Abstract
Heart failure (HF) is a significant clinical problem and an important public health issue due to the morbidity and mortality that it causes, especially in a population that is aging and affected by social stressors such as armed conflict. We aim to describe the inequalities and trends of HF mortality by educational level in Colombia between 1999 and 2017 compared with the cycles of the internal armed conflict during the same period. An observational study of ecological data panels, with aggregates at the national level, was conducted. Information from death certificates with HF as the basic cause of death (COD) was used. Variables of the year of death, sex, age, department of residence, and educational level were considered. Mortality rates adjusted for age were calculated. A joinpoint regression was used to model the trend of rates by educational level. We found that both men and women with primary education had the highest adjusted mortality rates: among men, RR_primary = 19.06 deaths/100,000 inhabitants, SE = 0.13 vs. RR_tertiary = 4.85, SE = 0.17, and similar differences among women. Mortality rates tended to decrease at all educational levels, with a greater reduction in people with higher educational levels. In both sexes, the behavior of the relative index of inequality showed significant inequality, albeit with a strong reduction during the last decade. Mortality due to HF in Colombia shows inequalities by educational level. In the prevention of HF, education should be considered a structural social determinant. In addition, we analyzed the potential role of the Colombian long-term armed conflict in the observed trends. We highlighted the role of the health sector, together with other sectors (education, work, and housing), in developing intersectoral public policies that contribute to the reduction of cardiovascular mortality disparities.
Keywords: Socioeconomic status, Health status disparities, Heart failure, Mortality, Colombia
1. Introduction
Globally, heart failure (HF) is a significant clinical problem and a major public health issue due to the morbidity and mortality that it causes, especially in an aging population [1]. In 1997, HF was identified as an emerging epidemic [2], whose prevalence has been estimated at 1–2% in the Western world, and whose incidence has been approximated at between 5 and 10 per 1000 people per year [3]. Globally, it has been observed that the prevalence of HF has been gradually increasing in the last 28 years worldwide and is unlikely to reverse in the next ten years [4]. This problem is reflected in the fact that HF has been included in the monitoring indicators of global and national policies such as the Sustainable Development Goals (SDGs) [5].
Heart failure is a clinical syndrome frequently associated with a structural or functional cardiac anomaly [6]. Worldwide, HF is more prevalent in women and the elderly [4]. The most frequent causes of HF are hypertension (HT), coronary artery disease (CAD), acute myocardial infarction (AMI), valvular disease, and atrial fibrillation. The risk factors include obesity, high blood pressure, and smoking. An incremental incidence has been observed mainly among individuals with a clinical history of diabetes mellitus (DM) [7].
Although there is a definition of HF, this syndrome is susceptible to misclassifications [8] in both the morbidity and mortality statistics. Mortality statistics are constructed from diseases or events that have been selected as the basic cause of death (COD). HF has been considered an intermediate COD (despite being a clearly defined clinical entity) because it has a basic cause that triggers the chain of events that lead to death. In general, physicians who have not had adequate training in the elaboration of the basic COD frequently use HF in death certificates [9].
Despite the efforts being made worldwide, there is still no early recognition of HF or timely and adequate treatment, leading to a high burden of disease. Moreover, the limitations in the characterization and treatment are even greater in low- and middle-income countries (LMIC) because the distribution of the syndrome in the population is unequal [10]. In addressing inequalities in health, educational level is relevant to the relationship of socioeconomic status with health and mortality. Evidence has indicated that educational level has a direct effect on the ability to generate income, have an occupation, have access to adequate nutrition, have housing, and have access to health services: elements that combined can promote a healthy life [11,12,13]. In addition, educational level can increase the ability to use information to make decisions that can improve the quality of life [14]. Different studies on morbidity and mortality have demonstrated a temporal trend where a low level of education presages HF [15,16,17,18,19,20,21].
On the other hand, an association between exposure to violence and the presence of cardiovascular diseases (CVD) has been found [22]. Some studies have shown that warfare and internal armed conflicts contribute to an increase in cardio-metabolic diseases by limiting access to healthcare services [23,24], and because the stress generated by violent events increases the allostatic load [25,26,27,28]. Specifically, armed conflict may lead to psychological trauma [28,29], physiological damage [30], and physical injuries directly caused by armed events (e.g., landmines) or by indirect mechanisms (an increase in the allostatic load due to the additive or combined effects of stress hormones (e.g., cortisol) on cardio-metabolic function) [23,24,31]. Studies in short and high-intensity war contexts have shown increases in different acute events of CVDs like ischemic heart diseases (IHD) and AMI [32,33,34], which can remain as chronic CVD conditions decades later [35,36,37], although none of these studies addressed how a low-intensity and long-term confrontation affects exposed populations.
In this sense, the Colombian case should be highlighted: for six decades, the country experienced a complex internal armed conflict with the participation of different actors, in which cycles of violence with different causes, intensities, and contexts occurred over time, as well as a de-escalation during this century [38,39,40,41].
The Colombian conflict has also been reported as causing the highest amount of internal displacement worldwide [42,43], as well as a large number of years of life potentially lost due to homicides [44,45]. The country is one of the most unequal territories in the region, and such inequality has been exacerbated by the internal armed conflict [38].
A previous inequalities spatial-focused study by the National Institute of Health found the relationship between the intensity of the armed conflict and cardiovascular mortality to be influenced by age, sex, and geographic setting [46].
Different from the abovementioned approaches, in this study, we aim to evaluate the role of socioeconomic inequalities in an acute CVD event, like those previously identified as increasing in high-intensity armed conflicts, evolving through time in a country with a long-term armed conflict. We use inequalities in mortality by HF as an explanatory variable in this study because HF [47] and its major causes, CAD [24,34,46,47], AMI [32,33], as well as major risk factors (DM, HT) [24,35,36,37], have previously been shown to more accurately reflect the potential effect of the armed conflict.
Knowledge of social health inequalities allows us to advance in recognizing the determinants of the health status of the Colombian population to evaluate the above-mentioned statements. Socioeconomic inequalities in HF mortality, considering the educational level and its temporal variations, have not yet been explored in the country. In summary, the objective of this study is to describe the inequalities and trends of HF mortality by educational level in Colombia between 1999 and 2017 and to compare how they have evolved alongside the cycles of the internal armed conflict.
2. Methods
An observational panel study of ecological data, aggregated at the national level, was designed to explore the inequalities of HF mortality by educational level.
The study used the same approach as previous studies [48,49].
2.1. Variables
To address this study, we obtained death and population counts by year, sex, five-year age group, and educational level as the explanatory variables. Educational groups were defined according to International Standard Classification of Education (ISCED) levels [50], as follows: (i) Primary: less than primary, primary, and lower secondary education (ISCED levels 0–2); (ii) Secondary: at least upper secondary education: upper secondary (e.g., high school) and post-secondary non-tertiary education (e.g., teacher training college) (ISCED levels 3 and 4); (ii) Tertiary, i.e., post-secondary level: technical, technological, and university education (ISCED 2011 levels 3–8, 1997 levels 3–6). We separately analyzed sex (men and women), as well as age groups: young: 25–44; middle-aged: 45–64; and senior: 65 and older. We chose the age of 25 as the lower limit for educational level, considering that almost all individuals will have accessed their highest educational level by this age [51].
