Summary
Background
Understanding the long-term outcomes and disability-adjusted life years (DALY) after out-of-hospital cardiac arrest (OHCA) is important to understand the overall health and disease burden of OHCA respectively, but data in Asia remains limited. We aimed to quantify long-term survival and the annual disease burden of OHCA within a national multi-ethnic Asian cohort.
Methods
We conducted an open cohort study linking the Singapore Pan-Asian Resuscitation Outcomes Study (PAROS) and the Singapore Registry of Births and Deaths from 2010 to 2019. We performed Cox regression, constructed Kaplan–Meier curves, and calculated DALYs and standardised mortality ratios (SMR) for each year of follow-up.
Results
We analysed 802 cases. The mean age was 56.0 (SD 17.8). Most were male (631 cases, 78,7%) and of Chinese ethnicity (552 cases, 68.8%). At one year, the SMR was 14.9 (95% CI:12.5–17.8), decreasing to 1.2 (95% CI:0.7–1.8) at three years, and 0.4 (95% CI:0.2–0.8) at five years. Age at arrest (HR:1.03, 95% CI:1.02–1.04, p < 0.001), shockable presenting rhythm (HR:0.75, 95% CI:0.52–0.93, p = 0.015) and CPC category (HR:4.62, 95% CI:3.17–6.75, p < 0.001) were independently associated with mortality. Annual DALYs due to OHCA varied from 304.1 in 2010 to 849.7 in 2015, then 547.1 in 2018. Mean DALYs decreased from 12.162 in 2010 to 3.599 in 2018.
Conclusions
OHCA survivors had an increased mortality rate for the first three years which subsequently normalised compared to that of the general population. Annual OHCA disease burden in DALY trended downwards from 2010 to 2018. Improved surveillance and OHCA treatment strategies may improve long-term survivorship and decrease its global burden.
Funding
National Medical Research Council, Singapore, under the Clinician Scientist Award (NMRC/CSA-SI/0014/2017) and the Singapore Translational Research Investigator Award (MOH-000982-01).
Keywords: Cardiac arrest, Out-of-hospital cardiac arrest, Disease burden, Long-term survival, Mortality
Research in context.
Evidence before this study
Before embarking on this study, we performed a literature review in the Medline and Embase databases. We used key search terms including “cardiac arrest”, “heart arrest”, “survival”, and “mortality” to retrieve studies from inception of each database until December 31, 2021. The majority of studies addressed short-term survival post-OHCA, including survival until 30 days after OHCA or hospital discharge. However, there has been a growing focus on long-term OHCA survivorship and outcomes from multiple domains, such as long-term survival, complications, and quality-of-life among the group of OHCA patients who survive beyond 30 days after OHCA or hospital discharge. Recent international studies in Italy and Australia based on cardiac arrest registries with regional coverage have shed light on this area of research, but results varied with a standardised mortality ratio (SMR) 23 times and five times that of the general population in the former and latter studies respectively. A recent systematic review conducted in 2021 revealed that 20.8% of long-term OHCA survivors were alive at 15 years of follow-up, with lower survival in Asia compared to other regions. There were no studies which measured disability-adjusted life years (DALYs) among post-OHCA survivors in the Asian context. As a whole, data in the Asian context appeared limited.
Added value of this study
Our study aimed to quantify the annual burden of OHCA estimated using DALYs after OHCA in the Asian context, as well as to describe long-term survival and factors associated with survival among OHCA survivors up to 10 years of follow-up. Our study linked the Singapore data from the Pan-Asian Resuscitation Outcomes Study, an international, multicentre, cardiac arrest registry which has complete national coverage in Singapore, to the national death registry. This allowed us to estimate the SMR for long-term OHCA survivors and calculate disease burden in terms of DALYs using a nationally representative sample which had comprehensive case capture. Our key findings were that (a) long-term survivorship of the OHCA cohort decreased through the follow-up period, (b) SMR decreased from the first to the fifth year of follow-up, and (c) total DALY attributable to long-term OHCA survivors varied although mean DALY decreased from 2010 to 2018. Our study is the first national Asian study to quantify long-term survival and disease burden of long-term OHCA survivors, to our knowledge, and thus represents an important contribution to current evidence.
Implications of all the available evidence
Taken together with existing evidence, our study suggests that adult OHCA continues to exert a large burden of disease, warranting an increased focus on OHCA with regard to public health policy. The available evidence suggests that SMR among OHCA survivors is the highest in the early years post-OHCA and eventually normalises to that of the general population. Furthermore, our study revealed a decreasing trend in DALYs despite contrary evidence from international studies, with these observed differences likely due to differences in surveillance or treatment strategies, ranging from community interventions to post-resuscitation care. Based on these findings, public health policy should pay close attention to OHCA survivors during the initial follow-up period, when they seem to be most vulnerable. Furthermore, additional data is urgently needed to investigate how and why the disease burden and long-term survival of OHCA varies, in order to guide research into treatment strategies for OHCA aimed at the various predictors of long-term survival, such as interventions to improve short-term neurological outcomes, which was a significant predictor of survival in our study.
Introduction
Out-of-hospital cardiac arrest (OHCA), or sudden cardiac arrest, is one of the leading causes of mortality worldwide.1,2 The global incidence of emergency medical services (EMS)-treated OHCA may range from 30 to 97.1 per 100,000 population among which the percentage surviving to discharge is an estimated 8.6%–9.9%.1, 2, 3, 4, 5, 6, 7 In Singapore, the age-adjusted incidence of OHCA was approximately 50.0 per 100,000 person-years and increased between 2011 and 2016, with survival rates of approximately 1.0–3.0% in the same period.4,8 OHCA thus poses a large health burden both locally and internationally.
