant´s description | Twenty‐two patients and their treating healthcare professional | |
| Health condition | Lung cancer | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Townsend 2013.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To examine how people with chronic illness use eHealth in their daily lives, how it affects patient‐provider relationships, and the ethical and practical ramifications for patients, providers, and service delivery." | |
| participant´s description | Sixty patients | |
| Health condition | Arthritis | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Multimodal for pain | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Tsai 2016.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To determine the level of satisfaction and experience of an eight‐week supervised home‐based telerehabilitation exercise program using real‐time videoconferencing in people with COPD" | |
| participant´s description | Eleven patients referred to a tertiary hospital pulmonary rehabilitation program in Sydney | |
| Health condition | Chronic Obstructive Pulmonary Disease (COPD) | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Respiratory | |
| Study design / Data collection approach / Data analysis approach | Mixed methods study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This study was supported by the New South Wales Agency for Clinical Innovation (ACI), New South Wales, Australia'' Quote:''The Authors declare that there is no conflict of interest" |
|
| Notes | Study purposively sampled | |
Tung 2012.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To explore how older people maintained and improved their self‐efficacy in managing home rehabilitation and their adherence to rehabilitation exercise programmes following orthopaedic surgery." | |
| participant´s description | Fifteen older people who had returned to their homes following orthopaedic Surgery | |
| Health condition | Orthopaedic Surgery | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) Exercise therapy |
|
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Turner 2011.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To explore the service and support needs of individuals with acquired brain injury "ABI" and their family caregivers during the transition phase from hospital to home" | |
| participant´s description | Twenty patients with acquired brain injury and 18 family caregivers | |
| Health condition | Brain injury | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The completion of this study was supported by an Australian Post‐Graduate Award held by Benjamin Turner'' Quote:"No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Tyagi 2018.
| Study characteristics | ||
| Country / Income of the Country | Singapore (HIC) | |
| Objective of study | Quote:"To explore the barriers and facilitators of telerehabilitation as perceived by stroke patients, caregivers, and rehabilitation therapists recruited from one of the largest trials of TeleRehabilitation in a developed Asian country to date" | |
| participant´s description | Thirty‐seven participants, including patients, their caregivers, and tele‐therapists | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews and focus groups/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''Supported by the Singapore Millennium Foundation (Grant Number: R e 608 ‐000 e 048 ‐592) and Saw Swee Hock School of Public Health Tele‐Health InnOvation Research (THOR) Program Grant (Grant Number: R e 608 e 000 e 120 ‐ 733)'' Quote:"No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Umb Carlsson 2019.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore residents’, staff members’ and rehabilitation professionals’ experiences of how a health‐promotion intervention affected the habits of people living in a group home regarding eating habits and physical activities and staffs’ ways of working" | |
| participant´s description | Five residents, six staff members and five rehabilitation professionals | |
| Health condition | Intellectual disability | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Promotion of healthy lifestyles | |
| Study design / Data collection approach / Data analysis approach | Qualitative approach/ Semi‐structured interviews/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publi cation of this article: This work was financially supported by Research and Development in So¨rmland, Sweden and Eskilstuna municipality, Sweden'' Quote:''The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article'' |
|
| Notes | Study purposively sampled | |
Valdés 2018.
| Study characteristics | ||
| Country / Income of the Country | Canada (HIC) | |
| Objective of study | Quote:"To identify the factors that influence the use of an at‐home virtual rehabilitation gaming system from the perspective of therapists, engineers, and adults and adolescents with hemiparesis secondary to stroke, brain injury, and cerebral palsy." | |
| participant´s description | Seven adults and three adolescents with hemiparesis. Also, therapists and engineers | |
| Health condition | Hemiparesis | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation and telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Van der Meer 2020.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To assess the needs, facilitators and barriers of the use of an e‐Health application from the perspective of both orofacial physical therapists and patients with TMD" | |
| participant´s description | Nine patients and eleven Orofacial Physical therapists | |
| Health condition | Temporomandibular disorders | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Descriptive study/ Open face‐to‐face interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | Quote:''This study was funded by the Dutch Organisation for Scientific Research (Nederlandse Organisatie voor Wetenschappelijk Onderzoek – NWO) [grant number 023.006.004]'' Quote:''There is no conflict of interest within this study'' |
|
| Notes | Study purposively sampled | |
VanderVeen 2019.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To explore the perspectives of health and social care professionals involved in stroke rehabilitation" | |
| participant´s description | Fourteen professionals with different backgrounds and roles in treating Dutch clients post stroke | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Multidisciplinary | |
| Study design / Data collection approach / Data analysis approach | Qualitative focus group study/ Focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | Quote:''The authors received no specific funding for this work'' Quote:''Competing interests: The authors have declared that no competing interests exist'' |
|
| Notes | Study purposively sampled | |
VanEngen‐Verheul 2017.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To determine factors identified by cardiac rehabilitation (CR) teams on what is needed to successfully implement a web‐based audit and feedback (A&F) intervention with outreach visits to improve the quality of CR care" | |
| participant´s description | Forty‐nine cardiac rehabilitation professionals | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Concept mapping/ Data collection and analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
VanVelsen 2016.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To understand what determines trust in portals that facilitate rehabilitation therapy, both from the perspective of the patient and the healthcare professional" | |
| participant´s description | Fifteen patients | |
| Health condition | Cerebrovascular accident, chronic back pain, chronic pain, and cerebral infarction | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Not specified | |
| Study design / Data collection approach / Data analysis approach | Cerebrovascular accident, chronic back pain, chronic pain, and cerebral infarction | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Vik 2009.
| Study characteristics | ||
| Country / Income of the Country | Norway (HIC) | |
| Objective of study | Quote:"To explore and describe how older adults who received home‐based rehabilitation perceived the staff during a period of six months when they received rehabilitation Specifically, the study focused on how the participants collaborated with and made use of the services from the staff" | |
| participant´s description | Three older adults over the age of 65 | |
| Health condition | Elderly | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Nursing in | |
| Study design / Data collection approach / Data analysis approach | Case study/ Qualitative interviews/ Grounded theory approach | |
| Funding sources for the study / Conflict of interest | Quote:''The authors would like to thank the participants for so willingly sharing their experiences with us, and Sør‐Trøndelag University College for financial support for this study'' Quote:"No information on conflict provided" |
|
| Notes | Study purposively sampled | |
Vloothuis 2020.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"How do the patient–caregiver couples exercise together? and what does exercising together bring about, besides more hours of practice?" | |
| participant´s description | Seven patients and seven caregivers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Explorative qualitative study/ Semi‐structured interviews/ Inductive thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
VonKoch 1998.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To explore differences between a therapy session with a stroke patient in two different contexts, the patient's home and in the hospital." | |
| participant´s description | Two therapists | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ participant observations and semistructured interviews and documents/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
VonKoch 2000.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To describe the content of a programme involving early hospital discharge and continued rehabilitation at home after stroke." | |
| participant´s description | Patients | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Semi‐structured interviews/ Analysis not specified | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wade 2016.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To develop a preferred governance and operational approach for a larger‐scale home telehealth service. " | |
| participant´s description | Nineteen participants: senior clinicians, health service managers and policy makers | |
| Health condition | It is not an especific illness | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | NA | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wakefield 2019.
| Study characteristics | ||
| Country / Income of the Country | USA (HIC) | |
| Objective of study | Quote:"To examine barriers and facilitators associated with site‐level implementation of a national home‐based Cardiac rehabilitation (HBCR) program in the Veterans Health Administration (VHA)" | |
| participant´s description | Sixteen Veterans Health Administration | |
| Health condition | Cardiac | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ /Framework analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wall 2017.
| Study characteristics | ||
| Country / Income of the Country | Australia (HIC) | |
| Objective of study | Quote:"To evaluate end‐user perceptions of a new asynchronous telepractice application, ‘SwallowIT’, designed to support patients to remotely complete intensive swallowing therapy during curative chemoradiotherapy (CRT) treatment for head and neck cancer (HNC).@ | |
| participant´s description | Fifteen patients | |
| Health condition | Cancer | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Questionnaires and semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Walsh 2018.
| Study characteristics | ||
| Country / Income of the Country | Ireland (HIC) | |
| Objective of study | Quote:"To engage with individuals with cardiovascular disease and other professionals within the health ecosystem to understand the personal, social, and physical factors that inhibit or promote their capacity to engage with physical activity." | |
| participant´s description | Thirty‐three patients | |
| Health condition | Cardiovascular diseases | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wentink 2019.
| Study characteristics | ||
| Country / Income of the Country | The Netherlands (HIC) | |
| Objective of study | Quote:"To identify end‐user requirements for a comprehensive eHealth program in stroke rehabilitation." | |
| participant´s description | Patients with stroke, their informal caregivers and health professionals | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews and focus groups/ Content analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wilms 2020.
| Study characteristics | ||
| Country / Income of the Country | Denmark (HIC) | |
| Objective of study | Quote:"This article suggests a new model for understanding the impact of computerized home training on the therapeutic alliance between the therapist, the patient and training assistants." | |
| participant´s description | A 75‐year old patient | |
| Health condition | Visual neglect and neglect dyslexia | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Communication | |
| Study design / Data collection approach / Data analysis approach | Qualitative Interpretative Phenomenological/Semi‐structured interviews /interpretive phenomenological analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wingham 2006.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To explore patients’ experience of MI (miocardial infarctation) and to identify the factors which influence the choice patients make given the option of hospital or home‐based CR (cardiac rehabilitation)" | |
| participant´s description | Seventeen patients | |
| Health condition | Ischaemic heart disease | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Interpretive phenomenological analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wingham 2014.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To understand stroke survivors and their caregivers’ experience and acceptability of using the Nintendo Wii SportsTM games (WiiTM) as a home‐based arm rehabilitation tool." | |
| participant´s description | Twenty patients and ten caregivers | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | Telerehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wingham 2015.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To identify the needs of caregivers supporting a person with heart failure and to inform the development of a caregiver resource to be used as part of a home‐based self‐management programme." | |
| participant´s description | Twenty‐six caregivers | |
| Health condition | Heart failure | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Cardiac | |
| Study design / Data collection approach / Data analysis approach | Qualitative study/ Semi‐structured interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wingham 2019.
| Study characteristics | ||
| Country / Income of the Country | UK (HIC) | |
| Objective of study | Quote:"To compare the caregiver outcomes between the REACH‐HF and control groups; and to report the views and perceptions of caregivers on their experience of using the REACH‐HF intervention." | |
| participant´s description | Twenty caregivers | |
| Health condition | Heart failure | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Activities in daily living (ADL) Exercise therapy |
|
| Study design / Data collection approach / Data analysis approach | Mixed methods/ Interviews/ Thematic analysis | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
Wottrich 2007.
| Study characteristics | ||
| Country / Income of the Country | Sweden (HIC) | |
| Objective of study | Quote:"To identify the meaning of rehabilitation in the home environment after stroke from the perspective of members of a multiprofessional team" | |
| participant´s description | Thirteen members of a multiprofessional outreach team (physical therapists, occupational therapists, speech and language therapists, and a social worker) | |
| Health condition | Stroke | |
| Mode of rehabilitation delivery | In‐person home‐based rehabilitation | |
| Type of rehabilitation provided | Exercise therapy | |
| Study design / Data collection approach / Data analysis approach | Empirical Phenomenological Psychological method/ Interviews/ Empirical Phenomenological Psychological method | |
| Funding sources for the study / Conflict of interest | ||
| Notes | This study was eligible but not sampled given that the data were not as thick as data from other eligible studies, and the study setting/population/mode of rehabilitation and type of rehabilitation provided is already covered in many of the other sampled studies | |
ACS: Acute coronary syndrome; ; ADL: activities of daily living; CoPs: Communities of practice; COPD: Chronic Obstructive Pulmonary Disease; HIC: high‐income country; LIMIC: Low‐ and Middle‐income country; ICBT: Internet‐delivered cognitive behavioural therapy; MND: motor neurone disease; NIV: non invasive ventilation; PROM; Patient Reported outcome measures; PGHD: person‐generated health data; sag: surface electromyography; ULD: upper‐limb dysfunction
Characteristics of studies awaiting classification [ordered by study ID]
Beunder 2015.
| Notes | Different language |
Friedrich 2015.
| Notes | Different language |
Hennemann 2018.
| Notes | Different language |
Jungbauer 2008.
| Notes | Different language |
Langberg 2014.
| Notes | Different language |
Stamm‐Balderjahn.
| Notes | Different language |
Differences between protocol and review
In our protocol, registered in OSF (https://osf.io/gmh74/), we proposed to consider different phases of the rehabilitation process (i.e. pre‐habilitation, acute rehabilitation care, sub‐acute rehabilitation care, post‐acute rehabilitation care and long‐term/chronic rehabilitation care) for characterizing studies included and defining the sampling of studies. However; it was not possible to clearly determine those phases in all the studies included.
Contributions of authors
Marcela Vélez: involved in all steps of the process
Luz‐Helena Lugo: involved in all steps of the process
Claire Glenton: protocol development, screening, data extraction reviewing, write‐up
Daniel Patiño: involved in all steps of the process
Ana‐María Posada: protocol development, screening, data extraction, matrix analysis, write‐up
Luisa‐Fernanda Mesa: protocol development, screening, data extraction, matrix analysis, write‐up
Stefano Negrini: Research conceptualization, reviewing the write‐up
Carlotte Kiekens: Research conceptualization, reviewing the write‐up
Maria‐Alejandra Spir‐Brunal: screening, data extraction
Kelly‐Mariana Cruz‐Sarmiento: screening, data extraction
Anne‐Stine Bergquist‐Roberg: screening, data extraction reviewing, write‐up
Sources of support
Internal sources
-
Universidad de Antioquia, Colombia
University of Antioquia pay the salaries of the Colombian researchers that participate in this review
External sources
-
Norwegian Ministry of Health and Care Services, Norway
This review was supported by funding from Norwegian Ministry of Health and Care Services for the project ‘Strengthening evidence‐informed decision making for health systems in Colombia’ (COL2101). This funding forms part of the Cooperation Agreement between the Norwegian Ministry of Health and Care Services and the Colombian Ministry of Health and Social Protection.