2.2. Mortality data
Individual and anonymized registries of all deaths due to HF for the period 1999–2017 were obtained from death certificates and collected by the Colombian National Agency of Statistics (DANE by its acronym in Spanish) [52]. Deaths coded I50 by the International Classification of Diseases 10th revision (ICD-10) [53], counted by sex, year, and educational level, with an age at death of at least 25 years old, were used for this analysis.
The codification of the COD in Colombia to classify each death according to cause is addressed in two steps: Firstly, the medical certificate of death, based on the basic guidelines for the analysis of mortality from PAHO/WHO, allows the identification of the COD according to the rules of the ICD-10. The basic COD is the disease or injury that set off the chain of pathological events that resulted in the death of the deceased. If other antecedent diseases contributed to the death, the doctor registers them on the certificate. Afterward, the Colombian Administrative Statistical Agency (DANE, by its acronym in Spanish) collects and processes the information on the death certificates to obtain the final COD according to international guidelines.
Since 1998, the data on Colombian death certificates have included information on the educational level of the deceased, but we used the data from 1999 onwards because we found, when examining the distribution of the level of education for various causes of death, that the information for 1998 seems to be unreliable and inconsistent, due to the possible lack of full collection coverage for that year.
Data on five demographic variables (year, sex, five-year age group, department, and urban/rural residence) were available for almost 100% of all the deaths, while data on educational levels were missing for 26.5% of 56,293 deaths. The proportion of deaths with missing information on education remained relatively stable during the period (results not shown). We used multiple imputation methods [54] implemented in SAS through the IMPUTE procedure to impute the educational level for these cases. In short, this procedure fits a sequence of regression models and draws values from the corresponding predictive distributions. The sequential regression procedure was applied based on a model that imputed educational level, healthcare insurance scheme, and marital status based on the demographic variables mentioned above as covariates, excluding an insignificant share of cases with at least one missing. We obtained five databases, each including five iterations. The results were virtually equal for the five resulting databases. Details of this method are explained elsewhere [54].
2.3. Population (denominators)
Estimates of population size are available from the DANE, based on demographic projects derived from the 2005 census. However, these estimates do not contain information on numbers by educational level. Therefore, we directly obtained mid-year population counts by age, sex, and educational level from microdata of the Colombian Demography Health Surveys (DHS) (22) that are collected for each five-year period (1995, 2000, 2005, 2010, and 2015). To calculate the population size in each educational group, we obtained population counts for the educational levels by year, sex, and five-year age group, according to the factors of expansion provided in the metadata of each survey. Subsequently, we calculated proportions for the educational levels, year, sex, and five-year age groups and multiplied these by the total population provided by DANE by year, sex, and five-year age group [55]. Finally, we made demographic projections to obtain population counts for the years in between each lustrum of the surveys using the demographic population analysis spreadsheets (PASEX) provided by the US Census Bureau, which interpolate and curb the trends [56].
2.4. Analysis
We performed all the analyses with the five multiple databases generated by the multiple imputation procedure. We used standard techniques as implemented in the PROC MIANALYZE procedure in SAS to combine estimates from all databases and adjust standard errors to account for uncertainty in the imputation [57]. All analyses were conducted in SAS® version 9.2.
To adjust both rates and standard errors for age at death, we first used the world population according to SEGI as the standard population [58], resulting in age-standardized mortality rates (ASMR) expressed per 100,000 person-years.
Annual trends in ASMR by sex and educational level were quantified by calculating the estimated annual percentage change (EAPC), which measures the average rate of change in the mortality rate per year (negative EAPC: decreasing trend, positive EAPC: increasing trend). To test whether an apparent change in mortality trends was statistically significant, we used a joinpoint regression, which fits a series of joined straight lines to age-adjusted rates and uses a Monte Carlo permutation method to identify the best-fitting point (called a joinpoint, the year in which a significant change in the mortality trend occurred), where the rate of increase or decrease changes significantly [59]. EAPC and joinpoints were determined based on the log-transformed ASMRs and their standard errors.
Additionally, we implemented Poisson regression models with the number of deaths as the dependent variable and the natural log of person-years as the offset variable. We also incorporated age and educational level as independent variables. We estimated rate ratios (RR by educational level) by using these Poisson regression models, comparing the mortality of all educational groups with the mortality in the highest educational group. To assess changes in inequalities ‘controlling’ for changes in the educational distribution, we estimated the relative index of inequality (RII), regressing mortality on the mid-point of the cumulative distribution of education, thereby taking into account the size of each educational group [60,61]. Values higher than 1 indicate educational inequalities favoring the more highly educated. We also calculated how RII evolved during the studied period by calculating an interaction term with year.
Lastly, to describe the association between HF and the Colombian armed conflict, we compared the cycles of lethal violence, as described in previous literature, with the educational inequalities and trends of HF mortality in Colombia between 1999 and 2017, obtained by our statistical analyses.
