Abstract
Objective:
Early life stress (ELS) occurring during childhood and adolescence is an established risk factor for later cardiovascular disease and dysregulated reactivity to acute social stress. This study examined whether ELS associations with baseline cardiovascular functioning, cardiovascular stress reactivity and recovery, and emotional stress reactivity vary across levels of emotion-oriented, task-oriented, and avoidant coping styles.
Methods:
The sample included 1,027 adolescents and young adults (Mean age 19.29 years; 50% females; 64% Black, 34% Non-Hispanic White) who reported on their ELS exposure and coping styles. Participants completed a standardized acute social stress test (the Trier Social Stress Test; TSST), with heart rate (HR) and blood pressure (BP) measured before, during, and after the TSST. Self-reports of negative emotions during the TSST indexed emotional stress reactivity.
Results:
Multiple regression models adjusting for demographic factors and body mass index (BMI) showed that ELS was associated with lower HR stress reactivity; avoidant coping was related to lower SBP and DBP during stress and lower SBP during recovery; and higher emotion-oriented coping and lower task-oriented coping predicted greater emotional stress reactivity. A consistent pattern emerged where emotion-oriented coping amplified the associations between ELS and maladaptive stress responses (blunted cardiovascular stress reactivity and recovery; enhanced emotional stress reactivity), whereas lower levels of emotion-oriented coping were associated with resilient profiles among those who experienced ELS (lower resting HR; lower emotional stress reactivity; average HR and BP stress reactivity and recovery). However, low levels of emotion-oriented coping also conferred a risk of higher BP during recovery for those with high levels of ELS.
Conclusions:
These results suggest that low to moderate levels of emotion-oriented coping promote optimal cardiovascular and emotional reactivity to acute stress among individuals exposed to ELS.
Keywords: early life stress, coping, blood pressure, stress reactivity
Introduction
The ability to appropriately respond to psychosocial stress is at the heart of human health. Acute stress immediately triggers activation of the sympathetic-adrenal medullary (SAM) pathway with consequent release of adrenaline and noradrenaline, which in turn stimulate reactive increases in heart rate (HR) and blood pressure (BP)(1). An appropriate SAM response to stress is associated with better health outcomes, whereas both exaggerated and blunted stress reactivity of the SAM system are maladaptive and precede the development of health problems(2). These relationships were highlighted by a comprehensive review of 47 prospective studies with healthy adults that showed exaggerated cardiovascular stress responses [i.e., higher elevation of systolic and diastolic blood pressure (SBP, DBP) and HR] predicted increased cardiovascular disease (CVD) risk over time (e.g., hypertension, intima-media thickness, coronary artery calcification, and sudden coronary death), whereas a blunted response to stress was associated with the development of obesity, poor health, and cognitive and emotional problems(3, 4). In some studies, a blunted HR response also predicted greater CVD risk, especially in Black individuals(5, 6).
A robust predictor of both CVD risk and cardiovascular (CV) stress response is early life stress (ELS), defined as adverse and stressful life events experienced during childhood and adolescence(7). ELS is associated with elevated resting SBP and DBP as early as in adolescence and young adulthood(8, 9) and serves as a robust risk factor for hypertension and CVD throughout the lifespan(10, 11). Studies have also found robust associations between ELS and CV reactivity to acute stress. Paradoxically, most studies show that adolescents and young adults who experienced higher levels of ELS exhibited lower (i.e., blunted) HR and BP reactivity to acute psychosocial stress(8, 12–16). However, a few studies reported opposite findings, linking ELS with exaggerated DBP stress reactivity in adolescents(17) and lower resting SBP in young adults(18).
Some of these discrepant findings may be explained by the presence of other risk or protective factors that amplify or mitigate the relationships between ELS and CV functioning. For example, two longitudinal studies linked ELS with CVD risk in adulthood only in individuals who received less supportive parenting as children, but not in those who received more supportive parenting(19, 20). Although no studies examined moderators of the links between ELS and CV reactivity to acute stress, recent stressful life events were more strongly related to blunted SBP stress reactivity in young adults with low emotional stability and low openness to experience(21). Additionally, recent stressful life events were related more strongly to blunted HR reactivity to acute stress for young adults with more close friends(22). Finally, a study with older adults found that ELS was associated with a blunted cortisol response to acute stress among individuals with a history of psychological distress, but with an augmented cortisol stress response among those without such history(23). These studies suggest that psychosocial factors may modify the associations between ELS and cardiovascular reactivity to acute stress.
One modifiable psychosocial factor that may alter the impact of ELS on CVD risk is coping. Coping refers to conscious efforts to regulate one’s behavior, cognitions, emotions, physiology, and environment in response to stressful events(24). Studies typically distinguish between engagement coping, such as task-oriented and emotion-oriented coping, which is directed toward the stressors or related thoughts and emotions, and disengagement coping, such as avoidance and denial, which involves orientation away from the stressor(25). In general, task-oriented coping tends to be associated with better health outcomes, whereas emotion-oriented and avoidant coping are linked with poorer health(26, 27). For instance, greater use of emotion-oriented coping predicted higher disease severity in cardiac patients over a 3-month follow up(28). Coping styles are also related to the acute stress response. For example, task-oriented coping was associated with an exaggerated HR response, whereas avoidant coping was related to a blunted HR response to acute stress(29). Further, both avoidant and emotion-oriented coping were related to higher emotional reactivity (i.e., more negative emotions) to acute stress(30).
Although ELS has been related to less adaptive coping styles (e.g., less task-oriented and more avoidant coping), there is variability in coping styles utilized by individuals exposed to similar levels of ELS(31). Thus, coping styles could moderate the associations between ELS and health outcomes, including stress reactivity. Indeed, one study with young Black adults found that chronic stress was associated with blunted HR reactivity to stress only for individuals using high levels of emotion-oriented coping(29), and another study with Black college students found that both task-oriented and emotion-oriented coping amplified the relationship between recent stressful events and DBP reactivity to acute stress(32). However, neither of these studies examining ELS, coping, and acute stress reactivity included CV functioning (e.g., BP and HR) at rest and during recovery from acute stress to better understand the roles of ELS and coping in CVD risk.
In this study, we examined whether coping moderates the associations between ELS and resting BP and HR, as well as cardiovascular and emotional reactivity to acute psychosocial stress and cardiovascular recovery from acute stress. These relationships were examined in late adolescence and young adulthood, when links between ELS and CVD risk typically emerge, and included three types of coping commonly investigated in coping research – task-oriented coping, emotion-oriented coping, and avoidant coping. Based on prior research, it was hypothesized that ELS would be associated with higher resting BP; lower HR and BP reactivity to stress; higher emotional reactivity to stress; and lower HR and BP during recovery. It was also expected that these relationships would be reduced by high levels of task-oriented coping and amplified by high levels of emotion-oriented and avoidant coping.
Method
Sample
This study used a community sample of 1,027 adolescents and young adults (mean age 19.29 years, SD=1.19, range 16 to 23 years; 50.2% females, 64.0% Black, 33.6% Non-Hispanic White, 2.4% Other race/ethnicity) who participated in Wave 4 of Healthy Passages conducted in Birmingham, Alabama, between 2012 and 2017(33). Youth were originally recruited from fifth grade general education classrooms in public schools in Birmingham, Alabama, using two-stage probability sampling (58% participation rate) in 2004–2006 and assessed in Waves 1–3 as part of the multi-site Healthy Passages study of adolescent health(34). Because CV reactivity to stress and coping were only assessed at Wave 4 (which was conducted at the Birmingham site only), data from previous assessments are not included in this report. Of the 1,594 participants in Wave 1, those included in this report were more likely to be Black (64% vs. 46%, p<.001) and have lower household income (M=7.55 vs 9.00, p<.001) than those not included, but the two groups did not differ in sex.
Procedures
All study procedures were approved by the University of Alabama at Birmingham Institutional Review Board. After providing informed consent, each participant was interviewed individually by a trained interviewer using computer-assisted technology. The first 60 minutes of the interview did not include sensitive or distressing questions; it included demographic information, academic and occupational history, family relationships, and leisure time activities. Then, participants completed the Trier Social Stress Test (TSST)(35), a standardized psychosocial test that reliably elicits strong physiological and psychological stress responses in both adults and adolescents(36, 37). The standard TSST procedures, including both speech and math tasks, were followed.
Participants were taken to a different room and asked to sit down in a chair next to a desk. A wrist cuff from a Vasotrac BP monitor(38) was attached to their non-dominant hand. BP and HR readings were taken every 30 seconds throughout the TSST, from baseline to recovery. Participants were asked to keep their wrist with the cuff in the same position on the armrest and not cross their legs. Then, they were asked to rest for five minutes (baseline) alone in the room; they could drink water and browse magazines on a table next to their chair.