Declarations of interest
Velez, Marcela: no financial conflicts of interest
Lugo‐Agudelo, Luz Helena: no financial conflicts of interest
Glenton, Claire: no financial conflicts of interest. CG is an EPOC editor but was not involved in the editorial process for this review
Patiño Lugo, Daniel F. : no financial conflicts of interest
Mesa Franco, Luisa Fernanda: no financial conflicts of interest
Velasquez, Juan Carlos: no financial conflicts of interest
Cruz Sarmiento , Kelly Mariana: no financial conflicts of interest
Posada, Ana: no financial conflicts of interest
Spir Brunal, Maria Alejandra: no financial conflicts of interest
Roberg, Anne‐Stine: no financial conflicts of interest
Negrini, Stefano: no financial conflicts of interest. SN holds the position of Scientific Director at ISICO (Italian Scientific Spine Institute). This position was assessed previously by the Cochrane CoI Panel in relation to SN position as Cochrane Rehabilitation Field Director and the Panel agreed that the “position at ISICO is viewed as a private practice situation and not as employment at a commercial for‐profit health company”
Kiekens, Carlotte: no financial conflicts of interest
A number of non‐financial issues, including personal, political and academic factors, could have influenced the review authors’ input when conducting this review. The review authors have discussed this further in the sections on reflexivity in the Methods and Results sections.
New
References
References to studies included in this review
Alary Gauvreau 2019 {published data only}
- Alary Gauvreau C, Le Dorze G, Kairy D, Croteau C. Evaluation of a community of practice for speech-language pathologists in aphasia rehabilitation: a logic analysis. 2019;19(1):1-14.. BMC Health Services Research 2019;19(1):1-14. [DOI: 10.1186/s12913-019-4338-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ando 2019 {published data only}
- Ando H, Ashcroft-Kelso H, Halhead R, Chakrabarti B, Young CA, Cousins R, et al. Experience of telehealth in people with motor neurone disease using non invasive ventilation. Disability Rehabilitation and Assistive Technology 2019 Sep 12;16(5):1-7. [DOI: 10.1080/17483107.2019.1659864] [DOI] [PubMed] [Google Scholar]
Argent 2018 {published data only}
- Argent R, Slevin P, Bevilacqua A, Neligan M, Daly A, Caulfield B. Clinician perceptions of a prototype wearable exercise biofeedback system for orthopaedic rehabilitation: a qualitative exploration. BMJ 2018;8(10):1-8. [DOI: 10.1136/bmjopen-2018-026326] [DOI] [PMC free article] [PubMed] [Google Scholar]
Banner 2015 {published data only}
- Banner D, Lear S, Kandola D, Singer J, Horvat D, Bates J, Iet al. The experiences of patients undertaking a 'virtual' cardiac rehabilitation program. Studies in Health Technology and Informatics 2015;209:9-14. [PMID: ] [PubMed] [Google Scholar]
Barclay 2020 {published data only}
- Barclay L, Lalor A, Migliorini C, Robins L. A comparative examination of models of service delivery intended to support community integration in the immediate period following inpatient rehabilitation for spinal cord injury. Spinal Cord 2020 May;58(5):528-36. [DOI: 10.1038/s41393-019-0394-x.] [DOI] [PubMed] [Google Scholar]
Bendelin 2018 {published data only}
- Bendelin N, Gerdle B, Andersson G. Internet-delivered aftercare following multimodal rehabilitation program for chronic pain: a qualitative feasibility study. Journal of Pain Research 2018 Sep 4;11:1715-28. [DOI: 10.2147/JPR.S157939] [DOI] [PMC free article] [PubMed] [Google Scholar]
Birkeland 2017 {published data only}
- Birkeland A, Tuntland H, Førland O, Jakobsen FF, Langeland E. Interdisciplinary collaboration in reablement - a qualitative study. Journal of Multidisciplinary Healthcare 2017 May 5;10:195-203. [DOI: 10.2147/JMDH.S133417] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodker 2015 {published data only}
- Bødker M, Juul Nielsen A. Providing rehabilitation online – invisible work and diagnostic agents. Journal of Health Organization and Management 2015;29(7):948-64. [DOI: 10.1108/JHOM-06-2014-0091] [DOI] [PubMed] [Google Scholar]
Boland 2018 {published data only}
- Boland P, Levack WM, Graham FP, Perry MA. User perspective on receiving adaptive equipment after stroke: A mixed-methods study. Canadian Journal of Occupational Therapy 2018 Oct;85(4):297-306. [DOI: 10.1177/0008417418800834] [DOI] [PubMed] [Google Scholar]
Booth 2007 {published data only}
- Booth S, Kendall M. Benefits and challenges of providing transitional rehabilitation services to people with spinal cord injury from regional, rural and remote locations. Australian Journal of Rural Health 2007 Jun;15(3):172-8. [DOI: 10.1111/j.1440-1584.2007.00880.x] [DOI] [PubMed] [Google Scholar]
Borade 2019 {published data only}
- Borade N, Ingle A, Nagarkar A. Lived experiences of people with mobility-relateddisability using assistive devices. Disability and Rehabilitation: Assistive Technology 2019;16(7):1-5. [DOI: 10.1080/17483107.2019.1701105] [DOI] [PubMed] [Google Scholar]
Brennan 2020 {published data only}
- Brennan L, Kessie T, Caulfield B. Patient experiences of rehabilitation and the potential for an mhealth system with biofeedback after breast cancer surgery: a qualitative study. JMIR Mhealth and Uhealth 2020 Jul 29;8(7):1-15. [DOI: 10.2196/19721] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brewer 2017 {published data only}
- Brewer LC, Kaihoi B, Schaepe K, Zarling K, Squires RW, Thomas RJ, et al. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digital Health 2017 Apr 24;3:1-8. [DOI: 10.1177/2055207617705548] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brouns 2018 {published data only}
- Brouns B, Meesters JJL, Wentink MM, Kloet AJ, Arwert HJ, Vliet Vlieland TP, et al. Why the uptake of eRehabilitation programs in stroke care is so difficult—a focus group study in the Netherlands. BioMed Central Journals 2018;13(1):1-11. [DOI: 10.1186/s13012-018-0827-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buimer 2017 {published data only}
- Buimer HP, Tabak M, Velsen L, Geest T, Hermens H. Exploring determinants of patient adherence to a portal-supported oncology rehabilitation program: interview and data log analyses. JMIR Rehabilitation and Assistive Technology 2017 Dec 14;4(2):1-12. [DOI: 10.2196/rehab.6294] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burkow 2015 {published data only}
- Burkow TM, Vognild LK, Johnsen E, Risberg MJ, Bratvold A, Breivik E, et al. Comprehensive pulmonary rehabilitation in home-based online groups: a mixed method pilot study in COPD. BMC Research Notes 2015 Dec 10;8:1-11. [DOI: 10.1186/s13104-015-1713-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caughlin 2020 {published data only}
- Caughlin S, Mehta S, Corriveau H, Eng JJ, Eskes G, Kairy D, et al. Implementing telerehabilitation after stroke: lessons learned from Canadian trials. Telemedicine Journal and E-Health 2020 Jun;26(6):710-9. [DOI: 10.1089/tmj.2019.0097] [DOI] [PubMed] [Google Scholar]
Chen 2019a {unpublished data only}
- Chen X, Lu W, Wen Z, Marrone g, Jiang W. Feasibility and acceptability of an exercise-based cardiac rehabilitation program “Baduanjin Eight- Silken-Movements with self-efficacy building for heart failure” (BESMILE-HF). Advances in Integrative Medicine 2019. [DOI: 10.1016/J.AIMED.2019.03.252] [DOI] [PMC free article] [PubMed]
Chen 2019b {published data only}
- Chen Y, Abel KT, Janecek JT, Chen Y, Zheng K, Cramer SC. Home-based technologies for stroke rehabilitation: a systematic review. International Journal of Medical Informatics 2019 Mar;123:11-22. [DOI: 10.1016/j.ijmedinf.2018.12.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cherry 2017 {published data only}
- Cherry CO, Chumbler NR, Richards K, Huff A, Wu D, Tilghman LM, et al. Expanding stroke telerehabilitation services to rural veterans: a qualitative study on patient experiences using the robotic stroke therapy delivery and monitoring system program. Disability Rehabilitation and Assistive Technology 2017 Jan;12(1):21-7. [DOI: 10.3109/17483107.2015.1061613] [DOI] [PubMed] [Google Scholar]
Choularia 2014 {published data only}
- Chouliara N, Fisher RJ, Kerr M, Walker MF. Implementing evidence-based stroke Early Supported Discharge services: a qualitative study of challenges, facilitators and impact. Clinical Rehabilitation 2014 Apr;28(4):370-7. [DOI: 10.1177/0269215513502212] [DOI] [PubMed] [Google Scholar]
Clark 2013 {published data only}
- Clark RA, Tideman P, Tirimacco R, Wanguhu K, Poulsen V, Simpson P, et al. A pilot study of the feasibility of an internet-based electronic Outpatient Cardiac Rehabilitation (eOCR) program in rural primary care. Heart, Lung & Circulation 2013 May;22(5):352-9. [DOI: 10.1016/j.hlc.2012.11.005] [DOI] [PubMed] [Google Scholar]
Cobley 2013 {published data only}
- Cobley CS, Fisher RJ, Chouliara N, Kerr M, Walker MF. A qualitative study exploring patients' and carers' experiences of Early Supported Discharge services after stroke. Clinical Rehabilitation 2013;27(8):750-7. [DOI: 10.1177/0269215512474030] [DOI] [PubMed] [Google Scholar]
Constantinescu 2017 {published data only}
- Constantinescu G, Loewen I, King B, Brodt C, Hodgetts W, Rieger J. Designing a Mobile Health App for patients with dysphagia following head and neck cancer: a qualitative study. JMIR Rehabilitation and Assistive Technologies 2017 Mar 24;4(1):1-11. [DOI: 10.2196/rehab.6319] [DOI] [PMC free article] [PubMed] [Google Scholar]
Conti 2015 {published data only}
- Conti A, Garrino L, Montanari P, Dimonte V. Informal caregivers’ needs on discharge from the spinal cord unit: analysis of perceptions and lived experiences. Disability and Rehabilitation 2015 Apr 10;38(2):159-67. [DOI: 10.3109/09638288.2015.1031287] [DOI] [PubMed] [Google Scholar]
Cottrell 2017 {published data only}
- Cottrell MA, Hill AJ, O'Leary SP, Raymer ME, Russell TG. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: a qualitative study. Musculoskeletal Science & Practice 2017 Dec;32:7-16. [DOI: 10.1016/j.msksp.2017.07.008] [DOI] [PubMed] [Google Scholar]
Damhus 2018 {published data only}
- Damhus CS, Emme C, Hansen H. Barriers and enablers of COPD telerehabilitation – a frontline staff perspective. International Journal of COPD 2018;13:2473-82. [DOI: 10.2147/COPD.S167501] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davoody 2014 {published data only}
- Davoody N, Koch S, Krakau I, Hägglund M. Collaborative interaction points in post-discharge stroke care. International Journal of Integrated Care 2014;14:1-18. [DOI: 10.5334/ijic.1549] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davoody 2016 {published data only}
- Davoody N, Koch S, Krakau I, Hägglund M. Post-discharge stroke patients' information needs as input to proposing patient-centred eHealth services. BMC Medical Informatics and Decision Making 2016 Jun 7;16:1-13. [DOI: 10.1186/s12911-016-0307-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deighan 2017 {published data only}
- Deighan C, Michalova L, Pagliari C, Elliott J, Taylor L, Ranaldi H. The Digital Heart Manual: a pilot study of an innovative cardiac rehabilitation programme developed for and with users. Patient Education and Counseling 2017;100(8):1598-607. [DOI: 10.1016/j.pec.2017.03.014] [DOI] [PubMed] [Google Scholar]
Delmar 2009 {published data only}
- Delmar C, Rasmussen B, Dolmer I. Staying in ‘the stream of life’: rehabilitation of older people in their own homes following total hip replacement. International Journal of Older People Nursing 2009;4(4):272-9. [DOI: 10.1111/j.1748-3743.2009.00174.x] [DOI] [PubMed] [Google Scholar]
Demain 2013 {published data only}
- Demain S, Burridge J, Ellis-Hill C, Hughes A, Yardley L, Tedesco-Triccas L, et al. Assistive technologies after stroke: self-management or fending for yourself? A focus group study. Health Services Research 2013;13(1):1-12. [DOI: 10.1186/1472-6963-13-334] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dennett 2020 {published data only}
- Dennett R, Coulter E, Paul L, Freeman J. A qualitative exploration of the participants' experience of a web-based physiotherapy program for people with multiple sclerosis: Does it impact on the ability to increase and sustain engagement in physical activity? Disability and Rehabilitation 2020 Oct;42(21):3007-14. [DOI: 10.1080/09638288.2019.1582717] [DOI] [PubMed] [Google Scholar]
DeVries 2017 {published data only}
- De Vries H, Kloek C, Bakker D, Dekker J, Bossen D, Veenhof C. Determinants of adherence to the online component of a blended intervention for patients with hip and/or knee osteoarthritis: a mixed methods study embedded in the e-exercise trial. TELEMEDICINE and e-HEALTH 2017;23(12):1002-10. [DOI: 10.1089/tmj.2016.0264] [DOI] [PubMed] [Google Scholar]
Dimaguila 2019 {published data only}
- Dimaguila G, Gray K, Merolli M. Patient- reported outcomes of using human-generated health data in sham rehabilitation technology: insights from stroke survivors. Studies in Health Technology and Informatics 2019;264:993-7. [DOI: 10.3233 / SHTI190373] [DOI] [PubMed] [Google Scholar]
Dinesen 2011 {published data only}
- Dinesen B , Seemann J, Gustafsson J. Development of a program for tele-rehabilitation of COPD patients across sectors: co-innovation in a network. International Journal of Integrated Care 2011;11(1):1-12. [DOI: 10.5334/ijic.582] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinesen 2013 {published data only}