3. Results
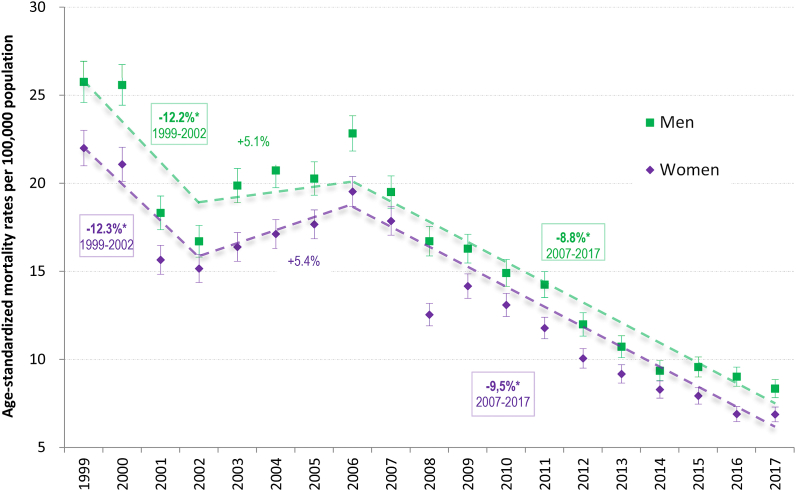
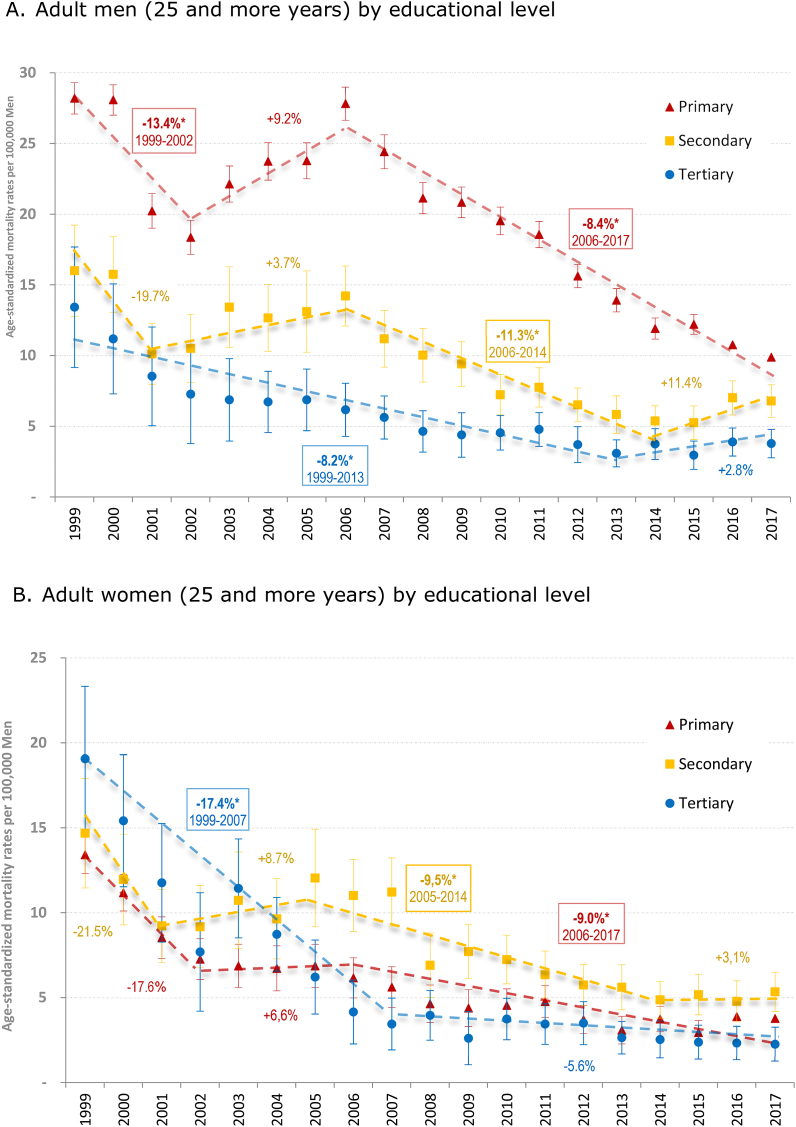
There were 56,293 adult (25 years of age and older) deaths due to HF in Colombia between 1999 and 2017, half of them women (50.1%). Of these deaths, 86.9% were among people who had attained primary education or lower, and 84.2% were among senior (65, and older) men and women (Table 1). Age-standardized mortality rates (per 100,000 person-years) were 15.6 for adult men (25+ years) and 13.1 for adult women (Table 2). Among both men and women, HF adult mortality decreased significantly from 1999 to 2002 (APC = −12% for both sexes), followed by a non-significant increase between 2002 and 2006, and a rapid decrease from 2006 to 2017 (APC = −8.8% and −9.3%, respectively, for adult men and women) (Fig. 1), for a total decrease along the period of 7% for both sexes. These oscillations are very similar (in both periods and percentages) for middle-aged and senior men and women (Fig. 2 panels B and C, respectively), -while oscillations for young adults (Fig. 2 panel A) are not as akin-, and also for all adults (25+ years old) with primary and secondary education, while tertiary-educated adult men and women had a more continuous decrease during the period (Fig. 3 panels A and B) of 6% (Table 2). Overall, all sex, age, and educational groups had a reduction in the ASMR during the period (non-significant for young women, who mostly had lower ASMR) (Table 1). Among seniors, the reduction in ASMR for the whole period was higher for those who were more highly educated (APC = −6.4% and −11.4%, respectively, for people) if compared with those with primary and secondary education, who had a lower reduction. This result is not as consistent among middle-aged and young men and women (Table 1).
Table 1.
Descriptives* by age groups and educational level of adult mortality for Hearth Failure (HF) in Colombia, 1998–2017.
| Age group | Educational levela | Deathsb | Population-year (thousands) | ASMRc with 95% CI | APCd of ASMRc |
Rate Ratios (RR)e with 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| APC | P | |||||||||
| Men | Adult Men (25 years and more) | Primary | 24,185 | 91,625 | 19.06 | (18.81–19.31) | −4.6 | 0.00 | 1.84 | (1-83-1.85) |
| Secondary | 2,904 | 75,242 | 9.00 | (8.59–9.41) | −5.5 | 0.00 | 1.65 | (1-63-1.67) | ||
| Tertiary | 983 | 44,565 | 4.85 | (4.52–5.18) | −6.5 | 0.00 | 1.00 | |||
| Young men (25–44 years) | Primary | 525 | 36,708 | 1.36 | (1.22–1.50) | −2.1 | 0.15 | 4.52 | (4-30-4.74) | |
| Secondary | 245 | 49,310 | 0.53 | (0.45–0.61) | −2.5 | 0.18 | 2.68 | (2-49-2.91) | ||
| Tertiary | 46 | 30,235 | 0.16 | (0.08–0.24) | −4.8 | 0.03 | 1.00 | |||
| Middle-age men (45–64 years) | Primary | 3,269 | 35,793 | 8.78 | (8.47–9.09) | −4.3 | 0.00 | 1.83 | (1-80-1.85) | |
| Secondary | 733 | 22,214 | 3.73 | (3.32–4.14) | −6.5 | 0.00 | 1.52 | (1-49-1.55) | ||
| Tertiary | 224 | 11,789 | 2.12 | (1.79–2.45) | −6.2 | 0.00 | 1.00 | |||
| Senior men (65 years and more) | Primary | 20,392 | 19,124 | 106.63 | (105.12–108.14) | −4.8 | 0.00 | 1.69 | (1-68-1.71) | |
| Secondary | 1,926 | 3,718 | 51.79 | (48.83–54.75) | −5.4 | 0.00 | 1.68 | (1-66-1.69) | ||
| Tertiary | 714 | 2,542 | 28.08 | (25.81–30.35) | −6.4 | 0.00 | 1.00 | |||
| Women | Adult Women (25 years and more) | Primary | 24,729 | 98,167 | 16.05 | (15.83–16.27) | −7.8 | 0.00 | 5.11 | (5-02-5.21) |
| Secondary | 2,990 | 83,948 | 7.15 | (6.88–7.42) | −3.8 | 0.01 | 2.40 | (2-37-2.47) | ||
| Tertiary | 502 | 50,872 | 2.96 | (2.63–3.29) | −7.5 | 0.00 | 1.00 | |||
| Young women (25–44 years) | Primary | 424 | 36,886 | 1.07 | (0.97–1.17) | −1.6 | 0.35 | 8.80 | (8-27-9.13) | |
| Secondary | 198 | 51,913 | 0.39 | (0.33–0.45) | −1.3 | 0.42 | 3.69 | (3-52-3.91) | ||
| Tertiary | 38 | 36,068 | 0.12 | (0.08–0.16) | −0.7 | 0.77 | 1.00 | |||
| Middle-age women (45–64 years) | Primary | 2,589 | 37,684 | 6.58 | (6.33–6.83) | −4.9 | 0.00 | 5.95 | (5-76-6.29) | |
| Secondary | 513 | 26,776 | 2.07 | (1.85–2.29) | −5.1 | 0.00 | 2.18 | (2-09-2.31) | ||
| Tertiary | 109 | 12,801 | 1.01 | (0.76–1.26) | −2.9 | 0.11 | 1.00 | |||
| Senior women (65 years and more) | Primary | 21,716 | 23,596 | 92.03 | (90.80–93.26) | −5.0 | 0.00 | 4.36 | (4-33-4.43) | |
| Secondary | 2,279 | 5,260 | 43.33 | (41.49–45.17) | −5.9 | 0.00 | 2.35 | (2-33-2.38) | ||
| Tertiary | 355 | 2,003 | 17.72 | (15.43–20.01) | −11.4 | 0.00 | 1.00 | |||
*Descriptives: a. Educational level after the imputation Primary=elementary or less. Secondary=up to any secondary level. Tertiary=post-secondary studies. b. Deaths due to Hearth Failure (HF) after imputation. c. Age-standardized mortality rates (ASMR) per 100 000 inhabitants and Standard error (SE), using SEGI Standard Population. All estimates for the educational level combine 5 databases generated by multiple imputations. d. Annual Percentage Change (APC) during the corresponding periods, depending on the Joinpoint model with no joinpoints for the whole period. e. Rate Ratios (RR) were calculated from Poisson regression models.