OHCA is defined as the loss of functional cardiac mechanical activity in association with an absence of systemic circulation, occurring outside of a hospital setting.1 Extensive research has been conducted on factors associated with short-term survival following OHCA.9, 10, 11 Recently, however, increased focus has been placed on the long-term outcomes of OHCA,12, 13, 14 including long-term survival and health-related quality of life during the additional years of life lived,12,15, 16, 17 which help evaluate the natural history and long-term impact of OHCA on the health burden of society.12,18,19 To quantify both the fatal and non-fatal disease burden of OHCA, several recent articles had applied the concept of disability-adjusted life years (DALYs) to OHCA.19, 20, 21 The DALY of a case is defined as the sum of the number of years of life lost (YLL) and the number of years lived with disability (YLD).22 Thus, one DALY is equal to one year of healthy life lost. The estimated annual DALYs after adult nontraumatic EMS-treated OHCA in the United States was 4,354,192 in 2016, with a rate of 1347 OHCA DALYs per 100,000 population (third highest cause of DALYs in the US).21
To our knowledge, data on the long-term outcomes of OHCA in Asia has been limited12 with no reports on DALYs after OHCA in Asia. We aimed to quantify the annual disease burden of OHCA estimated using DALYs in a national multi-ethnic Asian cohort and describe factors associated with long-term survival (up to 10 years follow up).
Methods
Study design
We conducted an open cohort study through the linkage of two national datasets, the Singapore data from the Pan-Asian Resuscitation Outcomes Study (PAROS),23 and the Singapore Registry of Births and Deaths (henceforth, the “death registry”)24 from 2010 to 2019. PAROS is an international, multicentre, prospective registry of OHCA in nine countries across the Asia–Pacific region established in 2009.23 PAROS is based on Utstein-style recommendations25 and has a data dictionary and taxonomy aligned with the Cardiac Arrest Registry to Improve Survival (CARES).26 The death registry is maintained by the Ministry of Home Affairs Immigration and Checkpoints Authority and includes data on the cause and date of death of all Singaporeans and permanent residents residing in Singapore.24 We then linked the PAROS data with the death registry to determine the survival status and duration of the OHCA survivors after OHCA. Data linkage was performed using the National Registration Identity Card (NRIC) numbers of each case, which is the unique national identification number in Singapore. There is legislative requirement to report death certifications according to the Registration of Births and Deaths Act of 1937, therefore ensuring complete and accurate ascertainment of nation-wide long-term mortality outcomes among OHCA cases.
Setting
This study was conducted in Singapore, an urbanized, multi-ethnic, densely populated island city-state located in Southeast Asia with a population of 5.7 million over a land area of 725.7 km2 (population density of 7810 per km2).27 The Singapore Civil Defence Force (SCDF) provides nationwide EMS in Singapore and is a fire-based system activated by a centralized “995” dispatch system.22,28 All ambulances have mechanical CPR devices, and all ambulance personnel are proficient in basic life support skills and can administer automated external defibrillators.28 Patients experiencing OHCA in Singapore typically receive treatment at the scene and are then transported to the hospital by EMS after a brief period of resuscitation, usually with ongoing CPR.4 In recent years, several new prehospital interventions have also been developed in Singapore and detailed description regarding EMS management of OHCA in Singapore can be found in a previous paper.29
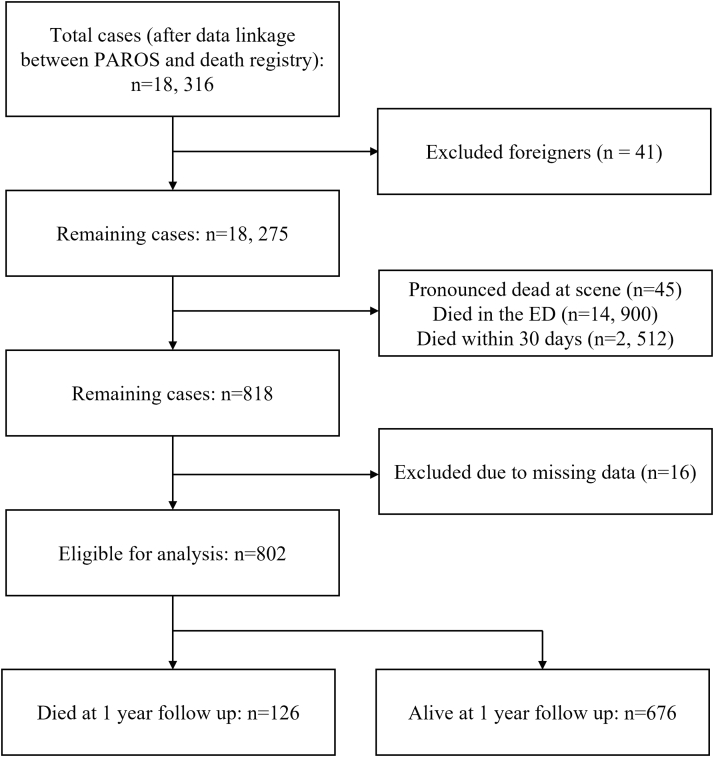
Study population and data collection
We included all cases with OHCA in the PAROS dataset (Singapore participants) in this study, defined as any OHCA conveyed by EMS or presenting at emergency departments, as confirmed by the absence of pulse, unresponsiveness, and apnea.23 As this study investigated the long-term outcomes of OHCA, we excluded all cases that demised within 30 days of the date of OHCA. We also excluded foreigners who had no follow-up data and hence no death information after linkage with the Singapore Death Registry, as they may have left the country. The date of OHCA was taken as the event date and the registry data were subject to annual audits for accuracy and inter-rater reliability. Outlier and illogical data were flagged and reviewed for final consensus among the registry coordinators. The study was approved by the Centralised Institutional Review Board (CIRB ref: 2018/2937) and qualified for exemption from full review as it analyzed de-identified data, with the Ministry of Health's Unit for Prehospital Emergency Care acting as a trusted third party.
Data collected from linkage of the two national databases included case demographics (age, sex, race), details of OHCA, initiation of targeted temperature management, and date and cause of death. Details of OHCA included the presenting rhythm (categorised as shockable, non-shockable, and unknown rhythm), the presence of a witness during the OHCA, the provision of bystander CPR, EMS response time (defined as time the call was received at dispatch to the time the ambulance arrived on scene and dichotomised to greater than 8 min and lesser than or equal to 8 min) and Cerebral Performance Category (CPC) categorised to CPC grades 1 and 2 versus CPC grades 3 and 4.