- Dinesen B, Huniche L, Toft E. Attitudes of COPD patients towards tele-rehabilitation: a cross-sector case study. International Journal of Environmental Research and Public Health 2013;10(11):6184-98. [DOI: 10.3390/ijerph10116184] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinesen 2018 {published data only}
- Dinesen B, Spindler H. The use of telerehabilitation technologies for cardiac patients to improve rehabilitation activities and unify organizations: qualitative study. JMIR Rehabilitation and Assistive Technologies 2018;5(2):1-11. [DOI: 10.2196/10758] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinesen 2019 {published data only}
- Dinesen B, Nielsen G, Andreasen JJ, Spindler H. Integration of rehabilitation activities into everyday life through telerehabilitation: qualitative study of cardiac patients and their partners. Journal of Medical Internet Research 2019 Apr 15;21(4):1-14. [DOI: 10.2196/13281] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dithmer 2016 {published data only}
- Dithmer M, Rasmussen J, Grönvall E, Spindler H, Hansen J, Nielsen G, et al. “The Heart Game”: using gamification as part of a telerehabilitation program for heart patients. Games for Health Journal 2016;5(1):27-33. [DOI: 10.1089/g4h.2015.0001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dobson 2019 {published data only}
- Dobson R, Herbst P, Candy S, Brott T, Garrett J, Humphrey G, et al. Understanding end-user perspectives of mobile Pulmonary Rehabilitation (mPR): cross-sectional survey and interviews. JMIR Formative Research 2019;3(4):1-11. [DOI: 10.2196/15466] [DOI] [PMC free article] [PubMed] [Google Scholar]
Doig 2009 {published data only}
- Doig E, Fleming J, Cornwell P, Kuipers P. Qualitative exploration of a client-centered, goal-directed approach to community-based occupational therapy for adults with traumatic brain injury. American Journal of Occupational Therapy 2009;63(5):559-68. [DOI: 10.5014/ajot.63.5.559] [DOI] [PubMed] [Google Scholar]
Donoso Brown 2015 {published data only}
- Donoso Brown E, Dudgeon B, Gutman K, Moritz C, McCoy S. Understanding upper extremity home programs and the use of gaming technology for persons after stroke. Disability and Health Journal 2015;8(4):507-13. [PMID: 10.1016/j.dhjo.2015.03.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dow 2007 {published data only}
- Dow B, McDonald J. The invisible contract: shifting care from the hospital to the home. Australian Health Review 2007;31(2):193-202. [DOI: 10.1071/AH070193] [DOI] [PubMed] [Google Scholar]
Dubouloz 2004 {published data only}
- Dubouloz CJ, Laporte D, Hall M, Ashe B, Smith CD. Transformation of meaning perspectives in clients with rheumatoid arthritis. American Journal of Occupational Therapy 2004;58(4):398-407. [DOI: 10.5014/ajot.58.4.398] [DOI] [PubMed] [Google Scholar]
Duggan 2013 {published data only}
- Duggan G, Keogh E, Mountain G, McCullagh P, Leake J, Eccleston C. Qualitative evaluation of the SMART2 self-management system for people in chronic pain. Disability and Rehabilitation: Assistive Technology 2013;10(1):53-60. [DOI: 10.3109/17483107.2013.845696] [DOI] [PubMed] [Google Scholar]
Edbrooke 2020 {published data only}
- Edbrooke L, Denehy L, Granger CL, Kapp S, Aranda S. Home-based rehabilitation in inoperable non-small cell lung cancer—the patient experience. Supportive Care in Cancer 2020;28(1):99-112. [DOI: ] [DOI] [PubMed] [Google Scholar]
Eliassen 2018 {published data only}
- Eliassen M, Henriksen N, Moe S. The practice of support personnel, supervised by physiotherapists, in Norwegian reablement services. Physiotherapy Research International 2018;24(e1754):1-8. [DOI: 10.1002/pri.1754] [DOI] [PubMed] [Google Scholar]
Emmerson 2018 {published data only}
- Emmerson KB, Harding KE, Lockwood KJ, Taylor NF. Home exercise programs supported by video and automated reminders for patients with stroke: A qualitative analysis. Australian Occupational Therapy Journal 2018 Jun;65(3):187-97. [DOI: 10.1111/1440-1630.12461] [DOI] [PubMed] [Google Scholar]
Eriksson 2011 {published data only}
- Eriksson L, Lindström B, Ekenberg L. Patients’ experiences of telerehabilitation at home after shoulder joint replacement. Journal of Telemedicine and Telecare 2011;17(1):25-30. [DOI: 10.1258/jtt.2010.100317] [DOI] [PubMed] [Google Scholar]
Essery 2017 {published data only}
- Essery R, Kirby S, Geraghty A, Yardley L. Older adults’ experiences of internet-based vestibular rehabilitation for dizziness: a longitudinal study. Psychology & Health 2017;32(11):1327–47. [DOI: 10.1080/08870446.2017.1310861] [DOI] [PubMed] [Google Scholar]
Feinberg 2018 {published data only}
- Feinberg J, Russell D, Mola A, Trachtenberg M, Bick I, Lipman T, et al. A Mixed Methods Evaluation of the Feasibility and Acceptability of an Adapted Cardiac Rehabilitation Program for Home Care Patients. Geriatric Nursing 2018;39(2):191–8. [DOI: 10.1016/j.gerinurse.2017.08.006] [DOI] [PubMed] [Google Scholar]
Folan 2015 {published data only}
- Folan A, Barclay L, Cooper C, Robinson M. Exploring the experience of clients with tetraplegia utilizing assistive technology for computer access. Disability and Rehabilitation. Assistive Technology 2015 Jan;10(1):46-52. [DOI: 10.3109/17483107.2013.836686] [DOI] [PubMed] [Google Scholar]
Forman 2014 {published data only}
- Forman D, LaFond K, Panch T, Allsup K, Manning K, Sattelmair J. Utility and efficacy of a smartphone application to enhance the learning and behavior goals of traditional cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention 2014;34(5):327-34. [DOI: 10.1097/HCR.0000000000000058] [DOI] [PubMed] [Google Scholar]
Forsberg 2014 {published data only}
- Forsberg A, Nilsagård Y, Boström K. Perceptions of using videogames in rehabilitation: a dual perspective of people with multiple sclerosis and physiotherapists. Disability and Rehabilitation 2014;34(4):338–44. [DOI: 10.3109/09638288.2014.918196] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frohmader 2015 {published data only}
- Frohmader T, Lin F, Chaboyer W. Patient perceptions of nurse mentors facilitating the Aussie Heart Guide: a home-based cardiac rehabilitation programme for rural patients. Nursing Open 2015;3(1):41-50. [DOI: 10.1002/nop2.34] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frohmader 2017 {published data only}
- Frohmader T, Lin F, Chaboyer W. Structures, processes and outcomes of the Aussie Heart Guide Program: a nurse mentor supported, home based cardiac rehabilitation program for rural patients with acute coronary syndrome. Australian Critical Care 2017;31(2):93-100. [DOI: 10.1016/j.aucc.2017.03.002] [DOI] [PubMed] [Google Scholar]
Frost 2019 {published data only}
- Frost J, Wingham J, Britten N, Greaves C, Abraham C, Warren F, et al. Home-based rehabilitation for heart failure with reduced ejection fraction: mixed methods process evaluation of the REACH-HF multicentre randomised controlled trial. BMJ Open 2019;9(8):1-12. [DOI: 10.1136/bmjopen-2018-026039] [DOI] [PMC free article] [PubMed] [Google Scholar]
Galvin 2014 {published data only}
- Galvin R, Stokes E, Cusack T. Family-Mediated Exercises (FAME): an Exploration of Participant’s Involvement in anNovel form of exercise delivery after stroke. Topics in Stroke Rehabilitation 2014;21(1):63-74. [DOI: 10.1310/tsr2101-63] [DOI] [PubMed] [Google Scholar]
Gélinas‐Bronsard 2019 {published data only}
- Gélinas-Bronsard D, Mortenson WB, Ahmed S, Guay C, Auger C. Co-construction of an Internet-based intervention for older assistive technology users and their family caregivers: stakeholders' perceptions. Disability and Rehabilitation. Assistive Technology 2019 Aug;14(6):602-11. [DOI: 10.1080/17483107.2018.1499138] [DOI] [PubMed] [Google Scholar]
Gell 2019 {published data only}
- Gell N, Tursi A, Grover K, Dittus K. Female cancer survivor perspectives on remote intervention components to support physical activity maintenance. Supportive Care in Cancer 2019;28:2185–94. [DOI: 10.1007/s00520-019-05038-y] [DOI] [PubMed] [Google Scholar]
Giesbrecht 2014 {published data only}
- Giesbrecht E, Miller W, Mitchell I, Woodgate R. Development of a wheelchair skills home program for older adults using a participatory action design approach. BioMed Research International 2014;2014:1-13. [PMID: 10.1155/2014/172434] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gilbert 2019 {published data only}
- Gilbert A, Jaggi A, May C. What is the acceptability of real time 1: 1 videoconferencing between clinicians and patients for a follow-up consultation for multi-directional shoulder instability? Shoulder & Elbow 2019;11(1):53-9. [DOI: 10.1177/1758573218796815] [DOI] [PMC free article] [PubMed] [Google Scholar]
Giunti 2018 {published data only}
- Giunti G, Kool J, Romero O, Zubiete E. Exploring the specific needs of persons with multiple sclerosis for mHealth solutions for physical activity: mixed-methods study. JMIR mHealth and uHealth 2018;6(2):e37. [DOI: 10.2196/mhealth. 8996] [DOI] [PMC free article] [PubMed] [Google Scholar]
Govender 2019 {published data only}
- Govender P, Naidoo D, Bricknell K, Ayob Z, Message H, Njoko S. 'No one prepared me to go home': Cerebrovascular accident survivors' experiences of community reintegration in a peri-urban context. African Journal of Primary Health Care &Family Medicine 2019 Apr 24;11(1):1-8. [DOI: 10.4102/phcfm.v11i1.1806] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustafsson 2014a {published data only}
- Gustafsson L, Fleming J, Cornwell P, Worrall L, Brauer S. STRENGTH and the health care team: Changing interprofessional and client-centered practices. Topics in Stroke Rehabilitation 2014;21(5):413-20. [DOI: 10.1310/tsr2105-413] [DOI] [PubMed] [Google Scholar]
Gustafsson 2014b {published data only}
- Gustafsson L, Hodson T, Fleming, J, Hoyle M. The impact of STRENGTH on the expected and actual transition to home experience. Disability and Rehabilitation 2014;36(26):2244-51. [DOI: 10.3109/09638288.2014.904937] [DOI] [PubMed] [Google Scholar]
Gustafsson 2019 {published data only}
- Gustafsson L, Östlund G, Zander V, Elfström M, Anbäcken E. “Best fit” caring skills of an interprofessional team in short-term goal-directed reablement: older adults’ perceptions. Scandinavian Journal of Caring Sciences 2019;33(2):498-506. [DOI: 10.1111/scs.12650] [DOI] [PubMed] [Google Scholar]
Hale 2005 {published data only}
- Hale L, Piggot J. Exploring the content of physiotherapeutic home-based stroke rehabilitation in New Zealand. Archives of Physical Medicine and Rehabilitation 2005;86(10):1933-40. [DOI: 10.1016/j.apmr.2005.04.011] [DOI] [PubMed] [Google Scholar]
Hale Gallardo 2020 {published data only}
- Hale-Gallardo JL, Kreider CM, Jia H, Castaneda G, Freytes IM, Cowper Ripley DC, et al. Telerehabilitation for rural veterans: a qualitative assessment of barriers and facilitators to implementation. Journal of Multidisciplinary Healthcare 2020 Jul 1;13:559-70. [DOI: 10.2147/JMDH.S247267] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harder 2017 {published data only}
- Harder H, Holroyd P, Burkinshaw L, Watten P, Zammit C, Harris P, et al. A user-centred approach to developing bWell, a mobile app for arm and shoulder exercises after breast cancer treatment. Journal of Cancer Survivorship 2017;11(6):732-42. [DOI: 10.1007/s11764-017-0630-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hathiramani 2019 {published data only}
- Hathiramani S, Pettengell R, Moir H, Younis A. Lymphoma survivors’ experience of participation in a home-based intervention post-chemotherapy. Quality of Life Research 2019;28(11):2951-5. [DOI: 10.1007/s11136-019-02244-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayward 2015 {published data only}
- Hayward K, Neibling B, Barker R. Self-administered, home-based SMART (sensorimotor active rehabilitation training) arm training: a single-case report. American Journal of Occupational Therapy 2015;69(4):6904210020p1-8. [DOI: 10.5014/ajot.2015.016055] [DOI] [PubMed] [Google Scholar]
Herber 2017 {published data only}
- Herber O, Smith K, White M, Jones M. ‘Just not for me’–contributing factors to nonattendance/noncompletion at phase III cardiac rehabilitation in acute coronary syndrome patients: a qualitative enquiry. Journal of Clinical Nursing 2017;26(21):3529-42. [DOI: 10.1111/jocn.13722] [DOI] [PubMed] [Google Scholar]
Heron 2019 {published data only}
- Heron N, Kee F, Mant J, Cupples M, Donnelly M. Rehabilitation of patients after transient ischaemic attack or minor stroke: pilot feasibility randomised trial of a home-based prevention programme. British Journal of General Practice 2019;69(687):e706-e714. [DOI: 10.3399/bjgp19X705509] [DOI] [PMC free article] [PubMed] [Google Scholar]
HeydariKhayat 2020 {published data only}
- HeydariKhayat N, Ashktorab T, Rohani C. Home care for burn survivors: a phenomenological study of lived experiences. Home health care services quarterly 2020;40(3):1-14. [DOI: 10.1080/01621424.2020.1749206] [DOI] [PubMed] [Google Scholar]
Higgins 2017 {published data only}
- Higgins R, Rogerson M, Murphy B, Navaratnam H, Mayordomo M, Barker L, et al. Cardiac Rehabilitation Online Pilot: extending reach of cardiac rehabilitation. Journal of Cardiovascular Nursing 2017;32(1):7-13. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hill 2016 {published data only}
- Hill A, Breslin H. Refining an asynchronous telerehabilitation platform for speech-language pathology: engaging end-users in the process. Frontiers in Human Neuroscience 2016;10:640. [DOI: 10.3389/fnhum.2016.00640] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hines 2017 {published data only}