After the 5-minute baseline, the interviewer returned and introduced the TSST speech and math tasks. Participants were told that they will give a speech and do some math in front of two people who will be judging their performance and who are trained in analyzing verbal and nonverbal signs of stress; they will also be videotaped so other researchers can evaluate their performance. To motivate effort, participants were asked to do their best on the tasks and informed that those performing in the top 20% would choose a special prize; the prizes (e.g., travel mug, nice notebook with a pen) were shown. For the speech task, participants were asked to imagine that they applied for a job and were invited to present themselves to the selection committee. They would have 5 minutes to introduce themselves and tell the committee why they are the best person for the position. Then, they were asked what job they would like to have and could realistically get right now, and describe the job and its duties. Two judges in white coats then entered the room (one Black, one White; one male, one female), introduced themselves, and provided more detailed instructions for the speech task, emphasizing the evaluative aspects of the tasks. Participants were given a pen and paper to prepare for the speech task for the next 5 minutes alone in the room, and told they would not be able to use the notes during the task.
After the 5-minute preparation period, the judges returned, collected the participants’ notes, turned on the camera, set down at a table facing the participant from several meters away, and instructed the participant to begin and speak for the full 5 minutes. The judges maintained neutral facial expressions and eye contact with the participant, occasionally taking notes; they did not provide any positive feedback (e.g., smiling, nodding). If the participants moved their wrist with the cuff or crossed their legs, the judges reminded them to keep their wrist on the armrest and uncross their legs. If the participants finished talking early, the judges asked them to continue for the full 5 minutes. After at least 3 minutes of the task, two prompts to speak for the full 5 minutes, and 10 seconds of silence, the judges asked one or two questions about the participants’ weaknesses, mistakes they made, or conflicts they have had with bosses or co-workers.
Next, the judges asked the participants to perform a mental arithmetic task for 5 minutes as quickly and accurately as possible. They explained that if the participants make a mistake, they will need to start over, and that they will be evaluated on speed, accuracy, and signs of stress. Participants were asked to start at 996 and serially subtract 13. If they were counting accurately, they were asked to do it more quickly. If they made a mistake, they were asked to start over. If participants made 3 mistakes in a row or showed signs of disengagement, they were given an easier serial subtraction task (e.g., 509 minus 7; then 407 minus 3; etc.). If the task was judged too easy, a more difficult task would be given (e.g., 2043 minus 17), but this did not occur in this study. At the end of the 5-minute math task, the judges thanked the participants, asked them to complete a questionnaire about their experiences with the task, and rest alone for a 5-minute recovery period.
After the 5-minute recovery period, the interviewer removed the wrist cuff and congratulated the participants on completing the tasks. The judges returned, provided positive feedback and debriefing, and invited the participants to ask any questions about the tasks. Each participant then selected one of the special prizes and was taken back to the interview room to finish the individual interview.
At the end of the interview, participants’ height was measured using a portable stadiometer and recorded to the nearest 0.1 cm. Weight was measured using a portable electronic scale and recorded to the nearest 0.01 kg. Two height and weight measurements were taken and if they differed by > 0.5 cm for height or > 0.5 kg for weight, a third measurement was taken. The average of the two closest values was used to compute body mass index (BMI).
Measures
Early life stress (ELS).
Using an adapted version of the Adolescent Life Change Event Scale(39), participants were asked whether they had experienced each of 26 stressful life events in their lifetime. The items included events happening both to the participants and their parents or family members, including relationship problems, financial problems, job loss, parental separation or divorce, trouble with the law, incarceration, crime victimization, serious illness or death, natural disasters, military service, and military deployment to a combat zone. Responses were coded on a 3-point scale of ‘Never’ (0), ‘More than 1 year Ago’ (1), and ‘During the last 12 months’ (2) and averaged for a continuous ELS score. For sensitivity analyses, the items were separated into five subscales – death (4 items), illness (5 items), interpersonal (8 items), criminal (4 item), and financial/job/other (6 items)(40, 41).
Coping.
Coping styles were measured with self-report on the Coping Inventory for Stressful Situations (CISS)(42). Participants were asked how often they engage in each of 48 activities when they encounter a difficult, stressful, or upsetting situation. The items comprise three 16-item subscales of task-oriented coping (e.g., analyze the situation, try to solve the problem, get organized), emotion-oriented coping (e.g., blame myself, feel anxious, get angry), and avoidant coping (e.g., do other things, get together with other people). The items were rated on a 5-point scale from ‘Do not use at all’ (1) to ‘Use very much’ (5) and were averaged to create the subscales of emotion-oriented coping (α=.86), avoidant coping (α=.82), and task-oriented coping (α=.89).
CV reactivity to stress.
Before the baseline TSST period started, a wrist cuff from a Vasotrac BP monitor(38) was attached to each participant’s non-dominant hand. HR and BP were recorded every 30 seconds during the 5-minute baseline, 5-minute speech task, 5-minute math task, and 5-minute recovery periods. Screening of individual values revealed a small number of failed readings (<0.25%). Out of range values (HR <38 or >230; SBP <58 or >250; DBP <38 or >145)(43, 44) were recoded to missing (1.43% of values). Baseline levels of HR and BP were then computed as the average of the last two baseline measurements (to allow participants to achieve a true baseline). The 10 HR and BP measurements taken during each period (speech, math, recovery) were averaged. Because the values were strongly correlated between the speech and math periods (r = .78 to .81, p<.001), these two were averaged. Finally, stress reactivity and recovery reactivity were computed by subtracting the baseline average from the stress (speech, math) average and recovery scores for HR, SBP, and DBP, respectively. For sensitivity analyses, stress reactivity was computed by subtracting the baseline average from average HR, SBP, and DBP during the 5-minute preparation period.
Emotional reactivity to stress.
A self-report questionnaire was administered immediately after the TSST to assess participants’ emotional reactivity to psychosocial stress. Participants were asked to rate their reactions to the speech and math tasks on a scale ranging from 1 (Not at all) to 5 (Very much). Nine items indexing negative emotional reactivity to stress (e.g., “During the tasks, I felt upset”, “angry”, “ashamed”, “irritated”, “hostile”) were averaged (α=.89).
Covariates.
Covariates included age (computed from date of birth and date of interview), self-reported sex (male, female) and race (Black, White, Other), BMI, and childhood family SES, computed as parent-reported household income in Wave 1 (average age 11) divided by poverty threshold for a household of the given size in the year of data collection.
Data Analyses
Descriptive statistics and bivariate correlations among all variables were examined. Responders to the TSST were classified as those with 10% or greater increase in HR, SBP, or DBP from baseline to the TSST speech and math tasks. Independent samples t-tests evaluated differences between TSST responders and non-responders in ELS, coping, and emotional reactivity.
Main analyses of the effects of ELS and coping on cardiovascular functioning and stress reactivity included three multivariate hierarchical linear regressions conducted in Mplus, using Full Information Maximum Likelihood to utilize all available data (N=1,027) and minimize bias from missing data (0.69% of data points were missing, primarily from family SES). The first model included resting HR, SBP, and DBP as outcomes. The second model predicted HR, SBP, DBP, and emotional reactivity to stress. The third model included HR, SBP, and DBP recovery reactivity. In each of these models, Step 1 included all covariates (age, sex, race/ethnicity, BMI, and childhood family SES), ELS, and the three coping variables (task-oriented, emotion-oriented, and avoidant coping). Step 2 added interactions between ELS and each coping variables. Significant interactions were followed by visualization of the continuous ELS effects on the outcomes estimated at high and low levels of coping (1 SD above and below the sample mean) using coefficients from the full regression model. Additionally, tests of regions of significance identified levels of coping at which ELS became significantly related to the outcome and the values of the ELS slopes at those levels of coping. Compared to more traditional simple slope tests which would test the significance of the ELS simple slopes at specific levels of coping (e.g., 1 SD below or above the mean), regions of significance are recommended by current methodological literature because they provide more detailed information (i.e., they identify the full regions of significance across the range of coping instead of testing significance at a few specific levels of coping) (45). Post-hoc power for significant effects of interest was computed with GPower 3.1.
Four sets of sensitivity analyses were conducted. First, multigroup modeling tested sex differences in the links between ELS, coping, and all outcomes. Specifically, for each of the three main models, a likelihood ratio test compared a model where all paths were constrained to be equal between males and females to a model where the main and interactive effects of ELS and the three coping variables were free to vary by sex. A significant test was followed by comparisons of the fully constrained model with a model where only one path at a time was freed to vary by sex. The second sensitivity analysis examined whether the cardiovascular stress reactivity results replicated during the preparation period before the speech task began. The third analysis tested replication across the speech and math tasks of the TSST. Instead of combining HR, SBP, and DBP across the speech and math portions of the TSST, they were analyzed separately for the speech task and the math task (one model for each). The final sensitivity analysis explored whether the main results replicate across different types of ELS. The three main models were rerun for each type of ELS – death, illness, interpersonal, criminal, and financial/job/other.