The primary outcome of interest was duration of survival after OHCA and was computed as the time from 30 days after the date of OHCA to the date of death as documented by the Singapore death registry. For the time-to-event analysis, the date of censoring was taken as the 30th of June 2020. The cause of death was determined from the death registry and was collected based on ICD 9 and ICD 10 codes reported by Singapore registered medical practitioners who announced the patient's death. ICD 9 and ICD 10 codes were harmonised using an open source R package, icdcoder.30
Statistical analyses
Baseline characteristics were presented as frequencies and proportions for categorical variables, and median (interquartile range) or mean (standard deviation) for continuous variables, as appropriate for the distribution of the data. In accordance with previous literature,31 we used a transport time of 8 min to dichotomise the cohort of OHCA survivors into two groups of similar size. Hypothesis testing was conducted using the Pearson Chi-squared test and the independent student t-test to compare baseline characteristics by death status at one year follow up.
To investigate the long-term survival of patients with OHCA, we conducted survival analyses and computed Cox proportion regression models to identify factors that were significantly and independently associated with survival. Covariates included in the cox-proportional models were demographics (age, sex, and race), details of OHCA (presenting rhythm, witnessed arrest, bystander CPR, EMS response time, and CPC category), and the initiation of targeted temperature management. In previous years, the median EMS response time in Singapore was found to be close to 8 min,4,29 with both local studies29 and international studies31 using the 8-min timepoint as a natural cut-off, hence we chose to use the 8-min timepoint as a cut-off here. The proportional hazards assumption was assessed. Missing data within variables was kept as a separate category to preserve the overall sample size. Kaplan–Meier survival curves were constructed for the overall population, and by key characteristics. The proportion surviving (and 95% CI) was calculated annually for up to eight years post-OHCA.
For the final model, we started with the most significant covariate identified on univariate analysis and used the likelihood ratio to assess whether inclusion of the next most significant variable would improve the fit of the model. This was done sequentially until all variables had been assessed. Interaction effects were also assessed for the variables in the multivariate model. A stratified analysis was performed by CPC category as we found significant interaction effects. Kaplan–Meier survival curves were constructed for the overall population, and by key characteristics. The proportion surviving (and 95% CI) was calculated for up to eight years post-OHCA.
We calculated the standardised mortality ratio (SMR) for each year of follow up (computed as the ratio of the observed number of deaths divided by the expected number of deaths). The expected number of deaths was defined as the age and sex indirect standardised, with the expected death rates at each year of OHCA and follow up year calculated from the Complete Life Table for Singapore Residents 2019.32 The top 10 causes of death categorized by ICD10 categories were tabulated.
To quantify the annual disease burden of OHCA in Singapore, the DALY following OHCA was calculated as follows: for each death, the YLL was calculated from the remaining standard life expectancy at the age of death, stratified by gender, while the YLD was calculated by assigning a disability weight (DW) based on their CPC score.19 Further details may be found in the Supplementary material Appendix S1. The DALY was a summation of YLL and YLD.20 The sum and average DALY, along with YLL and YLD was calculated annually from 2010 to 2018. The level of significance was set at 5% and the analysis was performed using Stata V16 (Stata Corp, College Station, Tx, USA).
Results
We included 802 cases in the analysis. 17,473 cases were excluded because they died within 30 days of OHCA, and 41 cases were excluded because these were foreigners with no cause of death or death date. The detailed population flowchart may be found in Supplementary Fig. S1. 126 cases had demised at one-year follow up. The mean age of the cohort was 56.0 (SD 17.8) and majority of the cohort was male (631 cases, 78.7%) and of Chinese ethnicity (552 cases, 68.8%). OHCA survivors who died at one year of follow up had significantly older age, a lower proportion of shockable presenting rhythm, and higher CPC category at baseline (Table 1). All survival estimates refer to survival among patients surviving to 30 days after OHCA, therefore fulfilling the inclusion criteria.
Table 1.
Baseline demographics and clinical characteristics of the OHCA cohort stratified by mortality at one year follow up.
| Factor | Whole Cohort (%) | Alive at 1 Year (%) | Died at 1 Year (%) | p-Valuea |
|---|---|---|---|---|
| Total N | 802 | 676 | 126 | |
| Gender | 0.054 | |||
| Male | 631 (78.7%) | 540 (79.9%) | 91 (72.2%) | |
| Female | 171 (21.3%) | 136 (20.1%) | 35 (27.8%) | |
| Age, mean (SD) | 56.0 (17.8) | 54.4 (17.5) | 64.9 (16.7) | <0.001∗ |
| Race | 0.99 | |||
| Chinese | 552 (68.8%) | 455 (67.3%) | 97 (77.0%) | |
| Malay | 96 (12.0%) | 83 (12.3%) | 13 (10.3%) | |
| Indian | 114 (14.2%) | 100 (14.8%) | 14 (11.1%) | |
| Other | 40 (5.0%) | 38 (5.6%) | 2 (1.6%) | |
| Bystander CPR | 0.39 | |||
| No | 316 (39.4%) | 262 (38.8%) | 54 (42.9%) | |
| Yes | 486 (60.6%) | 414 (61.2%) | 72 (57.1%) | |
| Arrest witnessed | 0.35 | |||
| No | 136 (17.0%) | 111 (16.4%) | 25 (19.8%) | |
| Yes | 666 (83.0%) | 565 (83.6%) | 101 (80.2%) | |
| Hypothermia therapy initiated | 0.42 | |||
| No | 554 (69.2%) | 463 (68.6%) | 91 (72.2%) | |
| Yes | 247 (30.8%) | 212 (31.4%) | 35 (27.8%) | |
| EMS ambulance response time | 0.59 | |||
| ≤8 min | 381 (47.5%) | 319 (47.2%) | 62 (49.2%) | |
| >8 min | 393 (49.0%) | 335 (49.6%) | 58 (46.0%) | |
| Missing | 28 (3.5%) | 22 (3.3%) | 6 (4.8%) | |
| Shockable first arrest rhythm | <0.001∗ | |||
| Non-shockable | 167 (20.8%) | 121 (17.9%) | 46 (36.5%) | |
| Shockable | 577 (71.9%) | 503 (74.4%) | 74 (58.7%) | |
| Unknown | 58 (7.2%) | 52 (7.7%) | 6 (4.8%) | |
| Cerebral performance category | ||||
| Grouped | <0.001∗ | |||
| 1-2 | 540 (67.5%) | 500 (74.2%) | 40 (31.7%) | |
| 3-4 | 257 (32.1%) | 171 (25.4%) | 86 (68.3%) | |
| Missing | 3 (0.4%) | 3 (0.4%) | 0 (0.0%) |
OHCA: Out-of-hospital cardiac arrest; SD: Standard deviation; CPR: Cardiopulmonary resuscitation; EMS: Emergency medical services. ∗p value < 0.05.