- Hines M, Brunner M, Poon S, Lam M, Tran V, Yu D, et al. Tribes and tribulations: interdisciplinary eHealth in providing services for people with a traumatic brain injury (TBI). BMC Health Services Research 2017;17(1):1-13. [DOI: 10.1186/s12913-017-2721-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hjelle 2017 {published data only}
- Hjelle K, Tuntland H, Førland O, Alvsvåg H. Driving forces for home‐based reablement; a qualitative study of older adults’ experiences. Health & Ssocial Care in the Community 2017;25(5):1581-9. [DOI: 10.1111/hsc.12324] [DOI] [PubMed] [Google Scholar]
Hoaas 2016 {published data only}
- Hoaas H, Andreassen HK, Lien LA, Hjalmarsen A, Zanaboni P. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Medical Informatics and Decision Making 2016 Feb 25;16:26. [DOI: 10.1186/s12911-016-0264-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffman 2017 {published data only}
- Hoffman A, Brintnall R. A Home-based exercise intervention for non–small cell lung cancer patients post-thoracotomy. In Seminars in Oncology Nursing 2017;33(1):106-17. [EMBASE: 10.1016/j.soncn.2016.11.011] [DOI] [PubMed] [Google Scholar]
Hwang 2017 {published data only}
- Hwang R, Mandrusiak A, Morris N, Peters R, Korczyk D, Bruning J, et al. Exploring patient experiences and perspectives of a heart failure telerehabilitation program: a mixed methods approach. Heart & Lung 2017;46(4):320-7. [DOI: 10.1016/j.hrtlng.2017.03.004] [DOI] [PubMed] [Google Scholar]
Inskip 2018 {published data only}
- Inskip J, Lauscher H, Li L, Dumont G, Garde A, Ho K, et al. Patient and health care professional perspectives on using telehealth to deliver pulmonary rehabilitation. ChronicRrespiratory Disease 2018;15(1):71-80. [DOI: 10.1177/1479972317709643] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jakobsen 2018 {published data only}
- Jakobsen F, Vik K. Health professionals’ perspectives of next of kin in the context of reablement. Disability and Rehabilitation 2018;41(16):1882-9. [DOI: 10.1080/09638288.2018.1450452] [DOI] [PubMed] [Google Scholar]
James 2018 {published data only}
- James N, Power E, Hogden A, Vucic S. Patients’ perspectives of multidisciplinary home-based e-Health service delivery for motor neurone disease. Disability and Rehabilitation: Assistive Technology 2018;14(7):737-43. [DOI: 10.1080/17483107.2018.1499139] [DOI] [PubMed] [Google Scholar]
Jansen‐Kosterink 2019 {published data only}
- Jansen-Kosterink S, Dekker-van Weering M, van Velsen L. Patient acceptance of a telemedicine service for rehabilitation care: a focus group study. International Jurnal of Medical Informatics 2019;125:22-9. [DOI: 10.1016/j.ijmedinf.2019.01.011] [DOI] [PubMed] [Google Scholar]
Jäppinen 2017 {published data only}
- Jäppinen A, Hämäläinen H, Kettunen T, Piirainen A. Postoperative patient education in physiotherapy after hip arthroplasty: patients' perspective. Musculoskeletal Care 2017;15(2):150-7. [DOI: 10.1002/msc.1153] [DOI] [PubMed] [Google Scholar]
Jelin 2012 {published data only}
- Jelin E, Granum V, Eide H. Experiences of a web-based nursing intervention—interviews with women with chronic musculoskeletal pain. Pain Management Nursing 2012;13(1):2-10. [DOI: 10.1016/j.pmn.2011.08.008] [DOI] [PubMed] [Google Scholar]
Jones 2007 {published data only}
- Jones M, Jolly K, Raftery J, Lip G, Greenfield S. ‘DNA’may not mean ‘did not participate’: a qualitative study of reasons for non-adherence at home-and centre-based cardiac rehabilitation. Family Practice 2007;24(4):343357. [DOI: 10.1093/fampra/cmm021] [DOI] [PubMed] [Google Scholar]
Jones 2017 {published data only}
- Jones F, McKevitt C, Riazi A, Liston M. How is rehabilitation with and without an integrated self-management approach perceived by UK community-dwelling stroke survivors? A qualitative process evaluation to explore implementation and contextual variations. BMJ Open 2017;7(4):1-11. [DOI: 10.1136/bmjopen-2016-014109] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jullamate 2007 {published data only}
- Jullamate P, from A, Rosenberg E, Pàul C, Subgranon R. Informal stroke rehabilitation: what are the main reasons of Thai caregivers? International Journal of Rehabilitation Research 2007;30(4):315-20. [DOI: 10.1097 / MRR.0b013e3282f14539] [DOI] [PubMed] [Google Scholar]
Kairy 2013 {published data only}
- Kairy D, Tousignant M, Leclerc N, Côté A, Levasseur M. The patient’s perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. International Journal of Environmental Research and Public Health 2013;10(9):3998-4011. [DOI: 10.3390/ijerph10093998] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kairy 2014 {published data only}
- Kairy D, Lehoux P, Vincent C. Exploring routine use of telemedicine through a case study in rehabilitation. Revista Panamericana de Salud Pública 2014;35:337-44. [PMID: ] [PubMed] [Google Scholar]
Kamwesiga 2017 {published data only}
- Kamwesiga JT, Tham K, Guidetti S. Experiences of using mobile phones in everyday life among persons with stroke and their families in Uganda - a qualitative study. Disability and Rehabilitation 2017 Mar;39(5):438-49. [DOI: 10.3109/09638288.2016.1146354] [DOI] [PubMed] [Google Scholar]
Kingston 2014 {published data only}
- Kingston G, Judd J, Gray M. The experience of medical and rehabilitation intervention for traumatic hand injuries in rural and remote North Queensland: a qualitative study. Disability and Rehabilitation 2014;37(5):423-9. [DOI: 10.3109/09638288.2014.923526] [DOI] [PubMed] [Google Scholar]
Knudsen 2019 {published data only}
- Knudsen MV, Laustsen S, Petersen AK, Hjortdal VE, Angel S. Experience of cardiac tele-rehabilitation: analysis of patient narratives. Disability and Rehabilitation 2019;43(3):370-7. [DOI: 10.1080/09638288.2019.1625450] [DOI] [PubMed] [Google Scholar]
Krishnan 2018 {published data only}
- Krishnan S, Pappadis M, Weller S, Fisher S, Hay C, Reistetter T. Patient-centered mobility outcome preferences according to individuals with stroke and caregivers: a qualitative analysis. Disability and Rehabilitation 2018;40(12):1401-9. [DOI: 10.1080/09638288.2017.1297855] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lahham 2017 {published data only}
- Lahham A, McDonald C, Mahal A, Lee A, Hill C, Burge A, Holland A. Home-based pulmonary rehabilitation for people with COPD: A qualitative study reporting the patient perspective. ChronicRrespiratory Disease 2017;15(2):123-30. [DOI: 10.1177/1479972317729050] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lai 2019 {published data only}
- Lai B, Wilroy J, Young H, Howell J, Rimmer J, Mehta T, Thirumalai M. A Mobile App to Promote Adapted Exercise and Social Networking for People With Physical Disabilities: Usability Study. JMIR Form Res 2019;3(1):e11689. [DOI: 10.2196/11689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawford 2018a {published data only}
- Lawford B, Delany C, Bennell K, Hinman R. “I Was Really Pleasantly Surprised”: firsthand experience and shifts in physical therapist perceptions of telephone‐delivered exercise therapy for knee osteoarthritis–a qualitative study. Arthritis Care & Research 2018;71(4):545-57. [DOI: 10.1002/acr.23618] [DOI] [PubMed] [Google Scholar]
Lawford 2018b {published data only}
- Lawford B, Delany C, Bennell K, Hinman R. “I was really sceptical... But it worked really well”: a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis and Cartilage 2018;26(6):741-50. [DOI: 10.1016/j.joca.2018.02.909] [DOI] [PubMed] [Google Scholar]
Lawson 2020 {published data only}
- Lawson DW, Stolwyk RJ, Ponsford JL, Baker KS, Tran J, Wong D. Acceptability of telehealth in post-stroke memory rehabilitation: A qualitative analysis. Neuropsychological Rehabilitation 2020 Jul 17;1:1-21. [DOI: 10.1080/09602011.2020.1792318] [DOI] [PubMed] [Google Scholar]
Learmonth 2019 {published data only}
- Learmonth Y, Kinnett-Hopkins D, Motl R. Capitalising on the opinions of persons with multiple sclerosis to inform the main trial–participant opinions from participation in a feasibility study, a qualitative extension study. Disability and Rehabilitation 2019;41(25):3071-8. [DOI: 10.1080/09638288.2018.1490823] [DOI] [PubMed] [Google Scholar]
Lee 2009 {published data only}
- Lee C, Herridge M, Matte A, Cameron J. Education and support needs during recovery in acute respiratory distress syndrome survivors. Critical Care 2009;13(5):1-11. [DOI: 10.1186 / cc8053] [DOI] [PMC free article] [PubMed] [Google Scholar]
Letts 2011 {published data only}
- Letts L, Ginis K, Faulkner G, Colquhoun H, Levac D, Gorczynski P. Preferred methods and messengers for delivering physical activity information to people with spinal cord injury: a focus group study. Rehabilitation Psychology 2011;56(2):128-37. [DOI: 10.1037/a0023624] [DOI] [PubMed] [Google Scholar]
Lindblom 2020 {published data only}
- Lindblom S, Ytterberg C, Elf M, Flink M. Perceptive dialogue for linking stakeholders and units during care transitions–a qualitative study of people with stroke, significant others and healthcare professionals in Sweden. International Journal of Integrated Care 2020;20(1):11. [DOI: 10.5334/ijic.4689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lou 2017 {published data only}
- Lou S, Carstensen K, Moeldrup M, Shahla S, Zakharia E, Nielsen CP. Early supported discharge following mild stroke: a qualitative study of patients’ and their partners’ experiences of rehabilitation at home. Scand Journal of Caring Sciences 2017;31(2):302-11. [DOI: 10.1111/scs.12347] [DOI] [PubMed] [Google Scholar]
Lovo 2019 {published data only}
- Lovo S, Harrison L, O'connell M, Trask C, Bath B. Experience of patients and practitioners with a team and technology approach to chronic back disorder management. Journal of Multidisciplinary Healthcare 2019;12:855-69. [DOI: 10.2147/JMDH.S208888] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lovo Grona 2017 {published data only}
- Lovo Grona S, Bath B, Bustamante L, Mendez I. Case report: using a remote presence robot to improve access to physical therapy for people with chronic back disorders in an underserved community. Physiotherapy Canada 2017;69(1):14-9. [DOI: 10.3138/ptc.2015-77] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lutz 2009 {published data only}
- Lutz B, Chumbler N, Lyles T, Hoffman N, Kobb R. Testing a home-telehealth programme for US veterans recovering from stroke and their family caregivers. Disability and Rehabilitation 2009;31(5):402-9. [DOI: 10.1080/09638280802069558] [DOI] [PubMed] [Google Scholar]
Lykke 2019 {published data only}
- Lykke S, Handberg C. Experienced loneliness in home-based rehabilitation: Perspectives of older adults with disabilities and their health care professionals. Global Qualitative Nursing Research 2019;6:1-12. [EMBASE: 10.1177/2333393619831661] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madden 2010 {published data only}
- Madden M, Furze G, Lewin R. Complexities of patient choice in cardiac rehabilitation: qualitative findings. Journal of Advanced Nnursing 2010;67(3):540-9. [DOI: 10.1111/j.1365-2648.2010.05509.x] [DOI] [PubMed] [Google Scholar]
Magne 2020 {published data only}
- Magne T, Vik K. Promoting participation in daily activities through reablement: a qualitative study. Rehabilitation Research and Practice 2020;2020:1-7. [DOI: 10.1155/2020/6506025] [DOI] [PMC free article] [PubMed] [Google Scholar]
Malmberg 2018 {published data only}
- Malmberg M, Sundewall Thorén E, Öberg M, Lunner T, Andersson G, Kähäri K. Experiences of an Internet-based aural rehabilitation (IAR) program for hearing aid users: a qualitative study. International Journal of Audiology 2018 Aug;57(8):570-6. [DOI: 10.1080/14992027.2018.1453171] [DOI] [PubMed] [Google Scholar]
Markle‐Reid 2020 {published data only}
- Markle-Reid, M, Valaitis R, Bartholomew A, Fisher K, Fleck R, Ploeg J, et al. An integrated hospital-to-home transitional care intervention for older adults with stroke and multimorbidity: a feasibility study. Journal of Comorbidity 2020;10:1-21. [DOI: 10.1177/2235042X19900451] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2018 {published data only}
- Martin S, Armstrong E, Thomson E, Vargiu E, Solà M, Dauwalder S, et al. A qualitative study adopting a user-centered approach to design and validate a brain computer interface for cognitive rehabilitation for people with brain injury. Assistive Technology 2018;30(5):233-41. [DOI: 10.1080/10400435.2017.1317675] [DOI] [PubMed] [Google Scholar]
Martinez 2017 {published data only}
- Martinez RN, Hogan TP, Lones K, Balbale S, Scholten J, Bidelspach D, et al. Evaluation and treatment of mild traumatic brain injury through the implementation of clinical video telehealth: provider perspectives from the Veterans Health Administration. PM&R: the journal of imjury, function and rehabilitation 2017;9(3):231-40. [DOI: ] [DOI] [PubMed] [Google Scholar]
Marwaa 2020 {published data only}
- Marwaa MN, Ytterberg C, Guidetti S. Significant others' perspectives on person-centred information and communication technology in stroke rehabilitation - a grounded theory study. Disability andRrehabilitation 2020;42(15):2115-22. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mawson 2014 {published data only}
- Mawson S, Nasr N, Parker J, Zheng H, Davies R, Mountain G. Developing a personalised self-management system for post stroke rehabilitation; utilising a user-centred design methodology. Disability and Rehabilitation: Assistive Technology 2014;9(6):521-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mawson 2016 {published data only}