Results
Sample Characteristics and Preliminary Analyses
The sample included 1,027 participants with mean age 19.29 years, SD=1.19; 50.2% females; 64.0% Black, 33.6% Non-Hispanic White, and 2.4% Other race/ethnicity. Average BMI was 26.65 (SD=7.62); the average ratio of age 11 household income to federal poverty threshold was 2.60 (SD=2.80). Descriptive statistics and correlations among key variables are shown in Table 1. The TSST elicited robust increases in HR, SBP, and DBP (16% to 22% over baseline) and moderate levels of negative emotional reactivity; 91% of participants were classified as responders based on 10% or greater increase in HR, SBP, or DBP. Results of t-tests indicated that responders had lower levels of ELS than non-responders (M=0.46 vs. 0.57, t(1025)=3.98, p<.001, Cohen’s d=0.40), but the two groups did not differ in coping styles or emotional reactivity to the TSST (p=.099 to .98). Bivariate correlations revealed that higher ELS was associated with more emotion-oriented and avoidant coping, higher baseline SBP, lower HR and SBP stress reactivity, less elevated HR during recovery, and higher emotional stress reactivity. Emotion-oriented and avoidant coping were associated with greater emotional reactivity to acute stress. Avoidant coping was also related to lower SBP and DBP stress reactivity and less elevated SBP during recovery. Task-oriented coping was associated with lower baseline HR, and emotional stress reactivity was associated with lower SBP and DBP stress reactivity. All of these correlations had small effect sizes.
Table 1.
Descriptives and Correlations of Key Variables
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| 1. ELS | 0.42 (0.21) | -- | ||||||||||||
| 2. Emotion Coping | 2.61 (0.69) | .33* | -- | |||||||||||
| 3. Avoidant Coping | 2.98 (0.63) | .11* | .35* | -- | ||||||||||
| 4. Task Coping | 3.64 (0.63) | .02 | .10* | .35* | -- | |||||||||
| 5. HR rest | 72.45 (13.03) | −.03 | .06 | .02 | −.07* | -- | ||||||||
| 6. SBP rest | 125.52 (19.33) | .07* | .01 | .01 | −.02 | −.06* | -- | |||||||
| 7. DBP rest | 68.16 (13.09) | .05 | −.01 | .00 | .00 | −.03 | .93* | -- | ||||||
| 8. Δ HR Stress | 14.64 (14.67) | −.11* | .00 | −.04 | .02 | −.24* | −.03 | −.07* | -- | |||||
| 9. Δ SBP Stress | 18.80 (21.80) | −.06* | −.03 | −.13* | −.01 | .07* | −.24* | −.22* | .24* | -- | ||||
| 10. Δ DBP Stress | 14.22 (12.59) | −.05 | −.01 | −.10* | −.01 | .05 | −.16* | −.24* | .26* | .86* | -- | |||
| 11. Δ HR Recovery | 3.11 (10.97) | −.06* | −.02 | −.01 | .01 | −.34* | .03 | −.01 | .59* | .11* | .12* | -- | ||
| 12. Δ SBP Recovery | 9.62 (18.28) | −.04 | −.02 | −.07* | .03 | .06 | −.36* | −.34* | .17* | .68* | .59* | .14* | -- | |
| 13. Δ SBP Recovery | 6.36 (14.65) | −.04 | −.03 | −.05 | .03 | .04 | −.25* | −.31* | .21* | .59* | .60* | .26* | .86* | -- |
| 14. EmReact | 2.60 (1.05) | .10* | .26* | .17* | −.03 | .06 | .01 | .01 | −.02 | −.10* | −.10* | .00 | −.03 | −.03 |
Note: N=1027; ELS – early life stress; Emotion Coping – emotion-oriented coping; Task Coping – task-focused coping; Δ – increase from baseline; EmReact – emotional reactivity
p<.05 or lower
Main Analyses
Standardized coefficients from the multivariate hierarchical regression models predicting CV baseline, stress reactivity, and stress recovery are presented in Tables 2, 3, and 4, respectively. After adjusting for covariates, ELS predicted lower HR reactivity to acute stress (Table 3). Emotion-oriented coping predicted higher emotional stress reactivity, whereas task-oriented coping predicted lower emotional stress reactivity and higher DBP during recovery. Avoidant coping predicted lower SBP and DBP reactivity to stress, as well as lower SBP during recovery. In Step 2, emotion-oriented coping interacted with ELS to predict baseline HR, all three indicators of CV stress reactivity, emotional reactivity to stress, and SBP and DBP recovery. All significant effects were of small magnitude. Post-hoc power for significant main effects of ELS and coping ranged from 0.64 to 0.99 (average 0.79). The post-hoc power for detecting the significant ELS by emotion-oriented coping interactions ranged between 0.47 and 0.86 (average 0.66).
Table 2.
Multivariate Regression Predicting Cardiovascular Baseline
| HR rest | SBP rest | DBP rest | ||||
|---|---|---|---|---|---|---|
| β [95% CI] | p | β [95% CI] | p | β [95% CI] | p | |
|
| ||||||
| Step 1 | ||||||
| Age | −.05 [−.11; .01] | .085 | −.05 [−.11; .01] | .084 | −.06 [−.12; .00] | .069 |
| Female | .23 [.17; .29] | <.001 | −.21 [−.27; −.15] | <.001 | −.19 [−.25; −.13] | <.001 |
| Black | −.14 [−.21; −.06] | .001 | .02 [−.06; .10] | .64 | .02 [−.06; −.10] | .60 |
| Other race | .03 [−.03; .09] | .38 | .00 [−.06; .06] | .92 | .01 [−.06; .07] | .86 |
| BMI | .12 [.06; .18] | <.001 | .22 [.16; .28] | <.001 | .21 [.15; .26] | .001 |
| Family SES | −.04 [−.12; .04] | .30 | −.02 [−.10; .05] | .55 | −.01 [−.08; .07] | .90 |
| Early life stress | −.02 [−.09; .04] | .50 | .06 [−.01; .12] | .078 | .06 [−.01; .12] | .078 |
| Emotion coping | .05 [−.01; .12] | .11 | −.01 [−.08; .06] | .79 | −.03 [−.09; .04] | .44 |
| Avoidant coping | .00 [−.07; .07] | .99 | .03 [−.04; .10] | .44 | .01 [−.06; .08] | .69 |
| Task coping | −.05 [−.11; .01] | .12 | −.02 [−.09; .04] | .51 | −.02 [−.08; .05] | .64 |
| Step 2 | ||||||
| ELS × Emotion coping | .08 [.01; .14] | .019 | −.01 [−.08; .05] | .56 | .00 [−.07; .06] | .94 |
| ELS × Avoidant coping | −.06 [−.13; .00] | .064 | .04 [−.03; .10] | .30 | .03 [−.04; .09] | .46 |
| ELS × Task coping | −.02 [−.09; .04] | .44 | .02 [−.04; .08] | .51 | .01 [−.05; .07] | .74 |
Note: N=1027; ELS – early life stress.
Table 3.
Multivariate Regression Predicting Cardiovascular and Emotional Stress Reactivity
| Δ HR Stress | Δ SBP Stress | Δ DBP Stress | Emotional Reactivity | |||||
|---|---|---|---|---|---|---|---|---|
| β [95% CI] | p | β [95% CI] | p | β [95% CI] | p | β [95% CI] | p | |
|
| ||||||||
| Step 1 | ||||||||
| Age | −.07 [−.13; −.02] | .012 | −.21 [−.26; −.15] | <.001 | −.18 [−.23; −.12] | <.001 | .02 [−.03; .08] | .41 |
| Female | .18 [.12; .24] | <.001 | −.18 [−.24; −.13] | <.001 | −.16 [−.21; −.10] | <.001 | .16 [.10; .21] | <.001 |
| Black | −.15 [−.23; −.08] | <.001 | −.07 [−.14; .00] | .051 | −.12 [−.19; −.04] | .002 | .17 [.09; .24] | <.001 |
| Other race | −.05 [−.11; .01] | .086 | −.02 [−.08; .04] | .49 | −.04 [−.10; .01] | .13 | .00 [−.06; .06] | .95 |
| BMI | .04 [−.02; .09] | .22 | .21 [.15; .26] | <.001 | .23 [.17; .28] | <.001 | .07 [.02; .13] | .012 |
| Family SES | .10 [.03; .17] | .009 | .01 [−.07; .08] | .88 | .00 [−.08; .07] | .91 | −.08 [−.15; −.002] | .046 |
| Baseline outcome | −.32 [−.37; −.26] | <.001 | −.41 [−.45; −.37] | <.001 | −.41 [−.45; −.36] | <.001 | -- | |
| Early life stress | −.09 [−.15; −.03] | .003 | −.02 [−.08; .04] | .53 | −.01 [−.07; .05] | .66 | .00 [−.06; .06] | .96 |
| Emotion coping | .05 [−.01; .11] | .12 | −.01 [−.03; .09] | .44 | .02 [−.04; .08] | .50 | .22 [.16; .28] | <.001 |
| Avoidant coping | −.03 [−.10; .04] | .36 | −.10 [−.16; −.04] | .002 | −.07 [−.13; −.003] | .040 | .05 [−.01; .12] | .13 |
| Task coping | .03 [−.04; .09] | .41 | .05 [−.01; .11] | .099 | .05 [−.01; .11] | .094 | −.08 [−.14; −.02] | .013 |
| Step 2 | ||||||||
| ELS × Emotion coping | −.06 [−.13; −.001] | .045 | −.07 [−.13; −.01] | .026 | −.09 [−.15; −.03] | .004 | .07 [.01; .13] | .035 |
| ELS × Avoidant coping | .00 [−.07; .06] | .99 | .02 [−.05; .08] | .63 | .05 [−.02; .11] | .15 | −.01 [−.07; .06] | .87 |
| ELS × Task coping | .02 [−.04; .08] | .59 | .00 [−.06; .06] | .93 | .01 [−.05; .07] | .77 | .00 [−.06; .06] | .99 |
Note: N=1027; ELS – early life stress; Δ – increase from baseline.