Test comparing alive and deceased at 1 year.
In the univariate cox proportional hazards model, age at arrest (HR 1.04, 95% CI: 1.03–1.05, p < 0.001), female sex (HR 1.35, 95% CI: 1.01–1.81, p = 0.046), and CPC category 3-4 (HR 4.20, 95% CI: 3.23–5.46, p < 0.001) were found to be significantly associated with mortality while shockable presenting rhythm (HR 0.44, 95% CI: 0.33–0.58, p < 0.001) and ‘other’ race (HR 0.26, 95% CI: 0.10–0.69, p < 0.007) were significantly associated with survival (Table 2). Fig. 1A shows the overall survival curve, and Fig. 1B and C shows the curves for subgroups by CPC category and shockable rhythm.
Table 2.
Demographic and clinical factors associated with survival on Cox-proportional hazards models.
| Covariate | Univariate analysis |
Adjusted analysis |
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Gender | ||||||
| Male | Reference | |||||
| Female | 1.35 | 1.01–1.81 | 0.046∗ | |||
| Age, every year increase | 1.04 | 1.03–1.05 | <0.001∗ | 1.03 | 1.02–1.04 | <0.001∗ |
| Race | ||||||
| Chinese | Reference | |||||
| Malay | 0.68 | 0.43–1.05 | 0.085 | |||
| Indian | 0.90 | 0.62–1.31 | 0.589 | |||
| Other | 0.26 | 0.10–0.69 | 0.007∗ | |||
| Bystander CPR | ||||||
| No | Reference | |||||
| Yes | 0.89 | 0.68–1.15 | 0.362 | |||
| Arrest witnessed | ||||||
| No | Reference | |||||
| Yes | 0.96 | 0.68–1.34 | 0.793 | |||
| Hypothermia therapy initiated | ||||||
| No | Reference | |||||
| Yes | 0.90 | 0.68–1.20 | 0.482 | |||
| EMS ambulance response time | ||||||
| ≤8 min | Reference | |||||
| >8 min | 0.95 | 0.73–1.24 | 0.713 | |||
| Shockable first arrest rhythm | ||||||
| Non-shockable | Reference | Reference | ||||
| Shockable | 0.44 | 0.33–0.58 | <0.001∗ | 0.70 | 0.52–0.93 | 0.015∗ |
| Unknown | 0.40 | 0.22–0.73 | 0.003∗ | 0.45 | 0.24–0.82 | 0.010∗ |
| Cerebral Performance Category | ||||||
| 1-2 | Reference | Reference | ||||
| 3-4 | 4.20 | 3.23–5.46 | <0.001∗ | 4.62 | 3.17–6.75 | <0.001∗ |
HR: Hazard ratio; 95% CI: 95% confidence interval; CPR: Cardiopulmonary resuscitation; EMS: Emergency medical services. ∗p value < 0.05.
Fig. 1.
Overall survival of out-of-hospital cardiac arrest patients in Singapore, in total (A), by shockable rhythm (B), and by Cerebral Performance Category (C).
In the multivariate cox proportional hazards model age at arrest (HR 1.03, 95% CI: 1.02–1.04, p < 0.001) and CPC category 3-4 (HR 4.62, 95% CI: 3.17–6.75, p < 0.001) were independently associated with mortality while shockable presenting rhythm (HR 0.75, 95% CI: 0.52–0.93, p = 0.015) was significantly associated with survival (Table 2). We found a significant interaction effect between CPC category and age (p < 0.001), as well as CPC category and a shockable first rhythm (p < 0.001) in a stratified analysis (Supplementary Table S1). Amongst those with CPC grades 1-2, age had a stronger effect on mortality (HR 1.05, 95% CI: 1.03–1.07) as compared to those with CPC grades 3-4 (HR 1.02, 95% CI: 1.01–1.03). In addition, amongst those with CPC grades 1-2, a shockable first rhythm had a significant protective effect (HR 0.36, 95% CI: 0.23–0.58) compared to those with CPC grades 3-4 (HR 1.02, 95% CI: 0.72–1.45).
The long-term survivorship of OHCA was reported for each year of follow up (Table 3). The proportion surviving at one year of follow up was 0.84 (95% CI: 0.81–0.87), at five years of follow up was 0.68 (95% CI 0.65–0.72), and at ten years of follow up was 0.62 (95% CI 0.57–0.67). The top three causes of death after OHCA based on ICD10 categories were pneumonia, chronic ischemic heart disease, and acute myocardial infarction (Supplementary Table S2). The age-sex SMR of the OHCA cohort compared to the standard Singapore population was shown in Fig. 2. At one year of follow up, the SMR was 14.9 (95% CI: 12.5–17.8) and this decreased to 1.2 (95% CI: 0.7–1.8) at three years follow up, and 0.4 (95% CI: 0.2–0.8) at five years follow up.
Table 3.