Table 2.
Descriptives* by age groups of adult mortality for Hearth Failure (HF) in Colombia, 1998–2017.
| Age groups | ASMRa with 95% CI | APCb of ASMRa |
Relative Index of Inequality (RII)c with 95% CI | ||||
|---|---|---|---|---|---|---|---|
| APC (%) | p | ||||||
| Adult Men | (25 years and more) | 15.58 | (15.40–15.76) | −6.60 | 0.00 | 1.90 | (1.89-1-91) |
| Young men | (25–44 years) | 0.71 | (0.67–0.75) | −4.80 | 0.00 | 5.93 | (5.80-6-28) |
| Middle-age men | (45–64 years) | 6.28 | (6.08–6.48) | −6.20 | 0.00 | 2.02 | (2.00-2-03) |
| Senior men | (65 years and more) | 90.73 | (89.55–91.91) | −5.60 | 0.00 | 1.61 | (1.60-1-64) |
| Adult Women | (25 years and more) | 13.11 | (12.95–13.27) | −6.70 | 0.00 | 10.04 | (9.89-10-14) |
| Young women | (25–44 years) | 0.53 | (0.49–0.57) | −4.70 | 0.00 | 14.41 | (13.70-15-33) |
| Middle-age women | (45–64 years) | 4.30 | (4.14–4.46) | −6.70 | 0.00 | 13.98 | (13.56-14-34) |
| Senior women | (65 years and more) | 78.91 | (77.91–79.91) | −5.70 | 0.00 | 8.57 | (8.43-8-70) |
*Descriptives: a. Age-standardized mortality rates (ASMR) per 100 000 inhabitants and Standard error (SE), using SEGI Standard Population. All estimates for the educational level combine 5 databases generated by multiple imputations. b. Annual Percentage Change (APC) during the corresponding periods, depending on the Joinpoint model with no joinpoints for the whole period. c. Relative Index of Inequality (RII) were calculated from Poisson regression models, encompassing the three educational levels: Primary = primary. Secondary = any secondary level. Tertiary = post-secondary studies.
Fig. 1.
Adult (25 years or more) Hearth Failure (HF) mortality separately by men and women, Colombia, 1998–2015. Hearth Failure (HF) adult (over 25 years of age) mortality rates were standardized using SEGI Standard Population. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05.
Fig. 2.
Adult (25 years or more) Hearth Failure (HF) mortality by age groups separately by men and women, Colombia, 1998–2015. A. Young adult (25–44 years) men and women. Hearth Failure (HF) mortality rates of young adult (25–44 years of age) men and women were standardized using SEGI Standard Population. The lower limit for educational level is 25 years of age considering that almost all individuals will have accessed their highest educational level by this age. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) by age group separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05. B. Middle-age adult (45–64 years) men and women. Hearth Failure (HF) mortality rates of middle-aged adults (45–64 years of age) men and women were standardized using SEGI Standard Population. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) by age group separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05. C. Senior adult (65 years and more) men and women. Hearth Failure (HF) mortality rates of senior adults (65 years old of age) men and women were standardized using SEGI Standard Population. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) by age group separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05.
Fig. 3.
Adult (25 years or more) Hearth Failure (HF) mortality by educational level separately by men and women, Colombia, 1998–2015. A. Adult men (25 and more years) by educational level. Adult (25 and more years) men by Educational levels: Primary=elementary or less. Secondary=up to any secondary level. Tertiary=post-secondary studies. Hearth Failure (HF) adult (over 25 years of age) mortality rates were standardized using SEGI Standard Population. The lower limit for educational level is 25 considering that almost all individuals will have accessed their highest educational level by this age. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) by educational group separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05. B. Adult women (25 and more years) by educational level. Adult (25 and more years) women by Educational levels: Primary=elementary or less. Secondary=up to any secondary level. Tertiary=post-secondary studies. Hearth Failure (HF) adult (over 25 years of age) mortality rates were standardized using SEGI Standard Population. The lower limit for educational level is 25 considering that almost all individuals will have accessed their highest educational level by this age. Markers: The points represent yearly adult age-standardized mortality rates (ASMR) by educational group separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05.
At all age groups, men and women with the lowest educational level had the highest ASMR (Table 1). In addition, ASMRs by age group were higher in men than in women for each educational level (Table 2), but the difference was much greater between higher-level and lower-level-educated adult men if compared with their women counterparts: RR for primary-educated men were 1.84 (95% CI: 1.83–1.85) and 1.65 (95% CI: 1.63–1.67) for those with a secondary education, both compared with those with higher education as a reference (Table 1). The same RR for adult women were much higher: RR/primary-women = 5.11 (95% CI: 5.02–5.21) and RR/secondary-women = 2.40 (95% CI: 2.37–2.47), compared with tertiary-educated adult women. Those differences are greater among younger people, and smaller among seniors (Table 1).