Table 4.
Multivariate Regression Predicting Cardiovascular Recovery
| Δ HR Recovery | Δ SBP Recovery | Δ DBP Recovery | ||||
|---|---|---|---|---|---|---|
| β [95% CI] | p | β [95% CI] | p | β [95% CI] | p | |
|
| ||||||
| Step 1 | ||||||
| Age | −.06 [−.11; .00] | .059 | −.13 [−.19; −.08] | <.001 | −.14 [−.20; −.09] | <.001 |
| Female | .11 [.05; .17] | <.001 | −.14 [−.20; −.08] | <.001 | −.11 [−.16; −.05] | <.001 |
| Black | −.10 [−.18; −.03] | .007 | −.074 [−.11; .03] | .28 | −.04 [−.11; .04] | .30 |
| Other race | −.05 [−.11; .01] | .073 | −.02 [−.08; .03] | .42 | −.03 [−.09; .03] | .36 |
| BMI | .15 [.09; .21] | <.001 | .16 [.11; .22] | <.001 | .14 [.08; .20] | <.001 |
| Family SES | .06 [−.02; .13] | .14 | −.03 [−.10; .04] | .44 | −.01 [−.08; .07] | .80 |
| Baseline outcome | −.40 [−.45; −.34] | <.001 | −.48 [−.52; −.43] | <.001 | −.40 [−.44; −.35] | <.001 |
| Early life stress | −.05 [−.11; .01] | .085 | −.01 [−.07; .05] | .80 | .01 [−.06; .07] | .87 |
| Emotion coping | .01 [−.06; .07] | .85 | .01 [−.06; .07] | .85 | −.02 [−.09; .04] | .49 |
| Avoidant coping | .00 [−.07; .06] | .97 | −.07 [−.13; −.002] | .043 | −.05 [−.11; .02] | .18 |
| Task coping | .00 [−.06; .06] | .96 | .05 [−.01; .11] | .080 | .07 [.01; .13] | .033 |
| Step 2 | ||||||
| ELS × Emotion coping | −.02 [−.09; .04] | .46 | −.07 [−.13; −.01] | .018 | −.07 [−.14; −.01] | .019 |
| ELS × Avoidant coping | .03 [−.04; .09] | .44 | .04 [−.03; .10] | .25 | .01 [−.05; .08] | .66 |
| ELS × Task coping | .00 [−.06; .06] | .89 | .01 [−.05; .07] | .74 | .04 [−.02; .10] | .21 |
Note: N=1027; ELS – early life stress; Δ – increase from baseline.
The significant interactions are visualized in Figures 1 and 2. Follow up analyses indicated that ELS was significantly associated with lower baseline HR at low levels of emotion-oriented coping (0.68 SD below the mean and lower, B ≤ −4.92, p<.05; Figure 1). At very high levels of emotion-oriented coping, ELS was related to higher baseline HR (3.03 SD above the mean or higher, B ≥ 11.31, p<.05). For all CV stress reactivity outcomes, ELS was significantly associated with lower reactivity above specific levels of emotion-oriented coping (for HR above 0.29 SD below the mean, B ≤ −4.58, p<.05; for SBP above 1.10 SD above the mean, B ≤ −8.46, p<.05; and for DBP above 0.86 SD above the mean, B ≤ −4.51, p<.05; Figure 2). Additionally, ELS was associated with higher levels of DBP stress reactivity at low levels of emotion-oriented coping (1.21 SD below the mean or lower, B ≥ 6.05, p<.05). Finally, ELS was related to higher emotional stress reactivity at very high levels of emotion-oriented coping (above 3.14 SD above the mean, B ≥ 0.91, p<.05) and lower emotional stress reactivity at low levels of emotion-oriented coping (below 2.29 SD below the mean, B ≤ −0.76, p<.05; Figure 2).
Figure 1.
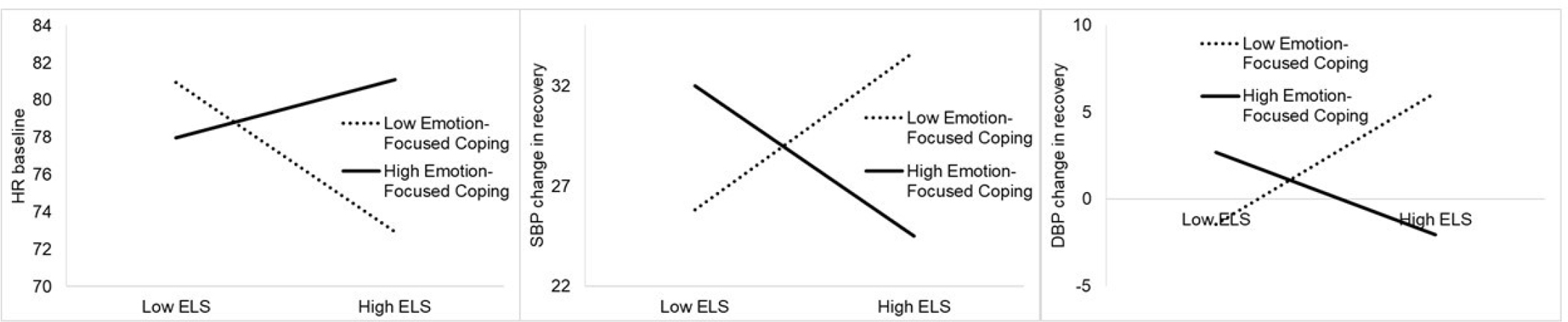
Emotion-oriented coping modifies the effects of ELS on resting HR and change in BP from baseline to recovery.
Note: The x-axis depicts the full range of ELS scores; high and low emotion-oriented coping are depicted at 1 SD above and below the mean based on results of the regression model with continuous ELS and coping variables.
Figure 2.
