Abstract
Life events, such as the COVID-19 pandemic, elicit increases in psychological stress and symptoms of anxiety and depression. In turn, these outcomes have negative implications for mental health. Emotion regulation strategies and prior adversity may moderate the degree to which life events affect outcomes which are linked to mental health. The purpose of the current study was to evaluate whether childhood adversity and emotion regulation strategy use interactively informed changes in outcomes linked to mental health following the onset of the pandemic in American Indian (AI) adults. AI adults (N=210) reported levels of childhood adversity, emotion regulation strategy use, symptoms of anxiety and depression, and psychological stress one month prior to the onset of the COVID-19 pandemic. One month following the declaration of the pandemic, they reported on their stress, symptoms of anxiety and depression once again. The interaction between expressive suppression and childhood adversity predicted changes in psychological stress and symptoms of depression (B = .26, t (198) = 4.43 p < .001, R2 change = .06) and (B = .23 t (199) = 4.14, p < .001, R2 change = .05) respectively. The findings indicate that expressive suppression may be a maladaptive emotion regulation strategy for AI adults who experienced high levels of childhood adversity. This work represents a first step in understanding the role of emotion regulation strategy use in predicting mental health-relevant outcomes in the context of a life event, in a community which is disproportionately affected by chronic mental health conditions.
Keywords: emotion regulation strategies, stress, American Indians, childhood adversity, mental health
Psychological stress, and symptoms of anxiety and depression are known risk factors for poor mental health (Cohen et al., 2016; Cohen et al., 2007; Plieger, et al., 2016; Van Dam et al., 2013; Kouros et al., 2016). As such, life events which give rise to increases in these outcomes can have adverse implications for mental health. It is well-documented that the onset of the novel Coronavirus disease 2019 (COVID-19) pandemic elicited increases in psychological stress, and symptoms of anxiety and depression (Cooke et al., 2020; Dos Santos et al., 2020; Lancet Infectious Diseases, 2020). Further, it is posited that these changes could amplify the symptoms of current mental health problems and elicit new ones (Chew at al., 2020; Horesh & Brown, 2020). This knowledge is of particular concern for populations such as American Indians (AIs), who have disproportionately high incidence of mental health conditions (Espey et al., 2014). However, to date, there is limited understanding of how psychosocial factors and previous experiences may moderate the degree to which life events affect mental health for this population.
Emotion Regulation Strategies, Psychological Stress, and Indices of Mental Health
A key pathway through which life events may impact psychological stress and indices of mental health is through emotion regulation strategy use (Breaux et al., 2021; Russell, Hutchison et al., 2021). While there are a wide range of identified emotion regulation strategies, expressive suppression and cognitive reappraisal are among the most widely researched (Gullone & Taffe, 2012). Expressive suppression refers to the inhibition of emotional expression to an emotion eliciting situation. Cognitive reappraisal refers to the cognitive reframing of thoughts about the emotion elicitor for the purpose of reducing the negative impact (Gross & John, 2003). The successful regulation of stress-related emotions is necessary in the maintenance of mental health (Gross & Munoz, 1995).
In general, research indicates that cognitive reappraisal is negatively associated with psychological stress and stress-related psychopathology while expressive suppression is positively related to psychological stress and stress-related psychopathology (Moore et al., 2008). Specifically, cognitive reappraisal training has related to adaptive cognitive responses to stressful situations (Jamieson et al., 2011), while use of expressive suppression in response to stress has been related to negative cognitive outcomes (Mohammed et al., 2021). Generally, systematic reviews and empirical research indicate more frequent use of expressive suppression and less frequent use of cognitive reappraisal in both anxious and depressed individuals. Specifically, anxiety disorders are associated with frequent use of expressive suppression as well as ineffective use of cognitive reappraisal. Further, research indicates depression is related to infrequent use of cognitive reappraisal (D’Avanzato et al., 2013; Dryman & Heimberg, 2018; Ehring et al., 2010).
Trauma and Adversity as Predictors of Emotion Regulation
Emotion regulation occurs at the biological, psychological, and social levels and has “typical” developmental trajectories (Ahmed et al., 2015). Across the lifespan, exposures and experiences can disrupt these trajectories. For example, evidence suggests childhood adversity disrupts the typical developmental trajectories of neural systems implicated in emotion regulation (McLaughlin, 2015). Specifically, chronic childhood interpersonal trauma exposure has been directly linked to emotion regulation difficulties, including limited strategy use, and Post Traumatic Stress Disorder (PTSD) symptoms across the lifespan (McLaughlin, 2015). Additionally, childhood trauma exposure has been linked to decreased automatic emotion regulation and increased sensitivity to emotional conflict (Marusak et al, 2015). Prior findings also indicate that use of specific strategies can exacerbate the negative effects of trauma on stress reactivity. Specifically, use of expressive suppression has been shown to result in increased stress reactivity in trauma exposed populations (Moore et al., 2008). Moreover, trauma exposure is often positively associated with use of expressive suppression (Boden et al., 2013).
Relatedly, prior work suggests that prior trauma or adversity may impact mental health through its influence on the use of emotion regulation strategies. For example, childhood adversity (i.e., emotional abuse) was linked to higher depressive and anxiety symptoms through more frequent use of expressive suppression and was linked to greater depressive symptomology though infrequent or ineffective use of cognitive reappraisal (Huh et al., 2017). The documented relationships between childhood adversity and emotion regulation strategy use may become increasingly evident in the context of current stressful life events such as the COVID-19 pandemic.
Compared to the general United States population, AIs experience disproportionately high rates of childhood trauma and adversity (Beals et al, 2013; Manson et al, 2005). While emotion regulation strategy use is implicated in the relationship between adversity and mental health in other ethnic minority groups, research is limited in AI populations (Carter et al., 2020; Tyra et al., 2021). Additionally, evidence suggests that culture plays a role in how we experience and express emotions. For example, culture can impact our use of and preference for cognitive reappraisal and expressive suppression as well as determine whether these strategies are adaptive or maladaptive (Ford & Mauss, 2015; Kwon et al., 2013; Matsumoto et al, 2008). However, to date, our knowledge of psychosocial and experiential predictors of emotion regulation strategy use in AI populations and its implication in shaping outcomes relevant to mental health in the context of a current stressor is limited.