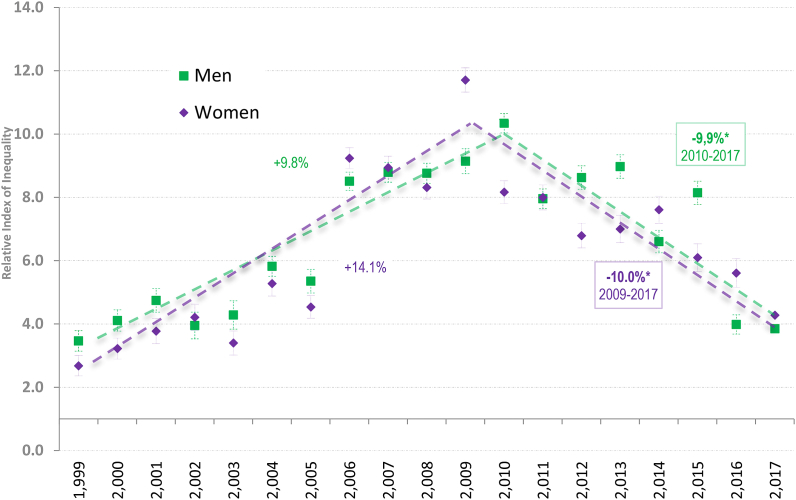
The RII was considerably higher in women (10.04, 95% CI: 9.89–10.14) than in men (1.90, 95% CI: 1.89–1.91), with greater inequalities in the 25–44-year-old groups for both sexes (Table 2). These results reinforce the previously mentioned findings on RRs obtained for these groups, although the SMRs were higher for men than for women (Table 1). RII trends show a significant increase between 1999 and 2009 for both sexes (APC = 9.83% and 14.06%, respectively, for adult men and women), followed by a significant decrease from 2009 to 2017 (APC = −9.96% and −9.98%, respectively, for adult men and women) (Fig. 4).
Fig. 4.
Trends in the Relative Index of Inequalities (RII) of Adult (25 years or more) Hearth Failure (HF) mortality by educational level separately by men and women, Colombia, 1998–2015. Relative Index of Inequality (RII) were calculated from Poisson regression models, encompassing the three Educational levels: Primary = elementary or less. Secondary = up to any secondary level. Tertiary = post-secondary studies. Markers: The points represent yearly Relative Index of Inequality (RII) separately by sex; the lines represent the trend lines between the joinpoints. The numbers adjacent to the lines represent the estimates of the annual percentage change (APC) during the corresponding periods, depending on the Joinpoint model; one star indicates statistical significance at α = 0.05.
4. Discussion
Colombia, like other countries in the Latin American region, is characterized by a high level of socioeconomic inequalities that affect the overall health situation. At the same time, and as a particular problem, the internal armed conflict has contributed to the increased burden of disease, economic instability, and restrictions on access to preventive medicine. Previous literature has reported that those with lower socioeconomic status are more exposed to armed conflict and its consequences [62,63,64]. According to the cycles of the internal armed conflict, there is an association with HF and, consequently, with its risk factors, which deserves to be properly analyzed. Considering this triad between armed conflict, socioeconomic inequities, and health status, this study shows the presence and persistency of inequalities by educational level in mortality for HF in men and women. Our study found the lowest mortality rate by HF among individuals with tertiary education; furthermore, inequalities were greater among the younger members of both sexes.
4.1. Analysis of results
All Colombian departments/provinces reported conflict events in their territories between 1985 and 2020, and at least 25 of the 32 reported more than 100,000 conflict events, totaling 10,608,112 [65].
A recent review study points out the critical association between armed conflict and the increase in cardiometabolic risk factors [66] that contribute to inequalities. This association has been interpreted as due to limited access to health attention [23] and restrictions in the implementation of public health action during active confrontations [66]. Furthermore, concordant with our present findings, a previous study shows a consistent reduction in mortality rates and inequities since 2010, coinciding with the finding of a steady decrease in homicide rates since 2002, with a brief peak in 2009 [38]. This allows us to suggest that lower exposure to armed conflict lowers the mortality by CVD [67], and fewer armed conflict confrontations diminish inequalities [38]. In summary, we interpreted our findings because of a combined phenomenon involving the consequences of armed conflict (such as the one observed in Colombia) and the introduction of a restriction of socioeconomic activities, which consequently limited preventive action to tackle HF [66].
Lower educational levels have been shown to be associated with a higher risk of HF events, such as increased diagnosis, hospitalizations, or deaths among chronic HF patients, in studies conducted worldwide [14,15,19,35,37], and in Colombia [39].
Additionally, some of these studies evaluated other socioeconomic variables such as occupation, sociocultural factors, and marital status, showing inequalities in HF mortality due to these variables. The aforementioned could be explained by what has been reported on the close relationship that exists between educational level and other social determinants of health, such as occupation and income level, and its impact on the health of individuals and populations [12].
However, there is still little knowledge about the relationship that may exist between the quality or content of education and mortality and how the educational level of individuals is associated with a variety of other economic and social characteristics throughout their lives, such as employment status, income, family training patterns, and access to medical care.
Although the ASMRs by HF were higher for men than for women, the educational inequalities in mortality by gender showed greater differences and higher values for RII in women. Some studies that considered gender as a sociodemographic variable of analysis for the risk of HF reported similar associations in men and women, higher risk in men than women [68], or variations between gender according to educational level [69].
Such differences between higher ASMR in men but greater RII in women are unexpected, but these could be explained by the premature death of men with HF due to other injuries of an external cause (including armed conflict), considering that in Colombia, 81% of violent deaths occur in men [70].
The results of this study also show that HF mortality rates decreased over the observed window for all educational and age groups, particularly since 2006, with the largest reduction being for those with a high educational level. A reduction in inequalities (RII) in men and women was observed since 2010. This result is consistent with the de-escalation of the internal armed conflict that reached its peak around 2002 and describes a continuous reduction since 2010 [71].
Concerning the oscillations of the internal armed conflict, a previous study handled the same joinpoint analyses used herein [38], using urban/rural homicide rates in Colombia (1992–2015) as a proxy for the intensity of the conflict. In that study, three critical inflection points that we use as a reference for this study were identified: 1997, 2002, and 2005/2006. In fact, these are essentially the same joinpoints in this study. Therefore, we can analyze these periods as follows.
-
(i)
For the whole period, those with a higher educational level (who predominantly reside in urban settings [72]) had a steady decrease in HF mortality—measured by the APC—over the whole period (1999–2017) (Table 2). Coinciding with this trend, the above-mentioned study (Vallejo et al., 2018) found a similar period (1999–2015) with a reduction or non-significant changes in urban homicide. Both urban homicide and HF among the higher educated reduced or did not have any meaningful change, apparently revealing that the benefits of the steady reduction of the internal armed conflict during 1999–2015/2017 privileged the most favored population, at least at the beginning of the analyzed period—that of the increasing violence.
-
(ii)
In the period 1997–2002, there was an increase in homicidal violence that was pronounced and statistically significant in rural but not urban settings, while the urban violence associated with drug cartels in the major cities largely reduced. It coincides with the escalation of the internal armed conflict. The reduction of HF during this period could have been driven by the de-escalation of the conflict in urban areas, in which around 70% of the Colombian population lives [72].
-
(iii)
From 2002 to 2005/2006, there was a pronounced reduction in homicides, in both rural and urban areas, among men and women, which can be attributed to a large extent to the increase in the operational capacity of the Security Forces [72]. This period coincides with stagnation in HF mortality, except for those more favored, in which the reduction of HF remained steady, as explained above. The national reduction in the intensity of the conflict, therefore, coincides with the stabilization of the mortality rate in HF among the less educated.