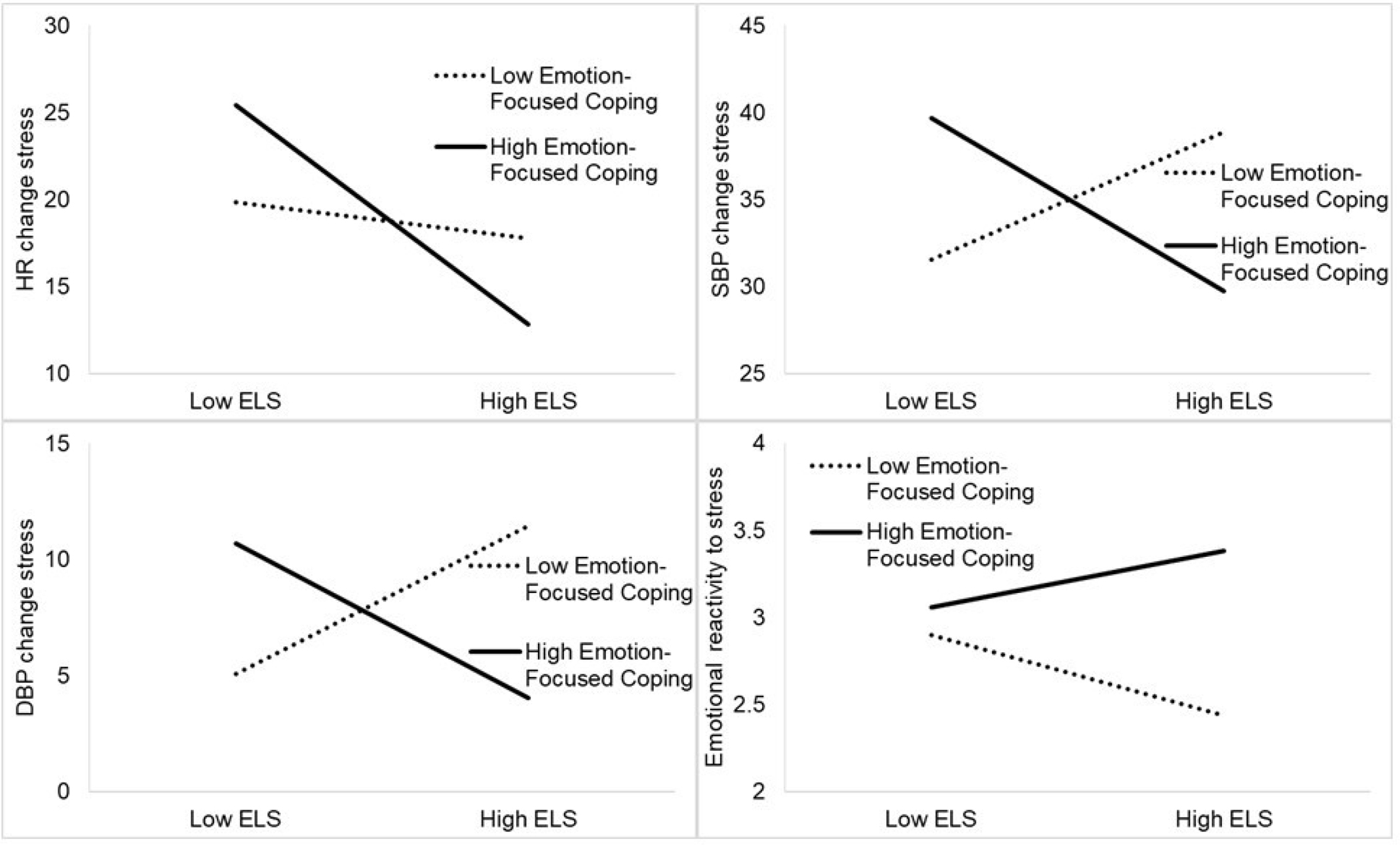
Emotion-oriented coping modifies the effects of ELS on cardiovascular and emotional reactivity to acute stress.
Note: The x-axis depicts the full range of ELS scores; high and low emotion-oriented coping are depicted at 1 SD above and below the mean based on results of the regression model with continuous ELS and coping variables.
During recovery, ELS was significantly associated with higher SBP and DBP at low levels of emotion-oriented coping (SBP: below 1.85 SD below the mean, B ≥ 11.32, p<.05; DBP: below 1.20 SD below the mean, B ≥ 6.90, p<.05). At high levels of emotion-oriented coping, ELS was related to lower SBP and DBP during recovery (SBP: above 1.39 SD above the mean, B ≤ −8.18, p<.05; DBP: above 2.10 SD above the mean, B ≤ −9.01, p<.05; Figure 1).
Sensitivity Analyses
The first set of sensitivity analyses used multigroup modeling to test sex differences in the main and interactive effects of ELS and coping on all outcomes. The stress reactivity model had to be split into two models for cardiovascular vs. emotional reactivity outcomes due to nonconvergence. The three models with cardiovascular outcomes (baseline, stress reactivity, and recovery reactivity) did not show any sex differences (χ2(21) ≥ 24.43, p ≥ .26). The model predicting emotional stress reactivity demonstrated sex differences (χ2(7) = 25.91, p < .001). Follow up tests of specific paths revealed a sex difference in the link between avoidant coping and emotional stress reactivity (χ2(1) = 4.73, p = .030), which was positive in females (β = .14, p = .002) and non-significant in males (β = .01, p= .76).
In the second sensitivity analyses, the multivariate regression predicted CV reactivity during the preparation period. There were no main effects of ELS or coping, but the interaction of ELS with emotion-oriented coping replicated for SBP and DBP preparation reactivity (β = −.07, p= .041 and β = −.07, p= .020).
The third set of sensitivity analyses repeated the multivariate regressions predicting CV reactivity to acute stress separately for the speech and math tasks of the TSST. The main effect of ELS on lower HR stress reactivity replicated across both speech and math tasks, but the interactions between ELS and emotion-oriented coping were only significant (p<.05) for CV reactivity (HR, SBP, and DBP) during the speech task and not during the math task. This may have been due to generally higher stress reactivity during the speech task compared to the math task [HR: M=16.08 vs. 12.33, t(1022)=8.81, p<.001; SBP: M=20.28 vs. 18.21, t(1022)=1.56, p=.12; DBP: M=13.39 vs. 12.47, t(1022)=2.29, p=.022]. Additionally, emotion-oriented coping was associated with higher HR and SBP stress reactivity during the speech task (β=.09, p=.006; β=.07, p=.034) but not during the math task, and task-oriented coping was related to higher HR stress reactivity during the speech task (β =.07, p=.020) but not during the math task.
The final set of sensitivity analyses repeated all models with specific subtypes of ELS (death, illness, interpersonal, criminal, and financial/job/other). In the model predicting baseline HR and BP, the significant interaction of ELS with emotion-oriented coping replicated for illness and interpersonal stressors. Additionally, an interaction between criminal stress and avoidant coping predicted baseline HR (β =−.07, p=.047). In the model predicting stress reactivity, the main effect of ELS on lower HR stress reactivity replicated for death, interpersonal, and criminal stressors. The interaction between ELS and emotional coping replicated as follows: with illness stress for HR stress reactivity; with interpersonal and financial stress for SBP stress reactivity; with illness, interpersonal, and financial/job/other stress for DBP stress reactivity; and with death-related stress for emotional reactivity. In the last model predicting CV recovery, the interaction between ELS and emotion-oriented coping replicated for interpersonal and financial/job/other stressors for both SBP and DBP, and for illness-related stress for DBP. A new main effect of interpersonal stress emerged for predicting lower HR in recovery (β =−.08, p=.009), and a new interaction emerged between criminal stress and task-oriented coping predicting DBP during recovery (β =.08, p=.007). In sum, across the seven ELS by emotion-oriented coping interaction effects significant in the main analyses, five replicated for interpersonal stress, four replicated for each illness-related and financial/job/other stress, one replicated for death-related stress, and none replicated for criminal stress.
Discussion
This was the one of the first studies to examine coping as a moderator of associations between ELS, baseline CV functioning, and reactivity to acute stress, including recovery from stress. The results replicated previous findings of ELS being associated with blunted HR stress reactivity in healthy adolescents and young adults(12–16), as well as links between coping and stress reactivity(29, 30). However, the present results also showed that the relationships between ELS, resting HR, and stress reactivity and recovery varied across levels of emotion-oriented coping typically employed to deal with stress. Specifically, ELS was only related to greater emotional reactivity, blunted HR, SBP, and DBP reactivity to stress, and lower SBP and DBP during recovery among individuals who frequently utilized emotion-oriented coping to deal with stress. These results suggest that emotion-oriented coping amplifies the adverse effects of ELS on heightened emotional reactivity and inadequate cardiovascular mobilization in response to acute stress. By contrast, among young people who did not frequently utilize emotion-oriented coping, ELS was associated with average HR and SBP response to acute stress, lower emotional reactivity to stress, and lower resting HR, but also higher DBP during stress and higher SBP and DBP during recovery. These results suggest that the ability to refrain from emotion-oriented coping may support cardiovascular and emotional resilience during acute stress in individuals who experienced ELS. However, low levels of emotion-oriented coping also confer risk for individuals with high levels of ELS exposure, who evidenced higher DBP reactivity to acute stress and higher BP during recovery compared to those with lower ELS. Sensitivity analyses showed that the main findings did not vary by sex; that emotion-oriented coping amplified the ELS effect on reduced BP mobilization also during the preparation period; that the cardiovascular stress reactivity results were mainly driven by the first speech task instead of the second math task; and that the results replicated most consistently across interpersonal, illness-related, and financial/job types of ELS.
Partially consistent with prior studies of adolescents and young adults(8, 9), ELS was correlated with elevated resting SBP in this study, although this relationship was of small magnitude and was no longer significant after adjusting for demographics, BMI and coping in the multivariate model. Although rarely conducted, longitudinal studies found that the effects of ELS on BP become more pronounced with increasing age in young adulthood (in 20’s and 30’s)(9, 46), suggesting that the present cohort may have been too young to detect meaningful associations between ELS and resting BP. Although the mechanisms linking ELS with elevated CVD risk have not been fully elucidated, studies with adolescents and young adults show that ELS is linked with vascular dysfunction, as well as oxidative stress and endothelin pathways, that may contribute to hypertension and cardiovascular risk as individuals age(47–49).