Purpose
As described previously, prior work indicates that trauma and adversity may inform one’s tendency to use specific emotion regulation strategies (Boden et al., 2013), which can then result in negative outcomes including maintenance of trauma related symptomology and heightened psychological responses to stressors (Moore et al., 2008; Short et al., 2018). However, most of the existing research in this area has been conducted in majority racial or ethnic groups and has not focused on AI populations.
Extending upon previous work, the purpose of the current study was to evaluate the relationships between childhood adversity, emotion regulation strategy use and changes in psychological stress and symptoms of depression and anxiety in the context of a life event: the COVID-19 pandemic. We hypothesized that emotion regulation strategy use would moderate the relation between childhood adversity and changes in psychological stress, and the relationship between childhood adversity and changes in symptoms of anxiety and depression in the context of the pandemic. Specifically, we predicted that childhood adversity would be positively related to changes in psychological stress, and symptoms of depression and anxiety for those individuals who reported low use of cognitive reappraisal and high use of expressive suppression. We predicted that these relations would exist beyond the contributions of age, sex, and SES, variables which are indicated as predictors of these outcomes (De France & Evans, 2020; Esbjørn et al., 2012; Nolen-Hoeksema & Aldao, 2011; Troy et al., 2017).
Methods
Participants and Procedure
This research utilized a Community Based Participatory Research (CBPR) approach and framework. CBPR emphasizes the importance of equitable involvement of both community members and researchers in all components of the research process. CBPR has been particularly successful in engaging underserved communities to address health disparities (Stacciarini, Shattell et al., 2011). After the onset of the COVID-19 pandemic, a long-standing Community Advisory Board (CAB) comprised of 4 members of the Blackfeet AI community, located in Northwest Montana met to discuss the opportunity to follow up with participants who had participated in a cross-sectional investigation before the onset of the pandemic. The CAB felt we had a unique opportunity to understand how emotion regulation strategy use would predict psychological responses to the pandemic as well as changes in indices of mental health. The CAB informed the study design and the selection of follow-up measures.
After receiving approval from the Montana State University Institutional Review Board, we contacted 300 AI participants from a previous cross-sectional survey study. These participants were originally recruited by Qualtrics using convenience sampling. Qualtrics draws participants from multiple managed research panels for groups which are harder to reach, including Ais. Qualtrics uses niche panels which are developed through specialized recruitment campaigns. To be eligible for this original study, participants had to identify as AI, currently live within the United States, and be at least 30 years old. Participants had provided their contact information for participation in possible follow-up studies. Out of the 300 contacted individuals, 210 American Indian adults agreed to participate and formed an online panel for future research projects. A minimum sample size of 200 was determined.
There were no statistically significant differences in age, biological sex, income, childhood adversity, levels of psychological stress, symptoms of depression or anxiety, or use of emotion regulation strategies between those individuals who chose to participate and those who did not. Data collection occurred across two time points. Time 1 occurred during the final week of February, 2020, and Time 2 data was collected during the final week of April, 2020. Participants were given $10 Amazon gift cards for the completion of surveys. Childhood adversity and use of emotion regulation strategies were measured at Time 1. Psychological stress and symptoms of depression and anxiety were measured at Time 1 and Time 2. The study was not preregistered. We report how we determined our sample size, all data exclusions (if any), all manipulations, and all measures in the study. The authors have all data and study analysis code used in these investigations, and these will be shared upon reasonable request.
Measures
Emotion Regulation Strategies
We used the Emotion Regulation Questionnaire (ERQ; Gross & John, 2003) to measure emotion regulation strategy use. The ERQ is comprised of 10 items; participants rate the degree to which they agree with a statement regarding their use of a specific emotion regulation strategy using a 5-point Likert-type scale: 1 (strongly disagree), 2 (disagree), 3 (half and half), 4 (agree), 5 (strongly agree). Higher scores indicate greater use of the strategy. Both the cognitive reappraisal subscale and the expressive suppression subscale of the ERQ showed good internal consistency (Cronbach’s α= .97 and .94 respectively).
Childhood Adversity
As a measure of childhood adversity, we used the Risky Families Questionnaire (RFQ) (Repetti et al., 2002). The RFQ is a 10-item self-report instrument which asks participants to report how frequently certain events occurred in their homes during the ages of 5–15 years of age. Example questions include “How often would you say there was quarreling, arguing or shouting between your parents?”, “How often did a parent or other adult in the household make you feel that you were loved, supported, and cared for?”, and “How often did a parent or other adult in the house push, grab, shove or slap you?”. While the RFQ does measure exposure to certain types of childhood trauma including verbal, emotional and physical abuse, it does not measure sexual abuse, making it distinct from other commonly used measures of childhood trauma such as the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 1994) or the Adverse Childhood Experiences Questionnaire (ACES) (Felitti et al., 1998). The Community Advisory Board (CAB) comprised of AI adults, preferred this questionnaire to these more commonly used measures, because in addition to trauma exposure, it considers the presence or absence of affection and warmth. Participants respond to the RFQ questions on a 5-point Likert Scale (1= Not at all, 5= Very often). Items measuring the presence of positive qualities in the family environment are reverse scored and all 10 items are summed to capture the overall risk in early family environments. The questionnaire showed very good internal consistency (Cronbach’s a=.91).
Psychological Stress
As a measure of psychological stress at Time 1 and Time 2, we used the Perceived Stress Scale-10 (PSS-10) (Cohen et al, 1983). The measure consists of 10 items which are used to measure the degree to which individuals perceive their life as unpredictable, uncontrollable, and overloading over the past month. Participants respond to each item using a five-point scale to indicate how often they felt a certain way (0= never, 1= almost never, 2=sometimes, 3= fairly often, 4= very often). There are four positively stated items which are reverse-scored. A total score is then calculated by summing all responses, with higher numbers reflecting greater overall perceived stress. For our analyses, we calculated a difference score to reflect changes in psychological stress from before the pandemic to after the onset of the pandemic by subtracting PSS-10 scores at Time 1 from PSS-10 scores at Time 2. The measure showed good internal consistency (Time 1: Cronbach’s α =.85. Time 2: Cronbach’s α = .88).