Survival by follow-up period of the out-of-hospital cardiac arrest cohort.
| Follow-up year | Population at risk | Deaths | Proportion surviving | 95% CI | |
|---|---|---|---|---|---|
| 1 | 675 | 127 | 0.84 | 0.81 | 0.87 |
| 2 | 539 | 50 | 0.78 | 0.75 | 0.80 |
| 3 | 414 | 23 | 0.74 | 0.71 | 0.77 |
| 4 | 296 | 13 | 0.71 | 0.68 | 0.75 |
| 5 | 196 | 11 | 0.68 | 0.65 | 0.72 |
| 6 | 129 | 5 | 0.66 | 0.62 | 0.70 |
| 7 | 89 | 3 | 0.65 | 0.60 | 0.69 |
| 8 | 49 | 2 | 0.62 | 0.57 | 0.67 |
| 9 | 26 | 0 | 0.62 | 0.57 | 0.67 |
| 10 | 3 | 0 | 0.62 | 0.57 | 0.67 |
95% CI: 95% confidence interval.
Fig. 2.
Yearly standardised mortality ratios (95% confidence interval) of out-of-hospital cardiac arrest patients in relation to the standard Singapore population in 2019.
The annual disease burden of long-term OHCA survivors in Singapore measured using DALYs were reported from 2010 to 2018 in Table 4. The total YLL increased from 303.1 in 2010 to 844.2 in 2015, followed by decreasing to 538.5 in 2018. The total YLD increased from 1.0 in 2010 to 8.6 in 2018. The total DALY increased from 304.1 in 2010 to 849.7 in 2015, followed by decreasing to 547.1 in 2018, while mean DALY decreased from 12.162 in 2010 to 3.599 in 2018 among long-term OHCA survivors.
Table 4.
Disability-adjusted life years lost for the out-of-hospital cardiac arrest cohort from 2010 to 2018.
| Year | Total YLL | Total YLD | Total DALY | YLL |
YLD |
DALY |
|||
|---|---|---|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||||
| 2010 | 303.1 | 1.0 | 304.1 | 27.6 | 16.4–38.7 | 0.07 | 0.05–0.09 | 12.2 | 4.9–19.4 |
| 2011 | 310.2 | 1.8 | 312.0 | 22.2 | 15.7–28.6 | 0.07 | 0.06–0.09 | 8.0 | 3.9–12.1 |
| 2012 | 371.4 | 1.8 | 373.2 | 18.6 | 15.1–22.1 | 0.06 | 0.05–0.08 | 7.8 | 4.8–10.8 |
| 2013 | 550.8 | 2.9 | 553.7 | 19.7 | 13.8–25.5 | 0.08 | 0.06–0.09 | 8.4 | 5.0–11.8 |
| 2014 | 624.8 | 2.8 | 627.6 | 21.5 | 17.8–25.3 | 0.06 | 0.05–0.07 | 8.0 | 5.3–10.8 |
| 2015 | 844.2 | 5.5 | 849.7 | 22.2 | 17.1–27.3 | 0.07 | 0.06–0.08 | 7.5 | 4.9–10.1 |
| 2016 | 731.6 | 7.7 | 739.3 | 18.8 | 14.7–22.8 | 0.07 | 0.06–0.07 | 4.8 | 3.2–6.4 |
| 2017 | 685.3 | 6.0 | 691.3 | 23.6 | 18.4–28.9 | 0.06 | 0.06–0.07 | 5.6 | 3.5–7.8 |
| 2018 | 538.5 | 8.6 | 547.1 | 20.7 | 16.3–25.2 | 0.07 | 0.06–0.07 | 3.6 | 2.2–5.0 |
YLL: Years of life lost; YLD: Years of healthy life lost due to disability; DALY: Disability-adjusted life years; 95% CI: 95% confidence intervals.
Discussion
We investigated the long-term survival of a large national Asian cohort who survived to 30 days after OHCA. The key findings of this study were that (a) long-term survivorship of the OHCA cohort decreased from 0.84 at one year of follow up to 0.62 at 10 years of follow up, (b) SMR decreased from 14.9 at one year of follow up to 1.2 and 0.4 and three and five years of follow up respectively, and (c) total DALY attributable to long-term OHCA survivors varied from 304.1 in 2010 to 849.7 in 2015 and finally to 547.1 in 2018, although mean DALY decreased from 12.2 in 2010 to 3.6 in 2018. To our knowledge, this is the first national Asian study to quantify the annual disease burden of OHCA over time using DALY and to describe the long-term survival of OHCA patients for up to 10 years, hence representing a significant contribution to the growing body of literature on the public health burden and long-term outcomes of OHCA.
In the Singapore Burden of Disease Study,33 cardiovascular diseases including OHCA were the leading cause of DALY, largely driven by YLL. However, the overall decrease in the mean DALY from 2010 to 2018 in our study suggests that the long-term burden per OHCA patient has improved in Singapore over time, whereas international data revealed an increasing burden of disease due to OHCA from 2013 to 2018 (possibly because of more precise national OHCA surveillance in the later years).20 This result from a cohort of initial OHCA survivors in a small city-state may have been influenced by nation-wide improvements to OHCA interventions,34 ranging from community interventions such as the MyResponder phone application to improve rates of bystander CPR and AED use35 to post-resuscitation interventions including coronary angiography (CAG) with percutaneous coronary intervention (PCI)36 and targeted temperature management (TTM).37, 38, 39 Although bystander CPR was not significantly associated with long-term survival in this study, the sum effect of these interventions may have improved short-term neurological outcomes, which was significantly associated with long-term survival here and elsewhere.40 Yet, this encouraging result should not imply that OHCA has a decreasing public health burden, since total DALY may increase in the future considering Singapore's aging population and the association between older age and mortality.