-
(iv)
Since 2005/2006, trends in homicide have continued to decrease in both rural and urban areas among men and women, with a minor stage of stagnation within the period around 2010 [38]. This coincides with a steady reduction in HF among all educational groups, much stronger among those with primary and secondary educational levels (Fig. 3 panels A and B), similar to the more pronounced reduction of homicidal violence among those in rural areas. In fact, the total reduction in the APC of the HF mortality for the whole period was higher for those with lower educational levels (Table 2).
Therefore, the de-escalation of the armed conflict seems to favor those most deprived, with noticeable reductions in HF mortality among the less educated (see iv), while the most privileged seem to have advantageous conditions, having lower homicide and HF mortality rates when the conflict escalates (see i).
4.2. Study limitations
This study was based on a large sample of information related to HF mortality registered in the country between 1999 and 2017. However, there were limitations, firstly due to the source of information, secondly, due to the imputation method, thirdly, due to the use of an educational level as a socioeconomic indicator; and fourthly, the non-consideration of other factors related to HF. Firstly, the use of a secondary source of information, as mentioned previously, could have contained a poor classification of HF when the COD was certified at the time of preparing the death certificate, which could cause a bias in the results presented. Establishing the underlying COD is difficult when the history of the disease is complex. Sometimes causes of death are ambiguously recorded. Added to this is the infrequency with which an autopsy is performed, whether the death occurs in a health service or not. This can lead to misclassification and, consequently, to the over-registration or under-registration of HF in people who were not diagnosed when they were alive and the subsequent impact on the results. However, the DANE classifies the basic COD in the mortality database, considering not simply a diagnosis but a combination of direct COD and up to three antecedent causes based on the codes that were recorded on the death certificate by the doctor. This limitation could explain the trend in the reduction of mortality rates evidenced in the results of the study.
The second limitation is that, given the lack of information on the level of education of the deceased, an imputation method was used to complete the missing data. Its use could cause, among other aspects, the appearance of biases, the underestimation of the variances, the overestimation of the correlations, or the underestimation of the confidence intervals [73].
In the case of the third limitation, the use of the educational level as a socioeconomic indicator, although it has advantages, also has disadvantages. One of the advantages is that the educational level, which is attained in the early phases of life, allows the classification of people who do not work. It is also an individual measure of socioeconomic position [74]. A disadvantage is that it has been indicated that, in general, individuals reach their highest level of education at the beginning of adult life, a situation that means that educational level does not allow a precise indication of current socioeconomic position [75]. On the other hand, although educational level has a close relationship with other sociodemographic variables, which justifies its use when evaluating people's living conditions, this can also represent a disadvantage given the possibility that these variables can be confusing.
Finally, as a fourth limitation, it should be considered that the association between HF and educational level may mediate other non-sociodemographic factors not considered in this study, such as HT, DM, and body mass index [76], among others.
5. Conclusions
The results of the study showed higher mortality rates due to HF in men than in women, with an increasing trend in 2002 and a significant decrease as of 2006, which is coincident with the cycles of violence that have been experienced in Colombia within its period of internal armed conflict. This could represent an opportunity.
Inequities according to educational level occurred in both sexes, suggesting that the lower the academic achievement, the higher the risk of death from HF. However, the differences were not only greater in women than in men but also differed among women according to their educational level. Despite the limitations mentioned in the study regarding the use of educational level as a variable, these results support the importance of incorporating the perspective of social determinants of health in the prevention of and approach to public health problems such as HF.
Considering that mortality from HF has been associated with high-intensity conflicts, the decrease in the internal armed conflict in Colombia can play an important role in reducing rates and inequities in mortality from HF, not only because of the reduction in stressors but also because those with lower socioeconomic status are more exposed to the violence that results from the conflict.
In the prevention of HF, the planning and evaluation of health actions should be considered to help reduce the inequities observed in research. In Colombia, the Ten-Year Public Health Plan, 2012–2021, incorporated the approach of social determinants of health, so it would be expected that through the different proposed strategies of promotion and education for health, it will be possible to reduce social inequities in health and, therefore, have a positive impact on reducing mortality from HF.
It is relevant to focus these strategies on the most disadvantaged sectors, usually those with the lowest educational level. For example, increased coverage and access to secondary and tertiary education in rural areas could improve the trends shown in the study, especially since these regions were the most affected by the internal armed conflict.
Health education also appears to have a promising place in promoting healthy lifestyles. Likewise, the health sector, together with other sectors (education, work, housing), may develop intersectoral policies that contribute to reducing disparities in cardiovascular mortality together with public health interventions aimed at controlling chronic diseases.
As they are included within the SDGs at the global and local level, these actions to promote health and prevent CVDs should be considered more seriously in the psychosocial rehabilitation strategies for victims of the internal armed conflict incorporated in the Final Agreement for the Termination of the Conflict and the Construction of a Stable and Lasting Peace [77], signed between the government of Colombia and the Revolutionary Armed Forces of Colombia–FARC.
Author contribution statement
Pablo Chaparro-Narváez: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Ivonne Andrea Ordóñez-Monak: Analyzed and interpreted the data; Wrote the paper.
Natalia Trujillo: Conceived and designed the experiments; Wrote the paper.
Carlos Andres Castañeda-Orjuela: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Ivan Arroyave: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
Natalia Trujillo and Ivan Arroyave was supported by Minciencias [832/2019].
Data availability statement
Data associated with this study has been deposited at Departamento Administrativo Nacional de Estadística–DANE, Colombia Estadísticas Vitales–Microdatos
http://microdatos.dane.gov.co/index.php/catalog/MICRODATOS/about_collection/22/5
Declaration of interest's statement
The authors declare no competing interests.