Symptoms of Anxiety and Depression
As a measure of anxiety and depression symptoms at Time 1 and Time 2, we used the Hospital Anxiety and Depression Scale (HADS) (Snaith, 2003). The HADS has 14 total items with 7 items in the depression subscale, and 7 items in the anxiety subscale. Individuals respond to each item using a four-point response category (0–3). Scores are cumulative, with possible scores ranging from 0–21 for anxiety and depression. Cronbach’s α for the anxiety subscale was 0.88 and Cronbach’s α for the depression subscale was 0.86 at Time 1, and .85 and .89 respectively at Time 2.
Data Analysis
Statistical Analyses were conducted using SPSS (Version 24; IBM, Armonk, NY). Continuous covariates were centered with z-scores prior to being used in analyses. We used hierarchical linear regression models to investigate whether childhood adversity moderated the relationship between emotion regulation strategies and changes in psychological stress following the onset of the COVID-19 pandemic. All variables were mean-centered prior to use in statistical models. In separate hierarchical linear regression models, we examined whether childhood adversity moderated the relationship between emotion regulation strategies and changes in symptoms of depression and anxiety following the onset of the pandemic. For statistically significant interaction effects, we used the Johnson-Neyman technique to identify specific regions of significance (Rast et al., 2014).
Results
Descriptive Statistics and Bivariate Correlations
The sample was predominantly female (59.5%) and the average age was 55. Participants self-reported their annual income using the following scale: Below $20,000 (1), $20,000-$40,000 (2), $40,001-$60,000 (3), $60,001-$80,000 (4), $80,001-$100,000 (5), and $100,001 and above (6). According to these categories, 22.9% of our sample were in the (1) category, 28.6% in the (2) category, 14.3% in the (3) category, 11.4% in the (4) category, 9.0 % in the (5) category, and 13.8% in the (6) category. The annual income levels observed in our sample reflect high poverty rates for AIs nationally (NCAI, 2020; UCSB, 2017). Descriptive statistics and bivariate correlations are listed in Table 1.
Table 1.
Means, standard deviations, and bivariate correlations.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| 1. Childhood Adversity | 22.58 | 10.72 | |||||||||
| 2. Expressive Suppression | 4.32 | 1.39 | .14* | ||||||||
| 3. Cognitive Reappraisal | 3.45 | 1.48 | −.02 | −.10 | |||||||
| 4. Depressive Symptoms (Time 1) | 9.45 | 1.68 | .10* | .08 | .04 | ||||||
| 5. Anxiety Symptoms (Time 1) | 9.86 | 1.82 | .23** | .08 | −.01 | .22** | |||||
| 6. Stress (Time 1) | 16.92 | 4.94 | .10** | .02 | −.10* | .16* | .22** | ||||
| 7. Change in Depressive Symptoms | 1.11 | 5.55 | .45** | .29** | −.01 | −.13 | .20** | .23** | |||
| 8. Change in Anxiety Symptoms | 1.18 | 5.57 | .39** | .21** | −.08 | .17* | .10 | .29** | .58** | ||
| 9. Change in Stress | 1.23 | 5.63 | .43** | .37** | −.01 | .05 | .09 | .03 | .53** | .63** | |
Note. M and SD are used to represent mean and standard deviation, respectively.
indicates p < .05.
indicates p < .01.
Emotion Regulation Strategy Use and Childhood Adversity as Predictors of Changes in Psychological Stress
We utilized a hierarchical linear model to investigate whether the interaction between childhood adversity and expressive suppression was a significant predictor of changes in psychological stress (i.e., the difference between levels of psychological stress measured at Time 1 and Time 2). In step 1, we entered age, sex, annual income, symptoms of depression and anxiety (Time 1), psychological stress (Time 1), cognitive reappraisal, childhood adversity, the interaction between childhood adversity and cognitive reappraisal, and expressive suppression. In step 2, we entered the interaction term between childhood adversity and expressive suppression.
The interaction term was a significant predictor of changes in psychological stress (B = 0.26, t (198) = 4.43 p < .001, R2 change = .06). Table 2 reports the full results of this model. Figure 1 depicts the pattern of the interaction with high and low values for each variable plotted at 1 standard deviation above and below the mean respectively. Simple slopes analyses revealed that the association between childhood trauma (as measured by the RFQ) and changes in psychological stress was statistically significant for AIs who reported high use of expressive suppression (i.e., 1 SD above the mean) (B = 3.49 t (198) = 49.36, p <.001) and for AI adults who reported low use of expressive suppression (i.e., 1 SD below the mean) (B = 0.59, t (198) = 8.34, p < .001). Simple slope analyses indicated that expressive suppression was a significant predictor of changes in psychological stress for AI adults who reported high levels of childhood trauma (i.e., 1 SD above mean) (B = 3.02, t (198) = 42.71, p < .001), but not for AI adults who reported low levels of childhood trauma (i.e., 1 SD below the mean) (B = 0.12, t (198) = 1.69, p =.09).
Table 2.
Summary of hierarchical linear regression model with childhood adversity and emotion regulation strategies predicting changes in psychological stress.
| Predictor | B | SE B | β | p | R2 |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −.06 | .03 | −.14 | .022 | |
| Sex | .07 | .66 | .01 | .918 | |
| Annual income | −.36 | .20 | −.11 | .068 | |
| Anxiety symptoms (Time 1) | .39 | .19 | .13 | .036 | |
| Depressive symptoms (Time 1) | −.67 | .19 | −.21 | <.001 | |
| Childhood adversity | 2.14 | .34 | .39 | <.001 | |
| Cognitive reappraisal | .22 | .32 | .04 | .480 | |
| Cognitive reappraisal × Childhood adversity | −.31 | .30 | −.06 | .295 | |
| Expressive suppression | 1.24 | .32 | .22 | <.001 | |
| Step 2 | |||||
| Age | −.07 | .02 | −.16 | .008 | |
| Sex | .06 | .63 | .01 | .926 | |
| Annual income | −.43 | .19 | −.13 | .024 | |
| Anxiety symptoms (Time 1) | .37 | .18 | .12 | .038 | |
| Depressive symptoms (Time 1) | −.68 | .18 | −.21 | <.001 | |
| Childhood adversity | 2.01 | .33 | .36 | <.001 | |
| Cognitive reappraisal | .23 | .30 | .04 | .489 | |
| Cognitive reappraisal × Childhood adversity | −.23 | .31 | −.04 | .470 | |
| Expressive suppression | 1.13 | .31 | .20 | <.001 | |
| Childhood adversity × Expressive suppression | 1.24 | .30 | .26 | <.001 |
Note: Sex was coded as follows: Female =1, Male =2
Statistically significant predictors are listed in bold
Figure 1.