Our results further add to a body of knowledge about long-term OHCA survival contributed to by various international studies. A cohort of 3449 OHCA survivors in Victoria, Australia, had a 10-year absolute survival of 70% and an SMR that approached that of the general population after 5 years of follow up.16 A study by Baldi et al. based in Lombardia, Italy, demonstrated a SMR which decreased from 23 (95% CI: 16.8–30.2) to 2.6 (95% CI: 1.03–4.8) from the first to fifth year of follow up using an approach to SMR analysis similar in concept to our approach.41 Lastly, a recent South Korean study also showed an all-cause mortality of 35.2% after 1 year of follow up and 62.7% after 5 years of follow up, suggesting that more than half of long-term survivors who died met their demise in the first year.42 These results support the hypothesis that mortality in initial OHCA survivors is greatest during the immediate period after OHCA with increased mortality up to 15-fold higher than the general population. This improves in the later years,43 suggesting that the longer patients survive beyond the initial 5 years after OHCA, the more likely they are to experience a life-span comparable to an age and sex-matched general population.2,18,39 Our findings that age at arrest, non-shockable presenting rhythm, and CPC category 3-4 were independently associated with higher risk of mortality are largely consistent with other studies worldwide.44,45 It has been previously hypothesised that traditional factors such as witnessed arrest, bystander CPR, and EMS response time influence long-term survival to a lesser degree than short-term survival.16 As Singapore is a small, developed, and densely populated city-state with a mature healthcare system,46 geographical factors in our study related to location of arrest and access to PCI-capable hospitals were also less of a concern compared to other countries.1,16 Lastly, we identified CPC grade to be an effect modifier of the association between age or shockable first rhythm and mortality. Our results suggest that older age and non-shockable first rhythm had stronger effects on mortality in OHCA survivors with CPC grades 1-2 as compared to those with CPC grades 3-4. Hence, in patients with CPC grades 3-4, poor neurological recovery may be the most important predictive factor for mortality in the long-term.16,47
The importance of short-term good neurological outcome to long-term survival implies that interventions to improve short-term neurological outcomes such as CAG, PCI, intensive care, and other post-resuscitation care strategies may in turn improve longer term outcomes. More data about the long-term complications of OHCA, such as acute myocardial infarction (which was the third-most common cause of mortality in this study) or recurrent cardiac arrest, are needed to guide the long-term management of OHCA survivors.48 This is also the case in Singapore, especially since our current findings are closely linked to future translational work and are part of an ongoing internal conversation exploring the long-term quality of life among OHCA survivors. Further research into these gaps will be important to elucidate the reasons behind changes in the burden of OHCA over the years, thereby guiding potential public health policies, although much remains unknown about the global burden of OHCA survivors in terms of DALY and what may ease this burden in the future.
Strengths and limitations
Our study is the first population-based Asian study to quantify the long-term survivorship of OHCA and the national disease burden exerted by this cohort of OHCA survivors. The strengths of our study include a nationally representative cohort of patients with comprehensive case capture via the linkage of two national cohorts using a nationalised identification number, and the prospective ascertainment of exposure, outcomes and follow up time in the cohort. Our study is based on the PAROS registry, which has population-level coverage, and in fact has complete national coverage because Singapore is an island city-state with few patients spilling over to non-surveilled healthcare systems and every hospital, as well as the sole emergency ambulance service, contributes data fully to PAROS. However, we were not able to capture quality-of-life outcomes among long-term OHCA survivors, which are important but often overlooked by resuscitation studies. Furthermore, another limitation was the relatively smaller cohort size of our study. This may have led to less stable weight calculations and larger fluctuations in annual trends for our reported outcomes, although we encourage readers to interpret the estimates in context of the 95% confidence intervals, which we have reported in the manuscript. Our study was also limited by the exclusion of foreigners treated in Singapore that had no date of death recorded or whose deaths were not captured as they were overseas, and by the exclusion of cases with 2nd episode cardiac arrest. The choice of DW to calculate the YLD for individual patients also influenced our study findings, although this choice was made to improve comparability of results and reflects current understanding of how cardiac arrest impacts long-term quality of life. The observational design of this study implies our results are limited to observed associations and cannot establish a causal link between covariates and outcomes. Furthermore, our results are vulnerable to confounding, although efforts to minimise these effects were made through our adjusted analyses.
Conclusion
Adult OHCA has a large burden of disease and should be a focus of public health policy. In this national study, initial survivors of OHCA had an increased mortality rate compared to the general population for the first three years, but subsequently normalised to that of the general population, while the annual disease burden of OHCA quantified using DALYs showed decreasing trends from 2010 to 2018. Further improvements in the surveillance and OHCA treatment strategies are needed to improve long-term survivorship and to decrease the global burden of OHCA.
Contributors
AFWH, MJRL, and MEHO were involved in conceptualisation. AFWH, MJRL, AE, PPP, and MEHO were involved in data collection. AFWH, MJRL, NG, and AE were involved in data analysis. AFWH, MJRL, JWY, AB, and NG were involved in manuscript drafting. AFWH, MJRL, JWY, AB, NG, PPP, and LT were involved in manuscript review.
Data sharing statement
The data that support the findings of this study are available from the PAROS investigators and National Registry of Diseases Office. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the authors with the permission of the PAROS investigators and National Registry of Diseases Office.
Ethics approval and consent to participate
The study was approved by the Centralised Institutional Review Board (CIRB ref: 2018/2937) and qualified for exemption from full review as it analyzed de-identified data, with the Ministry of Health's Unit for Prehospital Emergency Care acting as a trusted third party.
Declaration of interests
MEH Ong reports funding from the Zoll Medical Corporation for a study involving mechanical cardiopulmonary resuscitation devices; grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan-Asian Resuscitation Outcomes Study; an advisory relationship with Global Healthcare SG, a commercial entity that manufactures cooling devices; and funding from Laerdal Medical on an observation program to their Community CPR Training Centre Research Program in Norway. PP Pek reports previous accommodation for participation in Research Masterclass Laerdal. A Blewer reports previous involvement with the National Heart, Lung, and Blood Institute and Eunice Kennedy Shriver National Institute of Child Health and Human Development and Laerdal Foundation.
Acknowledgements
The authors would like to thank Ms Nur Shahidah, Ms Pek Pin Pin and the late Ms Susan Yap from Department of Emergency Medicine, Singapore General Hospital; Ms Nurul Asyikin, Ms Liew Le Xuan and Ms Joann Poh from Unit for Prehospital Emergency Care, Singapore General Hospital for their contributions and support to the Singapore OHCA registry. We would also like to acknowledge the Singapore PAROS Investigators: Michael YC Chia (Tan Tock Seng Hospital, Singapore); Yih Yng Ng (Tan Tock Seng Hospital, Singapore); Benjamin SH Leong (National University Hospital); Han Nee Gan (Changi General Hospital, Singapore); Wei Ming Ng (Ng Teng Fong General Hospital, Singapore); Si Oon Cheah (Urgent Care Clinic International, Singapore); Desmond R Mao (Khoo Teck Puat Hospital, Singapore); Nausheen Edwin Doctor (Sengkang General Hospital, Singapore); Shalini Arulanandam (past Chief Medical Officer from Singapore Civil Defence Force).