ELS was also correlated with blunted HR and SBP stress reactivity, lower HR during recovery, and higher emotional reactivity to acute stress. These associations were also of small magnitude. After adjusting for covariates, ELS only showed a unique association with lower HR stress reactivity, in line with a number of prior studies with adolescents and young adults(12, 13, 15, 16). Although a blunted CV response to stress has been traditionally viewed as protective for health, more recent research has linked it with the development of poor health outcomes, including obesity, self-reported poor health, and cognitive and emotional problems(3). Blunted HR response also preceded increased CVD risk, especially in Black individuals(5, 6). Thus, a blunted CV response to stress may reflect a dysregulated stress response system(7) arising from habituation to stress following chronic stress exposure during development.
Importantly, the relationships between ELS and reactivity to stress, as well as resting HR, varied across levels of emotion-oriented coping that individuals typically utilized to deal with stress. Specifically, ELS was associated with blunted reactivity to acute stress across HR, SBP, and DBP only when individuals utilized above average levels of emotion-oriented coping. At high levels of emotion-oriented coping (1.39 to 3.14 SD above the mean), ELS also became related to higher resting HR, greater emotional reactivity to stress, and lower SBP and DBP during recovery. Findings of this study extend previous results linking chronic stress with blunted HR stress reactivity only at high levels of emotion-oriented coping in Black young adults(29) to a broader range of cardiovascular outcomes (i.e., HR, SBP and DBP) in a racially diverse sample. The results are also consistent with a prior study finding that negative life events were associated with blunted SBP stress reactivity for individuals with low emotional stability(21). However, the results contrast with a report that linked recent stress with higher DBP stress reactivity at high levels of emotion-oriented coping in Black college students(32). Taken together, these findings suggest that under high levels of emotion-oriented coping, chronic or early life stress downregulate but recent stress upregulates BP responses to acute stress.
By contrast, individuals who experienced ELS but used low (below average) levels of emotion-oriented coping evidenced resilient patterns of functioning at rest and during acute stress, marked by lower resting HR, lower emotional reactivity to stress, and average HR and SBP stress reactivity. However, ELS was also associated with higher DBP during stress and higher SBP and DBP during recovery among these individuals, suggesting that low levels of emotion-oriented coping may be protective during acute stress but may not prevent delayed blood pressure increase after the acute stress abates. Collectively, the pattern of these moderating effects indicates that high levels of emotion-oriented coping potentiate ELS effects on emotional reactivity and blunted cardiovascular response, whereas low levels of emotion-oriented coping help ELS-exposed individuals cope with acute stress temporarily, with delayed blood pressure increase when acute stress terminates. In this context, average levels of emotion-oriented coping may be most adaptive for young people who experienced ELS, as they were accompanied by normative emotional and cardiovascular responses to stress and cardiovascular stress recovery. Various interventions help individuals develop more flexible ways of coping and employ optimal levels of emotion-oriented coping, including mindfulness-based(50, 51) and cognitive-behavioral stress management and emotion-regulation interventions(52, 53). In addition to traditional individual or group therapy sessions, these evidence-based intervention strategies are now easily accessible through many publicly available free or paid apps targeting stress management or mindfulness(54–56).
Importantly, the effects of ELS and coping on cardiovascular functioning did not vary by sex, despite evidence for sex differences in stress, coping, and physiological processes relating stress to cardiovascular risk(57–59). It is possible that sex differences in some of the studied relationships emerge later in life or are modified by other risk or protective factors that will need to be elucidated by future research (e.g., social support, psychological distress, risky health behaviors). Only one sex difference emerged in this study of avoidant coping being related to emotional stress reactivity in females but not males, in line with other research suggesting sex-specific associations between distinct coping styles and mental health(60).
Sensitivity analyses also indicated that the majority of interactive effects of ELS with coping on cardiovascular stress reactivity only replicated for the speech task and not the math task. This could be explained by greater stress reactivity experienced during the speech task, either because it was administered first or because it was inherently more stressful than the math task. Future studies that randomize the order of these two tasks will be able to disentangle these possibilities.
Finally, sensitivity analyses pointed to some types of stressors being more relevant to stress reactivity. Specifically, most robust effects were observed for interpersonal, illness-related, and financial/job/other types of stress. These results are consistent with a recent review summarizing decades of research on stressful life events and health, revealing that stressful events that threaten aspects of individuals’ core identity are most harmful to health; these events typically take the form of interpersonal problems, loss of social status, and employment difficulties(58). Indeed, many of the interpersonal events assessed in this study (feeling rejected, frequent conflicts, break ups, losing friends) may elicit sense of rejection, which is more strongly linked to poor health outcomes compared to other forms of interpersonal stress(58, 61). Likewise, experiencing serious illness in oneself, family members, and close friends and relatives confronts young people with mortality that may threaten their sense of self and alter their life trajectories(62). Finally, job/financial/other stressors in this study involved experiences of self or parent losing a job, financial stress, military employment and deployment, and natural disaster. These stressful experiences threaten individuals’ identities and financial security, and have been robustly associated with poorer health in prior work(58, 63). By contrast, this study found less robust effects for stressful events related to death (of close relatives and friends) and criminality (self or parent being in jail, crime victimization), which may occur relatively less frequently and may exert less chronic stress compared to interpersonal, financial, and illness-related stressors.
The interaction effects had small effect sizes (absolute values of standardized regression coefficients between .06 and .09), as would be expected for complex phenotypes and psychological research in general(64). Nevertheless, many of the associations between ELS and stress reactivity were of meaningful magnitude at high or low levels of emotion-oriented coping (e.g., at levels of emotion-oriented coping where ELS became significantly related to the outcomes based on regions of significance tests). For example, at high levels of emotion-oriented coping (0.86 to 2.10 SD above the mean), individuals with maximum ELS scores were estimated to have 10 points lower SBP and 5 to 11 points lower DBP during stress and recovery compared to those with minimum ELS scores, respectively. Similarly, at low levels of emotion-oriented coping (1.85 to 1.21 SD below the mean), individuals with maximum ELS scores were estimated to have 7 points higher DBP during stress, as well as 13 points higher SBP and 8 points higher DBP during recovery compared to those with minimum ELS scores. Given that the effects of ELS on cardiovascular risk only increase across the lifespan and may not become apparent until the late 20’s(9, 46), small effect sizes would be expected in late adolescence and emerging adulthood. However, these small effects may increase in magnitude with increasing age and progressing cardiovascular dysfunction(65).
Regardless of ELS levels, emotion-oriented coping was a unique predictor of greater emotional reactivity to stress, consistent with the emotionally reactive nature of this style of coping. By contrast, task-oriented coping was uniquely related to lower emotional reactivity to stress but also higher DBP during recovery, perhaps reflecting prolonged arousal from active coping. Finally, avoidant coping was a unique predictor of lower SBP and DBP during stress and lower SBP during recovery, likely reflecting disengagement from the stress tasks. These results extend previous findings linking task-oriented coping and lower avoidant and emotion-oriented coping with more adaptive stress responses(29, 30) and support the need for more research on the role of coping in CV reactivity to acute stress.
Together, these results suggest that reducing emotion-focused coping in young people exposed to ELS may mitigate the detrimental effects of ELS on blunted CV stress reactivity and subsequent poor health outcomes. However, very low levels of emotion-oriented coping may also be harmful by potentiating ELS effects on increased BP during and after stress. Thus, the best intervention goal may be the acquisition of various coping strategies and their flexible use in different stressful situations, while avoiding extreme use or non-use of emotion-oriented coping. Several types of psychological interventions effectively improve emotion regulation and reduce high levels of emotion-oriented coping. For example, 10 sessions of cognitive-behavioral therapy reduced emotion-oriented coping in adolescents and young adults with depression and substance use(66), and a three-week internet-administered mindfulness intervention produced large effects in reducing emotion-oriented coping and decreasing stress in college students(67). Research shows that internet-delivered psychological interventions are equally effective as traditional face to face therapy, but can be more accessible and practical(68, 69). Thus, young people who have experienced ELS may benefit from cognitive-behavioral or mindfulness-based therapies to adjust their coping styles that may be administered over the internet.
Limitations
In addition to the numerous strengths of this study, some limitations need to be acknowledged. First, ELS was assessed retrospectively and thus may be subject to recall bias. However, we expect this would have biased our findings toward the null hypothesis due to underreporting of ELS exposure. Second, the measure of ELS did not include some types of stressors, such as racial discrimination, that may be especially salient for Black and other racial/ethnic minority individuals. It also did not assess perceived severity of the stressful events. Third, coping was assessed through a self-report of generally used coping strategies, which may also contain some elements of bias. Although emotion-oriented and task-oriented coping match well with coping strategies used to deal with specific recent stressors(70), the coping strategies used during the acute stress manipulation were not measured. Next, some differential attrition occurred in the larger longitudinal study, with the current sample including more individuals who were Black and from lower-income households. Thus, the results may be less generalizable to people who are from more affluent backgrounds, non-Black, or from other geographic or cultural settings than those used in this study. Finally, perceptions of threat were not directly assessed during the TSST and this study did not measure vascular dysfunction or physiological pathways that may link ELS with CVD risk.