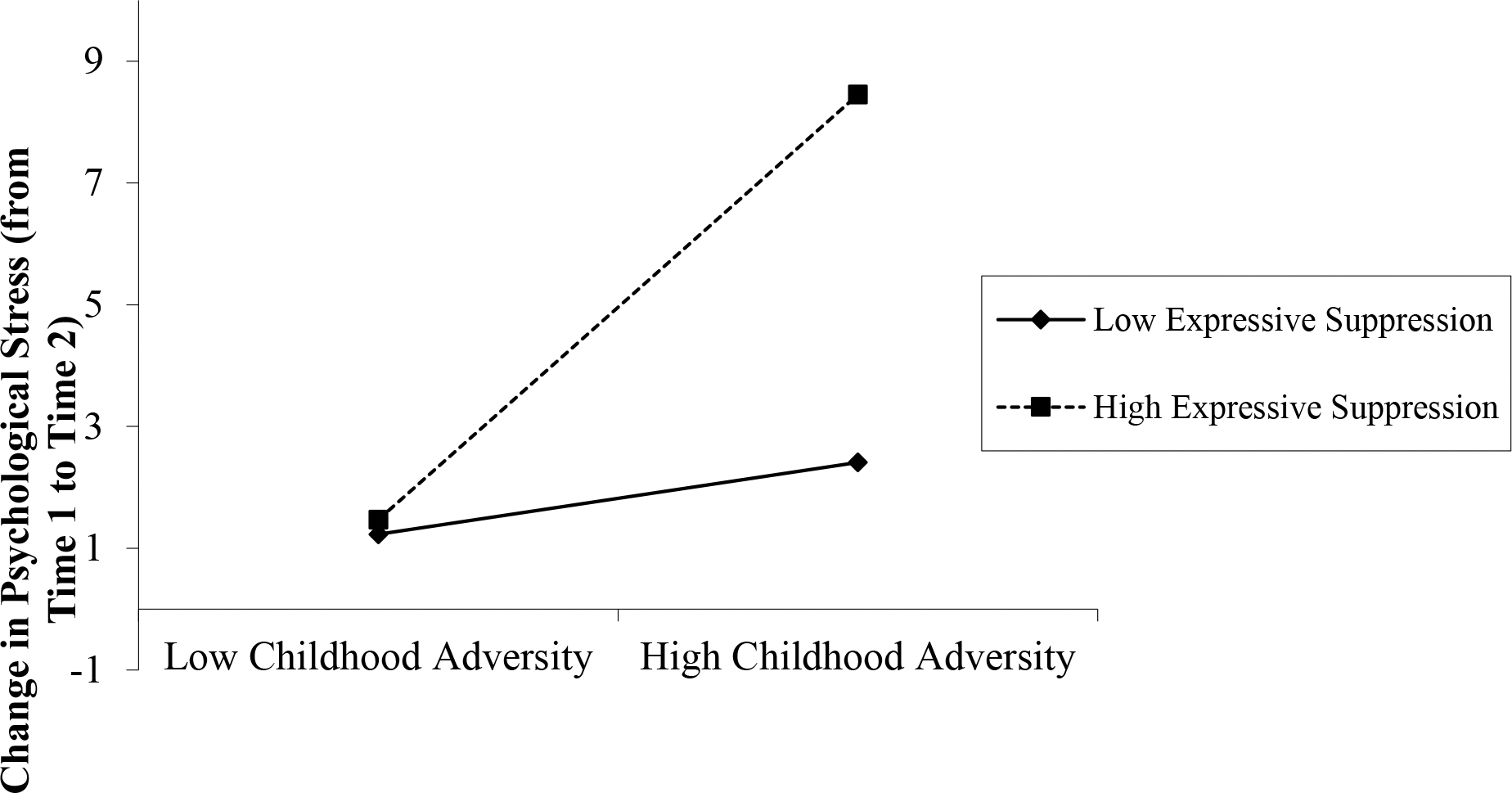
Changes in psychological stress following onset of COVID-19 pandemic as a function of expressive suppression and childhood adversity. Results from a linear regression controlling for age, sex, annual income, symptoms of depression and anxiety at Time 1, psychological stress at Time 1, cognitive reappraisal, and the interaction between cognitive reappraisal and childhood adversity.
Using the Johnson-Neyman technique (Rast et al., 2014), we identified regions of significance for the interaction between childhood adversity and expressive suppression as a predictor of changes in psychological stress associated with the onset of the COVID-19 pandemic. The relationship between childhood adversity (as measured by the RFQ) and changes in psychological stress was statistically significant for those individuals who had an average score of 3.20 or higher on the expressive suppression scale (possible range = 1–7). Johnson-Neyman analyses further indicated that the relationship between expressive suppression and changes in psychological stress was statistically significant for those individuals who had a score of 18 or higher on the RFQ scale (possible range 10–50).
In a separate hierarchical linear model, we tested whether the interaction between cognitive reappraisal and childhood adversity was a significant predictor of changes in psychological stress. We entered age, sex, annual income, symptoms of depression and anxiety (Time 1), psychological stress (Time 1), cognitive reappraisal, expressive suppression, childhood adversity and the interaction between childhood adversity and expressive suppression in step 1. In step 2, we entered the interaction term between childhood adversity and cognitive reappraisal. The interaction term was not a significant predictor of changes in psychological stress (B = −0.04, t (198) = −0.72, p = .47).
Emotion Regulation Strategy Use and Childhood Adversity as Predictors of Changes in Symptoms of Depression and Anxiety
Next, we investigated whether childhood adversity and emotion regulation strategies interactively informed changes in symptoms of depression and anxiety from before the pandemic to after the onset of the pandemic. In two separate hierarchical linear models, we tested whether the interaction between expressive suppression and childhood adversity predicted changes in symptoms of depression and anxiety (i.e., the difference in reported symptoms at Time 1 and Time 2). In these models, we entered age, sex, income, depressive and anxiety symptoms (Time 1), childhood adversity, cognitive reappraisal, the interaction between cognitive reappraisal and childhood adversity, and expressive suppression in step 1. In step 2, we entered the interaction term between childhood adversity and expressive suppression.