- Mawson S, Nasr N, Parker J, Davies R, Zheng H, Mountain G. A personalized self-management rehabilitation system with an intelligent shoe for stroke survivors: a realist evaluation. JMIR rehabilitation and assistive technologies 2016;3(1):e5079. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mendell 2019 {published data only}
- Mendell J, Bates J, Banner-Lukaris D, Horvat D, Kang B, Singer J, et al. What do patients talk about? A qualitative analysis of online chat sessions with health care specialists during a "Virtual" Cardiac Rehabilitation Program. Telemedicien Journal and E-Health 2019 Jan;25(1):71-8. [DOI: 10.1089/tmj.2017.0206] [DOI] [PubMed] [Google Scholar]
Moe 2016 {published data only}
- Moe A, Brataas HV. Interdisciplinary collaboration experiences in creating an everyday rehabilitation model: a pilot study. Journal of Multidisciplinary Healthcare 2016;9:173. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moe 2017 {published data only}
- Moe C, Brinchmann BS. Tailoring reablement: A grounded theory study of establishing reablement in a community setting in Norway. Health & Social Ccare in the Community 2018;26(1):113-21. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mohd Nordin 2014 {published data only}
- Mohd Nordin NA, Aziz NA, Abdul Aziz AF, Ajit Singh DK, Omar Othman NA, Sulong S, et al. Exploring views on long term rehabilitation for people with stroke in a developing country: findings from focus group discussions. BMC Health Services Research 2014 Mar 10;14(1):1-10. [DOI: 10.1186/1472-6963-14-118] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moraal 2013 {published data only}
- Moraal M, Slatman J, Pieters T, Mert A, Widdershoven G. A virtual rehabilitation program after amputation: a phenomenological exploration. Disability and Rehabilitation: Assistive Technology 2013;8(6):511-5. [DOI: ] [DOI] [PubMed] [Google Scholar]
Muller 2014 {published data only}
- Muller I, Kirby S, Yardley L. The therapeutic relationship in telephone-delivered support for people undertaking rehabilitation: a mixed-methods interaction analysis. Disability and Rehabilitation 2015;37(12):1060-5. [DOI: ] [DOI] [PubMed] [Google Scholar]
Nanninga 2015 {published data only}
- Nanninga CS, Meijering L, Schönherr MC, Postema K, Lettinga AT. Place attachment in stroke rehabilitation: a transdisciplinary encounter between cultural geography, environmental psychology and rehabilitation medicine. Disability and Rehabilitation 2015;37(13):1125-34. [DOI: ] [DOI] [PubMed] [Google Scholar]
Nasr 2015 {published data only}
- Nasr N, Leon B, Mountain G, Nijenhuis SM, Prange G, Sale P, et al. The experience of living with stroke and using technology: opportunities to engage and co-design with end users. Disability and Rehabilitation: Assistive Technology 2015;11(8):653-60. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ng 2013 {published data only}
- Ng EM, Polatajko HJ, Marziali E, Hunt A, Dawson DR. Telerehabilitation for addressing executive dysfunction after traumatic brain injury. Brain Injury 2013;27(5):548-64. [DOI: 10.3109/02699052.2013.766927] [DOI] [PubMed] [Google Scholar]
Nordin 2015 {published data only}
- Nordin A, Sunnerhagen KS, Axelsson AB. Patients’ expectations of coming home with very early supported fischarge and home rehabilitation after stroke-an interview study. BMC Neurology 2015;15(1):1-9. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nordin 2017 {published data only}
- Nordin C, Michaelson P, Eriksson MK, Gard G. It's About Me: patients' experiences of patient participation in the web behavior change program for activity in combination with multimodal pain rehabilitation. Journal of Medical Internet Research 2017;19(1):e22. [DOI: 10.2196/jmir.5970] [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Doherty 2013 {published data only}
- O'Doherty E. Nurses’ role in care home rehabilitation. Nursing times 2013;109(29):18-21. [ACCESION NUMBER: 00006203-201307240-00006] [PubMed] [Google Scholar]
O'Hara 2015 {published data only}
- O'Hara R, Jackson S. Integrating telehealth services into a remote allied health service: a pilot study. Australian Journal of Rural Health 2017;25(1):53-7. [DOI: ] [DOI] [PubMed] [Google Scholar]
O'Shea 2020 {published data only}
- O'Shea O, Woods C, McDermott L, Buys R, Cornelis N, Claes J, et al. A qualitative exploration of cardiovascular disease patients' views and experiences with an eHealth cardiac rehabilitation intervention: the PATHway Project. PLOS One 2020 Jul 6;15(7):1-17. [DOI: 10.1371/journal.pone.0235274] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ouegnin 2018 {published data only}
- Ouegnin A, Valdes K. Client preferences and perceptions regarding a written home exercise program or video self-modeling: a cross-sectional study. Journal of Hand Therapy 2018;33(1):67-72. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ownsworth 2020 {published data only}
- Ownsworth T, Theodoros D, Cahill L, Vaezipour A, Quinn R, Kendall M, et al. Perceived usability and acceptability of videoconferencing for delivering community-based rehabilitation to individuals with acquired brain injury: a qualitative investigation. Journal of International Neuropsychological Society 2020 Jan;26(1):47-57. [DOI: 10.1017/S135561771900078X] [DOI] [PubMed] [Google Scholar]
Oyesanya 2019 {published data only}
- Oyesanya TO, Thompson N, Arulselvam K, Seel RT. Technology and TBI: perspectives of persons with TBI and their family caregivers on technology solutions to address health, wellness, and safety concerns. Assistive Technology 2019 May 21;33(4):1-11. [DOI: 10.1080/10400435.2019.1612798] [DOI] [PubMed] [Google Scholar]
Palacios‐Ceña 2016 {published data only}
- Palacios-Cena D, Ortiz-Gutierrez RM, Buesa-Estellez A, Galan-Del-Rio F, Cachon Perez JM, Martinez-Piedrola R, et al. Multiple sclerosis patients' experiences in relation to the impact of the kinect virtual home-exercise programme: a qualitative study. European Journal of Physical and Rehabilitation Medicine 2016;52(3):347-55. [PMID: ] [PubMed] [Google Scholar]
Palazzo 2016 {published data only}
- Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, et al. Barriers to home-based exercise program adherence with chronic low back pain: patient expectations regarding new technologies. Annals of Physical Rehabilitation Medicine 2016 Apr;59(2):107-13. [DOI: 10.1016/j.rehab.2016.01.009] [DOI] [PubMed] [Google Scholar]
Palmcrantz 2017 {published data only}
- Palmcrantz S, Borg J, Sommerfeld D, Plantin J, Wall A, Ehn M, et al. An interactive distance solution for stroke rehabilitation in the home setting - a feasibility study. Informatics for Health & Social Care 2017 Sep;42(3):303-20. [DOI: 10.1080/17538157.2016.1253015] [DOI] [PubMed] [Google Scholar]
Pancer 2019 {published data only}
- Pancer M, Manganaro M, Pace I, Marion P, Gagnon DH, Laramée MT, et al. A web-based physical activity portal for individuals living with a spinal cord injury: qualitative study. JMIR formative Research 2019;3(3):e12507. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pani 2016 {published data only}
- Pani D, Piga M, Barabino G, Crabolu M, Uras S, Mathieu A, et al. Home tele-rehabilitation for rheumatic patients: impact and satisfaction of care analysis. Journal ofTtelemedicine and Telecare 2016;23(2):292-300. [DOI: ] [DOI] [PubMed] [Google Scholar]
Parker 2014 {published data only}
- Parker J, Mawson S, Mountain G, Nasr N, Zheng H. Stroke patients’ utilisation of extrinsic feedback from computer-based technology in the home: a multiple case study realistic evaluation. BMC Medical Informatics and Decision Making 2014;14(1):1-13. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2020 {published data only}
- Parker AM, Nelliot A, Chessare CM, Malik AM, Koneru M, Hosey MM, et al. Usability and acceptability of a mobile application prototype for a combined behavioural activation and physical rehabilitation intervention in acute respiratory failure survivors. Australian Critical Care 2020;33(6):511-7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Parsons 2018 {published data only}
- Parsons JG, Plant SE, Slark J, Tyson SF. How active are patients in setting goals during rehabilitation after stroke? A qualitative study of clinician perceptions. Disability and Rehabilitation 2018;40(3):309-16. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pasipanodya 2020 {published data only}
- Pasipanodya EC, Shem K. Provision of care through telemedicine during a natural disaster: a case study. Spinal Cord Series and Cases 2020;6(1):1-5. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Paul 2014 {published data only}
- Paul L, Coulter EH, Miller L, McFadyen A, Dorfman J, Mattison PG. Web-based physiotherapy for people moderately affected with Multiple Sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clinical Rehabilitation 2014;28(9):924-35. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pauwels 2018 {published data only}
- Pauwels C, Roren A, Gautier A, Linières J, Rannou F, Poiraudeau S, et al. Home-based cycling program tailored to older people with lumbar spinal stenosis: Barriers and facilitators. Annals of Physical and Rehabilitation Medicine 2018;61(3):144-50. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pearson 2016 {published data only}
- Pearson J, Walsh N, Carter D, Koskela S, Hurley M. Developing a web-based version of an exercise-based rehabilitation program for people with chronic knee and hip pain: a mixed methods study. JMIR Research Protocols 2016;5(2):e5446. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekmezaris 2020 {published data only}
- Pekmezaris R, Kozikowski A, Pascarelli B, Wolf-Klein G, Boye-Codjoe E, Jacome S, et al. A Telehealth-delivered Pulmonary Rehabilitation Intervention in underserved Hispanic and African American patients With Chronic obstructive pulmonary disease: a community-based participatory research approach. JMIR Formative Research 2020 Jan 31;4(1):1-8. [DOI: 10.2196/13197] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pettersson 2010 {published data only}
- Pettersson I, Fahlström G. Roles of assistive devices for home care staff in Sweden: a qualitative study. Disability and Rehabilitation: Assistive Technology 2010;5(5):295-304. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pfaeffli 2012 {published data only}
- Pfaeffli L, Maddison R, Whittaker R, Stewart R, Kerr A, Jiang Y, et al. A mHealth cardiac rehabilitation exercise intervention: findings from content development studies. BMC Cardiovascular Disorders 2012;12(1):1-9. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
PfaeffliDale 2015 {published data only}
- Pfaeffli Dale L, Whittaker R, Dixon R, Stewart R, Jiang Y, Carter K, et al. Acceptability of a mobile health exercise-based cardiac rehabilitation intervention. Journal of Cardiopulmonary Rehabilitation and Prevention 2015;35(5):312-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pierce 2004 {published data only}
- Pierce LL, Steiner V, Govoni AL, Hicks B, Thompson TL, Friedemann ML. Internet‐based support for rural caregivers of persons with stroke shows promise. Rehabilitation Nursing 2004;29(3):95-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pierce 2006 {published data only}
- Pierce LL, Steiner V, Hicks B, Holzaepfel AL. Problems of new caregivers of persons with stroke. Rehabilitation Nursing 2006;31(4):166-72. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pierce 2015 {published data only}
- Pierce LL, Steiner V, de Dios AM, Vollmer M, Govoni AL, Thompson T. Qualitative analysis of a nurse's responses to stroke caregivers on a web-based supportive intervention. Topics in stroke Rehabilitation 2015;22(2):152-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Pinto 2014 {published data only}
- Pinto JM, Martín-Nogueras A, Nations M. Illness experiences of persons with chronic obstructive pulmonary disease: self-perceived efficacy of home-based pulmonary rehabilitation. Cadernos de Saude Publica 2014 Jun;30(6):1270-80. [DOI: 10.1590/0102-311x00072313] [DOI] [PubMed] [Google Scholar]
Plow 2013 {published data only}
- Plow M, Finlayson M. A qualitative study exploring the usability of Nintendo Wii Fit among persons with multiple sclerosis. OccupationalTtherapy International 2013;21(1):21-32. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ranaldi 2018 {published data only}
- Ranaldi H, Deighan C, Taylor L. Exploring patient-reported outcomes ofhome-based cardiac rehabilitation inrelation to Scottish, UK and Europeanguidelines: an audit usingqualitative methods. BMJ Open 2018 Dec 16;8(12):1-10. [DOI: 10.1136/bmjopen-2018-024499] [DOI] [PMC free article] [PubMed] [Google Scholar]
Randall 2008 {published data only}
- Randall GE. The impact of managed competition on diversity, innovation and creativity in the delivery of home‐care services. Health & Social Care in the Community 2008;16(4):347-53. [DOI: ] [DOI] [PubMed] [Google Scholar]
Randström 2012 {published data only}
- Randström KB, Asplund K, Svedlund M. Impact of environmental factors in home rehabilitation--a qualitative study from the perspective of older persons using the International Classification of Functioning, Disability and Health to describe facilitators and barriers. Disability and Rehabilitation 2012;34(9):779-87. [DOI: 10.3109/09638288.2011.619621] [DOI] [PubMed] [Google Scholar]