Funding: This study was supported by grants from National Medical Research Council, Clinician Scientist Award, Singapore (NMRC/CSA/024/2010, NMRC/CSA/0049/2013 and NMRC/CSA-SI/0014/2017), National Medical Research Council, Clinician Investigator Salary Support Programme (NMRC/CSSP/0079/2018) and Ministry of Health, Health Services Research Grant, Singapore (HSRG/0021/2012). AFWH was supported by Khoo Clinical Scholars Programme, Khoo Pilot Award (KP/2019/0034), Duke-NUS Medical School and National Medical Research Council (NMRC/CS_Seedfd/012/2018).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2022.100672.
Contributor Information
Andrew Fu Wah Ho, Email: andrew.ho@duke-nus.edu.sg.
Singapore PAROS Investigators:
Michael Y.C. Chia, Yih Yng Ng, Benjamin S.H. Leong, Han Nee Gan, Wei Ming Ng, Si Oon Cheah, Desmond R. Mao, Nausheen Edwin, and Shalini Arulanandam
Appendix A. Supplementary data
Supplementary Fig. S1.
References
- 1.Myat A., Song K.J., Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391(10124):970–979. doi: 10.1016/S0140-6736(18)30472-0. [DOI] [PubMed] [Google Scholar]
- 2.Yan S., Gan Y., Jiang N., et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Empana J.P., Lerner I., Valentin E., et al. Incidence of sudden cardiac death in the European union. J Am Coll Cardiol. 2022;79(18):1818–1827. doi: 10.1016/j.jacc.2022.02.041. [DOI] [PubMed] [Google Scholar]
- 4.Lim S.L., Smith K., Dyson K., et al. Incidence and outcomes of out-of-hospital cardiac arrest in Singapore and Victoria: a collaborative study. J Am Heart Assoc. 2020;9(21) doi: 10.1161/JAHA.119.015981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berdowski J., Berg R.A., Tijssen J.G., Koster R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Nichol G., Thomas E., Callaway C.W., et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiguchi T., Okubo M., Nishiyama C., et al. Out-of-hospital cardiac arrest across the world: first report from the international liaison committee on resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 8.Ong M.E., Shin S.D., De Souza N.N., et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan asian resuscitation outcomes study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Hallstrom A.P., Cobb L.A., Yu B.H. Influence of comorbidity on the outcome of patients treated for out-of-hospital ventricular fibrillation. Circulation. 1996;93(11):2019–2022. doi: 10.1161/01.cir.93.11.2019. [DOI] [PubMed] [Google Scholar]
- 10.Sasson C., Rogers M.A., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 11.Andrew E., Nehme Z., Bernard S., Smith K. The influence of comorbidity on survival and long-term outcomes after out-of-hospital cardiac arrest. Resuscitation. 2017;110:42–47. doi: 10.1016/j.resuscitation.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 12.Chin Y.H., Yaow C.Y.L., Teoh S.E., et al. Long-term outcomes after out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2022;171:15–29. doi: 10.1016/j.resuscitation.2021.12.026. [DOI] [PubMed] [Google Scholar]
- 13.Lam T.J.R., Yang J., Poh J.E., et al. Long term risk of recurrence among survivors of sudden cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2022;176:30–41. doi: 10.1016/j.resuscitation.2022.04.027. [DOI] [PubMed] [Google Scholar]
- 14.Yaow C.Y.L., Teoh S.E., Lim W.S., et al. Prevalence of anxiety, depression, and post-traumatic stress disorder after cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2022;170:82–91. doi: 10.1016/j.resuscitation.2021.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Rey J.R., Caro-Codón J., Rodríguez Sotelo L., et al. Long term clinical outcomes in survivors after out-of-hospital cardiac arrest. Eur J Intern Med. 2020;74:49–54. doi: 10.1016/j.ejim.2019.11.024. [DOI] [PubMed] [Google Scholar]
- 16.Andrew E., Nehme Z., Wolfe R., Bernard S., Smith K. Long-term survival following out-of-hospital cardiac arrest. Heart. 2017;103(14):1104–1110. doi: 10.1136/heartjnl-2016-310485. [DOI] [PubMed] [Google Scholar]
- 17.Lahmann A.L., Bongiovanni D., Berkefeld A., et al. Predicting factors for long-term survival in patients with out-of-hospital cardiac arrest—a propensity score-matched analysis. PLoS One. 2020;15(1) doi: 10.1371/journal.pone.0218634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majewski D., Ball S., Bailey P., Bray J., Finn J. Relative long-term survival in out-of-hospital cardiac arrest: is it really improving? Resuscitation. 2020;157:108–111. doi: 10.1016/j.resuscitation.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Ginsberg G.M., Kark J.D., Einav S. Cost-utility analysis of treating out of hospital cardiac arrests in Jerusalem. Resuscitation. 2015;86:54–61. doi: 10.1016/j.resuscitation.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Coute R.A., Nathanson B.H., Panchal A.R., et al. Disability-adjusted life years following adult out-of-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12(3) doi: 10.1161/CIRCOUTCOMES.118.004677. [DOI] [PubMed] [Google Scholar]
- 21.Coute R.A., Nathanson B.H., Mader T.J., McNally B., Kurz M.C. Trend analysis of disability-adjusted life years following adult out-of-hospital cardiac arrest in the United States: a study from the CARES Surveillance Group. Resuscitation. 2021;163:124–129. doi: 10.1016/j.resuscitation.2020.10.048. [DOI] [PubMed] [Google Scholar]
- 22.Devleesschauwer B., Havelaar A.H., Maertens de Noordhout C., et al. Calculating disability-adjusted life years to quantify burden of disease. Int J Public Health. 2014;59(3):565–569. doi: 10.1007/s00038-014-0552-z. [DOI] [PubMed] [Google Scholar]
- 23.Ong M.E., Shin S.D., Tanaka H., et al. Pan-asian resuscitation outcomes study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18(8):890–897. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 24.ICA S . 2020. Report on registration of Births and deaths. [Google Scholar]