The interaction between childhood adversity and expressive suppression was a significant predictor of changes in depressive symptoms (B = 0.23 t (199) = 4.14, p < .001, R2 change = .05). Table 3 reports the full results of this hierarchical linear model. Figure 2 displays the pattern of the interaction, with high and low values for each variable representing one standard deviation above and below the mean respectively. Simple slopes analyses revealed that the relationship between childhood trauma and changes in depressive symptoms was statistically significant for AI adults who reported both low use of expressive suppression (i.e., 1 SD below the mean) and high use of expressive suppression (i.e., 1 SD above the mean) (B = 0.76, t (199) = 10.74, p < .001) and (B = 3.26, t (199) = 46.10, p < .001) respectively. Separate simple slopes analyses indicated that the relationship between expressive suppression and changes in depressive symptoms was statistically significant for AI adults who reported high levels of childhood trauma (i.e., 1 SD above the mean) (B = 2.38, t (199) = 33.65, p < .001), while the relationship was not statistically significant for AI adults who reported low levels of childhood adversity (i.e., 1 SD below the mean) (B = −0.12, t (199) = −1.69, p = .09).
Table 3.
Summary of hierarchical linear regression model with childhood adversity and emotion regulation strategies predicting changes in depressive symptoms.
| Predictor | B | SE B | β | p | R2 |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −.06 | .03 | −.14 | .022 | |
| Sex | .07 | .66 | .01 | .918 | |
| Annual income | −.36 | .20 | −.11 | .068 | |
| Anxiety symptoms (Time 1) | .39 | .19 | .13 | .036 | |
| Depressive symptoms (Time 1) | −.67 | .19 | −.21 | <.001 | |
| Childhood adversity | 2.14 | .34 | .39 | <.001 | |
| Cognitive reappraisal | .22 | .32 | .04 | .480 | |
| Cognitive reappraisal × Childhood adversity | −.31 | .30 | −.06 | .295 | |
| Expressive suppression | 1.24 | .32 | .22 | <.001 | |
| Step 2 | |||||
| Age | −.07 | .02 | −.16 | .008 | |
| Sex | .06 | .63 | .01 | .926 | |
| Annual income | −.43 | .19 | −.13 | .024 | |
| Anxiety symptoms (Time 1) | .37 | .18 | .12 | .038 | |
| Depressive symptoms (Time 1) | −.68 | .18 | −.21 | <.001 | |
| Childhood adversity | 2.01 | .33 | .36 | <.001 | |
| Cognitive reappraisal | .23 | .30 | .04 | .447 | |
| Cognitive reappraisal × Childhood adversity | −.13 | .29 | −.03 | .645 | |
| Expressive suppression | 1.13 | .31 | .20 | <.001 | |
| Childhood adversity × Expressive suppression | 1.22 | .30 | .23 | <.001 |
Note: Sex was coded as follows: Female =1, Male =2
Statistically significant predictors are listed in bold
Figure 2.
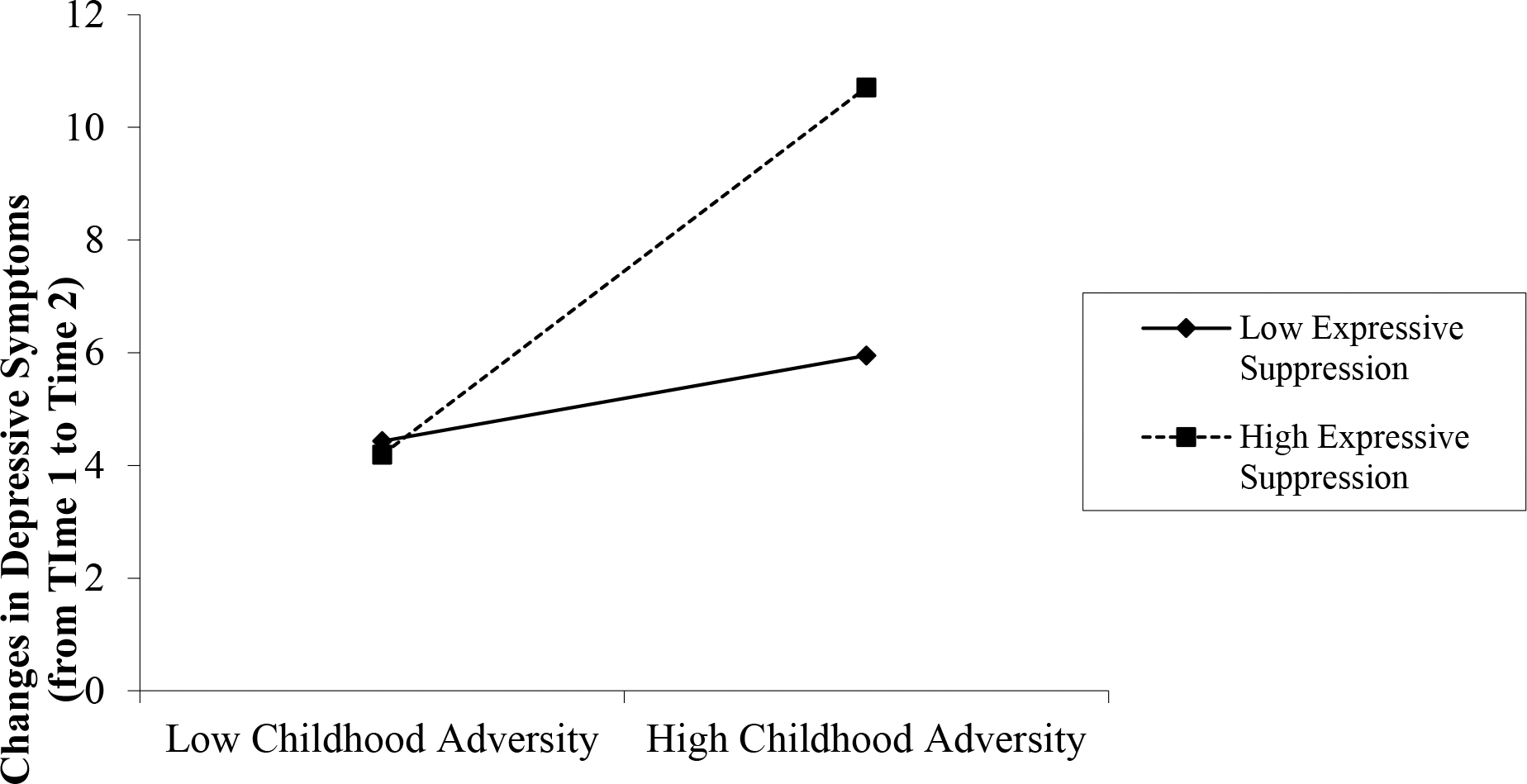
Changes in depressive symptoms following onset of COVID-19 pandemic as a function of expressive suppression and childhood adversity Results from a linear regression controlling for age, sex, annual income, symptoms of depression and anxiety at Time 1, cognitive reappraisal, and the interaction between cognitive reappraisal and childhood adversity.