Conclusions
In conclusion, this study identified emotion-oriented coping as a potentially malleable moderator that was associated with blunted CV reactivity to acute stress among young people who previously experienced ELS. By contrast, low levels of emotion-oriented coping were associated with resilient profiles among those exposed to ELS, including lower resting HR, reduced emotional reactivity to acute stress, and average CV reactivity and recovery in response to acute stress. Although not directly addressed by this study, these results suggest that psychosocial interventions that reduce emotion-oriented coping (e.g., cognitive-behavioral or mindfulness-based therapies) may help normalize the CV stress response system in young people with a history of ELS, and in turn prevent long-term health problems in these individuals. Future studies would benefit from measuring a broader set of ELS, including racial discrimination and pandemic-related stress, throughout childhood and adolescence to represent the cumulative presence of ELS with more accuracy, assess coping used during the acute stress induction, and include measures of vascular dysfunction and related physiological pathways to better understand the links between ELS, coping, and CVD risk. Future research should also evaluate the impact of interventions aiming to reduce emotion-focused coping on acute stress reactivity in individuals exposed to ELS.
Conflicts of Interest and Source of Funding:
The authors declare no conflicts of interest. This research was supported by the National Institute of Mental Health of the National Institutes of Health, grant number R01MH098348.
Abbreviations:
- ELS
early life stress
- HR
heart rate
- BP
blood pressure
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- CV
cardiovascular
- CVD
cardiovascular disease
- SAM
sympathetic-adrenal medullary
- TSST
Trier Social Stress Test
References
- 1.Chrousos GP. Stress and disorders of the stress system. Nature reviews endocrinology. 2009;5(7):374–81. [DOI] [PubMed] [Google Scholar]
- 2.Phillips AC, Ginty AT, Hughes BM. The other side of the coin: Blunted cardiovascular and cortisol reactivity are associated with negative health outcomes. International Journal of Psychophysiology. 2013;90(1):1–7. [DOI] [PubMed] [Google Scholar]
- 3.Turner AI, Smyth N, Hall SJ, Torres SJ, Hussein M, Jayasinghe SU, et al. Psychological stress reactivity and future health and disease outcomes: A systematic review of prospective evidence. Psychoneuroendocrinology. 2020;114:104599. [DOI] [PubMed] [Google Scholar]
- 4.Whittaker AC, Ginty A, Hughes BM, Steptoe A, Lovallo WR. Cardiovascular Stress Reactivity and Health: Recent Questions and Future Directions. Psychosomatic medicine. 2021;83(7):756–66. [DOI] [PubMed] [Google Scholar]
- 5.Matthews KA, Zhu S, Tucker DC, Whooley MA. Blood pressure reactivity to psychological stress and coronary calcification in the Coronary Artery Risk Development in Young Adults Study. Hypertension. 2006;47(3):391–5. [DOI] [PubMed] [Google Scholar]
- 6.Heponiemi T, Ravaja N, Elovainio M, Keltikangas-Järvinen L. Relationships between hostility, affective ratings of pictures, and state affects during task-induced stress. The Journal of Psychology. 2007;141(2):183–201. [DOI] [PubMed] [Google Scholar]
- 7.Agorastos A, Pervanidou P, Chrousos GP, Baker DG. Developmental trajectories of early life stress and trauma: a narrative review on neurobiological aspects beyond stress system dysregulation. Frontiers in psychiatry. 2019;10:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gooding HC, Milliren CE, Austin SB, Sheridan MA, McLaughlin KA. Child abuse, resting blood pressure, and blood pressure reactivity to psychosocial stress. Journal of pediatric psychology. 2016;41(1):5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su S, Wang X, Pollock JS, Treiber FA, Xu X, Snieder H, et al. Adverse childhood experiences and blood pressure trajectories from childhood to young adulthood: the Georgia stress and Heart study. Circulation. 2015;131(19):1674–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy MO, Cohn DM, Loria AS. Developmental origins of cardiovascular disease: Impact of early life stress in humans and rodents. Neuroscience & Biobehavioral Reviews. 2017;74:453–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loria A, Ho D, Pollock J. A mechanistic look at the effects of adversity early in life on cardiovascular disease risk during adulthood. Acta physiologica. 2014;210(2):277–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lovallo WR, Farag NH, Sorocco KH, Cohoon AJ, Vincent AS. Lifetime adversity leads to blunted stress axis reactivity: studies from the Oklahoma Family Health Patterns Project. Biological psychiatry. 2012;71(4):344–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luecken LJ, Roubinov DS. Hostile behavior links negative childhood family relationships to heart rate reactivity and recovery in young adulthood. International journal of psychophysiology. 2012;84(2):172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leitzke BT, Hilt LM, Pollak SD. Maltreated youth display a blunted blood pressure response to an acute interpersonal stressor. Journal of Clinical Child & Adolescent Psychology. 2015;44(2):305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Lü W. Effect of childhood maltreatment on cardiovascular response habitation to repeated psychosocial stress. International journal of psychophysiology. 2021. [DOI] [PubMed] [Google Scholar]
- 16.Voellmin A, Winzeler K, Hug E, Wilhelm FH, Schaefer V, Gaab J, et al. Blunted endocrine and cardiovascular reactivity in young healthy women reporting a history of childhood adversity. Psychoneuroendocrinology. 2015;51:58–67. [DOI] [PubMed] [Google Scholar]
- 17.Low CA, Salomon K, Matthews KA. Chronic life stress, cardiovascular reactivity, and subclinical cardiovascular disease in adolescents. Psychosomatic medicine. 2009;71(9):927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winzeler K, Voellmin A, Hug E, Kirmse U, Helmig S, Princip M, et al. Adverse childhood experiences and autonomic regulation in response to acute stress: the role of the sympathetic and parasympathetic nervous systems. Anxiety, Stress, & Coping. 2017;30(2):145–54. [DOI] [PubMed] [Google Scholar]
- 19.Lei M-K, Berg MT, Simons RL, Simons LG, Beach SR. Childhood adversity and cardiovascular disease risk: An appraisal of recall methods with a focus on stress-buffering processes in childhood and adulthood. Social Science & Medicine. 2020;246:112794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carroll JE, Gruenewald TL, Taylor SE, Janicki-Deverts D, Matthews KA, Seeman TE. Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proceedings of the National Academy of Sciences. 2013;110(42):17149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallagher S, O’Riordan A, McMahon G, Creaven A-M. Evaluating personality as a moderator of the association between life events stress and cardiovascular reactivity to acute stress. International Journal of Psychophysiology. 2018;126:52–9. [DOI] [PubMed] [Google Scholar]
- 22.Phillips AC, Carroll D, Ring C, Sweeting H, West P. Life events and acute cardiovascular reactions to mental stress: a cohort study. Psychosomatic medicine. 2005;67(3):384–92. [DOI] [PubMed] [Google Scholar]
- 23.Goldman-Mellor S, Hamer M, Steptoe A. Early-life stress and recurrent psychological distress over the lifecourse predict divergent cortisol reactivity patterns in adulthood. Psychoneuroendocrinology. 2012;37(11):1755–68. [DOI] [PubMed] [Google Scholar]
- 24.Compas BE, Jaser SS, Dunbar JP, Watson KH, Bettis AH, Gruhn MA, et al. Coping and emotion regulation from childhood to early adulthood: Points of convergence and divergence. Australian journal of psychology. 2014;66(2):71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Compas BE, Vreeland A, Henry L. Coping models of stress and resilience. The Oxford Handbook of Stress and Mental Health; 2020. [Google Scholar]
- 26.Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. Journal of behavioral medicine. 2002;25(6):551–603. [DOI] [PubMed] [Google Scholar]
- 27.Graven LJ, Grant JS. Coping and health-related quality of life in individuals with heart failure: an integrative review. Heart & Lung. 2013;42(3):183–94. [DOI] [PubMed] [Google Scholar]
- 28.Chiavarino C, Rabellino D, Ardito RB, Cavallero E, Palumbo L, Bergerone S, et al. Emotional coping is a better predictor of cardiac prognosis than depression and anxiety. Journal of Psychosomatic Research. 2012;73(6):473–5. [DOI] [PubMed] [Google Scholar]
- 29.Cavanagh L, Obasi EM. The moderating role of coping style on chronic stress exposure and cardiovascular reactivity among African American emerging adults. Prevention Science. 2021;22(3):357–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Villada C, Hidalgo V, Almela M, Salvador A. Individual differences in the psychobiological response to psychosocial stress (Trier Social Stress Test): the relevance of trait anxiety and coping styles. Stress and Health. 2016;32(2):90–9. [DOI] [PubMed] [Google Scholar]