Randstrom 2013 {published data only}
- Randström KB, Asplund K, Svedlund M, Paulson M. Activity and participation in home rehabilitation: older people's and family members' perspectives. Journal of Rehabilitation Medicine 2013 Feb;45(2):211-6. [DOI: 10.2340/16501977-1085] [DOI] [PubMed] [Google Scholar]
Randström 2014 {published data only}
- Randström KB, Wengler Y, Asplund K, Svedlund M. Working with 'hands-off' support: a qualitative study of multidisciplinary teams' experiences of home rehabilitation for older people. International Journal of Older People Nursing 2014 Mar;9(1):25-33. [DOI: 10.1111/opn.12013] [DOI] [PubMed] [Google Scholar]
Rayce 2020 {published data only}
- Rayce K, Rosenbek Minet L, Kidholm K, Vestbo J, Pedersen CD, Huniche L. Telemediated training in the home as a part of the everyday life and practice with very severe chronic obstructive pulmonary disease. Qualitative Health Research 2020;30(13):2132-45. [DOI: ] [DOI] [PubMed] [Google Scholar]
Reunanen 2016 {published data only}
- Reunanen MA, Järvikoski A, Talvitie U, Pyöriä O, Härkäpää K. Individualised home‐based rehabilitation after stroke in eastern Finland–the client's perspective. Health & Social Care in the Community 2016;24(1):77-85. [DOI: ] [DOI] [PubMed] [Google Scholar]
Rietdijk 2020 {published data only}
- Rietdijk R, Power E, Attard M, Togher L. Acceptability of telehealth-delivered rehabilitation: Experiences and perspectives of people with traumatic brain injury and their carers. Journal of Telemedicine and Telecare 2020 May 28;0(0):1-13. [DOI: 10.1177/1357633X20923824] [DOI] [PubMed] [Google Scholar]
Rizzo 2019 {published data only}
- Rizzo J, Bell A. Mental models of adherence: parallels in perceptions, values, and expectations in adherence to prescribed home exercise programs and other personal regimens. Disability and Rehabilitation 2019 Oct;41(20):2412-20. [DOI: 10.1080/09638288.2018.1466923] [DOI] [PubMed] [Google Scholar]
Rothgangel 2017 {published data only}
- Rothgangel A, Braun S, Smeets R, Beurskens A. Design and development of a telerehabilitation platform for patients with phantom limb pain: a user-centered approach. JMIR Rehabilitation and Assistive Technologies 2017;4(1):e6761. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sankaran 2019 {published data only}
- Sankaran S, Dendale P, Coninx K. Evaluating the impact of the HeartHab App on motivation, physical activity, quality of life, and risk factors of coronary artery disease patients: multidisciplinary crossover study. JMIR Mhealth Uhealth 2019;7(4):e10874. [DOI: 10.2196/10874] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saywell 2015 {published data only}
- Saywell N, Taylor D. Focus group insights assist trial design for stroke telerehabilitation: a qualitative study. Physiotherapy Theory and Practice 2015 Mar;13(3):160-5. [DOI: 10.3109/09593985.2014.982234] [DOI] [PubMed] [Google Scholar]
Schopfer 2020 {published data only}
- Schopfer DW, Nicosia FM, Ottoboni L, Whooley MA. Patient perspectives on declining to participate in home-based cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention 2020 Sep;40(5):335-40. [DOI: 10.1097/HCR.0000000000000493] [DOI] [PubMed] [Google Scholar]
Serpanou 2019 {published data only}
- Serpanou I, Sakellari E, Psychogiou M, Zyga S, Sapountzi-Krepia D. Physical therapists’ perceptions about patients with incomplete post-traumatic paraplegia adherence to recommended home exercises: a qualitative study. Brazilian Journal of Physical Therapy 2019;23(1):33-40. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shirai 2020 {published data only}
- Shirai T, Bulandres P, Choi JA, D’Ortenzio D, Moon N, Musselman K, et al. The use of a mobile educational tool on pressure injury education for individuals living with spinal cord injury/disease: a qualitative research study. Disability and Rehabilitation 2020;4:1-10. [DOI: 10.1080/09638288.2020.1771780] [DOI] [PubMed] [Google Scholar]
Shulver 2016 {published data only}
- Shulver W, Killington M, Crotty M. 'Massive potential' or 'safety risk'? Health worker views on telehealth in the care of older people and implications for successful normalization. BMC Medical Informatics and Decision Making 2016 Oct 12;16(1):1-15. [DOI: 10.1186/s12911-016-0373-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shulver 2017 {published data only}
- Shulver W, Killington M, Morris C, Crotty M. 'Well, if the kids can do it, I can do it': older rehabilitation patients' experiences of telerehabilitation. Health Expectations 2017 Feb;20(1):120-9. [DOI: 10.1111/hex.12443] [DOI] [PMC free article] [PubMed] [Google Scholar]
Silveira 2019 {published data only}
- Silveira SL, Richardson EV, Motl RW. Informing the design of exercise programs for persons with multiple sclerosis who use wheelchairs: a qualitative inquiry of perceived components. Disability and Rehabilitation 2019 Oct 16;43(13):1-11. [DOI: 10.1080/09638288.2019.1678073] [DOI] [PubMed] [Google Scholar]
Silver 2012 {published data only}
- Silver J, Ljungberg I, Libin A, Groah S. Barriers for individuals with spinal cord injury returning to the community: a preliminary classification. Disability and Health Journal 2012;5(3):190-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Sivan 2014 {published data only}
- Sivan M, Gallagher J, Holt R, Weightman A, Levesley M, Bhakta B. Investigating the international classification of functioning, disability, and health (ICF) framework to capture user needs in the concept stage of rehabilitation technology development. Assistive Technology 2014;26(3):164-73. [DOI: ] [DOI] [PubMed] [Google Scholar]
Smaerup 2017 {published data only}
- Smærup M, Grönvall E, Larsen SB, Laessoe U, Henriksen JJ, Damsgaard EM. Exercise gaming–a motivational approach for older adults with vestibular dysfunction. Disability and Rehabilitation: Assistive Technology 2017;12(2):137-44. [DOI: ] [DOI] [PubMed] [Google Scholar]
Spasić 2015 {published data only}
- Spasić I, Button K, Divoli A, Gupta S, Pataky T, Pizzocaro D, et al. TRAK app suite: a web-based intervention for delivering standard care for the rehabilitation of knee conditions. JMIR Research Protocols 2015;4(4):e122. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Standen 2015 {published data only}
- Standen PJ, Threapleton K, Connell L, Richardson A, Brown D J, Battersby S, et al. Patients' use of a home-based virtual reality system to provide rehabilitation of the upper limb following stroke. Physical Therapy 2015;93(3):350-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Stark 2019 {published data only}
- Stark A, Färber C, Tetzlaff B, Scherer M, Barzel A. Stroke patients' and non-professional coaches' experiences with home-based constraint-induced movement therapy: a qualitative study. Clinical Rehabilitation 2019 Sep;33(9):1527-39. [DOI: 10.1177/0269215519848813] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steihaug 2014 {published data only}
- Steihaug S, Lippestad JW, Isaksen H, Werner A. Development of a model for organisation of and cooperation on home-based rehabilitation–an action research project. Disability and Rehabilitation 2014;36(7):608-16. [DOI: ] [DOI] [PubMed] [Google Scholar]
Steihaug 2016 {published data only}
- Steihaug S, Lippestad JW, Werner A. Between ideals and reality in home-based rehabilitation. Scandinavian Journal of Primary Health Care 2016; 34(1):46-54. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stuifbergen 2011 {published data only}
- Stuifbergen A, Becker H, Morgan S, Morrison J, Perez F. Home-based computer-assisted cognitive training: feasibility and perceptions of people with multiple sclerosis. International Journal of MS Care 2011 Jan 1;13(4):189-98. [DOI: 10.7224/1537-2073-13.4.189] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sturkenboom 2016 {published data only}
- Sturkenboom IH, Nijhuis-van der Sanden MW, Graff MJ. A process evaluation of a home-based occupational therapy intervention for Parkinson’s patients and their caregivers performed alongside a randomized controlled trial. Clinical Rehabilitation 2016;30(12):1186-99. [DOI: ] [DOI] [PubMed] [Google Scholar]
Sureshkumar 2016 {published data only}
- Sureshkumar K, Murthy G, Natarajan S, Naveen C, Goenka S, Kuper H. Evaluation of the feasibility and acceptability of the 'Care for Stroke' intervention in India, a smartphone-enabled, carer-supported, educational intervention for management of disability following stroke. BMJ Open 2016 Feb 2;2(6):1-10. [DOI: 10.1136/bmjopen-2015-009243] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sørensen 2019 {published data only}
- Sørensen D, Christensen ME. Behavioural modes of adherence to inspiratory muscle training in people with chronic obstructive pulmonary disease: a grounded theory study. Disability and Rehabilitation 2019;41(9):1071–8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Tamm 1996 {published data only}
- Tamm M. Ethical dilemmas encountered by community-based occupational therapists in home care settings. Scandinavian Journal of Occupational Therapy 1996;3(4):180-7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Taule 2014 {published data only}
- Taule T, Råheim M. Life changed existentially: a qualitative study of experiences at 6–8 months after mild stroke. Disability and Rehabilitation 2014;36(25):2107-19. [DOI: ] [DOI] [PubMed] [Google Scholar]
Taylor 2015 {published data only}
- Taylor A, Morris G, Pech J, Rechter S, Carati C, Kidd MR. Home telehealth video conferencing: perceptions and performance. JMIR mHealth and uHealth 2015;3(3):e4666. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2016 {published data only}
- Taylor A, Wade V, Morris G, Pech J, Rechter S, Kidd M, et al. Technology support to a telehealth in the home service: qualitative observations. Journal of telemedicine and Ttelecare 2016;22(5):296-303. [DOI: ] [DOI] [PubMed] [Google Scholar]
Teriö 2019 {published data only}
- Teriö M, Eriksson G, Kamwesiga JT, Guidetti S. What's in it for me? A process evaluation of the implementation of a mobile phone-supported intervention after stroke in Uganda. BMC Public Health 2019 May 14;19(1):1-13. [DOI: 10.1186/s12889-019-6849-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thirumalai 2018 {published data only}
- Thirumalai M, Rimmer JH, Johnson G, Wilroy J, Young HJ, Mehta T, et al. TEAMS (Tele-Exercise and Multiple Sclerosis), a tailored telerehabilitation mHealth app: participant-centered development and usability study. 2018 JMIR mHealth and uHealth;6(5):e10181. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorup 2016 {published data only}
- Thorup CB, Grønkjær M, Spindler H, Andreasen JJ, Hansen J, Dinesen BI, et al. Pedometer use and self-determined motivation for walking in a cardiac telerehabilitation program: a qualitative study. 2016 BMC Sports Science, Medicine and Rehabilitation;8(1): 1-13. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Timmerman 2017 {published data only}
- Timmerman JG, Dekker-van Weering MG, Stuiver MM, Groen WG, Wouters MW et al. Ambulant monitoring and web-accessible home-based exercise program during outpatient follow-up for resected lung cancer survivors: actual use and feasibility in clinical practice. Journal of Cancer Survivorship 2017;11(6):720-31. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Townsend 2013 {published data only}
- Townsend A, Adam P, Li LC, McDonald M, Backman CL. Exploring eHealth ethics and multi-morbidity: protocol for an interview and focus group study of patient and health care provider views and experiences of using digital media for health purposes. JMIR Research Protocols 2013;2(2):e38. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2016 {published data only}
- Tsai LL, McNamara RJ, Dennis SM, Moddel C, Alison JA, McKenzie DK, et al. Satisfaction andexperience with a supervised home-based real-time videoconferencing telerehabilitation exercise program in people with chronic obstructive pulmonary disease (COPD. International Journal of Telerehabilitation 2016 Dec 15;8(2):27-38. [DOI: 10.5195/ijt.2016.6213] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tung 2012 {published data only}
- Tung YC, Cooke M, Moyle W. Sources older people draw on to nurture, strengthen and improve self‐efficacy in managing home rehabilitation following orthopaedic surgery. Journal of Clinical Nursing 2012;22(9-10):1217-25. [DOI: ] [DOI] [PubMed] [Google Scholar]
Turner 2011 {published data only}
- Turner BJ, Fleming J, Ownsworth T, Cornwell P. Perceived service and support needs during transition from hospital to home following acquired brain injury. Disability and Rehabilitation 2011;33(10):818-29. [DOI: 10.3109/09638288.2010.513422] [DOI] [PubMed] [Google Scholar]
Tyagi 2018 {published data only}
- Tyagi S, Lim DS, Ho WH, Koh YQ, Cai V, Koh GC, Legido-Quigley H. Acceptance of Tele-Rehabilitation by stroke patients: perceived barriers and facilitators. Archives of Physical Medicine Rehabilitation 2018 Dec;99(12):2472-7. [DOI: 10.1016/j.apmr.2018.04.033] [DOI] [PubMed] [Google Scholar]
Umb Carlsson 2019 {published data only}
- Umb Carlsson Õ. Health-promotion intervention in a group home: Perspectives of residents, staff and rehabilitation professionals. Journal of Intellectual Disabilities: JOID 2021 Jun;25(2):210-29. [DOI: 10.1177/1744629519874970] [DOI] [PubMed] [Google Scholar]
Valdés 2018 {published data only}