Using the Johnson-Neyman technique (Rast et al., 2014), we identified regions of statistical significance for the interaction between childhood adversity and expressive suppression in predicting changes in depressive symptoms. We found that the relationship between childhood adversity and changes in depressive symptoms was statistically significant for those individuals who had an average score of 3.30 or higher on the expressive suppression scale (possible range = 1–7). Separate Johnson-Neyman analyses indicated that the relationship between expressive suppression and changes in depressive symptoms was statistically significant for those individuals who had a score of 20 or higher on the RFQ (possible range 10–50). The second hierarchical linear model predicting changes in symptoms of anxiety showed that the interaction between childhood adversity and expressive suppression was not a significant predictor of changes in symptoms of anxiety (B = 0.10, t (196) = 1.37, p = .17). Supplementary Table 1 reports the full results of this model.
Finally, in two separate models, we tested whether childhood adversity and cognitive reappraisal interactively informed changes in symptoms of depression and anxiety. In these models, we entered age, sex, income, anxiety and depressive symptoms at Time 1, childhood adversity, expressive suppression, the interaction between expressive suppression and childhood adversity, and cognitive reappraisal in step 1. In step 2, we entered the interaction term between childhood adversity and cognitive reappraisal. The interaction between childhood adversity and cognitive reappraisal was not a statistically significant predictor of changes in depressive symptoms or symptoms of anxiety (B = −0.03, t (199) = −0.46, p = .65) and (B = −0.04, t (196) = −0.63, p = .53) respectively.
Discussion
To our knowledge, the current research is the first to explore the roles of childhood adversity and emotion regulation strategies in shaping changes in outcomes linked to mental health in an AI sample in the context of a life event. This is important considering the disproportionately high rates of childhood trauma, and mental health conditions in AIs compared to the rest of the population (Cohen, 2000; Lee et al., 2007). A key strength of this work is its use of Community Based Participatory Research (CBPR) methodology. All components of the research were informed by the knowledge of members of a Community Advisory Board comprised of AI adults. As such, the measures and methodologies were deemed culturally appropriate and relevant for an AI sample.
We found that in a sample of 210 AI adults and in the context of a real-life event, childhood adversity moderates both the relationship between expressive suppression and changes in levels of psychological stress, and the relationship between expressive suppression and changes in depressive symptoms following the onset of the pandemic. We did not find evidence in this sample to support the idea that childhood adversity moderates the relationship between cognitive reappraisal as an emotion regulation strategy and psychological stress related to the pandemic, or the relationships between childhood adversity and symptoms of depression and anxiety following the onset of the pandemic.
Our findings build upon previous research indicating that adversity informs emotion regulation strategy use (Boden et al., 2013; Short et al., 2018), and are in line with prior work suggesting that emotion regulation strategy use and prior adversity shape an individual’s psychological stress response to life events (Moore et al., 2008). Specifically, we found that greater reports of childhood adversity were associated with greater increases in psychological stress following the onset of the pandemic for AI adults who reported low levels of expressive suppression (i.e., 1 SD below the mean) and high levels of expressive suppression (i.e., 1 SD above the mean). However, the relationship between expressive suppression and increases in psychological stress was only statistically significant for those AI adults in our sample who reported high levels of childhood adversity, with greater reported use of expressive suppression being related to greater increases in psychological stress.
In a similar manner, simple slopes analyses revealed that the positive relationship between childhood adversity and changes in depressive symptoms following the onset of the pandemic was statistically significant for AI adults who reported both low and high levels of expressive suppression. However, as with changes in psychological stress, the positive relationship between expressive suppression and changes in depressive symptoms was only statistically significant for those AI adults in our sample who reported high levels of childhood adversity.
Our findings suggest that expressive suppression may be a particularly maladaptive emotion regulation strategy in adulthood for AIs who experienced high levels of childhood adversity with regards to predicting changes in psychological stress and symptoms of depression following the onset of a life event. These findings are in line with prior research suggesting that compared to cognitive reappraisal, expressive suppression is perhaps a more significant contributor to stress-related symptoms (Moore et al., 2008). Our findings did not support our hypothesis that childhood adversity and use of emotion regulation strategies would interactively inform changes in anxiety symptoms. Most of the extant work investigating the relationship between use of expressive suppression and anxiety focuses on social anxiety. Thus, one possible explanation for the null findings in this project is that the type of anxiety assessed was not limited to social anxiety. Moreover, some research indicates that childhood adversity is more strongly related to later depressive symptomology compared to anxiety symptomology (Phillips et al., 2015).
Given previous research on the buffering effects of cognitive reappraisal on mental health outcomes, one might have expected to find statistically significant relationships between cognitive reappraisal and both changes in psychological stress and depressive symptoms, Individual differences in the perception of the stressor may determine what is typically maladaptive or adaptive. For example, an individual’s sense of control of the stressor can dictate whether use of cognitive reappraisal is effective (Troy et al., 2013). Moreover, research indicates implementation of adaptive emotion regulation strategies is more dependent on context than the use of maladaptive strategies (Aldao & Nolen-Hoeksema, 2012).
Limitations
These findings are based on a small sample of AI adults and cannot be generalized to the AI population as a whole. It is also possible that these findings would differ as a function of geographical location or membership in particular tribal communities. The modest sample size and small effect sizes are important limitations of this research. While the observed effect sizes were relatively small, as summarized in a recent paper, while seemingly small effects may not be consequential in a single episode, psychological processes that affect the behavior of an individual repeatedly, could have important implications over time (Funder & Ozer, 2019).