- 31.Sheffler JL, Piazza JR, Quinn JM, Sachs-Ericsson NJ, Stanley IH. Adverse childhood experiences and coping strategies: Identifying pathways to resiliency in adulthood. Anxiety, Stress, & Coping. 2019;32(5):594–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clark R Subjective stress and coping resources interact to predict blood pressure reactivity in black college students. Journal of Black Psychology. 2003;29(4):445–62. [Google Scholar]
- 33.Adams J, Mrug S, Knight DC. Characteristics of child physical and sexual abuse as predictors of psychopathology. Child abuse & neglect. 2018;86:167–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Windle M, Grunbaum JA, Elliott M, Tortolero SR, Berry S, Gilliland J, et al. Healthy passages: A multilevel, multimethod longitudinal study of adolescent health. American Journal of Preventive Medicine. 2004;27(2):164–72. [DOI] [PubMed] [Google Scholar]
- 35.Kirschbaum C, Pirke K-M, Hellhammer DH. The ‘Trier Social Stress Test’–a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1–2):76–81. [DOI] [PubMed] [Google Scholar]
- 36.Helminen EC, Morton ML, Wang Q, Felver JC. Stress Reactivity to the Trier Social Stress Test in Traditional and Virtual Environments: A Meta-Analytic Comparison. Psychosomatic Medicine. 2021;83(3):200–11. [DOI] [PubMed] [Google Scholar]
- 37.Seddon JA, Rodriguez VJ, Provencher Y, Raftery-Helmer J, Hersh J, Labelle PR, et al. Meta-analysis of the effectiveness of the Trier Social Stress Test in eliciting physiological stress responses in children and adolescents. Psychoneuroendocrinology. 2020;116:104582. [DOI] [PubMed] [Google Scholar]
- 38.Belani KG, Buckley JJ, Poliac MO. Accuracy of radial artery blood pressure determination with the Vasotrac™. Canadian Journal of Anesthesia. 1999;46(5):488–96. [DOI] [PubMed] [Google Scholar]
- 39.Yeaworth RC, McNamee MJ, Pozehl B. The adolescent life change event scale: Its development and use. Adolescence. 1992;27(108):783. [PubMed] [Google Scholar]
- 40.McKee SA, Maciejewski PK, Falba T, Mazure CM. Sex differences in the effects of stressful life events on changes in smoking status. Addiction. 2003;98(6):847–55. [DOI] [PubMed] [Google Scholar]
- 41.Poulin MJ, Silver RC. When are assumptions shaken? A prospective, longitudinal investigation of negative life events and worldviews in a national sample. Journal of research in personality. 2019;83:103866. [Google Scholar]
- 42.Endler NS, Parker JD. Assessment of multidimensional coping: Task, emotion, and avoidance strategies. Psychological assessment. 1994;6(1):50. [Google Scholar]
- 43.McGrath JJ, Matthews KA, Brady SS. Individual versus neighborhood socioeconomic status and race as predictors of adolescent ambulatory blood pressure and heart rate. Soc Sci Med. 2006;63(6):1442–53. [DOI] [PubMed] [Google Scholar]
- 44.Bloomfield GS, Hogan JW, Keter A, Sang E, Carter EJ, Velazquez EJ, et al. Hypertension and obesity as cardiovascular risk factors among HIV seropositive patients in Western Kenya. PLoS One. 2011;6(7):e22288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour research and therapy. 2017;98:39–57. [DOI] [PubMed] [Google Scholar]
- 46.Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to blood pressure in the CARDIA study. Health Psychology. 2009;28(3):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jenkins ND, Rogers EM, Banks NF, Tomko PM, Sciarrillo CM, Emerson SR, et al. Childhood psychosocial stress is linked with impaired vascular endothelial function, lower SIRT1, and oxidative stress in young adulthood. American Journal of Physiology-Heart and Circulatory Physiology. 2021;321(3):H532–H41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Su S, Wang X, Kapuku GK, Treiber FA, Pollock DM, Harshfield GA, et al. Adverse childhood experiences are associated with detrimental hemodynamics and elevated circulating endothelin-1 in adolescents and young adults. Hypertension. 2014;64(1):201–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rafiq T, O’Leary DD, Dempster KS, Cairney J, Wade TJ. Adverse Childhood Experiences (ACEs) predict increased arterial stiffness from childhood to early adulthood: pilot analysis of the niagara longitudinal heart study. Journal of child & adolescent trauma. 2020;13(4):505–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jones DR, Lehman BJ, Noriega A, Dinnel DL. The effects of a short-term mindfulness meditation intervention on coping flexibility. Anxiety, Stress, & Coping. 2019;32(4):347–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nejati S, Zahiroddin A, Afrookhteh G, Rahmani S, Hoveida S. Effect of group mindfulness-based stress-reduction program and conscious yoga on lifestyle, coping strategies, and systolic and diastolic blood pressures in patients with hypertension. The Journal of Tehran University Heart Center. 2015;10(3):140. [PMC free article] [PubMed] [Google Scholar]
- 52.Kaluza G Changing unbalanced coping profiles-A prospective controlled intervention trial in worksite health promotion. Psychology and Health. 2000;15(3):423–33. [Google Scholar]
- 53.Ebert DD, Heber E, Berking M, Riper H, Cuijpers P, Funk B, et al. Self-guided internet-based and mobile-based stress management for employees: results of a randomised controlled trial. Occupational and environmental medicine. 2016;73(5):315–23. [DOI] [PubMed] [Google Scholar]
- 54.Christmann CA, Hoffmann A, Bleser G. Stress management apps with regard to emotion-focused coping and behavior change techniques: a content analysis. JMIR mHealth and uHealth. 2017;5(2):e6471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coulon SM, Monroe CM, West DS. A systematic, multi-domain review of mobile smartphone apps for evidence-based stress management. American journal of preventive medicine. 2016;51(1):95–105. [DOI] [PubMed] [Google Scholar]
- 56.Lau N, O’Daffer A, Colt S, Joyce P, Palermo TM, McCauley E, et al. Android and iPhone mobile apps for psychosocial wellness and stress management: systematic search in app stores and literature review. JMIR mHealth and uHealth. 2020;8(5):e17798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Murphy MO, Loria AS. Sex-specific effects of stress on metabolic and cardiovascular disease: are women at higher risk? American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 2017;313(1):R1–R9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cohen S, Murphy ML, Prather AA. Ten surprising facts about stressful life events and disease risk. Annual review of psychology. 2019;70:577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Soares ALG, Hammerton G, Howe LD, Rich-Edwards J, Halligan S, Fraser A. Sex differences in the association between childhood maltreatment and cardiovascular disease in the UK Biobank. Heart. 2020;106(17):1310–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Howerton A, Van Gundy K. Sex differences in coping styles and implications for depressed mood. International Journal of Stress Management. 2009;16(4):333. [Google Scholar]
- 61.Murphy ML, Slavich GM, Chen E, Miller GE. Targeted rejection predicts decreased anti-inflammatory gene expression and increased symptom severity in youth with asthma. Psychological Science. 2015;26(2):111–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Störmer C, Lummaa V. Increased mortality exposure within the family rather than individual mortality experiences triggers faster life-history strategies in historic human populations. PloS one. 2014;9(1):e83633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gallo WT, Bradley EH, Falba TA, Dubin JA, Cramer LD, Bogardus ST Jr, et al. Involuntary job loss as a risk factor for subsequent myocardial infarction and stroke: findings from the Health and Retirement Survey. American journal of industrial medicine. 2004;45(5):408–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bodner TE. Standardized effect sizes for moderated conditional fixed effects with continuous moderator variables. Frontiers in psychology. 2017;8:562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tang Z, Yu Y, Ng K, Sow D, Hu J, Mei J. Disease network delineates the disease progression profile of cardiovascular diseases. Journal of Biomedical Informatics. 2021;115:103686. [DOI] [PubMed] [Google Scholar]
- 66.Hides L, Carroll S, Catania L, Cotton SM, Baker A, Scaffidi A, et al. Outcomes of an integrated cognitive behaviour therapy (CBT) treatment program for co-occurring depression and substance misuse in young people. Journal of affective disorders. 2010;121(1–2):169–74. [DOI] [PubMed] [Google Scholar]
- 67.Messer D, Horan JJ, Turner W, Weber W. The effects of internet-delivered mindfulness training on stress, coping, and mindfulness in university students. AERA Open. 2015;2(1):2332858415625188. [Google Scholar]
- 68.Andrews G, Basu A, Cuijpers P, Craske M, McEvoy P, English C, et al. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. Journal of anxiety disorders. 2018;55:70–8. [DOI] [PubMed] [Google Scholar]
- 69.Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cognitive behaviour therapy. 2018;47(1):1–18. [DOI] [PubMed] [Google Scholar]
- 70.Shikai N, Nagata T, Kitamura T. Do people cope with situations as they say? Relationship between perceived coping style and actual coping response. Psychiatry and Clinical Neurosciences. 2014;68(2):154–9. [DOI] [PubMed] [Google Scholar]