References
- 1.Roger V.L. Epidemiology of heart failure. Circ. Res. 2013;113(6):646–659. doi: 10.1161/CIRCRESAHA.113.300268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braunwald E. Cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N. Engl. J. Med. 1997;337(19):1360–1369. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 3.Mosterd A., Hoes A.W. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lippi G., Sanchis-Gomar F. 2020. Global Epidemiology and Future Trends of Heart Failure. [Google Scholar]
- 5.United Nations . 2015. Transforming Our World: the 2030 Agenda for Sustainable Development. [Google Scholar]
- 6.Ponikowski P., et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 7.Lee D.S., et al. Relation of disease etiology and risk factors to heart failure with preserved or reduced ejection fraction: insights from the national heart, lung, and blood institute's Framingham heart study. Circulation. 2009;119(24):3070. doi: 10.1161/CIRCULATIONAHA.108.815944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ziaeian B., Fonarow G.C. Epidemiology and aetiology of heart failure. Nat. Rev. Cardiol. 2016;13(6):368–378. doi: 10.1038/nrcardio.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naghavi M., et al. Algorithms for enhancing public health utility of national causes-of-death data. Popul. Health Metrics. 2010;8(1):9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Legetic B., et al. Economic dimensions of non-communicable disease in Latin America and the caribbean. Disease control priorities. Companion. 2016;ume [Google Scholar]
- 11.Winkleby M.A., Fortmann S.P., Barrett D.C. Social class disparities in risk factors for disease: eight-year prevalence patterns by level of education. Prev. Med. 1990;19(1):1–12. doi: 10.1016/0091-7435(90)90001-z. [DOI] [PubMed] [Google Scholar]
- 12.Ross C.E., Wu C.-l. The links between education and health. Am. Socio. Rev. 1995:719–745. [Google Scholar]
- 13.Zimmerman E.B., Woolf S.H., Haley A. Population Health: Behavioral and Social Science Insights. Agency for Health-care Research and Quality; Rockville (MD): 2015. Understanding the relationship between education and health: a review of the evidence and an examination of community perspectives; pp. 347–384. [Google Scholar]
- 14.Christenson B.A., Johnson N.E. Educational inequality in adult mortality: an assessment with death certificate data from Michigan. Demography. 1995;32(2):215–229. [PubMed] [Google Scholar]
- 15.Christensen S., et al. Level of education and risk of heart failure: a prospective cohort study with echocardiography evaluation. Eur. Heart J. 2011;32(4):450–458. doi: 10.1093/eurheartj/ehq435. [DOI] [PubMed] [Google Scholar]
- 16.Ingelsson E., et al. Socioeconomic factors as predictors of incident heart failure. J. Card. Fail. 2006;12(7):540–545. doi: 10.1016/j.cardfail.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Soares G.P., et al. Evolution of socioeconomic indicators and cardiovascular mortality in three Brazilian states. Arq. Bras. Cardiol. 2013;100(2):147–156. doi: 10.5935/abc.20130028. [DOI] [PubMed] [Google Scholar]
- 18.Sui X., et al. A propensity matched study of the association of education and outcomes in chronic heart failure. Int. J. Cardiol. 2008;129(1):93–99. doi: 10.1016/j.ijcard.2007.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkins N.M., et al. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur. J. Heart Fail. 2012;14(2):138–146. doi: 10.1093/eurjhf/hfr168. [DOI] [PubMed] [Google Scholar]
- 20.Rathore S.S., et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am. Heart J. 2006;152(2):371–378. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Close G.R., et al. Socioeconomic status and heart failure in Sydney. Heart, Lung and Circulation. 2014;23(4):320–324. doi: 10.1016/j.hlc.2013.10.056. [DOI] [PubMed] [Google Scholar]
- 22.Konstam M.A., Konstam A.D. Gun violence and cardiovascular health: we need to know. Circulation. 2019;139(22):2499–2501. doi: 10.1161/CIRCULATIONAHA.118.039504. [DOI] [PubMed] [Google Scholar]
- 23.Krug E.G., et al. SciELO Brasil; 2003. Informe mundial sobre la violencia y la salud. [Google Scholar]
- 24.Stewart I.J., et al. Retrospective analysis of long-term outcomes after combat injury: a hidden cost of war. Circulation. 2015;132(22):2126–2133. doi: 10.1161/CIRCULATIONAHA.115.016950. [DOI] [PubMed] [Google Scholar]
- 25.Evans G.W., Schamberg M.A. Proceedings of the National Academy of Sciences. Vol. 106. 2009. Childhood poverty, chronic stress, and adult working memory; pp. 6545–6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans G.W., Kim P. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status–health gradient. Ann. N. Y. Acad. Sci. 2010;1186(1):174–189. doi: 10.1111/j.1749-6632.2009.05336.x. [DOI] [PubMed] [Google Scholar]
- 27.Juster R.-P., McEwen B.S., Lupien S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 28.Pat-Horenczyk R., et al. Relational trauma in times of political violence: continuous versus past traumatic stress. Peace Conflict: Journal of Peace Psychology. 2013;19(2):125. [Google Scholar]
- 29.Kuehn B.M. Am Heart Assoc; 2019. Growing Evidence Linking Violence, Trauma to Heart Disease. [DOI] [PubMed] [Google Scholar]
- 30.Thompson K.B., Krispinsky L.T., Stark R.J. Late immune consequences of combat trauma: a review of trauma-related immune dysfunction and potential therapies. Military Medical Research. 2019;6(1):1–13. doi: 10.1186/s40779-019-0202-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murali R., Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Ann. Behav. Med. 2005;30(2):155–163. doi: 10.1207/s15324796abm3002_8. [DOI] [PubMed] [Google Scholar]
- 32.Mirić D., et al. Trends in myocardial infarction in Middle Dalmatia during the war in Croatia. Mil. Med. 2001;166(5):419–421. [PubMed] [Google Scholar]
- 33.Zubaid M., et al. Could missile attacks trigger acute myocardial infarction? Acta Cardiol. 2006;61(4):427–437. doi: 10.2143/AC.61.4.2017304. [DOI] [PubMed] [Google Scholar]
- 34.Vasilj I., et al. Acute coronary syndrome frequency in western Herzegovina over the fifteen year period (1987–2001) Coll. Antropol. 2006;30(4):915–919. [PubMed] [Google Scholar]
- 35.Alastalo H., et al. Cardiovascular health of Finnish war evacuees 60 years later. Ann. Med. 2009;41(1):66–72. doi: 10.1080/07853890802301983. [DOI] [PubMed] [Google Scholar]
- 36.Keinan-Boker L., et al. Chronic health conditions in jewish holocaust survivors born during world war II. Isr. Med. Assoc. J.: Isr. Med. Assoc. J. 2015;17(4):206–212. [PubMed] [Google Scholar]
- 37.Howard J.T., et al. Hypertension in military veterans is associated with combat exposure and combat injury. J. Hypertens. 2020;38(7):1293–1301. doi: 10.1097/HJH.0000000000002364. [DOI] [PubMed] [Google Scholar]
- 38.Vallejo K., Tapias J., Arroyave I. Vol. 2018. BioMed research international; 2018. Trends of Rural/urban Homicide in Colombia, 1992-2015: Internal Armed Conflict and Hints for Postconflict. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dennis M. Political Violence and the Construction of National Identity in Latin America. Springer; 2006. National identity and violence: the case of Colombia; pp. 91–109. [Google Scholar]
- 40.Theidon K. Transitional subjects: the disarmament, demobilization and reintegration of former combatants in Colombia. Int. J. Trans. Just. 2007;1(1):66–90. [Google Scholar]
- 41.Nussio E., Oppenheim B. 2013. Trusting the Enemy: Confidence in the State Among Ex-Combatants. Available at SSRN 2246455. [Google Scholar]