Further, it is important to note that based on input from our CAB comprised of AI adults, we opted to use the Risky Family Questionnaire (RFQ) as a measure of childhood adversity, instead of more commonly used measures of childhood trauma. While the RFQ has been used in previous investigations focused on the role of emotion regulation in shaping health-relevant outcomes (Taylor et al., 2004), it is limited in that it does not measure sexual abuse. Future work should include a measure of sexual abuse, as it likely informs the measured outcomes.
It is also important to note that there are many emotion regulation strategies beyond those which were measured in the current work. Additionally, strategy use is only one of several conceptualizations of emotion regulation that can be assessed (i.e., emotion dysregulation or difficulties, emotional understanding, etc.). As such, future work should examine whether similar relationships would be observed for other emotion regulation strategies (i.e., problem-solving, distraction, acceptance, etc.) as well as other features of emotion regulation (i.e., awareness, difficulties, etc.) that would lead to a more holistic investigation of these relationships. In spite of these noted limitations, the current work makes an important contribution to a very limited understanding of emotion regulation strategy use and implication for mental health in AIs.
Conclusion
This research contributes to a growing body of literature on the mental health ramifications of life events such as the COVID-19 pandemic and adds to the robust literature on the enduring implications of childhood adversity (Short et al., 2018). They also add to findings indicating that emotion regulation strategies can impact the degree to which life events affect outcomes linked to mental health (Moore et al., 2008). Since high use of expressive suppression as an emotion regulation strategy appears to be maladaptive for AIs who report high levels of childhood adversity, specifically when predicting increases in psychological stress and depressive symptoms in the context of a life stressor, it will be important to identify which emotion regulation strategies associate with optimal mental health outcomes for these individuals. Previous research indicates that individuals who experience trauma utilize adaptive emotion regulation strategies which are not limited to cognitive reappraisal. It is possible that there are other protective emotion regulation strategies not captured by the most commonly used emotion regulation strategy framework. Research also indicates the importance of considering culture and context when investigating whether an emotion regulation strategy is adaptive or maladaptive (Ford & Mauss, 2015).
Future work should examine the relationships between adversity, emotion regulation strategy use and mental health in the context of life stress across cultures. While a more diverse sample consisting of adults from various racial and ethnic backgrounds would allow for more generalizability, we felt it was critical to focus on AIs, as they are underrepresented in the emotion regulation literature and have disproportionately high rates of childhood trauma and mental health conditions. Future work should continue to focus on underrepresented populations during global events, especially when these populations are likely to experience more pronounced ramifications of these events. Overall, these findings provide an impetus to consider how cultural context, prior adversity, and use of emotion regulation strategies in the context of stressful life events affect mental health.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National institutes of Health under Award Number U54GM115371, and P20GM104417. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Footnotes
The study was not preregistered. The authors have access to all data and study analysis code and these can be made available upon reasonable request.
References
- Ahmed SP, Bittencourt-Hewitt A, & Sebastian CL (2015). Neurocognitive bases of emotion regulation development in adolescence. Developmental cognitive neuroscience, 15, 11–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A, & Nolen-Hoeksema S (2012). The influence of context on the implementation of adaptive emotion regulation strategies. Behaviour research and therapy, 50(7–8), 493–501. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical psychology review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Croy C, Klein SA, Whitesell NR, Mitchell CM, & AI-SUPERPFP Team. (2013). Lifetime prevalence of posttraumatic stress disorder in two American Indian reservation populations. Journal of traumatic stress, 26(4), 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, & Foote J (1994). Childhood Trauma Questionnaire (CTQ) [Database record]. APA PsycTests. 10.1037/t02080-000 [DOI] [Google Scholar]
- Boden MT, Westermann S, McRae K, Kuo J, Alvarez J, Kulkarni MR, ... & Bonn-Miller MO. (2013). Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social and Clinical Psychology, 32(3), 296–314. [Google Scholar]
- Breaux R, Dvorsky MR, Marsh NP, Green CD, Cash AR, Shroff DM, Buchen N, Langberg JM, & Becker SP (2021). Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: protective role of emotion regulation abilities. Journal of child psychology and psychiatry, and allied disciplines, 62(9), 1132–1139. 10.1111/jcpp.13382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter S, Powers A, & Bradley B (2020). PTSD and self-rated health in urban traumatized African American adults: The mediating role of emotion regulation. Psychological Trauma: Theory, Research, Practice, and Policy, 12(1), 84–91. 10.1037/tra0000472 [DOI] [PubMed] [Google Scholar]
- Chew QH, Wei KC, Vasoo S, Chua HC, & Sim K (2020). Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Tropical Journal of Pharmaceutical Research, 61(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Gianaros P, & Manuck S (2016). A Stage Model of Stress and Disease. Perspectives on Psychological Science, 11(4), 456–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007. Oct 10;298(14):1685–7. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Cohen JI (2000). Stress and mental health: a biobehavioral perspective. Issues in mental health nursing, 21(2), 185–202. [DOI] [PubMed] [Google Scholar]
- Cooke J, Eirich R, Racine N, & Madigan S (2020). Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Research, 292, 113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Avanzato C, Joormann J, Siemer M, & Gotlib IH (2013). Emotion regulation in depression and anxiety: examining diagnostic specificity and stability of strategy use. Cognitive Therapy and Research, 37(5), 968–980. [Google Scholar]
- De France K, & Evans GW (2020). Expanding context in the role of emotion regulation in mental health: How socioeconomic status (SES) and developmental stage matter. Emotion. [DOI] [PubMed] [Google Scholar]
- Dos Santos C, Pico-Perez M, & Morgado P (2020). COVID-19 and Mental Health-What Do We Know So Far? Frontiers in Psychiatry, 11, 565698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryman MT, & Heimberg RG (2018). Emotion regulation in social anxiety and depression: A systematic review of expressive suppression and cognitive reappraisal. Clinical Psychology Review, 65, 17–42. [DOI] [PubMed] [Google Scholar]