- Valdés BA, Glegg SM, Lambert-Shirzad N, Schneider AN, Marr J, Bernard R, et al. Application of commercial games for home-based rehabilitation for people with hemiparesis: challenges and lessons learned. Games for Health Journal 2018;7(3):197-207. [DOI: ] [DOI] [PubMed] [Google Scholar]
Van der Meer 2020 {published data only}
- Meer HA, Pijper L, Bruxvoort T, Visscher CM, Nijhuis-van der Sanden MW, Engelbert RHet al. Using e-Health in the physical therapeutic care process for patients with temporomandibular disorders: a qualitative study on the perspective of physical therapists and patients. Disability and Rehabilitation 2020 Jun 16;16(1):1-8. [DOI: 10.1080/09638288.2020.1775900] [DOI] [PubMed] [Google Scholar]
VanderVeen 2019 {published data only}
- Veen DJ, Döpp CM, Siemonsma PC, Nijhuis-van der Sanden MW, Swart BJ, Steultjens EM. Factors influencing the implementation of Home-Based Stroke Rehabilitation: professionals' perspective. PLOS One 2019 Jul 25;14(7):1-16. [DOI: 10.1371/journal.pone.0220226] [DOI] [PMC free article] [PubMed] [Google Scholar]
VanEngen‐Verheul 2017 {published data only}
- Engen-Verheul MM, Peek N, Haafkens JA, Joukes E, Vromen T, Jaspers MW, et al. What is needed to implement a web-based audit and feedback intervention with outreach visits to improve care quality: a concept mapping study among cardiac rehabilitation teams. International Journal of Medical Informatics 2017;97:76-85. [DOI: ] [DOI] [PubMed] [Google Scholar]
VanVelsen 2016 {published data only}
- Van Velsen L, Wildevuur S, Flierman I, Van Schooten B, Tabak M, Hermens H. Trust in telemedicine portals for rehabilitation care: an exploratory focus group study with patients and healthcare professionals. BMC Medical I and Decision Making 2016;16(1):1-12. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vik 2009 {published data only}
- Vik K, Nygård L, Lilja M. Encountering staff in the home: Three older adults’ experience duringsix months of home-based rehabilitation. Disability and Rehabilitation 2009;31(8):619-29. [DOI: 10.1080/09638280802242114] [DOI] [PubMed] [Google Scholar]
Vloothuis 2020 {published data only}
- Vloothuis J, Depla M, Hertogh C, Kwakkel G, Van Wegen E. Experiences of patients with stroke and their caregivers with caregiver-mediated exercises during the CARE4STROKE trial. Disability and Rehabilitation 2020;42(5):698-704. [DOI: ] [DOI] [PubMed] [Google Scholar]
VonKoch 1998 {published data only}
- Koch LV, Wottrich AW, Holmqvist LW. Rehabilitation in the home versus the hospital: the importance of context. Disability and Rehabilitation 1998;20(10):367-72. [DOI: ] [DOI] [PubMed] [Google Scholar]
VonKoch 2000 {published data only}
- Von Koch L, Holmqvist LW, Wottrich AW, Tham K, De Pedro-Cuesta J. Rehabilitation at home after stroke: a descriptive study of an individualized intervention. Clinical Rehabilitation 2000;14(6):574-83. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wade 2016 {published data only}
- Wade VA, Taylor AD, Kidd MR, Carati C. Transitioning a home telehealth project into a sustainable, large-scale service: a qualitative study. BMC Health Services Research 2016;16(1):1-10. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wakefield 2019 {published data only}
- Wakefield BJ, Drwal K, Paez M, Grover S, Franciscus C, Reisinger HS, et al. Creating and disseminating a home-based cardiac rehabilitation program: experience from the Veterans Health Administration. BMC Ccardiovascular Disorders 2019;19(1):1-7. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wall 2017 {published data only}
- Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Examining user perceptions of SwallowIT: a pilot study of a new telepractice application for delivering intensive swallowing therapy to head and neck cancer patients. Journal of Telemedicine and Telecare 2017;23(1):53-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Walsh 2018 {published data only}
- Walsh DM, Moran K, Cornelissen V, Buys R, Cornelis N, Woods C. Electronic health physical activity behavior change intervention to self-manage cardiovascular disease: qualitative exploration of patient and health professional requirements. Journal of Medical Internet Research 2018;20(5):e163. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wentink 2019 {published data only}
- Wentink M, Bodegom-Vos L, Brouns B, Arwert H, Houdijk S, Kewalbansing P, et al. How to improve eRehabilitation programs in stroke care? A focus group study to identify requirements of end-users. BMC Medical Informatics and Decision Making 2019;19(1):1-11. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilms 2020 {published data only}
- Wilms IL. The computerized cognitive training alliance–A proposal for a therapeutic alliance model for home-based computerized cognitive training. Heliyon 2020;6(1):e03254. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wingham 2006 {published data only}
- Wingham J, Dalal HM, Sweeney KG, Evans PH. Listening to patients: choice in cardiac rehabilitation. European Journal of Cardiovascular Nursing 2006; 5(4): 289-94. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wingham 2014 {published data only}
- Wingham J, Adie K, Turner D, Schofield C, Pritchard C. Participant and caregiver experience of the Nintendo Wii SportsTM after stroke: qualitative study of the trial of WiiTM in stroke (TWIST). Clinical Rehabilitation 2015;29(3):295-305. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wingham 2015 {published data only}
- Wingham J, Frost J, Britten N, Jolly K, Greaves C, Abraham C, et al. Needs of caregivers in heart failure management: A qualitative study. Chronic Illness 2015;11(4):304-19. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wingham 2019 {published data only}
- Wingham J, Frost J, Britten N, Greaves C, Abraham C, Warren F, et al. Caregiver outcomes of the REACH-HF multicentre randomized controlled trial of home-based rehabilitation for heart failure with reduced ejection fraction. European Journal of Cardiovascular Nursing 2019;18(7):611-20. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wottrich 2007 {published data only}
- Wottrich AW, Von Koch L, Tham K. The meaning of rehabilitation in the home environment after acute stroke from the perspective of a multiprofessional team. Physical Therapy 2007;87(6):778-88. [DOI: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Beunder 2015 {published data only}
- Beunder C, Dekker JH, Brasser JA, Depla MF . [Home after a stroke; 'that's when it really begins'. A qualitative study into the needs for aftercare of stroke patients after being discharged home] [Thuis na een CVA: ‘Dan begint het pas’. Een kwalitatief onderzoek naar de behoefte aan nazorg van CVA-patiënten na terugkeer naar huis]. Tijdschr Gerontol Geriatr. 2015 Sep;46(4):196-203. [DOI: 10.1007/s12439-015-0139-z] [DOI] [PubMed] [Google Scholar]
Friedrich 2015 {published data only}
- Friedrich R, Hiesel P, Peters S, Siewiorek DP, Smailagic A, Brügge B. Serious games for home-based stroke rehabilitation. Studies in Health Technoogy and l Informatics 2015;213:157-60. [PMID: ] [PubMed] [Google Scholar]
Hennemann 2018 {published data only}
- Hennemann S, Beutel ME, Zwerenz R. ["Morbus Google" vs. e-Health: a qualitative study of acceptance and implementation of online-aftercare in inpatient rehabilitation] ["Morbus Google" vs. e-Health: Qualitative Untersuchung zur Akzeptanz und Implementierung von Online-Nachsorge in der stationären Rehabilitation]. Rehabilitation (Stuttg) 2018 Feb;57(1):14-23. [DOI: 10.1055/s-0043-102150] [DOI] [PubMed] [Google Scholar]
Jungbauer 2008 {published data only}
- Jungbauer J, Döll K, Wilz G. [Gender- and age-specific aspects of assistance need in caregivers of stroke patients: results from a qualitative panel study] [Geschlechts- und altersspezifische Aspekte des Hilfebedarfs bei Angehörigen von Schlaganfallpatienten - Ergebnisse einer qualitativen Längsschnittstudie ]. Rehabilitation (Stuttg) 2008 Jun;47(3):145-9. [DOI: 10.1055/s-2008-1076711] [DOI] [PubMed] [Google Scholar]
Langberg 2014 {published data only}
- Langberg H, Lindahl MP, Kidholm K, Dinesen B. [Rehabilitation using telemedicine] [Telerehabilitering]. Ugeskr Laeger 2014 May;176(10):1. [PMID: ] [PubMed] [Google Scholar]
Stamm‐Balderjahn {published data only}
- Stamm-Balderjahn S, Bartel S, Wilke K, Spyra K. [Development and Evaluation of herzwegweiser.de - An Informational website designed for post-rehabilitation support of cardiac patients and their healthcare professionals in Berlin-Brandenburg] [Entwicklung und Evaluation des Online-Portals herzwegweiser.de - Ein Informationsangebot für die Nachsorge kardiologischer Rehabilitanden und deren Behandler in Berlin-Brandenburg]. Rehabilitation (Stuttg) 2018 Feb;57(1):31-7. [DOI: 10.1055/s-0043-103503] [DOI] [PubMed] [Google Scholar]
Additional references
Agostini 2015
- Agostini M, Moja L, Banzi R, Pistotti V, Tonin P, Venneri A, Turolla A. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. Journal of Telemedicine and Telecare 2015;21(4):202–13. [DOI: 10.1177/1357633X15572201] [DOI] [PubMed] [Google Scholar]
Ames 2019
- Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 10. Art. No: CD013447. [DOI: 10.1002/14651858.CD013447] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 2017
- Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K, Taylor RS. Home-based versus centre-based cardiac rehabilitation. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No: CD007130. [DOI: 10.1002/14651858.CD007130.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Andrenelli 2020
- Andrenelli E, Negrini F, Sire A, Arienti C, Patrini M, Negrini S, Ceravolo MG. Systematic rapid living review on rehabilitation needs due to Covid-19: update to May 31st 2020. European Journal of Physical and Rehabilitation Medicine 2020;56(4):508-14. [DOI: 10.23736/s1973-9087.20.06435-7] [DOI] [PubMed] [Google Scholar]
Bettger 2020
- Bettger JP, Thoumi A, Marquevich V, De Groote W, Rizzo-Battistella L, Imamura M, et al. COVID-19: Maintaining essential rehabilitation services across the care continuum. BMJ Global Health 2020;5(5):1-7. [DOI: 10.1136/bmjgh-2020-002670] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bittner 2020
- Bittner AK, Wykstra SL, Yoshinaga PD, Li T. Telerehabilitation for people with low vision. Cochrane Database of Systematic Reviews 2020, Issue 8. Art. No: CD011019. [DOI: 10.1002/14651858.CD011019.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boldrini 2020
- Boldrini P, Garcea M, Brichetto G, Reale N, Tonolo S, Falabella V, et al. Living with a Disability during the Pandemic. ‘Instant Paper from the Field’ on rehabilitation answers to the COVID-19 emergency. European Journal of Physical and Rehabilitation Medicine 2020;56(3):331-4. [DOI: 10.23736/S1973-9087.20.06373-X] [DOI] [PubMed] [Google Scholar]
Booth 2016
- Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Systematic Reviews 2016;5:74. [DOI: 10.1186 / s13643-016-0249-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brennan 2009
- Brennan DM, Mawson S, Brownsell S. Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self management. Studies in Health Technology and Informatics [Información técnica de Stud Health] 2009;145:231-48. [PMID: ] [PubMed] [Google Scholar]
Ceravolo 2020a
- Ceravolo MG, Sire A, Andrenelli E, Negrini F, Negrini S. Systematic rapid "living" review on rehabilitation needs due to COVID-19: update to March 31st, 2020. European Journal of Pphysical and Rrehabilitation Mmedicine 2020;56(3):347-53. [DOI: 10.23736/S1973-9087.20.06329-7] [DOI] [PubMed] [Google Scholar]
Ceravolo 2020b
- Ceravolo MG, Arienti C, De Sire A, Andrenelli E, Negrini F, Lazzarini SG, et al. Rehabilitation and Covid-19: The Cochrane Rehabilitation 2020 Rapid Living Systematic Review. European Journal of Physical and Rehabilitation Medicine 2020;56(6):642-51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cheng 2017
- Cheng KK, Lim YTE, Koh ZM, Tam WW. Home-based multidimensional survivorship programmes for breast cancer survivors. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD011152. [DOI: 10.1002/14651858.CD011152.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chi 2020
- Chi NF, Huang YC, Chiu HY, Chang HJ, Huang HC. Systematic review and meta-analysis of home-based rehabilitation on improving physical function among home-dwelling patients with a stroke. Archives of Physical Medicine and Rehabilitation 2020;101(2):359-73. [DOI: 10.1016 / j.apmr.2019.10.181] [DOI] [PubMed] [Google Scholar]
Cieza 2021
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021;396(10267):2006-17. [DOI: 10.1016/S0140-6736(20)32340-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2006
- Clark D. The Elgar Companion to Development Studies Disability and Development. Edward Elgar Publishing, 2006. [Google Scholar]
Cobbing 2016
- Cobbing S, Hanass-Hancock J, Myezwa H. Home- based rehabilitation interventions for adults living with HIV: a scoping review. African Journal of AIDS Research 2016;15(1):77-88. [DOI: 10.2989/16085906.2016.1159968] [DOI] [PubMed] [Google Scholar]
Coupar 2012
- Coupar F, Pollock A, Legg LA, Sackley C, Vliet P. Home-based therapy programmes for upper limb functional recovery following stroke. Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No: CD006755. [DOI: 10.1002/14651858.CD006755.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Critical Appraisal Skills Programme 2013
- Critical Appraisal Skills Programme (CASP). Qualitative Appraisal Checklist for Qualitative Research. Critical Appraisal Skills Programme (CASP) 2013.