- 42.Shultz J.M., et al. Internal displacement in Colombia: fifteen distinguishing features. Disaster Health. 2014;2(1):13–24. doi: 10.4161/dish.27885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carrillo A.C. Internal displacement in Colombia: humanitarian, economic and social consequences in urban settings and current challenges. Int'l Rev. Red Cross. 2009;91:527. [Google Scholar]
- 44.Moreno C., Cendales R. Mortalidad y años potenciales de vida perdidos por homicidios en Colombia, 1985-2006. Rev. Panam. Salud Públic. 2011;30:342–353. [PubMed] [Google Scholar]
- 45.Cotte Poveda A. Empirical research on the relationship between violence and social development in Colombia. Ensayos Revista de Economia. 2012:37–56. [Google Scholar]
- 46.Instituto Nacional de Salud (INS) In: Salud N.d., editor. Bogotá DC; 2017. Consecuencias del Conflicto Armado en Salud en Colombia; Noveno Informe Técnico Observatorio. [Google Scholar]
- 47.Sekikawa A., et al. Coronary heart disease mortality trends in men in the post World War II birth cohorts aged 35-44 in Japan, South Korea and Taiwan compared with the United States. Int. J. Epidemiol. 1999;28(6):1044–1049. doi: 10.1093/ije/28.6.1044. [DOI] [PubMed] [Google Scholar]
- 48.Alvis-Zakzuk N.J., et al. Education and pneumonia mortality: a trend analysis of its inequalities in Colombian adults. BMJ open respiratory research. 2020;7(1):e000695. doi: 10.1136/bmjresp-2020-000695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ordonez-Monak I., Arroyave I., Cardona-Arango D. 2020. Educational Inequalities in Suicide in a Middle-Income Country: A Socioeconomic Approach of Mental Health. Suicide and Life-Threatening Behavior. (Special issue on public health approaches to suicide prevention) [DOI] [PubMed] [Google Scholar]
- 50.Unesco International. United Nations Educational, Scientific and Cultural Organization (UNESCO); Montreal, Quebec: 2012. Standard Classification of Education - ISCED 2011. [Google Scholar]
- 51.Arroyave I., et al. Socioeconomic inequalities in premature mortality in Colombia, 1998-2007: the double burden of non-communicable diseases and injuries. Prev. Med. 2014:41–47. doi: 10.1016/j.ypmed.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Departamento Administrativo Nacional de Estadística - DANE . 2017. Base de datos de mortalidad. [Google Scholar]
- 53.World Health Organization - WHO . W.H. Organization; 2010. International Classification of Diseases (ICD-10) Version: 2010. [Google Scholar]
- 54.Raghunathan T.E. What do we do with missing data? Some options for analysis of incomplete data. Annu. Rev. Publ. Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- 55.Departamento Administrativo Nacional de Estadística - DANE . 2020. Proyecciones de población por sexo y edades simples hasta 80 años y más, a nivel nacional y departamental. [Google Scholar]
- 56.United States Census, B. Population Analysis Spreadsheets. International Programs Center (IPC) - United States Census Bureau; Washington DC: 2011. Population analysis system (PASEX) [Google Scholar]
- 57.Sas Institute, I. In: User's Guide SAS/STAT® 9.2. Inc S.A.S.I., editor. SAS Institute Inc.; Cary, NC: 2008. The MIANALYZE procedure; pp. 201–233. [Google Scholar]
- 58.Ahmad O.B., et al. GPE Discussion Paper Series. World Health Organization; Geneva: 2001. Age standardization of rates: a new WHO standard. [Google Scholar]
- 59.National Cancer Institute and Statistical Research and Applications Branch. Joinpoint Regression Program; 2013. [Google Scholar]
- 60.Mackenbach J.P., Kunst A.E. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc. Sci. Med. 1997;44:757–771. doi: 10.1016/s0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 61.Harper S., et al. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992–2004. Am. J. Epidemiol. 2008;167(8):889–899. doi: 10.1093/aje/kwn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miller K.E., Rasmussen A. Mental health and armed conflict: the importance of distinguishing between war exposure and other sources of adversity: a response to Neuner. Soc. Sci. Med. 2010;71(8):1385–1389. [Google Scholar]
- 63.Onyut L.P., et al. Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugee settlement–an epidemiological study. Conflict Health. 2009;3(1):6. doi: 10.1186/1752-1505-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ricaurte J.C., et al. The invisible wounds of five decades of armed conflict: inequalities in mental health and their determinants in Colombia. Int. J. Publ. Health. 2019;64(5):703–711. doi: 10.1007/s00038-019-01248-7. [DOI] [PubMed] [Google Scholar]
- 65.Gobierno de Colombia and Departamento de la Prosperidad Social (DPS) Unidad para la Atención y Reparación Integral a las Víctimas. 2022. https://cifras.unidadvictimas.gov.co/ Available from:
- 66.Jawad M., et al. Impact of armed conflict on cardiovascular disease risk: a systematic review. Heart. 2019;105(18):1388–1394. doi: 10.1136/heartjnl-2018-314459. [DOI] [PubMed] [Google Scholar]
- 67.SALUD, I.N.D. and O.N.D. SALUD Consecuencias del conflicto armado en la salud en Colombia. Informe Técnico ONS. 2017;(9):1–340. [Google Scholar]
- 68.Ahmed M.I., et al. Gender-related dissociation in outcomes in chronic heart failure: reduced mortality but similar hospitalization in women. Int. J. Cardiol. 2011;148(1):36–42. doi: 10.1016/j.ijcard.2009.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Veronesi G., et al. Gender differences in the association between education and the incidence of cardiovascular events in Northern Italy. Eur. J. Publ. Health. 2011;21(6):762–767. doi: 10.1093/eurpub/ckq155. [DOI] [PubMed] [Google Scholar]
- 70.Instituto Nacional de Medicina Legal y Ciencias Forenses and Gobierno de Colombia Forensis, Datos para la Vida. Publicación anual que compila el comportamiento de las lesiones de causa externa a través de análisis descriptivos y según variables sociodemográficas, tiempo, modo y lugar. 2017. https://www.medicinalegal.gov.co/cifras-estadisticas/forensis Available from:
- 71.Calderón Rojas J. Etapas del conflicto armado en Colombia: hacia el posconflicto. Latinoamérica. Revista de Estudios Latinoamericanos. 2016;(62):227–257. [Google Scholar]
- 72.Gómez C.M., Valenzuela M.F., Plata J.O.R. Vol. 4. Departamento Administrativo Nacional de Estadística - DANE; 1998. Colombia: proyecciones anuales de población por sexo y edad. [Google Scholar]
- 73.García J.G., Albaladejo J.P., Fernández J.A.M. Métodos de inferencia estadística con datos faltantes: estudio de simulación sobre los efectos en las estimaciones. Estad. Espanola. 2006;48(162):241–270. [Google Scholar]
- 74.Valkonen T. Proceedings of the Symposium on Health and Mortality. 1997. The widening differentials in adult mortality by socio-economic status and their causes. in Health and mortality. Issues of global concern. [Google Scholar]
- 75.Huisman M., et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365:493–500. doi: 10.1016/S0140-6736(05)17867-2. [DOI] [PubMed] [Google Scholar]
- 76.Dégano I.R., et al. The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Sci. Rep. 2017;7(1):1–8. doi: 10.1038/s41598-017-10775-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paz A. Gobierno Nacional de Colombia; 2016. Acuerdo Final para la Terminación del Conflicto y la Construcción de una Paz Estable y Duradera. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data associated with this study has been deposited at Departamento Administrativo Nacional de Estadística–DANE, Colombia Estadísticas Vitales–Microdatos
http://microdatos.dane.gov.co/index.php/catalog/MICRODATOS/about_collection/22/5