- Ehring T, Tuschen-Caffier B, Schnülle J, Fischer S, & Gross JJ (2010). Emotion regulation and vulnerability to depression: spontaneous versus instructed use of emotion suppression and reappraisal. Emotion, 10(4), 563. [DOI] [PubMed] [Google Scholar]
- Esbjørn BH, Bender PK, Reinholdt-Dunne ML, Munck LA, & Ollendick TH (2012). The development of anxiety disorders: Considering the contributions of attachment and emotion regulation. Clinical child and family psychology review, 15(2), 129–143. [DOI] [PubMed] [Google Scholar]
- Espey DK, Jim MA, Cobb N, Bartholomew M, Becker T, Haverkamp D, & Plescia M (2014). Leading causes of death and all-cause mortality in American Indians and Alaska Natives. American journal of public health, 104(S3), S303–S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Ford BQ, & Mauss IB (2015). Culture and emotion regulation. Current opinion in psychology, 3, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funder DC, & Ozer DJ (2019). Evaluating effect size in psychological research: Sense and nonsense. Advances in Methods and Practices in Psychological Science, 2(2), 156–168. 10.1177/2515245919847202 [DOI] [Google Scholar]
- Gross JJ, & Muñoz RF (1995). Emotion regulation and mental health. Clinical psychology: Science and practice, 2(2), 151–164. [Google Scholar]
- Gross JJ, & John OP (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of personality and social psychology, 85(2), 348. [DOI] [PubMed] [Google Scholar]
- Gullone E, & Taffe J (2012). The Emotion Regulation Questionnaire for Children and Adolescents (ERQ–CA): A psychometric evaluation. Psychological Assessment, 24(2), 409. [DOI] [PubMed] [Google Scholar]
- Horesh D, & Brown AD (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 331–335. 10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- Huh HJ, Kim KH, Lee HK, & Chae JH (2017). The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. Journal of affective disorders, 213, 44–50. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- Jamieson JP, Nock MK, & Mendes WB (2012). Mind over matter: Reappraising arousal improves cardiovascular and cognitive responses to stress. Journal of experimental psychology: General, 141(3), 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouros CD, Morris MC, & Garber J (2016). Within-Person Changes in Individual Symptoms of Depression Predict Subsequent Depressive Episodes in Adolescents: a Prospective Study. Journal of abnormal child psychology, 44(3), 483–494. 10.1007/s10802-015-0046-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon H, Yoon KL, Joormann J, & Kwon JH (2013). Cultural and gender differences in emotion regulation: Relation to depression. Cognition & Emotion, 27(5), 769–782. [DOI] [PubMed] [Google Scholar]
- The Lancet Infectious Diseases. (2020). The intersection of COVID-19 and mental health. The Lancet Infectious Diseases, 20(11), 1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, ... & Chua SE. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry, 52(4), 233–240. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD, & Ai-superpfp Team. (2005). Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health, 95(5), 851–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marusak HA, Martin KR, Etkin A, & Thomason ME (2015). Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology, 40(5), 1250–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto D, Yoo SH, & Nakagawa S (2008). Culture, emotion regulation, and adjustment. Journal of Personality and Social Psychology, 94(6), 925. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Peverill M, Gold AL, Alves S, & Sheridan MA (2015). Child maltreatment and neural systems underlying emotion regulation. Journal of the American Academy of Child & Adolescent Psychiatry, 54(9), 753–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed A, Kosonogov V, & Lyusin D (2021). Expressive suppression versus cognitive reappraisal: Effects on self-report and peripheral psychophysiology. International Journal of Psychophysiology, 167, 30–37. [DOI] [PubMed] [Google Scholar]
- Moore SA, Zoellner LA, & Mollenholt N (2008). Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? BehaviourRresearch and Therapy, 46(9), 993–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The role of the family context in the development of emotion regulation. Social Development, 16(2), 361–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Congress of American Indians (NCAI) (2020). Indian Country Demographics. Retrieved from [https://www.ncai.org/about-tribes/demographics]. July 6, 2021.
- Nolen-Hoeksema S, & Aldao A (2011). Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personality and Individual Differences, 51(6), 704–708. [Google Scholar]
- Phillips AC, Carroll D, & Der G (2015). Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety, Stress, & Coping, 28(4), 357–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plieger T, Melchers M, Montag C, Meermann R, & Reuter M (2016). Life stress as potential risk factor for depression and burnout. Personality and Individual Differences, 101, 505. [Google Scholar]
- Rast P, Rush J, Piccinin A, & Hofer SM (2014). The identification of regions of significance in the effect of multimorbidity on depressive symptoms using longitudinal data: an application of the Johnson-Neyman technique. Gerontology, 60(3), 274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE (2002). Risky families: family social environments and the mental and physical health of offspring. Psychol Bull, 128(2):330–366. [PubMed] [Google Scholar]
- Russell BS, Hutchison M, Park CL, Fendrich M, & Finkelstein-Fox L (2021). Short-term impacts of COVID-19 on family caregivers: Emotion regulation, coping, and mental health. Journal of clinical psychology, 10.1002/jclp.23228. Advance online publication. 10.1002/jclp.23228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short NA, Boffa JW, Clancy K, & Schmidt NB (2018). Effects of emotion regulation strategy use in response to stressors on PTSD symptoms: An ecological momentary assessment study. Journal of Affective Disorders, 230, 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaith RP (2003). The hospital anxiety and depression scale. Health and Quality of Life Outcomes, 1(1), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacciarini JMR, Shattell MM, Coady M, & Wiens B (2011). Community-based participatory research approach to address mental health in minority populations. Community Mental Health Journal, 47(5), 489–497. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lerner JS, Sage RM, Lehman BJ, & Seeman TE (2004). Early environment, emotions, responses to stress, and health. Journal of personality, 72(6), 1365–1394. [DOI] [PubMed] [Google Scholar]
- Troy AS, Shallcross AJ, & Mauss IB (2013). A person-by-situation approach to emotion regulation: Cognitive reappraisal can either help or hurt, depending on the context. Psychological Science, 24(12), 2505–2514. [DOI] [PubMed] [Google Scholar]
- Tyra AT, Ginty AT, & John-Henderson NA (2021). Emotion Regulation Strategies Predict PTSS During the COVID-19 Pandemic in an American Indian Population. International Journal of Behavioral Medicine, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (USCB) (2017). American Indian and Alaska Native Heritage Month. Retrieved from [https://www.census.gov/newsroom/facts-for-features/2017/aian-month.html]. July 6, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