Damschroder 2009
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science: IS 2009;4:50. [DOI: 10.1186 / 1748-5908-4-50] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Sire 2020
- De Sire A, Andrenelli E, Negrini F, Negrini S, Ceravolo MG. Systematic rapid living review on rehabilitation needs due to Covid-19: update to April 30th 2020. European Journal of Physical and Rehabilitation Medicine 2020;56(3):354-60. [DOI: 10.23736/S1973-9087.20.06378-9] [DOI] [PubMed] [Google Scholar]
Dorjbal 2019
- Dorjbal D, Zanini C, Tsegmid N, Stucki G, Rubinelli S. Toward an optimization of rehabilitation services for persons with spinal cord injury in Mongolia: the perspective of medical doctors. Disability and Rehabilitation 2019;43(15):1-13. [DOI: 10.1080 / 09638288.2019.1696415] [DOI] [PubMed] [Google Scholar]
EP and RMBA 2018
- European Physical and Rehabilitation Medicine Bodies Alliance. White Book on Physical and Rehabilitation Medicine (PRM) in Europe. Chapter 8. The PRM specialty in the healthcare system and society. European Journal of Physical and Rehabilitation Medicine 2018;54(2):261-78. [DOI: 10.23736/S1973-9087.18.05152-3] [DOI] [PubMed] [Google Scholar]
Gelaw 2020
- Gelaw AY, Janakiraman B, Gebremeskel BF, Ravichandran H. Effectiveness of home-based rehabilitation in improving physical function of persons with stroke and other physical disability: a systematic review of randomized controlled trials. Journal of Stroke and Cerebrovascular Diseases 2020;29(6):104800. [DOI: 10.1016/j.jstrokecerebrovasdis.2020.104800] [DOI] [PubMed] [Google Scholar]
Gimigliano 2017
- Gimigliano F, Negrini S. The World Health Organization ‘Rehabilitation 2030: a Call for Action. European Journal of Physical and Rehabilitation Medicine 2017;53(2):155–68. [DOI: 10.23736 / S1973-9087.17.04746-3] [DOI] [PubMed] [Google Scholar]
Gonçalves‐Bradley 2017
- Gonçalves-Bradley DC, Iliffe S, Doll HA, Broad J, Gladman J, Langhorne P, et al. Early discharge hospital at home. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No: CD000356. [DOI: 10.1002/14651858.CD000356.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grundstein 2021
- Grundstein MJ, Fisher C, Titmuss M, Cioppa-Mosca J. The role of virtual physical therapy in a post-pandemic world: pearls, pitfalls, challenges, and adaptations. Physical Therapy & Rehabilitation Journal 2021 Sept 1;101(9):1-7. [DOI: 10.1093/ptj/pzab145] [DOI] [PubMed] [Google Scholar]
Gutenbrunner 2020a
- Gutenbrunner C, Nugraha B. Decision- making in evidence-based practice in rehabilitation medicine: proposing a fourth factor. American \journal of Physical Medicine & Rehabilitation 2020;99(5): 436-40. [DOI: 10.1097/phm.0000000000001394] [DOI] [PubMed] [Google Scholar]
Gutenbrunner 2020b
- Gutenbrunner C, Nugraha B, Gimigliano F, Meyer T, Kiekens C. International Classification of Service Organization in Rehabilitation: an updated set of categories (ICSO-R 2.0). Journal of Rehabilitation Medicine 2020;52(1):jrm00004. [DOI: 10.2340 / 16501977-2627] [DOI] [PubMed] [Google Scholar]
Hotta 2015
- Hotta F. Home rehabilitation. Japan Medical Association Journal 2015;58(1-2):40-3. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Housley 2016
- Housley SN, Garlow AR, Ducote K, Howard A, Thomas T, Wu D, et al. Increasing access to cost effective home-based rehabilitation for rural veteran stroke survivors. Austin Journal of Cerebrovascular Disease & Stroke 2016;3(2):1. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Kairy 2009
- Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disability and Rehabilitation 2009;31(6):427-47. [DOI: 10.1080/09638280802062553] [DOI] [PubMed] [Google Scholar]
Karimi‐Shahanjarini 2019
- Karimi‐Shahanjarini A, Shakibazadeh E, Rashidian A, Hajimiri K, Glenton C, Noyes J, et al. Barriers and facilitators to the implementation of doctor‐nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No: CD010412. [DOI: 10.1002/14651858.CD010412.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2015
- Khan F, Amatya B, Kesselring J, Galea M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD010508. [DOI: 10.1002/14651858.CD010508.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Knudsen 2019
- Knudsen MV, Laustsen S, Petersen AK, Hjortdal VE, Angel S. Experience of cardiac tele-rehabilitation: analysis of patient narratives. Disability and Rehabilitation 2019;43(3):370-7. [DOI: 10.1080/09638288.2019.1625450] [DOI] [PubMed] [Google Scholar]
Kuo 2019
- Kuo WY, Shyu YIL, Wang JS, Chen MC, Wu CC, Chen ML. Adherence to home-based rehabilitation in older adults with diabetes after hip fracture. Nursing Research 2019;68(5):383-9. [DOI: 10.1097/nnr.0000000000000371] [DOI] [PubMed] [Google Scholar]
Laver 2020
- Laver KE, Adey‐Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD010255. [DOI: 10.1002/14651858.CD010255.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation science: IS 2018;13(1):2. [DOI: 10.1186/s13012-017-0688-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCartan 2020
- McCartan CJ, Yap J, Firth J, Stubbs B, Tully MA, Best P, et al. Factors that influence participation in physical activity for people with bipolar disorder: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2020, Issue 3. Art. No: CD013557. [DOI: 10.1002/14651858.CD013557] [DOI] [PMC free article] [PubMed] [Google Scholar]
Means 2020
- Means AR, Kemp CG, Gwayi-Chore MC, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implementation Science 2020;15(1):1-19. [DOI: 10.1186/S13012-020-0977-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meyer 2014
- Meyer T, Gutenbrunner C, Kiekens C, Skempes D, Melvin JL, Schedler K, et al. ISPRM discussion paper: proposing a conceptual description of health-related rehabilitation services. Journal of Rehabilitation Medicine 2014;46(1):1-6. [DOI: 10.2340/16501977-1251] [DOI] [PubMed] [Google Scholar]
Mlenzana 2013
- Mlenzana NB, Frantz JM, Rhoda AJ, Eide AH. Barriers to and facilitators of rehabilitation services for people with physical disabilities: a systematic review. African Journal of Disability 2013;2(1):1-6. [DOI: 10.4102/ajod.v2i1.22] [DOI] [PMC free article] [PubMed] [Google Scholar]
Negrini 2020a
- Negrini S, Kiekens C, Heinemann AW, Özçakar L, Frontera WR. Prioritising people with disabilities implies furthering rehabilitation. Lancet 2020;395(10218):111. [DOI: 10.1016/S0140-6736(19)32623-6] [DOI] [PubMed] [Google Scholar]
Negrini 2020b
- Negrini S, Kiekens C, Bernetti A, Capecci M, Ceravolo MG, Lavezzi S, et al. Telemedicine from Research to Practice during the Pandemic. ‘Instant Paper from the Field’ on Rehabilitation Answers to the Covid-19 Emergency. European Journal of Physical and Rrehabilitation Mmedicine 2020;56(3):327-30. [DOI: 10.23736/S1973-9087.20.06331-5] [DOI] [PubMed] [Google Scholar]
Negrini 2020c
- Negrini S, Meyer T, Arienti C, Kiekens C, Pollock A, Selb M, et al. The 3rd Cochrane Rehabilitation Methodology Meeting: "Rehabilitation definition for scientific research purposes". European Journal of Physical and Rehabilitation Medicine 2020;56(5):658-60. [DOI: 10.23736/S1973-9087.20.06574-0] [DOI] [PubMed] [Google Scholar]
Negrini 2020d
- Negrini S, Donzelli S, Negrini A, Negrini A, Romano M, Zaina F. Feasibility and acceptability of telemedicine to substitute outpatient rehabilitation services in the COVID-19 emergency in Italy: an observational everyday clinical-life study. Archives of Physical Medicine and Rehabilitation 2020 Nov;101(11):2027-32. [DOI: 10.1016/j.apmr.2020.08.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Odendaal 2020
- Odendaal WA, Watkins JA, Leon N, Goudge J, Griffiths F, Tomlinson M, et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2020, Issue 3. Art. No: CD011942. [DOI: 10.1002/14651858.CD011942.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patton 2002
- Patton MQ. Qualitative Research & Evaluation Methods. First edition. London: Third Edition Thousand Oaks, CA: Sage, 2002. [HTTPS: us.sagepub.com/en-us/sam/qualitative-research-evaluation-methods/book232962] [Google Scholar]
Peretti 2017
- Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR rehabilitation and assistive technologies 2017;4(2):e7511. [DOI: 10.2196/rehab.7511] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rezaei 2019
- Rezaei M, Sharifi A, Vaccaro AR, Rahimi-Movaghar V. Home- based rehabilitation programs: promising field to maximize function of patients with traumatic spinal cord injury. Asian Journal of Neurosurgery 2019;14(3):634. [DOI: 10.4103/ajns.AJNS_86_17] [DOI] [PMC free article] [PubMed] [Google Scholar]
Romano 2021
- Romano M, Negrini A, Negrini S. Lessons learned in two months of exclusive application of telephysiotherapy instead of classical physiotherapy during the lockdown in Italy. Spine Journal 2021 Mar;21(3):366-9. [DOI: 10.1016/j.spinee.2020.10.023] [DOI] [PubMed] [Google Scholar]
Saragiotto 2016
- Macedo LG, Saragiotto BT, Maher CG, Yamato TP, Costa LO, Costa LCM, et al. Motor control exercise for nonspecific low back pain: a cochrane Rreview. Cochrane Database of Systematic Reviews 2016, Issue 16. Art. No: CD012085. [DOI: 10.1002/14651858.CD012085] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skempes 2021
- Skempes D, Kiekens C, Malmivaara A, Michail X, Bickenbach J, Stucki G. Supporting government policies to embed and expand rehabilitation in health systems in Europe: a framework for action. Health Policy 2021;21:S0168-8510. [DOI: 10.1016/j.healthpol.2021.06.014.] [DOI] [PubMed] [Google Scholar]
Steihaug 2016
- Steihaug S, Lippestad JW, Werner A. Between ideals and reality in home-based rehabilitation. Scandinavian Journal of Primary Health Care 2016;34(1):46-54. [DOI: 10.3109/02813432.2015.1132888] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stolee 2012
- Stolee P, Lim SN, Wilson L, Glenny C. Inpatient versus home-based rehabilitation for older adults with musculoskeletal disorders: a systematic review. Clinical Rehabilitation 2012;26(5):387-402. [DOI: 10.1177/0269215511423279] [DOI] [PubMed] [Google Scholar]
Tyagi 2018
- Tyagi S, Lim DS, Ho WH, Koh YQ, Cai V, Koh GC, et al. Acceptance of tele-rehabilitation by stroke patients: perceived barriers and facilitators. Archives of Physical Medicine and Rehabilitation 2018;99(12):2472-7.e2. [DOI: 10.1016/j.apmr.2018.04.033] [DOI] [PubMed] [Google Scholar]
Van Egmond 2018
- Van Egmond MA, Schaaf M, Vredeveld T, Vollenbroek-Hutten MM, Berge Henegouwen MI, Klinkenbijl JH, et al. Effectiveness of physiotherapy with telerehabilitation in surgical patients: a systematic review and meta-analysis. Physiotherapy 2018;104(3):277-98. [DOI: 10.1016/j.physio.2018.04.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ward 2008
- Ward D, Drahota A, Gal D, Severs M, Dean TP. Care home versus hospital and own home environments for rehabilitation of older people. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No: CD003164. [DOI: 10.1002/14651858.CD003164.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Widén 1998
- Widén Holmqvist L, Von Koch L, Kostulas V, Holm M, Widsell G, Tegler H, et al. A randomized controlled trial of rehabilitation at home after stroke in southwest Stockholm. Stroke 1998;29(3):591-7. [DOI: 10.1161/01.str.29.3.591] [DOI] [Google Scholar]
World Health Organization 2001
- World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. World Report on Child Injury Prevention 2001:1.
World Health Organization 2011
- World Health Organization. World report on disability. World Health Organization 2011;No. WHO/NMH/VIP/11.01:1–24.
World Health Organization 2019
- World Health Organization. Universal Health Coverage (UHC). World Health Organization 2019;0:1.