- 25.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task Force of the international liaison committee on resuscitation (American heart association, European resuscitation Council, Australian and New Zealand Council on resuscitation, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation Council of southern africa, resuscitation Council of Asia); and the American heart association emergency cardiovascular care committee and the Council on cardiopulmonary, critical care, perioperative and resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 26.McNally B., Stokes A., Crouch A., Kellermann A.L. CARES: cardiac arrest registry to enhance survival. Ann Emerg Med. 2009;54(5):674–683.e2. doi: 10.1016/j.annemergmed.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 27.Singapore DoS . 2021. Population and population structure. [Google Scholar]
- 28.Ho A.F., Chew D., Wong T.H., et al. Prehospital trauma care in Singapore. Prehosp Emerg Care. 2015;19(3):409–415. doi: 10.3109/10903127.2014.980477. [DOI] [PubMed] [Google Scholar]
- 29.Ho A.F.W., De Souza N.N.A., Blewer A.L., et al. Implementation of a national 5-year plan for prehospital emergency care in Singapore and impact on out-of-hospital cardiac arrest outcomes from 2011 to 2016. J Am Heart Assoc. 2020;9(21) doi: 10.1161/JAHA.119.015368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.icdcoder [computer program] 2015. [Google Scholar]
- 31.Chien C.Y., Tsai S.L., Tsai L.H., et al. Impact of transport time and cardiac arrest centers on the neurological outcome after out-of-hospital cardiac arrest: a retrospective cohort study. J Am Heart Assoc. 2020;9(11):e015544. doi: 10.1161/JAHA.119.015544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singapore DoS . Complete life tables for Singapore resident population. 2019-2020. 2021. [Google Scholar]
- 33.Epidemiology & Disease Control Division, Ministry of health, Singapore; Institute for Health Metrics and Evaluation . IHME; Seattle, WA: 2019. The burden of disease in Singapore, 1990–2017: An overview of the global burden of disease study 2017 results. [Google Scholar]
- 34.Pemberton K., Franklin R.C., Bosley E., Watt K. Long-term outcomes of adult out-of-hospital cardiac arrest in Queensland, Australia (2002-2014): incidence and temporal trends. Heart. 2021;107(16):1310–1319. doi: 10.1136/heartjnl-2020-317333. [DOI] [PubMed] [Google Scholar]
- 35.Wong X.Y., Fan Q., Shahidah N., et al. Impact of dispatcher-assisted cardiopulmonary resuscitation and myResponder mobile app on bystander resuscitation. Ann Acad Med Singap. 2021;50(3):212–221. [PubMed] [Google Scholar]
- 36.Lim S.L., Lau Y.H., Chan M.Y., et al. Early coronary angiography is associated with improved 30-day outcomes among patients with out-of-hospital cardiac arrest. J Clin Med. 2021;10(21):5191. doi: 10.3390/jcm10215191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pothiawala S. Post-resuscitation care. Singapore Med J. 2017;58(7):404–407. doi: 10.11622/smedj.2017060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chia Y.W., Lim S.L., Loh J.K., Leong B.S., Ong M.E.H. Beyond return of spontaneous circulation: update on post-cardiac arrest management in the intensive care unit. Singapore Med J. 2021;62(8):444–451. doi: 10.11622/smedj.2021115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Larribau R., Deham H., Niquille M., Sarasin F.P. Improvement of out-of-hospital cardiac arrest survival rate after implementation of the 2010 resuscitation guidelines. PLoS One. 2018;13(9):e0204169. doi: 10.1371/journal.pone.0204169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maynard C., Longstreth W.T., Nichol G., et al. Effect of prehospital induction of mild hypothermia on 3-month neurological status and 1-year survival among adults with cardiac arrest: long-term follow-up of a randomized, clinical trial. J Am Heart Assoc. 2015;4(3):e001693. doi: 10.1161/JAHA.114.001693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baldi E., Compagnoni S., Buratti S., et al. Long-term outcome after out-of-hospital cardiac arrest: an utstein-based analysis. Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.764043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho Y., Oh J., Shin J.H., et al. Long-term prognosis and causes of death among survivors after out-of-hospital cardiac arrest: a population-based longitudinal study. Resuscitation. 2022;173:31–38. doi: 10.1016/j.resuscitation.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 43.Rea T.D., Crouthamel M., Eisenberg M.S., Becker L.J., Lima A.R. Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation. 2003;108(10):1196–1201. doi: 10.1161/01.CIR.0000087403.24467.A4. [DOI] [PubMed] [Google Scholar]
- 44.Hiemstra B., Bergman R., Absalom A.R., et al. Long-term outcome of elderly out-of-hospital cardiac arrest survivors as compared with their younger counterparts and the general population. Ther Adv Cardiovasc Dis. 2018;12(12):341–349. doi: 10.1177/1753944718792420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bunch T.J., White R.D., Gersh B.J., et al. Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrillation. N Engl J Med. 2003;348(26):2626–2633. doi: 10.1056/NEJMoa023053. [DOI] [PubMed] [Google Scholar]
- 46.Tan C.C., Lam C.S.P., Matchar D.B., Zee Y.K., Wong J.E.L. Singapore's health-care system: key features, challenges, and shifts. Lancet. 2021;398(10305):1091–1104. doi: 10.1016/S0140-6736(21)00252-X. [DOI] [PubMed] [Google Scholar]
- 47.Hsu C.H., Li J., Cinousis M.J., et al. Cerebral performance category at hospital discharge predicts long-term survival of cardiac arrest survivors receiving targeted temperature management. Crit Care Med. 2014;42(12):2575–2581. doi: 10.1097/CCM.0000000000000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lindner T., Vossius C., Mathiesen W.T., Søreide E. Life years saved, standardised mortality rates and causes of death after hospital discharge in out-of-hospital cardiac arrest survivors. Resuscitation. 2014;85(5):671–675. doi: 10.1016/j.resuscitation.2014.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.